
22 minute read
Highlights - 51st Annual Scientific Meeting
from Gamma Gazette Winter Edition 2021 by The Australian and New Zealand Society of Nuclear Medicine
by ANZSNM
st 51

ANNUAL SCIENTIFIC MEETING HIGHLIGHTS


The 51st Annual Scientific Meeting of the ANZSNM was the Society’s first “live and local” event, with virtual presentations by guest speakers from Australia, New Zealand and around the world projected simultaneously to hubs in Auckland, Sydney, Geelong, Adelaide and Perth. It was a mammoth undertaking and perhaps a little over ambitious? But in the end it was a great success, with a record number of live and virtual attendees, more international guest speakers than ever before and an interactive platform where delegates could communicate directly with the speakers during and after the talks, view their favourite session again and catch up on sessions that they had missed.

The theme of our conference was Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine. This provided us with the potential to include a broad range of presentations covering clinical aspects of PET and nuclear medicine as well as therapy, preclinical imaging and research, teaching and impact of COVID19 to name just a few. We were honoured to have presentations by Dr Fabian Kiessling - RWTH Aachen University; Dr Rudi Dierckx - University Medical Center Groningen; Dr Fabien Hyafil Bichat Hospital - Paris; Dr Pek Lan Khong - The University of Hong Kong; Dr Arthur Braat - University Medical Centre, Utrecht; Dr Hossein Jadvar - University of Southern California; Dr Patrick Veit-Haibach - Joint Department Medical Imaging, Toronto; Dr. Tim van de Wyngaert - Antwerp University Hospital; Dr Alan Packard - Boston Children's Hospital/Harvard Medical School; Dr John Buscombe British - Nuclear Medicine Society; Dr Jun Hatazawa - Osaka, Japan; Dr Michael Van Dam - University of California; Dr Carlo Romano - Policlinico di Monza Healthcare Group and the Villa Maria Healthcare Group, Italy; Dr Alberto Signore and Dr Chiara Lauri - University of Rome; Dr Abass Alavi - University of Pennsylvania; Dr Elena Zamagni Bologna - University School of Medicine; Dr Phillip Kuo - University of Arizona, and Dr Irene Buvant - Institut Curie, France.
The Pioneer Lecture was provided by Dr Andrew McLauglin - Burwood Nuclear Medicine and the Lowenthal Lecture by Dr Darin O’keefe - Christchurch Hospital, New Zealand.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
As well as this we had a full complement of high quality local speakers including; Dr Kate Moodie, Dr Bill Macdonald, Dr Sherene Loi and Dr Hillary Martin for the interactive breast cancer expert panel discussion, Dr Judith Trotman, Dr Nathan Better, Dr Richard Gauci, Dr Michael Mond, Dr Grace Kong, Dr Chris Rowe, Dr Dale Bailey and Dr Kathy Willowson and concurrent sessions jam-packed with submitted abstracts and award presentations.
The semi-virtual format allowed us to have a more intimate, relaxed gala dinner on the Saturday evening with colleagues and friends within our state. Dinners were held at the Rockford in Adelaide, Rydges Geelong, Germone Restaurant in Auckland and Little Way in Perth.
We would like to particularly thank Daniel Badger and the Council along with Rachael Rogers from Event Studio who helped to make this event such a success. We also want to thank and acknowledge the important contribution of the branch representatives in each state, the many volunteers at each hub, the chairpeople and moderators without whom this ambitious project would not have been possible.
See you all in Brisbane in 2022!
Tracey Muir, Liesl Celliers, Stephanie O'Donnell and Andrew Cluff
2021 ASM Convenors
Take a peek at what you can expect by visiting our YouTube channel or clicking on the screen below.

https://https://bit.ly/2022ASMVideo
The virtual platform allowed delegates from all parts of
the world to attend the event
remotely, access all presenta-
tions, live Q&A sessions, network
with peers and engage with
industry partners.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine









SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine

Live Q&A with Prof John Buscombe - Moderated by Prof Dale Bailey

Live Q&A with Prof Fabian Kiessling - Moderated by Dr Giancarlo Pascali
Live Q&A sessions were held after most presentations. Delegates had the chance to submit their questions on the virtual chat and had the presenters answer them and provide their views on hot topics.

Live Q&A Session ARTNet with Prof Michael Hofman, and A/Prof Louise Emmett - Moderated by A/Prof Roslyn Francis Live Q&A with Prof Michael van Dam - Moderated by Dr Giancarlo Pascali


Live Q&A with Dr Patrick Veit-Haibach - Moderated by Dr Geoffrey Schembri

Live Q&A with Prof Pek Lan Khong - Moderated by A/Prof Eddie Lau

Live Q&A Physics Symposium with Prof Steven Meikle, Dr Irene Buvat, Dr Chong Chew, Mansour Alqahtani and Benjamin Crouch - Moderated by Dr Kevin Hickson

Telix Pre-Conference Symposium Live Q & A with A/Prof Nat Lenzo, Dr Hossein Jadvar and Dr Kathy Willowson - Moderated by Dr Danielle Meyrick
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine

Live Radiopharmacy Symposium Q&A with Dr Laurence Morandeau, Prof Christopher Rowe and Dr Stephen Taylor Live Keynote Q&A with Dr Fabien Hyafil - Moderated by Dr Abdul Ihdayhid



Live Cardiology and Vascular Q&A with Dr Barry Elison and A/Prof Nathan Better - Moderated by Prof Dale Bailey Live Keynote Q&A with Prof Phillip Kuo - Moderated by Prof Christopher Rowe

Live National Imaging Facility Q&A with Prof Graham Galloway, Dr Giancarlo Pascali and Dr Tien Pahm


Live event sites were a success and a hub for our delegates to get together in person, see each other and network after months of non-face-to-face events. We acknowledge Siemens for their sponsorship of the National Network dinner events.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine




t was great to be around everyone and have the community feeling. It was the BEST! So fantastic to talk and gather with colleagues!





SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Click here for more photos








SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Ingrid Burvenich
Shimazdu Award Winner
SHIMAZDU AWARD
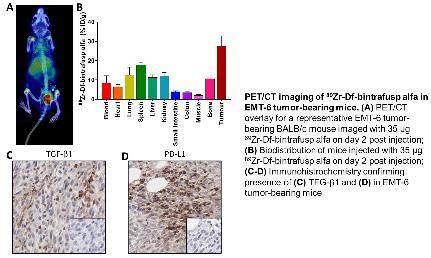
IN VITRO AND IN VIVO CHARACTERIZATION OF 89ZR-DF-RADIOLABELED BISPECIFIC ANTI-PD-L1/TGF-βRII FUSION PROTEIN BINTRAFUSP ALFA
By I Burvenich1,2, Y Goh1, N Guo1, H Gan1,2, A Rigopoulos1,2, D Cao1,2, Z Liu1,2, U Ackermann2,3,4 , C Wichmann1,2, A McDonald1,2, N Huynh1, G O'Keefe3,4, S Gong3,5, F Scott1,2, L Li6, W Geng6, A Zutshi6, Y Lan6, A Scott1,2,3,4,5
1Olivia Newton-John Cancer Research Institute, Melbourne, Australia, 2School of Cancer Medicine, La Trobe University, Melbourne, Australia, 3Department of Molecular Imaging and Therapy, Austin Health, Melbourne, Australia, 4Department of Medicine, University of Melbourne, Melbourne, Australia, 5School of Engineering and Mathematical Sciences, La Trobe University, Melbourne, Australia, 6EMD Serono Research & Development Institute, Billerica, USA
BACKGROUND: Bintrafusp alfa (M7824) is a next-generation type of PD-L1 targeting molecule allowing simultaneous targeting of
PD-L1 and trapping of transforming growth factor beta (TGF-ß).
AIMS: In preparation of a clinical bioimaging trial, this study aimed to generate 89Zr-labeled bintrafusp alfa investigational drug product and controls, and to perform the in vitro and in vivo characterization of 89Zr-Df-bintrafusp alfa and 89Zr-Df-control radioconjugates.
METHODS: Bintrafusp alfa (antiPD-L1 human IgG1 antibody fused to TGF-ß receptor II (TGF-ßRII)), avelumab (anti-PD-L1 human IgG1 control antibody), isotype control (mutated inactive anti-PD-L1 IgG1 control antibody), and trap control (mutated inactive anti-PD-L1 human IgG1 fused to active TGF-ßRII) were chelated with p-isothiocyanatobenzyl-desferrioxamine (Df). In vivo biodistribution studies were performed at different dose levels to identify tissue distribution and 89Zr-Df-bintrafusp alfa tumor uptake in a PD-L1/TGF-ß positive murine breast cancer model (EMT-6). The presence of PD-L1 and TGF-ß targets in different tissues was confirmed via immunohistochemistry.
RESULTS: Conditions for the Df-conjugation and 89Zr-radiolabeling of bintrafusp alfa and controls were established. PD-L1 binding and trapping of TGF-ß ligands of constructs was maintained after radiolabelling. A combined PET imaging/biodistribution study clearly showed the effect of protein dose on the amount of 89Zr-labeled bintrafusp alfa that can reach the tumor: by increasing the amount of unlabeled protein, uptake in lung and spleen can be reduced, and as a result, the blood pool activity as well as the tumor uptake of 89Zr-labeled bintrafusp alfa was increased. Results of PET/CT imaging of 35ßg 89Zr-labeled bintrafusp alfa are shown in the figure below.
CONCLUSION: Our results demonstrate that 89Zr-labeled bintrafusp alfa is now suitable for use in the bioimaging clinical trial study of 89Zr-bintrafusp alfa PET scans in patients with advanced or metastatic NSCLC receiving M7824 alone or in combination with chemotherapy.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Brylee Thomson
Curium Award Winner
CURIUM AWARD
16 VS 8 BIN EVALUATION OF LEFT VENTRICLE EJECTION FRACTION IN MYOCARDIAL PERFUSION IMAGING
By Thomson B1, NG W1, Pathmaraj K1,2, Lee ST1,2,3, Rowe, C1,4, Boktor R1,2,3
1Department of Molecular Imaging and Therapy, Austin Health; 2Olivia Newton-John Cancer Research Institute, Austin Health; 3School of Cancer Medicine, La Trobe University, 4Department of Medicine, The University of Melbourne
BACKGROUND: Myocardial Perfusion Imaging (MPI) is a reliable diagnostic tool used for assessing ischemic heart disease. Accurate left ventricular ejection fraction is important for optimal management of patients with cardiac disease, which is routinely performed during myocardial perfusion imaging. A previous internal study in our institution comparing the left ventricular ejection fraction (LVEF) on MPI using 8 bin data compared to gated blood pool scans (GBPS) showed a 4% underestimation of LVEF in MPI (20 seconds per step for 60 steps). Hence, we routinely added 4% to the LVEF generated from MPI. The new generation GE Discovery SPECT scanners offer advances in gamma camera crystal sensitivity and reconstruction parameters, which initiated a review of this practice. AIMS: To assess the difference and accuracy of LVEF calculation using 16 versus 8 bin gated data when performing MPI SPECT scans and to determine if the routine addition of 4% to the LVEF could be avoided.
METHODS: Using the GE Discovery DR, a new protocol involving MPI acquisition using 16 bins was implemented, which increased the acquisition time by 5 seconds per step and overall scanning time by 5 minutes. The data was converted to 8 bins by combining every two consecutive bins into one. Both sets of data were processed using standard reconstruction algorithms by a single technologist. LVEF was recorded and compared by two experienced nuclear medicine physicians.
RESULTS: 105 patients, with 165 datasets were evaluated. Matched pair t-test shows a statistically significant difference (P<0.0001) between the 8 bin and 16 bin acquisition. The 16 bin acquisition protocol had an average 4% greater LVEF compared to the 8 bin, as shown in the table below. The 16 bin acquisition improves temporal sampling, which coupled with resolution recovery, more accurately computes the LVEF compared to 8 bin gate acquisition.
CONCLUSION: The results demonstrate that a more accurate LVEF is generated by contemporary SPECT/ CT scanners using 16 bin gated acquisition. This has obviated the need to routinely add 4% to the MPI generated LVEF. This project has resulted in a change of practice for MPI processing and reporting in our department and has restored the confidence of our referring doctors in our MPI generated LVEF. combination with chemotherapy.
All Number of Scans 16 bins Range of EF(%) 16 bins Average EF(%) 8 bins Range EF(%) 8 bins Average EF(%)
Average difference in EF(%) 165 23-96 61 26-94 57 4.4
Stress 105 26-96 64 34-94 59 4.2
Rest 60 23-85 57 26-84 53 4.6
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Evyn Arnfield
AANMS Award Winner
AANMS AWARD
CLINICAL INSIGNIFICANCE OF [18F]PSMA-1007 AVID NONSPECIFIC BONE LESIONS: A RETROSPECTIVE EVALUATION
Evyn Arnfield
Royal Brisbane and Women's Hospital, Queensland
PURPOSE:[18F]PSMA-1007 offers advantages of low urinary tracer excretion and theoretical improved spatial resolution for imaging prostate cancer. However, non-specific bone lesions (NSBLs), defined as mild to moderate focal bone uptake without a typical morphological correlate on CT, are a common finding on [188F] PSMA-1007 PET/CT. The purpose of this study was to investigate the clinical outcomes of patients with [18F] PSMA-1007 avid NSBLs, to determine whether patients with NSBLs represent a higher risk clinical cohort, and to determine whether SUVmax can be used as a classifier of bone metastasis.
METHODS: A retrospective audit of 214 men with prostate cancer was performed to investigate the clinical outcomes of [18F]PSMA-1007 avid NSBLs according to defined criteria. We also compared the serum PSA, Gleason score and uptake time of patients with [18F]PSMA-1007 avid NSBLs to patients without [18F]PSMA1007 avid bone lesions. Finally, we analysed an SUVmax threshold to identify bone metastases using ROC curve analysis.
RESULTS: Ninety-four of 214 patients (43.9%) demonstrated at least one NSBL. No [18F]PSMA-1007 avid NSBLs met criteria for a likely malignant or definitely malignant lesion after a median 15.8-month follow-up interval (11.9% definitely benign, 50.3% likely benign, and 37.7% equivocal). There were no statistically significant differences in serum PSA, Gleason score and uptake time between patients with [18F]PSMA-1007 avid NSBLs and those without [18F]PSMA-1007 avid bone lesions. All NSBLs with adequate follow-up had SUVmax ≤11.1. The value of the highest SUVmax distinguished between NSBLs and definite prostate cancer bone metastases, whereby an SUVmax threshold of ≥7.2 maximised the Youden’s index. the absence of definite metastatic disease elsewhere, it is appropriate to classify those with SUVmax <7.2 as likely benign. NSBLs with SUVmax 7.2-11.1 may be classified as equivocal or metastatic, with patient clinical risk factors, scan appearance, and potential management implications used to guide interpretation.
CONCLUSION:[18F]PSMA-1007 avid NSBLs rarely represent prostate cancer bone metastases. When identified in
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
GMS POSTER AWARD
NO THEATRE TIME REQUIRED – THE USE OF LYMPHOSCINTIGRAPHY WITH SPECT/CT AND ULTRASOUND TO GUIDE PERCUTANEOUS FNA OF THE SENTINEL NODE IN A MELANOMA PATIENT
Danielle Nuske
GMS Poster Award Winner
In the photo, Danielle visiting Madame Curie's laboratory in Paris' Museum in 2018 Danielle Nuske1 & C. Ghee Chew1
1Department of Nuclear Medicine, Radiology SA, Calvary North Adelaide Hospital, South Australia
BACKGROUND: A 75-year-old female patient with right upper arm melanoma was referred for lymphoscintigraphy and ultrasound-guided fine needle aspiration (FNA) of the sentinel node.
PROCEDURE: 99mTc-NanoScan (54MBq / 0.4mL) was administered intradermally at the melanoma site. Before acquiring planar images the patient performed upper body exercises. The surface locations of the visualised axillary sentinel node were marked anteriorly and laterally. Metallic ECG buttons were placed at the marks prior to SPECT/CT. Ultrasound then guided the percutaneous sentinel node FNA biopsy. The aspirate slides were examined for radioactivity using a hand-held radiation monitor. Cytopathological analysis followed.
FINDINGS: The planar images showed prompt radiotracer uptake by a single right axillary lymph node. SPECT/CT localised the node depth at 1.5cm. Metallic landmarks on CT assisted ultrasound evaluation which guided nodal biopsy. Radioactivity of the aspirate slides noted at >10X background indicated radioactive sentinel nodal sampling. Lymphocytes in cytopathological analysis further confirmed lymph node sampling. No malignant cells were found.
OUTCOME: The patient avoided a more invasive surgical sentinel lymph node biopsy (SLNB). Subsequent management remained unchanged for a negative sentinel node biopsy.
DISCUSSION: While SLNB with pre-operative lymphoscintigraphy and blue dye is standard in earlystage melanoma, it has potential complications and contraindications. Ultrasound-guided percutaneous FNA of the sentinel node following lymphoscintigraphy is a viable, minimally invasive alternative which has been reported in the literature. The success of both techniques depends on prompt and accurate sentinel node identification. To improve biopsy yield our protocol includes: 1. routine post injection exercise to expedite and enhance nodal identification; 2. metallic button placement as CT landmarks; 3. radioactivity evaluation with a monitor to confirm sentinel nodal sampling.
CONCLUSION: Percutaneous FNA biopsy of sentinel node with lymphoscintigraphy SPECT/CT can be confidently performed and is less invasive than nodal resection.
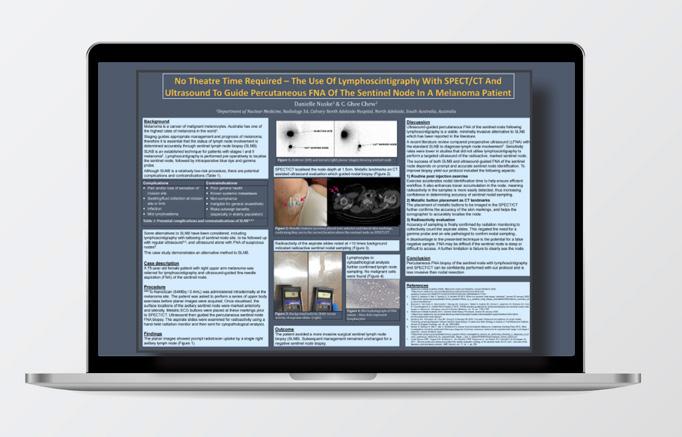
CLICK TO VIEW THE POSTER
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Candice Nish
Radpharm Award Winner
RADPHARM AWARD
THE BENEFITS OF STRESS: ACETAZOLAMIDE VERSUS EXERCISE IN PHACE SYNDROME
Candice Nish
Royal Brisbane and Women's Hospital, Queensland
CASE DESCRIPTION:A 13-year-old male patient with a complex history of left trigeminal nerve neuralgia, secondary to Posterior fossa brain malformations, Haemangioma, Arterial anomalies, Coarctation of aorta and Eye abnormalities (PHACE) syndrome, was investigated using cerebral perfusion SPECT/CT imaging.
PROCEDURES PERFORMED: A 99mTechnetium Ethylcysteniate Dimer (99mTc-ECD) baseline and 99mTcECD Acetazolamide challenge were acquired separately under normal parameters followed by a Single Photon Emission Computed Tomography (SPECT/CT). A 99mTc-ECD Acetazolamide exercise stress, using a treadmill, was also performed using the Bruce Protocol for approximately 8 minutes. At this point exercise induced symptoms became present and the patient was injected with 99mTc-ECD. The exercise stress was discontinued 1 minute later. A SPECT/ CT was performed for approximately 45 minutes to assess the vascular distribution of the radiotracer. General anaesthetic was used for all imaging as requested.
FINDINGS: Comparing the 99mTcECD exercise stress to the 99mTc-ECD baseline, a 10%-20% exercise induced decrease in perfusion to the right cerebral hemisphere was shown.
OUTCOME:Due to the results indicated by the nuclear medicine scan, the patient went on to have surgery which lead to significant improvement in the patient’s trigeminal neuralgia and quality of life. DISCUSSION:This case study indicates how, in nuclear medicine, functional imaging and the adaptability of scanning techniques to a patient’s needs, can aid in the diagnosis and treatment pathway of patients.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Nicola Evans
Nuclear Medicine Undergraduate Student Award Winner
NUCLEAR MEDICINE UNDERGRADUATE STUDENT AWARD
EFFECTS OF EXENATIDE ONCE WEEKLY ON INTRAGASTRIC DISTRIBUTION OF SOLIDS AND LIQUIDS AND PERCEPTIONS OF APPETITE, IN HEALTHY OVERWEIGHT SUBJECTS
Nicola Evans
University of South Australia
BACKGROUND: Obesity and type 2 diabetes are associated with increased morbidity and mortality; however, weight loss decreases complications. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) induce weight loss, although the mechanisms are poorly understood. Postprandial fullness is directly related to distal meal retention, and although the long-acting GLP-1RA, exenatide once weekly (QW), slows gastric emptying (GE), its effects on intragastric meal distribution and appetite sensations have not previously been evaluated.
AIM: To evaluate the effects of exenatide QW, on solid and liquid intragastric distribution and perceptions of appetite, in healthy overweight volunteers.
METHODS: Thirty-two overweight participants were randomised to receive either exenatide QW (6M, 10F; age: 59.9±0.9 years; BMI: 29.6±0.6kg/m 2 ) or placebo (6M, 10F; age: 60.6±1.2 years; BMI: 29.5±1.0kg/m 2 ) for eight weeks. At baseline and post-intervention, body weight was recorded, and GE and perceptions of appetite were measured for 120 minutes after a solid/ liquid meal, comprising 100g minced beef (radiolabelled with 20MBq 99m Tc-sulphur colloid) and 150mL 10% glucose (radiolabelled with 7MBq 67 Ga-EDTA). Regions-of-interest were drawn to generate intragastric meal distribution curves of the total, proximal and distal regions. Data are mean values ± the standard error of the mean, with P<0.05 considered statistically significant.
RESULTS: Exenatide QW induced a mean weight loss of 2.1±0.5kg (P=0.001). Exenatide QW also delayed total stomach solid (P=0.04) and liquid (P=0.02) GE, compared to placebo, with no significant changes to intragastric distribution. Post-intervention, there were no significant changes to perceptions of fullness (P=0.32), hunger (P=0.32), or desire to eat (P=0.54). Weight loss induced by exenatide QW appears unrelated to intragastric distribution, indicating that other mechanisms are involved.
CONCLUSION: In healthy overweight participants, eight weeks of treatment with exenatide QW slows solid and liquid GE with no significant changes in intragastric distribution and no effect on sensations of appetite, despite significant weight loss.
SPECIAL FEATURE 51st Annual Scientific Meeting Highlights: Key Collaborations, Key Impacts: Unlocking the Potential of Nuclear Medicine
Society Recognition
We congratulate all of the award winners on their excellence and success.
There are also two plenary lectures given by individuals that the Society wishes to honour by invitation to present — the Pioneer Lecture and the Lowenthal Lecture.
The Pioneer Lecture is given to an individual who has made a considerable contribution to the Society of Nuclear Medicine in Australia or New Zealand.
The Lowenthal Lecture, is awarded to an individual who has made a significant contribution over the years to the local nuclear medicine community. This year’s lecturers did not disappoint.
The two honorees for 2021 are well known to the ANZSNM community and need minimal introduction. Their presentations can be found on the ANZSNM site with the links below.
Dr Andrew McLaughlin
PIONEER LECTURER
CLICK TO WATCH
Dr Darin O'Keeffe
LOWENTHAL LECTURER
CLICK TO WATCH






Ashleigh Hull
Research Award recipient

PRE-CLINICAL STUDIES OF MUC1 TARGETED ALPHA THERAPY FOR PANCREATIC CANCER
Ashleigh Hull 1,2*, Yanrui Li 1, Dylan Bartholomeusz 2,3, William Hsieh 1,2 and Eva Bezak 1,4
1Cancer Research Institute and Allied Health and Human Performance Academic Unit, University of South Australia 2Department of PET, Nuclear Medicine & Bone Densitometry, Royal Adelaide Hospital, South Australia Medical Imaging 3Adelaide Medical School, The University of Adelaide, South Australia 4School of Physical Sciences, The University of Adelaide, South Australia
Pancreatic ductal adenocarcinoma (PDAC) is a highly aggressive malignancy with an unmet clinical demand. Despite advances in conventional therapies, surgery remains the only curative treatment option for PDAC, however its application is restricted to patients with locally advanced disease only (10 – 20% of cases). Several anatomical and physiological factors attribute to a lack of curative treatments for PDAC including the unfavourable location of the pancreatic vasculature which complicates surgical resections; the cellular heterogeneity of the pancreas which limits the effectiveness of a single treatment type; the stromal barrier that restricts the entry of intravenous substances including chemotherapy; and the hypoxic nature of PDAC which reduces the efficacy of external beam radiation therapy. Targeted alpha therapy (TAT) has ideal radiobiological properties to overcome these barriers however there have been few applications of TAT to PDAC. The aim of this project is to investigate the safety and feasibility of TAT for PDAC by developing and testing a novel alpha-immunoconjugate (AIC), 225Actinium-DOTA-C595. This AIC is designed to target cancer-specific mucin 1 epitopes (MUC1-CE) overexpressed on PDAC. A series of controlled in vitro experiments will be performed to assess the pharmacokinetics and cytotoxicity of 225Actinium-DOTA-C595 in MUC1-CE positive and negative PDAC cells. Complementary diagnostic and therapeutic radioimmunoconjugates, 64Copper-DOTA-C595, 99mTechnetium-DOTA-C595 and 177Lutetium-DOTA-C595, will also be prepared and tested for comparison purposes and for future use in biodistribution/beta therapy studies.







