THE SKINNY ON ANXIETY





MAY 6-12, 2018
If you’ve ever been hospitalized, you know how much nurses do and how critical they are to a well-run hospital and clinic. They dispense and monitor your medication, check your vitals, see to your comfort in the most uncomfortable situations, answer your questions, communicate with your family and keep your physicians updated on your condition! Even your personal doctor’s office needs a full complement of nursing staff to operate efficiently.
Nursing is one career that seems to be continuously growing. There are never enough nurses and their importance has not gone unnoticed or unappreciated. In fact, nursing has been voted the “most honest and ethical profession for the past 16 years” according to the American Nurses Association.
This year, Nurses Week starts May 6 and ends May 12, Florence Nightingale’s birthday! We at Central Florida Health are proud of our nurses and so thankful for such an experienced and dedicated team to help us provide the excellent medical

care we are known for. Wherever you may be during Nurses Week, take a moment to thank your nurses and let them know how much you appreciate all that they do.
The National Hospital Association has a celebration of its own, Hospital Week, that happens to run concurrently with Nurses Week and extends thanks and celebration to every member of the hospital system who promotes better health and a smooth running hospital.
Central Florida Health wants to take this opportunity to recognize the valuable contributions its
entire staff makes at both Leesburg Regional Medical Center and The Villages® Regional Hospital. The medical professionals in all of our departments are at the top of the
medical profession and we could not be prouder. To all our clinical and non-clinical team members—Thank you! We could not be on this journey without you. LEESBURG
600 E. Dixie Ave. Leesburg, FL 34748 352.323.5762
leesburgregional.org
1451 El Camino Real The Villages, FL 32159 352.751.8000
thevillagesregionalhospital.org
We Conduct Dementia Testing, ADHD Testing, Traumatic Brain Injury Testing and Learning Disability Testing.
MENTAL HEALTH AND SUBSTANCE ABUSE TREATMENT CENTER
We provide psychiatric evaluations, diagnosis, psychotherapy, and management of the following mental health conditions: Depression | Anxiety Disorders | Bipolar Disorder | ADHD | Adjustment Disorder Post Traumatic Stress Disorder (PTSD) | Memory Problems | Substance Abuse Psychiatric Medication Management Services | Psychotherapy & Counseling Services

Appointments available immediately

Are stem cells a miracle? Not exactly. However, stem cells are a highly e ective means of repairing damaged tissue. Stem cell therapy is a non-surgical procedure that gives the body the tools it needs to heal itself naturally. Stem cells repair damaged tissue and regenerate bone, ligaments, tendons, cartilage and muscle. Pain lessens and range of motion increases after a simple injection—without risk of infection.
Schedule a consult today to see if you are eligible for this cutting edge therapy.



The nation’s largest dermatology practice has three locations in The Villages ® community. We now accept UnitedHealthcare Medicare Advantage.

1503 Buenos Aires Blvd., Bldg. 100
The Villages, FL 32162
352.753.2812
Dr. Michael Bond (Retiring January 2018)
Dr. Michael Wangia
Dr. Christine Moorhead
Scott Clark, PA-C
Nicole Hwa, PA-C
Dori Hite, PA-C (Coming Soon)
Kimberly Neumann, Licensed Aesthetician
Lake Sumter Landing™
910 Old Camp Road Suite 166
The Villages, FL 32162
352.205.4959
Dr. Michael Bond (Retiring January 2018)
Dr. Michael Burton
Al Sy, PA-C
Kimberly Neumann, Licensed Aesthetician
Appointments: 866.400.DERM (3376)






After graduating with Honors from Howard University College of Medicine, Dr. Wangia attended University of Florida where he completed his dermatology residency serving as a chief resident. He also completed his dermatopathology fellowship training at UF where he served as an Assistant Professor of Dermatology. He was awarded “The Arnold P. Gold Humanism in Medicine Award”. Today, he is committed to providing compassionate, comprehensive and individualized dermatologic therapies.
Following a storied career, marked by excellence in patient care, Dr. Bond is retiring. Please join us in wishing him well.









The latest editions of Healthy Living, Lake & Sumter Style, Village Style, and Welcome to Lake County














Subscriptions: Order a subscription of your favorite magazine to be delivered directly to your home for just $84. Each subscription includes 12 consecutive issues of Healthy Living, Lake & Sumter Style, or Village Style. Choose 2 or more magazines for $108 per year. To order, call 352.787.4112 or mail us at: Subscriptions at Akers Media, P.O. Box 490088, Leesburg, FL 34749.
Change of address: If you are a seasonal resident or have moved, send your address change request to general@akersmediagroup.com or mail us at: Subscriptions at Akers Media, P.O. Box 490088, Leesburg, FL 34749.














Back issues: Order a single issue by mail for $7, or 2 or more single issues for $9. To

















Resveratrol is said to activate the longevity gene. Healthy Living cannot attest to that; however, this product was reviewed by staff members and did show improvement in hair and nail appearance. The basis of Resveratrol is proprietary TriActiv Technology, which is different in that it offers support at the cellular level. It’s made from organic French red wine grapes grown and harvested in organic vineyards. Added to that is the active and stable polyphenol from wild Japanese knotweed. This plant has a higher concentration of transResveratrol than red wine, which everyone knows is good for you. However, if you’re not a red wine drinker, this supplement is a great way to get the same or possibly better elements with one pill per day. According to WebMD, supplements like this may also be beneficial in reducing inflammation, lowering LDL or “bad” cholesterol, and reducing the chance of blood clots forming that lead to heart attacks.

Though Florida Hospital Waterman in Tavares has offered partial knee replacement with the Mako Robotic Arm, it is now the first hospital in Lake County to offer the total knee replacement, according to a press release. The Mako Robotic-Arm Assisted Total Knee Replacement is the latest advancement in joint replacement surgery and transforms the way the procedure is done. FHW’s team of orthopedic surgeons has the most experience in Central Florida doing robotic-assisted surgery procedures for joint replacement. The knee pain suffered by most patients is the result of deterioration due to arthritis, which can be very painful. By using the roboticarm assisted-surgery system, the surgeons have the ability to plan more accurately and place implants, reducing the variability within the total knee replacement procedure. “Being the only hospital in the area to offer the latest advancements in joint replacement technology is something that we pride ourselves on,” says Heather Wood, who has a master’s degree in nursing and is director of surgical services at the hospital. “The Mako system allows the surgeon to make the proper adjustments during surgery as necessary and guides the surgeon to help provide the most precise placement and alignment of the implant. We are incredibly excited to be able to offer this to our patients.”

A new program was launched recently by Florida Hospital Waterman, which partnered with the Friends of the Tavares Public Library to “give newborn babies the gift of a lifetime.” Each newborn will receive his or her first cloth book along with a tote bag for mom to carry everything needed for baby. Pictured from left to right: Millie Leon, Friends of the Tavares Library; Kathy Chastain, Florida Hospital Waterman; Tavares Mayor Lori Pfister; Director Gary Early, Tavares Public Library ; Georgia Skyers, director of critical care & women/children services, FHW; Amy Easley, FHW; Lynn Kirman, chief nursing officer, FHW; Dayna Hirsch, FHW; Valerie Madden, Tavares Public Library; Stacy Lucas-Austin, FHW; Norma Emerson, Friends of the Tavares Library.

One good way to rid the body of toxins is with nutrient-charged soups, says Cherie Calbom (www.juiceladycherie.com), a best-selling author and nutritionist whose latest book, “Souping is the New Juicing,” includes a toxicity quiz. “Soup can be a part of any detox program,” Cherie says. “What if you never changed the oil or filters in your car? Our bodies are a bit like our cars. They have filter systems that need to be cleaned out and fluids that need to be flushed out. That’s where soup comes in, offering an abundance of antioxidants, phytonutrients, vitamins, and minerals.” Cherie holds a master’s degree in whole foods nutrition from Bastyr University. Known as “The Juice Lady” for her work with juicing and health, she is the author of 33 books.

INGREDIENTS
5 garlic cloves, minced
1 TBSP. extra-virgin olive oil
½ TSP. sea salt

1 CUP broccoli, chopped
1½ CUPS spinach
1 CUP kale, chopped
1 CAN cannellini or great northern beans, drained
2 TSP. fresh turmeric, chopped or
1 TSP. dried turmeric
¼ CUP lemon juice (1½ lemons, juiced)
1 large bunch of cilantro, chopped
1 TBSP. all-purpose seasoning
1 bouillon cube
3½ CUPS of water
Sea salt and pepper to taste
1. On medium heat sauté garlic with olive oil and salt.
2. Add chopped broccoli and stir for five minutes.
3. Stir in spinach until the leaves are wilted, then add the rest of the ingredients.
4. Stir and simmer for 15 minutes.
‘‘
More than 7 million Americans are living with an artificial (prosthetic) knee (4.7 million) or hip (2.5 million), which may have significant future implications in terms of the need for ongoing patient care.
—American Academy of Orthopaedic Surgeons
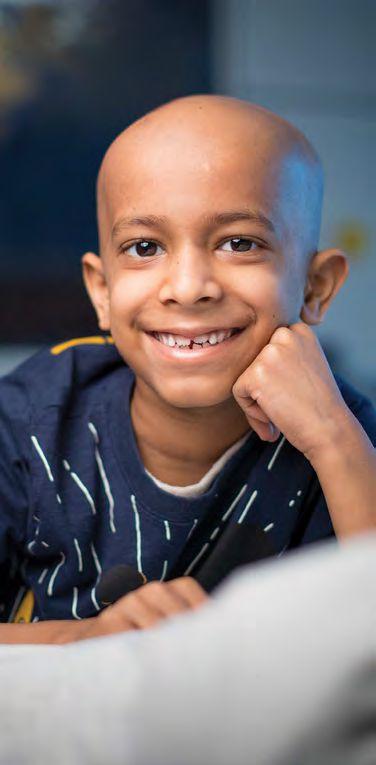
After fleeing Puerto Rico, a mother and son start a new life.

One hurricane was enough to make Sasha Guevarez think about leaving Puerto Rico. Two sealed the deal.
Hit with the one-two punch of hurricanes Irma and Maria in September 2017, Sasha and her 8-year-old son, Yael, fled for Clermont to move in with her godmother. They were among thousands of Puerto Ricans who migrated to Florida. The move was bittersweet, however, as Sasha’s partner and Yael’s father, Joel Grajales, stayed behind to complete mechanic’s training.

Still, the decision was easy.
Hurricane Maria devastated Puerto Rico for 24 hours, Sasha says, leaving the island without power and virtually underwater. At her home in the city of Florida, water sprayed through the windows like it was pumped from a fireman’s hose, she says. Sasha mopped continuously, never sleeping, to minimize flooding inside. Outside, satellite dishes floated by and roofs blew away.
“We were scared of all the things flying around and hitting the windows,” Sasha says. “The wind was so bad that it felt like the whole house was shaking, like an earthquake, and the windows [rattled] like someone was banging on them. You felt like all the things were going to fall on you.”
The cement house survived, but the family’s belongings were ruined.
“We didn’t lose our house, but we were losing everything else—my son’s education, the power, the water,” Sasha says.
Since the move, Sasha has made a difficult transition from stay-athome mom to breadwinner. During a typically hectic day, she takes Yael to school, works an hour as a crossing guard, cooks breakfast and lunch at Golden Corral, then returns for another hour at her crossing guard post, and picks up her son— all without a car.
Sasha, a graduate of the University of Puerto Rico with a degree in fine arts and photography, also makes and sells crocheted crafts and mosaic artwork. She hopes to parlay her talents into a job as an arts teacher.
She says Yael is adjusting well but misses his father, who, in turn, is alone in Puerto Rico while working and studying full time. She expects Joel to join her in August. For now, though, after moving from one Florida to another, Clermont couldn’t look any better to Sasha.
“I don’t really want to go back,” she says. “I want to stay here and make a life for me and my son, and for my husband to come here to be a mechanic and try to start a new life.”
As Lake County continues to grow, so does our need for high-quality health care. We are excited to announce our new facility – Orlando Health South Lake Hospital Emergency Room and Medical Pavilion at Blue Cedar – which will enhance your access to healthcare when you need it most.


It’s late at night and you’re getting sleepy. If you’re a guy, you may want vivid dreams of Angelina Jolie or another Hollywood hottie. If you’re a woman, your choices for a dream man might include George Clooney or the latest stud muffin from the movies.
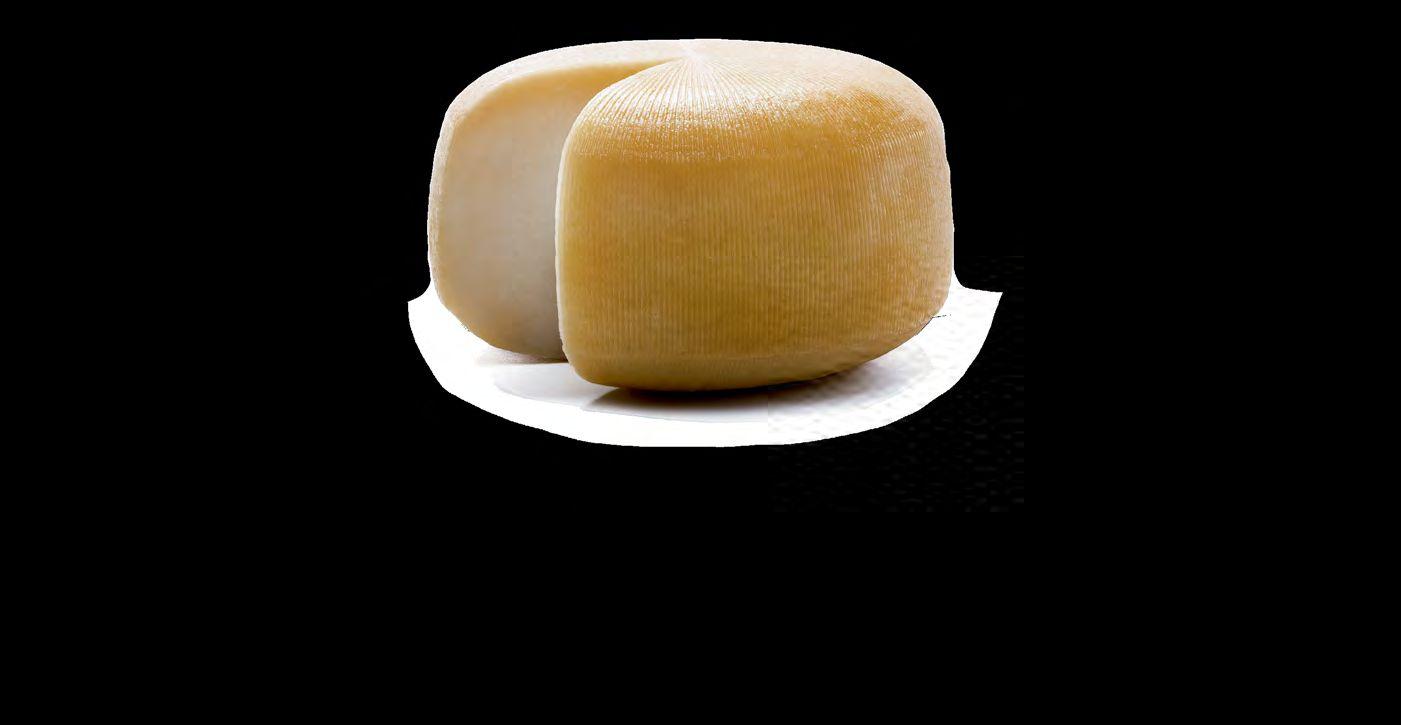
According to one study, you can dictate the dream you’re going to have. If you want to dream of celebrities, eat a chunk of cheddar cheese before bedtime.
Admittedly, the source of the study—the delightfully named British Cheese Board—may be accused of cheese bias.
One purpose of the study was to refute the old saying that eating cheese at night gives you nightmares. That old wives’ tale has been around a long time. In “A Christmas Carol,” Ebenezer Scrooge blamed “a crumb” of cheese for his ghostly encounters.
In an attempt to disprove that theory, the British Cheese Board fed cheese a half-hour before bedtime to 100 male and 100 female volunteers. Each participant was assigned one of several types of British cheese.
Happily, for the cheese board, the study did not reveal cheese produced nightmares. But strangely enough, the study showed different kinds of cheese led to different dreams. For example:
Cheddar cheese produced dreams about celebrities.
Red Leicester caused dreams of nostalgia, like childhood.
Lancashire cheese created dreams about work, which might be nightmares for some.
Stilton cheese produced outlandish, even weird dreams, such as soldiers fighting with kittens instead of guns or a vegetarian crocodile upset that it couldn’t eat children.
Cheshire cheese didn’t produce any dreams but provided peaceful sleep.
The sleep-inducing properties of cheese likely come from tryptophan, the amino acid found in milk, chicken, turkey, and peanuts. The body uses it to produce serotonin, which can produce a stable mood and sound sleep.
“Tryptophan is known to be something which is helpful in normalizing sleep and reducing stress levels,” says Nigel White, secretary of the British Cheese Board. “That seemed to make sense to us. What was really wacky was the type of cheese people were eating seemed to give them different types of dreams.”
Stick with cheddar cheese. Dreaming of Angelina Jolie is a lot more fun than dreaming of a distraught crocodile.
Sources
“Does Eating Cheese Give You Nightmares?” by Rebecca Turner, “World of Lucid Dreaming”, world-oflucid-dreaming.com/does-eating-cheese-give-you-nightmares.html
“Can Eating Cheese Really Give You Nightmares?” by Elizabeth Millard, Men’s Health, Dec. 15, 2017, menshealth.com/health/does-eating-cheese-cause-nightmares
“Does Eating Cheese Before Bed Give You Nightmares?” Science Alert, Oct. 30, 2014, sciencealert.com/ does-eating-cheese-before-bed-give-you-nightmares
“Does cheese give you nightmares?” by Claudia Hammond, British Broadcasting Corporation April 17, 2012, bbc.com/future/story/20120417-does-cheese-give-you-nightmares
“Does Eating Cheese Before Bedtime Really Give You Nightmares?” by Laura Barns, “Dreams”, dreams. co.uk/sleep-matters-club/eating-cheese-bedtime-really-give-nightmares/

























As active as you want to be.







Whilewomentodayarestrongerandmoretough-minded thaneverbefore,theystillfaceissuesevenin2018.This month,HealthyLiving isbringingthoseissuestolight.

Balancing career and family calls for organizational skills.
Story: Theresa CampbellA recent study of 2,000 working mothers of children ages 5 to 12 revealed the average mom works 98 hours per week—the equivalent of 2.5 full-time jobs. The findings from Welch Foods Inc. doesn’t surprise one local mom.
“I totally agree with it; I never sit down,” says Jeo (pronounced “Jo”) Watterson, 38, of Fruitland Park, a busy mother of five children. Her day begins at 6am and it’s shortly before midnight before she drifts off to sleep.
“There’s never a dull moment,” she says. “I am constantly cleaning or washing laundry, cooking meals, or taking somebody somewhere.”
The “somewhere” destinations are to and from school, ball games, dance classes, doctor appointments, and more.
She’s not complaining. Jeo and her husband of 15 years, Dane, love being parents to their four sons and one daughter: Kanyon, 14; Evah, 12; Kaysen, 10; Kynton, 4, and Kavyn, 1 1/2.
To earn a little extra family income, Jeo recently began working at night at the front desk of Dance Dynamix, where her daughter takes classes. From the dance studio, Jeo goes to a doctor’s office to clean it while her husband cares for the kids. He works


More women are reporting sexual harassment.
Story: Chris GerbasiDuring the past year, the #MeToo movement has exposed the issue of sexual harassment and sexual assault like never before. Many prominent leaders in all walks of life have resigned their positions, state and federal legislators have worked on new laws, and sexual harassment has been the focus of women’s marches around the country.
A correlation can be found between #MeToo and an increase in harassment complaints, says Victoria Mesa-Estrada, an employment lawyer for Florida Legal Services and a board member of the Florida Council Against Sexual Violence in Tallahassee. More women are seeking help from the council and, on the labor side, she’s seen a rise in workplace complaints.
Unfortunately, distinct differences exist among women when it comes to reporting incidents, Victoria says. Immigrants and low-paid workers are less likely to complain for fear of immigration issues or losing their job.
“A professional woman in an office with, say, a higher education than high school is more likely to try to get help,” she says. “A farmworker woman will not report it and will not ask for help.”

#MeToo has influenced groups such as the National Organization for Women (NOW), which in December announced the #EnoughIsEnough campaign. The goal is to develop strategies to address sexual harassment in workplaces and schools, with a special focus on low-paid workers.

Members of Lake NOW, a chapter based in Mount Dora, have embraced #MeToo because some of them have experienced harassment in the workplace, President Mary Flanagan says.
“It is a cultural shift,” she says. “It’s not just women stepping up but men stopping—thinking about what their behavior is and (realizing) it’s inappropriate.”
Of course, sexual harassment is not restricted to the workplace. Victoria says many cases involve women who are harassed in family settings by a relative or someone close to them. In any situation, however, the council has simple advice.
“We always advise them to first find a safe place and report it,” Victoria says.
• Don’t ignore sexual harassment—address the harasser and make it clear you want the behavior to stop.
• Report sexual harassment immediately so your employer can take action.
• Document incidents of sexual harassment and keep pertinent emails.
• If possible, do not quit your job or your legal rights could be jeopardized.
Source: Whittel & Melton law firm website

or widowed, should be savvy about their finances.
Elaine Bastl, a retiree living in The Villages, defied those 1950s stereotypes when she was growing up. She loved math and learned the value of a dollar from her father, who worked three jobs. Once Elaine married, she paid the household bills. But after nine years, she and her husband divorced.
Divorce or widowhood leaves many women in financial limbo. They should know everything about the family income, bank accounts, investments, mortgages, loans, credit cards, life insurance, and where financial documents are kept.


While raising two daughters and knowing she had to “figure things out for myself,” Elaine attended a financial seminar and received some good advice: pay yourself first. She set up bank accounts for each daughter and made deposits with each paycheck. She created a household budget and included her daughters in the process.
“I love budgets to this day,” Elaine says. “It’s a simple mathematical equation. It encouraged me to be aware of where the dollars go and where they’re coming from.”
Elaine eventually worked in a variety of fields, including public relations and marketing.
“I was always figuring out how to make enough money and how to save enough money, and do [things] for my daughters,” she says.
Budgeting in retirement remains a necessity. Women face greater economic challenges than men in retirement because they often have lower lifetime earnings, and they tend to live longer than their husbands, so retirement savings have to last a longer period.
Elaine passed her fiscal discipline on to her daughters, both of whom are married, employed, and taking care of their money—a task every woman should embrace, Liz says.
“At the end of the day, women hold all the power whether they know it or not,” Liz says. “With 99 percent of couples, women end up being the decision-makers.”
Domestic violence victims can find help through many resources.
Story: Chris GerbasiMost survivors of domestic violence suffer seven acts of victimization before they finally say, “I can’t do this anymore.”
That disturbing statement comes from Reenea Wheeler, a victim advocate at Haven of Lake & Sumter Counties. Each year, Haven aids 12,000 to 15,000 female victims of domestic violence and sexual assault, about 95 percent of whom have at least two children, she says.
“The one thing we always try to stress to them is to get out of the situation,” she says. “We stress the fact that they need to get away from the abuser.”
Unfortunately, Reenea says, that’s the most difficult choice for abused women to make, because the life they’re in is all they know, and their abusive partner may be the sole provider for the family. Domestic violence also knows no boundaries, such as age groups or race or ethnicity, she says.
In 2016, police agencies across Florida received 105,640 reports of domestic violence crimes, including 1,663 in Lake and 314 in Sumter, according to the Florida Department of Law Enforcement. About 80
percent of the cases statewide were categorized as “simple assault”; 179 were murders.
Leesburg police Detective James Dunagan sees his share of domestic violence cases.
“It is certainly a big problem in Leesburg,” he says. “All couples argue, and if you add drugs or family problems, it can escalate quickly.”
Many times, however, disputes come down to “he said/ she said.” Officers try to document everything possible in an effort to corroborate stories and possibly file charges.

“Victims often rescind their cooperation after things cool down, but in most states, including Florida, we can pursue criminal charges without the victim’s cooperation,” the detective says.
Police often refer victims to Haven, one of Florida’s 42 certified domestic violence centers offering crisis intervention, legal advocacy, children’s services, shelter at a confidential location, and a host of other services at no charge.
Of course, it’s impossible to know how many women don’t seek help, but Reenea sees one positive trend: more women are reporting their abusers.
“I think in this day and age, more women are willing because there are more service centers than there used to be 15 or 20 years ago,” she says.
• Florida domestic violence hotline: 1-800-500-1119
• Haven’s 24/7 domestic violence hotline: 352.753.5800 (or go to havenlakesumter.org)
• Sexual assault helpline for Lake and Sumter: 352.787.1379.
• Lake County Outreach Counseling Office, 2600 South Street, Leesburg, 8am-5pm Monday-Friday, 352.787.5889.
• Sumter County Outreach Counseling Office, 2748 County Road 470, Lake Panasoffkee, 9am-5pm Monday-Friday, 352.793.5365.
Find love with a click of a mouse.
Story: Theresa Campbell
In today’s busy society, online dating has evolved into the most widely accepted and practical way to meet people to date, according to Michelle Afront, author of “The Dang Factor, the Dude Factor, and the Profile Factor.”
However, she notes online dating takes time and effort.

“You’re likely going to go on many dates before your match is made,” Michelle says in a press release. “Do not focus on the bad dates or bad apples. Instead, focus on the potential matches who may end up being your life partner. Look for those with a similar socioeconomic, educational, and life status. Date those whose lives seem like they could mesh with yours.”
Celeste, 60, who enjoys winters in Leesburg, has found online dating can result in moments of excitement, disappointments, and a few winks from creeps.
“If nothing else, it put me in touch with a few men that I would never have met otherwise. I got to test my flirting skills after 33 years of marriage and three years of widowhood,” says Celeste, who asked that her last name be withheld.
When she first went online, Celeste noticed some teenage feelings of selfdoubt creeping in.
“It can feel like you’re back in high school, with the guys lined up in the hallway passing judgment on you. That’s not a good feeling,” she says. “It’s worse for the over-50 group because the pool of men is so small compared to women.”
However, she found it thrilling to be pursued by two men at the same time. “It made me feel young even if I ended up not liking either of them,” Celeste says.
She’s not giving up online dating just yet, as she intends to pursue some smaller sites, and she offered these words of advice to other women interested in online dating:
• Don’t spend more than an hour a day on the site. It’s not worth it. They always tell you not to talk “off the site,” but it’s more practical to do so.
• Get a “burner phone app” on your phone with a different phone number to talk with potential dates until you feel like you want to meet them.
• Talk on the phone. Texting creates a false intimacy. You learn a lot when you talk to someone on the phone.
Celeste also offered tips for men about their online profiles: “Stop taking photos in the bathroom mirror, in bed, and with your tongue hanging out. It’s just disgusting.”
Many seem to be open to the idea of a woman holding the highest office in the land.
Story: James Combs
In 2016, Hillary Clinton came oh-so-close to becoming the country’s first female president, besting Donald Trump in the popular vote but falling short in the Electoral College. Her defeat left many Americans wondering whether the country will ever have a woman president.
It’s a fair question, especially when you consider that women have risen to leadership positions, including president and prime minister, in 70 countries.
Americans seem to think women make effective leaders and have the right qualities to lead the country. That was evident when we walked the downtown streets of Eustis, Mount Dora, and Tavares and asked random locals and visitors this question: “Do you think a woman would make a good president?”
Here are their responses:
“Women are every bit as capable, hardworking, and intelligent as men. A female president would bring different perspectives, different backgrounds, and different life experiences to the White House.”
—Brandi
Cahill, Eustis


“I’m not a big fan of the current president and think we need change. If change means electing a female president, then I’m all for it. I don’t think Trump has much compassion for anybody. A woman would be much more compassionate to the elderly, minorities, and children.”

—Joseph
Davis, Mount Dora
“The United States is a world power, so there’s no reason why we haven’t had a female president. The best thing about electing a woman is that she will bring a kinder perspective to the White House. I do think we’ll see a female president in my lifetime.”
—Mary Hobson, Eustis“Sure, I want a female president as long as it’s not Hillary! I want a president with less baggage than her who doesn’t owe anything to anybody. Women see things in different ways than men, and we’re less hostile and more compassionate. That’s why I think a woman would make for a fantastic president.”
—Malena Doyle, Apopka“Having a female president is a good idea because it would show everybody that we’re truly free in this country. We’re the land of the free, so everybody should have an opportunity if they’re qualified.”
—Jesse
Pollock, Zellwood“I think a female president would be great for the country because it would show women that they can aspire to be whatever they want. I also think a female president would do good for everyone, not just fellow millionaires or billionaires.”
—Jorge Sota, Orlando

Did you know that doctors recommend checking your skin regularly? Our moles, blemishes, freckles, and other marks are unique. They can change over time, from aging or from seasonal variation, but also from skin cancer. How can you tell when you should see your doctor?
Learn your skin patterns. Skin self-exams work best in a well-lit room before a full-length mirror. Use a hand-held mirror for hardto-see places like the backs of your thighs. Examine all areas, including your palms and soles, scalp, ears, nails, and back.
Basal cell carcinoma accounts for about 80% of non-melanomas.
Squamous cell carcinoma accounts for about 20% of nonmelanomas.
Melanoma, though rare, is much more likely to grow and spread if left untreated.
Tell your doctor about any spots on your skin that are new or changing in size, shape, or color, or if you find any unusual sores, lumps, blemishes, or markings. Changes in how your skin looks or
Exposure to certain chemicals (like arsenic) can increase your risk of skin cancer.
Radiation exposure, especially for children who received radiation treatment, can increase the risk of skin cancer.
feels could be a cancer warning sign. Signs include skin that is red, swollen, scaly, or crusty, that feels itchy, tender, or painful, or that is oozing and bleeding.
Key warning signs for basal cell and squamous cell carcinomas include a new growth, a spot or bump that grows larger, or a sore that doesn’t heal within a few weeks. Key warning signs for melanomas also include mole changes. Sometimes even doctors can’t tell the difference between melanoma and an ordinary mole, another good reason to learn your skin and to be aware of any changes.
1. Exposure to ultra-violet (UV) rays from sun and from tanning beds
2. Light-colored skin
3. Previous skin cancer
4. Long-term or severe skin inflammation or injury.

When examining moles, use the ABCDE rule:
A=Asymmetry: One half of a mole or birthmark does not match the other.
B=Border: Edges are irregular, ragged, notched, or blurred.
C=Color: Color is not the same all over and may include different shades of brown or black, or may have patches of pink, red, white, or blue.
D=Diameter: Spot is larger than 6 millimeters across (about pencil eraser width).
E=Evolving: The mole’s size, shape, or color changes.
Also check to see if a spot looks different from all the other spots on your skin. If you see something that doesn’t look right or that causes you concern, tell your doctor.
91,270
The estimated number of melanoma cases that will be diagnosed in the U.S. in 2018
The estimated number of non-melanoma skin cancers diagnosed in the U.S. each year
Most of us are aware of the cause of skin cancer: Excess sun exposure. The important thing to note is the sun exposure in our youth and subsequent few decades which leads to the skin cancers that develop in our 50s, 60s, and 70s. Avoiding sun exposure at any age is worthwhile, but when we are with our grandchildren, urge either minimal Sun exposure or the liberal use of sunscreen, SPF 30 or more.


Minimum recommended SPF strength for sunscreen
92%
5-year survival rate among all people with melanoma of the skin, from the time of initial diagnosis
quick quote
“Skin has a good memory. Skin is like the ground we walk on every day; you can read a whole history in it if you know how to look”
— Caroline Kettlewell


and events—its actions enlivened with possibilities, respect, and humility.
The good news is every human being also is given the amazing gift of neuroplasticity, the ability of the brain to change neural connections that have become default habits. Self-compassion is vital in this transformation, shedding light on timeworn stories with outdated themes such as “I am helpless” or “I never finish things” by providing the strength, persistence, and self-confidence to question the source of such harmful beliefs, revealing them as the false messengers they are.
For nothing boosts a woman’s physical presence, glow of health, or unique beauty than being free to be her best self.
These three awareness tools can help you feel what parts of your life are truly yours, and what parts could use intense examination:


The “Yes, . . . and . . .” awareness tool minimizes reactive thinking and the “glass is half-empty” outlook. Here’s an example: “Yes, I’m feeling confused and irritated about the direction of my work, and today I noticed these feelings faded as I enjoyed much-needed time with my daughter.”
Choosing to reframe our daily circumstances brings mindfulness to restrictive patterns of good/bad, right/wrong, black/white—a “reality check” about the paradoxical aspects of life with its eye-opening acknowledgment that each day is filled with both difficult and positive aspects.
Be diligent in identifying old stories not of your own making, and the consequences you have carried as a result of these family tales and cultural assumptions. Seeing with clear eyes and listening with an open heart allow unresolved endings, uncelebrated beginnings, and all that life in-between to be reclaimed and rewritten. After years of suppressing or minimizing these stories, your attention, curiosity, and care can bring newly restored meaning and resilient strength to the threads of your life.
ABOUT
Mindfully choosing your spoken and written words, and listening deeply to others expand empathy, appreciation, and discernment. It is a profound attentiveness in both conversation with others and conversations with yourself. Listen well to your own voice, and remember: there are more than 7.5 billion other people on the planet, all with their own perspectives. Know that listening with compassion and consideration for others and yourself is a sacred act.
With a consistent practice of self-reflection, the hold of disempowering stories and self-talk diminishes—opening up a calmer way of living with compassionate power as your new source of clarity and well-being.
A renewed commitment to dreams and possibilities you’ve ignored, or once thought you were incapable of achieving, begins to bloom. If many of my coaching clients had not recognized the “should” or “should nots” that once ruled their lives, they still would be stuck in dead-end relationships and careers. Allowed into daily consciousness, the phrases “I can” or “I am worthy” literally take root and begin to flourish as the brain creates fresh neural connections—our wiser, reinvigorated patterns of thought, speech, and behavior.
In their novel “Sunlight and Shadow,” authors Sue Boggio and Mare Pearl remind us: “It struck her as miraculous that there was unlimited power and freedom in choosing what one thinks.”
To rise out of powerlessness is one of the most difficult actions you may ever take. Yet to do so changes everything— like a phoenix rising out of the ashes—and makes you whole again because you have survived searingly tough times and came back stronger, a woman whose nourishing wisdom and compassionate power now ripple out into the world. One person, one family, one community at a time.
THE WRITER → Nancy G. Shapiro is author of “The Book of Calm: Clarity, Compassion, and Choice in a Turbulent World.” Sections of this article were excerpted from the book. Nancy advocates calm as a professional certified coach, author, and workshop leader. Visit nancygshapiro.com.The calm of compassion is a woman’s best health and beauty secret.Story: Nancy G. Shapiro





A unique twist for chicken → DIFFICULTY: EASY
INGREDIENTS
1 medium to large head of cabbage
1 lb. chicken sausage
1 small bag of baby carrots (sliced)
1 yellow or white onion (sliced)
3 32-ounce boxes of chicken broth (organic with no MSG)
1/2 TSP. curry powder
Dash of pepper
Dash of thyme
1. Brown the chicken sausage in a large soup pot. Meanwhile, prep the veggies.
2. Chop up the head of cabbage into chunks and slice carrots and onion.
3. Once the sausage is browned, drain off any fat.
4. Then add the rest of the ingredients.
5. Simmer until the vegetables are soft.
I received my initial training and certification as a wellness coach at Spencer Institute.


I continued my training as a health coach at the Institute for Integrative Nutrition’s cutting-edge health coach training program. I studied more than 100 dietary theories, practical lifestyle management techniques, and innovative coaching methods with some of the world’s top health and wellness experts. My teachers included Dr. Andrew Weil, director of the Arizona Center for Integrative Medicine; Dr. Deepak Chopra, leader in the field of mind-body medicine; Dr. David Katz, director of Yale University’s Prevention Research Center; Dr. Walter Willet, chair of nutrition at Harvard University; Geenan Roth, best-selling author and expert on emotional eating; and other leading researchers and nutrition authorities.
At Total Nutrition and Therapeutics, I help you create a “sustainable” lifestyle change. Meeting you where you are in your journey and equipping you with practical tools to grow and learn new strategies; teaching you how to shop and plan meals; helping you create new ideas; and learning how to eat out are a few of the hands-on lessons you receive. I teach you how to live well for life!


‘‘
“My favorite thing to do is teach how to cook easy, healthy, budgetfriendly meals with minimal ingredients!”
—Jaime Alonso certified health coach





There are many easy ways to include more vegetables in your diet.
 Story: Melody Schoenfeld
Story: Melody Schoenfeld
Listen to your mother: eat your vegetables. Scientific evidence indicates she’s right. Green leafy vegetables may slow age-related cognitive decline and consuming more produce correlates with lower heart disease risk. High vegetable intake also lowers the of risk of some types of cancer and Type 2 diabetes. Vegetables even play a role in keeping wrinkles to a minimum and good skin health in general.
Of course, eating more vegetables is helped by other healthy choices, such as less junk food, more exercise, and less smoking, alcohol, and drug use. Regular salads don’t nullify a sedentary lifestyle or a smoking habit. Still, eating lots of veggies daily has plenty of benefits, and most Americans don’t eat enough of them.
If you shun green things on your plate or know someone who passes on the produce, I feel your pain. I often find myself feeding people disgusted by anything that grows in the ground.

These ideas worked for me:
Even the pickiest eaters may like veggies in soup form. An easy recipe: Throw chunks of root veggies (sweet potatoes, turnips, rutabaga, carrots, parsnips, etc., and/or winter squash) in a pot, slow cooker, or pressure cooker along with veggie broth, and cook until tender. Celery, broccoli, cauliflower, fennel, and mushrooms are great, too. Once soup is cooked, add bite-sized pieces of dark green veggies (bok choy, kale, spinach, chard, etc.) to wilt in the hot soup. Lentils or other beans, barley, or even alphabet noodles are great for soup, and you can also add the protein of your choice (I love seitan chunks). For a tomato-based soup,

Steam and puree broccoli or cauliflower and add to pasta dishes, mashed potatoes, or omelets/tofu scrambles. Use cooked, pureed winter squash in pancake, waffle, or French toast batter, or mix it into mac & cheese. Throw a handful of greens into a smoothie. Spread veggie puree onto the inside of bread before making grilled cheese sandwiches. Use very finely chopped greens in lasagna or baked ziti. Most of the time, the flavor or texture of the veggies is masked enough that veggie-deniers won’t notice.

4. USE HERBS!
Herbs pack a great nutritional punch. Play around with basil, cilantro, chives, sage, rosemary, thyme, parsley, garlic, and more in your cooking, or top popcorn with a mix of herbs. In the summer, I puree ginger and mint or basil leaves into lemonade.

3. MAKE PESTO.
Pesto is easy and delicious and makes eating extra veggies a snap. I’ve made it with basil, broccoli, carrot tops, kale, and arugula.
The basic recipe is this:
INGREDIENTS:
2 CUPS of the greens of your choice (I lightly steam broccoli first, but you may prefer it raw)
GARLIC, to taste (I LOVE garlic and use a full head or more; you may be happy with just 2 or 3 cloves. You can experiment with roasting the garlic in the oven at about 400 degrees F until slightly golden before adding it to the pesto—I love it that way, and it helps
DIRECTIONS:
avoid garlic breath).
½ CUP oil (adjust depending on your preferences)
¼ CUP nuts of your choice (pine nuts are traditional, but try walnuts, pistachios, hazelnuts, even macadamias! I don’t recommend using peanuts.)
Salt and pepper to taste
1. Mix everything in the food processor or blender until smooth. Some like to add a bit of parmesan cheese or nutritional yeast as well.
2. Top pizza, pasta, potatoes, tofu, beans, and more with this pesto, or add it to anything you think it will enhance.

3. Use your imagination—add it to other vegetables to up the taste factor!

6. TAKE A GREEN POWDER. If worse comes to worst and the only way you’ll take your veggies is to hold your nose and drink them fast, several veggie powders are available to add to your daily routine. It’s not ideal, but you’ll get a nutritional boost. And who knows, maybe you’ll browse the produce section a little more in the future.

5. STICK ‘EM IN SANDWICHES. Add spinach, sprouts (try broccoli sprouts!), tomato slices, peppers, onion, and fresh herbs like basil, and they’ll forget they’re munching healthy stuff. Pesto is a great sandwich spread, too!
ABOUT THE WRITER → Melody Schoenfeld is the author of “Pleasure Not Meating You: A Science-Based Approach to the Vegan Lifestyle (And Some Recipes, Too)” and has been a leader in the fitness industry for more than two decades. She owns Flawless Fitness, a personal training center in Pasadena, California, and Evil Munky Enterprises, a fitness equipment manufacturing company For more information, visit pleasurenotmeatingyou.com/ or connect on Facebook and Twitter.


The answer is an emphatic ‘Yes!’
Story: Nancy BryanThe best way to understand anxiety and weight is visualizing the body as a messaging system that dwarfs the distribution system of the post office. While you feel anxiety, your body undergoes a set of processes known as “the stress response” that calls forth a dazzling array of hormones (norepinephrine, cortisol, dopamine, and others). I’m focusing on cortisol, the hormone primarily responsible for fat formation.
Before he developed the South Beach Diet, Dr. Arthur Agatston, a cardiologist, noticed many of his obese cardiology patients at risk for developing type 2 diabetes had what is called “metabolic syndrome,” a condition with three wellrecognized symptoms: belly fat, insulin resistance, and reactive hypoglycemia.
Source: calmclinic.com
This was reinforced by Dallas and Melissa Hartwig’s book, “It Starts with Food.”
If you are chronically stressed-out, most of the stress you feel daily is in your subconscious. You may not be the only one blind to it; your doctor (possibly chronically stressed-out) may not see your problem is stress related.
Stress also causes the release of dopamine from the brain’s limbic system, which binds to specific receptors in the brain. The ultimately futile search for more gratification from addictive substances is the essence of how addiction works.
Let’s be crystal clear—with compulsive eating, food functions not as nourishment but as a narcotic, a substance capable of instilling an artificial feeling of calm and removing unwelcome awareness.
When my husband died nearly four years ago, my eating spiraled out of control. Because I was eating too much, I gained
weight steadily and faced widowhood getting fatter and fatter, which I certainly didn’t want.
I understood that if I wanted this unhealthy pattern to stop, I had to eliminate the foods I craved constantly, so right away I cut wheat, sugar, and dairy from my diet.
The results were dramatic and gratifying. Immediately my food cravings ceased; I ate normal portions of food at normal times of the day.
To my surprise, I pushed plates of food away, even with food on the plate. And I lost the excess weight I had gained.
I don’t need one more shred of evidence to convince me there are two starkly different modes of eating: first, the normal way (which people of normal weight use); second, the addictive, out-of-control way, which leads to insatiable cravings and unremitting weight gain. I know which way I’ll be following for the rest of my life.
ABOUT THE WRITER → Nancy Bryan, author of “Thin Is a State of Mind,” has spent her entire working life as an editor. She also has written a bestselling self-help book, and her work has appeared in Vogue, Self, Family Health, and various museum and computer-science publications

Cortisol is released during times of anxiety. Cortisol causes fat to build up around the midsection, and is one of the primary reasons that those with stress have trouble maintaining their weight.




Specializing in:
• Mini Face and Neck Lift with Smartlipo of Neck and Jowls
• Xeomin/Botox/Juvederm/Belotero/Radiesse
• Direct Neck Lift
• Torn Earlobe Repair
• Smartlipo (Laser Assisted Liposuction)

• Abdominoplasty (Tummy Tuck)
• Arm Lift
• Thigh Lift
• Body Contouring After Weight Loss
• Breast Augmentation

• Breast Reduction and Lift
• Skin Cancer Removal and Reconstruction






Often times the loss of a beloved spouse creates the need for a change in living environment. Betty Meadows and her family faced just such a choice. Moving was not easy. In fact between her grief and adjusting to a new home the family was at a loss as to what to do. “The Benton House staff assured us that it can take some time to adjust but not to worry.”
Sure enough, with love and time Betty was happy, thriving, and saying she never wants to live anywhere else. Her family is forever grateful. “Betty’s improvement was a miracle and we attribute it all to the patience, caring, knowledge and understanding of the Benton House staff.”
Betty says “Coming here has been the best thing for me. We’re like a family and we help each other, both the residents and staff. I just love it!”


A recent article in the New York Times notes new research says we’re being too tough on ourselves. Studies are nding that to grow, improve, or produce more requires more compassion than criticism, even from ourselves. “In our culture, the unwritten message is that being hard on yourself is the price you have to pay to get things done and meet the o en-impossible expectations, standards, and ideals we sometimes hold for ourselves,” author Laurie J. Cameron says. She o ers these three keys

Make friends with the voice in your head. Realize the worrying, scolding voice is trying to help you, keep you out of trouble, and make sure you’re okay. Greet the voice with “Thank you. I know you are trying to help. I am
Realize you are not alone. It is part of our common experience to struggle or have hard times. Realizing you are not the only one to fail, experience job loss, drop the ball, hurt others, or make mistakes helps you
Deepen your self-awareness. Pay attention to the language you use to talk to yourself. Would you say that to a friend? Practice talking to
 Story: Dr. Richard T. Bosshardt
Story: Dr. Richard T. Bosshardt
The statistics are sobering and frightening. Five times more people take antidepressant drugs today than just three decades ago. One in six American adults takes at least one psychiatric drug during a year. The situation is worse for women. One in five women take a psychiatric drug, double the rate for men. Some clinicians say these rates underestimate the actual rates because many cases go unrecognized and, therefore, untreated. What’s happening there?
I have noted this throughout my career. The majority of patients in my practice are women, and 20plus years ago it was unusual to see patients on drugs for depression and anxiety. Now, it seems most patients are, either chronically or on an as-needed basis. This is issue for me because patients who take these types of drugs on a regular basis may become resistant to the types of medications I use to sedate patients for surgery. Such patients sometimes tolerate doses of sedatives that would put down a horse. It makes surgery more difficult, and dangerous.
Even more concerning, however, is the possible long-term effects of being on such drugs. The top 10 psychiatric drugs used by adults in the United States are Zoloft, Celexa, Xanax, Ambien, Prozac, Desyrel, Klonopin, Ativan, Lexapro, and
Cymbalta. Eight of the 10 cause withdrawal symptoms when stopped or are classified as Schedule IV drugs by the Drug Enforcement Administration. This means there is possible risk of creating dependence and/or abuse. Ambien, for example, is a widely prescribed sleep aid. It is intended for short-term use, but I have seen many patients who have been on Ambien for years and take it more nights than not to help them sleep. Over time, they become physically and psychologically dependent on Ambien.
Many potential problems exist with long-term use of psychiatric drugs. First, we really do not understand well how they work. Second, we do not know the long-term effects of these drugs on the human body because many have not been around long enough to gather data.
We know they, like all drugs, have side effects, some of which can be serious and even life-threatening. A listing of these is too extensive to include here. Suffice to say they are not without risks, making it imperative they be prescribed judiciously and monitored carefully. For some, once you’ve been on them for a while, you cannot simply stop taking them. In addition to withdrawal symptoms, there is the possibility of worsening anxiety or depression, and suicides are not unheard of. This is why close
cooperation between patient and physician is so important. It’s important to know why. Why have anxiety and depression become the most prevalent mental illnesses? Why are so many women having issues with anxiety and/or depression? Is life more stressful now? Although it is difficult to come by statistics for depression and anxiety from a generation or two ago, it is widely agreed that we are seeing the highest rates of these conditions in history. Some leading psychiatrists call it an epidemic. Perhaps we are better at diagnosing them today than decades ago. We just don’t know. Another concern is whether we are too liberal in prescribing these drugs rather than trying to deal with anxiety and depression through non-pharmaceutical means. The latter takes time, and, in this time-pressured age, many physicians do not have, or will not take, the time to do anything but prescribe a drug.
Anxiety and depression are real conditions that range from mild to debilitating and may be life-threatening at
times. Women dealing with these issues should follow certain steps to get proper treatment:

• Seek to identify aspects of your life creating your feelings of anxiety and depression. If you can, change them. Situational anxiety and depression often resolve with change.
• Tell your primary physician if you are depressed or anxious. It is not a character fault or failing. It is not shameful or indicative of weakness. It simply is, and may be due to genetics, environment, and circumstances.
• Follow your physician’s instructions to the letter if you are prescribed medication(s).
• Seek periodic, regular follow-up to verify whether you need to continue the medication(s).
• Do not stop any medication without notifying your prescribing physician.
• Be wary of physicians who seem quick to prescribe medications without spending time to learn more about you and your condition and/or who do not do regular follow-up to assess your condition.
• Never share medication(s) with friends or family who may have the same issues. I see this a lot and it is extremely dangerous. If they need medication, it should come from their physician.
ABOUT THE WRITER → Dr. Richard T. Bosshardt graduated in 1978 from the University of Miami School of Medicine. In 1989, he founded Bosshardt & Marzek Plastic Surgery Associates, Lake County’s first practice to provide full-time cosmetic and reconstructive plastic surgery services.

ANOREXICS—

who eat excessive amounts of food and then usually purge to rid themselves of the calories.
BINGE EATERS— who eat excessive amounts but do not purge or use laxatives.
• Excessive weighing.
• Using appetite-suppressant drugs, laxatives, or diuretics.
• Exercising extremely often and compulsively.
More nuanced clues may also suggest an eating disorder’s insidious influence: Rigid rituals around eating. Secrecy. Depression. Heightened anxiety. Avoidance of situations where there is food. Withdrawal from friends and family. Tying self-worth and mood to the number on the scale. A mindset of “food is the enemy.”
None of these facts were of particular interest to me in 1966 when eating disorder first came courting. I was an out-of-state transfer student attending
• Only eating a few certain foods viewed as nonthreatening and low in calories and fat content.
• Preoccupation with food and dieting.
• Habitually eating large amounts of food in a short period of time with no apparent weight gain or a significant weight gain.
the University of Florida, unsure of a field of study. I was 1,000 miles away from my mom and dad for the very first time. And my high school boyfriend had just broken up with me.
I lacked a strong sense of self. I had deficient anger management skills. I was preoccupied with the width of my hips. I weighed myself daily—OK, sometimes hourly—and the needle on the scale determined my mood and my level of self-confidence. My grounding thought was to stay thin. When I was thin, I coped.
CHANGE IN APPEARANCE
• Large weight loss or gain
Soared. Commanded attention. I was no longer ordinary or invisible. I got second looks from the frat boys and teaching assistants. Cafeteria workers remembered me and student leaders knew my name. It was incredibly empowering. What teenager can resist that?
Help is available if you suspect your son or daughter is “flirting” with eating disorder. Talk to your pediatrician or school counselor. Treatment centers, psychologists, psychiatrists, and eating disorder associations abound.
ABOUT THE WRITER → Iris Ruth Pastor has published more than 700 columns in various outlets, including the Huffington Post, where she was named a “Must Read Blogger.” Her new memoir, “The Secret Life of a Weight-Obsessed Woman,” emphasizes that change and renewal are possible at any age and any stage and is available through major booksellers. For more information, visit irisruthpastor.com.
who starve their bodies. BULIMICS—Essential for mobility and often over utilized, the knee joint becomes susceptible to problems and injury. One type of knee injury commonly seen in an orthopaedic clinic is a meniscus tear.
The knee is made up of three bones: the femur (thigh bone), the tibia (shin bone) and the patella (knee cap). The meniscus, is a half moon-shaped, wedge-like cushion that lies between the bones in your knee joint allowing your weight to be equally distributed across the bones. Made up of cartilage, the wedges not only stabilize the knee, but also allow the joint to smoothly slide and move in many directions.
When the meniscus is torn or damaged, you lose part of that cushioning system; your weight is no longer applied evenly across your bones, so grinding and wearing occurs as bone meets bone. After time, arthritis of the knee joint develops as the stressed bones take on more of the burden of your weight.
Meniscus tears are most commonly caused by trauma (athletic injuries) and the aging process (as we age our cartilage becomes brittle.) When the injury occurs in athletes, the patient typically describes a “popping” sensation in his/her knee when participating in a sporting event. Surprisingly, most people are still able to walk after tearing their meniscus, and we often see athletes return to
the field after this type of knee injury. The seriousness of the injury is not apparent until later, when the knee becomes inflamed, feels painful, tight and may be quite swollen.
Symptoms of a torn meniscus may include (but are not limited to):

• knee pain;
• knee swelling, commonly referred to as “water on the knee,” or technically an “effusion;”
• hearing a popping or clicking within the knee; and
• limited motion of the knee joint.
Treatment after initial injury should follow the RICE formula (Rest, Ice, Compression and Elevation.) If the knee recovers fully after RICE treatment, then no other treatment may be necessary. However, if there are still problems with the knee, a piece of the meniscus may be torn or loose and floating around inside the joint causing the knee to lock, slip or pop. In some cases, the knee will catch or lock, and the patient will have to manually manipulate the joint to straighten it.
Unlike the athletes, older folks often don’t experience trauma when they injure their meniscus. Instead, the wear and tear on the joint over the years weakens the meniscus until, one day, a degenerative tear appears.
If you think you have a torn meniscus, you should see your physician to have this evaluated further. Your exam will include your physician taking a careful history of your symptoms, palpating the joint and noting areas of tenderness. X-rays and an MRI may also be ordered by your physician to better visualize what is occurring inside your joint. If a meniscus tear does appear on your MRI, the next step is to determine treatment, and most pointedly, whether or not surgery is indicated. Sometimes an individual is not a good surgical candidate or his/her meniscus tear symptoms are minimal, in this case, we can take a “wait and see” approach. Surgery is sought when the knee becomes problematic and interferes with day to day activities.
If surgery is indicated, your surgeon will recommend either a meniscus repair (repairing the tear) or a partial menisectomy (trimming and removing the torn or loose pieces of meniscus in your joint), based on your specific injury.
A meniscus repair is an attempt to fully restore the structure, and because it is a more extensive surgical procedure, requires a longer recovery. The failure rate is higher with meniscus repair because the delicate meniscus
PAID PROMOTIONAL FEATUREtissue lacks an adequate blood supply and does not heal well. However, if the repair is successful, the joint is healthier in the long run.
When the injured tissue has completely lost its blood supply or is tattered beyond repair, a partial menisectomy is performed. Menisectomy quickly relieves the most bothersome symptoms, has a faster recovery than meniscus repair, but, because a portion of the knee’s cushioning is removed, will not reduce the risk for further progression of arthritis.
Both meniscus repair and partial menisectomy are arthroscopic surgeries. The arthroscope gives your surgeon a clear view of the interior of your knee with the benefit of only a couple of small incisions (each, approximately one centimeter in length). Using tiny instruments your surgeon can trim frayed areas, suture tears and remove fragments of the meniscus that have broken loose.
The outcome of the surgery depends on several factors, including the severity of the particular injury, the degree of damage and associated arthritis. As mentioned earlier, recovery is dependent on the type of surgery (repair versus partial menisectomy), but most report only needing a couple of days off from work until they are up again. However, further recovery and return to more aggressive activities or physical labor often takes longer, and physical therapy may be beneficial for recovering full function of the knee in the 6-8 weeks following surgery.

Please note that although arthroscopy can effectively treat many problems, you may have some activity limitations even after recovery. A return to intense physical activity should only be done under

Dr. Rocca is Board Certified in Orthopaedic Surgery. Prior to joining The Orthopaedic Insitute, he practiced three years with the United States Navy. Dr. Rocca attended medical school at the University of Pennsylvania and completed his residency in Orthopaedic Surgery at the National Naval Medical Center. He also performed a fellowship in Hyperbaric Medicine at the Naval Undersea Medical Institute. Dr. Rocca practices out of TOI’s Gainesville location.

MESOS








Within Budget




There is hope for healing even after experiencing horrible abuse.
As a young adult, I was sexually assaulted, raped, forced to marry my ex-boyfriend rapist, and subjected to years of mental, emotional, physical, and sexual abuse. My innocence, and that of my infant daughter, was stolen along with my faith in humanity. Because I didn’t immediately tell anyone what happened, my life spiraled downward, propelled by the poison of doubt, guilt, shame, and fear. For years I silently suffered with depression, anxiety, nightmares, flashbacks, fibromyalgia, and the numerous physical, mental, and emotional side effects of severe post-traumatic stress disorder. Thankfully, my spirit chose to soar.
Eventually, I took ownership of my circumstances by quieting my noisy, busy, reactive mind and going within my true self. I did this in a meditative manner to safely review the horrific events I survived, seriously search
for a peaceful way to move forward in life and heal myself. The soulful solution was to forgive myself.
Initially, I wondered how I could heal by forgiving myself, and then the answer became clear. I was raised to forgive others when they hurt me with their words or actions once the situation was resolved. I was told to let go of things; holding on doesn’t do anyone any good.
I applied these life lessons toward forgiving myself. This allowed me to see my role in my life’s events without judgment or fear of judgment. I began to accept the truth of my role and the
choices I made during those circumstances.
Whenever I felt the rush and unease of shame, guilt, and self-doubt during flashbacks to events in my life, I inhaled deeply and consciously forgave myself for the past “mistakes” I made when our lives were threatened.
• My naivety.
• Deciding to be his friend.
• Not reporting the rape to police.
• Taking a shower and going to work instead of going to the hospital immediately upon regaining consciousness.
• Agreeing to his terms.
• Believing his threats.
As I eased into this practice of forgiving myself, the revisiting of past events in my mind became less and less frightening and more rewarding.
I felt great relief while forgiving myself and simultaneously surrendering these events to a higher power for forgiveness. “Let go and let God” was a phrase I often heard my mother say. Now I know how beneficial that mantra truly is. I became peaceful, less frightened, more confident, my overall health improved; life got better, and my belief in human kindness was restored. I treasure
• Not telling anyone about his violent temper, his mistreatment of Desirée and me, and his drug and alcohol addictions.
• Enduring his abusive behavior.

• Staying in a dangerous situation.
• Pretending everything was “normal.”
Forgiveness allows me to heal and be peaceful as I move forward in life. It does not mean what happened is all right. I value the lesson, and I leave the experience behind.Story: Itzabella Katchastarr
this skill, knowing it takes honesty, practice, and a firm conviction to never repeat such incidents.
My memoir, “Because I Didn’t Tell,” is raw. Abuse, betrayal, deceit, and disappointment are powerful experiences I share so readers will:
• Recognize if and when it is happening to them.
• Take action to reclaim their lives.
• Avoid having this happen to them or someone they love.
Trust your intuition—that gut feeling you
Don’t let
get when something doesn’t feel right. See the “red flags” that warn you of danger. Believe what you sense and feel.
I am so proud of those who are finding their courage to tell; every truth matters. Please seek a peaceful resolve for yourself; resist falling into the trauma and drama that revenge brings. Don’t allow the “fall out” to consume your thoughts and steal your bliss. Be peaceful now that you revealed your truth. Some things are God’s jobs.
I released victimhood by accepting that each tragic experience held a valuable lesson for me.

This wisdom empowered me to propel myself to fear-free, faith-filled fulfillment. I am triumphant and free!
“Because I Didn’t Tell” serves to globally encourage all other victims of abuse to speak up about their situation, to seek help and protection, and to release the grip of fear that keeps them silent. It is a safe place for readers to heal through forgiving themselves and gleaning wisdom from woe.
How do you choose to honor your self-worth?
ABOUT THE WRITER → Itzabella Katchastarr is the author of “Because I Didn’t Tell,” published by Balboa Press in July 2017, as well as an inspirational speaker, Reiki master, and founder of Healing House. Stay inspired at becauseididnttell.com.
We cannot change other people. My fear gave him power over me.
this happen to you. Don’t give your power away!










Women have sexu a

experienced sexual harassment and assault throughout history. Those who were targeted received little or no recourse. Predators have acted with impunity for too long. Time’s up, and
Those who we received little or no reco Predators have acted with impun an thank God.
party or a superior requesting sexual favors. You now have better options to report offenders without ruining your life or career.
Many women h cou stop it and could bel if u hea Since news the accusations fi
a tidal wave of female v has emerged to say #MeToo and fina heard is ste few ide para shift so other women don’t ever experience this.
Many women have felt that they couldn’t stop it and couldn’t speak up—or believed if they did speak up, they wouldn’t be heard. Since the news last fall of the accusations against film executive Harvey Weinstein, however, a tidal wave of female voices nally hold predators accountable. Being heard is step one, but it’s only the beginning. Here are a few ideas of what else we can do to continue this positive paradigm
DITCH THE SHAME GAME. How many of us have spent sleepless nights wondering if we could have done something different to prevent an offender’s actions? “What if I hadn’t said hello to him? What if I hadn’t been so nice? What if I hadn’t worn that dress? Maybe the incident wouldn’t have happened.” It’s time to silence this self-loathing. The reality is that the person would have acted that way regardless because that’s who he’s chosen to be: a predator. It has nothing to do with who you are, what you wear, or how you act. If he didn’t act that way towards you, he likely would have picked someone else. This is a pattern of behavior, and it’s on him, not you.


Now, might there have been some red flags you see more clearly in retrospect? Sure, but those are your learning opportunities. In the future, you’ll see the red flags from a mile away and can respond proactively to take control of the situation. For example, if you find yourself in a compromising or threatening scenario, here are a few ways you can get out of it quickly:
RE CO GN IZ E PR ED AT OR S’ M .O typicall and yo thou choices to avoid such and these choices ca calculated rather than your as much as you can. For accompany a co-worker to his hotel room on a trip. Sugge calling the shots.
Predators typically have a plan of attack. They want to get you alone and put you in a situation where you are vulnerable. We can make thoughtful choices to avoid such situations, and these choices can be calculated rather than fear-based. Take charge of your space as much as you can. For example, don’t accompany a male co-worker to his hotel room on a business trip. Suggest a public meeting place. Create or reframe situations so you are
• Pretend to throw up as if you suddenly have a bout of food poisoning and run to the bathroom.
• Belch or pass gas—seriously! Then run out of the room as if purely due assaulted.
• ant phone call, forgot your keys in the car, or forgot to pick up your child from
RE CO GN IZ E YO UR P OW ER . The fight sexu shown us W behavi

More than ever before in women no have to tolerate a butt at the
ght against sexual harassment continues, but if the #MeToo movement has shown us anything it’s that our voices are powerful. We as a people aren’t willing to put up with offender behavior anymore. More than ever before in history, women no longer have to tolerate a coworker grabbing their butt at the holiday
Women are standing up and standing together to say that harassment behaviors are no longer acceptable and that we no longer are willing to overlook them—and the public is standing with us. Create strategies for your safety, but use these from a place of power rather than fear if you can. Finally, the world has your back and it is time for all of us to soar to heights some tried to prevent us from reaching.
International bestselling author Ava Miles calls herself a divine rock star, something she believes everyone is deep down. Her new book series, “The Goddess Guides to Being a Woman,” invites female readers to reimagine what it means to be a modern woman on our own terms.
What if you develop sudden onset severe back pain, more unbearable than you ever imagined? If your pain is new or feels different from the chronic back pain you may already be experiencingwhich is currently being treated with exercise, pain medicines, and injections - it is recommended that you should visit your doctor or urgent care center immediately, because you may have a vertebral compression fracture in your spine. If you are able to pinpoint your pain with the touch of a finger to a specific vertebra, it is important to act quickly or it may become too late to repair it.
What is a compression fracture and why is time of the essence? A compression fracture is when a vertebrae cracks and becomes compressed or somewhat flatter than it was before the fracture. Think of an elderly person with a hunchback or curved spine. A hunchback, medically known as kyphosis, is often caused when the bones become frail and brittle from osteoporosis (loss of bone density) and the vertebrae begin to fracture one by one. As these vertebrae fracture, they become misshapen. The rectangular vertebrae become triangular or wedge-shaped, eventually creating a curve in the spine.
Once a vertebrae fractures it will heal on its own, but it takes several weeks or even months to do so, during which time the pain is often unbearable. In the past, doctors would put patients in a brace and prescribe medication, often in the form of narcotics, to help ease this pain. When

the compressed vertebrae heals on its own, it heals in its compressed state or compresses even further, sometimes flattening completely and reducing the height of the individual. At this point, nothing can be done to restore its integrity since the bone has hardened or scarred, making it impossible to fix.
Compression fractures can also be caused by an impact such as a fall, or from cancer which has metastasized to the spine. Unfortunately for many, a compression fracture can be a first indication of cancer, so do not ignore this sign - get a consultation immediately. If you had an X-ray, CT, or MRI indicating a compression fracture, insist that your physician acts quickly to refer you to a specialist for a kyphoplasty or vertebroplasty.
With a procedure called kyphoplasty, kyphosis can be a thing of the past! A Kyphoplasty procedure can stop pain instantly in over 95% of patients, as well as prevent further collapse of the vertebrae.
During the procedure, the physician uses image-guidance in the form of a C-ARM (which is a live X-ray) to obtain access and inject a plastic cement into the vertebrae to restore the integrity of the bone, often stopping pain completely and preventing further damage. The procedure is performed under conscious sedation and takes approximately 30 minutes under the expertise of an experienced specialist, such as an Interventional Radiologist. Although other specialists are now performing this procedure, an Interventional Radiologist should be your first choice, since they pioneered this procedure, and any imageguided procedure should always require a person trained in radiation safety.
Interventional Radiologists believe that limiting X-ray exposure to patients is crucial, which is something 352.261.5502 |
often overlooked by other physicians. An Interventional Radiologist such as Dr. Mark Jacobson, uses a mere fraction of the typical radiation exposure used by other specialists, including other radiologists. An Interventional Radiologist also uses minimally invasive surgical techniques with the least number of punctures (usually one per vertebra) and the smallest needles possible, thereby enhancing safety and reducing healing and recovery times.
In the case where a compression fracture is caused by a cancerous lesion, an Interventional Radiologist can also biopsy the bone and perform a radiofrequency ablation to alleviate pain prior to the kyphoplasty (this is not a replacement for, but complimentary to radiation treatments, because if a patient is in less pain, the treatments can be tolerated better).
This is why it is imperative to understand that not just anyone should perform your kyphoplasty, but someone trained in identifying the difference between a simple fracture caused by osteoporosis, and a fracture caused from a possible cancerous lesion. A trained expert will be able to offer to you the best options available.

ABOUT DR. MARK JACOBSON Dr. Jacobson has performed nearly 1000 kyphoplasties in his Lady Lake office and is the “go-to provider” for this procedure, not only because of the number of procedures performed and numerous happy patients, but also because of his participation in the research of radio-frequency ablation of cancerous spine tumors. Local, as well as out of town physicians entrust Medical Imaging & Therapeutics for treatment of their patients’ spine fractures. MIT is affiliated with the University of Florida College of Medicine as an Interventional Radiology training center for physicians in the interventional radiology residency and fellowship program.

Interventional Radiology procedures performed in a nurturing, safe, state-certified outpatient center





Government programs may create additional financial risks for hospitals.
Story: Joy Stephenson-LawsAt least 37 states have laws on the books allowing involuntary detention and treatment of substance abusers who have not committed a crime. In some states, the legal bar for such detention is high, requiring that the person threaten to harm themselves or another person. In other instances, a police officer may detain a person if the officer has “reasonable cause” to believe the person is in need of involuntary treatment. The amount of time the person may be held also varies from a few days to up to 90 days. Supporters of these statutes argue they are a necessary response to the rise in the number of Americans dying from both street and prescription drugs.
At the same time, an increasing number of states now require some form of drug testing for public assistance recipients. At least 15 states have passed legislation requiring drug testing or screening for public assistance applicants or recipients, according to the National Conference of State Legislatures. At least another 20 proposed bills that are in some stage of the legislative process. Some of these apply to all applicants while others require such testing only if there is a reason to believe the applicant is engaging in illegal drug activity or has a substance abuse disorder. As would be expected with these types of laws, many are facing some sort of court challenge, either on federal or state level.

These laws all have in common a desire to save public funds and motivate those with substance abuse issues to go through some form of rehabilitation. Measuring how successful these programs are at achieving either or both of
these objectives depends to a great degree on how they work, who is doing the measuring, and how “success” is defined.
Even if the politics of these programs are open for debate, the magnitude of the problem—and its impact on families, communities, and the health-care system— cannot be denied.
Recent estimates are at least 8 percent of the U.S. population suffered from substance abuse at one point or another in their lives. Looking at the population of the United States on some sort of public assistance—which is estimated at 20 percent and expanding—most studies show this group does not necessarily have substance use or abuse levels higher than the general population. However, there are others that project up to 20 percent of these recipients used an illegal substance in the previous year.
These numbers are significant. Also significant is the impact of requiring even a small percentage of these individuals to participate in outpatient or inpatient treatment programs have on the health-care system.
About 14,500 specialized drug treatment facilities provide a variety of services to people with substance abuse disorders, according to the National Institutes of Health. Unfortunately, this capacity is not projected to be sufficient for the existing demand since, by some reports, there already aren’t enough treatment beds for those who want them. In fact, some states have waiting lists for treatment. Add to this group those compelled into treatment and the lack of capacity becomes even more critical.

The anticipated demand created by involuntary treatment has the potential to make most health-care providers’ precarious financial situations even worse if they are required by state authorities to provide services to these individuals.
Hospital providers need to carefully monitor and manage three key areas:
DEMAND WILL STRAIN ALREADY STRAPPED RESOURCES. Typically, hospital reimbursement for these types of services is low and made only after a hospital expends huge resources to obtain monies from government and private payers. Most hospitals already operate on razor-thin margins of less than 3 percent, so increases in expenses not reimbursed could wreak havoc on a provider’s balance sheet. Furthermore, while there is variation across facility type, the average hospital bed occupancy rate is approximately 67 percent. This leaves little room for reallocating inpatient beds to inpatient rehabilitation nor to dedicating additional space to outpatient care.
UNCERTAINTY OVER WHO PAYS. Given the uncertainty of the Medicaid program, which, according to the Washington Post, is the “the largest source of funding for behavioral health treatment, like addiction recovery and substance abuse prevention,” any changes to the mental health and substance abuse requirements could greatly impact providers in general, especially if they must provide substance abuse rehabilitation services to a growing population.
and psychiatrists. All these fields play a role in substance abuse rehabilitation and counseling. As a result, achieving appropriate staffing levels may create greater demand for these professions. Until that demand is readily met, salaries may increase disproportionately, creating additional drag on sustainability.
The programs to force people into rehabilitation do not necessarily mean financial “doom and gloom” for providers. A prudent provider can take steps to address the financial and operating challenges posed by the potential increase in demand for substance abuse programs. These include utilizing financial forecasting that appropriately accounts for costs associated with increasing inpatient and outpatient substance abuse rehab and counseling capacity.
Providers might consider negotiating reimbursement rates that result in more reasonable compensation for the medically necessary services required by this type of treatment. For example, they can negotiate payments to reduce the administrative burdens caused by nonsensical denials and dilatory payer tactics. These types of payments include a percentage of billed charges and per diem amounts. Additionally, any agreement to accept these patients should include an irrefutable presumption of medical necessity when they are involuntarily admitted. Without these safeguards, hospital providers increase the risks of rendering uncompensated services.
ABOUT THE WRITER → Joy Stephenson-Laws is founding and managing partner of Stephenson, Acquisto, and Colman (sacfirm.com), a leader in health-care reimbursement law. To date, the firm has recovered more than $1 billion in unreimbursed, denied, or disputed medical claims. In this role, she leads a diverse team of attorneys, doctors, nurses, technology professionals, and health-care provider operations specialists.

Dr. Rondon received his Medical Degree from Central University of Venezuela in 2000. He completed his general surgery residency from LKH-Graz Austria, and St John Hospital and Medical Center Detroit, Michigan. His internship was completed at Graduate Hospital, Philadelphia, PA. He received his Fellowship from the University of Texas Southwestern Medical Center, in minimally invasive and bariatic surgery.
He began practice by providing general surgery and advanced laparoscopic surgery services to the undersized area of the Appalachian region for two hospitals in the area of Kentucky and West Virginia.He provided care as a emergency department physician and Chief of Surgery for Tug Valley ARH Regional Medical Center in South Williamson, Kentucky.
He and his family relocated to Florida where he began practicing in February 2018 as a Board Certified General Surgeon with Mid-Florida Surgical Associates. The group provides surgical care for the communities of Lake, Orange and Sumter counties. The group is proud to announce Dr.Rondon as a member of their staff.


Almost daily there are references to mental health issues in the news. According to the National Institute of Mental Health, mental illnesses are common in the United States. One in six U.S. adults lives with a mental illness (44.7 million in 2016).
In Leesburg, there is now a safe, comfortable place to receive the help that may be needed—the Senior Behavioral Health Center at Leesburg Regional Medical Center.

“We offer short-term care for behavioral health issues and review each patient on a case-by-case basis,” says Christopher Adams, an advanced registered nurse practitioner and director of the center. “We will go out into the community to perform assessments, and our goal is compassion and education. We want to get patients back to their lives in good health.”
Adil A. Mohammed, MD, is the board-certified psychiatrist who oversees patient treatment, including medication management, group and individual psychotherapy, and recreational therapy. He received his medical degree from Saint Petersburg State Medical Academy, completed his internship at Mount Sinai School of Medicine Program in New York City, and his residency training was completed at
Temple University Hospital in Philadelphia.
“The level of psychiatric care couldn’t be much higher than it is at the Senior Behavioral Center,” Dr. Mohammed says. “You don’t even have to go through the hospital to be admitted. If you or a family member knows there is a problem that needs immediate attention, you can call the behavioral unit directly, and the staff will help you with admittance.”
The Leesburg Regional Medical Center (LRMC) Senior Behavioral Health Center is a 21-bed specialty unit that offers inpatient treatment for mature adults suffering from depression, anxiety and suicidal thoughts. Individual, group and family therapy is provided by a team of social
workers, activity therapists, physical therapists and is led by physicians. Once a patient is admitted, they will be seen daily by a psychiatrist. The unit does not handle cases that involve involuntary commitment. Patients must be able and willing to voluntarily sign themselves in for treatment.
Family members may be the first to realize a problem is becoming acute enough to require hospitalization. Depression often results in changes in sleep patterns or appetite (not eating or stress eating). Psychosis may include auditory or visual hallucinations, and paranoia, which leads the patient to believe someone wants to harm them.
If you’re caring for a parent who begins having delusions (fixed false beliefs
about themselves, others, or their environment), it’s difficult to help them. If the patient is yelling and cursing, these aggressive behaviors can signal problems too. It’s also difficult to help someone who is taking their medication incorrectly or refusing to take it.
All of these symptoms can mean it’s time to take measures and seek the help a caregiver cannot provide. Getting that help at the Senior Behavioral Health Center is not only good for the patient, it aids the caregiver. There are few things worse than the feeling of knowing you’ve done all you can do and have nowhere to turn.
“The patient must be competent and able to sign themselves in for admittance,” Christopher says. “They want to get better, and we can teach them how to do that.
We’ve found there is a big need in Leesburg and The Villages® for follow-up care, day treatment, and partial hospitalization.”
Once the patient has completed treatment at the Senior Behavioral Health Center, the staff works to continue treatment once they leave. They may continue to see Dr. Mohammed or another psychiatrist, so they can follow through on their treatment plan.

“Everything is very confidential. Nothing is revealed even to the hospital,” Christopher says. “No one can be told a patient is here.”
However, that does not mean the patient is completely cut off from friends and family. The center has visiting hours twice daily, and the staff encourages family to interact with the patient and even conduct family therapy as indicated.
The center, formerly an inpatient rehabilitation
hospital, has been beautifully and meticulously renovated. There is a kitchenette that always has healthy snacks along with a full washer and dryer. Everything in the center was designed for the safety and comfort of patients.
“We are committed to every detail of our patients’ healing experience, even down to providing blanket warmers, which patients often find very comforting,”
Christopher says. “Clinically, in addition to Dr. Mohamed, we have a whole treatment team that includes a physician, registered nurse, social worker, activity therapist, and me.”
Michael Smith, who is a registered social worker, says he finds his work at the center very rewarding. “What I like is helping other people, and the team is very supportive of one another, which makes a difference.”
With the team meeting and discussing each patient’s needs, it means patients receive treatment specifically for their problems. “I think we try to treat their conditions with different treatment modalities,” Dr. Mohammed says. “Some conditions have a great prognosis, but whatever it is, we try to be realistic and educate them about their prognosis
and be compassionate at the same time.”
Many times, older adults may have changes in behavior and emotions that require the specialized treatment offered at the Senior Behavioral Center. With the combination of medical treatment, rehabilitative, and physical care under the supervision of those who specialize in the treatment and therapy needed for aging, these individuals can be restored and begin to live a full life again.

700 N. Palmetto Street Leesburg, FL 34748
(located on the 3rd floor) LeesburgRegional.org
We will go out into the community to perform assessments, and our goal is compassion and education.
We want to get patients back to their lives in good health.
— Christopher Adams










Keep your world open to every possibility, with help from Lake Eye.
From capturing the radiance of a grandchild’s smile to topping your best golf score, you depend on your eyes for nearly everything you do – and your eyes depend on you to keep them healthy and ready for new adventures.

Lake Eye has everything you need for general and restorative eye care, including comprehensive eye exams from Board Certified ophthalmologists, the most advanced, high-tech treatments for cataracts, macular degeneration and other issues, and a full-service optical department for the latest fashion eyewear and specialty lenses. It’s everything you need, all in one place, from caring professionals who have been serving the area with pride for 40 years.

My father may no longer be invincible, but he’ll never be invisible.
Story: James CombsIn her prime, your mom was a real-life Energizer Bunny, hopping from one task to another without breaking a sweat. Now, she walks with a cane. In his younger years, your Herculean-like father could split wood like a lumberjack. Today, he rarely ventures outside due to unrelenting back pain.
Accepting that your parents are no longer invincible is frightening. I never reached this state of acceptance until the age of 42. It happened in March when an oncologist uttered horrifying words to my dad:
“You have lung cancer.”
There was no reason for this. He quit smoking more than 30 years ago. He and my mom regularly ride bicycles at various trails throughout Florida. There was no family history of lung cancer. He never vacationed near Chernobyl.
For me, the horrific news came with a harsh dose of reality. The superhero who taught me how play basketball and shoot a gun, the idol who escaped the poverty of Appalachia to make something of himself, the indestructible man who at age 70 seemed to be in really good health suddenly was… Mortal?
It was a bitter pill to swallow. Thoughts I’ve never had before raced through my head. If I lost a parent, I’d lose part of myself. Our immediate family would never be whole again. Staring at his empty seat would completely take the joy out of Thanksgiving and Christmas.
Sure, I have friends who have lost parents. In fact, I’ve even lost some friends. However, it took my dad being diagnosed with a horrible disease to truly grasp the fragility of life and to come to the realization that he is indeed vulnerable.
Now that I’ve had time to ponder this reality, I’ve accepted that it’s not such a bad thing. In fact, knowing he’s not invincible is one of the traits I now most admire about my dad. I know now that my dad has fears—the same fears that sometimes nag at me. I realize that he is a normal person who, like me, is capable of getting hurt and needing help. Most importantly, I realize my dad is more real and closer to me than I could have ever imagined.
Not because he’s a superhero.
Because he’s human.
Over forty years ago, Dr. Saroj Tampira followed his heart and embarked upon a career journey that finally led him to the Village Heart and Vein Center. His arrival completed the vision of the Center founder Dr. Georg Couturier to provide total care for patients with heart and/or vascular diseases. Dr.Tampira’s journey literally began with a medical degree earned at Madihol University—the number one university in Thailand. Internship and residency at the University
of Louisville Hospital followed. In 1978 he completed a Fellowship with Tulane University in New Orleans. His specialty is interventional cardiology—clearing and repairing blocked veins and arteries—and he is one of a very select group of talented cardiologists skilled enough to pursue blockages below the knee in individuals who need help.Today, many patients and procedures later, all of us in Central Florida are fortunate indeed that his heart and his journey brought him here.

