INCLUSIVE CULTURES A new LGBTQ+ framework Rebuilding lives Settling disputes Looking overseas A balancing act Supporting people affected by homelessness Navigating employment tribunals Technology best practice Enabling care home visits DECEMBER 2022 www.caremanagementmatters.co.uk





Are your care staff being weighed down by the burden of maintaining paper-based care records? Using a Digital Care Planning System doesn’t have to be daunting! A simple way for staff to create care plans and log care as it happens Used by over 3,500 care providers 40% Staff retention increase Number 1 choice for care staff More time to care Reduces stress Facilitates teamwork Book a demo with us today Scan me to find out more 01483 357 657 hello@personcentredsoftware.com www.personcentredsoftware.com
Social care insights
Simon Bottery rewrites A Christmas Carol
Inside CQC
Debbie Ivanova, Director for People with a Learning Disability and Autistic People, outlines what needs to happen to improve the way we support people receiving care in hospital settings.
CMM News
Into Perspective
CMM asks the experts about what can be done to increase coproduction on care planning.
Celebrating Excellence
Find out about the 2022 winners of the Compassion Award and the Leadership Award at the Markel 3rd Sector Care Awards.
Event Review

A look at the Berkshire, Buckinghamshire and Oxfordshire CMM Insight conference.
What’s On?
Straight Talk
Melanie Weatherley MBE of Lincolnshire Care Association shares her thoughts on the CQC’s State of Care report.
In this issue REGULARS
The evolving recognition of identity: How to create and maintain inclusive cultures
NHS Confederation’s Health and Care LGBTQ+ Leaders Network has set out six pillars of inclusivity. Dr Layla McCay, Director of Policy at NHS Confederation and Executive Lead of the Network shares the details.
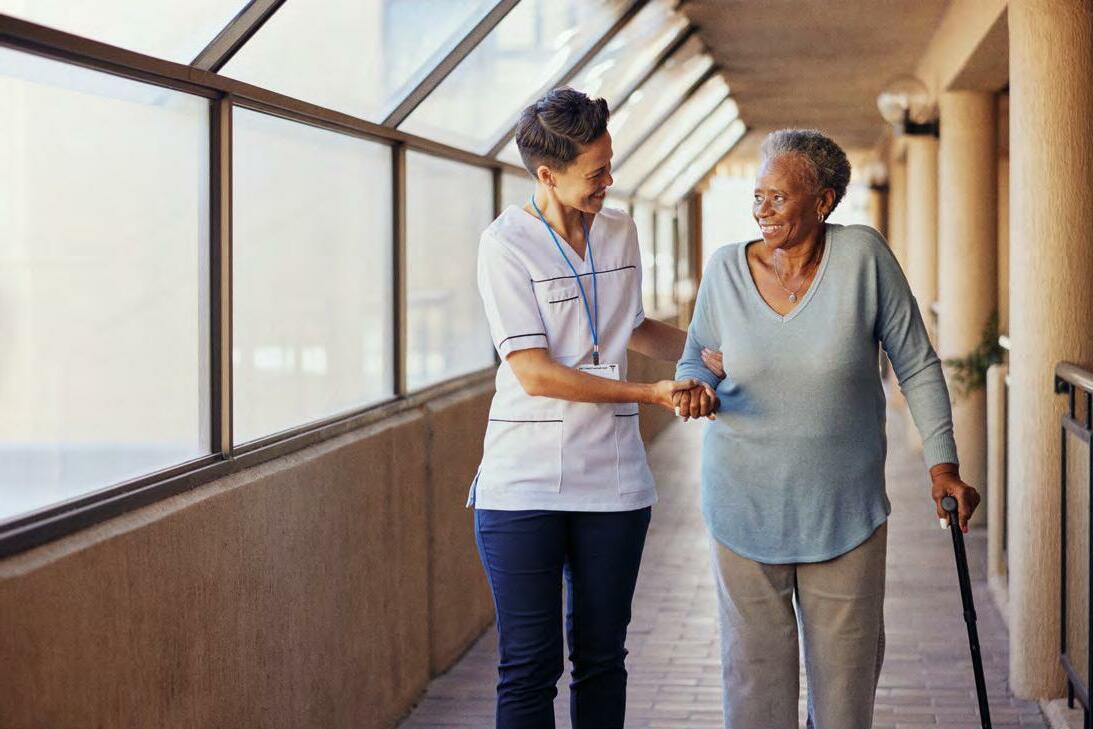
A balancing act: Working with local health teams to facilitate care home visits How can providers ensure the least restrictive measures are in place this winter? Helen Wildbore, Director of the Relatives and Residents’ Association, offers her advice on balancing opinion.

Rebuilding lives: Enabling the right care for people affected by homelessness
Rebecca Sycamore, Executive Director of Strategy and Development at St Mungo’s, offers suggestions on improving social care support for people who have experienced homelessness.



Settling disputes: Preparing for employment legal challenges
CMM asked Alan Lewis, Employment Partner at Constantine Law, what lessons can be learnt from the pandemic.
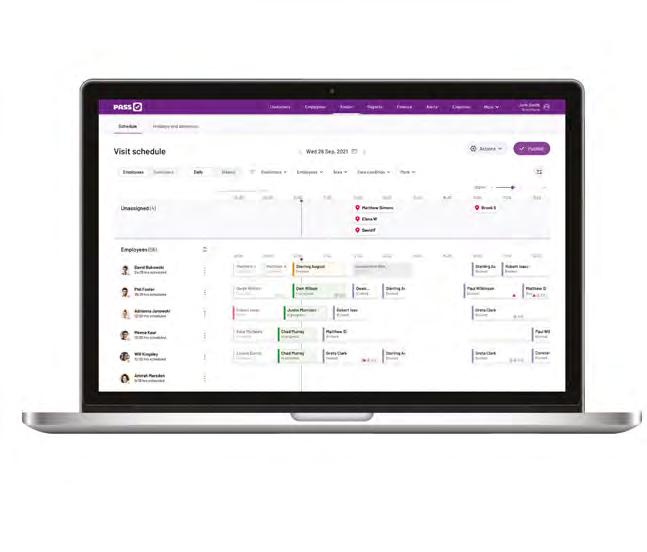
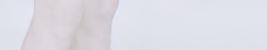
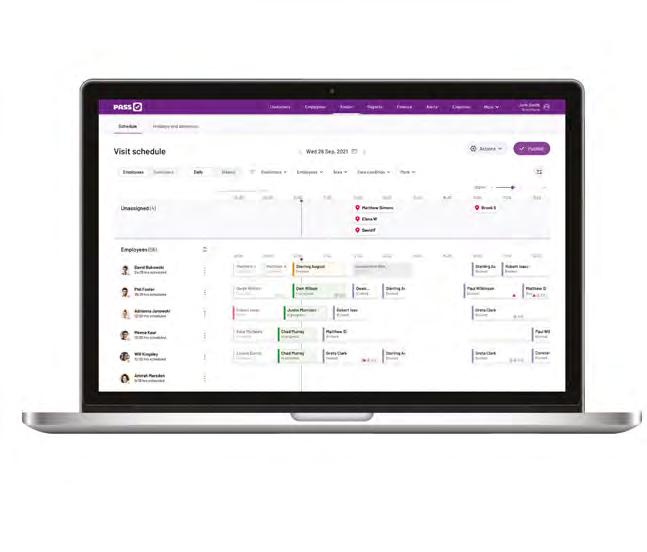
Looking overseas: How technology is being implemented across the globe
Technology is at the top of the agenda for many, so what can we learn from other countries? Andrew Coles, of Person Centred Software, shares best practice.
CMM December 2022 3
FEATURES
05 07 09 30 46 48 49 50
39 25
37
20 25 33
42 20 33 42
CONTRIBUTORS
EDITORIAL
editor@caremanagementmatters.co.uk

Editor: Olivia Hubbard
Commissioning Editor: Angharad Burnham

Content Editors: Aislinn Thompson, Henry Thornton

PRODUCTION
Designer: Rebecca Mendil
Director of Creative Operations: Lisa Werthmann Studio Manager: Jamie Harvey
ADVERTISING

sales@caremanagementmatters.co.uk 01223 207770

Assistant Advertising Manager: Aaron Barber aaron.barber@carechoices.co.uk
Director of Sales: David Werthmann david.werthmann@carechoices.co.uk
SUBSCRIPTIONS
Non-care and support providers may be required to pay £50 per year. info@caremanagementmatters.co.uk 01223 207770 www.caremanagementmatters.co.uk

Care Management Matters is published by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2022 CCL REF NO: CMM 19.9
@blimeysimon

Simon Bottery Senior Fellow in Social Care, The King’s Fund


@CQCProf

Debbie Ivanova Director for People with a Learning Disability and Autistic People, Care Quality Commission (CQC)
CMM magazine is officially part of the membership entitlement of:

@AnnaSeverwright
Severwright Co-convenor, Social Care Future

@learningdiseng

Jordan Smith Self-advocate and Co-chair, Learning Disability England's Representative Body

@LaylaMcCay
@relresuk @CQCProf
Dr Layla McCay Policy Director, NHS Confederation and Executive Lead, Health and Care LGBTQ+ Leaders Network.
Helen Wildbore Director, Relatives and Residents Association (R&RA)
@StMungos
Rebecca Sycamore Executive Director of Strategy and Development, St Mungo’s
@AlanLewisCL
Alan Lewis Employment Partner, Constantine Law
4 CMM December 2022
Andrew Coles Chief Executive, Person Centred Software
Christina Earl Head of Innovation and Business Development, Surrey Choices
David Higham Founder and Chief Executive, The Well Communities CIC
Melanie Weatherley MBE Chair, Lincolnshire Care Association
@SurreyChoices @PersonCentredSW @thethewell2 @MelanieWeathe12
Anna
SOCIAL CARE INSIGHTS
From Simon Bottery
Simon Bottery finds an unpublished version of A Christmas Carol with a Scrooge who doesn’t understand social care but with a surprise twist at the end.
Reader, I have discovered a long-lost – but sadly unfinished – version of Charles Dickens’ A Christmas Carol It focuses (anachronistically, I know) on adult social care.
In it, a mean-spirited character –he’s still called Scrooge – really doesn’t like social care. He doesn’t see the value it brings to people. He’s dismissive of the arguments that it enhances people’s wellbeing and makes us a better society in which to live. He distrusts the evidence that it supports economic growth. He’ll occasionally give it some money to help stave off problems in the health service (though he’s a bit curmudgeonly about that, too, thinking it a ‘bottomless pit’).
But he never gives more than he thinks is strictly necessary and it’s always a one-off donation, never the long-term regular income that social care needs.


All this changes one night when Scrooge is visited by three ghosts. The first ghost shows Scrooge that he’s always been dismissive of social care. He’s never really understood it or known many people who drew on it. He doesn’t think that he himself will ever need it. This Scrooge had his chance in 1948 to give it the same love, and money, as the health service but didn’t.
Scrooge isn’t convinced though. He doesn’t think the ghost fully understands fiscal responsibility.
The second ghost shows Scrooge social care as it is now. It takes him to the home of an elderly woman who is left isolated and in pain because her needs aren’t thought high enough to qualify for support, to the home of a younger disabled man who gets some support but not enough to allow him to live the independent life he wants and he visits a home
care worker who is stressed, exhausted and poor because she’s overworked and underpaid.
Still Scrooge isn’t convinced. He thinks that the ghost should reconsider the potential for cost savings and service efficiencies.
The third ghost terrifies Scrooge by showing him the future of social care if he continues on this path. Reader, I can’t fully describe to you what the ghost shows Scrooge because it is too scary. But it involves people being left cold and alone because there are not enough workers, 'for sale’ signs on care businesses and thousands of people selling their homes to pay for their care. It is, in truth, perilously close to what the second ghost has shown him.
Unfortunately, we don’t know for sure how Dickens intended this version of A Christmas Carol to end. However, from the author’s
handwritten notes, we suspect that Dickens didn’t necessarily plan the heartwarming about-turn that Scrooge makes in the famous, published novel.
Instead, it seems he intended a surprise reveal about the identity of Scrooge himself. Some believe that Dickens planned to unmask Scrooge as the leader of a semi-secret fiscal cult, thousands of people strong and operating at the heart of Government, which has had malign influence over social care policy for decades.
Others see the villain being revealed as the social care sector itself, so indecisive that it can’t decide what it really wants or unite to help bring it about – a sort of social care version of Hamlet.
But still others believe Dickens had something more philosophical in mind, with Scrooge revealed as, well, us. In this version, the public knows little about social care, prefers not to think about ageing and disability and prefers its money to be spent on shiny new hospitals. As a result, there is little pressure on politicians to bring about real and lasting reform in social care. In this last version, Dickens is holding up a mirror to our society and forcing us to face a reality we don’t like.
Which version is the real one? Perhaps all three. But the moral of the published version of Scrooge is that – in the right circumstances –attitudes (and policies) can change. And that, as Dickens knew, is a thought to get us through the cold, winter nights.
Happy Christmas.
CMM December 2022 5
Simon Bottery is a Senior Fellow in Social Care at The King’s Fund. Email: S.Bottery@kingsfund.org.uk Twitter: @blimeysimon
Which version is the real one? Join the discussions online and share your feedback on Simon’s column at www.caremanagementmatters.co.uk
Every need, quickly covered. Cards that put care first.

Help employees make urgent purchases on the go with Soldo prepaid cards. Without the hassle, without the paperwork – so they can get right back to caring.


“Now, when employees need to purchase anything, they can have the right funds in a matter of seconds. They can buy what they need and go back to their job helping residents straight away.”
Cairn Mhor, Residential Care for Children
Learn
how Soldo can empower your team at soldo.com/care
BROOKLYN SIMMONS HOME MANAGER
I’m sure many of you, like me, are driven by equal measures of outrage and delight.
When we see people living in services of their choice, organised around their needs and wishes, great things happen. However, this too often isn’t the case and, as our recently published State of Care report has shown, people with a learning disability and autistic people continue to face huge inequalities when accessing and receiving health and social care. This includes our Out of sight – Who cares? report which highlighted the consequences of people not getting the right care and support in the community when they need it. Only four of the recommendations for change have been partially met and 13 haven’t been met at all. It’s nowhere near good enough.
State of Care shows that while admission to hospital should be temporary, poor environments, lack of discharge planning and difficulties in finding suitable community placements is leading to people with a learning disability and autistic people staying in hospital for years. In our latest publication Who I am Matters we explore people with a learning disability and autistic people’s experiences in acute hospitals, focusing on their stories to illustrate what needs to change.
When hospital care isn’t right the consequences can be devastating. This report shines a light on the impact these failings have on people and their families. The foreword is difficult but important reading for all of us. It’s written by Oliver McGowan’s mum. Oliver was 18 when he died in hospital. The multi-agency review into the death of Oliver McGowan found that Oliver’s death was potentially avoidable. When we looked at Oliver’s story, alongside other multi-agency reviews, trends and themes started to emerge which led to us conducting our own review.
During February and March 2022, we visited eight hospitals in England. We saw pockets of excellent work. Particularly from specialists and people who had really good personal experience of people with a learning disability and autistic people in their own lives. However, nowhere did we see this happening in a way which was joined up or consistent. We looked at:
• Access to care.
• Communication.
• Care and treatment in hospital.
• Protected characteristics and equality of care.
• Workforce skills and development.
Access to care
Everyone has the right to expect access to the
Inside CQC
Debbie Ivanova, Director for People with a Learning Disability and Autistic People, outlines what needs to happen to improve the way we support people receiving care in hospital settings.

care they need when they need it and that appropriate reasonable adjustments are made to meet people’s individual needs. Whether it’s about who’s accompanying the person or how messages are given or explained, what’s important is that these adjustments start right at the first point of contact.
Communication
This is equally about how you communicate and how you listen. There are stories in our report where people were really not listened to. When time isn’t taken to make sure people's communication and ways of understanding are tailored to their individual needs, it’s difficult and sometimes impossible to provide good care. There isn’t a one size fits all solution.
Care and treatment in hospital
Everyone has the right to be fully involved in their care and treatment. We found many cases where this wasn’t happening, with not enough listening, communication, adjustments and involvement.
Protected characteristics
We found staff lacked understating around protected characteristics and equality of care, with a tendancy to focus on one aspect of the person. The protected equality characteristics of people with a learning
disability and autistic people will also be about age, race and sexual orientation. Often those risk being overshadowed because staff lack knowledge and understanding about inequalities overall.
Workforce skills and development
We saw some great practice, but specialist practitioners and teams can’t hold the sole responsibility for improving people’s experiences of care.
We must react differently
As well as being a key equality issue our findings show this is a critical patient safety issue. All too often we lose focus on people’s health needs in social care meaning they can be late getting support. Providers need to make sure staff have up-to-date training and the right skills to communicate, respect and understand people with a learning disability and autistic people. It’s about the whole piece not just the provision of care.
My challenge to everyone is to recognise that every person is going to be different and to respect that individuality. We must react differently. Now is the time for action and I encourage all health and care leaders to use the learning from our report to drive improvement – to recognise and respect each person's humanity and individuality and respond differently.
CMM December 2022 7
Debbie Ivanova is the Director for People with a Learning Disability and Autistic People at the Care Quality Commission (CQC). Twitter: @CQCProf
Share your feedback on the CMM website. Do you have a question for the CQC?
DEBBIE IVANOVA
Email editor@caremanagementmatters.co.uk
Learn how Sage can help:

software that helps care homes thrive
• Increase revenues by 25% without adding additional headcount.
• Save over 400 person-hours annually.
Download product brochure
• Streamline your operations and automate your financials.
CQC State of Care report published
The Care Quality Commission’s (CQC) annual assessment of the state of health and social care in England has been published. The report looks at the quality of care over the past year.
This year – based on CQC’s inspection activity, information received from the public and those who deliver care alongside other evidence – the CQC's assessment is that the health and care system is gridlocked and unable to operate effectively.
According to the CQC, most people are still receiving good care when they can access it. However, too often, people are
not able to access the care they need. Capacity in adult social care has reduced and unmet need has increased. Only two in five people are able to leave hospital when they are ready to do so, contributing to record-breaking waits in emergency departments following a decision to admit, and dangerous ambulance handover delays.
As part of the work, which included a series of co-ordinated inspections across the urgent and emergency care pathway in 10 Integrated Care Systems (ICSs), CQC convened a group of 250 health and care leaders – they described the
system they work in as ‘in crisis’ and shared their fears that the risk of people coming to harm represents a worrying new status quo.
CQC's State of Care reports that health and care staff want to provide good, safe care but are struggling to do so in a gridlocked system. This is reflected in growing public dissatisfaction with health and care services – which is mirrored in staff dissatisfaction. More staff than ever before are leaving health and social care and providers are finding it increasingly challenging to recruit, resulting in alarmingly high vacancy rates which have a direct impact on people’s care.
Chancellor delivers Autumn Statement
The Chancellor of the Exchequer, Rt Hon Jeremy Hunt MP, addressed the nation to outline the Government’s future financial plans.
The following financial commitments were outlined:
• The Government will make available up to £2.8bn in 202324 and £4.7bn in 2024-25 to help support adult social care and discharge in England. This includes £1bn of new grant funding in 2023-24 and £1.7bn in 2024-25.
• Further flexibility for local authorities will be given on council tax and a delay to the rollout of adult social care charging reform from October 2023 to October 2025.
• The Government is giving local authorities in England additional flexibility in setting council tax by increasing the referendum limit for increases in council tax to 3% per year from April 2023. Local authorities with social care responsibilities will be able to increase the adult social care precept by up
to 2% per year.
• £600m will be distributed in 2023-24 and £1bn in 2024-25 through the Better Care Fund to get people out of hospital on time into care settings, freeing up NHS beds for those who need them.
• £1.3bn in 2023-24 and £1.9bn in 2024-25 will be distributed to local authorities through the Social Care Grant for adult and children’s social care.
• £400m in 2023-24 and £680m in 2024-25 will be distributed through a grant ringfenced for adult social care to help support discharge.
• The National Living Wage will increase from £9.50 an hour for over-23s to £10.42 from April 2023.
While the Government recognises that some businesses may continue to require energy support beyond March 2023, the overall scale of support the Government can offer will be significantly lower and targeted at those most affected
to ensure fiscal sustainability and value for money for the taxpayer.
Richard Murray, Chief Executive of The King’s Fund, said, ‘The significant additional funding announcement for social care indicates the Government’s recognition of the perilous state of the sector. However, increases to the National Living Wage, hikes in energy prices and ongoing inflationary pressures will all add to social care providers’ costs. It also remains unclear how much of the additional funding may have to come from council tax rises and where today's proposals leave local authority finances overall.’
Dr Jane Townson, Chief Executive of the Homecare Association, said, ‘We have already seen the impact of the lack of capacity in homecare, with over half a million people on council waiting lists for care and thousands of people stuck in hospital unable to be discharged home. In turn, this is having a negative impact on waiting times for ambulances and treatment in the NHS. The
In response to CQC's latest State of Care report, Dr Rhidian Hughes, Chief Executive at the Voluntary Organisations Disability Group (VODG), said, ‘Government has the power to repair the gridlock reported by CQC, but political distractions and turbulence risk setting us off course. Government should provide £500m in financial support to enable social care services to overcome the difficult winter ahead. With a shared social care vision for the future, adequate funding and better pay and security for the workforce, we can enable millions of disabled people to live independent and fulfilling lives.’
Chancellor has recognised the fact that homecare simply cannot meet the demand, and we welcome the substantial investment.’
Adding, ‘We are concerned that some of the funding is based on increasing council tax. Councils in areas of higher deprivation with lower house prices will receive less funding for any increase in the rate. This will increase existing inequalities, exacerbating the post code lottery for care.’
Professor Vic Rayner OBE, Chief Executive of the National Care Forum (NCF), said, ‘I fear that for the remainder of this parliament, the ambition for reform of social care has been put on the back burner. There is little in this budget that talks to the vision of developing care with people at its heart. Social care is about people, not packages and whilst discharge is vital, great social care changes lives and matters to us all and it is imperative that over the next two years the Government keeps its commitment to develop care that is fit for the future.’
CMM December 2022 9 NEWS
ADASS president delivers conference speech
The Association of Directors of Adult Social Care Services (ADASS) President, Sarah McClinton, delivered a speech at the National Children and Adult Social Care Conference (NCASC).
The ADASS President said the sector must continue to focus on people and told delegates: ‘Be under no illusion, things have never been so bad.’
In November, ADASS published its Autumn Survey 2022. Fewer than one in 10 directors think they could manage with existing resources over the next few months. Three in four say they could not cope if a large care provider were to fail. 93% called for an immediate further injection of funding to be used flexibly at local level – in addition to a £500m 'discharge fund.'
Sarah McClinton said, ‘We need the future to be different; we can’t have more of the same


and we know what can work. As winter approaches, we need that Coffey money urgently. 'Successive governments of all political shades have promised to reform social care to make it genuinely fit for the 21st century. None have, so far, delivered on that promise.’
She concluded, ‘Adult social care cannot be an afterthought. At its very best it helps people to live active lives, to contribute, to work, to train, to volunteer, to have a safe home, to live free from abuse. It’s an opportunity – an opportunity to help people to build independence, an opportunity to support interdependency in our communities. We know how it can be, and how it can change lives.
‘How we look after each other says a lot about us as a society: we all owe it to each other to get it right.’
Care England asks PM to ‘save our sector’
Care England has written to the Prime Minister, the Rt Hon Rishi Sunak MP, calling for the Conservative manifesto promise to ‘fix social care’ to be delivered in his premiership. Points include:
• Reform delays – Any delay to the £1.36bn funding provisioned for the Fair Cost of Care to address historic underfunding of social care and move fees closer to a Fair Cost of Care will have catastrophic effects. The original timeframe for reform introduced by the 2019 election-winning Government must be respected.
• Energy – To withdraw the current measures of support after 31st March 2023 would be an immense oversight by the Government. It must be ruled out as a matter of urgency.
• Funding – Current funding provisions are insufficient and the Government must commit
to substantial increases in funding to stabilise the sector and enable it to move towards a sustainable footing.
• Workforce – Despite being the social care sector’s greatest asset, it is currently in a rapidly worsening crisis. We urge the Government to introduce a fully funded workforce plan.
Professor Martin Green OBE, Chief Executive of Care England, said, ‘Care providers deliver essential care to many of society’s most vulnerable; Mr Sunak has the opportunity and responsibility to ensure these individuals, and the high-quality care they receive, are protected in the long and short term. Care England is looking forward to building on our long history as a critical friend to Government and assisting in a pragmatic Government response that is needed to save our sector.’
10 CMM December 2022 NEWS
Now is the time to go digital uk.autumn.care info@autumn.care 0800 009 2121 10 key reasons care providers are choosing to go digital, what will yours be? 10 KEY REASONS BOOK A DEMO Book a demo to find out how AutumnCare can help
DHSC publishes £500m Discharge Fund plan


The Department of Health and Social Care (DHSC) has published details of how the £500m Discharge Fund will be distributed to help free up hospital pressures and reduce strain on the NHS.
£300m will be given to integrated care boards (ICBs) to improve bed capacity and £200m for local authorities to bolster the social care workforce, increasing capacity to take on more patients from hospitals.
Local authorities and ICBs will work together to agree on spending across their regions, introducing tailored solutions which speed up discharge and benefit patients in their area.
Allocations will be published in due course with payments to be made in the coming weeks, following the announcement of the fund earlier this year. A second tranche of funding will be distributed in January 2023,
delivering support across winter.
On tackling the COVID-19 backlogs, the Health and Social Care Secretary, Steve Barclay, emphasised the importance of close working between the DHSC and NHS England to reduce variation and tackle wider recovery challenges.
Helen Whately, Minister of State for Care, said, ‘Our Discharge Fund will get more people cared for in the right place at the right time. We’re asking hospitals and the social care system to work together to help patients and carers too, who often take on a lot of the burden of caring when someone leaves hospital.’
Adding, ‘The Discharge Fund will boost the social care workforce and in turn reduce pressures on the NHS and hospital staff, as it frees up beds and helps improve ambulance handover delays.’
Carers UK State of Caring 2022
New findings by Carers UK reveal that unpaid carers, and the older and disabled people they support, are facing serious difficulties receiving NHS treatment and their health is deteriorating as a result.
A third of carers (34%) waiting for specialist treatment or an assessment have been waiting more than a year – with a similar proportion, 31%, saying the person they care for has also been waiting for more than a year.
It is affecting a third (32%) of carers’ attendance at work, rising to 45% of carers who have been waiting for more than 18 weeks. Two thirds of carers (67%) waiting for treatment say it is having a negative impact on their mental or physical health, with many left in pain and unable to carry out their caring role. A lack of reliable support from care services in
the community is seeing one in five carers (22%) tell Carers UK that their loved one’s emergency admission into hospital could have been prevented with higher quality care and support in place.

Helen Walker, Chief Executive of Carers UK, said, ‘Gridlock in hospitals and lengthy NHS waiting lists, combined with a perpetual shortage in care services and the cost-of-living squeeze, is forming the perfect storm for unpaid carers to collapse. They have nowhere to turn.’
Carers UK is also urging the new Prime Minister to uprate carer benefits in line with inflation at the earliest opportunity so that hard-pressed carers can afford to eat and heat their homes.
You can read the report, State of Caring 2022 on the Carers UK website.
When industry knowledge and wisdom are needed, when a discreet sale is desired, our clients choose DC Care to sell their healthcare business. SALES | ACQUISITIONS | APPRAISALS | CONSULTANCY 01937 849 268 www.dccare.co.uk sales@dccare.co.uk specialist healthcare business agents Independent expertise Nationwide knowledge Bryn Estyn, Rhyl, North Wales - Reg 24 SOLD specialist healthcare business agents 20TH ANNIVERSARY DC Care is delighted to confirm the sale of Bryn Estyn Care Home, an immaculately presented residential care home registered for a maximum of 24 residents, located in the North Wales town of Rhyl. NEWS CMM December 2022 11
The Oliver McGowan Mandatory Training launches
The Oliver McGowan Mandatory Training on Learning Disability and Autism, to assist health and care staff caring for and supporting people with a learning disability and autistic people, has been launched following a long campaign.
To help with the development, the training has been developed in partnership with Health Education England, Department for Health and Social Care, Skills for Care and NHS England, and is available for staff across the health and care sector to access.
The training is named after Oliver McGowan, who died in 2016 after being given antipsychotic medication, despite warning
that it was unsuitable for him, highlighting a lack of understanding of the needs of people with a learning disability or autistic people. Oliver’s mother, Paula successfully launched a campaign to make training on caring for people with a learning disability and autistic people mandatory for all health and care staff.
The Health and Care Act 2022 introduced a requirement that Care Quality Commission (CQC) registered service providers must ensure their staff receive training on learning disability and autism that is appropriate to their role.
The Oliver McGowan Mandatory Training comes in two tiers and is designed so staff receive the right level of mandatory training.
Tier one has been designed for staff who need general awareness of the support autistic people or people with a learning disability may need, while tier two is for people who may need to provide care and support for autistic people or people with a learning disability.
Paula McGowan OBE said, ‘I have been humbled to observe all health and care colleagues working collaboratively to strive for this change. There is more work to be done but the journey has now started, and I truly believe we are on the right trajectory to achieve better health and care outcomes for neurodivergent people.’
Skills for Care launches workforce planning campaign
Skills for Care has launched a campaign to support social care providers with #PlanningForSuccess, by providing information and resources all about effective workforce planning.
The latest campaign from Skills for Care aims to demystify workforce planning and to guide employers on how to get started, as well as highlighting the benefits of planning for now and the future.
Workforce planning encompasses many elements, from recruiting new staff, to retaining and developing current staff, managing safe staffing levels and contingency plans and thinking about what roles you need to have in place to meet the growing and changing needs of people drawing on care and support.
Skills for Care hopes its latest spotlight
will help social care providers to realise they’re already doing many elements of workforce planning in their day-to-day business management. The campaign also aims to provide support in continuing to analyse, plan and review the process to be as effective as possible.
The campaign will run across Skills for Care’s website, social media and other communications channels with blogs and articles sharing expert insight and real-life case studies, as well as signposting to further resources and other support.
The launch of this campaign comes following the release of Skills for Care’s State of the Adult Social Care Sector and Workforce in England report, which highlights the current recruitment and retention challenges facing the sector, with
vacancy rates at their highest on record. The report also highlights the need to think about long-term capacity for the sector, with a growing demand for care and the estimated need for an extra 480,000 people working in social care by 2035. In addition, the findings suggest that we may lose approximately 430,000 people in the next 10 years if those aged 55 and over decide to retire.
With the winter months upon us, the #PlanningForSuccess campaign will also touch on preparing for winter and contingency planning.
Visit the Skills for Care website www.skillsforcare.org.uk to find out more about the campaign.
Follow the campaign on social media using #PlanningForSuccess.
Dementia charities call for workforce support
Alzheimer’s Society, people affected by dementia, and a cross-party group of MPs have called on the Government in Parliament to listen to people with dementia and urgently address the social care workforce crisis.
The group urged the Government to prioritise the social care workforce, providing better pay, career progression and mandatory dementia training to ensure people with dementia can live the lives they want to.
With the number of people living with dementia in the UK set to rise to 1.6 million by 2040, from 900,000 today, the pressures on the social care system are set to grow even further.
Alzheimer’s Society said it was critical to creating a workforce now which could
deliver the care people with dementia need. Currently, people with dementia make up 70% of residents in care homes and 60% of people who access homecare.
The Workforce Matters report from the All-Party Parliamentary Group on Dementia, chaired by Debbie Abrahams MP and supported by Alzheimer’s Society, calls for a 10-year People Plan to create a social care workforce that is skilled and supported to provide high-quality personalised care for people living with dementia.
Kate Lee, Chief Executive of Alzheimer’s Society, said, ‘Providing good social care isn’t just about getting someone up and showered and given their medication. It’s about giving people purpose, and dignity and allowing them to have a good quality of life. Sadly, one in four people told us they
didn’t feel at all involved in the care they received. My mum has dementia, and I know that personalised care is just so important for her wellbeing.’
She added, ‘Prime Minister Rishi Sunak must prioritise social care. We need to see better pay and career progression, mandatory training in dementia, and an audit of the current workforce's knowledge and skills. A People Plan is the only way to build a better system for people with dementia, their families and hardworking care staff.’
The call to reform the social care workforce comes after 26,000 Alzheimer’s Society campaigners signed the charity’s open letter to the Prime Minister, with ambassador Vicky McClure’s heartfelt plea to her social media followers raising signatures by over 8,000.
12 CMM December 2022 NEWS


































CMM December 2022 13 LOVE LAUNDRY We understand how important laundry equipment is to your care or nursing home. Our goal? To make it simple. Made for you Bespoke laundry and finance options to suit you. Safe and sound Helping you create an infection-free environment. Count on us Professional, approachable and at your service. 08000 546 546 WASHCO.CO.UK
Report outlines financial pressures for providers
A financial impact assessment report, commissioned by members of the Care Quality Commission (CQC) Market Oversight Scheme, has revealed that independent care and support providers are reaching a financial tipping point that risks denying people with learning disabilities and autism their right to decent, fulfilling and stable care.
Three quarters of those surveyed expect to make losses or at best break even this year. For the last five years, financial settlements haven’t kept pace with increases in costs, putting considerable pressure on the finances of these organisations.
The report reveals how providers are being forced to stop supporting people, handing back responsibility to local authorities due to consistent losses on the day-to-day operation of services. All chief executives interviewed
for the research believe that these contract hand backs will accelerate over the next 18 months, with a direct impact on the quality of life of people whose support has become unaffordable. The report also reveals that care and support providers are struggling to pay employees the full UK Living Wage or higher. Just four providers involved were able to pay staff as much as 2% above the Living Wage.
Furthermore, the report estimates a rise in agency costs by 157% over the next year, rising from £56m in 2020/21 to £144m 2022/23. If this trend continues, agency staff costs are likely to increase between £175m and £220m by 2023/24.
The CQC’s Market Oversight Scheme was set up to protect care and support recipients from the impact of a Southern Cross healthcare-style collapse that put 30,000 people’s care at risk in 2015.
Call for voluntary register for paid carers
The National Association of Care and Support Workers (NACAS) and Institute of Health and Social Care Management (IHSCM) are calling for the immediate professionalisation of the care industry through the development of a voluntary register for paid carers much like the Nursing and Midwifery Council’s and other health and social care colleagues.
Both organisations have combined forces to address the emerging need for professionalising the care industry and the care workforce within England in a bid to improve recruitment and retention and raise the profile of the profession.
The recent CQC State of Care report highlights the need for a registration process for carers, just like doctors, nurses and other healthcare professionals, just as they do in other devolved nations but currently not in England.
For employers, it will mean attracting and retaining team members from an early age into a profession of choice and the ability to offer a career path.
For the social care workforce, it means professional and public recognition, value and integrity with the prospect of a vocation for life.
For the public, it offers professional governance, bringing much-needed reassurance to those in receipt of care and their families that additional checks are taking place on those providing care.
Liz Blacklock, Director of Operations at NACAS, said, ‘It’s time for a fundamental change in the industry. The population is ageing and the need for professional care services will only keep growing. This is an indisputable fact. We need social care to be the best it can be.’
Such a register could include and support training passports, quicker and safer recruitment, paid job trials.
Care Foundations
We work with thousands of home care start-up agencies, so we understand what it takes to get up and running. Let Access guide you through CQC certification and beyond.

Packages offering up to 25% now available.
Packaging up all the software you need to establish, run and grow a successful home care business. up to
Contact the Access Start-up Team to find out more: theaccessgroup.com/carefoundations
% off start-up software packages
14 CMM December 2022 NEWS
25
Resources to support sector during energy crisis

Community Integrated Care has co-produced a new programme –Taking Charge – to help provide education and guidance to the social care sector through the energy crisis. It gives free support to people who deliver social care, enabling them to reduce energy bills in their home lives and for the people they support.
The programme is accessible to many people who access social care, with interactive, fun and engaging energy saving webinars, and easy read resources to support people who need more adapted communications.

The campaign is led by Oliver Thomason, who has a learning disability and is employed by Community Integrated Care as an Inclusion Coordinator. It offers a unique and inclusive approach to education. According to research by Scope, people with disabilities, and those who access social care, typically face far higher energy usage than the wider population.
The National Care Forum (NCF) has been drawing attention to the growing energy pressures and their impact on the sector, alongside the ongoing workforce shortages for months. Professor
Vic Rayner OBE, Chief Executive of NCF, said, 'The eye watering increases in energy costs is a very serious concern among our members, even after the Government capped prices through the Energy Bill Relief and Energy Price Guarantee Schemes. For social care workers, the steep rises in the cost of living and energy costs alongside the continued reluctance of Government to guarantee the funding for better pay, terms and conditions, means that the next few months will be very hard. The lives and wellbeing of the people
Industry recognition in palliative care
A specialist Cambridgeshire care provider has recently been accredited with the Gold Standards Framework (GSF) for its provision of end of life care.
The GSF centre in end of Life Care is the national training and coordinating centre for all GSF
programmes, enabling generalist frontline staff to provide a ‘gold’ standard of care for people nearing the end of life.
Askham Hall, which is one of the five specialist care homes within Askham Village Community that specialises in palliative
care, achieved this accreditation through an evidence based systematic approach. Askham Hall’s services consistently aligned with the ambitions of GSF to improve the quality of care for all people nearing the end of life — in line with their preferences.
who access care and support services are also significantly impacted, and many are not enjoying the same support the Government is giving to other households.
'It’s encouraging to see such an innovative, co-produced support programme from Community Integrated Care. This will provide much needed practical support to people accessing care services and care workers. However, this can’t be the responsibility of providers alone, we also need more action from Government.'
The home also received specialist training delivered through interactive workshops, distance learning using the GSF Virtual Learning Zone and through supporting training materials customised for teams within the organisations.

CMM December 2022 15 NEWS
WANT TO TRY? Call 0800 086 2462 Find out more
STAY SAFE WITH SMART WIRELESS NURSE CALL Safer, more efficient care
www.c-t.co.uk

Bradford college boosts care sector skills
Bradford College has announced enrolment on health and social care courses is at an all-time high. Student numbers have vastly increased over the last three years, with nearly 400 health and social care students now training at the college. Over 120 additional students commenced courses in the last academic year alone.
Bradford College delivers a level two Diploma in Health and Social Care which provides students with a licence to practice in the sector. Students work with nearly 30 local employers to achieve care certificates, allowing them to undertake valuable work placements while addressing local skills shortages. Students can then progress on to level three programmes or into employment.
One local employer benefitting from working with Bradford
College students is Britannia Care, a registered residential care home specialising in mental health conditions, dementia, and physical disabilities. This employer has a proud history of ‘providing diverse care to diverse communities’ for over 30 years.
Anis Khan, Director at Britannia Care, said, ‘Britannia Care has partnered with Bradford College since 2019, bringing initiatives such as wellbeing, fitness, and cooking classes to our residents and staff team. Our positive partnership continues as we look forward to welcoming 20 new health and care students to Britannia. They will be working alongside our fantastic staff team and will gain valuable experience in caring and supporting our residents to a high standard.’
The British Sign Language 999 service
A deaf paramedic at London Ambulance Service is urging British Sign Languages (BSL) users to download a brand-new app so they can make 999 calls by video.
The 999 BSL service means people with hearing or speech loss can be instantly connected to a video call with a BSL interpreter should they need life-saving help.
Paramedic Richard Webb-Stevens (who has been awarded the Queen's Ambulance Medal for Distinguished Service) said, ‘This is such a brilliant innovation for the deaf community and means sign language users get the same access to emergency services as any other user.
‘If you haven’t already downloaded the 999 BSL app, please do it today – it could save your life or the life of a loved one.’
The revolutionary service is free to use and connects 999 callers to the BSL interpreter who will then relay the conversation to the 999 call handler for all emergency
services: ambulance, police, fire or coastguard.
At London Ambulance Service (LAS), it means call handlers ask exactly the same questions they would in a voice call.
Previously, people with hearing or speech loss have had to rely on a text message service and it meant call handlers were advised to ask fewer questions to avoid any delays in organising help for the patient.
The new service also allows LAS call handlers to give deaf callers instructions on how to give CPR – cardiopulmonary resuscitation –essential life-saving treatment for someone in cardiac arrest.
Richard has now made a video explaining how British Sign Language users can call 999 to encourage more people to familiarise themselves with the video translation service.
Early analysis of 999 BSL calls shows they are just as quick as a voice call – and take about half the time of the text system.
IN FOCUS
The Mayhew Review: Future proofing retirement living
WHAT’S THE STORY?
The Government must build 50,000 new homes for older people each year to tackle the UK’s housing and social care crisis – one in four of all new homes – a new report has urged.
In response to the findings in the report, Future Proofing Retirement Living: Easing the Housing with Care Crisis, leading academic on ageing societies, Professor Les Mayhew, says that with the number of over-65s set to race past 17 million by 2040, the Government should initiate an accelerated programme of constructing older people’s housing.
Professor Mayhew says that achieving this growth would help older people stay healthy for longer and reduce the burden on the NHS and care homes. Each new home would free up housing and surplus bedrooms for younger families and first-time buyers, making housing more affordable. And new developments could play a major part in revitalising declining high streets.
Integrated Retirement Communities providing communal facilities and social care have a particularly important role to play. New Zealand, Australia and the US are far more advanced in this regard – with 10 times the number of older people living in this kind of setting as here – but Mayhew says the UK needs to go much further than even these countries.
WHAT WERE THE FINDINGS?
Professor Mayhew, whose commission this year drew on
evidence and input from over 40 experts, highlights the concrete steps the Government needs to take to reach the levels of older people’s housing required:
• Launching the Older People’s Housing Taskforce immediately.
• Reforming planning rules to make it easier to build housing suitable for later life.
• Putting older people’s housing on a level playing field with all other developments.
• Cutting Stamp Duty so it is the same for last-time buyers as first-time buyers.
• Ramping up the financial advice available for older people looking to move.
The Older People’s Housing Taskforce was announced by the Government in February but has yet to launch.
WHAT DID THE EXPERTS SAY?
Professor Les Mayhew of the International Longevity Centre – UK and Bayes Business School said, ‘Our findings show that we need to aim big and hit the 50,000 mark on a yearly basis when it comes to new homes for older people. If we do so, the benefits will be huge – for the health and wellbeing of older people, for the NHS, and for younger people getting on the housing ladder. The proposals in my review do not add to public expenditure –investment is not the problem. It just needs co-ordinated action and the weight of Government to get behind it.’
CMM December 2022 17 NEWS
NEWS / IN FOCUS
NEWS FROM ACROSS THE GLOBE
Australian SAGE Delegation meets UK care leaders
Person Centred Software (PCS) and the National Care Forum (NCF) welcomed the Australian Studying and Advancing Global Eldercare (SAGE) Delegation to the UK.
The evening was a night of international exchange, discussing and sharing best practice strategies in adult social care in the UK and residential aged care in Australia that could be shared, tailored, or adopted as appropriate.
The Australian SAGE delegation consisted of Chief Executives of small to large
organisations in the Australian aged care sector. The drinks reception was part of their tour in the UK, where they visited multiple care providers across the country to gain knowledge of:
• How care homes are managed and run in the UK.
• Innovative products implemented in the care homes.
• Any challenges that they have faced.
The evening included speeches from Andrew Coles, Chief Executive of Person-Centred
Software, Nathan Jones, Senior Policy, Research and Projects Officer at National Care Forum, Justin Dover, CoChief Executive Officer of Alino Living (located in the heart of the Central Coast of NSW) and Judy Martin, Director of the SAGE programme.
Judy said, ‘I'm delighted with the networking opportunity the PCS and NCF event provided. You can never underestimate the power of collegial and international exchange, where, no matter where we are in the world,
Attracting more men to work in social care
Social services directors who are members of the European Social Network (ESN) met in Brussels to highlight staff shortages in social services and social care across Europe, a trend which has become further exacerbated during and after the COVID-19 pandemic. The directors requested specific policies and programmes to promote the attractiveness of the sector, support recruitment across all populations and ensure retention.
In the context of the European Parliament's Gender Equality Week, the ESN says it’s important that policy makers put forward ideas to break down barriers in gender diversity. Employing more men could help fill shortages. Many men might be put off by stereotypes of social work and social care jobs being traditionally female-led jobs. The ESN said, 'We should raise awareness of the wide variety of roles in the profession, and make sure the
message reaches out to men. It is important to start soon and to convey to everyone, including young men and career advisers, the opportunities that are available and offer new ones through apprenticeships, vital care, military and mental health, or research.'
In the context of the future European Recommendation on care, the ESN proposes that the Commission works with national governments to put in place specific social services
Japan’s population problem forces changes
Japan's Government is planning dramatic changes to the national pension scheme and healthcare payments as supporting the country's ageing population strains public finances.
Advances in healthcare are enabling more Japanese people to live longer than ever before, with Government statistics released in August showing that a Japanese woman can expect
to live to the age of 87 and a man to reach 81 years old.
At the same time, however, the number of births in 2021 fell to a post-World War II record low of just over 811,000. The number of working-age people is also shrinking as more people enter retirement.
In response, the Ministry of Health, Labor and Welfare is expected to propose significant changes to the pension scheme
that all Japanese people are required to contribute to, mandating an extension to the period that people have to pay premiums from the present 40 years to 45 years.
The ministry also intends to increase contributions to the national healthcare system paid by older citizens. Additional fees for medical treatment are also expected to be increased.
our industry's challenges are similar. Network and exchange opportunities like this provide thought leadership to all the challenges we face.’
Liz Jones, Director of Policy of the National Care Forum, added, ‘NCF is delighted to support the return of the SAGE tour, bringing together providers from Australia and the UK. This is an important and unique opportunity to share experiences and lessons learned, particularly from the past few years, and foster relationships across the globe.’
workforce strategies that, amongst others, improve the attractiveness of the sector, its development and resources. This involves the need to think of different ways of getting people and particularly men into the profession through fostering care ambassadors, male champions, pushing recruitment drives aimed at people with experience of care and school leavers, student work experiences and mentorship programmes.
The coronavirus pandemic proved the robustness of Japan's healthcare system, as Japan had one of the lowest COVID-19 death rates in the world. However, without changes, Japan runs the risk that paying for its health and welfare system will become unsustainable.
A final decision on the government's proposals is expected in 2024.
18 CMM December 2022 NEWS NEWS
NEWS
• We at Promised Care can assure you that we are amongst the few agencies, if not the only agency, that provides comprehensive training to our staff, tailored according to Skills for Care standards and CQC minimum standards required for safe care to any vulnerable person.


• It is good practice for our staff to have a brief induction from the home manager or senior staff on the first day of their shifts. This includes fire exits and safety locations in the event of emergency and brief background information on each resident’s care plan.
• Our staff are suitably trained to provide safe care to residents. This includes using effective communication, encouraging residents to eat and drink to promote hydration and good body weight and documenting fluid and food intake and output. Our staff will report in good time to relevant people, any changes observed in the care of the residents they work with, as they assist in their personal care activities. Our staff will also engage residents in mind-stimulating activities in the home. As former care managers we understand the plight of care home managers, and the challenges of managing day-to-day care activities when you have staff shortages.
• Our management team includes dedicated trainers with previous care experience, and professional qualifications in nursing, social work and training. We provide staff with theoretical learning and hands-on training, on how they are expected to provide care to residents in any structured care environment, such as: Nursing Homes, Home Care, Residential Care Homes, Day Care Centres and Supported Living, including people with Mental Health Conditions.
Our health care assistants would have the option to work with service users, who
require home care support
in their own homes to:
Older people in need of help. Sensory impairment. Mental health. Palliative care. Physical disability. Respite care, 24-hour live-in care. Supported living. Bedside support on admission in hospital until you are discharged home. Overseas accompaniment to visit relatives, friends, or exotic places.
Please visit our website for more information.
Web: www.promisedcare.co.uk Tel: 0208 842 3329 Mobile: 07792 448150, 07969 013855 Email: info@promisedcare.co.uk leanonmecc@protonmail.com
David J. Cheesman RMN, Social Worker & Training Manager
Nobel Baxter
Public Health, MBA & RGN - Service Coordinator CREATING A BETTER TOMORROW OUR SERVICES ARE AVAILABLE 24 HOURS A DAY, 7 DAYS A WEEK, 365 DAYS A YEAR. Why should you choose Promised Care agency staff to cover shifts in your care home? WE ALSO PROVIDE PRIVATE HOME CARE SERVICES (CQC
ACTIVITIES 9)
Mr
Mr
BSc
REGULATED
Promised Care Ltd specialises in recruiting, training and supplying vetted health care assistants to work in various nursing homes, residential care homes and supported living environments for people with learning disabilities, physical disabilities and people with mental health conditions.
CREATING INCLUSIVE CULTURES:

20 CMM December 2022
SIX PILLARS OF INCLUSIVITY TO SUPPORT LGBTQ+ PEOPLE
Dr Layla McCay, Director of Policy NHS Confederation and Executive Lead of the NHS Confederation’s Health and Care LGBTQ+ Leaders Network, outlines the six key pillars of inclusivity needed to create and maintain inclusive cultures where LGBTQ+ people feel supported and empowered.
It is not widely understood that people who are LGBTQ+ in the UK are more likely to experience physical and mental health problems than the general population. These health inequalities are largely driven by prejudice, discrimination and exclusion, which affect health in two main ways. Firstly, they increase the likelihood that LGBTQ+ people will be subject to health risk factors, for example, low self-esteem, alcohol, bullying, assault, family rejection and homelessness. Secondly, they affect the ability of LGBTQ+ people to access the right healthcare when they need it. Some people will even avoid seeking healthcare for fear of having a negative experience due to health professionals’ responses to their sexuality or gender. A recent survey by the LGBT Foundation tells us one in five LGBTQ+ people have witnessed homophobic or transphobic remarks by healthcare staff.
These disparities do not only affect the general public and people needing to access healthcare, but they also affect staff working in health and care. Recent NHS Staff Survey data revealed that the LGBTQ+ workforce is at disproportionately high risk of experiencing physical violence from patients, bullying, harassment and/or abuse from colleagues. For example, on the NHS People
Promise indicator ‘we are compassionate and inclusive’, the overall score for lesbian and gay staff is 7.1 compared to 7.3 for heterosexual colleagues. The scale of the gap varies by indicator, with the biggest gap between health and wellbeing where the score for heterosexual staff is six compared to 5.6 for lesbian and gay staff. The gaps in experience for transgender staff are even wider and there is also a gap in experience for those identifying as bisexual.
The NHS, along with other health and care organisations, seeks to provide fair access to health and care for all, to improve the health of all parts of the population and to be an inclusive employer. And yet, the data along with feedback from members of the NHS Confederation’s Health and Care LGBTQ+ Leaders Network, exposes that we are still on that improvement journey.
Inclusion framework
The COVID-19 pandemic only served to make things worse for LGBTQ+ people, disproportionately affecting their health and wellbeing and further exacerbating health inequalities. It also served as a catalyst for the

CMM December 2022 21
NHS Confederation’s Health and Care LGBTQ+ Leaders Network, in collaboration with the NHS Confederation’s Mental Health Network, to develop the LGBTQ+ Inclusion Framework.
The framework supports leaders of NHS and other health and care organisations to better deliver on their role in reducing health disparities, being inclusive employers and creating genuine improvement for LGBTQ+ staff, patients and population. It recommends six key pillars of inclusivity for organisations to build to create and maintain inclusive cultures. These are the principals of the six pillars:
1. Visible leadership and confident staff.
2. A strong knowledge base.
3. Being non-heteronormative and non-cisnormative in everything we do.
4. Systematic collection and reporting of data.
5. Listening to service users.
6. Proactively seeking out partners to co-deliver services.
Leading the way
Visibility matters: having staff who feel confident and who can be their authentic selves really makes a difference. If they feel safe to do so, LGBTQ+ leaders should try to be visible and non-LGBTQ+ leaders should model good allyship. This will help to ensure diversity in the workforce, diversity of leadership and that organisational policy reflects the experiences of LGBTQ+ staff.
Staff should have the opportunity to belong to an LGBTQ+ staff network, ensuring that this diverse group is part of the decision-making process across the organisation. If anyone experiences distress, exclusion and/or conflict in the workplace because they are LGBTQ+, people should be confident that their employer will provide support.
Having a strong knowledge base is also important. This means leaders and staff understanding the specific needs of LGBTQ+ people, the health inequalities they face and the variance of experience between the L,G,B,T,Q and + identities, particularly that of transgender people. Employers can create a safe space for staff to learn about LGBTQ+
experiences and how they can be inclusive, including in terms of intersectionality between protected characteristics.
Another key behaviour is not assuming a person’s gender identity or sexual orientation. Being heterosexual (a person who is sexually attracted to people of the opposite sex/ gender) or cisgender (a person whose gender identity corresponds with the sex the person was identified as having at birth) should be considered a possibility, not a default. When designing, commissioning and delivering services and policies, ensuring inclusivity is also considering whether they address the specific needs of LGBTQ+ people.
Collecting data
It is helpful to take responsibility for collecting and reporting data. Proactively seeking specific gender identity and sexual orientation information from all patients and carers, and reporting this to the NHS data sets, can help organisations understand and better meet the diverse needs of their population.
to design more inclusive services and reduce inequalities.
Strengthening delivery
Another pillar is the importance of listening to service users. Organisations have a statutory duty to include service users and community groups in the design and commissioning of services. When co-producing and commissioning services, it is important to include LGBTQ+ voices so they can help to make these services more inclusive for that population. This includes the needs of LGBTQ+ children and young people, particularly around mental health. Organisations can then use that insight to create targeted interventions with measurable outcomes.
Finally, it can be very helpful to proactively seek out partners to co-deliver services. The knowledge and reach of third sector and community organisations closely connected with the local LGBTQ+ population can help ensure that services are being designed or commissioned with diverse local needs in mind.
Actions speak louder than words
Asking staff about their gender identity and sexual orientation is also important, but its value hinges on employers working to make sure LGBTQ+ people feel confident and safe in sharing that information about themselves. Once data is collected, separating it out for analysis is important – LGBTQ+ people are of course not one homogenous group and good analysis to better understand the issues specific to local LGBTQ+ communities will empower organisations
Implementing change can be daunting, particularly across an entire organisation. That’s why we have invited a number of health and care organisations to pilot the framework’s pillars. The organisations took our framework, identified areas to start working on and found that small steps can lead to big changes. This is a complex time for LGBTQ+ staff, patients and carers. Health and care leaders want LGBTQ+ staff and service users to know that their best interests are being considered, are at the heart of decision-making and, ultimately, that their places of work and their care settings are safe.
To download the LGBTQ+ Inclusion Framework and supporting tools, visit https://www.nhsconfed.org/publications/ health-and-care-lgbtq-inclusion-framework
Using the pillars of this framework is a way of being more intentional about inclusion. CMM
Dr Layla McCay is the Policy Director at the NHS Confederation and Executive Lead of the Health and Care LGBTQ+ Leaders Network. Email: lgbtqnetwork@nhsconfed.org Twitter: @LaylaMcCay
Have you successfully implemented an inclusion framework to support the LGBTQ+ community in your care setting? Share your insights and experiences. Visit www.caremanagementmatters.co.uk
22 CMM December 2022
CREATING INCLUSIVE CULTURES: SIX PILLARS OF INCLUSIVITY TO SUPPORT LGBTQ+ PEOPLE >
“When co-producing and commissioning services, it is important to include LGBTQ+ voices so they can help to make these services more inclusive”










































• Available in 11 sizes, from 18mm-40mm (Ø) • Longer length – 130mm • Large buffer/comfort zone to prevent backflow and sheaths blowing off • Latex-FREE • Customise/remove excess length (scissors provided) • Perfect fit/size for all A bag for all seasons and occasions Short and strong. No more embarrassing leaks? • Specifically designed for wheelchair users • 700ml and 1300ml sizes • Shaped to the contours of the bended knee • Available in 9 sizes, from 18mm-35mm (Ø) • Shorter length – 75mm • Stronger adhesive • Buffer/comfort zone to prevent backflow and sheaths blowing off • Latex-FREE Bendi Bags • Traditionally shaped leg bag • 600ml and 1000ml sizes • 7cm shorter in length than many 750ml bags – no unsightly taps dangling Comfort Bags • Ideal for sun, sports and even some short clothing • 500ml capacity • Dress as YOU want, not to cover the leg bag Discreet Bags 11 sizes 9 sizes Urology products that make a difference Unique features and benefits often designed by end users. Available on prescription FREE HOME DELIVERY SERVICE Providing a personal service from a professional team. For your FREE information pack contact 0800 999 5596 or email prescriptions@manfredsauercare.co.uk For more information, please contact the helpline on: 01604 595 696 quoting CMM/D/J helpline@manfred-sauer.co.uk Or visit: www.manfred-sauer.co.uk


24 CMM December 2022 Call, email or click online to book your training needs today! T: 01622 766078 E: info@edify-consultancy.co.uk W: www.edify-consultancy.co.uk EXPERTS IN CARE TRAINING Trusted providers to some of the largest care organisations in the UK… ... and the very smallest. Over 160 course options with face to face, virtual and online delivery options. All-in-one PASS with Roster Scan me Digital care management for today and tomorrow Scheduling • Payroll • Invoicing • Reporting
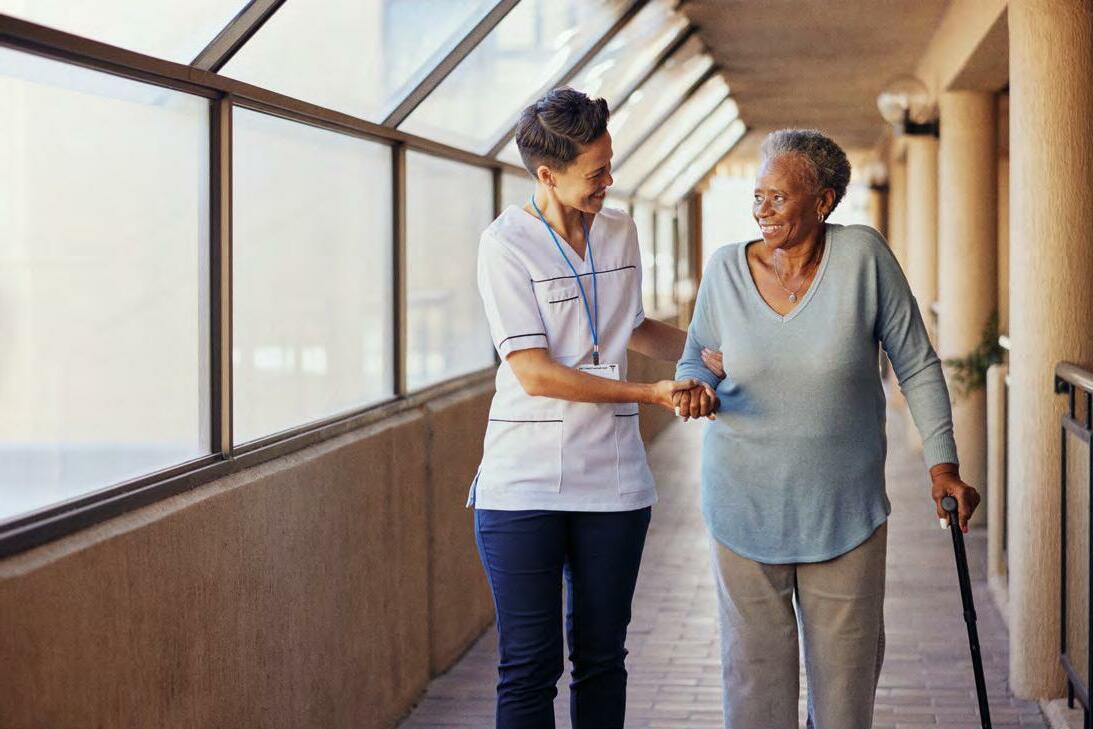
A BALANCING ACT

Working with local health teams to facilitate care home visits
The social care sector is continuing to balance the needs of the people it cares for against any imposing threat of infection. How can providers ensure the least restrictive measures are in place this winter? Helen Wildbore, Director of the Relatives & Residents Association, shares the impact of tough measures on people and offers her advice on pushing back to local health teams.
CMM December 2022 25
CRISPR. Diagnostics. 2021;11(5):823. 3. MedTech Europe. The Value of Diagnostic Information in Acute Respiratory Infections — Observations From the COVID-19 Pandemic. Accessed November 2021. https://www.medtecheurope.org/wp-content/uploads/2021/04/vodicase-on-respiratory-disease_case-study.pdf. 4. Moore N, et al. Evaluation of the Alere™ i Influenza A & B 2 Assay. Poster presented at: ASM Clinical Virology Symposium; 2018; West Palm Beach, Florida. 5. Abbott. ID NOW™ Product Inserts. 6. Abbott. Data on File. ID NOW™ Strep A 2 Clinical Trial. © 2022 Abbott. All rights reserved. All trademarks referenced are trademarks of either the Abbott group of companies or their respective owners. Any photos displayed are for illustrative purposes only. Any person depicted in such photos is a model. COL-15642 08/22


















IMAGINE IF YOU COULD QUICKLY DIFFERENTIATE BETWEEN THE SYMPTOMS OF YOUR RESIDENTS’ RESPIRATORY INFECTIONS 1-3 ID NOW ™ RAPID MOLECULAR RESPIRATORY TESTING PLATFORM ID NOW™ IS AN EASY-TO-USE CONNECTABLE INSTRUMENT WHICH PROVIDES POSITIVE RESULTS FOR: • SARS-CoV-2 in 13 minutes or less 5 • Influenza A & B in as little as 5 minutes , with 95% detected within 7 minutes 4 and negative results in 13 minutes 5 • RSV in 13 minutes or less 5 • Strep A in as little as 2 minutes , with 99% detected within 3 minutes 6 and negative results in 6 minutes 5 SCAN TO LEARN MORE ABOUT ID NOW ID NOW ™ PLATFORM ID NOW™ - Helping you to put your residents’ needs first by treating them quickly, and isolating where needed. 1. NHS England and NHS Improvement. Primary Care Bulletin. Updated June 29, 2021. Accessed November 2021. https://www.england.nhs.uk/ coronavirus/primary-care/other-resources/primarycarebulleting/june2021. 2. Zhou H, Tsou JH, Chinthalapally M, Liu H, Jiang F. Detection and Differentiation of SARS-CoV-2, Influenza, and Respiratory Syncytial Viruses by
The year 2022 has been incredibly difficult for people relying on services and for people running services.
The threat of COVID-19 continues, staff shortages are crippling services and the sector is stretched to breaking point. Whilst the rest of the country has gone back to normal, people in care are now the only ones left living under COVID-19 guidance. That guidance is much improved – all restrictions on visiting were removed in March, except infection prevention and control measures during an outbreak when residents can have a minimum of one visitor at a time. However, our helpline hears access with loved ones continues to vary across the UK.
Visiting still a postcode lottery
Many care settings have welcomed relatives and friends back with open arms, recognising the vital importance of these relationships to wellbeing and quality of life. However, some care homes have been reluctant to do so. We conducted a survey (with campaign group Rights For Residents) of over 650 people who had a relative or friend in care. We found between April-September 2022 where care homes had an outbreak, 60% of respondents said there were additional visiting restrictions in place (beyond one visitor at a time as stipulated in Government guidance). 11% reported residents were not allowed any visitors at all.
Often the barrier lies not with the care home but with the local health protection/public health team. Our survey found that in 67% of cases where no visitors at all were allowed during outbreaks, the care home said it was following advice from public health teams or the local authority. This is a pattern we have been hearing on our helpline too.
We wrote to local health protection/public health teams in September expressing concern about their role in imposing such restrictions, on behalf of a coalition of organisations representing both care providers and residents. The letter reminded the local health teams of their legal duties to protect residents' rights, including to family life, wellbeing and autonomy (as protected in Article 8 of the Human Rights Act).
Relative reality
The letter also stressed the importance of ensuring during outbreaks the one visitor at a time rule is followed – this was introduced in March 2022 and replaced the role of essential caregivers, due to concerns about carer burnout.
“The pressure is so immense and distressing. It is ruining my life and relationships. I can't sleep, it overshadows everything I do. I feel permanently guilty when I am not by my mother's side. I get home after a four-hour round trip and know I cannot continue like this. But I do. The worry is constant and there is no end in sight.” Daughter and essential caregiver, February 2022
Isolation and separation of older people from their family and friends is damaging to both mental and physical health, as well as to quality of life. Our helpline hears daily of the impact on residents: losing weight, speech and mobility, the depression and loneliness of lack of touch, the feeling of abandonment, lifelong relationships fading from memory in the fog of dementia.
Even outside of outbreaks, 45% of respondents to our survey said the care home was implementing visiting restrictions. What can seem like minor restrictions on visiting can have a huge impact on residents' quality of life and sense of belonging. Booking systems, time limits, restrictions on days of week or times of day for visiting can make people’s homes feel like institutions and severely limit who they can see.
“I cannot give quality time, comfort, support, or some refreshment to my loved one while our visits are spent this way [with a time limit].” Survey respondent, September 2022
For relatives and friends, the same feelings of isolation and separation are mixed with anxiety and fear of what is happening behind closed doors when they are not on hand to support with eating, or to spot when a loved one is in pain.
“I am still forced to leave after our allotted time together and so I never even see my loved one being given meals or drinks now. It is all really worrying, and I am totally powerless.” Survey respondent, September 2022
Caregiver concerns
There is also the guilt many relatives tell us they feel about a loved one going into care, of no longer being able to cope but still wanting to be involved as partners in care. Being denied this role makes the feelings of guilt even more overwhelming.
“The day of admission was profoundly challenging. I felt an overwhelming sense of betrayal like Judas Iscariot as I took her by the hand, trustingly, to admit her. I was advised that it would be best for me not to visit for up to two weeks to allow her to 'settle'” Sir Al Aynsley-Green, March 2022
A constant theme on our helpline is of powerlessness. Relatives tell us they feel powerless to speak out to raise issues and concerns.
There are so few care options available and it is all too easy for care providers to end the contract or ask residents to leave. When the power imbalance is so skewed, relatives are afraid of being seen as a ‘problem’ or a ‘pain’ and people’s homes can feel precarious.
“My request for Essential Care Giver status [in line with Government guidance at the time] was denied. I was told this was only for situations where the presence of a relative was required to deliver essential care. When I said that this was not what the guidance stated, the care home manager insisted that I was wrong and issued notice to leave…Mum died a week before the notice to leave was due to expire. Sitting with my mother’s body was the longest time I had been allowed to spend with her since she had entered the care home 16 months before.” Ann, R&RA helpline client, March 2022
CMM December 2022 27 A BALANCING ACT: WORKING WITH LOCAL HEALTH TEAMS TO FACILITATE CARE HOME VISITS
>
>
> Pushing back
As our survey results showed, care homes are often facing a barrier from local health teams when trying to facilitate meaningful visiting during outbreaks. What can be done? Here are some tips on pushing back:
• Explain the guidance: don’t assume the local health team is aware of the latest version of the guidance setting out that during outbreaks residents can have one visitor at a time as a minimum, but residents' individual needs will need to be considered.
• Focus on the law: remind local health teams of their own legal duties to protect residents' rights to family life, wellbeing and autonomy under the Human Rights Act and to ensure the least restrictive option under the Mental Capacity Act – more information can be found in R&RA’s guide ‘Visiting and the Law’: https://www.relres.org/ visiting-guide-providers/
• Use our letter: send your local health team the letter signed by a coalition of organisations urging them to comply with the law and the guidance: https://www.relres.org/letterisolation-2/
• Frame your discussion around wider wellbeing: remind local health teams they have to consider residents' wider wellbeing, not just the risk from the virus but also the risk from isolation from relatives/ friends – this means protecting their rights to dignity, family life, liberty, autonomy, etc.
• Be honest and transparent: let residents and families know you are facing a barrier from the local health team and what you are doing to challenge this, otherwise they will fear the worst about why they are being kept apart.
• Work together with families: consider asking them to contact
the local health team to question the advice, to help reopen the discussion.
• Seek support: speak to the Relatives & Residents Association confidential helpline if you have concerns about your visiting practice or advice from the local health team: 020 7359 8136 and helpline@relres.org
Support from family carers is not an optional extra; it is fundamental to good quality of life and intrinsic to basic good care. To ensure this happens across the sector and is no longer a postcode lottery, we are calling for the role of Care Supporter to be enshrined in law. It would give people needing care a right to the support of a relative or friend across health and care settings. This call has cross-party political support and the backing of over 30 organisations including many care providers. If you would like to join us in this call, please get in touch: https://www.relres.org/ care-supporter/ CMM
The Care Quality Commission (CQC) on visiting
Why is it important that residents in care homes should be able to receive visitors if they want to?
CQC: Care homes are people’s homes, and residents should be able to welcome family and friends as they did before they became a resident. Residents also have consumer rights, which help to ensure that they are treated fairly and protected if things go wrong. They have these rights, whether they pay all the costs of their care, or whether some or all of the costs are paid for by their local authority, NHS or health and social care trust.
It is important that people’s family and loved ones are able to help plan their care and support as much as they want them to. This sort of involvement is an essential characteristic of person-centred care. Clearly, such involvement is better enabled by family, friends and carers being able to visit relatives in their home, talk to the staff who care for them, and give their feedback – both positive and negative – to the provider.

The Care Quality Commission (CQC) told CMM, ‘We expect providers to encourage and enable visiting wherever possible. In the event restrictions have to be put in place, they should be done in line with the Department of Health and Social Care's guidance and with advice from local Directors of Public Health. If they deviate from the guidance, a full risk assessment should be undertaken in informed discussion with people using services, their representative and local system partners, with the rationale and outcomes fully documented.’
CMM would like to hear how you have been facilitating visitors and how, despite potential push backs from local authorities and health teams, you have overcome challenges to enable successful visits. Visit www.caremanagementmatters.co.uk
28 CMM December 2022 A BALANCING ACT: WORKING WITH LOCAL HEALTH TEAMS TO FACILITATE CARE HOME VISITS
Helen Wildbore is the Director of the Relatives & Residents Association. Email: helen.wildbore@relres.org Twitter: @relresuk

Into Perspective
The current landscape
A recent report from The King’s Fund would suggest not, no. The report, titled Towards a New Partnership Between Disabled People and Health and Care Services: Getting our Voices Heard, analyses research conducted alongside Disability Rights UK into the current landscape of disabled people’s involvement in health and care planning. The report highlights existing best practice examples but summarises that there are also several instances where the involvement of disabled people is lacking or felt ‘tokenistic’.
In addition, the report distinguishes between actions required of health and care organisations and of disabled people’s organisations (DPOs) to facilitate meaningful co-production. According to The King’s Fund, health and care organisations should broaden their understanding of the societal barriers impacting on disabled people, while DPOs should do more to support health and care organisations to interact more productively with disabled people.
In an ideal world
The Social Care Institute for Excellence (SCIE) makes a series of recommendations to ensure that co-production is implemented effectively. Focusing on themes of culture, structure, practice and review, the recommendations fundamentally state that people who draw on care and support services should be involved from the outset of care planning, through to the delivery and ongoing monitoring of services.
SCIE also emphasises the importance of organisations
IN
clearly defining what co-production will mean to them from the outset of care planning to ensure that it is implemented correctly, without deviation from the principles agreed. Organisations that achieve this will be best placed to deliver meaningful co-production initiatives that bring about positive change.
The heart of the problem
Disability Rights UK, in co-production with Norah Fry Centre for Disability Studies at the University of Bristol, argues in its position paper, Co-production – How Disabled People can (not) Break the Mould in Service/ Workforce Development and Commissioning, that there is a distinction between ‘systems’ and ‘people’ that is standing in the way of co-production.
The paper understands that ‘people’ who draw on health and care services, due to their vulnerability, will gravitate towards the bigger ‘system’, unaware of their own power to influence service planning and delivery through co-production. In turn, the paper suggests that the ‘system’ and its personalisation agenda has not gone far enough to empower the ‘people’ to be involved in enacting substantial co-production in the planning and delivery of health and care services. Lastly, the paper puts forward that ‘people’ can lose a sense of their peer identity as a result of interacting with the current ‘system’ and the resources ‘people’ possess are not being utilised sufficiently.
The following perspectives come from two people with lived experience of drawing on services.

30 CMM December 2022
HOW CAN THE VIEWS OF DISABLED PEOPLE BE PRIORITISED
CARE PLANNING AND DELIVERY?
The sector is well aware of ‘co-production’ and its role in successful care planning and delivery. But is the demonstrated value of co-production being embraced fully by commissioners and service providers? Are disabled people’s views truly being heard, acted upon and continuously monitored?
We are your greatest asset
Don’t just listen, take action
Anna Severwright, Co-convenor, Social Care Future @AnnaSeverwright

Personally, I would change this question to ‘how can disabled and older people play an active role in the design and delivery of social care?’. Because we have the knowledge, passion and solutions to bring positive change. It shouldn’t be a ‘nice to have’, it’s an essential part of designing social care that works well for everyone.


As someone who draws on social care, I am too often invited to meetings as the ‘lived experience voice’. Or I see organisations ask for people’s views on their plans. The problem is that these situations (and many others) usually have no genuine scope to influence or co-design. So, what does need to happen?
• Build relationships. Often very last minute we are asked to ‘find someone with lived experience’. We can tell when we are a ‘tick box’ and not valued for our expertise and skills. Working well together needs trust and openness and these take time to build.
• Start early. Bring us in early so we are part of creating the solutions (and you don’t have to fix it later). And not just for the design phase but delivery and evaluation too.
• Work differently. Too often
we are expected to fit into your organisation. Meetings may need to be in different places, at different times and held in different ways to allow everyone to genuinely participate. Compensate people fairly for their time and work. Cut the jargon (it’s better for everyone!).
• Widen the voices. There are some disabled people who are heard less than others, due to other inequalities. This takes active effort and working with people from those communities to bring in those wider voices.
• Don’t just listen. Too often I give my views and then hear nothing. Or I see the final result and realise that our views were ignored. If you aren’t going to take action on what you hear, don’t waste our time.
• Be honest. We are realistic and pragmatic; be honest about the challenges and what can be done or not.
• Go further. Long-term disabled people should be employed in organisations and roles in the social care sector.
This shouldn’t be a ‘nice to have’; we bring expertise and skills that are vital to create a social care that everyone can thrive in.
How can the views of disabled people be prioritised in future care planning and delivery? It's a question I have often thought about along with other members of Learning Disability England. It is the driving force behind Good Lives: Building Change Together, which many paid supporter organisations and professional bodies are using to really examine their practice and make changes.
are conversations about planning care, there are only professionals at the meeting. In any other walk of life, if you need to work out the right thing to do or understand if it is working, you go to the expert. We are your greatest asset.
For me, to live a good, long and happy life, the number one thing is to be healthy – mentally as well as physically. To have the things in my life that many people take for granted: a place I can call home, a job I love, the right support for me when I need it. How can you prioritise my views – and those of other disabled people? By putting us at the centre of assessing whether the support is meeting our needs. Seeing us as equal, human.
For me, it feels as simple as saying: by treating lived experience with equal if not more weight than evidence gathered from professionals, through things like the ARC England Learning Disability Research Unit. What they share is valuable but only part of the picture. Too often when there
Good Lives has this at its heart. And I ask every professional to work out what their part is in making this happen. To take Good Lives’ work as a starting point and embed it in what you do. It's not complicated stuff. We just need to talk to each other, listen to each other, then plan together. When things break down, it's almost inevitably because people haven't listened. So, my challenge to you is to think about how you are going to listen more, listen better and how you will transform what you hear into more people living good lives.
31
Jordan Smith, Self-advocate and Co-chair of Learning Disability England's Representative Body @learningdiseng
• Governance documents • Audit Tools • Dependency Tool • Clinical Policies & Procedures • FREE Downloads • Risk Assessment Templates • PRN Protocols E-Document Shop Now OPEN!
“For me, it feels as simple as saying: by treating lived experience with equal if not more weight than evidence gathered from professionals”
As part of a national legal firm with over 150 specialist health lawyers, we cover all aspects of health care related law and practice.



We have a long history of providing market-leading legal advice to care providers. Our large team of specialist and experienced care homes lawyers advise our regulated care business clients daily across wide-ranging areas including:
,
weightmans.com
32 CMM December 2022
■
■
■
■
■
■
Inquests and inquiries
Safeguarding and investigations
Employment and HR advice including immigration
Refinancing and restructuring advice
CQC issues and regulatory advice
Commercial disputes and debt recovery weightmans Health @weightmans
To find out more about the care services we can offer, contact Andrew Parsons
Partner, at andrew.parsons@weightmans.com Applications for the Care Sector integrated into Microsoft Teams HR Rostering Time & Attendance Property Maintenance Enquiry Management Compliance Care Management. www.CarePoint365.co.uk Tel: 020 4558 1503 email: getintouch@carepoint365.co.uk


CMM December 2022 33
Rebecca Sycamore, Executive Director of Strategy and Development at St Mungo’s, a national charity dedicated to ending homelessness and rebuilding lives, explains what action must be taken to improve care and support for people experiencing homelessness.
Enabling the right care for people affected by homelessness
Living on the streets is frightening, tough and isolating. It is well documented that people who live on the streets have significantly poorer health and die on average some 30 years before the general population.
Lee, who has lived experience of rough sleeping and who is now a resident at one of our CQC-registered care homes, Hilldrop Road, described what rough sleeping can be like: ‘When the weather was good it was tolerable but when it snowed or there was torrential rain, getting dry was a real difficulty, waking up in the sleeping bag all wet. You just have to sit there, it’s all you can do.’
For people like Lee, sleeping rough takes a huge toll on their physical and mental health. This can mean premature ageing, a legacy of frailty and life-limiting conditions, but we simply don’t hear about this and the life-changing consequences that living on the streets can have.
A growing need
In order to recover from homelessness and to go on to live a happy and fulfilling life, people will often need support. This support comes in all shapes and sizes and St Mungo’s provides most types – from being a ‘safety net’ for people managing their own tenancies to hostels with staff on-site 24 hours a day.
However, some people will need more care than many homelessness services are able to provide. There is also the question of what options are available for people who need additional support with eating and/or washing and for people living with dementia.
that meets these needs. There are a number of reasons for this. The key reason is that there is a very limited supply of specialist care homes that are able to cater for the full range of needs common to people with experience of homelessness.
At St Mungo’s we know how much expertise and experience is needed – we run two registered care homes for people who have been homeless. We also know that because our clients have often been exposed to multiple traumas, they may have drug or alcohol dependencies and may have significant mental health issues as well as physical care needs. Due to the significant level of need, mainstream care homes are often unsuitable.
And then there is demand – a lot of demand. As one of our care managers said, ‘We could fill this home twice over with the referrals we get’.
We also have a stretched adult social care system and while there is progressive and positive work going on – such as the Local Government Association and Association of Directors of Adult Social Services guidance and the work of the Greater London Authority and London Councils’ ‘Life off the streets’ group – we know that getting our clients’ care needs recognised and responding to them can be challenging.
Promoting best practice
There can be a lack of awareness and understanding of this as a specific issue among some social service and health care professionals.
We need to address this and improve efficacy of adult social care teams when working with people experiencing complex needs. The charity has been pleased to see the new Rough Sleeping Strategy make a commitment to promote best practice for social workers and social care staff.
The Government should also emphasise the importance of timely and thorough care needs and adult safeguarding assessments for people experiencing complex need. These must recognise the different circumstances of people who are experiencing rough sleeping or homelessness.
This question was at the heart of the Life Changing Care review, which we published in August 2022. St Mungo’s undertook the Life Changing Care review first and foremost to improve the care and support we provide to our clients. We chose to publish the results to shine a spotlight on this issue and for this to lead to a wider conversation with key partners to ensure action. Our research was developed in partnership with the co-clinical lead of the Homeless Health Programme at Healthy London Partnerships, Dr Caroline Shulman. It collates data from 31 of our non-CQC-registered services and reflects the needs of our 1,442 clients.
What we confirmed was what we knew anecdotally – that there is a significant number of clients across our organisation who have additional physical or health care needs.
Our survey found these include people requiring support with dementia (5%) and people who experience poor mobility (8%).
The review also found that despite a significant level of need, many of our clients are not receiving the care
In delivering the future vision for adult social care, including the delivery of the Integration White Paper and the Adult Social Care White Paper, the Government should encourage the integration of funding. The funding should be made available to all the different partners, including social care, health and homelessness.
Local authorities, sub regions and/or regions should also jointly commission and pool budgets with health when targeting this cohort, integrating homelessness into local health and care strategies. The health and care needs of people with experience of homelessness, are often equivalent to much older populations. It is therefore important that older people who find themselves homeless are supported with appropriate health and care provision. This should include multidisciplinary peripatetic inclusion health teams that provide in-reach into supported accommodation and specialist care homes for people with complex care needs.
Homelessness organisations are an integral part of creating life-changing care and enabling those with lived experience of homelessness to access it. We recommend embedding the Voices of Stoke Care Act Toolkit into existing case management processes, in order to support staff and clients to communicate with adult social care
34 CMM December 2022
LIVES: ENABLING THE
FOR PEOPLE
BY HOMELESSNESS
REBUILDING
RIGHT CARE
AFFECTED
in
>
“There is a very limited supply of specialist care homes that are able to cater for the full range of needs common to people with experience of homelessness”









36 CMM December 2022 For more information visit www.painchek.com/uk/ or call 0333 577 3397 PainChek® Universal provides a fast and reliable way of identifying and quantifying pain for all residents, regardless of their ability to self-report their pain. PainChek’s assessment tool is a clinically-validated medical device that utilises AI and facial analysis technology to give a voice to those who cannot reliably self-report their pain, such as those living with dementia or other cognitive impairment. This is combined with the Numeric Rating Scale (NRS) for those who can self-report, giving care providers a holistic tool to better monitor and treat pain at the point of care. Enabling best-practice pain management. Insurance you can trust, made simple. Call for a free quote today or visit www.phoenixsrs.co.uk 01273 977221 Phoenix Specialist Risk Solutions Ltd are authorised by the Financial Conduct Authority – FRN: 809579, as an Appointed Representative of Exchequer Risk Management Ltd – FRN – 616500 Life & Critical Illness Care Home Insurance Commercial Insurance Business Protection We understand that the nature of the care industry can be unpredictable. We want to make sure you’re covered in the face of any risk. Our industry experience means we know what types of risks you face, so speak to us today to discover how we can keep your business protected. Phoenix Specialist Risk Solutions, O ce 1, The Design Quarter, 129-130 Edward Street, Brighton, East Sussex, BN2 0JL
their own language. This will increase the likelihood of a successful referral by clearly specifying how presenting needs map against the ‘eligibility regulations’ contained in the Care Act 2014.
It is also important that homelessness organisations also develop Care Act policies and procedures to help standardise their approach where Care Act eligible needs are identified and to raise awareness and understanding of the availability of care support. This should include mechanisms for escalation where individual needs continue to go unmet. This will support organisations in ensuring that people experiencing homelessness and rough sleeping are provided with appropriate support.
Strengthening strategies
Further research should be commissioned on the barriers people with experience of homelessness face when accessing a Care Act pathway, to inform the best solutions to this issue. In addition, there is a need to build evidence on the outcomes and cost effectiveness of social care interventions for people with lived experience of homelessness.
We sent an early copy of Life Changing Care to the Department of Levelling Up, Housing and Communities (DLUHC), to inform the development of the new Rough Sleeping Strategy which was published on 3rd September. The Government took note of some of our recommendations which we welcome. The strategy recognised that many people sleeping rough experience early onset frailty equivalent to people who are in their 80s. However, people struggle to access the long-term care and support (including through Care Act Assessments) that they need or do not access primary care services. The Government has now set an expectation in the strategy – that the Housing Transformation Fund should expand the supply of
specialist care for this group over the next three years.
The strategy will also improve how different services work together for people sleeping rough, including supporting partners within the new Integrated Care Systems (ICSs) to develop joined-up local strategies that bring together housing, healthcare and homelessness. This will be supported by new statutory guidance: Duty to Cooperate Guidance on Inclusion by NHS bodies and local authorities, which will highlight the needs of people who sleep rough and be explicit in how partners should work to address them.
The strategy has also secured a commitment from the Chief Social Worker’s office to promote best practice guidance for engaging, assessing and providing support to someone experiencing homelessness, including rough sleeping. This will help to ensure that social workers and social care staff are empowered to deliver the highest-quality care and, in turn, improve the experience and outcomes for those people in need.
Changing lives
The new Rough Sleeping Strategy is a welcome step forward on this important issue. The challenge now is delivering on its ambitions. There are pressing issues on the Government’s agenda, notwithstanding the cost-of-living crisis which could easily transform into a homelessness crisis.
We strive to reach our aim of ending rough sleeping in this country and to prevent it happening in the first place. We will continue to get more people off the streets and into accommodation. However, we must make sure that we all work together to enable the right care and accommodation for people and a place to call home. The right care is truly life changing.
For more information about St Mungo’s, visit www.mungos.org.uk/ CMM
What role do you think care providers should play in supporting people affected by homelessness? Share your feedback on the strategies and points discussed in this article. Visit www.caremanagementmatters.co.uk

CMM December 2022 37
Rebecca Sycamore is the Executive Director of Strategy and Development at St Mungo’s. Email: Rebecca.sycamore@mungos.org Twitter: @StMungos
REBUILDING LIVES: ENABLING THE RIGHT CARE FOR PEOPLE AFFECTED BY HOMELESSNESS >
UK
An inspiring care model enhancing retention & wellbeing




As experienced Care Home practitioners we provide training to teams in sustainable innovation and leadership, to embed companionship, partnership working and wellbeing designed to build enriched quality of life into care homes. Developing a culture of care with wellbeing, positive relationships and inclusion at its heart, in a 6 x 1hr per week online training programme. Develop how to address loneliness, helplessness and boredom with companionship, partnerships and meaningful quality of life.
38 CMM December 2022
• 07483
Contact us today and join the care evolution Call today on 01626 868192
359472 or visit www.eden-alternative.co.uk
SETTLING DISPUTES : PREPARING FOR EMPLOYMENT LEGAL CHALLENGES


A care home failed to make reasonable adjustments by forcing a vulnerable care worker to work through the pandemic, rules tribunal. Alan Lewis, Employment Partner at Constantine Law, outlines the lessons to be learnt from this.
The outcome of an employment tribunal, which took place this year involving a care home, provides a number of lessons for employers in the adult social care sector. In the case, a clinically extremely vulnerable care worker who was forced to work during the COVID-19 pandemic against NHS advice, won a disability discrimination claim as a result of the employer’s failure to make reasonable adjustments.i
Case background
Ms Devaney was employed as a carer and team leader by Porthaven Care Homes. On 21st March 2020 she received a letter from the NHS, as did many people in the UK at the time, informing her that she was clinically extremely vulnerable. This was because she suffered with Crohn’s disease and the letter instructed that she was not to leave her house and had to avoid all face-to-face contact for at least 12 weeks. This was commonly known at the time as ‘shielding’.
Unfortunately for Ms Devaney, her employer did not account for her condition and the serious consequences it could have for her during the pandemic. It considered her to be in the ‘at risk’ category. Ms Devaney was in fact in the
‘very high risk’ category.
On 18th March 2020, Porthaven provided all staff with a guidance letter to the effect that it would pay Statutory Sick Pay (SSP) for 14 days for those employees who were ‘at risk’ and had to self-isolate.
Ms Devaney received another letter from the NHS in April 2020, which advised that she sign up to the Government register of clinically vulnerable people and which reminded her that she should not leave her home. The letter said it could be produced to her employer to show that she could not work outside her home and that she did not require a GP fit note.
In line with the advice in that letter, and after receiving a further letter extending her shielding period, Ms Devaney was absent from work from 23rd March to 31st July 2020. She returned to work on 3rd August.
Because of Porthaven’s decision to pay only SSP during the whole of the 19-week absence period, Ms Devaney experienced what the tribunal described as a ‘significant financial loss’, because her normal weekly wage of £405 became as low as £95 per week on SSP.
There had been a specific request by Ms Devaney on 26th March 2020 that her employer place her on furlough under the Coronavirus Job Retention Scheme. Porthaven >
CMM December 2022 39
> could then have claimed a grant under the Scheme for 80% of Ms Devaney’s wages and she was prepared to forgo the remaining 20%, rather than just receive SSP. Porthaven, however, said that because Ms Devaney was a key worker and the care home was still operational, furlough did not apply. This was in fact incorrect.
The employment tribunal found that Porthaven either ‘deliberately and/or through an oversight, failed to acknowledge the difference between workers who were clinically extremely vulnerable and those who were merely vulnerable’. It decided that, as a care provider, the company could have reasonably been expected to know the difference.
The tribunal found the company liable for disability discrimination because it had failed in its duty to make reasonable adjustments under section 20 of the Equality Act. There are lessons to be learned for employers in the adult social care sector. There were three areas of misunderstanding that led to Porthaven’s liability in this case, which could be an issue for other providers arising from events during the pandemic. Before looking at those three areas in more detail, it is important to note that the period from mid-March 2020 onwards was extremely stressful and distressing to businesses in the care sector, to their residents and the residents’ families and friends. Therefore, there can be no doubt that care operators were under significant pressure.
Key mistakes
Firstly, Porthaven had failed to appreciate the difference between ‘at risk’ and ‘at very high risk’. It had not properly considered Ms Devaney’s severe condition and the impact that exposure to COVID-19 would have on Ms Devaney because of her condition.
The second mistake was a failure to appreciate how the law on disability discrimination operates. All employers must ask themselves four questions when dealing with an employee who is disabled as defined by the Equality Actii:
1. Is there a provision, criterion or practice (PCP) – or, put simply, a rule that puts a disabled person at a substantial disadvantage compared with persons who are not disabled? In the Devaney case, the PCP was the policy of only paying care staff their full wages if they attended work in person during the pandemic in 2020, and if they did not, they would only be paid SSP.
2. If there is such a rule, does the employer know, or could it reasonably be expected to know, that that the employee is likely to be placed at any such disadvantage?
3. If yes, are there steps that could be taken by the employer to avoid such disadvantage? In the Devaney case, Porthaven could have placed Ms Devaney on furlough and claimed a grant under the Scheme.
4. If so, would it be reasonable for the employer to take those steps? The tribunal in the Devaney case found that it would have been entirely reasonable. This is because there would have been no cost to the company in putting Ms Devaney on furlough and claiming the grant under the Scheme.
The third mistake was a failure to recognise that the furlough scheme
References
could be used for those clinically vulnerable employees who were required to shield.
Facing challenges
It is quite possible that there may be many providers of adult social care who, albeit unwittingly, have made errors during the pandemic period in the way they have dealt with employees.
From an employment law point of view, the worst-case scenario for a care provider is a lengthy and drawn-out employment tribunal claim for discrimination, perhaps lasting between two and three years. A case can take up a lot of management resource and cost tens of thousands of pounds in legal fees which, in nearly all cases, will not be recoverable from the claimant, even if there is a finding of no liability for the company. If the company is found to be liable, it may face a significant uncapped award of compensation, plus an award for injury to feelings alone as high as £50,000. This is not to mention the bad press arising from the fact that all tribunal judgments are published online by the Tribunals Service and can be accessed by a simple Google search.
Care providers may draw some comfort from the fact that there is a three-month time limit from the date of discrimination for the employee to file their claim with the tribunal, although that time limit can be extended if the tribunal thinks it is just and equitable to do so.
Provider protection
What can employers in the care sector do to protect themselves? Documenting procedures is vital. Cases are often won and lost on paperwork, or a lack of it. Many providers will have insurance to cover tribunal claims. If a claim is threatened or received, the company’s insurance broker should be notified immediately, because the insurer may insist on certain steps being taken. Any negotiations to resolve matters with employees who complain should always be carried out on a ‘without prejudice’ basis. Also, it’s important that any negotiations involve the employee entering into a binding settlement agreement prepared by the company’s lawyers or HR advisers to ensure they cannot issue or continue with proceedings.
Management in particular should be regularly trained on how to deal with equality and diversity issues and keep records of training received, to show its attempts to maintain best practice. Getting it wrong can be a time-consuming and expensive business – a headache employers in the sector could well do without.
The Advisory, Conciliation and Arbitration Service (ACAS) offers free training for employers and employees via e-learning, which includes equality and diversity training: www.acas.org.uk/onlinetraining. Paid-for training is available by other providers, including www.highspeedtraining.co.uk and www.keystonetrainingltd.co.uk. I hope providers find these points of reference useful. The height of the COVID-19 pandemic may be over but the long-lasting impact of such a significant global emergency may only just be truly coming to light.
CMM has approached Porthaven Care Home for comment but is yet to receive a response. CMM
iP Devaney v Porthaven Care Homes No 2 Limited (case number 2304184/2020)
iiA person is disabled under the Equality Act 2010 if they have a physical or mental impairment that has a ‘substantial’ and 'long-term' negative effect on their ability to do normal daily activities. 'Substantial’ means more than minor or trivial. 'Long-term’ means the effect has lasted 12 months or more or is likely to do so.
What’s your response to this case and do you think the Government guidance was clear in relation to shielding and furlough leave for care workers? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
40 CMM December 2022 SETTLING DISPUTES: PREPARING FOR EMPLOYMENT LEGAL CHALLENGES
Alan Lewis is an Employment Partner at Constantine Law. Email: Alan.lewis@constantinelaw.co.uk Twitter: @AlanLewisCL
Care Management System

Providing
Included in the suite: Care and Support, our care planning platform. Policies and Procedures.





Quality Assurance, our audit and inspection records app. Supervision and appraisal records.
Mandatory Training (with Matrix) and Care Certi cate.
CMM December 2022 41 Over 80,000livesworldwidechanged
care
care.
the intelligent software solution for
home and domiciliary
Care England 2023 Conference & Exhibition Thursday 16 March 2023 Church House Conference Centre, Westminster, London Don’t miss out! Book your place now! Exhibition and seminars: Learn from the specialists Engage with 40 leading product and service suppliers in the exhibition and choose from 12 seminars in the afternoon session. Find out more about their contribution to the successful delivery of quality care. First speakers confirmed! The first speakers have now been lined up to present at the Care England Conference & Exhibition, ‘Thriving Not Just Surviving’. Visit the Care England website for up to date information.

Looking Overseas:
HOW TECHNOLOGY IS BEING IMPLEMENTED ACROSS THE GLOBE
For some time now, the UK Government has urged social care providers to embrace the world of digital to improve health and social care integration. In this article, Andrew Coles, Chief Executive of Person Centred Software, unearths the latest trends on ageing and looks to the Netherlands and Australia to share models of innovation.
Technology keeps improving every year, bringing us new innovations and helping us to improve project delivery worldwide. In the field of adult social care, digital technology has the potential to transform services and offer a wealth of opportunities.
Digital technologies played a critical role in supporting people receiving care, care providers and care organisations throughout the pandemic. As a result, despite many
challenges, the adult social care sector and the UK Government have continued to adapt at scale and pace to provide support for communities.
Policy proposals
Integrating health and social care services has been a long-standing goal for many years, with several policies having been written and published in the last decade.
In 2014, NHS England published a strategy called Five Year Forward View, which outlined a vision to transform the NHS and social care in England to become more integrated. The NHS Long Term Plan then followed, published in 2018, to set out additional steps towards integration. Then, in 2021, a White Paper was published: Integration and

innovation: working together to improve health and social care for all, setting forth legislative change to enable better integration in England. Finally, in 2022, the Health and social care integration: joining up care for people, places and populations policy was published, setting out measures to make integrated health and social care a universal reality for everyone across England, regardless of their condition and where they live.
Understanding trends
The Centre for Ageing Better reports that almost 11 million people in the UK are aged 65 and over, representing 19% of the UK population. Over the next ten years, the number of people aged 65 and older is projected to rise to 13 million, that's 22% of the population.
According to our National Health Service, in England, it is estimated that around 676,000 people are affected by dementia. Across the UK, the number is estimated to be around 850,000, which is predicted to rise exponentially to 1.6 million by 2024. The King's Fund reports that around 15 million people
in England have a long-term condition, which is rising. Most people are receiving good care, yet more could be done to support effective pathways for people with long-term conditions, preventing health problems from escalating and avoiding hospital admissions.
The British Medical Journal (BMJ) reports that an increasing number of people are waiting for treatment. The latest figures show:
• A record of over 6.84 million people waiting for treatment.
• 2.67 million patients are waiting over 18 weeks for treatment, a further increase from last month.
• 377,689 patients are waiting over one year for treatment, which is over 365 times the 1,032 people waiting over a year pre-pandemic in July 2019.
• A median waiting time for treatment is 13.3 weeks, which is significantly higher than the pre-COVID duration.
It is therefore important to keep track of health and care statistics to better understand trends in the population, patterns of medical conditions and the ever-growing need for healthcare. The adoption of digital social care records
CMM December 2022 43
>
and other care technologies, such as Person Centred Software’s digital care planning systems, will give care providers more time to care and strives to improve quality, efficiency and outcomes for those living and working within the sector.
Further afield: Australia
While the UK's social care providers are undergoing a digital transformation, with 30% currently using paper-based systems and 30% partially digitalised, Australia has already embraced digital solutions and is way ahead of the game. Innovative technologies have long been used to improve healthcare delivery in Australia's health sector. In recent years, digital technologies have made healthcare services and products more accessible and available, particularly during the COVID-19 pandemic, enabling providers and users to improve health outcomes and strengthen data systems.
Shifting the focus
The Aged Care Workforce Report revealed that the workload for aged care staff is increasing. During the past year, 94% of workers experienced an increase in workload due to COVID-19 regulations. Also, 85% of workers reported a higher workload after the introduction of the 2019 Aged Care Quality Standards. By 2021, 85% of workers reported increased workloads due to COVID19 regulations and 74% reported increased workloads due to Aged Care Quality Standards. Both numbers increased by 10% in 2022.
Managing an increasing volume of paperwork requires aged care workers to have the right tools. Last year, the Australian Government approved the development of the Australian National Aged Care Classification (AN-ACC) and replaced the Aged Care Funding Instrument (ACFI). The AN-ACC will reduce the administrative burden of completing assessments and offers consistency in the types of assessments used. With this switch, documentation has shifted from primarily funded-driven, as with ACFI, to documentation with a re-enablement approach. AN-ACC helps address critical issues around care quality, including appropriate staffing and more transparent and equitable funding. It puts the focus of funding in aged care directly back on the care needs of the residents. Person Centred Software's globally recognised Clinical Care System was Australia's first fully mobile clinical documentation system. In addition to being
fully mobile, carers can evidence care at the point of delivery, and the icon-driven interface streamlines the entire process, which encourages carers to record and evidence more care notes.
A role model: The Netherlands
By 2040, the number of Dutch people aged 75 and older is expected to double, reaching almost 2.5 million. The Netherlands spends among the highest proportions of GDP on elderly care. The Dutch Government is concerned that the share of the workforce helping the sick and frail could rise from oneseventh to one-third.
In the Netherlands, the healthcare system is based on several principles that are more or less universal:
• Access to care for all.
• Solidarity through medical insurance (which is compulsory for all and available to all).
• High-quality healthcare services.
Due to an ageing population, rising healthcare costs and a staff shortage, the Netherlands is moving away from complexity and regulatory burdens to more innovative, data-driven and digital approaches. With the early adoption of digital health, a highly developed health information infrastructure and efficiently digitised primary care, the Dutch life sciences and health ecosystem is already a role model.
Recently, the Government's policy has been to help more and more older adults live comfortably at home because it's cheaper to do so than to put people in nursing or care homes. Homecare organisations assist older adults living in their own homes by helping them with day-to-day activities, such as getting in and out of bed, getting outside, dressing, eating and drinking, using the toilet and personal hygiene. Care software in the Netherlands provides medical and social care to people at home. An assessment by trained nurses is carried out to identify the person’s needs and to develop a tailored care plan. The aim is to define care objectives for each problem area and to monitor progress continuously. In addition, the software helps to guide and document the entire care process.
Technological innovations have supported integrated care for a relatively long time. As a result, a number of technological innovations are in place locally and nationally that support integrated care, including electronic client/patient records that enable GPs, homecare agencies and hospitals to exchange client information.
The Dutch Government is constantly developing new and improved artificial intelligence systems to cut down expenditures. For example, new AI technology is currently being developed to assist the elderly in taking care of themselves.
Provider take-homes
The Australian Government has acknowledged aged care workers' demand for more pay and has pledged to cover any potential pay rise for aged care workers. The UK should follow suit; if care workers were paid competitive wages, particularly for lower-paid employees, it would significantly reduce staff turnover in the care sector.
In the Netherlands, care providers are incentivised to innovate and research how technology can enable better outcomes. Consequently, new technology has been embraced with positive results, meaning other territories can look to follow suit with less risk of failure.
The Netherlands has also redefined what a care home looks and feels like, making them more community based. Suitable housing and healthcare facilities for the elderly are a priority for the Government. For example, Hogeweyk Dementia Village in the Netherlands features 23 uniquely styled homes furnished around the period when residents’ short-term memories stopped adequately functioning. The houses resemble the 1950s, 1970s and 2000s because it helps residents feel at home. Its residents are served and cared for by 250 full-time and part-time geriatric nurses and specialists who wander the town and hold various occupations in the village, such as cashiers, grocery-store attendees and post-office clerks.
Championing independence
The UK is far from alone in facing the implications of an ageing population. To reduce pressure on adult social care and the NHS, as well as ensure people can live fulfilled lives, we must support older people to live as independently as possible, in line with the Dutch Government's policy. A similar strategy is in place in Australia, helping people stay as healthy as possible for as long as possible. What’s key in the ongoing discussions is that healthcare providers must evolve to meet the challenges of an ageing and growing population and, at the same time, champion independence to help ease pressures. CMM
LOOKING OVERSEAS: HOW TECHNOLOGY IS BEING IMPLEMENTED ACROSS THE GLOBE 44 CMM December 2022
What types of technology software has your organisation benefited from? And what’s your reaction to the Dutch and Australian models outlined in this article? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
>
Andrew Coles is the Chief Executive of Person Centred Software.
Email:
hello@personcentredsoftware.com Twitter: @PersonCentredSW






Care Choices Ltd 3, Valley Court Offices, Lower Rd, Croydon, Nr Royston, SG8 0HF (01223) 207770 www.carechoices.co.uk Care Information Search for Care Blog Publications Useful Contacts Contact Us Details Features Care Choices is the reliable place to find the care that’s best for you and the information you need. Whether you’re looking for a care home or ideas on staying independent at home, this website has been designed to make it easy for you. ENHANCE YOUR PROFILE TODAY www.carechoices.co.uk 01223 206967 І paul.ocallaghan@carechoices.co.uk * Minimum booking period is 1 year. Price excludes VAT. For full details of opportunities to promote your service on the website, contact us. Promote your service to care seekers for as little as £4.71 per week*
CELEBRATING EXCELLENCE
Markel 3rd Sector Care Awards


CMM is thrilled to share the stories of two outstanding individuals. Firstly, Christina Earl, Head of Innovation and Business Development at Surrey Choices, tells the story of her colleague Karen Breakspear, winner of the Compassion Award. Secondly, we hear from David Higham, Founder and Chief Executive of The Well Communities CIC, who won the Leadership Award.
Karen Breakspear, Surrey Choices
One of the simplest, but most powerful of Surrey Choices’ values is ‘be kind’. Our nominee and winner of the Compassion Award at the Markel 3rd Sector Care Awards 2022, Karen Breakspear, really demonstrates this value, along with all our core values. Surrey Choices is a local authority trading company owned by Surrey County Council who provide a range of services for disabled people from Shared Lives to day activities in the community.
Above and beyond expectations
Karen works for our award-winning Supported Employment Service (EmployAbility), which helps people find their perfect job matches, whether that be full-time, paid work or a few hours per week volunteering. Karen works just 20 hours a week, but in that time, she often ranks amongst the top performers in the Supported Employment Service team against others who are working full
time (37.5 hours). In the year of her nomination, Karen achieved 30 outcomes for her job seekers –five paid jobs, 18 work experience placements and seven voluntary placements.

Karen was even able to continue to find opportunities during lockdown. Karen offers every single job seeker a personalised service, along with building extraordinarily strong relationships with other stakeholders. Karen continues to work with employers, jobcentres, families and other professionals. She shows creativity and a commitment to breaking down barriers to work and inclusion and is a real inspiration to her colleagues and the people we support.
‘Karen Breakspear is a phenomenal individual and one of the most kind-hearted and loving people I know. I have known Karen for about three to four years and throughout that time she has been extremely supportive to me in all of my employment endeavours. From changing jobs to dealing with employment paperwork, not to mention
46 CMM December 2022
her assistance in helping me find stable and secure work during COVID-19 so that I might avoid being furloughed. Karen Breakspear is an extraordinary individual who we are all better for knowing.’ A jobseeker supported by EmployAbility.
Creating lasting relationships
However, Karen’s ability to form such strong relationships is only part of the reason for her nomination. During the pandemic, Karen volunteered to work additional hours with Surrey Choices’ emergency weekend and evening respite service – Flexi-Choices. Supporting people whose family were in crisis due to lockdown and at risk of family breakdown. For this work, Karen had to adapt her skills as she worked with a range of people – from those with very complex learning disabilities to others who were just struggling emotionally to cope with lockdown.
One young lady was demonstrating risky behaviours, mainly relating to drugs and relationships. Karen was not judgmental but raised her self-esteem and suggested alternative lifestyle choices. It was challenging to encourage her to engage, but Karen was persistent and consistent. Eventually, the young lady built a trusted relationship with Karen and started to change her behaviours including looking for paid work and finding a regular partner.
‘[She] is more engaged with Karen than all other professionals involved in her care. It is clear that the client's welfare is at the heart of everything she does and her dedication to her work is obvious.’ Mental health social worker
We would like to thank the Markel 3rd Sector Care Awards for allowing us to celebrate some of the amazing work that happens every day in social care but is often unnoticed. Even in these tough times, compassion in social care is essential at all levels and it is a good reminder to us all to embed this into our practice, as it is not only desirable, but really does improve outcomes for everyone.
2012, and a further four sites quickly followed in Lancashire and Cumbria.
Shaping effective recovery
The Well reflects my vision of what recovery services should look like – inclusive, nonjudgemental, inspirational and effective. It focuses on peer mentoring; my view is that long-term recovery can happen through the therapeutic value of one person with lived experience helping another. I set up The Well with my own money and with no blueprint to follow. Instead, I used my experience, vision and determination to create what has now become a leading provider of recovery services in the region. I often say that now is my time to ‘give back’ to society after taking from it for so many years.
The Well Communities CIC is a peer-led organisation that provides a range of services and initiatives to support mental health and addiction recovery. The organisation’s aim is to minimise the harm caused by problematic alcohol and substance misuse. Our key beneficiaries are drug and alcohol users and offenders, individuals experiencing mental health difficulties and their families. We provide housing, hospital and street outreach, therapeutic programmes and activities, ‘Through the Gate’ support and peer-run community hubs. Our community hubs offer people a chance to create a new future for themselves, co-produced with people who have successfully turned their lives around after seeking help.
Successful partnership working
In the past 10 years, we have co-produced various workstreams with statutory and Voluntary, Community, Faith and Social Enterprise (VCFSE) partners to identify (by determining community need through bootson-ground, locality-based community activism) and address health inequalities in cohorts with historically complex needs.
provides activities and support for people who are keen to move out of addiction or who have recently done so and are struggling.
Grow from within
Over 70% of individuals who use The Well’s services have histories of criminal offending and prison. This is also reflective of our staff who have similar histories. It is this personal and professional experience that helps us to achieve our objectives.
Currently The Well Communities CIC employs 64 staff, of which 60% have used our services. The Well has a grow your own model, meaning that the very people we support will be our next volunteers and staff. 60% of the staff at The Well have come through our support services. This enables us to always listen to the people we serve, but more so, they are the very people that drive the organisation as they shape, design and deliver our services. CMM
David Higham is
dave@thewell2.co.uk Twitter @thethewell2

David Higham, The Well Communities CIC
I left prison for the last time in 2007. Since then, I have dedicated my life to supporting others with drug and alcohol addiction through both voluntary and paid employment. Seeing a big gap locally in the support for people leaving prison with an addiction, I decided to set up The Well. The first hub was launched in Lancaster in
Our model is a whole-system approach with lived experience at the very heart of the hub. Much of our work also involves local placedbased community activism, including initiatives such as a social supermarket and food growing sovereignty schemes. A multi-thematic delivery ensures that there is no adoption of a one size fits all approach. A boots-on-ground approach links individuals with ground level needs with services, avoids missed appointments, provides genuine lived experience peer-to-peer support, creates mutual aid capacity (where currently there is none) and fosters long-term appropriate and relevant engagement.
The Well brings together people who are in stable, abstinent recovery from substance misuse to use their lived experience of addiction to support and help others. The Well also
Headline Sponsor

The Leadership Award was kindly sponsored by
The Markel 3rd Sector Care Awards is run specifically for the voluntary care and support sector. Visit www.3rdsectorcareawards.co.uk to view the 2022 event winners and find out more about next year’s event. Sponsorship opportunities are available.
With thanks to our sponsors: National Care Forum, Learning Disability England, The Care Provider Alliance, Association of Mental Health Providers and VODG.
Founder and Chief Executive of The Well Communities CIC. Email:
Christina Earl is Head of Innovation and Business Development at Surrey Choices. Email: christina.earl@surreychoices.com Twitter: @SurreyChoices
CMM December 2022 47
In this issue of CMM, we look back on the Berkshire, Buckinghamshire & Oxfordshire Care Association Conference.
The conference, in association with Berkshire Care Association, Milton Keynes and Buckinghamshire (MKB) Care Association and the Oxfordshire Association of Care Providers (OACP) took place at The Doubletree by Hilton St Anne’s Manor, Wokingham, on 20th October 2022. The conference sought to bring the quality of a national conference to a local stage, focusing on the issues that matter to providers in Berkshire, Buckinghamshire and Oxfordshire.
The day included presentations from high-level sector representatives, offering expert insight into the local picture, along with an exhibition of carefully selected services and products and a choice of interactive workshops to delve into a subject further. There were also several networking opportunities with like-minded providers and senior decision-makers from the independent care and support sector to learn more about delivering best practice in a changing market.
A hub of information
Delegates absorbed a powerful opening from the conference’s Chair, Fidelma Tinneny, Founding Member of Berkshire Care Association, who highlighted the sector’s strengths and objectives despite the barrage of financial and personnel challenges it continues to face.
Following this, the day’s keynote speech
was delivered by Matilda Moss, Head of Integrated Commissioning at Buckinghamshire County Council. Matilda presented the view from the council, which provided an overview of the changes providers can expect as a result of the latest Government reforms and how the local authority in Buckinghamshire aims to work alongside and support services. Next up was Dan Hayes, Chief Executive Officer at The Orders of St John Care Trust. Dan shared a provider’s view of how increased access to technology is helping to support people in a person-centred way against the backdrop of the latest Government reforms and White Papers.
In amongst exhibition viewing and an unmissable panel discussion featuring the conference’s speakers, Neil Eastwood, Founder and Chief Executive at Care Friends, dissected the timely subject of care worker recruitment. Neil communicated the latest thinking, research and innovation, drawing on his connections with employers of care staff from around the world.
Complementing the conference’s agenda, a selection of interactive workshops covered legal updates relating to the Care Quality Commission (CQC), how technology can help improve CQC inspections and the use of Artificial Intelligence (AI) in social care.
Neil Grant, Partner at Gordons Partnership, explained how services can best prepare for the changes to minimise the risk of regulatory intervention and downgrading of ratings. Peter Ellis, Director at Intelligent Care Software, discussed some of the reasons why social care
providers should consider using digital care management software. Lastly, Vayyar Imaging Ltd explored how simple pieces of equipment that use AI can benefit the sector in a non-intrusive way.
The conference’s afternoon offering picked up where the morning left off, discussing the sector’s hot topics and their application to the adult social care landscape in the area. Delegates were joined by Catherine Mountford, Director of Governance at Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board, who revealed changes to Integrated Care Boards and Systems, including a whistlestop tour of how the local system will work, its aims and priorities.
In addition, Richard Ayres, Social Care Adviser at Care England, examined the Fair Cost of Care exercise and Amy Morgan, Youth Development Lead at The Prince’s Trust, closed the conference by summarising how it works with and supports young people to access employment and start their careers in the health and social care sector.
Our thanks go to the conference’s sponsors and exhibitors for making the event possible.
Book now
Book your tickets today for the CMM Insight Lancashire Care Conference, taking place on 30th November in Blackburn. View the conference’s full agenda by visiting the CMM website and join the conversation on Twitter by tagging @CMM_Magazine and using the hashtag #CMMInsight. CMM
EVENT REVIEW
20th October 2022, Wokingham CMM INSIGHT BERKSHIRE, BUCKINGHAMSHIRE & OXFORDSHIRE CARE ASSOCIATION CONFERENCE 2022 Look out for announcements about CMM Insight events happening in 2023 @CMM_Magazine #CMMInsight
48 CMM December 2022
www.caremanagementmatters.co.uk
WHAT’S ON?
Event: Date/Location: Contact:
Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact:
The NCF CEO Conference 28th-29th November 2022, London www.nationalcareforum.org.uk/events
Embracing apprenticeships, Skills for Care 30th November 2022, online www.skillsforcare.org.uk/news-and-events
Liberty Protection Safeguards 15th December 2022, online www.socialcareconferences.co.uk
Digital Technology and Transformation in Homecare 19th January 2023, London www.digitalsocialcare.co.uk/events
The Managers Conference 2023 (hosted by The National Care Forum, Skills for Care, in association with Association for Real Change (ARC) 13-14th March 2023, Leicester www.nationalcareforum.org.uk/events/themanagers-conference-2023
Care England Conference and Exhibition 2023 16th March 2023, London www.careengland.org.uk/events/care-england
CMM EVENTS


Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact:
The Lancashire Care Conference 30th November 2022, Blackburn www.caremanagementmatters.co.uk/event
Markel 3rd Sector Care Awards 3rd March 2023, Birmingham www.caremanagementmatters.co.uk/event/ markel-3rd-sector-care-awards-2023
The Bloody Awesome Parents Awards (BAPS) 20th April 2023, Leicester www.myfamilyourneeds.co.uk/baps
CMM December 2022 49
Please mention CMM when booking your place. Sign up online to receive discounts to CMM events.
FREE PROVIDERS Non-care providers receive a three month free trial, £50 per year thereafter. *Cannot be used in conjunction with any other offer. Sign up at www.caremanagementmatters.co.uk @CMM_Magazine SIGN UP FOR Yes, that’s right. Absolutely free. Gain CPD points Access extended features and additional content Read latest news email alerts Comment on features and debate on important subjects Get discounts to CMM Insight events* Access archived editorial Receive a digital edition of CMM (10 issues per year)
MELANIE WEATHERLEY MBE • CHAIR • LINCOLNSHIRE CARE ASSOCIATION

We need to be making sure we’re looking after our existing workforce wherever we can.
Good leadership will be vital for local systems as they become established during challenging times for all services. We’re lucky in Lincolnshire to be working closely with excellent colleagues across the health and care system to support our colleagues in the field – in particular, innovative joint working is being developed to reduce avoidable visits to hospital. We know that this is not replicated everywhere and that all too often care providers are not included.
Care homes and homecare providers in Lincolnshire are doing everything that they can to recruit and develop more staff, including looking overseas, but I agree with the CQC’s report, social care needs substantial, sustained funding to survive.
The Care Quality Commission’s (CQC’s) latest State of Care report paints a bleak picture of the state of our current system. Far too often, people aren’t able to access the care they need, with devastating consequences. The sector is fundamentally underfunded by the Government and all we’re doing is sticking plasters on these problems to help keep the NHS afloat.
The heart of these problems stem from a calamitous lack of staffing in social care. Shortage of staff continues to place a momentous strain on services, and now we’re also contending with rising costs due to inflation, increases in energy bills and the cost of fuel for travel; the list goes on and the pressure is piling high.
Capacity in adult social care has reduced and unmet need has increased, according to CQC’s annual report, with only two in five people able to leave hospital when they are ready to do so. This is contributing to record-breaking
waits in emergency departments and dangerous ambulance handover delays. People can’t get care where they need it, as there’s just not enough people to look after them.
The challenges we’re now facing have developed from deep-rooted, inadequate underinvestment and lack of recognition for the social care sector. Recruitment struggles in the sector aren’t a new thing; in fact, this has been an issue for years, and we are in serious need of a drastic overhaul. People aren’t wanting to work in a service that is underfunded and underpaid, it’s not a desirable career route in its current state. This needs to fundamentally change.
Many will turn to the question – why can't care providers just pay their staff more? The truth is inflation is affecting everyone the same way it’s affecting us, but we can’t hike our prices up as other businesses can. The cost of caring is increasing, and we simply can’t
charge our end users more for the service they need. Care isn’t a luxury, it’s a necessity. Social care is fantastic at making money go a long way, but if we haven’t got any, we can’t work miracles.
If it hasn’t already been made clear, there needs to be a real investment in social care and a push for decent wages for the thousands of social care workers across our country. We can’t improve social care on our own. We need funding – and adequate funding at that – to be trickled down from the top. The Department of Health and Social Care needs to take action and take action now.
Recruiting needs to be the focus. We need to look at new ways to recruit people into the sector, can we target the 55+ age bracket? Can we offer incentives for people to return to the workforce who have been out of the sector since the pandemic? Can we offer more flexible working arrangements to adapt to people’s lifestyles?
Our workforce is fabulously resilient; this was evidenced particularly well during the pandemic when we were left without adequate support. However, the drop in the number of people employed in the social care sector, when demand is rising, is very worrying, but not surprising, as many are exhausted and disillusioned.
It is likely that this winter will present as much of a challenge as the pandemic. We need to attract new staff and retain and motivate those that we have. We must recognise the value of our workforce in pay, as well as development and career opportunities. The level of skill and compassion that they show in caring for our most vulnerable citizens deserves far more than current funding levels allow providers to pay. A well-motivated and fully staffed social care sector is essential in supporting the NHS through winter, as well as enabling individuals to live fulfilled lives.
And does your organisation actively encourage applicants from people aged 55+? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
What are your comments and response to the CQC’s State of Care
50 CMM December 2022
Winter is looming and the sector is bracing for a difficult time. Here, Melanie Weatherley MBE sets out her thoughts on what needs to be done locally and by Government to ease pressures.
Melanie Weatherley MBE is Chair of Lincolnshire Care Association. Email: melanie@walnutcare.co.uk Twitter: @MelanieWeathe12
report?
The Care Innovation Challenge is a hackathon-style creative weekend of idea generation and prototype trialling in July 2023. With cash prizes for the top spots, expert mentoring and guaranteed media coverage this is an opportunity not to be missed.


You can apply as a team or as an individual. Teams must be 2-3 people. Visit www.careinnovationhub.org.uk

Who can apply? • University students • Entrepreneurs • Working professionals • • People with lived experience of care and support
REGISTER NOW Want to h elp i mp rove th e qual ity of li fe of thos e receiving care in the U K? The Care Innovation Hub hosts an annual incubator programme that brings together innovators and problem solvers with care providers and people with lived experience to create solutions to key challenges









BOOK YOUR TICKETS NOW Friday 3rd March 2023 The Grand Hotel, Birmingham W1K 6JP www.3rdSectorCareAwards.co.uk @3rdSectorCare #3rdSectorCareAwards 3RD SECTOR MARKEL CARE AWARDS OrganisedbyHeadlinesponsorSupportedby Don’t miss this chance to celebrate