Exclusive VIP Access at the Care Show
Take time to relax and try some of our award-winning dishes in our VIP Lounge
Chat to us about all things food; from catering for residents with specialist diets to elevating your dining experience



Discover how you can serve delicious, nutritious meals hassle-free, all whilst saving you time & money


11th & 12th OctoberNEC, Birmingham
Scan the QR Code to secure your spot in our VIP Lounge or visit apetito.link/careshow


In this issue
Social Care
Professor Vic Rayner OBE, Chief Executive of The National Care Forum (NCF), reflects on the recent Global Ageing Conference and explains how, together, we can change the story of ageing care.

Inside CQC
The new assessment framework is for providers, local authorities and integrated care systems, and applies from registration. Mary Cridge, Director of Adult Social Care at CQC, shares the latest updates from the regulator.
CMM News
Into Perspective
This month, our experts review how the sector can best capitalise on international talent to ease workforce pressures and CMM delves into the latest workforce statistics.
Celebrating Excellence
Robert Lamacraft, a chef at St Martins Housing Trust’s Highwater House, won the Creative Arts Awards at the Markel 3rd Sector Care Awards 2023. CMM finds out how Robert uses art to engage residents.
Event Review
CMM shares its reflections on the Global Ageing Conference at the Scottish Event Campus in Glasgow, hosted in conjunction with The National Care Forum (NCF) and The Global Ageing Network.
What’s On?
Straight Talk
A new landmark study has highlighted personal safety concerns within the healthcare sector. Naz Dossa, Chief Executive of Peoplesafe and BSIA Chair of the Lone Working Group, shares his insights on the topic of workforce safety.
Supporting an ageing population: How prepared is the UK Government?
According to a recent Health Foundation report, an additional 2.5 million people in England will be living with major illnesses such as cancer, diabetes, dementia and depression by 2040. Dr Carole Easton OBE, Chief Executive at the Centre for Ageing Better, explains how we can support an ageing population.
The power of communication: Delivering BSL in care homes CMM caught up with Teri Devine, Director at RNID, the charity supporting people who are deaf, have hearing loss or tinnitus, to understand how care professionals can effectively communicate with deaf residents and residents with hearing loss in an accessible way.
Care Innovation Challenge: CMM meets the finalists

This month, CMM concluded the finalist interviews and spoke to Ben Howard from Team Careberry, Belinda McLean from Team Kit and Haoyu of Team Night Safety.
A generation of care: Gen Z’s role in shaping the future of care
What are some of the barriers for young people working in social care? Amanda Marques, Business Solutions Director at Cohesion Recruitment, outlines the current barriers when recruiting Gen Z and shares tips to help providers.
Everyone deserves gold standard care at the end of life
The Gold Standards Framework Centre (GSF) charity is committed to improving care for people in the final years of life in any setting. Keri Thomas OBE, Founder and Chair of The GSF Centre CIO, updates on the charity’s new training.

EDITORIAL
editor@caremanagementmatters.co.uk

Editor: Olivia Hubbard
Commissioning Editor: Angharad Burnham







Content Editors: Aislinn Thompson, Henry Thornton
PRODUCTION
Designer: Rebecca Mendil

Director of Creative Operations: Lisa Werthmann

Studio Manager: Jamie Harvey
ADVERTISING
sales@caremanagementmatters.co.uk
01223 207770
Advertising Manager: Aaron Barber aaron.barber@carechoices.co.uk

Director of Sales: David Werthmann david.werthmann@carechoices.co.uk
SUBSCRIPTIONS
Sign up to receive the latest magazines and news for FREE. info@caremanagementmatters.co.uk
01223 207770
www.caremanagementmatters.co.uk
Care Management Matters is published by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2023 CCL REF NO: CMM 20.7
CMM magazine is officially part of the membership entitlement of:
SOCIAL CARE INSIGHTS

From Professor Vic Rayner OBE
Professor Vic Rayner OBE reflects on the recent Global Ageing Conference in Glasgow and explains how, together, we can change the story of ageing care.
Last week, I had the pleasure of co-hosting the Global Ageing Conference in Glasgow, alongside Scottish Care and Global Ageing Network. As a global gathering of 650 people, there was plenty of perspectives, optimism and passion for the future of care and support. Having had time to reflect on the conference, I’d like to share some initial thoughts.
The global context of ageing
This conference was timely, coming while global societies face ageing population challenges. By 2050, one in six people in the world will be over 65. The number of people over 80 is likely to increase from 143 million in 2019 to 426 million in 2050. Mansur Dalal, Deputy Chair of CommonAge, reminded delegates that ‘senior care is an idea whose time has come’ with millions more people needing care in the coming decades and not just in ‘high-income western countries’.
Indeed, countries like India and the entire continent of Africa, while having much younger populations than western countries, also have rapidly growing older populations and a shortage of care workers. This context must be kept in mind when thinking about national policy development.
International collaboration
We face a crisis in which the highly skilled
workforce (domestic or migrants) is not recognised or properly renumerated for their skills by the state, indicating how our society currently regards adult social care. We need to unify to address this injustice. International recruitment to support a global social care workforce needs to be radically rethought in the face of rapidly changing demography.
We, as a global community, need to work together to move away from the ‘extraction’ of staff from lower-income countries that Dr Leon Geffen, Director of the Samson Institute for Ageing Research in Cape Town, referenced in his presentation at the International Workforce Summit. We should use our global influence to build an ethical framework which ensures that people working in care, wherever they are in the world, are valued equally for the work that they do.
A human rights approach
In her keynote address, Claudia Mahler, the United Nations (UN) Independent Expert on the Human Rights of Older Persons, called for the UN to adopt a Convention on Human Rights for older adults to help form a global consensus on a human rights-based approach to social care reform and recruitment which would help deal with the entrenched inequalities that are creating a barrier to meaningful reform.
Changing the story of ageing care

A theme of the conference was the need to rethink how we conceptualise ageing. Sir Geoff Mulgan, Professor of Collective Intelligence, Public Policy and Social Innovation at University College London, said our societies don’t like thinking about ageing and see it through a negative lens, which influences how we talk about and perceive social care and how we imagine the future. He posited several ‘shifts’ required to move from this pessimistic vision to one which celebrates people living longer.
These shifts include recognising care is fundamental to the economy, generating jobs and enabling people to live healthier, dignified lives for longer. As people live longer, but work less, they have more time and can often still be involved in the wider economy, and importantly, have fun! This requires a rethink about what it means to be healthy, more focus on social and mutual support, and community rather than the ‘curative and medical models’ policymakers fixate on. Technology will feature, but other innovation is also important – such as coaching, further study and career changes for older adults.
We need a better story about care and the ageing process. Ageing doesn’t suddenly begin at 65 and is not the same for everyone – with the right support, community and agency, people can remain healthy and independent for longer and continue to participate in society.



























Mary Cridge is Director of Adult Social Care at the Care Quality Commission. In her latest column for CMM, Mary updates on the regulator’s progress towards rolling out its new assessment framework.

INSIDE CQC
Mary Cridge
There’s always a real sense of renewal and fresh starts around this time of year, as the leaves begin to change, and children begin their new school years. This year's no different as we continue to move towards our new way of working.
We’ve brought together our colleagues into new integrated assessment and inspection teams and invested in and continue to test and deploy new technologies. Our pilot assessments of local authorities and integrated care systems are underway. We’re also beginning to share detailed guidance about our new assessment framework.
The new assessment framework is for providers, local authorities and integrated care systems, and applies from registration. Its focus is on what matters to people who use health and social care services and their families.
There are changes, yes, but there’s also a lot that remains the same. The regulations, ratings and the five key questions (is it safe, is it caring, is it effective, is it responsive, is it wellled?) remain. Under each of the key questions, however, there are new quality statements and we’ll be asking you for evidence to demonstrate how you meet these. The quality statements cover lots of the same areas as the key lines of enquiry (KLOEs).
Change can be unsettling, but I believe that this is a change for the better. The new framework enables a fair playing field for all providers. Some elements will look different, but it’s important to remember that the legal responsibilities remain unchanged.
Please provide us with your best evidence of how you’re meeting the quality standards. The better you know your service and the stronger your information, the better our understanding will be.
While hearing the voices of the people using services and our observations of care remain critical to us, our new regulatory approach allows us to be more flexible about how, and when, we collect evidence. Our new integrated teams, technology and a flexible methodology means we’ll be able to collect evidence more regularly and in more appropriate ways. This means we’ll also be able to carry out more assessments and update our ratings more
frequently than we do now. This helps us respond more flexibly to changes in quality.
One of the next big steps is to invite providers to sign up to our new portal. We’re doing this in stages, and we’ll let providers know when it’s their time to join the portal. Please make sure that your contact details are fully up to date so that when we send the invitation to join the platform, the right person receives it.
Sharing improvement
One of the themes in our strategy is to seek out and share improvement where we see it. We recently inspected a residential home for older adults. In their first inspection, St Mary’s Riverside near Hull was ‘Outstanding’ overall, excelling in the areas of caring and well-led. People told us the care they received exceeded their expectations and that staff went above and beyond to ensure people were treated with care, dignity and respect. In addition, an excellent variety of activities and events were available so people could lead meaningful lives.
Spending time being creative can enrich our lives immeasurably. September sees the fifth annual National Day of Arts in Care Homes. The aim of the day is to champion, promote and encourage arts engagement in care settings and highlight the health and wellbeing benefits.
Organised by the National Activity Providers Association (NAPA), this year sees a week-long celebration building to the national awareness day on Sunday 24th September. Exploring our creativity can help us practise long-held skills or learn new ones. As my colleague James Bullion, Chief Inspector of Adult Social Care and Integrated Care, said, ‘Celebrating arts and creativity in care settings is a powerful way to give voice to people’s experience, and it nourishes our wellbeing. It’s great to shine a spotlight on its value and transformative effect.’
Arts and crafts can keep our hands dexterous and our minds sharp. Just think of the potential to share skills and creative ideas between residents through workshops or activities. How will you be using creativity and arts to demonstrate your commitment to supporting people’s lives?
OnePlan
Staff Rostering
With a single click, you can build a rota from one to four templated weeks. You can automate this process, allowing the system to automatically build rotas.
Client Management
With OnePlan’s client management area, you can manage clients’ incident reports and holidays, create full risk assessments and control clients’ care plans.

Along with ECM (electronic call monitoring) and NFC (near-field communication) technology, OnePlan gives you the availability for real time information to help monitor client care.

Finance

Create chargeable and payable rates based around your own company’s services. Rates change based around events such as time of day, day of week and duration of call.

Electronic Call Monitor
e ECM feature allows staff to clock in and out of clients’ calls, giving more accurate times.
Tracking
OnePlan’s tracking service allows you to track staff on an individual and company-wide base.
Rota View
e staff have visibility through the OnePlan app to view the rota seven days forward one day back.
Instant Messaging
With OnePlan’s free instant messaging, staff in the field are able to field communicate back to the office and vice versa.
Reporting
e reports have been designed to help manage the business. Examples of reports include staff and client reports, medication reports and many more.

Care Plans
You can make care plans visible to your staff on the mobile devices through OnePlan’s app.
Task List
You can create client specific tasks and objectives to completed on visits.

So ware is a cloud-based staff rostering so ware system for the domiciliary care industry, using the latest in cutting-edge technology for person-centred care.
NHS winter vaccine rollout kicks off with care
Residents of older adult care homes and people who are housebound will begin receiving their COVID-19 and flu vaccinations as the NHS kickstarts its winter vaccinations campaign. The adult COVID-19 and flu vaccination programme, which was brought forward following the emergence of a new COVID-19 variant, will prioritise those at greatest risk.
Starting with care homes and people who are housebound, other eligible groups will begin to be invited to get their top-up protection ahead of winter. NHS staff have prepared for the earlier start of the programme with 3,500 sites – more sites than ever before – taking part in the campaign this year to make it as easy as possible for people to get protection.
offered a vaccination sooner by GP surgeries or other local NHS services. The NHS is encouraging people to get both vaccinations as soon as they can and not delay, due to the risk of the new COVID-19 variant and ahead of the winter period. With the programme brought forward, vaccine providers will be given an additional payment of £10 for each COVID-19 vaccination they administer to care home residents from 11th September to 22nd October 2023. They will also be given a separate one-off payment of £200 for each completed care home by the end of 22nd October 2023. For other eligible groups, vaccine providers will receive an additional £5 acceleration payment for each COVID-19 vaccination administered to eligible people between 11th September and 31st October 2023.
APPOINTMENTS
Anchor
Two new Non-executive Directors have been appointed to Anchor’s Board. Elizabeth Froude was Group Chief Executive at Platform, operating coast to coast through the Midlands. Fred Angole was Finance Director and Deputy Chief Executive of YMCA St Paul’s Group, a supported housing provider providing accommodation and wellbeing services to vulnerable young Londoners.
Wilton Lodge
People will be able to book their jabs from 18th September, through the NHS website, the NHS App or by calling 119. Eligible groups may also be
NHS Director of Vaccinations and Screening, Steve Russell, said, ‘The NHS flu and COVID vaccination programmes have been very effective in protecting those at greatest risk and we will work at speed to ensure they are protected once again this year, starting with care homes and those who are housebound.’
Birmingham City Council issues Section 114 notice
Birmingham City Council has issued a Section 114 (S114) notice, informing Government that it can no longer balance its budget. The council is to halt all spending other than on statutory services, including adult social care. The council has cited a £760m bill for Equal Pay claims and an in-year financial gap within its budget as the main reasons for the S114 notice.
Cllr Tim Oliver, Chairman of the County Councils Network (CCN), said, ‘CCN’s member councils are currently not in the same position as Birmingham City Council or other authorities who have issued S114 notices this year, who clearly face particular financial issues alongside the spending pressures impacting all councils.
‘But while CCN member councils are efficient and well-run councils, the level of overspends they face are clearly unsustainable. We are calling for further action from Government in the Autumn Statement, otherwise county
authorities could face unpalatable decisions further down the line.’
Despite the council’s reassurance that it would continue to provide essential services, the sector has responded with concern about the impact of the S114 on adult social care.
Professor Martin Green OBE, Chief Executive of Care England, commented, ‘Time and time again Care England has warned that the lack of money going to local systems fails to meet the levels of care needed locally. Local authorities are required to find an equilibrium between a legally balanced budget and delivering public services but are restricted by inadequate central Government funding, and their ability to raise the necessary funding locally.
‘Time has run out for Birmingham, and the Government must immediately unlock essential funds for all local authorities to ensure adult social care and our public services are uninterrupted.’
Wilton Lodge in Hull, providing dementia care, has appointed a new manager. With a background in health and social care, Joycelyn Tsekpo brings significant experience to Wilton Lodge, having worked extensively in both the NHS and the social care sector for over 15 years. Most recently, Joycelyn was the manager of Alderson House Care Home in Bridlington.
SweetTree Home Care Services
SweetTree Home Care Services, providing domiciliary care solutions, has announced the appointment of Denis Repard as its new Chief Executive Officer. With a distinguished career in the healthcare industry and a proven track record of successful leadership, Denis Repard is prepared to lead SweetTree into a new era of growth and innovation.
Care Provider Alliance
The Care Provider Alliance has announced Dr Jane Townson OBE, Chief Executive Officer of the Homecare Association, as its new Chair. Jane follows Nadra Ahmed CBE, Chief Executive of the National Care Association, who served as the CPA’s Chair for the past 12 months.
"Vaccine providers will be given a one-off payment of £200 for each completed care home by 22 October."
New research on financial challenges for older people
New research from Independent Age shines a light on the unique financial challenges for older people from minoritised ethnic communities.
Older people from minoritised ethnic communities are being let down when it comes to escaping poverty, as language barriers, Government mistrust and a lack of effective promotion of financial support stand in their way, according to new research from the charity.
Independent Age, which supports all older people facing financial hardship, analysed census data and spoke to organisations and individuals to develop a better understanding of the shared and unique challenges faced by those from Black, Asian and minoritised ethnic communities, one of the most at-risk groups when it comes to experiencing poverty in later life.
Its analysis found that 29% of older Asian/
Asian British and 25% of older Black/Black British/Black Welsh: African people are living in poverty. Both figures are much larger than the overall pensioner poverty rate of 18%.
Independent Age’s analysis also revealed that older people from Black and Asian communities are less likely to own their homes and are more likely to rent in the social and private sectors. Almost half (49%) of Black/Black British/Black Welsh: African older people in the UK rent social housing. This much higher than the national average for older people renting social housing which is currently 13%.
Also, the analysis showed that one in five (21%) older people from an Arab background rent in the private sector. People who rent in later life are more likely to be at risk of living in poverty in older age because many face high costs and insecurity.
Previous research from Independent Age
White Paper on longevity and ageing
The International Longevity Centre (ILC) has launched a new programme to develop a new Longevity White Paper detailing the necessary changes to seize the opportunities of an ageing population.
The project aims to:
• Present a positive, solution-focused vision for the UK and the world.
• Advocate for longevity to be recognised in government planning and thinking.
• Encourage businesses to maximise the ‘longevity dividend’.
Supported by Aviva, the Longevity White Paper will identify evidence-based solutions for an ageing society.
The ILC is consulting experts in ageing and longevity in multiple fields, including technology, climate change, international relationships, children and youth policy, and media communications in hopes of developing solutions for everyone.
David Sinclair, ILC Chief Executive, said, ‘We want to help forge a new vision for the 100-year life and a society where we all live happier, healthier and more fulfilling lives, where tomorrow is better than today and where future generations are better off.
‘Governments, policymakers, businesses, and employers need to develop and implement solutions to meet this ambition.’
Doug Brown, Chief Executive of Aviva UK
New report on disability rights
In a new report submitted to the United Nations (UN), the Equality and Human Rights Commission (EHRC) warns that many disabled people continue to face discrimination in the UK, and the situation continues to worsen, particularly in light of current cost-of-living pressures.
Produced in collaboration with the other equality bodies and national human rights institutions (NHRIs) in Britain and Northern Ireland, the report follows a 2016 UN inquiry
into the state of rights for disabled people in the UK, after which the UN published a list of 11 recommendations for the UK Government to protect the rights of disabled people. This inquiry was held under the Convention on the Rights of Persons with Disabilities' (CRPD) Optional Protocol.
Kishwer Falkner, Chairwoman of the EHRC, said, 'Alongside other human rights and equality bodies in Britain and Northern Ireland, we urge the governments in London
highlighted how Black pensioners are at the greatest risk of long-term poverty with 17% of Black older people experiencing poverty for seven to nine years during a nine-year period, compared to 6% for all pensioners.
Morgan Vine, Head of Policy and Influencing at Independent Age, said, 'While older people on a low income across the UK face many similar challenges, especially as the cost of living continues to stretch people’s budgets to breaking point, our findings clearly show that minoritised ethnic communities are facing some unique barriers which must be overcome.
'Our older population is growing and becoming more diverse. Independent Age wants everyone to be able to live with dignity; we don’t want anyone in later life to be left behind.’
Visit the Independent Age website to read the research findings in full.
and Ireland Life, said, ‘We cannot ignore this fact – the UK’s population is ageing. We must prepare for the challenges and embrace the opportunities that come with our longer lives.
‘Aviva already helps millions of people prepare for and live through later life. We are therefore delighted to support the ILC in their important work and we look forward to building on their insights.’
Over the coming months, ILC will release a series of thematic briefing papers setting out the issues of concern, sharing new statistics and inviting solutions. The final version of the Longevity White Paper will be officially launched at the ILC’s Future of Ageing 2023 Conference on 7th December 2023.
and Cardiff to address the problems faced by disabled people and take action to address the UN’s recommendations from 2016.’
Dr Rhidian Hughes, Chief Executive of the Voluntary Organisations Disability Group (VODG), said, 'It is deeply concerning that seven years after the initial findings of the Committee on the Rights of Persons with Disabilities to improve the lives of disabled people across the UK, evidence again finds the Government to be failing disabled people.’

Care group sets out autumn campaign strategy
Campaigners have unveiled an autumn campaign strategy to get politicians to tackle the crisis in the care of vulnerable adults. The Independent Care Group (ICG) plans to target party conference season to press for positive change in social care.
New adult social care sector workforce survey
its own election manifesto for the General Election and stepping up its lobbying and campaigning activities for the benefit of the sector.
Mr Padgham said, ‘The party conference season offers a golden opportunity for the political parties to show what they plan for the future of social care. We look to them for bold new ideas to support social care, tackle the inequalities that currently exist and prepare the sector for an exciting future.’
The adult social care sector is being urged to complete a new workforce survey to capture its experiences and support improvements over time. Skills for Care, in partnership with Ipsos and the University of Kent, has launched the survey on behalf of the Department of Health and Social Care (DHSC).
capacity and training – and the forms of support which could make adult social care a better place to work.
The data collected through the survey will aid Government's decisions on how to support the adult social care sector and workforce.
ICG Chair Mike Padgham has written to the health teams of the Conservatives and Labour, urging them to make social care a priority.
The ICG is also offering to share its expertise with politicians as well as preparing
The ICG has already set out its broad wishes in its Five Pillars of Social Care Reform document which has been sent to the Government and to the Labour health team to try and influence their thinking on social care. Visit the ICG website for more details on its campaigning work.
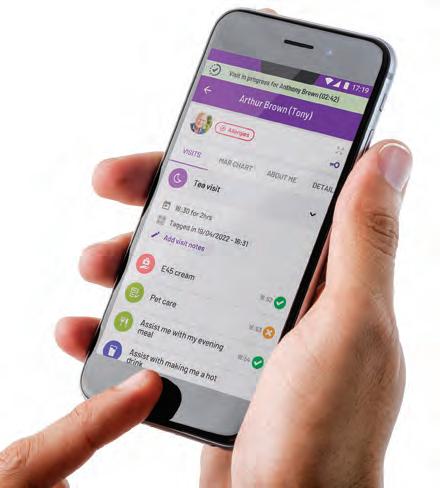
An easy way to manage your care organisation
Caregraphy is an advanced health and social care management system for creating and managing records like notes, care plans, scheduling, eMARs, and a lot more. It is also geared to improve your competence for Ofsted and CQC compliance.
The survey is open to people working in any care-related role across all settings in adult social care, including personal assistants and employees in local authority adult social care departments.
The survey will contribute to Government’s understanding of working conditions and experiences for the adult social care workforce – such as working hours, pay,
Oonagh Smyth, Chief Executive Officer at Skills for Care, commented, 'We are pleased to provide this important opportunity for everyone working in social care to share their experiences with the Government to inform its thinking on policies that will better support people working in social care.’
The survey is available to complete now on the Ipsos website at https://ipsos.uk/ ascworkforce
Being easy to use, Caregraphy enhances efficiency allowing you to focus on improving outcomes for your clients. Trusted by providers of supported accommodation, children’s homes, family assessment and other residential settings, Caregraphy is an easy choice.
We are not just a software provider, but we are committed to partnering with you to ensure Caregraphy meets your needs.
Book a demo today and see how to succeed with Caregraphy!
+44 3333 583 123 www.caregraphy.com
"A golden opportunity for the political parties to show what they plan for the future."
Critical care admissions study published
A new study by the Cicely Saunders Institute at King’s College London has found that critical care admissions for people with dementia are going down but increasing in the last year of life.

The study included people with dementia identified from South London and Maudsley NHS Foundation Trust, which covers four South London boroughs (Southwark, Lambeth, Croydon, Lewisham).
This study does not compare these trends with critical care admissions data for people without dementia in their last year of life.
In the first study of its kind, the Empowering Better End of Life Care (EMBEDCare) team at King’s College London and University
College London were able to track critical care admissions of people with dementia in South London by linking data from the South London and Maudsley’s Clinical Record Interactive Search (CRIS) with national hospital records.
Emel Yorganci, lead author and ESRC PhD Training Fellow at King’s College London, said, 'As the number of people living and dying with dementia is increasing, understanding how we can provide high-quality, equitable care to people with dementia until the end of their lives must be a priority.’
The paper, Survival and critical care use among people with dementia in a large English cohort, is published in Age and Ageing.
New analysis of adults receiving NHS CHC
New analysis has revealed the number of adults receiving NHS Continuing Healthcare (CHC) assessments is yet to return to pre-pandemic levels. This includes the proportion that are deemed eligible for the funding package, according to retirement specialist Just Group.
NHS CHC is an NHS-provided package that fully funds people’s care where there is primarily a ‘health need’. This means that qualifying treatment or care is typically for serious, long-term or complex conditions which may have arisen from a disability, accident or illness which affects the individual’s day-to-day care needs. NHS CHC is not means-tested and is available to people regardless of their wealth or assets.

The latest figures obtained
from NHS England show the number of people being assessed as eligible for CHC funding each year has dropped by 32% from 15,963 people in 2018/19 to 10,847 people in 2022/23.
Stephen Lowe, Group Communications Director at Just Group, commented, 'Whilst the people completing the CHC process and being deemed eligible may be an increasingly rare group, it remains one of the most financially generous benefits on offer – helping patients in full with the financial costs associated with serious, complex and long-term medical conditions.’
For the latest statistics relating to the activity of NHS CHC in England, visit the NHS England website.


No-fault eviction every 16 minutes
A no-fault eviction notice drops through the letterbox of an older private renter every 16 minutes, new research from Shelter reveals.
The research, conducted by YouGov and funded by The Co-operative Bank, shines a spotlight on the struggle older renters in England face in keeping a roof over their heads. Nearly three in ten (28%) private tenants over the age of 55 reported living in fear of being evicted by their landlord.
People who receive Section 21 notices have only two months to move out and their landlords do not have to give a reason for evicting them. But a third of all private renters (34%) say the last time they moved, it took them longer than two months.
Shelter is urging the
Government to scrap no-fault evictions and protect at-risk renters from the threat of Section 21.
Polly Neate, Chief Executive of Shelter, said, 'Older renters may already be retired or planning for retirement at this point in their lives. They shouldn’t have knots in their stomachs, constantly afraid that their landlord is going to kick them out of their home for no reason.’
Nick Slape, Chief Executive Officer at The Co-operative Bank, said, 'Fighting inequality across the UK is extremely important to our customers, and that’s why we’re campaigning for better rights for renters alongside Shelter.’
Visit the Shelter website for more information about the research findings.

New blood test to detect Parkinson’s
Research has revealed a new test to detect problems with mitochondria in blood cells which could be used to diagnose Parkinson’s. The research, published in Science Translational Medicine, showed that the test focused on detecting DNA damage in the mitochondria.
Mitochondria are the energy-producing batteries that power cells that stop working properly in brain cells affected by Parkinson's.
Mitochondria contain their own DNA, and earlier studies in post-mortem brain tissue from people with Parkinson’s have revealed that mitochondrial DNA becomes damaged because of the condition.
This new research indicates that this mitochondrial
DNA damage can also be detected in blood cells from people with Parkinson’s and could potentially be further developed to provide a definitive diagnostic test, something that currently doesn’t exist for Parkinson’s.
Claire Bale, Associate Director of Research at Parkinson’s UK, commented, 'Further work is now needed to understand and develop the full potential of this new test. We are hopeful that definitive biological tests for Parkinson's – whether it is this new mitochondrial blood test or another – will be ready to be used within the next few years.’
To read the new research in full, visit the Science Translational Medicine website.
Extra £50m home adaptation funding
£50m has been allocated to local authorities to help older people and those with disabilities live safely and independently in their own homes.
delivered through the Disabled Facilities Grant and comes on top of the annual £573m already provided to local authorities for home improvement services.
Minister for Adult Social Care, Helen Whately, said, ‘If you’re older or living with a disability, a well-adapted home gives you independence and safety.
Dementia researchers joined forces
More than 100 visitors came to a University of Northampton event to hear from leading experts in dementia innovation and research.
Education (ADRE) and NDRIC.
Delivered jointly by the Department of Health and Social Care and the Department for Levelling Up, Housing and Communities, eligible disabled people of all ages will be able to apply to their local authority for a grant to adapt their home to better meet their needs.
Available to homeowners, private renters and those in social housing, the funding will be
‘Living in your own home can be impossible after illness or injury without changes like wheelchair ramps, handrails or a stairlift.

‘This new funding will help thousands more people have homes fit for their needs – and faster. When time is of the essence, this fund will help local authorities do urgent and smallerscale adaptations more quickly.’
For more information, visit the Foundations website.

The conference – held on Wednesday 23rd August –covered the most impactful solutions to support independent living for people who have dementia. The aim was to showcase and celebrate over a decade of research in this field completed by the University of Northampton’s Dementia Research and Innovation Centre (NDRIC) which was founded and co-led by Professor Jacqueline Parkes and Associate Professor, Dr Alison Ward.
‘Dementia Pathways on Your Doorstep’ was jointly delivered by the Academy for Dementia Research and




Professor Jacqueline Parkes, lead person of University of Northampton’s Dementia Research and Innovation Centre and Founder/Director of ADRE, said, ‘The conference allowed us the chance to tell the evolving story of how we tackle dementia and its enormous impact on people and communities and isolate the key next steps in our journey.’
Jane Beaumont, Director of ADRE, added, ‘People who attended – from esteemed researchers and carers and people who have a diagnosis of dementia – told us they felt there was a tangible sense of community, a real family vibe to the event. Those who have attended similar conferences felt it was unlike those activities.’
"This new funding will help thousands more people."


Scotland’s care workforce grows
Scotland’s care workforce grew by 1.5% to 211,510 people from 2021 to 2022, according to a newly published report.
The Scottish Social Service Sector: Report on 2022 Workforce Data report, published by the Scottish Social Services Council (SSSC), shows the workforce makes up around 8% of all Scottish employment or one in 13 jobs.
The report shows the biggest workforce increases were in housing support/care at home and day care of children's services and nurse agencies. This reflects the move towards more care being provided in people’s own homes and the expansion of free early learning and childcare.
The report combines administrative data collected
by the Care Inspectorate with data collected by the SSSC directly from local authorities to form a comprehensive picture of the paid workforce employed in the social service sector in Scotland at the end of 2022. The SSSC is an official statistics provider.


SSSC Acting Chief Executive, Maree Allison, said, ‘As Scotland’s social work, social care and children and young people workforce continues to grow, it’s a good time to recognise the valuable contribution they make helping people live the lives they want but also their contribution to the economy.’
You can download the Scottish Social Service Sector: Report on 2022 Workforce Data report from the SSSC website.
Paragon Skills acquired by Knovia Group
Knovia Group has announced the acquisition of leading care sector education and training provider, Paragon Skills. Knovia is a group of sectorfocused businesses supporting the adoption of impactful and relevant technology to drive sustainable change and innovation. Alongside Paragon Skills, who work with over 7,000 learners and 1,500 employers a year, Knovia has also announced the acquisition of Tempdent, a leading dental training provider and recruitment agency.
This acquisition comes as part of a strategic expansion of Knovia Group within the education and training sector, enabling all group companies to work in partnership and strengthen their overall performance within their
National Suicide Prevention Strategy
WHAT’S THE STORY?
Government has pledged to reduce England’s suicide rate within two and a half years with the launch of a new National Suicide Prevention Strategy. Government will be taking action to aid specific groups at risk of suicide. More than 100 measures being taken include:
• A new national alert system to notify relevant authorities – like schools, universities and charities – of emerging methods of suicides and risks, and any required actions that can reduce access or limit awareness.
experience losing a friend or relative to suicide.
Government continues to outline that children in schools across England will have access to a dedicated mental health support team by the end of March 2025. Mental health support teams intervene where a mild-to-moderate mental health issue is identified and ensure children and young people are both protected and supported.
WHAT DO THE EXPERTS SAY?
dedicated sectors. The new group structure will not affect the day-to-day operations of either company, both companies will continue to operate as usual delivering education within their chosen sectors.
Ben Pike, Chair at Knovia, commented, ‘We are excited to be launching Knovia as a platform that supports the ambitions of the businesses and leaders within our group. With our human-centred, technology-supported learning models, we are committed to building a scalable and sustainable education group. Both Paragon Skills and Tempdent share a best-inclass approach to learning and a passion to deliver the measurable social impact that underpins our group objectives.’
• Fresh guidance issued to first responders, recognising new and emerging methods and how such incidents should be dealt with.
• Near real-time surveillance of trends in tragic suicides to be introduced on a national scale this year –enabling more timely and targeted actions.
• A Government pledge to collaborate with countries around the world to target and stop suppliers of dangerous and lethal substances at the source.
WHAT WILL THE IMPACT BE?
Government states that its new strategy will enable thousands more people approaching a crisis to get the support they need, and fewer loved ones will
Minister for Mental Health, Maria Caulfield, said, ‘The impact of suicide on individuals and loved ones is devastating. This strategy will bolster the work this Government is already undertaking to reduce the number of suicides and help us intervene where needed as early as possible.’
Health and Social Care Committee Chair, Steve Brine MP, said. ‘I welcome the Government’s target to reduce suicide rates with the new national strategy to provide help and support for people at a point where it can save lives and change futures.
‘Ministers have recognised that underlying the strategy’s success is the need for a bigger mental health workforce. We’ll be monitoring the Government’s ambitious target to grow this workforce by nearly three-quarters by 2037.’
Visit GOV.UK to read the new strategy in full.
New report on human rights in Lithuanian social care system
The Seimas (Parliament) Ombudspersons’ Office of Lithuania has published a report on human rights in the Jurdaičiai social care home, which also shows the general situation in all similar institutions.
The head of the Seimas Obmudspersons’ Office, Erika Leonaitė, stated that even though the living conditions are generally adequate, there are still many problems in the system due to the slow and ineffective reorganisation of care institutions. The Ombudsperson has recommended that care institutions should move
towards deinstitutionalisation and prepare individuals to live in local communities.
During the inspection of the Jurdaičiai social care home, it was discovered that there were individuals who, with appropriate assistance, could live in the local community, which should be a goal under the reorganisation of care institutions. However, the problem is that there is a lack of housing for such individuals, forcing them to remain in the care home.
Moreover, due to the reorganisation of the social care
International Day of Care and Support for Older People Declared
The Global Ageing Network has established 7th September as the International Day of Care and Support for Older People, an annual opportunity for individuals, organisations and countries to honour caregivers – especially the caregiving professionals serving older people in hospitals, nursing homes, home care agencies and across the long-term care sector. The announcement was
made during the 2023 Global Aging Conference, a gathering of more than 400 professionals from more than 40 countries in Glasgow. The first celebration will occur in 2024.
Current Global Ageing Network Board Chair, Jiří Horecký, PhD, MBA, of the Czech Republic, shared the news during the opening session of the conference, ‘We all benefit when trained caregivers are available, supported and respected,’ said Dr Horecký. ‘The International Day of Care and Support for Older People provides the ideal occasion to show the vital impact of these individuals on nearly every family on the planet.’
system, the number of available places in social care homes is reduced each year, but a waiting list to get into these institutions still exists. Seimas Ombudsperson Erika Leonaitė suggested that this means that there are no proper alternatives to institutional care in Lithuania.
The Jurdaičiai social care home is providing information for its residents in simple language and the infrastructure is generally adapted for residents with disabilities or impairments. However, psychological services for the residents were insufficient.
Residents also lack the skills which would allow them to live in the local community, such as using public transportation and financial literacy.
Currently, there are about 30 institutional care homes in Lithuania, which together house about 6,000 residents with disabilities. The aim of deinstitutionalisation is to establish 42 community residential homes for 300 people by the end of this year.
To read the report in full, visit the Seimas (Parliament) Ombudspersons’ Office of Lithuania website.

European Care Strategy – One year on

One year ago, the European Commission presented the European Care Strategy. One year on, several actions have been launched to ensure high-quality affordable and accessible care services and to improve the situation of care providers. This has taken place in close co-operation with Member States, social partners and stakeholders.
Among other actions, Member States appointed national longterm care co-ordinators/contact points to design and monitor national reforms. This is the first in a planned series of mutual learning events among national co-ordinators and experts focused on quality for long-term care.
To support national reforms, 18 Member States are tapping into the Recovery and Resilience Fund. Additional EU funding
support is also available through European Social Fund+, European Regional Development Fund, European Agricultural Fund for Rural Development, the Just Transition Fund, the Horizon Europe or Digital Europe programmes. Moreover, at least five Member States will receive technical assistance to design long-term care reforms from the European Commission.
The strategic partnership between the European Commission and the World Health Organization will support the training of informal carers and help Member States design national reforms. The Commission and the Social Protection Committee will keep improving data collection for better evidence and monitoring of long-term care.
"We all benefit when trained caregivers are available, supported and respected."



Supporting an ageing population:
How prepared is the UK Government?
A recent report paints a gloomy picture of the nation’s future health needs. Dr Carole Easton OBE, Chief Executive at the Centre for Ageing Better, argues that this needn’t become reality if we take a more preventative and forward-thinking approach to our ageing population now.
Reading the recent report from The Health Foundation and its projections of levels of ill-health among adults in the near future, one could be forgiven for feeling extremely pessimistic about one’s own health and for the future wellbeing of the country.
The Health Foundation’s analysis, carried out in partnership with academics at the University of Liverpool, details how an additional 2.5 million people in England will be living with major illnesses such as cancer, diabetes, dementia and depression by 2040.
The study predicts that 9.1 million people in England will have a major illness by 2040 – an increase of 37% compared with 2019. Individuals can expect to be living with major illness for 12.6 years in 2040 compared to an average of 11.2 years in 2019.
What makes this research even more concerning is that it confirms previous research, which shows that the poorest people in society are those who will experience the worst deterioration in their health.
For example, Ageing Better’s 2022 State of Ageing report highlighted the existing 19-year gap in healthy life expectancy between the richest and poorest and this gap is only expected to grow.
But this gloomy vision of future generations
struggling and suffering through later life must be challenged.
Tackling societal issues
Overburdened public services are not an inevitable consequence of an ageing population; living longer does not have to mean extended ill-health.
Much more must be done to tackle societal causes of poor health and this response needs to be delivered across society. It means reconfiguring the way we think about ageing.
Too often, short-term political cycles mean that politics delivers short-term responses on policy issues when we need to look at the bigger picture and deliver meaningful change over a longer time period.
What we need is more prevention to reduce the need for more cures further down the line.
In 2019, Ageing Better worked with the Office for Health Improvement and Disparities on a consensus statement on healthy ageing.
The statement identified key principles for healthy ageing, including three principles that should guide the Government’s approach to tackling health risk factors:
• Putting prevention first – specifically, interventions targeted at an individual
level such as strength and balance classes, smoking cessation support and treatment for alcohol dependence.
• Ensuring good homes and communities to help people remain healthy, active and independent as they age.
• Narrowing inequalities across the life course to ensure that everybody has the same opportunities to achieve a good education, good work, financial security, and a decent home.
Four years on, these principles remain equally important and relevant, if not more so. But are they any more apparent in Government policy than they were four years ago?
Our politics has undergone substantial turmoil in that time, and it feels as if short-termism continues to have its day.
Failure to take more proactive and preventative action now to improve how we all age is a guaranteed recipe to building up insurmountable problems in the future.
The NHS is already buckling under the pressure. The social care system in this country has been predicted to implode by 2029. And the only reason it hasn’t already is because of the tireless work of unpaid carers who contribute the equivalent of more than four




million jobs in the sector.
Both health and care services are likely to be overwhelmed by the numbers projected in the Health Foundation report. We need action now therefore to avoid that nightmare scenario becoming a reality.
This action goes far beyond increasing investment in health and social care to keep up with demand.
Investing more in preventative health programmes and work to promote ‘active travel’ and encourage physical activity can help the population move towards later life in better health.
Reforms must go further
We need to ensure that homes are safe, healthy and accessible and we need to improve practice at work. We also need to tackle inequalities and ensure that communities are inclusive.
The quality of housing can have a tremendous impact on health and subsequently impacts on the pressures felt by health and social care.
The annual cost to the NHS attributed to low-quality housing is £1.4bn for first-year treatment costs alone.
Spending £1 on improving warmth in ‘vulnerable’ households can result in £4 of health benefits; £1 spent on home improvement services to reduce falls is estimated to lead to savings of £7.50 to the health and care sector.
Poor housing costs lives. And it is the poorest and most vulnerable people who are paying the greatest price for years of government neglect and inaction.
That is why we need a national plan to make all homes safe. This should include a mechanism for local delivery, such as Good Home Hubs – a national network of local one-stop shops for information and support to help people improve and maintain their own homes.
Previous research published by the Centre for Ageing Better reveals that making small changes to homes, such as installing handrails, ramps and level-access showers, alongside simple home repairs, could play a significant role in relieving pressure on the NHS and social care.
The research also found minor home aids and adaptations can greatly improve the quality of life for people losing mobility. Studies show that people’s difficulties with
‘Activities of Daily Living’ can be reduced by 75% – these include washing, bathing, going to the toilet, dressing and eating.
As well as adapting existing homes, the failure to build sufficient accessible homes enabling disabled and older people to live independently and with dignity is short-sighted and a false economy.
Currently less than one in ten homes in England provide the basic features for even the lowest level of accessibility. The Government needs to fulfil its 2019 manifesto pledge to raise minimum accessibility standards for new homes to help reduce future social care costs and pressure on NHS capacity.
Staying in work can be extremely beneficial for employees’ health and wellbeing. But more support is needed from Government and employers to help employees manage health conditions in the workplace.
This will become increasingly important as the number of working-age people with long-term health conditions rises.
Supporting employee health
Older workers are more likely than younger workers to be managing multiple long-term conditions, and health conditions are the main driver of older workers exiting the labour market before they reach state pension age.
The Government’s recent support for Private Members’ Bills on carer’s leave and flexible working conditions is welcomed.
Supporting carers to stay in work and to find the right balance between work and their caring responsibilities could help reduce demand on social care.
A recently passed Private Members' Bill granted workers the right to five days' unpaid carer’s leave.
But extending this to ten days of paid carer’s leave per year, and a right to up to six months of unpaid carer’s leave, will put this country on an even better footing to meet the needs of our changing demographics and growing ageing population.
Government could also make further efforts to reduce the stigma associated with disability through a public campaign to tackle ableism and ageism in the workplace, support part-time work, improve access to occupational health and introduce financial support for SMEs who support workers while on long-term sickness absence.
Community connection
To support people to age well, we also need to create local communities which are age friendly.
Creating communities where independence can be maintained for as long as possible can also help lower demands on social care services.
This requires empowering, resourcing and directing local Government to respond to significant demographic changes and take action on issues that matter to local older populations, including public transport and digital exclusion.
This could be done through funding and support to ensure that every local authority has the resources it needs to become an Age-friendly Community – a community where people can age well and live a good later life.
Clock is ticking
All of these policies will develop significant change over time and will hopefully avert the worse-case scenarios for 2040 envisaged in the Health Foundation report.
But unfortunately, our current political era is marked by instability. The lifespan of a Government minister is measured in months, so few are prepared to stake their reputation for change measured in decades.
That is why we need other advocates for long-term, societal reform within the corridors of power. And that is why the Centre for Ageing Better believes we need a Commissioner for Older People and Ageing (COPA) for England to ensure older people that policymaking across Government considers the long-term needs of our ageing population.
Wales and Northern Ireland already have commissioners who are improving the lives of older people and protecting their rights.
England has an independent commissioner protecting children’s rights but no one with the legal power to do the same for older people.
Without such a figure, the concern is that the political lens will never look beyond the next election.
And that short-term thinking is guaranteed to ensure that the Health Foundation’s vision of 2040 becomes a reality. CMM


THE POWER OF COMMUNICATION
DELIVERING
S L B
IN CARE HOMES
International Week of Deaf People, International Day of Sign Languages and World Deaf
Day were all recognised in September. CMM caught up with Teri Devine, Director at RNID, the charity supporting people who are deaf, have hearing loss or tinnitus, to understand how care professionals can effectively communicate with deaf residents and residents with hearing loss in an accessible way.
It’s estimated that 25,000 people use British Sign Language (BSL) as their main language across the UK, although the total number of people who use BSL (not necessarily as their main language) is likely to be much higher.
Deaf Sign Language users in care homes can be incredibly isolated, as they are often the only sign language user. Staff and residents are usually unable to communicate fully with them. This may make it harder for staff to monitor residents’ needs and wellbeing, and without regular contact with other deaf people who use BSL, deaf residents may even start to forget their own language. This has sadly been the case for my own mother whose ability to sign has decreased with lack of use.
Residents with hearing loss can also be at risk of isolation, especially if their hearing aids are not maintained and if staff don’t communicate with them in an accessible way. 70% of people over 70 have hearing loss, so it’s essential that care home staff have a good understanding of how to support people.

Learning BSL
British Sign Language (BSL) is the most common form of sign language in the UK. It was recognised as a language in 2003 and legally as an official language of Britain in 2022.
BSL involves a combination of hand shapes and movements, lip patterns, facial expressions and shoulder movements. It has its own grammar and is structured in a completely different way from English.
If you have residents who are deaf sign language users, some basic BSL training for staff can help make a positive difference. Being able to sign ‘good morning’, ‘can I help you’, or understand if someone is tired, worried or ill >



can make residents feel less isolated. RNID offers several remote training options for organisations including a live course delivered by an experienced deaf trainer or an e-learning module for staff to complete at their own pace. Our courses can help your staff have a basic conversation with a deaf resident and learn useful everyday signs such as greetings, fingerspelling and questions. Our Start to Sign course also covers useful contexts like Deaf culture, BSL structure and using facial expressions. For understanding the challenges that deaf residents and residents with hearing loss face and how to help, our Deaf Awareness training is also a great option.
Understanding hearing loss
If you suspect someone has hearing loss, their GP should refer them to audiology for a full hearing test and if appropriate, provide hearing aids. As a first step, you could help them do RNID’s free online hearing check, but this may not be appropriate for residents with diagnosed or suspected dementia who may not be able to complete the check.
Residents with hearing loss may:
• Comment that other people seem to mumble.
• Need things repeated.
• Struggle to follow conversations in noisy places or when in a group.
• Watch your lips when you are talking.
• Turn the television up too loud.
• Shout when in conversation without realising.
• Appear less engaged than others, particularly in group activities. Hearing loss and dementia can often be confused with each other, so it’s important to ensure residents with diagnosed or suspected dementia are referred for a hearing assessment, and that this is repeated every two years as recommended by NICE.
Hearing aids
Being aware of who is wearing or should be wearing hearing aids and knowing some basics is also important. Carers should:
• Check batteries are inserted correctly and don’t need changing – they should be replaced every seven to ten days.
• Ensure that rechargeable hearing aids have enough battery life and are recharged as often as recommended, for example every night.
• Check that the ear mould or tubing is not blocked with wax, that it’s not hard, twisted or split, and that there is no condensation in the tubing.
• Check that the volume control is not turned down, and that the wrong program is not being used, for example the loop setting if they aren’t using a loop system.
• Check the hearing aid is not whistling in the person’s ear – whistling is good as this means the hearing aid is working but if it whistles in the person’s ear this may suggest that it is not inserted securely, wax is present in the ear, or that the earpiece no longer fits and needs replacing.
If everything has been checked and the aid has been turned on and off to reset it but it’s still not working, it needs to be taken to audiology to be repaired.
RNID can provide support for care homes where there are multiple hearing aid users by running a one-off support session to provide hearing checks and maintenance. Many audiology departments have postal systems for simple repairs or may offer basic training to care home staff.
Aughnacloy House in Lurgan, Northern Ireland received Hearing Health training from the local RNID team. Connie Mitchell, Home Manager, said, ‘The training provided by RNID staff to my teams was professional, useful and informal enough for my staff to feel comfortable to ask questions. Staff feedback has always been positive.
‘The training supported newly recruited staff to learn more about communicating with our residents and supported them to be more confident in handling hearing aids and understand how to ensure they are working correctly.
‘We all benefited from the knowledge shared, particularly about changing batteries
regularly and regarding preventing falls. Hearing deficiencies are very common in our care home residents and to have the opportunity to have the RNID Hearing Health training and continued support would be an asset to all care homes.’
Like dentures or glasses, hearing aids can easily be misplaced or lost in bed, in a tissue, or on a table in a common area. This can result in having to wait a long time for a replacement and cause significant distress to the wearer.
It’s essential to record if a resident has a hearing aid, if they have one for each ear, and to create a system to keep them safe such as placing them in a named container whenever they are removed.
Communication
RNID’s communication tips are a useful resource for communicating with deaf residents and residents with hearing loss in an accessible way.
Care staff should always ask the person what support they need and record this information in their care plan, in line with NHS England’s Accessible Information Standard.
People who use (BSL) may be at risk of worse care and poor health if they cannot communicate in a meaningful way. To improve the quality of care, you should:
• Provide a fully qualified and registered BSL interpreter if the person needs one, in line with the Accessible Information Standard.
• Make sure there are opportunities for people who use BSL to stay in touch with family and friends, Deaf organisations and other community groups, either face-to-face or remotely.
For more information about supporting people who are deaf or have hearing loss, visit rnid.org.uk, or contact RNID by phone: 0808 808 0123 or email contact@rnid.org.uk
INTO PERSPECTIVE HOW CAN THE SECTOR BENEFIT FROM AN INFLUX OF INTERNATIONAL TALENT?

international recruitment fund. In February 2023, Government awarded this funding to help employers overcome some of the main barriers to international recruitment it had identified, including administrative complexity and costs but also challenges with issues like pastoral support, housing and travel.
Addressing challenges
Case studies from UNISON, the UK’s largest union representing members employed in the public, voluntary and private sectors, have revealed that some migrant staff who have travelled to the UK to take up jobs in social care are being forced to pay back thousands of pounds in fees, housed in sub-standard accommodation and forced to share beds with colleagues.
Furthermore, the Migration Advisory Committee’s Review of adult social care 2022 report summarised that using the immigration system to address shortages in social care has ‘costs’, including the risk of exploitation of potentially vulnerable workers. The report specifies situations where workers are isolated within the care environment as being more susceptible to exploitation.
Looking forward
between 2021/22 and 2022/23. Here, two sector experts examine the impact.
According to Skills for Care’s report, one of the factors behind the increased number of international recruits entering the sector is the fact that care workers were added to the Shortage Occupation List in February 2022. The decision to include care workers on the Shortage Occupation List was made in December 2021 following the Migration Advisory Committee’s recommendations.
Skills for Care’s report continues to
highlight that the increased number of international recruits entering the sector is also responsible for the increased starters' rate in the independent sector from 32% to 34% in 2022/23. In addition, further information from Skills for Care in the form of its Adult Social Care Workforce Data Set indicates that international recruitment may have contributed to a decrease in the turnover rate in the independent sector in 2022/23 from 32% to 30%, as the turnover rate for international recruits was around half that of people recruited domestically.
Key benefits
The Local Government Association’s Overseas recruitment bite-size guide for social care providers in England outlines several benefits that providers have experienced as a result of overseas recruitment, including loyalty and commitment, access to a future supply chain and increased potential for succession planning.
Sector employers may also be incentivised to recruit internationally to access Government’s recently announced £15m
Analysis from The King’s Fund states that immigration policy should be designed with the social care sector in mind, citing the example that high-salary thresholds as part of a points-based immigration system do not cater to the rate of pay currently being offered by providers who are looking to recruit internationally. Despite this, Government’s response in April 2023 to the Health and Social Care Committee’s Report on Workforce: recruitment, training and retention in health and social care, re-affirmed that it has no plans to reduce the minimum salary requirement for care workers, directly disagreeing with a recommendation from the Committee. Lastly, research from The Migration Observatory at the University of Oxford examined the medium- to long-term implications for the development of policy to improve recruitment and retention in the sector. It argues that workforce shortages do not seem to result from immigration policy, given the number of Health and Care Visas issued in recent years. Rather, that a lack of action on pay and conditions for domestically trained workers is hindering lasting recruitment and retention.
Skills for Care’s The size and structure of the adult social care sector and workforce in England reported an increase of 50,000 internationally recruited direct care providing roles in the independent sectorKarolina Gerlich, Chief Executive Officer, Care Workers’ Charity @CareWorkersFund



70,000 people have been recruited from abroad into direct care-providing roles after adult social care was added to the Shortage Occupation List in February 2022. This is great news for vacancy rates and recruitment, showing that there are people who are willing to come here to work.
It is essential that care workers remain on the Shortage Occupation List and that care providers continue to recruit from abroad. Especially since Brexit, free influx of workers from Europe has stopped. What we must remember is that these people are often coming a long way for a demanding job, so they must be properly supported.
Firstly, the hours promised must be in place as we have heard of care workers on international visas not having enough work. Apart from it being a requirement for their visa, they need the hours to pay for accommodation and food.
Having come from abroad,
many workers do not have family to live with or get support from, so it is essential that basics are met. Being careful about not tying accommodation to employment in an unhealthy way which traps the person, is also critical. I have heard of cases where the modern slavery line was almost crossed because of poor delivery of good intentions.
Supporting the mental wellbeing of international recruits is another consideration. Moving from abroad to a different culture is very straining on mental health (I have personal experience with that). There is a lot to learn – such as language (idioms), behaviours that are expected but do not happen (no afternoon tea everywhere?!), things that were unexpected (regional accents) and more.
To benefit from international recruitment, all providers should offer good pastoral care. This includes language and culture lessons so people feel part of society, not excluded from it.
Fae Mell, Managing Director, Kata Care Solutions Ltdwww.linkedin.com/company/kata-care
The sector is on the cusp of an exciting transformation thanks to the infusion of international talent. This isn't just about the numbers; it's about the multitude of benefits it brings.
Imagine having a wider pool of compassionate and skilled professionals at your service.
International recruitment opens the doors to a vast talent pool, ensuring that care providers can find the right people to fill the ever-growing number of direct care roles.
One of the things we've all heard about is the shortage of skilled workers. International talent is like a ray of sunshine on a cloudy day, bridging that gap and making sure we have enough hands on deck to meet the rising demand for care services.
And don't you just love the idea of ethical recruitment practices? We're not just hiring anyone; we're doing it responsibly and fairly. Our commitment to the World Health Organization's guidelines means we're making sure international recruitment is done with a big heart, caring for
both our sector and the talented professionals joining us.
International talent isn't just about skills; it's about stories, experiences and perspectives from around the world. It's like adding a splash of colour to a canvas. These diverse backgrounds lead to innovation and better care, making each day brighter for those in our care.
Finally, think of this as a delightful collaboration. We're bringing together professionals from different walks of life, creating a symphony of expertise. It's a continuous learning experience. This collaboration is nurturing growth and improvement in our sector.
The surge of international talent in the UK care sector is nothing short of heartwarming. It's bolstering our workforce, ensuring ethical recruitment and infusing diversity and collaboration. Together, we're painting a picture of a future where quality care knows no bounds, and that's something to celebrate with a smile.
It is essential that basics are met
International talent is like a ray of sunshine on a cloudy day
The Care Innovation Challenge: CMM meets the finalists
Hosted by The National Care Forum (NCF), the Care Innovation Challenge 2023 took place on 1st – 2nd July at Coventry University’s TechnoCentre. CMM has caught up with all five Challenge finalists to find out more about their innovative ideas. This month, we concluded our interviews and spoke to Ben Howard from Team Careberry, Belinda McLean from Team Kit and Haoyu of Team Night Safety.
CMM Meets Team Night Safety
CMM: What prompted you to get involved with the challenge and what’s your idea?

Haoyu: I combined my experience of caring for my relatives during COVID-19 (when I was back in China) to come up with a technological system to support caring for people during the night. I wanted to develop a system that did as much work as a human – but reduced the need

for humans to work in care settings. I did a lot of research in Japan about how we can care for elderly people by using technology in care settings to increase efficiency and reduce the requirement for human resources.
CMM: What are some of the key features of the product?
Haoyu: The aim is to produce an integrated system to support smaller providers when they are caring for someone overnight. For example, if a person has several tech products looking after them, such as a motion sensor or a medical device measuring glucose, then this one system will gather all of the information in one central place and hopefully we can use artificial intelligence to summarise this information to help providers. For example, if someone was moving into a different room and had a fall, the piece of technology would alert the caregiver and they can come and provide help. Diseases such as cancer change over time, so the systems can keep monitoring those conditions and see what is going on and can provide some basic judgements.



CMM: Have you considered the cost implications for providers?
Haoyu: We have explored the cost in the market and it’s more expensive than we thought for products such as the sensors. We thought we might look into targeting medical start-ups as a way of reducing the cost. There are still more newcomers on the market, and I think that between ourselves, the care provider and start-ups – there is certainly opportunity for collaboration.
CMM: What do you hope to show the judges at the final?
Haoyu: We hope to show the market size to the judges and have a clear plan on how this product can develop and we hope to share part of the product at the show, to show that this can work in the market, and this can secure a profit.
CMM: How did you find the Challenge weekend overall?
Haoyu: It was a lovely weekend. Even though it was a competition, everyone helped each other and shared ideas. At one point, I was surrounded by five mentors, and everyone was very friendly. I think I definitely learnt more about the care sector as a result of the Challenge weekend.

with other people from different care sectors – as we are only one part of the sector. We wanted to challenge our idea – to see what we can do to improve.
CMM: What is your idea in a nutshell?
Ben: Careberry provides a software that’s an all-in-one toolkit for care providers and we would hope to build our new idea into the system. The idea is ‘smart care cost’ and it’s a fair estimation cost for care and support for individuals – the provider completes some information about the individual being cared for, postcode, how the care is being funded, whether that’s through social services or it’s privately funded, and what the system will do is calculate a fair cost for care. In terms of overhead costs, travel, training etc, it will work with a bunch of different algorithms in the background to show providers how they can reduce costs in that postcode area. It’s for providers to have the oversight to say this is why we need to charge this. We know from experience that as long as you can demonstrate it to the local authority that this is why the costs are needed.
CMM: Have you conducted any market research?
Ben: We want to make it available as a feature, but we are exploring it as its own entity – not just Careberry customers. We plan to offer it to our existing customers and get feedback from them. Because we have our own domiciliary care company and a nursing home, we have access to data and can trial it with our own customers. We have the environment to test in both and have gathered research and information – we have that aspect ready.
CMM: What feedback have you received on your idea?
CMM: How did you find the Challenge weekend overall?
Ben: I got way more out of it than I thought. The mentors blew me away – Ben from the accounting background, he told us a touching story, how he reduced cost but was still able to provide the same level of support. It was great to speak to other participants – it was really fascinating to see how we can put all our brains together and come up with something really revolutionary and that’s what we ended up doing. We started with an idea, and it really wasn’t perfect at all but through the feedback and the mentors talking to us, we made it as perfect as we could. We came with a nugget of an idea and walked away with a gold bar.
We have followed NCF for a long time now; seeing them put so much hard work and effort into getting all of this ready is touching for us. They were all so helpful; it was a really great event, a great day.
CMM: Where would you invest the money if you won?
Ben: The prize money would go straight back into perfecting the algorithms – straight back into the development. At Careberry, we update every two weeks, so we don’t stop development and we don’t plan to stop development any time soon. It’s all onwards and upwards!
CMM Meets Team Careberry
CMM: How did you find out about the Care Innovation Challenge weekend?
Ben: The Managing Director of Careberry has been following the Challenge and during a team meeting, he brought up the idea of competing in the Challenge. We thought we have some good ideas and wanted to connect

Ben: The feedback we got from the mentors was it wasn’t very clear what the idea was – it has the potential but wasn’t clear on how it will work. We spoke to Ben from Marrgo – he was a very good mentor to sit down with and discuss the idea. Once we did the elevator pitch, we discussed about the terminology to make it clearer, and we have been perfecting our pitch to be more precise and clearer about what the benefit is. The issue with other tools is that they aren’t live and not real time – we plan to have it part of our system – it's based off their real-time data – live information. It’s real-time data based on the provider’s own data.
CMM Meets Team Kit
CMM: Why did you and your team colleague Yani decide to get involved in the Challenge?
Belinda: I have worked in the health and social care sector for over 30 years, and I currently work as an Occupational Therapist. I have had many ideas on how we can support people better, across a range of areas ranging from
transportation, moving and handling, to equipment. I had heard about Hackathons – it sounded really exciting and I felt like I could contribute to it in some way.
I met Yani at the event, who is a doctor and that was probably one of the loveliest aspects of taking part – it was a lovely surprise to find a doctor who is not in the social care sector in her everyday but is linking back to the patient's journey – so she understands the importance of the functioning of a good social care sector and was interested in developing a way of getting equipment on discharge from hospital. She was on the same table as our mentor, Ann Taylor from Hilton Nursing Partners.
CMM: What’s your idea?
Belinda: Our idea is all about delivering small items of equipment for people who need it – rather than waiting for an Occupational Therapy assessment. It turns out there is something that has been developed by Millbrook Healthcare. It would only be small items of equipment that could be easily installed by a service user or a family member by a smart triage app or a computer, but Millbrook have done this in partnership with Milton Keynes. We are still at a very early stage of chatting to people to decide if we are going to take it forward. I have spoken to some of my colleagues, people who do community assessment for
equipment and they think there is a gap – so there is definitely a gap for something but it's whether it can be done in such a way that it can be a one-stop-shop set-up. It is complicated to try and pull together.
CMM: How does the current offering work?
Belinda: The Millbrook app does it via a series of questions – the individual in need of care either gets the equipment there and then or waits for the equipment. On the one hand, it could be through linking social care providers or it could be something that could empower the individual to purchase privately. It gives power to the individual drawing on care and ensures that they aren’t at home without equipment to make their life easier and to stay at home for longer.
Anyone can do this assessment. It is to empower people and their family and prevents people going on the OT waiting list and if the assessment is done and they don’t fit the criteria, they do go on the waiting list. We would hope there is willingness from equipment companies to do this at scale.

CMM: How did you find the Challenge weekend?
Belinda: Speaking to Clenton and colleagues at TLAP was really important to hear directly from people who draw on care and support services. Even though the pace was fast at the
Challenge, you understand why because it really encourages people to move quickly and progress with an idea. We’ve got to throw out more ideas and hopefully the one good idea will go forward!

The proof of our idea is that it’s already been done! There is something to do – it’s just whether we join forces and look at what they've done or try and extend it.
CMMFor
the five finalists it all comes down to the next few weeks and the continued mentorship they will receive as they prepare for the final at The Care Show at the Birmingham NEC on 11th and 12th October. Meanwhile, applications have opened for The Care Innovation Challenge 2024! Visit the Care Innovation Hub website: https://careinnovationhub.org.uk/challenge/ and follow #CareInnovationChallenge for ongoing updates and the final reveal of the winning project.Participants unite in a singalong of ‘Thank you for being a friend’ by Tony Christie and Music for Dementia to coincide with BBC Radio 2’s campaign to shine a light on those unsung heroes who
workin
careand
care for their loved ones.Rich Amos, member of Think Local Act Personal (TLAP) and Care Innovation mentor, offers his expert guidance to
participants.

A GENERATION OF CARE:
Gen Z’s role in shaping the future of care
How do we close the vacancy gap in the social care sector and attract young people? Amanda Marques, Business Solutions Director at Cohesion Recruitment, outlines the current barriers when recruiting Gen Z and shares tips to help providers with their recruitment strategies.
We need to look at the future of social care. Current vacancy levels are at 152,000 and the number of filled posts has still not returned to 2020/2021 levels. Adult social care has a higher vacancy rate than the NHS and the economy as a whole and we can see continuous movement between roles due to issues with the cost-of-living crisis. With 18.6% of the UK population over 65, demand will only be heading in one direction – up! How can we close this vacancy gap? The clear and obvious solution is to appeal to the next generation.
To give an overview of the sector, the average age of a person working within adult social care is 45 years old, with 25% of the workforce being over 55 years old and only 10% of the workforce under 24 years old. This is not an insignificant statistic, especially when the workforce is 1.6 million and roles within the social care industry make up
13% of the UK’s jobs, only being beaten by retail and wholesale work. Young people are clearly under-represented in social care. With 11.4% of 16-24-year-olds unemployed in May 2023, the highest unemployment rate of any age group by a significant margin. We therefore need to look at the barriers to working for young people, in general, and with specifics to social care.
Breaking barriers
Illness. It may surprise you to hear but one in four unemployed young people are not working due to ill health, which includes mental health. This has risen from one in 10 not working due to ill health in 2012. Illness is especially prominent in small towns and villages, where social care roles are harder to recruit for. Not only do these periods of absence affect the local economy; but it can often become difficult for people to secure employment following a period of absence. Most people who are unemployed due to ill health remain unemployed for over two years. Mental health conditions are the most common reason for young people to not be working. We need to explore how we can help people and what can be put in place to help those who do have ill health get into and stay in roles.
The after-effects of the pandemic. COVID-19 exacerbated mental health conditions that were already apparent. 67% of people under 25 believed that the pandemic would have a long-term negative effect on people’s mental health. As well as this, we are all aware of the impact that COVID-19 had on people’s education, particularly with regards to learning becoming virtual and the typical school and university experience being disrupted. 83% of young people believed that COVID-19 has had a negative impact on their career prospects. This highlights not only the mental health conditions caused by the pandemic, but the anxiety around finding work.
Lack of understanding. Social care is also, in many cases, not seen as a viable career option for young people, despite the vast opportunities and need for more workers. This begins from school, where we can see a gear towards university. For example, in a Prospects survey, 43% said that a degree has a better reputation. With lower wages and a lack of understanding of the social care sector and what is available, young people are not looking to move into this sector. We need to bridge the gap between young people and social care and find a way to rewrite the narrative.
So, what can the Government do, on a country-wide scale, in order the address the issues?
Better funding. Perhaps one of the biggest suggestions is for better funding and a focus on the disparity of wages between front-line social care workers and healthcare assistants in the NHS. A 41 percentage uplift would be required for this disparity to end, a monetary difference of £8,036. There needs to be a workforce plan for social care and for the sector not to be ignored in favour of the NHS. Care England and the National Care Forum are both working hard to influence the Government to this end. Doing this is the start of helping to stabilise and sustain the current system.
Highlight the pathways. Clearly defined career pathways are also important. Focusing on this will allow young people a better understanding of where a career in care can take them and the ways that they can advance. Showing care to be a lifelong career, especially in an era of uncertainty post pandemic and in the midst of an economic crisis, will be incredibly beneficial. Digitalisation alone presents a huge opportunity to bring young people into a social care setting.
Support school outreach. In order to harness young talent locally, school and college outreach are vitally important for providers. There should be a focus on targeting young people to influence and persuade them earlier that social care is a career of choice. This can be linked in with a Gen Z attraction strategy. Young people want to do a job with social value, and what better job does that than working in social care? Outreach should also focus on interacting with the parents. Parents want to support their children in finding work and work experience. Why not introduce parents to social care as a place where their children can receive this? Flexibility in shifts is critical in attracting young people – with most wanting to work full-time in the summer and part-time while studying. The sector is missing out on positive pass-through of thousands of young people who could be working while studying health and social care or other allied health courses. Support community outreach. Not only should there be a focus on highlighting social care to students and parents, but also to the wider community. For example, we can look at projects such as Care Home Open Week. This year’s Care Home Open Week was record breaking – so many homes got involved. The activities that take place are a great way to have young people join in and understand better what care homes do. Considering how recruitment days can be linked with schemes like this can also be incredibly helpful for attracting young people. The pandemic meant that social care settings had to become closed. Now is the time to throw open the doors!
It is also vital for care providers to explore how they can attract young people, as well as receiving support from the Government.
Learning from the above. While one size does not fit all, using outreach and pathway investigations in whatever ways do work is incredibly important. Use what you know about what Gen Z want from a role – the chance to make a difference, flexibility, to bring their values – and use that to target Gen Z. Young people want to hear from others like them, so do create collateral with them in mind and use existing young workers as ambassadors.
Buddy systems. Providers can explore not only how training is provided but also what support can be offered. As we know that there is a large issue with illness and mental health, looking at the implementation of buddies within workplaces will aid with young people feeling supported.
Understand Gen Z. Care providers need to be prepared for Gen Z to enter their workforce and demonstrate that they are willing to learn from them and understand them. Considering the age of the current social care workforce, the generational difference could cause conflict, so encouraging everyone to learn from each other and for Gen Z to make a positive impact on the places they work, will aid in encouraging and keeping Gen Z within the industry.
Rise to the challenge
If we don’t find a way of engaging with young people to join the social care workforce, then the recruitment and workforce challenges will only get worse. The Government needs to show that it sees social care as as valuable as the NHS. Providers need to show that social care is a valuable industry to be part of. Existing teams and decision-makers also need to flex their ways of working to accommodate and welcome young people. Gen Z are looking for roles that have social value; it’s up to the sector at large to rise to the challenge and make the case to join! CMM
“Use what you know about what Gen Z want froma role – the chance to make a difference, flexibility, to bring their values – and use that to target Gen Z.”
Your go-to solution for health and social care recruitment in the West Midlands, Staffordshire, and South West regions.
At Meridale, we understand the importance of having a reliable and dedicated team of nurses, healthcare assistants, support workers, and social workers in the healthcare industry.

That’s why we have made it our mission to provide exceptional recruitment services to ensure that your healthcare facility is staffed with the best talent available.
Our team of experienced recruiters have a keen eye for identifying top talent in the healthcare industry, and we pride ourselves on our ability to match the right candidate with the right position. Whether you’re looking to fill a permanent role or require temporary staff, we can help.
At Meridale, we take the time to understand your needs, and we work with you to find a solution that fits your budget and meets your requirements. We take care of the entire recruitment process from start to finish, so you can focus on what matters most - providing quality care to your patients. With our extensive network of healthcare professionals, we can quickly and efficiently fill your staffing gaps, ensuring that your facility runs smoothly and that your patients receive the best possible care.
Our staff have the opportunity to manage their work-life through our own user-friendly company app
Choose
info@meridalerecruitingsolutions.co.uk

UK
THE ALTERNATIVE WELLBEING TRAINING PROGRAMME
Eden is a modern model of care enhancing the wellbeing of ALL those involved in the giving and receiving of care. Working in partnership with the team, residents and families to bring meaning, spontaneity, and joy to people’s lives.

Hosted LIVE by Geoffrey Cox and Margot Whittaker RGN BSc, sharing over 20 years experience in social care.
7 week online programme • 1 hour sessions • Weekly workbooks • Non-prescriptive • £100 per person for the 7 week course • 17 hours CPD • Project planning


www.eden-alternative.co.uk enquiries@eden-alternative.co.uk
01626 868192 / 07843 359472

EVERYONE DESERVES GOLD STANDARD CARE AT THE END OF LIFE

The Gold Standard Framework (GSF) charity and a coalition of leading providers is calling on the Government to promote best practice in care for people in their final years of life through improved workforce end of life care training and support. Professor Keri Thomas OBE, Founder and Chair of The GSF Centre CIO, and Julie Armstrong Wilson, Chief Operating Officer of The GSF Centre CIO, share insights on GSF’s training offering and why Government must invest in the workforce.
We believe that everyone deserves gold standard care at the end of their lives and that no one should be left to die without the care, support, and dignity they deserve. We all have a role to play in this, most notably in social care because end of life care is everyone’s business. In our ageing population, dementia is now the leading cause of death, along with frailty and multi-morbidities of old age, and most care for people with dementia is given by care homes and domiciliary care providers. Care professionals therefore have an increasingly vital role to play to ensure that more people receive
quality end of life care. However, despite evidence of the benefit of training the social care workforce, this large and invaluable workforce is often unrecognised and unsupported to provide such vital care for people living out their final years of life.
At The Gold Standards Framework Centre (GSF) charity we are committed to improving care for people in the final years of life in any setting, given by any care provider. We recently celebrated our 25th anniversary as the UK's leading provider of End of Life Care (EOLC) training for generalist front-line staff. GSF’s
Keeping abreast of the key issues in policy and regulation is a challenge for care providers.
Keeping abreast of the key issues in policy and regulation is a challenge for care providers.
Keeping abreast of the key issues in policy and regulation is a challenge for care providers.
At Care England we provide our members with a daily flow of policy news, regulation changes, media updates and more. This gives access to the latest information and advice from one well connected, reliable source. Wouldn’t that save time and worry in your care business too?
At Care England we provide our members with a daily flow of policy news, regulation changes, media updates and more. This gives access to the latest information and advice from one well connected, reliable source. Wouldn’t that save time and worry in your care business too?
At Care England we provide our members with a daily flow of policy news, regulation changes, media updates and more. This gives access to the latest information and advice from one well connected, reliable source. Wouldn’t that save time and worry in your care business too?
To find out more about the benefits of membership, visit www.careengland.org.uk, email info@careengland.org.uk or call 08450 577 677
To find out more about the benefits of membership, visit www.careengland.org.uk, email info@careengland.org.uk or call 08450 577 677.
To find out more about the benefits of membership, visit www.careengland.org.uk, email info@careengland.org.uk or call 08450 577 677

well-recognised EOLC training and accreditation in EOLC particularly focuses on enabling the social care workforce and is the only training programme to have established objective accreditation. Since this was introduced in 2008 thousands of care professionals have completed the process and many care homes are now being accredited for the sixth time, over 18 years since originally trained.
End of life care – a national priority
At our landmark 25th anniversary event, we reflected on things past, present and also future, celebrating a quarter century of success whilst also affirming the huge need for this work in the future. We feel more needs to be done to support our hardworking health and care teams to meet challenges ahead. The importance of our workforce, especially in social care, is often unrecognised by Government; yet modest investment could enhance, empower and upskill the three million front-line health and care workforce (1.2 million NHS and 1.8 million social care) to provide quality care for many more people in their last years of life.
enabling generalist front-line workforce to speak with one voice, known as the Coalition of Frontline Care. It will call on Government to increase resources for training and support for the generalist workforce, who provide the vast majority of hands-on care for people in the last years of life.
Greater Government investment in the health and care workforce could create three areas of positive outcomes – for individuals and families, the workforce and public finances. More people in their final years would receive better quality care, face fewer crisis hospital admissions, and have a better chance of being able to die at home in their own bed, thereby reducing the level of distress for their families. A stronger, more resilient workforce with improved morale and greater job satisfaction would help temper the current workforce crisis. Also, if the health and care systems worked better together it would significantly reduce the number of hospitalisations, saving money, while freeing up access to beds and reducing waiting times – it’s a potential ‘win-win-win’ for everyone.
A third of the NHS budget is spent on people in their last year of life and, if current trends continue, the number of deaths in England and Wales is predicted to rise by 25% by 2040, with home/care home death rates set to almost double2. Without appropriate support this is in danger of reverting to crisis over-hospitalisation and poor-quality home care3. Add to this the fact that 30% of hospital beds are filled with people in the last year of life, many of whom will be among the 80% of care home residents who are in the last year of life and who, on average, will endure three unplanned admissions, almost half of which could be avoided4.
We also commissioned a survey reflecting shifting public trends1. Most respondents said they would prefer to die at home or in a care home, reflecting other national surveys. There was also a concerning lack of public awareness of end of life care, with half those surveyed admitting they had scant knowledge of the care and support available and almost two thirds saying they would appreciate a discussion with professionals about available options. But most significantly, two thirds (67%) of those surveyed backed a call for the Government to provide more resources and training for EOLC as a national priority.
A call to Government
Partnering with Care England and other leading health and social care bodies we developed a coalition of national organisations committed to
Delivering excellence with GSF
There is also clear evidence that more people could be enabled to die at home with better staff training and stronger support5. We know this is possible to achieve, due to the experience of our frontrunner GSF accredited teams of health and social care professionals. Over 25 years, GSF has trained over 5,000 teams, about half a million staff and accredited over 2,000 teams, enabling millions of people to benefit from more proactive, personalised care.
Those teams talk about the transformational effect GSF has had on them and the people they’re caring for. Rekha Govindan, a Registered Manager at Chegworth Nursing Home, Sutton, said, ‘We are grateful to GSF for the structured framework,
>
“There is clear evidence that more people could be enabled to die at home with better staff training and stronger support.”
10 THOUSAND Proud to have supported over
care workers with over
£5.6 MILLION IN GRANTS AND SUPPORT

Support us to help even more

which has enabled Chegworth Nursing Home to be able to provide high-quality palliative care to our residents. We can distinguish between the times before and after our involvement with GSF. We truly believe that GSF has made a big difference in the entire palliative care society.’
GSF is a tried and tested, systematic, evidence-based programme optimising care for people in their final years of life, whatever their condition, wherever they are. GSF teaches the core system-based skills and competencies to teams, including early recognition of decline, enabling open and honest advance care planning conversations, and proactive future planning to enable tailored care. This supports more people to live well before they die and to die well in the place and manner of their choosing. Teams can complete the training either in-person or remotely. While the GSF training is in-depth and robust, it’s also manageable and cost-effective for teams, with the cost of training and accreditation for a whole care home, agency or team equivalent to one to two weeks of a resident’s stay or two nights in hospital.
The investment in training and support for the generalist front-line workforce could enable the provision of proactive, personalised, well-co-ordinated end of life care for millions more. It would complement the increased access to specialist palliative care mandated in the Health and Care Act 2022, improving appropriate referrals to palliative care services. It would reap significant system-wide benefits for all, but notably enhance the social care workforce, often omitted from policy developments, as in NHS England's Long Term Workforce Plan.
Without concerted action by Government to support high-quality end of life care, we risk the under-valuing and depletion of our precious over-stretched health and social care workforce. This in turn will lead to over-hospitalisation causing pressures throughout the health service and reduced access for those acutely unwell patients, as well as delayed discharges and increased waiting times with excessive waste of public resources. But above all, we risk a poor experience of care for individuals in the later stages of their life and their families, and fewer
people being able to die well where they choose.
Strengthening the system
Our workforce is our strength. The social care workforce is committed, motivated and able to meet the challenges of the future if they receive good training, enablement and support. Our challenge now is to alert Government to the need to upskill the front-line workforce, to create a health and care system that works together, to provide better care, ‘gold standard’ care, for all in their final years of life. CMM
Coalition of Frontline Care: Letter and Press Release www.goldstandardsframework.org. uk/coalition-of-frontline-care
25th Anniversary: GSF is celebrating 25 years this year. See our website for more information: www.goldstandardsframework. org.uk/25-years-of-gsf. Here you will be able to view a testimonial video (https:// vimeo.com/835571706), a summary video of the last 25 years of GSF (https://vimeo. com/837596505) and an online event summarising its history, impact showcasing front-line GSF Accredited teams and discussing future EOLC needs with a panel of experts (https://vimeo.com/838992771).
Contact us if you share this vision or would like to know more about GSF. You can email us at info@gsfcentre.co.uk, or visit www.goldstandardsframework.org.uk for more information. You can also search for a GSF Accredited care home near you here: www.goldstandardsframework.org.uk/ accredited-organisations and view GSF International work here: www.gsfinternational.org.uk
GSF Awards Conference: And if you want to know more about the GSF Accreditation Awards on 29th September, visit www.goldstandardsframework.org.uk/ gsf-awards-2023. You can also follow us on X (formally Twitter): @gsfcentre or on LinkedIn.
uk/reports/end%20of%20life-care/
Professor Keri Thomas OBE is the Founder and Chair of The GSF Centre CIO. Email: keri.thomas@gsfcentre.co.uk
CELEBRATING EXCELLENCE IN CREATIVE ARTS
Robert Lamacraft, a chef at St Martins Housing Trust’s Highwater House, won the Creative Arts Awards at the Markel 3rd Sector Care Awards 2023. Here, Dr Jan Sheldon, Chief Executive Officer at St Martins, explains how Robert uses art to engage residents.

Highwater House is a residential service run by Norwich-based homelessness charity St Martins. It is for people who have a dual diagnosis, which means both mental illness and issues with problematic substance use. The 22 people who live at the home have experienced abusive and traumatic events in their lives and are unable to cope with independent living. The approach of St Martins’ team members is to build relationships with the people they support using whatever tools they can to interest and inspire them.
A flexible approach

One of these tools is art. Robert Lamacraft, who has worked at the home for many years as a chef, started an art group and invited residents to join in. He discovered that people didn’t always engage with structured, timetabled activities – perhaps from being

institutionalised when in prison or hospital – it can be too much to ask of someone to commit to being in a certain place at a certain time.
Instead, Robert got the art materials out at the end of his shift, or sometimes in the evenings, and invited people to join in. Some observed from a distance, and gradually became more engaged in the creative process, picking up paintbrushes themselves and talking about what they would like to create.
Inspiring creativity
Studies have shown that expression through art can help people with depression, anxiety and stress, which was the premise for running the activities at Highwater House. The benefits of relaxation were apparent, and one person said, ‘When doing art, my mind closes to my problems and the art flows, like music. I find it a peaceful place when I can create.’
Robert said, ‘Over the time I have run the art group I have listened to the residents talk about their lives, their childhood memories, and the life they have had. They have suffered from terrible amounts of trauma and have addictions. They told me so many interesting stories about their lives. Some good memories that brought a smile to their faces or sad, traumatic events that they had to live through and survived.’
creates a feeling of shared community, and residents point out their individual contributions with pride.
The art project had such a positive impact, thanks to Robert’s dedication, that St Martins’ team members entered Robert into the Creative Arts Award category in the Markel 3rd Sector Care Awards.
Maintaining standards
Some wonderful scenes have been made using all sorts of materials, including paints, printing techniques and slate. An exhibition was held in the home, judged by an independent panel from another service in St Martins.
Working as a team
Repeatedly, residents said they wanted their stories recorded, and to share what had happened to them but didn’t necessarily have the means to articulate it.
With Robert’s guidance, the Highwater House residents embarked on an ambitious piece on a large canvas called ‘Journey of Life’. It resembles stained glass and depicts a timeline of memories. The bottom right of the canvas is the darkest part of the piece, marking the start of their journey of homelessness, addiction and trauma.
Other sections depict happy times, such as holidays, the feeling of safety and favourite foods. The finished piece hangs on the wall at Highwater House and
Winning the award was an honour for Robert, also giving a boost to the residents at Highwater House. A history of homelessness, poor mental health and addiction can strip a person of their sense of self, leaving them feeling unwanted and marginalised. Winning an award like this validates their place in their community and celebrates a positive contribution they have made to something outside of their usual experience.
Highwater House is registered with the Care Quality Commission (CQC) and been rated ‘Outstanding’ since March 2019. The team works hard to maintain the Outstanding rating. In partnership with Norfolk & Suffolk Care Support, St Martins arranges regular meetings for care providers in Norfolk who have achieved an Outstanding rating from CQC. The group supports each other to continually move forward, recognising the importance of not resting on what has already been achieved.
The power of art
The same approach is taken within all the activities at the home, including the art group. Robert is continually thinking up new ideas. The next project is a large canvas exclusively about what makes the residents happy. Another creation in the pipeline is mini canvases that will be painted on an individual
Nominations are now open for the Markel 3rd Sector Care Awards 2024

CMM is delighted to announce that nominations are now open for the Markel 3rd Sector Care Awards 2024.The ceremony will be held on Friday 15th March 2024 at The Grand Hotel, Birmingham. If you would like to nominate a person or team to be considered for an Award, follow the process on CMM’s dedicated web page. Nominations will close on Friday 27th October 2023.

Don't miss your chance to attend the Markel 3rd Sector Care Awards 2024 – early bird tickets are now on sale. You can also stay up to date with the awards on social media. Join the conversation on X (formerly 'Twitter') by following @3rdSectorCare and using the hashtag #3rdSectorCareAwards
The Markel 3rd Sector Care Awards is run specifically for the voluntary care and support sector. Visit www.3rdsectorcareawards.co.uk to view the 2023 event winners and find out more about next year’s event.
basis and displayed all together in a family group. The group is making the most of the warm weather and decorating slates and stones outside in the garden area.
The day-to-day running of the home consistently considers the psychological needs of each resident including their thinking, emotions, personalities and past experiences. It is an approach to support people out of homelessness and social isolation – in particular those who have experienced complex trauma or are diagnosed with a personality disorder. Rather than being an ‘add-on’ or an extra activity, art is an important way for people to express themselves and truly feel they belong somewhere they can call home.
Email: jan.sheldon@stmartinshousing.org.uk
X: @TheSheriffHat @stmartinsnfk
Key dates for your diary
Nominations open:
Friday 1st September 2023.
Nominations close:
Friday 27th October 2023.
Judging day:
Friday 26th January 2024. This will take place online and all finalists must be in attendance.
Awards ceremony:
Friday 15th March 2024.
"Art is an important way for people to express themselves."CMM
AGED CARE ON A GLOBAL SCALE
CMM was delighted to join 650 attendees from 48 countries at the Scottish Event Campus in Glasgow for the 2023 Global Ageing Network’s biennial conference in conjunction with Scottish Care and the National Care Forum (NCF).

The Global Ageing Conference on 7th and 8th September offered an unprecedented opportunity to explore and debate the urgency of sustainability in every aspect of aged care and support, from Government policies, overall ecology and built environments to operations and front-line workforce, and its impact on individuals who live with the experience of care and support. On the agenda for the two-day Global Ageing Conference was the role of technology and AI, human rights, research and new models of care and the role they will play in the future of ageing. Keynote speaker, academic and writer Sir Geoff Mulgan CBE discussed subjects such as preventing loneliness in later life, and enabling people to retain meaning and purpose as they age, as well as how we encourage younger people to contemplate what ageing will mean for them. Headline sponsor, UK Research and Innovation (UKRI)'s Innovation Hub, at the conference was a major attraction in the exhibition hall and UKRI has been a key player in The Healthy Ageing Challenge, which aims to help people remain active, productive, and independent and socially connected across generations for as long as possible.
New awareness day launches
The Global Ageing Network took the opportunity at the conference to announce a new awareness day in recognition of older people – 7th September will now be known
as ‘The Global Older People’s Care and Support Day’. Katie Sloan, Chief Executive of The Global Ageing Network, told CMM, ‘We want governments to look at ageing as an investment and not as an expense – so we really need to reframe our thinking around ageing. Ageing is real; it’s a part of life. What’s good is some countries are beginning to acknowledge it and only then can we see ageism dissipate.’
Closer to home
Joseph Musgrave, Chief Executive of Home and Community Care Ireland (HCCI), told the room that the HCCI had ‘found its voice’ and is now ‘trusted by the Government’. We heard that after 18 months of discussion with the Irish Government, carers are now guaranteed the Minimum Living Wage – 13 Euros and 10 cents an hour. Previously, Irish carers were only guaranteed 9.50 Euros an hour. oseph Musgrave told the conference that ‘unless we have a workforce that is empowered and stable, innovation will never take off.
Global perspectives
Professor Vic Rayner OBE, Chief Executive of The National Care Forum (NCF) and Conference co-host, said, ‘We need to welcome in more perspectives and ideas from the wide-ranging research and innovation that’s taking place around the world and be dynamic and agile enough to implement learnings that can create real change. We also need to change the language we use around older people and remove ageism from our societies as Claudia Mahler said in her keynote address, because ultimately social care for all people, regardless of age, matters to us all.’
Australian aged care
CMM took the opportunity of sitting down with Sue Thomson, Chief Executive of McLean Care in Australia, to find out more about the current challenges impacting on the Australia aged care sector. McLean Care has a revenue base of over 50 million Australian Dollars and has led the way in supporting smaller providers during the cost-of-living crisis by forming an Alliance to buy electricity and medical supplies in bulk – to enable a better cost solution for smaller providers who are struggling to purchase. Remote providers in New South Wales are really struggling from a staffing component. There is a shortage across the acute care sector, disability sector and even doctors and nurses. ‘There has got to be some sort of solution,’ Thomson says. ‘It is nowhere near the degree that third world countries are experiencing but there are definitely health inequalities in the remote space, so McLean Care is designing a virtual ward solution that can put clinicians at the bedside.’
Visit www.caremanagementmatters.co.uk/ aged-care-on-a-global-stage/ to read the full write-up of the event. CMM
WHAT’S ON?
Event:
Date/Location: Contact:
Event: Date/Location: Contact:
Event:
Date/Location: Contact:
What the Digital Future Holds for Social Care Providers
3rd October 2023, Brighton and Hove
www.eventbrite.co.uk/e/what-the-digitalfuture-holds-for-social-care-providerstickets-684875369667
Community Care Live
10th-11th October 2023, London
www.communitycarelive.co.uk
Digital Health and Care Congress (The King’s Fund)
11th October 2023, London
www.eventbrite.co.uk/e/digital-health-and-carecongress-2023-in-person-conference-registration598009872627?aff=ebdssbdestsearch
Event:
Date/Location: Contact:
Event:
Date/Location: Contact:
Event:
Date/Location: Contact:
The Care Show Birmingham
11-12th October 2023, Birmingham
www.careshow.co.uk
The Integrating Health and Social Care Conference South 2023
19th October 2023, London
www.convenzis.co.uk/events/the-integratinghealth-and-social-care-conference-2023
Recruiting for Values in Adult Social Care
24th October 2023, Winchester
www.eventbrite.co.uk/e/recruiting-for-values-inadults-social-care-tickets-540966032967

CMM EVENTS
Event:
Date/Location: Contact:
Event:
Date/Location: Contact:
The Yorkshire and The Humber Care Association Alliance (YHCAA) Conference
18th October 2023, Doncaster
www.caremanagementmatters.co.uk/events/
CMM Insight Online – In association with the National Care Forum (NCF)

19th October 2023, Virtual Lisa Werthmann, Director 01223 207770
lisa.werthmann@carechoices.co.uk
www.caremanagementmatters.co.uk/webinar
Please mention CMM when booking your place. Sign up online to receive discounts to CMM events and for more information on our upcoming events in 2023.
www.caremanagementmatters.co.uk
@CMM_Magazine #CMMInsight
STRAIGHT TALK
Naz Dossa, Chief Executive of Peoplesafe and BSIA Chair of the Lone Working Group, shares insights from a landmark study highlighting personal safety concerns within the healthcare sector and discusses how care providers can improve employee safety.

Everyone deserves to feel safe in the workplace but, for many, that’s sadly not the case. Alarmingly, a landmark study conducted into perceptions of personal safety at work found that 6.8 million employees worry about their safety on a weekly basis. Disturbingly, many employers underestimate the level of concern, or are unaware of it completely.
In the healthcare sector specifically, one in four employees worry about their safety at least once every week. And, while safety concerns are rife across all industries, health and care workers are 94% more likely to worry about their safety than those in white-collar jobs.
59% of health and care workers are concerned about the dangers of entering the home of a member of the public, a common social care job requirement that poses additional risk.
Only very recently, two companies were fined a combined total of more than £400,000 after staff working at a South Wales mental health hospital were subjected to violent attacks by patients over a three-year period.
HSE Principal Inspector, Anne Marie Orrells, has pointed out that care providers should have adequate arrangements to effectively plan and organise preventative measures to prevent violence towards staff and other patients.
But is that happening across the board?
The reality is that public-facing industries such as healthcare are facing increased aggression from frustrated and angry patients and their families. 74% of health and care workers, including doctors, nurses, carers, and
social workers, are concerned about aggressive behaviour from patients, while 44% say they have received verbal or physical abuse from a member of the public.
This growing sense of feeling, and being, unsafe is naturally having a negative impact on job satisfaction. Results show that those who experience a negative work-related event are less satisfied in every aspect of their role, not just pay but also career development, wellbeing and safety. It’s simple, if people don’t feel safe, they aren’t happy – it’s a basic need, a human right if you will.
So, employers are also feeling the impact. Unsurprisingly, negative experiences involving safety issues often contribute to decisions to leave a job. In fact, one in four have left a job due to a safety concern in the last five years. This is bad news for businesses and policy makers across the UK currently facing a recruitment and retention challenge in many front-line care roles.
Reviewing safety concerns and putting solutions in place to improve protection increases job satisfaction, employer brand and staff retention. We need to shift the dial on the importance of social care employee personal safety by supporting owners and operators to act in the best way possible and we’re calling on employers and the Government to work together.
The 1974 Health and Safety at Work Act made it a minimum legal requirement for employers to actively protect the health, safety and welfare of their staff. This legislation was further bolstered by The Management of Health and Safety at Work
Regulations Act of 1999, which requires employers to carry out assessments to mitigate any health and safety risks.
The reasonableness of a protective measure can be determined by considering the potential risk of harm to the employee compared to the cost and practicality of putting the safety measure in place.
Compliant employers follow the rules. But it’s the smartest employers that take the extra step, realising that healthy, happy, motivated, and focused staff who feel safe and appreciated can improve overall business performance. They understand that achieving this may require going beyond existing basic compliance.
Working with an increasing number of businesses across all work sectors, including social care, who are taking action to protect their employees both in and out of the workplace, 24/7, Crimestoppers has partnered with Peoplesafe, to encourage people to ‘Step Up. Stay Safe.’ – calling on all UK employers to act.
Some care providers already have, and are going beyond, the basic legal duty of care to provide reassurance to employees in and outside of working hours. It’s just one way to demonstrate a desire and willingness to support their wellbeing. But only by providing greater protection and peace of mind through recognised standards across the board, do I believe we can make a genuine difference.
Find out how you can step up to keep your staff safer at https://crimestoppers-uk.org/ news-campaigns/campaigns/step-up-stay-safe