
















Dr Gwen Chin ADAWA President
As we head towards the end of the year, I am pleased to provide an update on one of our recent activities and share details about an exciting upcoming event.
First, I want to extend my congratulations to the Oral Health Education Committee for their outstanding work in bringing Dental Health Week to the WA public. This year, we hosted a stand in Forrest Chase on Saturday, 10 August, which was met with great enthusiasm from the public. It was a resounding success, attracting a significant number of visitors eager to learn more about oral health. Our dental volunteers engaged with the community through interactive demonstrations, educational materials, and one-on-one discussions. The aim was to raise awareness about the importance of oral hygiene, regular dental checkups, and the impact of diet on dental health. An ADA survey found that parents did not realise that their children should be seeing their dentist as soon as possible and this was one of the messages that was passed on by the volunteers. Feedback from
CEO Trevor Lovelle
President Dr Gwen Chin
Editorial Brooke Evans-Butler
attendees was overwhelmingly positive, and many expressed their appreciation for the practical advice and resources provided. These types of events not only strengthen our relationship with the community but also reinforces our commitment to promoting oral health education.
Looking ahead, I am excited to announce the upcoming Young Dentists' Conference, scheduled for Saturday, 30 November 2024. This event is specifically designed for our recent graduates, offering them a unique opportunity to network, learn, and grow within our profession. Topics will cover the latest advancements in dental technology, clinical management of situations and improving clinical expertise. There will also be ample time for networking, allowing our young professionals to connect with peers and mentors. This conference is an invaluable resource for those beginning their careers, providing them with the tools and knowledge needed to thrive in the dental field. If you are a member who has graduated in the last five years, I encourage you to attend and take full advantage of this opportunity.
Designer Michelle Walker Advertising Business Development Manager Shaden Kanaan
The Recent Graduates and Student Liaison Committee is excited to announce the Young Dentists’ Conference is back in 2024 – to be held on Saturday 30th November at ADA House.
This highly anticipated event, sponsored by DPL, will feature esteemed interstate and local speakers including Dr Colm Harney, Dr Nishant Vaishnav, Dr Glen Liddelow and Dr Martin Webb, who will share their insights on key issues relevant to young dentists. Physiotherapist, Rob Nicholls, who will share insights into Physiotherapy for TMD.
Book your seat at adawa.com.au
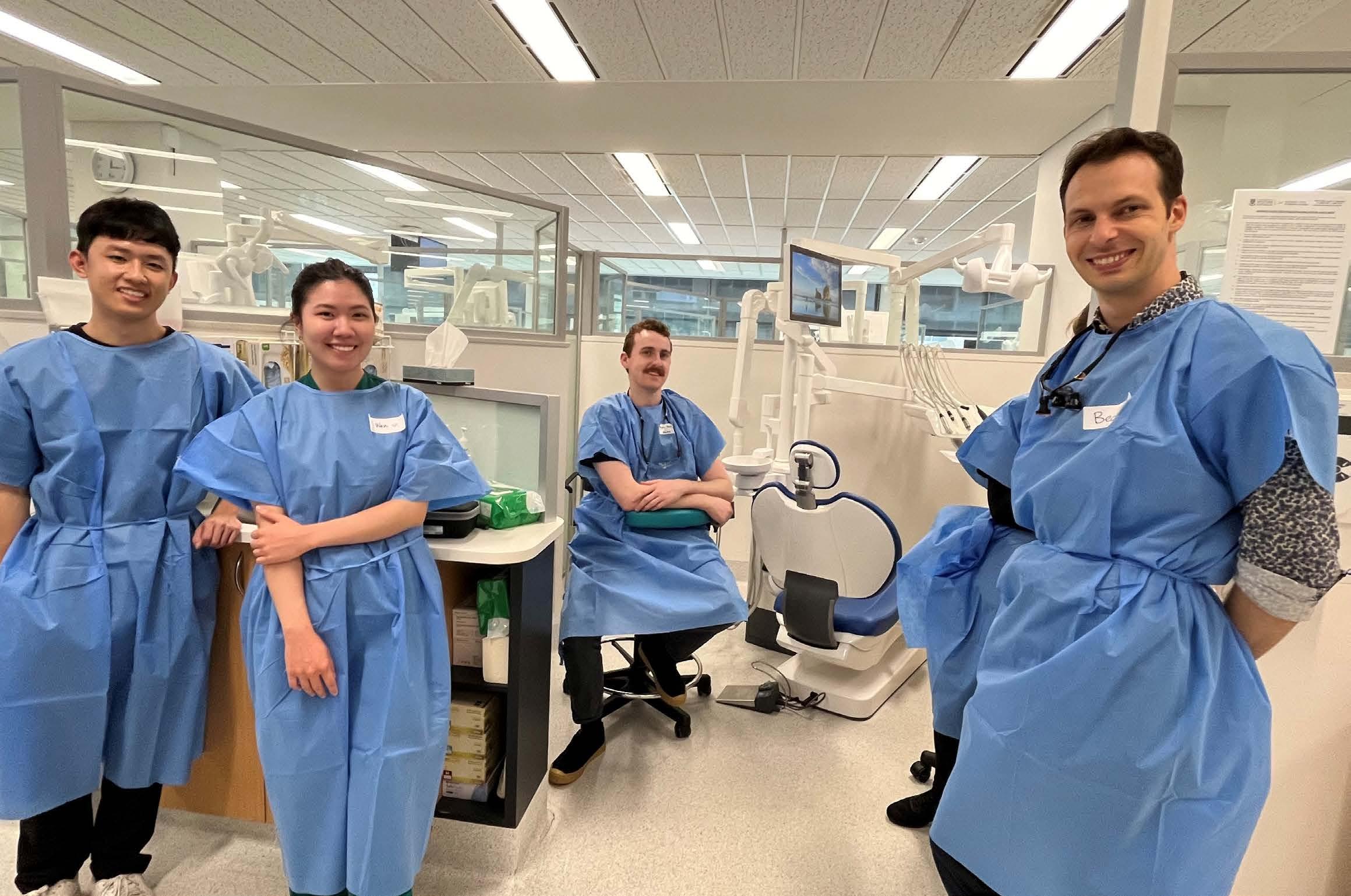
The giving nature of dentists was once again apparent at the latest ADA DHF Rescue Day at OHCWA.
It was another wonderful turn-out for the ADA Dental Health Foundation Dental Rescue Day in August, which saw over 40 worthy patients treated pro bono.
Hosted by UWA Dental School and OHCWA, referred patients in urgent need of dental care were seen by volunteer dentists, and OHT’s, with the support of dental assistants, UWA Dental Students and North Metropolitan TAFE DCA students.
A special thanks goes to Dr Robert Anthonappa (Dean and Head of UWA Dental School) and Dr Michelle Huang (Clinical Operations Manager of the Oral Health Centre of WA) for allowing the use
of the student clinic, as well as Daniel Hopkins and the helpful OHCWA staff. Thanks also goes to Dr Tracey Gold, Dr Lida Sayadelmi and Andrea Paterson, whose organisation of these wonderful events behind-the-scenes is always above-and-beyond.
Thank you also to Colgate and Piksters, whose generous donations meant the patients were able to take home a selection of oral health products.
Interested in giving back? Contact Andrea Paterson, ADA DHF State Coordinator WA, wa@adadhf.org.au to enquire about volunteerism opportunities.
Thank you to the volunteers:
Dr Tracey Gold
Dr Lida Sayadelmi
Dr Russell Gordon
Dr Chandrama Banerjee
Dr Wendy Patak
Dr Hayden Jones
Dr Brigitte O’Brien
Dr Mary Todd
Dr Sally McMullen
Dr Benny Sheriff
Dr Grace Cooper
Dr Maheransh Chopra
Dr Richard Kozlowski
Dr Paola Miki Haga
Dr Gabby Thompson
Dr Stephen Chan
Dr Rebecca Vo
Dr Vicky Ross
Dr Wan Zhi Tay
Dr Bede van Schakjik
Dr Mohanad Abbas
OHTs
Ryan Stallard
Jade Martens
Fiona Ligertwood
Volunteer dental staff
Jan Matthews
Jo Robertson
Nonna Degtyar
Abbie Kozlowska
Claudia Banciu
Ash Basita
Rujoola Wagh
Ashton Foo
Jordan Stanley

Ranudi De Silva
Rohan Manaloor
Jim Rae
Henry Miao
Wen Phua
Esther Eichner
Samantha Toh
Maaz Naveed
Jaskaran Dhillon
Kaylee Wong
Yu Wen Phua
Jieun Kim
Linda Eagle
North Metropolitan TAFE DA Students
Alexandra James-Davy (Lecturer)
Mikayla, Shaina and Ami (students)


13 May 1926 – 2 September 2024

Dr Ron Townsend passed away on September 2, 2024 at 98-years-old.
In the dental profession, Ron was known as ‘The Legend’ due to his lifelong professionalism and his commitment to ethical practice, his wise counsel, and his mentoring of fellow dentists, in respect for the responsible positions he had held and his belief in fairness for all.
Life did not start fairly for young Ron.
When Ron’s father Frank died in 1941, Ron was forced to leave school early and did not complete his Junior Certificate of Education as he needed to work to help his family’s difficult circumstance.
Like so many intelligent, but underprivileged youngsters of the time, Ron attended night school to pass the equivalent of today’s Year 10 exams and continued studying at night to gain a qualification in Accountancy.
During World War II, Ron joined the Royal Australian Airforce the moment he turned 18 – and began training to become a pilot. He did not complete his pilot training due to the end of the war and declaration of peace. On discharge from the RAAF in 1945, he was given the opportunity to undertake any course of study that he wished. He chose dentistry.
In an interview four years ago with respected dental historian and mutual
friend, Dr Lynnette Loreck, she described Dr Townsend as: “A pragmatist, a dreamer and ethical to a fault”. She went on to say in her excellent article: “Dr Ron Townsend will always fight for what he believes is fair and right.”
On the subject of the reputation of the Dental Profession, Ron stated: “I worked so damned hard to get to be a dentist, I won’t let its reputation be messed up!”
Ron was a great clinical dentist for just over 40 years. He held many leadership and committee roles over his career, but Ron described his two most satisfying periods were after his retirement from private practice in 1992.
The first was the period between 1995 to 2003, when he was a Consultant for the Australian Dental Association’s Dental Cases Committee (DCC); and the second period between 2005-2010, was when Ron accepted the invitation from myself as President of the Dental Board of Western Australia, to assist managing a backlog of complex, unresolved dento-legal complaints. Both these important roles required intelligence, due diligence, integrity and patience, plus Ron’s enormous amount of common-sense.
In his earlier role, in 1995, the Australian Dental Association with the support of Sir

Paul Bramley and Dr David Phillips OBE of the Medical Protection Society and its subsidiary, Dental Protection Limited, London, appointed Ron a DPL Liaison Officer.
With his gift of language and his considerable experience in problem resolution, Ron would mediate between patients and dentists, communicating with both equally, to endeavour to prevent complaints reaching a conflict and/or legal stage.
In his capacity as a consultant in this field, Ron won intra- and inter-professional respect, and, in so doing, he reflected a light on our profession—that dentistry is a profession to be admired.
In 1994, it was my honour as President of the Australian Dental Association (WA branch), to present Ron with his Honorary Life Membership of our Association for his valuable contribution to the Association and to ethical practice. He proudly displayed this honour on his bookshelf for all to see in his retirement unit in Booragoon.
When illness forced Ron to retire from this role in 2003, the then Director of Dental Protection Limited, Dr Kevin Lewis, flew from London to attend Ron’s retirement party. Dr Lewis wrote the following in the editorial of their International Journal,
Riskwise: “Ron’s superb case handling skills and massive experience made him a highly respected member of this small group of specialists in the dento-legal field internationally. Ron has been up there amongst the very best of them, and his skill and experience is not easy to replace.”
Finally, in 2010 when all State Health Boards entered the National Registration Scheme, only then did Ron and Freda truly retire to their beautiful rural property in Brigadoon.
A highlight of Ron’s professional career was when he was the guest of Lord Colwyn and Dr David Phillips OBE at a ‘Members Only’ dining hall in the House of Lords, London. They had flown Ron to London on the pretext of a DPL meeting, but this really was just a beautiful way of saying thank you.
He often wondered and asked me: “How did a kid who left school at 14, end up in a place like that?”.
I happily answered: “Ron, it’s because you are a Legend”.
Farewell great friend and colleague, you will be missed by many.
Written by Dr John R. Owen AM
Photo by Dr Lynnette Loreck

Dr John Owen AM had many causes for celebration recently, with his 70th birthday, 40 years of Midland Orthodontists and 16 years of the Kimberley Dental Team.
240 guests attended an ‘Extravaganza’ event in August for a triple celebration –Dr John Owen AM’s 70th birthday, 40 years of Midland Orthodontists and 16 years of the Kimberley Dental Team.
“2024 is a big year because we could jointly celebrate my 70th birthday, the practice's birthday and also completing 16 years of Jan and my Foundation, the Kimberley Dental Team,” John says.
“Over the years, it’s been great to work with 10 associates, two locums, and with my son David since 2000 and with so many incredible team members.
I sincerely thank everyone.
“I have never thought the practice was about me; the practice has its own identity because of the atmosphere and reputation all of us have created and maintained over the years,” he adds. “We are all proud that we are an important part of the community, having assisted generations of families over the past four decades.
“To our general dental and specialists who not only support Midland Orthodontists, but
also support us with volunteering their time and skills, often with their team members or with donations towards the Kimberley Dental Team, a huge thank you – you are family.”
The evening also celebrated 16 years of the Kimberley Dental Team, which John says he and Jan have had the pleasure of putting together an incredible 88 volunteer ‘A’ teams for the volunteer trips.
“Through KDT, we have met and helped so many incredible kids, many who are now young adults, plus so many great families in communities, ranging from Broome to Kundat Dura in the East on the Northern Territory border and from Kalumburu in the north to Balgo and Mulan in the Kutjungka region, just above the Great Sandy Desert in the South.
“The team and our community engagement is again based on the great values of respect, trust and importantly, reliability.
Congratulations once again to John, Jan and members of Midland Orthodontists and the Kimberley Dental Team on these significant anniversaries.




At Smith Coffey, we’ve spent over 50 years providing specialised financial services to dentists, helping them achieve their financial goals while they focus on delivering quality patient care. We understand the unique challenges you face, whether it’s managing cash flow, navigating tax complexities, or planning for the future, and we’re here to ensure your finances are working as hard as you do.
Our expertise spans a range of services, from taxation and superannuation strategies to securing mortgages and finance for property purchases. We also offer tailored personal risk insurance solutions, including income protection, to safeguard your financial wellbeing in the event of illness or injury. Whether you're investing in your dream home, expanding your practice, or ensuring your income is protected, our team can help you make informed financial decisions that suit your unique circumstances.
Dentists trust Smith Coffey because we know your industry inside and out. We tailor our services to your specific needs, helping you build a robust financial foundation for both your personal and professional life.
Let Smith Coffey be your trusted partner in achieving financial freedom. Contact us today to find out how we can help you secure your financial future.


At AMA Financial Services, we are dedicated to helping dentists across Australia make informed financial decisions, simplify complex processes, and achieve their financial goals. Whether you’re looking to secure your financial future, find the right finance, or protect your dental practice, our team of experts is here to assist you every step of the way.
Taking control of your financial future is crucial, but knowing where to begin can be overwhelming. Our financial planners provide personalised advice tailored to your unique goals, whether you’re managing cashflow, building wealth, planning for retirement, or protecting your finances. We help you navigate the complexities of money management, offering peace of mind and setting you on the path to financial freedom.
• Free financial health checks with a licensed Financial Adviser.
• Discounts on the development of a comprehensive financial plan.
• Access to member only financial seminars & webinars.
• Discounted ongoing wealth management (service) packages.
AMA Services (WA) Pty Ltd. ABN 47 008 671 458 t/as AMA Financial Planning is an Authorised Representative of Consultum Financial Advisers Pty Ltd. ABN 65 006 373 995 l AFSL 230323 an Australian Financial Services Licensee.
Navigating the home loan market can be challenging, with numerous products and fluctuating interest rates. Our mortgage brokers simplify the process, doing the legwork to find the best loan for your needs. Whether you’re a first-time homebuyer, refinancing, or looking for a competitive investment loan, our brokers work for you—not the bank—to secure the best possible deal, saving you time and money.
AMA Finance Brokers special offer for ADAWA members
For a limited time only! ADA members are eligible to receive up to $4K refinance cashback on home loans successfully settled between 1 June 2024 and 31 October 2024.
• Net loan value up to $750,000 - $1,000,000 receive up to $1,000 cashback.
• Net loan value up to $1,000,001 - $1,500,000 receive up to $2,000 cash back.
• Net loan value above $1,500,000 receive $4,000 cashback.
*Terms and conditions apply.
Running a dental practice involves significant risks, and choosing the right insurance cover is vital. Our insurance brokers develop strategies to protect your practice, manage your policies throughout the year, and guide you through the claims process. With us, you receive ongoing support and personalised advice, ensuring your practice is protected against the unexpected.
• Access to member only insurance seminars & webinars
AMACIS Pty Ltd trading as AMA Insurance Brokers ABN 40 064 488 106 AFS License No. 235312
Tailored specifically for dental professionals, AMA Financial Services’ Tax and Accounting team provides expert advice delivered by certified accountants and tax advisors. Whether you own a private dental practice or are employed on a contractual basis, we ensure your tax obligations are professionally managed, allowing you to focus on patient care.
As a dentist, your primary focus is on providing excellent clinical care, but managing a practice also requires effective business strategies. AMA Consulting helps optimise the success of your practice with strategic business planning, HR consulting, recruitment support, and business optimisation advice. We help streamline your operations, allowing you to focus on what matters most—your patients.
Disclaimer: The information above is general in nature and may not be relevant to your individual circumstances. You should refrain from acting in reliance on this information without first obtaining suitable professional advice. You should obtain and consider the relevant Product Disclosure Statement (PDS) before making any decision to acquire a product.
Phone: 1800 262 346
Email: info@amafinancialservices.com.au
Web: www.amafinancialservices.com.au
On meeting with dentists, Sally and Justina, it quickly becomes apparent they are both passionate about smile design.
Sally recently completed her Masters in Aesthetic Dentistry at King's College in London, where she did her thesis on Smile Design and Ageing, while Justina went to Romania in 2022 to learn about Smilecloud from the founder, Florin Cofar. They are both looking forward to sharing this passion with attendees at a dinner course at the University Club on November 14.
“Smile design is a systematic way of looking at the elements that make up a beautiful smile,” Sally explains. “You systematically analyse the patient you have, and you keep the attributes that are positive, and see if you can enhance those that aren’t positive.
“You come up with a treatment plan to create a bespoke smile for that patient on your computer,” she says. “Our lecture will be teaching that smile design part of a patient’s treatment plan, which the attendees will then be able to apply to their patients. I think it is translatable to the people attending for those wanting to lift their basic dentistry to become more organised, more structured and of a higher quality.
“I like to see us as smile architects,” Justina adds. “It is similar to building a house or doing a renovation. It always comes down to the planning. We know we want to have a great outcome, but the patient doesn’t know what that looks like either. This planning is trying to know exactly what the end-result is going to look like.”

The lecture will be an in-depth exploration of digital smile design – covering the upto-date literature behind the cornerstone principles of smile design. This will be followed by a step-by-step demonstration of how to apply these concepts using just PowerPoint or Keynote.
At the cutting edge of digital smile design is cloud based software. The second part of this lecture will explore this exciting technology and demonstrate the workflow that allows for a truly natural and harmonious smile customised to each individual.
When asked who should attend the course, Justina says dentists who are interested in doing more cosmetic work should attend.
"Being able to execute things in a more planned and practicable way and better communicate with the technicians ensures higher quality results," she explains.
The Smile Design Dinner is the first time Sally and Justina have presented together, and they are looking forward to sharing their passion about the topic.
“I remember when I came out of Dental School, I hoped there were more courses happening about this at that time,” Justina says. “Now, given the opportunity and my experience, I hope I can share with other dentists passionate about
5 minutes with Drs Sally McMullen and Justina Teo
What three words best describe you?
Justina: I have done an enneagram, so my top three enneagrams were challenger, achiever and leadership.
Sally: Creative, lover of learning and an empath.
If you weren’t in dentistry, what would you be doing for a living?
Justina: It was probably going to be something with journalism or media because you are on your feet, you are taking to people all the time and you are using your creative skills as well.
Sally: It was do anything I could to get into dentistry, but otherwise I had an interest in architecture.
What do you enjoy doing in your spare time?
Justina: I’m usually with my two little kids, but I also try to stay active. I love
upskilling and levelling up their smile makeover game. It will hopefully be useful and inspirational.”
“We want attendees to know we are approachable,” Sally adds. “We are all learning and happy to share our knowledge. The whole game is changing.”
Drs Justina Teo and Sally McMullen will be presenting Digital Smile Design Dinner on November 14 at University Club. To book go to our website, adawa.com.au/product/digitalsmile-design-dinner
doing yoga and going for big walks in nature, usually with an audiobook playing in the background. Staying fit helps me keep up with my kids and do my job well! Before the kids, I used to love baking, but now I don’t have as much time for it. My husband and I have a little side project we started this year—the Australian Digital Dentistry Academy, where we run courses and study clubs focused on digital dentistry, which has been keeping us busy. Oh, and I’m also trying to finish off some home renovations!
Sally: I am a mum to three kids. I try to do a bit of exercise for mental and physical health. I play netball. I love socialising with all the ladies from netball, and I do a bit of Pilates.
Wishing you and your loved ones a joyful holiday season and all the best for 2025!
We would like to extend our heartfelt thanks to all our referrers for your trust and collaboration this year.
As the only radiology practice in Western Australia with onsite oral and maxillofacial radiologists, we are proud to continue providing a radiology service well beyond quality scans and reports.
Our team of five oral and maxillofacial radiology specialists is always available to discuss your clinical cases and provide advice, whether over the phone or in person.
Thank you for choosing us as your imaging partner. We look forward to working with you in 2025!
Warm wishes from Bernard Koong, Tom Huang, Dayea Oh, May Lam, John Biun, and the team at Envision Medical Imaging!
Contact Us
p: 08 6382 3888
e: info@envisionmi.com.au
Wembley 178-190 Cambridge St Wembley WA 6014
Our Imaging Services
• X-ray
• Ultrasound
• CT
• MRI
• OPG, Lateral & PA Ceph
• Cone beam CT
• Nuclear medicine
• PET-CT
Booragoon OPG/Ceph & CBCT only
Suite 3B/175 Davy St, Booragoon WA 6154

In this day and age, everything is about how we communicate. Digital smile design allows you to keep the design in your hands and communicate better with your laboratory. Understanding and staying up-to-date with the possibilities of modern CAD technologies ensures you are equipped to deliver the best available patient care.
This evening lecture will be an in-depth exploration of digital smile design. This will be followed by a step-bystep demonstration of how to apply these concepts using PowerPoint or Keynote.
At the cutting edge of digital smile design is cloud-based software. The second part of this lecture will explore this exciting technology.
Dr Sally McMullen is an experienced general dentist who has built her practice on a biologically-respectful and aesthetic mindset. Since graduating over 14 years ago, Sally has worked at top practices in Claremont and South Perth. She has recently completed a Master’s of Aesthetic Dentistry from the esteemed King’s College in London where she has enjoyed the collegiality and perspectives of other high calibre general and aesthetic dentists from around the world. When not pursuing her passion for dentistry, Sally is mother to three young children.
Dr Justina Teo graduated with honours from the University of Western Australia. She went on to complete a Masters clinician implant program with Loma Linda University, and gained her fellowship with the Royal Australiasian College of Dental Surgeons. Her daily work is focused on cosmetic dentistry and full arch implant rehabilitations. She returns from Romania, having learnt all about Smilecloud from the creator himself, Florin Cofar.

3.0 CPD Saturday NOV 23 9.00am-12.30pm ADA HOUSE $363 members
COURSE OUTLINE
Difficulties encountered during endodontic treatment can be a cause of frustration for both clinician and patient. Complications may impact the outcome of the endodontic treatment. Clinicians should understand how each of these complications can occur, be prevented and predictably rectified. It is also important for clinicians to understand the impact of a specific complication on the treatment prognosis and to appreciate how this may differ in each case.
TOPICS COVERED
• Incomplete analgesia
• Perforation – pulp chamber - root
• Instrumentation separation
• Unexpected anatomy
• Ledging
• Calcification in the root canal system
• Hypoclorite injuries
• Who to contact when things go wrong
• Obturation errors
THE PRESENTERS
Dr Stephen Kwang
Dr Jane McCarthy
Dr Colm Harney
Dr Gaurav Vasudeva
Dr Shahrzad Nazari
The annual WADA Golf Spring Cup was held in September at the Vines Resort, Ellenbrook. The Lakes/Ellenbrook combined course was host to 14 keen golfers vying for the perpetual trophy and prizes donated by our major corporate sponsor Med and Dent WA. The weather provided us with an interesting day of rain and sun (Spring in the Valley really) for golf. An early lunch in the Greenside Café was followed by a challenging 18 holes on the combined course. The Lakes Course is a stern test with considerable water in play.
In a closely fought contest, Graeme Washbourne secured the win on 33 pts on countback from Michael Welten on 33 pts and third was Dean Martin, also on 33 pts.
Post-match presentations and hospitality were enjoyed by all. We were joined for the afternoon by representative of Med and Dent WA, Craig Botes, to award the Med and Dent WA trophy and celebrate with the various winners of the day. As always, our thanks are extended to our corporate partners for their support of WADA Golf.
Our final fixture for the year will be held at Royal Fremantle Golf Course on 22 November, with players competing for the Lester Charlesworth Trophy. This will be followed in the evening by the annual presentation dinner to mark the end of the golfing year and awarding of the Cec White Trophy for the champion dental golfer of the year.

4th hole Jun Liew Swan Valley Laboratory
5th hole

Michael Welten WADA Golf
6th hole Kang Kim Med and Dent WA
7th hole
Michael Welten Health Practice Brokers
8th hole Russell Gordon The Health Linc
3rd Hole (Longest drive)
Michael Whitford Insight Dental Ceramics
1st place on 33 pts – Graeme Washbourne
2nd place on 33 pts – Michael Welten
3rd place on 33 pts – Dean Martin
4th on 32 pts – Jun Liew
5th on 30 pts – Greg Yap
All interested golfers are welcome to join us for this event and are encouraged to contact me for further information.
Good golfing
Frank Welten
WADA Golf Captain Dentistgolf@gmail.com

By Dr Annalene Weston, Dentolegal Consultant, Dental Protection Limited
Truth in many ways could be considered to be a rigid and fixed concept, as surely, there is only one truth? This belief is predicated in the concept that truth is linked to fact. The issue however is that every individual’s perception of facts differs dependent upon many variables; what they have experienced, what they believe they have experienced and critically, what they WANT to believe they have experienced (sometimes well ‘after the fact’ and through the lens of strong emotions). Is truth then a rigid and immovable object, or elastic like a rubber band? And if it IS elastic how far can the band be stretched before it snaps, and do we as clinicians ever get stung by the recoil?
How many times have you had a reasonable conversation to find after the event that the other party heard something completely different to what you said? Irish playwright George Bernard Shaw once said, “The single biggest problem with communication is the illusion that it has taken place”.
Skilled communicator as you may be, many occasions can and will arise whereby the message you believe that you transmitted differs vastly from the message received. Many factors seep into this, some from you, some from your surroundings and some seated in the recipient. Truthfully, are you always giving your undivided attention? Even if you are not sat phone in hand, are you really listening, or is your mind wandering across your perpetual to-do list, your worries, your woes, or places that you would rather be? Loose language and hurried explanations have landed many a practitioner in hot water when they find the patient didn’t fully understand the meaning of a risk that eventuated, and that they therefore had no consent.
Is your recipient truly listening? Are they even able to if your environment is noisy and bustling with incessant distractions? Are you setting either of you up for success if your surroundings are frenetic?
Attention is a finite resource, and you also need to hold firmly in your mind that many patients do not bring the best version of themselves to the practice due to anxiety and fear, and when we are fearful, we are hardwired to shut off higher level thinking to allow our amygdala to drive the bus. The corollary of this is a decrease in our ability to learn new things, as we are primed instead to respond to danger. Add distraction and overly complex or inherently lazy explanations into the mix and we have a recipe for disaster.
Perspective is everything when it comes to forming a point of view, and in some instances, a patient can believe they have been harmed by treatment, despite all evidence to the contrary. This is termed a Perceived Injurious Experience (PIE). PIEs can quickly transform into an articulated grievance where the patient not only believes you have harmed them but will move to verbalise this in a ‘name and
shame’ manner – this has been aptly termed as ‘naming, blaming and shaming’. Oftentimes, these beliefs can springboard out of the Karpman Drama Triangle whereby the patient for whom you have tried your absolute hardest turns on you, and all your effort, kindness and attempts to go the extra mile count for nought and rebound to hit you squarely in the face. Remember, you will never win an argument with a patient. Ever. And, if a patient has formed a strong view that they have been wronged, they are unlikely to take your word for it that they were not, as their truth to them has become absolute. In these situations, the involvement of an independent third party such as the regulator is not to be feared, as these are often the only people who can influence the patients’ point of view.
Sometimes, it doesn’t serve us to face the truth, either because the truth hurts, or, because it doesn’t get us what we want. On these occasions, individuals may cling to their own version of events, knowing deep down inside the dishonesty of this, because it suits their agenda to do so. More often, people will lie to themselves or convince themselves of the facts, as admitting they are wrong, or bending to reach a compromise is for them, a push too far.
As a clinician, listening to a complaint which is a flagrant lie can be incredibly challenging, but remember it is often far more nuanced than that. So, what can we do to protect ourselves from others who approach the facts with a flexible view of the truth?
As proceduralists, we are highly skilled at documenting the procedures we perform. Equally, we are often more casual than we ought to be at documenting the discussions we have with the patient - if there is a difference in truth, it usually lies within what was said rather than what was done. The unpopular but rigid truth (especially in
legal claims) is that the only true way to evidence what was discussed is through your clinical records, so time needs to be taken to consider how these discussions can be captured well. If you are unsure, Dental Protection has resources that can help.
Listening isn’t the same as agreeing
There is often a window of opportunity where a patient can be bought back on side, but it does involve actively listening to what they have to say, even if you don’t agree. Never fear that letting someone air their grievance is in some way agreeing with their point of view. We all like our feelings to be validated, particularly when we are emotional, and it is not unreasonable to afford your patients this respect. Utilising active listening skills to help a patient feel that they are understood is the critical factor to successfully navigate through difficult conversations.
Don’t take it personally
People are entitled to their opinions, even if they don’t align with ours. While it can feel hurtful and downright offensive when someone doesn’t agree with our perspective, or actively opposes it, getting upset about it only causes you more grief and drama. It resolves nothing. Perhaps seek feedback from a trusted peer so that you can use the disagreement of truth as an opportunity for learning and growth.
Regretfully, occasions can and do occur where the person stretching the truth is in fact the clinician. This is very, very dangerous. As professionals, we are held to a higher standard than our patients, with inherent responsibilities such as a duty of candour, the obligation of open disclosure and the requirement to be deemed a ‘fit a proper person’ suitable to hold registration. Stretching the truth, whether that be in the information we give patients, the documentation we keep or the items we claim is not something we can do, as the consequences to our reputation and registration can be severe, even catastrophic in nature.
So, while the truth may indeed be an elastic construct, dependent upon on one’s perspective and beliefs, as professionals, the elasticity of truth is not something we can afford to put to the test.
References
1 https://law.hofstra.edu/currentstudents/academics/ academicresources/readingassignmentsandsyllabi/2015-16/ spring/upperdivision/lawyersandsocialchange/grossman/sa ratfelstinernamingblamingclaiming.pdf

Dentists are routinely faced with the dilemma of how to diagnose and manage a cracked tooth. This lecture provides a diagnostic protocol and evidence based management strategies to enable appropriate treatment.
All dentists dread it when they see a crack in a tooth. It can be a superficial crack in enamel or one of those cracks that when you start chasing is never ending. It’s a bit like taking wallpaper of a wall you never know where it is going. Where do you stop. This lecture will look at management of cracks from a practical restorative point of view.
Dr Graham Carmichael is a Board registered Prosthodontist and director of the Brånemark Center in West Perth. He obtained a BDSc from the University of Western Australia and has a Doctor of Clinical Dentistry in Prosthodontics from the University of Sydney. Dr Carmichael holds fellowships with the Royal Australasian College of Dental Surgeons, International College of Dentistry and the Australian and New Zealand Academy of Prosthodontics. He is a consultant prosthodontist at Perth Children’s Hospital and lectures nationally and internationally on all aspects of Prosthodontics.
Dr Shahrzad Nazari, Endodontist
This case is all about long-term outcome of the treatment even before it is an option being either considered or discussed with the patient. In many situations, there is a difference between what can be done and what we should do. To clarify, I am going to present a case, which is a good example of what needs to be done and why it is necessary to consider the long-term outcome of the treatment during case selection phase.
A lovely female patient in her fifties was referred to me for endodontic assessment and management of a broken instrument inside the MB root canal of a tooth 17. The patient had a history of mild to moderate pain, which was started almost 25 years ago. The patient’s first dentist who filled the tooth had warned the patient that the tooth might need root canal treatment or even extraction.
When I consulted with the patient, I already had her current dentist’s referral and her most recent radiographs. The dentist had started the 17’s root canal treatment, however, the patient had some ongoing pain with the tooth on the next visit. Considering that the patient was a grinder, and she was wearing an occlusal splint, a plan to checking
and to adjusting the occlusion accompanied by placing a SS band over the tooth to protect it further had been made by the dentist. Unfortunately, a rotary file broke in the curved MB root canal during the root canal preparation session. Having a conversation with the patient, the dentist referred her to me for assessing and possibly managing the case afterwards.
Upon my examination, tooth 17 was diagnosed with incomplete Root Canal Treatment (RCT) with possibly not infected Root Canal System (RCS) with chronic apical periodontitis due to previous decay, restorations broken down or cracks. As part of endodontic consultation, the patient and I discussed future treatment options.
Looking at the pre-operative radiograph sent by the dentist, the broken piece of file seemed to be outside of the MB root. We decided to obtain a CBCT scan to assess the relationship of the file to the floor of the maxillary left sinus. The scan showed that the right maxillary sinus was involved with large inflammatory reaction.
I explained to the patient that flareup episodes of the chronic sinusitis are potentially likely to mimic the
symptoms of a periapical pain after completion of the RCT as long as the inflammation of the sinus persists. The patient remembered that she had always been suffering from complications of sinusitis for a long time, however, she has not been referred to see her GP or an ENT specialist. Having dealt with so many years of persistent pain, the patient decided to seek her dentist’s help to remove the tooth 17.
As I mentioned above, pre-assessment of a case will save us time, will prevent further complications and will improve patients’ trust to the profession and its members.
The scan’s report showed that “the instrument measures approximately 4.2 mm with approximately 1.8 mm beyond apical foramen. The pical 0.8 mm of the instrument extenders superior to the right maxillary antral base. Polypoidal mucosal thickening noted in the right maxillary sinus, in part in response to 17’s inflammatory pathology.”

Dr Sivitra Sivarajan Perth Oral Medicine and Dental Sleep Centre
The COVID-19 pandemic has profoundly affected global health, influencing various medical conditions and exacerbating existing health issues. Among these, temporomandibular disorders (TMD) have emerged as a significant concern.
TMDs encompass a range of conditions that affect the temporomandibular joints and the associated muscles, leading to pain and functional impairments. Common symptoms and signs include jaw pain, jaw locking, limited jaw movement, and headache.
The risk factors for TMDs are multifactorial.
Biological, psychological and social factors contribute to these risk factors.
Recent research suggests that the stress and anxiety heightened by the COVID-19 pandemic have significantly impacted the prevalence and severity of TMD. There have been theories on why this has occurred and these include:
• Increased stress and anxiety
The pandemic has been a major source of psychosocial stress due to health concerns, economic instability, and social isolation. Studies have shown a strong correlation between increased stress levels and TMD symptoms. Elevated stress during the pandemic has been associated with a rise in sleep and awake bruxism, which can exacerbate TMD.
• Changes in daily routines
Lockdowns and remote work arrangements have led to extended screen time and poor posture, contributing to muscular strain. Prolonged computer use and inadequate ergonomic setups during the pandemic have worsened musculoskeletal disorders in general, including TMD.
• Altered access to dental care
The pandemic resulted in a significant reduction in non-urgent dental visits. Many individuals postponed necessary dental treatments due to health concerns and lockdowns, potentially leading to the worsening of untreated TMD.
• Economic stressors
Financial difficulties have been a major stressor for many during the pandemic. Economic strain has been linked to increased muscle tension and bruxism, further exacerbating TMD.
Strategies for Managing TMD related the pandemic requires a multimodal approach. These may include:
• Stress management
Incorporating techniques such as mindfulness, meditation, and regular physical activity can help alleviate stress and its impact on TMD.
• Ergonomic adjustments
Improving posture and taking frequent breaks from screens are essential for reducing muscular strain. Ergonomic interventions have been shown to alleviate musculoskeletal issues associated with prolonged computer use.
• Dental care
Maintaining regular dental visits and treatments is crucial for managing TMD early and effectively.
• Physiotherapy
Engaging in jaw physiotherapy and targeted jaw exercises can enhance jaw function and relieve pain. Physiotherapy plays a key role in managing TMD signs and symptoms.
• Healthy eating
Adopting a balanced diet and consuming softer foods can reduce strain on the jaw. Nutritional adjustments can support overall management of TMD.
In summary, the COVID-19 pandemic has underscored and intensified various health issues, including TMD. Understanding the interplay between the pandemic and TMD is crucial for developing effective management strategies. By addressing stress, improving daily routines, ensuring regular dental care and making lifestyle adjustments, individuals can better manage their TMD during periods of significant stress and challenging times. Ongoing research and heightened awareness will be essential in addressing the long-term effects of the pandemic on temporomandibular disorders as well as oral health and overall health and wellbeing.
Li, D. T. S., & Leung, Y. Y. (2021). Temporomandibular Disorders: Current Concepts and Controversies in Diagnosis and Management. Diagnostics (Basel, Switzerland), 11(3), 459. Balasubramaniam, R., Patel, J., Shanmugasundaram, K., & Singer, S. R. (2024). The Effect of Coronavirus Disease 2019 and Other Emerging Infections on Dentistry. Dental clinics of North America, 68(4), 627–646.
Dr Mehdi Valizadeh
Dental implant complications need not mean removal and replacement. Careful diagnosis, meticulous treatment and post op care can help patients keep their implants.
A 67-year-old gentleman was referred with the chief complaint of having discomfort in the area of implant supported bridge (31 and 41). The clinical and radiographic examination revealed presence of inflammation, lack of attached mucosa, as well as progressive bone loss since installment of the implant. The diagnosis of active periimplantitis #31 implant was made. Due to the patient's satisfactory plaque control and low levels of full mouth plaque score, a surgical management was indicated. This included a surgical debridement, partial implantoplasty in the exposed part, as well as soft tissue conditioning in order to increase the band of attached mucosa in the form of free gingival grafting. This treatment in combination with regular CIST (Implant Supportive Therapy) resulted in elimination of the inflammatory component (BOP and progressive bone loss) as well as facilitation of the self-performed plaque control via tissue graft.
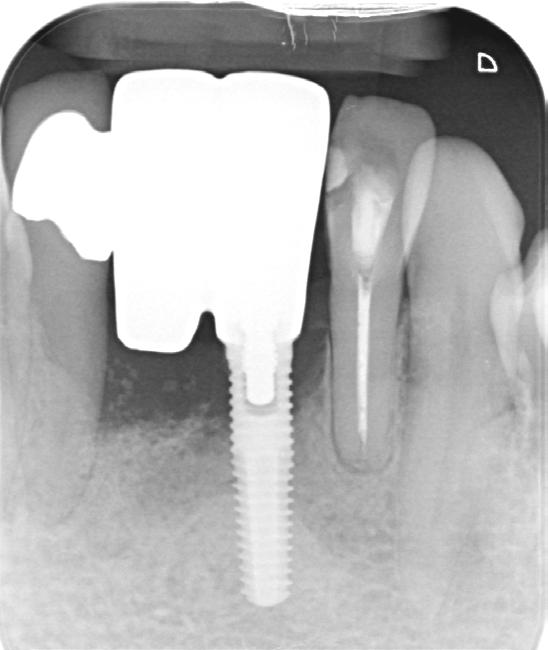




1. Radiographic view of implant in 31 position with marginal bone loss.
2. The clinical view represents exposed threads, lack of attached mucosa, and patient discomfort.
3. Intra-operative view of partial implantoplasty as well as soft tissue conditioning in the form of free gingival graft.
4. Immediate post-operative view after instalment of the suprastructure.
5. One-year post-op representing the elimination of the inflammatory condition as well as mature graft for the facilitation of the plaque removal.
Elevated risks for suicidal ideation, depression and anxiety have been reported among chronic temporomandibular pain patients, especially those with additional chronic musculoskeletal pains. Elevated depression and anxiety scores have been reported in chronic orofacial pain patients compared to pain-free subjects in controlled studies. A retrospective study found that trigeminal neuralgia accounted for 25% of suicide attempts. Primary headaches account for 1% of all suicide deaths, with cluster headaches and migraines accounting for about 70% of suicides attributed to primary
headaches. Chronic pain intrudes upon sleep, and it is recognised that sleep and pain have a bidirectional relationship, which is further modified by psychological morbidities. Insomnia too increases the risk of suicide. Therefore undertaking a risk assessment for psychological morbidities in patients presenting with persistent orofacial pain is essential.
Suicidal ideation needs to be differentiated from suicidal action plans and suicide action. Multiple variables can mediate progress from ideation to action plan. Chief amongst these are depression, hopelessness, anxiety, and other psychological morbidities, as well as means to action.
Suicide is the 15th most common cause of death, and in 2014 accounted for about 1.4% of all deaths worldwide, with the WHO predicting the trend to continue, if not increase, into 2030. Therefore action to help prevent thoughts of suicide and the development of suicidal action plans is imperative. Opportunity restriction may impede suicide action.
Non-suicidal self-injury (NSSI) is supposedly a mechanism via which progression to suicidal action may occur, hence enquiring with a patient about any such NSSI incidents would be worthwhile. Depression, hopelessness and impulsivity contribute overwhelmingly to suicide attempts too. Directly discussing the reason for suicide ideation is therefore invaluable. Even though the idea of suicide is to end one’s own life, the actual motivations seem to differ between subjects and could encompass feelings of hopelessness, desperation to escape, dealing with an unbearable state of mind, communication, and altering one’s environment. There may also be a genetic contribution, and a family history of attempted or actioned suicide seems to strongly predict suicidality in a subject. Multiple theories for suicide ideation exist, and these include psychological aches, feelings of burdensomeness and reduced
belongingness, attempts to reduce aversive self-awareness, help-seeking and communicating one’s distress, and problem-solving. Internal reasons for suicide are stronger predictors of suicide attempts than help-seeking reasons since the latter evokes a sense of social connectedness. Hence the latter is generally thought not to result in action, or result in self-harm, but not suicide.
The Scale of Suicidal Ideation created by Beck has a long history of validity, consistency and test-retest reliability, and is also one of the few clinician-administered questionnaires that help predict suicide attempts. It is important to consider that not everyone who ideates develops an action plan, following which not everyone who develops such an action plan sees it through to an attempt.
No gold standard for suicide intervention treatment exists. Three therapies seem to help with preventive strategies:
1. Dialectical Behaviour Therapy is a combination of cognitive therapy and acceptance and commitment therapy.
2. Cognitive Therapy for Suicide Prevention.
3. Collaborative Assessment and Management of Suicide Risk (CAMS), which is a newer therapy that rests upon building a strong therapeutic inter-relationship between the subject and the health care provider.
All of the above have randomised control trials proving their efficacy.
Means-restriction will help prevent action-plan to attempt conversion. In understanding what motivates the conversion of an ideation to an attempt, it is useful to construct an ideation-toaction framework which, posits that ideation needs a stimulus to transform into attempt. Three theories have been developed to help explain the mechanism of conversion. The interpersonal theory supposes that while hopelessness and desperation can motivate ideation one needs to be able to overcome
the fear of pain and death to attempt suicide. Another theory is the motivationvolition theory which supposes the need for means to present themselves to convert ideation to action. Lastly, the most recent theory is the 3-step theory, which delves into a logical three-step process to ascertain the transformation from ideation to attempt. Common to all these theories is the concept that everyone attempting suicide presents three variables that contribute to an attempt. These are dispositional (genetic factors, traits that we are born with, such as a low pain threshold), acquired (multiple episodes of pain, poor management of pain, failed treatments) and practical (availability of lethal weapons, time when no one is around, lethal medications) variables.
Assessment of every chronic pain patient utilising the biopsychosocial paradigm of pain management would involve a thorough psychosocial evaluation of the patient. Combined with motivational interviewing techniques, a therapeutic relationship can be developed with the patient and discussion of difficult topics such as suicidal thoughts or action plans could be ventured into. Prompt identification of such patients, compassion and a non-judgmental attitude, with referral to a psychologist or emergency admission to a psychiatric hospital could save a life. Ready resources are available if needed by following this link: https://www. healthywa.wa.gov.au/Articles/J_M/Mentalhealth-emergency
If you or anyone you know needs help, call Lifeline, 13 11 14.
Abramson, Lyn Y, Gerald I Metalsky, and Lauren B Alloy. "Hopelessness Depression: A Theory-Based Subtype of Depression." Psychological review 96, no. 2 (1989): 358.
Almoznino, Galit, Rafael Benoliel, Yair Sharav, and Yaron Haviv. "Sleep Disorders and Chronic Craniofacial Pain: Characteristics and Management Possibilities." Sleep Medicine Reviews 33 (2017/06/01/ 2017): 39-50. https://doi.org/https://doi.org/10.1016/j. smrv.2016.04.005
https://www.sciencedirect.com/science/article/pii/ S1087079216300119
Barløse, Mads, Nunu Lund, and R Jensen. "Sleep in Trigeminal Autonomic Cephalagias: A Review." Cephalalgia 34, no. 10 (2014): 813-22.
Baumeister, Roy F. "Suicide as Escape from Self." Psychological review 97, no. 1 (1990): 90.
Beck, Aaron T, Maria Kovacs, and Arlene Weissman. "Assessment of Suicidal Intention: The Scale for Suicide Ideation." Journal of consulting and clinical psychology 47, no. 2 (1979): 343.
Bertoli, Elizangela, and Reny de Leeuw. "Prevalence of Suicidal Ideation, Depression, and Anxiety in Chronic Temporomandibular Disorder Patients." Journal of Oral & Facial Pain & Headache 30, no. 4 (2016).
Bertolote, José Manoel, and Alexandra Fleischmann. "Suicide and Psychiatric Diagnosis: A Worldwide Perspective." World psychiatry 1, no. 3 (2002): 181.
Brown, GK, GR Henriques, C Ratto, and AT Beck. "Cognitive Therapy Treatment Manual for Suicide Attempters." Philadelphia, PA: University of Pennsylvania (2002).
Gunnell, David, Ravindra Fernando, Medhani
Hewagama, WDD Priyangika, Flemming Konradsen, and Michael Eddleston. "The Impact of Pesticide Regulations on Suicide in Sri Lanka." International journal of epidemiology 36, no. 6 (2007): 1235-42.
Hjelmeland, Heidi, Keith Hawton, Hilmar Nordvik, Unni Bille Brahe, Diego De Leo, Sandor Fekete, Onja Grad, et al. "Why People Engage in Parasuicide: A Cross Cultural Study of Intentions." Suicide and Life Threatening Behavior 32, no. 4 (2002): 380-93.
Ji Lee, Mi, Soo-Jin Cho, Jeong Wook Park, Min Kyung Chu, Heui-Soo Moon, Pil-Wook Chung, Jae Myun Chung, et al. "Increased Suicidality in Patients with Cluster Headache." Cephalalgia 39, no. 10 (2019): 1249-56. https://doi.org/10.1177/0333102419845660. https://journals.sagepub.com/doi/ abs/10.1177/0333102419845660
Jobes, David A. Managing Suicidal Risk: A Collaborative Approach. Guilford Publications, 2023.
Joiner, Thomas E. "Why People Die by Suicide." Harvard University Pres (2005).
Karamat, A., J. G. Smith, L. N. F. Melek, and T. Renton. "Psychologic Impact of Chronic Orofacial Pain: A Critical Review." [In eng]. J Oral Facial Pain Headache 36, no. 2 (Spring 2022): 103-40. https://doi. org/10.11607/ofph.3010
Klonsky, E David, and Alexis M May. "The Three-Step Theory (3st): A New Theory of Suicide Rooted in the “Ideation-to-Action” Framework." International Journal of Cognitive Therapy 8, no. 2 (2015): 114-29.
Klonsky, E. David, Alexis M. May, and Boaz Y. Saffer. "Suicide, Suicide Attempts, and Suicidal Ideation." Annual review of clinical psychology 12, no. 1 (2016): 307-30. https://doi.org/10.1146/annurevclinpsy-021815-093204.
Linehan, Marsha. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford press, 1993. May, Alexis M, and E David Klonsky. "Assessing
Motivations for Suicide Attempts: Development and Psychometric Properties of the Inventory of Motivations for Suicide Attempts." Suicide and Life Threatening Behavior 43, no. 5 (2013): 532-46.
Muehlenkamp, Jennifer J. "Self Injurious Behavior as a Separate Clinical Syndrome." American Journal of Orthopsychiatry 75, no. 2 (2005): 324-33.
O'connor, Rory C. "Towards an Integrated Motivational–Volitional Model of Suicidal Behaviour." International handbook of suicide prevention: Research, policy and practice (2011): 181-98.
O'Connor, Rory C, and Matthew K Nock. "The Psychology of Suicidal Behaviour." The Lancet Psychiatry 1, no. 1 (2014): 73-85.
Organization, World Health. "Projections of Mortality and Causes of Death, 2016 to 2060." 2020.
Pridmore, Saxby, and S Auchincloss. "Book Review: Preventing Suicide: A Global Imperative." (2015).
Simon, Thomas R, Alan C Swann, Kenneth E Powell, Lloyd B Potter, Marcie-jo Kresnow, and Patrick W O'Carroll. "Characteristics of Impulsive Suicide Attempts and Attempters." Suicide and LifeThreatening Behavior 32, no. Supplement to Issue 1 (2001): 49-59.
Tang, Nicole KY, and Catherine Crane. "Suicidality in Chronic Pain: A Review of the Prevalence, Risk Factors and Psychological Links." Psychological medicine 36, no. 5 (2006): 575-86.
Thertus, Ketty. "The Psychological Impact and Management of Trigeminal Neuralgia." Trigeminal Nerve Pain: A Guide to Clinical Management (2021): 215-27.
Vandekerckhove, M., and Y. L. Wang. "Emotion, Emotion Regulation and Sleep: An Intimate Relationship." [In eng]. AIMS Neurosci 5, no. 1 (2018): 1-17. https://doi.org/10.3934/Neuroscience.2018.1.1.

Dr Hezel Cohen, Specialist Prosthodontist
Dentistry for seniors is dedicated to addressing the unique oral health needs of older adults, with the goal of preserving their quality of life and overall health as they age. As the senior population continues to grow, the importance of geriatric dentistry becomes increasingly evident. This field tackles a variety of age-related dental concerns and advocates for effective care strategies.
Older adults commonly encounter dental challenges such as an elevated risk of gum disease, tooth decay, and oral cancer. Contributing factors include reduced salivary flow, decreased taste sensation, and various systemic health conditions. Additionally, medications frequently prescribed to seniors can affect oral health, leading to dry mouth or altered taste, which further complicates dental care.
Dentists caring for older adults address these issues with customised preventive and therapeutic strategies. Regular dental check-ups are essential for the early detection and management of conditions such as periodontal disease, decay and oral infections. These professionals also emphasise the importance of maintaining oral hygiene and may suggest specialised products or techniques tailored to the needs of the patient.
Prosthodontics is another critical aspect of geriatric dentistry. Many seniors require dentures or dental implants to replace missing teeth, which can influence nutrition and speech. Prosthodontists caring for older adults ensure that these prosthetics are well-fitted and functional, thereby improving the patient’s quality of life.
Furthermore, geriatric dentistry often involves a collaborative approach, working alongside other healthcare providers and specialists to address the broader health needs of seniors. This comprehensive method ensures that oral health is seamlessly integrated into the overall care plan, including considerations for diabetes management and cardiovascular health.
In summary, geriatric dentistry plays a vital role in meeting the complex oral health needs of older adults. By delivering specialised care and advocating for preventive practises, prosthodontists significantly contribute to the well-being and quality of life of the aging population.
Dr Hezel Cohen will be contributing further articles about addressing oral health in the senior population in future editions of the Western Articulator.






West Coast Dental Depot has over twenty years experience supplying and installing dental equipment. We have the range, knowledge and experience to ensure you and your surroundings work in perfect harmony. From design through to completion, we will make your surgery transformation an easy and enjoyable experience – all within your budget. Talk to West Coast Dental Depot, we know how to put it all together.



My Implant Dentist was recently awarded as the WA State Winner for the Dental Health Services category at the Australian Achiever’s Awards. My Implant Dentist was also named the WA State Winner for the Embracing Innovation category of the Telstra Business Awards. Congratulations to Dr Kent Tan and the team!

Congratulations to Dr John Buckland, who received his pin for 40 years of continuous ADAWA membership at the September General Meeting. Congratulations John!
We are thrilled that Panetta McGrath Lawyers have renewed their Premium Partnership with us for another exciting year. The relationship ADAWA has with Panetta McGrath has gone from strength to strength and the support the Panetta McGrath team gives our members is always appreciated. pmlawyers.com.au

Thank you to Greg LeGuier, Chief Financial Officer at AMA Western Australia, who came to the September General Meeting to talk to our members about AMA Financial Services. As AMA Financial Services is one of our Premium Partners, it was a great opportunity for our members to learn more about their services. AMA also sponsored the General Meeting.
We are pleased to announce that Smith Coffey has come onboard as one of our premium partners. For over 50 years, Smith Coffey has specialised in providing financial services for dentists. To find out more about Smith Coffey, visit smithcoffey.com.au

Mortgage Broking, Financial Planning and General Insurance Broking. As financial planning, mortgage, and insurance broking specialists, we have a deep understanding of the unique complexities and challenges faced by businesses in your industry. Given our extensive experience working with health and medical professionals, we are pleased to offer exclusive discounts/benefits on our services to members of the ADA (WA). Phone 1800 262 346 or email info@amafinance.com.au
Bunnings Trade can partner with your business to provide support with quotes, project management and product sourcing, even if it’s something we don’t stock in-store. Benefit from exclusive pricing* on a wide range of products and services. For more info on PowerPass or to sign up and link your existing membership, email Organisationswa@bunnings.com.au
*Terms and conditions apply. See trade. bunnings.com.au/powerpass for full details.

At BOQ Specialist, we understand that a highly personalised service is what dental professionals need. We offer a full range of finance products and services, tailored to your needs no matter where you are in your career. With over 30 years of experience in dental finance, our focus is on building long-term relationships with our clients so that you can make financial decisions that are right for you. boqspecialist.com.au

For over 50 years, Smith Coffey has specialised in providing financial services for dentists. We offer expertise in taxation, superannuation, mortgages, and personal risk insurance. Trust us to help you achieve financial freedom while you focus on patient care. Contact us today! smithcoffey.com.au

We are excited to offer a member benefits program exclusive to ADAWA members. As a member of ADAWA, the member benefits program entitles you to an initial 30-minute consultation in person, by phone, or via video conference. ADAWA members are also eligible for a 15% discount on our standard hourly rates - ADAWA referral required pmlawyers.com.au

Medifit is an award-winning dental design and construction company, providing a comprehensive solution for dentists and dental specialists looking to build new premises or renovate their existing practices. Established in 2002, the company has designed and built hundreds of successful practices across Australia from their Head office in Perth. Contact Medifit and get the practice you deserve. medifit.com.au

STS Group Australia is a family owned, WA business and industry leader in infection control and we have been serving the WA dental community for over 30 years. You’ll know us as Mocom Australia, offering a range of infection control and reprocessing equipment in Australia and New Zealand, STS Health, providing service and education throughout WA and STS Professional, manufacturer of infection control testing devices and related consumables. sts-group.com.au




Dr Liz Lam – new addition to the team
Dr Liz Lam commenced practice as a specialist periodontist with Dr Melanie McAlpine at Western Periodontics & Implants in February 2024. To our great delight she has been a sensation with both patients and staff. Liz has a passion for conservative periodontal care and has demonstrated high level surgical skills combining biological materials and soft tissue management for optimal patient outcomes.
T (08) 9227 9002
E reception@westernperiodontics.com.au
W westernperiodontics.com.au


Dr Anchalee Jennings-Lowe new addition to the team
Taylor Road Periodontics & Dental Implants proudly welcomes Dr Anchalee Jennings-Lowe to the practice as a Specialist Periodontist. She is accepting referrals for all aspects of periodontics, implant surgery, and peri-implantitis prevention and management.
T (08) 6382 0699
E admin@taylorrdperiodontics.com.au
A 3/150 Stirling Highway, Nedlands WA 6009
W taylorrdperiodontics.com.au


Dr Dipika Mistry – new addition to the team
Dr Dipika Mistry has joined the team at Morley Orthodontic Centre. After spending time in general practice, Dipika completed her Doctor of Clinical Dentistry in Orthodontics in Sydney in 2019. She enjoys all aspects of orthodontics, including clear aligner therapy and growth modification. Dipika brings to the practice a compassionate and cheerful disposition. Her evidence-based planning and clinical skills support our efforts to provide orthodontic care in a friendly and supportive environment.
T (08) 9276 9888
E reception@morleyorthodontic.com.au
A 25 Wellington Road Morley, WA 6062
W morleyorthodontic.com.au
Did you know
As an ADAWA member, you can submit a professional notice that will be published for three editions in the Western Articulator, free of charge. For details and requirements, email media@adawa.com.au

At AMA Financial Services, we are committed to helping dentists across Australia achieve their financial goals. Whether you’re looking to secure your financial future, find the right finance, or protect your dental practice, our expert team is here to guide you.
We offer comprehensive, tailored financial solutions with a client-focused approach, ensuring personalised service and trusted advice. We help you confidently navigate the complexities of the financial world, with your success as our top priority.
We offer personalised financial advice, helping dentists make informed decisions and achieve their financial goals. Our approach supports you in gaining control of your financial future.
AMA Finance gives you access to a range of loans from Australia’s top lenders. We simplify the process, manage negotiations, and ensure a stress-free experience from start to finish.
AMA Insurance Brokers specialise in simplifying insurance for dental professionals, offering cover for your practice, personal needs, and business, so you can focus on what matters.
Our specialists manage all tax and accounting needs for dentists, ensuring your tax obligations are handled professionally, allowing you to focus on patient care.
We provide strategic business planning, HR consulting, and recruitment support to optimise the success of your practice,
Phone: 1800 262 346
Email: info@amafinancialservices.com.au
Web: www.amafinancialservices.com.au
