
5 minute read
FUNDING
Presenting at the 2023 SAVS annual meeting in Rio Grande, Puerto Rico, Amin A. Mirzaie—a pre-medical student at Emory University—offered observations on The National Institutes of Health’s (NIH) “modestly” aligned vascular surgical funding distribution in the context of the current Society for Vascular Surgery (SVS) priorities.
Mirzaie began by remarking on contemporary delegation of NIH funding, referring to a “precipitous and slow decline” in public service funding in the period 2006–2016. Yet, during the same time period, he continued, the NIH received a US$2 million budget increase, spurring Mirzaie and fellow authors to investigate the char- acteristics of “rare” NIH-funded projects granted to vascular surgeon-scientists. They sought to extract the amounts, types and content areas, and determine their alignment with current SVS research questions—rhetorically setting their research intentions for the audience, Mirzaie asked: “Who is being funded? […] Do funded projects align with SVS priorities?”
Estimating a total of $12 million is awarded to “all active projects,” Mirzaie et al extracted grant research characteristics in instances where a vascular surgeon was a principal investigator (PI). Identifying 53 active NIH awards given to 40 U.S. vascular surgeon-scientists, Mirzaie reiterated that
“only 1%” are receiving these awards. He noted funded vascular surgeon-scientists are an average of 15.9 years out of training, with 37.5% being women—“much higher” than other sub-specialties.
On NIH and SVS research priorities, Mirzaie posed that eight out of 53 active projects given to vascular surgeon-scientists “directly addressed” any SVS primacies. He noted that four SVS priorities included in the most recent 2021 refresh were not “fulfilled by any NIH projects.”
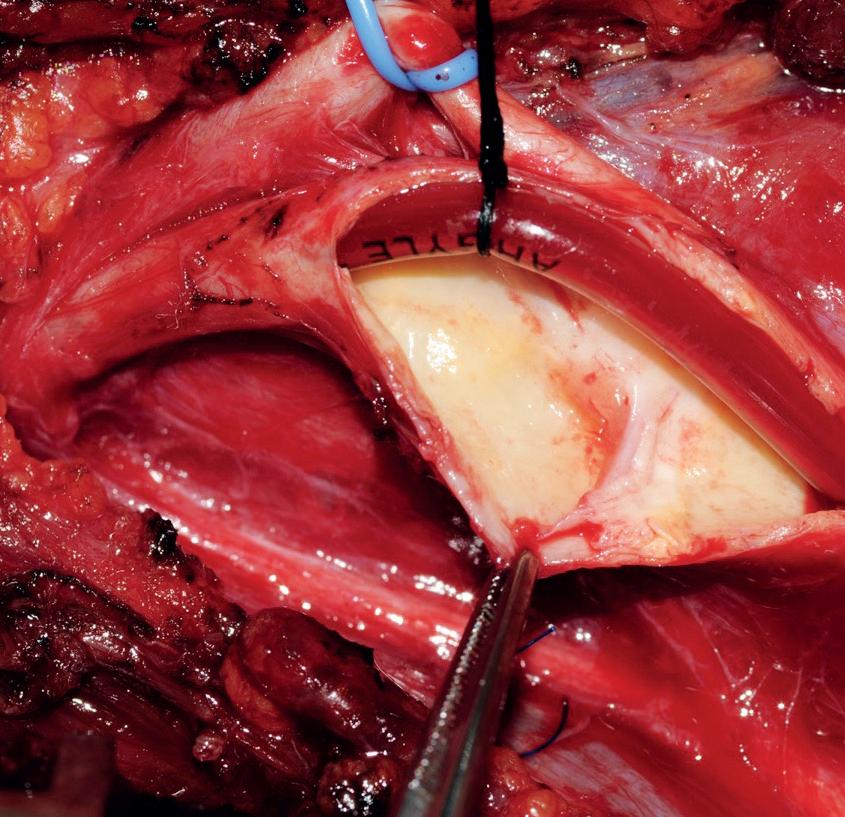
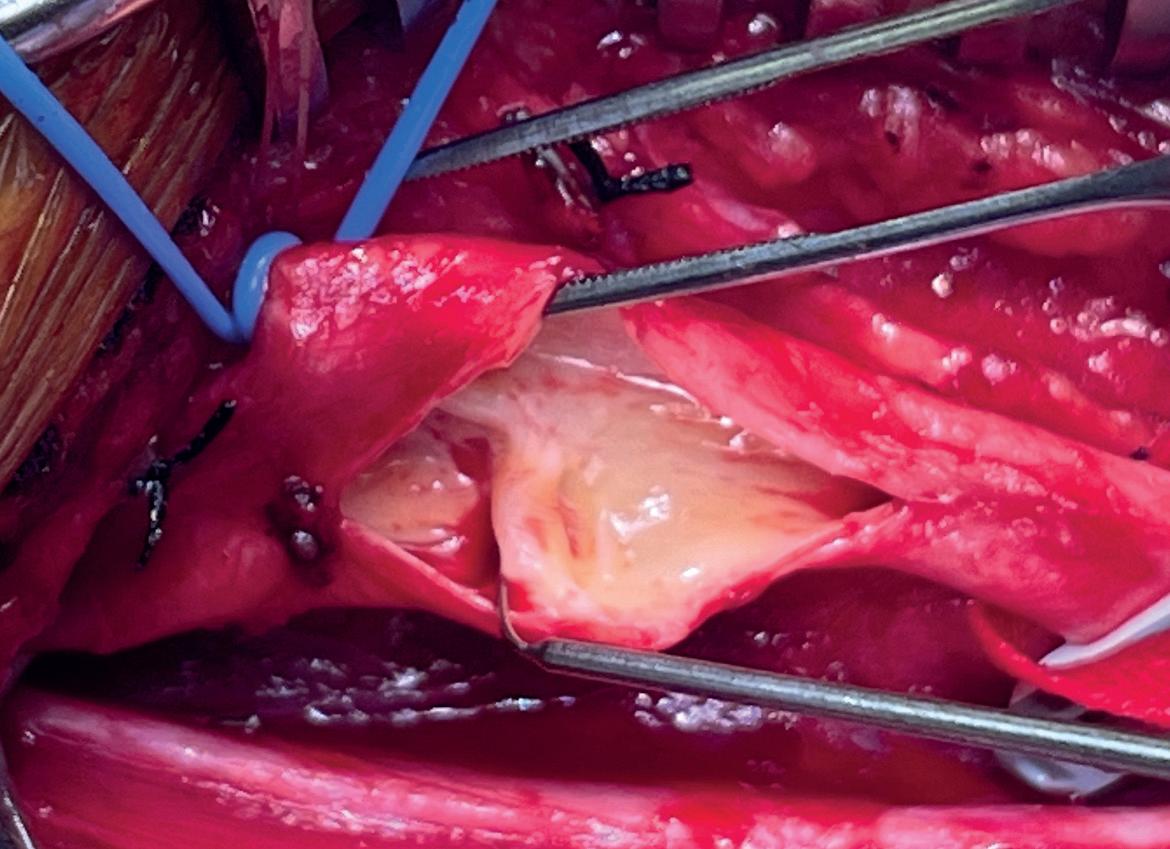
“Moving forward this shows that we need more funded vascular surgeons and better coverage of SVS priorities,” said Mirzaie.—Eva Malpass management is unacceptable for symptomatic carotid web. Recurrent stroke occurred in all patients managed early in our experience with medical therapy alone. We have since adopted an aggressive interventional approach in cases of symptomatic carotid web, with no postoperative stroke reported over an average follow-up of 26 months.”
The findings offer key insights, Brinster reflects in an interview with Vascular Specialist after the SAVS meeting. For one, when confronted with a patient who has minimal carotid stenosis, especially a younger patient, “and especially a younger African-American woman under 50 years old, which comprised one third of our series—astronomical when you think about it—this pathology must be ruled out,” Brinster explains. “And the most efficient way to rule that out in a stroke patient is with a high-powered CTA, particularly examining the sagittal projections, That is really where carotid web is most readily identified. It is very easy to miss in the axial and the coronal projections in the scan.”
Clayton Brinster
FMD occurs distally in the internal carotid artery—anatomically in a different region. It appears radiographically totally differently than web. Web appears as a shelf-like projection in the carotid bulb, whereas FMD has a very classical string-of-beads appearance in the more distal carotid. Third, the pathologic specimens of carotid web are completely different than pathologic and histologic examination of traditional FMD.” The concerning point, Brinster says, “is that referring to carotid web as simply a form of carotid FMD—which has a well-established treatment paradigm that includes medical management and balloon dilation—I think confuses practitioners.”
This may lead to either undertreatment, or mistreatment, and recurrent stroke in these patients, he argues. “It would be totally inappropriate to balloon angioplasty these lesions,” Brinster adds, with the risk of recurrent stroke “astronomical.” alluded to a genetic basis ,from Central and West African descent, through the Caribbean.” The historical migration patterns of the American South, particularly through the port of New Orleans, “is no coincidence” in the context of the findings contained in the series presented by the Ochsner group, Brinster points out. He now hopes to join forces with the physicians behind the Caroweb registry, first by creating and leading a national consortium in the U.S.
“The more people who know about it and the more people involved, the more strokes we can prevent,” Brinster says. “I can’t tell you how many people came up to me at the Southern meeting, and said, ‘I have seen this once or twice before and I didn’t know what to do. Now, I will.’ There is a lot more work to be done for these patients.”
Second, carotid web demands its own characterization, Brinster says. In the literature, the condition has traditionally been referred to as a form of carotid fibromuscular dysplasia (FMD), he notes.
“In addition to medical management being totally unacceptable for symptomatic carotid web, carotid web needs to be thought of as an independent pathology from traditional carotid FMD,” Brinster relates. “Traditional carotid
Aaa
FIVE-YEAR OUTCOMES OF ESAR IN PATIENTS WITH SHORT NECK
Cohort analysis shows no migrations, a low rate of ruptures, and positive sac regression, researchers say.
FIVE-YEAR OUTCOMES IN PATIENTS
with short neck abdominal aortic aneurysms (AAAs) undergoing endosuture aneurysm repair (ESAR) using Heli-FX EndoAnchors with an Endurant stent-graft in the ANCHOR registry showed a freedom from all-cause mortality of nearly 70%,
Meanwhile, that younger African-American female portion of the cohort is set to form the basis of at least one dimension of further digging. Thus far, Brinster says the group have only performed a pathologic evaluation on the cases they have analyzed. But, he continues, “what we really need to do is a fresh tissue analysis, and a genetic analysis of the tissue,” he reveals. “If this is based on sex and race, then it most certainly must have a genetic component. The larger French registry [of carotid web cases], called Caroweb, has from aneurysm-related mortality of 90%, from aneurysm rupture of 95.6%, and from any secondary procedures of 77%, lead study author Frank R. Arko, MD— who disclosed a consultancy relationship with and receiving research funds from device maker Medtronic—told SAVS 2023.
The cohort, with a mean age of 72, included 70 patients with an infrarenal neck length greater than 4mm and less than 10mm enrolled from 2012–2015 and fitted with the Heli-FX EndoAnchor system, which was designed to improve the fixation and seal of aortic stent-grafts. At five years, the patient group had clinical and imaging follow up compliance rates of 85% and 70%.
Some 11 patients had a total of 16 secondary procedures. None of the conversions had open repair that were for type Ia
There are hurdles to be crossed, but a potential roadmap appears to be forming. And that could involve a screening dimension.“If we try to prove some sort of genetic disposition, that could lead to more effective screening,” Brinster says. “It may be worth screening family members of those with carotid web to rule out the pathology.” Still, carotid web is a “very tricky thing to screen for without a family member who has been diagnosed, and because ultrasound is not as reliable as CAT scans, and CAT scanning, of course, is expensive and you need contrast,” he adds.

Ultimately, an opportunity beckons, Brinster says. “We have an opportunity with the size of the series, and the fact it was presented at the Southern [annual meeting], to change the way people manage carotid web—and hopefully avoid recurrent strokes in a vulnerable population.” endoleaks, although there were patients who had this type of endoleak, Arko said. “The type of secondary procedures were endovascular in the majority, and there were three conversions to open repair.”
Through five years, eight had type Ia endoleaks, three of which were resolved by the next follow-up, reported the vascular chief from Sanger Heart & Vascular Institute in Charlotte, North Carolina. There were two type Ib endoleaks, 13 patients who had a type II, and there were no type III endoleaks.
After five years, 68.2% of the registry subjects had sac regression, 13.6% had stable sacs, and 18.2% had increased sac diameter as compared to their one-month measurements, the study authors showed.
“Patients with infrarenal necks of between 4 and 10mm implanted with the Endurant II/IIs in combination with the Heli-FX EndoAnchor system showed durability of treatment through five years,” Arko concluded before the SAVS 2023 gathering in Rio Grande, Puerto Rico. “There is a need for close and lifelong surveillance in these patients with hostile necks due to occurrence of late events that appears to be appearing at around the three-year time period.
“The study is certainly limited by the small sample size and further prospective randomized controlled trials are needed, and these will be performed in the near future.”—Bryan Kay








