1. Introduction
People with a learning disability have worse physical and mental health than people without a learning disability and are more likely to experience a number of health conditions.
On average, males with a learning disability die 22 years younger than males from the general population, and females die 26 years younger than females from the general population (Learning Disability Mortality Review (LeDeR) 2021).
Legally, additional measures must be taken to reduce inequalities and remove barriers to access for these people (Equality Act 2010). At The Rotherham NHS Foundation Trust, we want to ensure staff:
• are referring anyone with a learning disability to the ‘Learning Disability and Autism Team’ or encouraging self-referral
• are making reasonable adjustments for them
• are equipped to deal more effectively with the particular needs of each individual
Learning disability is different for every person; this can be mild, moderate or severe and the person will require varying levels of support.
‘Valuing People’ (2001) explains that a learning disability includes the presence of:
• A significantly reduced ability to understand new or complex information, to learn new skills (impaired intelligence with an IQ below 70)
• A reduced ability to cope independently (impaired social functioning), which started before adulthood, with a lasting effect on development
Many people with a learning disability live independent lives.
Patients with a learning disability have a special indicator (flag) on the Trust Electronic Patient Record system Meditech.
Learning disability patients may need assistance with;
• Following instructions
• Understanding and processing information
• Understanding abstract concepts such as time or directions
• Phrases used in conversation without expanding on the content
If the person coming to the Trust does not live in Rotherham, they will not have a flag on their record, as that information comes from the Rotherham GP register.
Another way to find out if someone has a learning disability is by asking them if they have a Hospital Passport.




Please take time to read through the important information in someone’s Hospital Passport; information inside often saves time and avoids unnecessary negative situations. We are required by law to record, meet and share their communication needs (Accessible Information Standard, 2016).





The Hospital Passport gives important information about a person’s everyday needs and wishes. The Hospital Passport information should be completed by the person themselves, or someone who knows that person really well, ideally before they attend for their care.
This document should be regularly reviewed, as a person’s health and social needs will change over time.
This information can be used to assess whether someone’s condition has changed.
This document does not serve as consent to treatment or any other intervention. Consent must still be sought in every single context and the mental capacity of that person assessed. The passport is available on the Hub, or you can ask the Learning Disability and Autism Team or the Community Learning Disability Team. It is also included as an appendix in the Trust’s Learning Disability Policy.
The LD + A Team is made up of a Learning Disability and Autism Matron and Nursing Associates. The team is available Monday to Friday 8am – 4pm. Outside of these hours please consult the patient, their Hospital Passport and family / carers.

Email: rgh-tr.learningdisabilityandautismteam@nhs.net
Telephone: 01709 42 8371 (answerphone service available)
Nursing Associates visit autistic people and people with learning disability throughout the day and give them the help and support they need while in hospital, ensuring reasonable adjustments are made to their care pathway. The team also give support to people coming through Urgent and Emergency Care, Outpatients and planned surgery.
They can help you to support patients in the following ways:
• Facilitate open and easy access for young people and adults with learning disabilities and/or autism accessing Trust services
• Give specialist advice and support for professionals in relation to personalised care and reasonable adjustments
• Provide accessible information
• Actively assist patients with learning disabilities and/or autism and their carers when using our services
• Provide support and advice regarding best interests, consent, advocacy, mental capacity and safeguarding
• Coordinate and assist the facilitation of learning disability or autism awareness training and further education to professionals to meet the needs of young people and adults with learning disabilities and/or autism
• Ensure that the views of patients and their carers are taken into account
Do you think you would be a great advocate for autistic people?
Would you like to gain further knowledge and understanding of how to care for this patient group?
If yes - then please become a learning disability champion for your ward or department!
Contact the Learning Disability and Autism Team on ext. 8371 today
A reasonable adjustment is a change or alteration to the current care pathway that is acceptable to the person and the organisation.
We have a duty under the Equality Act 2010 to make reasonable adjustments. This means to consider things that could be reasonably changed e.g.
letting the person stay in a cubicle if it would make their stay better,
organise for them to be listed first on a surgery list if they would like this to avoid undue waiting and anxiety,
let family members stay overnight with them in the Trust,
letting the person have access to food outside of designated mealtimes.
If someone requires assistance, welcoming carers to visit at any time can be beneficial to staff, patients and carers.
Our Trust has pledged to let carers of people with learning disabilities or autism visit at any time of the day or night.
We can arrange for carers to stay in the hospital overnight if the patient and carer would like this.
A weekly parking pass is available
A weekly parking pass in available at a concessionary rate for family members or carers who are visiting someone in hospital for a period longer than 7 days. These are to be issued by a senior member of staff working on the ward who must inform the Reception Desk/Security Office by completing the Trust’s ‘Parking Concessionary Proforma’, that the patient’s stay in hospital is likely to be more than 7 days.
Free Parking Pass
Free parking is issued by a senior member of staff within the outpatient department, ward or service who must advise the Reception Desk or Security Office, by completing a Free Parking Authorisation Proforma.
Free parking will be available for:
• Patients who are required to attend frequent Outpatient clinics (3 times a month or more)
• Parents with children who are inpatients
• Cancer patients
Free parking is issued by a senior member of staff within the outpatient department, the Ward or Service who must advise the Reception Desk/Security office, by completing a Free Parking Authorisation Proforma.
Blue Badge Holders
There is an opportunity for blue badge holders, who use hospital services on a frequent basis, to be provided with a blue badge holders Trust car pass. Where this is applicable a senior member of staff from the ward/departments/service/clinic should provide the blue badge holder with a Blue Badge Car Pass Application Form.
The capacity of an autistic person or person with a learning disability to consent should be assumed in the first instance, however, if there is doubt, a Mental Capacity Assessment should be completed.
It is not acceptable or legal for a parent or carer to give consent on behalf of an adult with a learning disability.
This may not apply if the person with a learning disability does not have capacity and their family member or carer has a Lasting Power of Attorney or Court Appointed Deputy for Health and Welfare and authority to approve medical treatments. These views can be taken into consideration by the clinician when making a best interest decision.
If there is not a close relative who can support in the best interest process the individual is entitled to the services of an independent mental capacity advocate (IMCA) which staff can refer patients directly to. The referral form to Advocacy Services is available on the Hub.
The Mental Capacity Act Lead may be contacted for guidance if required to arrange this.
Always check the person’s Hospital Passport for things that could trigger a distressed reaction. This information will be found in the ‘Likes and Dislikes’ section.
Examples of what can trigger an emotional reaction in someone with a learning disability can include; noise, touch / unexpected touch, hospital bed curtains being closed (can feel claustrophobic), not being warned about / told what is going to happen in detail, not wanting pillows on a hospital bed etc.
Increased stress can heighten emotional responses.
If someone is distressed, the best thing you can do is not encroach on their personal space, ask if they need time on their own, ask if they need support from someone else or if they would like you to stay, and encourage deep breathing to refocus.
Introduce yourself; say your name, explain your role and why you are there, what is going to happen and what that will involve, you may need to break this down in great detail.
For example, Hello my name is Jenny, I am a nurse, I am here to change your continence pad, that will mean I will have to move the bedding down, remove your continence pad and give you a wash, is that okay with you? I will ask you if I need you to move or if I need to move you.
Some people will need time to process the information that you are telling them. You can say ‘Would you like me to come back in 5 minutes?’. This will give the person time to think about what they have just been told and process that information.
Use of language – Do not use over-medicalised terminology, explain in plain English what the matter is with them, what treatment will be put in place, and when they will go home.
Sometimes resources can help communication with autistic people or people with learning disabilities. Please find some resources in the back of this folder, or use the resources in your area’s ‘Communication Station’.
People use many methods to self-soothe. This can be called ‘stimming’. Stimming can be a variety of things, but not every person will do this and what each person does can vary.
‘Stimming’ can include behaviours such as rocking, swinging, ticking, clapping/flapping hands, humming, rolling eyes, grinding teeth, squinting, licking, chewing, sucking on objects, wiggling / tapping fingers, staring at objects, lining up/stacking objects, dropping things to hear their sound… the list goes on.
Stimming is a self-soothing coping mechanism and should not be stopped. Stimming can be a sign of distress, so if there is something obviously causing the distress, such as pain or loud noises, removing that may stop the stimming. If the patient is not causing disruption and is in no obvious distress, stimming is a harmless activity.
However, if someone is disrupting other patients, you may wish to find them an alternative soothing activity or another area for them to continue stimming.
• Speak to the patient and their carer (if present) to establish if they have any additional needs. If they are unaccompanied, and there is an identified need for support, you should attempt to identify a carer or relative and make contact with them as soon as possible.
• Details of the carer and contact numbers should be clearly documented in the demographics section of Meditech, but can also be found within the Hospital Passport.
• Request to see their Hospital Passport if they have it, as this may contain useful information to support decision making.
• If appropriate, fast-track autistic people or people with learning disabilities through the system. Where possible, keep their waiting time as short as you can.
• Contact the LD + A Team to make them aware of this person.
The Trust has a bespoke pathway referral system through Day Surgery, which may be appropriate for some people with a learning disability.
If the person is coming to the Trust for a planned surgery and they are not from Rotherham, they will not have a learning disability flag on their record, as our information is from the Rotherham GP register. The LD + A Team put a special indicator on Meditech, as soon as they are alerted to an out of area patient coming to the Trust, usually via a pre-operative assessment, the Day Surgery Unit, or the surgical ward.
• Pre-op assessments can be supported by the LD + A Team, or if in a pre-op assessment you identify someone has a learning disability, make the LD + A Team aware.
• The Hospital Passport is shared with the multidisciplinary team (MDT), so theatre staff, anaesthetists, consultants etc. for them to read. This helps us with our planning.
• For planned surgeries an MDT will form to discuss a bespoke plan for each individual patient.
• The plan may include how we will get clinical checks undertaken; home visits can be undertaken to get information.
The MDT plan all aspects of the admission; including all reasonable adjustments needed for them to receive their care.
This may include:
• If they need to be first on the list to avoid waiting
• If they need to take any medications before leaving home
• Arranging parking with security
• Planning who will accompany the patient to hospital and in anaesthetic rooms
• Arranging a cubicle
• Deciding if a Best Interest Meeting should be held, or if the person is able to consent to the investigation and or treatment
• Planning how to help with any phobias they may have e.g. needles, masks etc.
• Providing patient information in an appropriate format
The LD + A Team are involved with complex cases of discharge planning with other professionals and the Trust Integrated Discharge Team (IDT). Discharges may need input from the IDT if the person requires changes to care packages. This is on a Meditech referral system when someone is medically well enough to leave hospital.
The LD + A Team would liaise with Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) if the patient has an allocated professional involved from their service. If the patient would find benefit from contact with the RDaSH team, referral can be made at this point (either by the LD + A Team or therapy team).
Family would be involved in the discharge process, as well as any care providers.
On the day of discharge the patient / carer should be issued with a copy of the patient’s discharge report detailing the patient’s care needs on discharge and arrangements for support in the community, a copy is also sent to the patient’s GP. If the Community Learning Disabilities Team is involved, the discharge plan should be sent to them.
If an autistic or learning disabilities patient needs to attend an out-patient appointment, the LD + A Team can be contacted to attend the appointment with them. They can also organise community support.
If a reasonable adjustment is required, this will be marked on the patient record in order that this can be considered in future outpatient appointments. This may be earlier appointments or waiting in quieter areas.
Ensure the format of any patient information provided meets the patient’s needs. Contact the LD +A Team for information and support with Easy Read materials.
Mencap, the UK charity for those with learning disabilities, give the following advice:
1. Beware of missing a serious illness; important medical symptoms can be ignored because they are seen as part of someone’s disability.
2. Be more suspicious that the patient may have a serious illness and take action quickly.
3. Find out the best way to communicate; ask friends, family and carers for help.
4. Listen to parents and carers, especially when someone has difficulty communicating; they can tell you which signs and behaviours indicate distress.
5. Don’t make assumptions about a person’s quality of life. They are likely to be enjoying a fulfilling life.
6. Be clear on the law about capacity to consent; when people lack capacity you are required to act in their best interests.
7. Ask for help.
8. Remember the Equality Act; it requires you to make ‘reasonable adjustments’ so you may have to do some things differently to achieve the same health outcome.
Aleesha is a valued and enthusiastic member of the FJYPB. She has ambitions of becoming a F amily Law Barrister and a British wheelchair tennis paralympian Aleesha has cerebral palsy which affects her muscles, balance and co -ordination on her right side.
From her experience of working with various professionals
Aleesha has produced a series of TOP TIPS for family justice practitioners working with children and young people with disabilities.
• Respect me and my disability. 1
• See me for what I can do, not what I can't do. 2
• Educate yourself about my disability 3
• Ask me questions about my disability and how it affects me. 4

Adapt your working style to suit my needs. (For example, I have cerabral palsy which afects my right side. I can draw pictures with my left hand but you have to allow me time to do this properly - I can do most things as long as I have support.) 5
• Be creative with the tools you use with me. 6
• Do not make assumptions about me. 7
• Do not talk about me and do not talk down to me. 8
• Speak in simple language and always listen to me. 9
• Always Include me. 10
Useful Contacts and Links:
TRFT Learning Disability and Autism Team
Email: rgh-tr.learningdisabilityandautismteam@nhs.net
Phone: 01709 42 8371 (answerphone service available)
Available Monday to Friday 8am – 4pm.
Outside of these hours please consult the patient, their Hospital Passport and family / carers.
RDaSH Community Learning Disability Team – Adult Services
Phone: 01709 447744 for reception; the team works on a mobile basis.
220 Badsley Moor Lane, Rotherham, S65 2QU
Available Monday – Friday 9am - 5pm
Outside these hours, emergency support should be forwarded to the Duty Social Work Team 01709 822330
SpeakUp
Speakup is run by and for people with learning disabilities and /or autism, offering advocacy, information, training, social opportunities.
Phone: 01709 720462
Email: team@speakup.org.uk
Galax Business Centre, Fitzwilliam Rd, Eastwood Trading Estate, Rotherham S65 1SL
Rotherham Parent and Carers Forum
Rotherham Parent Carers Forum supports parents of children with disabilities. They provide peer support and advice on navigating the world of Special Educational Needs.
Email: admin@rpcf.co.uk
Phone: 01709 296262
Rotherham Advocacy Partnership (RAP)
Provides advocacy for adults, parents and young people with learning disabilities/difficulties, additional needs, dual diagnosis of LD and mental health in Rotherham and South Yorkshire.
Phone: 01709 365030
1st Floor, Osbourne House, 1-2 Highfield, Doncaster Road, Rotherham, S65 1DZ.
Mencap
Learning Disability Helpline: 0808 808 1111
(9am to 3pm, Monday to Friday)
Email: helpline@mencap.org.uk
Website: www.mencap.org.uk
NHS England Learning Disabilities
Website: www.england.nhs.uk/learning-disabilities
Patient Information:
Easy Health
Website: www.easyhealth.org.uk
Over 390 easy read health resources that include pictures and simple text, Easy Health’s information is accessible to anyone who finds written information hard to understand, including people with learning disabilities.
Plain English Campaign
Website: www.plainenglish.co.uk
11. Introduction
Autistic people with a learning disability are more susceptible to physical health issues.
Autistic people without a learning disability are at higher risk of mental health problems, including higher than normal suicide rates and die 12 years earlier on average, than the general population, with suicide being the greatest cause of this.
Overall, Rotherham’s rates of autism diagnosis are higher than the national average, with most of these being younger people. This may mean a lot of people, especially older people, will not have had a formal diagnosis. Over the next 15 years, a substantial increase in autism diagnoses is expected in the Rotherham area.
We have a duty to offer anyone with a disability reasonable adjustments, whether they have a formal diagnosis or not. If the patient tells you that they have undiagnosed autism or you believe that they may benefit from the support of the Learning Disabilities and Autism Team, you can still refer.
At The Rotherham NHS Foundation Trust, we want to ensure staff:
• are asking autistic people if they would like to be referred to the ‘Learning Disability and Autism Team’, or encouraging self-referral
• are making reasonable adjustments
• are equipped to deal more effectively with the particular needs of each individual
Autism is a lifelong developmental disability which affects how people communicate and interact with the world. 1 in 100 people are on the autism spectrum (National Autistic Society).
Autism is a spectrum condition and affects people in different ways. One third of autistic people also have a learning disability. Some people will be able to live fairly independently - although they may need a degree of support to achieve this - while others may require lifelong, specialist support. Some autistic people do not have accompanying learning disabilities, but may still have specific learning difficulties, such as dyslexia.
Autistic patients may have their diagnosis recorded on the Trust Electronic Patient Record system; Meditech as a special indicator. This special indicator should be a signal to you to find out more about how this affects that person, and to find out how you need to adjust care provision to meet their needs.
Autistic people may have been taught to conceal or minimise autistic behaviours in public. This ‘masking’ can cause high levels of stress and exhaustion. An autistic person who presents as ‘high functioning’ may become more ‘visibly autistic’ in times of stress, for example becoming nonverbal.
An autistic person could be a leading expert on nuclear physics but unable to remember to brush their teeth or clean their clothes.
Two key difficulties required for a diagnosis include:
• Social communication and social interaction challenges
• Restricted, repetitive and/or sensory behaviours or interests
Many autistic people hide their autism from other people in order to seem more ‘normal’. This is called ‘masking’. This process can be incredibly tiring, as the autistic person is consciously trying to do things that more neurotypical people may do automatically. This means they might be trying to hide their reactions to uncomfortable things, such as loud noises, bright lights, or being touched. They may be trying to actively focus on conversations, and consciously be trying to remember to make eye contact and make the appropriate facial expressions, while trying to stop any stims or anything that might be seen as ‘different’.
This effort might mean that an autistic person can seem ‘normal’, but if another unexpected event occurs, such as pain or a hospital visit, they might lose their ability to mask, or may become emotionally overwhelmed.
Autistic people’s challenges can include:
• difficulties with interpreting both verbal and non-verbal language like gestures or tone of voice
• being unable to speak or have limited speech while other autistic people have very good language skills
• struggling to understand sarcasm or tone of voice
• taking things literally and not understanding abstract concepts
• needing extra time to process information or answer questions
• repeating what others say to them (called echolalia); this can sometimes be used to communicate generally, with learned phrases
• social interaction
Autistic people often have difficulty ‘reading’ other people - recognising or understanding others’ feelings and intentions - and expressing their own emotions. This can make it very hard to navigate the social world. Autistic people may:
• appear to be insensitive
• seek out time alone when overloaded by other people
• not seek comfort from other people
• appear to behave ‘strangely’ or in a way thought to be socially inappropriate
• find it hard to form or maintain friendships
Some autistic people are non-verbal, or selectively mute, meaning that they do not speak, or only speak in environments where they feel secure e.g. at home. Although a person may not use spoken word, there are plenty of other ways to communicate.
Sometimes resources can help communication with autistic people or people with learning disabilities. Please find some resources in the back of this folder, or use the resources in your area’s ‘Communication Station’.
With its unwritten rules, the world can seem a very unpredictable and confusing place to autistic people. This is why they often prefer to have routines so that they know what is going to happen. They may want to travel the same way to and from school or work, wear the same clothes or eat exactly the same food for breakfast.
Change to routine can also be very distressing for autistic people and make them very anxious. This could include having to adjust to big events like Christmas or moving house, facing uncertainty at work, or something simpler like a bus detour that can trigger their anxiety.
IMPORTANT
My medication and my medical history:
Please do not assume there is nothing wrong with me if I don’t express pain the in the same way.
How I experience pain:
For example, do you rub the part of your body that hurts? For other examples of what to put here, see the guidance notes at www.autism.org.uk/hospitalpassport
Please don’t make any changes to my medication without first talking to:
Name:
Role: Phone number:
How I communicate:
For example, do you use Makaton?
For other examples of what to put here, see the guidance notes at www.autism.org.uk/hospitalpassport
I am autistic. Please do not assume that I do not have mental capacity. The Mental Capacity Act has five key principles:
1. Every adult has the right to make his or her own decisions and must be assumed to have capacity to do so unless it is proved otherwise.
2. People must be supported as much as possible to make a decision before anyone concludes that they cannot make their own decision. If a lack of capacity is established it is still important to involve the person as far as possible in making decisions.
3. People have the right to make what others regard as an unwise or eccentric decision. Everyone has their own values, beliefs and preferences which may be different to other people. They should not be treated as lacking capacity for that reason.
4. Anything done for, or on behalf of, a person who lacks capacity must be done in their best interests.
5. Anything done for, or on behalf of, people without capacity should be the least restrictive of their basic rights and freedoms.
Information on the Mental Capacity Act is available from www.publicguardian.gov.uk
Things that make me happy
Other things you should know about me (please refer to page 6 of the guidance notes for examples)
Things I struggle with that cause me distress
For example, are you scared of needles?
For other examples of what to put here, see the guidance notes at www.autism.org.uk/hospitalpassport
How I communicate pain:
For example, do you groan when something is hurting you?
For other examples of what to put here, see the guidance notes at www.autism.org.uk/hospitalpassport
Ways to help me avoid distress
For example, does being told you’re getting an injection and you can look away help?
For other examples of what to put here, see the guidance notes at www.autism.org.uk/hospitalpassport
About autism Autism is a lifelong developmental disability that affects how people perceive the world and interact with others.
Autistic people see, hear and feel the world differently to other people. If you are autistic, you are autistic for life; autism is not an illness or disease and cannot be ‘cured’. Often people feel being autistic is a fundamental aspect of their identity. Autism is a spectrum condition. All autistic people share certain difficulties, but being autistic will affect them in different ways. Some autistic people also have learning disabilities, mental health issues or other conditions, meaning people need different levels of support. All people on the autism spectrum learn and develop. With the right sort of support, all can be helped to live a more fulfilling life of their own choosing.
The National Autistic Society 393 City Road London EC1V 1NG
Switchboard: 020 7833 2299 Autism Helpline: 0808 800 4104 Minicom: 0845 070 4003
Please take time to read through the important information in someone’s Hospital Passport; information inside often saves time and avoids unnecessary negative situations. We are required by law to record, meet and share their communication needs (Accessible Information Standard).
TRFT uses the National Autistic Society’s ‘Hospital Passport for Autistic People’, however there are other variations that you may see being used by individuals. All will contain important information about a person’s everyday needs and wishes.
The Hospital Passport information should be completed by the person themselves, or someone who knows that person really well, ideally before they attend for their care.
This document should be regularly reviewed, as a person’s health and social needs will change over time.
This information can be used to assess whether someone’s condition has changed.
This document does not serve as consent to treatment or any other intervention. Consent must still be sought in every single context and the mental capacity of that person assessed. The passport is available on the Hub, or you can ask the Learning Disability and Autism Team or the Community Learning Disability Team. It is also available on the National Autistic Society’s website.
The LD + A Team is made up of a Learning Disability and Autism Matron and Nursing Associates.
The team is available Monday to Friday 8am – 4pm. Outside of these hours please consult the patient, their Hospital Passport and family / carers.
Email: rgh-tr.learningdisabilityandautismteam@nhs.net
Telephone: 01709 42 8371 (answerphone service available)
Nursing Associates visit autistic people and people with learning disability throughout the day and give them the help and support they need while in hospital, ensuring reasonable adjustments are made to their care pathway. The team also give support to people coming through Urgent and Emergency Care, outpatient’s and planned surgery.
They can help you to support patients in the following ways:
• Facilitate open and easy access for young people and adults with learning disabilities and/or autism accessing Trust services
• Give specialist advice and support for professionals in relation to personalised care and reasonable adjustments
• Provide accessible information
• Actively assist patients with learning disabilities and/or autism and their carers when using our services
• Provide support and advice regarding best interests, consent, advocacy, mental capacity and safeguarding
• Coordinate and assist the facilitation of learning disability or autism awareness training and further education to professionals to meet the needs of young people and adults with learning disabilities and/or autism
• Ensure that the views of patients and their carers are taken into account
Do you think you would be a great advocate for autistic people?
Would you like to gain further knowledge and understanding of how to care for this patient group?
If yes - then please become a learning disability champion for your ward or department!

Always check the person’s Hospital Passport for things that could trigger a distressed reaction. This will be found in the ‘Likes and Dislikes’ section.
Examples of what can trigger an emotional reaction in an autistic person can include; noise, touch / unexpected touch, hospital bed curtains being closed (can feel claustrophobic), not being warned about / told what is going to happen in detail, textures, eye contact, too much information given too quickly etc.
If someone is distressed, the best thing you can do is not encroach on their personal space, ask if they need time on their own, ask if they need support from someone else or if they would like you to stay, encourage deep breathing to refocus.
Autistic people may experience over- or under-sensitivity to sounds, touch, tastes, smells, light, colours, temperatures or pain. For example, they may find certain background sounds like beeping, which other people ignore or block out, unbearably loud or distracting. This can cause anxiety or even physical pain.
Many autistic people avoid everyday situations because of their sensitivity issues. Hospitals can be particularly overwhelming and cause sensory overload. There are many simple adjustments that can be made to make environments more autism-friendly. Contact the LD + A Team for more information tailored to your area.
Anxious episode / disengagement, sometimes called a ‘meltdown’ or ‘shutdown’
When everything becomes too much for an autistic person, they can go into an anxious episode where they disengage. These are very intense and exhausting experiences.
A meltdown happens when someone becomes completely overwhelmed by their current situation and temporarily loses behavioural control. This loss of control can be verbal (e.g. shouting, screaming, crying) or physical (e.g. kicking, lashing out, biting) or both.
Disengagement appears less intense to the outside world but can be equally debilitating. Disengaging can be a response to being overwhelmed, but may appear more passive - e.g. an autistic person going quiet or ‘switching off’.
One autistic woman described having a shutdown as: ‘just as frustrating as a meltdown, because of not being able to figure out how to react how I want to, or not being able to react at all; there isn’t any ‘figuring out’ because the mind feels like it is past a state of being able to interpret.’
An autistic person in this state may not present as being in pain or feeling unwell in a conventional way.
Anxiety is a real difficulty for many autistic adults, particularly in social situations or when facing change. It can affect a person psychologically and physically and impact quality of life for autistic people and their families.
It is very important to find coping mechanisms to help reduce their anxiety. However, many autistic people have difficulty recognising and regulating their emotions.
People use many methods to self-soothe. This can be called ‘stimming’. Stimming can be a variety of things, but not every person will do this, and what each person does can vary.
‘Stimming’ can include behaviours such as rocking, swinging, ticking, clapping/flapping hands, humming, rolling eyes, grinding teeth, squinting, licking, chewing, sucking on objects, wiggling / tapping fingers, staring at objects, lining up/stacking objects, dropping things to hear their sound… the list goes on.
Stimming is a self-soothing coping mechanism and should not be forcibly stopped. Stimming can be a sign of distress so if there is something obviously causing the distress, such as pain or loud noises, removing that may stop the stimming. If the patient is not causing disruption and is in no obvious distress, stimming is a harmless activity. However if you someone is disrupting other patients, you may wish to find them an alternative soothing activity or another area for them to continue stimming.
Many autistic people have intense and highly focused interests, often from a fairly young age. These can change over time or be lifelong. Autistic people can become experts in their special interests and often like to share their knowledge. A stereotypical example is trains but that is one of many. Greta Thunberg’s intense interest, for example, is protecting the environment.
Like all people, autistic people gain huge amounts of pleasure from pursuing their interests and see them as fundamental to their wellbeing and happiness.
Being highly focused helps many autistic people do well academically and in the workplace but they can also become so engrossed in particular topics or activities that they neglect other aspects of their lives.
• Speak to the patient and their carer (if present) to establish if they have any additional needs. If they are unaccompanied, and there is an identified need for support, you should attempt to identify a carer or relative and make contact with them as soon as possible.
• Details of the carer and contact numbers should be clearly documented in the demographics section of Meditech, but can also be found within the Hospital Passport for Autistic People.
• Request to see their Hospital Passport if they have it, as this may contain useful information to support decision making.
• If appropriate, fast-track autistic people or people with learning disabilities through the system. Where possible, keep their waiting time as short as you can.
• Contact the LD + A Team to make them aware of this person.
The Trust has a bespoke pathway referral system through Day Surgery, which may be appropriate for some autistic people.
If the person is coming to the Trust for a planned surgery and they are not from Rotherham, they will not have an autism flag on their record, as our information is from the Rotherham GP register. The LD + A Team put a special indicator on Meditech, as soon as they are alerted to an out of area patient coming to the Trust, usually via a pre-operative assessment, the Day Surgery Unit, or the surgical ward.
• Pre-op assessments can be supported by the LD + A Team, or can identify someone has a learning disability, to make the LD + A Team aware.
• The Hospital Passport for Autistic People is shared with the multidisciplinary team (MDT), so theatre staff, anaesthetists, consultants etc. for them to read. This helps us with our planning.
• For planned surgeries an MDT will form to discuss a bespoke plan for each individual patient.
• The plan may include how we will get clinical checks undertaken; home visits can be undertaken to get information.
The MDT plan all aspects of the admission; including all reasonable adjustments needed for them to receive their care.
This may include:
• If they need to be first on the list to avoid waiting
• If they need to take any medications before leaving home
• Arranging parking with security
• Planning who will accompany the patient to hospital and in anaesthetic rooms
• Arranging a cubicle
• Deciding if a Best Interest Meeting should be held, or if the person is able to consent to the investigation and or treatment
• Planning how to help with any phobias they may have e.g. needles, masks etc.
• Providing patient information in an appropriate format
The LD + A Team are involved with complex cases of discharge planning with other professionals and the Trust Integrated Discharge Team (IDT).
Discharges may need input from the IDT if the person requires changes to care packages. This is on a Meditech referral system when someone is medically well enough to leave hospital.
The LD + A Team would liaise with Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) if the patient has an allocated professional involved from their service. If the patient would find benefit from contact with the RDaSH team, referral can be made at this point (either by the LD + A Team or therapy team).
Family would be involved in the discharge process, as well as any care providers.
On the day of discharge the patient / carer should be issued with a copy of the patient’s discharge report detailing the patient’s care needs on discharge and arrangements for support in the community, a copy is also sent to the patient’s GP. If the Community Learning Disabilities Team is involved, the discharge plan should be copied across to them.
If an autistic or learning disabilities patient needs to attend an out-patient appointment, the LD + A Team can be contacted to attend the appointment with them. They can also organise community support.
If a reasonable adjustment is required, which may be documented in their ‘Hospital Passport for Autistic People’, this should be marked on the patient record in order that this can be considered for future outpatient appointments. This could include having an earlier appointment or waiting in a quieter area.
Ensure the format of any patient information provided meets the patient’s needs. Contact the LD +A Team for information and support with Easy Read materials.
Matthew is a valued and enthusiastic member of the FJYPB as well as being a part of other youth groups in his local area. He has experience of private law proceedings and has Asperger Syndrome.

From his experience of working with various professionals Matthew has produced a series of TOP TIPS that help him feel at ease and able to effectively engage in services. Matthew would like to share these with all professionals who work with him and other children and young people who have Autism.
•I like professionals to talk to me calmly. 1
•Don’t talk over me, let me finish talking first and wait for me to answer your questions. 2
•Don’t treat me or speak to me like a baby. 3
•Give me simple questions so I don’t get confused. 4
•Always use eye contact and ask me if I understand. 5
•Never try to force me to do things I don’t want to do. 6
•Never make false promises. If you’re doing something I will always think it is a promise. 7
•I like it when I am given good feedback. 8
•I don’t tend to show much emotion if any at all. 9
•I am a creature of habit and I like routine. 10
•When I get upset I like to be left alone in a safe environment. 11
•Make sure you always listen to me as sometimes I get frustrated and I can lose my temper 12
Useful Contacts and Links:
TRFT Learning Disability and Autism Team
Email: rgh-tr.learningdisabilityandautismteam@nhs.net
Phone: 01709 42 8371 (answerphone service available)
Available Monday to Friday 8am – 4pm.
Outside of these hours please consult the patient, their Hospital Passport and family / carers.
Rotherham Adult Neurodiversity Support Service (RANSS)

Support service for neurodiverse adults (18+) with a Rotherham GP. Offer person centred post-diagnostic support from Peer Support Workers with lived experience of autism or ADHD alongside group workshops. Meet ups and activities for all neurodiverse adults – autistic and/or ADHD (diagnosed, awaiting assessment, or self-identifying).
Email: admin@rpcf.co.uk
Phone: 01709 296292
Website: www.ranss.co.uk
The National Autistic Society

Website: www.autism.org.uk
Please visit the website to get the correct phone number for whatever you require.
SpeakUp
Speakup is run by and for people with learning disabilities and /or autism, offering advocacy, information, training, social opportunities.
Phone: 01709 720462
Email: team@speakup.org.uk
Galax Business Centre, Fitzwilliam Rd, Eastwood Trading Estate, Rotherham S65 1SL
Rotherham Parent and Carers Forum
Rotherham Parent Carers Forum supports parents of children with disabilities. They provide peer support and advice on navigating the world of Special Educational Needs.
Email: admin@rpcf.co.uk
Phone: 01709 296262
Easy Health
Website: www.easyhealth.org.uk
Over 390 easy read health resources that include pictures and simple text, Easy Health’s information is accessible to anyone who finds written information hard to understand, including people with learning disabilities.
Plain English Campaign
Website: www.plainenglish.co.uk
Resources on the Hub
• TRFT Learning Disability Policy
• Best Interest Form
• Hospital assessment for people with learning disabilities. (Traffic Light Assessment)
• DisDat Tool – Disability Distress Assessment Tool
• The Rotherham NHS Foundation Trust Strategy for People with a Learning Disability/and or Autism
• Accessible Writing for People with Learning Disabilities
• Autism (NICE Guideline)
• Equal Access for People with Learning Disabilities
• Getting it Right for People with Learning Disabilities
• Joint Safeguarding Children and Adult Services Governance Structure
• Meeting the health needs of people with learning disabilities: RCN Guidance for Nursing Staff
The sunflower is a globally recognised symbol for non-visible disabilities, also known as ‘Hidden Disabilities Sunflower’ or ‘invisible disabilities’.
Not all disabilities are visible – some are not immediately obvious. They include autism, chronic pain, and learning difficulties as well as mental health conditions, mobility, speech impairments, and sensory loss such as speech, sight loss, hearing loss, or deafness. They also include respiratory conditions as well as chronic conditions such as diabetes, chronic pain, and sleep disorders when these significantly impact day-to-day life. Although you may not be able to see these invisible impairments and conditions, they’re still there.
People living with these often face barriers in their daily lives including a lack of understanding and negative attitudes. So some choose to wear the Sunflower to discreetly identify that they may need support, help, or just a little more time.
Offer a sunflower lanyard/badge to your patients with hidden disabilities if available, appropriate and safe.

The Trust have worked with AccessAble to produce access and navigation guides for the hospital. These can be accessed from the Trust or AccessAble websites
www.therotherhamft.nhs.uk
www.accessable.co.uk/the-rotherham-nhs-foundation-trust
or by downloading the AccessAble app
These guides contain information about accessibility and facilities, such as toilet facilities and parking. They clearly show areas of the Trust, which can help people who are unfamiliar with the hospital to navigate around, and can help to reduce any anxiety caused by an unfamiliar environment.
The AccessAble guides also include instructions for common routes people may take around the hospital, complete with photographs of each area, detailed directions to where you need to be and accessibility information.
This information comes in an easy read format too, to assist anyone who may struggle to read a lot of information.
These could be helpful to show patients the way around, to help patients visualise their visit to the hospital or to find the nearest accessible facilities.
Picture cards are a method of assisting communication between staff and patients. Always check the Hospital Passport to see if a patient likes to use picture cards.
Some people with a learning disability may prefer to communicate using only picture cards. Some people may use a combination of verbal speech and picture cards.
To indicate a picture, the patient may point to it, some people may move their head to help the staff member move their finger to the topic the patient would like to raise, some people may use another gesture e.g. making a sound when the staff member points to the correct picture. Picture cards included in these resources:
• Impairments and Conditions
Physical / Visual / Hearing
• Communication
Language translation
British Sign Language
Electronic aid
Makaton
Lip reading
• Things I may need
Hearing aid / False teeth
Glasses
• Dietary needs
Kosher / Gluten free / Vegetarian
Halal / Dairy free / Vegan
• The body - site of pain
• Tests and observations
Pulse / Oxygen level / Temperature
Hearing test / Urine test / Blood pressure
Eye test / Ultra sound probe
• Test and treatment
Finger blood test (capilliary)
Naso-gastric / Canula
PEG Feeding / Blood test
Injection / Stitches / Catheter
Heart monitor / Suppository
Drip / EEG / Enema
CT Scan / Ultrasound / X Ray
Lying down / MRI Scan
Surgery / Sitting down
Standing up
• Personal Hygiene
Hand gel / Bath / Deodorant
Wash / Shower / Brush teeth
• Personal Care
Toiletries / Nail care / Hair care
Shave / Mouth care
Periods
• Going home
Home / Car / Patient transport
Taxi / Discharge lounge

















Finger blood test (capillary)



Blood test
Nas o- gastric Injection





























Care of a Patient with a Learning Disability And/Or Autism in Rotherham NHS Foundation Trust


Traffic Light Assessment
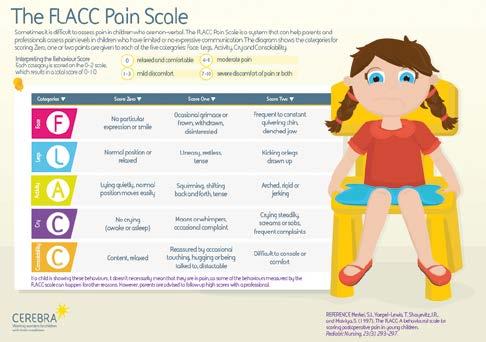
Pain Scale - FLACC
The FLACC tool can be used with anyone who has difficulty communicating that they are in pain.

This document is confidential and can only be shared with health care staff and people who I have given consent. This assessment gives hospital staff important information about you. Please take it with you if you have to go into hospital. Ask the hospital staff to hang it on the end of your bed.
Please note: Value judgements about quality of life must be made in consultation with you, your family, carers and other professionals. This includes Resuscitation Status.
Make sure that all the Health Care Staff who look after you read this assessment
Name:
Likes to be known as:
NHS Number:
Date of birth: Tel no:
GP: Address:
Next of Kin:
Key Worker/main carer: Professionals involved: Religion:
Allergies:
Current Medication:
Current Medical conditions:
Brief Medical history:
Level of comprehension/ capacity to consent:
Relaitionship Relationship
Tel no: Tel no:
Medical interventions – how to take my blood, give injections, take temperature, medication, BP etc
Behaviours that may be challenging or cause risk:
Heart (heart problems) –
Breathing (respiratory problems) -
Eating & drinking issues -
CommunicationHow to communicate with me
Information sharingHow to help me understand things
Seeing / hearing –
Problems with sight or hearing
Eating (swallowing) –
Food cut up, choking, help with feeding.
Drinking (swallowing) –Small amounts, choking
Going to the toilet –
Continence aids, help to get to toilet
Moving around –
Posture in bed, walking aids.
Taking medication –
Crushed tablets, injections, syrup
Pain –
How you know I am in pain
Sleeping –
Sleep pattern, Sleep routine
Keeping safe –Bed rails, controlling behaviour, absconding
Personal care –
Dressing, washing etc.
Level of supportWho needs to stay and how often.
Things I would like to happen Likes / dislikes
THINGS I LIKE
Please do
THINGS I LIKE
this:
Please do this
THINGS I DON‛T LIKE
Don‛t do this:
THINGS I DON’T LIKE
Thin Completed by: Date: ? ?
Don’t do this:
Think about – what upsets you, what makes you happy, things you like to do i.e. watching TV, reading, music. How you want people to talk to you (don‛t shout) Food likes, dislikes, physical touch / restraint, special needs, routines, things that keep you safe
Think about – what upsets you, what makes you happy, things you like to do i.e. watching TV, reading, music. How you want people to talk to you (don’t shout). Food likes, dislikes, physical touch/restraint, special needs, routines, things that keep you safe.