NAVIGATING 2023 What providers need to know Getting ahead Shifting mindset Resource Finder Preparing for the CQC framework Developing a wellbeing plan Technology FEBRUARY 2023 www.caremanagementmatters.co.uk












22-23 March 2023 NEC Birmingham
THE CARE COMMUNITY REGISTER FREE UKCAREWEEK.COM
UNITING
Professor Martin Green Chief Executive, Care England
Jayne Connery Director/Founder, Care Campaign for the Vulnerable
Lucy Buxton Nurse and NLP Trainer/Coach, LjB Coach Consultancy ltd
Amrit Dhaliwal CEO, Walfinch
Kerry Southern-Reason Managing Director, The Care Home Interiors Company
Anthony Snape Director of Technology, The Care Quality Commission
Social Care Insights
Simon Bottery updates on international recruitment policy and reviews its importance within the Government’s wider social care workforce recruitment strategy.
Inside CQC
While we await further updates on the CQC’s winter inspection process, a CQC spokesperson answers three questions relating to regulation and visiting.
CMM News
Into Perspective
In this issue, our sector experts consider how employers can create a multigenerational social care workforce.
Celebrating Excellence
CMM is delighted to announce the Markel 3rd Sector Care Awards finalists for 2023 and we find out what impressed the judges.
Event Review
CMM reviews the Global Social Prescribing Arts for Brain Health Conference.
What’s On?
Straight Talk
Kathy Roberts, Chief Executive of the Association of Mental Health Providers, updates on the provision of mental health services and reveals the details of a new campaign.
In this issue REGULARS
Navigating 2023: The journey continues Professor Vic Rayner OBE, Chief Executive of the National Care Forum (NCF), outlines the key factors she believes will influence care providers in 2023.

Preparing for the new CQC framework: 13 ways providers can plan ahead The Care Quality Commission (CQC) announced a new strategy which will bring all health and social care providers under one single framework. Helen Fuller, Director at Care 4 Quality, shares her tips on how to prepare.
The tipping point: Understanding the funding gaps in social care

Richard Ayres, Social Care Advisor to Care England, delves into the detail of Government’s funding measures and outlines next steps for the Fair Cost of Care exercise.
Shifting mindset: Why you need to think differently about staff wellbeing


Staff wellbeing should be as important as the wellbeing of people in care, writes Sophie Coulthard, Principal Consultant at Judgement Index. In this article, Sophie explains how develop a robust wellbeing plan.
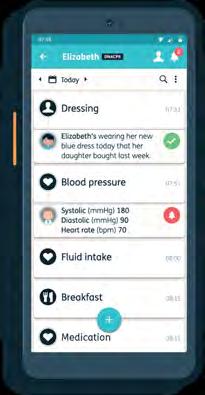
Resource Finder: Technology
CMM profiles some of the leading technology companies, specialising in adult social care, to help providers implement technology solutions effectively.

CMM February 2023 3
FEATURES
05 07 09 30 46 48 49 50
40 25
40
20 25 33 36
20 33 36
EDITORIAL
editor@caremanagementmatters.co.uk


Editor: Olivia Hubbard
Commissioning Editor: Angharad Burnham





Content Editors: Aislinn Thompson, Henry Thornton
PRODUCTION
Designer: Rebecca Mendil

Director of Creative Operations: Lisa Werthmann
Studio Manager: Jamie Harvey
ADVERTISING
sales@caremanagementmatters.co.uk 01223 207770
Advertising Manager: Aaron Barber aaron.barber@carechoices.co.uk
Director of Sales: David Werthmann david.werthmann@carechoices.co.uk



SUBSCRIPTIONS
Non-care and support providers may be required to pay £50 per year. info@caremanagementmatters.co.uk 01223 207770 www.caremanagementmatters.co.uk
Care Management Matters is published by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2022
CCL REF NO: CMM 20.0
CMM magazine is officially part of the membership entitlement of:
4 CMM February 2023
Kathy Roberts Chief Executive, the Association of Mental Health Providers
@KathyRobertsMH
CONTRIBUTORS @blimeysimon Simon Bottery Senior Fellow in Social Care, The King’s Fund Dr Emily Andrews Deputy Director of Work, Centre for Ageing Better @emilyishness @CQCProf Phil Pegler Managing Director, Bluebird Care @bluebirdcare Richard Ayres Social Care Advisor to Care England @CareEngland Helen Fuller Director, Care 4 Quality @Care4Q @CQCProf Professor Vic Rayner OBE Chief Executive, The National Care Forum (NCF) @vicrayner Sophie Coulthard Principal Consultant, Judgement Index @judgementindex CQC Care Quality Commission
Are you getting the benefit of the CMM website? Sign up today to start getting more from CMM. It’s FREE for care providers.
www.caremanagementmatters.co.uk
SOCIAL CARE INSIGHTS
From Simon Bottery
Immigration is helping ease England’s short-term social care recruitment problems but a longer-term solution requires wider action, says Simon Bottery.

One of the more surprising and outspoken reports covering social care came out just before Christmas, by a body whose main remit isn’t even social care.
The Migration Advisory Committee (MAC) is an independent, advisory non-departmental public body, sponsored by the Home Office. As the name implies, it advises the Government on immigration policy. Yet it has recently taken quite an interest in social care.

That’s mainly because in July 2021 the Government asked it to look at immigration and recruitment in the adult social care sector. Very quickly, it recommended changes –accepted by the Government – to make it easier for migrant care workers to come to the UK.
Care workers became eligible for the Health and Care Worker Visa and the occupations were placed on the Shortage Occupation List (SOL).
But the MAC didn’t stop there. In its next report, it said that immigration was not really the key to solving problems in adult social care recruitment at all. Rather, it said, ‘properly funding social care to allow improvements in pay and conditions’ was the real issue. This time the response from Government was stony silence.
Roll forward to Christmas 2022 and the MAC published its annual report for the year. It demonstrated that hell hath no fury like a non-departmental public body scorned. The MAC said, ‘The conditions now faced by the social care
sector are unsustainable’, yet the Government ‘appears to have no ambitions to raise pay in a material and properly funded way.’ Icily, it said, ‘We look forward to seeing a full response from the Minister for Immigration and the Secretary of State for Health and Social Care as soon as possible.’
What are the messages for social care policy from this long-running saga?
Firstly, most obviously, that pay is critical to recruitment but that the care sector – for a number of reasons – is failing to pay staff enough to recruit even sufficient workers to fill existing vacancies. This is a critical, longterm issue that the Government has so far – to the MAC’s annoyance – studiously ignored. That must change.
Secondly, that immigration can clearly help alleviate some of the short-term recruitment issues in social care – and is in fact already doing so. Since the visa and Shortage Occupation List changes in December 2021, growth in visa applications for senior care workers have more than doubled (to 14,000 in the year to September 2022), and there were nearly 15,000 applications for care workers between February and December 2022. This will not solve the recruitment crisis, but it will help – and there is even some polling evidence to suggest that the public supports it.
Thirdly, however, we should acknowledge that the level of recruitment needed in social care in coming years cannot be met simply by overseas recruitment. Skills for Care estimates that 480,000 new care workers will be required by 2035. Even if we set aside the ethical issues about overseas recruitment, it is inconceivable that immigration can contribute that number. In 2018, non-British people made up only one in seven social care workers in England and that percentage had been consistent for several years.
Work on how we recruit and retain the next generation of care workers needs to begin in earnest.
CMM February 2023 5
Simon Bottery is a Senior Fellow in Social Care at The King’s Fund. Email: S.Bottery@kingsfund.org.uk Twitter: @blimeysimon
What is your experience of international recruitment? Share your feedback on the points raised in this column. Visit www.caremanagementmatters.co.uk
Learn how Sage can help:


software that helps care homes thrive
• Increase revenues by 25% without adding additional headcount.
• Save over 400 person-hours annually.
product
• Streamline your operations and automate your financials. Download
brochure
Inside CQC
AN INTERVIEW WITH THE REGULATOR
The regulator is working on some significant changes in 2023. While we await further updates on regulation and inspection from the regulator, providers and leaders in care put forward their questions to the CQC. This month, we discuss the new framework, regulation and unannounced inspections of care homes.
Question: How does the CQC plan to help provides navigate the new world of regulation?
CQC: Our new single assessment framework is for providers, local authorities and systems. It focuses on what matters to people who use health and social care services and their families. It will let us provide an up-to-date view of quality. It covers all sectors, service types and levels – from registration, to how we look at local authorities and integrated care systems.

Quality statements will set clear expectations of providers, based on people’s experiences and the standards of care they expect.
We will:
• Use a range of information to assess providers flexibly and frequently. Assessment is not tied to set dates or driven by a previous rating.
• Collect evidence on an ongoing basis and can update ratings at any time. This helps us respond more flexibly to changes in risk.
• Tailor our assessment to different types of providers and services.
• Score evidence to make our judgements more structured and consistent.
• Use inspections (site visits) as a vital tool to gather evidence to assess quality.
• Use data and insight to decide which services to visit. When on site, we will
observe care and talk to staff and people who use services.
• Produce shorter and simpler reports, showing the most up-to-date assessment.
We’ll continue engaging on our new ways of working and give providers plenty of notice before regulatory changes are likely to affect you. We’ll provide full provider guidance on the new approach plus a range of other content, such as videos and podcasts. Sign up to our email bulletins for the latest updates, watch our videos on YouTube or catch up with our podcasts.
Question: Would the CQC be able to clarify what ‘smarter/dynamic regulation’ means? It suggests a shift in the effort of regulation from the CQC to providers – is this the intention?
CQC: We’ve developed a new regulatory model. This new single assessment framework will change the way we operate and allow us to give a more up-to-date view of quality across health and social care – it will be smarter and more dynamic. You can find the quality statements and evidence categories on our website.
We’ll move away from our current ‘monitor, inspect, and rate’ approach, towards a more flexible approach where inspections won’t be set by frequency and where ongoing assessment of quality will be proportionate to risk. Assessment won’t always be tied to
inspection and won’t be tied to set dates or driven by a previous rating. As part of this, we will use a range of information to assess providers flexibly and frequently.
We’re working with other national organisations who collect data to avoid duplication and additional burden being placed on providers around data collection. We’ll also work with formalised integrated care systems for the same purpose. While this work isn’t completed, we've made the commitment to rationalise where we can minimise the burden on providers.
Question: What is the CQC’s understanding on the impact of unannounced visits to registered care homes. For example, where the manager may not be present, meaning staff are being required to neglect their support duties?
CQC: We would still undertake an inspection in absence of the registered manager who should ensure there are appropriate staff still in place to meet the needs of the people using the service safely and effectively. We understand a registered manager can’t be present 24/7.
If a registered manager wasn’t present, we would talk on the day with the most senior person on duty, following up with the registered manager or registered provider off site after the inspection if necessary.
We would, of course, consider the impact of any inspection on the operation of a service as delivering safe care is always the priority.
CMM February 2023 7
Do you have a question for the CQC? Get in touch with CMM by emailing: editor@caremanagementmatters.co.uk or send us message on Twitter: @cmm_magazine
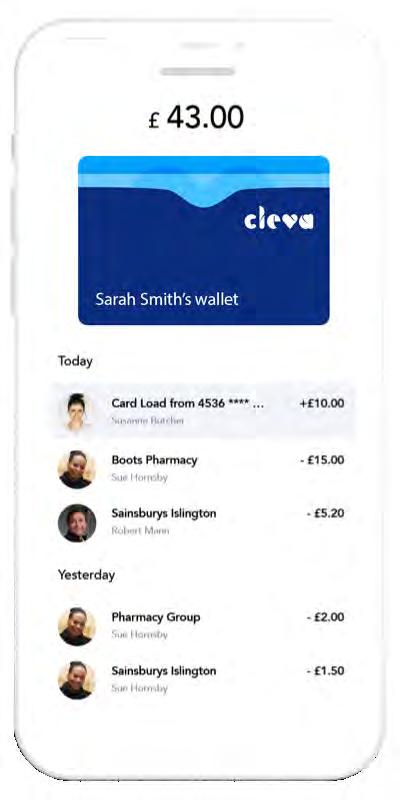
Since the introduction of Cleva’s card and app we no longer have to manually reconcile every




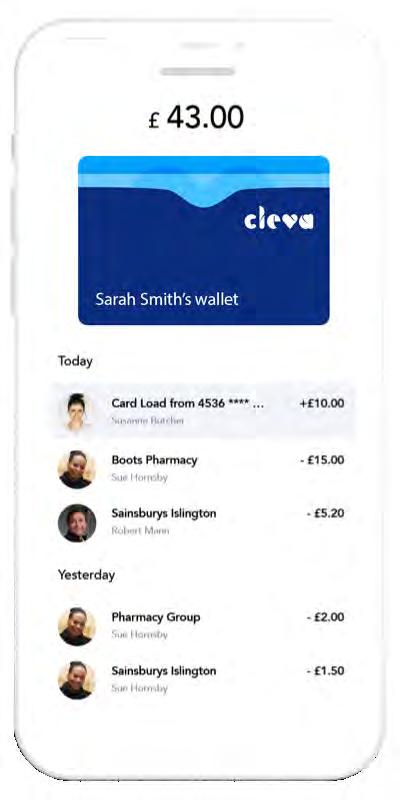
The fact that Cleva does this automatically is incredible - it’s a much more efficient system and a solution where everyone wins!
spending with our shopping card for carers
Revolutionise
payment.
Home
Cleva lets your care team shop for clients, safely and simply. Find out more at clevacard.com Want to see Something Cleva? “ “ Mastercard is a registered trademark and the circles design is a trademark of Mastercard International Incorporated. The Cleva card is issued by Transact Payments Limited pursuant to licence by Mastercard International Incorporated. Transact Payments Limited is authorised and regulated by the Gibraltar Financial Services Commission
Greg Brown, Franchise Owner
Instead Reigate and Tandridge
DHSC outlines hospital discharge plan
The Government plans to make available up to £200m of additional funding to immediately buy short-term care placements, to allow people to be discharged safely from hospitals into the community.
The move aims to free up hospital beds so people can be admitted more quickly from A&E to wards, reducing pressure on emergency departments and speeding up ambulance handovers. There are currently around 13,000 people occupying hospital beds in England who are fit to be discharged. The
plan will involve six areas trialling innovative long-term solutions to free up hospital beds and make sure patients get the right care at the right time, which could be rolled out across the NHS if successful.
Professor Martin Green OBE, Chief Executive of Care England said, ‘It is the right policy to discharge people from the hospital when they are medically fit, but again, the Government has sought to impose this on the care sector without proper consultation. This policy will fail unless it is driven by a
national approach with a proper NHS tariff and specification. If the Government leave it to localism, it will fail.’
Reacting to the news and the detail of the Government’s plan, Simon Bottery, Senior Fellow in Adult Social Care at The King’s Fund told CMM, ‘The detail of this on a local level will be critical because what needs to happen is the NHS needs to work really closely with local authorities to make sure people are getting the rehabilitation and the care and support they need in the right place to regain independence.’
Professor Vic Rayner OBE, Chief Executive of the National Care Forum said, ‘The emergency funding is indeed welcome. This is a situation where care homes can and do make a real difference, enabling people to leave the acute system, gain support and rehabilitation and then continue their journey home. This is already happening in many parts of the country and the additional funding will make this happen at pace. However, in the rush to discharge it is important that the strategic lessons are learned.’
Care sector recognised in New Years Honours
The social care sector has been widely recognised in the 2023 New Year Honours list. Key leaders in the care sector included Dr Jane Townson, CEO of the Homecare Association, who has been awarded an OBE for her services in the homecare sector, with a particular focus on the COVID-19 pandemic.
Nadra Ahmed OBE DL, Executive Chair, National Care Association also received a New Year Honours for her services to social care and Martin Jones, Chief Executive of Home Instead also received recognition for his services to older people. Professor Deborah Sturdy OBE has
also been awarded a CBE in the 2023 New Year Honours list.
On receiving the award, Dr Jane Townson OBE said, ‘To be recognised with an OBE is humbling and I am very grateful to those who nominated me. May the spotlight shine on all homecare workers, managers, and leaders, who dedicate themselves to improving the lives of others with the utmost compassion and commitment.
Nadra Ahmed OBE DL, Executive Chair, National Care Association, said, ‘It was a very pleasant surprise and bit overwhelming. It is a huge honour personally
but also important that colleagues working in social care has been recognised in this way. It feels like it highlights the recognition that social care needs to be at every table when looking at supporting people who need care and support across the country.’
Home Instead’s Chief Executive UK and International, Martin Jones, has been awarded an MBE in the 2023 New Year Honours for services to older people. Martin’s introduction to the care sector was through his father who needed support due to frailty in old age.
Speaking about the award, Martin Jones,
Chief Executive of Home Instead UK and International said, ‘I am proud and humbled to receive this award, particularly as it is for services to older people. Home Instead’s mission is to expand the world’s capacity to care – we want to make the world a better place to age in. For this to become reality, companies like Home Instead, the Government and broader society need to ensure that there is the infrastructure, resource and, importantly, people in place.’
Martin said that the integration of health and social care is critical, as is a mindset where old age is celebrated and revered.
APPOINTMENTS
Amber Housing
Amber Housing has appointed Peter Hall as its new Chair and appoints three new board members, Ashely Beaton, Nichola Harrison and Teresa Ocansey.
Belong
Specialist dementia care provider, Belong, has named Caroline Baker as its new Head of Dementia and Care Quality.
Community Integrated Care
Community Integrated Care has announced the appointment of Jim Kane as its new Chief Executive Officer. Since 2019, Jim has served as the charity’s Chief Financial Officer.
Elizabeth Finn Homes
Olivia Curno will join as the Chief Executive of Elizabeth Finn homes at the end of March 2023.
Hartford Care
Hartford Care has welcomed David Martins, who joins the company in a newly created role as Head of Sales and Marketing to support Hartford Care’s growth strategy.
Lilian Faithfull Care
Lilian Faithfull Care has announced that Suzanne Booker has taken over as Interim Chief Executive of its charity.
Salutem Care and Education
Michael Albero has been promoted to expand the role as Head of Regulation and Compliance, now also encompassing DPO (Data Protection Officer) and policy at Salutem Care and Education. Sally Jobling has been promoted to the role of Divisional Director for Supported Living.
CMM February 2023 9 NEWS
DHSC updates Discharge Fund guidance
The Department of Health and Social Care (DHSC) has set out further detail on how the £500m Adult Social Care Discharge Fund will be distributed, as well as conditions governing its use.
In a letter addressed to the social care sector from the Minister of State (Minister for Social Care), Helen Whatley, the sector heard how the following funding will be allocated:
• £200m will be distributed to local authorities, based on the adult social care relative needs formula (RNF). £300m will be distributed to integrated care boards (ICBs), targeted at those areas experiencing the greatest discharge delays. This is based on a combination of both: A fairshares distribution based on 2022 to 2023 ICB weighted populations (25% of ICB funding) a discharge metric flexed to reflect the size of the ICB weighted population (75% of ICB funding).
• The fund can be used flexibly on the interventions that best enable the discharge of patients from hospital to the most appropriate location for their ongoing care.
The Government added that funding should prioritise those approaches that are most effective in freeing up the maximum number of hospital beds and reducing bed days lost within the funding available, including from mental health inpatient settings. Funding can also be used to boost general adult social care workforce capacity, through staff recruitment and retention, where that will contribute to reducing delayed discharges.
The sector is said to expect the publication of the Workforce Recruitment and Retention Fund (WRRF) evaluation, to support the sector to prepare for this winter and support local areas in developing their plans on how to best utilise the workforce portion of this Fund.
Ombudsman reviews length of care home visits
Councils need to ensure any care visits they arrange give enough time for care workers to do their job properly, the Local Government and Social Care Ombudsman has said.
The warning comes after Warrington Metropolitan Borough Council was found to have allocated 15-minute care calls to more than 300 people in the region, despite national guidance stressing these were ‘not usually appropriate’.
In one case, which led to the Ombudsman’s wider investigation, care workers had sometimes stayed for just three minutes, despite the family paying for the full visit.
Michael King, Local Government and Social Care Ombudsman, said, ‘At the heart of this investigation are people, often vulnerable, who rely on care visits to give them the dignity and quality of life they rightly deserve.
Adding, ‘We are increasingly looking at complaints from a human rights perspective – and councils need to consider the
Chancellor of the Exchequer responds to letter
The Rt Hon Jeremy Hunt MP has responded to a letter, which put forward a series of questions following the Autumn Statement announcements.
On 28th November 2022, Baroness Andrews, Former Chair of The House of Lords Adult Social Care Committee, sent a letter to the Chancellor to understand the detail of the Government’s suggested funding objectives and support for the social care sector.
In relation to the funding breakdown, the Chancellor outlined £1bn of new grant funding in 23-24 and £1.7bn in 24-25. £600m of this in 23-24 and £1bn in 24-25 will be distributed through the Better Care Fund to get people out of hospital on time and into appropriate
care settings, aiming to free up NHS beds for those that need them. The Chancellor also said that £1.3bn in 23-24 and £1.9bn in 24-25 has been generated in savings from delaying the rollout of adult social care charging reform and will be distributed to local authorities through the Social Care Grant, ringfenced for adult and children’s social care. The Chancellor also wrote that the Government has listened to the concerns of local government and have taken the difficult decision to delay the planned adult social care reforms.
The Government is increasing the referendum limit for increases in Council Tax to 3% per year from April 2023. In addition, local authorities with social care responsibilities will be able to
increase the adult social care precept by up to 2% per year.
The Government expects local authorities to exercise restraint in setting Council Tax, balancing the extra income for local services against the tax burden on residents and cost of living pressures. Local authorities have the flexibility to design their own working age Local Council Tax Support schemes to protect their most vulnerable residents.
The letter confirmed that the Government will continue to take account of the ability of each local authority to raise Council Tax in its wider decisions on the allocation of funding within the Local Government Finance Settlement (LGFS). Further details will be set out by the Department for Levelling Up,
rights of service users to have a private life when commissioning or delivering care.
‘Councils also need to make sure that the care they arrange is sufficient to meet people’s needs. When looking at visits which may require care workers to dress, wash or feed a person, 15-minutes is rarely enough.’
The Ombudsman used its powers to widen an investigation when it appears other people may be affected by similar issues. This led to the Ombudsman finding 313 other people in Warrington had also been receiving these short calls.
The Ombudsman has the power to make recommendations to improve processes for the wider public. In this case the council will investigate a 10% sample of the people currently receiving 15-minute care calls to see if this is enough to meet their needs. Should this sample review identify anyone who should not be receiving such calls, the council will carry out a full review of all 313 cases.
Housing and Communities in due course.
Baroness Andrews asked the Chancellor to clarify the estimated 200,000 figure for care packages. Responding, he said the illustrative figure of an estimated 200,000 care packages was used to contextualise how many care packages the funding announced in the Autumn Statement could be equivalent to. It is based on an assumed average long-term care package of around £37,500 per annum. The Chancellor said that local authorities are best placed to identify and support the care needs of their local populations and, for example, may decide to prioritise the acuity of care rather than the quantity.
10 CMM February 2023 NEWS
Helping to simplify and digitise the care sector


CMM February 2023 11 Book a demo with us today 01483 357 657 www.personcentredsoftware.com
Centred Software offers a wide
of products,
the most widely used Digital Care Planning
to improve the quality and efficiency
the
social and health care settings, our Digital Care System provides a
of features focused on joining up health and social care.
your residents GP records in under 2 minutes
within our Digital Care System
all parties involved in the direct care of a patient to have access to shared information within
Person
range
including
System in the UK. Working
of
journey when transitioning between
variety
View
from
GP Connect Allows
England National Record Locator (NRL) Feel confident knowing that all critical resident information and relevant medical history are being shared with the urgent care providers who need it Hospital Pack
me to find out more
Scan
COVID-19 infections rise in UK countries
According to data published by the Office for National Statistics (ONS), COVID-19 infections continued to increase in England and Scotland and increased in Wales in the week ending 28th December 2022.
In Northern Ireland, COVID-19 infections increased in the week ending 22nd December 2022.
The estimated percentage of people living in private households (those not in care homes or other communal establishments) testing positive for COVID-19 is as follows:
• 4.52% in England (one in 20 people).
• 5.70% in Wales (one in 18 people).
• 6.43% in Northern Ireland (one in 16 people).
• 4.05% in Scotland (one in 25 people)
Meanwhile, the number of deaths involving COVID-19 increased
to 450 in England, Wales and Northern Ireland in the latest week (ending 23rd December 2022), accounting for 3.0% of all deaths in those countries.
Because of the recent bank holidays, data for Scotland is not available so ONS cannot provide a UK figure for the latest week.
Since COVID-19 reached the UK in early 2020, more than 500 million tests have been reported, more than nine in every 10 people aged 12 years and over have received at least two vaccinations and more than 150,000 people have died.
The ONS COVID-19 infection survey, run independently of Government testing, has conducted tests on hundreds of thousands of weekly samples to provide the best estimate of the scale of the pandemic, with a peak of one in 13 people infected in England in March 2022.
New minimum price for homecare
The Homecare Association has published its minimum price for homecare for April 2023 to March 2024. This minimum fee rate for the purchase of homecare by local authorities and the NHS has been calculated at £25.95 per hour. This allows for full compliance with the National Living Wage (£10.42 per hour) and the delivery of sustainable, good quality, regulated homecare services.
The minimum price has increased from last year (£23.20 per hour) due to a 9.7% increase in the National Living Wage from April 2023, and inflation in operating costs, including high fuel prices and rising rent, rates and utilities.

The Homecare Association believes care workers should be paid much more than the legal minimum to recognise the skill and responsibility of their roles and to improve retention and recruitment of staff. Also reported
are calculated fee rates required to enable payment of the Real Living Wage (£10.90 per hour), a wage equivalent to NHS Band 3 with 2+ years’ experience (£11.85 per hour), the London Living Wage (£11.95 per hour) and a competitive labour market wage rate (£13.64 per hour) of between £26.79 and £31.55 per hour. Many providers are already paying above the National Minimum Wage, some as high as £15-17 per hour, but this is only possible with hourly fee rates to match.
Homecare Association’s Chief Executive, Dr Jane Townson said, ‘Too many local authorities and the NHS continue to commission homecare at fee rates far below the true cost of delivering care. Persistently underestimating providers' costs risks diminishing the availability of services, the experience of the workforce, and providers' ability to comply with the legal requirements placed on them.'
12 CMM February 2023 NEWS
New learning network established

The Care Provider Alliance (CPA) and NHS England are convening a new learning network that will host a series of online sessions exploring emerging practice and innovative models of partnerships working.
The new arrangements for Integrated Care Systems offer a real opportunity to meaningfully include adult social care providers as key strategic partners.
To launch the network, a learning summit will be held on 26th January 2023, with a focus on developing strategic models of engagement with adult social care providers.
Speaking about the new network, CPA Chair, Nadra Ahmed said, ‘Social care providers can bring knowledge, insights and skills to the emerging integrated care systems – if they are engaged as genuinely strategic partners
–not simply as the providers of services under a contract. This new learning network will enable us to share ideas and experiences and to ensure that all care providers are included – from residential and home care, to supported living and communitybased services.
‘The Care Provider Alliance and NHS England plan to continue to work together to showcase emerging good practice and innovative models of partnership working.’
As this will be the first in a series of learning network sessions, the session will also consider topics for future, more focused, thematic sessions which may include: digital transformation and data sharing; workforce recruitment, retention and development; and developing and commissioning specialist services.
NCF and Skills for Care announce partnership

The National Care Forum (NCF) and Skills for Care have announced a partnership to host The Managers Conference 2023 to champion and support the crucial role of managers in adult social care.
Hosted by NCF and Skills for Care, and in collaboration with ARC England, the conference will bring together managers from across the country to share knowledge, ask questions and network with colleagues.
The conference will provide an opportunity to share, learn and find solutions and answers to the challenges managers face on a daily basis, and help them and their teams provide the highest quality care.
Professor Vic Rayner OBE, Chief Executive of the National Care Forum said, ‘Managers perform an incredible role within organisations –and with this in mind – we are very proud to provide a fantastic
conference jam-packed with development opportunities to enhance their expertise and provide them with opportunities to connect and learn from each other.’
Oonagh Smyth, Chief Executive of Skills for Care said, ‘We know that managers are busy and so we are focusing on opportunities for practical development and the importance of hearing from others, drawing on what we know through our close work with managers, employers, and stakeholders across the sector.’
The programme includes a mix of main plenary sessions and practical workshops, as well as panel discussions. Managers will have the opportunity to think about how to deliver great care, as well as ways to support and lead their staff, through workshops and discussions around topics including team working, being confident with difference, delivering outstanding care and recruitment.
A truly integrated system covering all your care needs, designed by care managers and professionals. Care and support records, audits and inspections, action plans and reports, policies and procedure, training and care certificate, rota and roster and eMAR (coming soon). When choosing a care management system , beeeeeee clever... ...CARE is what we do! 01424 400060 info@careis.net www.careis.net Intelligent, Intuitive, Cost Effective NEWS CMM February 2023 13


HR Enquiries Management Compliance Property Maintenance Microsoft Solution Partners for the Care Sector We focus only on the Care Sector and are specialists in SharePoint, MS Teams, Office 365, Outlook, InTune, Autopilot, PowerApps, Power Automate and all other things Microsoft. Get in touch to find out more by Visiting our website at www.CarePoint365.co.uk Emailing us at GetInTouch@CarePoint365.co.uk Call us on 020 4558 1503 Integrated modules available in Teams for Rostering Care Planning (coming soon) Time & Attendance
Leeds Building Society partners with Dementia UK
Dementia UK, the specialist dementia nurse charity, in partnership with Leeds Building Society, is launching free face-toface ‘Closer to Home’ clinics, to provide life-changing support to individuals and families living with dementia across the UK.
The clinics will be held in different Leeds Building Society branch locations over the coming months, bringing emotional and practical support to those impacted by dementia through the charity’s specialist dementia nurses, known as Admiral Nurses.
The national tour of face-to-face clinics will offer a safe, comfortable and private space for families, carers and friends to discuss any aspect of dementia and receive the specialist support of Admiral Nurses.
In April 2020, Dementia UK and Leeds Building Society announced
a four-year partnership to raise £500,000 to help over 2,500 families living with dementia across the UK. As part of this partnership, the innovative ‘Closer to Home’ project was also launched in June 2021, to improve access to dementia care and support.
Through fundraising by the Society, colleagues and members, the target of £500,000 has now been reached and because of it, the charity has been able to develop and deliver the project and enabled families to book a virtual appointment with a specialist dementia nurse. Between June 2021 and November 2022, over 3,200 families have been helped through ‘Closer to Home’ virtual clinics, held over the phone or video call. The face-to-face clinics will now allow more families to access the services.
Statistics on caring for people with disabilities
New statistics on the health and care of people with learning disabilities have been published by NHS Digital.
Information on key health issues of people with conditions, including autism, is among the new data being released in the Health and Care of People with Learning Disabilities, 2021 to 2022
The report summarises statistics relating to 56% of those patients in England who are recorded by their GP as having a learning disability and 0.5% of the patients included in this publication were recorded by their GP as having a learning disability in 2021-22.
Some of the key statistics included in the report were:
• The percentage of patients who had a learning disability and have been diagnosed with autism had a statistically significant increase each year from 21.4% in 2017-18 to 30.7% in 2021-22. The percentage
of patients without a learning disability who have a diagnosis of autism has increased by 0.3 percentage points to 0.9% over the same period.
• 71.8% of patients with a learning disability had a Learning Disability Health Check in 2021-22, a statistically significant increase from 58.8% in 2017-18. However, this is a statistically significant decrease of 3.4 percentage points from 75.2% in 2020-21.
• The percentage of patients with a learning disability who were prescribed antipsychotics decreased each year between 2017-18 (15.5%) and 2021-22 (14.5%), with a statistically significant decrease between 2017-18 and 2021-22. Patients without a learning disability who were prescribed antipsychotics has remained stable at 0.9% over the same period.
IN FOCUS
Unfair to Care report: 2022/23
WHAT’S THE STORY?
Community Integrated Care, in partnership with Korn Ferry, has published a new report, UNFAIR TO CARE: Understanding the social care 2022-23 pay gap and how to close it, which seeks to understand the social care pay gap and how to close it.
For decades, the social care sector has been calling for greater investment, fair pay and a coherent workforce strategy. In July 2021, Community Integrated Care sought to bolster the case for action by shifting the debate from one of moral subjectivity to objective fact.
WHAT WERE THE FINDINGS?
The 2022 edition of Unfair to Care reveals that social care support workers would need a 41% pay rise – equalling £8,036 – to have parity with their direct equivalents within the NHS, Band 3 Healthcare Assistants. It would take 23 years for current rates of uplift to deliver parity with the NHS. The report demonstrates that modern frontline social care requires complex technical and emotional skills, to effectively support people who commonly have complex medical and behavioural needs, proving that social care is significantly undervalued.
The financial gap between the NHS and social care workers opened by a further £590 this year – £8,036 this year compared to £7,447 in last year’s report. Report authors argue that it is likely this rise was driven by exceptional circumstances. Many providers are currently subsidising pay through their limited financial reserves.
WHAT DID THE EXPERTS SAY?
Rhidian Hughes, Chief Executive, Voluntary Organisations Disability Group said, ‘As we face a costof-living crisis – where domestic prices have more than doubled and food prices have increased by more than 13% – care workers cannot afford to be underpaid. Nor should they be. The chronic staffing shortages in social care will continue to escalate until the Government takes action to address the root cause of the problem – unfair and unequal pay.
‘We warmly welcome this report – the recommendations contained within it are right and they are achievable.’
Professor Vic Rayner OBE, Chief Executive of the National Care Forum said, ‘This is a really valuable report, building on the benchmarking work delivered last year by Community Integrated Care. It brings together insights from across the care and support sector which highlight, yet again, the level of skill needed to be a care and support worker and just how demanding it is to provide high-quality, person-centred care and support.
‘Unfair To Care also offers some very powerful stories from care and support workers, highlighting how difficult it is to remain in a job they love because of the current low levels of pay and the rising cost of living. The public perception research by Ipsos shows that the public believe in the importance of our social care workforce to society and all the evidence in this report shows the urgency of investing in that workforce now, addressing the current pay disparities and longer-term planning for the future of this essential workforce.’
CMM February 2023 15 NEWS
NEWS / IN FOCUS
New hiring toolkit aims to make recruitment safer
A first-of-its-kind Better Hiring Toolkit has launched, providing an essential guide for care sector employers to make safer, informed recruitment decisions.
It has been compiled as a collaboration between safeguarding experts at the Better Hiring Institute, the Disclosure and Barring Service, Reed Screening, Skills for Care, Dominic Headley & Associates and VBA Consulting.
With social care staff and volunteers providing support for some of the most vulnerable people in society, the toolkit is focused on the safety of the people employers are entrusted to care for and the staff who carry out their roles.
Among the key ambitions of the Better Hiring Toolkit are:
• A desire to raise standards in the care sector.
• To provide a one-stop shop for
industry best practice.
• Encourage an increase in sharing information – including Barring referrals.
Whilst sharing effective references and conduct information for staff working in social care settings has always been an essential part of safe and fair recruitment, many employers experience challenges in obtaining and providing them. Some employers refuse to complete references, others provide insufficient information and sometimes, appropriate ‘evidence of conduct’ is not provided – a legal requirement made by the Care Quality Commission.
Those responsible for recruitment within care sector organisations are being urged to download and share the toolkit within the hiring community: www. betterhiringinstitute.co.uk/industrybest-practice/health-social-care
Cost-of-living grants to support care workers

Florence has partnered with the Healthcare Workers' Foundation to support the charity in its mission to provide additional hardship grants to workers suffering financial hardship.
A recent study of over 1,000 nurses, health and social care workers, discovered that two thirds (63%) of nurses and healthcare workers are having to choose between food and fuel to combat rising energy bills. The findings, found that nearly one in five (14%) nurses have started using food banks since the cost-of-living crisis started, while a further third (30%) know colleagues who have.
Four in five (79%) of nurses and healthcare professionals say the rising cost of living is already negatively impacting their mental health. As a result, over half (51%) have had to take time off to recover from stress and burnout and over a third
(35%) say they’ve already seen a significant increase in mental health related staff absences.
A staggering 94% of nurses and healthcare staff are calling for the Government to match pay in-line with inflation, currently increasing at nearly its fastest rate in 40 years, driven largely by the rising cost of food and fossil fuels. But a pay rise might be too little too late, as over a quarter (28%) of nurses and healthcare staff are already planning to leave the profession in search of better pay, further adding to the chronic staffing crisis the NHS is experiencing.
Julie Child, Chief Executive at the Healthcare Workers’ Foundation said, ‘Our support initiative aims to lessen some of the possible financial hardships many members of the healthcare workforce may be facing. After all, everyone benefits from a good healthcare system.’
16 CMM February 2023 NEWS
York brain injury hospital to open in 2023
The construction of The Disabilities Trust’s new specialist brain injury facility at York’s historic Terry’s chocolate factory site, which started in February 2022, is due to be completed in Spring 2023.
Once completed, the steel framed and concrete structure, spanning 5,000m2 over two floors, will feature technology coupled with psychology-led, homely interior design, which will be
weaved throughout the hospital’s four wards and step-down flats, dedicated support and therapy areas and outdoor facilities, including a rooftop terrace.
This new hospital will provide high-quality neurobehavioural rehabilitation for adults with complex needs following a brain injury, helping individuals to take part in life fully and to help live independent lives wherever possible.
Knight Frank sells six care homes
Knight Frank has sold a portfolio of six care homes which were owned and operated by Morris Care Limited to Impact Healthcare REIT. The purchase price was £56m, which will partly be paid in cash and partly with an issue of Impact shares.
The portfolio comprises 438 high quality beds, of which 400 have en suite bathrooms, with five homes in Shropshire and one in Cheshire.

Morris Care enjoys a strong local reputation for delivering high acuity care and has established good working relationships with the local NHS Clinical Commissioning Groups. The vendors have granted a licence for the homes to continue to trade under the Morris Care brand for three years and the operational management team of Morris Care will transfer to Welford Healthcare,
Irene Sobowale, Chief Executive at The Disabilities Trust said, ‘This new hospital will be a flagship for innovation and will create a benchmark for several brain injury hospitals and rehabilitation centres in the UK that The Disabilities Trust is planning to open over the next few years helping people living with brain injury regain skills they have lost.’
The majority of the people
which will manage the homes, on 35-year lease terms.
Julian Evans, Head of Healthcare at Knight Frank, said, ‘We are pleased to have advised Morris Care on the sale of their best-in-class care home portfolio to Impact REIT. The transaction is a credit to the Morris family and all staff associated with the care business, in providing a firstclass service, which has been
the Trust supports are able to move on to live independently following their stay. However, a small number continue to require care and support following their rehabilitation. The Trust has, therefore, purchased another site just over a mile away from the new hospital. This site will be developed to create self-contained supported living flats for people with a brain injury, acting as a continuum from the new hospital.
created over the past 25 years. The business is now under the excellent management of Welford Healthcare.
‘Despite an uncertain political and economic climate, this transaction is yet another endorsement for the robustness of UK healthcare real estate.’
Knight Frank said record volumes of capital is being deployed into UK healthcare.
February 2023 17 NEWS
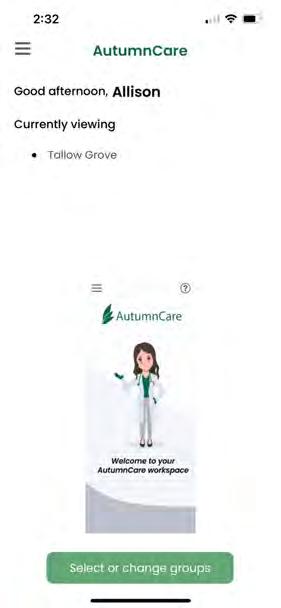
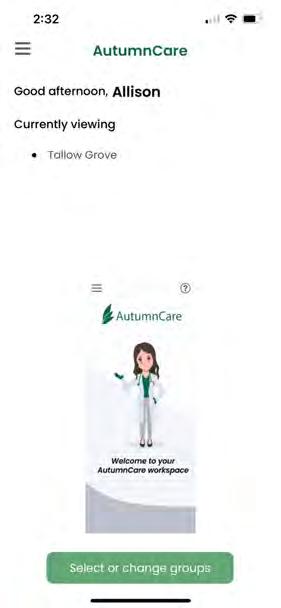
Now is the time to go digital uk.autumn.care info@autumn.care 0800 009 2121 10 key reasons care providers are choosing to go digital, what will yours be? 10 KEY REASONS BOOK A DEMO Book a demo to find out how AutumnCare can help
NEWS FROM ACROSS THE GLOBE
Swedish city receives accessibility award
The Swedish city of Skellefteå received the 2023 Access City Award in recognition of its longterm commitment and innovative approach to enhancing accessibility for persons with disabilities.
Accessibility is included in all Skellefteå’s plans, ensuring that public spaces such as playgrounds and streets are equipped with tactile information signs and ground heating, to ensure that snow and ice are not an impediment. The city’s central park and nearby river area have tactile paths and maps, seating and an outdoor elevator.
An SMS-service for blind and partially sighted persons provides information on road construction and potential obstacles across the city. Public buses are also fully accessible thanks to low floors, ramps, text screens and audio announcements. Skellefteå also offers training for young people with intellectual disabilities to explore technology and ways of working to help them lead an independent adult life.
The Access City Award was launched in 2010 and is one of the actions under the Strategy
for the rights of persons with disabilities 2021-2030 to build a union without barriers. It rewards European cities which have showcased best practices and illustrated efforts to ensure equal access to housing, public transport, information and communication technologies and other services for persons with disabilities and older citizens.
The Spanish city of Córdoba and Slovenia’s capital Ljubljana were awarded the second and third place prizes. Three other cities received a special mention
COVID-19 deaths in Australian aged care
The number of COVID-19 deaths in Australian residential aged care has again exceeded 100 a week, increasing to levels not seen in months.
Health department data shows 738 outbreaks are now active in residential aged care facilities, down from 915 outbreaks in the week to 23 December. There are 3,949 cases among residents and 1,661 staff cases associated with the current 738 outbreaks.
The total number of COVID-
19-related deaths reported by aged care providers during the pandemic has now risen to 4,612. That’s an increase of 120 reported deaths in the space of one week, the data shows. COVID-19 was the cause of 5.8% of all deaths in aged care facilities during this time.
However, Government data also shows that just 3.3% of COVID-19 cases in aged care resulted in death in 2022, far below the rate of 33% in 2020.
The Australian Government’s COVID-19 vaccination program is
delivering in-reach vaccine services for aged care residents and workers across Australia, through Commonwealth vaccine providers, primary care and self-vaccination services by aged care providers. The Government continues to provide all residential aged care facilities with access to COVID-19 vaccination clinics to ensure residents have every opportunity to get their fourth dose. As of 5th January 2023, there were 157,885 residents eligible for fourth doses.
Parkinson’s Foundation expands global network
The Parkinson's Foundation has announced the latest expansion of its Global Care Network with a new membership program for senior living communities and home care agencies – Community Partners in Parkinson's Care. The membership program prepares organisations to provide quality education and tools that equip staff to care for people with Parkinson's disease (PD).
Community Partners in Parkinson's Care provides a full
curriculum of PD education through virtual and in-person training. Utilising the train-the-trainer model, the membership program educates site champions at each location and provides the necessary tools to educate at least 70% of staff at their site. This program, formerly the Struthers Parkinson's Care Network, part of the Struthers Parkinson's Centre in Minnesota (a Parkinson's Foundation Centre of Excellence), has been continuously
expanding and now includes more than 100 member sites across North America.
Joan Gardner, RN, BSN, National Program Co-Director, alongside Rose Wichmann, PT, said, ‘The Community Partners in Parkinson’s Care membership program is comprised of senior living communities and home care agencies that have committed to improving care and providing support to people living with
for their efforts in becoming more accessible: Hamburg (Germany), for its built environment; Grenoble (France), for its transport network; and Mérida (Spain), for its information and communication technologies.
The awards were presented today by Vice-President for Values and Transparency, Věra Jourová and Commissioner for Equality, Helena Dalli, at the 2022 European Day of Persons with Disabilities Conference, organised by the European Commission together with the European Disability Forum.
In total 134,569 residents (85.2% of eligible residents) have received a fourth dose, noting more residents have become eligible following recent infection.
The Government delivered three-day PPE packs from the national medical stockpile to all aged care facilities ahead of summer and is providing outbreak PPE upon request. It is also providing in-reach COVID-19 pathology testing until 30th April for residential aged care homes experiencing an outbreak.
PD and their families. We are proud to include members of individual organisations as well as full corporate networks who are trained to prepare, empower and motivate staff with ongoing support from PD experts.’
Affecting an estimated one million Americans, Parkinson’s disease is the second-most common neurodegenerative disease after Alzheimer’s and is the 14th-leading cause of death in the U.S.
18 CMM February 2023 NEWS NEWS
NEWS








































•Available in 11 sizes, from 18mm-40mm (Ø) •Longer length – 130mm •Large buffer/comfort zone to prevent backflow and sheaths blowing off •Latex-FREE •Customise/remove excess length (scissors provided) •Perfect fit/size for all A bag for all seasons and occasions Short and strong. No more embarrassing leaks? •Specifically designed for wheelchair users •700ml and 1300ml sizes •Shaped to the contours of the bended knee •Available in 9 sizes, from 18mm-35mm (Ø) •Shorter length – 75mm •Stronger adhesive •Buffer/comfort zone to prevent backflow and sheaths blowing off •Latex-FREE Bendi Bags •Traditionally shaped leg bag •600ml and 1000ml sizes •7cm shorter in length than many 750ml bags – no unsightly taps dangling Comfort Bags •Ideal for sun, sports and even some short clothing •500ml capacity •Dress as YOU want, not to cover the leg bag Discreet Bags • Large • Customise/remove 11 sizes • Available • Buffer/comfort 9 sizes Urology products that make a difference Unique features and benefits often designed with input from end users. Available on prescription FREE HOME DELIVERY SERVICE Providing a personal service from a professional team. For your FREE information pack contact 0800 999 5596 or email prescriptions@manfredsauercare.co.uk For more information, please contact the helpline on: 01604 595 696 quoting CMM/F helpline@manfred-sauer.co.uk Or visit: www.manfred-sauer.co.uk

As the New Year bells fall silent, the work of 2023 begins in earnest. The turmoil and challenge of 2022 makes it likely that most of those working in care will not be starting the year refreshed and recharged; more likely they will be peeking over the horizon with trepidation about what the next 12 months may bring. Fair assessment? Or grounds for optimism? Let’s take a look at the year ahead and see what it is likely to bring.
Winter pressures
The notion of winter pressures is something with which all those working in care will be familiar. The ‘surprising’ arrival of winter often brings a flurry of roundtables and engagement with care providers that begins in October and ends in November and which can be frustrating to all parties. Nothing systemic is resolved and, once the headlines are exhausted, the attention gets shifted on, and people get forgotten. Members tell us repeatedly about the things that would really make a difference; they are most definitely not rocket science, and of course involve having people at the heart of all decision making.
Integration – the journey continues
This year we will be having discussions about all things health and care integration in earnest with the new bodies in town, the Integrated Care Systems (ICSs). 2023 will mark their first full year in operation. We know that the proper engagement of care providers has been patchy at best, and frustrating and unproductive at its worst. This has to be one of our positive objectives for the year ahead. There’s an increasing number of voices advocating for proper social care involvement at the top table, and we will continue to push for this. With this in mind, all eyes will be on the forthcoming investigation into ICSs commissioned by the Chancellor and being enacted by Patricia Hewitt, and the Health and Social Care Select Committee report on accountability following its inquiry.
Regulation
The world of regulation was expecting a seismic change in early 2023. However, right at the end of 2022 it became

CMM February 2023 21
>
2023 is officially upon us, and we’re all wondering what the year ahead will bring. Here, Vic Rayner of National Care Forum (NCF) outlines the key factors she believes will influence care providers in the coming 12 months.
clear that the date for instigation of this regulatory shake up has been delayed. The Health and Care Act of 2022 brought new powers to the Care Quality Commission (CQC) to enable it to take a more system wide view as a regulator and, with that, bringing a need to regulate both local authorities and ICSs to look at their role in ensuring good health and care for the communities they serve.
This runs alongside the introduction of a Single Assessment Framework for all services that CQC regulates. The implementation of this appears to have been more challenging than anticipated, and the latest pronouncement only specifies that it will appear later in the year.
At a time when there are calls for more and more decisions to be made at a local level, and huge pressures on all parts of the system, a delay in understanding how this is really working in practice seems unhelpful for those who are already experiencing a system that does not meet their needs. It is hoped that a proper explanation of the reasons behind the delay and clarification on when the reforms will be implemented will be forthcoming early in 2023.
COVID-19 Inquiry
As we move forward in the year, we are expecting the COVID-19 Inquiry to take centre stage. There are only three modules that have been outlined in detail, and they cover preparedness, engagement and the health service.
The way in which the Inquiry has been structured means that it is likely that there will be a social care perspective in each and every one of the modules. However, there will also be a dedicated module for social care which we anticipate hearing more detail on early in the New Year. The way in which this is scoped and shaped will determine how much the other vital areas – such as vaccination, PPE, community health and the rights of people receiving care and support – are wrapped up in this one module or need to be spread throughout.
Workforce
It is likely that the workforce challenges of 2022 remain, and are in many cases amplified in the year ahead. The very compelling Unfair to Care report from Community Integrated Care at the end of 2022 laid out in no uncertain terms just what needs to be done to ensure
that care workers receive parity of pay with comparative jobs in the health service.
As many other colleagues in public services enter into periods of industrial action, the focus on the importance of pay to reward people’s contributions to communities should not exclude that of care staff. We know that there is to be a significant increase in National Living Wage in April of this year, but it remains a stain on our sector that this minimum level of payment remains the majority pay level for front line care staff. Local authorities received funding at the end of 2022 that was to support workforce recruitment and retention, and it is hoped that care workers are directly benefiting from this £200m additional funding, however, it is frustrating that it is once again short-term and rushed. The Care Workers’ Charity continues to report increasing calls on its funds and the ongoing cost of living crisis is putting pressure on colleagues in every part of our sector.
Escalating costs
Rising costs are impacting on all elements of care delivery. This includes the costs of fuel to deliver homecare, energy prices within care and support settings, food costs, uniforms, trips out and of course salaries and meeting terms and conditions. Alongside that, many organisations are facing huge concerns about the rising costs of borrowing.
The double whammy of massive care inflation – where everything in the basket is rising exponentially – alongside the increased cost of loans will make the beginning of the year a truly uncomfortable period for many. It is imperative that there is full recognition of this in the local government fees that will be being communicated in the first few months of 2023.
The draft local government settlement was put out for consultation on 19th December, and it details the additional funding put forward for adults’, and children’s, social care as well as the overall uplift. Government frames the overall uplift, which is the total allocation from central government to local authorities, as a 9% uplift intended to cover the inflationary costs inherent in their delivery of services. Clearly a core and growing proportion of their overall spend is on social care, so it certainly should be expected that this uplift is reflected in fee rates for the year ahead. However, this also recognises the very significant increases that are likely to face self-funders of care, and this is of course against the poorly communicated
backdrop of the postponement of the introduction of the social care cap and adjustment to the means test. Providers are likely to find themselves having to manage some complex communications as they move between navigating fee rates with authorities, and understanding the implication for self-funders in order to ensure sustainable services for the year ahead.
Innovation
In light of the many problems facing those delivering and receiving care, it is fair to say that finding a positive note can be a challenge. However, innovation remains both an opportunity and a necessity if we are to find a way to deliver the care that people want, at the time that they need it.
The Care Innovation Hub provides a great showcase to bring together people who want to make change happen. Colleagues from Think Local Act Personal were at the heart of the last challenge, and it made a huge difference to all the teams, but it was of particular note that the mentoring and support offered by a colleague with lived experience transformed the ideas of the winning team. People receiving care and support, and the workforce, have to be at the heart of all future innovations in the sector, whether digital, environmental or in models of delivery. We ignore their voices at our peril.
International opportunities to learn
Learning from across the world has to be an important strategy for us all in 2023. The growing focus on international recruitment across the care sector shows us that the delivery of care is very much a global enterprise. The NCF has teamed up with Scottish Care to co-host the Global Ageing Network in Glasgow in 2023. This will bring speakers and experts from all around the world to the UK to share their knowledge, and of course to learn from what works in the UK.
In a time when everything we talk about seems to be predicated by terms like ‘challenging’, ‘difficult’ and ‘worst ever’, it is vital to open our eyes and ears to hear about the art of the possible.
Whilst the year ahead feels heavy, it is ever more important to see ourselves as part of a global ecosystem that is evolving at pace around the world. We should take strength from that, as social care matters to us all. CMM
Join the discussions on forecasts for 2023 and share your feedback on the article. Visit www.caremanagementmatters.co.uk
22 CMM February 2023
Professor Vic Rayner OBE is Chief Executive of National Care Forum. Email: vic.rayner@nationalcareforum.org.uk Twitter: @vicrayner
NAVIGATING 2023: THE JOURNEY CONTINUES >




























LOVE LAUNDRY We understand how important laundry equipment is to your care or nursing home. Our goal? To make it simple. Made for you Bespoke laundry and finance options to suit you. Safe and sound Helping you create an infection-free environment. Count on us Professional, approachable and at your service. 08000 546 546 WASHCO.CO.UK



learn to love your admin. within reason, obviously. Our software makes running a care home easier, more efficient, and more profitable. It lets your staff get more done, with less effort. Request a demo today, commitment free, hassle free, at @ coolcare.co.uk
PREPARING FOR THE NEW CQC FRAMEWORK:
WAYS PROVIDERS CAN PLAN AHEAD
With a new framework expected for Care Quality Commission (CQC) inspections, providers need to know what is changing. Here, Helen Fuller, Director at Care 4 Quality, sets out what the new Framework will bring and how you can prepare.
The Care Quality Commission (CQC) announced a new strategy which will bring all health and social care providers under one single framework to provide more consistency across services. This new regime is currently being piloted with a small number of providers and a subsequent rollout across the board is expected in Autumn 2023.
As such, care providers will be expected to implement certain
changes in the context of CQC’s four new areas of focus, as outlined in its publication, A new strategy for the changing world of health and social care:
• People and communities: Regulation that’s driven by people’s needs and experiences, focusing on what’s important to people and communities when they access, use and move between services.
• Smarter regulation: Smarter, more dynamic and flexible regulation that provides up-to-date and high-quality information and ratings, easier ways of working with CQC and a more proportionate response.
• Safety through learning: Regulating for stronger safety cultures across health and care, prioritising learning and improvement and collaborating to value everyone’s perspectives. >
CMM February 2023 25
• We at Promised Care can assure you that we are amongst the few agencies, if not the only agency, that provides comprehensive training to our staff, tailored according to Skills for Care standards and CQC minimum standards required for safe care to any vulnerable person.

• It is good practice for our staff to have a brief induction from the home manager or senior staff on the first day of their shifts. This includes fire exits and safety locations in the event of emergency and brief background information on each resident’s care plan.
• Our staff are suitably trained to provide safe care to residents. This includes using effective communication, encouraging residents to eat and drink to promote hydration and good body weight and documenting fluid and food intake and output. Our staff will report in good time to relevant people, any changes observed in the care of the residents they work with, as they assist in their personal care activities. Our staff will also engage residents in mind-stimulating activities in the home. As former care managers we understand the plight of care home managers, and the challenges of managing day-to-day care activities when you have staff shortages.
• Our management team includes dedicated trainers with previous care experience, and professional qualifications in nursing, social work and training. We provide staff with theoretical learning and hands-on training, on how they are expected to provide care to residents in any structured care environment, such as: Nursing Homes, Home Care, Residential Care Homes, Day Care Centres and Supported Living, including people with Mental Health Conditions.
Our health care assistants would have the option to work with service users,
their own homes to:
who require home care support in

Older people in need of help. Sensory impairment. Mental health. Palliative care. Physical disability. Respite care, 24-hour live-in care. Supported living. Bedside support on admission in hospital until you are discharged home. Overseas accompaniment to visit relatives, friends, or exotic places.
Please visit our website for more information.
Web: www.promisedcare.co.uk Tel: 0208 842 3329 Mobile: 07792 448150, 07969 013855 Email: info@promisedcare.co.uk leanonmecc@protonmail.com
David J. Cheesman RMN, Social Worker & Training Manager
Nobel Baxter
Public Health, MBA & RGN - Service Coordinator CREATING A BETTER TOMORROW OUR SERVICES ARE AVAILABLE 24 HOURS A DAY, 7 DAYS A WEEK, 365 DAYS A YEAR. Why should you choose Promised Care agency staff to cover shifts in your care home? WE ALSO PROVIDE PRIVATE HOME CARE SERVICES (CQC
9)
Mr
Mr
BSc
REGULATED ACTIVITIES
Promised Care Ltd specialises in recruiting, training and supplying vetted health care assistants to work in various nursing homes, residential care homes and supported living environments for people with learning disabilities, physical disabilities and people with mental health conditions.
• Accelerating improvement: Enabling health and care services and local systems to access support to help improve the quality of care where it’s needed most.
Running through each theme are two core ambitions:
• Assessing local systems: Providing independent assurance to the public of the quality of care in their area.
• Tackling inequalities in health and care: Pushing for equality of access, experiences and outcomes from health and social care services.
For many care providers, the CQC regulations are the linchpin for how they operate their services – following these regulations ensures that highquality, safe and compassionate care is being provided at all times. Here’s what you need to know to ensure your care service is prepared.
Why is CQC launching a new strategy?
In essence, the new strategy is designed to simplify and refine the oversight of risk that is happening within care services.
health and care services across England have joined forces, regionally, to create integrated care systems (ICS). This is to help ensure that information is interoperable and to help improve the lives of people who work and live in the area.
It’s not surprising that CQC has taken a similar approach, with a focus on assessing local systems and also refining its framework to a single source, rather than having lots of different variations. Here’s what the regulator is planning to focus on and 13 ways you can prepare.
The format of inspections
The current timetable of on-site inspections will be replaced by frequent monitoring and engagement calls to assess risk. These are known as Direct Monitoring Activity (DMA) calls.
These phone calls are based on a set of questions with a focus around the key lines of enquiry (KLOEs). Questions will be asked around:
• The continued relevance of the registered service user bands, checking that the service is providing the regulated activity appropriately.
• Mental Capacity Act (MCA), consent, best interests and Liberty Protection Safeguards.
• Risk management and safeguarding people.
• Care planning.
• Safe staffing.
• Medication.
• Infection control.
• Activities and lifestyle choices.
• Stakeholder feedback.
• Governance and provider oversight.
Inspectors will also ask servicespecific questions around any other intelligence that they have received from third parties, such as the local authority.
replaced by a single framework, which will be used across all providers from initial registration application. The aim is to simplify the process and provide a coherent and joined-up service history.
The key questions will remain, but the KLOEs will be replaced by ‘I’ statements. This will help the regulation to be driven by people’s needs and their experiences of the health and care service.
These ‘I’ statements will be underpinned by ‘We’ statements. These statements outline the expectations of how providers are meeting the ‘I’ statements. They are quality indicators and there will be between four and 10 ‘We’ statements beneath each ‘I’ statement.
Evidence will then be reviewed under one of six categories (more information on evidence categories below) to ascertain if the quality statements are being met.
Ratings
There will be no change to the current rating categories; however, there is the possibility of CQC having the ability to change a service’s rating without an on-site inspection, based on the findings and information gathered during a remote monitoring call.
Partnerships
There will be increased focus on information gathering from care providers’ partners and stakeholders and you may be asked for contact details of relatives and staff as part of the remote monitoring process.
Evidence categories
The COVID-19 pandemic highlighted that the existing CQC strategy wasn’t really fit for purpose, in that care providers were reactive to risk assessments, rather than identifying risk in services as they were happening and having the capacity to encounter and handle the risk.
In addition, in the past 12 months,
CQC will inform you of the outcomes of the call. If your service is identified as ‘very high risk’, you will receive further engagement calls and can also expect on-site inspection activity.
Key lines of enquiry
The current service frameworks will be
The evidence categories recently went to consultation, and it is proposed that each service type will be asked to provide a list of evidence under each of the five key questions and topics (Safe, Effective, Caring, Responsive and Well-led).
Evidence will fall under one of six categories:
1. People’s experiences.
2. Feedback from staff and leaders.
3. Feedback from partner organisations and stakeholders.
4. Observations.
5. Processes.
CMM February 2023 27 PREPARING FOR THE NEW CQC FRAMEWORK: 13 WAYS PROVIDERS CAN PLAN AHEAD
>
“The existing CQC strategy wasn’t really fit for purpose, in that care providers were reactive to risk assessments, rather than identifying risk in services as they were happening.”
> 6. Outcomes.
The quality of the evidence will be reviewed by inspectors with an assessment made under the following:
• Independence.
• Compassion and dignity.
• Partnership working.
• Promoting healthier lives.
• Improving outcomes.
• Rights and equality of staff.
• Equality and access to care provision.
• Environmental sustainability.
• Governance and leadership.
• Best practice and innovation.
A score will be made against each of the six evidence categories, which will then be calculated and will determine a rating for the care service.
What can providers do to prepare?
Here are 13 things we recommend all care providers do ahead of time:
1. Work with your care team and staff. Share information about the strategy with them as it becomes available. Add it as an item to your team meeting agendas, share the CQC resources with them, and make quality and compliance a cultural value in your care facility.
2. Join CQC’s Citizen Lab. This gives you the opportunity to have early access to what CQC is thinking, as well as share your opinion on the upcoming changes.
3. Keep your CQC presentation/
Personal Information Record up to date. This will save you time in the long run as it will be requested!
4. Look at the DMA questions for care providers. Start to gather evidence and write your answers before the call.
5. Keep a record of innovation and creativity within your care service. Make sure you can evidence the impact on people and the wider facility.
6. Reach out to other services. Are you part of leadership forums and healthcare groups in your area? Networking and sharing information and best practices helps to drive innovation and improvement across services.
7. Make sure your audits are up to date and clearly reflect any changes made/actions taken in response to audit findings.
8. Survey people who use your service, including friends, family and visiting professionals – how do you utilise this feedback?
9. Treat external stakeholders and the local authority in the same way as you do the CQC – they will be asked for feedback.
10 Ensure your evidence is well organised. Think about the new evidence categories and how you will present this to CQC.
11. Consider implementing a compliance software system. Electronic systems and processes can save a significant amount of time.
12. Involve people who use your service and their families as much as possible in your service’s
development. Consider asking people who use services to join interview panels.
13. Remember, CQC is looking at how care providers work together within systems to help achieve shared care goals, so:
• Increase your understanding and awareness of the care system you belong to.
• Identify local healthcare themes and trends.
• Consider the pressure points in secondary care – is there any way you can support with this?
• Look out for any initiatives in your area with which you could join forces to support the ongoing national aims of reduction in health inequalities, reducing hospital admissions due to Urinary Tract Infection, and early detection of pressure damage which could lead to tissue breakdown.
Positive outcomes
It is still difficult to ascertain the actual impact the new framework will have on managers and providers directly. The increased monitoring and contact activity will help to forge better relationships between the regulator and some providers, which will be a positive outcome. Also, the new model of inspection and monitoring will certainly demonstrate a stronger partnership with local authorities and external bodies and may well prove to be much more responsive to the risk level for each service. CMM
What has been your reaction to the strategy and what questions do you have for the regulator? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
28 CMM February 2023 PREPARING FOR THE NEW CQC FRAMEWORK: 13 WAYS PROVIDERS CAN PLAN AHEAD
Helen Fuller is Director at Care 4 Quality Ltd. Email: helen@care4quality.co.uk Twitter: @Care4Q









THE CARE HOME BROKERAGE PROFESSIONALS Due to huge demand, we urgently require care homes throughout the country, contact our Managing Director Nick Greaves in confidence on 07943 107 887 or nick@ngacare.co.uk Holbrook Hall Derbyshire The Chestnuts South East Kibworth Knoll Leicestershire LD Portfolio Midlands Hazelford Care Home East Midlands The Leys Home Counties LD Portfolio Midlands Woodheyes Leicestershire 36 bedrooms Residential care home Converted & extended Kingsthorpe View Midlands
Into Perspective
HOW
EMPLOYERS CREATE A MULTIGENERATIONAL SOCIAL CARE WORKFORCE?
with 8% of respondents saying they have been discriminated against on the grounds of their age, what can employers do to address the imbalance and create a multigenerational workforce?
Something for everyone
UK-wide consultancy, TPP Recruitment understands that in order to create an inclusive, multi-generational workplace, it is important to understand the needs of each generation and how they will differ from one another. The King’s Fund writes that, increasingly, flexible working is seen by staff as a critical factor in how attractive an employer is. With stress and burnout and a desire for improved work-life balance as key factors in staff leaving or reducing hours as reported by the Nuffield Trust, increased flexibility can be a significant incentive for people to remain working in health and care, says flexible working consultancy Timewise.
financial incentives, but that physically demanding frontline care work may not appeal to this demographic. Instead, social care employers looking to attract returnees could review their provision of support roles as a means of creating a multigenerational workforce.
Government’s role
In a survey forming part of the 2020 Deloitte Global Human Capital Trends report, only 6% of respondents strongly agreed that their leaders were equipped to lead a multigenerational workforce effectively. In addition, contributing to its vision of what should be in a workforce strategy for a growing social care sector, the Local Government Association
states that the ‘entire social care workforce must strive for equality of outcomes, focusing on freedom, independence, safeguarding, prevention and on good advice, so that we are able to support good lives, and give dignity and respect’. Given that a recent survey conducted by the ADP Research Institute found that ageism is the most common form of perceived discrimination in the workplace,
Government’s action plan for adult social care, published at the height of the COVID-19 pandemic, called upon former sector professionals to return and provide additional support at a time of great public need. While COVID-19 rates have declined, the cost of living has risen and among those aged 50-70 who have left work since the pandemic, 52% were more likely to have increased worries around finances according to the Office for National Statistics. John Forth, a Senior Lecturer in Human Resource Management at Bayes Business School, suggests that recruitment welcomes an opportunity for ex-sector professionals to return due to
The House of Commons Health and Social Care Committee’s Workforce: recruitment, training and retention in health and social care report calls upon Government to research and publish health and social care workforce projections covering the next 20 years. In the committee’s view, these should include current staffing levels, future staff projections and an assessment of whether sufficient numbers are being trained in each profession, specialty and sub-specialty. With access to this information, social care employers could be better placed to assess how a multigenerational workforce could be utilised most effectively based on emerging skill gaps. Greater transparency from Government can only help employers to fulfil the increasing need for a diverse multigenerational workforce.
Moreover, the committee's report urges Government to pass recruitment and retention funds directly to providers to be invested in local recruitment campaigns, arguing that local providers are best suited to understand recruitment challenges in their local areas. The job-seeking demographic will differ regionally, and social care employers should receive financial backing to lead multigenerational recruitment in their respective areas.
30 CMM February 2023
CAN
Skills for Care estimates that if the number of adult social care posts grows proportionally to the projected number of people aged 65 and over in the population between 2021 and 2035, an increase of 27% (480,000 extra posts) would be required by 2035. The sector must act fast to meet this demand, tapping into the potential of a multigenerational workforce.
The sector cannot afford to overlook older workers
Dr Emily Andrews, Deputy Director of Work, Centre for Ageing Better @emilyishness

The job market is changing, and employers are facing huge challenges in overcoming skills and labour shortages. With an ageing population and more people working later in life, older workers are key to filling these gaps. That’s good news: older workers are good for productivity, and multigenerational teams are the best for innovation. With up to 500,000 more care staff needed by the middle of the next decade, the sector cannot afford to overlook the benefits of this large and underused talent pool.
Yet in a recent Ageing Better commissioned survey, 45% of UK adults aged 50 and over indicated that they feel employers view them more negatively than younger applicants. Too many older workers are frozen out of the job market due to age bias in recruitment processes. There are more than one million older workers currently unemployed or inactive but who would like to work. Finding ways for them to return to work will help sectors under strain, such as the care sector, as well as adding billions to the country’s economy.
Steps can be taken to attract more older workers into the social care workforce. Employers can develop age-friendly recruitment practices by debiasing job adverts, including a diversity statement
emphasising age-inclusivity and circulating vacancies widely across multiple platforms.
ONS research into 50–70-yearolds who left the labour market during the COVID-19 pandemic and were considering a return to work found that flexible working hours was the most important factor in choosing a new job. For many older workers, it is not just a preference but essential for balancing work with caring responsibilities or health conditions. The social care sector is well-placed to deliver this flexibility.
Providing carers leave, occupational health support and skills training for employees of all ages is also essential to building a multigenerational workforce.
Social care providers keen to address urgent labour shortages and maximise the potential of older workers should sign our Age-friendly Employer Pledge. The initiative requires employers to commit to one action a year to improve the recruitment, retention and development of older workers, identify a senior sponsor for age-inclusion and ensure that age is specifically named within their equality, diversion and inclusion policies.
There is lots of good practice already in the social care sector – and pledged employers can showcase what they do well.
Opportunities should be available to everybody at any stage of life
Phil Pegler, Managing Director, Bluebird Care @bluebirdcare


At Bluebird Care we believe that anyone can offer support and comfort to people if they have the right values, regardless of their age. We pride ourselves on our intergenerational workforce –with our passionate, caring team members ranging from ages 18 to into their 70s.
While there is (rightly) a sectorwide focus on introducing younger people to a career in care, we also appreciate that people can join care from any background and with any life experience.
Our Bluebird Care Merton office recently ran a recruitment campaign for over 55-year-olds, based on our organisational-wide value that fulfilling, exciting, challenging and rewarding opportunities should be available to everybody at any stage of life. In the social care sector, working with older people, we understand that more than most, and so it is up to us to carry that message and actively set about being generationally inclusive in all we do.
Digital technology reaps huge benefits for the social care workforce in terms of information sharing and collating, management, recruitment and planning. However, we must not fall into the trap of relying only on digital communication. We
make it a priority that everything is accessible, understandable and engaging for our workforce – including those who may not be as familiar with digital technology, who we support with ongoing training and development in this area.
Creation of flexible working programmes is also key to nurturing an intergenerational workforce. As employers we can easily offer accommodating contracts that fit around an individual’s life and preferences. From those just embarking on their careers, to more experienced professionals looking to re-enter the working world and give back to the community, flexible arrangements can empower people of all ages to forge their career in social care.
Amidst serious workforce pressures, providers cannot afford to be anything other than fully inclusive and open minded when it comes to recruitment. But, beyond that, adapting recruitment and operational processes to build an intergenerational workforce can foster a sense of mentorship, knowledge-sharing and a more dynamic workplace. These are all crucial tenets of a rewarding environment for those carrying the responsibility and privilege of providing care.
31
• Governance documents • Audit Tools • Dependency Tool • Clinical Policies & Procedures • FREE Downloads • Risk Assessment Templates • PRN Protocols E-Document Shop Now OPEN!







32 CMM February 2023 UK As experienced Care Home practitioners we provide
embed
care
Developing a culture of care with
positive
in a 6 x 1hr per week online training programme. Develop how to address loneliness,
and
companionship, partnerships and meaningful quality of life. An inspiring care model enhancing retention & wellbeing Contact us today and join the care evolution Call today on 01626 868192 • 07483 359471 or visit www.eden-alternative.co.uk Insurance you can trust, made simple. Call for a free quote today or visit www.phoenixsrs.co.uk 01273 977221 Phoenix Specialist Risk Solutions Ltd are authorised by the Financial Conduct Authority – FRN: 809579, as an Appointed Representative of Exchequer Risk Management Ltd – FRN – 616500 Life & Critical Illness Care Home Insurance Commercial Insurance Business Protection We understand
the
of the care industry can be unpredictable. We want to make
you’re covered in the face of any risk. Our industry experience means we
risks you
us today to discover
we
protected. Phoenix Specialist Risk Solutions, O ce 1, The Design Quarter, 129-130 Edward Street, Brighton, East Sussex, BN2 0JL
training to teams in sustainable innovation and leadership, to
companionship, partnership working and wellbeing designed to build enriched quality of life into
homes.
wellbeing,
relationships and inclusion at its heart,
helplessness
boredom with
that
nature
sure
know what types of
face, so speak to
how
can keep your business
THE TIPPING POINT:
Understanding the funding gaps in adult social care
The Government announced a sweep of funding measures in 2022– but what’s the breakdown of the figures? And what are the next steps for the Fair Cost of Care exercise? Richard Ayres, Social Care Advisor to Care England, delves into the detail.

The Chancellor’s Autumn Statement was underwhelming for adult social care (ASC) providers and its self-funded residents. We heard how the planned reforms to level-up funding between those who fund their own care and those funded by their local authority, will be delayed for two years. The lifetime cap on care would have seen no individual pay more than £86,000 towards their care costs and the enhanced means test was set to increase from £23,250 to £100,000 along with Section 18(3) of the Care Act. This would permit those funding their own care to request that their local authority arranges care to meet eligible needs, in the same way as those who are supported by the means test. However, plans have stalled.
Funding breakdown
The Chancellor has said that the funding for these reforms will be used to help fund social care and announced:
• £2.8bn in 2023/24 made up of £1.8bn provided by way of a Social Care Grant (split adults and children). £1bn to adult social care split: £600m for hospital discharges and £400m ringfenced for ASC.
• £4.7bn in 2024/25 made up of £3bn provisioned by way of a Social Care Grant (split
between adults and children).
£1.7bn to adult social care: £1bn for hospital discharges and £700m ringfenced ASC.
Part of the funding is to be raised by increases of up to 2% for Council Tax, which some councils will be reluctant to do given local elections and the lead into a general election. Councils have also said that children’s social
care is also in need of funding and expects 50% of the Social Care Grant to be afforded to them accordingly.
The ASC sector will see an increase of 92p per hour in the National Living Wage from April 2023, a welcome rise of 9.7% for our care workers. The Chancellor shared that the Office for Budget Responsibility (OBR) forecast for inflation in 2023 is 7.4%. This will
collectively require councils to pay over 9% to providers in fee uplifts just to stand still, which totals around £2bn for the sector.
This prompts us to question the Chancellor’s Autumn Statement award because ASC is likely to see less than the £2bn necessary to fund inflation and demographic change alone, before addressing the hospital discharge challenge.
CMM February 2023 33 >
Any shortfall will need to be funded from efficiencies by councils who will no doubt look to ASC to contribute.
Hospital discharge funding
In respect of the hospital discharge challenge, we know that the £500m for 2022-23 pertaining to hospital discharges is split £300m to ICBs to improve bed capacity and £200m is given to local authorities to bolster the social care workforce. In its November 2022 press release, relating to the £500m for 2022-23, the Department of Health and Social Care (DHSC) said, that 'Local areas will be free to spend this money on initiatives which will have the greatest impact in their area on reducing discharges into social care, which in most areas will mean prioritising home care' and in the same press release, the Minister of State for Care, Helen Whatley, said, 'People should be cared for in the best place for them' thus not ruling out care homes as a destination. A further £200m fund to support ICBs was then announced on the 13th January 2023 titled ‘Discharge funding for step down care’, which is aimed at freeing up hospital beds up to the 31st March 2023 and states that this funding should be used to purchase 'bedded step-down capacity, plus associated clinical support for patients with no criteria to reside but who cannot be discharged with the capacity available through existing funding routes or the ASC £500m Discharge Fund announced previously.' Detailed plans for the 2023-24 £600m and 2024-15 £1bn discharge funding are yet to be announced.
Data remains critical
The DHSC awarded £162m to councils in 2022 to move toward the Fair Cost of Care (FCoC). Thousands of care homes contributed to the FCoC exercise in the summer of 2022. Whilst councils are not obligated to share their findings from this exercise until February and their Market Sustainability Plans in March 2023, a small number have been open and shared their findings with care providers already.
Care England acknowledges and supports providers who have written to local authorities asking for this information to be shared in advance of February and March 2023. Care England has also requested data by way of Freedom of Information Requests aimed at helping providers to understand critical information. It is hoped that this data would help providers plan for winter, as costs increase
significantly beyond the levels of inflation paid by councils in 2022. Providers can use this data to consider changes to their business models, including the number of underfunded local authority residents they are able to offer care to.
The FCoC data is critical for care providers to understand the gap between the current rates paid by councils and the FCoC – it’s what the remaining reforms targeted and what funded councils seek to move toward. Councils were due to receive a further £600m in 2023-24 and again in 2024-25. However, the Chancellor has now removed this committed funding from the table and leaves just £162m for the two years to help councils move toward the FCoC. Some councils have sought to pay one-off funding to care providers, thus not increasing fees to move closer toward the actual FCoC. Councils argue that the funding is not recurrent despite the DHSC stating to the contrary.
Your voice matters
Care England encourages care providers to request engagement between now and February/March 2023 to help councils understand the workforce challenges locally and financial pressures on providers. It will also help to reach a more common understanding of the data from the FCoC exercise. Councils are under Care Act obligations to consider the data they have access to and to determine the sustainability of the local market. This is not a once-a-year obligation but an ongoing requirement. Although it is acknowledged that insufficient funding has been awarded to councils in recent years to pay the FCoC, the DHSC has been clear that care providers need to initially work with their local authorities if they experience financial hardship. It is not yet clear what the DHSC is going to do with the information it also holds in respect of the FCoC.
Clearly, additional funding is necessary to avoid widespread collapse of the sector. This is despite repeated narrative from DHSC citing that £7bn has been injected into social care over the next two years. After considering the risk of Council Tax not being increased nationally to the full 2%, the pressures on older people, child and learning disability provision, workforce pressures driven by over 165,000 vacancies and 30%+ attrition levels, on top of rising agency costs, hospital discharge requirements and the Chancellor's comment citing 200,000 more individual care packages – there is simply not enough funding to combat inflation at its current and predicted levels as well.
A new year reality
Looking forward to this new year ahead of us –what can social care providers expect? I asked Professor Martin Green OBE, Chief Executive of Care England, to offer his analysis. He said, ‘Pretty dismal if nothing changes would be the most accurate summary. Councils require around £2bn next year just to stand still for ASC, based on the announced 2023 National Living Wage (NLW) uplift and the Office for Budget Responsibility (OBR) inflation forecast. The Chancellor has offered £2.8bn, which we know around £900m will go to child social care and £600m will go toward hospital discharges. We also know that councils are not all likely to increase Council Tax by the full amount, which leaves no more than £1.3bn to address inflation and demography, over £700m short of what is needed on top of the remaining unfunded gap left in 2022. This gap saw council fee uplifts based on September 2021 forecasts for inflation of sub 4%, which were a far cry from the 11.1% we saw in November 2022.’
Martin Green OBE concludes, ‘The Local Government Financial Settlement falls short of addressing inflation for 2023 and as such, ASC will again start 2023 in a deficit position on already fragile foundations closer to its tipping point that any other time in history due to the cost of living crisis, energy uncertainty and a strained workforce, working on fumes, covering over 165,000 vacancies, up 52% in 2022, whilst the economy is seeing a 38 year low in unemployment, leaving little by way of positivity for 2023 and the challenges ahead for adult social care providers.’
On the point about the energy uncertainty – to keep 2023 renewal costs sustainable, accessing the best possible advice will again be key and to maximise energy supplier interest and ensure offers are keenly priced whilst minimising excessive risk premiums. Care England intends to offer care providers the opportunity to combine energy volumes, to maximise significant economies of scale, and is issuing an exclusive Care England tender for 2023-24 Gas and Electricity renewals and is looking to launch further opportunities for care providers to reduce operational costs during what we know to be challenging months ahead. I urge all providers to stay united, share best practice and keep up to date with support packages and opportunities to engage in the coming months. In the meantime, I’ll be closely watching what this Government does next and await the significant support this sector so desperately needs. CMM
34 CMM February 2023 THE TIPPING POINT: UNDERSTANDING THE FUNDING GAPS IN ADULT SOCIAL CARE
How have you reacted to the Government’s announcements and what is your feedback on the analysis shared? Visit www.caremanagementmatters.co.uk
>
Richard Ayres, Social Care Advisor to Care England. Email: rayres@careengland.org.uk Twitter: @CareEngland
Caring for the Care sector.


We have listened to senior care professionals’ experiences of the impact of Covid-19 on their sector. Read insights and recommended approaches to tackle current challenges and build a stronger future for care homes.
The Future of Care

0343 777 3187 mielecarehome.co.uk @mieleProf Miele Professional
Download your copy here
laundry
dishwashing
Miele offer reliable, high quality
and
solutions to provide long term support and protection to staff and residents.
Covid-19 and beyond: challenges impacting & influencing residential care The pandemic has changed the care industry for the foreseeable future. Challenges that care home professionals have struggled with for years have become increasingly difficult whilst other issues have been given more attention, resulting in tighter measures to better protect staff and residents. This report explores some of the key issues experienced by care home professionals during the pandemic and how these are shaping the future. Open

Shifting mindset:
Why you need to think differently about staff wellbeing

The social care sector has demonstrated some excellent wellbeing initiatives but how does an organisation ensure wellbeing projects become a permanent part of the company ethos? Sophie Coulthard, Principal Consultant at Judgement Index, shares how providers can develop a robust wellbeing plan that puts staff at the heart of its delivery.
Wellbeing has moved up the agenda in recent years, which has been largely driven by employees who are seeking a better work/ life balance and challenging the companies they work for to prioritise staff wellbeing. Care companies face a different and, possibly, bigger challenge. Outside of a corporate setting where yoga classes, flexible working and meditation apps might be the norm, we must consider how the care sector can embrace a culture of wellbeing that supports staff with as much emphasis as it places on its clients.
It starts with a subtle shift in mindset –that staff wellbeing should be as important as the wellbeing of people in care. After all, as Richard Branson said, ‘If you look after your staff – they’ll look after your customers.’ It sounds simple but taking meaningful action to support staff wellbeing takes time, patience and some creativity.
Understanding needs
If you’re embarking on a wellbeing journey with your team, then don’t announce an
initiative without understanding what the individual needs are first. Too many companies launch wellbeing projects that have no connection to the real wellbeing needs of its employees and therefore wellbeing is often seen by the workforce as ‘fluffy’ and lacking substance.
Start with an anonymised survey, asking for detailed feedback on what would improve wellbeing. Focus on key areas of wellbeing such as financial, physical, emotional and social. Ask questions in a way that will give you valuable data and not just stats, such as:
• Do you have a particular financial concern around heating, food, buying school uniforms etc?
• Does your work cause you any physical discomfort such as bad back, sore feet etc?
• Do you ever feel anxious about coming to work? If so, why?
• What areas do you feel underconfident about in work?
• Were you part of any social clubs or have hobbies growing up?
• If you could spend a day off work doing things that fulfil you, what would you do? >
CMM February 2023 37
These questions might seem strange; but could draw out patterns in staff wellbeing, such as a common financial concern. While you may not be able to directly support, you will have a clearer picture of the things weighing on your employees’ minds and may be able to provide educational resources or access external support.
Use these questions during supervisions to go deeper with individuals. By asking about where they might feel underconfident and anxious at work, it can help you to identify training needs and understand who might benefit from a mentor or buddy at work.
The questions around social wellbeing and understanding past hobbies can help you identify how to build community at work, either through social clubs or pairing team members with clients who have similar interests.
When you’ve finished gathering the results of the survey, find a way to present it back to your team. This is an important step to keeping them involved and informed, after all, the information is about them. Present the key findings in a meeting and write up some notes for a notice board or newsletter. Make three or four suggestions for next steps and ask for ideas from your team. It’s also worth keeping copies for your CQC evidence folder.
People first
The next step is to put together a plan that can be mapped over a year but broken down into quarters and months. This will ensure that wellbeing stays as a priority and doesn’t ‘drop off’ after the initial buzz and momentum dies down. This will also mean that wellbeing gets sewn through the culture of the company, rather than being a one-off initiative that doesn’t materialise into real, tangible results.
Our research has found three common wellbeing areas that often require development for care staff. They are:
• Self-esteem.
• Self-criticism.
• Personal stress.
I’m prepared to say that building confidence and increasing self-esteem should be the number one priority of any care company when it comes to wellbeing.
By placing an emphasis on this, you will build a team of self-leaders who are comfortable in themselves and their ability to make decisions and this can reduce the
pressure on management, freeing them up to focus on more strategic areas of the business. Self-esteem is about how people feel about themselves and how they value themselves. This can be a challenge in a sector that is often portrayed negatively by the media and where there is so much compliance and awareness around what’s a risk, unsafe, or wrong. Of course, compliance is essential for safety, but it does mean a lot of focus within care is on the negative instead of the positive.
How can you increase positivity in your team and build self-esteem? On a collective basis, start by introducing some positive markers. Encourage the team to share their successes, including what went well that day, what someone else did that was great and what they did that was great. Promote the use of phrases such as ‘well done’ and ‘thank you’. Simple words that we don’t use enough. Every morning, remind staff to say ‘great job’ to someone else that day. It sounds cheesy but it's a foundational building block to increasing positivity. It's important that ALL staff are given the recognition, regardless of role or number of hours worked. A greater level of self-esteem amongst the whole team will undoubtedly aid retention.
Use any one-to-one time with staff to highlight their natural strengths and talents as you see them. They may be highly capable but underconfident in their abilities. Use a coaching style of leadership to encourage them to find solutions for themselves, ask open questions and resist the temptation to provide the answer. By doing this, you’ll build confidence in individuals and learn who you can empower more and who needs more attention and support.
This approach of seeking feedback and new ideas, encouraging appreciation and recognition within the team, coaching individuals and building trust and empathy, aligns with human-centred leadership. This is a leadership ethos that puts people first and can create a work environment where people and their wellbeing can flourish.
Building trust
It’s not possible to promote wellbeing within a company without also shining a spotlight on the culture and leadership. An environment without a good, people-focused leader will not foster a positive culture and, in turn, the wellbeing of individuals will likely
be affected.
Wellbeing can very much be driven by the leader. It also helps to have a structure and plan to carry it through the year. Start by reviewing what you already do that might support wellbeing and make a note of anything that can be instantly added to your wellbeing plan.
Next, think about how you can incorporate wellbeing support into your one-to-one meetings. Being aware of whether someone is going through a difficult time and/or feeling low might mean you can make adjustments for them to make work easier during that time. It can also help prevent mistakes or compliance issues, which often happen when someone is under a lot of stress.
One of our clients offers its staff an off-record personal risk assessment. Any time a member of staff feels they are struggling with their mental health, they are able to talk it through with the manager, completely confidentially and the notes are not kept in their personal file. This has helped to build trust between the team and management and has had a positive impact on absence rates and compliance within the home.
For the wider team, having a library of personal development resources can be a great way to launch a culture of wellbeing. This can include books, podcasts and even YouTube videos and Ted Talks, which could be shared at the start of a week with a prompt for discussion at the end of the week. This opens the conversation about wellbeing with the team, creates buy-in and makes it an ongoing topic. Why not also create Wellbeing Champion roles to carry the initiative forward and collate resources on reducing self-criticism, developing resilience and coping with stress.
Planning for success
Ultimately, wellbeing is not always linear. A member of staff might go through a difficult time and struggle to cope regardless of how many wellbeing initiatives you have in place. What’s important, is that you have built a culture where staff feel safe to share their struggles without judgement and can feel valued and understood by their employer.
If you can adopt a human-centred approach when building your wellbeing plan, by consulting and involving the team as much as possible and always considering both the collective and the individual, then this is the best chance of success. CMM
Does your organisation use any other the methods outlined in this article? How have you embedded wellbeing into your company culture? Visit www.caremanagementmatters.co.uk and share your feedback on the article.
38 CMM February 2023
Sophie Coulthard is a Principal Consultant at Judgement Index. Email: sophie@judgementindex.co.uk Twitter: @judgementindex
SHIFTING MINDSET: WHY YOU NEED TO THINK DIFFERENTLY ABOUT STAFF WELLBEING >
Care England 2023 Conference & Exhibition
Thursday 16 March 2023






Church House Conference Centre, Westminster, London Don’t miss out! Book
Exhibition and seminars: Learn from the specialists
Engage with 40 leading product and service suppliers in the exhibition and choose from 12 seminars in the afternoon session. Find out more about their contribution to the successful delivery of quality care.
First speakers confirmed!


The first speakers have now been lined up to present at the Care England Conference & Exhibition, ‘Thriving Not Just Surviving’.

Visit the Care England website for up to date information.
Supporting care services to go digital
Trusted by over 2,800 care services across a wide variety of care types
Customisable and easy to use

Integrates with eMAR, pain management apps, falls prevention apps, GP Connect and more
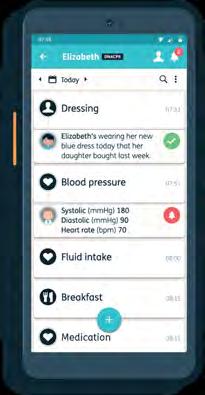
Proud to be an Assured Supplier for the NHS Transformation Directorate Digital Social Care Records DPS


"Nourish was a game changer for our company."

Sarah Beaumont, Associated Wellbeing

CMM February 2023 39
www.nourishcare.co.uk 023 8000 2288 caring@nourishcare.co.uk Your Digital Social Care Records Platform
To find out how we can help you access NHSE Digital Funding, contact us to book a free personalised demo today
your place now!
RESOURCE FINDER: Technology
The care sector continues to benefit from the latest technological innovations. This Resource Finder gives you information on some of the sector’s leading providers, to help you enhance your digital offering and stay ahead.
Access Health, Support and Care
Tel: 0845 345 3300 • Email: HSC.Access@TheAccessgroup.com Website: www.theaccessgroup.com/en-gb/health-social-care/ care-management-software
SECTORS
• Residential care homes.
• Nursing homes.
• Domiciliary care.
• Supported living.
• Hospices.
• Local authorities.
SERVICES
• Care management software.
• Scheduling and rostering.
• Medication management.
• Care compliance.
• Policies and procedures.
• Learning for care.
COMPANY INFORMATION
With over 30 years of experience, our portfolio of integrated solutions empowers care professionals across small, medium and large services to focus on the individual and deliver high quality care.
Our ecosystem of care management software is the most widely used in the UK and addresses all aspects of care supervision, from its commissioning through to its delivery.
Its interconnected and comprehensive nature enables the delivery of safe and efficient care, with the person placed firmly at the centre. Hear more about our solutions:

Care Planning: An all-in-one care planning and management solution, enabling you to deliver high quality, safe and personalised care more efficiently.
Scheduling and rostering: Manage your care delivery, rota software for care homes, home care rostering, scheduling for care workers, payroll preparation, or HR management and more.
Medication management: An eMAR system that enables you to deliver the right medication at the right time. Record administration accurately and get alerts when medication is missed.
Care compliance: The only complete governance tool in care, helping you to monitor governance, regulatory compliance, care audits and clinical compliance across your business.
Learning for care: Endorsed by Skills for Care, our eLearning software makes your training more manageable, engaging and cost effective.
Policies and procedures: This platform allows you to easily manage all your health and social care policies, procedures, documents and forms in one place.
Ready for a personal tour of our products? Have a chat with our care team today and find out how our solutions can benefit you.
40 CMM February 2023
AutumnCare
Tel: 0800 009 2121
Email: info@autumn.care

Website: uk.autumn.care
SECTORS
• Residential care homes.
• Nursing homes.
• Supported living.
• Hospices.
• Domiciliary/Homecare.
SERVICES
• Digital care planning.
• eMAR.
• AutumnCare mobile.
• Family app.
COMPANY INFORMATION
AutumnCare is a digital care planning and medication management (eMAR) solution designed for all care providers enabling the migration to a digital system and providing the foundations for outstanding care.
AutumnCare caters to all your care planning, medication management and family communication needs whilst eliminating manual processes and double entry of data, drastically reducing the administrative burden on care staff.
AutumnCare care planning
Our comprehensive digital care planning software provides each care recipient with a comprehensive person-centred care plan providing full oversight to the care worker, the care provider, the family and most importantly the care recipient.
Within the care planning software, you will have access to a comprehensive library of care charts, forms and assessments that can be tailored to each organisation’s specific requirements.
AutumnCare mobile
Mobile is a point-of-care digital
care app. Designed to replicate a carer’s workflow, the app facilitates more thorough, accurate record-keeping on the go, without detracting from faceto-face time with care recipients.

Medicate (eMAR)
AutumnCare Medicate promotes safer and more efficient medication management whilst reinforcing the six Rs of administration. Fully integrated with AutumnCare Care Planning, all data flows seamlessly between systems to provide prompts and alerts relating to medication management.

Medicate manages the whole medication administration process from the safe delivery of medication through to the automation of stock control. This helps to ensure that the correct medication is available and administered to the right person at the right time.
Family app
AutumnCare Family is an app designed to enhance family engagement. Care providers can communicate directly with family members, keeping them connected wherever they may be.
The app features a a secure two-way messaging system that ensures family members are kept abreast of all care and leisure activities of their loved ones.
Book a demo today to discover how AutumnCare can benefit your care provision now and in the future.
CarePlanner Ltd

Tel: 0117 214 0125
Email: enquiries@care-planner.co.uk Website: www.care-planner.co.uk
SECTORS
• Homecare.
• Recruitment agencies.
PRODUCT
• Rostering and scheduling.
• Invoices and timesheets.
• Call administration.
• Record keeping.
• Reports.
• Application Programming Interface (API).
• Local authority interconnector.
COMPANY INFORMATION
Social care is changing. The policy push is towards joinedup services and systems and if you want to be at the forefront of this new approach, you will need innovative software that facilitates these new digital connections without losing sight of the personal connections that will always define social care.
CarePlanner customers often save days of administration time each week as well as simplifying tasks and tracking for care workers. With appointments scheduled and tracked through one system, invoices and payroll can be automatically produced with far greater accuracy and less manual involvement. Our internationally recognised customer experience and innovations enable agencies to achieve more with less,
improving accuracy and quality of the care given.
User experience is paramount at CarePlanner. Our system is intuitive and customisable, empowering providers to develop their service over time and digitise at their pace. Our system can be shaped to meet the requirements of your service, whether you are looking to change to a system that better understands and meets the needs of your service, or you are just starting out.
This is because we match our technology with our support teams to ensure our users get everything they need from CarePlanner. Our personal connections shape both our service and our software and the sincerity and understanding of our approach are why we won gold at the International Customer Experience Awards 2022.
Through communication and understanding we align with users on the future direction of both your service and our system and how we can best grow together.
So why not book a demo and find out why 500 new customers joined us last year alone?

CMM February 2023 41 RESOURCE FINDER: TECHNOLOGY
CarePoint 365

Tel: 0204 558 1503
Email: getintouch@CarePoint365.co.uk
Website: www.CarePoint365.co.uk
SECTORS
• Care homes.
• Homecare.
• Assisted/supported Living.
• Mental health support.
• Learning disabilities.
SERVICES
• Rostering software in Microsoft Teams.
• Leave and availability management.
• Time and attendance software.
• HR software for employee management.
• CRM enquiries management software.

• Property maintenance software.
• Virtual reality solutions.
• Office365 solutions.
COMPANY INFORMATION
Using the right technology solution for your care service will improve efficiency, save costs and improve staff worklife balance. However, many systems are expensive and overly complicated.

CarePoint365 provides an easy-to-use solution within Microsoft Teams and can be used as a single application for almost every aspect of your care service. This means that

users will be able to access the solution through one familiar interface. CarePoint365 further leverages common features of Office365 such as Outlook Calendar, Outlook Email, Tasks, Alerts, PowerBI and Workflow so that the end user can carry out all their administrative and reporting tasks within Office365. Users will not need to login to different solutions.
Rostering and HR: Manage rotas, staff leave requests, timesheets and payroll data along with onboarding and termination of staff.
CRM: Track enquiries, marketing and service user fees. Integrate with pre-assessments for client onboarding.
Property Maintenance: Track workorders and contractor progress and spend, planned preventative maintenance and risk assessments.
MED
e-care Healthcare Solutions
Tel: 0161 232 4575 • Email: info@mede-care.co.uk Website: www.mede-care.co.uk

SECTORS
• Residential care homes.
• Nursing homes.
• Dementia care homes.
• Supported living/retirement care villages.
SERVICES
• eMAR.
• Care plans.
• Integrates with pharmacy providers and other care technology providers.
COMPANY INFORMATION
MED e-care gives you the data you need to make the best decisions for those in your care. We are proud to be working with care providers such as HC-One, Prime Life and Care UK to ensure joined up care, single entry of data and first-class medication management.
MED e-care’s eMAR and Care Plans support you with:
• Complete management of the resident care lifecycle.
• Reducing risk.
• Operational effectiveness.
• Increased staff productivity.
• Increased staff morale.
• Driving quality improvement.
• Meeting CQC/regulatory requirements.
Our GDPR compliant software combines to create a seamless, flexible, electronic health record that can easily be adjusted to reflect the needs of your
residents, carers, nurses and organisation.
Don’t just take our word for it, see what our customers have to say.
Steve Hamlet, Operations Manager, Sandstone Care Group said, ‘This is a revelation! It ensures we always have medication and it’s always booked in to be administered to the resident. The whole medication process is quicker and safer now. We did not have any stress and nothing went wrong. I’ve had no complaints from staff (and they would definitely flag it if it was a nightmare) – so that speaks for itself.’
James Park, Operations, Kingdom Homes said, ‘Initially the team were nervous about a completely remote implementation of a new care technology. We knew we owed it to our residents and care staff to try as the positives of using eMAR speak for themselves. We are extremely happy with the training, implementation and the eMAR technology.’
Visit our YouTube page to have a look at our eMAR demo video or we can book you in with a live demo – whichever you’d prefer.
42 CMM February 2023 RESOURCE FINDER: TECHNOLOGY
Person Centered Software
Planday Limited
Tel: 020 3630 1574
Email: marketing@planday.com
Tel: 01483 357657
• Email: hello@personcentredsoftware.com Website: www.personcentredsoftware.com

SECTORS
• Residential care homes.
• Nursing homes.
• Dementia care homes.
• Supported living/retirement care villages.
• Mental health support.
• Learning disabilities.
• Local authorities.
• Domiciliary care.
SERVICES
• Digital care planning system.
• Fully mobile and icon driven.
• Clinical handheld device.
• Effective handover and staff messaging.
• Built-in speech to text.
• Accidents and incidents.
• Observations and charts.
• Fluid and nutrition monitoring.
• API integration and reporting.

• Electronic medicines management integration.
• Body map/wound care.
• Electronic activities evidence.
• Relatives gateway.
• Group reporting.
• GDPR-compliant recordkeeping.
• ATLAS eMAR.
• Digital reception.
• Nursecall messaging service.
• Joined up care.
• Maintenance and asset management.
• DSCR funding.
COMPANY INFORMATION
Person Centred Software provides one of the most widely used digital care planning systems within social care, used by over 3,500 care homes. This is the first fully mobile and easy to use system providing care staff with icon-driven software to record over 50 care notes per resident per day, something which can't be done on paper or
indeed with many other systems.
Person Centred Software also provides a range of other products around digitalising care, such as ATLAS eMAR, a Digital Reception and a Nursecall Messaging Service.
Reduce time spent on paperwork, give staff more time to spend with residents, get support with regulatory compliance and improve the quality of care for residents.
Tara Cross, Registered Care Manager at Mulberry house said, ‘I like how the Digital Care System relies heavily on icons; it makes it perfect for our carers where English is not their first language. Writing care notes can often be challenging, but with Person Centred Software's icon buttons, information is now recorded quickly and easily.
‘The Digital Care System has so many other features, like the body map, where you can track the progress of a wound or infection and the oral care feature, which enables staff to evidence how they support residents to maintain good oral health. The fluid and nutrition monitoring features help the team keep track of what fluid and food has been provided and consumed in the last 24 hours. I could be here all day if I mentioned all the features!’
Website: www.planday.com/uk

SECTORS
• Care homes.
• Nursing homes.
• Retirement homes.
• Hospices.
• Care home management.
• Residential care.
• Administration.
• Staff scheduling.
PRODUCT
• Shift planner.
• Mobile app.


• Punch clock.
• Reporting.
• Staff communication.
• Staff management.
• Payroll.
• Point-of-sale.
• Human resources.
• Integrations.
COMPANY INFORMATION
Planday from Xero is a workforce management tool with more than 350,000 employee users across Europe and the UK. Our goal is to help save our customers time and money by reducing manual staff management and admin tasks.
Less admin, more freedom to do great work. Empower your people to thrive with time-tracking, scheduling and communication – all connected in one place, accessible from anywhere. We help reduce the complexity of managing your business by integrating with your payroll and PoS system and allow you to easily manage your staff from anywhere with easy access on the mobile app or desktop. Whether you're an employee or employer, Planday makes your day work. Please click here or scan the QR code below to book a demo.
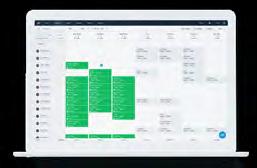
CMM February 2023 43 RESOURCE FINDER: TECHNOLOGY
Qwikify
Tel: 0800 689 3596
Email: info@qwikify.com Website: www.qwikify.com

SECTORS
• Care homes.
• Homecare.
• NHS.
PRODUCTS
• Digital care records/electronic care planning.
• Policies and procedures.
• Document automation.
• Consultancy/bespoke digital product development.
COMPANY INFORMATION
Qwikify instantly generates documents on demand helping organisations automate time consuming paper processes. Easy to use workflows allow users to automatically generate, update and review documents in seconds from smart templates.
A powerful template builder allows users to create completely custom solutions.
Qwikify provides automated solutions for digital care records/electronic care plans, policies and procedures, audits, assessments, quality assurance, health and safety or any other type of document or record.


Qwikify’s unique features are its speed and customisation:
• Speed – users can generate documents in seconds. For example, care homes users can create a full set of person centred care plans in under 15 minutes, a process which typically takes several hours by paper or traditional care planning systems.
• Customisation – users can create their own custom solutions using the powerful Qwikify template builder.
Unique IQ
Tel: 0800 888 6868
Email: sales@uniqueiq.co.uk Website: www.uniqueiq.co.uk

SECTORS
• Homecare SERVICES
• Rostering system.
• Electronic call monitoring.
• eMAR.
• Digital care planning
• Mobile app
COMPANY INFORMATION
As care has grown more complex, so has the way you do things. It’s time to bring it all together.
IQ:caremanager is Unique IQ’s next generation software designed specifically for home care providers. Built upon our award-winning existing software systems which our care customers know and love, IQ:caremanager brings together the tools you need to plan, deliver, monitor and manage homecare.

Plan – organise your care provision.
Care managers and supervisors can process referrals, manage care packages and quickly schedule carers to cover visits.
• Scheduling and rostering.
• Client/carer best matching.
• Client records.
• Care planning.
Deliver – empower your people to provide high quality care. While out at a visit, carers can use our mobile app to clock in and out of visits, record notes and access the information they
need about the people they are caring for.
• eMAR.
• Mobile app.
• Clock in/clock out.
• Client and family portal.
Monitor – get a better understanding of your organisation’s care provision Our real-time monitoring technology helps care managers stay on top of the day’s visits.
• Dashboards.
• Report builder.
• Alerts and reminders.
• Live status and GPS.
Manage – oversee your people and processes.
Our software comes with a suite of HR and finance tools to help manage a team of carers.
• Carer records.
• Incident handling.
• Invoicing and payroll.
• Mini-CRM.
We’ve been working with homecare providers for more than 15 years. So IQ:caremanager has been built using all of that experience, knowledge and passion for the care sector. It’s not about software. It’s about care.
44 CMM February 2023 RESOURCE FINDER: TECHNOLOGY
The Care Workers' Charity

The Care Workers’ Charity is calling upon UK businesses working in the adult social care sector to collectively raise £2.5 million every year for care workers by donating £500 annually or £50 monthly on a recurring donation basis to support our work – equivalent to supporting one care worker through our support programmes. Your support will enable our charity to keep our programmes open to care workers across the UK, providing essential hardship funds, mental health support and training, raising awareness and advocacy.

CELEBRATING EXCELLENCE 2023 FINALISTS ANNOUNCED
Markel 3rd Sector Care Awards
CMM is delighted to announce the Markel 3rd Sector Care Awards finalists for 2023 and we hear from some of the judges to find out what really stood out for them on judging day.
Over the last eight years, the Awards have grown and become a highly respected fixture on the care sector events calendar. CMM is looking forward to welcoming everyone at The Grand Hotel in Birmingham on 3rd March 2023, where the ceremony finale will take place.

The Awards shine a spotlight on so many worthy individuals and organisations that improve the lives of people with tremendous challenges up and down the country. The entries demonstrate the diversity and capability of organisations in the not-forprofit sector, all of which do so much good.
Professor Vic Rayner OBE, Chief Executive of The National Care Forum, spoke of ‘the art of possible’ on page 21, and this really resonates with the ethos and the extraordinary feats of our Awards finalists.

As Vic comments, ‘In a time when everything we talk about seems to be predicated by terms like “challenging”, “difficult” and “worst ever”, it is vital to open our eyes and ears to hear about the art of the possible.’ This is exactly why the awards are so important – the strength and passion and unwavering dedication that is within so many working in this sector is what the Awards truly champion.
The Awards judging day is a highlight of the year for Team CMM and offers judges
and sponsors the opportunity to step inside the lives of those working in the 3rd sector and hear the raw and honest accounts of their experiences. Our judging panel included experts from Choice Support and the Royal Hospital Chelsea (RHC). Thank you to all judges who joined us on Friday 2nd December to meet the finalists virtually and to hear about their incredible achievements.
An incredibly important event
Ruth Horton, Quality and Safeguarding Manager and Mental Capacity Act Lead at Choice Support, was invited to judge at this year’s Awards. Reflecting on her first judging experience, Ruth said, ‘It was fantastic to have the opportunity to meet each of the finalists and listen to their stories and see the passion they held for their roles. I learnt through these conversations about different areas of the care sector, such as dementia support, and how people find ways to make sure others’ needs are met.’
Just like so many of the other judges, Ruth held onto some memorable moments from the interviews. Ruth continues, ‘There were many stand-out comments made by the finalists, but one in particular really summarised the importance of why we need events such as these. The judges asked, “What
46 CMM February 2023
would success look like?” The finalist replied, “I want to get to the point where the charity doesn’t exist anymore.” Being a judge for the Awards has been a pleasure to take part in and I welcome the opportunity to do it again next year (please).’
Judge Joanne Bosanquet, Chief Executive of the Foundation of Nursing Studies, thoroughly enjoys the judging experience. Joanne told finalists that the day is ‘a highlight of her entire year’ and she continues to be astounded and moved by every Awards entry.
Claire Henry MBE, Visiting Researcher Palliative and End of Life Care Study Group, University of Cambridge, has been a judge for many years. Commenting on her 2022 judging experience, Claire told CMM, ‘It is a privilege to hear about all the amazing people working in the sector and how they are making a difference to people’s lives. What stood out to me from the finalists was their passion, drive and not taking no for an answer. A memorable quote from the day for me was, “It’s the little things that make the biggest difference to people”.’
Judges were impressed by the infectious positivity of the finalists, their enthusiasm and their strong links to the community. Finalists displayed such a high level of dedication and judges applauded the way organisations were filling gaps in the sector by implementing lifesaving and people-first innovations. Leadership and empowerment were also key themes from the judging, along with a relentless approach to make change happen.
CMM would like to thank all of our sponsors and partners for their continued support. The 3rd Sector Care Awards is a wonderful opportunity for our sponsors to meet the people behind projects of excellence and we look forward to everyone coming together in March.
Our 2023 finalists
The Markel 3rd Sector Care Awards 2022 finalists are:
Dementia
Care
• Emma Kiss, Activities Co-ordinator, Outlook Care.
• Badger Wing Team, Foxburrow Grange.
• Wilshaw House Day Centre Team.
End of Life Care
• The End of Life Partnership.
• St Helena Hospice.
• Jariena Patel, Making Space.
Making a Difference
• Karolina Gerlich, Chief Executive, The Care Workers’ Charity.
• Mette Le Jakobsen, Surrey Choices.
• Nicholas Kee Mew, Trustee of Age UK Enfield and Woodford and Wanstead Charity.
Compassion
• Andrew Noblett, Support Worker, Making Space.
• Anne Marie Coulter, Activities Co-ordinator, Swarthmore Residential Care Home.
• Jorawar Singh Rathour, Founder, London Homeless Welfare Team.
Leadership
• Margaret Kerry, Trustee, Prospects Trust.
• Salli Jeynes, Chief Executive Officer, End of Life Partnership.
• Keren Wilkinson, Chief Executive, Amica Care Trust.
Book your tickets
Development and Innovation
• No Barriers Here Team, Mary Stevens Hospice.
• Anxiety UK.
• Pay What You Can Afford, Therapy Links UK.
Creative Arts
• Community Integrated Care and Open Eye Gallery.
• Skaped.
• Robert Lamacraft, St Martin’s.
Community
Engagement
• Woodhall Community Centre.
• Love Community CIC.
• The Princes Centre.
Campaigning for Change
• P0hwer, My Dignity, My Rights.
• The Care Workers’ Charity.
• Navigating Menopause, Trekstock.
Technology
• Chasing the Stigma.
• Community Integrated Care and Okta, Digital Inclusion Partnership.
• Ngage NE Ltd, Leadership Team.
Collaboration (Integration)
• Jewish Care Social Work and Community Support Team.

• The Shrewsbury Ark, Staff and Volunteers.
• Community Integrated Care’s Inclusive Volunteering Programme, with Sport England, Rugby League World Cup 2021, UEFA Women’s Euro 2022, World Gymnastics Championships, Super League and RFL.
Markel UK will once again be the headline sponsor of the Markel 3rd Sector Care Awards. Join us as we welcome our winners in a face-to-face lunchtime ceremony at The Grand Hotel, Birmingham on 3rd March 2023.
Book your tickets by following the link below.. Please also talk to us about sponsorship, another fantastic way to be a part of the celebrations. You can take a look at last year’s winners and finalists to see what truly makes the Markel 3rd Sector Care Awards such a remarkable event or watch the Virtual Awards Ceremony here
To stay up to date with the Awards, don’t forget to follow us on Twitter: @3rdSectorCare #3rdSectorCareAwards
Visit www.caremanagementmatters.co.uk/event/markel-3rd-sector-care-awards-2023
CMM February 2023 47
Headline Sponsor
The A.R.T.S. for Brain Health webinar series has gathered leaders in dementia prevention, innovative creative ageing and Social Prescribing to debate the role of arts and wellbeing in protecting against cognitive decline, including the onset of dementia symptoms. This webinar, in partnership with the Global Social Prescribing Alliance and the final in the series, was hosted by Veronica Franklin Gould, President at Arts 4 Dementia and chaired by Michael Dooley, Treasurer at the College of Medicine.
Global Social Prescribing
Dr Bogdan Chiva Giurca, Development Lead and Hamaad Khan, Development Officer at the Global Social Prescribing Alliance presented Social Prescribing advances from around the world and shared success stories from the alliance’s student champion scheme, in which arts and medical students interact with Arts for Brain Health participants. One participant, Ron Bennett, spoke extensively about his lived experience of participating in Drama for All at Southwark Playhouse after approaching his GP with mental health concerns.
Introducing Ron, Hamaad explained, ‘Ron was an Arts 4 Dementia participant; and I can say from my personal experience then as a neuroscience graduate, I was able to see neurodegeneration beyond its physical symptoms that we talk about, and social prescribing as a treatment or as a coping
mechanism to help increase wellbeing and wellness in individuals with something that wasn't afforded to me in my university education. So, I can speak from personal experience to say how transformative it is, because we all know that health exists beyond the membrane of our biology.’
Social prescription pathway
Sian Brand, Co-Chair of the Social Prescribing Network oversaw presentations on social prescription pathways from Australia, Singapore and Portugal. Professor Kheng Hock Lee, Director and Deputy Chief Executive Officer, Education and Community Partnerships at SingHealth Community Hospitals shared details of Singapore’s artfocused approach to social prescribing, ‘Largely with the help of art therapists, that was seconded to us from our National Arts Council, we were convinced of the importance of art activity in the sense that it can be an extension of reminiscence therapy. It allows our patients to express their emotions and explore meaning, and it helps them to communicate to their peers as well as to the health care workers; and it improves their self-esteem and confidence. They enjoy it, they feel relaxed, and it's a way for them to engage and socialise.’
Arts on prescription pathway
Alexandra Coulter, Director of the National
Centre for Creative Health, led arts on prescription pathway presentations from Italy, Austria and Canada. Sonia Hsiung, Director at the Canadian Institute for Social Prescribing (CISP) summarised the challenges Canada faces in its efforts to co-ordinate Social Prescribing nationally, ‘I think you get the picture here that while we have very strong momentum, all of our initiatives are regional. They are time-limited by funding and ad hoc. So, unlike the UK, we don't have a system-wide investment into this type of practice anywhere. This also means that engagement with arts and cultural organisations, and the pathways to connect people to arts-based interventions, are highly dependent on the region, on the specific project funding, and on organisational specific initiatives.’
Funding sustainable arts prescription programmes
Closing the conference, Tim Anfilogoff, Head of Community Resilience at Hertfordshire and West Essex Integrated Care Board, introduced the final debate on funding sustainable arts prescription programmes, with Mags Patten of Arts Council England, Chris Easton of NHS Charities Together and Joshua Ryan, the National Academy for Social Prescribing’s Thriving Communities Lead.
To watch the Global Social Prescribing Arts for Brain Health Conference back in full, or read the transcript, visit the Arts for Brain Health website.
EVENT REVIEW
6th December 2022 GLOBAL SOCIAL PRESCRIBING ARTS FOR BRAIN HEALTH CONFERENCE Look out for announcements about CMM Insight events happening in 2023 @CMM_Magazine #CMMInsight www.caremanagementmatters.co.uk 48 CMM February 2023
EXPERTS IN CARE TRAINING

Edify Training gives you 100% training compliance, which significantly reduces staff turnover. Imagine Sunday evening facing your week ahead, with a full team and 100% ready for any inspection of training records. That sounds like a peaceful night’s sleep.
WHAT’S ON?
Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact: Event: Date/Location: Contact:
The Future of Social Care Technology 8th February 2023, online www.digitalsocialcare.co.uk/events/the-future-ofsocial-care-technology-artificial-intelligence
Take a virtual tour of the Adult Social Care Workforce Data Set (ASC-WDS) (Skills for Care) 22nd February 2023, online us06web.zoom.us/webinar/register/WN_ MgcfWtddQ6ySSzU672NYWQ
Health and Care Explained, The King’s Fund 21st-22nd February 2023, online www.kingsfund.org.uk/events/health-and-careexplained-2023
The Managers Conference 13-14th March 2023, Leicestershire www.nationalcareforum.org.uk/events/themanagers-conference-2023
Care England Conference and Exhibition 16th March 2023, London www.careengland.org.uk/events/care-england2023-conference-and-exhibition
UK Care Week 2023 22nd-23rd March 2023, Birmingham NEC www.ukcareweek.com
CMM EVENTS
Event: Date/Location: Contact: Event: Date/Location: Contact:
CMM Insight Online - In association with the National Care Forum 23rd March 2023, 12:00-13.30, online
Lisa Werthmann, Director Email: lisa.werthmann@carechoices.co.uk Tel: 01223 206964

CMM Insight Online - In association with the National Care Forum. 25th May 2023, 12:00 – 13.30, online Lisa Werthmann, Director Email: lisa.werthmann@carechoices.co.uk Tel: 01223 206964
Please mention CMM when booking your place.
Sign up online to receive discounts to CMM events and for more information on our upcoming events in 2023. www.caremanagementmatters.co.uk
@CMM_Magazine #CMMInsight
CMM February 2023 49
T: 01622 766078 E: info@edify-consultancy.co.uk W: www.edify-consultancy.co.uk
Call, email or click online to book your training needs today!
What a worry staying training compliant and retaining staff can be...
KATHY ROBERTS • CHIEF EXECUTIVE • ASSOCIATION OF MENTAL HEALTH PROVIDER

our country needs every day.
In Poverty, economic inequality and mental health, our Associate member, the Centre for Mental Health, found rates of depression, serious mental illness, and suicide (not to mention nearly every physical illness and injury) worsen with increased poverty and deprivation.
Roberts, Chief Executive of the Association of Mental Health Providers, updates on the provision of services and what needs to happen to ensure mental health equality across the UK.
Official data currently states one in four adults and one in 10 children experience mental illness but barely a week goes by without a new report about this nation’s worsening mental health.
The NHS Mental Health Bulletin 2021-22 annual report reveals over three million people were known to be in contact with secondary mental health, learning disabilities and autism services at some point in the year. Year on year, this is an increase of 16.2%.
Whilst the Mental Health Investment Standard has continued to be met nationally and regionally, these statistics clearly show that demand for services is outstripping supply of funding and resources.
Significant variation across the country regarding the money that local authorities and NHS systems have to spend on mental health means that the support a person receives is dependent on where they live, and even less accessible if they belong to a marginalised community.
The report suggests over half
of UK adults report feeling either anxious, depressed, and/or unable to cope due to concerns about their finances. It goes on to say one in six people have experienced suicidal thoughts or feelings as a result of the rise in the cost of living this year.
Today, more than ever before, we are facing a crisis in our community’s mental health and in the provision of services by the VCSE (Voluntary, Community and Social Enterprise).
Data has long played a role in how public services respond to complex problems, yet until now there has been a significant gap in the ability to link VCSE, independent and NHS mental health provision.
Our national network of over 300 care and support providers has shared with us their service information.
In partnership with mapping and spatial data analytics experts Esri, we have created a visual resource to show where mental health services are located and the
gaps in provision.
Through this tool, we can bring together a community of practice to provide our integrated care system partners the ‘weapon’ to tackle this inequality and the ability to clearly see the impact of solutions which focus on place-based access to mental health services.
Our data shows 844 active CQC-registered services providing mental health care and support across the country. However, we wanted to move beyond the lens of the NHS and the regulator. This data does not include individuals accessing services through non-clinical pathways.
We have mapped 1538 mental health service locations across the country. Our mapping tool provides details of our 696 Association members, whose combined annual turnover is £5.02bn, plus other small VSCE mental health organisations that deliver extensive support to address health inequalities at place level.
These VCSE organisations are providing vital, sometimes lifesaving services, for one in eight people across the UK, preventing conditions from deteriorating and/or relapse.
Collectively we challenge inequality and injustice locally, regionally and nationally, and the VCSE sector provides the diverse range of mental health care services
Clearly now with our data, even in some of the most deprived areas of the country, such as North and East London, Greater Manchester, we have not harnessed the full power of VCSE provision through effective communication or commissioning practices to appropriately serve the needs of these communities.
If more people could access the mental health care and support they needed close to home, undoubtedly there would be less pressure on acute and crisis services and urgent care within the NHS.
Nobody should be told they are too complex to be seen, because this goes beyond the impact on health services; poor mental health affects the economy.
The Health and Safety Labour Force Survey (LFS) found stress, depression or anxiety accounted for £17m lost due to work-related ill health in 2021/22.
Through our campaign ‘Mental Health Equality Now’, we are calling on the Government to protect and promote the Nation’s mental health by;
1. Recognising the VCSE Mental Health sector as critical to the nation’s health and care.
2. Utilising our knowledge and expertise, by knowing who we are, what we do and where we are.
3. Ensuring the VCSE Mental Health sector has sustainable ongoing and future funding.
4. Enabling everyone in every community to have fair and equal access to mental health services and support.
the UK and will you be supporting the Mental Health Equality Now campaign? Visit www.caremanagementmatters.co.uk and share your feedback on the column.
How would you review the Government’s approach to improving mental health
50 CMM February 2023
Kathy
Kathy Roberts is the Chief Executive of the Association of Mental Health Providers. Email: kathy@amhp.org.uk Twitter: @AssocMHP
service provision across
CRISPR. Diagnostics. 2021;11(5):823. 3. MedTech Europe. The Value of Diagnostic Information in Acute Respiratory Infections — Observations From the COVID-19 Pandemic. Accessed November 2021. https://www.medtecheurope.org/wp-content/uploads/2021/04/vodicase-on-respiratory-disease_case-study.pdf. 4. Moore N, et al. Evaluation of the Alere™ i Influenza A & B 2 Assay. Poster presented at: ASM Clinical Virology Symposium; 2018; West Palm Beach, Florida. 5. Abbott. ID NOW™ Product Inserts. 6. Abbott. Data on File. ID NOW™ Strep A 2 Clinical Trial. © 2022 Abbott. All rights reserved. All trademarks referenced are trademarks of either the Abbott group of companies or their respective owners. Any photos displayed are for illustrative purposes only. Any person depicted in such photos is a model. COL-15642 08/22


















IMAGINE IF YOU COULD QUICKLY DIFFERENTIATE BETWEEN THE SYMPTOMS OF YOUR RESIDENTS’ RESPIRATORY INFECTIONS 1-3 ID NOW ™ RAPID MOLECULAR RESPIRATORY TESTING PLATFORM ID NOW™ IS AN EASY-TO-USE CONNECTABLE INSTRUMENT WHICH PROVIDES POSITIVE RESULTS FOR: • SARS-CoV-2 in 13 minutes or less 5 • Influenza A & B in as little as 5 minutes , with
detected within 7 minutes 4 and negative results in 13 minutes 5 • RSV in
minutes or less 5 • Strep A in as little as 2 minutes , with 99% detected within
minutes 6 and negative results in 6 minutes 5 SCAN TO LEARN MORE ABOUT ID NOW ID NOW ™ PLATFORM ID NOW™ - Helping you to put your residents’ needs first by treating them quickly, and isolating where needed. 1. NHS England and NHS Improvement. Primary Care Bulletin. Updated June 29, 2021. Accessed November 2021. https://www.england.nhs.uk/ coronavirus/primary-care/other-resources/primarycarebulleting/june2021. 2. Zhou H, Tsou JH, Chinthalapally M, Liu H, Jiang F. Detection and Differentiation of SARS-CoV-2, Influenza, and Respiratory Syncytial Viruses by
95%
13
3







Care Choices Ltd 3, Valley Court Offices, Lower Rd, Croydon, Nr Royston, SG8 0HF (01223) 207770 www.carechoices.co.uk Care Information Search for Care Blog Publications Useful Contacts Contact Us Details Features Care Choices is the reliable place to find the care that’s best for you and the information you need. Whether you’re looking for a care home or ideas on staying independent at home, this website has been designed to make it easy for you. ENHANCE YOUR PROFILE TODAY www.carechoices.co.uk 01223 206967 І paul.ocallaghan@carechoices.co.uk * Minimum booking period is 1 year. Price excludes VAT. For full details of opportunities to promote your service on the website, contact us. Promote your service to care seekers for as little as £4.71 per week*