4 minute read
Improving cultural competency and safety in primary health care
Findings from Aboriginal Community Consultations in the Midwest, Perth, South West, and Goldfields regions of Western Australia
Breaking down barriers to care for Aboriginal people in Western Australia
Advertisement
Improving the cultural competence of primary health care services might not be the first thing that springs to mind when trying to tackle the significant disparity in health care access and outcomes faced by the almost 80,000 people in Western Australia (WA) who identify as Aboriginal. But with the gap in life expectancy for Aboriginal men and women continuing to exist at 15.1 and 13.5 years lower than non-Indigenous Western Australians1, at WA Primary Health Alliance, as the operator of WA’s three Primary Health Networks, we knew something fundamental had to change. This dire situation is also reflected at a national level, where despite the National Closing the Gap Commitments, the 2019 National Aboriginal and Torres Strait Islander Health Survey showed an increase in the percentage of Aboriginal people with chronic conditions and in those who were overweight; showed no improvement in the percentage of people with psychological distress; and showed lower rates of access to health care services.2
WA Primary Health Alliance identified the need to develop a cultural competency framework to build on, and improve, cultural safety and access to primary health care services for Aboriginal people.

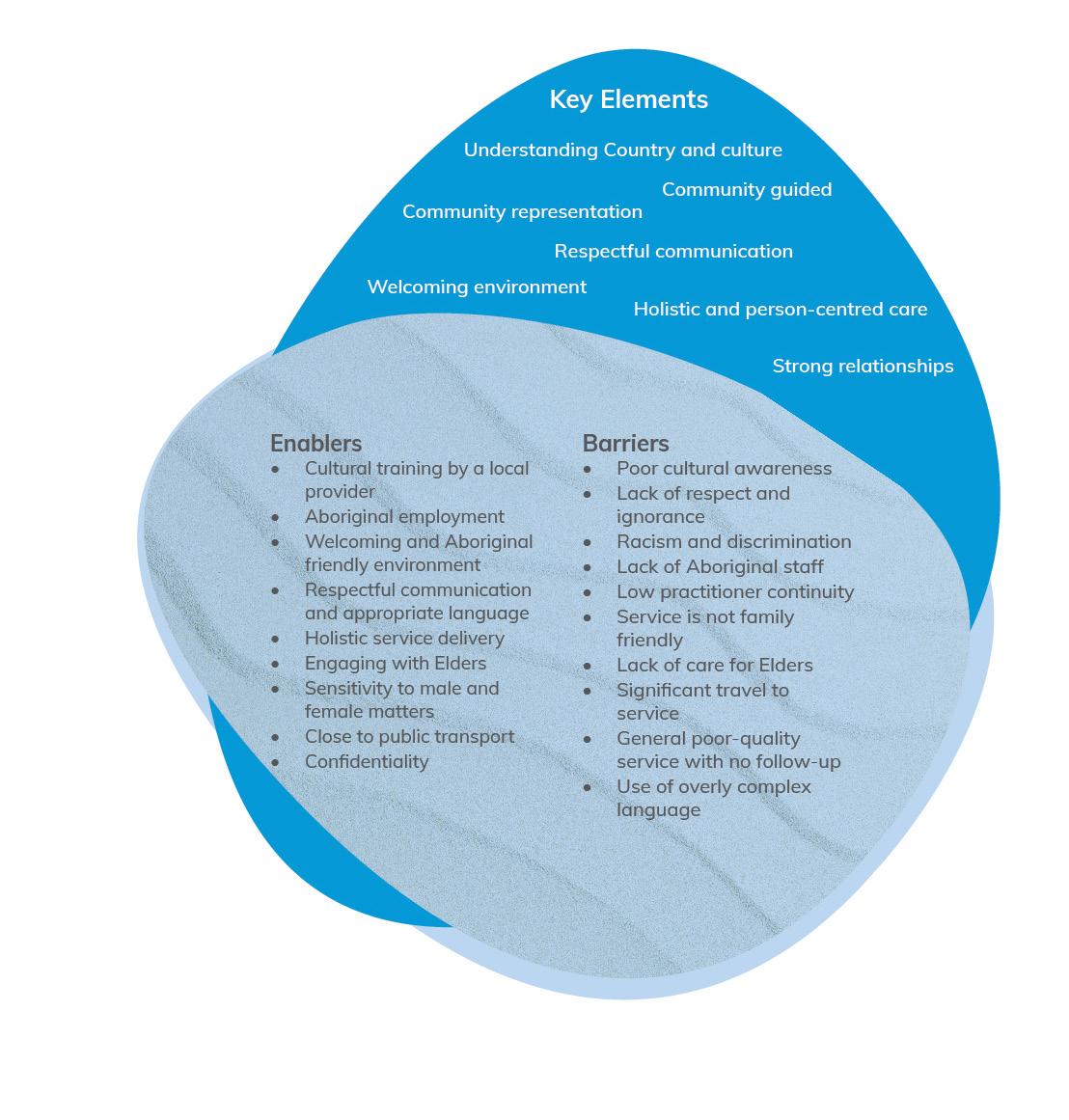
Figure 1: Feedback from community consultations on what enables a service to be culturally safe on, and improve, cultural safety and access to primary health care services for Aboriginal people.
Acknowledging that the Aboriginal Community Controlled Health Sector was already advanced in providing culturally safe care, we wanted to learn from its best practice and understand how to apply those strengths to improve the way other primary health care services we commission are delivered.
Safe services are usually developed and implemented in partnership with local Aboriginal health teams and organisations, Elders and communities and are delivered by culturally competent staff members.
We recognised the importance of hearing directly from Aboriginal people and communities on what makes a service culturally safe and accessible. We engaged Aboriginal consultant, Kambarang Services, to facilitate four participatory group consultations in the Midwest, Perth, South West, and Goldfields regions of WA, with 120 Aboriginal community members and Elders attending.
Participants were asked to describe what enables a service to be culturally safe, what barriers prevent them from accessing a service and the key elements to explore in developing the Framework. The feedback we received was rich and highly informative.
It showed that barriers still exist that prevent Aboriginal people from accessing appropriate primary health care services. Improving cultural competency of services can be achieved by listening to, and acting on, what Aboriginal people say, and this supports them to feel culturally safe. Services that commit to cultural training; Aboriginal workforce development; holistic personcentred care; and community engagement can create welcoming environments for Aboriginal people, increasing access and meeting their cultural and health care needs.
We are using the feedback to inform the development of the Framework, which will establish clear actions and standards to improve the level of cultural competency in primary health care services and cultural safety for Aboriginal people using those services. It is important to recognise that improving cultural competency and safety cannot be achieved simply by implementing cultural training, or by any one key element, but is a journey that is built upon ongoing learning, commitment, resources and continuous quality improvement processes.
WA Primary Health Alliance is now on a learning journey towards authentic partnerships with Aboriginal communities and we will use the Framework to hold ourselves accountable to a high standard of cultural competence — to our board, staff and, most importantly, community members.
Once complete, the Framework will complement our Innovate Reconciliation Action Plan and Aboriginal Health Strategy, which further demonstrate our commitment to Aboriginal people. Due to be launched this year, the Framework will be a key part of WA Primary Health Alliance’s commitment to equity, inclusion and diversity. It will be at the heart of who we are as an organisation and the change we are striving for on behalf of our Western Australian communities most at risk of adverse health outcomes. ha
References:
1. 2016 Census: Aboriginal and/or Torres Strait Islander Peoples QuickStats
2. https://www.abs.gov.au/statistics/people/aboriginal-andtorres-strait-islander-peoples/national-aboriginal-and-torresstrait-islander-health-survey/latest-release

MARK GRIFFIN Senior Advisor Aboriginal Health, WA Primary Health Alliance (WAPHA)









