ARCHIVE
Academic and Research Archive

All the works published in this volume are the submitted works of AMSA-UPN members from 9 -

All the works published in this volume are the submitted works of AMSA-UPN members from 9 -



All the works published in this volume are the submitted works of AMSA-UPN members from 9 -

All the works published in this volume are the submitted works of AMSA-UPN members from 9 -


Greetings, People of Tomorrow!
AMSA UPN adalah organisasi yang bersifat keilmuan, nonpolitik, non sectarian, nonprofit, dan terbuka yang berlandaskan filosofi Knowledge, Action, dan Friendship. AMSA UPN tidak hanya terfokus pada isu kesehatan yang ada di sekitar, namun terfokus juga pada perkembangan setiap membernya.

Pada kesempatan kali ini, AMSA UPN, divisi ARC, mengeluarkan ARCHIVE Vol. dengan tujuan untuk memaksimalkan aspek Knowledge pada setiap member. Diharapkan ARCHIVE Vol. dapat memberikan bekal kepada setiap member untuk berlatih menghadapi dunia kedokteran yang kian berkembang dan membiasakan diri melakukan penelitian maupun literasi jurnal
Melalui publikasi ARCHIVE Vol , AMSA UPN hadir untuk membantu proses pembuatan publikasi ilmiah maupun cabang lomba lainnya pada saat member ingin berpartisipasi dalam perlombaan
Saya ingin memberikan rasa terima kasih yang sebesar besarnya kepada Yudivaniel Zihono sebagai Executive Board of ARC, Theresia Leonita sebagai Vice Executive Board of ARC, seluruh member ARC, dan kontributor karya yang sudah dicantumkan pada ARCHIVE Vol. , karena jerih payah individu yang sudah saya sebutkan sebelumnya, ARCHIVE Vol. dapat dipublikasikan dengan baik.
Terima Kasih AMSA UPN. "Exploring Ability, Boost to Infinity" Viva AMSA!
Representative of AMSA-UPN Universitas Pembangunan Nasional Veteran JakartaGreetings, People of Tomorrow!
Buku Academic, Research, and Creative Archive atau disingkat sebagai ARCHIVE merupakan program kerja AMSA-UPN dengan tujuan memberikan dorongan pada member AMSA-UPN untuk membuat karya. ARCHIVE juga berfungsi sebagai arsip dari karya-karya member AMSA-UPN yang sudah pernah dikirimkan untuk lomba dan submisi karya di AMSA, seperti Pre-Conference Competition East Asian Medical Students' Conference (PCC EAMSC), Indonesia Medical Students' Training and Competition (IMSTC), Pre-Conference Competition Asian Medical Students' Conference (PCC AMSC), AMSA International Summit, National Research Proposal Competition (NRPC), R-Ticles, dan kompetisi yang diselenggarakan oleh AMSA-Universitas.
Edisi kali ini merupakan edisi pertama dari ARCHIVE dan sudah berhasil mengumpulkan karya dari berbagai cabang lomba dan submisi seperti Scientific Paper, Scientific Poster, Public Poster, Photography, dan Research Proposal. Kami harap dengan adanya edisi pertama ini, akan ada semakin banyak member AMSA-UPN yang tertarik untuk membuat karyanya dan mengikuti lomba di AMSA.
Saya juga ingin mengucapkan terima kasih kepada seluruh member AMSA-UPN yang sudah mengikuti kompetisi dan submisi karya di AMSA, Executive Board AMSA-UPN, Vice Executive Board divisi ARC, dan seluruh pihak yang berkontribusi dalam pembuatan ARCHIVE. Tanpa bantuan dari seluruh pihak tersebut, ARCHIVE tidak akan mungkin terbentuk dan menginspirasi member AMSA-UPN untuk mengembangkan kemampuan akademik dan penelitiannya.

"Exploring Ability, Boost to Infinity" Viva AMSA!
 Head of ARC Division AMSA-UPN Universitas Pembangunan Nasional Veteran Jakarta
Yudivaniel Zihono
Head of ARC Division AMSA-UPN Universitas Pembangunan Nasional Veteran Jakarta
Yudivaniel Zihono

HUBUNGAN KONSUMSI KATERING DIET SEHAT TERHADAP PERUBAHAN KOMPOSISI TUBUH PADA MAHASISWA PROGRAM STUDI KEDOKTERAN DI DKI JAKARTA
Proposal NRPC AMSA Indonesia 2021/2022
Yudivaniel Zihono 1910211106
Rahayu Dewi Kusumawardhani 1910211051
Nadhila Sarasvati Buwana 1910211083
Theresia Leonita 2010211080
AMSA-Universitas Pembangunan Nasional Veteran Jakarta Asian Medical Students’ Association Indonesia (AMSA Indonesia) 2021




Puji syukur kami panjatkan kepada Tuhan Yang Maha Esa karena berkat rahmat Nya lah, peneliti dapat menyelesaikan proposal penelitian mengenai “Hubungan Konsumsi Katering Diet Sehat terhadap Perubahan Komposisi Tubuh pada Mahasiswa Program Studi Kedokteran” dengan segala keterbatasan yang ada. Proposal penelitian ini dibuat dalam rangka mengikuti kompetisi National Research Proposal Competition (NRPC) AMSA Indonesia. Dalam proses pembuatan proposal ini, peneliti dapat belajar banyak mengenai keadaan gizi masyarakat di Indonesia, tren katering diet sehat, serta pentingnya penyelesaian dari masalah gizi di Indonesia.
Kami sebagai peneliti menyadari kelemahan dan keterbatasan yang ada dalam proposal penelitian ini, sehingga kami meminta bimbingan dari dokter pem bimbing kami. Dengan bantuan tersebut, proposal penelitian ini dapat dilaksanakan untuk meningkatkan kesadaran dan pemahaman pada konsumsi katering diet sehat dalam memengaruhi perubahan komposisi tubuh di Indonesia.
Kami sebagai peneliti juga menyadari bahwa proposal ini masih jauh dari sempurna. Maka dari itu, kami mohon maaf sebesar besarnya apabila terdapat kesalahan kata. Kami sangat terbuka terhadap segala kritik dan saran demi menyempurnakan proposal penelitian ini, sehingga penelitian ini nantinya dapat dilaksanakan. Dengan demikian, kami berharap proposal ini dapat bermanfaat bagi peneliti dan pembaca.
LEMBAR PENGESAHAN ..................................................................................................... 2 HALAMAN PERNYATAAN ORISINALITAS ................................................................... 4 KATA PENGANTAR .............................................................................................................. 5 DAFTAR ISI............................................................................................................................. 6 DAFTAR TABEL .................................................................................................................... 8
DAFTAR GAMBAR ................................................................................................................ 9 DAFTAR LAMPIRAN .......................................................................................................... 10 PENDAHULUAN .................................................................................................................. 11
1.1. Latar Belakang ........................................................................................................ 11 1.2. Rumusan Masalah dan Pertanyaan Penelitian .................................................... 13 1.2.1. Rumusan Masalah ........................................................................................... 13 1.2.2. Pertanyaan Penelitian ...................................................................................... 13 1.3. Tujuan Penelitian .................................................................................................... 14 1.3.1. Tujuan Umum .................................................................................................. 14 1.3.2. Tujuan Khusus ................................................................................................. 14 1.4. Manfaat Penelitian .................................................................................................. 14 1.4.1. Bidang Pengabdian Masyarakat .................................................................... 14 1.4.2. Bidang Kesehatan Masyarakat ....................................................................... 14 1.4.3. Bidang Perekonomian ..................................................................................... 14 TINJAUAN PUSTAKA ......................................................................................................... 15 2.1. Tinjauan Pustaka .................................................................................................... 15 2.1.1. Overweight dan Obesitas.................................................................................. 15 2.1.2. Komposisi tubuh .............................................................................................. 16 2.1.3. Aktivitas Fisik .................................................................................................. 20 2.1.4. Diet Sehat .......................................................................................................... 21 2.1.5. Katering Diet Sehat.......................................................................................... 31 2.2. Kerangka Teori ....................................................................................................... 34 KERANGKA KONSEP ........................................................................................................ 35 METODE PENELITIAN ...................................................................................................... 36 4.1. Ruang Lingkup Penelitian ...................................................................................... 36 4.1.1. Tempat Penelitian ............................................................................................ 36 4.1.2. Waktu Penelitian .............................................................................................. 36
Tabel 1. Daftar Pangan Penukar Satu (1) Porsi Gula ........................................................ 26
Tabel 2. Daftar Makanan Bahan Penyedap Tinggi Natrium ............................................ 26
Tabel 3. Daftar Makanan Siap Saji Tinggi Natrium .......................................................... 26
Tabel 4. Daftar Pangan Penukar Satu (1) Porsi Minyak Lemak Tak Jenuh ................... 27 Tabel 5. Daftar Pangan Penukar Satu (1) Porsi Minyak Lemak Jenuh ........................... 27
Tabel 6. Anjuran Jumlah Porsi Menurut Kecukupan Energi untuk Kelompok Umur 19 29 tahun perorang perhari .................................................................................................... 30 Tabel 7. Angka Kecukupan Energi, Protein, Lemak, Karbohidrat, Serat, dan Air yang dianjurkan (per orang per hari) ........................................................................................... 31
Tabel 8. Deskripsi Distribusi Populasi Penelitian Menurut Sosio Demografis ................ 45 Tabel 9. Deskripsi Distribusi Populasi Penelitian Menurut Aktivitas Fisik, Keikutsertaan Katering Diet Sehat, dan Frekuensi Konsumsi Katering Diet Sehat ................................ 46 Tabel 10. Tabel Nutrisurvey Hasil Food Recall per 3x24 Jam .......................................... 47 Tabel 11. Tabel Nutrisurvey Hasil Food Recall per 30 hari .............................................. 47
Tabel 12. Perbedaan Rata-Rata Sebelum dan Sesudah Konsumsi Katering Diet Sehat pada Perubahan Komposisi Tubuh ...................................................................................... 47
Tabel 13. Hubungan Konsumsi Katering Diet dengan Perubahan Komposisi Tubuh ... 48
Tabel 14. Analisis Multivariat Variabel Bebas dan Perancu Terhadap Perubahan Komposisi Tubuh Setelah 30 Hari ....................................................................................... 48
Gambar 1. Tumpeng Gizi Seimbang .................................................................................... 29
Gambar 2. Piring Makanku: Sajian Sekali Makan ............................................................ 29
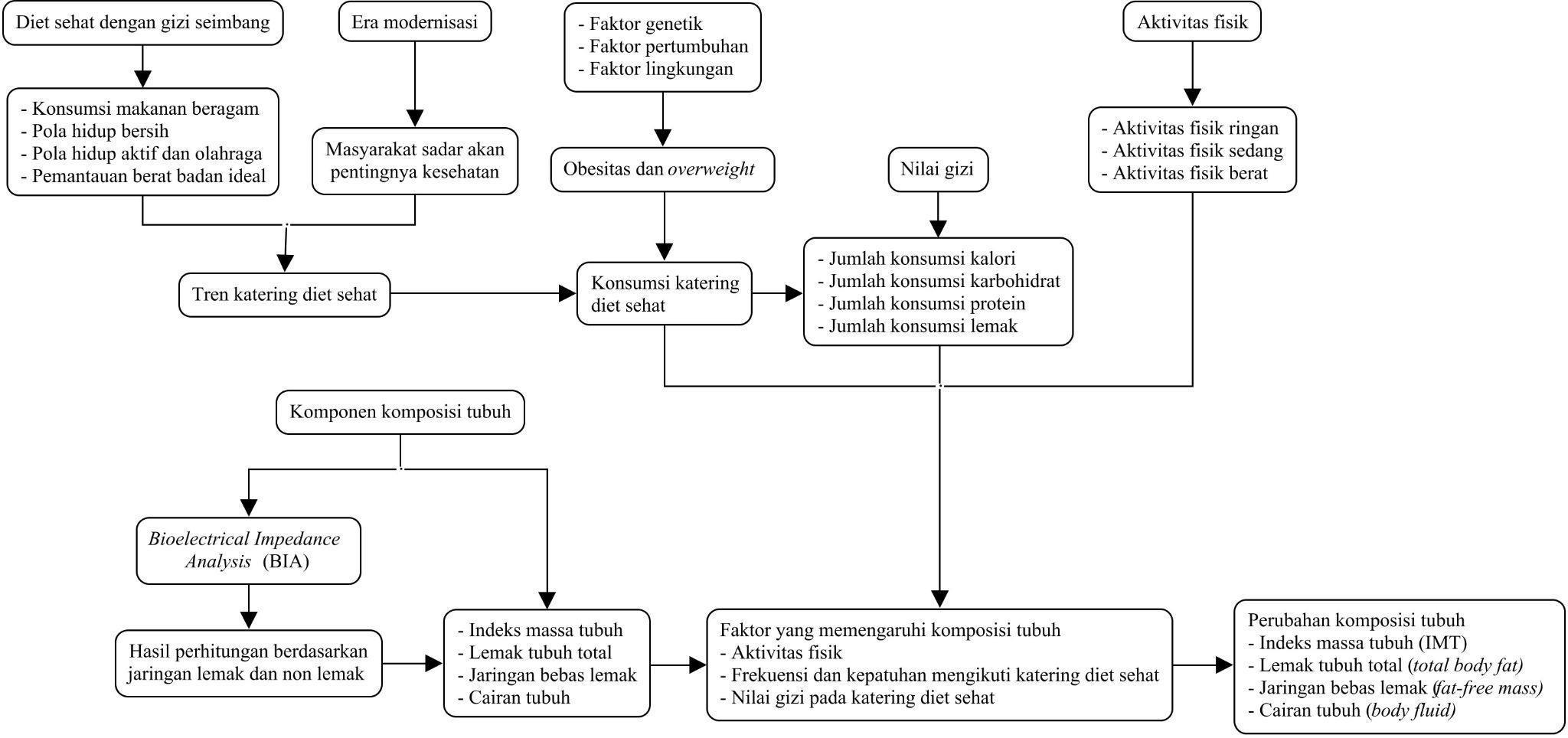
Gambar 3. Kerangka Teori Hubungan Konsumsi Katering Diet Sehat terhadap
Perubahan Komposisi Tubuh ............................................................................................... 34
Gambar 4. Kerangka Konsep Hubungan Konsumsi Katering Diet Sehat terhadap
Perubahan Komposisi Tubuh ............................................................................................... 35
Gambar 5. Cara Pengumpulan Data ................................................................................... 43
INFORMED CONSENT ........................................................................................................ 53
KUESIONER FREKUENSI KONSUMSI KATERING DIET SEHAT .......................... 54
KUESIONER AKTIVITAS FISIK ...................................................................................... 55
FORMULIR FOOD RECALL 24 JAM
Kondisi obesitas dan overweight adalah salah satu bentuk malnutrisi yang menjadi permasalahan dalam kesehatan masyarakat di negara berkembang seperti Indonesia. Kelebihan berat badan ini dapat menjadi risiko dalam berkembangnya penyakit lain yang dapat menurunkan kualitas hidup seperti penyakit jantung, darah tinggi, dan diabetes, yang secara tidak langsung dapat berdampak terhadap produktivitas masyarakat[1]. Menurut RISKESDAS, pada tahun 2013, prevalensi overweight pada usia >18 tahun di Indonesia sebesar 11,5% dan meningkat 2,1% menjadi 13,6% pada tahun 2018. Sedangkan, prevalensi obesitas pada usia >18 tahun menurut pada tahun 2013 meningkat enam persen dari 14,8% menjadi 21,8% pada tahun 2018[2]
Seiring dengan perkembangan teknologi di era globalisasi, mayoritas orang cenderung memilih gaya hidup yang lebih mudah dan cepat. Hal ini dapat mengubah seseorang menjadi malas bergerak yang merupakan sedentary lifestyle. Seseorang dengan gaya hidup tersebut akan cenderung memiliki hidup yang santai seperti duduk, membaca, berbaring, menonton televisi, dan lain-lain[3] Sedentary lifestyle dapat menyebabkan terjadinya penumpukan lemak tubuh karena kurangnya aktivitas sehingga mengakibatkan overweight dan obesitas. Bersamaan dengan terjadinya pandemi COVID 19 pada saat ini, mayoritas aktivitas sehari hari harus dilakukan secara daring sehingga mengurangi frekuensi dari aktivitas fisik yang normalnya dilakukan. Hal ini mengakibatkan sedentary lifestyle menjadi semakin marak terjadi pada masyarakat[4]. Khususnya gaya hidup ini banyak ditemukan di kota kota besar seperti DKI Jakarta[3].
Salah satu langkah yang dapat dilakukan untuk mencegah bentuk dari malnutrisi seperti obesitas dan overweight akibat sedentary lifestyle adalah melalui pola diet yang sehat. Pola diet sehat yang dapat dilakukan antara lain menyeimbangkan konsumsi kalori, membatasi konsumsi lemak, mengganti konsumsi lemak jenuh menjadi lemak tidak jenuh, menghindari lemak trans yang diproduksi secara industrial, dan membatasi asupan gula serta garam[5]. Namun, dengan berlangsungnya proses globalisasi yang pesat, terjadilah perubahan pola hidup yang memengaruhi dari pola makan. Sekarang ini masyarakat cenderung mengkonsumsi makanan tinggi akan energi, lemak, gula, dan
garam. Sedangkan makanan yang mengandung serat tinggi seperti buah, sayur, dan biji bijian lebih sedikit konsumsinya[5]
Dengan mempertimbangkan dari adanya perubahan pola makan akibat proses globalisasi dan juga meningkatnya sedentary lifestyle, muncul berbagai tren untuk mempertahankan pola makan sehat seperti katering diet sehat. Konsep dari katering diet sehat adalah pengiriman makanan rendah kalori setiap hari dengan memperhatikan kenyamanan konsumen agar tidak perlu repot mempersiapkan ataupun memikirkan makanan yang dikonsumsinya[6]. Perbedaan paling signifikan antara katering diet sehat dan katering makanan biasa adalah perhatiannya terhadap nutrisi dan kalori dengan klaim dapat mempertahankan status gizi sehat melalui penurunan berat badan. Namun, klaim mengenai perbaikan status gizi ini masih perlu diteliti lebih lanjut dan tidak hanya berdasarkan dari penurunan berat badan.
Salah satu aspek yang dapat menentukan secara akurat dari status gizi dan penurunan berat badan adalah komposisi tubuh. Komposisi tubuh sendiri meliputi massa lemak dan massa bebas lemak, tidak semata mata dari berat badan dan Indeks Massa Tubuh (IMT) saja. IMT tidak selalu berbanding lurus dengan massa lemak dan massa bebas lemak sehingga tidak dapat memberikan gambaran keadaan obesitas yang sesuai pada seluruh populasi. Sebagai contoh binaragawan memiliki persentase massa lemak yang normal tetapi memiliki berat badan yang berlebih. Sedangkan terdapat individu yang memiliki persentase massa lemak tinggi namun memiliki IMT dalam batas normal, contohnya pada skinny fat. Beberapa studi yang sudah ada hanya mengacu pada IMT dan hanya memberikan gambaran secara umum mengenai kegemukan dan tidak banyak studi yang membahas mengenai komposisi tubuh[7]. Umumnya konsumen katering diet sehat berasal dari kalangan dengan tingkat ekonomi menengah ke atas yang memiliki penghasilan cukup untuk berlangganan katering tersebut. Kalangan seperti mahasiswa kedokteran termasuk ke dalam kelompok yang mayoritas termasuk ke status perekonomian menengah ke atas. Selain itu, dengan jadwal kuliah yang cenderung lebih sibuk dari mahasiswa lain dalam kegiatan akademiknya, mahasiswa kedokteran menjadi salah satu kelompok yang dapat diuntungkan dan memiliki kecenderungan untuk berlangganan katering diet sehat dalam rangka memenuhi kebutuhan gizi di tengah kesibukannya. Kelompok mahasiswa kedokteran juga cenderung memiliki aktivitas fisik yang relatif sama berdasarkan dari pengalaman dan observasi peneliti yang aktivitasnya tidak memerlukan banyak gerak tubuh. Hal tersebut dapat dikategorikan dalam sedentary lifestyle
Oleh karena itu, hubungan antara konsumsi katering diet sehat terhadap perubahan komposisi tubuh akan peneliti fokuskan pada mahasiswa kedokteran yang termasuk dalam kelompok yang memenuhi mayoritas ciri konsumen katering diet sehat yaitu yang status ekonominya menengah ke atas, dilanda kesibukan, dan ce nderung memiliki sedentary lifestyle, sehingga hal ini menjadi suatu perhatian yang perlu diteliti lebih lanjut. Penelitian ini bertujuan untuk membuktikan apakah katering diet sehat dapat menjadi salah satu opsi alternatif untuk memenuhi kebutuhan diet pa da masyarakat dan menimbulkan perbaikan pada status gizi melalui perubahan komposisi tubuh.
1.2.1. Rumusan Masalah
Dengan meningkatnya prevalensi obesitas dan overweight, masyarakat semakin sadar akan kebutuhan diet sehat. Pada era modern ini, banyak orang yang memilih katering diet untuk memenuhi diet sehatnya. Namun, tidak diketahui secara pasti kualitas diet pada katering diet sehat tersebut dalam memengaruhi perubahan komposisi tubuh seseorang. Oleh karena itu, perlu diketahui hubungan konsumsi katering diet sehat terhadap perubahan komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta.
1.2.2. Pertanyaan
1. Apakah konsumsi katering diet sehat memiliki hubungan terhadap perubahan komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta?
2. Apa bentuk perubahan komposisi tubuh yang terjadi setelah mengonsumsi katering diet sehat pada mahasiswa kedokteran di DKI Jakarta?
3. Bagaimana komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta?
4. Bagaimana tingkat konsumsi katering diet sehat pada mahasiswa kedokteran di DKI Jakarta?
5. Bagaimana nilai gizi dalam katering diet sehat dan menu makanan sehari hari mahasiswa kedokteran di DKI Jakarta?
6. Apakah nilai gizi dalam katering diet sehat yang dikonsumsi mahasiswa kedokteran di DKI Jakarta dapat memenuhi kebutuhan gizi?
1.3.1. Tujuan Umum
Untuk mengetahui apakah ada hubungan antara konsumsi katering diet sehat terhadap perubahan komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta.
1.3.2. Tujuan Khusus
1. Untuk mengetahui hubungan konsumsi katering diet sehat terhadap perubahan komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta.
2. Untuk mengetahui bentuk perubahan komposisi tubuh setelah mengonsumsi katering diet sehat pada mahasiswa kedokteran di DKI Jakarta.
3. Untuk mengetahui komposisi tubuh pada mahasiswa kedokteran di DKI Jakarta.
4. Untuk mengetahui tingkat konsumsi katering diet sehat pada masyarakat di DKI Jakarta.
5. Untuk mengetahui nilai gizi dalam katering diet sehat dan menu makanan sehari hari mahasiswa kedokteran di DKI Jakarta.
6. Untuk mengetahui pemenuhan kebutuhan gizi dalam katering diet sehat yang dikonsumsi mahasiswa kedokteran di DKI Jakarta.
1.4.1. Bidang Pengabdian Masyarakat
Meningkatkan kesadaran masyarakat DKI Jakarta akan pentingnya pola hidup sehat guna mempertahankan status gizi sehat.
1.4.2. Bidang Kesehatan Masyarakat
Mencari solusi alternatif untuk memperbaiki angka malnutrisi pada masyarakat DKI Jakarta.
1.4.3. Bidang Perekonomian
Meningkatkan potensi perkembangan bisnis makanan katering diet sehat.
2.1.1.
Menurut WHO (2020), malnutrisi didefinisikan sebagai kekurangan, kelebihan, maupun ketidakseimbangan pada konsumsi energi atau nutrisi[8]
Salah satu jenis malnutrisi adalah kelebihan konsumsi energi atau nutrisi, sering disebut sebagai overweight dan obesitas.
Obesitas sendiri adalah kejadian akumulasi lemak berlebih sehingga bisa menjadi suatu risiko yang menyebabkan berbagai gangguan kesehatan. Sedangkan overweight merupakan keadaan yang mendekati obesitas. Seseorang dapat dikategorikan sebagai overweight ketika beratnya melebihi batas tinggi pada umumnya. Selain overweight. Untuk pengukurannya biasa menggunakan perhitungan Indeks Massa Tubuh (IMT). Pada usia dewasa, seseorang disebut overweight bila IMT nya berjumlah 23 24.9, sedangkan obesitas pada 25 ke atas[9]
Obesitas dan overweight memiliki banyak penyebab seperti faktor genetik, tidak adekuatnya sumber makanan yang dikonsumsi, dan lingkungan yang menginduksi kebiasaan tertentu yang mengubah pola makan. Semua faktor di atas sangat berperan dalam meningkatkan angka malnutrisi[10].
a. Faktor genetik
Pada beberapa orang, genetik dapat memengaruhi adanya malnutrisi. Pada keluarga yang memiliki riwayat overweight maupun obesitas, kemungkinan untuk terjadinya gangguan tersebut pada keturunannya cukup tinggi. Hal tersebut bisa disebabkan karena adanya mutasi pada gen leptin, membuat seseorang mengalami rasa lapar yang berlebih[10]
b. Faktor pertumbuhan
Kebiasaan makan juga sangat memengaruhi dari risiko terjadinya malnutrisi. Kebiasaan makan yang tidak baik yang sejak masa kecil dapat berlanjut dan menyebabkan kebiasaan makan yang kurang baik juga saat dewasa. Kebiasaan makan ini seringkali diatur oleh orang tua. Hal ini menyebabkan anak anak merasa tertekan dan tidak dapat mengonsumsi makanan secara leluasa. Akibatnya, ketika anak beranjak dewasa dan
memiliki kebebasan untuk memilih makanan yang akan dikonsumsi, mereka akan memilih untuk mengonsumsi makanan yang diinginkan walaupun tidak memiliki kandungan gizi yang adekuat[10].
c. Faktor lingkungan
Lingkungan sekitar juga berperan dalam bagaimana seseorang memilih makanan yang ingin dikonsumsinya. Saat ini sudah banyak jenis makanan cepat saji yang terjangkau dan lebih mudah untuk didapatkan. Selain itu, kebiasaan hidup sedentari juga memengaruhi kadar energi yang digunakan. Kebiasaan konsumsi makanan yang mengandung gula juga dapat berperan dalam terjadinya overweight dan obesitas[10]
1. Definisi Komposisi Tubuh
Komposisi tubuh terdiri dari komponen berat tubuh seseorang yang mencangkup jaringan non lemak serta jaringan lemak. Evaluasi status kesehatan seseorang dapat dilakukan dengan penilaian komposisi tubuh. Terdapat empat komponen dari komposisi tubuh, yaitu jaringan bebas lemak (fat free mass), jaringan lemak tubuh total (total body fat), cairan tubuh (body fluid) dan mineral tulang (bone mineral) Menurut WHO terdapat 4 komposisi kompleks dari komposisi tubuh manusia yaitu:
a. Komposisi atomik
Komposisi ini merupakan akumulasi enam elemen yaitu hidrogen, oksigen, karbon, nitrogen, fosfor dan kalsium. Selain itu terdapat juga sulfur, kalium, natrium, klorida, magnesium sebesar 2% dari berat badan dan 40 elemen lain dengan jumlah <10 gram[11].
b. Komposisi molekular
Komponen molekular dibagi menjadi lima kategori, yaitu protein, lemak, glikogen, air, dan mineral. Namun, secara sederhana dibedakan menjadi massa lemak dan massa bebas lemak.
c. Komposisi selular
Terdapat tiga komponen dari komposisi selular yaitu massa sel tubuh, cairan ekstrasel, dan bagian pada ekstrasel.
d.
Jaringan terbentuk dari kumpulan dari sel sel dan nantinya jaringan jaringan tersebut akan membentuk organ tubuh (jaringan adiposa, tulang, otot skeletal, kulit, dan organ visceral lainnya).
Penilaian komposisi tubuh secara kasar dapat menggunakan indeks massa tubuh (IMT), tetapi pengukuran IMT dinilai kurang akurat dalam menentukan berat tubuh yang sehat. Metode yang paling akurat untuk menilai komposisi tubuh adalah dengan menimbang berat di bawah air. Penilaian ini didasarkan bahwa jaringan non lemak lebih padat dibanding air dan jaringan lemak kurang pada dibanding air. Komposisi tubuh kemudian akan ditentukan dengan persamaan dalam persentase antara lemak dengan densitas tubuh[12]
Lemak, otot, cairan badan, kerangka merupakan komposisi tubuh yang nilainya dapat berubah. Seiring dengan modernisasi dan pola hidup sedentari, energi yang dikeluarkan menurun karena berkurangnya aktivitas fisik. Penurunan energi ini menyebabkan persentase lemak dalam komposisi tubuh semakin membesar. Aktivitas fisik memiliki pengaruh terhadap komposisi tubuh, ketika seseorang cenderung jarang melakukan kerja fisik akan terjadi penimbunan lemak yang nantinya akan mengakibatkan peningkatan berat badan.
a. Lemak Tubuh Total (Total Body Fat)
Massa lemak tubuh memiliki pengaruh terhadap tingkat kebugaran seseorang. Komposisi lemak tubuh yang diukur adalah persentase lemak tubuh total dan lemak viseral[13]. Normalnya orang dewasa memiliki persentase lemak tubuh total sebesar 20 25% untuk perempuan dan untuk laki laki 15 25% dari total berat badan[14]
Lemak visceral atau lemak organ merupakan lemak yang diakumulasi dalam jaringan adiposa area rongga perut. Lemak viseral dapat melekat pada organ organ di dalam rongga perut jika terakumulasi. Normalnya lemak viseral pada orang dewasa bernilai 1 9, bernilai tinggi pada 10 14, dan bernilai sangat tinggi pada 15 30[15]. Jika nilainya melebihi akan menimbulkan obesitas sentral dan peningkatan risiko penyakit degeneratif. Total persentase massa bebas lemak dan massa lemak
tubuh dapat menjadi petunjuk mengenai status gizi seorang individu serta sebagai parameter apakah seseorang beresiko memiliki suatu penyakit yang berhubungan dengan status gizi.
b. Massa Bebas Lemak (Fat Free Mass)
Massa bebas lemak atau fat free mass (FFM) merupakan massa non lemak yang terdiri dari massa otot rangka yang pada laki laki bernilai 33.3% 39.3%, pada perempuan bernilai 24.3% 30.3% [16], mineral 6.8%, dan cairan tubuh 73.8% serta memiliki densitas 1.1g/cm[14]. FFM dipengaruhi oleh faktor usia, jenis kelamin, dan juga kebugaran fisik seseorang[17]
Berdasarkan penelitian, terdapat perbedaan indeks massa bebas lemak antara jenis kelamin perempuan dan laki laki, yaitu laki laki cenderung memiliki nilai yang lebih tinggi dibanding dengan perempuan pada kategori usia remaja sehat 10 14 tahun. Indeks massa bebas lemak bersamaan dengan indeks massa lemak dapat membedakan individu individu yang, misalnya, dengan nilai BMI tinggi dan, secara bersamaan, menunjukkan indeks massa bebas lemak yang rendah dan indeks massa lemak tinggi (kelebihan berat badan atau obesitas), dan mereka yang juga dengan BMI tinggi tetapi indeks massa bebas lemak tinggi dan indeks massa lemak yang rendah (hipertrofi otot, yang cukup sering terjadi pada remaja laki laki)[18].
Persentase cairan tubuh merupakan salah satu komposisi tubuh manusia yang berperan dalam berbagai fungsi seperti metabolisme, transportasi substrat, homeostasis seluler, pengaturan suhu, dan lain lain[19]. Pada orang dewasa terdapat sekitar 60% air dari total berat badan tubuh. Namun, faktor ini bervariasi sesuai dengan jenis kelamin, usia, dan komposisi tubuh secara keseluruhan. TBW sendiri dibagi menjadi dua pembagian utama yaitu cairan intraseluler (ICF) dan cairan ekstraseluler (ECF)[20].
Persentase cairan tubuh biasanya dikaitkan dengan persentase lemak, sehingga berkontribusi ke status obesitas[19]. Hal ini terjadi karena jaringan adiposa mengandung lebih sedikit air dibandingkan
dengan jaringan lain, sehingga akan ada perbedaan antara Total Body Water (TBW) antara individu kurus dengan individu obesitas[20]
3. Perhitungan Komposisi Tubuh berdasarkan Bioelectrical Impedance Analysis (BIA)
Salah satu cara termudah untuk mengukur komposisi tubuh adalah dengan menggunakan timbangan Bioelectrical Impedance Analysis (BIA). Prinsip dari BIA adalah dengan mengalirkan arus bolak balik (AC) dengan frekuensi tertentu ke tubuh manusia. Kemudian dari arus bolak balik tersebut didapatkan suatu tegangan yang dapat diukur untuk mengetahui besar nilai impedansi tubuh [21]
Pengukuran komposisi tubuh menggunakan BIA ini memodelkan tubuh manusia bak suatu rangkaian yang terdiri dari resistor dan juga kapasitor. Sel pada tubuh manusia yang dapat diibaratkan sebagai resistor diantaranya adalah membran sel yang terdiri dari cairan seperti cairan ekstraseluler dan cairan intraseluler. Membran sel tersebut sifatnya konduktif sehingga bisa merepresentasikan resistor pada tubuh manusia. Sementara membran sel yang terdiri dari lemak memiliki sifat non konduktif dan menjadi kapasitor dalam tubuh manusia. Saat arus bolak balik dialirkan pada frekuensi tertentu ke tubuh manusia, akan didapatkan tegangan dan impedansi sehingga dapat mengukur dari komposisi lemak dan non lemak pada tubuh. Persamaan yang melambangkan hubungan antara arus yang dialirkan, impedansi tubuh, dan tegangan yang dihasilkan pada BIA ini dapat dilihat di bawah [21] .
� = � �
Keterangan:
Z = Impedansi tubuh (ohm)
V = Tegangan yang dihasilkan (volt)
I = Arus yang dialirkan (ampere)
1.
Aktivitas fisik adalah suatu gerakan tubuh yang terjadi akibat kerja otot rangka sehingga adanya peningkatan pengeluaran energi. Aktivitas yang dilakukan mencangkup segala aktivitas di kehidupan keseharian mulai dari aktivitas di sekolah, rumah tangga, lingkungan kerja, maupun pada waktu senggang. Secara umum, aktivitas fisik yang dikategorikan berdasarkan intensitas dan besaran kalori dibagi menjadi tiga yaitu ringan, sedang, berat[22].
a. Aktivitas fisik ringan
Aktivitas ini memerlukan tenaga yang sedikit dan umumnya tidak memberikan perubahan dalam laju pernapasan. Saat melakukan aktivitas fisik yang ringan seorang individu masih dapat menyanyi dan berbicara dengan jelas. Rata rata energi yang dilepaskan selama melakukan aktivitas fisik ringan adalah < 3.5 kcal/menit. Sebagai contoh yang termasuk aktivitas ringan adalah berjalan santai dan duduk bekerja di depan komputer[23].
b. Aktivitas fisik sedang
Aktivitas fisik yang akan menyebabkan tubuh sedikit berkeringat, serta peningkatan laju pernapasan dan denyut jantung. Ketika melakukan aktivitas ini seorang individu masih dapat berbicara, tapi tidak bisa bernyanyi dengan jelas. Rata rata energi yang dilepaskan saat melakukan aktivitas fisik sedang adalah 3.5 - 7 kcal/menit. Sebagai contoh aktivitas sedang adalah berjalan cepat (kecepatan < 5 km/jam), memindahkan perabot perabot ringan, dan olahraga rekreasional seperti bulu tangkis, tenis meja, dansa, serta bersepeda pada lintasan datar[24].
c. Aktivitas fisik berat
Aktivitas fisik yang saat dilakukan tubuh akan mengeluarkan banyak keringat, serta ada peningkatan tinggi dari denyut jantung dan laju pernapasan sampai bisa kehabisan napas. Rata rata energi yang dilepaskan ketika melakukan aktivitas berat adalah > 7 kcal/menit. Sebagai contoh aktivitas berat adalah berjalan sangat cepat (kecepatan
> 5 km/jam), berjalan mendaki bukit, mengangkut barang berat, serta bermain olahraga seperti bersepeda dengan lintasan mendaki, bola basket, badminton kompetitif, dan sepak bola[25].
3. Hubungan Aktivitas Fisik dengan Komposisi Tubuh
Aktivitas fisik memiliki kaitan dengan IMT, persentase lemak tubuh, dan angka kejadian obesitas[14]. Rendahnya aktivitas fisik merupakan masalah yang dapat menyebabkan penumpukan massa lemak tubuh dan perubahan berat badan. Peningkatan massa lemak dapat meningkatkan resiko terhadap berbagai penyakit degeneratif. Selain dari berat badan, aktivitas fisik juga memengaruhi dari komposisi tubuh, khususnya pada massa lemak dan massa bebas lemak. Namun, perubahan berat badan tidak selalu membuahkan hasil yang sebanding dengan status komposisi tubuhnya. Individu yang IMT nya diklasifikasikan sebagai overweight bisa saja memiliki massa lemak tubuh yang dalam batas normal, contohnya seperti pada binaragawan yang massa ototnya lebih tinggi. Oleh karena itu, frekuensi dan jenis aktivitas fisik yang dilakukan seorang individu dapat memengaruhi komposisi tubuh dalam cara yang berbeda beda[7]
1. Definisi Makanan, Nutrisi, dan Zat Gizi Makanan adalah segala sesuatu yang dimakan atau diminum, yang dapat memenuhi kebutuhan energi, sebagai zat pembangun, pengatur, dan perlindungan terhadap tubuh. Asupan jenis dan jumlah makanan yang tepat dapat memastikan kebutuhan nutrisi yang baik sehingga dapat memelihara kesehatan tubuh, yang dapat dilihat dari penampilan, efisiensi, dan kesejahteraan emosional seseorang.
Nutrisi didefinisikan sebagai makanan yang bekerja di dalam tubuh. Nutrisi mencakup segala hal yang terjadi sejak makanan dimakan sampai digunakan untuk berbagai fungsi fisiologis dalam tubuh. Terdapat lebih dari 40 nutrisi penting yang disediakan oleh suatu makanan dan pada akhirnya digunakan untuk menghasilkan ribuan zat yang diperlukan untuk kehidupan dan kebugaran fisik[26 27]
Zat gizi merupakan komponen makanan yang dibutuhkan oleh tubuh dengan jumlah yang cukup untuk tumbuh, berkembang, dan menjalani
kehidupan yang sehat. Zat gizi meliputi air, protein, lemak, karbohidrat, mineral, dan vitamin. Studi mengenai ilmu gizi berkaitan erat dengan nutrisi apa yang dibutuhkan oleh tubuh, berapa jumlah yang dibutuhkan, alasan seseorang membutuhkannya dan di mana bisa mendapatkannya[26].
Diet mengacu pada makanan atau minuman apa pun yang seseorang konsumsi setiap hari. Termasuk dalam hal ini adalah diet normal yang seseorang konsumsi dan diet yang dikonsumsi orang secara berkelompok (diet asrama). Diet juga dapat diaplikasikan pada orang sakit dengan memodifikasinya dan diterapkan dalam bagian terapi mereka (diet terapeutik). Sedangkan menurut WHO, definisi sehat mengacu pada kondisi tubuh yang sehat, baik bebas dari penyakit, kebugaran fisik, mental maupun emosional[26].
Diet yang cukup dan seimbang didefinisikan sebagai menyediakan dalam jumlah cukup semua nutrisi penting yang berguna dalam memenuhi kebutuhan seseorang. Nutrisi yang cukup, optimal, dan baik menunjukkan bahwa asupan zat gizi esensial sudah tepat jumlah dan proporsinya. Hal ini juga menyiratkan bahwa penggunaan nutrisi tersebut dalam tubuh berjalan dengan baik sehingga tingkat tertinggi kesehatan fisik dan mental dipertahankan sepanjang siklus hidup[26].
Diet yang baik memerlukan pengetahuan yang baik pula terhadap ilmu gizi itu sendiri. Perawatan gizi (Nutritional Care) adalah penggunaan pengetahuan gizi tersebut dalam perencanaan makanan dan persiapan makanan dengan cara yang dapat diterima dan menarik untuk diet seseorang. Hal ini melibatkan penilaian pola makan yang ada dan memperbaikinya dengan cara yang dapat diterima. Sedangkan perencanaan gizi bersifat individual supaya sesuai dengan kebutuhan dan latar belakang orang tersebut[26].
Seseorang yang menjalani diet membutuhkan rencana untuk memilih pola makan yang cukup sederhana dan menarik sehingga semua orang termasuk pelajar muda dan juga anggota keluarga yang lanjut usia dapat memahami dan mengikutinya. Para ahli gizi telah menyusun perencanaan praktis tersebut, yang dikenal sebagai panduan makanan untuk diet sehat.
Hal ini akan membantu memastikan nutrisi yang baik melalui pemilihan makanan yang tepat[26 27]
Menurut Kemenkes RI (2014), diet sehat dan seimbang dapat dilakukan melalui pemenuhan gizi seimbang dengan kalori seimbang. Zat gizi yang diperlukan untuk mencapai kondisi sehat antara lain karbohidrat, lemak, protein, mineral, dan vitamin. Kebutuhan akan zat gizi dan energi tersebut bergantung pada usia, jenis kelamin, berat serta tinggi badan, iklim, dan aktivitas fisik.
Pola makan adalah perilaku yang paling penting dalam pengaruhnya dengan keadaan gizi, karena asupan gizi dipengaruhi oleh jumlah dan kualitas dari makanan dan minuman yang berperan dalam kesehatan seseorang. Gizi yang baik dan seimbang berperan penting dalam terbentuknya berat badan yang normal dan membuat tubuh kebal terhadap penyakit infeksi[28 29]
Pola makan masyarakat sekarang ini belum mencerminkan rekomendasi pesan gizi seimbang[28 29]. Menurut Riskesdas (2013), 93,5% penduduk dengan usia > 10 tahun belum mengkonsumsi asupan sayuran dan buah buahan sesuai anjurannya. Selain itu, konsumsi protein per orang dan perhari yang sumbernya adalah protein nabati seperti sereal dan kacang kacangan, kualitas protein yang dikonsumsi tersebut dikategorikan rendah. Konsumsi makanan dan minuman dengan gula, garam, dan lemak yang tinggi pada masyarakat pun masih di atas anjuran. Pada bayi usia di bawah 6 bulan, asupan air per hari serta cakupan ASI eksklusifnya pun juga masih rendah[28 29] .
Beberapa faktor seperti kesediaan pangan dan pola makan bervariasi pada setiap negara. Oleh karena itu, panduan makan untuk suatu negara, contohnya adalah Basic Four yang digunakan oleh Amerika Serikat, tidak cocok jika diterapkan di negara lain, seperti India dan Indonesia yang memiliki perbedaan dalam pola makan dan kesediaan pangan[23, 25 26] . Pendidikan dan penyuluhan gizi di Indonesia dimulai dari prinsip 4 Sehat 5 Sempurna yang terinspirasi dari Basic Four Amerika Serikat dan dikenalkan oleh Prof. Poorwo Soedarmo yang merupakan Bapak Gizi Indonesia. Menu makanan ini meliputi makanan pokok, lauk pauk, sayuran
dan buah buahan, serta minum susu yang menjadikan menu tersebut sempurna[28 30]
Dengan adanya perkembangan ilmu dan masalah gizi yang berubah, slogan 4 Sehat 5 Sempurna sudah tidak relevan untuk diterapkan. Prinsip yang dihasilkan dari konferensi pangan sedunia (Roma, 1992), yaitu Nutrition Guide for Balanced Diet, dipercaya dapat menyelesaikan beban ganda gizi di Indonesia (kekurangan dan kelebihan gizi). Indonesia mengadopsinya dan dikenal sebagai Pedoman Gizi Seimbang[28 31] .
Pedoman Gizi Seimbang (PGS) merupakan susunan makanan harian yang terdiri atas berbagai zat gizi dalam jenis dan jumlah yang cukup untuk memenuhi kebutuhan tubuh. Gizi seimbang dalam PGS merujuk pada empat prinsip, yaitu keberagaman makanan, pola hidup bersih, aktivitas fisik dan olahraga, serta menjaga berat badan ideal. Konsep 4 sehat 5 sempurna memiliki perbedaan dengan PGS. Sebelumnya kebutuhan semua orang dari berbagai golongan disamaratakan, namun pada PGS tiap kelompok usia, jenis kelamin, status kesehatan, dan aktivitas fisik, memerlukan gizi yang menyesuaikan dengan kondisinya[31]
a. Mengonsumsi makanan beragam
Selain ASI untuk bayi 0-6 bulan, makanan lain tidak ada yang memiliki seluruh jenis zat gizi yang diperlukan untuk tubuh. Sebagai contoh sumber utama kalori yaitu nasi yang merupakan karbohidrat, tetapi kandungan vitamin dan mineralnya sedikit; sayur dan buah tinggi akan kandungan vitamin, mineral, dan serat, tetapi sedikit kalori dan protein[28 29]. Beberapa hal yang dapat dilakukan:
1) Banyak makan sayur dan cukup buah. Sayur dan buah adalah jenis makanan yang tinggi akan zat gizi berupa vitamin, mineral, dan serat pangan. WHO merekomendasikan konsumsi sayur dan buah setidaknya 400 g/orang/hari, yaitu 250 g sayur (2½ porsi/2½ gelas sayur setelah dimasak dan ditiriskan) dan 150 g buah (3 buah pisang ambon ukuran sedang/1½ potong pepaya ukuran sedang/3 buah jeruk ukuran sedang). Terdapat anjuran yang berlaku bagi orang Indonesia untuk mengkonsumsi sayur dan buah sebanyak 400 600 g/orang/hari bagi remaja dan orang dewasa. Sebaiknya porsi sayur
memenuhi ⅔ dari jumlah rekomendasi konsumsi sayuran dan buah.
2) Konsumsi sumber tinggi protein. Kelompok sumber protein hewani terdiri dari daging hewan kelompok ruminansia (daging kambing, daging sapi, daging rusa dll), daging unggas (daging bebek, daging ayam dll), ikan dan juga seafood, telur dan susu serta hasil olahan lain yang serupa. Sedangkan untuk kelompok sumber protein nabati didapatkan dari sumber seperti kacang kacangan dan hasil olahan yang serupa. Walaupun keduanya sama sama menyediakan protein, masing masing kelompok memiliki kelebihan dan kekuranganya. Oleh karena itu, kedua kelompok ini perlu dikonsumsi dengan kelompok pangan lain.
Kebutuhan protein hewani sejumlah 2 4 porsi, sama dengan 2 4 potong ukuran sedang daging sapi dengan berat 70 140 g; atau 2 4 potong ukuran sedang daging ayam dengan berat 80 160 g; atau 2 4 potong ikan ukuran sedang dengan berat 80 160 g dalam sehari. Protein nabati dibutuhkan sejumlah 2 4 porsi sehari, sama dengan 100-200 g atau 4-8 potong tempe ukuran sedang; atau 200400 g yang setara dengan 4 8 potong tahu ukuran sedang.
3) Variasikan makanan pokok.
Utamanya makanan pokok memiliki kandungan karbohidrat, selain itu dapat mengandung vitamin B1 (tiamin), B2 (riboflavin), dan mineral lainnya. Variasi ini bisa dilakukan dengan memilih makanan tinggi karbohidrat lain, seperti nasi merah, roti, jagung, dan kentang. Setidaknya pola makanan pokok yang beragam ini dilakukan dalam sehari atau sekali makan.
4) Kurangi dan batasi makanan tinggi gula, garam, dan lemak. Hal ini dikarenakan ketiga zat tersebut dapat menambah resiko penyakit tidak menular apabila dikonsumsi secara berlebihan. Zat tersebut banyak ditemukan pada kudapan manis padat energi dan makanan instan. Gula yang beredar di masyarakat juga berada pada makanan dengan karbohidrat sederhana lain (tepung, roti, kecap), buah
manis, jus, dan soda. Gula tersebut tidak hanya terdapat pada gula yang umum diketahui seperti gula tebu dan gula aren. Satu porsi gula tebu atau yang biasa dikenal dengan gula pasir dengan takaran satu sendok makan (10 gram) memiliki kandungan gizi 37 kalori dan 9 gram karbohidrat.
Tabel 1. Daftar Pangan Penukar Satu (1) Porsi Gula
Umumnya masyarakat mengonsumsi garam (NaCl) yang berasal dari garam dapur/meja. Apabila konsumsi natrium terlalu berlebihan dapat meningkatkan risiko peningkatan tekanan darah.
Tabel 2. Daftar Makanan Bahan Penyedap Tinggi Natrium


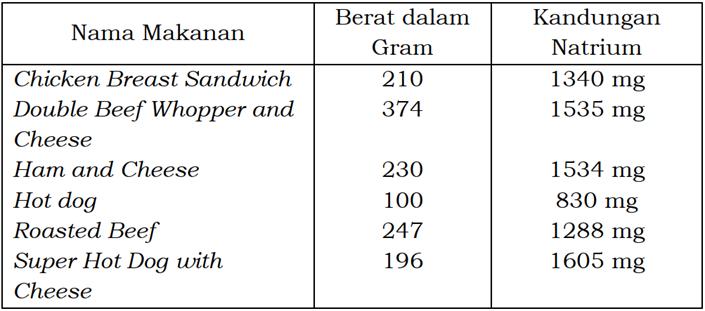
Tabel 3. Daftar Makanan Siap Saji Tinggi Natrium
Rekomendasi konsumsi lemak dan minyak adalah < 25% dari kebutuhan energi. Konsumsi lemak yang melebihi persentase rekomendasi ini dapat menyebabkan pengurangan konsumsi makanan lain dan menimbulkan sensasi kenyang yang lebih lama.
Hal ini dikarenakan pada sistem pencernaan lemak akan bertahan lebih lama dibanding protein dan karbohidrat. Menurut kandungan asam lemaknya, minyak memiliki 2 kelompok:
a) Lemak Tak Jenuh
Satu satuan penukar mengandung 50 Kkal dan 5 gram lemak. Tabel 4. Daftar Pangan Penukar Satu (1) Porsi Minyak Lemak Tak Jenuh
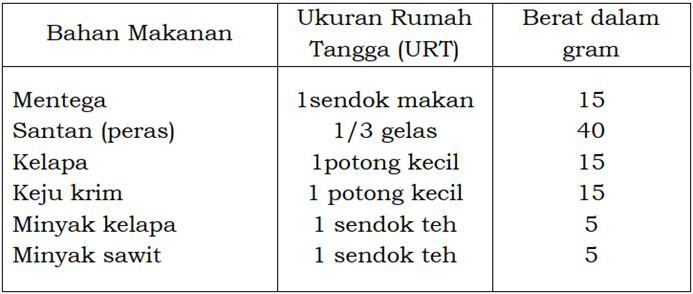
b) Lemak Jenuh

Satu satuan penukar mengandung 50 Kkal dan 5 gram lemak. Tabel 5. Daftar Pangan Penukar Satu (1) Porsi Minyak Lemak Jenuh
5) Biasakan sarapan. Jika menyukai cemilan, sebaiknya porsi sarapan dibuat menjadi ¼ dari total makanan dalam satu hari. Apabila tidak, porsi sarapan sebaiknya memenuhi setidaknya ⅓ dari total makanan dalam satu harinya.
6) Minum air putih yang cukup. Sebaiknya meminum sekitar delapan gelas setiap hari untuk mencegah dehidrasi.
7) Perhatikan label pada kemasan makanan. Hal ini bertujuan agar dapat mengontrol pemilihan dalam konsumsi produk makanan olahan menurut kandungan gizinya.
b. Pola hidup bersih
Pola hidup bersih diperlukan untuk menghindarkan seseorang terhadap sumber infeksi dan penyakit infeksius itu sendiri.
c. Pola hidup aktif dan olahraga
Aktivitas fisik berperan dalam memperlancar metabolisme dalam tubuh sehingga berhubungan erat dengan pemenuhan gizi seimbang.
d. Pemantauan berat badan ideal
Berat badan normal diartikan sebagai berat badan yang proporsional terhadap tinggi badannya, ia merupakan suatu indikator keseimbangan zat gizi di dalam tubuh yang disebut dengan Indeks Massa Tubuh (IMT). Oleh karena itu, pemantauan berkala terhadap berat badan khususnya untuk memastikan masih dalam batas IMT normal harus dijadikan bagian dari pola hidup dengan gizi seimbang. Secara global, suatu panduan pangan (Food Guide) divisualisasikan dengan gambar atau bentuk seperti gasing, piramida, pagoda, dan sebagainya, hal ini mengikuti nilai yang sedang berkembang di negara masing masing. Indonesia sendiri memiliki dua visual Gizi Seimbang, yaitu Tumpeng Gizi Seimbang dan Piring Makanku, Sajian Sekali Makan[28 29]
Tumpeng Gizi Seimbang merupakan sebuah penjelasan tentang panduan ukuran atau porsi makanan dan minuman disertai aktivitas fisik, termasuk pola hidup bersih dan pemantauan berat badan. Empat lapis yang terdapat pada visualisasi ini memiliki arti bawah Gizi Seimbang berdasar pada 4 pilar yaitu konsumsi pangan yang beraneka ragam, aktivitas fisik, pola hidup bersih, dan pemantauan berat badan ideal. Lapisan bawah ke atas berurutan dari makanan pokok yang paling besar sampai gula, garam, dan lemak yang paling kecil. Hal ini menunjukkan porsi yang dibutuhkan setiap orang perharinya[28 29] .
Gambar 1. Tumpeng Gizi Seimbang Visualisasi Piring Makanku, Sajian Sekali Makan digunakan sebagai panduan bagi masyarakat untuk menyajikan makanan dan minuman mereka setiap kali makan. Setengah dari piring, yang berarti setengah dari porsi makanan, dianjurkan dipenuhi oleh sayuran dan buah buahan dari total jumlah makanan setiap kali makan. Sedangkan setengahnya lagi terdiri dari makanan pokok dan lauk pauk yang menyertainya. Sayuran dianjurkan memiliki porsi yang lebih banyak dari buah, begitu juga dengan porsi makanan pokok yang dianjurkan melebihi porsi lauk pauk. Gambar air putih di sebelah piring menunjukkan bahwa seseorang juga dianjurkan minum setiap kali makan yang jumlahnya disesuaikan dengan kebutuhan. Selain itu, untuk penerapan pola hidup bersih tidak lupa harus mencuci tangan termasuk peralatan makan[28 29] .

Gambar 2. Piring Makanku: Sajian Sekali Makan

Pedoman Gizi Seimbang juga memiliki anjuran yang mengatur berapa jumlah porsi yang diperlukan menurut kecukupan energi. Anjuran ini termasuk untuk berbagai kelompok umur, tiap orang, dan tiap harinya. Berikut ini adalah tabel anjuran untuk kelompok umur 19 29 tahun yang sesuai dengan kriteria mahasiswa pada penelitian ini: Tabel 6. Anjuran Jumlah Porsi Menurut Kecukupan Energi untuk Kelompok Umur 19 29 tahun perorang perhari
Ket:
1. Nasi 1 porsi = ¾ gelas = 100 gr = 175 kkal 2. Sayuran 1 porsi = 1 gelas = 100 gr = 25 kkal 3. Buah 1 porsi = 1 buah pisang ambon = 50 gr = 50 kkal 4. Tempe 1 porsi = 2 potong sedang = 50 gr = 80 kkal 5. Daging 1 porsi = 1 potong sedang = 35 gr = 50 kkal 6. Ikan segar 1 porsi = 1/3 ekor = 45 gr = 50 kkal 7. Susu sapi cair 1 porsi = 1 gelas = 200 gr = 50 kkal 8. Susu rendah lemak 1 porsi = 4 sdm = 20 gr = 75 kkal 9. Minyak 1 porsi = 1 sdt = 5 gr = 50 kkal
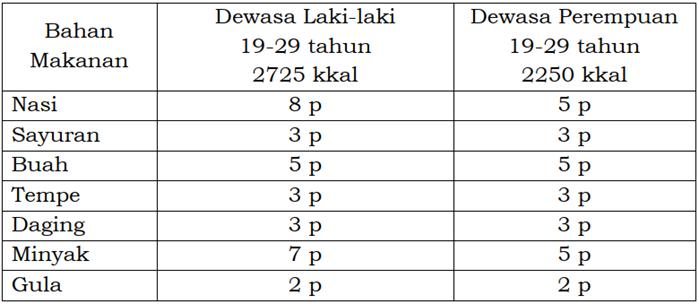
10. Gula = 1 sdm = 20 gr = 50 kkal
*) sdm : sendok makan **) sdr : sendok teh p : porsi
4. Angka Kecukupan Gizi
Pola makan setiap orang tidak harus sesuai dengan menu rekomendasi dari Pedoman Gizi Seimbang. Namun, setidaknya menu makanan tersebut
memenuhi Angka Kecukupan Gizi (AKG) yang dianjurkan bagi bangsa Indonesia. Berdasarkan PMK No.28 Tahun 2019, Angka Kecukupan Gizi (AKG) untuk kelompok usia 16 18 tahun dan 19 29 tahun adalah sebagai berikut[28 29]:
Tabel 7. Angka Kecukupan Energi, Protein, Lemak, Karbohidrat, Serat, dan Air yang dianjurkan (per orang per hari) AKG Laki-laki Perempuan
16 18 tahun 19 29 tahun 16 18 tahun 19 29 tahun
BB 60 kg TB 168 cm BB 52 kg TB 159 cm BB 55 kg TB 159 cm
Energi (kkal) 2650 2650 2100 2250 Protein (g) 75 65 65 60 Lemak (g)
● Total ● Omega 3
● Omega 6
85 1,6 16
75 1,6 16
70 1,1 11
65 1,1 12
Karbohidrat (g) 400 430 300 360 Serat (g) 37 37 29 32 Air (ml) 2300 2500 2150 2350
Katering merupakan suatu pelayanan industri kuliner yang bergerak di pelayanan jasa makanan[32]. Berasal dari kata to cater, katering diartikan sebagai tempat yang menyajikan menu makanan dan minuman untuk masyarakat umum[33]. Jasa makanan ini menawarkan menu yang bervariasi dari sarapan, makan siang, makan malam, kudapan, hingga hidangan pencuci mulut. Beberapa katering juga menyediakan menu makanan yang beragam yang mencangkup hidangan dari berbagai negara seperti Jepang, Indonesia, hingga India[33] Dewasa ini, jasa-jasa katering tidak hanya fokus untuk sekedar menyajikan makanan bagi konsumennya saja, tetapi juga menawarkan menu makanan sehat untuk memenuhi kebutuhan tertentu
konsumennya, seperti menu makanan tanpa garam, rendah lemak, rendah karbohidrat, ataupun rendah kalori[34]. Katering yang menyediakan makanan dengan kandungan gizi khusus seperti tersebut juga akrab disebut sebagai katering diet dan sehat.
Pada era modern ini, tingkat kepedulian masyarakat terhadap betapa pentingnya konsumsi makanan bergizi dan penerapan pola hidup yang sehat mulai meningkat. Hal tersebut dapat terjadi karena kondisi tingkat polusi, tekanan pekerjaan, peningkatan kesediaan makanan instan, penggunaan bahan pengawet, dan faktor faktor lain yang dapat berkontribusi terhadap munculnya berbagai masalah kesehatan di masyarakat[35]. Menu makan yang baik tidak hanya meliputi frekuensi yang cukup di setiap harinya, tetapi juga perlu memperhatikan kelengkapan gizi dalam makanan serta porsi makanan yang diatur dengan baik agar terjaga status kesehatan seorang individu[36] Meningkatnya kesadaran dan kepedulian masyarakat terhadap kesehatan melalui pola makan sehat ini akhirnya mendorong peluang usaha yang menjanjikan pada tata boga berupa katering yang menyediakan menu makanan sehat dan cocok untuk keperluan diet[35]. Dalam kondisi ini, jasa katering diet dan sehat telah menjadi tren di masyarakat guna menjaga pola hidup yang sehat di tengah tengah kesibukan mereka.
3. Hubungan Katering Diet Sehat dengan Penurunan Berat Badan dan Komposisi Tubuh
Di kota kota besar seperti pada Ibu Kota Jakarta, berbagai brand katering diet sehat tumbuh dengan pesat akibat tren pada masyarakat. Masing masing brand ini tidak hanya menawarkan menu dengan berbagai diet untuk memenuhi kebutuhan pelanggan, tetapi mereka juga menjamin adanya penurunan berat badan yang akan turun dalam waktu beberapa hari minggu[35]. Berbagai testimoni telah diberikan pelanggan yang mengkonsumsi brand brand katering diet sehat. Namun, sejauh ini belum diketahui dengan pasti apakah penurunan berat badan yang dialami pelanggan sepenuhnya dikarenakan konsumsi katering diet sehat tersebut.
Bila kita melihat dari komposisi makanan yang disediakan katering diet sehat ini, tiap brand memberikan menu diet yang bervariasi untuk memenuhi kebutuhan konsumen. Contohnya, seperti salah satu brand katering diet sehat
di Jakarta yang menawarkan paket makanan tanpa garam dan nasi dalam paket program diet 13 hari. Tujuan dari dibatasinya komponen garam dan nasi bertujuan untuk memenuhi keinginan konsumen untuk menurunkan berat badan mereka dalam waktu singkat[35]. Sementara, ada jasa katering lain menawarkan program diet yang tetap mengandung garam dan nasi namun lebih memperhatikan ke output kalori pada menu mereka sehingga tidak membatasi konsumen dari makanan makanan tertentu, namun diolah sedemikian rupa agar kalori untuk satu porsi makanan masih di kisaran di bawah 500 kalori.
Berbagai katering diet sehat yang berdiri sekarang menyediakan tren diet yang sedang populer dan berkembang pesat di masyarakat, khususnya untuk alasan penurunan berat badan. Ada katering diet yang menyebutkan menu diet mereka berdasarkan komposisi makronutrien seperti diet rendah karbohidrat tapi tinggi lemak, diet rendah karbohidrat tapi tinggi protein, ataupun sekedar diet rendah kalori secara keseluruhan. Namun keefektifan menu makanan yang disediakan katering diet sehat seperti di atas masih menjadi perdebatan. Banyak pertanyaan muncul mengenai menu diet yang disediakan katering diet sehat ini mulai dari besar kalorinya, komposisi makronutrien dan mikronutrien, keefektifannya dalam menurunkan berat badan, sampai apakah menu katering diet sehat ini sudah teruji secara ilmiah untuk memperbaiki status gizi konsumen melalui penurunan berat badan[37].
Katering diet sehat sekarang ini lebih difokuskan dan diminati karena kemampuannya untuk menurunkan berat badan konsumen. Sudah ada berbagai testimoni yang beredar di media sosial mengenai penurunan berat badan yang dialami setelah mengkonsumsi katering diet sehat ini. Namun, sampai sekarang belum ada penelitian yang menunjukkan dengan jelas hubungan dari konsumsi katering diet sehat ini dengan status gizi pasien yang lebih detail seperti menggunakan parameter berupa komposisi tubuh. Penurunan berat badan melalui pengukuran perubahan komposisi tubuh terdiri antara lain seperti lemak tubuh total, massa bebas lemak, dan cairan tubuh. Belum diketahui pasti apakah penurunan berat badan pasien yang terjadi setelah konsumsi katering diet sehat ini diakibatkan kare na memang adanya penurunan massa lemak saja, atau penurunan komponen lain dari komposisi tubuh.
Gambar 4. Kerangka Konsep Hubungan Konsumsi Katering Diet Sehat terhadap Perubahan Komposisi Tubuh

4.1.
4.2.
4.3.
4.1.1. Tempat Penelitian
Penelitian akan dilaksanakan secara lokal di DKI Jakarta meliputi Jakarta Pusat, Jakarta Utara, Jakarta Timur, Jakarta Barat, Jakarta Selatan, dan Kepulauan Seribu.
4.1.2. Waktu Penelitian
Penelitian akan dilakukan pada Januari 2022 hingga Maret 2022.
4.1.3. Disiplin Ilmu Penelitian
Penelitian ini berkaitan dengan ilmu gizi dan ilmu kesehatan masyarakat.
Penelitian ini menggunakan desain penelitian observasional deskriptif dengan studi potong lintang dengan instrumen berupa kuesioner frekuensi konsumsi katering diet sehat dan kuesioner aktivitas fisik Baecke. Peneliti mengukur konsumsi katering diet sehat, aktivitas fisik, dan perubahan komposisi tubuh setelah mengonsumsi katering diet sehat selama 30 hari secara bersamaan. Selama 30 hari tersebut, peneliti juga akan meminta responden untuk mengisi formulir Food Recall setiap 3 hari untuk mencatat apa saja yang mereka konsumsi. Responden penelitian ini hanya diambil berdasarkan kriteria inklusi dan eksklusi yang sudah ditetapkan dalam studi.
4.3.1. Variabel independen dalam penelitian ini adalah konsumsi katering diet sehat pada mahasiswa program studi kedokteran di DKI Jakarta.
4.3.2. Variabel dependen dalam penelitian ini adalah perubahan komposisi tubuh pada mahasiswa program studi kedokteran di DKI Jakarta.
4.3.3. Variabel perancu dalam penelitian ini adalah aktivitas fisik individu, frekuensi dalam mengonsumsi katering diet sehat, dan hasil analisis nilai gizi dari Nutrisurvey.
No. Variabel Definisi Alat Ukur Cara Ukur Hasil Ukur Jenis Data
1. Umur Lama hidup sejak dilahirkan sampai sekarang yang dihitung dalam tahun.
2. Jenis Kelamin Perbedaan jenis seks yang dimiliki sejak lahir dan dibedakan menjadi laki laki dan perempuan.
3. Pendidikan Jenjang pendidikan terakhir responden di program studi kedokteran.
4. Keikutsertaan dalam Katering Diet Sehat
Keikutsertaan responden dalam mengonsumsi katering diet sehat.
Kuesioner Pengisian kuesioner secara daring Isian singkat Ordinal
5. Frekuensi Konsumsi Katering Diet
Frekuensi responden dalam mengonsumsi katering diet dalam waktu satu hari.
Kuesioner Pengisian kuesioner secara daring 1 = Laki-laki 2 = Perempuan Nominal
Kuesioner Pengisian kuesioner secara daring 1 = Preklinik 2 = Klinik Ordinal
Kuesioner Pengisian kuesioner secara daring 0 = Tidak 1 = Ya Nominal
Kuesioner Pengisian kuesioner secara daring 1 = 1 kali 2 = 2 kali 3 = 3 kali
Ordinal
Sehat dalam Satu Hari
6. Frekuensi Konsumsi Katering Diet Sehat dalam Satu Minggu
Frekuensi responden dalam mengonsumsi katering diet dalam waktu satu minggu.
Kuesioner Pengisian kuesioner secara daring 1 = 2 hari (weekend) 2 = 5 hari (weekday) 3 = 7 hari
7. Frekuensi Konsumsi Katering Diet Sehat dalam 30 Hari
Frekuensi responden dalam mengonsumsi katering diet dalam waktu 30 hari.
Kuesioner Pengisian kuesioner secara daring 1 = 1 minggu 2 = 2 minggu 3 = 3 minggu 4 = 4 minggu
Ordinal
Ordinal
8. Aktivitas Fisik Frekuensi gerakan tubuh yang dilakukan responden untuk mengeluarkan energi.
9. Berat Badan Parameter antropometri untuk menggambarkan massa tubuh seseorang.
Kuesioner Baecke Pengisian kuesioner secara daring Aktivitas ringan Aktivitas sedang Ordinal
Timbangan Pengukuran pada hari pertama dan 30 hari setelahnya secara luring
Kilogram Skala
10. Tinggi Badan Jarak ketika seseorang berdiri tegak dengan posisi anatomis dan posisi kepala pada bidang dari ujung kepala hingga lantai.
11. Pemenuhan Gizi
Responden Nilai gizi responden berdasarkan menu makanan, bahan makanan, waktu makan, dan ukuran porsi makan yang meliputi kalori, karbohidrat, protein, dan lemak.
Meteran Pengukuran pada hari pertama dan 30 hari setelahnya secara luring
Meter Skala
12. Lemak Tubuh
Total (Total Body Fat)
Formulir Food Recall dan Nutrisurvey
Pengisian formulir per tiga hari dan analisis Nutrisurvey
0 = Tidak 1 = Ya Nominal
13. Jaringan Bebas Lemak (Fat Free Mass)
Pengukuran persentase lemak tubuh total dan lemak viseral. Timbangan Body Composition Scale
Pengukuran massa protein (otot rangka dan otot non rangka), mineral, dan cairan
Timbangan Body Composition
Pengukuran pada hari pertama dan 30 hari setelahnya secara luring
Persentase Skala
Pengukuran pada hari pertama dan 30 hari setelahnya
Persentase Skala
(Body Fluid)
tubuh. Scale secara luring
Larutan yang terdiri atas air sebagai pelarut dan zat tertentu sebagai pelarut.
Timbangan Body Composition Scale
Pengukuran pada hari pertama dan 30 hari setelahnya secara luring
Persentase Skala
4.5.1. Populasi Target
Populasi target pada penelitian ini adalah mahasiswa kedokteran di Indonesia.
4.5.2. Populasi Terjangkau
Populasi terjangkau pada penelitian ini adalah mahasiswa kedokteran di DKI Jakarta.
4.6.1. Kriteria
1. Responden yang merupakan mahasiswa program studi kedokteran di DKI Jakarta.
2. Responden yang menyetujui informed consent dan bersedia mengikuti kuesioner serta pengukuran komposisi tubuh.
3. Responden yang akan mengonsumsi katering diet dalam rentang waktu sampai 30 hari ke depan.
4.6.2 Kriteria Eksklusi
1. Responden memiliki riwayat penyakit, seperti diabetes mellitus dan hipertensi.
2. Responden mengonsumsi obat pelangsing.
4.7.
Teknik pengambilan sampel adalah accidental sampling dimana responden yang diambil adalah responden yang ada dan bersedia di DKI Jakarta.
Keterangan: � = (��)2 ×�×(1 �) � 2
n = Jumlah Sampel Minimal
a = Derivat Baku Alfa = 1.645 P = Proporsi Kategori Variabel yang Diteliti = 0.13 d = Presisi = 0.1 � = (1.645)2 × 0.13 × (1 0.13) (0.1)2 � = 0.30605 0.01 � = 30.605 � ≈ 31 �����
Sampel ditambah sebanyak 100% untuk menghindari bias sampel, sehingga total sampel pada penelitian ini adalah 62 orang.
4.8.1.
Instrumen ini digunakan sebagai bentuk persetujuan dan ketersediaan antara peneliti dengan responden sehingga data data yang diperoleh oleh peneliti dapat digunakan untuk menunjang penelitian ini. Jika responden menandatangani Informed Consent, maka responden setuju untuk mengikuti keseluruhan dari penelitian.
4.8.2.
Kuesioner survei digunakan untuk menentukan distribusi populasi penelitian. Kuesioner ini meminta responden untuk memberikan data yang mencangkupi usia, jenis kelamin, tingkat pendidikan, serta frekuensi konsumsi katering diet baik dalam hitungan satu hari, satu minggu, maupun 30 hari
4.8.3. Kuesioner
Kuesioner ini digunakan untuk menilai tingkat aktivitas fisik yang dilakukan responden dalam kegiatan sehari harinya. Pertanyaan yang terdapat pada kuesioner ini meliputi intensitas serta frekuensi saat bekerja, olahraga, dan saat senggang. Kuesioner ini diambil berdasarkan The Questionnaire of Baecke, et al. for Measurement of a Person's Habitual Physical Activity dari Baecke, Burema, Frijters, 1982.
4.8.4. Formulir Food Recall
Formulir Food Recall ini digunakan untuk mencatat nilai gizi yang dikonsumsi oleh konsumen baik itu dari menu makanan katering diet sehat atau di luarnya. Responden mengisi formulir ini per 3 hari, dengan total pengisian selama 30 hari adalah 10 kali. Isi formulir mencangkup menu makanan, waktu makanan, bahan makanan, dan ukuran porsi makan. Nilai gizi yang dinilai dalam penelitian ini antara lain total kalori, karbohidrat, protein, dan lemak. Hasil pencatatan formulir ini akan dimasukkan ke dalam Nutrisurvey untuk dianalisa.
4.8.5. Timbangan Body Composition Scale
Instrumen ini digunakan untuk menilai perubahan komposisi tubuh yang dihitung berdasarkan lemak tubuh total, jaringan bebas lemak, dan cairan tubuh.

Peneliti akan menyebarkan kuesioner dalam bentuk Google Form di sosial media. Kuesioner dapat langsung diisi oleh responden. Pengisian kuesioner akan menghabiskan waktu sebanyak 10 15 menit. Jenis data yang diperoleh adalah kategorik. Kemudian peneliti akan mendatangi responden yang memenuhi kriteria inklusi untuk diukur komposisi tubuhnya sebelum dan sesudah 30 hari mengonsumsi katering diet. Pengambilan data akan menghabiskan waktu sebanyak 15 20 menit. Jenis data yang diperoleh adalah numerik. Selama periode 30 hari tersebut, peneliti juga meminta responden untuk mencatat pola konsumsi responden dalam formulir Food Recall setiap 3 hari. Pencatatan ini akan menghabiskan waktu sekitar 10 15 menit. Jenis data yang diperoleh adalah kategorik. Alur penelitian dapat diringkas menjadi berikut:
Gambar 5. Cara Pengumpulan Data
Setelah pengumpulan data, data akan diolah dan dianalisis dengan uji statistik menggunakan program SPSS untuk data komposisi tubuh. Untuk data nilai gizi makanan berdasarkan Food Recall akan menggunakan Nutrisurvey. Selanjutnya akan diperoleh suatu kesimpulan dalam bentuk tabulasi. Hal ini dicapai dengan langkah langkah sebagai berikut:
1. Editing: pemeriksaan ketidaklengkapan atau kesalahan dari jawaban kuesioner.
2. Coding: hasil penelitian dari jawaban kuesioner diubah ke dalam kode. Pada variabel konsumsi katering diet, pernyataan yang menyatakan konsumsi katering diet akan diberikan kode 1 untuk jawaban “Ya” dan kode 0 untuk jawaban “Tidak”.
3. Entry: proses memasukkan data ke dalam komputer.
4. Cleaning: proses pemeriksaan, pembersihan, dan pemulihan data apabila terdapat kesalahan pada langkah entry dan coding
4.11.1.
Analisis univariat adalah sebuah teknik analisis yang dilakukan pada satu variabel. Data yang diperoleh adalah distribusi frekuensi mengenai konsumsi katering diet sehat, aktivitas fisik, dan frekuensi serta kepatuhan mengikuti katering diet sehat.
4.11.2.
Analisis bivariat adalah sebuah teknik analisis yang dilakukan untuk melihat hubungan antarvariabel yang diteliti. Penelitian ini akan menggunakan uji statistik T berpasangan untuk meneliti apakah adanya perbedaan signifikan antara konsumsi katering diet sehat dengan perubahan komposisi tubuh responden sebelum dan sesudah 30 hari mengonsumsi katering diet sehat. Penelitian ini juga menggunakan uji statistik Pearson untuk meneliti kekuatan korelasi antara konsumsi katering diet sehat dengan perubahan komposisi tubuh responden sebelum dan sesudah 30 hari mengonsumsi katering diet sehat
4.11.3.
Analisis multivariat adalah sebuah teknik analisis yang dilakukan untuk melihat hubungan antarvariabel yang diteliti dengan pertimbangan variabel perancu. Penelitian ini menggunakan regresi logistik untuk metode analisis multivariat.
Tabel 8. Deskripsi Distribusi Populasi Penelitian Menurut Sosio Demografis
Variabel
Usia 16 18 tahun 19 21 tahun 22-23 tahun ≥ 24 tahun
Jenis Kelamin Laki laki Perempuan Pendidikan Preklinik Klinik
Jumlah Responden n %
Tabel 9. Deskripsi Distribusi Populasi Penelitian Menurut Aktivitas Fisik, Keikutsertaan Katering Diet Sehat, dan Frekuensi Konsumsi Katering Diet Sehat
Variabel
Aktivitas Fisik Aktivitas ringan Aktivitas sedang
Keikutsertaan dalam Katering Diet Sehat Tidak Ya
Frekuensi Konsumsi Katering Diet Sehat dalam Satu Hari
1 kali 2 kali 3 kali
Frekuensi Konsumsi Katering Diet Sehat dalam Satu Minggu
Frekuensi Konsumsi Katering Diet Sehat dalam 30 Hari
2 hari (weekend) 5 hari (weekday) 7 hari
1 minggu 2 minggu 3 minggu 4 minggu
Jumlah Responden n %
Tabel 10. Tabel Nutrisurvey Hasil Food Recall per 3x24 Jam
Analisis Food Record
Jenis Makanan Jumlah (gram) Energi (kkal) Karbohidrat (gram) Protein (gram) Lemak (gram)
Tabel 11. Tabel Nutrisurvey Hasil Food Recall per 30 hari Gizi Hasil Analisis Jumlah Rekomendasi/Hari Persentase Pemenuhan
Energi (kkal) Karbohidrat (gram) Protein (gram) Lemak (gram)
Tabel 12. Perbedaan Rata-Rata Sebelum dan Sesudah Konsumsi Katering Diet Sehat pada Perubahan Komposisi Tubuh
Variabel Waktu P value Sebelum Sesudah
Lemak Tubuh Total (Total Body Fat)
Jaringan Bebas Lemak (Fat-Free Tissue)
Cairan Tubuh (Body Fluid)
Tabel 13. Hubungan Konsumsi Katering Diet dengan Perubahan Komposisi Tubuh Variabel
Konsumsi Katering Diet Komposisi Tubuh Sesudah 30 Hari
Konsumsi Katering Diet r
Komposisi Tubuh Sesudah 30 Hari
P value
Tabel 14. Analisis Multivariat Variabel Bebas dan Perancu Terhadap Perubahan Komposisi Tubuh Setelah 30 Hari Variabel
Aktivitas Fisik Frekuensi Konsumsi Katering Diet Sehat Pemenuhan Kalori
Pemenuhan Karbohidrat
Pemenuhan Protein Pemenuhan Lemak
Perubahan Komposisi Tubuh Setelah 30 Hari
P Value OR 95% CI
Lower Upper
1. 1 dari 4 Penduduk Dewasa Mengalami Obesitas Direktorat P2PTM [Internet]. Direktorat P2PTM. 2021 [cited 16 November 2021]. Available from: http://p2ptm.kemkes.go.id/artikel sehat/1 dari 4 penduduk dewasa mengalami obesitas
2. Badan Penelitian dan Pengembangan Kesehatan. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) 2018. Jakarta: Kementerian Kesehatan RI; 2018.
3. Desmawati. Gambaran Gaya Hidup Kurang Gerak (Sedentary Lifestyle) dan Berat Badan Remaja Zaman Milenial di Tangerang, Banten. JURNAL ILMIAH KESEHATAN MASYARAKAT : Media Komunikasi Komunitas Kesehatan Masyarakat [Internet]. 2019 Dec 25 [cited 2021 Nov 16];11(4):296 301. Available from: https://jikm.upnvj.ac.id/index.php/home/article/view/50/36
4. Muflihah N, Wardhani RR. Identifikasi Sedentary Behaviour di Masa Pandemic Covid 19; Narrative Review [Internet]. Journal Physical Therapy UNISA. 2021 [cited 2021 Nov 16]. Available from: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=aXgFNpI AAAAJ&citation_for_view=aXgFNpIAAAAJ:Y0pCki6q_DkC
5. World Health Organization. Healthy diet [Internet]. 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/325828/EMROPUB_2019_en_23536 .pdf
6. Rizkita F, Windasari N. FACTORS AFFECTING YOUNG ADULT CONSUMERS’ ATTITUDE ON HEALTHY FOOD CONSUMPTION AND DIETARY CATERING PURCHASE INTENTION. SBM ITB [Internet]. 2019 [cited 2021 Nov 16];372. Available from: https://core.ac.uk/download/pdf/324148509.pdf
7. Jaya DV, Kumala M. Hubungan aktivitas fisik dengan komposisi tubuh mahasiswa Fakultas Kedokteran Universitas Tarumanagara Angkatan 2013. Tarumanagara Medical Journal [Internet]. 2020 May 15 [cited 2021 Nov 16];2(2):231 8. Available from: https://journal.untar.ac.id/index.php/tmj/article/view/7833
8. World Health Organization. Malnutrition [Internet]. Who.int. World Health Organization: WHO; 2020. Available from: https://www.who.int/news room/fact sheets/detail/malnutrition
9. Joshi R, Malla R, Bhattarai MD, Shrestha DB. Prevalance of Gestational Diabetes Mellitus in Overweight Pregnant Women in Urban Antenatal Clinic at 24 28 Weeks of
Gestation. Medical Journal of Shree Birendra Hospital [Internet]. 2017 Dec 23 [cited 2021 Dec 3];16(2):55 62. Available from: https://www.researchgate.net/publication/322026558_Prevalence_of_Gestational_Dia betes_Mellitus_in_Overweight_Pregnant_Women_in_Urban_Antenatal_Clinic_at_24 28_Weeks_of_Gestation
10. Kansra AR, Lakkunarajah S, Jay MS. Childhood and Adolescent Obesity: A Review. Frontiers in Pediatrics [Internet]. 2021 Jan 12 [cited 2021 Nov 16];8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7835259/
11. Sherwood, Lauralee. Introduction to Human Physiology. 8th ed. Amerika Serikat: Brooks/Cole, Cengage Learning; 2013
12. Thibault R, Genton L, Pichard C. Body composition: Why, when and for who? Clinical Nutrition. 2012 Aug;31(4):435 47.
13. Amelia WR. Indeks Massa Tubuh sebagai Salah Satu Parameter Status gizi [Internet]. 2009 [cited 2021 Nov 16]. Available from: http://lib.ui.ac.id/file?file=digital/124734 S 5648 Hubungan%20antara Literatur.pdf
14. Munawaroh MM. Komposisi Lemak Viseral, Basal Metabolic Rate (BMR), Dan Usia Sel Terhadap Indeks Masa Tubuh (IMT) Pada Remaja. Jurnal Untuk Masyarakat Sehat (JUKMAS). 2021 Apr 30;5(1):110 9.
15. OMRON. Frequently Asked Questions | Omron Healthcare [Internet]. www.omronhealthcare ap.com. [cited 2021 Dec 3]. Available from: https://www.omronhealthcare ap.com/sg/faqs/weight management
16. OMRON. Instruction Manual Full Body Sensor Body Composition Monitor and Scale Model HBF 510 2 Before Using the Monitor [Internet]. [cited 2021 Dec 3]. Available from: https://omronhealthcare.com/wp-content/uploads/hbf-510w-instructionmanual.pdf
17. Institute of Medicine (US) Subcommittee on Military Weight Management. Factors That Influence Body Weight [Internet]. Nih.gov. National Academies Press (US); 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK221834/
18. Durá Travé T, Gallinas Victoriano F, Malumbres Chacón M, Moreno González P, Ahmed Mohamed L, Urretavizcaya Martínez M. Reference Values of Fat Mass Index and Fat Free Mass Index in Healthy Spanish Adolescents. Nutricion hospitalaria. 2020;37(5), 902 908. https://doi.org/10.20960/nh.03161
19. Fauziyyah Hana Chaerani, Luh Desi Puspareni, Iin Fatmawati, Nanang Nasrullah. PENGARUH PEMBERIAN MEAL REPLACEMENT TINGGI PROTEIN KEDELAI
TERHADAP : Berat Badan, Persen Cairan Tubuh, Dan Persen Lemak Tubuh Pada Dewasa Obesitas Di AVR Fit Nutrition Club [Internet]. repository.upnvj.ac.id. 2020 [cited 2021 Nov 16]. Available from: https://repository.upnvj.ac.id/7013/
20. Sirait RH. Bahan Kuliah [Internet]. Available from: http://repository.uki.ac.id/2783/1/CairanTubuh20191.pdf
21. Kementerian Kesehatan Republik Indonesia. Apa Definisi Aktivitas Fisik? [Internet]. Direktorat P2PTM. 2019 [cited 2021 Nov 16]. Available from: http://p2ptm.kemkes.go.id/infographicp2ptm/obesitas/apa definisi aktivitas fisik
22. Kementerian Kesehatan Republik Indonesia. Aktivitas Fisik Ringan [Internet]. Direktorat P2PTM. 2018. Available from: http://p2ptm.kemkes.go.id/infographic p2ptm/obesitas/aktivitas fisik ringan
23. Kementerian Kesehatan Republik Indonesia. Aktivitas Fisik Sedang [Internet]. Direktorat P2PTM. 2018. Available from: http://p2ptm.kemkes.go.id/infographic p2ptm/obesitas/aktivitas fisik sedang
24. Kementerian Kesehatan Republik Indonesia. Aktivitas Fisik Berat [Internet]. Direktorat P2PTM. 2018 [cited 2021 Nov 16]. Available from: http://p2ptm.kemkes.go.id/infographic p2ptm/obesitas/page/39/aktivitas fisik berat
25. Mudambi S. R. Fundamentals of Foods, Nutrition and Diet Therapy. India: New Age International; 2007.
26. Raymond J. L, Morrow K. Krause and Mahan’s Food and the Nutrition Care Process. Maryland Heights: Elsevier Health Sciences; 2020.
27. Kementerian Kesehatan RI. PMK No. 41 tentang Pedoman Gizi Seimbang. Jakarta: Kementerian Kesehatan; 2014.
28. Kementerian Kesehatan RI. Pedoman Gizi Seimbang 2014. Jakarta: Permenkes RI,(41); 2014.
29. Pratama, P. A., Zulkarnain, E., & Ririanty, M. (2018). Efektivitas Media Promosi “Piring Makanku” Pedoman Gizi Seimbang Sebagai Panduan Sekali Makan (The Effectiveness of Media promotion" Piring Makanku" Balanced Nutrition Guidelines as a Guide Once Packed). Pustaka Kesehatan, 6(1), 53 59.
30. Setyawati, V. A. V., & Hartini, E. (2018). Buku Ajar Dasar Ilmu Gizi Kesehatan Masyarakat. Deepublish.
31. Iqbal M. Pengaruh Knowledge of Healthy Food dan Health Awareness terhadap Behavioral Intention pada Konsumen Jasa Katering Makanan Sehat di Ana Kitchen Garut [skripsi]. Bandung: Universitas Pendidikan Indonesia; 2021.
32. Anjasari E, Nikmawati E. E, Setiawati T. Manfaat Hasil Belajar “Bisnis Makanan Diet” sebagai Kesiapan Membuka Usaha Katering Diet. Media Pendidikan, Gizi, dan Kuliner. 2015;4(1)
33. Fadhilla E. Anteseden dari Behavioral Intention pada Jasa Katering Makanan Sehat [skripsi]. Jakarta: FEB Trisakti; 2018.
34. Siswanto E. Bisnis Menu Diet Sehat. Yogyakarta: Laksana; 2018.
35. Fauziah R. Model Pengelolaan Menu Sehat terhadap Keputusan Mahasiswa dalam Membeli Makanan: Survei pada Mahasiswa Manajemen Industri Katering FPIPS UPI [skripsi]. Bandung: Universitas Pendidikan Indonesia; 2012.
Perkenalkan kami mahasiswa S1 Fakultas Kedokteran Universitas Pembangunan Nasional Veteran Jakarta. Saat ini kami sedang melaksanakan penelitian di bawah AMSA Indonesia yang berjudul “Hubungan Konsumsi Katering Diet Sehat terhadap Perubahan Komposisi Tubuh pada Mahasiswa Program Studi Kedokteran di DKI Jakarta” . Penelitian ini merupakan lanjutan dari kompetisi National Research Proposal Competition yang diadakan AMSA Indonesia.
Pada penelitian ini, kami akan meminta waktu 10 15 menit untuk mengisi kuesioner yang telah kami sediakan, serta kunjungan dari kami untuk diukur berat badannya 30 hari setelah pengisian kuesioner ini. Selain itu, kami juga meminta ketersediaan responden untuk mencatat waktu makan, menu, bahan, serta ukuran porsi makanan yang dikonsumsi per 3 hari selama 30 hari dalam formulir yang telah kami sediakan. Semua informasi yang tertulis dalam kuesioner ini, termasuk data pribadi dan data penelitian, akan dijaga kerahasiaannya.
Partisipasi Saudara/i dalam penelitian ini bersifat sukarela. Meskipun demikian, kami harap agar Saudara/i dapat menjadi responden penelitian ini karena partisipasi Saudara/i sangat dibutuhkan. Demikian permohonan kami, atas perhatian dan kerja sama Saudara/i dalam penelitian ini, kami ucapkan terima kasih.
Setelah membaca dan memahami penjelasan dari peneliti, dengan ini saya, Nama : Alamat : Secara sukarela menyatakan bahwa saya (SETUJU/TIDAK SETUJU) untuk berpartisipasi menjadi responden dalam penelitian ini. Apabila ada kekurangan di kemudian hari, saya bersedia untuk dihubungi dan diminta keterangan/informasi lebih lanjut.
Jakarta,...............................
Responden
Jenis Kelamin
Laki laki / Perempuan Tempat/Tanggal lahir Usia Alamat Tingkat Pendidikan a. Preklinik b. Klinik
Keikutsertaan dalam Katering Diet Sehat a. Ya b. Tidak
Frekuensi Konsumsi Katering Diet Sehat dalam Satu Hari
Frekuensi Konsumsi Katering Diet Sehat dalam Satu Minggu
Frekuensi Konsumsi Katering Diet Sehat dalam 30 Hari
a. 1 kali b. 2 kali c. 3 kali
a. 2 hari (weekend) b. 5 hari (weekend) c. 7 hari
a. 1 minggu b. 2 minggu c. 3 minggu d. 4 minggu
The Questionnaire of Baecke, et al. for Measurement of a Person’s Habitual Physical Activity
1. Apa pekerjaan utama anda?
a. Aktivitas rendah (menulis, mengemudi, penjaga toko, mengajar, dll)
b. Aktivitas sedang (kerja pabrik, pertukangan, pertanian, dll) c. Aktivitas berat (pekerjaan dermaga, pekerja konstruksi, olahraga profesional)
2. Di tempat kerja seberapa banyak anda duduk?
a. Tidak pernah b. Jarang c. Kadang-kadang d. Sering e. Selalu
3. Di tempat kerja, seberapa banyak anda berdiri?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Selalu
4. Di tempat kerja, seberapa banyak anda berjalan?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Selalu
5. Di tempat kerja, berapa kali anda mengangkat benda berat?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Selalu
6. Setelah bekerja, apakah anda merasa lelah?
a. Sangat sering b. Sering c. Kadang kadang
7. Di tempat kerja, apakah anda berkeringat?
d. Jarang e. Tidak pernah
a. Sangat sering b. Sering c. Kadang kadang d. Jarang e. Tidak pernah
8. Bila dibandingkan orang yang sebaya dengan saya, pekerjaan saya termasuk?
a. Lebih sangat berat b. Lebih berat c. Sama berat d. Lebih ringan e. Lebih sangat ringan
Indeks Olahraga Pertanyaan Jawaban
9. Olahraga apa yang paling sering anda lakukan? Sebutkan!
a. Intensitas rendah (biliard, melaut, bowling, golf, dll) b. Intensitas sedang (badminton, bersepeda, menari, berenang, tenis) c. Intensitas tinggi (bertinju, bola basket, sepak bola)
10. Berapa jam anda melakukan olahraga tersebut dalam seminggu?
a. < 1 jam b. 1 2 jam c. 2 3 jam d. 3 4 jam d. > 4 jam
11. Berapa bulan anda melakukan olahraga tersebut dalam setahun?
a. < 1 bulan b. 1 3 bulan c. 4 7 bulan d. 7 9 bulan e. > 9 bulan
12. Olahraga apa yang kedua paling sering anda lakukan? Sebutkan!
a. Intensitas rendah (biliard, melaut, bowling, golf, dll) b. Intensitas sedang (badminton, bersepeda, menari, berenang, tenis) f. Intensitas tinggi (bertinju, bola basket, sepak bola)
13. Berapa jam anda melakukan olahraga tersebut dalam seminggu?
a. < 1 jam b. 1 2 jam c. 2 3 jam d. 3 4 jam c. > 4 jam
14. Berapa bulan anda melakukan olahraga tersebut dalam setahun?
a. < 1 bulan b. 1 3 bulan c. 4 7 bulan d. 7 9 bulan d. > 9 bulan
15. Bila dibandingkan orang yang sebaya dengan saya, aktivitas saya selama waktu senggang?
a. Sangat lebih banyak b. Lebih banyak c. Sama banyak d. Kurang e. Sangat kurang
16. Selama waktu senggang apakah anda berkeringat?
a. Sangat sering b. Sering c. Kadang kadang d. Jarang f. Tidak pernah
17. Selama waktu senggang apakah anda berolahraga?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Selalu
18. Selama waktu senggang apakah anda menonton televisi?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Selalu
19. Selama waktu senggang apakah anda berjalan jalan?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering f. Selalu
20. Selama waktu senggang apakah anda bersepeda?
a. Tidak pernah b. Jarang c. Kadang kadang d. Sering e. Sangat sering
21. Berapa menit anda berjalan/bersepeda per hari ke dan dari bekerja, sekolah, berbelanja?
a. 5 menit b. 5 15 menit c. 15 30 menit d. 30 45 menit f. >45 menit
Tanggal: Hari ke : Waktu Makan Menu Makanan Ukuran URT Berat dalam gram
Pagi/Jam: Selingan Pagi/Jam: Siang/Jam
Selingan Siang/Jam:
Malam/Jam: Selingan Malam/Jam:
Keterangan: URT: Ukuran Rumah Tangga
Berat dalam gram: tidak perlu diisi responden
Tahap Persiapan
No. Keterangan Jumlah Satuan Biaya satuan (Rp) Total
1. Biaya etik 500.000,00 500.000,00 Subtotal 500.000,00
Tahap Pelaksanaan
No. Keterangan Jumlah Satuan Biaya satuan (Rp) Total
1. HHadiah E-Money untuk responden 10 orang 20.000,00 200.000,00
2. Biaya transport 600.000,00 600.000,00 Subtotal 800.000,00
Tahap Pelaporan
No. Keterangan Jumlah Satuan Biaya satuan (Rp) Total
1. Biaya Cetak Karya Tulis Ilmiah 100 lembar 1.000,00 100.000,00
2. Jilid Karya Tulis Ilmiah 1 eksemplar 10.000,00 10.000,00
Subtotal 110.000,00
Total Anggaran
Tahap Biaya
Tahap persiapan 500.000,00
Tahap pelaksanaan 800.000,00
Tahap pelaporan 110.000,00
SUBTOTAL 1.410.000,00














 Be careful, Madam!
Gammarezka Fitra Fajar AMSA Universitas Pembangunan Nasional “Veteran” Jakarta
Be careful, Madam!
Gammarezka Fitra Fajar AMSA Universitas Pembangunan Nasional “Veteran” Jakarta
In this new era of technology, we know that public health services is one of the most important things to maintain health in the world, including Indonesia. General Directory of National Army said that the prevalence of road accident that lead to mortality is 3 people in one hour and 30% caused by the environment . So, we can conclude that zebra cross is very important thing to safe our life, especially in the metropolitan city like Jakarta, one of the busy and populous city in Indonesia, and i’d like to say ‘Thank you’ for health care services that can reduce prevalence of road accident by creating a zebra pattern like traf fic sign, also known as zebra cross. Sometimes people can be careless and this can lead to a very dangerous situation especially when they crossed a road, because road accident can happened everytime and can lead to trauma. So, what should we do to reduce the incident of trauma caused be road accident? I think the public health and th e goverment can be collaborate to create a zebra cross in the small cities, because we know that not every c ities have zebra cross, furthermore medical student can help the public health to share about how zebra cross can be a very important things to be our guardian angel when we cross the road.
The aim of the photo is to remind the society and public health services about how important zebra cross for people when they cross a road.
Zebra cross can reduce the prevalence of road accident and can decrease a change of mortality rate in Indonesia.

Background :
Neither one of us wants to have an accident, so do the workers. But it can occur anytime, anywhere. Therefore, Occupational Safety and Health (as known as K3) is one of the government regulations that guarantees our safety and health at work.
Objective :
In this photo, a man standing with a broom on his hand and the yellow ‘thing’ on his head. Yes that’s a helmet but it’s special and different ! Actually, besides the yellow color, people can enter this place with any different color to wear on their head. Red for the safety man team, grey for workshop team, green for formwork and finishing team, white for the consultant or visitor, and this man on the photo wearing the yellow one, represent that he is a part of cleaning service team.
The main point is : even a cleaning service who has a smallest risk of trauma since they don’t directly exposed by the build up process of the construction still guaranteed for his occupational safety and health as we can see he’s wearing that yellow helmet, and boots for working.
That long green banner though, welcoming us to the area while reminding that we must wearing safety equipment to keep us protected by the unwanted possibility of accidents.
Conclusion :
Those all shows an excellent effort from the government in ensuring the safety of workers and preventing cases trauma in the work field . We can prove that by seeing even my closest environment has been implementing it. From the smallest possible exposure to the highest, or even anyone who’s gonna step into the area is required to wear their safety equipment. That includes you! If you want to be a visitor, make sure your helmet, boot and safety belt are already settled, ok?

University of Pembangunan Nasional Veteran Jakarta Muhammad Bariq Rifqi Pasha, Khoirunnisa Qurrota’ayun Nur Utami
A burn is an injury to the skin or organic tissue caused by heat , radiation, chemicals, or others WHO estimated 180.000 deaths every year caused by burns. In Indonesia, the prevalency of burn injury is more than 2 million cases per year.
Burn degree classification: first degree burns affecting superficial epidermal, second degree burns affecting epidermis and part of the dermis, third degree burns affecting the epidermis and the dermis, and fourth degree burns affecting epidermis, dermis and subcutis, the skin is often burnt away and the tissue underneath may appear pale or blackened
First aid for patient with burn wounds are: cool the burn with cool running water for 20 minutes don't use ice or creams, clothes that's near the burnt area of skin should be removed but don't move anything that's stuck to the skin, cover the burn by placing a layer of cling film over it a clean plastic bag could also be used, and call for a help if The burn penetrates all layers of skin, the skin is leathery, charred looking, with white, brown, or black patches.

Nabilah Nurul Fitri, Nirmala Radia Hasanah, Sarah Salsabilla Gaeahanny, Bella Adisya Kansha
Background : Pictorial Health Warning (PHW) is one of the government’s way of suppressing the usage of Cigarettes in Indonesia. We feel that although PHW is already being implemented since 2014 in Indonesia, the demand and purchase of Cigarettes are still soaring and exceed the desire number. The percentage of active smokers over the age of 5 in 2015 to 2017 has increased from 22.79% to 23.48% and Indonesia is still one of the country with the highest number of smokers in the world. Around 225.700 people per year in Indonesia has passed away due to smoking or other tobacco related disease.
Objective : It shows that the effectiveness of PHW as a form of health communication from the government to public is still not yet adequate in reducing the cigarettes usage, thus we intend to engage Indonesia’s health care to escalate it by proposing the 4S move. The 4S (Stick, Show, Spread, Synergy) move correlates to the PCC theme to provide information and spread awareness with regards to “Communication in Health”, which, in our case, is to improve the effectiveness of PHW in Indonesia through health communication.
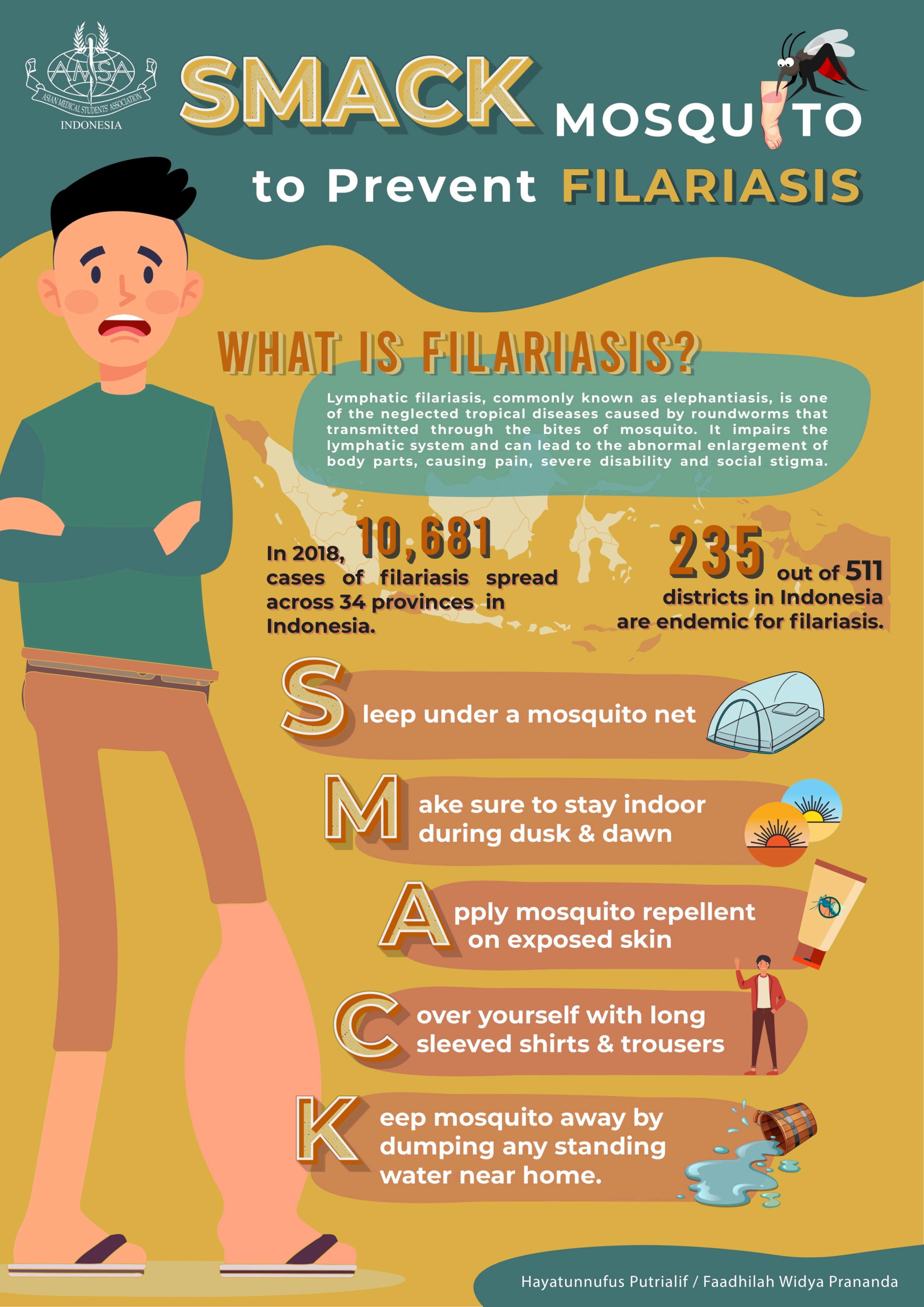
Lymphatic filariasis, commonly known as elephantiasis, is one of the most neglected tropical diseases in the world. According to WHO, more than 120 million people in 2000 were infected, with about 40 million disfigured and incapacitated by the disease. In Indonesia, there were 10,681 cases of filariasis spread across 34 provinces in 2018. It is reported that 235 out of 511 districts/cities in Indonesia are endemic for filariasis. This number indicates that many of the Indonesian population lives in areas at high risk of contracting filariasis.
A person can be affected with filariasis by parasites transmitted through the bites of infected mosquitos. In Indonesia, there are three species of parasitic filarial worms, namely Wuchereria bancrofti, Brugia malayi and B. timori. The damage caused by the disease is not only physical, but also mental due to the social stigma for patients and their caretakers. Indirectly, this disease has an impact on reducing the work productivity of patients and leading to financial losses.
For this reason, this poster aims to increase public knowledge on how to prevent larvae carrying mosquito bites. After seeing this poster, authors hope that people will no longer underestimate mosquito bites, especially for those who lives in endemic areas. Thus transmission can be avoided and the burden of disease and disability caused by filariasis can be reduced.

Introduction :
The COVID 19 pandemic urged everyone to carry out all activities at home such as washing which then accidentally leaves a pool of water that can be a place for mosquitoes to breed, gardening without using clothes that cover all of the arms and legs so that it makes it easier for mosquitoes to bite, etc. Moreover, by the end of the year in Indonesia, we have entered the rainy season where there is a high probability that the number of mosquitoes will increase, including Aedes aegypti. That leads to an increa se in the cases of Dengue Fever or worse, Dengue Hemorrhagic Fever, and also Dengue Shock Syndrome.
Objective : Our project focused on how to prevent Dengue Hemorrhagic Fever. Dengue is the most prevalent and widespread human arboviral disease in the 21st century. Consider ing this pandemic situation, the incidence of Dengue Hemorrhagic Fever is at the peak, proven b y the data from the Indonesian Ministry of Health, it was recorded that there were 71,633 cases in 2020. The knowledge of how to prevent the etiology will help to decrease the incidence rate and increase the awareness to control the mosquito bite
Conclusion : We are currently in a pandemic era, we do not want anyone to underestimate the prevention of Dengue Hemorrhagic Fever because we are too focused on COVID 19.
Reference:
1. Pang X, Zhang R, Cheng G. Progress towards understanding the pathogenesis of dengue hemorrhagic fever. Virol Sin. 2017 Feb;32(1):16 -22. doi: 10.1007/s12250-016-3855-9.
Epub 2016 Nov 14. PMID: 27853992; PMCID: PMC6702245 .
2. Centers for Disease Control and Prevention. Dengue and Dengue Hemorrhagic Fever [Internet]. CDC. [cited 2020 Dec 08]. Available

Theresia Leonita, Claudia Sabrina Wilhelmina Sidabutar Correspondence E mail: theresialeonitaa@gmail.com
Background: The world has faced an outbreak known as COVID 19 in 2019. Since then, social restrictions were imposed to break the chain of coronavirus transmission. Several hospitals in Indonesia have begun to establish telemedicine services to broaden access to health care and prevent the spread of the coronavirus. In this situation, technology might be an option that makes it easier for the community to get. The Ministry of Health of the Republic of Indonesia (Kemenkes) has also innovated by producing an application called SehatPedia to provide and create conveniently accessible and free healthcare services and information for the population. By implementing telemedicine including telemonitoring, telementoring, and teleconsultation in Indonesia, it is expected to increase the health services to the maximum.
Objective: To get optimal health services, people must know the implementations and telemedicine services in Indonesia, one of them is SehatPedia.
Description of poster: Telemedicine services with digital health concepts to make an efficient healthcare system nationwide have increased As evidence, the shift from face to face with doctors to online telemedicine application during pandemic has increased into 600% SehatPedia, as one of telemedicine provided by government, makes healthcare more efficient without "WALL” namely Waiting in line at the health facility for a long time, pay An expensive medical bill, Limited access to healthcare services due to distance, and Limited health facilities in some areas in Indonesia
Impact : After reading this poster, we hope that public interest and knowledge will increase to use telemedicine applications provided by the government so that equity and health services can be achieved
Conclusion: The implementation of telemedicine in Indonesia makes healthcare services during COVID 19 the most secure interactive system Telemedicine makes it more accessible by allowing patients to get healthcare information and treatment from the comfort of their own homes
Keywords: Healthcare, Indonesia, SehatPedia, telemedicine

Theresia Leonita, Claudia Sabrina Wilhelmina Sidabutar, Cheryn Adelyna Shakila e-mail: theresialeonitaa@gmail.com
Kanker payudara adalah keganasan pada jaringan payudara yang berasal dari epitel duktus atau lobulus kelenjar payudara. Gejala kanker payudara meliputi benjolan pada payudara, luka sulit sembuh, cekungan atau tarikan di payudara, tekstur kulit payudara seperti kulit jeruk, dan keluarnya cairan dari puting. Kanker payudara menyumbang jumlah kasus baru terbanyak di dunia setiap tahunnya. Pada tahun 2020, kasus baru kanker payudara di Indonesia sebanyak 30.8% seluruh kasus kanker yang menjadikan 1 dari 8 wanita menderita kanker payudara. Namun, angka kasus kanker payudara ini tidak diimbangi dengan kapasitas fasilitas kesehatan yang dapat menangani kanker payudara di Indonesia. Hingga sekarang, Indonesia baru memiliki 13 rumah sakit rujukan nasional kanker dan 188 dokter spesialis penyakit dalam hematologi onkologi medik sehingga banyak dari pasien kanker payudara terlambat mendapatkan tatalaksana.
Telementoring Extension of Community Healthcare Outcomes (ECHO) merupakan salah satu alternatif murah dan berdampak besar karena mengurangi biaya transportasi dan mempersingkat waktu tatalaksana sehingga pasien dapat mendapatkan penanganan sedini mungkin dan mencegah adanya komplikasi. Telementoring ECHO memiliki prinsip pembelajaran menggunakan teknologi untuk memperbanyak sumber daya (Amplification), menyediakan pelayanan kesehatan terbaik untuk mengurangi kesenjangan (Best Practice), belajar berdasarkan kasus (case-based learning), dan hasil pembelajaran diawasi dengan web-based database. Telementoring ECHO menghubungkan tim spesialis dengan tenaga kesehatan primer melalui konferensi video untuk mengkonsultasi keluhan pasien sehingga para ahli memberikan umpan balik berupa pendampingan dan pelatihan penanganan penyakit.
Dengan adanya telementoring ECHO, tenaga kesehatan primer dapat mengasah kemampuan klinis, kepercayaan diri, dan pengetahuan untuk menangani pasien dengan penyakit kompleks dan penyakit terumum yang ada pada komunitas tersebut terutama pada kanker payudara.
Telementoring ECHO, diharapkan dapat memperluas akses dan meningkatkan kapasitas fasilitas kesehatan terhadap penatalaksanaan spesialistik kanker payudara. Harapan dengan dibuatnya poster ini dapat meningkatkan pengetahuan dan kesadaran terhadap pentingnya

Authors : Gracella Faustine1, Gammarezka Fitra Fajar1, Rahmah Salsah Hudriyah1, Shofiyah Hasya1
1AMSA Pembangunan Nasional Veteran Jakarta University ABSTRACT
Introduction: Health care is demanded to accommodate the needs of each patient, especially patients with speech disabilities. Therefore we recommend the provision of Augmentative and Alternative Communication (AAC). The availability of AAC, both low tech and high tech type in health care is expected to enhance patient provider communication.
Aim: This review aims to find out how important and effective the provision of AAC as a facility to help patients with speech disabilities in achieving effective communication with clinicians in health care.
Materials and methods: This review is conducted using studies from reliable databases s uch as PubMed, Science Direct, ProQuest, EBSCO, and Clinical Keys and 8803 studies were identified. Contents then were screened using PRISMA statement guidelines and four final studies were obtained after full text journal reading. Afterwards, the quality and validity are assessed using JBI critical appraisal indicators.
Results: Communication between patients and health care providers is important because of its contribution to quality of care. It was proved that AAC could improve patient provider communication, expressing patients’ needs, opinions, thoughts, and ability to adapt. Also, both low tech and high tech AAC were proved to be useful and could be implemented in health care
Conclusion: There is still lack of awareness from health care providers in using AAC to help patients with speech disabilities, however it has been proven that AAC has a significant role in breaking communication barriers and providing patient provider effective communication.
Keyword: “Augmentative and Alternative Communication” OR “AAC” AND “Speech Disabilities” OR “Speech Impairment” AND “Healthcare”.
Authors
Gracella Faustine
Gammarezka Fitra Fajar Rahmah Salsah Hudriyah
Shofiyah Hasya
PEMBANGUNAN NASIONAL VETERAN JAKARTA UNIVERSITY

Communication is a daily process that requires a two way interaction to achieve an intended goal. In the medical field, communication becomes a fundamental and critica l aspect to reach successful therapeutic process and outcomes. Thus, health care is demanded to provide a supportive environment for effective patient provider communication which leads to improvement of patient satisfaction, therapy continuity, and increased positive outcomes.
Patient provider communication in health care practice often meets several obstacles that decrease the effectiveness of communication. Individuals with speech disabilities often encounter ineffective communication (i.e., individuals who have an acquired or congenital disability that affects the ability to perform spoken language in order to fulfill daily communication needs) (Therrien & Light, 2018). On the other hand, communication disabilities tend to have an adverse impact on healt h care quality services provided by physicians, health professionals, and other health care providers. Also, patients’ safety, outcomes, satisfaction, and health care costs may cause problems for patients with communication disabilities (Blackstone & Pressman, 2015)
Speech disabilities or so called speech sound disorder s are inability to receive, send, process, and comprehend concepts or verbal, nonverbal and graphic symbol systems. Speech sound disorder s classified into organic or functional disorder. Organic speech sound disorders caused by neurological, structural, or sensory impairment. Organic speech disorder s can be classified into three main characteristics: 1) Motor or neurological disorder such as childhood apraxia of speech and dysarthria; 2) Structural abnormalities such as cleft lip or palate; and 3) Sensory or perceptual disorders such as hearing impairment. On the other hand, functional speech sound disorders are idiopathic. Functional speech sound disorders are referred to as articulatio n disorder and phonological disorders. Articulation disorders can be known as disability in production of speech sound and phonological disorders focus on predictable, rule based errors that affect more than one sound (ASHA, 2017).
However, for many people who have speech sound disorder or with complex communication needs, natural speech is an ineffective method of expression or unders tanding. Therefore, the use of Augmentative and Alternative Communication (AAC) is required to achieve participation in both patients and providers. AAC is defined as a strategy or technique used by the person aimed at maximizing individual communication skills for functional and effective communication ab out their needs and preferences (ASHA, 2016). It can combine various processes that add, complement, or replace individual speech, thus helping them express their thoughts or ideas.
AAC strategies can be broadly classi fied into unaided and aided AAC (ASHA, 2016) Unaided AAC is considered as the oldest category, given its reliance on the interpretation of facial expressions and voluntary motor movements, such as sign language, to deliver non verbal messages.
Another category is aided AAC that also divides into low and high tech. Low tech AAC utilizes basic tools, such as books and display boards with extended lexicons of images and phrases to aid the communication process. High tech AAC encompasses the use of electronic devices to achieve an AAC target. Devices falling under this category, such as smart devices and dedicated AAC devices, integrate hardware and software to support user’s communication needs (Elsahar et al, 2019).
Unfortunately, the importance of AAC availability in hospitals remains unnoticed and not considered as a major concern in health care. Lack of evidence based research about AAC service provision just shows how important it is to focus our attention on this ma tter. Whereas a survey by Judge et al (2017) in the UK shows highly variable levels of service provision and a mean of 0.0155% also the maximum figure of 0,08% individuals known to be using powered communication aids in service catchment population (Judge et al, 2017). Health care providers also admit the limited time to communicate with patients and limited knowled ge about AAC tools in hospitals (Hemsley et al, 2016). Communication barriers remain a concern because in many countries including Indonesia, there is lack of comprehensive studies about provision of AAC in health care settings. This study aimed to find out how important and effective the provision of AAC as a facility to help patients with speech disabilities in achieving effective communication with clinicians in health care.
A systematic review of the published literature was structured using the Pr eferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines. The authors were using independent selection, review, and appraisal of studies to approach the systematic review. In order to find relevant and reliable studies, the authors use several database s such as PubMed, Science Direct, ProQuest, EBSCO, and Clinical Keys, with keyword “Augmentative and Alternative Communication” OR “AAC” AND “Speech Disabilities” OR “ Speech Impairment” AND “Healthcare”. Studies gained were screened by including the exclusion and inclusion criteria to get sources that match the topic. Inclusion criteria include : studies published between 2015 2020, studies published in English, and studies related to Augmentative and Alternative Communication (AAC) for people with speech disabilities, while the exclusion criteria include: systematic review studies, inaccessible and ineligible studies, people with mental illness, people who undergo speech therapy, unaided AAC, and temporary functional speech disorder condition. Afterwards, to obtain reliable data, an assessment of the quality and validity of the literature used was carried out using JBI critical appraisal indicators. The entire process of the systematic review could be seen in Figure 1.
Figure 1. Flowchart of the Systematic

The search of keywords on various databases and other sources resulted in a total of 8803 articles. 7395 studies were gained after duplicates were removed and resulted in 115 articles after titles and abstract were screened. Another 100 articles were excluded based on exclusion criteria. Lastly, 15 full text studies were assessed for eligibility and four articles were suitable for our systematic review. Important data such as author(s) name and year of publications, study design, population, country, primary medical conditions, AAC type, study results, and limitation of study were included in Table 1. Studies examined using JBI critical appraisal indicators to check its quality. JBI score of all articles could be seen in Table 2 which located on the appendix , whereas the entire process shown in Figure 1.
The communication between patients and health care providers is widely regarded as important because of its contribution to q uality of care (Stans et al, 2018) Unfortunately, interacting with the health care provider presents a challenging set of scenarios for patients with speech disabilities who suffer from acquired brain injury and physical limitations as their primary health conditions. They explained that they could not understand difficult words or that the health care provider did not understand them because of their speech problems. This study highlights that the health care providers are often unaware that using AAC can empower patients to be more involved in conversations. Based on some patient statements, the use of conventional semiotics is a very helpful system, such as writing, for expressing themselves during a conversation. Whereas for health care providers, conversations with photos, a picto book, or written information by using a computer can also help patients to understand or remember what they said. Therefore, it is important to gain insight into the potential of AAC and how it can help both patients and health care providers to achieve equal participation in dialogue conversations or other communication strategies (Stans et al, 2018).
Another study conducted by Naro et al (2019) shows the effectiveness of AAC training (AAC T) in patients with early stage of Amyotrophic Lateral Sclerosis (ALS). The use of low tech AAC proved to be useful in improving communication, expressing patients’ needs, preventing loss of motivation, supporting their daily activities, also increasing self esteem and autonomy. The study also reveals a significant reduction of burden owned by caregivers and an increasing amount on psychological and emotional basis. By providing AAC services to ALS patients, we give patients the opportunity to express their needs, opinions, thoughts, and ability to adapt (Naro et al, 2019)
Stans et al (2018) Qualitative Study : Observatio ns and semi structured interviews
People with acquired brain injury and physical limitations and their professionals
Netherlands Brain injury and physical limitations
Low tech & high tech AAC : writing, photos, a picto book and computer
Health care providers are aware of the importance of preparation, in moderation time, a suitable environment and consider nonverbal communication in conversational dialogue. However, both patients and service providers still struggle with the use of adequate communication strategies, such as verbal communication and AAC due to lack of knowledge.
The limitations of this study relate to the potential for bias in sampling and socially acceptable answers during the interview.
Moffatt et al (2015) Qualitative Study :Web based survey and Group Observatio n
Clinicians with their aphasia patients who participated in Group Theraphy Session.
Germany Aphasia High Tech AAC : Smart Devices
According to the study there is increased enthusiasm in adapting high tech AAC devices in aphasia patient because high tech AAC devices are more ergonomically effective and cheaper also carry less stigma than traditional AAC devices.
The limitation of this study is low enthusiasm of clinicians about the AAC applications.
Naro et al Experiment 10 patients Italy Amyotroph Low Tech This study of AAC training (AAC T) The main limitation of the
(2019) al design with Amyotrophic Lateral Sclerosis (ALS) and their caregivers.
ic Lateral Sclerosis (ALS)
AAC: Communi cation tables
were divided into 2 phases, AAC intervention (AAC I) for three months followed with AAC-familiarization (AAC F) for another three months. Wilcoxon test showed significant improvements in most of the variables investigated, such as global cognitive functioning, adaptive coping strategies, mood, and QoL.
study is the small size of the sample and the lack of a control group.
et al (2019) Experiment al design :
A single subject, alternating treatment design
Three elementary school children between 6 9 years old
USA Down syndrome, polymicrog yia and encephalo macia
HighTech VSD and Low Tech Isolated Symbol
All three participants showed higher engagement with high-technology VSD than the low tech isolated picure symbols.
The largest limitation of the current study is small number of participant (n=3). The study only using two AAC technology option with their clinical relevance. It is difficult to tell participants’ engangement towards hightech AAC because of the short intervention.
On the other hand, according to Holyfield et al (2018) augmentative and alternative communication method using high tech VSD and low tech isolated symbols found to be effective for participants with speech disabilities. Participants for this study are three elementary school children between 6 9 years old with speech disabilities and underlying medical conditions. Participants known to have different primary health conditions that are down syndrome, polymicrogyria, and encephalomalacia. Study session for all of the participants was over an 8 week period. Duration per session approximately 5 minutes, and occured in the SLP therapy room. The study was using color photo in AAC app on a 10.2 inch touchscreen tablet for the high tech VSD and color printed isolated picture symbols for the low tech AAC. All three participants showed higher engagement using high tech color photo VSD than low tech isolated picture symbols because of the several features that only present on the high tech VSD. First was the technology itself, high technology may be interesting for t he children. Other than that, the high tech VSD uses voice output in their app as response to selection and can make a higher interest for the children not to mention the use of color photo VSDs itself (Holyfield et al, 2018).
In addition, application of AAC in health care is in line with current technological developments. The emergence of new devices has made a positive contribution to the development of high tech AAC that can be applied in health care. A research was conducted through an online survey fo r clinicians who are treating aphasia patients and observation on application of various types of AAC in focus groups with aphasia patients. The results show an increased enthusiasm for the use of high tech AAC devices such as the iPad and iPod Touch (Moffatt et al, 2015). It was found that high tech AAC devices are the most successful for face to face, one to one conversations, conversation in supportive locations such as rehabilitation clinics, and with familiar partners such as spouses. It is known that the most frequently used device is DynaVox, which is an assistive device that has been widely used by aphasia patients, although in fact the most recommended device is t he iPad which has a more general function. It is known that patients refer to use more familiar device, also it was said that the participants had already invested too much time, effort, and money into DynaVox (Moffatt et al, 2015).
Another important thing to notice from the survey is we should consider the advantages and disadvantages of using high tech AAC. The advantages of using high tech AAC include less stigma compared to traditional devices, and also they are more ergonomically effective. These devices are also cheaper than traditional options, while the drawbacks are limited software, lower volume, less durable, screen hard to read, and screen hard to use (Moffatt et al, 2015). To overcome the existing disadvantages, it is suggested that in the future the development of high tech AAC devices must be adjusted based on the user's existing low-tech proficiencies and hopefully could create integrated applications that enhance the
learning process, also reduce the customization needed to set up an AAC device. If we can overcome these challenges, affordable low cost smart mobile devices could significantly aid communication and improve the quality of life for individuals who have aphasia (Moffatt et al, 2015).
In this systematic review, each study has several limitations. The largest limitation of the reviewed studies is the small number of participants, thus the studies unable to represent the whole population. Some of the studies also have a potential bias due to less homogeneous target groups and lack of control groups. Besides that, all of the current studies conducted in developed countries do not cover the whole world population. However, studies regarding AAC provision are still lacking. Lastly, there is limitation in technical, amount, and variety of AAC technology used in the study.
Through the process of undergoing assessment in each of the chosen studies, we can conclude that there is still lack of awareness from health care providers in using AAC to improve patients’ satisfaction and achieve equal participation for patients with co mmunication disabilities. However, it has been proven that AAC has a significant role in breaking communication barriers and providing patient provider effective communication. Further studies regarding AAC potential, implementation, and provision in health care settings need to be conducted, especially in developing countries such as Indonesia.
1. American Speech Language Hearing Association. (2016). Scope of practice in speech language pathology.
2. American Speech Language Hearing Association. (2017). Speech sound disorders: articulation and phonology. Practice Portal. Nd.
3. Antonino Naro, M. D., Bramanti, P., Simona Portaro, M. D., & Calabrò, R. S. (2019). Augmentative and alternative communication improves quality of life in the early stages of a myotrophic lateral sclerosis. Functional neurology, 34(1), 35 43.
4. Blackstone, S. W., & Pressman, H. (2016). Patient communication in health care settings: New opportunities for augmentative and alternative communication. Augmentative and Alternative Communication, 32(1), 69 79.
5. Elsahar, Y., Hu, S., Bouazza Marouf, K., Kerr, D., & Mansor, A. (2019). Augmentative and alternative communication (AAC) advances: A review of configurations for individuals with a speech disability. Sensors, 19(8), 1911.
6. Hemsley, B., Georgiou, A., Hill, S., Rollo, M., Steel, J., & Balandin, S. (2016). An integrative review of patient safety in studies on the care and safety of patients with communication disabilities in hospital. Patient education and counseling, 99(4), 501 511.
7. Holyfield, C., Brooks, S., & Schluterman, A. (2019). Comparative effects of high tech visual scene displays and low tech isolated picture symbols on engagement from students with multiple disabilities. Language, speech, and hearing services in schools, 50(4), 693 702.
8. Judge, S., Enderby, P., Creer, S., & John, A. (2017). Provision of powered communication AIDS in the United Kingdom. Augmentative and Alternative Communication , 33(3), 181 187.
9. Stans, S. E., Dalemans, R. J., Roentgen, U. R., Smeets, H. W., & Beurskens, A. J. (2018). Who said dialogue conversations are easy? The communication between communication vulnerable people and health care professionals: A qualitative study. Health Expectations, 21(5), 848 857.
10. Moffatt, K., Pourshahid, G., & Baecker , R. M. (2017). Augmentative and alternative communication devices for aphasia: the emerging role of “smart” mobile devices. Universal Access in the Information Society, 16(1), 115 128.
Study 1 (Stans et al, 2018)
Study 2 (Moffatt et al, 2015)
1. There is congruity between the stated philosophical perspective and the research methodology Yes Yes
2. There is congruity between the research methodology and the research question or objectives Yes Yes
3. There is congruity between the research methodology and the methods used to collect data Yes Yes
4. There is congruity between the research methodology and the representation and analysis of data Yes Yes
5. There is congruity between the research methodology and the interpretation of results Yes Yes
6. There is a statement locating the researcher culturally or theoretically No Unclear
7. The influence of the researcher on the research, and vice versa, is addressed Unclear Yes
8. Participants and their voices are adequately represented Yes Yes
9. The research is ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body
Yes No
10. Conclusions drawn in the research report flow from the analysis, or interpretation, of the data Yes Yes
Study 3 (Naro et al, 2019)
Study 4 (Hoyfield et al, 2019)
1. There is no ambiguity regarding the independent and dependent variables exploring causal relationships Yes Yes
2. All the participants included in any comparisons were similar Yes Yes
3. All the participants included in any comparisons were receiving similar treatment/care, other than the exposure or intervention of interest Unclear No
4. There was a control group No No
5. There were multiple measurements of the outcome both pre and post the intervention/exposure Yes No
6. Follow up was complete and if not, there were differences between groups in terms of their follow up adequately described and analyzed Yes Yes
7. There were outcomes of participants included in any comparisons measured in the same way Yes Yes
8. The outcomes were measured in a reliable way Yes Yes
9. The statistical analysis used was appropriate Yes Yes
Assessment of Mesenchymal Stem Cells Therapy as A Potential Treatment to Improve Neurological Function in TBI Patients: A
Rahmah Salsah Hudriyah1, Namira Salma Ghinanafsi2, Yudivaniel Zihono3, Michelle Imanuelly4
1Faculty of Medicine, Pembangunan Nasional Veteran Jakarta University, Jakarta, Indonesia
2Faculty of Medicine, Pelita Harapan University, Tangerang, Banten, Indonesia
Introduction: Traumatic Brain Injury (TBI) has become a major etiology in persistent disability in children and young adults, causing mortality and morbidity in several cases Injury in the brain tissue usually causes neurological degeneration Although there are no definite treatments that can cure neurological impairment, it has been found that various stem cell therapy may have beneficial effects for patients with neurological deficits This systematic review was made to find out whether stem cell treatments are possible for improving neurological impairments
Objective: This study aims to evaluate the potential of mesenchymal stem cells (MSCs) as a therapy in TBI patients to improve neurological functions.
Materials and Method: This systematic review was conducted based on the PRISMA guideline. Studies included are the cohort and randomized controlled trials which were collected from various electronic databases, such as PubMed, ScienceDirect, ProQuest, and Cochrane, with no year limitation. The inclusion is assessing the after effect of MSCs transplantation in TBI patients to the improvement of neurological function. Joanna Briggs Institute (JBI) critical appraisal tools are used to assess the quality of each study.
Result: Seven studies were included in the review. Two of the studies which conducted in humans show improvement in motor function, sensation and balance function, and self care ability based on neurological assessment tools. Another improvement was shown in persistent vegetative state patients that were able to perform relaxed muscular tension and enhanced motor power after MSC transplantation. Five other studies were using rats as samples showing positive results in improved neurological function after MSC transplantations based on Neurological Severity Score and Rotarod assessment
Conclusion: This systematic review provides qualitative evidence suggesting that mesenchymal stem cells could be utilized as potential therapy for TBI patients to improve neurological function and prognosis
Keywords: Mesenchymal Stem Cells; Traumatic Brain Injury; Neurological Functions
Assessment of Mesenchymal Stem Cells Therapy as A Potential Treatment to Improve Neurological Function in TBI
Rahmah Salsah Hudriyah1, Namira Salma Ghinanafsi2, Yudivaniel Zihono3, Michelle Imanuelly4
1Faculty of Medicine, Pembangunan Nasional Veteran Jakarta University, Jakarta, Indonesia
2Faculty of Medicine, Pelita Harapan University, Tangerang, Banten, Indonesia
Traumatic brain injury (TBI) is one of current major sources of death worldwide, becoming the most notable cause of long lasting disability in children and young adults.1 According to World Health Organization, TBI has become the main problem of human mortality and morbidity even more since 2020.2 It is known for the poor prognosis with its prevalent disabilities mostly found in survivors which are motor dysfunction, psychological and social cognitive deficit that not only could burden their own daily life, but also their family and closed ones.3
During the past 24 years, there’s been a gradual improvement of the prehospital and intensive care of TBI and a development of management in evidence-based guideline indeed 4 However until this date, the current strategy of routine medical intervention still has little benefit to none in patients who has suffered from TBI for more than one year 5 Therefore, developing any modern alternative therapy modalities is needed for the clinical treatment breakthrough
(MSCs) have been looked into as the treatment of TBI due to their effects in neural regeneration and neurotrophic MSCs are heterogenous multipotent, fibroblast like adult cells found in the stromal compartment which can be isolated from bone marrow and perivascular tissue 7
MSCs grow with intrinsic potential of differentiation that couldn’t be found in any other cells 8 In recent years, several studies have investigated MSCs potential in neuroprotective effects and ability to migrate toward the damaged brain tissue, helping the repairment by replacing damaged cells with more differentiation while also releasing an abundance of useful anti inflammatory cytokines and growth factors, thus can be seen in a significant improvement of neurological function manifestation.7
According to Cox et al., it is found that neurological impairment in acute neurological injuries can be improved with the beneficial effect of various stem cell therapy such as mesenchymal stem cells (MSCs), neural stem cells (NSCs), multipotent adult progenitor cells (MAPCs), and endothelial progenitor cells (EPCs).6 Additionally, mesenchymal stem cells
Furthermore, TBI could break the impermeability of the blood brain barrier, letting immune cells to invade and activate glial cells to create a hostile microenvironment, triggering immune response and the secretion of inflammatory mediators even affecting other systems such as endocrine 9 So, recognizing that the logical target will be both localized delivery in intracerebral and also systemic to peripheral could lead to secondary cell death 10 This indicates that direct transplantation and systemic delivery of MSCs therapy with its
therapeutic effect may be an effective choice for TBI.
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta analysis (PRISMA) criteria
This review includes all studies that involved:
a. Types of participants
Authors included any studies involving both male and female adults with no significant age difference who showed lack of motor ability and or neurological dysfunction during the study period after getting diagnosed with severe TBI for at least 1 month. Working diagnosis of TBI was based on clinical manifestation and radiologic neuroimaging, such as head computed tomography and MRI
b Types of intervention These patients did not have any serious complications or chronic illness and did not undergo any pharmacological treatment that could have affected the functional assessment result and no other
abnormalities related to the stem cell transplantations were found.
c Types of outcome measures
The expected outcomes are improvement of neurological function which is including but not limited to motor activity, balance, muscle movements range and control that was assessed and graded with: (1) Fugl Meyer Assessments (FMA) and Functional Independence Measures (FIM); and (2) Persistent Vegetative State Evaluation by alertness and awareness which is characterized by a lack of response to the environment.
This review includes all studies that involved:
a. Types of participants
This included studies using rats as the animal model published in English. There is no limitation for gender, age, species, or year published. Studies not published in English and using other animals than rats were excluded
b Types of intervention
There is no intervention added that could interfere with the assessment process
c Types of outcome measures
Studies on rats were assessed by a group of modified Neurological
Severity Scale (mNSS) tests, which is an adjustment of Neurological Severity Scale (NSS) for rats, between the groups of cell transplantation and the control group for evaluation whether the stem cell transplantation can improve their neurological deficit The performance included from the rats’ motor, sensory, reflex, movements, and beam walking tests NSS was graded on a scale of 0 to 18 as maximum score in which 0 point indicates the ability to perform the tasks normally while the higher the NSS score, the more severe the injury is.
Studies included are any randomized controlled trials (RCT) and cohort study using mesenchymal stem call to treat the neurological function in TBI patients. Review, case reports, case series, conference abstracts are excluded. Only English studies are included and no limited published year is applied
The authors did literature search through several electronic databases and search engines, including PubMed, Cochrane, ProQuest, and ScienceDirect, with keywords used in search were “mesenchymal stem cell”, “MSC”,
“mesenchymal stromal cell”, “traumatic brain injury”, and “TBI'' such a presented in Table 1 No time and language restriction is applied To simplify collecting and extracting the study collections, authors used the Zotero program
Studies were collected from several databases according to its congeniality with keywords mentioned before After duplicates were removed, retrieved journals were screened based on their titles and abstracts. Thereafter, full text assessment was done to select eligible studies based on inclusions and exclusions criteria. At the end, 7 studies were selected for the review. Discrepancies among the review team were solved by discussion.
Eligible studies were reviewed and several characteristics of studies were extracted. The studies characteristics include: title and JBI assessment score, author's name, year of publication, country of performed study, study design, sample size and characteristic, evaluation or assessment tools, result, and limitation of the study Any disagreements were solved through discussion among the review team
The quality of each study was assessed using JBI critical appraisal tools. These tools classify its indicators based on study design of reviewed study From 7 eligible studies, 6 are randomized controlled trials and 1 cohort study The summary of studies quality assessment pictured in Table 3 and Table 4.
A search was conducted from several databases, a total of 2256 studies were found. Thereafter, through title and abstract screening 21 journals identified as relevant. After inclusion and exclusion criteria screened, a total of 7 studies were eligible for this review (Tian et al, 2013; Wang et al, 2013; Zhao et al, 2012; Mahmood et al, 2004; Anbari et al, 2014; Mahmood et al, 2006; Bonilla et al, 2009). PRISMA flow chart shown in Figure 1 to summarize search and selection methods in this review
Seven studies assessed the effect of Mesenchymal stem cells on improving neurological function in post traumatic brain injury cases Two studies evaluated the MSC effect on humans, the other 5 studies were conducted by using rats as samples (Table 2)
In human studies there is still limited source due to limited use and trials of MSC as treatment for TBI patients Authors only found 2 studies that fulfilled eligibility criteria for human studies Two studies involved were conducted in different study designs, including randomized control trial and cohort study Both of the studies are performed in China
Study conducted by Tian et al involved 97 patients who had a diagnosis of severe TBI based on clinical evidence and neuroimaging. And these patients did not have other serious complications (eg, cachexia, pulmonary infection, and gastrointestinal bleeding). Patients involved in this study were stabilized before receiving bone marrow mesenchymal stem cell (BMSC) transplant voluntarily. This study concluded that BMSC therapy improves consciousness and motor functions in patients with TBI. Also, there is a significant effect of patients' age and time elapsed between injury and therapy in improving the outcome of BMSC therapy
Wang, et al conducted a A randomized single blind controlled clinical study in 40 patients with sequelae of TBI Twenty patients in the treatment group underwent human umbilical cord mesenchymal stem cell (UCMSC) transplantation via lumbar
puncture. In this study MSC was acquired from a fresh umbilical cord with written consent of the parents The study showed significant improvement in neurological function and self care after 6 months follow-up Characteristics of included studies are presented in Table 1
All studies involving rats as samples used randomized controlled clinical trials study design Four of the studies used wistar rats with a total sample 88 rats consisting 68 female rats and 20 male rats. Two studies use female wistar rats, while another two use male wistar rats. One of the studies conducted by Zhao et al. used a total of 90 male Sprague Dawley rats. Almost all of the studies using intravenous injection for MSC administration, one study conducted by Bonilla et al. used intracerebral transplantation method. Four of the studies were using bone marrow mesenchymal stem cells, one study used human umbilical cord blood mesenchymal stem cells to treat TBI in rats Characteristics of included studies are presented in Table 1
Mesenchymal stem cell in improving neurological function in human Studies involving human clinical trials of Mesenchymal stem cells in TBI patients showed positive results in improving patient neurological function
One of the initial trials in using mesenchymal stem cells to treat TBI was done by Wang et al in 2013 In his findings Wang evaluated the effect of MSC using Fugl Meyer Assessment (FMA) and (Functional Independence Measures) FIM scoring FMA score was established to provide a numeric score of motor status such as motor function, balance, sensation qualities and joint function in hemiplegic patients (1) while FIM score designed to measure degree of disability based on independencies of patient’s performance (2). FMA scores after TBI patients treated with MSC demonstrated an improvement in upper extremity motor subscore, lower extremity motor subscore, sensation subscore and balance subscore in the stem cell transplantation group at 6 months after the transplantation (P<0.05). This result showed a significant improvement of neurological function compared to FMA score at the baseline and the control group. The FIM score results also exhibited significant improvement (P<0.05) in the patient self care sub score, sphincter control sub score, mobility sub score, locomotion sub score, communication sub-score and social cognition sub-score This result showed a significant improvement of neurological function compared to FIM score at the baseline and the control group 25
Tian et al. conducted a study on identifying the effect of bone marrow MSC in 97 patients with TBI Among 24 patients in vegetative state, 11 patients showed a significant post therapeutic improvement (P=0 24) Three patients expressed responsive eyeball tracking, 2 groaning, 5 responsive tearing, 2 swallow fluid blood Twenty seven of 73 patients showed significant improvement in motor function (P=0 025) Ten patients with muscle spasticity expressed muscular tension relaxed partly, 10 showed enhancement of motor power, 3 showed reducement of uncoordinated muscle movement. Tian et al. also measured the effect of patient’s age and time elapsed between injury and therapy on improving outcome after MSC therapy. The result showed young patients have a better outcome than the older one (P<0.05) and the earlier cellular therapy begins in the subacute stage of TBI, the better the results (P<0.05). 24 All of the results mentioned above concluded an improvement in neurological function after MSC therapy in TBI patients
A study conducted by Zhao et al used 90 male sprague rats to analyze the effect of human umbilical cord blood mesenchymal stem cells (hUCB MSC) as a treatment for
TBI patients. The study identified survival and migration of hUCB MSC through histological view, behavioural analysis, angiogenesis measurement, and level of cytokine secretion Histological findings showed migration and survival of hUCB-MSC through Bromodeoxyuridin(BrdU) labelled hUCB MSC expression in the injured cerebral cortex at 14 days after hUCB MSC transplantation The number of BrdU labeled hUCB MSC (/400 fold field of view) was 76 17 ± 8 30, 62 33 ± 8.40, 54.33 ± 7.50, 45.50 ± 6.59, and 28.67 ± 2.73, respectively at 3, 7, 14, 21, and 28 days following hUCB MSC transplantation, revealing a decreasing trend. Zhao et al. also observed less pathological change (breakdown of tissue, neuronal degeneration, shrunken cell bodies, cell swelling, lysis, disrupted cell membranes, and clumped cells with condensed nuclei) in rats who received hUCB MSC transplantation after TBI compared to model group of TBI without any treatment Another effect of hUCB MSC in rats with TBI is decreased number of apoptosis in brain tissues compared to the model group Apoptotic rate between transplantation and model groups show significant differences
Transplantation hUCB MSC also increased neurotrophic factor expression surrounding injury areas, promoted angiogenesis and
related cytokine expression surrounding injured brain tissue in TBI rats. One week after hUCB MSC transplantation
Neurological severity scores (NSS) were decreased compared to the model group The following weeks (14,21, and 28 days) NSS were significantly decreased, this result indicating decreased injury severity in the rat model of TBI 19
rats, and 3) Elevated NGF, BDNF, and bFGF expression in the injured site. The neurological function of rats was studied by using Rotarod Motor Test and modified Neurological Severity Scores (mNSS) In rotarod motor test rats are tested using an accelerating Rotarod Motor Test Both rotarod motor test and mNSS show a significant improvement compared to the control group on day 15 after TBI 20
Similar findings were found in a study conducted by Anbari et al This study showed migration and differentiation of BrDU labeled MSC into the parietal lobes of injured brains in rats after MSC transplantation in rats with TBI. NSS scores were also evaluated through this study. NSS showed no differences between the groups of traumatic brain injury and cell transplantation at 1 and 7 days post injury (P>0.05), respectively. Even so, there is significant improvement in rats motoric function 14 days after injury (P=0.01).22
Mahmood et al conducted a study to investigate the effects of intravenous administration of marrow stromal cells (MSCs) on the expression of growth factors in the rat brain after traumatic brain injury (TBI) This study key findings are 1) Migration of MSCs after brain injury into the injured hemisphere, 2) Improvement in the functional outcome of MSC treated
A study conducted by Bonilla et al investigated the efficacy of bone marrow MSC delayed transplantation to improve neurological sequels after TBI. This study used 20 female adult Wistar rats that received allogeneic BMSC from adult male wistar rats. All rats were tested on rotarod motor test and mNSS test daily 10 days before TBI, 2 months after TBI, and 2 months after intracerebral BMSC administration. BMSC transplanted rats showed significant differences compared to the control group. Significant recovery was detected through increased Rotarod score in 2 weeks and decreased mNSS in 6 weeks after BMSC transplantation 23
In a study conducted by Mahmood et al , the effect of BMSC transplantation in improving neurological function was assessed using designated NSS scores These tests were performed by all rats before TBI; after TBI they were performed
at 1 and 2 weeks and biweekly thereafter.Treatment of rats with 4 x 106 or 4 x 106 BMSCs 1 week after TBI promoted an improvement in the NSS scores at 10 and 12 weeks after TBI In a comparison of the effect of different doses of BMSCs on NSS scores, 4 x 106 BMSCs showed better efficacy than 2 x 106 BMSCs and the same efficacy as 4 x 106 BMSCs Therefore, 4 x 106 BMSCs seems to be the optimal dose 21
Mesenchymal stem cells are multipotent, fibroblast like cells that are acquired from several tissues with regenerational ability. The most utilized adult MSC is acquired from bone marrow tissues and adipose tissues.8 Other sources of MSC that improved tissue renewal could be acquired from young adult tissues, umbilical cord tissue and placenta, these tissues are normally discarded at birth.8 Its ability to reduce inflammatory reaction, enhance immunomodulatory response through expression of several cytokine and immune cell release, anti-apoptotic, trophic, and angiogenic effects improve neurological function in several brain injury cases 10
months after the primary insult, and could induce biochemical and physiological events that lead to neuronal cell death 15 Neuronal cell death could affect patients neurological status such as motoric and sensory function
In recent studies it is known that mesenchymal stem cells could improve neurological function in Traumatic Brain Injury by several mechanisms that lead to renewal of damaged brain tissues This promising ability of MSC has been proven by several laboratory findings which have been reviewed in this paper Two clinical studies conducted by Tian et al. and Wang et al. proved that both umbilical cord and bone marrow MSC could give therapeutic effects that reflected in improvement of neurological functions in TBI patients. Therapeutic mechanisms that highlighted in both studies are neuroprotective, anti inflammatory, proliferation and differentiation of MSC into the phenotype of damaged and lost cells, trophic support and manipulations of the environment to stimulate endogenous neural repair and regeneration.24,25
In traumatic brain injury patients, initial injury forces caused primary brain injury such as tissue distortion and destruction in early post injury period 14 The secondary brain injury in TBI patients occurred after hours to days even
More detailed mechanism of MSC in repairing damaged brain tissues in TBI patients was shown in 5 laboratorial studies with rats as samples Histological assessment was done and proved that MSC transplantation could increase survival and migration of transplanted MSC, inhibited cell apoptosis, ameliorated pathological changes, promoted angiogenesis,
and increased expression of neurotrophic growth factors.24,25
Those repairment mechanisms are reflected in improvement of neurological function assessed using FMA score, FIM score, and evaluation in patients with vegeatative state In patients with increased FMA score after 6 months follow up there is significant improvement in ability to control upper and lower extremity motor, sensation, and balance function FIM score is also used to measure a patient's self care ability Significant improvements in FIM score were also observed 6 months after MSC transplantation. FIM score evaluation showed improvement in self care sub score, mobility sub score, locomotion sub score in TBI patients compared with the control group.25 Another improvement in neurological function was shown in patients with persistent vegetative state (PVS) at 1 month after acute traumatic brain injury that received MSC transplantation. PVS patients were able to express relaxed muscular tension and enhanced motor power. Also its known that younger patients and earlier transplantation improve the therapeutic effect of MSC transplantation 24
are measured in mNSS include motor (muscle status and abnormal movement), sensory (visual, tactile and proprioceptive), reflex and balance status 18 Rotarod score analysis also showed improvement in neuromuscular coordination in rats model with TBI
Mesenchymal stem cells (MSCs) ability to form several types of tissue become a breakthrough therapy to treat diseases that undergo tissue injury. Availability of MSC in several body tissues is easily obtained and does not require complex procedure. Thus, MSC therapy becomes promising. However, there is no detailed information regarding the best method for MSC administration. All of the studies mentioned above commonly use intravenous injection, only one study performed intracerebral transplantation. Also measurement of effective MSC transplantation dosage was done by only one of the studies, therefore we could not establish standard dosage for MSC transplantation in TBI patients
Five reviewed studies showing an improvement of neurological function through decreased modified neurological severity score (mNSS) in rats model with TBI 19 23 MNSS is used in assessing multiple deficits and can be good for testing over periods of 30 60 days Points that
This study concludes there is significant improvement of neurological function in patients with traumatic brain injury (TBI) after receiving mesenchymal stem cells (MSCs) transplantation. Several indicators were used to
measure improvement in TBI patients and all of them showed significant improvement compared to the control group Therapeutic effect of MSC transplantation is the key in tissue repairment of TBI patients
This review recommends further clinical trials to investigate the efficacy and safety of mesenchymal stem cells (MSCs) therapy as treatment for TBI patients.
The authors declared that there are no competing interests in this study.
1 Feigin VL, Theadom A, Barker Collo S, Starkey NJ, McPherson K, Kahan M, et al Incidence of traumatic brain injury in New Zealand: a population based study Lancet Neurol 2013;12:53 64
2 Maas, A I R , Menon, D K , Adelson, P D , Andelic, N , Bell, M J , Belli, A , et al (2017) Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 16, 987 1048.
3. Peng W, Sun J, Sheng C, Wang Z, Wang Y, Zhang C et al. Systematic review and meta analysis of efficacy of mesenchymal stem cells on locomotor
recovery in animal models of traumatic brain injury. Stem Cell Research & Therapy 2015;6(1) doi:10 1186/s13287 015 0034 0
4 Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM Guidelines for the management of severe traumatic brain injury Neurosurgery 2017 Jan 1;80(1):6 15
5 Xiong Y, Mahmood A, Chopp M Emerging treatments for traumatic brain injury. Expert opinion on emerging drugs. 2009 Mar 1;14(1):67 84.
6. Cox CS. Cellular therapy for traumatic neurological injury. Pediatric research. 2018 Jan;83(1):325 32.
7. Zhou Y, Shao A, Xu W, Wu H, Deng Y. Advance of stem cell treatment for traumatic brain injury. Frontiers in cellular neuroscience. 2019 Aug 13;13:301.
8. Pittenger MF, Discher DE, Péault BM, Phinney DG, Hare JM, Caplan AI Mesenchymal stem cell perspective: cell biology to clinical progress NPJ Regenerative medicine 2019 Dec 2;4(1):1 5
9 Galindo LT, Filippo TR, Semedo P, Ariza CB, Moreira CM, Camara NO, Porcionatto MA Mesenchymal stem cell therapy modulates the
inflammatory response in experimental traumatic brain injury. Neurology research international 2011 Oct;2011
10 Bonsack B, Corey S, Shear A, Heyck M, Cozene B, Sadanandan N, Zhang H, Gonzales Portillo B, Sheyner M, Borlongan CV Mesenchymal stem cell therapy alleviates the neuroinflammation associated with acquired brain injury CNS neuroscience & therapeutics 2020 Jun;26(6):603 15
11 Fugl Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13 31. PMID: 1135616.
12. Linacre, J. M., Heinemann, A. W., Wright, B. D., Granger, C. V., & Hamilton, B. B. (1994). The structure and stability of the functional independence measure. Archives of Physical Medicine and Rehabilitation, 75(2), 127 132. doi:10 1016/0003 9993(94)90384 0
13 Andreas Bender, Ralf J Jox, et al 2015 Persistent Vegetative State and Minimally Conscious State. 2015; 112(14): 235 242 doi:10.3238/arztebl.2015.0235
14 Pittenger, M F , Discher, D E , Péault, B M , Phinney, D G , Hare, J M , & Caplan, A I (2019) Mesenchymal
stem cell perspective: cell biology to clinical progress. NPJ Regenerative medicine, 4(1), 1 15
15 Peng, W , Sun, J , Sheng, C , Wang, Z , Wang, Y , Zhang, C , & Fan, R (2015) Systematic review and meta-analysis of efficacy of mesenchymal stem cells on locomotor recovery in animal models of traumatic brain injury Stem cell research & therapy, 6(1), 47 https://doi org/10 1186/s13287 015 003 4 0
16 Greve, M W , & Zink, B J (2009) Pathophysiology of traumatic brain injury. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine: A Journal of Translational and Personalized Medicine, 76(2), 97 104.
17. Xiong, Y., Mahmood, A., & Chopp, M. (2009). Emerging treatments for traumatic brain injury. Expert Opinion on Emerging Drugs, 14(1), 67 84. doi:10.1517/14728210902769601
18. Schaar, K.L., Brenneman, M.M. & Savitz, S I Functional assessments in the rodent stroke model Exp & Trans Stroke Med 2, 13 (2010) https://doi org/10 1186/2040-7378-2-13
19 Zhao, J , Chen, N , Shen, N , Zhao, H , Wang, D , Shi, J , & Xue, H (2012) Transplantation of human umbilical cord blood mesenchymal stem cells to treat a rat model of traumatic brain
injury. Neural regeneration research, 7(10), 741.
20 Mahmood, A , Lu, D , & Chopp, M (2004) Intravenous administration of marrow stromal cells (MSCs) increases the expression of growth factors in rat brain after traumatic brain injury Journal of neurotrauma, 21(1), 33 39
21 Mahmood, A , Lu, D , Qu, C , Goussev, A , & Chopp, M (2006) Long term recovery after bone marrow stromal cell treatment of traumatic brain injury in rats Journal of neurosurgery, 104(2), 272 277.
22. Anbari, F., Khalili, M. A., Bahrami, A. R., Khoradmehr, A., Sadeghian, F., Fesahat, F., & Nabi, A. (2014). Intravenous transplantation of bone marrow mesenchymal stem cells promotes neural regeneration after traumatic brain injury. Neural regeneration research, 9(9), 919.
23. Bonilla, C., Zurita, M., Otero, L., Aguayo, C., & Vaquero, J. (2009).
Delayed intralesional transplantation of bone marrow stromal cells increases endogenous neurogenesis and promotes functional recovery after severe traumatic brain injury Brain Injury, 23(9), 760-769
24 Tian, C , Wang, X , Wang, X , Wang, L , Wang, X , Wu, S , & Wan, Z (2013) Autologous bone marrow mesenchymal stem cell therapy in the subacute stage of traumatic brain injury by lumbar puncture Exp Clin Transplant, 11(2), 176 181
25. Wang, S., Cheng, H., Dai, G., Wang, X., Hua, R., Liu, X., ... & An, Y. (2013). Umbilical cord mesenchymal stem cell transplantation significantly improves neurological function in patients with sequelae of traumatic brain injury. Brain research, 1532, 76 84

PubMed ("Mesenchymal Stem Cell" OR "MSC" OR "Mesenchymal Progenitor Cell" OR "Bone Marrow Stem Cell") AND ("Traumatic Brain Injury" OR "Traumatic Head Injury" OR "Traumatic Brain Injuries" OR "Traumatic Head Injuries")
Science Direct ("Mesenchymal Stem Cell" OR "MSC" OR "Mesenchymal Progenitor Cell" OR "Bone Marrow Stem Cell") AND ("Traumatic Brain Injury" OR "Traumatic Head Injury" OR "Traumatic Brain Injuries" OR "Traumatic Head Injuries")
ProQuest ((traumatic brain injuries) OR (traumatic brain trauma) OR (traumatic brain damage) OR (traumatic head injury) OR (traumatic brain injury)) AND (neurological deficit) AND ((mesenchymal stem cell) OR (Mesenchymal Stromal Cells) OR (Mesenchymal Stem Cells))
38
776
1735
Cochrane Mesenchymal Stem Cell AND Traumatic Brain Injury 9
Tian C et al, 2013 Cohort Patients with Persistent vegetative state: 24 Disturbance motor activity: 72
Wang et al, 2013 RCT Patients with Sequelae of TBI: 40
China Bone Marrow Grade principle of PVS
Significant Improvement in PVS Grade: P=0.24 Motor function: P=0.025
China Umbilical Cord
Fugl-Meyer Assessment s (FMA) Functional Independen ce Measures (FIM)
Significant Improvement (after 6 months) in FMA scores: P<0.05) FMI scores: P<0.05
Zhao et al, 2012 RCT Sprague Dawley rats (Male): 90 China Human Umbilical Cord Blood
Mahmood A et al, 2004
Mahmood A et al, 2006
Anbari F et al, 2014
Bonilla C et al, 2009
NSS Significant improvement of NSS score: P<0 05
RCT Wistar rats (Male): 12 Michigan Bone Marrow Rotarod motor test mNSS
Significant improvement of mNSS score and Rotarod Test
RCT Wistar rats (Female): 40 Michigan Bone Marrow NSS Significant improvement of NSS score
RCT Wistar rats (Male): 16 Iran Bone Marrow NSS Significant improvement of NSS score
RCT Wistar rats (Female): 20 Spain Bone Marrow Rotarod motor test mNSS
Significant improvement of mNSS score and Rotarod Test
Was true randomization used for assignment of participants to treatment groups? 1 0 1 1 0 0
Was allocation to treatment groups concealed? 1 0 0 0 0 1
Were treatment groups similar at the baseline? 1 1 1 1 1 1
Were participants blind to treatment assignment? 0 0 1 0 1 1
Were those delivering treatment blind to treatment assignment? 0 0 0 0 0 0
Were outcomes assessors blind to treatment assignment? 1 1 0 1 0 0
Were treatment groups treated identically other than the intervention of interest? 1 1 1 1 1 1
Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed?
1 1 1 1 1 1
Were participants analyzed in the groups to which they were randomized? 1 1 1 1 1 1
Were outcomes measured in the same way for treatment groups? 1 1 1 1 1 1
Were outcomes measured in a reliable way? 1 1 1 1 1 1
Was appropriate statistical analysis used? 1 1 1 1 1 1
Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?
1 1 1 1 0 1
Total 11 9 10 10 8 10
Tian et al., 2013
Were the two groups similar and recruited from the same population? 1
Were the exposures measured similarly to assign people to both exposed and unexposed groups? 1
Was the exposure measured in a valid and reliable way? 1
Were confounding factors identified? 1
Were strategies to deal with confounding factors stated? 0
Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)? 1
Were the outcomes measured in a valid and reliable way? 1
Was the follow up time reported and sufficient to be long enough for outcomes to occur? 1
Was follow up complete, and if not, were the reasons to loss to follow up described and explored? 1
Were strategies to address incomplete follow up utilized? 1
Was appropriate statistical analysis used? 1
Total 10
TELETHON: Telemedicine Towards a Healthier Indonesia
[Correspondence E-mail: nielzhn1@gmail.com]
Introduction: Parkinson's disease (PD) is one of the most neurodegenerative diseases caused by degeneration of dopaminergic neurons in the substantia nigra pars compacta, reduced striatal dopamine, and the presence of Lewy Bodies. The prevalence of this disease ranges from 18 to 328 cases per 100,000 population with an incidence of 4.5 to 21 cases per 100,000 population. Currently, drug therapy is the treatment of choice for patients with PD. VR and exerg ames have been proven to improve balance function and daily life activities of patients with PD.
Objective: This systematic review aimed to evaluate the efficacy of VR and exergaming in improving postural instability for PD patients Methods: This systematic review was made using the Preferred Reporting Items for Systematic Reviews and Meta analyses (PRISMA) method to review and select the literature used objectively. Assessment of study bias was also carried out using the Risk of Bias (RoB 2) tool by Cochra ne for RCT studies and the Risk Of Bias in Non randomised Studies of Interventions (ROBINS I) for other studies.
Results and Discussion: We found 8 eligible studies with different study designs yielded a total of 194 patients with Parkinson’s Disease, t reated with home based virtual reality or home based exergaming. The studies were done in several places (Slovenia, Taiwan, Australia, Canada, Israel, and Italy) and published from 2012 to 2022. Three studies assessed the effect of virtual reality, while five studies assessed the effect of exergaming. Interventions were done for several sessions which were then assessed with its standardized respective tool, which includes BBS, BBT, FGA, TUG, MDS UPDRS, and Cohen U3. Author also found improvement in BBS, BBT, FGA, and TUG scores across all experimental results.
Conclusion: Home based virtual reality and exergaming telerehabilitation hold promise and potential as a feasible and valid alternative option for reducing postural i nstability in Parkinson’s Disease patients.
Keywords: Exergaming, Parkinson’s Disease, Postural Instability, Telerehabilitation, Virtual Reality
TELETHON: Telemedicine Towards a Healthier Indonesia
Introduction: Parkinson's disease (PD) is one of the most neurodegenerative diseases caused by degeneration of dopaminergic neurons in the substantia nigra pars compacta, reduced striatal dopamine, and the presence of Lewy Bodies. The prevalence of this disease ranges from 18 to 328 cases per 100,000 population with an incidence of 4.5 to 21 cases per 100,000 population. Currently, drug therapy is the treatment of choice for patients with PD. VR and exergames have been proven to improve balance function and daily life activities of patients with PD.
Objective: This systematic review aimed to evaluate the efficacy of VR and exergaming in improving postural instability for PD patients
Methods: This systematic review was made using the Preferred Reporting Items for Systematic Reviews and Meta analyses (PRISMA) method to review and select the literature used objectively. Assessment of study bias was also carried out using the Risk of Bias (RoB 2) tool by Cochrane for RCT studies and the Risk Of Bias in Non randomised Studies of Interventions (ROBINS I) for other studies.
Results and Discussion: We found 8 eligible studies with different study designs yielded a total of 194 patients with Parkinson’s Disease, treated with home based virtual reality or home based exergaming. The studies were done in several places (Slovenia, Taiwan, Australia, Canada, Israel, and Italy) and published from 2012 to 2022. Three studies assessed the effect of virtual reality, while five studies assessed the effect of exergaming. Interventions were done for several sessions which were then assessed with its standardized respective tool, which includes BBS, BBT, FGA, TUG, MDS UPDRS, and Cohen U3. Author also found improvement in B BS, BBT, FGA, and TUG scores across all experimental results.
Conclusion: Home based virtual reality and exergaming telerehabilitation hold promise and potential as a feasible and valid alternative option for reducing postural instability in Parkinson’s Di sease patients.
Keywords: Exergaming, Parkinson’s Disease, Postural Instability, Telerehabilitation, Virtual Reality
Parkinson's disease (PD) is a neurodegenerative disease caused by degeneration of dopaminergic neurons in the substantia nigra pars compacta, reduced striatal dopamine, and the presence of Lewy Bodies.1 This progressive disease will lead to movement disorders such as bradykinesia, static tremor, postural instability, and rigidity. This disease will get worse over time causing balance difficulties along with worsening cognitive function and a decrease in the patient's quality of life 2
PD is also one of the most common neurological diseases and affects 1% of people over 60 years of age. The prevalence of this disease ranges from 18 to 328 cases per 100,000 population with an incidence of 4.5 to 21 cases per 100,000 population.3 Currently, drug therapy is the treatment of choice for patients with PD. Unfortunately, this treatment is only effective in the first year after onset and not all symptoms can be treated with drug therapy. In addition, deep brain stimulation is also used as a treatment option by implanting electrodes in the brain to stimulate certain areas and overcome the symptoms of PD patients. However, improper intraoperative position or parameter stimulation can stimulate the peripheral nerve conduction bundle and cause adverse reactions 4 Another study with long term rehabilitation showed improvements in motor and cognitive function in patients with PD. Unfortunately, in its implementation in the clinic, this rehabilitation relies on rehabilitation therapies, financial conditions, the safety of the patient, and also training places.5 Therefore, it is very difficult for PD patients to undertake long term rehabilitation.
In recent years, research on virtual reality (VR) and exergaming as therapy has become a hot topic in neurorehabilitation research 6 VR itself can be defined as a virtual environment from a computer where a person can interact naturally and produce a sense of immersion in that environment. Exergame which is a combination of exercise and games can also increase the patient's motivation by getting physical exercise from a game 7 The potential transfer effect in virtual reality and exergaming is one of the therapeutic potentials in patients with PD which combines motor and cognitive function therapy at the same time, with VR and exergaming, patients can perform physical movements while exercising their cognitive f unctions.8 Several studies also show that VR and exergames can improve balance function and daily life activities of patients with PD 9 To our knowledge currently, there are no systematic reviews specifically assessing VR and exergaming in treating patients with PD. Therefore, this
systematic review aims to investigate the effects of VR and exergaming in overcoming patients with PD.
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta Analysis (PRISMA) criteria.
We conducted a comprehensive literature search through Cochrane, Google Scholar, Proquest, PubMed, Researchgate, and ScienceDirect for studies assessing the effectiveness of home based virtual reality and exergaming as treatments for postural or gait instability in patients with Parkinson’s Disease. This search used keywords such as “Parkinson’s Disease” AND “Postural Instability” AND Rehabilitation AND Telemedicine AND (“Virtual Reality” OR Exergaming).
For eligibility criteria, we used inclusion criteria: (1) type of study, randomized controlled trials, non randomized controlled trials, pilot studies, case report, and randomized parallel studies; (2) study population, Parkinson’s Disease patients with posture or gait instability; (3) intervention, home based treatment and used either virtual reality or exergaming as treatment; (4) outcomes, posture stability and movement scores using its respective tool in mean, standard deviation, and p value on both pre post or intervention control; and (5) include pre treatment and other treatment as control. Meanwhile, our exclusion criteria: (1) references not in English or Indonesian language; (2) unsuitable study design; (3) studies with irretrievable full text articles; and (4) studies that are not completed yet at the time of retrieval. Duplicate removal was done manually and screening of titles as well as abstract of studies was carried out according to criteria of accessibility by four independent reviewers. Any disagreements were discussed into consensus.
We extracted included studies using predetermined outcome sheets in tabular form to include the following data: (1) author and year of publication; (2) study characteristics, including study location, study period, and study design; (3) study population, including sample size, mean/range age, and Hoehn Yahr Scale; (4) intervention, including name of intervention,
frequency, and assessment tool used; and (5) study outcomes, including the efficacy of virtual reality and exergaming in improving postural instability for Parkinson’s Disease patients in terms of its mean difference and significance (p) values. Study characteristics were assessed qualitatively by four reviewers.
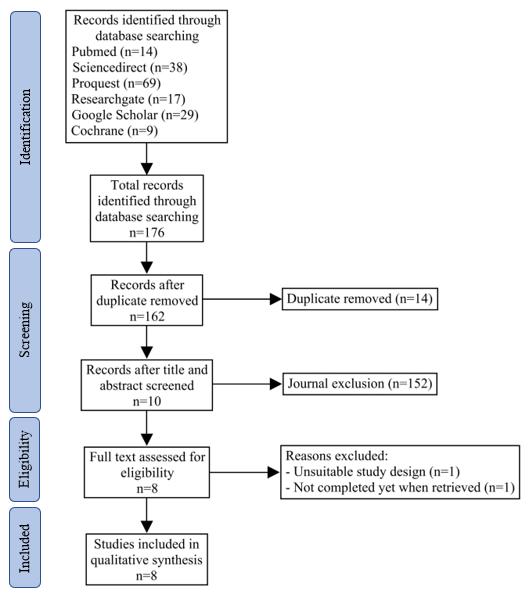
Figure 1. Literature search strategy based on PRISMA Statement
Several studies were included in our systematic review based on our literature searching with certain inclusion and exclusion factors. We found 8 eligible studies for systematic review. Those were included because each study is suitable according to our inclusion criteria. Included studies were all described in a table of characteristics shown in Appendix 2. Detailed literature search procedures were stated in Figure 1.
Eight studies with different study designs yielded a total of 194 patients with Parkinso n’s Disease, treated with home based virtual reality or home based exergaming, which were included for qualitative analysis. The studies were done in several places (Slovenia, Taiwan, Australia, Canada, Israel, and Italy) and published from 2012 to 2022. T he mean age of participants included was ranging from 18 and above which were further randomized into the intervention group and control group, or several follow up intervention groups. Three studies assessed the effect of virtual reality in improving postural and gait instability, while five studies assessed the effect of exergaming in improving postural and gait instability. Interventions were done for several sessions which were then assessed with its standardized respective tool, which includes BBS, BBT, FGA, TUG, MDS UPDRS, and Cohen U3 10 17 Detailed study outcomes were shown in Appendix 1.
The efficacy of virtual reality on patients with Parkinson's disease can be seen based on the research data in Appendix 3., Cikaljo et al. conducted a study comparing 3D and 2D. In 3D media, it was found that there was an increase in effort (Cohen U3 = 0.8) and interest (Cohen U3 = 0.5) with the end result being faster and more efficient (Cohen U3 = 0.9) While 2D reduced tension because it was easier to use (Cohen U3 = 0.3) 17
Improvement of Parkinson's Disease is supported by a study conducted by Yuan et al. using Interactive Video Game Based (IVGB). Better progress was found in patients who carried out the experiment in the second 6 weeks period with the acquisition of P value Berg Balance Scale (BBS) <0.0001; Modified Falls Efficacy Scale (MFES) 0.03; Multi-Directional Reach Test (MDRT) on the left 0.05; Maximum Step Length (MSL) on the right posterior 0.004 and left posterior 0.003. However, there is a slight significant change in MDRT on the right which is 0.09. According to Appendix 3., patients that underwent IVGB in their first 6 weeks period experienced setbacks. It is possible that the absence of control or further intervention contributed to the setbacks. A study by Yuan et al. also suggests that the multi directional step task and target directed stepping task of IVBG can improve motor coordination, ability to stand on one leg, and functional stepping, although IVBG exercise did not improve all MDRT and MSL subscales in the included sample 12
Cikaljo et al., also conducted a study using exergaming media at home groups and outpatient hospitals. The use of exergaming can increase BBT, decrease JHFT and UPDRS III in both groups.13 The Jebsen Hand Function Test uses units of time so that if the results decrease, there will be better progress because it is faster.
Research in Australia by Song et al. using home based step training resulted in an increase in Functional Gait Assessment (p value = 0.27) and a decrease in Stepping Performance (p value = 0.02).14 Stepping performance also uses time units.
The pilot study in Ottawa, Canada by Esculier et al., using the Nintendo Wii Fit and Balance Board resulted in significant changes in Parkinson's Disease patients with the results of CBM Scale (p value = 0.001), STST (p value = 0.01), TUG (p value = 0.04 ), 10 minutes Walk Test (p value = 0.001) and POMA (p value = 0.05).15
Yang W et al., conducted a comparison of experiments using VR Balance Training with Conventional Balance Training, found significant changes in patients with BBS results (p value = 0.001), DGI (p value = 0.001), TUG (p value = 0.001) and PDQ 39 (p value = 0.047).10 There were no significant effects in the 8th week follow up and instead it showed setbacks.
A case report from Tel Aviv Medical Center found an improvement in patients using the virtual reality treadmill method. Although there was no change in the Hoehn and Yahr Scale in patients, there were positive changes, such as an increase in gait speed in patient A from 2.8 km/h to 3.8 km/h and inpatient B from 3 km/h to 3.8 km/h, an increase in walking endurance from 15 minutes to 45 minutes and decreased MDS UPDRS.16 Patients also experience increased confidence in mobility which indicates an improvement in quality of life.
The current pandemic era requires medical personnel and patients to take advantage of technology in various fields, primarily in medical rehabilitation. Neurorehabilitation with virtual reality that has been widely carried out in clinics or conventionally so far has been quite good in improving the outcomes of patients with Parkinson's Disease. However, there are still some obstacles and challenges that conventional virtual reality rehabilitation has.
Patients need to go to the clinic/hospital to get the training, even though most patients with Parkinson's Disease themselves have poor mobility, especially with manifestations of postural instability. With the need for more mobilization, the time required will also increase.11
Conventional rehabilitation is also estimated to require higher costs because the tools used are specifically for rehabilitation training only. Meanwhile, home based virtual reality can take advantage of compatible technology equipment that the patient already owns to save costs. This is in accordance with the study by Gandolfi et al., the total cost required for conventional rehabilitation with SIBT in the clinic was €28,899.80, greater than home based virtual reality, which only required a total cost of €23,299.00. 11
Although telerehabilitation is carried out at home, it does not mean that the patient is doing their own training. Patients still have to be monitored by a physiotherapist connected via telecommunications such as Skype 11,16 Based on the research of Gandolfi et al., patients whom a physiotherapist monitored said that he could increase his exercise commitment. Because if it is self administered, the level of patient participation will be reduced 11 Study by Yuan et al., also declares that the IVBG program in this study provides various benefits for elderly patients with mild-to-moderate Parkinson's Disease. Compared to conventional stepping and balance training, auditory, and visual feedback exercises are pretty interesting for the patients. In addition, the direct feedback that patients get also increases their sense of accomplishment, thereby motivating them to do their best 12
In addition to seeing from the patient's perspective, telerehabilitation with virtual reality also has benefits from a physiotherapist's perspective. The study by Pablo et al. , was conducted with simultaneous multi participant, which means one physiotherapist can monitor two patients directly. Both of them stated that it was feasible to do so. This saves the physiotherapist's time and can reach more patients for rehabilitation training.16
The resulting outcomes for home based virtual reality must be equal to or even better than conventional rehabilitation. In general, the outcomes of home based virtual reality were not significantly worse than conventional rehabilitation. The study by Cikajlo et al., stated that the assessment of the UPDRS III scale from the homegroup showed a decrease from 24.6 + 6.3 to 22.9 + 7.3 after intervention for ten days with exergaming training for more than two
weeks. This is comparable to the change of the UPDRS III scale in the clinic sample group, which decreased from 31.2 + 10.9 to 28.8 + 10.9 16 Another study by Yang W et al., reported an increase in the Berg Balance Scale (BBS) value in patients who did 12 sessions of exercise, where each session took 50 minutes in 6 weeks. Changes in this value are relatively the same in the sample who intervened with home based virtual reality and conventional exercises. In the VR sample, the BBS value increased from 46.9 to 50.3, while for the conventional sample the value increased from 46.9 to 51.1 16
Another study by Gandolfi et al., also reported the same thing. This study compares Home VR Balance Training using the Nintendo Wii Fit system (TeleWii) and in clinic SIBT. In addition to using the BBS scale, this study also assessed posture instability with the Dynamic Gait Index (DGI) scale. In the home VR training sample group, the initial DGI value was 20.39 + 2.56 and increased to 21.24 + 2.56 after seven weeks of training. Meanwhile, for the SIBT in clinic sample group, the DGI value increased from 19.34 + 2.49 to 21.18 + 2.15. Another aspect that is also assessed and essential is the Activities Balance Confidence scale (ABC). This study states that respondents from both groups reported increased individual self confidence in carrying out activities 11
This systematic review highlights the positive role of recent rapid technological developments in the field of medical rehabilitation. This can be a consideration for neurological rehabilitation centers in Indonesia to develop more virtual reality based and exergaming teleneurorehabilitation for neurological diseases with posture disorders, such as Parkinson's Disease.
The limitation of this study lies in the relatively minimal number of reference studies. This is reinforced by initial searches on search engines such as Cochrane, Google Scholar, ProQuest, Pubmed, Researchgate, and Sciencedirect, which show studies with a number of 176 excluding exclusions and inclusions used in screening journals that will be used in this systematic review. In addition, the limitations of this systematic review are seen in the type of virtual reality used. This paper presents all the possibilities of virtual reality that can be used and does not focus on only one type.
As a further recommendation, further research is needed on protocols and unclear guidelines regarding the types of activities that can be carried out. This can help the physiotherapist and the patient so that the results obtained are more effective. Follow up on patients' comfort and interest in home based virtual reality also needs to be initiated because only a few research explains this. Hopefully, there will be more research and a holistic approach regarding virtual reality and exergaming based telerehabilitation to enhance rehabilitation care at home in people with Parkinson's Disease.
Home based virtual reality and exergaming telerehabilitation hold promise and potential as a feasible and valid alternative option for reducing postural inst ability in Parkinson’s Disease patients. It is also believed to increase adherence to long term exercise and have a beneficial effect on patient mobility and confidence.
We have nothing to declare.
We declare that we have no competing intention for completing for completing this review.
1. Weintraub D, Hauser RA, Elm JJ, Pagan F, Davis MD, Choudhry A. Rasagiline for mild cognitive impairment in Parkinson’s disease: A placebo controlled trial. Mov Disord. 2016 May;31(5):709 14.
2. Canning CG, Paul SS, Nieuwboer A. Prevention of falls in Parkinson’s disease: a review of fall risk factors and the role of physical interventions. Neurodegener Dis Manag. 2014;4(3):203 21.
3. Tysnes OB, Storstein A. Epidemiology of Parkinson’s disease. J Neural Transm. 2017 Aug;124(8):901 5.
4. Baizabal Carvallo JF, Jankovic J. Movement disorders induced by deep brain stimulation. Parkinsonism Relat Disord. 2016 Apr;25:1 9.
5. David FJ, Robichaud JA, Leurgans SE, Poon C, Kohrt WM, Goldman JG, et al. Exercise improves cognition in Parkinson’s disease: The PRET PD randomized, clinical trial. Mov Disord. 2015 Oct;30(12):1657 63.
6. Liu BB, Ding QN, Zhu WS. Research progress on the role of virtual reality technology in rehabilitation of nervous system diseases. Chinese J Contemp Neurol Neurosurg. 2018 Mar;18(3):222 5.
7. Koçer A, Oktay AB. Nintendo Wii assessment of Hoehn and Yahr score with Parkinson’s disease tremor. Technol Health Care. 2016 Mar;24(2):185 91.
8. Dyshel M, Arkadir D, Bergman H, Weinshall D. Quantifying Levodopa Induced Dyskinesia Using Depth Camera. Proc IEEE Int Conf Comput Vis. 2015 Feb;2015 February:511 8.
9. Xiao Xiao W, Hong Wei D, Hang L, Ai Hong W. Effects of Virtual Reality on Balance and Activities of Daily Living in Patients with Parkinson’s Disease: A Meta Analysis. Chin J Rehabil Theory Practice. 2017. p. 1443 9.
10. Yang WC, Wang HK, Wu RM, Lo CS, Lin KH. Home based virtual reality balance training and conventional balance training in Parkinson’s disease: A randomized controlled trial. J Formos Med Assoc [Internet]. 2016;115(9):734 43. Available from: http://dx.doi.org/10.1016/j.jfma.2015.07.012
11. Gandolfi M, Geroin C, Dimitrova E, Boldrini P, Waldner A, Bonadiman S, et al. Virtual Reality Telerehabilitation for Postural Instability in Parkinson’s Disease: A Multicenter, Single Blind, Randomized, Controlled Trial. Biomed Res Int. 2017;2017.
12. Yuan RY, Chen SC, Peng CW, Lin YN, Chang YT, Lai CH. Effects of interactive video game based exercise on balance in older adults with mild to moderate
Parkinson’s disease. J Neuroeng Rehabil. 2020;17(1):1 11.
13. Cikajlo I, Hukić A, Zajc D. Exergaming as Part of the Telerehabilitation Can Be Adequate to the Outpatient Training: Preliminary Findings of a Non randomized Pilot Study in Parkinson’s Disease. Front Neurol. 2021;12(March):1 11.
14. Song J, Paul SS, Caetano MJD, Smith S, Dibble LE, Love R, et a l. Home based step training using videogame technology in people with Parkinson’s disease: a single blinded randomised controlled trial. Clin Rehabil. 2018;32(3):299 311.
15. Esculier JF, Vaudrin J, Bériault P, Gagnon K, Tremblay LE. Home based balance training programme using Wii Fit with balance board for Parkinson’s disease: A pilot study. J Rehabil Med. 2012;44(2):144 50.
16. Cornejo Thumm P, Giladi N, Hausdorff JM, Mirelman A. Tele Rehabilitation with Virtual Reality: A Case Report on the Simultaneous, Remote Training of Two Patients with Parkinson Disease. Am J Phys Med Rehabil. 2021;100(5):435 8.
17. Cikajlo I, Peterlin Potisk K. Advantages of using 3D virtual reality based training in persons with Parkinson’s disease: A parallel study. J Neuroe ng Rehabil. 2019;16(1):1 14.
Databases
Keywords Articles
Pubmed (Parkinson) AND (Postural Instability OR Balance OR Gait OR Postural Imbalance) AND (Telemedicine OR Telerehabilitation OR Tele*) AND (Virtual Reality OR Exergaming)
Sciencedirect "Parkinson's Disease" AND ("Postural Instability" OR Gait) AND Rehabilitation AND Telemedicine AND ("Virtual Reality" OR "Wii Fit" OR “Exergaming”)
Proquest “Parkinson’s Disease” AND “Postural Instability” AND Rehabilitation AND Telemedicine AND “Virtual Reality”
14
38
69
Researchgate Telemedicine AND "Parkinson's Disease" AND (Gait OR "Postural Stability") 17
Google Scholar Parkinson’s Disease Virtual Reality Telerehabilitation Postural Instability (manual searching) 29
Cochrane (Parkinson) AND (Postural Instability OR Balance OR Gait OR Postural Imbalance) AND (Telemedicine OR Telerehabilitation OR Tele*) AND (Virtual Reality OR Exergaming)
9
1 Yuan et al, 2020
Taipei Medical University Hospital, Taipei
June 2014 January 2019
Randomized controlled trial
n = 24; 2 groups consist 12 person each group.
60 80 1 3 interactive video game based (IVGB)
12 weeks trial. First 6 weeks, Group A engaged in an IVGB exercise program, followed by a 6 weeks period without exercise. Group B participants completed the opposite,
• 36 Item Short Form Health Survey (SF-36)
• Modified Falls Efficacy Scale (MFES)
• Berg Balance Scale (BBS)
• Multi-Directional Reach Test (MDRT)
• Maximum Step Length (MSL)
2 Cikajlo et al, 2021 Slovenia Non Randomized Control Trial
n=28, m=12 & f=16
Home group= 62.3 + 7.3 Outpatient hospital= 69.5 + 4.5
2 3
Telerehabilitat ion system using computer (exergaming)
10 days of exergaming over 2 weeks, each daily session lasting maximum 1 hour
• Box and Blocks Test (BBT)
• Jebsen Hand Function Test (JHFT)
• Unified Parkinson’s Disease Rating Scale (UPDRS part III)
3 Song et al, 2018 Australia 12 weeks
Single Blinded Randomized Control Trial
4 Esculier et al, 2012 Ottawa, Canada 6 weeks Pilot Study
n=60, m=24 & f=36
Intervention= 68 Control= 65
UPDRS part 3 > 32 and UPDRS part 3 < 32
Home based step training using videogame technology.
nPD=11, F=5, M=6 PD=48 80 H=49 81
UPDRS Score = 18.4
2 3 sessions per week and a choice stepping reaction time once a week, 15 20 minutes per session
• Functional Gait Assessment (FGA)
• New Freezing of Gait Questionnaire (NFOGQ)
• Montreal Cognitive Assessment adjusted for education level (MOCA)
Balance Training Programme
40 minutes for 3 days per week during 6
• Activities-specific Balance and Confidence (ABC) Scale
nHS=9, F=4, M=5
using Nintendo Wii Fit and Balance Board
weeks. Data was taken in week 3 and 6
• Timed Up and Go (TUG)
• 10 minutes’ Walk Test
• Sit to stand Test (STST)
• Performance Oriented Mobility Assessment (POMA)
• Community Balance Mobility Scale (CBM)
5 Yang W et al, 2016
New Taipei City, Taiwan 8 weeks Randomized Control Study n=23, ex=11, ct=12 55 85 3
PD: VR Balance Training CT: Conventional Balance Training
For all groups, 12 training sessions, each session took 50 minutes, for 6 weeks. Follow up in week 8
• Berg Balance Scale (BBS)
• Dynamic Gait Index (DGI)
• Timed Up and Go (TUG) Test
• 9-item Parkinson’s Disease Questionnaire (PDQ 39)
• Unified Parkinson’s Disease Rating Scale (UPDRS III)
6 Pablo C et al, 2021
Tel Aviv Medical Center, Israel
May 2019 2020 Case Report 2 people 46 & 67 3 (Both of them)
Treadmill virtual reality system Consists of: treadmill, a TV screen, a depth camera (Microsoft Kinect) + Microsoft HD camera, personal computer installed with the VR simulation
Weekly sessions. Each session took three walking periods of 5 15 mins and 5 10 min of rest breaks between each period
• Feasibility and adherence to the training: number of sessions participated and self report of the patients and therapist
• Change in preferred gait speed: measured on the treadmill
• Walking endurance: duration of walking time between the first and last sessions
• Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS UPDRS) and Hoehn and Yahr
No Authors, Year Study location Study period Study design
• The Activities Specific Balance Confidence Scale
• Berg Balance Scale (BBS)
8 Gandolfi et al, 2017 Veneto, Italy 7 weeks RCT
76 (n = 38 home VR telerehab ilitation; n = 38 in clinic SIBT)
> 18 years old 2.5 3
Home VR Balance Training using the Nintendo Wii Fit system (TeleWii) and in clinic SIBT
21 sessions of 50 minutes each, 3 days/week for 7 consecutive weeks
• Activities Balance Confidence scale (ABC)
• 10 Meter Walking Test (10MWT)
• Dynamic Gait Index (DGI)
• Parkinson’s Disease Quality of Life questionnaire (PDQ 8)
8
Cikaljo and Peterlin Potisk, 2019
Slovenia May 2018 Decemb er 2018
randomized parallel study n = 20 60 79 2 3
3D Virtual Reality and non immersive 2D
3 weeks 10 session each group
• Mac Skilling p
• Cohen U3
First 6 weeks period
GROUP A
BBS : 1.0 + 3.8
MFES : 8.3 + 17.0
1 Yuan et al, 2020
MDRT- R : 8.5 + 7.4 MDRT L : 6.9 + 5.9 MSL R.Post : 4.3 + 13.4 MSL- L. Post : 2.9 + 14.3
GROUP B
BBS : 1.4 + 6.7
MFES : 8.1 + 14.1 MDRT R : 0.5 + 5.5 MDRT L : 0.8 + 5.8 MSL R.Post : 6.7 + 8.9 MSL L. Post : 6.7 + 7.7
BBT
Home group= 52.9 + 12.9 Outpatient Hospital= 44.6 + 9.3 JHFT
Second 6 weeks period
GROUP A
BBS : 3.1 + 4.9
MFES : 6.5 + 15.0 MDRT- R : -2.7 + 8.6 MDRT L : 2.7 + 8.3 MSL R.Post : 6.4 + 9.3 MSL- L. Post : -5.9 + 8.3
GROUP B
BBS : 9.9 + 7.2
MFES : 21.3 + 35.7 MDRT R : 2.2 + 4.2 MDRT L : 3.6 + 6.2 MSL R.Post : 7.5 + 11.5 MSL L. Post : 5.9 + 9.2
Home group= 56.6 + 13.6 Outpatient Hospital= 49.1 + 9.8 JHFT
First 6 weeks period
BBS : 0.85 MFES : 0.02 MDRT R : 0.003 MDRT L : 0.004 MSL- R.Post : 0.63 MSL L. Post : 0.43
Second 6 weeks period
BBS : <0.0001 MFES : 0.03 MDRT- R : 0.09 MDRT L : 0.05 MSL R.Post : 0.004 MSL L. Post : 0.003
2 Cikajlo et al, 2021
Home group= 50.8 + 13.5 Outpatient Hospital= 67.7 + 24.4 UPDRS III
Home group= 24.6 + 6.3 Outpatient Hostpital= 31.2 + 10.9
FGA
Intervention= 22.7 + 4.7 Control= 23.8 + 4.7
3 Song et al, 2018
Stepping Performance
Intervention= 824 + 176 Control= 847 + 221 NFOGQ
Intervention= 4.4 + 7.1 Control= 4.7 + 9.0
Home group= 44.5 + 9.8 Outpatient Hospital= 63.2 + 25.9 UPDRS III
Home group= 22.9 + 7.3 Outpatient Hostpital= 28.8 + 10.9
Intervention= 22.5 + 4.2 Control= 22.7 + 4.5
Stepping Performance
Intervention= 798 + 169 Control= 794 + 88 NFOGQ
Intervention= 4.9 + 7.2 Control= 3.5 + 8.1
BBT 0.003 JHFT 0.068 UPDRS III 0.005
FGA 0.27 Stepping Performance 0.02
ABC Scale
PD : increase 1.0 points HS : decrease 1.0 points CBM Scale
PD : increase 15.0 points HS : increase 7.5 points STST
CBM Scale
4 Esculier et al, 2012
5 Yang W et al, 2016
BBS VR : 46.9 CT : 46.9 DGI PD : 16.9 CT : 17.4 TUG PD : 22.9 CT : 21.1 PDQ-39 PD : 29.2 CT : 31.7 UPDRS-III PD : 22.5 CT : 21.7
PD : increase 5.0 repetitions HS : increase 2.5 repetitions TUG
PD : 1.9 seconds less HS : 1.2 seconds less 10-minutes’ Walk Test PD : 0.7 seconds less HS : 0.4 seconds less POMA PD : increase 4.0 points HS : no changes (max.28 points)
Week 6 BBS VR : 50.3 CT : 51.1 DGI PD : 21.0 CT : 20.6 TUG PD : 19.6 CT : 18.0 PDQ 39 PD : 23.8 CT : 26.4 UPDRS III PD : 25.1 CT : 18.5 Week 8
PD : 0.001 HS : 0.02 STST PD : 0.01 HS : 0.01 TUG PD : 0.04 HS : 0.001 10-minutes’ Walk Test PD : 0.001 HS : POMA PD : 0.05 HS :
BBS : Week 6 > week 0 : 0.001 Week 8 > week 0 : 0.003 DGI
Week 6 > week 0 : 0.001 Week 8 > week 0 : 0.001 TUG Week 6 > week 0 : 0.001 Week 8 > week 0 : 0.001
PDQ-39
Week 6 > week 0 : 0.047 Week 8 > week 0 : 0.022
Before After p value BBS
VR : 49.6 CT : 49.8 DGI PD : 20.0 CT : 20.1 TUG PD : 20.7 CT : 18.8 PDQ-39 PD : 24.6 CT : 25.2 UPDRS-III PD : 22.5 CT : 16.9
6 Pablo C et al, 2021
Gait speed 2.8 km/h (A); 3 km/h (B) Walking endurance: 15 mins Confidence in mobility: 45% (A); 55% (B) MDS UPDRS: 29 (A); 30 (B) Hoehn and Yahr Scale 3
Both of participants were ambulatory but had difficulties in outdoor walking and complex environment
MEAN (SD) TeleWii/SIBT BBS
- Before T0: 48.63 + 6.31 / 45.61 + 7.97
Gait speed: 3.8 km/h (A); 3.8 km/h (B) Walking endurance: 45 mins
Confidence in mobility: 67% (A); 70% (B) MDS UPDRS: 26 (A); 28 (B) Hoehn and Yahr Scale: 3 (no changes)
Participants were able to walk outdoors for longer distances without any assistance No falls were sustained during training
MEAN (SD) TeleWii/SIBT BBS
After T1: 52.37 + 3.29 / 49.82 + 5.70
8 Gandolfi et al, 2017
ABC
- Before T0: 70.31 + 18.17 / 64.12 + 21.37
10 MW
Follow Up T2: 51.84 + 4.53 / 49.66 + 6.59
ABC
After T1: 79.62 + 14.16 / 72.52 + 21.20
Follow Up T2: 76.34 + 15.98 / 71.73 + 19.92
Post hoc analysis within group differences TeleWii/SIBT BBS
After T1: <0.001* / <0.001* Follow Up T2: 0.002* / <0.001*
ABC After T1: <0.001* / <0.001*
- Before T0: 1.59 + 0.49 / 1.46 + 0.42
DGI
- Before T0: 20.39 + 2.56 / 19.34 + 2.49 Falls
- Before T0: 0.58 + 1.44 / 1.84 + 5.30
PDQ-8
- Before T0: 30.72 + 15.54 / 30.53 + 16.04
10-MW
After T1: 1.62 + 0.43 / 1.60 + 0.44 - Follow Up T2: 1.57 + 0.42 / 1.52 + 0.37
DGI
- After T1: 21.24 + 2.56 / 21.18 + 2.15 Follow Up T2: 21.32 + 2.81 / 21.05 + 2.54
Falls
After T1: 0.38 + 1.33 / 0.61 + 1.81 - Follow Up T2: 0.29 + 0.94 / 0.81 + 3.31
PDQ-8
After T1: 24.16 + 14.78 / 24.21 + 15.85 - Follow Up T2: 25,82 + 14.89 / 23.91 + 13.20
LCD/2D Cohen U3 Interest : 0.5 Effort : 0.5
- Follow Up T2: <0.001* / <0.001*
10 MW
- After T1: n.s / 0.035* Follow Up T2: n.s / n.s
DGI
After T1: 0.005* / <0.001* Follow Up T2: 0.008* / <0.001*
Falls
After T1: n.s / n.s Follow Up T2: 0.034* / n.s
PDQ-8
After T1: <0.001* / 0.016* - Follow Up T2: 0.01* / 0.006*
8 Cikaljo and Peterlin Potisk, 2019 -
Perceived competence : 0.8 Pressure : 0.3
VR/3D Cohen U3 Interest : 0.5 Effort : 0.8 Perceived competence : 0.9 Pressure : 0.5
Mac Skilling p Interest : 0.995 Effort : 0.418 Perceived competence : 0.037* Pressure : 0.422
Appendix 4.
Risk of bias assessment with Cochrane Risk-Of-Bias tool for randomized trials
Cochrane Risk Of Bias Tool for Randomized Trials
Studies
Randomization
Concealed Allocation
Blinding of Participants and Personnel
Incomplete Outcome Data
Blinding of Outcome Assessment
Selective Reporting Overall Quality of Studies
Yuan et al, 2020 + + + + + + Good Cikaljo and Peterlin Potist, 2019 + + + + + + Good Song et al, 2018 + + + + + + Good Gandolfi et al, 2017 + + + + + + Good Yang W. et al, 2016 + + + + + + Good
Note: “+”: low risk of bias, “ “: high risk of bias, “?”: unclear risk
Good quality: All criteria met (i.e. low for each domain)
Using the Cochrane ROB tool, it is possible for a criterion to be met even when the element was technically not part of the m ethod. For instance, a judgment that knowledge of the allocated Interventions was adequately prevented can be made even if the study was not blinded, if EPC team members judge that the outcome and the outcome measurement are not likely to be influenced by lack of blinding.
Fair quality: One criterion not met (i.e. high risk of bias for one domain) or two criteria unclear, and the assessment that this was unlikely to have biased the outcome, and there is no known important limitation that could invalidate the results
Poor quality: One criterion not met (i.e. high risk of bias for one domain) or two criteria unclear, and the assessment that this was likely to have biased the outcome, and there are important limitations that could invalidate the results
Appendix 5. Risk of bias assessment with Cochrane Risk-Of-Bias In Non-randomized Studies of Interventions
Cochrane Risk Of Bias In Non randomized Studies of Interventions Tool
Studies
Confounding Factor Participants Selection
Classification of Intervention
Deviation from Intended Intervention
Missing Data Outcome Measurements Selection of Result Overall Quality of Studies
Pablo C. et al, 2021 + + + + + + + Good Cikaljo et al, 2021 + + + + + + + Good Esculier et al, 2012 + + + + + + + Good
Note: “+”: low risk of bias, “ “: high risk of bias, “?”: unclear risk
Good quality: All criteria met (i.e. low for each domain)
Using the Cochrane ROB tool, it is possible for a criterion to be met even when the element was technically not part of the m ethod. For instance, a judgment that knowledge of the allocated Interventions was adequately prevented can be made even if the study was not blinded, if EPC team members judge that the outcome and the outcome measurement are not likely to be influenced by lack of blinding.
Fair quality: One criterion not met (i.e. high risk of bias for one domain) or two criteria unclear, and the assessment that this was unlikely to have biased the outcome, and there is no known important limitation that could invalidate the results
Poor quality: One criterion not met (i.e. high risk of bias for one domain) or two criteria unclear, and the assessment that this was likely to have biased the outcome, and there are important limitations that could invalidate the results