
8 minute read
The Bare Bones — Ultrasound Assisted Fracture Reduction
Joseph Zarraga, DO; Carissa Jeannette, DO; Max Cooper, MD RDMS

Figure 1: Radiographs of the distal humerus fracture, described as oblique, angulated, comminuted fracture of the distal diaphysis of the humerus. Shown as pre-and and post reduction. (a) Pre-reduction x-ray shows significant displacement, read by radiology as “a varus angulation” of the distal fragment by 43 degrees. A distance of the overriding part of the distal fragment was found to be 1.02 cm. (b) Post reduction x-ray showing significant reduction of displacement. Read by radiology as “significantly improved alignment following reduction with no significant residual angulation.”

Abstract
Extremity fractures are common injures that are evaluated and treated daily in the ED.1 The vast majority of fractures require conservative management in the ED and orthopedic surgery follow up as an outpatient for definitive treatment and management. However, in cases where there is significant displacement, angulation, and or neurovascular compromise, reduction of these fractures in the ED should be promptly pursued. Point of care ultrasound (POCUS) is a readily available tool in EDs worldwide that can be useful during fracture reductions to ensure adequate reduction and overall procedural success. In this case report, we review basic steps for management of displaced fractures and how POCUS can assist in successful reduction.
Intro
We present a case of a distal humerus fracture with moderate displacement, angulation, and comminution. The ED course of these cases is usually straightforward, with pain control, reduction with or without sedation, and post reduction splinting being the mainstays of management. However, difficult cases tend to require multiple reduction attempts and X-rays to guide effort. These procedures can be labor-intensive, siphoning providers and resources away from the rest of the department. We demonstrate the utility of POCUS as an adjunct that can give near realtime feedback during fracture reductions, which can not only potentially lower the number of attempts, radiation exposure, and resource utilization but also allow for better overall outcomes.
Case
A 23-year-old female with no known past medical history, presented to the ED from home for a right arm injury. Just prior to arrival, the patient states that she was wrestling with her siblings, when one of them accidentally fell on her upper arm. She states that she immediately had pain in her upper arm and near her elbow, prompting her to immediately call 911.
The Emergency Medical Service (EMS) providers called our medical command physician for clearance to administer fentanyl for analgesia, as she was in severe pain. EMS also stated that she had an obvious deformity of the distal humerus, just proximal to the elbow. Initial evaluation by medics reported no immediate neurovascular compromise, with intact sensation, motor, and pulses distal to the injury.
Upon arrival to the ED, she had improvement in her pain status. EMS had placed her arm in a position of comfort and applied a temporary splint to the affected area. She was placed on the monitor and had normal vital signs. Removal of the temporary splint revealed a right arm deformity of the posterolateral aspect of the humerus, just proximal to the elbow. There was no tenting of skin, open wounds, or ecchymosis, and distal sensation, motor function, and pulses were intact. Physical exam did not reveal additional signs of trauma.
X-rays were performed of the right shoulder, humerus, and elbow and demonstrated an oblique, angulated, comminuted fracture of the distal diaphysis of the humerus. The radiologist measured a varus angulation of the distal fracture fragment of 43 degrees and a distance of the overriding part of the distal fragment of 1.02 cm.
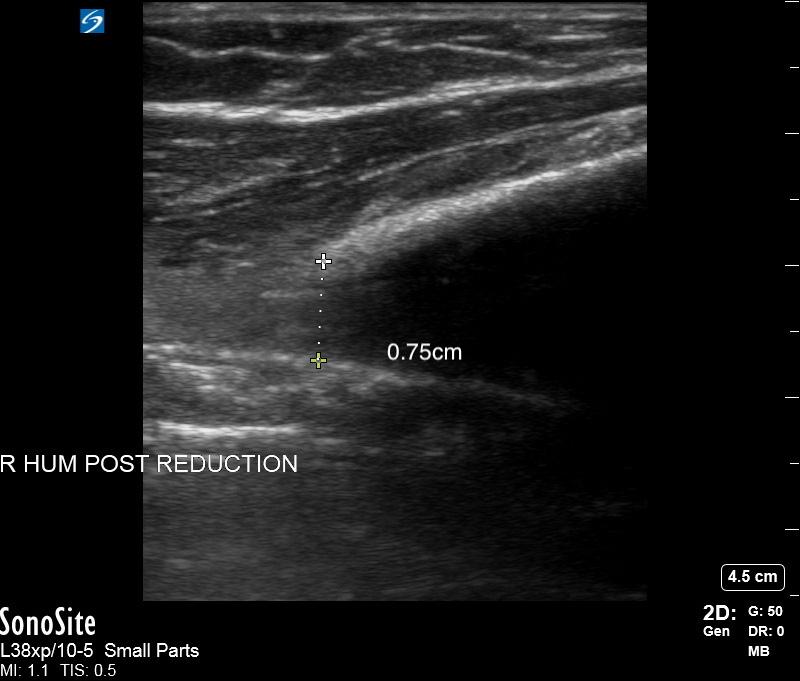
She was consented for procedural sedation using propofol and ketamine. Given the amount of displacement, we brought the ultrasound to the bedside to obtain real time feedback of our reduction efforts. When the patient was adequately sedated, the dressing was removed and the displacement of the fractured humerus was measured to be 0.82 cm using a linear ultrasound probe in a longitudinal view. After one attempt at reduction, we remeasured the displacement at 0.75 cm, though the
>>
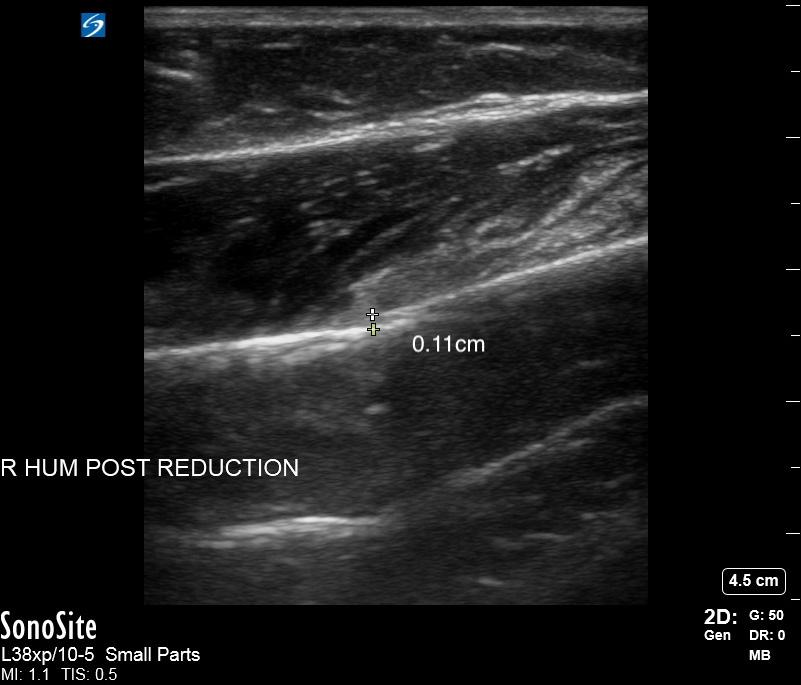
external angulation seemed to improve. After our second attempt, the segment was measured at 0.11 cm. She was splinted and a repeat portable X-ray showed “significantly improved of alignment following reduction with no significant residual angulation.”
Discussion
Extremity fractures are commonly seen in the ED and diagnosis is often accomplished by X-ray. Fractures requiring sedation and reduction are often very apparent to ED physicians on presentation. This case is an example of such a fracture. Upon initial X-ray, the degree of angulation and displacement was noted to be significant and we believed that multiple attempts at reduction would be required for satisfactory alignment.
These cases are optimal for utilization of POCUS as an adjunct for successful reduction. To do this, pre-reduction ultrasound of the affected extremity is performed at the bedside, looking for disruption of cortical alignment. The disruption is measured with calipers and saved in order to compare with after reduction results ─ reduction is considered successful when there is satisfactory reduction in displacement and angulation as noted on POCUS.
Few studies regarding outcomes of US assisted fracture reductions have been performed. Sensitivity and specificity of determining successful reduction under US guidance has been found to be 97.5% and 95%, respectively.2 Successful reduction of fractures may not be affected by using POCUS in combination with traditional X-ray. However, there are additional benefits that ease the process.
By using the US at bedside, it is much easier to monitor reduction progress with the ultrasound after each attempt. Traditionally, when adequate reduction is believed to be achieved by the performing physician, the extremity is splinted and confirmatory X-ray is performed. In difficult reductions, X-rays may indeed show inadequate approximation, requiring removal of the splint and further attempts. In addition, it can lead to increased resource utilization and decreased procedural efficiency, which could affect department flow and wait times.3 Radiation exposure as well as sedation time and medication usage could rise with repeated reduction attempts. In this case of a 23-year-old female with a distal humerus fracture that required sedation and reduction, we were able to avoid additional intra-reduction X-rays, further medication, and achieve a relatively quick reduction.
Figure 2: US of the distal humerus fracture pre-reduction, measured to be displaced at 0.83 cm.

Figure 3: US of distal humerus after first attempt at reduction under conscious sedation, measured to have displacement at 0.75 cm, with a 0.08 cm difference. After first reduction, a satisfactory “clunk” was felt, but bedside US showed that there was room for further improvement. Figure 4: US of distal humerus after second attempt at reduction under continued conscious sedation, with successful approximation. Distance measured to be 0.11 cm, significantly improved from the first displacement measurement of 0.83 cm.
Questions and Takeaways
What makes this presentation and management reportable?
This case shows the ability of POCUS to assist in guiding fracture reductions.
What is the major learning point?
This report highlights the potential for utilizing POCUS during difficult fracture reductions in order to potentially reduce time to reduction, overall radiation, medications used, and number of reduction attempts.
How might this improve emergency medicine practice?
This case hopes to demonstrate to ED physicians of an underutilized tool that has multiple benefits in a common EM procedure.
Conclusion
Displaced extremity fractures are a common presentation in the ED that can be time and resource intensive. This case report highlights using POCUS not as a replacement, but rather a supplement to traditional X-ray to assist in reduction that can increase efficiency and efficacy. POCUS is an effective tool and aid in displaced extremity fractures.
References
1. 1. Kozaci N, Ay MO, Akcimen M, et al. Evaluation of the effectiveness of bedside point-of-care ultrasound in the diagnosis and management of distal radius fractures. The American Journal of Emergency Medicine. 2015;33(1):67-71. 2. Bozkurt O, Ersel M, Akarca FK, Yalcinli S, Midik S, Kucuk L. The diagnostic accuracy of ultrasonography in determining the reduction success of distal radius fractures. Turkish Journal of Emergency
Medicine. 2018;18(3):111-118. 3. Socransky S, Skinner A, Bromley M, et al. (July 07, 2016) Ultrasound-
Assisted Distal Radius Fracture Reduction. Cureus 8(7): e674. 4. 4. Ultrasound G.E.L. - POCUS in the Reduction of Distal Radius
Fractures. emDOCs.net - Emergency Medicine Education. http://www. emdocs.net/ultrasound-g-e-l-pocus-in-the-reduction-of-distal-radiusfractures. Published February 7, 2020.
why aaem?
AAEM is the leader within our field in preserving the integrity of the physician-patient relationship by fighting for a future in which all patients have access to board certified emergency physicians and physician rights are protected.

It ’ s a challengIng tIme for emergency physIcIans - aaem recognIzes that and were doIng somethIng about It.
we ’ ve contInued to fIght for your due process rIghts — aaem worked closely wIth the sponsors of newly Introduced legIslatIon. we ’ ve had your back durIng covId-19 — read our posItIon statements and letters to government offIcIals advocatIng for you durIng thIs pandemIc. we protect your practIce rIghts — we ’ re actIvely workIng to address app Independent practIce to create a balanced workforce through both posItIon and polIcy statements. we ’ re advocatIng for a solId future for our specIalty - we ’ re workIng wIth the newly formed em workforce commIttee for a future wIth a balanced work force. we ’ re commItted to dIversIty, equIty, and InclusIon – the aaem dIversIty, equIty, and InclusIon commIttee Is workIng hard to brIng members resources and awareness, IncludIng statement on the death of george floyd and the statement agaInst federal regulatIon. we joIned the clear message beIng sent that #thIsIsourlane. we are the front lIne provIders, and we wIll be at the forefront of the solutIon, whIch Is why we sIgned on to support affIrm.










