
58 minute read
Cost-Effective
by AOPA
Cost-Effective Collections Tips for updating financial policies and processes to ensure faster payments and more reliable income
NEED TO KNOW
Given escalating healthcare costs and a rise in provider bankruptcies, now is the time for facilities to re-examine their billing and collection practices.
Some facilities are setting the expectation that a copay is due at the time of visit and requiring that a credit card be kept on file for future balances.
Whether adopting new billing software or just revamping existing procedures, it’s important to work closely with staff members and patients to explain new policies.
To ensure a smooth transition to new collections procedures, O&P facilities should offer flexibility in how visitors pay their bills—including accepting payments online.
When accepting credit card data, facilities must remain in compliance with rules set forth by the Payment Card Industry Data Security Standards.
MOST HEALTHCARE PROVIDERS see their primary goal as helping patients get well—or, in the case of O&P clinicians, helping patients improve mobility and return to activities. But healthcare providers are being forced to focus on their bottom lines as facilities become increasingly dependent on out-of-pocket payments from consumers while the U.S. economy continues to struggle.
“As the healthcare industry is changing, it’s forcing providers to not only be empathetic to patients’ needs, but also to collect, because patients now have higher-deductible plans, or they can’t afford insurance—let alone pay for the equipment or the materials they’re getting,” says Jennifer Leon,
Jennifer Leon vice president of Brightree’s Patient Collections Divisions and a speaker at AOPA’s Virtual National Assembly in September.
In addition, many O&P facilities continue to use outdated collections processes that rely heavily on paper—while many of their patients have adopted new technologies and online bill payment methods at home. Eighty-three percent of consumers prefer electronic methods for medical bills, according to the 2019 InstaMed Consumer Healthcare
Payments Survey. And 66 percent of consumers are willing to consider switching providers for a better payment experience.
Right now, the timing may be perfect for O&P facilities to re-examine their billing practices, adopt technologies to facilitate the process, and implement procedures that will lead to faster and more reliable patient collections, according to Leon. She recommends implementing a new policy at the end of the year or beginning of a new year, because patients understand that policies and insurance coverage usually change at that time. “This really is the key time to do it— when you’re starting a fresh new year.”
As O&P facilities seek to upgrade their collections procedures, Leon suggests a four-pronged approach: change, coach, cater, and collect.
Change Your Outlook As patients’ expected contributions to their healthcare costs are growing, O&P facilities must adopt strategies to collect that money—beginning with the first visit. Studies have shown that 60 percent of patients leave a healthcare facility without paying any money, which is a mistake, according to Leon.
She points to the example of newer walk-in healthcare clinics. Many set the expectation upfront that a copay is due at the time of visit, and they require that a payment card be kept on file for any future balances that insurance may not cover. These facilities are doing their due diligence to secure their assets and to facilitate the collection process for future balances, says Leon. She suggests that O&P facilities consider similar models.
“Once you set the expectation up front that the patient is going to have a balance due, chances improve you’re going to get paid,” she says. This also reinforces to patients that insurance is unlikely to cover 100 percent of their appointments and devices. “And if you take that a step further and you not only set the expectation, but you also save a card on file for future use, then you’re almost at 100 percent guaranteed you will get paid—unless, of course, if the card declines or expires.”

Capturing payment data at first visit—in a way that adheres to Payment Card Industry (PCI) Data Security Standards (DSS) (see sidebar)—is a new way of operating at many facilities, but such a transition could be easier than you think. At Specialized Orthopedic Solutions (SOS) in Chatsworth, California, staff members began collecting card data at first appointments when it switched to a new patient portal solution in early 2019. “Now, we obtain a credit card and keep it on file” within the PCI-compliant system, says Micah Davis, the facility’s operations manager. SOS has seen a rapid decline in unpaid bills and accounts sent to collection since it implemented this process, according to Davis.
Coach to Your New Policy After deciding to adopt new billing software or revamp existing procedures, it’s important for leaders to work with both staff members and patients to explain the new policies.
First, meet with key stakeholders among staff to discuss the need for the change, suggests Leon. “You have to be transparent with your staff. You have to tell them exactly how much debt the facility wrote off last year.” Then explain the plan to fix the problem— which may include discussing financial obligations and capturing credit card information at first visits, adopting a new PCI-compliant billing portal, and/ or setting up patient payment plans—and the importance of every staff member working together to implement new processes. Staff education is key because embracing new collections procedures represents a culture shift, says Leon. “Your staff are going to say things like, ‘We’ve never had to do this before, why are we doing it now?’ So be clear with your communication; be upfront with why you’re changing.”
After educating staff, “you have to coach your patients that your policy has changed,” says Leon. Provide staff with clear and concise scripting and talking points for communicating with patients. “It really doesn’t need to be hard,” says Leon. “We need to keep it simple” when explaining the new policy to patients.
“Educate patients that they will have a balance due for these services,” and offer payment plans. She recommends that O&P facilities draw up financial agreements before offering services to consumers. “If you are letting them walk out the door with any type of service, and there’s a chance that they may not pay you for it because you are billing them later, you need to secure a financial agreement to hold that patient responsible for services rendered,” she says.

Payments Experts Explain PCI Compliance

O&P facilities that accept credit cards are required to comply with the Payment Card Industry (PCI) Data Security Standard (DSS) requirements, a set of requirements intended to ensure that all companies that process, store, or transmit payment card information maintain a secure environment. In order for a healthcare facility to be PCI compliant, it must “have the appropriate technology, personnel, and processes in place to limit opportunities for credit card account data to be compromised or stolen,” explains Richard Rohena, PCI-ISA, manager of compliance services at Global Payments Integrated.
“There’s a big myth that only large providers have to be PCI compliant,” says Zach Gleason, healthcare sales manager at BillingTree. In fact, small healthcare providers are particularly vulnerable and more susceptible to breaches of card data because “hackers are looking for small companies that don’t have large IT departments,” he says.
While there is some concern among healthcare providers that PCI compliance is costly, “it actually saves companies from huge breaches that would be much more costly,” according to Gleason. He points to fines, the loss of patient trust, and the future inability to accept credit cards as potential outcomes of a data breach.
Gleason recommends that O&P facilities use a PCI-compliant solution to input card data. “Your credit card processing terminal, your online processing system—all must be PCI compliant,” he says.
Rohena offers the following “do’s and don’ts” to facilitate PCI compliance:

Do’s: Don’ts:
Do work closely with your acquiring bank and thirdparty service providers to ensure all security protocols meet PCI requirements. Do limit storage of cardholder data, when possible, to reduce the risk of data being compromised and dissuade bad actors. Do implement proper policies, procedures, and training to ensure data security is part of your businessas-usual operations. Don’t transmit or send cardholder data through channels that may not be secure, such as messaging technologies like chat or text. Don’t allow any default, shared, or guest accounts to be enabled on systems within the cardholder data environment. Don’t forget to routinely inspect point-of-interaction devices for unauthorized or suspicious activity.
Financial agreements should be presented during a “financial consultation” when seeing new and existing patients, says Leon. “We jump right away to just helping the patient without looking at the entire picture from a 30,000-foot perspective,” she says. After meeting with new patients for the first time, facilities should go over the diagnosis and O&P intervention, “then move into how we are going to accommodate and help you pay for this,” says Leon.
New payment policies will be easier to implement if facilities offer price estimates up front, adds Leon. Price estimates help patients understand their financial responsibility, recognizing that both the total amount of care and expected contribution from insurance represent estimates—not exact amounts.
Cater to Patients’ Needs To ensure a smooth transition to new collections procedures, O&P facilities should “cater” to patients by offering both transparency about expectations and flexibility in how patients pay their bills—while adopting strategies that increase the likelihood of being paid, says Leon.
Studies have shown that 75 percent of consumers are confused by their healthcare bills, according to Leon. She encourages facilities to examine their bills from a fresh perspective: “If you received one of your bills in the mail, would you understand it?” she asks. Bills should be easy to read, right to left, and top to bottom.
Using an alpha-split system, according to patient last name, to send bills throughout the month could improve a facility’s collection strategy and result in more staff time to respond to billing questions and concerns, according to Leon. For example, if you send out bills for patients with A-F names the first week, G-N names the second week, etc., “that will produce a steady stream of cash flow while preventing a deluge of billing questions at one time during the month,” she says.
To ease the transition in requiring cards on file, Leon recommends accommodating various types of payments, including flexible spending cards, debit cards, checks, ACH payments, and credit cards—“because the last thing the patient wants to find is you weren’t willing to accept” their preferred method of payment.
Of course, when accepting payment card data, facilities must remain in compliance with rules set forth by the PCI DSS. “You cannot store credit card information in your laptop or in a binder; it has to be secured in a locked space and the card numbers encrypted, which is usually facilitated via a PCI-compliant software solution,” Leon explains. When a patient is ready to give their card number, a receptionist can log on to a PCI-compliant Zach Gleason virtual billing terminal and input the credit card info directly into the system, rather than write it down or input it into an Excel spreadsheet, says Zach Gleason, healthcare sales manager at BillingTree, which provides integrated payments solutions to healthcare and other vertical industries. “Then it will be tokenized, encrypted, and secured, with only the last four digits viewable to facility staff,” and it will be accessible for future transactions, Gleason explains.
An alternative method of collecting patient card data is via secure PIN-pad devices that are EMV-chip enabled and offer point-to-point encryption, says Gleason. These devices can be made available at the counter for patients to input their own credit card data without any staff ever seeing card information.
Leon also recommends e-delivery of the notification of the patient’s monthly statement—but not the actual statement, due to HIPAA and privacy rules. E-mailed notification can drive patients to the facility’s online bill pay

site, resulting in faster cash flow back to the office. “Patients want transparency, and many want to view and pay their bills at their leisure,” says Leon.
O&P business managers should create a simple online payment process, too. “Patient portal payments have increased approximately 34 percent each year,” says Leon. “If you are not allowing your patients to pay their healthcare bills online, or even giving them easy ways to pay,” they may move on to another provider that does. She recommends that facility websites feature an easy “Pay Online” button on their home page. A prominent pay button lets patients know exactly where to go to pay their bills, says Leon.
In addition, setting thresholds in the payment portal for minimums due can help businesses cope with decreased cash flow from outstanding balances and payment plans. “Because O&P care can be costly, we need to be able to accommodate payment plans that fit our patients’ ability to pay” while balancing our books, says Leon. But “the last thing you want to do is take a $5 payment on a $10,000 balance,” she says. Longer payment plans should be the exception—for struggling patients— rather than the rule.
As an alternative to paying online, consider offering patients the ability to pay by SMS text or through interactive voice responses, a telephony menu system, says Gleason, who notes that these options could also help to reduce staff time. Of course, mail-in payments should continue as an option for those patients preferring traditional methods.
Collect—and Boost Profits Once a facility has adopted new processes—and perhaps implemented new technology such as a PCI-compliant billing solution and patient portals for credit card acceptance—it can expect to see improved cash flow.
At SOS, implementing a new system last year has led to an increase in patient collections, a significant drop in the number of accounts referred

to collection agencies, and fewer writeoffs. “We love the ability to set up payment plans and the ability for patients to manage payments on their own,” says Davis, adding that patients appreciate the flexibility and transparency of their new processes and procedures. “It’s a seamless process.”
The cost of implementing these new systems “is insignificant compared to the value that it brings,” says Davis. “It’s well worth the investment.”
Most importantly, involving all employees in the collections process is key to boosting collections. “Many clinicians expect this to be ‘billing’s job,’ but that’s the wrong attitude,” says Leon. To see their companies stay profitable, all employees should collaborate in the collections process, and refrain from giving away products or services. “Clinicians must understand that it’s OK to be empathetic to patients’ situations, but they need to involve the financial consultation team when discussing payments,” she says.
Ultimately, business owners should hold staff accountable to the objectives and goals of the new collection strategy. “We’re one team,” says Leon. “We have one message.”
Christine Umbrell is a contributing writer to O&P Almanac. Reach her at cumbrell@contentcommunicators.com.
EDITOR’S NOTE: Missed this session at the 2020 Virtual National
Assembly? Registered participants can access all educational and exhibitor content online until December 31. Visit https://aopa-virtual-national. pathable.co and login using your registration credentials.
Contingency Planning During the COVID Pandemic
COVID-19 teaches us that emergency preparedness goes beyond regulatory requirements
CE Editor’s Note: Readers of CREDITS Compliance Corner are now eligible to earn two CE credits. After reading this column, simply scan the QR code or use the link on page 40 to take the Compliance Corner quiz. Receive a score of at least 80 percent, and AOPA will transmit the information to the certifying boards.
EARN 2 QUIZ ME! BUSINESS CE CREDITS P.40
THE WORLD IS QUITE a different place now than it was a year ago. COVID-19 has impacted lives and workplaces in ways that were once unimaginable and, without a doubt, has tested the preparedness plans we built and intended to rely on during times of crisis. As we continue to navigate uncharted territory, the need to be flexible and innovative—while maintaining compliance to regulatory standards—has underscored the importance of contingency plans that allow us to continue caring for patients who rely on us every day, pandemic or not.
Like many other healthcare professionals, orthotists and prosthetists have made some critically important decisions and adjusted to “the new normal” since the onset of COVID-19. Fortunately, every accredited O&P practice has a contingency plan on file, as required by Section 1 of the CMS Quality Standards. Ideally, the plan helped provide much needed guidance and direction as the COVID-19 virus rapidly spread. More likely, the plan lacked the level of detailed guidance needed during a global pandemic, and instead served as an outline for important discussions and decisions.
During the plan’s initial implementation phase, many O&P practitioners recognized the need to expand contingency plans, adding details and outlining new and revised procedures to guide operations during the pandemic. Now is the time to reassess what we put (or didn’t put) on paper, as well as what we’ve learned from COVID-19. Preparing now for future coronavirus surges, or any other crises, can help safeguard the health and safety of our employees, patients, and businesses.
Challenges Presented by COVID-19
Without a doubt, COVID-19 changed the way we think about crisis management and the steps that healthcare providers must take to be prepared. Prior to 2020, most contingency plans were designed in anticipation of things like tornados, hurricanes, workplace violence, or security breaches—specific events, each with an identifiable beginning and end, followed by a period of recovery.
Most practitioners never considered the possibility of a global health pandemic that would impact operations for weeks, months, or even years.
Contingency plans written before COVID-19 certainly did not provide clarity and direction on delivering patient care with universal masking policies in place or how to maintain social distancing in the office.
The magnitude of challenges presented during the pandemic has been eye-opening in many ways and reveals that much more time and thought must be devoted to thorough, action-oriented contingency planning as we think ahead to the future. The pandemic has forced all of us to quickly adapt to new ways of operating. It has forced healthcare providers to put systems in place to sustain services in the midst of the crisis, while strategically planning for recovery. It has affirmed that “checking the box” on the regulatory side (e.g., creating and filing a contingency document because it is required) cannot suffi ciently prepare anyone when the world shuts down and the health and safety of employees and patients are on the line.
Create an Actionable Contingency Plan
As you rethink your facility’s contingency plan, leveraging key takeaways and lessons learned from the COVID-19 public health emergency is critical. Your experience should guide you in developing an updated version of your contingency plan that is relevant and actionable. Building your plan for the future, however, is a process that requires time, thought, and energy. It’s important to be as detailed as possible because unexpected events can be disorienting and chaotic. This is the document you will retrieve, reference, and live by every day. Some important things to consider:

1. Put yourself in the shoes of a patient who relies on you. Consider the patient journey under normal circumstances, when there is no crisis in play. Think about the experience your patient has, and all the processes they go through, from the time they schedule their first appointment to the time they are released from your care. Start by identifying standard processes and procedures—such as the physical exchange of clipboards, paperwork, and insurance cards— and consider a digital exchange of information that can be completed prior to the office visit.
2. Build a process map that identifies potential changes to the patient journey. With that list of standard processes and procedures in hand, consider how each step could change when typical daily operations are impacted by a crisis. For example, with limitations on the number of individuals who can be in a waiting room, what directions do you want patients to follow when they arrive for an appointment?
What kind of signage should be posted? What adjustments do you need to make to optimize your practice’s functionality? Can technology be used for nonbillable, nonacute patient interaction, such as confirming if a brace is being worn correctly? What procedures would you need to put in place to maximize both patient experience and outcomes, both short and long term?
3. Consider how COVID-19 has impacted patient and provider interactions. What questions and concerns do your patients typically have? Are they delaying care due to fear of potential virus exposure? What steps have you taken to provide continuity of care in a new or different way?
4. Use your process map and scenario planning to document improvements to your actionable contingency plan.
Based on your answers to the questions above, start writing. Document any new or revised processes. Include scenario-based sections to address the specifics, such as appointment check-in and check-out procedures.
Will you establish a reception desk outside the facility door to collect paperwork and perform patient temperature checks? Incorporate as much detail as possible, whether you are creating a brand new contingency plan or improving an existing version.
5. Account for timing. Create a detailed timeline, noting milestones that will be important on day one, day two, and through the 30-, 60-, and 90-day timeframes. Planning should account for a full 12-month period as well as adjustments that may be required if dynamics change or another crisis strikes.
6. Identify the turning point.
Monitoring local, state, and federal mandates is important as you make decisions on how to pivot your practice from “management of the crisis” to “recovery from the crisis.” Stay informed about what’s happening in the world, in your community, and within your patient population. This will help you determine when to implement gradual changes and allow you to resume to “business as usual” over time.
Assemble an Implementation Team You Can Trust
It’s one thing to put a great plan on paper. It’s another to have the right people in place, informed and ready to act immediately when a crisis occurs. It is a good idea to proactively identify members of your team who remain level-headed when times get tough.
Assembling an implementation team you can trust is critically important and should be completed long before your practice operates in crisis mode.
The people you will rely on in the midst of a crisis are likely the same people who offer valuable perspectives as you consider scenarios that could occur. Ask them to be involved in the process of creating your contingency plan. Encourage open, honest dialogue about what should be included in the plan and alternative approaches to consider, based on their valuable experience and knowledge. Also, bear in mind that those who hold various roles within your organization will have different perspectives to offer. Your receptionist will contribute differently from an administrative manager, who will contribute differently from clinical staff members. This level of inclusion will create an open environment that demonstrates all opinions are valued.
Along those same lines, put some thought into who will lead your practice through the crisis. Is it you? Or is the job best suited for a trusted colleague who has demonstrated an aptitude for success when the pressure is on? Think about the roles and responsibilities your designated leader will take on, and the system of support that needs to be built around that person. Who else from your practice should be assigned key roles? Who will be responsible for training? Who will oversee communication? Be sure to account for skill sets, capacity, and ability to adapt under stressful circumstances.
These planning processes and conversations not only will help you build and improve your plan; they also will ensure everyone understands process changes that go into effect during critical incidents and is prepared to respond quickly, when necessary.
The Time to Plan Is Now
Living through COVID-19 has emphasized the importance of emergency preparedness and the need for a solid contingency plan, packed with actionable details.
The time to plan and anticipate the next crisis is now.
Matthew Gruskin, MBA, BOCO, BOCPD, CDME, leads the direction, strategy, policies, and day-to-day operations of the business accreditation and professional certification programs at the Board of Certification/Accreditation. With a focus on credentialing program standards and the delivery of excellent customer service, he also shares his experience and expertise with audiences as both a speaker and an author.
Take advantage of the opportunity to earn two CE credits today! Take the quiz by scanning the QR code or visit bit.ly/OPalmanacQuiz.
Earn CE credits accepted by certifying boards:
www.bocusa.org
Ferrier Coupler Options!
Interchange or Disconnect
The Ferrier Coupler provides you with options never before possible: Enables a complete disconnect immediately below the socket in seconds without the removal of garments. Can be used where only the upper (above the Coupler) or lower (below the Coupler) portion of limb needs to be changed. Also allows for temporary limb replacement. All aluminum couplers are hard coated for enhanced durability. All models are interchangeable.
Model A5
The A5 Standard Coupler is for use in all lower limb prostheses. The male and female portions of the coupler bolt to any standard 4-bolt pattern component.


















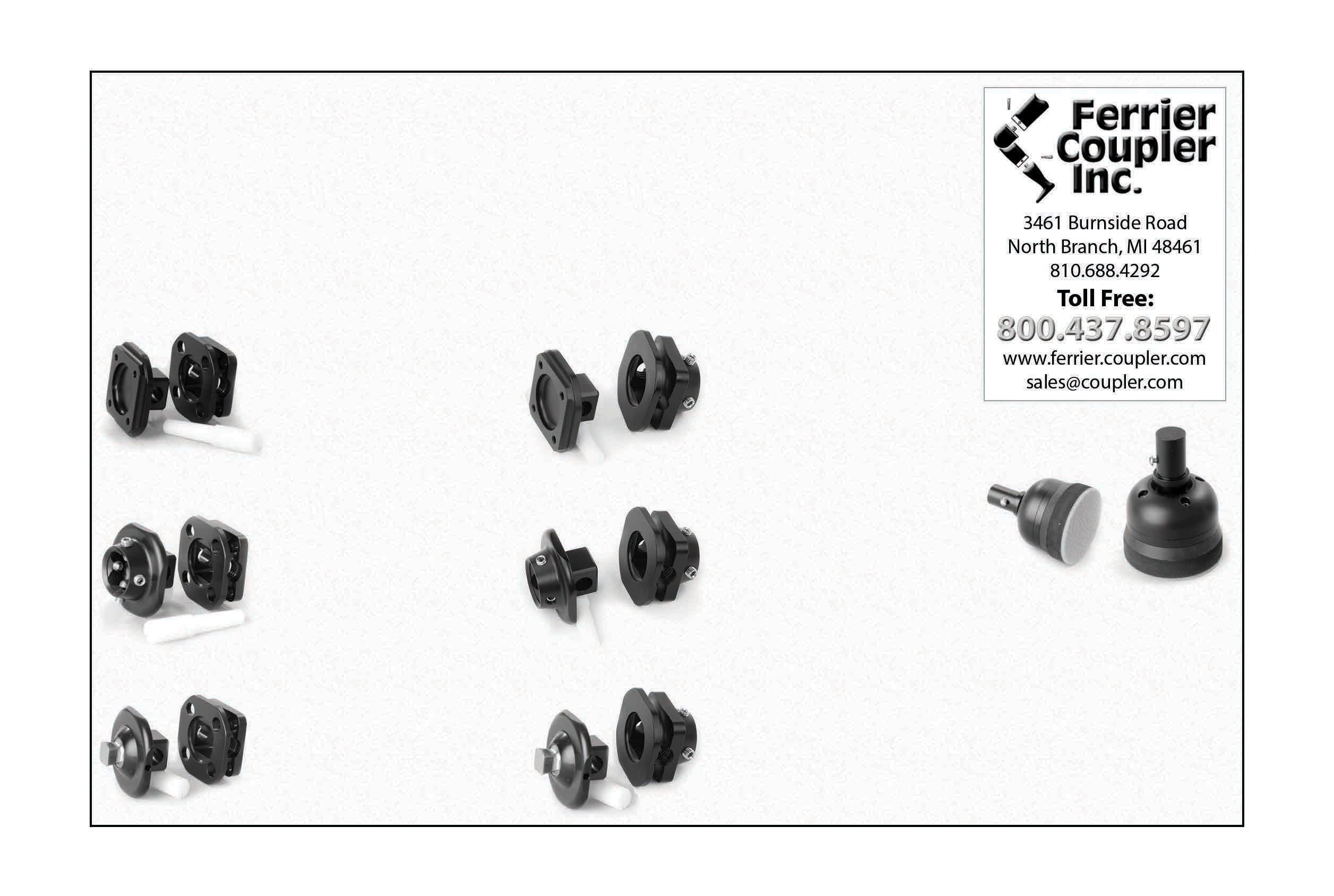
Model FA5
NEW! The FA5 coupler with 4-bolt and female pyramid is for use in all lower limb prostheses. Male portion of coupler is standard 4-bolt pattern. Female portion of coupler accepts a pyramid.
Model F5
The F5 Coupler with female pyramid receiver is for use in all lower limb prostheses. Male portion of the coupler features a built-in female pyramid receiver. Female portion bolts to any standard 4-bolt pattern component. Model FF5
NEW! The FF5 has a female pyramid receiver on both male and female portions of the coupler for easy connection to male pyramids.
Model P5
The Ferrier Coupler with an inverted pyramid built in. The male portion of the pyramid is built into the male portion of the coupler. Female portion bolts to any 4-bolt pattern component. Model FP5
NEW! The FP5 Coupler is for use in all lower limb prostheses. Male portion of coupler has a pyramid. The Female portion of coupler accepts a pyramid. Model T5
The Trowbridge Terra-Round foot mounts directly inside a standard 30mm pylon. The center stem exes in any direction allowing the unit to conform to uneven terrain. It is also useful in the lab when tting the prototype limb. TheThe unitunit isis waterproof and has a traction base pad.

International Collaborator
Australian/Swedish researcher studies how O&P patients leverage their attentional capacity to manage their disabilities and complete tasks
O&P Almanac introduces individuals who have undertaken O&P-focused research projects. Here, you will get to know colleagues and healthcare professionals who have carried out studies and gathered quantitative and/ or qualitative data related to orthotics and prosthetics, and find out what it takes to become an O&P researcher.
NERROLYN RAMSTRAND, BPO (HONS), PhD, believes collaboration is one of the keys to advancing O&P research. In fact, she has pursued several international partnerships over the course of her career.
An orthotist/prosthetist with dual citizenship in Sweden and Australia, Ramstrand currently serves as a professor of prosthetics and orthotics at Jönköping University in Jönköping, Sweden—the only higher education institution in the country offering education for clinical prosthetists and orthotists and O&P technicians.
“Most of my time is spent on research and administrative duties within the university,” explains Ramstrand. She recently served as associate dean of research, until she began a new role in September as advisor to the president of Jönköping University. “In my new position, I will focus on strategic issues related to internationalization for the whole university for 50 percent of my time and will continue with my research for the remainder of my time.”
Throughout her career, Ramstrand has fostered working relationships with several O&P experts in the United States—both privately and through her work with the International Society for Prosthetics and Orthotics (ISPO). She has collaborated with U.S researchers and clinicians on numerous occasions, including working on systematic reviews with Phil Stevens, MEd, CPO, FAAOP; as a team member developing systematic review guidelines for the American Academy of Orthotists and Prosthetists; and in developing numerous symposia in conjunction with Stefania Fatone, BPO (Hons), PhD. Ramstrand currently serves as one of four editors-in-chief of Prosthetics and Orthotics International, together with Fatone; Brian Hafner, PhD; and Michael Dillon, BPO (Hons), PhD.
Dual Interests
Ramstrand, who grew up in Australia, says her career choice was a “natural combination” of her parents’ professions: Her father worked as a civil engineer and her mother was a nurse. “The O&P profession appealed to me at the time as it was very much hands-on, and I wasn’t sure that I was ready for a desk job,” she says.
After completing her bachelor’s studies in O&P at La Trobe University in Australia, she realized that research appealed to her, and she applied for a government scholarship to pursue a doctorate. She earned her PhD from La Trobe in 2000—while sharing an office with Fatone, another La Trobe graduate—and completing
a doctoral thesis on “Visual Search Strategies and Decision Making in Observational Gait Analysis.”
Over the past two decades, Ramstrand has taught many undergraduate O&P courses. Some topics at Jönköping University have included “O&P Introduction,” “O&P Theory,” “Models and Perspectives on Health and Disability,” and “Clinical Gait Analysis,” among others. Included in her teachings is an emphasis on the importance of research, according to Ramstrand; the O&P curriculum in Sweden carves out time for research-related activities.
“Our students are taught about the principles of evidence-based practice in the first semester of their studies,” she says. “Throughout the education, they are encouraged to motivate clinical decisions with evidence from research.” She explains that the university’s researchers are actively involved in teaching, and research findings are presented to students in all levels of the program. “In their final year of studies, our bachelor students are required to conduct a major research project,” she says.
Jönköping University also offers a recently introduced master’s program in product development, specializing in assistive technology. The master’s is open to graduate prosthetist/orthotists as well as engineers and is conducted in close collaboration with industry partners. “Within the program, partners are invited to submit manufacturing and design problems, which the students are required to work with and present a solution back to the partner organization.”
Ramstrand’s Research
Over the past five years, Ramstrand has become interested in exploring the effects that prostheses and orthoses may have on attentional demand of users, and whether design alterations can affect the attentional load required to perform specific tasks. “The premise of this work is that an individual with disabilities must use a large proportion of their attentional capacity to manage their disability, and that this signifi cantly affects the extent to which they can attend to other tasks,” she says.

Ramstrand discusses design of an ankle-foot orthosis with her colleague, Christoffer Wadman.
To measure attentional load, her team in Jönköping has been working with portable brain imaging technology (functional near-infrared spectroscopy) to record patterns of activity in the prefrontal cortex, which plays a key role in performance of functions such as switching attention, working memory, and inhibiting inappropriate responses. “To date, most of our research has focused on studying brain activity during gait of individuals fitted with microprocessor-controlled knees versus mechanical knees, but we have begun to explore other types of O&P interventions,” she says. These include the effects of finger orthoses on hand function—a study that was recently accepted and will be published in Prosthetics and Orthotics International—as well as the effects of virtual reality training for myoelectric arm prostheses under a grant recently received with collaborators from Orebro University and Chalmers University.
Ramstrand anticipates that the attentional load research will provide evidence for payors regarding the benefits of one prosthesis design over another or, in the case of orthoses, “the research may provide evidence to support prescription of a device over no device.”
In another study, Ramstrand recently received funding for a collaborative project to study means of better incorporating end-user design preferences into service provision and manufacturing of O&P devices. “Product design is a new area of research for me,” she says, “and I am enjoying learning about different approaches that could be applied in O&P applications.”
After some interesting qualitative research conducted with O&P users in Cambodia, Ramstrand also has applied for funding with partners from Queens University, Belfast, Exceed Worldwide, and the Royal University of Phnom Penh, to study the mental health of O&P users in Cambodia. “Cambodia has a severe shortage of mental health workers, and our intention with this project will be to identify and test screening tools that can be applied by O&P clinicians and to train community health workers to provide basic mental health services,” she explains.
Looking to the future, “I would like to see more research focusing on the relative effects of O&P devices on individuals’ ability to participate in activities that they feel are important,” says Ramstrand. “As a profession, we are quite good at focusing on body functions and the biomechanical effects
of devices we prescribe, but we often forget that we are also likely affecting other very important aspects of a person’s life.” While she concedes that it’s difficult to measure the potential benefits of O&P devices on outcomes related to participation, “I would like to see us incorporating these types of outcomes into our research.”
Out-of-Office Activities
In addition to her responsibilities at Jönköping University, Ramstrand has spent time as an ISPO member for several years, and served as a consultant for ISPO on the development of an O&P program at the University of Zambia.
She also stays busy working as a consultant to the Swedish police since 2009, serving as an expert witness providing forensic analysis of gait in criminal cases. She is called to court to testify once or twice a year—including during a high-profile “helicopter robbery,” which made national news.
Notable Works
Nerrolyn Ramstrand, BPO (Hons), PhD, co-editor-in-chief of Prosthetics and Orthotics International, is the author or co-author of dozens of peer-reviewed articles and conference presentations. Some of her most impactful contributions include the following: • Ramstrand, N., Rusaw, D., Möller, S. “Transitioning to a Microprocessor-
Controlled Prosthetic Knee—Executive Functioning During
Single- and Dual-Task Gait.” Prosthet Orthot Int, 2020; 44:1:27-35. • Möller, S., Rusaw, D., Hagberg, K., Ramstrand, N. “Reduced Cortical
Brain Activity With the Use of Microprocessor-Controlled Prosthetic
Knees During Walking.” Prosthet Orthot Int, 2019; 43:3:263-271. • Ramstrand, N., Ramstrand, S. “Competency Standards for Newly Graduated
Prosthetist/Orthotists in Sweden.” Prosthet Orthot Int, 2018; 42:4:387-393.
Ramstrand is married to a Swedish orthotist/prosthetist, Simon Ramstrand. The couple shares two sons, ages 9 and 12. The family pursues non-O&P-related projects as they renovate a “run-down bed-and-breakfast” they recently purchased, located by a large lake. “Among my academic qualifications, I could add basic plumbing, tiling, carpentry, and painting,” she says. “I also got myself certified as a chimney sweep.”
Amid all of these activities, Ramstrand keeps an eye out for new opportunities to connect with professionals across the globe. She continues to search for ways to expand the O&P research well with studies that are inclusive and involve many perspectives.
EARN 8 CEs


Virtual Coding and Billing Seminar
NOVEMBER 9-10, 2020
Get the latest on coding, billing, and reimbursement policy, join our experts November 9 and 10 for the AOPA Virtual Coding and Billing Seminar.
It is what you’ve come to expect from our Coding and Billing seminars but tweaked and condensed slightly to offer it virtually. Content will be presented from Noon-4:00 PM ET both days. REGISTER BY OCTOBER 20 AND RECEIVE A FREE 2020 QUICK CODER.
COST: Before October 20: $295 for members $395 for nonmembers.
After October 20: $320 for members $420 for nonmembers.
Earn 8 CE credits.
Learn more and register at www.aopanet.org/education/coding-billing-seminar. Questions? Contact Devon Bernard at dbernard@AOPAnet.org.
www.AOPAnet.org
Co-OP

AOPA’s Co-OP
The O&P Compendium
We ARE AOPA ADVOCACY | RESEARCH | EDUCATION

An online reimbursement, coding, and policy resource, the site includes a collection of detailed information with links to supporting documentation for the topics most important to AOPA Members.
O&P’s best kept secret, the Co-OP incorporates a crowdsourcing component, which is vetted by AOPA sta , to garner the vast knowledge and experience of the membership.
Resources include: • State-specifi c insurance policy updates, • L-code search capability, • Data and evidence resources, • And so much more!
Learn more and sign up at www.AOPAnet.org/co-op.
Adapting Care During COVID-19
New York prosthetic facility debuts remote assistance program
OWNER ERIK SCHAFFER, CP, founded A Step Ahead Prosthetics more than 20 years ago, after 14 years in the industry. While his focus was helping patients of all ages gain their mobility, he quickly became known for pushing the development of sports devices for amputee athletes. Business grew rapidly, and today the facility provides a full range of upper- and lowerextremity prosthetic solutions.
The main office, in Hicksville, New York, occupies more than 20,000 square feet, including a 6,000-square-foot fabrication lab and a division dedicated to creating lifelike silicone skins. A sister office in Boston has expanded the company’s geographic reach; it occupies about 10,000 square feet and offers the same services, except billing, which is centralized in New York.
A Step Ahead, with 32 employees, serves patients from nearly every state in the United States in addition to countries on every continent, Schaffer says.
The size of the facility gives it certain advantages. “The complexity of our research and development department is unique to the industry,” he says. “We have a full-time biomechanical engineer and product designers on staff. Our New York lab is equipped with a five-axis CNC carving router, 3D printers, and a complete metal shop with mills, lathes, and other specialized equipment,” Schaffer says. “We take ideas from concept through A Step Ahead’s main office is based in Hicksville, New York.

FACILITY:
A Step Ahead Prosthetics
LOCATIONS: Hicksville, New York, and Boston
OWNER:
Erik Schaffer, CP
HISTORY:
21 years
Owner Erik Schaffer, CP, works on a device in his facility’s 6,000-squarefoot fabrication lab. fruition, all in-house.” The result, he says, is an exceptional approach to specialty work and fully customized devices, all in record time.
The large gait area in the New York facility features hydraulic ramps, a treadmill, a gym, and the Solo-Step ceiling-mounted harness training system. A new space is devoted exclusively to training upper-extremity amputees.
Schaffer believes in a multidisciplinary team approach to prosthetic care, and he works closely with surgeons to ensure optimal outcomes for amputees, including osseointegration, when appropriate. “We work with hospitals on approvals [from the U.S. Food and Drug Administration] and IRBs [investigative research boards] to bring technology to fruition,” he says.
The SkinTones™ division of A Step Ahead offers handmade silicone prosthetic covers as well as replacements for the breast ears and noses. “Our approach to creating anatomically correct prostheses includes the adoption of high-end 3D scanners that allow us to create mirror-like images of existing limbs,” he says.
About 10 years ago, one of Schaffer’s four daughters had the idea to fit a doll with a prosthesis as a gift for her friend with limb loss. Schaffer took on the challenge, modifying the doll to fit it with a custom-made prosthetic leg that matched that of the friend. The idea took off, and today A Step Ahead is the official prosthetic provider for American Girl® dolls. “I’ve made thousands since then,” says Schaffer, who invites children with limb loss to send in their American Girl doll for a fitting, free of charge. Thanks to donations, A Step Ahead gives away a certain number of dolls to children whose families can’t afford them.
During the pandemic, Schaffer developed the facility’s remote assistance program, which and maxillofacial areas, including
enables patients to schedule a virtual consultation and then ship their prostheses or skin covers to the facility for repairs and adjustments. During the lockdown, they extended the service to nonpatients as well. “We’ve done virtual consultations with amputees in Panama, Sri Lanka, and Ethiopia, as well as those all over the United States,” he says.
Schaffer is most proud of his facility’s approach to insurance. A staff of billing specialists and practitioners develops and implements strategies to ensure the best possible outcome for patients. “We fight for our patients’ rights,” he says. “The insurance companies are dictating care, and caregivers are conceding to whatever they will allow. While I still have air in my lungs, I will continue to fight for my patients and their right to the most appropriate treatment for their situation.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net.
During these one-hour sessions, AOPA experts provide up-to-date information on a specific topic. Webinars are perfect for the entire staff—they’re a great teambuilding, money-saving, and educational experience! Sign up for the entire series and get two conferences free.
Entire Series ($990 Members/ $1,990 Nonmembers). Register at http://bit.ly/2020AOPAwebinars. Looking to develop a new product? Want to see who is currently using what product? AOPA members can access the CMS Data Portal to access comprehensive, easy-to-use, easyto-read, Medicare Part B orthotic and prosthetic claims data from the last five years; previous years are available with special request. You can download customized reports for use in your own reports and marketing material.
The data is updated annually to ensure you have the most recent data at your fingertips. Just set your search parameters, and in a matter of minutes you’ll get data to help you do the following:


Webinars
UPCOMING WEBINAR WEDNESDAY NOV. 11 RAC Audits: What Are They Looking At? The November 11 webinar will examine the rules governing the recovery audit contractor (RAC) program, the different types of audits conducted by the RAC, and what areas the RAC is currently auditing. Hear an expert discuss these issues and tips for
Download Data From the CMS Data Portal
avoiding potential RAC audits. Understand the current market in terms of size, geographic distribution, and provider specialty. Predict growth and opportunities. Compare historical and projected growth rates in Medicare. Identify new product opportunities.
This CMS Data Portal is free to AOPA members. To access it, all you need is your AOPA member username and password. Visit the AOPA website, or contact Devon Bernard at dbernard@AOPAnet.org.
UPCOMING WEBINAR WEDNESDAY DEC. 9 New Year: New Codes, Fees, and Updates Don’t miss one of the most anticipated webinars of the year. AOPA’s coding and billing experts will provide up-todate analysis and interpretation of the newest HCPCS codes and changes for the upcoming year. Presenters will recap the 2020 Medicare changes and share updates on what to expect in 2021.

DATA AT YOUR FINGERTIPS
FREE
ACCESS AOPA Offers Members Free Access
to AOPAversity
AOPA knows you and your employees are being tremen- offer. We hope this benefit offers you additional support dously impacted by COVID-19. To help, we are offering during this uncertain time. Contact Ryan Gleeson at you, our AOPA members, the ability to access our online rgleeson@AOPAnet.org with any questions. learning management system, AOPAversity, for free for the rest of 2020. It is our hope that this will make it easier to navigate the current unprecedented situation.
What does this mean? You and your employees can now access all 72 online offerings, which are prerecorded videos available on demand.
If you do not currently have an AOPAversity account, visit https://myaopaconnection.org to create a profile. You will need your AOPA member ID and the Zip code affiliated with your membership when you create your profile to access the free offering. Already have a profile? Log in at www.AOPAnetonline.org/aopaversity. Your username is the email used to create your profile.
This offer is valid through Dec. 31, 2020, and excludes any refunds to purchases made prior to the start of this


AOPA Offers COVID-19 Responses, Guidance, and Resources


AOPA leadership has continued to closely follow the spread of the coronavirus disease (COVID-19) and its widespread impacts. We also have been taking your calls and emails and hearing firsthand how extremely difficult and uncertain things are for you, your businesses, and your patients.
To that end, we are responding with support. We are responding with outreach to legislators about how they can best support the O&P profession. We are responding by providing guidance on regulations like documentation, telehealth, and stay-at-home orders. We are responding by pulling together resources. We are responding by creating a space on the Co-OP to share your experiences and strategies with one another.
All of this information can be found on the newly developed COVID-19 Response and Resources webpage,




www.AOPAnet.org/resources/covid-19. We will be updating this webpage frequently with actions, guidance, and resources, and will be pushing out updates via email, Smartbrief, and AOPA’s social media channels. As the situation evolves daily, we encourage you to also follow the guidance being issued from the Centers for Disease Control and Prevention (CDC), the World Health Organization, and your local, state, and federal government. The CDC website features resources and guidance for healthcare facilities; visit www.cdc.gov/ coronavirus/2019-ncov/healthcare-facilities.
Thank you for all you continue to do for your patients and the O&P profession. The AOPA Board of Directors and staff are here to support you. If you have questions, concerns, or needs, do not hesitate to reach out to any of the staff at info@AOPAnet.org.
O&P PAC Update
The O&P PAC Update provides information on the activities of the O&P PAC, including the names of individuals who have made recent donations to the O&P PAC and the names of candidates the O&P PAC has recently supported. The O&P PAC recently received donations from the following AOPA members*:
Curt Bertram, CPO Jeffrey Brandt, CPO George Breece Terri Bukacheski, CP Erin Cammarata, CTO Tina Carlson, CMP Christina Cox Steven Ehretsman Don Foley Eve Lee, MBA, CAE Jim Liston, CP F. Daniel Luitjohan, CP Jeff Lutz, CPO Brad Mattear, CFo, CPA, LO Martin McNab, CPO Wendy Miller, BOCO Matthew Nelson, CPO Ricardo Ramos, CP, LP Bradley Ruhl Michael Schlesinger Lesleigh Sisson, CFo, CFm Bernie Veldman, CO Regina Weger Dennis Williams, CO, BOCO Scott Williamson, MBA Larry Word, CPO Ann Yamane, CO James Young Jr., CP, LP, FAAOP Claudia Zacharias, MBA, CAE
NEW MEMBERS
Welcome New AOPA Members
THE OFFICERS AND DIRECTORS of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
Fourroux Prosthetics Inc. - STL 9665 Page Avenue Overland, MO 63132 314/551-2341 Affiliate

The purpose of the O&P PAC is to advocate for legislative or political interests at the federal level that have an impact on the orthotic and prosthetic community. The O&P PAC achieves this goal by working closely with members of the House and Senate and other officials running for office to educate them about the issues, and help elect those individuals who support the orthotic and prosthetic community.
To participate in, support, and receive additional information about the O&P PAC, federal law mandates that eligible individuals must first sign an authorization form, which may be completed online: bit.ly/aopapac.
*Due to publishing deadlines this list was created on Sept. 14, 2020, and includes only donations and contributions made or received between Jan. 15 and Sept. 14, 2020. Any donations or contributions made or received on or after Sept. 14, 2020, will be published in a future issue of O&P Almanac.
Grace Rehab Inc. 901 N. McDonald Street, Ste. 906 McKinney, TX 75069 972/984-1851 Bobby Bailey Patient-Care Facility
Point Designs 1216 Commerce Court, Ste. 3 Lafayette, CO 80026 720/600-4753 Levin Sliker Supplier Streamline Orthotics and Prosthetics LLC 615 S. Vandeventer Avenue St. Louis, MO 63110 314/289-9100 Kelly Vogl Patient-Care Facility
Walker Orthotics and Prosthetics 205 Redmond Road Rome, GA 30165 706/232-4383 Grant Espy, MBA Patient-Care Facility
ALPS Prosthetic Socks
The ALPS prosthetic sock is lightweight and soft, providing cushioning and comfort for a superior fit. Available in one-, three-, and five-ply, the socks are manufactured with Coolmax® fibers to create a moisture management system that moves perspiration away from the body and through the fabric, where it can evaporate quickly. They accommodate volume fluctuation and can be worn alone or with one’s prosthesis. The Coolmax® fibers allow a cool, comfortable wear. These socks keep their shape over time; minimal stretch and will not mat down. Ones with a distal hole are only available with plastic reinforcement. The plastic reinforced hole prevents fraying of the seam around the distal hole. This sock is offered in various length and thickness, and you can choose between Narrow, Medium, and Wide.
Call us or visit www.easyliner.com for more information.

Apis

Apis custom program offers practitioners best options and services for patient compliance. All products are covered under risk-free guaranteed-fit promise. We stand firmly behind our words.
Call us at 1-888/937-2747.
Fabtech Epoxy Meter Mixer
Making your fabrication life easier! Our Epoxy Meter Mixer offers a faster, cleaner, and accurate way for you to meter your RESTECH+ Epoxy resin ratio every time! • Our resin pump meter mixing system has one-gallon resin reservoirs, for the
A and B sides, for a total of two gallons. • Keeps your mixing station clean and organized! • Accurately dispenses up to three quarts of unmixed two-part RESTECH+ epoxy resin per minute. • All you have to do is mix the resin. • No more gram scale!

Call for more details! Contact 800/322-8324 or visit www.fabtechsystems.com.
The Original Preflexed Suspension Sleeve
ESP created the Flexi family of suspension sleeves as a comfortable, durable, and cost-effective alternative to traditional suspension sleeves. Preflexed at 43 degrees for maximum comfort and natural unrestricted movement.
For more information, call ESP LLC at 888/932-7377 or visit www.wearesp.com.

LEAP Balance Brace
Hersco’s Lower-Extremity Ankle Protection (LEAP) brace is designed to aid stability and proprioception for patients at risk for trips and falls. The LEAP is a short, semirigid ankle-foot orthosis that is functionally balanced to support the foot and ankle complex. It is fully lined with a lightweight and cushioning Velcloth interface, and is easily secured and removed with two Velcro straps and a padded tongue.
For more information, call 800/301-8275 or visit www.hersco.com.
Naked Prosthetics
Naked Prosthetics designs and manufactures high-quality prosthetic devices specifically for finger loss. Our mission is to assist people with digit amputation(s) and positively impact their lives with fully articulating, custom finger prostheses. Our product aims to restore the ability to perform most tasks, supporting job retention and an active lifestyle. Our customers have lost fingers to power tools, equipment malfunctions, injury in the line of military service, random accidents, and infections; in some cases, multiple digits have been lost. NP provides a viable functional prosthesis, as opposed to a passive cosmetic solution. Our design mimics finger motion and utilizes the remainder of an amputee’s digit to power the device.
For more information, visit www.npdevices.com.

Proteor Rush Rogue®
The PDAC approved RUSH ROGUE® provides the most realistic and dynamic foot and ankle motion available. The Vertical Loading Pylon (VLP) provides vertical shock relief while offering +/- 8 degrees of torsion, allowing the user to push the foot and themselves to the limits. The RUSH ROGUE is made of our advanced fiberglass composite, which is 3X more flexible than conventional prosthetic feet. The roll-through characteristics of the foot provide exceptional energy return with no “dead spot.” The RUSH ROGUE is also available in the EVAQ8 elevated vacuum and H2O models. #goROGUE
The Harmony System: A Strong Connection
As an active vacuum volume management system for transtibial prostheses, the Harmony P4 System creates vacuum between the liner and socket, resulting in an unprecedented socket fit.
Compared to a valve or pin system, benefits include: • Reduced volume fluctuations • Improved suspension • Reduced forces within the socket • Improved proprioception • Promotes residual limb blood circulation.
To learn more, call your sales rep or visit professionals.ottobockus.com.
WalkOn® Carbon Fiber AFO
WalkOn ankle-foot orthoses (AFOs) are prefabricated from advanced prepreg carbon composite material designed to help users with dorsiflexion weakness walk more naturally. WalkOn AFOs are lightweight, low profile, and extremely tough. Their dynamic design can help patients achieve a more physiological and symmetrical gait, offering fluid rollover and excellent energy return. WalkOn offers a full range of AFO sizes and designs, including the WalkOn Reaction junior pediatric sizes.
Fast and easy to fit, the WalkOn footplate is trimmable and can be shaped with scissors, often requiring only one office visit.

Contact us at 800/328-4058 or professionals.ottobockus.com for details.
Spinal Technology Inc.
Spinal Technology Inc. is a leading central fabricator of custom spinal and scoliosis orthoses. Our ABC-certified staff orthotists collaborate with our highly skilled, experienced technicians to provide the highest quality products and fastest delivery time, including weekends and holidays, as well as unparalleled customer support in the industry.
Spinal Technology is the exclusive manufacturer of the Providence Nocturnal Scoliosis® System, a nocturnal bracing system designed to prevent the progression of scoliosis, and the patented FlexFoamTM spinal orthosis.
For information, contact 800/253-7868 or visit www.spinaltech.com.

AOPA Supplier Plus Members
Thank you to our 2020 AOPA Supplier Plus Members for their continued support of the association.



The Xtern Foot Drop AFO by Turbomed Orthotics
Think outside the shoe! This oneof-a-kind orthosis (AFO) is a game changer for foot drop patients: the Xtern is totally affixed outside the shoe to maximize comfort, prevent skin breakdown and rubbing injuries. Its flexibility promotes maximal ankle range of motion and calf muscle strength. The Xtern allows running, walking, and even mountain hiking as long and as far as you want without any restrictions, and moves from sandals to boots flawlessly.
Turbomed’s innovative products are designed in Quebec, Canada, sold in over 26 countries, and distributed by Cascade in the United States. Visit turbomedusa.com to get your life back!
MAKING LIVES BETTER
Tel: 727.528.8566 Tel: 800.574.5426 www.easyliner.com info@easyliner.com
Opportunities for O&P Professionals
Job Location Key:
- Northeast - Mid-Atlantic - Southeast - North Central - Inter-Mountain - Pacific
Hire employees and promote services by placing your classified ad in the O&P Almanac. Include your company logo with your listing free of charge.
Refer to www.AOPAnet.org for content deadlines. Ads can be posted and updated any time online on the O&P Job Board at jobs.AOPAnet.org. No orders or cancellations are taken by phone. Send classified ad and payment to: O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711 or email jburwell@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
O&P Almanac Careers Rates
Color Ad Special
1/4 Page ad 1/2 Page ad
Member
$482 $634
Nonmember
$678 $830
Listing Word Count
50 or less 51-75 76-120 121+
Member
$140 $190 $260 $2.25 per word
Nonmember
$280 $380 $520 $5 per word
ONLINE: O&P Job Board Rates Visit the only online job board in the industry at jobs.AOPAnet.org.
Job Board
50 or less
Member
$85
Nonmember
$280
For more opportunities, visit: http://jobs.AOPAnet.org.
SUBSCRIBE
A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P.
WANTED!
A few good businesses for sale.
Lloyds Capital Inc. has sold over 150 practices in the last 26 years.
If you want to sell your business or just need to know its worth, please contact me in confidence.
Barry Smith Telephone: (O) 323/722-4880 • (C) 213/379-2397 Email: loyds@ix.netcom.com
AOPA’s O&P Career Center
Connecting highly qualified O&P talent with career opportunities

EMPLOYEE Research who is hiring Apply online for job openings Free résumé review
EMPLOYER Post your job in front of the most qualified group of O&P professionals Search anonymous résumé database to find qualified candidates Manage your posted jobs and applicant activity easily on this user-friendly site.
Career Opportunities...

California CO-Sacramento CO-Modesto CPO-Salinas
Oregon
CPO –Corvallis & Salem

To apply, submit resume to: c careers@pacmedical.com


Established in 1987, Pacific Medical Prosthetics and Orthotics has become a tenured company in the industry for superior patient care, products and services.
The positions we offer are created for candidates that are looking to create opportunity, self-driven, motivated, and enjoy serving and helping others.
A competitive salary, benefits and profit sharing are offered based on position/experience.
Our Culture & Commitment “We will serve and help others grow personally, professionally, and strive to put others needs first and foremost as demonstrated by our positive attitude, teamwork and professionalism.”
AD INDEX
Advertisers Index
Company ALPs American Board for Certification in Orthotics, Prosthetics, & Pedorthics Amfit Apis Footwear Company Cailor Fleming Insurance ESP LLC Fabtech Systems LLC Ferrier Coupler Inc. Hanger Hersco Naked Prosthetics Ottobock PROTEOR USA Spinal Technology Inc. Tamarack Habilitation Technologies TurboMed Orthotics Page 15
47 13 20 41 5 32, 33 40 16, 17 1 29 C4 9 21 7 3 Phone 800/574-5426
703/836-7114 800/356-3668 888/937-2747 800/796-8495 888/WEAR-ESP 800/FABTECH 810/688-4292 877/4HANGER 800/301-8275 888/977-6693 800/328-4058 855/450-7300 800/253-7868 763/795-0057 888/778-8726 Website www.easyliner.com
www.abcop.org www.amfit.com www.apisfootwear.com www.cailorfleming.com www.wearesp.com www.fabtechsystems.com www.ferrier.coupler.com www.hanger.com/diversity www.hersco.com www.npdevices.com www.professionals.ottobockus.com www.proteorusa.com www.spinaltech.com www.tamarackhti.com www.turbomedorthotics.com

APPLY ANYTIME. TEST ANYWHERE. Become a BOC-certified orthotic fitter, www.bocusa.org mastectomy fitter, or durable medical equipment specialist. Exams are offered year-round: in-person at test centers and select conferences and online from the location of your choice with a live, remote proctor! Visit www.bocusa.org/certification/apply.
Cascade Dafo Institute Nine free ABC-approved online education courses to enhance your clinical practice. Take anytime, anywhere, and earn up to 14.5 CE credits. Visit cascadedafo.com or call 800/848-7332.
2020
October 8–10
South Carolina Society of Orthotists and Prosthetists (SCSOP) NC/SC Combined Meeting. SCSOP hosting. Greenville, SC. For more information, visit https://scsop.org.
October 1–31
ABC: Written and Simulation Certification Exams. ABC certification exams will be administered for orthotists, prosthetists, pedorthists, orthotic fitters, mastectomy fitters, therapeutic shoe fitters, orthotic and prosthetic assistants and technicians in 350 locations nationwide. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
October 14
New Technical Credits—Clinician’s WEBINAR Corner: Fitters and Techs. For more information, visit www.AOPAnet.org.
October 15–17 (New rescheduled date; online) Tennessee Society of Orthotists and Prosthetists (TSOP) Annual Meeting. Rescheduled from April. Now online. For more information, visit www.tennsop.org.
October 27–29
OT World.connect 2020. A Virtual World Congress with more than 250 participants from more than 20 countries will be accompanied by digital presentations on industry innovations. For more information, visit www.ot-world. com/index-en.html.
November 1
ABC: Application Deadline for Winter CPM Exams. All practitioner candidates have an additional 30 days after the application deadline to complete their residency. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/ individual-certification.
November 1
ABC: Practitioner Residency Completion Deadline for December Written & Simulation Exams. All practitioner candidates have an additional 30 days after the application deadline to complete their residency. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
November 9–10
SEMINAR AOPA Virtual Coding and Billing Seminar. Join our experts, get the latest on coding, billing, and reimbursement policy. For more information, visit www.AOPAnet.org.
WEBINAR
visit www.AOPAnet.org.
November 11
RAC Audits: What Are They Looking At? For more information,
December 1
ABC: Application Deadline for February Written & Simulation Exams. Applications must be received by December 1 for individuals seeking to take the February written and simulation certification exams. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
December 1
ABC: Practitioner Residency Completion Deadline for Winter CPM Exams. All practitioner candidates have an additional 30 days after the application deadline to complete their residency. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
December 9–14
ABC: Written and Simulation Certification Exams. ABC certification exams will be administered for orthotists, prosthetists, pedorthists, orthotic fitters, mastectomy fitters, therapeutic shoe fitters, orthotic and prosthetic assistants, and technicians in 350 locations nationwide. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
WEBINAR
www.AOPAnet.org.
December 9
New Year: New Codes, Fees, and Updates. For more information, visit
2021
January 1
ABC: Practitioner Residency Completion Deadline for February Exams. All practitioner candidates have an additional 30 days after the application deadline to complete their residency. Contact 703/836-7114, email certifi cation@ABCop.org, or visit ABCop.org/individual-certification.
January 10–11
ABC: Orthotic Clinical Patient Management (CPM) Exam. ABC Testing Center, Tampa, FL. Contact 703/836-7114, email certification@ABCop. org, or visit ABCop.org/individual-certification.
January 24–25
ABC: Prosthetic Clinical Patient Management (CPM) Exam. ABC Testing Center, Tampa, FL. Contact 703/836-7114, email certification@ABCop.org, or visit ABCop.org/individual-certification.
February 1
ISPO 18th World Congress Deadline for Symposia and Instructional Courses. For more information, contact the ISPO World Congress team at info@ispo-congress.com or call +49/341-678-8237.
March 29
ISPO 18th World Congress Deadline for Free Papers. For more information, contact the ISPO World Congress team at info@ispo-congress.com or call +49/341-678-8237.
May 12–14
New York State Chapter of American Academy of Orthotists and Prosthetists (NYSAAOP) Meeting. Rivers Casino & Resort, Schenectady, NY. For more information, visit nysaaop.org/meeting.
September 9–12
AOPA National Assembly. Boston. For more information, visit www.AOPAnet.org.
November 1–4
ISPO 18th World Congress. Expo Guadalajara Convention & Exhibition Centre in Guadalajara, Mexico. For more information, contact the ISPO World Congress team at info@ispo-congress.com or call +49/341-678-8237.
THE LIGHTER SIDE

“NO, NO!… I ASKED FOR A HIPAA MANUAL!”
Calendar Rates
Let us share your next event!
Phone numbers, email addresses, and websites are counted as single words. Refer to www.AOPAnet.org for content deadlines. Send announcement and payment to: O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711, fax 571/431-0899, or email jburwell@AOPAnet.org along with VISA or MasterCard number, the name on the card, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
Words/Rate
25 or less 26-50 51+
Color Ad Special
1/4 page Ad 1/2 page Ad
Member
$40 $50 $2.25/word
$482 $634
Nonmember
$50 $60 $5.00/word
$678 $830 For information on continuing education credits, contact the sponsor.
Questions? Email info@aopanet.org.
Championing the O&P Agenda
Updates from Arkansas, California, Kansas, and New York
Each month, State by State features news from O&P professionals about the most important state and local issues affecting their businesses and the patients they serve. This section includes information about medical policy updates, fee schedule adjustments, state association announcements, and more. These reports are accurate at press time, but constantly evolve. For up-to-date information about what is happening in your state, visit the Co-OP at www.AOPAnet.org/resources/co-op.
COVID-19 Updates
AOPA is maintaining statespecific updates related to the coronavirus disease (COVID-19) on all state pages of the Co-OP. Please visit your state’s page for additional information.
Prior Authorization Reminder
CMS began Medicare prior authorization for six prosthetic codes in the four states previously selected for the initial rollout— Pennsylvania, Michigan, Texas, and California—on September 1. The prior authorization program for prosthetics will be implemented nationally on Dec. 1, 2020.
Arkansas
Blue Cross Blue Shield (BCBS) Arkansas has updated its Myoelectric Prosthetic and Orthotic Components for the Upper Limb Medical Policy with the addition of an investigational statement for osseointegrated lower-limb prosthetic devices, with or without microprocessor control:
An osseointegrated upper-limb prosthetic device does not meet member benefit certificate primary coverage criteria that there be scientific evidence of effectiveness. For individuals with/without primary coverage criteria, an osseointegrated upper-limb prosthetic device is considered investigational. Investigational services are specific contract exclusions in most member benefit certificates of coverage.
AOPA has reached out to BCBS Arkansas with a request for additional information regarding this policy update—specifically, the implications of this policy for patients with osseointegrated implants and their access to prostheses and prosthetic services.
California
In light of the ongoing COVID-19 pandemic, the efforts of the California Orthotic and Prosthetic Association (COPA) toward increasing the Medicaid fee schedule have been put on hold. COPA’s Board of Directors has shifted its focus to protecting access to prostheses and orthoses for Medicaid beneficiaries, given the expected budgetary impacts as a result of the pandemic. The organization has scheduled meetings with state legislators.
For additional information, contact the COPA Board of Directors at admin@californiaoandp.com.
Kansas
AOPA has requested a medical review of BCBS of Kansas’s current Adjustable Cranial Orthoses for Positional Plagiocephaly and Craniosynostoses Medical Policy, citing contradictions in the policy language—similar to those in the Health Care Services Corp. policy successfully challenged by AOPA and others, and subsequently revised earlier this year.
New York
AOPA continues to work with the New York State Chapter of the American Academy of Orthotists and Prosthetists (NYSAAOP) to help O&P practices fight for change to the orthotics and prosthetics Medicaid fee schedule, which is more than 33 years old. Members of NYSAAOP have secured two state legislators to champion efforts to raise the Medicaid fee schedule for O&P. To learn more about how you can get involved, email ted@carecrafters.com.
Submit Your State News
To submit an update for publication in the State by State department of O&P Almanac, email awhite@AOPAnet.org.
DATA AT YOUR FINGERTIPS


Access comprehensive, easy-to-use, easy-to-read Medicare Part B orthotic and prosthetic claims data from the last five years in a matter of minutes. The data is updated annually to ensure you have the most recent data at your fingertips.
NEW!
Resources include:
Understand the current market in terms of size, geographic distribution, and provider specialty Predict growth and opportunities Compare historical and projected growth rates in Medicare Identify new opportunities.

We ARE AOPA ADVOCACY | RESEARCH | EDUCATION


