
4 minute read
Strength In Numbers
Strength in Numbers Join the movement to gather data that will help hospitals improve performance, better hold commercial payers accountable
By Travis Gentry, CEO, and Kari Kemper, Vice President of Client Services, Hyve Health
Editor’s Note: The AHA Vitality Index™ is a program of the American Hospital Association. It is not to be confused with the Arkansas Hospital Association’s data program, through which we support member hospitals by providing access to timely and accurate data and statistics. When used together, the information gleaned from the two programs can supercharge your perspective on your hospital's priorities.
Now more than ever, hospitals and health systems need operational and financial data they can trust and better understand how they are performing compared to the rest of the field. That’s where AHA Vitality Index™, which allows hospitals to anonymously benchmark their operational performance, can help.
With just a few clicks, hospitals can uncover how often their organization's payment claims are denied, determine if those denial rates vary by payer service line, and compare their organization’s metrics to other deidentified providers and peer groups. A hospital can determine how to address an issue by understanding the cause. Is it an internal operational issue impacting just their hospital? Is it a payer-specific issue in which the hospital is being treated unfairly versus its peers?
Scan this QR Code to read Addressing Commercial Health Plan Challenges to Ensure Fair Coverage for Patients and Providers
Scan this QR Code to read Commercial Health Plans’ Policies Compromise Patient Safety and Raise Costs
DELAYING AND DENYING COVERAGE
Part of a high-functioning revenue cycle is the ability to get appropriately reimbursed for the care provided. In recent years, it has become apparent that certain commercial health insurer practices are delaying and denying coverage for medically necessary care.
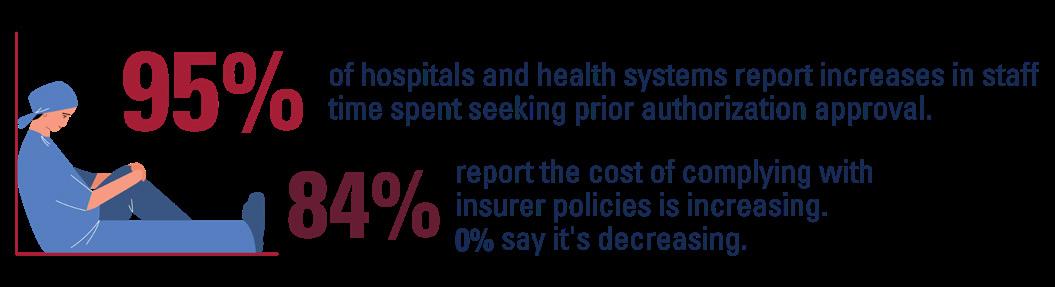
This year, the American Hospital Association (AHA) released two reports on these burdensome practices that have garnered significant media attention by showing how some commercial health insurers, including Medicare Advantage plans, can cause dangerous delays in care, place undue burden on the health care workforce, and add billions of dollars in unnecessary costs to the health care system. These include things like inappropriate and excessive use of prior authorization, mid-year changes in coverage that restrict where patients can access care (i.e., site of service and pharmaceutical white bagging policies), and unwarranted requests for additional medical records and other tactics to delay payment. Indeed, hospitals report a significant increase in accounts receivables as they await payment for medically necessary, covered care.
Government officials have taken note. The Office of Inspector General for the U.S. Department of Health and Human Services recently found that a large portion of denied prior authorization requests and claims for payment for care provided to Medicare Advantage enrollees should have been approved. Another report from the U.S. Surgeon General citing concerns about health care worker burnout pointed to some of the administrative burdens placed on providers, such as prior authorizations, as one of the major drivers of provider fatigue. Recently, the state of Georgia issued a substantial fine against a large payer for several conduct issues.
HERE, THE VITALITY INDEX CAN HELP TOO
Using data in the Vitality Index, hospitals and health systems can better prepare themselves for discussions with payers about appropriate performance on various revenue cycle metrics. For example, hospitals will be better equipped to discuss standards regarding the timeliness of payments, acceptable rates of accounts receivables, and more. These new data points will take the conversation from what historically has been anecdotal and provide empirical

To learn more, contact Mark Brand, American Hospital Association Licensing Account Manager at mbrand@aha.org or 312-893-6810 or scan the QR code to fill out the “Request Demo” form online.
evidence providers can use to prove that negative payer behaviors are occurring.
In addition, with a critical mass of hospitals participating, the Vitality Index may offer a statistically valid sample of payer performance data at the state and national levels to help inform policymakers and government oversight bodies.
State hospital associations are always close partners of the AHA and its work. We see the ability to take the data and the insights gained as a resource to the state hospital associations and their members as they engage with state lawmakers and policy leaders to shed light on these burdensome commercial payer practices.
How can hospitals and health systems get involved? We have created a process designed to make it very easy to participate. We are very sensitive to the fact that hospitals have many operational demands, often juggling multiple IT projects. We do not ask participants for custom extracts, which would take additional time and resources to create. Instead, we ask participants to submit the raw data for three years of historical claims and remits. Data transmission is via The PHI Scrubber™, a utility software solution that deidentifies specific elements in health care claim and remit files, ensuring that all Protected Health Information is removed before leaving the hospital environment, maintaining compliancy with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Safe Harbor Rule. The data is normalized across all participating deidentified hospitals, allowing for meaningful and actionable analysis.

Take a Closer Look
RECOVER. EVERY. DOLLAR.
Gaps in reimbursement strategies are causing you to lose millions of dollars each year. Staffing issues, new processes and government regulations all contribute to reimbursement dollars falling through the cracks, going uncollected.
In less than 3 years, HORNE has recovered more than $33 million in unreimbursed Medicare funds for 33 hospitals.
HORNE experts understand both Medicare reimbursement and data in the healthcare industry. We use proprietary analytic tools to resolve discrepancies, identify missed value and, most importantly, find those dollars.
The dollars are there, let us take a closer look. We can help.
HORNE.com/medicare-reimbursement









