
6 minute read
The CRY Centre for Cardiac Pathology has transformed our understanding of YSCD
By CRY Chief Executive Dr Steven Cox
This is CRY’s 25th anniversary year. CRY was founded in 1995 to prevent young sudden cardiac deaths and to support families after a tragedy. One of the areas where CRY has transformed the way we understand young sudden cardiac death is through establishing and funding the CRY Centre for Cardiac Pathology. As well as helping families after a tragedy, it has resulted in CRY funded research which has changed policy and medical practice throughout the world.
In 2008, the CRY Centre for Cardiac Pathology (CRY CCP) was launched with donations of £175,000 in memory of Sebastian and Howard English.
The CRY CCP is an international cardiac referral centre. The service is led by expert cardiac pathologist Professor Mary Sheppard, with a team of staff funded by CRY. Young sudden cardiac death is often the first symptom of a cardiac condition and specialist pathology is required to identify the disease and bring the genetic implications of a potentially inherited disorder to the attention of relatives. When a cause of death is “unascertained” and the deceased is aged 35 or under, the centre will provide a free, fast-track cardiac diagnostic service.
More than 80% of UK coroners are now routinely referring to this centre when there is a young sudden cardiac (or unascertained) death. The centre is also increasingly being referred autopsy material suitable for genetic testing which is becoming so important to correlate with the cardiac findings to further help the family understand the cause of death. CRY aims to remove the unnecessary suffering of the family by reducing the wait to know what has caused the death.
As well as helping a family understand the cause of death, expert cardiac pathology not only informs a family that first-degree relatives need to be screened, but also informs the type of screening the families require. If the investigations report a SADS death, then the family should be offered a series of cardiac tests including an ECG, echo, exercise test, holter monitor and an ajmaline (provocation) test to help identify ion channelopathies. However, if the microscopic pathological investigations show a structural problem (by identifying myocardial disarray), then the family should be offered an MRI instead of the ajmaline test. This will help to identify structural heart conditions like cardiomyopathies.
Establishing the CRY centre was essential as:
• Families were not being given a clear cause of death when a person died suddenly. Initial post-mortem investigations just need to exclude foul play/criminal activity.
• Coroners did not have the funding to conduct additional post-mortem investigations. The initial post-mortem cost less than £100, whereas an expert cardiac post-mortem would cost more than 10 times this.
• When an expert pathologist was asked to provide an opinion it could take up to 2 years for the investigations to be completed.
• There was a low awareness of the implications and importance of family screening for relatives who may also be at risk, if the cause of death was due to a genetic condition.
The CRY CCP has been supported with significant donations in memory of Hannah Turberville and many other young people, including more than £700,000 donated since 2008 in memory of Sebastian and Howard.
This has resulted in thousands of bereaved families receiving the support and information they need. Now, at the CRY CCP, a full expert cardiac post-mortem report will have been issued within 2 weeks of receiving the referral. The report also ensures the family will have a better understanding of the cause of death and the clinical information that will inform the way first-degree relatives are tested for the same inherited condition. Furthermore, the funding the CRY CCP has received has led to vital research which has transformed the way we understand young sudden cardiac death, impacting international guidelines for how these deaths should be investigated and reported.
More than 2,500 expert cardiac post-mortems on young people (aged 35 and under) have been conducted by Professor Sheppard’s team at the CRY CCP. In 97 (4%) of these investigations it was concluded that the cause of death was due to arrhythmogenic right ventricular cardiomyopathy (ARVC). This conclusion of ARVC was a different cause of death to the one identified at the initial post-mortem. Prior to the investigations the cause of death was sudden arrhythmic death syndrome (SADS), with possible negative repercussions on family screening. This is because first-degree relatives may have been investigated with the wrong sets of cardiac tests, since vital information about the post-mortem was lacking. We have found that arrhythmogenic cardiomyopathy is now more frequently diagnosed compared to hypertrophic cardiomyopathy in our database.

Professor Mary Sheppard at the CRY CCP in 2014.
More than 10 years of funding the CRY CCP has resulted in the largest database of expert cardiac investigations of young sudden cardiac deaths in the world. This has enabled ground-breaking research which has transformed the understanding of young sudden cardiac death in the UK and abroad.
Recent papers have reported:
• Athletes with ARVC are 6 times more likely to die during exercise than athletes with other cardiac conditions.
• ARVC is the strongest predictor of death during exercise.
• ARVC is a condition which affects both ventricles, not just the right ventricle – this is essential for investigating firstdegree blood relatives with the inherited condition.
• The incidence of sudden cardiac deaths due to ARVC is significantly higher in athletes compared to the general population.
• In 78% of deaths caused by hypertrophic cardiomyopathy there are no symptoms prior to death and in most sudden death victims the diagnosis was made only at the post-mortem examination.
• SADS deaths are the leading cause of young sudden cardiac death.
• 80% of SADS deaths occur at rest or during sleep.
• 90% of SADS death occur with no prior symptoms.
• In 13% of SADS deaths it is possible to identify the gene(s) which caused the death.
• We have helped to establish international guidelines for how post-mortem investigations should be conducted after an unascertained or young sudden cardiac death.
Since 2008 Professor Sheppard has contributed to more than 100 journal articles about cardiac pathology and been awarded international recognition. She was recently appointed president of the Association for European Cardiovascular Pathology. Professor Sheppard also leads important research projects in the field. She has been invited to lead in Cyprus on the investigation of young sudden deaths, and collaborates with groups in Denmark and Holland who are doing similar work. The research is also identifying undiscovered, significant findings, like idiopathic fibrosis in the heart (areas of scar in the heart with no clear cause) and idiopathic left ventricular hypertrophy (muscle thickening) – possibly a novel cardiac condition.
In 2018, the World Health Organisation released the new ICD codes (International Classifications of Disease). In the latest ICD codes both SADS and ARVC were identified as important causes of death and given their own specific ICD codes. Without question the work conducted at the CRY CCP and the research published by the centre has played an instrumental role in highlighting the importance of cardiac pathology and these specific conditions. This has resulted in these new ICD classifications, which will have a major impact on recognising the importance of these conditions and finally allow data to be gathered to influence policy and practice in the years to come.
For more information on the CRY CCP, go to www.cry-ccp.org.uk
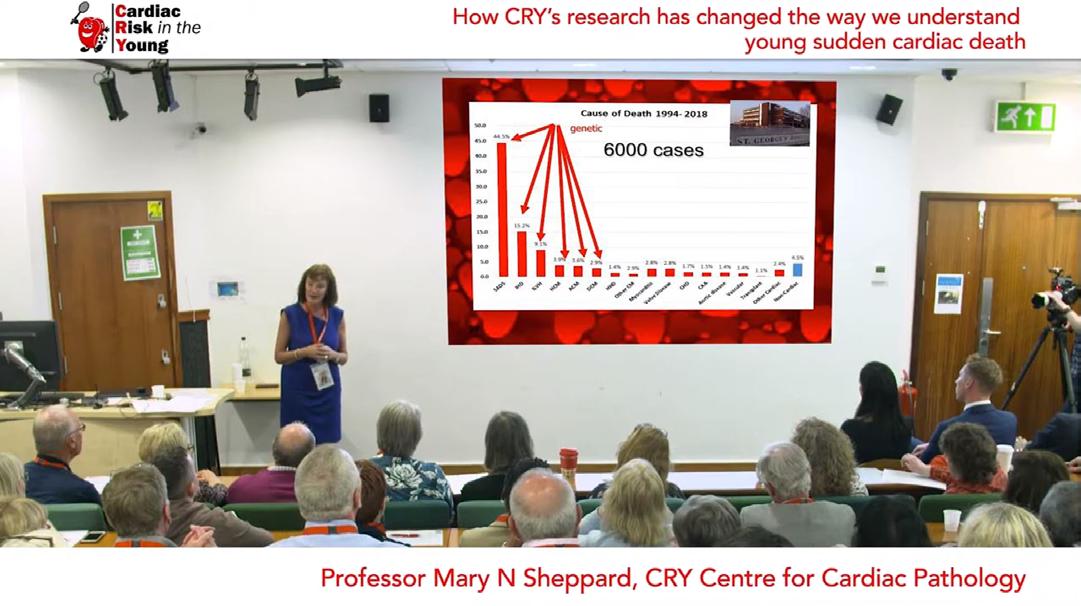
Professor Sheppard presenting at CRY's Family Research Day.
To watch Professor Sheppard’s presentation about how CRY’s research has transformed our understanding of the causes of young sudden cardiac death, go to bit.ly/3aiOEky






