Meet our team!
Taanya Shenbaga Kumar (Co-Founder, Co-Head, Editor & Designer)“

Once again, thank you to all of you who have supported the MDVJ. This edition has been particularly challenging due to our Year 13 life, however our Editorial team and Aisha have supported and motivated me throughout the process. The duties of being the Head and managing editing and designing at the same time were definitely tiring, nevertheless I enjoyed the process and my friendship and compatibility with my team improved as the making of MDVJ progressed. Thank you to all contributors who worked hard for their article, some of these articles were very eye-catching and intriguing to learn about! Thank you to Mariam, who created such a masterpiece that shares the message of doctors keeping their patients alive quite literally. Yet again, looking back at the final product of all our hard work makes me feel proud of us all. Since this may be our (current Head and editorial team’s) final MDVJ, letting go of our duties seems quite emotional, as I made so many happy memories during our group talks and meeting new contributors for MDVJ. I wish the next MDVJ team all the best for their future editions . And finally, I hope all readers and contributors of MDVJ will find their love for the fields, and look forward to a life dedicated to their chosen career path. Thank you all once again.”
Aisha Yaqoob (Co-Founder, Co-Head and Editor)“Another fantastic year of effort from our team and the contributors! We are so privileged to be able to share our and our contributor’s hard work via the MDVJ . Isabella, our Chief Editor, who once again encouraged us and pushed her own limits to reach the final point of editing, and our editors–Umamah, Rukaiyya and Kelly – who, despite the ongoing assessments and stressful university application, became our pillars and led to the finish of the MDVJ on time. And our Illustrator, Mariam, whose hand skills brought an artwork to life and gave us this beautiful heart. And finally, our contributors, reading your articles and interests the different aspects of medicine, dentistry and even law was an insightful experience for me as the Head. I hope you all enjoyed the journey as much as I did and I wish the future MDVJ team all the best!”
Isabella Li (Chief Editor)
“After such a long and tiring year, I am very proud of our team and myself for persevering through to finish another edition. I learned so much from all the articles we received, and it even became a source of wider reading for our interview preparation! But the highlight of being part of the MDVJ team is how much my friendship progressed with the Heads and the editors. I have made some close friendships and funny moments through the MDVJ, and I cannot thank our school enough for providing us with such an amazing opportunity that I will treasure for a lifetime. Although it is sad to let go of my Chief Editor position and hand it down to the next person, I am glad that we received this opportunity in the first place, and I look forward to any future opportunities such as this which I take part in. Good luck to the future
Chief Editor and MDVJ team and I hope you all enjoy the process as much as I did. “
 Ifkar Editor Kelly Chae Editor Rukaiyya Anas Editor
Umamah
Mariam Seedat Illustrator
Ifkar Editor Kelly Chae Editor Rukaiyya Anas Editor
Umamah
Mariam Seedat Illustrator

A brief case study on the lethal viral infection: Tick

Borne Encephalitis

A parasite is an organism that resides either within a host organism or on its surface. Parasites rely on their host for survival as they obtain food and nutrients from it, which can be extremely damaging to the organism (1). One way in which they affect the host organism is by transmitting harmful diseases with painful, chronic symptoms. A notorious and highly lethal disease transmitted by such parasites is Tick-Borne Encephalitis (TBE), a disease caused by the TBE virus (TBEv) that is transmitted by ticks, and its clinical presentations have shown a range of severe, excruciating conditions that may last for the rest of the victim’s life (2).
This highly fatal disease is notably sporadic, with approximately 5,000–13,000 TBE cases reported each year worldwide (3). In the EU, around 3,000 to 4,000 notified clinical cases of Tick-borne Encephalitis (TBE) occurred in 2020 (4). With a noted 20% of the affected people being children, this, if mathematically calculated, would be around 600 to 800 children affected in the EU that year. In the UK, TBE was not a known condition, until 2019, when Thetford Forest in the East of England and the Hampshire/Dorset border were found to contain ticks that transmit the virus (5). Although it may not be such a fatal attacker within Europe; in Asia, especially Japan, and Eastern China, fatality rises up to 20% of total cases; furthermore, frequent and long-term neurological complications are common symptoms in the aftermath of infection(6).
Around 50% of the clinical presentations of TBE patients are Meningitis (an infection that occurs in Meninges, the three barrier membranes: Dura mater, Arachnoid mater and Pia mater, each surrounding the Brain and the Spinal cord), this induces symptoms such as headaches, fevers and neck stiffness(7,8). Additionally, approximately 40% of TBE clinical presentations lead to Meningoencephalitis (inflammation of the Meninges and the Brain tissues, potentially causing seizures, personality changes and amnesia) (7,9). This displays symptoms of Meningitis, as well as impaired consciousness and motion, palsy, delirium and breathing difficulties. A more atypical clinical representation of TBE is Meningoencephalomyelitis (inflammation of Brain tissues, Spinal cord and Meninges causing changes in the cerebrospinal fluid, leading to quick deterioration (7,10). This can cause fever, behavioural changes, and lethargy with a noted elevation of leukocyte counts. Other internal changes include swelling or Hyperaemia, which means an increased amount of blood supply that may potentially lead to Haemorrhages (blood leakage from a ruptured blood vessel in the brain parenchyma, in addition to dulling of the Meninges), which is found in less than 10% of these representations. The rarest clinical representation is Radiculitis (this is pain radiating due to pressure on the nerve root as it departs the spinal column) (11,12). The inflammation of the Brain tissue, Meninges and Spinal cord caused by the TBE exerts pressure, causing pain in certain areas of the body, depending on where the inflammation is present. For example, if inflammation occurs in the cervical spine region, it may cause Cervical spondylosis (‘wear-andtear of bones and tissues, especially seen in older patients), for which the symptoms are swelling in facet joints, “pins and needles” and occasionally pain in the limbs (13). TBE has no known cure, therefore the treatment is focused on relieving symptoms presented. If the patient’s symptoms require emergent care, they may be admitted to intensive care in order to relieve severe forms
The Role Of The Brain In An Individual’s Personality
By Aisha Yaqoob, Yr. 13Labelled the most complex organ in the body, the brain is a fascinating structure which governs our every move. It controls thought, memory, emotion, touch, motor skills, vision, breathing, temperature, hunger and every other process that regulates our bodies (1). However, it is easy to observe the physical results of the workings of the brain, such as walking. But what about the mental results? To what extent is the biological chemistry of the brain involved in one’s personality, and how much of it is due to environmental effects?
First, we shall label the parts of the brain associated with personality. There are two hemispheres: the left and the right. One of the most popular theories states that a person will be dominant on one side more than the other. It is said that dominance ofthe left hemisphere makes a person more reliant on logical thinking leading to increased verbal skills and analytical thinking whereas the dominance of the right hemisphere leads to increased intuition, perception and creativity (2). Psychologist Stephen Kosslyn states that ‘a deeper understanding of these mechanisms and the role of brain structure specifies the way in which a person interacts with their environment’ (2). This theory suggests that the brain is biologically designed to be more dominant on one side, which then affects how an individual interacts with their environment.
Stephen Kosslyn developed another theory explaining the role of the brain in personality with Wayne Miller. The foundations of this theory split the brain into two major parts: top and bottom. The theory states that the interaction of the two parts is what determines one’s personality: “The top part plans and executes while the bottom classifies and interprets information about the world that we receive” (2). Individuals who use both systems have the ability to plan effectively and easily adapt to new circumstances. Those who use the bottom brain more tend to have insight and can better interpret their experiences but are less able to take initiative for complex tasks. If the brain’s top system is more developed, the person would be very creative but have a low adaptation capacity. Those who do not rely on either of the two systems tend to get “lost” in the facts and requests of those around them and are quite easily affected by the environment (2)

So now we know the brain plays a huge role in personality development, we can look at the personality traits shown. A study which used a questionnaire called the ‘NEO five-factor inventory’, showed that personality traits can be split into five groups: neuroticism, extraversion, openness, agreeableness and conscientiousness (3). Each one of these groups was associated with a different biological structure of the brain. For example, neuroticism is a personality trait underlying mental illnesses, such as anxiety disorders, and is linked to a thicker cortex and a smaller area and folding in some brain regions (3).
One way in which we can truly understand the role of the brain in personality is by looking at a case study. Phineas Gage wasa 25year-old railroad foreman involved in a tragic accident in 1848. Whilst using an iron rod to tamp explosive powder into a hole, the powder ignited and sent the rod hurtling upward piercing Gage’s cheek passing through the frontal lobe of his brain and exiting the top of his skull (4). According to doctors of the time, it was a miracle that he managed to survive. Although, the accident resulted in a major change in behaviour. His friends described his personality as ‘greatly changed’, stating that he was ‘no longer Gage’, and he became known to often make plans but fail to carry them out. This is major evidence supporting the idea that the brainand its intricate structures are essential in personality development. We know that the frontal lobe plays a key role in planning, decision-making, problem-solving, judgement and impulse control and the prefrontal cortex, covering the frontal lobe, is associated with the expression of personality.
Although both nature and nurture play a significant role in the development of one’s personality, large-scale twin studies suggest that there is a strong genetic component (5). Twin and adoption studies indicate that human personality is around 30% to 60% heritable. So, although both factors are important, one can not deny that the role of the brain is vastly important in determining the personality of an individual, and it is this idea that can help us to combat mental health issues with medical treatments and surgeries to better the lives of those we can.
References:

1. Brain Anatomy and How the Brain Works | Johns Hopkins Medicine
2. Your Brain Structure Is What Determines Your Personality - Learning Mind (learning-mind.com)
3. How the Structure of Your Brain Influences Your Personality (newsweek.com)
4. How Phineas Gage’s Brain Injury Changed His Personality - Explore Psychology 5. Are Personality Traits Caused by Genes or Environment? (verywellmind.com)
Surrogate Pregnancy: Benefits and Limitations
 By Isabella Li, Yr. 13
By Isabella Li, Yr. 13
Surrogacy is an arrangement whereby a woman agrees to become pregnant on behalf of another person or couple who will be the child’s parent(s) after birth. There are two types of surrogacy: traditional and gestational surrogacy. Traditional surrogacy is when a woman is artificially inseminated with the father’s sperm and uses her own egg to conceive the baby, thus she is both the gestational and genetic mother (1). Gestational surrogacy is when an embryo, created from a donor egg or from the commissioning parents, is implanted into the surrogate mother, as a result, she is not genetically related to the child (1). The benefits and limitations of surrogate pregnancy will be discussed to form a conclusion.

Surrogacy can be an incredible experience for both parties in the process. For hopeful parents who are struggling with fertility, it holds the power of fulfilling people’s dreams of parenthood. It is often thought to be a ‘treatment’ option for infertility or an alternative to adoption. For example, it can help same sex couples to create a family, offering support for the LGBTQ community (2). For the surrogate mothers, surrogacy can be a rewarding gift as they can feel a deep sense of pride, knowing they helped another family. There are also other benefits: for example, surrogacy can create relationships as many intended parents become close with their surrogate, developing meaningful bonds which last a life time (2); surrogacy is often legally protected as there is usually a legally binding contract between both parties, outlining everyone’s expectations, which are negotiated prior to embryo transfer.
However, surrogate pregnancy comes with many limitations.
First, traditional surrogacy carry the risk of infections and STDs (sexually transmitted diseases). This is because the sperm donor is not screened, nor is there screening for common genetic disorders (1).
Secondly, the increase in gestational surrogacy means there is an increasing demand for eggs (1). This means many women are being persuaded by adverts to donate or sell their eggs. To do this, a woman is required to undergo IVF (In vitro fertilisation) treatment which stimulate the ovaries to produce more eggs than the normal one per month. The most common risk associated is Ovarian Hyper Stimulation Syndrome, which is an excessive response to fertility drugs given to stimulate egg production (1). The ovaries develop too many egg follicles, from which fluid would leak into the abdomen, and the symptoms range from mild (for example nausea) to severe (such as blood clots) (3). Other complications include ovarian torsion and rupture of a cyst, which can cause serious bleeding (1).
Thirdly, all pregnancies have complications and risks. This ranges from minor complications (such as morning sickness and heartburn) to more severe ones (for example, pre-eclampsia, serious perineal tears and haemorrhage), which can be fatal and life changing (for example, causing serious mental health problems, such as PTSD (post traumatic stress disorder)). (1,4).
Not only are there health risks for mothers, there are also health risks for the child. A study in the USA looked at 124 surrogate mothers and the outcomes of their pregnancy. They found that the babies had increased adverse perinatal outcomes, including preterm birth and low birth mass (1). Finally, there will be many legal and health risks if the arrangement is broken down. Surrogate mothers may develop feelings of attachment for the child they carried, thus being forced to separate from their baby may cause mental health issues. The commissioning parents may no long want the child during surrogacy, which would cause more complications.
In conclusion, although surrogate pregnancy does have several benefits, it is outweighed by the limitations. Improving IVF treatments, test tube babies, and adoptions may be better options for those who want to create a family, without risking the health of another individual.
Perinatal Mental Health - Why is it such an unspoken aspect of Pregnancy?
Pregnancy is a unique journey that women go through. From the first x-ray scan of the baby to finding out its gender and preparing for its arrival, there are many different aspects of the journey experienced with friends and family that make it memorable and enjoyable. However, although the physical health of the woman and baby are looked after, the mental health during pregnancy is usually unspoken of and disregarded in many cases.
Perinatal Mental Health refers to the mental health of women during pregnancy and up to 1 year following the birth of the child. Perinatal mental illness ‘affects up to 27% of new and expectant mums and covers a wide range of conditions’. As many as 1 in 5 women develop a mental illness during pregnancy and after birth. According to a survey conducted by the Royal College of Obstetricians and Gynaecologist (RCOG), 81% of women had suffered with a maternal mental health problem, with these health conditions ranging from low mood to psychosis. (1) These occurrences are quite normal, as pregnancy can bring a mix of feelings - from happiness to anxiety due to a variety of reasons. Women mainly experience Depression and Anxiety, however they may also suffer from bipolar disorder, PTSD, OCD, panic attacks and eating disorders.(2)
Presenter and life coach Anna Williamson explains her thoughts following the birth of her first child. ‘I suffered from severe anxiety and ill mental health. After the birth of my first baby I was in a very dark place. I remember thinking to myself, this little baby is so perfect and beautiful, he doesn't deserve to have a rubbish mother. And at the very very worst moment, I did think, it was better if I wasn’t here.’ (3) In the UK specifically, the main cause of maternal deaths that occur after pregnancy is suicide. This is evidently due to the detrimental impact negative mental health during pregnancy has if not treated. However, almost half of women in the UK have no access to mental health services.(4) The change in care was only made in 2020, allowing women to have access to specifically dedicated NHS teams and perinatal clinics dedicated to pregnant women to help them to cope with anxiety and depression. Prior to this, support has been non-existent.(5) But why has this been so?
In the past, as the significance and awareness of mental health in general increased, the awareness of mental health regarding pregnancy did not. RCOG’s survey revealed that ‘Women experienced low rates of referral, long waits, regional variation of care, a lack of continuity of care, misunderstanding and stigma.’ There is a lot of stigma attached to perinatal mental health, as well as mental wellbeing of pregnant women not really being taken into consideration or talked about by healthcare professionals. Below are some statistics from the RCOG survey of the thoughts women had regarding their mental health, which gives an insight into why perinatal mental health, due to some misunderstandings, may not have been acted upon until recently
• 40% of respondents were worried that their mental health problems would be noted on their medical records
• 32% of women didn’t realise healthcare professionals would help.
• 28% felt there was stigma attached to mental health problems.
• A further 28% felt embarrassed about their mental health problems.
• 27% felt that it as normal to experience these problems as part of pregnancy
• 23% felt unsure of what to do


• 23% felt that the clinicians were unapproachable.
• 19% were not asked if they were experiencing any mental health problems. These statistics are directly taken from the report and survey by the RCOG.(6)
The vitality of awareness regarding perinatal mental health by women and other members of the community is key in tackling the issue. Should such perinatal mental health problems go untreated, it can have a negative impact on the expectant mother and on the child’s development for the rest of his or her life. Thankfully, the NHS has acted on this misjudged problem by making maternal mental health a priority by the government. Five years ago, there were very limited Perinatal Mental Health services available to women, and the majority of counties and regions in the country didn't have a specialist community team dedicated to this specialty. Now, there are over 44 local NHS specialist Perinatal Mental Health community services allowing over 13000 women to receive support. (7)
The RCOG’s key priorities for women regarding perinatal mental health are: support being provided by healthcare professionals, local access to Perinatal Mental Health services at regular times, partners being supported and all conditions associated should be treated. (8) The NHS shows a promising trajectory for Perinatal Mental Health, as it will remain and increase in the UK. However it is crucial that more women are aware of such support so that these problems can be treated efficiently and the number of maternal mental health problems decreases in the future.
References:
1. https://www.rcog.org.uk/for-the-public/rcog-engagement-listening-to-patients/maternal-mental-health-womens-voices/ 2. https://kidshealth.org/en/parents/pregnant-mental-health.html 3. https://www.youtube.com/watch?v=uTD5mn4tAPQ 4. https://www.rcog.org.uk/for-the-public/rcog-engagement-listening-to-patients/maternal-mental-health-womens-voices/ 5. https://www.youtube.com/watch?v=uTD5mn4tAPQ 6. https://www.rcog.org.uk/media/xcmi3djo/maternal-mental-health-infographic.pdf 7. https://www.england.nhs.uk/mental-health/perinatal/ 8. https://www.rcog.org.uk/media/3ijbpfvi/maternal-mental-health-womens-voices.pdf
By Umamah Ifkar, Yr. 13As technology advances with time, patients may have to rely on robots to survive. With the rise and development of artificial intelligence (AI), new technologies may become more readily present in healthcare. An example of this is a type of AI known
as ‘machine learning’, which has been evolving medicine in ways which will change the future for everyone.


Machine learning are computer systems that can perform tasks that normally require human mental intelligence, such as complex decision making, visual and auditory perception and recognition, and facing unexpected challenges(1). It uses algorithms that have the capacity to learn and respond to data, adjusting and improving performance in response to feedback and different inputs and outputs. Machine learning is progressively playing an increasingly important role in helping healthcare organisations tackle new and complex issues. For example it can help to improve diagnostics, manage population health, accelerate drug discovery, and modernise care support.
In terms of increasing the competency of investigating symptoms and data, machine learning helps to structure and analyse information, making it more quicker and efficient – whether it’s concerning precision diagnosis using genomic sequencing, early cancer detection, or advanced cancer visualisation (1).
By developing a better understanding of the health of a population, health care professionals can make rigorous data-driven decisions to care for millions. Using advanced machine learning models can help to understand how a population changes over time to identify the most appropriate treatment for lots of patients (2).
Machine learning can help in the rapid experimentation for drug discovery , enabling smart manufacturing to post market surveillance to detect negative events. It can assist in efficiently discovering, developing, trialling, and the commercialisation of medicines. This means that scientists and doctors (and other medical associates) can easily make and prescribe treatments.
AI can help to simplify and automate processes to help improve efficiency, reduce hospital waste, and decrease physician burnout. At Houston Methodist, a hands-free voice assistant has been created to make contact-less solutions to improve patient safety and experiences. In the operating rooms, the voice assistant helped before, during and after operations. It allowed surgeons to start and stop verbal timers and also allow staff to complete verbal checklists concerning the surgery (3).
AI needs human surveillance since machines operate logically which means they can ‘miss’ behaviour and actions that a physician would normally take into consideration. It may also overlook social factors that can play into prescribing appropriate treatments to patients. This system may not consider patient preferences and economic restrictions. There is also the possibility that it may lead to unemployment. Although it reduces clinician fatigue and perhaps even cost in certain cases, it may displace professionals who have spent many years and lots of money in their education and practising in their specialty. Furthermore, since AI is generally dependent on networks, it can become susceptible to security risks (4). So, does AI play a part in the future of our health? Its doubtless potential in advancing and improving healthcare systems globally demonstrates how it is clearly a valuable and effective asset in caring for our societies. Despite some of the challenges AI faces, this ingenious technology gives capacity for life-changing benefits to the medical sector. Whether it’s doctors or patients, lives are being saved everywhere.
NanoKnife: The use of Induced Cell Polarisation to cause Apoptosis.
Amongst the various advancements in the medical field, only very few expose the patients’ body to a direct supply of electricity, due to the risk of electrocution and other risk factors in the patient which may lead to further complications or even death. However, a tool named ‘NanoKnife’ induces an electric field around the targeted cell/cells leading to cell destruction on the patient, without causing accidental damage to the nearby cells (1). With a very low risk of electrocution, it allows certain, delicate treatments to take place without using highly invasive surgeries. This technique mainly aids in different tumour-based procedures, such as pancreatic tumour treatments, is deemed to be safe and has passed its trials, assessed by the FDA, in January 2018 (2). It is particularly used in tumours that are hard-to -reach and are very close to arteries, veins and other organs, where the chances of surgical errors causing severe repercussions is very high. Therefore, this device allows the surgeons to operate and kill cancerous cells without harming other body parts.
The NanoKnife works by inducing an electric field around the targeted cell. It consists of two needles: one with a p.d of +1500V and one which is held on the other side of the cell, with a p.d of -1500V (3). This sends nanosecond pulsed electric fields (nsPEF), which are micro to millisecond impulses that cause a form of electrostatic force to be induced (4).This results in the cell membrane having a polarisation occur in the membrane and the organelles present in the cell, which was originally at 0V.
As the charges in the cells are attracted to the anode and cathode, the forces pulling the charges cause nanopores to occur on the cell, eventually leading to a full rupture of the cell membrane, causing Lysis and ultimately destroying the cell.
Pros

• The efficiency of the procedure is proven to be better than current cancer treatments, such as radiotherapy and chemotherapy. This is because it is very targeted and allows precise alterations to the voltage and movement of the needle ends, therefore it is very controlled.
• Short procedure, as it does not require follow-up appointments. This is due to the immediate death of the cells caused by the high voltage application on the cells and less need for postoperative care.
• Less invasive than many procedures, and so it has less surgical complications and also has short recovery time after surgery.
Cons:
• It is still an invasive procedure, as it pierces through the skin and flesh, and needs anaesthesia to be present during the procedure.
• Uses extremely high voltage, therefore a lot of risk assessments must be undertaken, and the instruments must be checked for any damages to ensure the voltage doesn’t affect other parts of the patient or cause an electric current.
• Still has the possibility of damaging nearby cells and blood vessels, as the cells are manually targeted (using CT or Ultrasound) by the surgeons and there is a margin of human error that may cause rupture of cells or blood vessels, done by the high p.d. However, the benefits outweigh the costs, and with precise using and manipulation of the voltage and equipment, this instrument implements a fascinating combination of Physics and Medicine to help remove internal tumours and potentially save lives using the precision of surgeons and the mechanics of Physics.
References:
1. Bos, W. van den, Bruin, D.M. de, Muller, B.G., Varkarakis, I.M., Karagiannis, A.A., Zondervan, P.J., Pes, M.P.L., Veelo, D.P., Heijink, C.D.S., Engelbrecht, M.R.W., Wijkstra, H., Reijke, T.M. de and Rosette, J.J.M.C.H. de la (2014). The safety and efficacy of irreversible electroporation for the ablation of prostate cancer: a multicentre prospective human in vivo pilot study protocol. BMJ Open, [online] 4(10), p.e006382. doi:10.1136/bmjopen-2014-006382.
2. Marshall, S. (2019). FDA approval to initiate NanoKnife DIRECT clinical study. [online] Interventional News. Available at: https:// interventionalnews.com/nanoknife-direct-clinical-study/#:~:text=In%20January%202018%2C%20the%20FDA.
3. Musko, B. (n.d.). NanoKnife IRE Cancer Treatment Abroad | EuroTreatMed. [online] Euromed. Available at: https:// eurotreatmed.co.uk/treatments/oncology/nanoknife-ire/.
4. Kiełbik, A., Szlasa, W., Novickij, V., Szewczyk, A., Maciejewska, M., Saczko, J. and Kulbacka, J. (2021). Effects of high-frequency nanosecond pulses on prostate cancer cells. Scientific Reports, [online] 11(1), p.15835. doi:10.1038/s41598-021-95180-7.
By Taanya Shenbaga Kumar, Yr. 13How Gene Therapy Could Help Cure the Leading Cause of Vision Loss
Age-related Macular Degeneration (AMD) is a disease which results in the severe loss of central vision. It is the most common cause of vision loss (affecting over 600,000 people in the UK (1) and 11 million people in the US (2)) amongst people aged 50 and over. This disease affects the clarity of vision as it makes images distorted, blurred and indistinct, making it difficult to read, drive and recognise faces. In late stage AMD, straight lines can become wavy, objects can look smaller than normal, colours can seem less bright and the patient may experience hallucinations. This makes peoples’ lives increasingly more difficult as the simple daily tasks they used to carry out are now an everyday struggle. There is no known cause of the disease, but the risk can be lowered by not smoking, maintaining a healthy blood pressure and including the recommended daily intakes of vitamins.



The two types of this disease are wet and dry. Dry AMD accounts for 80% of the cases (1). This happens when light-sensitive cells in the macula (part of the retina at the back of the eye responsible for most of our central vision) slowly break down, and form the deposits of a protein called Drusen. Therefore there is a loss of vision in this area. The key factor in dry AMD is the complement system (a system of proteins in our immune system that fights bacteria). These proteins are overactive and attack the retinal cells in a similar way in which they would attack bacteria, therefore the macula is affected. There are currently no effective treatments for this disease.
However, due to the important scientific achievement in the 20th century of gene transfer therapy, there has been hope for patients with the untreatable disease. Gene therapy is a technique that modifies a person’s genes by replacing the gene causing the disease with a healthy copy of the gene. The eye is one of the most suitable targets for gene therapy, as it is easily accessible and allows local application with reduced risk of systemic effects.
A new technique inserts copies of the gene producing the protein, which counteracts the inflammation, into cells of the retina to slow and even stop the degeneration. This is done by using AAV (Adeno Associated Virus) as a vector (non-pathogenic) as it is known to get into retinal cells. In order to do this, the eyes’ clear internal jelly must be removed; this is done by a type of key hole surgery. Following this, a needle narrower than a human hair, creates a small fluid filled blister under the retina, and the virus can then release the synthetic gene which can now be used by the cell to make the missing protein. This surgery normally lasts about an hour and is done under local anaesthetic. After the procedure, there is a small area of retinal detachment which usually lasts 24 hours, until the fluid slowly gets absorbed by the retina. In the following weeks, the internal jelly is naturally restored by the body, and the patient should start to see more of their central vision as the cells in the macula are renewed.
The first procedure was carried out on 17th January 2019 at John Radcliffe Hospital in Oxford, and a Phase 2 clinical trial (3) is soon to be conducted. The estimated study completion date is 31st October 2025, after which 250 patients over the age of 55 with the disease should have received the surgery, in hope that this technique can help millions of people around the world to see what they once saw before.
By Riya Hasija, Yr. 12Should Neurology and Psychiatry be combined?
Neurology focuses on the nerves and the nervous system, and a neurologist is a doctor who treats disorders which may arise there. These can involve impaired behaviour, cognition and speech, and can include Parkinson’s Disease, Epilepsy, Alzheimer's Disease, Autism Spectrum Disorder, and many more.
Psychiatry focuses on mental illnesses; these are illnesses involving abnormalities in behaviour, emotions, and thoughts. They include Depression, Schizophrenia, Obsessive Compulsive Disorder, and many more. A psychiatrist is a doctor who treats these. However, what exactly distinguishes Neurology from Psychiatry in modern medicine?
For many centuries, these fields were considered as one. Researchers, including Hippocrates, would study the brain and the mind together in a field known as Neuropsychiatry. Some scientists in the 19th Century believed that eventually, a physical, biological cause would be found for all mental illnesses (2).
However, there were many who opposed this view, believing that treating ‘insanity’ was not the job of a physician. As time passed, more and more began to agree with this. In academia, neurologists and psychiatrists had little interest in working with each other, as their theories would conflict with each other (1). Neurologists took on disorders with more physical and biological signs, whereas Psychiatrists took on psychological disorders, thought to have only minor physical aspects. Later on, Freud’s theories drastically changed the world of Psychiatry, with the introduction of techniques such as psychoanalysis and new perspectives towards mental abnormalities and their treatment. This caused the two fields to separate further from each other, as psychoanalysis was considered by many to be unscientific and non-medical. Psychiatry was essentially isolated from the rest of the medical world.
However, recent developments in medicine have caused people to question whether this split is beneficial or not (3). Studies have shown physical and chemical changes to the brain in many psychological disorders. For example, brain scans and postmortem studies have shown depression to be linked to abnormalities in serotonin, dopamine, and norepinephrine levels(4). Drugs such as serotonin-norepinephrine reuptake inhibitors and selective serotonin reuptake inhibitors, which block the reuptake of these chemicals in the brain, have been demonstrated to be an effective treatment for depression. This clearly suggests that depression is a brain disorder, similar to neurological disorders such as Parkinson’s which also involve imbalance in dopamine levels.
Further evidence shows a significant proportion of patients with epilepsy go on to develop comorbid psychiatric illnesses, especially depression (5). Between 30 and 50 percent of children with epilepsy develop a psychiatric disorder. Those who experience generalised seizures are more prone to developing issues with attention, whereas those who experience seizures involving the limbic system are more prone to issues with behaviour and personality. This further portrays how neurological and psychiatric disorders are interlinked in a complex manner.
It is also important to look at the overlap between the 2 fields. For example, autism is considered a neurological developmental disorder, which affects behaviour, communication and cognitive abilities (6). A child with autism would often see a team of professionals, including both a child neurologist and a child psychiatrist. This complex condition has been studied widely in both of these fields. Similarly, conditions such as ADHD (attention deficit hyperactivity disorder) and dementia are also studied in both fields. This indicates how undoubtedly similar the 2 fields are.
The existence of a split between neurology and psychiatry has caused a range of issues for the medical world. It complicates treatments for many patients; is a patient with dementia better off seeing a neurologist or a psychiatrist? As more developments in neuroscience are being made, psychiatric disorders have been found to be more similar to neurological disorders, making the distinction between neurology and psychiatry increasingly unclear. Merging these two fields would overcome this issue, encouraging further collaboration between neurologists and psychiatrists, and paving the way for innovative, collaborative research. It would also solve the growing issue of underfunding in psychiatry, in both patient care and research. Furthermore, the treatment processes for patients would be much more simplified and accessible. For all the reasons explored above, I believe that merging psychiatry and neurology would benefit funding, research, and patient care, and would be rewarding to the medical field.
By Zahra Yousaf, Yr. 13References:
1.

https://pubmed.ncbi.nlm.nih.gov/14698691/
2. https://www.lrb.co.uk/the-paper/v32/n19/mikkel-borch-jacobsen/which-came-first-the-condition-or-the-drug
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478930/
4. https://www.news-medical.net/health/Norepinephrine-and-Mental-Health.aspx

5. https://www.massgeneral.org/children/epilepsy/education/mental-health-and-behavior
6. https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd
Chemical Warfare is the use of toxic chemical substances during military operations in warfare, in order to kill, maim or injure an enemy force [1]. It was first officially used in Belgium, on the 22nd of April 1915, where an attack was launched by the Germans against the Allied line of the northern end of the Ypres salient. Almost immediately, the chlorine gas cylinders, which had been embedded in the ground by German specialists, created strife and devastation amongst the soldiers [2]. The symptoms included irritation of lung tissue (leading to choking and eventual death), blurred vision, inflammation of skin, blisters and nausea [3]. The infamous choking agent, chlorine gas, was used extensively throughout WW1 by both sides; its most known attack being the first chemical assault in Belgium, where more than 150 tonnes of it was used against the Allies [4,6].
Due to the nature of the attack being against two adjacent French colonial divisions, a 5–6-mile gap had been created in the Allied line defending the city, allowing for the surprised Germans to advance [2]. This caused immediate terror and chaos, leading to a panicked and hasty retreat from the Allies.
Over 1000 French and Algerian soldiers were killed by this “slow moving wall of gas,” while another 4000 were injured [4]. A British officer had stated that amidst the pandemonium, he saw “A panic-stricken rabble of Turcos and Zouaves with gray faces and protruding eyeballs, clutching their throats and choking as they ran, many of them dropping in their tracks and lying on the sodden earth with limbs convulsed and features distorted in death [2].” Furthermore, despite there having been previous intelligence reports about “strange cylinders” prior to this attack, the soldiers had still been blindsided, with virtually no technology to protect them from this new weapon. Many had even tried to use “linen masks soaked in water” and “respirators made from lint and tape,” but unfortunately this had no effect in the fight against this horrifying new weapon [2,4]. Succeeding this initial attack, both sides of the war armed themselves with the technology and operational tactics of gas warfare, leading to the synthesis of more chemical weapons such as mustard gas, phosgene, diphosgene etc. [2,5]. Overall, the use of chemical weapons in the first World War caused nearly 100,000 deaths, while over another million were caused by attacks after WW1 [5]. During WW2, the Nazi’s had used hydrogen cyanide to kill millions of people in the gas chambers of Auschwitz and other extermination camps [7]. However, in the war itself, chemical warfare was not used, mainly due to all the major participants already having possessed key defences such as gas masks, protective clothing, and detectors [6].
Furthermore, despite chemical warfare taking credence to a proportionally low number of deaths during World War 1, it still had its lasting effects on the people. Many suffered psychological damage including trauma and PTSD, from the “gas fright”, while those who survived being exposed to chemical agents, and those who worked with them, had severe health consequences in the years after [4] An example includes the physical long-term effects of mustard gas: chronic bronchitis and pulmonary fibrosis [9]. Another example is the psychological long-term effects of sulphur mustard: somatization, depression and phobic anxiety [8].
Throughout the years, various legislations and acts have been put into place in order to hinder the use of chemical weapons. Examples are: The Chemical Weapons Act 1997, The Geneva Protocol signed in 1925, and The Hague Conference signed in 1899 [1]. Nevertheless, despite these agreements in place, chemical weapons are still in use by countries. Whether it is by actually using them (April 4, 2017 - Chemical weapons used to attack dozens of people in Syria's northern Idlib province), or by just stockpiling for future use (Russia has over 40000 in stockpiling), most countries are still taking part in some form of
mustard in order to treat psoriasis. In the 1940’
chemotherapy. However, while some problems of


CRISPR-Cas9 is a gene editor that can cut, split and replace segments of DNA, DNA base pairs, or even select a specific base and change it in a less expensive way in comparison to other methods of gene editing. This system is based on a bacterial immune system that aids bacteria against virus attacks by cutting a small amount of the virus’ DNA when it first attacks the bacteria, and then using this DNA segment to identify the virus if it attacks in the future, allowing it to defend itself quicker and more efficiently (1). This immune system of some bacteria is called Clustered Regularly Interspaced Short Palindromic Repeats, i.e. CRISPR for short (2). Cas9 is a programmable nuclease (a type of enzyme that can break or split Nucleotides) that breaks the DNA at specific locations (3). When the cleavage occurs, the cell starts to repair this to restore itself to its original structure. This process is, however, prone to errors as different bases can connect to the wrong pair and bases may be unpaired with their complementary base pair. Although these issues mostly end up as silent mutations, it is possible that they may lead to genetic disorders. In order to correct this, a new, proper set of DNA is placed on the unrepaired area and this stops genetic mutations forming during the tear. The Cas9 has a sgRNA (single guide Ribonucleic Acid) that locates which specific part of the DNA needs to be broken. Scientists have found a way to change the coding in the sgRNA and this means that it is now possible to forge the Cas9 to go to any specific area of the DNA that they want it to break. This is how errors are rectified. In order to use this technology against cancer cells, CRISPR-Cas9 can be used to strengthen Killer T-cells. Killer T-cells are cells that detect foreign bodies and destroy them, similar to security cells (4). Cancer cells can sometimes “dodge” these cells or even go completely undetected. Editing the DNA in these Killer T-cells and increasing their effectiveness will make sure that fewer cancer cells go undetected and so the cancer cell production is halted. This can be done by coding the sgRNA to change the DNA codes and replace them with the coding for extra protection, extra detection of surface proteins and faster destruction (in other words, faster engulfing of such cells) codes. Although the chances of tumour growth are reduced, the risks of getting cancer (or even a recurrence of cancer) is not reduced. This procedure does not prevent the future growth of cancers. There can also be circumstances where the Killer T-cells may not be able to detect or destroy the cells, as we do not know if the method will be completely effective. Another way to stop the cancer is by deactivating PD-1 and PD-L1. PD- 1(Programmed cell Death-1) and PD-L1 (Programmed cell DeathLigand 1) are proteins that bind to each other to deactivate the Killer T-cells (5). By programming the Killer T-cells to avoid or destroy the PD-1 and PD-L1, Killer T-cells can work better, without obstruction. Hence, cancer cells are less likely to go undetected and the Killer T-cells can kill the cancer cells at an early stage. Another way of stopping cancerous cells from progressing or even destroying them is by programming the cells to self-destruct. The process of Apoptosis (programmed cellular death) is when the cell kills itself when it becomes dangerous and harmful for the body (6). This mechanism is found in all cells. It happens in cancerous cells (or cells that “fail to function” as normal) when a signal from the tumour suppressor gene triggers the cell to produce some killer proteases that cause lysis of the cell and destroy it (7). When a mutation alters the tumour suppressor gene in cancer cells, it stops coding for apoptosis, resulting in the cell continuing to divide too much. If the tumour-suppressing gene is rectified or even modified to be stronger, the cancer cells can self-destruct and the cancer tissues will eventually die. These methods can be used on all types of cancers as they are both caused by uncontrollably dividing cancer cells.
 By Taanya Shenbaga Kumar, Yr. 13
By Taanya Shenbaga Kumar, Yr. 13

CML: What is it and how is it formed?
Leukaemia is a cancer of the white blood cells (WBCs) of the body. CML is a type of slow-growing leukaemia, and starts when WBCs develop a genetic mutation called the BCR-ABL fusion gene that starts to grow uncontrollably in the bone marrow cells and the bloodstream.
Blood cells can be viewed directly under the microscope to look at the different types of cells (Fig 1). There are many types of blood cells, from red blood cells which carry oxygen to the body and white blood cells which help the body fight infection.
Figure 1: Blood film showing different cell types. Figure 2: Blood film of a patient with normal feature

Approximately 9000 Americans are diagnosed with CML every year, of which 1000 die. It can affect people of all ages, but 70% of patients diagnosed with CML are over 50 years old. 15% of all new leukaemia cases are CML (1). CML is not passed down through generations because the DNA changes occur in a person’s lifetime, not before birth. Some risk factors for CML are age (the older a person is, the more likely they are to have CML), gender (it is slightly more common in males than females) and exposure to ionising radiation (2).
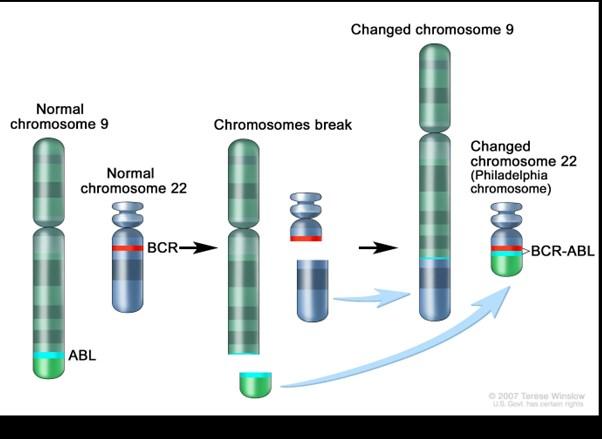
Due to the cancer growing slowly, one in two patients are asymptomatic, but some symptoms are: Extreme fatigue and weakness, caused by anaemia (shortage of red blood cells), weight loss, caused by splenomegaly (enlarged spleen) pushing on the stomach and decreasing the appetite, fever, night sweats and pain in the upper left abdomen, due to splenomegaly These symptoms are caused by the leukaemia cells affecting the growth of normal blood cells in the blood marrow. This will cause anaemia, leukopenia (shortage of white blood cells, which increases the likelihood of infections), neutropenia (shortage of neutrophils, a type of white blood cell that helps fight bacterial infections), and thrombocytopenia (shortage of platelets, which can make a patient bruise or bleed easily), and splenomegaly in 45-75% of patients (due to an increased number of leukaemia cells being stored). Patients that are affected by CML will often have an increased white blood cell count, but these are leukaemia cells and do not protect against infections. They will also have an increased platelet count, but they do not function in the way they normally do (3). The cause of the increased white blood cells in CML is due to an abnormal chromosome of the blood cells called the Philadelphia Chromosome. The Philadelphia Chromosome is formed when parts of chromosomes 9 and 22 break off and join together abnormally. This is called a reciprocal translocation and puts together 2 genes in close proximity, BCR and ABL (Diagram 4). This mutation is found in all patients with CML.
Diagram 4: How the Philadelphia Chromosome is Formed
The Philadelphia Chromosome changes the DNA of the cells so that the enzymes, called tyrosine kinases, are produced. These enzymes cause the cells to grow in much higher numbers than normal, resulting in leukaemia.
There have been many advances in the diagnosis and treatment of CML due to the research of the disease by various scientists. CML is commonly split into three phases, depending on how many blasts (immature white blood cells) are in the bloodstream or the bone marrow (4):
• Chronic phase (CP), in which most patients are diagnosed. 10% blasts in the blood and bone marrow and the symptoms are quite mild. Treating this is often in order to reduce symptoms of the CML.
• Accelerated phase (AP), in which there are 15-30% blasts, and a very low platelet count. The cancer does not respond to treatment as well as in the chronic phase.
• Blast phase (BP), also known as acute phase or blast crisis, in which the blast cells are over 20%, and found in clusters in the bone marrow. They have spread to organ tissues outside of the bone marrow, leading to symptoms a lot like acute leukaemia.
References :
1. The American Cancer Society, “Cancer Facts & Figures”, January 12th 2022, accessed at https://www.cancer.org/cancer/chronic-myeloid-leukemia/about/statistics.html
2. American Society of Clinical Oncology, “Leukemia - Chronic Myeloid - CML: Treatment Options”, June 19th 2018, accessed at www.cancer.net/cancer-types/leukemia-chronicmyeloid-cml/introduction



3. American Society of Clinical Oncology, “Leukemia - Chronic Myeloid - CML: Symptoms and Signs”, May 14, 2018, accessed at www.cancer.net/cancer-types/leukemia-chronicmyeloid-cml/symptoms-and-signs.
4. Adam Rowden, “What to know about the history of chronic myeloid leukemia”, 29th September 2021, accessed at https://www.medicalnewstoday.com/articles/history-ofchronic-myeloid-leukemia
Figure 1: Patel, Hitesh, 23rd January 2022, “Blood Film Showing Different Cell Types”


Figure 2: Patel, Hitesh, 23rd January 2022, “Blood Film of a Patient with Normal Features”
Figure 3: Patel, Hitesh, 23rd January 2022, “Blood Film of a Patient with CML”
Figure 4: Winslow, Terese, “How a Philadelphia Chromosome is Formed”
By Uma Patel, Figure 3: Blood film of a patient with CML, with higher no.of WBCs,Treatment prospects of CML
There are three types of therapies used to treat chronic myeloid leukaemia (CML): targeted therapy, chemotherapy and immunotherapy. However, treatments are always being reconsidered (1).
Targeted therapy targets the cancer tissue (such as the proteins and genes) while also limiting the damage afflicted to the healthy cells. This is done by using tyrosine kinase inhibitors (TKIs), which prevent the tyrosine kinase enzymes from multiplying, so CML cells stop growing. Targeted therapy has some side effects (such as inflammation of the liver, which means patients should be tested for hepatitis). For CML at the moment, five TKIs are available: Imatinib, which was the first TKI available in 2001; Dasatinib; Nilotinib; Bosutinib; and Ponatinib, which has possible strong side effects but is the only TKI that is effective in patients with the T315I mutation cells. They all have the suffix ‘ -inib’ because they ‘inhibit’ the tyrosine kinase enzymes that make the cancer cells grow faster. 35% of patients treated with Imatinib developed a resistance to it, and therefore the other four TKIs were developed. When the TKI is not taken regularly, the CML could start to resist it, so tests need to be carried out regularly to ensure the drugs are still working. To measure the effectiveness of TKIs on individual patients, regular check-ups are done every three months during the first year to check that the levels of white blood cells and platelets are healthy, there are no abnormal cells in the blood, the spleen has returned to the normal size and the patient has no symptoms anymore. Also, a patient will be tested to see if they have had a complete cytogenetic response (CCyR), which means at least 20 blood cells in a bone marrow aspirate have no Philadelphia Chromosome (which requires doing a bone marrow biopsy), and also a major molecular response (MMR) which is when the BCR-ABL:ABL ratio is less than 0.1%. Even if the patient has seemed to recover well, they still need to continue taking the TKIs throughout their life, in order to prevent the leukaemia from returning.
Chemotherapy targets cancer cells and kills them by preventing them from growing and reproducing. Hydroxyurea is used as a drug to reduce the white blood cell count before the leukaemia is diagnosed, but this does not reduce the percentage of cells with the Philadelphia Chromosome.
Immunotherapy is used to increase the body’s immune system in order to fight the abnormal cancerous cells. For example, a drug called Interferon (IFN-a) is given regularly as an injection to reduce the white blood cell count and was the primary treatment for CML before Imatinib was produced. However, it can cause many flu-like side-effects, such as fatigue and a fever, especially when given for a long period of time. Immunotherapy is more useful to treat CML than the use of TKIs when the patient is pregnant, because TKIs are not safe to use during pregnancy, but overall, TKIs are more effective and cause fewer side effects.
Another way of treating CML is to carry out a haematopoietic stem cell transplantation (HSCT). This is when the bone marrow cells that are affected by CML are replaced with haematopoietic stem cells that will be able to grow into healthy bone marrow, which is not cancerous. This process often causes many side effects, which is why it is a less popular option today, but is the only treatment that is able to completely cure CML. Only allogeneic (ALLO) stem cell transplants are used to treat CML, which is using donated stem cells, as opposed to autologous (AUTO) stem cell transplants which use stem cells from the patient.
Symptoms and side effects of the treatments are reduced using palliative care. This mainly is used to improve the patient’s quality of life, for example by giving medication and practising stress reducing techniques (2).
In 1865, Fowler’s solution was the first treatment for CML and consisted of a 1% solution of arsenic trioxide. However, this was discontinued due to many patients developing chronic arsenic poisoning. Between 1900 and 1950, radiation therapy was used to treat the symptoms caused by splenomegaly, but this treatment also killed many healthy cells, causing severe side effects in most patients, such as diarrhoea, fatigue, and hair loss. In the 1950s, chemotherapy was developed, leading to busulfanan and hydroxyurea being the main treatment options for CML, but these drugs only controlled the white blood cell count and did not kill the leukaemia. In the 1980s, the immunotherapy drug IFN-a was first used successfully and improved survival rates for patients with CML, but it caused many severe side effects due to lower levels of white blood cells being produced to fight infection. However, it was the first drug that killed the fusion gene and brought a CCyR in some patients, leading to the discovery that patients who achieved CCyR lived longer than patients who did not. HSCT was also developed to treat CML successfully but resulted in very high mortality rates. These treatment options were extremely limited. Then Imatinib, the first TKI, was introduced by the FDA in 2001 and this greatly enhanced the treatment options and survival rate for patients with CML (3).
Phase 1: In 2001, a study of 54 patients in the chronic phase (CP) of CML (CP-CML) who had previously failed therapy with IFN-a. They took daily doses of over 300mg of Imatinib, and resulted in 98% achieving a complete haematological response (CHR: no symptoms of CML) and 13% achieving a CCyR. This showed that Imatinib was quite effective in reducing the blast count and was able to reduce the number of fusion genes of a patient in the chronic phase. The dose of 400mg was chosen, as it achieved the optimum concentration in the bloodstream to inhibit the BCR-ABL gene.
Phase 2: this was a study of a larger number of patients who were in various stages of CML. For the 235 patients in the accelerated phase (AP) taking 400-600mg Imatinib daily, 34% achieved a CHR and 82% saw responses. For the 260 patients in the blastic phase (BP) also taking 400-600mg daily, 8% achieved a CHR and 52% saw responses. This showed that Imatinib was more effective in reducing the blast count of patients in the AP compared to the BP, although it is still quite effective. These trials also found that higher doses were more effective in achieving a CHR, so the Food and Drug Administration (FDA) approved the dose of 600mg to treat patients in the AP and BP. For the 454 patients in the CP taking 400mg daily, 95% achieved a CHR and 41% achieved a CCyR. There were very few, insignificant side effects including rashes, diarrhoea, and nausea, and only 2% of patients discontinued the trial consequently. This showed that Imatinib did cause side-effects, but also proved to be considerably more effective in patients in the CP compared to in the AP or BP.
Phase 3: IRIS (International Randomised Study of Interferon and STI571) was a study of 1,106 CML patients in the CP taking 400mg Imatinib daily. The purpose of the trial was to compare the effectiveness of the immunotherapy drug, IFN-a, with the new drug Imatinib. In the initial report, Imatinib achieved a CCyR in 76% patients compared to only 15% of IFN-a patients. Imatinib was also tolerated better, and only 3% Imatinib patients compared to 30% IFN-a patients discontinued because of side effects. After 8 years, the trial concluded that Imatinib was more effective in treating CML than IFN-a because 83% of patients being treated with Imatinib achieved a CCyR, the rate of progression to AP/BP decreased, and the overall survival rate was 85% (or 93% if only CML-related deaths are considered). This trial revolutionised the way CML is now treated, as it introduced TKIs into the treatment options (4).


In recent years, TKIs are becoming seen as less effective, as most patients still have some CML cells after many years of the treatment, and there are many negative side effects. About 40% of patients who have achieved an MMR with Imatinib and 50% of patients who have achieved a MMR with Dasatinib can discontinue their treatment without having another Philadelphia Chromosome. A study by the Nordic CML study group (NCMLSG) discontinued TKI treatment in 132 CP-CML patients who had been treated with either Imatinib, Dasatinib or Nilotinib for 3 years and had an MMR for at least one year. Treatment-free remission (TFR), not needing to take TKIs, is becoming the goal for CML treatment, as it improves the patient’s quality of life, reduces the risk of long-term complications, and reduces the cost of treatment (5).
In conclusion, the treatment options for CML have greatly improved since the 19th century. Data from the National Cancer Institute shows that 65% of CML patients are alive 5 years after diagnosis, which shows a large improvement since the early 1900s, when the treatment options were ineffective and CML was viewed as incurable. However, the TKIs that are used today are noticeably more effective and leads to long-term control of CML without chemotherapy.
Reference: https://www.cancer.net/cancer-types/leukemia-chronic-myeloid-cml/types-treatment https://www.cancer.org/cancer/chronic-myeloid-leukemia/treating/bone-marrow-stem-cell.html https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3243359/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894842/ https://doi.org/10.3324/haematol.2019.242891
By Uma Patel,Lasers: the saviour of recipient and donor twins
Twin-to-Twin Transfusion Syndrome (TTTS) is a rare pregnancy condition, where the blood circulation through a set of monochorionic twins’ placenta is unbalanced, causing major developmental issues in the foetuses (1). This occurs in around 10% of identical twins pregnancy with a shared placenta and blood vessels (2). As the blood vessels in the placenta are shared, there may be abnormally high levels of blood entering one of the foetuses (labelled as the “recipient”), and the other foetus receives lower levels of blood (labelled as the “donor”). This mainly occurs when there is arterio-venous (AV) anastomosis, where the vein of the donor twin that brings back nutrient-rich blood from the placenta is diverted to the recipient twin, causing an imbalance in the placental blood and amniotic fluid transfusion (3). This condition leads to anaemia and organ failure in the donor twin, and the recipient twin may have cardiovascular dysfunction and heart failure due to the higher volume of blood entering it (4).
There are very specific criterias for diagnosing and classifying TTTS. One is that the amniotic sac for one of the twins must be 2cm or less in size (Oligohydramnios), whereas the other twin must have an amniotic sac of 8cm or more (Polyhydramnios) (2). Once diagnosed with TTTS, the classification from the different stages is as follows:
1. Stage 1: The TTTS twins meet the criteria for the abnormal amniotic sac sizes.
2. Stage 2: The donor twin reaches severe anaemia and as a result, the bladder is small and “invisible” due to low urine production to keep the foetus alive.
3. Stage 3: High levels of strain in the recipient twin’s heart as a result of high blood levels.

4. Stage 4: The recipient twin’s heart has a high strain level and leads to heart failure (Hydrops).
5. Stage 5: Death of one of the foetuses.

In Stage 1, the chances of recovery is ~50% if the patient has Arterio-arterial (AA) anastomosis (where there is a connection between an artery from each of the babies). Unfortunately, if the condition has progressed to Stage 2 and the twins have an AV anastomosis or Veno-venous (VV) anastomosis, they have a 80-90% chance of losing one or both of the twins (1,2). The best treatment option for Stage 2 or higher TTTS is Fetoscopic laser photocoagulation, also known as Intrauterine Laser Ablation (1,2).
Fetoscopic laser photocoagulation (FLP) is a procedure where a fetoscope is inserted into the uterus and it acts as a channel for a laser fibre insertion (5). Firstly, local anaesthesia is used and using ultrasound, the fetoscope is monitored as it is navigated towards the recipient twin. The needle in the fetoscope is replaced with a laser fibre and moved around to locate the blood vessels connecting the twins. The laser fibre coagulates the blood vessels to restrain the blood flow through the vessels, ultimately the connecting vessels between the donor twin and the recipient twin are blocked. After around 2 weeks, the excessive amniotic fluid and blood flow in the recipient twin returns to normal, and the blood flow and amniotic fluid in the donor returns to higher values (6,7).
There is a 10-15% risk in using this method, and the three main risks associated with this procedure are:
• Water breaking
• Going into Labour
• Losing one or both twins
Compared to 80-90% chance of losing one or both of the twins, the risk of undergoing this procedure is much smaller, hence it is a much preferred procedure (2). However, there is still only a 65% chance that both twins will be alive after the procedure, and only 80-85% chances of at least one out of the two twins surviving. Furthermore, twin(s) born after undergoing FLP in the uterus have an 11% chance of having long-term neurologic injuries, including cerebral palsy and cognitive deficiencies (1).
References:
1. https://fetus.ucsf.edu/ttts/ 2. https://www.youtube.com/watch?v=XG1fd387vck
3. Couck, I., & Lewi, L. (2016). The Placenta in Twin-to-Twin Transfusion Syndrome and Twin Anemia Polycythemia Sequence. Twin Research and Human Genetics, 19(3), 184-190. doi:10.1017/thg.2016.29 4. https://www.hopkinsmedicine.org/health/conditions-and-diseases/twintotwin-transfusion-syndrome-ttts#:~:text=One%20twin%20%E2%80%94% 20the%20donor%20twin,heart%20and%20other%20cardiac%20complications. 5. https://www.hopkinsmedicine.org/gynecology_obstetrics/specialty_areas/fetal_therapy/fetal-interventions-procedures/fetoscopic_laser_surgery.html 6. https://www.nice.org.uk/guidance/ipg198/documents/intrauterine-laser-ablation-of-placental-vessels-for-the-treatment-of-twintotwin-transfusionsyndrome-interventional-procedures-overview2 7. https://www.hopkinsmedicine.org/gynecology_obstetrics/specialty_areas/fetal_therapy/fetalinterventions-procedures/fetoscopic_laser_surgery.html
By Taanya Shenbaga Kumar, Yr.Ectogenesis:

Is it possible for the rendering of the human womb to become obsolete?

The discovery and development of ectogenesis is beginning to prove that foetuses do not need a living uterus to develop and grow, and the creation of the artificial womb demonstrates how the period that a foetus is gestated outside the body can be prolonged.
Complete ectogenesis means the gestation of a developing embryo, from conception to birth, happens entirely outside the womb. On the other hand, partial ectogenesis can be divided into two interpretations. One interpretation of `partial ectogenesis’ is the transfer of a partially developed embryo or foetus from the female body to an external womb for the remainder of the gestation period. Another interpreted form of partial ectogenesis is that which is used more commonly today, referring to when premature infants are transferred to incubators, to continue their development in a neonatal unit.
Just recently, the Weizmann institute were able to grow mouse foetuses with fully formed organs successfully using ectogenesis. In this new approach, the mouse embryos were removed from their mothers at day 5 of gestation and grown for 6 more days in an artificial womb. This artificial womb included nutrient filled vials, incubators connected to ventilation- which provided oxygen and carbon dioxide to the embryos- resembling the environment of a biological uterus. When day 11 of development was reached, the embryos in the artificial womb became identical to those in the wombs of living mice, where the embryo had grown by tenfold, had blood, a beating heart, and a fully developed brain. (2)
In addition to these recent developments, the Children’s Hospital of Philadelphia has developed a biobag; a way to gestate sheep foetuses, with the bag replacing the placenta with an oxygenator plugged into the lamb’s umbilical cord, filled with an amniotic fluid replacement with which the lamb breathes and swallows. (3)
These research projects across the world are beginning to open many doors to the possibility of artificial gestation and with several benefits, it may be the answer to some of the extensive problems many people face today. According to the NHS, one in seven couples who would normally be able to conceive face difficulty in doing so, and because of this, medical intervention is necessary. (1) Ectogenesis will allow women who are unable to carry their own child, single men, and gay couples to have biological children without needs for a surrogate. This could also improve prospects for infertile women, women born without a uterus or those women who have lost their uterus due to cancer or other medical issues. It would allow them to remove the risks and expectations of pregnancy and childbirth, eliminating commercial surrogacy. Ectogenesis could also boost the survival rates of premature infants to around 22 – 24 weeks by using a sealed biobag which would mimic the maternal womb, with umbilical cord access, and therefore improve the quality of life for these babies.
Medical scientist Dr Nauf Al Bender mentions ‘To this day, morbidity, and mortality rates for premature babies (born before 28 weeks of gestation) remains high. (1) Artificial wombs would transform treatment and grant severely premature babies the ability to better develop lungs and important organs before being brought into the world. However, as revolutionary as human ectogenesis sounds, it also comes with many social, legal, and ethical issues. For example, both parties will be gestating this embryo/foetus in an artificial placenta, meaning they will hold an equal say and share into the child’s life, and this may prove to be a difficult concept when deciding custody rights in a courtroom. Artificial wombs may also further increase the gap between the rich and poor as wealthy parents will lean towards ectogenesis and an artificial womb whereas those who cannot afford this will continue to use women’s bodies to gestate their babies. This may lead to potential discrimination and raises questions such as, how can we prevent invasive publicity and ensure that the patients’ origin stories are not subject to negative publicity and ridicule? If this technology does soon become a reality, who will be liable for injuries or issues in a lawsuit? The manufacturers, the clinics or possibly even the parents? Will artificial wombs receive government funding and who will receive access to subsidies? What thresholds will patients be required to meet? As we enter this breakthrough in modern medicine, we must remember to consider the consequences in terms of government, law, and whether ectogenesis will be safe for our future generations.
By Safaa Patel, Yr.Professionalism’: Why is it necessary in a healthcare setting?
Universally, it is agreed that in any role, whether paid or unpaid, one must conduct themselves in a particular way; most refer to this as ‘professionalism’. The Cambridge Dictionary (2022) (1) defines professionalism as ‘the combination of all the qualities that are connected with trained and skilled people’. On the surface, it is understandable that individuals should remain ‘professional’ during their hours of work; it both ensures the completion of task to the best of one’s ability, regardless of external issues, as well as presenting a positive image of the profession from the perspective of both customers and consumers. However, in a healthcare setting, there is more at stake. It is not just a business; in the UK, one of the most fundamental rights of all citizens is the right to comprehensive service from the NHS, available to all, irrespective of gender, race, disability, age, sexual orientation, gender reassignment, religion, belief, pregnancy and maternity or marital and civil partnership status. For any doctor, dentist or other healthcare provider, adhering to the strict code of professionalism as detailed by The NHS Constitution for England (2021) (2) holds much more importance than merely maintaining an image.
What is the role of a doctor? In the simplest of terms, the role of a doctor is to heal. In reality, the process is a whole lot more complicated. Usually, it begins with a patient feeling unwell, or noticing a strange symptom. Then, they have a choice: either they ignore the issue, or they see a doctor. A vital factor in this decision is the patient’s impression of the medical profession. It is exceptionally important that every patient feels safe in a healthcare environment; just one negative interaction in a healthcare setting could fatally jeopardise the doctor-patient relationship which the NHS relies on in order to provide the greatest possible service to the country. Professionalism ensures that a patient feels comfortable enough to both enter a medical environment and share possibly intimate details with someone who is essentially a stranger. This aids both the diagnosis process and overall public health, therefore necessary to any doctor in order to fulfil their responsibilities to their patients.
On the other hand, irrespective of the patient experience, a clinical environment is nearly always a learning environment. Students attend placements, observe and gather information to both further their knowledge of the field and build on their communication skills. Without a decent role model to follow, there is a risk of complacency within the new generations of doctors, who may receive the message that the patient rights of respect and confidentiality are simply formalities. Ultimately, this learnt complacency is detrimental to patient care, maintaining that it is more important than ever that medical professionals uphold the professional characteristics of integrity, compassion, altruism and a willingness to collaborate within a clinical situation, setting a precedent for all around them Additionally, due to the rise of social media in modern times, now more than ever it is essential for medical workers to maintain the highest standards and behave exactly according to the NHS values. Medical professionals must abide by the rules as exactly as possible in order to acquiesce to the rising demand of accountability in the public eye. Each individual employee has a responsibility to maintain public trust in the healthcare profession; it is imperative that professional boundaries are not overstepped, and each patient is dealt with in an appropriate manner. In the court of public opinion, even the smallest misstep can result in calls for job termination and legal compensation, possibly ruining faith in the NHS and its workers. A medic’s priority is always the patient; causing uncertainty undermines their primary goal, which is to treat the patient. If a patient does not contact a medical professional about their symptoms, how will they be treated?
To conclude, professionalism in healthcare is truly paramount to the fulfilment of the shared values of every worker in the field. Maintaining a respectful and moral standard of conduct creates a safe environment for both staff and patients, ensuring that the service provided remains and continues to be the greatest that it can be for the country.
References:
(1) Cambridge Dictionary (2022) ‘Professionalism’ Available at: https://dictionary.cambridge.org/dictionary/english/professionalism


(2) The NHS Constitution for England (2021) ‘Principles that guide the NHS’ Available at: https://www.gov.uk/government/publications/ the-nhs-constitution-for-england/the-nhs-constitution-for-england
By Khadijah Ahmed, Yr. 13‘
UCD and iMCD: the unknown hematologic killers

Castleman disease, abbreviated to CD, is a range of diseases with the same primary feature of enlarged lymph nodes with abnormal characteristics (1). According to a study conducted in 2017, the 5-year survival period for patients with CD is 80.3%, meaning that amongst the 6500 to 7700 new cases of CD in the USA, only around 1280-1500 people do not live past 5 years after their diagnosis (2,3). A decade ago, a minimal number of treatments were available for this group of diseases. However, recently, the focus on improving the number and quality of treatments has increased due to the input of research from organisations such as the Castleman Disease Collaborative Network (CDCN), the National Organization for Rare Disorders (NORD), and universities such as the University of Pennsylvania (4-6).
Castleman disease has 4 subtypes:
• Unicentric Castleman disease (UCD)
• POEMS-associated Multicentric Castleman disease
• HHV-8-associated multicentric Castleman disease (HHV-8-MCD)
• Idiopathic multicentric Castleman disease (iMCD) (7)

Unicentric Castleman disease (UCD) is a disease that is usually presented as the proliferation of a lymph node or a group of neighbouring lymph nodes. A particular case presentation, called the hyaline vascular variant (when lymphoid follicles are scattered in lymphoid tissue masses with increased proliferation), is seen in most patients diagnosed with UCD(8). Unlike most medical conditions, UCD is found predominantly in younger patients, especially around the age group of 33 years old and below (9). Patients with UCD can be asymptomatic, or, similar to iMCD, be presented with symptoms similar to other conditions, such as mass effects on surrounding organs and/or tissue. For example, a case reported in 2022 shows how a doctor misdiagnosed UCD as a pancreatic mass during a physical examination and after CT, and MRI scans. Due to insufficient information on UCD, a doctor’s ability to give the correct diagnosis is limited to the few facts and symptoms that also clash with other more common diseases. However, the right diagnosis was given after pathological and immunohistochemical tests and biopsies were conducted. (10) Idiopathic multicentric Castleman disease, simplified to iMCD, is a rare disease that attacks the lymphatic system and causes abnormal inflammation of lymph nodes. This disease has features similar to autoimmune diseases and is also shown to occur or be diagnosed alongside autoinflammatory and autoimmune diseases (11). Certain diseases such as rheumatoid arthritis, adult-onset Still disease, and IgG4-related diseases present features that are similar to features presented in iMCD. Therefore, this makes it harder to diagnose the disease as it may be mistaken or misdiagnosed for another similar condition (11,12). Unlike UCD, iMCD does not cause proliferation or other extreme forms of physical alterations in lymph nodes. Therefore, diagnosing this is considerably harder than UCD. Although there are many differences between the two diseases, they are both rare and lethal. Unfortunately, other than the HHV-8-MCD, there are no definite factors that cause the other 3 types of Castleman disease.
References:
1. https://rarediseases.org/rare-diseases/castlemans-disease/ 2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5765290/ 3. https://emedicine.medscape.com/article/2219018-overview 4. https://cdcn.org/ 5. https://rarediseases.org/rare-diseases/castlemans-disease/#:~:text=Castleman%20disease%20describes%20a%20group,when% 20reviewed%20under%20the%20microscope. 6. https://www.pennmedicine.org/departments-and-centers/department-of-medicine/divisions/translational-medicine-human-genetics/ research/castleman-disease-research-at-penn 7. https://www.webmd.com/hiv-aids/castleman-disease 8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5620771/#:~:text=Hyaline%20Vascular%20Variant%20(HV%2DCD,of%20germinal% 20centres%20%5B7%5D. 9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5765290/ 10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8855184/ 11. https://academic.oup.com/rheumatology/advance-article-abstract/doi/10.1093/rheumatology/keac481/6673927? redirectedFrom=fulltext 12. https://rarediseases.org/rare-diseases/castlemans-disease/
By Taanya Shenbaga Kumar,The Long term effects of COVID 19
‘’
By George Gkikas, Yr. 12Long Covid’’ refers to prolonged symptoms following infection with SARS-CoV-2 (COVID-19) that are not explained by an alternative diagnosis (1). Mild or moder-
ate Covid-19 infection symptoms last for approximately 2-3 weeks in most people, but for some, long-term effects can cause long-lasting health problems. For those patients, life is a constant search for treatment, relief and answers.
The more severe and prolonged the initial experience with Covid-19, the greater the risk of Long Covid. Being vaccinated lowers the risk of severe illness and the risk of long-term effects. But more than 2 years into the pandemic, researchers still have very few answers to the long-term effects of covid and their treatments.
The big surprise in Covid is that people who were never that sick in the acute phase still have persistent problems which lower their quality of life. Possible causes of Long Covid:
1) long-term damage from the initial illness such as inflammation in the heart, lungs and blood vessels.
2) Disruption of the microbiome, the trillions of bacteria in our gut that have a wide range of effects on our health.
3) The immune system mistakenly attacks healthy tissue after the virus is gone
4) An immune reaction to remnants of the Covid -19 virus that can remain in the body months after the initial infection.
The most common symptoms of Long Covid are (2): Fatigue, shortness of breath, cognitive problems, loss of smell and muscle ache Fatigue can be described as difficulty with daily activities such as washing and dressing, low exercise tolerance and impaired ability to work, resulting in reduced quality of life (3,4,5). Shortness of breath during physical activity one year after recovering from the infection may indicate a decrease in heart performance (3,4,5) When looking in detail at heart function by cardiac ultrasound, subtle cardiac abnormalities were observed. Cognitive problems were observed in Long Covid sufferers, with the most common being difficulty in concentrating, brain fog and problems finding the right word in speech (4,5) Loss of smell (anosmia) in Long COVID sufferers can be long-term. These patients are three times more likely to be endangered by smoke inhalation, delayed detection of gas leaks and spoiled food. (6,7).
The musculoskeletal system can be affected by Long Covid, causing myalgia, arthralgia, muscle weakness and skeletal muscle damage. These symptoms can persist for months decreasing the quality of life of numerous individuals as these pains can make exercise and other physically demanding tasks difficult. The ‘’cytokine storm’’ a deregulated release of numerous cytokines by the immune system after SARS-CoV-2 infection in the lungs, results in exacerbated inflammation that can promote multiorgan injuries (8).The key risk factor associated with an increased risk in Long Covid included( 9):
· Age- with 1.2% of 20 years old experiencing impacts on daily life and 4.8% of 60-year-olds. Debilitating symptoms are roughly 4 times as common in 60-year-olds than in 20-year-olds
· Being female
· Having poor pre-pandemic mental health and poor general health
· Having asthma
· Being obese Hopefully, as our knowledge of Covid-19 increases, more studies in this field will be developed and the treatment which Long Covid sufferers will receive will rid them of the ailments of Long covid and allow them to be healthy again. References:
1. BMJ 2022;378 DOI https://doi.org/10.1136/bmj-2022-072117
2. Long Covid: Long terms effects of Covid-19- John Hopkins medicine 3. Office for National Statistics Technical article: Updated estimates of the prevalence of post-acute symptoms among people with coronavirus in the UK:26 April 2020 to August 2021
World Health Organisation. A


The

 By Martha Brennan,
By Martha Brennan,
Although, for many of us, everything has returned to normal after the pandemic first started to affect our lives in March 2019, the long-lasting legacy of COVID can still be seen all around, over two and a half years later. So, where can we see this today?
Firstly, the pandemic affected many workers’ physical, mental and emotional wellbeing as they were thrust into the COVID wards of the hospitals, specifically the staff on the medical front lines. It is important to note that this workforce was especially vulnerable to the infection as a considerable percentage of patients have been identified as healthcare workers – this figure was 19% of all cases in the USA (4). General practitioners were the highest risk specialty for deaths among doctors, while the highest risk nursing specialty was mental health (4). Although the number of cases within the healthcare profession is still a minority in the holistic overview of COVID’s effect on the world’s population, a significant proportion of healthcare workers who were infected went on to develop long-COVID, experiencing severe and long-term symptoms, or tragically dying after contracting COVID on the wards (especially in the early days of COVID when there were no vaccinations or even any PPE).
Along with the physical effects of COVID, many experienced emotional suffering (2). This includes constant stress due to the unknown, overwhelming pressure and the frustration of the slow response of the government and consequently the nation. The healthcare profession also experienced an increase of staff with mental health conditions such as anxiety, depression and post traumatic stress disorder (PTSD) that has gone on to affect their daily lives, both work and family related (2). Primarily caused by feelings of isolation and helplessness, it is now reported that just over two thirds of staff (69%) said their ability to do their job was impaired because of the state of their mental health, with 45% of the correspondents meeting the criteria for PTSD (5).
Not only did healthcare workers suffer from the above conditions in this time– the population, both in the UK and worldwide, experienced the same issues as, after all, healthcare workers are only human. As a long-lasting effect of COVID, mental health has become even more important with more self-help services becoming available and more awareness of mental illnesses. An example of this is the enhanced emphasis on the importance of the ‘Britain Get Talking’ campaign which (although it was launched in 2019) has rose in popularity since the start of the pandemic (7). Lower income demographics have been particularly affected by mental health problems, along with young people, disabled people, and people living in more deprived areas. Reduced social interaction and feelings of isolation, concerns about access to healthcare and medication, and financial stress are contributing factors (8).
To further this the effect of COVID has been felt by multiple branches of the NHS such as inpatient and outpatient facilities, care homes, hospices and dental surgeries. Cancer care, which often involves immunosuppressive therapy, tumour resection, and inpatient treatment, has been disproportionately affected by Covid-19. Chemotherapy treatment plans have had to be revised to minimise the frequency of chemotherapy visits and the degree of immunosuppression as, for obvious reasons, a suppressed immune system would cause many complications with the ever-present possibility of contracting COVID (3). Furthermore, elective surgeries, both for cancer and other reasons, had been cancelled due to the high risk of being in hospital during the first wave which has now significantly lengthened waiting lists, angering patients who are currently living in considerable pain or discomfort or with mobility issues. Similar to this issue, appointments and referrals have been cancelled, this is most evident when looking at dental appointments – a major backlog has been caused in the system with many patients not being able to make an appointment (22%) and 17% of patients having had their appointments cancelled completely (9).
In ways good and bad, today’s world has been both temporarily and permanently transformed along with the lives of many people from all over the world. Economies have been damaged, education has been disrupted, over 6,000,000 lives have been lost worldwide (1) and health inequalities have been exacerbated but perhaps the most important and obvious outcomes of the pandemic are the effect on the population’s general health, both physical and mental. References: 1. https://covid19.who.int/ 2. https://www.bma.org.uk/advice-and-support/covid-19/what-the-bma-is-doing/covid-19-the-impact-of-the-pandemic-on-the-medicalprofession 3. https://www.nejm.org/doi/full/10.1056/NEJMms2009984 4. https://gh.bmj.com/content/5/12/e003097 5. https://www.ucl.ac.uk/news/2022/may/how-covid-19-surge-impacted-mental-health-nhs-staff 6. https://www.thelancet.com/journals/lanwpc/article/PIIS2666
Private VS NHS Dentistry
Many people have debated whether they should turn to private or NHS dentistry when in need of particular treatment or simply for their 6-month check-up appointments. But what exactly is the difference between these two? Is private dental care so exceptional that it is reserved solely for those of higher socio-economic backgrounds? And is the exponential growth of the UK population putting a major strain on the NHS?
Firstly, private dentistry is renowned for being pricier but not completely unaffordable for most of the population. Nevertheless, some may argue that the extra money spent could be opening up doors to benefits the NHS just can’t provide. Swapping out the rapid, fast paced dynamic of the NHS, private dentistry offers a slower and more relaxed atmosphere, with appointments lasting up to over an hour depending on the type of treatment being administrated. For example, private treatment ensures that patients not only get the (1) best practical results, but also the most satisfying aesthetic and cosmetic finish. The additional price also increases the freedom and flexibility of materials used as there is no funding restrictions and the focus is put on the quality of treatment. This is because the patient pays for exactly what they want, whether it be porcelain, chrome, or acrylic for their dentures, for example. All treatments are available in private healthcare, despite possibly not being granted by its NHS counterpart. For example, private treatment means that highly popular orthodontic treatments such as Invisalign can be offered to patients; even if not strictly necessary.
A common myth of NHS dentistry is that it is free. Whilst this was originally the case back in 1948 with the birth of the NHS, that pledged to provide free medical and dental treatment “from the cradle to the grave”, this free service quickly collapsed in 1952, and dental treatment was no longer gratuitous. Whilst the government helps to subsidise some of the cost, limits have been established to control treatments offered, to fit within the budget. Consequently, this often means the cosmetic aspect is largely sacrificed to be cost effective for taxpayers. Patients lose some control over their choice of treatments and check-ups, with their treatments also being categorised into bands of treatment, corresponding to the complexity of the treatment required (2). Band 1 treatment (£23.80) (3) includes the most basic of treatments such as a scale and polish, moulds of teeth and orthodontic assessments. Band 2 treatment (£65.20) encompasses fillings, mouth guards and oral surgeries. Band 3 treatments (£282.80) offers bridges, crowns, and dentures. Band 4 emergency treatment (£23.80) covers examinations, x-rays and draining abscesses. However, patients can be entitled to free NHS care if they meet the following criteria (2):
· You are under 18 or are a full-time student under the age of 19.
· You are expecting a baby or have had a baby in the last 12 months.
· You are named on a Tax Credit NHS Exemption Certificate.
· You are named on NHS HC2 certificate.
The advantages and disadvantages of both types of treatments is also another highly debated topic. The advantages of private treatment include a wide range of treatments for all types of dental issues, ranging from fillings to cosmetic treatments. A better patient-dentist rapport is built as more time is spent with the dentist and they can spend more time preventing future problems rather than just curing them. Nevertheless, it is comparatively more expensive than NHS treatment despite the occasional discounts made and there is no exemption to fees; even if you fit the criteria mentioned above that are entitled to free NHS care.
The benefits of NHS dentistry is that the use of the bands means there are fixed prices depending on complexity of treatment and if you came back for more treatments within the same band, within two months, it is included in the cost you paid for the first treatment. There is also more financial help for those pregnant/ in education. On the contrary, NHs dentistry lacks variety and availability as they focus on the health of teeth and gums, not including cosmetic treatment, which is becoming increasing more popular, with an annual 5% rise in these treatments (4). Moreover, due to time restraints, the aim shifts to purely fixing existing problems rather than preventing any future ones as they are under pressure by the NHS to meet targets and quotas set by the government if they are to maintain their constant subsidy from them.
In conclusion, both private and NHS dentistry offer bespoke services to maintain a good standard of public health. As no type of dentistry is considerably better than the other, many people weigh up the pros and cons of both before choosing between them. There are lots of tools to help with the comparison to ease the decision-making process. Overall, as of present, 14.5% of the UK population claim to “prefer private dentistry” and this figure is estimated to increase as the desire for more aesthetics and cosmetic treatments continues to grow.
References:
1.

https://www.harlowdental.com/what-are-differences-between-nhs-and-private-dentistry
2. https://www.bamboodental.co.uk/news/private-dentist-versus-nhs-dentist-which-should-you-pick/
3. https://www.nhs.uk/nhs-services/dentists/dental-costs/what-is-included-in-each-nhs-dental-band-charge/
4. https://www.dentalreview.news/people/60-dental-company-profiles/4378-bacd-rise-and-rise-of-cosmetic-dentistry

5. https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/07/GP-Survey-Dental-Results-Summary-PDF938KB.pdf
By Kelly Chae, Yr. 13Why is there a sudden increase in demand for cosmetic dental treatments?

Cosmetic dentistry is generally used to refer to any dental work that improves the appearance and sometimes, the functionality of the teeth. Cosmetic dentistry procedures are usually elective instead of being essential, however, some treatments also provide restorative benefits. There are some common procedures such as: inlays and onlays, composite bonding, dental veneers, teeth whitening and implants. (1)
Dentistry has changed and developed over the past few years and is continuously doing so. Recently, cosmetic dentistry has become more popular and normalised as there was a sudden rise in the need for cosmetics during the 90’s and this marked the difference between a normal dentist and a cosmetic dentist. There seems to be the same common reason why people want a cosmetic procedure done; that being the desire for a natural and beautiful smile which can not only improve their smile, but their overall appearance. By achieving this, it can improve their confidence massively and maybe even reveal so many more opportunities for them as they were too insecure to reach out for them before.
The rise of social media has contributed to the sudden surge in the demand for cosmetic dentistry. Social media has allowed patients to become more connected with dental professionals and patients commonly seek out dentists that have been endorsed by social media influencers. (2) Social media, with its widespread use, has a great influence on today’s society, as it affects our perception of beauty and aesthetics, hence the view of our physical appearance changes. Thus, the desire for physical improvement increases, which consequently raises the demand for cosmetic intervention. This is especially true when it comes to cosmetic dentistry. Since a smile is deemed as an important factor in determining the face attractiveness, an aesthetically pleasing smile is dependent on tooth position, size, shape, and colour. (3)

Another contributing factor to the increase in demand is Covid 19 and ‘the Zoom boom’. During lockdown, life transitioned from being in-person to an online setting from school lessons to business meetings. During these Zoom calls, people would find themselves looking at their appearance more and analysing their features, particularly their smile. As a result of this, more people wanted to spend the money had saved due to refunded, cancelled, or disrupted holidays. This extra money was put towards dental treatments such as teeth whitening or teeth straightening with an ultimate cosmetic purpose. (4)
Personally, I think the Zoom boom was a minor contributing factor, however, social media and its influence is still the main reason for the rise in demand for cosmetic dental treatments. Most mobile users have at least one social media platform which is where a certain beauty standard is portrayed, and this is what sparks the development of many insecurities in people of all ages. This is where the ‘want’ of an aesthetic procedure becomes a ‘need’. Another reason I think people are starting to want cosmetic dental procedures done is due to all the marketing different brands do to persuade people to buy their products. Some brands claim to straighten teeth with aligners in 3 months or some may even show excellent changes with before and after pictures which would appeal to many potential customers and make them buy the cosmetic products which, in turn, helps the company and brand profit whilst claiming astonishing results sure to boost people’s confidence which would provide cosmetic dentists with an intrinsic reward.
References: 1. https://www.colgate.com/en- us/oral-health/dental-visits/five-types-of-cosmetic-dentistry-procedures 2. https://dentistry.co.uk/2022/06/09/the-history-of-cosmetic-dentistry-over-the-last-25-years/ 3. http://jamdsr.com/uploadfiles/16SocialMediavol7issue5p63-67.20190614051242.pdf 4. https://dentistry.co.uk/2020/09/18/zoom-covid-boosted-interest-cosmetic/
By Safa Khan, Yr. 13Why was poor dental hygiene in the Middle Ages a myth?
It is easy to think of the dreadful images of old-fashioned barber-surgeons pulling teeth out using terrifying instruments called ‘pelicans’ and believe that so much has changed regarding dentistry. However, this is not the case. We may like to believe that dentistry in the Middle Ages was a shadow of what it is today, however, the truth is, it’s more similar than we ever imagined. From anaesthetics to fillings to dental books, dentistry was very advanced in the Middle Ages, condemning beliefs of poor dental hygiene as false.
In the Middle Ages, oral hygiene was far from poor. This is shown through Al Tasrif, the medical encyclopaedia written by an Arabic surgeon called Abulqasis in Córdoba. Within the 30 volumes, he describes the tartar removal methods, emphasising the role of oral hygiene and recommending the use of tooth-cleaning rods and powders. Drawings of devices for removing dental tartar can be found in older copies of Abulqasis’ treatise. (1) Furthermore, Trotula De Ruggiero, who is considered to be the first female physician in the history of the Medieval Medical School of Salerno, reported widely on dental care. She recommended a home-made deep mechanical cleansing and whitening, using a powder of white marble to brush the teeth with, as-well as date’s burn pits, wrapped in wet wool inside a linen rag – their very own medieval toothbrush. Mouthwash was also recommended, in the form of alcoholic ‘good wine’, followed by a daily brush with a clean white rag. As for throughout the day, she recommended a medieval ‘chewing gum’, in the form of aromatic herbs like mint, eucalyptus, fennel and parsley, that were to be chewed on to keep the teeth and gums clean as well as giving a pleasant smell. She also provided a remedy for gingivitis: quicklime, natural sulphur, orpiment and incarcerated pumpkin and pepper. The dust was distributed on the diseased gums, which were previously washed with great mullein roots, boiled with vinegar. Oral hygiene was more advanced than we remember, with a daily brushing routine recommended to all and advancing treatments for disease. (2)
The Middle Ages also saw the beginnings of restorative dentistry, as practiced by Abu Baker Muhammad Ibn Zakaria ar. Razi cured carious teeth with a wool compress dipped into boiling oil or a cauterising iron. By inserting opiate into the tooth, ar. Razi could then fill it with myrrh and a camphor filling is dropped into the root of the tooth. The use of oil to alleviate the symptoms of decayed teeth is still used today, as home remedies involving clover oil and oil pulling are deemed as less conventional natural remedies. Ar. Razi would also recommend drilling open the tooth and filling the tooth with burning oil to get rid of the pain. It is also mentioned in Al-Fahir, that decay is caused by acidic moisture and filling the teeth is necessary to prevent moisture getting to the tooth and to relieve pain. ‘Tancer’ was recommended as a filling material and it’s explained to be a metallic salt that exists with gold or copper on the surface, commonly used by a tin man or plumber. Hollow teeth could also be filled using gold leaf, as recommended by Giovanni Arcolani, a professor of Medicine and Suregry at Italy. This shows that dental hygiene wasn’t poor as clinicians had knowledge of the causes of decay and could treat it similarly to the way in which it’s treated today as this clearly resembles the treatment current dentists use to treat decayed teeth by drilling away the decayed bone and filling the tooth with composite or amalgam. (3)(4)
Dentures, used by Etruscans, were made from human or ox teeth, fixed in by gold rings surrounding the existing teeth. These were one of the earliest examples of golden bridges. In the 14th Century, ‘Guy de Chaulic’ made a noteworthy contribution, as physician to the Pope, as he gave several guidelines for the care and cleansing of teeth in order to prevent decay. He advised to replace lost teeth using other human teeth or artificial teeth made up of bone. (4)
However, it seems that not everybody had good oral hygiene in the Middle Ages, as a study of deciduous-tooth wear in children living in the Middle Ages concluded that the frequency of tooth wear caused by caries was over 50% for the sample. The frequency of this increased with age, as without a good oral hygiene routine, teeth do decay and wear down. (5) In another study on the frequency of dental caries in the Middle Ages, it’s shown that caries were present in 74.9% of the population. Caries is decay of the teeth, caused by a build-up of acid which can be prevented by a good oral hygiene routine. The prevalence of bone loss and dental caries clearly shows a lack of good dental hygiene. (6)
Furthermore, although many of the dental practices in the Middle Ages had some reasonable justification proven by modern science, nothing can justify the belief of the tooth worm. The tooth worm was believed to cause caries and al-Gazaar recommends purifying it using mustard, henbane, and a dog’s tooth. Avicenna also stood by henbane fumigation to get rid of tooth worm. His method consisted of taking four grains of henbane and leek seeds, kneading them with two onions and goat fat until they’re smooth, making pills from it and burning the pill under the patient’s head is completely rooted in superstition rather than a scientific method. Guy Chaulic also suggested burning hyoscyamus seeds on charcoal so the worms would ‘fall off’. The belief of the tooth worm could have negatively affected oral hygiene, as physicians would turn to less conventional methods of treatment rather than the modern procedures. (7)
In conclusion, dentistry was fairly advanced in the Middle Ages, as good oral hygiene practices were recommended, and the beginnings of restorative dentistry had begun. Dentistry in the Middle Ages laid the foundation for the work of Paré and Pierre Fauchard, who is considered to be the Founder of Modern Dentistry as he authored Le Chirurgien dentiste in 1728, which was the first scientific book dedicated to the topic. Fauchard recommended washing the mouth every morning and rubbing with a wet sponge, using ethanol and water as a cleaning solution. He recommended using a sponge rather than a cloth so as not to disturb the teeth and rub too hard. I believe that without advancements in the Middle Ages, dentistry could not have progressed so rapidly in the Renaissance. (8) References: 1. The development of dentistry, 1000–2000 - The Lancet 2. https://www.nature.com/articles/sj.bdj.2016.528
By Humairah Thagia, Yr. 13

Antibiotic resistance and its effects in Dentistry
Antibiotic resistance is one of the biggest challenges facing modern medicine and global health.
From the discovery of penicillin by Sir Alexander Fleming in 1928, all the way through to the most recent innovations, antibiotics have proved essential in improving healthcare and saving lives (1). Therefore, antibiotic resistance poses a significant threat to human health as this growing resistance will have severe repercussions for patients around the world.
Effective antibiotics are prerequisites for both preventive and curative measures in protecting patients from potentially life-threatening diseases and ensuring invasive procedures, such as surgery, can be carried out at low risk. Bacterial resistance occurs due to a random mutation in the DNA of individual bacterial cells (2). This mutation protects the bacterial cell from the effects of the antibiotic and so the bacteria now becomes antibiotic resistant (3) - this is evident through a growing number of infectious such as pneumonia and tuberculosis which were previously treated with antibiotics now becoming harder to treat as the antibiotics used to treat them become less effective.
There are two main ways to help slow down or prevent the growth of bacterial resistant strains: Only use antibiotics when prescribed by a health professional and always finish the full course of antibiotics to kill the bacteria. According to UNICEF it is recorded that dentists are responsible for over 10% of antibiotic prescriptions, so a dental professional has a clear responsibility to engage, commit and contribute to global, national and local efforts to tackle resistance (4).
For patients with a spreading dental infection, effective antibiotics are vital. However, overuse and over prescription of antibiotics by dentists has been widely reported as a UK study found an 80% rate of unnecessary use of antibiotics for treating acute dental conditions (5). Infections that are resistant to antibiotics therefore pose a serious risk to dental patient safety. Furthermore, ensuring access to the right care for the patient at the right time is critical in reducing antibiotic use as patients needing to wait for access to the right care often receive more antibiotics than they normally would if the care was immediately available (6). For example, a UK based clinical audit found 40% of children awaiting extraction of infected teeth under general anaesthetic received antibiotics (7).
So how can a dental team increase their efforts towards tackling antibiotic resistance? According to the FDI world dental federation, the three key areas for the dental team contribution in an effort to tackle antibiotic resistance are: awareness raising, infection prevention and control and optimising the use of antibiotics (stewardship).
To raise awareness, the FDI encourages the development of educational programmes and also strongly encourages dentists to provide the necessary information for their patients regarding antibiotic resistance.
For infection, prevention and control, the FDI acknowledges that along with antibiotic stewardship programmes, infection prevention and control programmes should be implemented.
For antibiotic stewardship, the FDI encourages and supports the national dentistry association to actively engage in their antimicrobial resistance national action plan framework and to implement antibiotic stewardship programmes in dentistry at local and national levels. (8)
In conclusion, organisations and practises providing dental care are responsible for creating an environment for appropriate management of patients. To limit the spread of antibiotic resistance certain guidelines have been put in place from educational systems to national action plans. However, ultimately, we are all responsible for using antibiotics only when necessary.
References:

1, Antibiotic resistance in bacteria - natural selection and evolution - BBC https://www.bbc.co.uk/bitesize/guides/zpp74qt/revision/5
2, https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/mutation-and-selection/

3, World health organisation - antibiotic resistance https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
4, UNICEF - time is running out - a technical note of antibiotic resistance https://www.unicef.org/documents/time-running-out
5, Cope AL, Francis NA - antibiotic prescribing in UK general dental practise https://onlinelibrary.wiley.com/doi/abs/10.1111/cdoe.12199
6, The impact of dental caries and its treatment under general anaesthetic https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/09/HospitalDentistryReport-Sept21j-1.pdf
7, House of commons, Health and social committee. Oral evidence: Antimicrobrial resistance https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/962/962.pdf
8, FDI world dental federation - Antibiotic stewardship in dentistry https://www.fdiworlddental.org/antibiotic-stewardship-dentistry
By Akshat Kamath, Yr. 12Tooth whitening procedures: are the risks worth it?
Tooth whitening procedures are one of the most frequently practiced and requested dental procedures by the public worldwide, especially in the United Kingdom. The public is more demanding of whiter, more perfect smiles and as a result of this, many different options of tooth whitening has been made available. From products such as whitening toothpastes and gels, to highly concentrated bleaching agents being applied to teeth under professional supervision, the possibilities of achieving a bright white smile are endless. However, we must consider whether the harmful side effects that come with this type of treatment are really worth it?
The “natural” white colour of teeth is often compromised due to stains accumulated over time from wine, tea, coffee, smoking, etc. [1]. Whitening formulations for home use (e.g., toothpastes in combination with toothbrushes) and professional use in the dental practice (e.g., bleaching or professional dental cleaning) try to address this problem. In this context, whitening is defined as any means to increase the visual whiteness of a tooth. Additionally, an increasing number of oral care products also tend to focus on teeth whitening. Lifestyle habits like smoking or consumption of red wine or black tea can lead to darker teeth [2]. However, it must be acknowledged that tooth colour in general also depends on age of the tooth [3].
A study published in the BDJ about the dangers of using over the counter teeth whitening products found that sodium chlorite, the active ingredient found in three over-the-counter products, could, in the presence of acid, 'significantly reduce the hardness of the teeth and increase the likeliness for future surface abrasions of the teeth.’ [4]
Furthermore, some risks to teeth bleaching also include; sensitivity, gum irritation and technicolour teeth. Teeth whitening procedures such as bleaching may cause an increase in the sensitivity of your teeth to temperature, pressure and touch. This could be a result of high concentration bleach or hydrogen peroxide being used in the clinic. Excessive tooth whitening may also damage enamel and exposed dentin.
To conclude, although tooth whitening is a commonly used procedure which has visibly aesthetic short-term results, the long-term damage it may cause to your teeth is often irreversible.
References:
1. Joiner A. Whitening toothpastes: A review of the literature. J. Dent. 2010;38(Suppl. 2):e17–e24. doi: 10.1016/j.jdent.2010.05.017.
2. Silva E.M.D., Maia J.N.D.S.M., Mitraud C.G., Russo J.D., Poskus L.T., Guimaraes J.G.A. Can whitening toothpastes maintain the optical stability of enamel over time? J. Appl. Oral Sci. 2018;26:e20160460. doi: 10.1590/1678-7757-2016-0460
3. Algarni A.A., Ungar P.S., Lippert F., Martinez-Mier E.A., Eckert G.J., Gonzalez-Cabezas C., Hara A.T. Trend -analysis of dental hard-tissue conditions as function of tooth age. J. Dent. 2018;74:107–112. doi: 10.1016/j.jdent.2018.05.011
4. [Greenwall-Cohen J, Francois P, Silikas N, Greenwall L, Le Goff S, Attal J P. The safety and efficacy of 'over the counter' bleaching products in the UK. Br Dent J 2019; 226: 271-27

 By Zahra Shahzad, Yr. 13
By Zahra Shahzad, Yr. 13
There are currently 105,754 patients in the UK on the national transplant list. 17 people die every day in the UK waiting for an organ transplantation that could have saved their life. The sheer number of patients awaiting organ transplantations has led to the opinion that the criteria needed for an organ transplantation should be reassessed to ensure that precious organs are not misused. (3)
The criteria considered when an organ is in process for transplantation has been a highly debated topic in recent years, with many people arguing that individuals should be more eligible for an organ transplantation than their peers, due to certain circumstances, such as age. However, should committees start considering the morals and beliefs of potential recipients in the face of the current organ shortage?
It is already a precedent that doctors should choose the best match when considering options for an organ transplant. The patient with the best chance of a successful operation should be granted priority in receiving an organ, and doctors often must make hard choices to deem who would be more likely to survive the surgery; and for how long.
Patients are prioritised for donations depending on:
· Their urgency status
· Their blood type (and how closely it matches the donor’s)

· The donor's weight and height are compared to the recipient

· The level of risk at which the recipients’ antibodies may react negatively towards the donated organ
· Longer travel time can have an adverse effect on heart function, so it's important to reduce the distance between donor and recipient.
· Once the above factors have been considered, how long the patient has waited is considered. (1)
Whilst these continue to remain the reasons behind deciding when it comes to recipients, it could be argued that morals and beliefs should be an important considering factor when deciding the receiver of an organ transplant; the common vote may decide that an old man with kidney failure is more deserving of an organ transplant than an abusive alcoholic. Whilst the old man may have a shorter survival rate, the future of the abusive alcoholic may cause more distress to the people around them and therefore be more of a liability in the long term of the operation. (2)
However, it is also important to consider the potential of recipients; it’s possible that the alcoholic could change their ways, and it wouldn’t be fair to compromise a possible life based on one’s own judgement. Therefore, organ transplantation is such a sensitive topic, and why committees are told to overlook more personal details of potential recipients when coming to a decision on who should receive the organ. Committees should be objective and hopeful that recipients will make the most of their new future. In conclusion, whilst organ transplantation will most probably persist as quite a controversial topic in future, it remains a fact that the moral background and personal beliefs of a patient should never be a subject of issue in any medical setting. Healthcare professionals should take care to stay objective throughout their time in the hospital, and the current criteria for organ transplantation does not seem to require any radical changes; for now.
References:
1. https://www.nhsbt.nhs.uk/organ-transplantation/heart/receiving-a-heart/how-does-the-offering-system-work/
2. https://www.cbc.ca/news/health/organ-donation-ethics-how-doctors-decide-who-gets-a-transplant-1.2936439
3. https://www.organdonor.gov/learn/organ-donation-statistics
By Rukaiyya Anas, Yr. 13Should organ transplantation committees consider a patient’s morals and personal beliefs when choosing a recipient for an organ?
How has Medical Law affected how patients are treated today?
In January 2009, the Labour Government introduced the NHS constitution for England, where patients were told they had 25 rights which included areas search as access to health services; quality of care; access to nationally proved treatments; respect; consent; confidentiality; informed choice; involvement in their own healthcare and complaint and redress. It was claimed it brought together “in one place for the first time in the history of the NHS what staff patients and public can expect from the NHS”.
Although this was a significant development in British healthcare, it was not the first endeavour to formulate a list of patient’s rights. From the 1960s, organisations such as Patient’s Association, the Customer’s Association, and the Community Health Councils claimed to represent the patient with concerns about a patient’s access to information, their ability to complain and the presence of medical students during consultations and treatments. (1) Two case studies have been included below to highlight that medical law and courts today endeavour to act in the best interests on the patient even if the patient refuses consent.
Re W (A minor) (Medical Treatment: Court’s jurisdiction) [1992]
In this case, a young girl, aged 16 was suffering from anorexia nervosa and was placed in a specialist adolescent unit. As her conditioned worsened, it was proposed that she be transferred to a unit that specialised in the treatment of eating disorders, but she refused. The Family Law Reform Act 1969 gave her the power to refuse consent to medical treatment and stated that the court could not override her wishes. However, the judge rejected this submission adopting the view of Lord Donaldson of Lymington MR in Re R (A minor) (Wardship: Consent to Treatment) [1992] that if a child was competent to consent to treatment but refused this consent, the court had power to override the wishes of the child and consent to treatment. He held the court needed to strike a balance between taking into consideration the wishes of the child and the harm the child would be exposed to if her continued control of diet was lengthened into a chronic state that would influence her intellectual development and the development of her reproductive organs. The child appealed. On the appeal against the decisions, it was held if the child's welfare was threatened by significant risk to her life or irreparable damage to health, the court should intervene and override child’s refusal of treatment, see Re E (A minor) (Wardship: Medical Treatment) [1992]. The Judge found the child was of sufficient understanding to make to make an informed decision. Before the Court of Appeal, it was acknowledged and accepted it was a feature of anorexia nervosa that it had the capability to destroy the ability to make an informed choice; it was doubtful whether the judge was right to conclude that the child was of sufficient understanding to make the informed decision. However, the judge was correct to order, at the time the matter was put before him, that the child be moved to an eating disorder unit against her wishes. (2)
Re P (Medical Treatment: Best Interests) [2004]
In this case, a 16-year-old patient at an NHS trust hospital suffered from a hypermobility syndrome which could lead to serious bleeding. Doctors advised a blood transfusion should take place if bleeding was to occur, but the patient also refused consent. He explained, as a Jehovah's Witness, his religion forbade blood transfusions, a decision his parents had agreed with. Later, he suffered a ruptured aorta which could have been fatal if his condition deteriorated, and no blood was administered. The hospital sought a declaration from the court that it would be lawful to administer blood to the patient against the patient’s wishes and those of his parents’ if his condition became life-threatening. The court agreed to make the order but added the blood was only to be administered if no other form of treatment was available. The court’s primary duty and concern is to ensure that the child survives until the age of majority. However, it should be careful when refusing to adhere to the wishes of an older child: the older the child, the more respect should be given to their wishes, especially if their wishes on a particular treatment would only delay inevitable death for a short period of time.
The case highlights the court was reluctant to allow even a mature and capable older child to refuse life-saving treatment but in this case, it was designed to respect the patient's wishes by only allowing the administration of blood as a last resort. (3)
Health and Care Act 2022


This Act was given royal assent in April 2022, making it the most recent to affect how patients are treated today. The changes brought about by this Act include targeted changes to public health, social care and the oversight of quality and safety. The fact that the Act puts emphasis on integrating care suggests it will lead to improvements in the population health as well as the patient experience, especially for those living with multiple conditions. However, the Act can only achieve so much by establishing a framework that allows services to collaborate to better meet patients’ needs. In practice, this will take time and depend on how effectively local organisations, leaders and clinical teams are able to work together to implement these alterations to see a more positive change to how patients are treated today. It is significant they are permitted time to make a success of this. (4)
References:
1. Patients´ Rights and the National Health Service in Britain, 1960s–1980s - PMC (nih.gov)
2. Re W (A Minor) (Medical Treatment: Court's Jurisdiction) - Case Law - VLEX 804572145
3. Re P (Medical Treatment: Best Interests) - Case Summary - IPSA LOQUITUR
4. The Health and Care Act: six key questions | The King's Fund (kingsfund.org.uk)
By Fatima Ghanchi, Yr.Common medical interview questions: Can you answer them ?

1. Why do you want to be a doctor? 2. What makes a good doctor? 3. Which quality do you think is the most important in a doctor? 4. What qualities do you have that mean you will be a good doctor? 5. What do you feel are the good and bad points about being a doctor? 6. How would you balance your outside interests with studying a degree? 7. How do you cope with stress? 8. What are your best and worst qualities? 9. What responsibility do you have? 10. What do you think will be your greatest challenge in completing medical school or learning how to be a doctor? 11. What will you do if you are not accepted to medical school? 12. Do you read any medical publications? 13. Tell me about any medical advances and issues you have heard about recently. 14. What is the difference between primary care and secondary care?
Common dental questions: Can you answer them? 1. Why do you want to do dentistry? 2. What are the pros and cons of dentistry? 3. What do you want to specialise in? 4. Why would you work in a dental practice? 5. Do you have any insight into the field of dentistry? 6. Why would you want to be a dentist in a hospital? 7. In what ways do your personal struggles affect your work? 8. Tell me an interesting fact about dentistry you learned recently. 9. How would you address an unhappy patient? 10. Do you think your own dentist is good at communicating with patients? 11. What can you tell me about preventative Dentistry? 12. What is Orthodontics? 13. Why do dentists recommend the fluoridation of water supplies? 14. What are the arguments against fluoridation of water supplies? 15. How would you organise a campaign to improve dental health? 16. How are NHS dentists funded? Is it the same for GP’s? 17. Should dental treatment be free on the NHS? 18. What articles have you read recently about Dentistry? 19. What can you bring to this Dental School?
