CARE ENGLAND Savings, Solutions, and Sustainability

Understanding workforce data
How to retain talent
A matter of life and limb
Foot care in care homes
In a spin
The hidden costs of in-house laundry



The hidden costs of in-house laundry

Save thousands of £ each year and halve the time spent in your kitchen.
Over 200 nutritious meals made with sustainably-sourced ingredients
Easy to order, store, cook and serve
Guaranteed nutrition and safety: our meals are tested in our onsite laboratory



Caters to every taste, dietary and cultural preference including dysphagia, dementia and malnutrition
No need for a chef
TobookaFREEtastingcall0808 239 2399orvisit carehomes.apetito.co.uk


Welcome from CQC
James Bullion CBE shares the latest updates from the regulator regarding the new assessment framework.
Money saving updates
The Care England team shares its pick of offers and saving opportunities not to be missed.
In the hot seat: An interview with Tandeep Gill, PainChek Find out why investing in digital solutions, such as Artificial Intelligence, could really pay off in the long term.
Data to aid workforce retention
Jim Thomas, a Social Care and Health Workforce Expert, explores what data can help, what data to ignore, how to spot a trend and how non-numeric data can help to retain the workforce.
Member spotlight: National Care Group National Care Group has achieved considerable expansion and completed numerous acquisitions. National Care Group’s Commercial Director, Mike Ranson, tells us how it has achieved that growth.
Holiday pay: The importance of getting it right
Care providers have become familiar with hiring staff on flexible contracts but the law surrounding holiday pay and how to calculate it can be complex. Catherine Meenan, an Associate at Weightmans LLP, explains the law changes and what to consider.




How to… Refurbish a care home on a budget
Jay Dodhia and Palvi Dodhia, Founders of Serene Care Ltd, share their top tips for how to plan for a refurbishment and save costs.
Foot health: A matter of life and limb
Leona Calderbank, Co-Director of Care Home Podiatry, shares what care providers must consider about foot health and explains how best to support people.
Legal matters
Ramjeet Kandola and Laura Jordan, Partners at Anthony Collins Solicitors, explain what providers can do to prepare for challenging fee negotiations.
The surprisingly high hidden costs of in-house laundry
Helene Jones, UK Head of Care Homes at Elis, explores some of the hidden factors driving the benefits of moving in-house laundry to a professional outsourced laundry service.
Members' voice: Your questions answered Care England provides the answers to support providers on the Energy Savings Opportunity Scheme and CQC Assessment Framework, and also updates on workforce and immigration policy.
14 Charlotte Lezard Policy and Public Affairs
15 George Appleton
Head of Policy, Care England












EDITORIAL



editor@caremanagementmatters.co.uk
Editor: Olivia Hubbard
Content Editor: Aislinn Thompson
PRODUCTION

Designer: Ruth Keating, Director: Lisa Werthmann
Studio Manager: Jamie Harvey
ADVERTISING
13
Advertising Manager: Aaron Barber aaron.barber@caremanagementmatters.co.uk
James Bullion CBE, Chief Inspector of Adult Social Care and Integrated Care at the CQC, shares the latest updates from the regulator regarding the new assessment framework and explains what providers need to consider in 2024.
2024 brings with it a year of new approaches for CQC. By the spring, all regulation will be done against our new assessment framework. This includes our assessments of how local authorities are performing against their duties under Part 1 of the Care Act.
Assessing local authorities and integrated care systems (ICSs) represents the largest extension of our regulatory responsibilities in over a decade. It offers an opportunity for us to see and present a more holistic view of the system and the services within it.
We will be able to look across a whole system to see the journeys that people have to navigate to access health and social care. The aim of our local authority assessments is to increase transparency and local accountability. Also, to make good practice, positive outcomes and outstanding quality easier to spot locally and share nationally.
We’ll start to roll out our full assessments of local authorities during 2024. We're using the learning from our five pilot assessments to inform our full approach and will carry on

developing and refining this throughout the year. Our updated guidance gives an overview of our plans, including the evidence we'll be using and how we'll collect it. Our new framework will help us determine during these assessments where commissioning arrangements are facilitating the meeting of needs and sustainability of care – also a ministerial priority for Government. We expect to see an authority level approach to this in terms of both cost and environmental sustainability.
In addition to the system-level assessments, our new assessment framework is being rolled out to all providers in England. Colleagues in the South were the first to be assessed under the new framework and providers across the remaining regions will all have moved across by March 2024. We have produced support and guidance to help you prepare for these changes.
One key message I’m keen to share is that these changes are really about how we are assessing services. What we’re looking at remains much the same. The regulations haven’t changed –and our job remains to ensure
that health and care services provide people with safe, effective, compassionate, high-quality care. We’ll also continue to encourage those services to improve. The framework is very much about a person’s experience of care. Our ambition is always to regulate through the eyes of people who use services and those who care for them.
The new regulatory approach is designed to be more responsive, streamlined and flexible. New online systems will help provide greater consistency. The new provider portal’s simpler processes and easier contact methods support the ability to change a rating more quickly when you improve. The new framework contains quality statements that will help individual providers and systems alike focus on their improvement, innovation and sustainability.
In our most recent State of Care report, we are vocal about how sustained work on social care reform to make the system fairer, along with an industry level workforce strategy, is in everyone’s interests. Our report noted that the increases in the cost of living mean some providers are struggling to pay wages in line with inflation. In some instances, people are reducing their care packages because of price rises. Coupled with local authority budgets failing to keep pace with the rising costs and increases in numbers of people needing care, risks of ‘unfair care’ are elevated.
We have big ambitions and responsibilities to deliver through our regulation. And supporting the sustainability of the social care sector through our regulatory activities and sharing examples of good existing practice across the country support that.

HC-One has taken a significant step in its innovative digital transformation journey through a collaboration with Radar Healthcare to enhance resident care across its 260+ homes in England, Scotland and Wales through a new and improved reporting system.
Radar Healthcare’s system has been integrated into HC-One care homes as a key component of their digital care programme, reflecting HC-One’s commitment to cultivating a culture of organisational learning.
By incorporating Radar Healthcare’s software, HC-One is at the forefront of the care sector, not only identifying potential concerns as early as possible but also supporting the practical implementation of valuable insights and improvements. This approach enables HC-One to thoroughly analyse data related to incidents, audits, and feedback, and use these as learning opportunities to improve the quality of care provided to residents.
With over 19,000 colleagues delivering exceptional care to more than 13,400 residents across the UK, including specialised care for dementia and nursing needs, the partnership between HC-One and Radar Healthcare has all the tools to drive continuous improvement and shared learning throughout the entire organisation.

HC-One has streamlined its operations by implementing Radar Healthcare as its central system for risk management. This roll out is across it’s entire portfolio of 260+ care homes which collectively care for over 13,400 residents.

Data is delivered in an insightful way through Radar Healthcare, ensuring residents receive the best possible care and quality of life.

By integrating medication management, digital care plans, and Radar Healthcare’s event reporting and learning system into one platform, HC-One is at the forefront of technological advancement in the industry.

HC-One deliver around 7 million care interactions a year, which its teams can more effectively evaluate, build from and share learnings on thanks to Radar Healthcare.
Agency staff are less reliable and more expensive and with one in 10 care jobs now unfilled, recruiting isn’t easy. With the average care employee working 31 hours a week, care providers require more staff than other industries to fill the same number of shifts and the average care home would only need each member of staff to work one extra shift every three weeks to eliminate their demand for agency staff.
On-Demand Pay is an employee benefit that allows staff to access their income as they earn it, without impacting provider cashflow or payroll processes. By rewarding hard work instantly, you incentivise shift uptake because people are far more inclined to work for a more immediate reward. This motivates staff to pick up more hours and has reduced the number of unfilled shifts by 62% for some providers – even if the actual rate of pay is the same. In fact, combined with its ability to attract staff and halve staff turnover, it can significantly reduce your agency spend in a matter of weeks. These benefits explain why many of the biggest providers and the NHS already offer it and if we want to compete as an employer, we have to offer the same benefits!
Richard Ayres, Care England. Email: rayres@careengland.org.ukAt times, we need to spend a little to make savings. Below are five ways where very significant savings or return on investment can be achieved to solve some of the most critical challenges faced by care providers, namely workforce recruitment and retention, increasing care fees from public funders, wastage and freeing up care workers' time delivering care to a higher standard. These five solutions offer either significant savings, increased efficiency, or increased fees.
CareCubed is the national care costing tool used by over 500 providers and 60% of councils to benchmark costs and create a fair and sustainable care market. Care England has negotiated a sizeable discount for care providers on behalf of the sector, to access a transformative solution that delivers immediate and significant financial benefits.
This tool is used by a diverse range of care providers to help understand costs, provide a benchmark updated to reflect real-world changes and give providers and commissioners a consistent ‘common currency’ to work in an effective and transparent way. CareCubed streamlines discussions, opens-up opportunities to develop new services and creates a fairer and more sustainable market.
Ensuring a fair price is crucial for both care providers and commissioners and we encourage all providers to adopt and engage with the tool as a consistent national framework to ensure sustainable care fees. For more information email hello@levelft.com or visit www.careengland.org.uk/wp-content/ uploads/2024/01/Level-One-Pager-3.pdf.
For more information and to access the significantly discounted pricing. Please visit www.carecubed.org/careengland.
Waterless, a pioneer in sustainable healthcare solutions, recently launched the world's first 100% biodegradable shampoo capable of transforming hygiene practices in the healthcare sector, providing an environmentally friendly alternative to traditional non-recyclable shampoo caps used for bed-bound or mobility-impaired people. The product offers a convenient, rinse-free solution for hair washing and significantly reduces the time to deliver personal care to residents.
The Nilaqua Shampoo Wrap is manufactured in the UK and is entirely crafted from biodegradable materials. It is a sustainable alternative, providing the convenience and effectiveness of traditional shampoo caps while addressing environmental concerns.
The process significantly reduces carer time with personal care and eliminates the need for additional water or rinsing.
Waterless is committed to leading the change, providing other time-saving, quality, eco-friendly and cost-effective products to save carers time with personal care.
All products are available from Care England distributors. For more information and to purchase directly visit www.norinse.co.uk or review the full product range online at www.waterlessltd.co.uk.
Recycling food waste significantly reduces costs and environmental impact. Segregating waste reduces contamination, decreases landfill costs and enhances recyclability. Anaerobic digestion plants play a crucial role in converting food waste into renewable biogas, preventing methane from being released from landfills, and yield a nutrient-rich fertiliser that enriches soil and replaces chemical alternatives, supporting a circular economy and reducing carbon emissions associated with transporting chemical fertilisers.
Danish pressure care expert Levabo has expanded its pressure ulcer prevention range to include a new automatic lateral turning system, which helps reduce and avoid the risk of pressure issues and speeds up healing and recovery. The system increases comfort and healing and significantly reduces the time associated with repositioning, freeing up time for staff to perform other tasks and activities.
The Turn All fits any standard bed with a removable mattress and was developed to support clinicians and carers in the regular turning of immobile patients with minimal disruption.
Supporting the body along its entire length, the Turn All utilises a 30-degree lateral positioning to relieve tissue compression and restore blood flow.
Furthermore, a five-degree opposing lift counteracts shear, a tissue injury that can occur when the tissue between the bone and subfloor is displaced.
Available from leading lower limb and pressure care distributors Algeos, Turn All is the latest in a range of innovative pressure offloading products for people at risk of developing pressure ulcers.
To find out more about the range of pressure ulcer prevention and treatment products from Levabo, visit http://bit. ly/3tJTcyA or call 0151 448 1228.
Businesses can cultivate a healthier environment and reap substantial financial rewards from recycling food waste of up to £19,000 per annum for a 70-bed care home. The removal of food waste lightens general waste bins, leading to less frequent collections and reducing costs incurred from overweight charges. Experience shows that when businesses actively segregate waste, they gain a clearer understanding of the waste produced, empowering proactive measures to reduce it. Keenan Recycling is the only national food waste collection company and is on a path to Net Zero by 2030, decarbonising its fleet with alternative fuels and providing clients with detailed waste data analysis essential for maximising cost savings.
For more information, please visit www.keenanrecycling.co.uk or contact info@keenanrecycling.co.uk or 0800 644 6618.


“The changes CareHomeLife has made, through the provision of the incontinence system, have improved the quality of life for residents. The process saves staff time and really helps us keep on top of everything.”

“CareHomeLife have an amazing ethos. Excellent pricing and quality all laced with courtesy. A wonderful company to deal with.”

“We guide our clients toward products that will do the job better; saving them time, effort, energy and waste. That’s the true meaning of value”
EDDY FISHWICK, CHAIRMAN,CAREHOMELIFECareHomeLife is challenging and changing the way you buy consumables and equipment, and making it possible to do so much more, with much less.
Book a free, no-obligation review to discover where you can make savings today.


Care England speaks to Tandeep Gill, Head of Business Development (UK and Ireland) at PainChek, to learn how providers can use AI technology to future-proof their business, become more efficient and adopt a more person-centred approach to care.
Care England: Given the increased financial pressures facing providers, why should care providers continue to invest in technology?
Tandeep Gill: I would encourage care providers to think about tech as a tool that they can use to improve efficiency. See it as an investment, rather than a cost. Also, providers shouldn’t underestimate the value it can add in helping them to future-proof their business.
Technology can also help drive productivity and improve job satisfaction, giving carers more time to interact with residents. Care must be person-centred to attract and retain the most passionate and committed workers. It can also enhance overall resident care and satisfaction, leading to valuable word-of-mouth referrals and driving up occupancy by attracting more residents to providers.
The collection of data allows for a broader analysis of the entire care home. Providers will be able to identify what we call the ‘pain burden’ across their entire estate and evaluate how well pain is being managed. This can help avoid the unnecessary moving of residents to high-acuity settings and reduce the level of costly one-to-one care, therefore lessening the need for agency staff.
CE: Can digital transformations result in financial savings?
TG: Yes, absolutely. How much money is saved will depend on the nature of the business, the efficiency of implementation and the specific technologies that are adopted. Artificial Intelligence (AI) can assist, rather than replace, human decision-making and can help remove the need for the workforce to spend time completing mundane tasks. This gives care staff more time to focus on fostering a more person-centred approach.
The Department of Health and Social Care is investing money to support the sector, and we’re hopeful that funding will be available from Integrated Care Boards (ICBs) to accelerate digital adoption. I’d encourage providers to speak to their ICBs, as I think there’s an opportunity for funding there.
CE: How should SMEs go about looking for a credible tech provider to meet their needs?
TG: It’s important to look at the evidence first and to find out whether a claim has been proven and always check the credibility of the research. Consider what problem (or problems) you’re trying to solve and how technology can help. Ask questions, such as:
‘What do we spend most of our time doing?’ and ‘What information are we lacking?’
Choose scalable digital solutions; does the digital solution integrate, and ask: What does the roadmap look like?
Think about whether the tech is easy to use because successful adoption of digital tools relies on that. Providers also need to consider whether the technology complies with regulatory and industry standards and whether it provides robust security features to protect sensitive business data.
CE: How does PainChek differ from the other pain assessment tools that are out there?
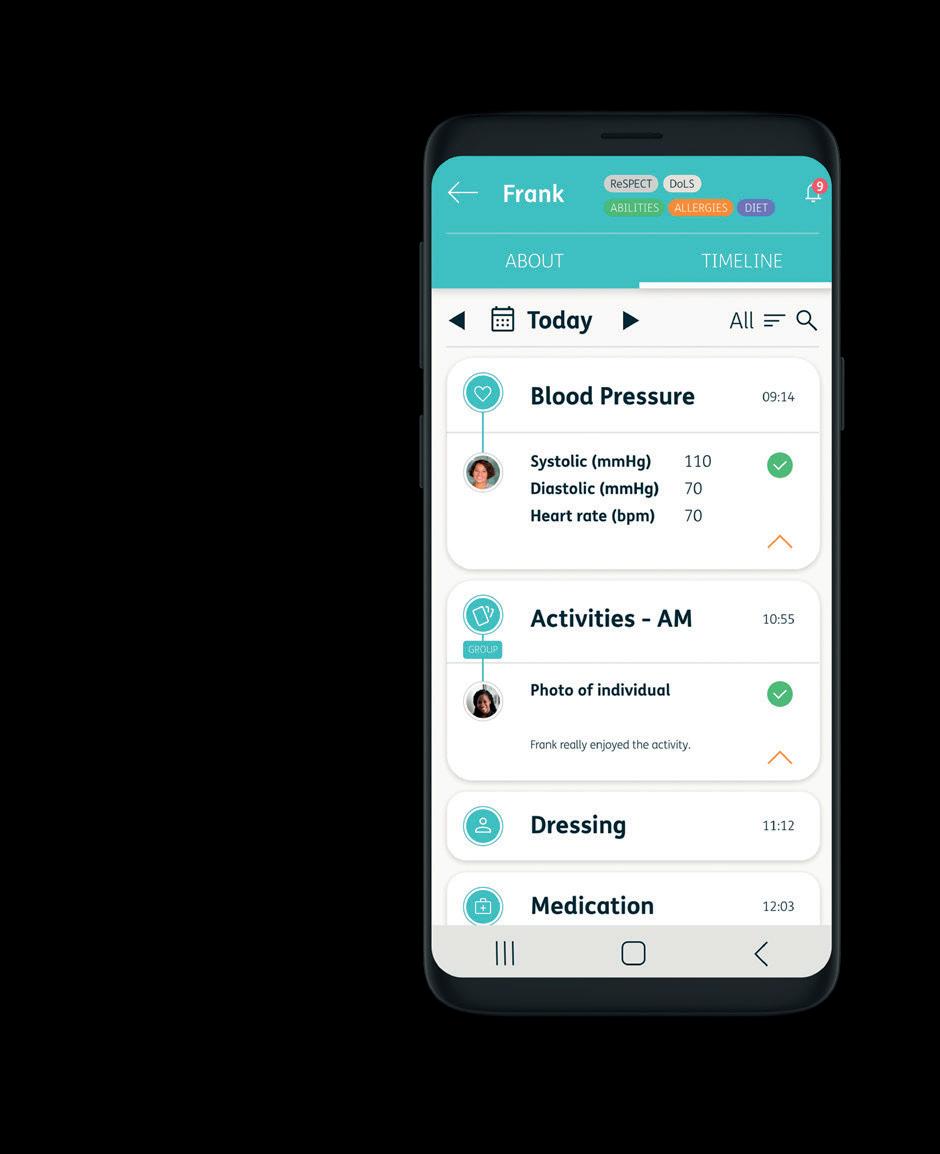
TG: There are a number of technological solutions available to care providers. PainChek is a pain assessment system, which incorporates a mobile app, an eLearning product and a digital analytic suite. It’s these three features that help to make PainChek unique.
The technology is used to assess pain levels and captures the facial micro-expressions that are indicative of pain. That’s combined with a pain checklist that covers the voice, body, behaviour, movement, and activity of the resident. The checklist then generates a pain severity score.
Traditional tools may rely on more subjective assessments. These types of methods are often underutilised, due to their subjective nature. For people who are unable to self-report, it becomes difficult to assess, time-consuming and cumbersome, because those assessments aren’t designed to be used at the point of care.
PainChek’s approach to pain assessment can help to remove assessor bias and help simplify the record-keeping process. It’s worth bearing in mind that providers can integrate the tech system with other digital clinical systems, including DSERs (NHS Approved Digital Social Care Records [DSCRs]) - such as PCS, Nourish, Access Care and Clinical, Care Vision and Care Control Systems.
This helps data to move seamlessly between different clinical operating systems to improve accuracy, data integrity and data consistency.
There’s also a data analytic suite, with features for data collection and reporting. This allows providers to collate evidence (for the regulator) and can contribute to a more systemic understanding of pain patterns.
CE: What evidence are you able to share to demonstrate PainChek’s impact?
TG: PainChek has been linked to a 42% reduction in falls, a
42% reduction in what we call ‘stress and distress’ (distressed reactions or behaviour), and a 50% reduction in dependency scores amongst residents after six months, all recently documented in the Scottish Social Care Nurses Network Journal
A recent workshop organised by the CQC as part of their ‘Capturing Innovation to Accelerate Improvement’ project looked at the experiences of Orchard Care Homes. Orchard has adopted PainChek and embedded it into their practices, and it’s helped them deliver high-quality care for their group. Using PainChek, they’ve been able to reduce levels of stress and distress, which has led to a 10% decrease in antipsychotic medication use, across all 23 homes. We’ve written a peerreviewed article about this with Orchard, which has just gone into the Journal of Psychiatry. PainChek has been mapped against all the CQC Quality Statements, and it supports 20 out of 34 of these.
Cheryl Baird, Director of Quality and Care at Orchard Care Homes, said, ‘Managing pain alone is not a silver bullet, but it is important to get this right first, as pain is the most under-recognised symptom experienced by those living with dementia. Whilst we still see slips and trips, the ability to look at potential causes and minimise injury risk has been incredible. A fracture can severely impact an
older person living in care, even reducing life expectancy, so this work is vitally important.’
CE: How much training is involved in using a tech tool such as PainChek?
TG: The change management required for PainChek is minimal. There’s a CPD training programme available, which helps build skills within the tool itself, and helps create a broader understanding of pain and dementia.
A UCL study recently published in the Lancet found that 1.7 million people in England and Wales could be living with dementia by 2040 – that’s over 40% more than previously thought. Given the health and social care workforce is already stretched, we need to take an innovative approach to meeting the needs of this vulnerable group of people, and the use of technology is key to achieving this.
CE: Have you got any workshops or webinars available?
TG: Yes, we have webinars available on our website and there’s a PainChek Academy. Here, providers will find an open portal to e-learning, so anyone can pick up a module and do some training. We also deliver training in-person, directly to carers and residents.
Visit https://painchek.learnworlds. com/ for more information.
Tandeep Gill is the Head of Business Development (UK and Ireland) at PainChek. Email: tandeep.gill@painchek.com @PainChek







In this article, Jim Thomas, a Social Care and Health Workforce Expert, explores what data can help, what data to ignore, how to spot a trend and how non-numeric data can help to retain the workforce.
The article will focus on:
• The impact of pay on retention.
• How to understand sickness trends.
• In-work benefits.
• Flexible working.
• How to project future retention.
Three rules to consider:
1. Have I got ready access to the data?
2. Is the data in a format I can use?
3. Does the data help make decisions I can explain to others?
Data to focus on might change depending on what you are trying to understand, how easy it is to access in a format that makes sense and what you want to use the data for.
For workforce retention, important data includes exit interviews and supervision records. A well-designed exit interview gives an honest picture of why someone is leaving be that pay, promotion, flexibility, benefits, their manager, or co-workers. Supervision records can offer a picture of how staff feel. If there are no supervision records, you might wonder if the workforce has a safe space to explore their concerns. If you look at workplace incidents (falls, moving and handling mistakes and medication errors) you might find places where the workforce does not have regular supervision, and this might link to issues retaining workers in a particular part of your organisation.
Choosing which data to ignore is equally important as you can lose a lot of time looking at data that doesn’t aid decision making. Ask yourself three questions before looking for data:
1. Can I understand and explain the data to others without needing specialist help?
2. Will the data help compare my workforce with other similar workforces meaningfully?
3. Is the data recent, or over a long enough period to be useful? Continued →










These questions will help decide which data to use and what to ignore. If you need external help to understand the data, are any costs associated? Also, will external data analysis be able to understand the context in which your workforce is operating fully?
When comparing data, you need to decide how similar your workforce is to the comparison data. Is it helpful to compare retention data for home care workers and residential care workers? Probably not, as the factors that people have in mind when they choose to work in a certain type of employment will differ.
Some people may prefer working alone or one-on-one or in the same place every day in a residential care environment. Some people might prefer work that fits in with other personal commitments, or roles that don’t require them to work in the evenings or at weekends. Some roles are cross-transferable and could be useful to compare, such as registered managers. You might want to look at the factors that keep people in those roles (such as pay, support, training opportunities and personal development opportunities).
A trend is an up or downshift in data over time. To spot a trend make sure that the data is specific enough, over a long enough period, and can draw meaningful conclusions. You also need to think about anomalies that might impact the validity of the data. For example, the pandemic. However, it’s still worth asking – what did we do during this period that improved or didn’t improve retention? You might have a particular part of your workforce where turnover is much higher than other parts of your workforce. You could look back over the last five years to see if this is something that has just occurred or has been happening for a longer period. The questions you might then ask are: Has something happened in that workplace to create this trend? Is it that workers are being asked to do things that they don’t feel are part of their role? Has there been a change in management that has had a positive or negative impact on the workforce? Have contracting arrangements changed, impacting job security? If the trend shows that turnover always goes up in school holidays, think about how you can adapt your workforce patterns of employment to reduce turnover.
Non-numeric data includes case examples, personal testimony and witness statements. This data can help explain decision making and add detail to the numerical data. Data might show a reduction in turnover and improved worker retention over the last six months, but it won’t tell you why. For example, if you add a narrative to the data that explains how a new training programme has made the workforce feel more confident and valued, you add colour to the data that gives a more rounded picture of what does and doesn’t help to hold on to the workforce.
Pay is one of the factors that influences retention, but it can be a red herring. People will change jobs for improved pay and most people who work in social care are not paid at a rate comparable to the knowledge and skills that are required to work in social care. It can be a red herring because often the wrong data is used to make comparisons about pay. To change the narrative, you need to change the data comparisons you are making to challenge pay rates and stop comparing roles that are paid at a similar rate to social care roles (for example, retail workers and leisure industry workers) and start comparing roles based on like-for-like knowledge and skills.
Like-for-like roles include health care assistant roles, nursing roles, allied health care roles, and technical roles in industries such as engineering and specialised sporting support roles.
The other thing to consider when looking at pay data is other linked benefits, such as enhanced pension provisions, free uniforms, family support, annual leave provision and overtime rates.
To understand sickness trends, you need to look backwards and understand if there are trends. For example, times of the year when sickness is higher (school holidays, certain national holidays). Is there a link between short-term sickness and longerterm sickness? Are there different levels of sickness amongst people in different roles? If you combine your exploration of the data with back-to-work interviews you will begin to build a picture of the factors that impact sickness and what you might do about it.
For example, a gradual or sudden change in the level of support that workers have to offer people could result in more injuries at work; for example, moving and handling injuries and personal harm from supporting people whose behaviour is challenging. You might need to implement new training and development programmes and review the impact these programmes have on sickness levels.
In-work benefits are closely linked to pay such as enhanced pension provisions, free uniforms, family support, employee assistance programmes, annual leave provisions, and overtime rates etc. From a data perspective, you need to test the impact that different in-work benefits might have on retention. The starting point for this should be the cost of providing an in-work benefit. For example, improved overtime pay may reduce the use of agency staff, which may retain the workforce more effectively and result in staff and the people they support feeling better about the place they work as well.
Flexible working can also be linked to pay and in-work benefits and comes in many forms. It can be a contract where someone only works on specific days, doesn’t work during school holidays, or takes account of someone’s additional family care responsibilities. This might mean that sometimes they need to change their working pattern at short notice. For example, if someone can only work 10 hours a week during term time and you can accommodate that, you might increase workforce retention. This is because you can show how, as an organisation, you can flex the way you are organised to meet not only the needs of the people your organisation supports but your workforce as well.
This is one of the most difficult things to do and you need to look backwards and explore the factors that have enabled you and other organisations to improve retention. You could start by using something such as the Best Companies survey to help you understand your workforce. For example, through such a survey you might discover that your workforce feels that support that improves their wellbeing at work or home is not as good as you thought it was. You can then look at what you can put in place to improve wellbeing and then do the survey again after 12 months to see what has changed.
Any source of data is only as good as the accuracy with which it has been collected. How well it has been kept up to date, how long it has been collected, and how many people/organisations have contributed to it. A survey of 10 is less useful than a survey of a thousand when it comes to drawing conclusions from the data.
Skills for Care’s Adult Social Care Workforce Data set is an important source of workforce data. It is regularly updated and can be explored at an individual service level by a group of services in a local area, and by a care group at a regional and national level. Because there is so much data in the Adult Social Care Workforce Data set it’s important to know what you want from it before you dive in. If you are looking at it from a retention perspective, then look for these three things:
1. Pay rates.
2. How long do people stay in particular jobs?
3. The age ranges of people in different roles.
These three data points will help build a picture of how to compare other similar organisations.
The Office of National Statistics is also a valuable source of data (although less specific to the social care workforce) but can help compare your workforce data with other workforce data sources. If you are looking at data from a retention perspective, then look for these three things:
1. Pay rates for similar jobs.
2. Workforce mobility – how long do people stay in different jobs?
3. The age range of workers in different industries.
Be open to case examples, personal narratives and witness statements to add context.
These three data points help us to understand what other industries are doing to retain their workers and potential learnings for your organisation.
The Commission for Care Quality’s reports such as The State of Care are a useful source of generic data to help decide on the retention issues you might want to explore. Individual inspection reports are a way to explore retention challenges for similar organisations. Identify four similar organisations (homecare/ residential), location (rural/city/town) and number of employees. Choose two reports that are rated outstanding and two that are rated inadequate. Then look at the following:
• Turnover of workers – what percentage leave per annum?
• Manager stability – how long do managers stay in post?
• Absence rates – number of absences and duration.
This data might not always be easy to find but will give you an indication of things that you might be able to use in your organisation to improve retention.
Data is one of the many tools to help with workforce retention and the amount available can be overwhelming. Therefore, it’s important to think about what data to use, why you want to explore it, and how it can help. I would urge you not to limit yourself to just numerical data and to be open to case examples, personal narratives and witness statements to add context. Sometimes, less data can often be more than enough.
Jim Thomas is a Social Care and Health Workforce Expert. Email: jim.thomas@longhouseman.co.uk
@Longhouseman
Deadline fast approaching!
Funding is being provided by the Department of Health and Social Care!
By adopting a digital social care record, carers will be able to:
Have instant access to information: no more waiting around!
Record Real time information: An efficient & person-centred way to evidence care!
Improve compliance with the regulator: All information in one system!
The most widely used system by care providers of all sizes in the UK!
Over 30,000 beds live on GP connect already connected

Enabling access and sharing data with Shared Care Records
A UK based team covering support, development & technical aspects, designed to ensure our customers gain the best experience
Gives each nurse, carer and home manager more time to care
Everything you need in one place throughout your digital journey
95% of our 6,000+ care homes are rated as Good or Outstanding


National Care Group has achieved considerable expansion and completed numerous acquisitions during a time when many providers have had to hand back packages of care, scale back or close services. National Care Group’s Commercial Director, Mike Ranson, tells us how it has achieved that growth and expansion and offers advice in the form of five strategies to focus on.
Without a doubt, social care is moving through a period of significant challenge, which is likely to result in a change of practice and behaviour in commissioning teams and providers alike. This type of challenge and change has been a constant in the working-age adult sector for two decades. There is, therefore, an extraordinary amount of learning and experience already being applied to the question of sustainability and the maximisation of potential that challenging times bring with them.
A stable base on which to grow is an obvious place to start, but that platform needs to be capable of flexing to ensure
we remain efficient at times of both growth and retraction. Whether that flexibility is at a service level, due to support packages starting or ending, or at an organisational level, due to the integrations of new businesses. Understanding our fixed and variable structures and associated costs places us in a position to sustain our business and react swiftly to opportunities when they present themselves.
As an organisation, National Care Group (NCG) has taken time to position itself within the market and establish the platform most appropriate to that position. In doing so, we can quickly assess what opportunities would be advantageous to us and those which might lead to us overextending the business.
We maintain an eye on our market share in specific sectors and localities to ensure we are not ‘overexposed’ to any significant changes in organisations or commissioning strategies. This does not mean we shy away from diversification; far from it, diversification is one tactic we use to avoid being overexposed and to mitigate against that risk.
As a larger organisation, we have ‘buying power’ and an ability to negotiate down some of our costs, such as insurance and utility bills, without affecting service quality. However, leverage is also gained from the partnerships we form and our ability to demonstrate value, over and above the service paid for.
It feels obvious to say, but knowing the extent to which you can ‘grow’ your services within the current management and support structures before you need to increase costs is vital. Sometimes saying no to another support package is more financially advantageous than saying yes.
Should you decide to grow past your current capacity, be realistic about how long it will take you to increase your income. Consider recruitment, property development timescales, and delays to registration, as a minimum. Do you know when you will break even between cost and income? Do you have the cash flow or lending facility in place to get to that point?
Building a reputation as a trusted and integral part of the local system and paying attention to our communication with commissioners, significantly enhances our understanding of the demand, opportunity, and challenges. This all contributes to the insight we have at NCG into the market as a whole and how it is moving.
It is difficult to understand the imperative for growth or acquisition when an organisation is unable to maintain a sustainable level of occupancy or activity within its existing services. Part of achieving that outcome is recognising our co-dependency with our commissioning partners; it is easy to focus on what we require without considering what others
in the ‘partnership’ need. An approach of treating each support package or contract in isolation may get you a better margin on one support package. Being combative in your approach may win the point but not the business. Helping with this problem may mean you are asked to help with several others and not relegated to the ‘only when there is no other option’ pile.
For NCG, collaboration and consultation are critical factors that have contributed to our success. Our results are our responsibility alone, but we are reliant on commissioners and people with support needs demanding and wanting what we provide. The best route to achieving this outcome is to provide what they want, not just what we want to do. It may be more difficult and not quite what you had in mind but a slight adjustment to plans at the start could mean the difference between opening one unsuccessful service or opening one that is successful, every year for the foreseeable future.





When creating our service models, we consider what we know about the structures required to provide a quality service and deliver the expected outcomes. We look to understand the economies of scale required to provide sustainability and the demand for particular service models or focus.
This, along with the contractual frameworks that might support or impinge on our ability to trade, enables us to be clear with potential commissioning partners about how we will approach the development of a new service solution, the benefits of that, and the costs associated. The same detail enables us to quickly assess how an existing service might be repositioned to respond to changing demand.
All these considerations give us a clear position on the overall level of funding required to maintain a service with an acceptable level of return. Depending on the contract framework we can then make a feasibility decision in respect of the hourly rates on offer or discuss affordability
with the commissioning team. Preferably before we have committed significant capital.
With a considerable history of acquisitions completed over the past six years, we have developed a robust process of feasibility assessment and a strong combined sense within the management team of what’s driving performance. The process we follow when looking at growth and achieving a sustainable platform gives us a clear focus for considering acquisitions. As well as the strategic ‘fit’ the key questions are, can we add value, is the business sustainable, or could it be sustainable as part of NCG?
With legal and financial due diligence, taxes, and other transaction fees likely to amount to 10% of the acquisition price, being able to undertake this ‘high level’ assessment of a potential acquisition upfront ensures we do not commit time and resources to formal processes unnecessarily. It also enables us to commit to a process from the start.



Holiday Pay for irregular hours and part-year workers in the care sector and beyond is notoriously complicated. Catherine Meenan, Associate at Weightmans LLP, outlines the law surrounding holiday pay for these workers and explains the changes which could make the thorny issue of holiday pay easier for employers.
Who knew holiday pay could be such a controversial and complex issue? The social care sector requires a fluid workforce to help manage fluctuating demand for services which may arise for a variety of reasons, including covering sickness and holiday absence and turnaround of staff.
To help with flexible working patterns which are essential to recruit and retain care workers, care providers are used to hiring ‘irregular’ hours workers and ‘part-year’ workers. However, offering flexibility comes with the challenge of trying to work out holiday entitlements and holiday pay accurately and in accordance with the law.
In this article, we will take you through the latest changes to holiday pay law and explain how providers can ‘save money’ if they effectively manage the process and understand each employee’s working pattern.
In recent years, in the wake of complex UK and European case law, the calculation and payment of holiday pay has given rise to significant challenges for employers. The case law, which we will summarise
briefly below, has introduced uncertainty, complexity, and an administrative burden on employers. This, in turn, has given rise to claims against employers for unpaid holiday pay.
As a result of the uncertainty, the Government launched two consultations in 2023 to review various elements of holiday pay. In this article, we explore:
• A brief history of the law on rolled up holiday pay and the calculation of holiday pay for part year and irregular hours workers.
• The results of Government consultations on rolled up holiday pay and the calculation of holiday pay for part year and irregular hours workers.
• What businesses in the care sector and beyond need to do to ensure compliance and reduce the risk of claims.
The definition of irregular hours workers could apply to some agency workers, casual workers, and zero hours workers, all of which are common working arrangements in the care sector. The legal definition is set out in the Employment Rights (Amendment, Revocation and Transitional Provision) Regulations 2023 as follows:
'(a) a worker is an irregular hours worker, in relation to a leave year, if the number of paid hours that they will work in each pay period during the term of their contract in that year is, under the terms of their contract, wholly or mostly variable;

Get free, expert support from Digital Care Hub – run by social care providers, for social care providers.
Digital Care Hub is the new name for Digital Social Care. We provide free advice and support on data protection, cyber security and using technology. www.digitalcarehub.co.uk/contact-us

From December, Better Security, Better Care are launching a free data and cyber security e-learning resource for frontline care staff that will satisfy key requirements in the Data Security & Protection Toolkit (DSPT).
A new Return on Investment (ROI) tool will be available from the end of November to help care services estimate
an indicative return on investment and financial savings from adopting a piece of technology.
The tool has been developed in partnership with ARC England and tested with care providers. It’s free to use with a full user guide.
You can access the eLearning resource and the ROI tool on the Digital Care Hub website using the QR code above.
'(b) a worker is a part-year worker, in relation to a leave year, if, under the terms of their contract, they are required to work only part of that year and there are periods within that year (during the term of the contract) of at least a week which they are not required to work and for which they are not paid.'
It was, historically, the usual practice for employers to calculate and pay holiday pay for those workers on flexible contracts in the following (simple) way:
• Holiday pay was calculated by paying workers on flexible contracts 12.07% of their remuneration for work done in each pay period (the Percentage Approach). The benefit of the Percentage Approach was that holiday pay was broadly proportionate to the amount paid to full-time workers.
• Holiday pay was paid on a ‘rolled up’ basis. (Rolled up holiday pay [RHP] is where a worker receives an enhancement [12.07% of pay] with every payslip to cover their holiday pay, as opposed to receiving holiday pay only when they take annual leave.)
However, this changed due to a number of decisions on holiday pay. The issue of rolled up holiday pay was referred to the European Court of Justice; a 2006 legal case concluded that rolled up holiday was unlawful on the basis that the practice disincentivised taking leave.
In July 2022, the Supreme Court handed down its judgment on Harpur Trust v Brazel. This case concerned the calculation of holiday pay and entitlement of a permanent part-year worker on a zero-hours contract. The judgment held that the correct interpretation of the Working Time Regulations 1998 is that holiday entitlement for part-year workers should not be pro-rated so that it is proportionate to the amount of work that they actually perform each year. Part-year workers are entitled to 5.6 weeks of statutory annual leave calculated using a holiday entitlement reference period to determine their average weekly pay, ignoring any weeks in which they did not work. As a result of this judgment, part-year workers are now entitled to a larger holiday entitlement than part-time workers who work the same total number of hours across the year.
There were challenges in this approach in that it led to potentially complicated
calculations for employers trying to calculate average weekly pay.
However, the Government is keen to address this disparity to ensure that holiday pay and entitlement received by workers is proportionate to the time they spend working. At its extreme, for example, the case meant that an exam invigilator on a ‘permanent’ contract throughout the year, but who only worked a couple of weeks in the year, could be entitled to 5.6 weeks’ holiday, payable in accordance with average weekly earnings.
In view of the impact of the Supreme Court decision on sectors that engaged irregular and part-year workers, the Government announced two consultations: one addressing the calculation of holiday entitlement and another addressing (amongst very many other things) rolled up holiday pay.
As the Consultation on the calculation of holiday pay recognised, ‘Over time, holiday pay and entitlement legislation has become complex and, in some cases, can be challenging for employers to follow due to changes in case law’.
The outcomes of the two consultations were published jointly. Of relevance to the calculation of and rolling up of holiday pay, the following changes were announced:
(a) Rolled up holiday pay for irregular or part-year workers will be permitted. This is conditional on holiday being calculated on the basis of the Percentage Approach, the holiday pay being paid at the same time as pay for work done, and holiday pay must be itemised on the payslip. There are different rules applying to the payment of rolled up pay for those workers on statutory leave and on some kinds of family-related leave.
(b) Holiday pay for part-year and irregular hours workers for holiday years from April 2024 can once again be paid in accordance with the Percentage Approach. This has the effect of accruing payment for annual leave as the worker works, instead of being based on pay in the previous 52 weeks worked.
The draft statutory instrument came into force on 1st January 2024. The changes will come into effect on 1st April 2024 for those holiday leave years starting on or after that date.
@Weightmans_Empl
How do the proposed changes affect your costs?
The option of paying and calculating holiday pay in this simplified way for part-year/ irregular hours workers has been largely welcomed by employers. In large part, the changes simplify processes to be followed by employers and, crucially, for most employers, will reduce the amount of holiday pay due to part-year or irregular hours workers. If applied correctly, the reforms should also mitigate risk of unpaid holiday pay claims.
To save this money, and mitigate the risk of these claims, we would suggest you take the following steps:
1. Identify workers who are entitled to holiday pay
The new regulations do not change the requirement to pay workers holiday pay. However, it is always worth ensuring that workers who are entitled to holiday pay are receiving it. Otherwise, you risk potentially sizeable, backdated unpaid holiday pay claims.
2. Transparency is key Transparency around the calculation and timing of holiday pay payments is key. Make sure to clearly set out a separate payment for holiday pay on payslips. It can be categorised as ‘Holiday Pay’ or, very often, ‘WTD’ (for example, Working Time Directive). It would also be helpful, in agreements and/ or policies and/or in other communications, to explain the method of calculation of holiday pay adopted.
If you do not itemise holiday, you run the risk of an employee arguing that they have not received any holiday pay at all.
3. Encourage workers to take leave
Just because holiday pay can now be rolled up and no longer has to be paid at the point a worker takes holiday, that does not mean that workers can work without taking any holidays.
Employers still bear the burden of making sure that workers take their holiday, and it is important as part of an employer’s duty for the health and safety of its workforces that its employees take the appropriate breaks.
We would suggest including a provision to this effect in a (signed) contract and
reminding workers at regular intervals (via the Intranet for example) to take their leave.
4. Conduct a review of relevant agreements/policies
Following Harper v Brazel, many (though not all) employers changed their holiday pay payroll calculations. For many, these changes were also reflected in policies and/or contracts with part-year or irregular hours workers.
If you were one of those employers, and choose to revert to the Percentage Method, you will need to change your payment practices and communication of that pay.
Before communicating this change, however, we would suggest reviewing how many people will be affected by the change and what the relevant contracts and policies say. It will be important that any change in the calculation of holiday pay is not contradicted by any relevant contract/policy.
Beware that if the way in which you pay holiday pay is set out as a contractual term, or if the contract/agreement does not permit you to amend or vary the terms of the agreement, you may have to seek to agree to the change with workers or, alternatively, unilaterally agree the change. Although unusual amongst irregular/ part-year workers, it is always worth checking whether there is a union that will need to be consulted on the changes.
The development of holiday entitlement and holiday pay has evolved significantly over the years. The impact of the Harpur Trust v Brazel Supreme Court Decision had an adverse impact on those employers who engaged irregular hours and part-year workers, including the care sector. The solution offered by the Government following its Consultations should assist employers in determining the correct level of pay simply without the need for complex calculations which will ultimately create savings and make the workforce sustainable.
If you would like further information in relation to holiday pay law and/ or would like to ask our expert team your questions, do get in touch with Weightmans LLP by emailing: catherine.meenan@weightmans.com






Amidst the financial constraints of care home management, Jay and Palvi Dodhia at Serene Care share their thoughts on transforming care homes on a budget with residents in mind.
A welcoming, homely environment is paramount for care home residents. It fosters wellbeing, improves quality of life and attracts potential residents. However, maintaining and upgrading care homes can be financially daunting, especially for smaller providers.
With all of our care homes purchased as loss-making turnarounds, budget constraints could have posed a significant hurdle to realising our vision of warm, supportive 'homes away from home' at Serene Care. Yet, our team embraced resourcefulness and creativity, not just working within budget limitations, but putting residents at the heart of every decision as we transformed our homes.
Most importantly, we prioritise changes that significantly impact residents' lives and are readily noticeable to inspectors and visitors. But before embarking on a refurbishment journey, we also always carry out a Costbenefit analysis. We ask ourselves, if this will this investment yield financial returns. We analyse potential benefits like increased occupancy rates, improved CQC ratings (leading to higher occupancy and funding) and enhanced reputation, especially with the local community.
Meticulous planning is key to avoiding budget overruns. Involve staff in identifying problem areas and desirable changes early (even prior to completion). Design enhancements should prioritise mobility and accessibility with familiar, homely decor and easy-to-clean furnishings. Furthermore, ensure everything that is done is dementia friendly as well.
Being budget-conscious doesn't have to mean being tech-averse and we firmly believe that investing in the right technology from day one can help turn the care homes around even quicker, especially digital care management systems, which are now considered essential for any provider.
Smart technology can be your budget-friendly ally, enhancing resident comfort and fostering social connection.
Picture residents enjoying a comfortable temperature year-round thanks to smart thermostats adjusting to changing seasons and individual preferences. These automated systems not only offer comfort but also contribute to significant energy savings,
reducing running costs and supporting your budget. We have also embarked on adding solar panels that will be cost-positive. They pay for themselves immediately given they can be fully funded at costs that are less than what we would pay for the equivalent electricity from the grid.
A fresh coat of paint in calming colours can dramatically transform a space. Declutter hallways and rooms to create a sense of spaciousness. Introduce new, co-ordinated soft furnishings and curtains for a touch of warmth. Create variety in room decor to aid memory and orientation. Optimise lighting with energyefficient options that promote safety and a homely ambience. Display artwork and objects of interest to stimulate residents' minds. These are all just a few things we take into account.
Keep large windows and skylights clear. This brightens the space and elevates the mood and daytime sunlight can significantly reduce reliance on artificial lighting, lowering energy costs and contributing to a more sustainable future. There are also artificial options which are low cost but can mimic natural sunlight for those darker spaces too.
Introduce a touch of the outdoors with indoor plants. They are vibrant ambassadors of serenity and life. Lush green leaves not only enhance the visual appeal but also act as natural air purifiers, removing toxins and improving the overall air quality, creating a healthier environment for residents. Choose low-maintenance varieties like the resilient snake plant or calming lavender, ensuring they pose no risk to residents, especially those with dementia who might be drawn to interact with them.
tactile textures that soften the feel of hard floors. Play with lighting, employing dimmer switches to create intimate areas for quiet conversation or reading.
Make the space truly their own by encouraging residents to personalise it with cherished photos, family heirlooms, or even artwork they've created. This adds a layer of familiar comfort and allows them to express their individuality. Memory boxes are a great way for residents with dementia to find their way as well.
Allowing residents to bring in their own furniture not only reduces our costs but gives them a sense of familiarity. But don't neglect the functional aspects. Ensure furniture is appropriately sized and positioned for easy access and comfortable use. Clear clutter to create a sense of visual peace and make navigating the space easier. Remember, these seemingly small details can have a profound impact on the way residents experience their environment.
Don't let unused corners gather dust in your care home. Try creating a tranquil reading nook tucked away in a quiet corner, bathed in gentle natural light from a strategically placed skylight. Why not try a cosy reflection zone, adorned with soft furnishings and calming décor offering residents a space to unwind and contemplate? Or perhaps, think of a small exercise area tucked away, equipped with gentle resistance bands and light weights, encouraging residents to maintain their physical wellbeing in a private, non-intimidating space.
By repurposing these unused spaces, you're not just maximising the available square footage. You're creating nooks that cater to diverse needs and preferences, giving residents more options to enjoy their time within the care home. A reading nook, for instance, can become a literary haven, fostering intellectual engagement and social interaction through book clubs or shared reading sessions. A reflection zone can offer a sanctuary for prayer, meditation, or simply a quiet moment to collect thoughts.
Think of soft furnishings like plush throws and cushions that embrace residents in comfort. Introduce rugs in warm colours and Continued →
The exercise area can empower residents to maintain their physical wellbeing, boosting confidence and promoting an active lifestyle. These areas don’t cost a fortune to create and can be added to your marketing collateral that showcases the benefits of your home.
Speak to your local authority and see what support there is for care homes. We have received help with energy efficiency measures and training for our staff which can very quickly add up. Supplementing this with volunteers and support from local community groups has meant that we are able to not only implement our refurbishment faster but have support from the local community in doing so which creates significant goodwill.
Instead of the upheaval often associated with renovation, we adopted a meticulous phased approach at Serene Care ensuring minimal disruption and maximum resident comfort. For example, we began by upgrading the upstairs lounges and bedrooms while residents continued enjoying social gatherings in nearby areas. This preserved cherished routines and ensured planned activities never
missed a beat. We gently replaced worn carpets, upgraded lighting and introduced modern amenities all while respecting the familiar atmosphere around them.
Our phased approach ensures that progress doesn't come at the cost of comfort. We empower residents to remain at the helm, prioritising their wellbeing and respecting their routines every step of the way.
Breathing new life into a care home on a budget requires creativity, resourcefulness and a deep understanding of the needs and preferences of the residents. By prioritising resident wellbeing, focusing on low-cost interior cosmetic changes and utilising technology and smart solutions, we can create warm, supportive and homely environments that enhance the quality of life for the residents.
Ultimately, it is the small, thoughtful touches and the attention to detail that make a big difference in creating a care home that feels like a true ‘home away from home’ for its residents. By embracing a residentcentred approach and working within budget constraints, we have shown that care home providers can create environments that promote wellbeing, dignity and a sense of belonging for their residents on a budget.
Jay and Palvi Dodhia are the founders of Serene Care Ltd. Email: info@serene.care @palvi_dodhia


INCLUDE:
consistent stream of up-toindustry news, research, guidance to stay informed compliant with evolving regulations.
A consistent stream of up-todate industry news, research, and guidance to stay informed and compliant with evolving regulations.
MINT, our exclusive funding and market intelligence platform to help secure higher fees and significantly enhance financial performance.

MINT, our exclusive funding and market intelligence platform to help secure higher fees and significantly enhance financial performance.
Exclusive events such as webinars, workshops, and conferences which are designed to empower and inspire care service delivery.
Exclusive events such as webinars, workshops, and conferences which are designed to empower and inspire care service delivery.
discounts and free goods and services, reduce costs and income to enhance provision.
Exclusive discounts and free audits on goods and services, proven to reduce costs and recover income to enhance provision.
Opportunity to connect with peers, share insights, and collaborate with industry leaders to enhance knowledge and skills through special interest groups.
Opportunity to connect with peers, share insights, and collaborate with industry leaders to enhance knowledge and skills through special interest groups.
Be part of a louder voice, benefit from sector relationships with government and advocate for our collective needs and interests.
Be part of a louder voice, benefit from sector relationships with government and advocate for our collective needs and interests.
CHOOSE CARE ENGLAND?
the collective experience and expertise o f our membership, we deliver solutions to the most pressing challenge s facing your organisation and your voice on a national scale. By joining Care England, you are helping to change your organisation needs to thrive by:
Guided by the collective experience and expertise o f our membership, we deliver innovative solutions to the most pressing challenge s facing your organisation and amplify your voice on a national scale. By joining Care England, you are helping to drive the change your organisation needs to thrive by:
solutions to offset inflation


Enhancing workforce development
Providing solutions to offset inflation
recruitment and retention



Enhancing workforce development
Supporting funding negotiations
Improving recruitment and retention
national reform reflects your needs



Supporting funding negotiations
Informing the regulatory landscape
Ensuring national reform reflects your needs
transform your care services?
code or contact Daryl Garcia at dgarcia@careengland.org.uk or 0845 057 7677.

Informing the regulatory landscape

Scan the QR code or contact Daryl Garcia dgarcia@careengland.org.uk or 0845 057 7677.
SCAN HERE
*Terms and conditions apply, see website for details.

*Terms and conditions apply, see website for details.
In the hustle and bustle of managing a care home, it's easy to overlook the importance of foot health. If your first thought is that foot health merely involves routine toenail trims, you're not alone. However, it's time to challenge this perception. Leona Calderbank, Co-Director of Care Home Podiatry, leads the first national Podiatry service solely dedicated to serving care homes. In this article, Leona shares what care providers must consider about foot health and explains how best to support people.
Quality foot health treatments, delivered by certified professionals, should support your staff while significantly enhancing the quality of life for your residents, preventing falls and hospitalisations and even reducing the risk of amputation and premature death. Yes, you read that correctly, foot health really is a matter of life and limb.
The truth is most of your residents will have some foot health concerns. A big study of older adults1 found:
• A quarter of adults over the age of 65 live with foot pain.
• 75% of older adults suffer from a nail condition.
• 60% have toe deformities.
• 58% have problematic calluses or corns.
• Bunions, cracked skin, ingrown toenails, fungal infections and ulcerations (wounds) are also common.
You might be thinking these conditions sound pretty minor, and yes, they can be, but they can also be early warning signs of more serious problems. For example, corns and calluses are caused by pressure on the skin – exactly the same thing which causes
pressure sores and foot ulcers, which can lead to functional impairments, reduced mobility, and increased risk of infection. Not what you want for your residents. Having a qualified, regulated professional in place to catch and treat these problems early helps prevent these more damaging or dangerous problems from occurring for your residents.
Having a foot concern affects your residents' mobility which significantly affects their quality of life. Studies have shown that foot pain significantly reduces people’s ability to walk, and their ability to carry out physical activities and interact socially2
Foot pain leads to a more sedentary lifestyle with reduced physical activity. This is associated with various health issues, including cardiovascular diseases, obesity, and respiratory problems, all of which can contribute to your residents' mortality.
Impaired mobility naturally results in a loss of independence, affecting your residents' ability to perform daily activities. This loss of autonomy may lead to social isolation and a decline in cognition and mental wellbeing, which not only impacts on your residents' overall health and longevity but also increases demands on your care staff.

Care professionals can now access volunteer support through the NHS and Care volunteer responders programme.
Volunteers help in simple ways. Check In and Chat volunteers provide friendly phone calls to people in need of a bit of extra companionship. Community response volunteers help with delivering essential shopping and medication.
The service is free of charge and open for referrals now.
Half of all care home residents fall every year. Falls are one of the most common causes of unplanned hospitalisation, hip fracture, and death in older adults living in care homes3
Recent scientific studies have shown that having a foot problem greatly increases your chance of having a fall. Foot pain, toe deformities and bunions are particularly linked to an increased fall risk4.
We’ve seen care homes investing money in all sorts of gadgets to reduce falls, but have you covered the basics that your residents are already paying for? Foot checks by qualified, regulated clinicians should be part of your routine fall assessments.
One in four care home residents currently has diabetes5, with numbers expected to significantly increase over the next 30 years. Foot problems are one of the most serious issues faced by people living with diabetes. If your visiting foot health provider is just cutting your residents with diabetes' toenails, it is definitely time to reconsider your foot care provider.
Poorly controlled diabetes can cause the health of your residents' feet to deteriorate significantly:
• Loss of feeling – Diabetes can lead to nerve damage which causes tingling, burning pain and permanent loss of feeling in your residents' feet.
• Decreased circulation – Diabetes can contribute to the build-up of blockages in blood vessels, meaning less blood gets through. Healthy blood flow is essential to keeping bodily tissues alive.
• Foot deformity – Feet can begin to change shape as a result of changes in the muscles of the feet and legs. This often starts with clawing of the toes and can progress to developing a high-arched foot. These changes in shape make the foot more prone to rubbing in footwear and increase the pressure and friction on the sole of the foot when walking.
These changes then place your residents at high risk of very serious diabetic foot conditions including:
• Diabetic foot ulcers – wounds that can take months or even years to heal. Diabetic foot ulcerations can lead to infections, sepsis, the need for limb amputations and even death. Diabetic foot ulcerations have a higher mortality rate than breast, prostate and colon cancers6 The mortality rate within five years of a foot ulceration can be as high as 75%6
• Gangrene – where there is no longer enough blood supply to keep your residents' toes or feet alive and they start to turn black. In some cases, surgery can be performed to improve circulation, but in most cases, surgical removal (amputation) is required.
Given the health implications of poor foot health, you
would probably assume that every older person is entitled to foot care on the NHS. Sadly, and worryingly, that’s not the case.
NHS Foot Health departments generally have strict rules around who receives treatment. These are associated with the way your local NHS services are paid for by Integrated Care Systems (ICSs). To receive NHS foot care your residents generally must meet one or both of the following criteria:
1. Have a medical condition which places the foot 'at risk'.
2. Have a foot condition.
Only people who fall into criterion one would qualify for regular foot care, and even then, wait times between appointments are almost always over three months (except for those with diabetic foot wounds). That’s certainly not enough to prevent foot health issues from escalating and potentially impacting on the wider health of your residents.
Of course, you probably already know this and think you’ve got it covered by accessing a private foot care provider. However, the private sector brings a whole new set of problems…
Are you aware that there are currently no rules, regulations or professional guidance governing who can provide foot health treatments to your residents? Literally anyone can do it.
If your residents need oral health treatments, you will only allow a dentist to treat them. What about foot health? Are you certain you are only using a qualified and regulated podiatrist/chiropodist? Anyone can turn up to your home, call themselves a foot care specialist and charge your residents to treat their feet… no qualifications or training are legally required. All they require is the consent of their patient. This has led to a huge variation in the quality and safety of care being delivered across the care home sector.
While you would definitely notice if your visiting dentist was going from resident to resident in a communal area using the same toothbrush, do you notice if your foot health provider does the same cutting toenails? No changing of instruments, no changing of gloves, no hand washing, no respect for your residents' dignity, and on their part no training or membership to any regulatory body to know that they are putting your residents at risk. The lack of regulations on who can provide foot care to your residents means you should never assume a visiting provider is qualified and regulated. Putting aside that an individual with no qualifications will not be able to treat the conditions and pick up on the early warning signs previously mentioned, not ensuring your visiting providers are qualified (and Health and Care Professions Council [HCPC] registered) leaves both your care home staff and residents extremely vulnerable.
You would expect in an industry as well established and monitored as care homes, with a service that is so essential and as widely accessed as foot health, that there must be some clear and comprehensive guidance for you on what your residents should have access to? Unfortunately, you’d be wrong.
The National Minimum Standards, Care Home Regulations 3rd ed 2006 sets out the Department of Health and Social Care's (DHSC) key guidelines for care homes in the UK. This document states that foot health should be part of your residents’ initial needs assessment and that you should provide access to chiropody.
That is it. Nothing further to guide you through the confusing process of finding an appropriate foot health provider and then knowing what services they should be providing to adequately fill the gaps left by NHS services. This is all the more worrying when you consider just how confusing the private foot care industry is.
As standard, private foot health is paid for directly by care home residents, meaning your care home is not directly involved in the transaction between the resident and the clinician. Too often this results in poor sharing of information between the clinician and your nursing team, resulting in a lack of continuity of care and foot health concerns escalating. This all too often culminates in your residents needing treatment that could, and should, have been avoidable. Similarly, with the resident-clinician transaction the private provider is not at liberty to add to a resident’s care plan, potentially leading to your nurses making significant errors in care. This was one of the CQC’s key criticisms of dental care in the care home sector.
In most cases, a visiting foot health provider will only have an informal agreement with the care home manager with no established contract or terms of business in place. This can lead to inconsistent and questionable clinical standards and health, safety, and infection control practices. With no formal contract in place, who is responsible for your residents’ feet – is it the employed nursing staff or the foot care provider who turns up every six to 10 weeks with no contract?
The lack of regulations and professional guidance on who can deliver foot health treatments to your residents, coupled with the lack of regulations and professional guidance on what these treatments should look like, create the perfect storm for inadequate foot health provision across the care home sector. This should not be neglected, especially when foot health has such a significant impact on your residents' overall
health outcomes.
To mitigate this, Care Home Podiatry’s ‘Campaign for Better Foot Health’ has put together a detailed step-bystep ‘how to’ guide. The guide simplifies the process of sourcing a foot health provider and provides clarity on the services you, and most importantly your residents, should be receiving for their investment. You can access this free guide here:
Your residents are already paying for their foot health treatments. The only difference between these treatments being a simple toenail trim or being comprehensive healthcare treatments that prevent pressure sores, ulcerations, falls, amputations, and mobility issues, is you demanding that your residents get what they rightly deserve.
It's time that your residents and your staff get more out of your foot health provider. It really is a matter of life or limb.
1. Dunn, J.E., Link, C.L., Felson, D.T., Crincoli, M.G., Keysor, J.J. and McKinlay, J.B., 2004. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. American journal of epidemiology, 159(5), pp.491-498.
2. López-López, D., Becerro-de-Bengoa-Vallejo, R., Losa-Iglesias, M.E., Palomo-López, P., RodríguezSanz, D., Brandariz-Pereira, J.M. and Calvo-Lobo, C., 2018. Evaluation of foot health related quality of life in individuals with foot problems by gender: a cross-sectional comparative analysis study. BMJ open, 8(10), p.e023980.
3. Rapp, K., Becker, C., Cameron, I.D., König, H.H. and Büchele, G., 2012. Epidemiology of falls in residential aged care: analysis of more than 70,000 falls from residents of bavarian nursing homes. Journal of the American Medical Directors Association, 13(2), pp.187-e1.
4. Menz, H.B., Auhl, M. and Spink, M.J., 2018. Foot problems as a risk factor for falls in communitydwelling older people: a systematic review and meta-analysis. Maturitas, 118, pp.7-14.
5. Sinclair, A.J., Gadsby, R., Penfold, S., Croxson, S.C. and Bayer, A.J., 2001. Prevalence of diabetes in care home residents. Diabetes Care, 24(6), pp.10661068.
6. Robbins, J.M., Strauss, G., Aron, D., Long, J., Kuba, J. and Kaplan, Y., 2008. Mortality Rates and Diabetic Foot Ulcers: Is it Time to Communicate Mortality Risk to Patients with Diabetic Foot Ulceration?. Journal of the American Podiatric Medical Association, 98(6), pp.489-493.

In the ever-evolving landscape of social care, negotiating funding and securing the necessary resources has become an increasingly complex challenge for providers. Having the right evidence and insights becomes paramount at the negotiating table. Fraser Rickatson, Policy and Public Sector Officer at Care England, discusses its new Market Intelligence Tool, a game-changer designed to equip care providers with the latest funding and market data.
Negotiating fees and securing the proper level of funding from local authorities and ICBs is a well-known challenge for providers, exacerbated by significant rises in cost and public funding pots reducing over many years. While social care cannot be delivered on a shoestring, providers are often forced to do 'more for less', operating on unsustainable margins. Now more than ever, it is critical to have the right evidence available to strengthen their position at the negotiating table. However, knowing what evidence to collect, and maintaining this information as accurately as possible, can be difficult when both time and resources are already stretched. MINT, Care England’s Market Intelligence Tool, is a solution which gives care providers the latest funding and market data to offer a lifeline ensuring that, at a local level, they are well-equipped to secure the funding needed from public funders.
MINT hosts a funding dashboard for every commissioning local authority in England, offering evidence of what fee rates each local authority said they’ll pay, what rates they are actually paying and what rates they should be paying with regional comparisons and MINT allows for comparison between specific authorities or historic financial data. MINT hosts exclusive data that’s not available elsewhere. It identifies the commissioning practice for every local authority for the next three years, including data on current and future local capacity and demand.
This information is partnered with a breakdown of how each authority has used recent funding to increase fees, reduce waiting times and support recruitment and retention.
MINT doesn’t just give access to funding information but offers an in-depth analysis of local areas to help understand the provider's position within the market. Taking data from the CQC, MINT projects a heatmap of any area, identifying all the local competitors and giving insight into their size, service type, occupancy and CQC rating. In addition, providers can see how much each local authority is paying competing providers by different service types, which is important data to help build a case for further funding or negotiating fees. MINT highlights nearby pharmacies and health services, providing relevant contact information and their CQC rating (where applicable) to help understand which organisation’s relationships can be forged locally.
The data within MINT is ever-expanding and evolving to develop sector data to ensure residential care providers have all the information essential to ensure a successful negotiation of care home fees. Some of the latest data sets include average private fees per service type per local authority area and in addition, as local authorities and ICBs move toward eco-friendly practices, the tool offers written confirmation on how provider ESG strategies will influence their commissioning practice. MINT also contains key data insights on continence, CHC and FNC payments for every ICB including average minimum and highest rates offered.
Having access to all this information is important. It is equally important to know how to use this effectively. MINT provides users resources developed by Care England, their legal partners, and wider stakeholders to guide care providers with the process of challenging and negotiating fees, utilising the information provided, including briefings, recordings, template letters and calculation sheets. MINT contains all the contact information individual providers need to engage with at both local authority and ICB level, to ensure their voices are heard.
The ambition with MINT is to ensure that care providers are the most informed people at the negotiating table and have this critical information accessible in an instant. Knowledge is power and MINT empowers care providers to secure the funding needed to not only survive, but to thrive.

Providers continue to face significant challenges in not being paid fair and sustainable rates to meet the needs of the people they care for. Ramjeet
Kandola and Laura Jordan, Partners at Anthony Collins Solicitors, explain what
providers can do to prepare for challenging fee negotiations.
Years of underfunding by central Government has led to public bodies not receiving the extra funding required to increase provider fee rates. The latest 9.8% increase in the National Living Wage, along with the freezing of the employers’ national insurance threshold, will have a considerable impact on a provider’s cost base. Inflation remains high and the Local Government Association recently reported that one in five local authorities are at risk of serving a Section 114 notice (according to the Local Government Act 1988). Social care is deemed a core service and therefore should not be impacted; however, the long-term viability of many providers is increasingly coming under scrutiny.
Firstly, providers should determine the actual cost of care to establish whether the contract with the commissioner is both sustainable and considers the best interests of the individual.
If the data shows the commissioner is not paying at a sufficient level to preserve the best interests of the person supported, the contract with the commissioner should be
reviewed carefully to establish whether it provides for an automatic uplift or whether there is a discretion to review fees. Negotiating will always be recommended as a starting point to agree on terms amicably and to maintain a good working relationship with the commissioner. Contracts contain many levers providers can utilise to exert pressure on commissioners. Providers should be proactive and assertive.
Remind the local authority of their duties and obligations under the Care Act 2014 and the statutory guidance that accompanies it. Inform the authority of the reasons for the review; it may be because the rates are insufficient for care to be provided in compliance with statutory wage requirements and at the level of quality required, or due to the provider’s necessary costs to deliver great-quality care outweighing the fees being received.
Providers should establish a clear narrative with their operational, commercial and finance colleagues. Be clear on the objective and what the minimum price is that must be achieved so that they can negotiate properly and confidently. There needs to be a long-term plan and colleagues need to be persistent in bringing commissioners to the negotiating table.
It is important to review the local authorities’ market sustainability plans and market position statements available on their websites, along with market sustainability

improvement fund reporting and capacity plans (many of which are available via the Care England MINT system and website) to ascertain specifically what the local authority’s key priorities, challenges and target areas are.
For health-funded placements, ICBs are required to have regard to the National framework for NHS continuing healthcare and NHS-funded nursing care document for the NHS (the 'Framework'), and the NHS payment scheme (specifically section 3), which sets out the principles which must be applied when agreeing on any payment approach in the best interests of people. Under the Framework, ICBs are required to promote transparency and ensure that providers and ICBs engage constructively when agreeing to a payment approach. It is worth reviewing the Framework of individual ICBs and ascertaining whether ICBs have accountability and transparencyrelated policies, to see if they are complying with their own arrangements and the NHS payment scheme. This will no doubt assist as a lever to ensure there is transparency in their decision-making.
It may well be worth providers reminding ICBs of the requirement for the continuing healthcare decision-making process to be person-centred. Providers should help the person supported to express their wishes as part of any negotiations and remind ICBs that they are under a statutory duty to involve service users. It may be helpful for an advocate to be appointed for the person supported to assist with ensuring their voice is heard in relation to the ongoing funding of their care.
Providers should also remind ICBs that the Framework requires ICBs to ensure that fees paid are based on genuine costs of the individual’s needs, and/or the provider’s actual costs and must not therefore be setting arbitrary assumed costs or limits.
Also, submitting a Freedom of Information Request can often be beneficial to ascertain information on what the commissioner is paying others and how they are calculating fees. Finally, as some ICBs are failing to even respond to fee negotiations, one way of seeking engagement from the ICB is to submit a formal complaint to the ICB internal complaints team.
If negotiations fail, it may be necessary to check any termination clauses in the contract with the commissioner if the contract is not sustainable and the best interests/care needs of the person cannot be supported due to the low funding. Threatening termination (if termination is permitted without cause) may also lead to the commissioner negotiating on more favourable fees for the provider if the provider genuinely is unable to sustain services needed at the rates paid.
If a person’s needs cannot be met by the low fees paid by the commissioner, then given the risk to the supported person’s wellbeing as the safety of their placement is under threat, providers could also consider if reporting a safeguarding concern against the local authority is an option. Ultimately, it is important to ensure that commissioners are behaving appropriately and hold them accountable if not. Along with reporting a safeguarding concern, providers can also escalate concerns to ADASS, the LGA and the Parliamentary Health Service Ombudsman (in the case of ICBs). Anthony Collins can assist providers should they wish to pursue these routes as part of negotiations.
The ultimate sanction could be the threat of a judicial review claim against the commissioner if they are failing to comply with its public law duties.
If negotiations fail then unfortunately it may be that more formal legal action, depending on the prospects of success, must be taken. Gathering evidence by way of financial information is therefore key throughout the process.
Ramjeet Kandola is a Partner at Antony Collins Solicitors.
Email: ramjeet.kandola@anthonycollins.com
Laura Jordan is Head of Corporate Law at Anthony Collins.
Email: laura.jordan@anthonycollins.com


Helene Jones, UK Head of Care Homes at international multi-service provider Elis, explores some of the hidden factors driving up the cost of care home laundry.
Care homes with an in-house laundry facility are rarely able to say with accuracy how much in-house laundry costs. From investment in equipment to repair and maintenance, utilities, staff wages, agency costs, lost or damaged garments, and laundry supplies, there are a number of elements that need to be factored in. With inflation remaining high and energy unit rates rising once again, the cost of in-house laundry continues to increase.
Care providers need to be able to control costs and forecast expenditure and a professionally managed laundry service can ensure high-quality and efficient laundry management at all times, meaning the benefits of moving in-house laundry to a professional outsourced laundry service provider are not to be overlooked.
A review of in-house laundry processing in 48 care homes with an average of 37 beds showed that a typical facility of this size has two 13kg washers and two 13kg dryers running an average of 12 loads in each per day. This results in an astonishing and almost unbelievable cost of around £50 per resident per week to launder in-house.
The average cost was calculated using electricity, gas and water consumption rates for the washing and drying machines, detergent costs and hands-on staff time of 30 minutes per load at minimum wage, including loading and unloading the machines and minimal ironing and folding.
Astounded by the hidden cost of in-house laundry, Care England calculated the cost of a single full-time employee managing a laundry in a 40-bed care homes with two washers and dryers. This included the cost of energy consumption. Care England calculated the cost of labour and energy consumed alone to be around £35 per week without the additional
cost of consumables, equipment hire/purchase and maintenance costs.
A like-for-like comparison with professional laundry services highlighted that outsourcing provides an average cost saving of 35% even before savings on machine costs, maintenance and spending on replacement linen are factored in.
When it comes to initially setting up an in-house laundry facility, one of the major decisions to consider is whether to purchase or rent laundry equipment. With rental options, there is a reduced upfront cost and the supplier takes responsibility for upgrading and maintaining the machines. However, these agreements can come at a premium price point. One tactic is for equipment providers to tie care homes into lengthy contract terms or sell new contracts before expiry, tying care providers into even longer-term and sometimes more costly contracts for multiple years. This can mean that costly maintenance contracts are included.
Purchasing laundry equipment upfront is a major capital investment, especially considering the cost of commercial-grade machines capable of meeting the heavy demands of laundry duties within the care home. While it does have the advantage of providing the facility with full ownership of the equipment, and there are some tax advantages to CapEx, the ongoing costs associated with repair and maintenance can be unpredictable and quickly add up over time, especially if the equipment is not well managed or regularly inspected, tested and maintained.
It is estimated that around half of all care homes with in-house laundry facilities suffer
a machine breakdown once every six months, and for some this can occur as many as four times per year, causing significant disruption. As well as this disruption, equipment failure can have major financial implications. Not only is there the cost to service and maintain items, including parts and labour, but there may also be the requirement to outsource laundry services at short notice temporarily. Some care homes have no option but to use the local launderette, for which there can be a premium to pay.
Energy is a significant element of in-house laundry costs. Energy commodity price volatility began mounting in December 2021 when reports of a potential Russian invasion of Ukraine increased. In the first two weeks after the invasion, the prices of oil, coal and gas went up by around 40%, 130% and 180% respectively.
Initial support was provided in the form of the Energy Bill Relief Scheme, which was applied to energy usage by non-domestic customers in Great Britain and Northern Ireland from 1st October 2022. This was later replaced by the Energy Bills Discount Scheme which is set to expire on 31st March 2024 and offers nothing to care home providers unless the energy rate increases by around 300% from late 2023 levels. As energy unit rates have once again risen as a result of global gas prices, it is difficult to predict what the future may hold.
Last year, energy regulator Ofgem admitted that some suppliers may be charging small companies rates that cannot be justified and Care England warned that care home energy bills had soared by 500%, leaving a third of establishments across England considering closure because of ‘financially crippling’ running costs. Care home operators or managers are keenly aware of the impact of high prices and market volatility but have not always considered exactly where their energy is being used and the most effective ways of reducing consumption.
In-house laundry is an energy-intensive process and as well as the power required to wash garments, there is also the drying and pressing to consider. Consumer group Which? has suggested that domestic households can save energy by washing at lower temperatures, but unfortunately, this is not an option for care homes due to infection control and prevention guidelines and the need to ensure compliance with the Department of Health’s HTM01-04 policy.
Water consumption is another major contributor to utility costs in care home laundries. With high volumes of laundry being processed daily, water usage can quickly add up and inefficient or outdated washing machines can consume more water than necessary. A professionally managed laundry service can deliver enhanced operational efficiencies. For example, by the end of 2021, Elis had successfully reduced water consumption per kilogramme of linen delivered in its European laundries by 40% compared to 2010 levels and aims to increase to 50% by the end of 2025. Targets like these are not currently on the agenda or even possible for most care services.
Some of the ways in which this improvement in water consumption can be achieved include optimising the amount of detergent according to the actual weight of the textiles and utilising new types of detergent and activation technologies in a controlled environment, with carefully monitored programmes and processes which are not possible in a care home.
When it comes to in-house laundries, when staff members manually measure and dispense detergent there is a risk of error in dosing. Too little detergent can lead to ineffective cleaning, while overdosing is not only a waste of resources but can also cause build-up or residue in machines resulting in clogs and decreased performance. This can lead to ineffective laundry and increased maintenance and repair costs, further adding to the overall cost of in-house laundry.
While automated dosing systems can help to address such issues, they can do little to mitigate against the rising cost of consumables such as detergents and fabric conditioners. This is one area where the effect of high inflation has been keenly felt over recent months, resulting in additional impact on the bottom line for many care home facilities. Professional laundry service providers can purchase detergents at bulk rates, generating significant savings compared to individual care homes purchasing detergents independently.
‘Time is money’ rings true when it comes to care home staff who collect garments, load machines, and wait for wash and dry cycles to finish, then press, fold, and sort items before they are returned to each resident. In-house laundry is a never-ending, resourcefully
draining process that requires significant and constant input from employees at times, detracting valuable staff from the provision of care.
Those laundering in-house will understand how time-intensive this can be, especially considering the high volume of laundry that needs to be processed daily. Time spent searching for lost or misplaced items can also have an adverse effect, as well as causing distress to residents if items cannot be relocated and can lead to significant replacement costs by the care provider.
Space is a major issue for care homes. While it has been traditional to install, equip and operate in-house laundries, those that have chosen to outsource this service have benefited greatly from the opportunity to reclaim valuable space. This could be space that is used for other operational activities, staff areas, storage, to provide enhanced facilities for residents and/or other revenue opportunities.
Cupboards for storing clean linen and a separate area for handling soiled items are still required to ensure compliance with Government HTM01-04 guidelines for the decontamination of linen for health and social care. However, these are likely to take up a significantly smaller area than a typical, in-house, infection-control-compliant laundry.
As well as providing a rental and reprocessing service for flat linen items, professional laundry service provider Elis offers a personal service for laundering residents’ clothing where every resident is provided with their dedicated mesh bags, with separate bags available for delicate garments where each bag is typically labelled with the resident’s name and a unique QR code. Bags are collected and scanned on arrival at the facilities. They are then tracked through the washing, drying, and finishing process before being wrapped and returned. As a result, items linked to individual residents are traceable throughout the entire laundering process, leaving less room for error and resulting in a smoother and more efficient service.
Insurance premiums can also be reduced due to a lower risk of fire or staff injury, while
using a flat linen hire service where the laundry company provides all linen and towels offers further financial benefits by freeing up capital that would otherwise be used to purchase items.
As professional laundry suppliers operate on an industrial scale, they can process items more efficiently and pass savings on to customers by using machines designed to process the equivalent of around eight to 10 conventional loads of washing in one go and using energy recovery to ensure the environmental impact of the laundry process is much lower than can be realistically achieved in a care home.
Outsourcing laundry services relieves employees from the task of dealing with equipment breakdowns and maintenance issues so, instead of spending time troubleshooting or managing machine servicing schedules, staff can dedicate their energy to residents’ needs. Ultimately, this means more time for resident interactions, personalised care, and engaging activities that will contribute to residents’ happiness and wellbeing, as well as staff morale.
Staff can also be repurposed from working full or part-time in a laundry to providing frontline care or fulfilling other essential roles, helping to reduce the cost of agency staff and overtime etc.
There is no ‘one size fits all’ approach to laundry but we know that there are significant savings to be made from outsourcing to a professional laundry service for some care providers, as evidenced in recent case studies. This is why Care England has proudly partnered with Elis to offer care providers the opportunity to complete a cost-benefit analysis for in-house vs outsourced laundry services. Care homes of all sizes are invited to take part, from individual facilities to larger corporations, to accurately identify the ‘tipping point’ for each provider at which outsourcing laundry services becomes a more viable option in terms of costs and resources.
For more details on outsourced care home laundry services or to complete a cost-benefit analysis for your organisation, please contact: Helene.Jones@elis.com.
Helene Jones, UK Head of Care Homes at international multi-service provider Elis. Email: Helene.Jones@elis.com @ElisGroup
At Care England, we are always keen to hear from our members and we strive to answer any questions and queries our members may have. In this issue of Savings, Solutions, and Sustainability, George Appleton, Head of Policy at Care England, and Charlotte Lezard, Policy and Public Affairs Officer at Care England, provide the answers to support providers on the Energy Savings Opportunity Scheme and CQC Assessment Framework, and also update on workforce and immigration policy and share how to navigate an inquest.
Q: Work has begun on our organisational ESG strategy. This has been made easier thanks to Care England’s SMART system. Can I clarify whether the Energy Savings Opportunity Scheme (ESOS) is mandatory for companies that employ more than 250 people?
George Appleton: I am pleased to hear SMART has been helpful! As per GOV.UK, for the qualification date for the third compliance period of ESOS (31st December 2022) a large undertaking is any UK company that either: employs 250 or more people, or; has an annual turnover in excess of £44m, and an annual balance sheet total in excess of £38m. You must take part in ESOS if your undertaking is part of a corporate group which includes another UK undertaking or UK establishment which meets these criteria. I don’t believe you would have been contacted as an organisation; it is a self-registration process, details of which can be found through GOV.UK.
Q: What tips does Care England have for providers to help navigate the impact of an inquest and to be ready to deal with any action arising?
Charlotte Lezard: Many providers will at some point be involved in an inquest by virtue of the delivery of
care and services to the elderly and vulnerable. As soon as there is a death of a service user, the provider must notify CQC if the person died whilst a regulated activity was being provided and the person’s death may have been a result of the regulated activity or how it was provided. The death may also be reported to the coroner’s office. Following this, investigations may progress. Providers should follow a protocol or checklist to minimise disruption to the business and to enable them to respond to concerns raised swiftly.
Care England’s legal partner, Weightmans, has prepared ‘Practical tips to prepare for an inquest’ which is available through the Care England website. Care England members can also avail themselves of 15 minutes' free consultation with one of the Weightmans' solicitors. To redeem this offer, please contact info@ careengland.org.uk.
Q: How significant do you anticipate the migration changes to the number of dependants able to come with an overseas recruit will be?
GA: On 4th December, the Home Secretary announced significant changes to the immigration system,

14

CLICK TO BOOK
This conference focuses on what Care England and the sector is doing to improve the quality of care, with presentations from key sector and government figures, and both exhibits and seminars from leading product and service suppliers.
16 -
A free event held by Care England and DP Events for care providers to net work with sector peers, and meet specialist suppliers, including an overnight stay at the Crowne Plaza Hotel, Stratford-upon-Avon.
24 -
London
including an increase in the minimum annual salary required for employees applying for a skilled worker visa in the UK from £26,000 to £38,700; however, those on health and care visas will be exempt, as well as measures to stop workers from bringing dependants.
Care England had no insight into the immigration announcement but is now working with the Department of Health and Social Care and the Home Office on what the key issues will be for the sector.
Care England’s Chief Executive, Professor Martin Green OBE, gave evidence to the Health and Care Select Committee on 19th December 2023 to discuss the magnitude of these changes.
Care England has a panel of international recruitment experts on hand to discuss these issues with care providers which is available on the Care England website.
Q: As we approach the fee uplift period, what resources are available to support care providers?
CL: Care England has continued to work at all levels of Government, from ministers to senior cabinet members, to highlight the key issues affecting the adult social care sector and the principles which underpin good practice in the context of funding decisions, including what good engagement looks like, maintaining transparency in decisions, and how decisions are made based on the availability of provision within the local market etc.
Care England is working to establish a priority of local authorities to engage with. To do this, we will be using the data we have available to care providers via our Market Intelligence System, MINT, as well as wider data from the cabinet minutes, to help understand the rationale for funding decisions and how these should be escalated and challenged.
We also have work that has been produced by some of our legal partners which gives Care England members an arsenal of template letters and information to help influence and challenge fee decisions. These are available via the Members Area of the Care England website.
Q: The CQC’s new single assessment framework has a quality statement on environment sustainabilitysustainable development. How can providers prepare to be assessed on this?
GA: According to the CQC’s website, environmental sustainability will be assessed in NHS trusts (at trust level) and as part of the ICS assessments for the first year of the Single Assessment Framework. Other service types will not be assessed on the environmental sustainability quality statement for the first year.
While the CQC is still developing its approach to assessing this quality statement, we can anticipate the CQC will look at what your service is doing to mitigate any negative impact your service has on environmental issues, and how people you support and who work in your service are making a positive contribution to reducing their impact on the environment.
To prepare, it’s worth making sure your staff know what environmental policies you have in place, on issues such as renewable energy, sustainable transport, food waste etc. SMART has a dedicated ESG module which outlines areas a provider can consider when working towards ESG targets.
Care England knows how important it is for providers to be informed, so we hosted a webinar with sector experts RSM and CQC on how to make ESG work in the care sector. You can find a copy of the recording by visiting https://www.careengland.org.uk/events/esgwhat-is-the-direction-of-travel-for-the-care-sector/.



If you work in adult social care, Macmillan’s Social care community on the Learning Hub is the go-to place for free education and training on cancer care.
There are over 20 on-demand e-learning courses, bitesize resources and virtual classrooms to develop your knowledge and skills in supporting people affected by cancer.
This community is for all staff working in adult social care who want to improve their understanding of cancer and skills in supporting people affected by cancer. This includes staff working in residential care, nursing homes, home care, sheltered accommodation, assisted living and day centres.
In the community you’ll find the following topics:
• Cancer awareness
• Cancer and other conditions
• Communication skills
• Personalised care
• Palliative and end of life care
Scan the QR code to log in or register for an account, then search ‘Social care community’
Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). Also operating in Northern Ireland.


Proud to have supported almost care workers with over
£
Support us to help even more
