Executive Summary
Carilion Clinic is committed to joining with our partners to pursue the essential work of improving and maintaining the health of the Roanoke Valley in accordance with our mission. Periodically assessing the health concerns of each community is a key component of addressing community needs Every three years, the Roanoke Valley Community Health Assessment (RVCHA) aims to uncover issues, indicate where improvement is needed and track and promote progress in key areas so that there is demonstrated, ongoing change. The CHA process and the public availability of its findings enable and empower our community to effectively improve and maintain health.
Carilion, Healthy Roanoke Valley (HRV) and the Roanoke City and Alleghany Health Districts (RCAHD) collaborated to conduct the 2024 RVCHA alongside additional community partners, all of whom comprise the Community Health Assessment Team (CHAT) After review and discussion of the data collected, the 2024 RVCHA led the CHAT to identify six priority health issues in the community.
Community Health Improvement Process
Carilion believes in continuous quality improvement. The triennial CHA serves as a formal way of identifying community needs and developing plans to address them It shapes the ways we support our mission in the community and encourages collaboration and alignment with clinical teams Not only does this process identify current needs and disparities, but also helps to ensure we are regularly evaluating and shifting to meet emerging needs

Priority Health Needs
In collaboration with the CHAT, we identify key health needs to align resources and other efforts for the following three years. The CHAT reviews extensive data, asks questions and participates in a consensus-building prioritization process. The 2024 RVCHA resulted in the following health priorities: Chronic Disease Overweight/Obesity Heart Disease Hypertension



Drivers of Priority Health Needs
The CHA process focused on prioritizing health conditions and outcomes, rather than a broader focus on their root causes. We recognize that access to healthcare and other services and the social determinants of health (SDOH) are key facilitators of good health and well-being. As such, we focused on those and other health factors as a strategic component of action planning. The key drivers of each priority health condition, as identified by the CHAT, are discussed in the corresponding sections of this report.
Board Adoption
This document was approved by the CMC Board of Directors on September 17, 2024, and formally adopted as the 2024 Roanoke Valley Community Health Assessment.
Disclaimers
This document has been produced to benefit the community. Carilion encourages the use of this report for planning purposes and is interested in learning of its utilization. Comments and questions are welcome and can be submitted to Carilion at communityoutreach@carilionclinic.org
Members of the leadership team reviewed all documents prior to publication. Every effort has been made to ensure the accuracy of the information presented in this report; however, accuracy cannot be guaranteed. Members of the Roanoke Valley CHAT cannot accept responsibility for any consequences that result from the use of any information presented in this report.
Carilion began conducting CHAs prior to the IRS adoption of the 501(r)(3) standard which requires not-for-profit hospitals to conduct a Community Health Needs Assessment (CHNA) every three years. While meeting the CHNA requirement, Carilion maintains the longstanding formal name Community Health Assessment for our process and reports. A crosswalk of this document based on the 501(r)(3) standards can be found in Appendix A.
Our Partners
Community Health Assessment Leadership Team
The CHA Leadership Team collaborates to guide major functions of the CHA including CHAT recruitment, data collection/analysis and shaping meeting structure. In addition to Carilion staff, membership includes leadership from the local health districts and the regional health coalition, Healthy Roanoke Valley. Carilion organizes and facilitates leadership team meetings.
• Carilion Clinic:
o Shirley Holland, Vice President, Community Health and Development
o Molly Roberts, Manager, Community Benefit
o Ashley Hash, Community Health Improvement Program Manager
o Holly Ostby, Community Health Improvement Program Manager
o Nicholas (Nick) Bilbro, Community Benefit Analyst
• Roanoke City and Alleghany Health Districts:
o Dr. Cynthia Morrow, Health Director
o Kristin Adkins, Population Health Manager
• Healthy Roanoke Valley
o Leslie Clark, Director, Family Health Strategies, United Way of Roanoke Valley
Community Health Assessment Team
The CHAT is a dynamic group of health and human service agency leaders, individuals/organizations serving/representing the interests of priority populations and local representatives from various community sectors. The following community partner organizations participated in the 2024 RVCHA:
Adult Care Center of the Roanoke Valley
Disability Services/ SDOH-Focused Organization
Black Father Family Community Leaders
Blue Blaze Consulting Grant Writing
Botetourt County Library Library
Bradley Free Clinic Healthcare
Carilion Clinic Healthcare
CHIP of Roanoke Valley Maternal and Child Health
City of Roanoke Local Government
Commonwealth Catholic Charities
Council of Community Services
Craig County Public Schools
Refugee Population
Homeless Services
Local School System
Craig County Local Government
Family Service of Roanoke Valley Mental Health
Feeding Southwest Virginia Food Access
Financial Empowerment Center Finance
Organization Name
FREE Foundation
Freedom First Credit Union
Goodwill Industries of the Valley
Habitat for Humanity Roanoke Valley
HCA LewisGale Medical Center
Healthy Homes Roanoke
Huddle Up Moms
Local Environmental Agriculture Project (LEAP)
Leffel Consulting Group, LLC
Legal Aid Society of Roanoke Valley
New Horizons Healthcare
Presbyterian Community Center
Radford University Carilion
Rescue Mission
Restoration Housing
Roanoke City & Alleghany Health Districts
Roanoke City Fire-EMS
Roanoke City Public Libraries
Roanoke City Public Schools
Roanoke Redevelopment and Housing Authority
Roanoke Regional Chamber of Commerce
Roanoke Valley-Alleghany Regional Commission
Roanoke Valley Collective Response
Salem Public Schools
United Way of Roanoke Valley
Virginia Harm Reduction Coalition
Organization Type
SDOH-Focused Organization
Mission-Focused Partner/Business
SDOH-Focused Organization
Affordable Housing
Healthcare
Housing
Maternal and Child Health
Food Access
Community Leaders
Legal Aid
FQHC
SDOH- Focused Organization
Higher Education
Homeless Services
Affordable Housing
Public Health
Public Safety
Library
Local School System
Housing
Chamber of Commerce
Economic Development
Mental Health and Substance Use
Local School System
United Way
Harm Reduction
To see a list of specific 2024 CHAT participants, please see Appendix B.
Data Team
Additional data support was provided by the Virginia Department of Health Division of Population Health Data.
• Khristina Morgan, Community Health Epidemiology Regional Coordinator
• LeeAnn Gardner, Community Health Epidemiologist, Central Shenandoah Health District
• Taiwo Ilechie, Community Health Epidemiologist, Roanoke City and Alleghany Health Districts
Our Process
The first step in the ongoing community health improvement process is to conduct a CHA. Every three years, Carilion follows the formal process described below to identify community needs and develop plans to address them. The 2024 RVCHA officially began on October 2, 2023 with a data presentation and concluded with the final CHAT meeting on June 10, 2024
STEP 1: Define Community Served
Carilion Roanoke Memorial Hospital (CRMH) and Carilion Roanoke Community Hospital, collectively referred to as Carilion Medical Center (CMC), are located in Roanoke, Virginia. CRMH includes a Level 1 Trauma Center, a Neonatal Intensive Care Unit, Carilion Children’s Hospital and 718 patient beds. Offering a wide range of inpatient and outpatient care, specialty care such as the Institute for Orthopaedics and Neurosciences and the Cardiovascular Institute, medical education and fellowships, CRMH was ranked as tied for the third best hospital in the state by U.S. News and World Report.1 Additionally, Carilion Roanoke Community Hospital houses a highly skilled inpatient rehabilitation unit.
The service areas for Carilion’s CHAs are determined by unique patient origin of the hospital in each respective market. Focus is placed on areas that are considered Medically Underserved Areas (MUAs) and Health Professional Shortage Areas (HPSAs).
In fiscal year 2023, CMC served 123,461 unique patients. Patient origin data revealed that during this year, 84.3% of patients served by CMC lived in the following localities:
• Roanoke City (29.5%)
• Roanoke County (22.9%)
• Franklin County (10%)
• Botetourt County (8.2%)
• Salem (6.9%)
• Bedford County (6%)
• Craig County (0.8%)

These localities make up the service area for the 2024 RVCHA, excluding Franklin County, which is also served by Carilion Franklin Memorial Hospital (CFMH) in Rocky Mount, Virginia. CFMH also conducted its own CHA of Franklin and Henry counties concurrently. Franklin County secondary data are included so that complete data for the Metropolitan Statistical Area (MSA) will be available in this report. Please note that while Bedford County is
1 https://www.carilionclinic.org/locations/carilion-roanoke-memorial-hospital
included in the service area, it is not part of the Roanoke MSA. Carilion participates in the Bedford County CHA conducted by our neighboring health system, Centra.
Additional Community Demographics
The Roanoke MSA, commonly known as the Roanoke Valley, includes the cities of Roanoke and Salem and the counties of Botetourt, Craig, Franklin and Roanoke. The Valley is nestled among the Blue Ridge Mountains with the City of Roanoke at its heart. Roanoke is a destination place, rich in cultural diversity, the arts, shopping, recreational opportunities, natural beauty and services not available in more rural areas of the region.
In addition to Carilion, key safety net providers in the region include the Veterans Administration Medical Center, a federally qualified health center, free clinics, local offices of the VDH and other service organizations. Despite these entities’ presence, thousands of low-income, uninsured and underinsured residents do not have sufficient access to affordable healthcare services.
The localities within the service area have significant disparities in size, population and social determinants of health. The Weldon Cooper Center for Public Service predicts positive population change by 2040 for all communities except Craig County, which may have very slight population loss.2
Table 1. Select Demographics of the RVCHA Service Area
Source: US Census Bureau, ACS, 2018-2022.
2 https://www.coopercenter.org/virginia-population-projections
Table 2. Income Data for the RVCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Specific to Carilion Medical Center inpatients and outpatients in fiscal year 2023, 23.43% received Medicaid while 4.39% were self-pay, a proxy for uninsured.3
Table 3. Insurance Status of RVCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Roanoke City, the urban hub of the service area, is more racially and ethnically diverse than the rest of the MSA. All localities are below the state average for the percentage of the population identifying as Hispanic or Latino, with the highest percentage (6.9%) in Roanoke City.
3 Strata internal data
Table 4. Racial Demographics, RVCHA Service Area
Source: US Census Bureau, ACS, 2018-2022
Roanoke City is uniquely segregated, divided into quadrants (Northwest, Northeast, Southwest and Southeast) separated geographically by railroad tracks, the Roanoke River and Interstate 581. These quadrants vary significantly in the demographic and economic make-up of their residents. Two of the quadrants Northwest and Southeast have federal designations as Medically Underserved Areas (MUAs). These areas are home to a large proportion of the lowincome individuals and families in the city who may be uninsured, underinsured or are Medicaid recipients facing additional barriers due to cultural differences. MUAs are also present in Bedford County, Botetourt County, Craig County and Franklin County.4
Target Population
The target population for Carilion Clinic’s CHA projects consists of underserved/vulnerable populations disproportionately impacted by the social determinants of health, including poverty, race/ethnicity, age, education, access and/or lack of insurance. Data are reviewed where available by different life stages, including parents of children and adolescents, women of childbearing age, adults and the elderly. Other considerations include race, ethnicity and income levels. All patients are included in this assessment regardless of insurance payments or financial assistance eligibility. Distinct efforts are taken to ensure the CHA reflects those residing in Medically Underserved Areas and Health Professional Shortage Areas
STEP 2: Convene Community Health Assessment Team (CHAT)
A 70-member CHAT participated in the assessment activities Hearing voices from across our service area is crucial to the success of a CHA. Broad-interest community reach is a main qualification when inviting individuals to join the CHAT. In addition to the HRV Steering Committee, we also invited representatives from the RCAHD, local governments, the local school system, social service organizations, other community organizers and nonprofit leaders.
4 https://data.hrsa.gov/tools/shortage-area
The CHAT met four times throughout the process, with each meeting serving a distinct purpose.
• Meeting 1: Introduction and Overview of the Process; Launch of Community Health and Well-Being Survey
• Meeting 2: Data Presentation and Data Walk
• Meeting 3: Prioritization of Needs and Discussion
• Meeting 4: Action Planning: Key Drivers and Impact/Feasibility Activity
Each meeting built on the one prior and fostered dialogue amongst CHAT members. Meetings were held in person with interactive opportunities to participate and engage with data and facilitated discussions with other CHAT members.
The RCAHD team was engaged from the beginning of the planning process (spring of 2023) throughout the assessment period and CHAT meetings. RCAHD’s involvement helped shape all aspects of this assessment. The team identified community partners to serve on the CHAT, provided discussion points and suggestions on structure of CHAT meetings and offered feedback on the prioritized needs. Additionally, RCAHD representatives were active on the CHAT and participated in all CHAT activities including the Stakeholder Listening Session and the prioritization activity.
In addition to RCAHD, the CHAT included other individuals or organizations serving or representing the community’s medically underserved, low-income and minority populations. Examples include:
• Free clinics (e.g., Bradley Free Clinic, Fralin Free Clinic)
• Federally Qualified Health Centers (e.g., New Horizons Healthcare)
• Public school systems (e.g., Roanoke City Public Schools)
• Community-based social support organizations (e.g., Presbyterian Community Center, Legal Aid Society of the Roanoke Valley, Feeding Southwest Virginia, Blue Ridge Literacy)
• The United Way of Roanoke Valley
These organizations and individuals helped gather community input by distributing the Community Health Survey. CHAT member input was solicited through the Stakeholder Survey and Focus Group. Combined, these efforts led to the identification and prioritization of community health needs.
STEP 3: Collect and Review Relevant Health Data
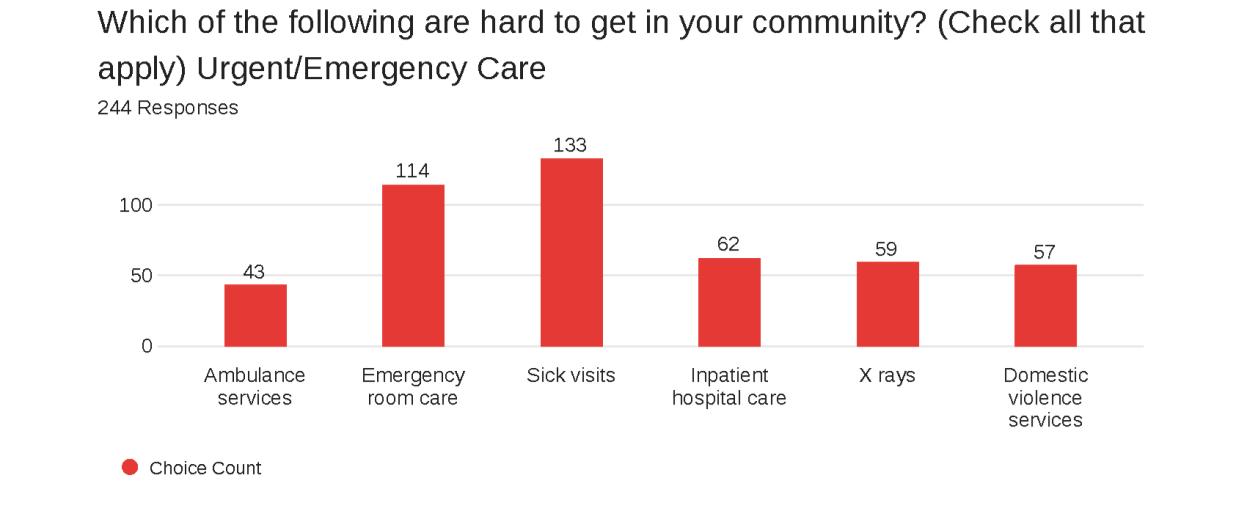
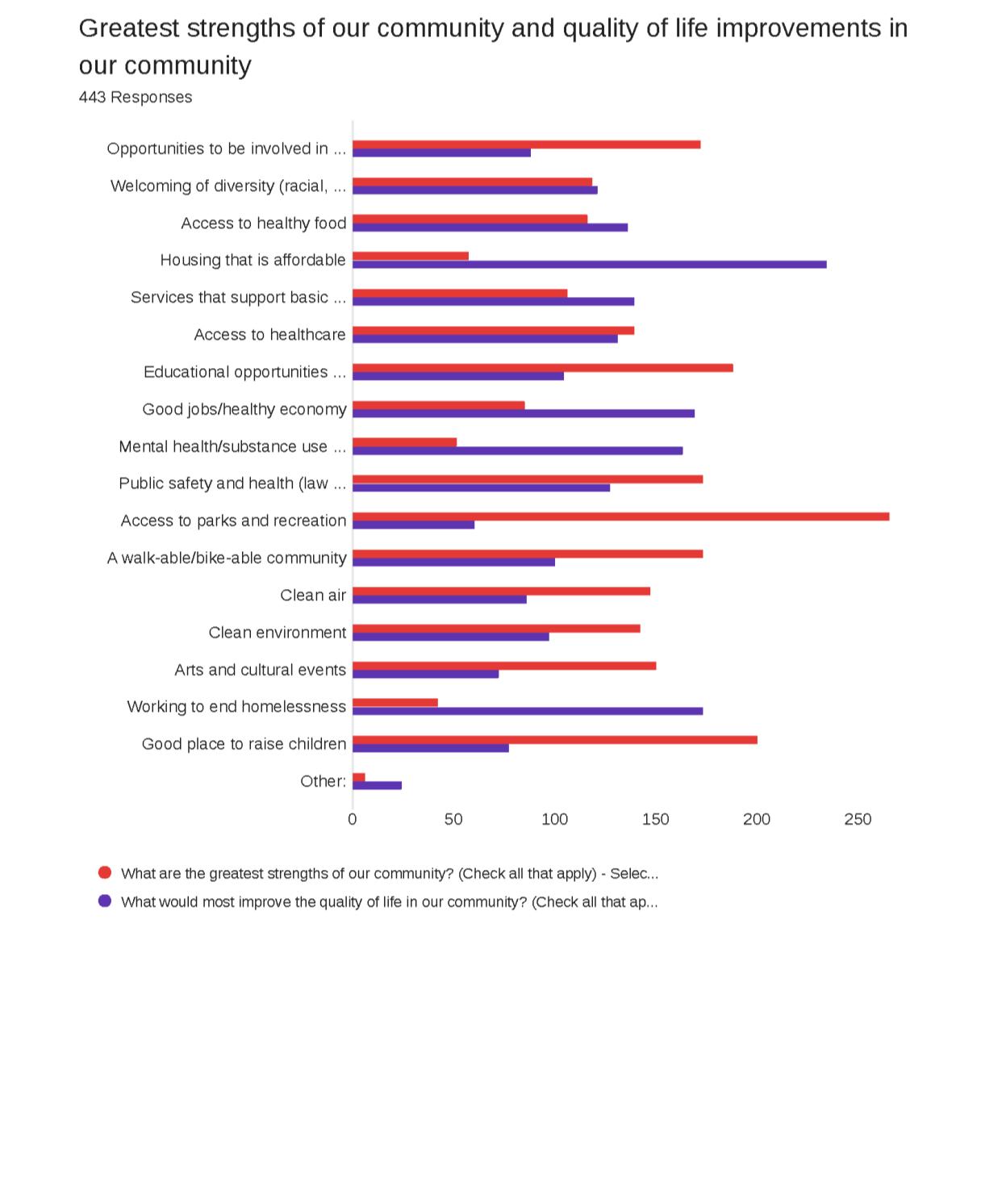
Various data were collected and shared with the CHAT regularly, including primary and secondary data on health outcomes, health status, socioeconomic factors and quality of life. Secondary data served as a key driver of the process, with primary data adding community context and perspectives to understand the needs of subpopulations within the community.
Community Health and Well-Being Survey
A Community Health and Well-Being Survey was conducted as part of the RVCHA. This survey was used to evaluate the health of the community and identify potential geographic areas to target improvements. Input and oversight of survey development was provided by the CHAT and the CHA leadership team
A 27-question survey instrument was developed and asked questions about access to care and other services, health status, community strengths, quality of life, subjective well-being and
demographics (Appendix C: Community Health and Well-Being Survey). The survey instrument included commonly used questions and metrics from the following established community surveys:
• Cantril’s Ladder
• Community Themes and Strengths Assessments, National Association of County and City Health Officials (NACCHO), Mobilizing for Action through Planning and Partnerships (MAPP)
• Community Healthy Living Index, YMCA
• Behavioral Risk Factor Surveillance System, CDC
• National Health Interview Survey, CDC
• Youth Risk Behavior Surveillance System, CDC
• Martin County Community Health Assessment, Martin County, North Carolina
• Previous Roanoke Valley Community Health Surveys
The population of interest for the survey was Roanoke Valley residents 18 years of age and older. Surveys were distributed from October 2023 through December 2023. A drawing for a $50 grocery store gift card was offered as an incentive for those completing the survey.
The following subpopulations were especially targeted for sampling:
• Underserved/vulnerable populations disproportionately impacted by the social determinants of health, including:
o Poverty
o Race/ethnicity
o Education
o Lack of insurance
A non-probability sample method was used, where respondents were not randomly selected. Although the survey was available to all residents living in the Roanoke Valley, oversampling of the targeted subpopulations occurred through specific outreach efforts through community partners. Oversampling ensured that needs and assets specific to this subpopulation of interest were captured.
The survey instrument was available in both English and Spanish via the following methods:
• Qualtrics link and QR code
• Phone line (888-964-6620)
• Paper surveys (collected by volunteers and/or staff of partner agencies)
Outreach strategies for survey distribution included:
• Media coverage by the local television and newspaper announcing the URL for the survey
• Facebook, including geographically targeted advertisements
• Flyers and posters distributed throughout the community with survey URL and phone line information
• Survey URL posted on partner agency websites
• Recruitment of participants on site at CHAT member organizations
In total, 547 surveys were collected and validated. Full survey results and validation methodology can be found in Appendix D
All responses were entered into Qualtrics by survey respondents or, in the case of surveys completed on paper, by Carilion staff. Surveys were analyzed and reported using Qualtrics and Microsoft Excel
Stakeholder Listening Sessions and Survey
CHAT members were invited to provide an additional perspective on the needs and barriers to health facing our community during an HRV all-partner meeting that also included other community stakeholders. Carilion staff from across the organization facilitated small group discussions. To quantify focus group data, participants were asked to complete the Stakeholder Survey. A summary of the data can be found in Appendix E.
Community stakeholders, leaders and providers were encouraged to complete the Stakeholder Survey after participating in a listening session. The online survey was shared at the CHAT meetings and via email. Surveys were analyzed and reported using Qualtrics and Microsoft Excel.
Community Listening Sessions
Community members were invited to participate in Community Listening Sessions to collect qualitative data to further understand health-related needs. RCAHD facilitated sessions with clients of the Virginia Harm Reduction Coalition and students at Virginia Western Community College. Attendees of a Black Father Family Fireside Chat also had the opportunity to provide their input. A summary of the data can be found in Appendix E.
Secondary Data
Secondary data came from two primary sources: SparkMap and the Virginia Department of Health (VDH) Division of Population Health Data. SparkMap is a product from the University of Missouri that quickly and accurately aggregates data across geographies for 80+ indicators from publicly available sources such as the American Community Survey, County Health Rankings and the CDC. Secondary data analysis was provided through SparkMap’s tables, maps and visual diagrams depicting indicators that are better or worse than the state average, trends over time and comparisons across different population segments such as race and life cycle.
A team of VDH epidemiology staff provided and analyzed data from specific VDH departments which was a critical component of the data walk. Data provided included mortality due to specific chronic diseases, incidence rates of sexually transmitted infections, sociodemographic data, cancer rates and others. VDH was also able to provide data broken down by gender and race/ethnicity for many health topics.
Table 5. Data Sharing Summary
STEP 4: Prioritize Community Health Needs
Using their community knowledge, data collectively reviewed and additional data requested and shared, CHAT members were asked to complete an electronic survey to prioritize community health needs. The community health needs included for prioritization were specific health conditions or health outcomes reflecting those conditions which contribute to morbidity and mortality in the service area. The prioritization survey matched the structure utilized during the data walk at CHAT Meeting 2. This resulted in the identification of 13 community health needs.
During CHAT Meeting 3, CHAT members completed a dot voting activity to further refine the priority list, and a discussion ensued to determine the final prioritized need based on scope of issue, burden on community and feasibility to address at the community level based on CHAT member perspectives and perceptions Appendix F summarizes the prioritization activity, including the results of each exercise component.
The 2021 RVCHA and the subsequent Implementation Strategy were posted publicly though multiple electronic channels and shared widely by community partners. An email address was provided for submission of written comments, but none were received for consideration in the identification and prioritization of health needs.
STEP 5: Strategic Planning to Address Priority Health Needs
The final CHAT meeting served as a springboard into both hospital and community action planning. The prioritized needs were again reviewed and a two-part activity ensued. CHAT members identified key drivers of the prioritized health outcomes/conditions using the Robert Wood Johnson County Health Rankings framework as reference. Following the identification of drivers, an impact and feasibility analysis was completed in small groups to help identify leading strategies for community change.
Our Impact: Evaluation of Actions Taken in Response to 2021 RVCHA
The prioritized needs established in the 2021 RVCHA fell into four categories: mental health, socioeconomic factors, primary care and COVID-19. Key strategies included health education, grant funding to address SDOH, establishing the LIFT Center at Fallon Park Elementary School, a community health worker intervention and support for the efforts of community partners in addressing community needs, both directly and indirectly. Below is a snapshot of outcomes from these efforts through June 30, 2024.


Our Priority: Health Equity
Carilion is part of a growing movement of health system stewards committed to unlocking our community’s potential to thrive. We, along with key partners, strive to identify and address health and socioeconomic factors that impact our communities’ health and well-being. We know that where you live is an important contributing factor of health status and outcomes. We are committed to advancing a culture of health where policies, systems, education, research and resources align for optimal health status.
Our mission calls for us to meaningfully address health inequities and disparities. Equity is a key lens for the CHA process, guiding our actions as we seek to understand community health needs. As we move forward into developing community heath improvement strategies, we will remain focused on identifying and serving those who need it most, seeking to broaden the potential for everyone across our communities to thrive.
The Area Deprivation Index (ADI), a tool developed by the University of Wisconsin-Madison, sheds light on what are considered disadvantaged areas of the community based on census block groups (neighborhoods).5 This granular data helps emphasize the importance of conditions that shape our daily lives. The image below shows the extreme variation seen across the service area in ADI scores and illustrates challenges experienced in the most rural locations. Data used in creating the index includes factors for income, education, employment and housing quality some of the key social determinant factors that influence health outcomes.


5 https://www.neighborhoodatlas.medicine.wisc.edu/
Figure 1. RVCHA Area Deprivation Index Map
As we work to improve health equity across our region, our guiding principles include improving access to care and addressing SDOH. This assessment focuses on those principles in the context of specific prioritized health outcomes. To expect a shift in health outcomes, we must focus on improving the underlying factors that lead to them seen in the figure below in a coordinated manner. We will be addressing specific SDOH needs as aligned with the CHA focus areas.
Figure 2. Social Determinants of Health

Figure source: Institute for Clinical Systems Improvement; Going Beyond Clinical Walls: Solving complex Problems, 2014. Graphic designed by ProMedica and shared by the American Hospital Association.

Our Priority: Addressing Chronic Disease
Our prioritization process resulted in the elevation of three specific chronic diseases for focus: overweight/obesity, heart disease and hypertension. The following data indicates potential areas for opportunities.
Data shows need
• Residents of the service area have a higher-than-average occurrence of:
o Physically unhealthy days
o Obesity
o Heart disease
• Health disparities exist in Roanoke City census tracts with high incidence of hypertension
Why This Matters
Community indicates need
• Concern for overweight/obesity and high blood pressure indicated through community survey
• Stress, a contributing factor of chronic disease, was also identified as a concern through the community survey
According to the Institute for Health Metrics and Evaluation (IHME), high body-mass index (BMI), high blood pressure and dietary risks are within the top 10 risks driving death and disability. In other words, these are some of the key impacts on overall health, well-being and life expectancy.6 Additionally, chronic diseases are a leading driver of healthcare costs.7
Data below shows physically unhealthy days and obesity across all service area localities as reported by the CDC’s Behavioral Risk Factor Surveillance System (BRFSS). In both metrics, Roanoke City leads the service area as the highest, followed by Franklin and Craig Counties This shows the challenges both within the urban community of Roanoke City and the more rural surrounding counties.
Figure 3. Physically Unhealthy Days

6 United States | Institute for Health Metrics and Evaluation (healthdata.org)
7 https://www.cdc.gov/chronic-disease/about/index.html

High blood pressure is another indicator reported on through BRFSS. When reviewing by census tract, key differences are apparent in Roanoke City, with Northwest Roanoke City census tracts disproportionately affected in comparison to other parts of the City and the service area at-large.
Figure 5 High Blood Pressure



Figure 4. Adults With Obesity
Key Drivers
Community partners identified many key drivers of these chronic diseases, including access to healthy foods, education of prevention and disease management, culture/readiness to change and the impact of stress and trauma According to the CDC, many preventable chronic diseases are caused by the same behaviors, which include smoking, poor nutrition, lack of physical activity and excessive alcohol use. By adopting strategies to influence these behaviors, we can ultimately impact multiple diseases with efficiency.
Resources Available
There are many resources available in Roanoke to address the prioritized chronic diseases and their key drivers. A full resource list is available in Appendix G. Key resources to address chronic diseases in the Roanoke Valley include:
• Prevention education and chronic disease management programming through local healthcare providers
• Safety net clinics
• Community organizations working to improve access to healthy foods and physical activity
• Community health worker programs, connecting people to healthcare and social support services

Our Priority: Addressing Mental Health and Substance Use
Our prioritization process resulted in the elevation of mental health challenges, substance use and overdoses as focus areas. The following data indicates potential areas for opportunities.
Data shows need
• Compared to Virginia’s average, residents of the service area have a higher occurrence of depressive disorder
• Overdose deaths vary; high need in some localities
• Higher occurrence of mentally unhealthy days than physically unhealthy days
Why This Matters
Community indicates need
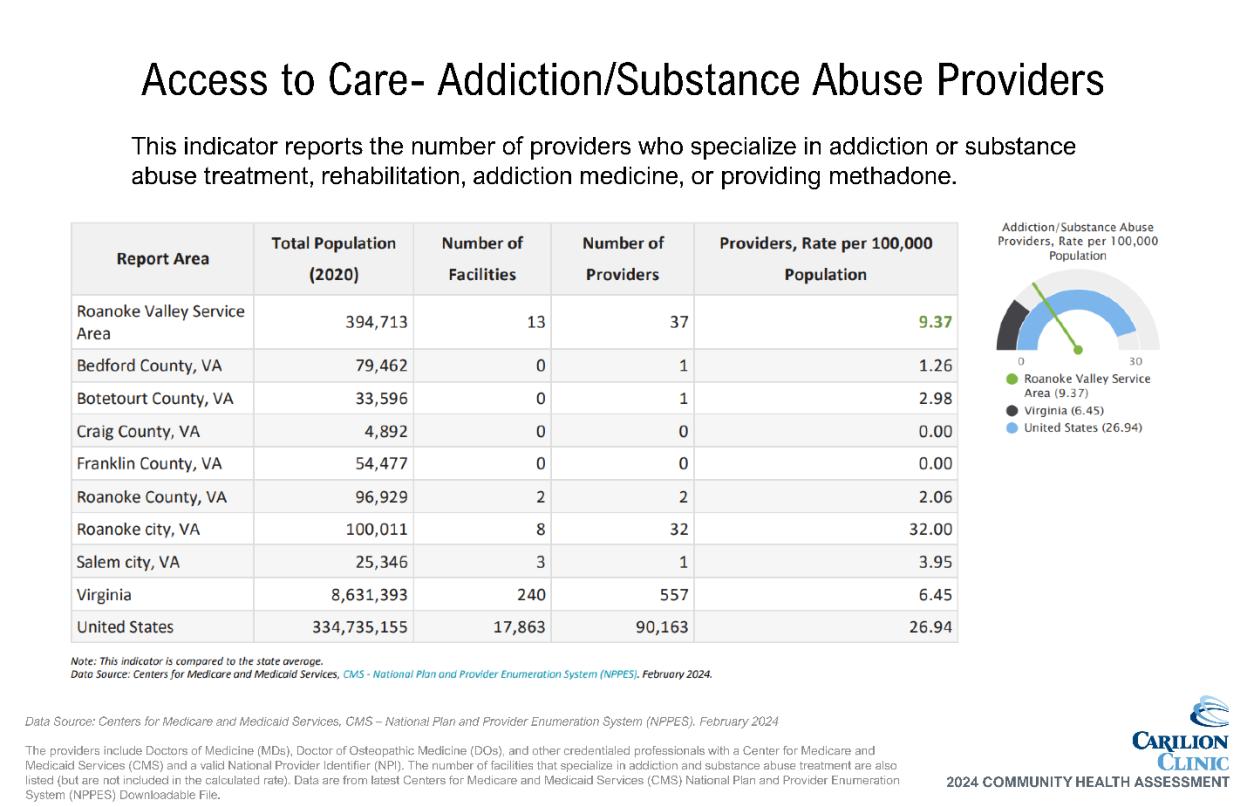
• Concern for access to mental health counseling and outpatient substance use treatment indicated through community survey
According to IHME research, drug use disorders are the number two cause of death and disability in the United States. Depressive disorders and anxiety disorders, both mental health challenges, are ranged at fifth and eighth, respectively.8 All of these health conditions have been worsening in recent years, especially in relation to the impacts of the COVID-19 pandemic
Adults with depressive disorder and cigarette smoking are both reported through BRFSS for the service area localities. All are higher than Virginia’s average, with Craig County experiencing highest rates of depressive disorder and Roanoke City highest rates of cigarette smoking
Figure 6. Adults with Depressive Disorder

8 United States | Institute for Health Metrics and Evaluation (healthdata.org)
Figure 7. Cigarette Smoking Prevalence

Overdose deaths are particularly high in Franklin and Roanoke Counties, Salem and Roanoke City. The Roanoke City rate is over twice that of Virginia overall. No data is available for Craig County due to small population sizes.
8. Deaths From Overdose

Key Drivers
Community partners identified many key drivers of substance use, including poverty, trauma, mental health challenges and cultural acceptance. Identified drivers of mental health challenges included trauma, the home environment, financial circumstances and housing instability. Mental health and substance use are intertwined. Both areas can benefit from some of the same strategies, especially related to prevention. However, there are key differences in effective
Figure
strategies with individuals who are actively experiencing challenges in those topic areas, which allows for all community partners to have a role in the work to address them.
Resources Available
There are many resources available in Roanoke to address mental health and substance use, and their key drivers. A full resource list is available in Appendix G. Key resources to address mental health and substance use in the Roanoke Valley include:
• Public and private mental healthcare providers
• Psychiatric services
• Inpatient and outpatient substance use treatment
• Peer recovery specialists

Our Priority: Addressing Interpersonal Violence
Our prioritization process resulted in the elevation of interpersonal violence as a focus area. The following data indicates potential areas for opportunities
Data shows need
• Deaths from firearms are higher than average in most localities
• Deaths from assault are higher than average in Roanoke City
Why This Matters
Community indicates need
• Concern for neighborhood safety indicated through community survey
The American Public Health Association issued a policy brief in 2018 recommending that violence be deemed a public health crisis 9 Since that time, data shows that violence in our communities has increased. Violence as defined by the policy brief refers to “the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or a community, which either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment, or deprivation.” This encompasses a wide range of challenges including child maltreatment, elder maltreatment, intimate partner violence, bullying and broader community violence.
The impact of violence is far-reaching and includes not only the directly affected individual, but also those who are exposed indirectly and the community at-large. Gun violence, for example, continues to be an issue of national concern and negatively impacts entire groups of people in addition to direct victims. While all localities except for Craig County have a higher rate of firearm deaths than the Virginia average, the rate for Roanoke City is nearly twice the average. Disparities exist within gun violence injuries in Roanoke City, with a disproportionate impact on young Black males. Deaths from assault (or homicide) are too few to report in all localities except for Roanoke City, which has a rate of nearly three times the Virginia average.
9 https://apha.org/policies-and-advocacy/public-health-policy-statements/policydatabase/2019/01/28/violence-is-a-public-health-issue


Key Drivers
Community partners identified many key drivers of interpersonal violence, including lack of accountability, mental health and substance use challenges, lack of family/social support, lack of community connection, trauma and unhealthy relationships. Interpersonal violence can be very closely related to both SDOH and mental health and substance use challenges, further emphasizing the importance of cross-cutting strategies to address multiple health priorities.
Figure 9. Firearm Deaths
Figure 10. Assault Deaths
Resources Available
There are many resources available in Roanoke to address interpersonal violence and its key drivers. A full resource list is available in Appendix G. Key resources to address interpersonal violence in the Roanoke Valley include:
• Local social services and law enforcement departments
• Shelters for families affected by violence
• Gun buyback events and gun lock distribution
• Safe Kids Southwest Virginia coalition
Next Steps
Carilion Medical Center Health Improvement Strategy
Carilion will continue to work with partners and develop a Community Health Improvement Plan for the Roanoke Valley, with expected completion before the end of calendar year 2024. Key focus areas will include not only the priority health outcomes, but also cross-cutting ways to address those outcomes by improving access to care and addressing SDOH.
Carilion also participates in a planning process with Healthy Roanoke Valley, leading to the development of a community-wide strategic plan to address health needs in conjunction with hospital-specific strategics. This community-wide plan will be reviewed and updated regularly with partners to reflect completed and ongoing initiatives and emerging needs.
Appendices
Assess the health needs of the community.
those needs.
Health needs include requisites for improvement of maintenance of health status in the community at large.
Health Needs Include requisites for improvement of maintenance of health status in particular parts of the community.
Identify resources potentially available to address them.
Solicit and take into account input from persons representing the broad interests of the community, including those with special knowledge of public health.
Include all of the following sources to Identify and prioritize significant health needs and identify potentially available resources:
of medically underserved, low-income, and minorities in community served, or individuals/organizations serving or representing them.
Document the CHNA in a written report that is adopted for the hospital facility by an authorized body. Definition of community served and how this was determined. 7-10
Description of process and methods used to conduct the CHNA. 7-14
F
F
501R Requirement Page
Description of how broad-interested community input was solicited and taken into account. 10-14
Description of the process and criteria used to identify needs as significant. 14, Appendix F
Prioritize the significant needs. Appendix F
Description of resources potentially available to address identified significant health needs. 20, 23, 26, Appendix G
Evaluation of impact of actions taken to address previous CHNA-identified significant health needs. 15
Describe the data and other information used in the assessment. 18-26; Appendix H
Describe the method of collecting and analyzing this data and information. 7-14
Identify any CHNA- related collaborative or contracted parties n/a
Describe how Carilion takes into account input received from persons representing broad interests of the community:
Input provided. 5-6,10-14
How and over what time period input provided. 5-6, 10-14
Name, nature, and extent of organizations providing input. Appendix B
Describe medically underserved, low-income, or minority populations being represented by those providing input. Appendix B Adopted by Board 3
Appendix B: CHAT List
First
Name Last name Organization Type Organization Name
Kristin Adkins Public Health Roanoke City & Alleghany Health Districts
Corey Allder Education Roanoke City Public Schools
Elizabeth Arthur Education Salem City Public Schools
Zenith Barrett SDOH Goodwill
Ryan Bell Community leaders Black Father Family
Maureen Best Food Access LEAP
Nick Bilbro Healthcare Carilion Clinic
Aaron Boush Healthcare Carilion Clinic
Guy Byrd Disability Services Adult Care Center of the Roanoke Valley
Jim Cady Community Leader Craig County
Lee Clark Homelessness Rescue Mission
Leslie Clark United Way United Way of Roanoke Valley
Danny Clawson Harm Reduction Harm Reduction Coalition
Mandy Cribb Local Government City of Roanoke
Kim Cromer Healthcare HCA LewisGale
Matthew Crookshank Local Government Roanoke City Human Services
Donna Davis SDOH Goodwill
Daniel Driver Local Government City of Roanoke
Helen Ferguson Housing Healthy Homes Roanoke
Anne Marie Green Homelessness Council of Community Services
Frederick Gusler Housing Roanoke Redevelopment & Housing Authority
Keevie Hairston Healthcare Carilion Clinic
Rachel Hale Public Safety Roanoke Fire-EMS/City of Roanoke
Robin Hamiln Healthcare-Carilion Carilion Family Practice Roanoke Salem
Elizabeth Hart Healthcare HCA LewisGale
Hunter Hartley Legal Aid Legal Aid Society of Roanoke Valley
Krae Heath Faith Community Presbyterian Community Center
First
Name Last name Organization Type Organization Name
Linda Hentshel Mental Health Family Service of Roanoke Valley
Shirley Holland Healthcare Carilion Clinic
Jeremy Holmes Economic Development
Roanoke Valley-Alleghany Regional Commission
Rachel Hopkins Maternal & Child Health CHIP of Roanoke Valley
Stephanie Hackett United Way United Way of Roanoke Valley
Pam Irvine Food Access
Feeding Southwest Virginia
Jill Jeter Education Roanoke City Public Schools
Sallie Beth Johnson Higher Education Radford University Carilion
Wayne King Public Safety Roanoke County Fire and Rescue
Bilge Kolosine Refugee Population Commonwealth Catholic Charities
Beth Leffel Community leaders Leffel Consulting Group, LLC
Aziza Longi Local Government Roanoke City - Intern
Samara Lott Public Health Roanoke City & Alleghany Health Districts
Amber Lowery Library
Don Mankie Food Access
Roanoke City Public Libraries
Feeding Southwest Virginia
Brandon Meginley Finance Financial Empowerment Center
Pam Milkowski Homelessness Rescue Mission
Annie Morgan United Way United Way of Roanoke Valley
Khristina Morgan Public Health
Cynthia Morrow Public Health
Roanoke City & Alleghany Health Districts
Roanoke City & Alleghany Health Districts
Cheryl Mosley United Way United Way of Roanoke Valley
Robert Natt Mental Health Collective Response
David Nova Grant writing Blue Blaze Consulting
Jaclyn Nunziato Maternal & Child Health Carilion Clinic/Huddle Up Moms
Holly Ostby Healthcare Carilion Clinic
Julie Phillips Library Botetourt County Library
Dave Prosser Mission-focused Partners/Businesses Freedom First Credit Union
First Name Last name Organization Type Organization Name
Robin Ramsey SDOH/DME Access FREE Foundation
Mona Raza Legal Aid Legal Aid Society
Molly Roberts Healthcare Carilion Clinic
Kelly Sandridge Education Roanoke City Public Schools
Kayla Scott Healthcare Lewis Gale Medical Center
Caitlin Sharkey Healthcare Bradley Free Clinic
Eric Sichau Economic Development Roanoke Regional Chamber of Commerce
Kori Silence Local Government Roanoke City - Intern
Alexandra Smith Legal Aid Legal Aid Society of Roanoke Valley
Jonathan Stewart FQHC New Horizons Healthcare
Isable Thornton Housing Restoration Housing
Andrew Tressler Faith Community Carilion Clinic - Chaplain
Gerri VanDyke Education Craig County Public Schools
Nicole Wert Public Health VDH
Hope White Public Health Roanoke City & Alleghany Health Districts
Autumn Williams Maternal & Child Health CHIP of Roanoke Valley
Betty Wolfe Housing Habitat for Humanity Roanoke Valley
Appendix C: Community Health and Well-Being Survey





Appendix D: Survey Results and Validation Methodology
Due to the nature of the Community Health and Well-Being Survey and its public availability through online methods, data validation was necessary. To validate survey responses, data was filtered by zip codes within Carilion’s entire service area. These responses were used for further data analysis.
























Appendix E: Qualitative Data Results


















Appendix F: Prioritization Table
Activity Prioritization Survey Dot Voting Activity
Method Using their community knowledge, data collectively reviewed, and additional data shared, CHAT members were asked to complete an electronic survey to prioritize community health topics:
• The survey matched the structure utilized during the data walk at CHAT Meeting 2
• First prioritized broad categories, then specific topics within those categories
• CHAT facilitators ranked the following to develop results:
o Broad categories (resulting top 3 indicated by bold type below)
o Topics within each of the 3 top broad categories
o Remainin g topics
• Results include:
o Top 3 topics of
Using the results of the Prioritization Survey, the group was asked to individually choose 5 topics to prioritize:
• The CHAT facilitators hung pages around the meeting room, each with one of the topics from the Prioritization Survey results.
• Each CHAT meeting attendee was given 5 dot stickers and instructed to place one sticker on each of the 5 topics they felt were most important to address in the next three years.
• After voting was completed, the CHAT facilitators quickly tallied and ranked the results.
• The CHAT was presented with the top 5-7 topics, unranked. The number of results presented depended on any ties and how closely votes were distributed. If topics were additional (i.e. not in the true top 56), CHAT facilitators noted this to the group
Group Discussion
The group was asked to reflect on the results of the dot voting exercise. The following points were made during that discussion:
• Mental Health vs. Substance Use vs. Overdose
o Poor mental health should be considered separately from Substance Use
o Differences between problematic substance use and nonproblematic/saf e substance use
o Generally, group agreed that when thinking of substance use, that typically means SUD in our minds
• Areas are so interrelated, thinking more broadly and then connecting back together may be helpful
• Also need to consider different people affected and how that is represented in the dataage group, health disparities, etc.
Activity Prioritization Survey Dot Voting Activity
each of the top 3 broad categories
o Top 4 topics of the remaining categories and separated them visually on the screen.
Results * Mental Health/Substance Use
• Substance use
• Poor mental health
• Overdoses
Chronic Disease
• Overweight/ obesity
• Diabetes
• Heart disease
Injury/Violence
• Domestic violence/intimate partner violence
• Motor vehicle crashes
• Firearm injuries/deaths
Maternal/Child Health & Infectious/Communicable Disease
• Teen pregnancy
• Infant mortality
• STIs
• Hepatitis C
Top 7:
• Substance use
• Poor mental health
• Overdoses
• Overweight/obesit y
• Heart disease
• Firearm injuries/deaths
• Domestic violence/intimate partner violence
Group Discussion
Top 5:
• Mental Health
• Substance Use (including overdoses)
• Violence (Interpersonal Violence)
• Obesity
• Heart disease/Hypertension
Include strategies specific to (but not limited to):
-maternal health
-environmental health
*Results are not presented in any ranked order.
Appendix G: Resources to Address Prioritized Needs
The following organizations have been identified in the community that address the prioritized needs. Additional community resources are available, but the included list was considered representative of the primary organizations addressing each topic area at the time of this report’s publication.
Appendix H: Data Packets
The following pages include secondary data shared with the CHAT as well as chronic disease hospitalization data accessed through the Virginia Hospital and Healthcare Association (VHHA) Analytics data portal.
Among many data points, Roanoke City is worse than the rest of the service area. Many things may contribute to this, one of those being that Roanoke City is the urban hub of the region.
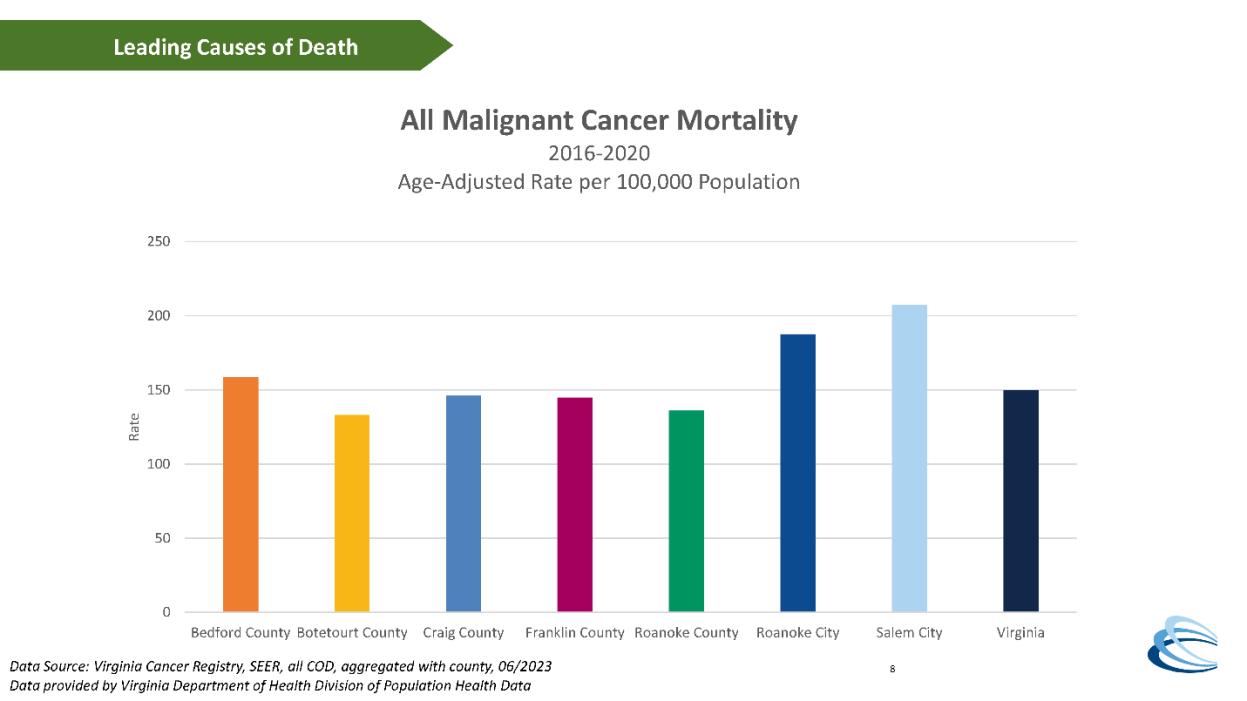
Leading causes of death (2018-2021); generalized across service area
1. Diseases of the heart
2. Malignant neoplasms
3. COVID-19
4. Accidents (unintentional injuries)
5. Cerebrovascular diseases
Mental Health/Substance Use
• Overdose deaths higher than state average across all localities; Roanoke City much higher than other localities
Maternal/Child Health
• Teen birth rates are extremely high in Roanoke City, but relatively low in all other localities.
Injury/Violence
• Firearm injury is an issue in Roanoke City, while less so in other localities.
Infectious/Communicable Disease
• STIs (chlamydia, gonorrhea, syphilis) much higher in Roanoke City than in other localities, and well above the state rates.
• Rate of new diagnosis of hepatitis C infection seems to be on a decreasing trend
Chronic Disease
• Chronic diseases are generally higher across region than Virginia average, though differences are relatively small (just a few percentage points)
• Roanoke City, Craig County, and Franklin County tend to be more consistently on the higher end and particularly with stroke, COPD, and general poor health
• Coronary heart disease is higher than VA average in all localities and highest for Craig and Franklin Counties