
25 minute read
CMS Finalizes Regulatory Changes and Updates Physician Payment System
Each year, the Centers for Medicare & Medicaid Services (CMS) issues regulations that impact the reimbursement of physicians. On November 2, 2021, CMS finalized a rule updating payment policies and rates for physicians paid under the Medicare Physician Fee Schedule in 2022. The final rule illustrates the importance of the AAN’s regulatory advocacy efforts on behalf of neurologists and their patients. CMS expects payments across the specialty of neurology to stay at current levels in 2022, with variations depending on the individual provider’s practice. However, all specialties are also potentially facing a 3.7-percent reduction in the conversion factor used to formulate payments under the Medicare Physician Fee Schedule. The AAN is working with physician associations from across the house of medicine to fight against these potential cuts, which recently resulted in having 247 members of the US House of Representatives sign a letter urging congressional leaders to act on this issue before the end of the year.
Evaluation and Management (E/M) Visits
Like in previous years, CMS continues its ongoing review of E/M code sets. The AAN remains highly supportive of the new coding and payment structure implemented on January 1, 2021, and lauds the agency for moving forward with implementation. For 2022, the agency is refining several policies to align with the revised E/M visit codes guidelines which took effect January 1, 2021. Four new principal care management codes will be available for neurologists to use in 2022, recognizing the comprehensive services provided for a single high-risk disease. CMS is refining its policies for split or shared E/M visits to reflect the evolving role of advanced practice providers (APP) and changes to the practice of medicine. For 2022, CMS defines split or shared E/M visits as those provided in the facility setting by a physician and an APP in the same group and expands to include new patient encounters. CMS has decided on a new, time-based definition of the “substantive portion” of a visit that must be furnished by the physician to bill split (shared), but this change will not be implemented until 2023, as the AAN requested.
Telehealth Regulations
As expected, the final rule codified that the telehealth services added to the Medicare telehealth services list under the temporary “category 3” during the COVID-19 public health emergency (PHE) be removed from the list after the PHE ends. These services will have to be submitted to be made permanent under either category 1 or 2. However, CMS acknowledges that there has not been sufficient time to collect the utilization data needed on these telehealth services for submission and approval. Therefore, CMS will retain all telehealth services added due to the PHE through calendar year 2023 so that they can be analyzed and submitted for the 2023 and 2024 fee schedules for permanent inclusion. This is a welcome decision by CMS as it gives providers a clear timeframe during which they can continue to use these temporarily approved telehealth services and allows for the much-needed study of these services for their potential permanent inclusion. The AAN was glad to see that CMS accepted our recommendation that the requirement for an in-person visit every six months to be reimbursed for telehealth services be raised to a 12-month period. This will relieve an undue obstacle to the continuation of care provided via telehealth. CMS also finalized its proposal to allow another physician in the same specialty and practice to fulfill this requirement should the original physician be unavailable, as the AAN requested. CMS has finalized the change to the requirements of telehealth provision to permanently allow audio-only telehealth services for the diagnosis, evaluation, or treatment of mental health disorders when the patient’s home is the originating site. Only providers who are set up to provide full audio/visual telehealth services can make use of audio-only services; this is to ensure that it is the patient’s aversion or inability to use audio/ visual services that leads to an audio-only visit. The AAN was supportive of this change as it represents a logical adjustment of regulation to match the incorporation of technology in the provision of care.
Appropriate Use Criteria
CMS will delay the beginning of the payment penalty phase of the Appropriate Use Criteria (AUC) program to no sooner than January 1, 2023, or the January 1 that follows the declared end of the COVID-19 Public Health Emergency. The flexibilities offered by CMS are intended to consider the impact
of COVID-19 on providers and their beneficiaries. The current payment penalty phase of the AUC program was to begin at the start of 2022. This is a welcomed change. We continue to advocate for modifications to the AUC program recognizing its potential burden on neurologists.
Quality Payment Program
The rule includes finalized policies related to the Quality Payment Program (QPP), which includes the Merit-based Incentive Payment System (MIPS), Advanced Alternative Payment Model (APM), and MIPS Value Pathways (MVPs). For the MIPS track, CMS finalized increasing the 2022 performance threshold to 75 points from 60 points, as well as the exceptional performance bonus to 89 points from 85 points. For the Quality and Cost components, CMS finalized decreasing the weight of the MIPS Quality component to 30 percent from 40 percent and increasing the weight of the MIPS Cost component to 30 percent from 20 percent. For Improvement Activities, CMS finalized seven new activities, including three that are dedicated to promoting health equity. For Promoting Interoperability, small practices are now automatically exempt from the component, and it will be reweighted to Quality and Improvement Activities. Practice Email Ad—Half Page Horizontal> AN Placed in AANnews 8.25 x 5.25 +0.125 bleed, 4C“How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the dead line for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” “Is there a code for…?” “Can the payer…?” “What form should I…?” “Who can tell me…?” “What is the best…?” “How do I…?” “When is the deadline for...?” Got practice management questions? Get answers in one business day. Just ask. practice@aan.com CMS finalized its policy awarding doubled bonus point opportunities to clinicians caring for complex patients during
the COVID-19 public health emergency, while also finalizing the removal of bonus point opportunities for reporting additional outcome and high priority measures. For the APM track, CMS finalized extending the CMS Web Interface reporting option through 2024, thus delaying the plan to sunset this reporting mechanism by two years. MIPS Value Pathway The rule finalized seven MIPS Value Pathways (MVPs) or sets of defined measures and activities related to a specialty or condition, beginning in 2023. Included in the set is an MVP titled "Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes" which features measures and activities related to caring for stroke patients and may be relevant to some neurologists. The AAN actively engaged with CMS during the development process at CMS’s invitation and provided extensive comments on the proposed stroke MVP. In addition to foundational population health measures and Promoting Interoperability measures, the stroke MVP features nine quality measures and nine improvement activities to choose from and one cost measure relevant to stroke care. In the rule, CMS also finalized policies on reporting and scoring expectations, which closely align with current MIPS policies. The AAN will develop resources for neurologists interested in transitioning to MVPs for the 2023 performance year.
Why Is AAN Advocacy Important to You?
Another energetic, intense, and successful year of AAN advocacy is coming to a close. Watch for a roundup of advocacy highlights in the January 2022 issue of AANnews and draw inspiration from these colleagues who have committed themselves to advocating for neurology.
First: If you don’t stand for something, you’ll fall for anything. Second: To be an advocate is to have courage, independence, and passion for the things that matter. AAN advocacy allows us to educate decision makers about the impact of their public policy decisions on the people and communities that we represent and care about.” ―Ann H. Tilton, MD, FAAN
It protects the future of neurology. If one in six of the world's population suffers from a neurologic disorder, we cannot afford to be silent.” ―Wayne E. Anderson, DO, FAHS, FAAN, AAN
Board of Directors
We need new treatments for the disorders and conditions we treat. We need more research for better understanding of the disorders and conditions we see. We need to speak on behalf of our patients who as a result of their diseases and disorders are physically unable to meet the policymakers or, if they can, unable to speak effectively. We need innovative health care delivery and reimbursement models in order to optimize and sustain the care we provide. In short...advocacy is brain.” ―Samir Belagaje, MD, FAAN
Advocacy is leaving our health care system better than we found it! Seeing patients every day, one can’t help but imagine the ways our health care delivery system can be improved. Advocacy is how we make those changes happen.” ―Jason L. Crowell, MD
AAN advocacy is important to me because it allows me to make a difference for my patients and colleagues on a larger scale than I'm able to on my own or in my current position. When lawmakers are uninformed on what neurology is and how our patients are affected by their disease, we cannot expect them to make health laws that provide significant impact to our daily lives.” ―Tyler J. Allison, MD
My advocacy is inspired by patients and powered by the AAN.” ―Gorazd B. Stokin, MD, PhD, FAAN
The amount of behind-the-scenes work that the AAN advocacy group does is remarkable. It is important to me because the effects of AAN advocacy really have tangible benefits to patients with neurological disease and neurologists, more so than most know. Initiatives have ranged from protecting physician and patient time, helping prescription drug coverage, expanding access to telehealth, and so much more. It's been a pleasure and privilege contributing even a tiny bit to the effort.” ―Ilya Bragin, MD
L to R: Ilya Bragin, MD, and Umer Najib, MD, at the 2019 Palatucci Advocacy Leadership Forum.

L to R: Sylvia Josephy, MD; Tyler J. Allison, MD; Kara Stavros, MD; Aileen Antonio, MD, at the 2019 Palatucci Advocacy Leadership Forum. L to R: Jason L. Crowell, MD; Belinda A. Savage-Edwards, MD, FAAN; William A. Kilgo, MD, at the 2019 Neurology on the Hill.

Capitol Hill Report
Capitol Hill Report presents regular updates on legislative and regulatory actions and how the Academy ensures that the voice of neurology is heard on Capitol Hill. It is emailed to US members twice monthly and is posted at AAN.com/view/HillReport. Below are some recent highlights.
Medicare Cliff: Will Congress Save Us—Or Push Us Over?
Latest Advocacy News
The AAN sent a letter endorsing the Bringing Regulatory
Advances into Neuroscience (BRAIN) Act (H.R. 5435), which would establish a Neuroscience Center of
Excellence at the FDA. A majority of the House of Representatives (227 members) have now cosponsored the Improving
Seniors’ Timely Access to Care Act (H.R. 3173), a priority bill supported by the AAN to address prior authorization burden. Sens. Roger Marshall (R-KS),
Kyrsten Sinema (D-AZ), and John Thune (R-SD) have also recently introduced a Senate version of the bill. This overwhelming bipartisan and bicameral support makes a bold statement to congressional leadership that this bill must move this year. The AAN joined a letter led by the AMA urging the administration to address unfair business practices with respect to electronic payments in health care. The AAN joined a letter with other medical specialties to the House and Senate Armed Services Committees opposing a proposed reduction in military medical billets by 12,801 positions and urging the committees to prohibit such reductions for a year and require a GAO study before any reductions move forward. Issue in Focus
Lawmakers Highlight Need to Avert Medicare Cliff While Congress has become more partisan over the years, many of the AAN’s top priorities unite Congress rather than divide it. The most recent example was a letter by US Reps. Ami Bera, MD (D-CA) and Larry Bucshon, MD (R-IN), expressing concern and urging action to address the upcoming "Medicare Cliff," which is scheduled to reduce physician reimbursements by 9.75 percent on January 1 without congressional intervention. With the support of the AAN’s advocacy efforts, their letter garnered 247 signors, a majority the House of Representatives, a truly amazing feat. This looming cut is the result of three policies created by Congress, which are discussed in more detail at AAN.quorum.us/campaign/36023/. The AAN, working in collaboration with the entire House of Medicine, have urged Congress to avert the Medicare Cliff as soon as possible. AAN staff are discussing this issue with policy makers at every opportunity and hundreds of Academy members raised this issue during congressional office visits during Neurology on the Hill and the recent AAN Legislative Summit. The trillion-dollar reconciliation legislation being debated by Democrats in Congress does not currently include a resolution to this issue, which means the next opportunity to fix this will likely be in December as part of a large year-end bill containing numerous provisions. We need to keep the pressure on Congress to address this issue, which will have disastrous consequences if not averted. Help us keep the pressure on Congress—urge your lawmakers to prioritize this issue using the AAN’s Advocacy Action Center.
Need Year-end CME? Explore AAN Online Education Opportunities!
Only AAN members have free and discounted access to a variety of exclusive online CME and self-assessment resources. Browse all the convenient programs and get started fulfilling your requirements today at AAN.com/learn.
Free with Membership*
Neurology Question of the Day Earn up to 29 self-assessment CME per year by answering short daily questions on topics from multiple neurology subspecialties.
Earn up to 8 self-assessment CME per exam with content designed to help neurologists meet the American Board of Psychiatry and Neurology self-assessment and lifelong learning component (part 2) for Continuing Certification.
Learn about relevant clinical and practice topics while earning a range of CME credits with the AAN’s convenient suite of exclusive online education courses.
The most widely read and highly cited peer-reviewed neurology journal Discounted with Membership
2021 AAN Conferences—Available On Demand
Listen to on-demand recordings of any or all the AAN’s 2021 conferences including: Annual Meeting On Demand—up to 68 CME Sports Concussion Conference On Demand— up to 10.25 CME Fall Conference On Demand—offering up to 42.5 CME (available late December 2021) APP Neurology Education Series—up to 12 CME
READY Preparing for the neurology boards? Up for recertification? Looking for a solid foundational knowledge in neurology? Get ready with these convenient online courses. Choose from the Board Prep Edition (no CME offered), Continuing Certification (Second Edition) (up to 15 self-assessment CME), and new Advanced Practice Provider Edition (up to 8 self-assessment CME).
Earn CME credits by reading two editor-selected articles per week and completing corresponding online exams. Earn 0.5 CME credits per podcast (up to 24 CME per year).
*Free access may vary by membership type Earn up to 20 AMA PRA Category 1 Credits™ toward selfassessment CME with each issue of the AAN’s official CME journal. Supplement with Continuum Audio to listen to conversations with Continuum authors and earn CME.
BUNDLE AND SAVE20%
In celebration of achieving 1,900 APP members, the AAN is offering a limited-time 20-percent discount until December 22, 2021, when you bundle two unique CME and onboarding opportunities for APPs: APP Neurology Education
Series and NeuroReady: APP Edition. Visit the
Online Learning Center at AAN.com/learn to learn more and purchase.
Latest on Behavioral Neurology and Psychiatry in December Continuum
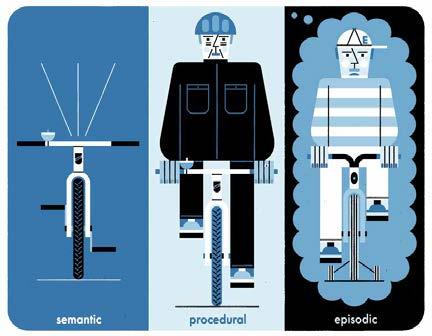
The current issue of Continuum: Lifelong Learning in Neurology® provides neurologists with new insights on behavioral neurology and psychiatry. Guest Editor Michael S. Jaffee, MD, FAAN, said, “The articles in this issue illustrate how many of the signs and symptoms of behavioral neurology and psychiatry can be part of the presentation of neurological disorders from a variety of neurology subspecialties as well as the importance of assuring these issues are included in a management plan. These articles include discussions of new and emerging treatments using innovative mechanisms and modalities.” Content for this issue includes: Clinical Approach to Cognitive and Neurobehavioral
Symptoms / Meredith Wicklund, MD, FAAN Language and Aphasias / Stephen E. Nadeau, MD Memory Dysfunction / Roberto Fernandez-Romero, MD,
MPH, PhD; D. Malcolm Spica, PhD Executive Dysfunction and the Prefrontal Cortex /
David T. Jones, MD; Jonathan Graff-Radford, MD Upper Limb Apraxia / Kenneth M. Heilman, MD, FAAN Spatial Neglect and Anosognosia After Right Brain Stroke /
A.M. Barrett, MD, FAAN, FANA, FASNR Behavioral and Cognitive Aspects of Concussion /
Russell M. Bauer, MD; Michael S. Jaffee, MD, FAAN Cognitive Rehabilitation / Lindsey Kirsch-Darrow, PhD;
Jack W. Tsao, MD, DPhil, FAAN Psychosis / Uma Suryadevara, MD; Parunyou Julayanont,
MD Mood Disorders / Shae Datta, MD; Uma Suryadevara, MD;
Josepha Cheong, MD Posttraumatic Stress Disorder and Anxiety-Related
Conditions / John B. Williamson, PhD; Michael S. Jaffee,
MD, FAAN; Ricardo E. Jorge, MD Obsessive-Compulsive Disorders / Carol Mathews, MD Interprofessional Internet Consultations: The Potential
Benefits and Perils of eConsults / Joseph S. Kass, MD, JD,
FAAN; Rachel V. Rose, JD, MBA The Transformation of Documenting and Coding: Evaluation and Management Codes for Outpatient Neurology Services / Raissa Villanueva, MD, MPH, FAAN; Neil A. Busis, MD, FAAN; Bruce H. Cohen, MD, FAAN; Luana Ciccarelli, CPC, CRC Twilight and Me: A Soliloquy / Daniel Alejandro Drubach, MD, FAAN The issue includes a postreading self-assessment and test with the opportunity to earn up to 20 AMA PRA Category 1 Credits™ toward Self-assessment CME. AAN members pay only $399 per year for a subscription to Continuum® and Continuum® Audio. Subscribe now by contacting Wolters Kluwer at (800) 361-0633 or (301) 223-2300 (international) or visit shop.lww.com/continuum. AAN Junior members who are transitioning to neurologist memberships are eligible to receive a 60-percent discount on the already low member rate for the Continuum and Continuum Audio subscription.
Jaffee DECEMBER 2021 VOL. 27 NO. 6
Behavioral Neurology and Psychiatry
EDITOR-IN-CHIEF: STEVEN L. LEWIS, MD, FAAN GUEST EDITOR: NAME TEEKAY, MD
Transforming Leaders Program Graduates Transform Their Careers, Selves
The AAN’s Transforming Leaders Program (TLP) was created specifically for innovative, mid-and senior career leaders with the advanced knowledge and skills and aspirations to transform their practice community and field of neurology. No other program in the country matches its caliber of training, which incorporates executive-level coaching, mentoring, and a fully customized intensive leadership development program. Graduates are quick to praise the program’s truly transformative influence on their careers through maximizing of talent, minimizing weakness, and honing conflict resolution and mindfulness in decision-making—90 percent stating it increased their confidence in understanding, analyzing, and solving problems, and 100 percent stating they learned strategies for working better in teams. 2019 TLP graduate Thabele (Bay) Leslie-Mazwi, MD, and 2017 graduate Barbara C. Jobst, MD, FAAN, are no exceptions—Jobst having been recently named the chair of the Department of Neurology at Geisel School at Dartmouth and Neurology Service Line leader at Dartmouth-Hitchcock Health, and Leslie-Mazwi recently named the chair of the Department of Neurology at the University of Washington.
Leslie-Mazwi
Can you explain a specific skill you learned that you feel has successfully contributed to your career since participating in the TLP program? “I think it's impossible to point to one single and isolated skill that has been instrumental from my TLP experience. We learned a wide range of skills, and I find I apply variations of them daily. “However, one of the key takeaways for me was a different conceptualization of what leadership is. Viewing leadership as a learned skill that we practice and refine (as opposed to an intrinsic talent) makes leadership feel remarkably accessible to everyone. We are all leaders in our daily lives in some form. It might be within our families or friendship circles, within our divisions, within our departments, or at a larger regional or national level. The TLP brought focus to all the various facets of leadership, from developing a vision to inclusivity to managing people and change to connecting, and more. I found it a truly transformational year.” How you were able to apply some of that knowledge and skills, and what were the outcomes? “I found that the skills that I learned during the program equipped me to influence through leadership the change I hope to see around me, based on my defined priorities. This took several forms and occurred at various levels. One example was working on the adaptation of our regional triage response for stroke in the northeast US to the threat posed by the first surge of COVID-19. However, beyond the direct application of theory and techniques, the program gave me the perspective to explore opportunities that I otherwise might not have considered or pursued. While I have always been eager to positively impact the world around me and the field of neurology, I felt increasingly empowered to do so as a result of my TLP experience and the years that followed it. “Most recently, I assumed the position of chair of the department of neurology at the University of Washington in Seattle. The department is remarkably strong and deep with an extraordinarily accomplished faculty.. We serve a population that encompasses all of Washington state and the neighboring states—Idaho, Montana, Wyoming, and Alaska—too; in total, 27 percent of the US landmass. It is an incredible responsibility. I am so excited to see where we take the department together during this historical time of tremendous growth and change in neurology.”
Jobst
Can you explain a specific skill you learned that you feel has successfully contributed to your career since participating in the TLP program? “The TLP was instrumental to acquire skills about project management and how to advance initiatives within the neurologic community. Through TLP I became motivated and focused on advancing the self-management institute I founded: The HOBSCOTCH Institute. HOBSCOTCH stands for Home-based Self-management and Cognitive Training Changes Lives and is a unique behavioral program that helps adults with epilepsy who have self-identified memory or thinking problems. The program is now disseminated nationally. "I cannot overemphasize the value of the peer group of my TLP class to which I still have close connections. My TLP peers are still a support group for many professional issues. In addition, learning from my peers was very helpful. It was interesting to hear how other institutions approach problems and it was refreshing to interact with peers from other subspecialties. Just being together with this talented group of people was very inspiring. The friendships forged throughout the TLP were actually a great support when I later was diagnosed with cancer, of which I was luckily cured later on.
“The TLP added additional value through coaching, which helped me to gain self-awareness.” How you were able to apply some of that knowledge and skills, and what were the outcomes? “The TLP also taught me about my strengths and challenges which made me a more efficient leader. It also taught me about the importance of vision and how to clearly communicate it. My strengths are that I can easily develop a vision and plan and I am naturally drawn to innovation and creative ideas. It can be challenging to communicate your ideas to a team and as well as having the patience until everybody is on board. The TLP taught me some communication techniques that were helpful in making my research team, as well as the epilepsy center that I was directing, successful. And the ability to clearly communicate a vision certainly helped during the interview process for the neurology department chair at Dartmouth, a position which I now hold. “I credit the AAN’s TLP and the Executive Leadership Program in Academic Medicine program, which is another leadership development course I have taken, for helping me make big leaps in my career, not only in becoming the neurology department chair at Dartmouth and bringing national attention to both Dartmouth and HOBSCOTCH, but also being named the Louis and Ruth Frank Professor of Neurosciences. It taught me skills and provided peer support that would not have been available to me otherwise." Learn more about the TLP at AAN.com/TLP.
Thank you to the organizations supporting this program in part:

Alnylam Pharmaceuticals, Inc. Bristol Myers Squibb Novartis Pharmaceuticals, Inc. Supernus Pharmaceuticals, Inc. Seattle: April 2 –7 Virtual Experience: April 24–26
Get Ready for the Great Neuro Reunion!
Reunite with your neurology community from around the globe at the Annual Meeting to experience the most comprehensive educational offerings and largest scientific program in the field with options to participate in person, virtually, or both.
Save when you register by February 17!
AAN.com/AM
UCNS Accreditation and Certification in Clinical Neuromuscular Pathology Approved for Inclusion in CLIA Guidelines
The United Council for Neurologic Subspecialties certification and accredited fellowship training in Clinical Neuromuscular Pathology (CNMP) have been approved under the Clinical Laboratory Improvement Amendments (CLIA) of 1988 as a qualification to practice neuropathology. Having the Centers for Medicare & Medicaid Services approval means that physicians who have successfully completed a UCNS-accredited training program in CNMP and/or have a UCNS certification in the subspecialty are approved by Health and Human Services to examine and provide reports for neuromuscular pathology. The CLIA guidelines will be updated to include UCNS certification/fellowship training as a qualification to practice neuropathology and will be incorporated into the State Operations Manual, also known as the Interpretive Guidelines under 42 C.F.R. § 493.1273(c), D5605, during its next revision. CLIA laws regulate all clinical and anatomic pathology practices, and meeting the regulations is required for Medicare and Medicaid funding. “We are grateful to the UCNS for championing the cause of neurologists with interest in the Clinical Neuromuscular Pathology subspecialty,” said Mazen Dimachkie, MD, CNMP, subspecialty representative to the UCNS Board of Directors, who is also director of the Neuromuscular Division at The University of Kansas Health System, certified in Neurology by the American Board of Psychiatry and Neurology, and certified by the UCNS in CNMP. “The inclusion by CMS of UCNS certification and fellowship training into the CLIA guidelines is a major step forward that will benefit patients with neuromuscular disease and CNMP certified physicians.” The neurologic subspecialty of CNMP differs from neuropathology because it is highly integrated with the clinical management of neuromuscular disease. All UCNS-accredited CNMP training programs incorporate the evaluation of muscle and nerve in the context of clinical patient care. This clinical patient care aspect is what makes the CNMP fellowship training distinctly different from neuropathology. The UCNS has been accrediting CNMP fellowship programs since 2012 and certifying physicians in the subspecialty since 2015. The next UCNS CNMP Certification Examination will be offered in 2023. Fellowship training programs seeking UCNS accreditation may apply throughout the year with deadlines of June 1 and December 1 for the biannual application review cycles. Visit UCNS.org for more information about certification and accreditation.
Applications for Interventional Neurology Certification Now Available
The online application period for the inaugural UCNS Interventional Neurology Certification Examination is now open. The online application, eligibility criteria, and examination content outline are available at UCNS.org. The deadline to apply is March 1, 2022, and the examination will take place September 12 through 16, 2022.
Key dates at-a-glance: March 1, 2022—Application Deadline March 15, 2022—Extended Application Deadline ($500 fee applies) May 2, 2022—Examination Registration Opens September 12–16, 2022—Examination Week

UCNS Announces New Neuro-oncology Diplomates
The United Council for Neurologic Subspecialties is pleased to announce the names of the 43 physicians who passed the 2021 UCNS Neuro-oncology Certification Examination. There are now 326 physician diplomates certified in Neuro-oncology.
Ashley Elimar Aaroe, MD
Iyad Alnahhas, MD
Brian Magne Andersen, MD
Marissa Ann Barbaro, MD
Alipi Bonm, MD
Ivan Darin Carabenciov, MD
Elizabeth Coffee, MD
Christine Alexis Cordova, MD
Ahmad Daher, MD
Husain Danish, MD
Myreille D'Astous, MD
Maria Diza Ordonez, MD
Kevin Bradford Elmore, MD
Ekokobe Fonkem, DO Joshua Friedman, MD Justin Goranovich, MD Matthias Holdhoff, MD, PhD Maya Hrachova, DO Amandeep Kalra, MD, FACP David Olayinka Kamson, MD Albert Kim, MD Peter Kim, MD Mary Jane Lim Fat, MD Justin Low, MD Maria Jill MacDonald, MD Nazanin Majd, MD Divya Mella, MD Alexander C. Mohler, MD Donna Molaie, MD Alexander Ou, MD Peter Chei-way Pan, MD Surabhi Ranjan, MD Lindsay Jade Robell, MD Erika Santos Horta, MD Fernando Santos-Pinheiro, MD Sasmit Sarangi, MBBS Jessica D. Schulte, MD Kaylyn Sinicrope, MD Matthew A. Smith-Cohn, DO Kate Elizabeth Therkelsen, MD Zachary Vaslow, MD Jessica Alice Wilcox, MD Maxim Yankelevich, MD
Physicians in the United States and Canada who meet the eligibility requirements may apply for certification in Neuro-oncology. The next Neuro-oncology certification examination will take place in 2023. Visit UCNS.org to view a complete list of all diplomates certified in Neuro-oncology, UCNS-accredited training programs, and information about Neuro-oncology certification.
CHP: 21 Patient Reported Outcome Measures Ad—Half Page Horizontal> AN
Placed in AANnews 8.25 x 5.25 +0.125 bleed, 4C
Make Your Patient Your Partner
Invest in the outcomes that matter most to your patients. Learn about common Patient Reported Outcome (PRO) scales and tools used in neurology at AAN.com/PRO.


