Diversity and Inclusion in the Workplace (Healthcare) Part 2



Organizations must ensure benefits and opportunities that exist, be offered to all their employees. No one should be left behind or excluded due to differences, whatever they may be.
Promoting ideas of social justice, equal rights, and fairness across the organization and for all employees is one way to accomplish this. All concepts and measures relating to inclusivity must be actively sponsored and encouraged. All forms of discrimination, racism, and exclusivity must be removed for the benefit of the organization and the employees.
One way to promote social justice, equal rights, and opportunities is to promote inclusivity in all its forms and aspects. But what is inclusivity, and how can it promote social justice and equal rights and opportunities for all? What are the benefits, if ever, if society practices and promotes it? Finally, what aspects of society are in dire need of inclusivity? There are two types of inclusion: regular or partial inclusion and the other is full inclusion. This metaphor explains the subgroups: Inclusion is like Pregnancy: you either are or are not. There is no such thing as partially pregnant, so one cannot be partially inclusive.
Promoting inclusivity is easier in theory than in practice, for biases abound against the marginalized, minorities, women, and people of different genders and mental and physical disabilities. They have been victims of the patriarchal society, majority, the powerful, and the dominant classes throughout history.
Think about the idea of inclusive design, whether we are talking about preplanned communities, products, applications, or even fashion, we must think of others, namely, those who are frequently ignored, and not considered.
Some clothing designs have a tag that designate ‘one size fits all’ meaning it can be worn by anybody without regard to their body habits. Tools and other devices should be available for use, user friendly and operable by anyone1 .
Designs must also cater to specific needs, sensibilities, desires, and specific values. Designs for urban planning and buildings, for instance, must consider the needs of everyone. Specific examples are pathways designed for the elderly and persons with disabilities and comfort rooms tailored explicitly for those belonging to different genders1 .
But let us belabor what should be obvious. In planning for inclusive design, the contributions of those who belong to protected classes, minorities, and the like must be solicited. In designing clothing, for instance, the opinions of the minorities could be solicited to account for their sensibilities. Opinions of women and those of different genders must also be considered and given weight, especially if designing for them. This is the deciding factor in what creates awareness of differences and makes people cognizant of the existence3
Volume 13│Issue 3│Fall/Winter 2022 Carilion Clinic Roanoke Campus
Continued on page 3
Pam Lindsey, MSN, RN - Magnet Program Director & Monica Coles, DNP, APRN, MEDSURG - BC, ACNS-BC, CDP - Gerontology Clinical Nurse Specialist
ARTICLES/NOTIFICATIONS
Carilion
Reviewers
Nancy Altice, DNP, RN, CCNS, ACNS-BC
Desiree Beasley, MSN, RN, CCNS, CCRN-K
Sarah Browning, DNP, RN-BC
Charles Bullins, DNP, RN, AGACNP-BC
Sarah Dooley, MPH, BSN, RN
Cindy W. Hodges, MSN, RN-BC, FCN
James Ingrassia, MSN, RN
Pam Lindsey, MSN, RN
Laura Reiter, DNP, RN, CCRN, CNRN
1 Diversity and Inclusion in the Workplace (Healthcare), Part 2
CDP 5 Pre-procedure Preparation for Gastrostomy Tube Placement
RN-BC, CMSRN, ACNS-BC 7 Fingernail Polish and Infection Control
MSN, RN, CCNS, CCRN-K 10 Vaping - Is It Safer Than Smoking? Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS
13 Carilion Foundation - Nursing Scholarship Awarded 14 Recognitions 20 Carilion Nursing Editorial Board Information 21 Conference Corner 22 SHINE Awards 25 Virtual Journal Club Information 26 Citations and Recognitions 27 Carilion Nursing Research Classes - 2023 Schedule 28 See Where Our Nurses Have Presented Their Work 29 External Conference Information
Pam Lindsey, MSN, RN; Monica Coles, DNP, APRN, MEDSURG-BC, ACNS-BC,
Cindy Ward, DNP,
Amy Lucas,
RECOGNITION/EVENTS
Nursing Research Editorial
Editor
in
Chief
Board: Chris Fish-Huson, PhD, RN, CNE -
-
-
Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC Page 2 Within REACH
This submission is meant to build on the previous article wherein inclusion was noted to be instrumental in the representation of how well an organization establishes a culture that demonstrates respect for every member of the workforce. It promotes a welcoming atmosphere, motivates employees to perform at their highest level and fosters an inclusive work environment that empowers people to be their authentic selves6 .
An inclusive workplace is defined as a work environment that makes every employee feel valued while also acknowledging their differences and how these differences contribute to the organization’s culture and business outcomes. An inclusive workplace is characterized by affirmative action, wherein any impact of bias, discrimination, or unequal opportunity is negated2 An inclusive workforce: celebrates diversity, weaves it into the organizational fabric, and does not pretend that the playing field is level or that all enjoy equal footing. They instead acknowledge differences and systemic differentiation and take responsibility for ensuring equal opportunity for all. Many organizations lose momentum by not ensuring employees feel included.
An inclusive workforce is one where everyone receives the same treatment. In 2019, a survey found that three in five U.S. employees had experienced or witnessed discrimination based on age, race, gender, or sexual identity at work2. Other studies conducted in 2018 found that companies in the top quartile for racial and ethnic diversity are 35% more likely to have financial returns above their industry medians5. And those with gender diversity are 21% more likely to have better returns5. In addition, organizations who are more diverse and inclusive can experience stronger business performance across several areas, including: creativity, productivity, employee retention, skills, and cultural insights5 .
Building a culturally diverse and inclusive workforce is not just the right thing to do, it’s good for business; it gives the organization a positive review, brings a wealth of different perspectives to the table, and encourages growth within6. Awareness of the business case for inclusion and diversity is on the rise6. While social justice typically is the initial impetus behind these efforts, organizations have increasingly begun to regard inclusion and diversity as a source of competitive advantage, and specifically as a key enabler of growth6. Yet progress on diversification initiatives has been slow, and organizations are still uncertain about how they can most effectively use diversity and inclusion to support their growth and value-creation goals6 Inclusion is a concept. There are eight building blocks that make up the foundation of inclusion and can be used individually or organizationally1:
1. Employees share opinions openly with others when they feel like they have a voice.
2. Feeling like one is part of an environment that knows and values them, provides a sense of belonging.
3. A company that cares about an individual’s strength and experiences makes them feel unique among their peers.
4. Employees that feel heard and appreciated have a greater sense of value and satisfaction.
5. Giving employees access to learning and development opportunities demonstrates caring about their ideas, aspirations, and growth.
6. Break down silos by encouraging a collaborative environment regardless of role or department
Page 3 Practical Applications of Nursing Inquiry
(Continued from page 1) Continued on next page
7. Support from managers, diversity, or affinity groups gives employees access to resources that help them understand their organization’s commitment to their wellbeing and growth.
8. Explaining why an inclusive workplace is important helps leaders, managers, and employees align strategically.
Organizational leaders must be the prime movers of inclusivity and set an example. By actively promoting inclusivity through words and deeds, they can take the lead4 These are only some areas where an organization can advance the cause of inclusivity. It is not exhaustive and as much as possible, inclusivity must be promoted everywhere to ensure that discrimination and exclusion become outdated1 .
The zest for greater inclusivity within our organization is only part of the overall fight for social justice, equal rights, and opportunities for all of us. It does not mean, though, that it is far less significant. If ever, victory in the fight for inclusivity will indicate whether the organization will have more successes or more setbacks in the fight for equality.
What is next for our organization?
Remember: Inviting someone to the dance is diversity, asking them to dance is inclusion!
References
1. (2017). Inclusion Research POV. Limeade. Retrieved November 1, 2022, from https:// www.limeade.com/wp-content/uploads/2021/06/Inclusion-POV.pdf
2. (2019). Increasing Investment in Diversity & Inclusion: Evidence from the Growing Job Market. Glassdoor. Retrieved November 1, 2022, from https://www.glassdoor.com/research/
3. Bersin by Deloitte. (2017). High-impact diversity and inclusion: Maturity model and top findings.
4. Bourke, J. Garr, S., van Berkel, A., & Wong, J. (2017). Diversity and inclusion: The reality gap. Retrieved November 1, 2022 from Center for Talent Innovation website: https:// www2.deloitte.com/insights/us/en/focus/human-capital-trends/2017/diversity-and-inclusion-atthe-workplace.html

5. Hunt, V., Yee, L., Prince, S., & Dixon-Fyle, S. (2018). Delivering through diversity. Retrieved November 1, 2022 from McKinsey & Company website https://www.mckinsey.com/businessfunctions/ organization/our-insights/delivering-through-diversity
6. Sherbin, L., & Rashid, R. (2017). Diversity doesn’t stick without inclusion. Harvard Business Review.
Page 4 Within REACH
Pre-Procedure Preparation for Gastrostomy Tube Placement
Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC - CRMH Clinical Nurse Specialist
Gastrostomy tubes are placed for those patients unable to take nutrition orally. Gastrostomy tubes may be placed surgically, endoscopically, or radiologically. Surgical placement may be done laparoscopically or as an open procedure. Endoscopic placement is generally less expensive and takes less time. Radiologic placement is done with fluoroscopic or CT guidance and requires that the stomach be insufflated with air1,2. No difference in morbidity or mortality has been found between surgical gastrostomy and percutaneous endoscopic gastrostomy1,3,4. A practice question arose regarding pre-procedure preparation/fasting for gastrostomy placement. The purpose of this review is to identify best practice related to fasting prior to gastrostomy tube placement.
When to Use Gastrostomy Tubes
Gastrostomy tubes are recommended for medium or long-term enteral feeding. Patients receiving feedings via gastrostomy may have less occurrences of missed feedings and increased weight gain compared to those receiving feeding via nasogastric tube5. More permanent feeding tubes should be considered if feeding is expected to be needed for longer than four weeks2,6,7,8
Search Strategy
Resources searched included UpToDate, Health and Education Research Online (HERO), American College of Gastroenterology, American Gastroenterological Association, American Society for Gastrointestinal Endoscopy, World Gastroenterology Organization, British Society of Gastroenterology, North American Society for Pediatric Gastroenterology, Hepatology & Nutrition, European Society of Gastrointestinal Endoscopy, Society of Interventional Radiology, American Society of Anesthesiologists, American College of Surgeons, Royal College of Surgeons of England, and the National Institute for Health Care and Excellence. The search term used was pre-procedure preparation for PEG placement. A total of 18 articles or guidelines were reviewed with 14 included in this review. Three of the articles found were systematic reviews of descriptive or qualitative studies. The other 11 were literature reviews or clinical practice guidelines.
Pre-procedure Fasting
There is no universally accepted standard for pre-procedure fasting9. The American Society of Anesthesiologists recommend the following guidelines for patients having procedures requiring general anesthesia, regional anesthesia, or procedural sedation and analgesia: clear liquids up to two hours before procedures; light meal, nonhuman milk, or infant formula up to six hours before procedures; additional fasting time of eight hours or more for meals with fried foods, fatty foods, or meat10,11,12. The Society of Interventional Radiology also recommends allowing clear liquids up to two hours before the procedure.
When to Begin Tube Feeding
Tube feeding may begin four hours or less post-procedure5,6,13. Early initiation of feeding following gastrostomy tube placement may potentially decrease hospital length of stay by achieving tube feeding goal rates earlier8. The European Society for Paediatric Gastroenterology, Hepatology, and Nutrition recommends initiating feeding as early as three hours post-procedure in stable children with no complications14 .
Implications for Practice
When preparing a patient for gastrostomy tube placement, the provider typically orders the patient to remain fasting after midnight regardless of the procedure time, and to keep the patient fasting after the procedure until the following morning before resuming or starting tube feeding. Based on the evidence found in this review, tube feeding could be continued up until six hours prior to the
Page 5 Practical Applications of Nursing Inquiry
gastrostomy tube placement and feedings resumed four hours after placement. This would improve patient outcomes, resulting in less time without nutrition and could result in earlier achievement of goal tube feeding rate and decreased length of stay.

Resources
1. DeLegge MH. Gastrostomy tubes: Placement and routine care. UpToDate. 2022. Retrieved October 12, 2022 from https://www.uptodate.com/contents/gastrostomy-tubes-placement-and-routine-care?search=peg% 20placement&source=search_result&selectedTitle=1~89&usage_type=default&display_rank=1#H59179605
2. Long S, Fernando D, Boyd C, Katrivesis J, Park H. Interventional techniques to support enteral nutrition. Dig Dis Interv. 2022; 6(1), 52 – 60. doi: 10.1055/s-0042-1742295
3. Herb J, Rodriguez-Ormaza N, Cunningham C, Bartl N, Jadi J, Charles A, Reid T. Gastrostomy tube outcomes among surgical and non-surgical services: A retrospective review. Am Sur. 2021 Advance online publication. Doi: 10.1177/00031348211047173
4. Varone A, Stephen A, Kheirbek T, Adams C, Cioffi W. Outcomes of PEG placement by acute care surgeons compared to those placed by gastroenterology. Surg Endosc. 2022. Advance online publication. doi: 10.1007/ s00464-002-09262-2
5. Boullata JI, Carrera AL, Harvey L, et al. ASPEN Safe Practices for Enteral Nutrition Therapy Task Force. ASPEN Safe Practices for Enteral Nutrition Therapy. J Parenter Enteral Nutr. 2017; 41(1), 15-103. doi:10.1177/0148607116673053
6. NICE. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. CG32. 2017. https://www.nice.org.uk/guidance/cg32/chapter/1-Guidance#enteral-tube-feeding-in-hospital-and-thecommunity
7. Rajan A, Wangrattanapranee P, Kessler J, Kidambi TD, Tabibian JH. Gastrostomy tubes: Fundamentals, periprocedural considerations, and best practices. World J Gastrointest Surg. 2022; 14(4), 286 – 303. Doi: 10.4240/wjgs.v14.i4.286
8. Wei M, Ho E, Hegde P. (2020). An overview of percutaneous endoscopic gastrostomy tube placement in the intensive care unit. J Thorac Dis 2020; 13(8), 5277 – 5296. doi: 10.21037/jtd-19-3728
9. Early DS, Lightdale JR, Vargo JJ, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018; 87(2). 327 – 337. doi: 10.1016/j.gie.2017.07.018
10. American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to health patients undergoing elective procedures. Anesthesiology, 2017; 126(3), 376 – 393. doi: 10.1097/ALN.0000000000001452
11. American Society of Anesthesiologists Committee on Standards and Practice Parameters. Practice guidelines for moderate procedural sedation and analgesia 2018. Anesthesiology, 2018; 128, 437 – 479. Doi: 10.1097/ ALN.0000000000002043
12. Tam AL, Heran MKS, Sangha BS, et al. Society of Interventional Radiology standards division 2019 document review. J Interv Radiol, 2020; 31, 282 – 283. doi: 10.1016/j.jvir.2019.10.007
13. Roveron G, Antonini M, Barbierato M, et al. (2018). Clinical practice guidelines for the nursing management of percutaneous endoscopic gastrostomy and jejunostomy (PEG/PEJ) in adult patients: An executive summary. J Wound Ostomy Continence Nurs, 2018;45(4), 326 – 334. doi: 10.1097/WON.0000000000000442
14. Homan M, Hauser B, Romano C, et al. Percutaneous endoscopic gastrostomy in children: An update to the ESPGHAN position paper. J Pediatr Gastroenterol Nutr, 2021;73(3), 415 – 426. doi: 10.1097/ MPG.0000000000003207
Page 6 Within REACH
Fingernail Polish and Infection Control
Amy Lucas, MSN, RN, CCNS, CCRN-K - CRMH Clinical Nurse Specialist
Background & Significance
The nail enhancement business earns billions of dollars each year (Reinecke & Hinshaw, 2020) and there are many options to choose from that vary in price, durability, and ease of application and removal. One of the cheapest and easiest products to use is nail polish. Per Carilion policy, fingernail length should be less than ¼ inch long, nail polish should be freshly applied with no chipping (Centers for Disease Control and Prevention, 2002; World Health Organization, 2009). Healthcare workers should understand what is allowed by policy and how the choice can affect patient outcomes. This article discusses the evidence behind the current recommendations for traditional and gel nail polish.
Traditional nail polish is a varnish applied to the nail plate that dries through evaporation (Wałaszek et al., 2018; Wood & Van Wicklin, 2015). This is inexpensive, easy to apply and offers many color options. Traditional polish tends to lose integrity quickly, in some cases within a day of application (Blackburn et al., 2020). Gel polish, sometimes called Shellac, is a varnish that is applied to the nail plate but must be cured under an ultra-violet (UV) light to dry (Wałaszek et al., 2018, Reinecke & Hinshaw, 2020). Gel polishes are more expensive and can last for two weeks without chipping, but once integrity is lost, removal is more difficult (Wood & Van Wicklin, 2015). While traditional nail polishes can be removed at home in a matter of minutes, removal of gel polish requires soaking in acetone or being filed off, which is usually done in the salon (Wood & Van Wicklin, 2015).
While nail polish can lead to complications such as dermatitis or malignancy related to the UV light (Putek et al., 2020; Reinecke & Hinshaw, 2020), the biggest concerns for healthcare facilities are related to infections. Chips in nail polish or the gap between the color and the cuticle as the nail grows could harbor pathogens. There are concerns that an impaired gel polish manicure will be maintained instead of repaired due to the cost and time involved, increasing the risk for contamination and for spreading infection. There have also been concerns that those with enhanced nails may not perform adequate hand hygiene to protect the manicure (McNeil et al., 2001; Ward, 2007).
Literature Review
A literature search was performed using Carilion’s HERO database and ancestry search. Keywords used included: fingernail and infection control or hand hygiene, fingernail and infection control, fingernail and healthcare worker, nail enhancement and infection, nail polish and hand hygiene, gel nails and infection. Ten articles were identified that studied the impact of fingernail polish on infection prevention. Most of the studies were qualitative or correlational, but there were a few well-controlled studies and one Cochrane Review.
There is little evidence that freshly applied traditional nail polish increases risk of infection for patients, though there is an association between long fingernails and increased bacterial load. Fagernes and Lingaas (2011) cultured a convenience sample of direct care staff during their shift and did not find any impact from nail polish but found nail length significantly associated with increased bacteria. Hardy et al. (2017) performed a randomized crossover trial in a veterinary clinic comparing polished to non-polished fingers and found that the only variable associated with higher bacterial counts was nail length greater than 2mm. A Cochrane review published in 2014 was unable to determine if nail polish affected the number of bacteria on the skin after a surgical scrub (Arrowsmith & Taylor, 2014). Tank & Çelik (2018) also looked at polish and the surgical scrub by comparing cultures taken at baseline and after performing a surgical scrub. While
Page 7 Practical Applications of Nursing Inquiry
samples taken from hands with nail polish after performing a surgical hand scrub did grow more bacteria, the difference did not reach statistical significance when compared to the cultures taken before the scrub or to the other hand that was not polished. Blackburn, et al (2020) performed a randomized study of oncology nurses and found fewer bacteria on polished nails versus unpolished nails when the polish was one day old, but the polish rapidly degraded after the first day and was associated with an increase in all types of bacteria with the gram-positive bacteria reaching statistical significance.
Studies examining gel polish found unclear results. A review of the literature published between 1978 and 2018 found few studies and contradictory results but the main findings were that traditional polish could impact quality of a surgical scrub if the polish was damaged, and that gel polish may be associated with lower quality of hand scrub (Olivares et al., 2020). Hewlett et al (2018) studied workers after applying gel polish and traditional polish each to one finger, and the others natural. Both gel and traditional polish became more contaminated over time with the amount plateauing in the second week. The traditional polish had the most bacteria prior to hand hygiene on day 7 but the gel polish had a smaller decrease in bacteria after hand hygiene than either natural or traditional polished nails. Ultimately, there was not a statistically significant difference between the three options after hand hygiene but this was because there were fewer bacteria on the gel nails pre-cleaning. The final two studies looked at natural, polished, and artificial nails with both sampling staff who already had the nail enhancements in place. Artificial nails were found to harbor more bacteria than either polished or natural nails, however in one study there was not a clear delineation between uv-cure polish and uv-cured artificial nails in the results making it difficult to tell if the increased bacteria was associated with a specific type of uvcured product after hand hygiene (Edel et al., 1998; Wałaszek et al., 2018).
The study designs and amount of control varied but they found similar results. Freshly applied traditional nail polish does not appear to increase risk of spreading pathogens however, breaks down soon after application. Gel polish also appears not likely to contribute to the spread of infection but there is concern for findings that hand hygiene does not remove as many bacteria. It is unclear if this is related to a characteristic of the polish or an unconscious action by the wearer but could lead to spread of pathogens. More research is needed to further investigate this phenomenon. Long nails were associated with increased bacteria in several studies.
Implications for Practice
The Carilion Hand Hygiene Policy is an Infection Control Department policy and applies to all employees who provide direct care or who interact with items that will be used for patients. This policy is consistent with evidence. Healthcare workers can safely use nail polish as long as the integrity is intact and the nails are short. Those who work wearing impaired polish or long nails risk not only professional consequences but risk patient safety.
References
Arrowsmith, V.A., Taylor, R. (2014). Removal of nail polish and finger rings to prevent surgical infection. In Cochrane Database of Systematic Reviews (Vol. 2014, Issue 8). John Wiley and Sons Ltd. https:// doi.or/10.1002/14651858.CD003325.pub3
Blackburn, L., Acree, K., Bartley, J., DiGiannantoni, E., Renner, E., & Sinnott, L.T. (2020). Microbial growth on the nails of direct patient care nurses wearing nail policy. Oncology Nursing Forum, 47(2), 155-164. https:// doi.org/10.1188/20.ONF. 155-164
Centers for Disease Control and Prevention. (2002). Guideline for Hand Hygiene in Health-Care Setting Recommendations of the Healthcare Infection Control Practices Centers for Disease Control and Prevention. MMWR, 51(RR-16), 1-45
Page 8 Within REACH
Practical Applications of Nursing
Edel, E. ;, Houston, S. ;, Kennedy, V. ;, & LaRocco, M. (1998). Impact of a 5-minute scrub on the microbial flora found on artificial, Ppolished, or natural fingernails of operating room personnel. Nursing Research, 47(1), 54–59. https: ovidsp.dc2.ovid.com ovid-a/ovidweb.cgi
Fagernes, M., & Lingaas, E. (2011). Factors interfering with the microflora on hands: A regression analysis of samples from 465 healthcare workers. Journal of Advanced Nursing, 67(2), 297–307. https://doi.org/10.1111/j.1365 2648.2010.05462.x
Hardy, J. M., Owen, T. J., Martinez, S. A., Jones, L. P., & Davis, M. A. (2017). The effect of nail characteristics on surface bacterial counts of surgical personnel before and after scrubbing. Veterinary Surgery, 46(7), 952–961. https: doi.org/10.1111 vsu.12685
Hewlett, A. L., Hohenberger, H., Murphy, C. N., Helget, L., Hausmann, H., Lyden, E., Fey, P. D., & Hicks, R. (2018). Evaluation of the bacterial burden of gel nails, standard nail polish, and natural nails on the hands of health care workers American Journal of Infection Control, 46(12), 1356–1359. https://doi.org/10.1016/j.ajic.2018.05.022
McNeil, S. A., Foster, C. L., Hedderwick, S. A., & Kauffman, C. A. (2001). Effect of hand cleansing with antimicrobial soap or alcohol-based gel on microbial colonization of artificial fingernails worn by health care workers. Clinical Infectious Diseases, 32, 367–372. https://academic.oup.com/cid/article-abstract/32/3/367/282937
Olivares, F., Vergara, T., Véliz, E., & Dabanch, J. (2020). Impacto del uso de anillos y uñas esmaltadas en la calidad de la hygiene de manos en el personal de salud. Revista Chilena Infectologia, 37(1), 23–31. www.revinf.cl
Putek, J., Przybyła, T., Szepietowski, J. C., Baran, W., & Batycka-Baran, A. (2020). Side-effects associated with gel nail polish: A self-questionnaire study of 2,118 respondents. Acta Dermato-Venereologica, 100(18), 1–5. https://doi. org/10.2340/00015555-3684
Reinecke, J. K., & Hinshaw, M. A. (2020). Nail health in women[Formula presented]. International Journal of Women’s Dermatology, 6(2), 73–79. https://doi.org/10.1016/j.ijwd.2020.01.006
Tank, D. Y., & Çelik, S. (2018). Effect of use of nail polish on bacterial colonization after surgical handwashing in operating room nurses: A preliminary study. Cukurova Medical Journal, 43(3), 698–705. https://doi.org/10.17826 cumj.383360

Wałaszek, M. Z., Kołpa, M., Różańska, A., Jagiencarz-Starzec, B., Wolak, Z., & Wójkowska-Mach, J. (2018). Nail microbial colonization following hand disinfection: A qualitative pilot study. Journal of Hospital Infection, 100(2), 207 210. https:doi.org/10.1016/j.jhin.2018.06.023
Ward, D. J. (2007). Hand adornment and infection control. British Journal of Nursing, 16(11), 654–656. http:// web.b.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=1&sid=24206a4c-2426-4b49-a445-87c8bc02142a 40sessionmgr103
Wood, A., & Van Wicklin, S. A. (2015). Clinical Issues-June 2015. AORN Journal, 101(6), 701–708. https: doi.org/10.1016/j.aorn.2015.03.004
World Health Organization. (2009). WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. https://www.ncbi.nih.gov/books/NBK144013/
Page 9
Inquiry
Vaping - Is it safer than smoking?
- Pulmonary/Trauma Focus
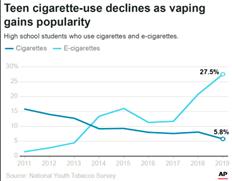
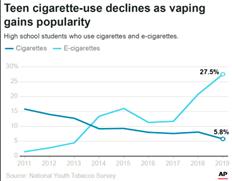
Electronic cigarettes appeared in the United States between 2006-2007.1 From the beginning, vape companies have advertised their products as being a safe alternative to combustible tobacco (smoking) without solid evidence of this claim. Since the beginning of the product appearing the in the United States, the FDA (US Food and Drug Administration) has tried to regulate the products; however, the companies producing the vape products, primarily tobacco companies, have been a step or two ahead of the regulations. Vaping exploded in 2014, with more than a tripling of people using vape products. More alarming was the rapid increase in youth using vape products as a first experience with nicotine, not as a method of cessation of a tobacco product. This may have been related to the products being pleasingly flavored and targeted advertising. Until that time, sales of vape products were mostly to adults who used the product as a smoking cessation aide. This all changed with the formation of Juul and advertising by young influencers on social media.1 The number of new smokers of combustible tobacco had been slowly decreasing over the decades since the first surgeon general’s report in 1988 that identified the health risks of tobacco and the addictiveness similar to heroin or cocaine.2 It was thought that by the next generation (2000’s), smoking would become almost non-existent. Vaping has changed that trajectory.
What is vaping?
Vaping is the use of some type of base/battery and a heating element that vaporizes a liquid allowing the user to inhale the product.1 The amount of nicotine varies, and since the product is not regulated, the labeling is not reliable. There is now a fifth generation of vaping products that have been manufactured to be easier to conceal by youth using the products. The liquid used in this product is called “vape juice”. The juice contains 10% water, food flavoring, nicotine and 90% of either vegetable glycerin or propylene glycol (yes, that is the same as the chemical in antifreeze). Most products use a combination of both. Both products increase mucus production and produce toxic aldehydes when heated. The flavors are food safe, not lung safe. For example, vanilla and cinnamon flavors cause cytotoxicity and ciliary dysfunction when inhaled. Butter flavored (diacetyl) can cause pulmonary toxicity leading to bronchiolitis obliterans. When tested, it has also been found that levels of nicotine are significantly higher in US products (59 mg/ mL) when compared to products in the UK (18 mg/mL).
Is vaping safer than smoking?
Maybe. Do they help smokers quit using combustible tobacco? Again, maybe. But we have proven smoking cessation medications that have been shown to be safe and effective since 1984. The reason people may not have had success with the over-the-counter nicotine replacement therapy may be due to
 Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS - CRMH Clinical Nurse Specialist
Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS - CRMH Clinical Nurse Specialist
Page 10 Within REACH
Adults (https://news.gallup.com/poll/1717/tobacco-smoking.aspx) Youth (https://khn.org/news/vaping-by-the-numbers/)
under-dosing. This will be discussed later. So, is there evidence about vaping leading to the decreased use of combustible tobacco? In a 2019 study of 886 adult smokers, twice as many smokers quit using e-cigarettes (19% versus 9.9%) than Nicotine Replacement Therapy (NRT).3 A longitudinal study of 2 years found that people using e-cigarettes were more likely to remain cigarette free.4 In both studies, the people who quit using tobacco were still using the e-cigarette. England found in their country, with lower nicotine levels, no advertising of e-cigarette products and low youth vaping rates, e-cigarettes were a vgood substitute for smoking combustible tobacco.5 A systematic review of 577 studies identified those who used e-cigarettes had higher quit rates than those who did not use e-cigarettes6, however no major organization (US Preventative Services Task Force, American Cancer Society, American Thoracic Society or the Centers for Disease Control)7-10 have recommended using e-cigarettes as a stop smoking method. The National Academy of Science, Engineering, and Medicine acknowledges that while e-cigarettes are “not without health risks, they are likely to be far less harmful than smoking combustible tobacco cigarettes”.11

What are the risks of vaping?
The main health risk identified so far is using the vaping product as a gateway to cigarettes use. This is particularly true in youth, but other non-smokers have progressed from e-cigarettes to combustible tobacco. There was also an outbreak of E-cigarettes or Vaping Associated Lung Injury in 2019.12 This was traced to the use of vitamin E acetate in illicit THC vaping products.
These injuries peaked in September of that year with 2,807 hospitalizations and 68 deaths recorded, primarily in younger 18–34-year-old people using vape products. The takeaway from this outbreak is the lack of research and regulation of the products. They cannot be assumed to be safe.
What is the best way to quit smoking?
The best way to quit using any product that contains nicotine is counseling and pharmacological support. At any time, about 50-70% of smokers want to quit using tobacco products.13 It usually takes about six quit attempts before completely stopping, but that statistic is from trying to quit “cold turkey”.10 Nicotine Replacement Therapy (NRT) is very effective in helping people control their cravings. Most people do not use enough of the NRT product. See table below for recommendations.14
Number of cigarettes/pouches
smokeless tobacco
1 ½ packs per day OR > 2 cans/pouches per day
NRT Product
21 mg patch every day PLUS 1-15 pieces of 4 mg NRT gum/lozenges per day
½ packs per day OR 1 can/pouch per day
< ½ pack per day OR Weighs < 45 kg (100 lbs)
14 mg patch every day PLUS 1-15 pieces of 2 mg NRT gum/lozenges per day
21 mg patch every day PLUS 1-15 pieces of 2 mg NRT gum/lozenges per day ½-1 pack per day OR < 1 can/pouch per day
14 mg patch every day PLUS 1-15 pieces of gum/lozenges per day
The suggested weaning method of multiple NRT products is to decrease the use of the gum/lozenges; then decrease the patch amounts, but others have had success with weaning patches first, followed by reduction of the gum/lozenges. Some people may choose to keep using NRT long-term, which also occurs with e-cigarettes, and like e-cigarettes, using NRT long term is associated with less carcinogens and toxins when compared with combustible tobacco.15
NRT Gum Weaning
Weeks 1-6
Weeks 7-9
Weeks 10-12
1 piece every 1-2 hours
1 piece every 2-4 hours
1 piece every 4-8 hours
Page 11 Practical Applications of Nursing Inquiry
NRT Patch Weaning
Strength as ordered Weeks 3-4 Decrease to next lower strength
Weeks 1-2
Weeks 5-6 Decrease to next lower strength Weeks 7-9 Decrease to next lower strength or discontinue
In conclusion, use of vaping or electronic cigarettes MAY assist in people who use combustible tobacco products to quit their use; however, is the health risk to the youth of American a risk we are willing to take?
References
1. Dinardo, P., Rome, E. (2019). Vaping: The new wave of nicotine addiction. Cleveland Clinic Journal of Medicine, 86(12), 789798.
2. United States Office on Smoking and Health. (1988). The health consequences of smoking: nicotine addiction: a report of the surgeon general. DHHS publication retrieved 12/13/2022 from https://stacks.cdc.gov/view/cdc/22014
3. Hajek, P., Phillips-Waller, A., Przulj, D., et al. (2019). A randomized trial of E-cigarettes versus nicotine replacement therapy. New England Journal of Medicine, Retrieved 2/14/2019 from NEJM.org, 629-637.
4. Kalkhoran, S., Chang, Y., Rigotti, N. (2020). Electronic cigarettes use and cigarette abstinence over 2 years among US smokers in the population assessment of tobacco and health study. Nicotine & Tobacco Research, 728-733.
5. Whelan, S. (2017). Highest smoking quit success rates on record. Public Health England. Retrieved 12/13/2022 from: www.gov.ek/government/news/highest -smoking quit success-rates on record#.
6. Kalkhoran, S., Glanta, S. (2019). E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respiratory Medicine, 4(2), 116-128.
7. US Preventive Services Task Force. (2021). Interventions for tobacco smoking cessation in adults, including pregnant persons. JAMA, Retrieved 12/13/2022 from: https://www.uspreventiveservicestaskforce.org/uspstf/announcements/finalrecommendation-statement-interventions-tobacco-smoking-cessation-adults-including-pregnant-persons#:~:text=January% 2019%2C%202021%20%E2%80%94%20The%20U.S.%20Preventive%20Services,to%20proven%2C%20safe%20methods% 20to%20help%20them%20quit
8. Leona, F., Zhang, Y., Evers-Casey, S., et al. (2020). Initiating pharmacologic treatment in tobacco dependent adults. American Thoracic Society Documents, Retrieved 12/13/2022 from: https://www.obgproject.com/2020/10/09/americanthoracic-society-initiating-pharmacologic-treatment-in-tobacco-dependent-adults/#:~:text=ATS%20Smoking%20Cessation% 20Recommendations%201%20Varenicline%20superior%20for,patch%20No%20difference%20in%20SAEs%20compared% 20to%20bupropion
9. American Cancer Society. (2019). E-cigarettes should not be used to quit smoking. American Cancer Society Position Statement on Electronic Cigarettes, Retrieved 12/13/2022 from: http://pressroom.cancer.org/eCigs2019#:~:text=ACS%E2%80% 99s%20new%2C%20clarified%20position%20is%3A%20No%20youth%20or,e-cigarettes%20should%20not%20be% 20used%20to%20quit%20smoking
10. Centers for Disease Control and Prevention. (2021). Electronic Cigarettes. Retrieved 12/13/2022 from: https://www.cdc.gov/ tobacco/basic_information/e-cigarettes/index.htm
11. National Academies of Science, Engineering and Medicine. (2018). New report one of the most comprehensive studies on health effects of e-cigarettes; Finds that using e-cigarettes may lead youth to start smoking , adults to stop smoking. Retrieved 12/13/2022 from: https://www.nationalacademies.org/news/2018/01/new-report-one-of-most-comprehensive-studies -on-health-effects-of-e-cigarettes-finds-that-using-e-cigarettes-may-lead-youth-to-start-smoking-adults-to-stop-smoking
12. Xantus, G., Gyamathy, A., Johnson, C. (2020). Smoldering ashes: burning questions after the outbreak of electronic cigarette or vaping associated lung injury. Postgraduate Medical Journal, 6(1141), 686-692.
13. Rigotti, N., Kruse, G., Livingstone-Banks, J., Hartmann-Boyce, J. (2022). Treatment of tobacco smoking: a review. JAMA, 327 (6) 566-577.
14. Lindson, N., Chepkin, S., Ye, W., et al. (2019). Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Systematic Reviews, Issue 4.
15. Shahab, L., Goniewicz, M., Blount, B., et al. (2017). Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: a cross-sectional study. Annals of Internal Medicine, 166 (6), 309-400.
Page 12 Within REACH
ANDREA GEE Patient Care Tech
Carilion Nursing Resource Pool
Andrea has been a Patient Care Tech in the CRMH Resource Pool for 2 years. She is currently attending Radford University in their ABSN program. Andrea works, attends school and cares for her family.
Andrea was awarded a scholarship from the Doris & Lynn Morris Scholarship Fund.
The award is managed by the Carilion Foundation.
Andrea was chosen by the board members of the Carilion Foundation after submitting her application through the Carilion Nursing Administration department, who screens the applications and forwards exceptional candidates on for review and voting by the board members.


Comments from her directors:
• “
Andrea genuinely wants her patients to receive the best care possible and goes our of her way to provide that, every shift.”
• “She (Andrea) already knows and embraces the requirements for excellent patient care.”
• “Andrea not only establishes workingrelationships with nurses, physicians,physical therapists, dietary, etc.she serves as a preceptor and mentor to new staff. She is essential in establishing their foundation for providing good patient care and advocacy. It is exciting to see that Andrea is continuing to see our opportunities to further advance her education.”
Page 13 Practical Applications of Nursing Inquiry
Natalie Pinegar, RN CRMH 11 West Outstanding
Preceptor Award

Natalie was one of the first nurses to receive the new Outstanding Preceptor Award. As a preceptor at CRMH, Natalie helps prepare the next generation of nursing professionals. Natalie was nominated by her mentee Patrick Henry Community College student Allison Boaz. Allison stated “ Natalie has always encouraged me to go after any opportunity available to me on the floor, which has boosted my confidence so much more She always knows the right thing to say to help make the patient experience top notch and to help them through a difficult time in their life Natalie is absolutely amazing in the leadership position.”
Commitment! Commitment!

Strohman, RN CRMH Emergency Department Outstanding Preceptor Award

Nicole was also among the first 2 nurses to receive the new Outstanding Preceptor Award. Nicole was nominated by her mentee Radford University Student Celeste St. John. In her submission, Celeste commented “Nicole went over and beyond each shift that I worked with her, even during the rough days…...I had never been part of a conscious sedation before, and she explained every detail to me throughout the procedure…..during this whole externship, she has made it a point to stop and teach me which I really appreciated. She made sure that I was able to see procedures that residents were doing she was a phenomenal mentor and I have learned so much in just the short time I have been working with her.”

Page 14 Within REACH
Nicole
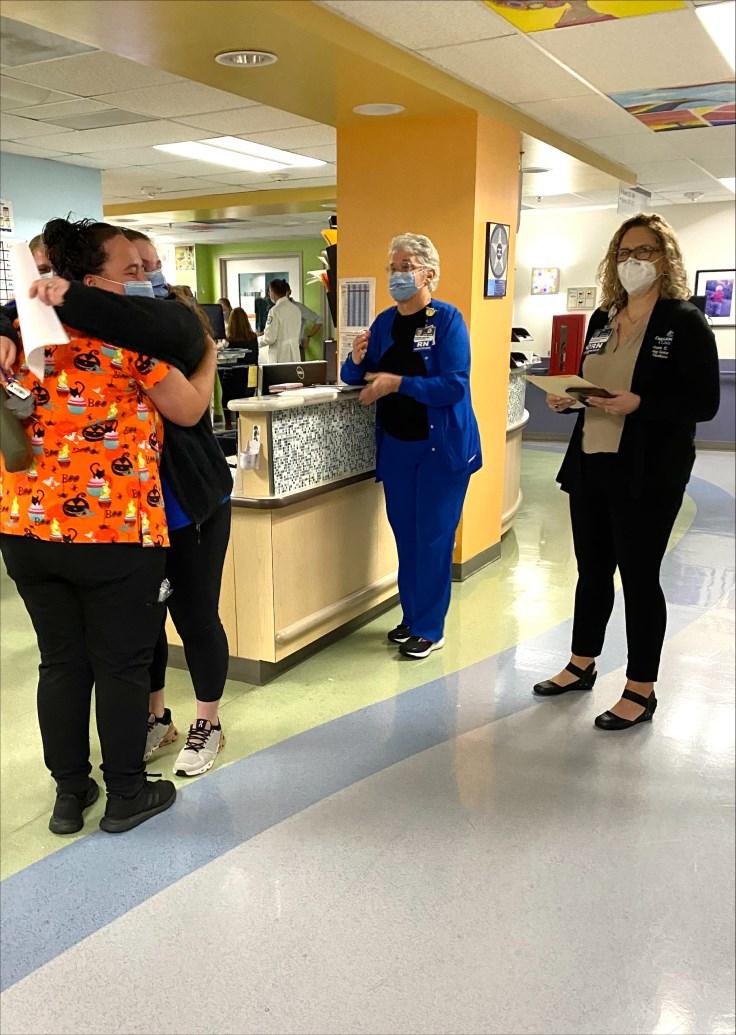
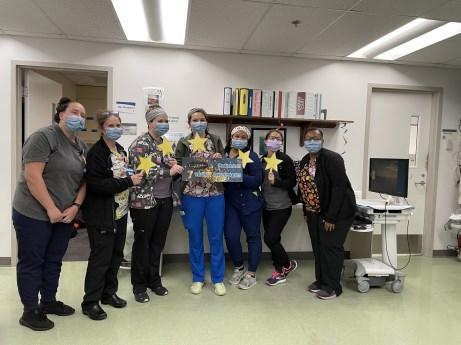
CRMH Pediatrics and PICU CLABSI Celebration


Congratulations to CRMH Pediatrics and PICU who have just celebrated ZERO CLABSIs! Pediatrics has seen 7 years without a CLABSI and PICU has gone 3 years with no CLABSIs. About 10% of pediatric central line associated bloodstream infections (CLABSI) are associated with severe sepsis, causing organ damage or dysfunction that requires ICU results in death. (June 2020 Pediatrics, (145),




•
• PICU has gone THREE years without a CAUTI!
• Pediatrics has gone ONE year without a CAUTI!
Page 15 Practical Applications of Nursing Inquiry
Commitment!
Commitment! CRMH NICU/PICU/PEDS Zero Celebration for Carilion Children’s
Thank you for your commitment to keeping our patients safe!
Congratulations to Carilion Children’s for the following AMAZING accomplishments!
NICU has gone ONE year without a Pressure Injury!
Thank you for your commitment to keeping our patients safe! ~From WOW Wall post~
Harvey, DNP, RN, ACNS-BC, CCRN, TCRN, FCCM 2021 Magnet Nurse of the Year - Empirical Outcomes CMC Board of Directors - Recognition

Ellen received continued recognition for her exciting 2021 Magnet Nurse of the Year Award at the CMC Board of Directors Meeting September 13, 2022, where she was presented with a plaque by Dr. Suzanne Kramer and Board Member Damon Williams.

Commitment Collaboration!
Margaret Perry, MSN, RN-BC TEACH Educator Mentorship Award


The TEACH Educator Mentorship award recognizes an individual who has demonstrated excellence in counseling and guidance towards others’ teaching practices, and/or educational research. The award is sponsored by Virginia Tech Carilion School of Medicine and Radford University Carilion. In Margaret’s 10 years as an exceptional educator her commitment and passion have helped develop new educators from novice to expert. She has mentored many MSN students and advised colleagues and peers. Margaret has also worked with numerous nursing and allied health professionals to guide, develop, and provide assistance in the evolution of education modalities used in our organization.
~from WOW Wall Post by Christy Sutphin 10/31/22~

Page 16 Within REACH
Ellen
Commitment!
Manning, RN CRMH 10M PCU Outstanding Preceptor Award




The Nursing Center of Excellence (NCE) presented the Outstanding Preceptor Award to Kim on October 19, 2022. Leaders from the NCE presented her with the award alongside her team members and nursing leaders. Kim has worked for the organization for 42 years and is an outstanding preceptor to new hires, nursing students, & nurse externs.
~From WOW Wall post by Lauren Miley 10/31/22~
Commitment!
Lexie Pollard Eades,
RN CRMH Pediatrics Outstanding Preceptor Award
The Nursing Center of Excellence (NCE) presented the Outstanding Preceptor Award to Lexie alongside her team members and unit leaders. Lexie’s commitment and compassion are ever present as she takes the “utmost care to teach, explain, demonstrate, and reinforce the education and knowledge” that new hires and nursing students need to be the best nurses they can be.
~From WOW Wall post~
Page 17 Practical Applications of Nursing Inquiry
Kim
Sara Sartin, RN CNRV Labor & Delivery Outstanding Preceptor Award
Clinical Educator, Wendy Worrell, RN submitted the nomination and shared that “One of Sara’s greatest gifts is her compassion and non judgmental attitude when caring for our Birthplace patients and modeling this for our new employees”.


~From WOW Wall post~
Compassion! Commitment!
Tamara Wooolwine, RN CRMH O-P Prep Outstanding Preceptor Award

Susan Hall, RN submitted the nomination for Tamara saying “when Tamara orients someone, they are completely ready for the job.” Tamara’s commitment and compassion toward not only her patients, but also to her Carilion Clinic family deserves to be recognized and celebrated.
~From WOW Wall post~

Page 18 Within REACH
Commitment!
$1,000 Grant Award from American Trauma Survivors Society




Ottilia and the CRMH TSN are the recipients of a grant from the American Trauma Society. This inaugural “TSN Site Grant Program” will support our shared ATS mission: “Saving Lives, Improving Care. Empowering Survivors”. The $1,000 grant will be aimed at our Peer Visitation and Support Program which has been a mainstay of the CRMH TSN program.
~From WOW Wall post~
Compassion!
Ball, RN CGCH Emergency Department CGCH Ripple Award

The Patient Experience Team at CGCH selects one colleague each month that makes a significant impact to the Patient Experience that is provided at our facility. Sherry was nominated by her peers for her willingness to always “jump in and help, no matter the situation.” Sherry has provided exceptional care for her patients, for example, in an emergency situation, encouraging the patient that needed to be flown out; driving the husband of that patient who needed emergency surgery to another facility. These are actions that go above and beyond the normal day to day care she provides.
~From WOW Wall Post submitted by Ashley Graham~
Page 19 Practical Applications of Nursing Inquiry
Ottilia Lewis, RN - Trauma Outreach Coordinator & the CRMH Trauma Survivors Network (TSN)
Sherry
The Carilion Nursing Research Department has established an Editorial Review Board for Carilion initiatives such as the Magnet® and Pathway’s to Excellence documents, to support other unit specific applications, and our internal nursing publication Within REACH. We welcome anyone who enjoys writing, would like to learn about peer editing, and may wish to be considered for the Carilion Clinic Nursing Editorial Board.
If interested in serving as an editor, please notify Chris Fish-Huson, PhD, RN, CNE, Sr. Director, Nursing Research & Evidence-Based Practice at cdhuson@carilionclinic.org or 540-981-7536


Page 20 Within REACH
CONFERENCE CORNER
Ochsner 14th Annual EBP/Nursing Research Conference, New Orleans, LA

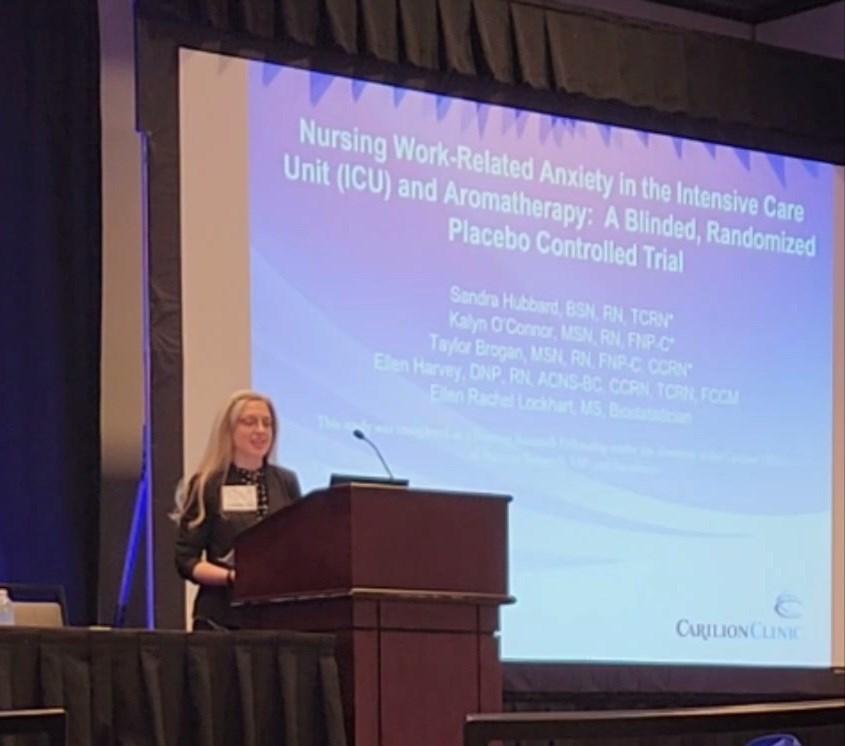
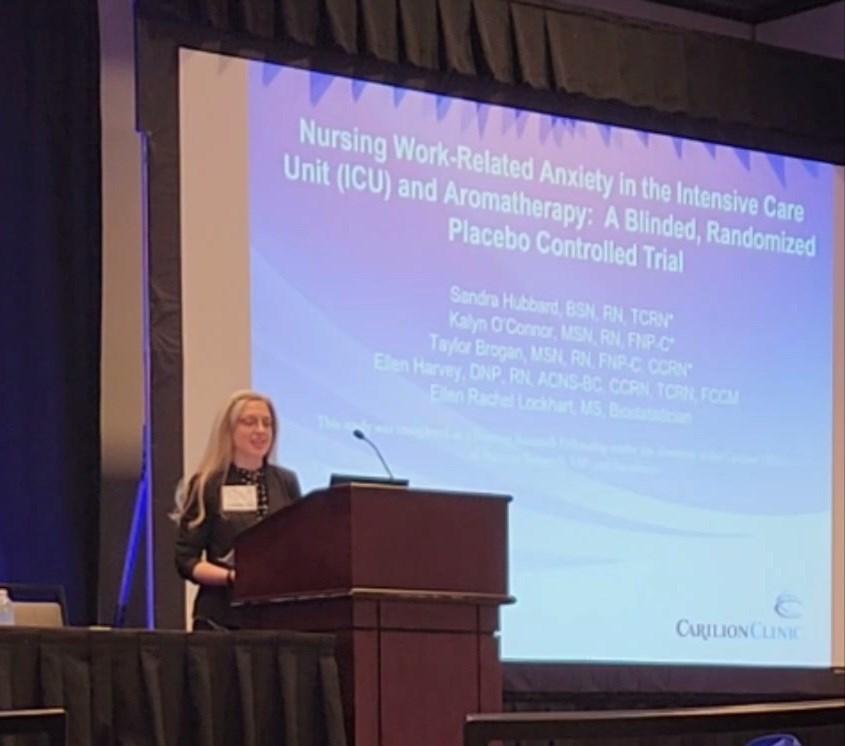
Sandy Hubbard, BSN, RN, TCRN CRMH 9M ICU was invited to present her 2020 Nursing Research Fellowship Teams work titled Nursing Work Related Anxiety in the ICU and Aromatherapy: A Randomized, Blinded, Placebo-Controlled Trial in New Orleans, October 14, 2022.
Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS; Amy Lucas, MSN, RN, CCNS, CCRN-K & Kim Ramsey, MSN, RNC-NIC, ACCNS-N, CPST CRMH Clinical Nurse Specialists were invited to present at the Annual Respiratory Nursing Society & Interprofessional Collaboration at the Hotel Roanoke on August 22, 2022. The presentations were:

• Vaping is Better than Smoking - Donna Bond
• Life After Sepsis - Amy Lucas
• The Evolution of Surfactant Therapy: Helping Babies Breathe - Kim Ramsey
Page 21 Practical Applications of Nursing Inquiry
Annual Respiratory Nursing Society & Interprofessional Collaboration, Roanoke, VA
l-r: Kim Ramsey, Donna Bond, Amy Lucas



Page 22 Within REACH QUALITY AWARDS: PioneerAwardWinner-FoleyFreeED Rachelle Balthis - Wrenn Brendel - Keven Broyles, D.O. - LeAnn Creasy - Matthew Davis - Timothy Dobson - Doris Duff - Timothy Fortuna, D.O. - Stephanie Hodges - Ashlie Ikenberry - Alison Martin - Gary Meadows - Mike McKennaSharon McKinney - Victoria Samarasinghe CRMH Emergency Department PioneerAwardFinalist-TelemetryBatteryChangeProject Christina Monk - Kayla Radford - Sumanth Raja - Karyn Reese - Branden Robertson - Shannon Robertson - Charles Suba CRMH Med Surg Administration, Quality & Patient Safety, Process Improvement, 9M PCU, Quality & Patient Safety, Virtual Care Cetner, Transfer Center EnterpriseAwardWinner-ReducingExternalVentricularDrain(EVD) AssociatedVentriculitis Mia Anglin, P.A. - Anthony Baffoe-Bonnie, M.D. - Wrenn Brendel - Joseph Cannon - Ellen Harvey - Mai Jatta - Kathleen Manchin - Brad McDaniel - Kelsey McWey, P.A., Shannen Plaster, N.P. - Kim Ramsey - Laura Reiter - Cara Rogers, D.O. - Megan Simmons - Angela Wolfe CommunityDistinctionAwardFinalist:EffectsofLaborSupport EducationonNursing Megan Barefield - Casey Delph - Katlyn Horton - Kimberly Hurst - Danielle Liddle - Jeryl Maurer - Wendy Worrell CNRVMC The BirthPlace HonorableMentionforSustainability:JourneytoZeroHarm Ghislaine Cady - Ross Cleveland - Michelle Franklin - Linda Keele, M.D. - Donald Kees, M.D. - Karrie Moses - Lisha Osborne - Patrick Randolph CRMH Pediatrics/PICU/NICU *Red highlighted names = nursing staff PRESIDENT’S AWARD: Kim Manning, RN CRMH 10M PCU
Page 23 Practical Applications of Nursing Inquiry VALUES AWARDS: (Collaboration) HonorableMention:CognitiveTherapyProgram Monica Coles - Lisa Hebert-Meritt - Rhonda Ihlenburg - Lisa Sprinkel - Sarah Stubbs, M.D. - Melissa Stump - Virgil Thompson - Brain Unwin, M.D. Carilion Home Health and Hospice, Department of Geriatrics VALUES AWARDS: (Compassion) HonorableMention:CodeLavender Suzanne Bowser - James Bunch - Joe Elmore - David Fox - Loresa HeywardKeith Little - Cindy Meadows - Sunny Miller - Andrew Tressler CRMH 7M PCU, Pastoral Care VALUES AWARDS: (Courage) HonorableMention:ConversionfromPCUtoICUDuringCovid-19 Surge Becca Butterworth - Hannah Dooley - Teniola Emmanuel - Melissa Goad - Ann Ikunyua - Amber Janney - Mary Lee - Tiffany Lytton - Kimberly Miller - Louis Sarmiento - Ella Son - Leigha Stanley - Jodi Wilson CRMH 8S ICU VALUES AWARDS: (Curiosity) AwardWinner:HeartLegacyProgram Renee Altizer - Robyn Angle - Sarah Browning - Joe Castiglioni - Jon Evens - Jay Markell - Cathy Miles - Lisa Sprinkel - Kelly Sweeney - Rob Urquhart - Heather White Carilion Home Health & Hospice, Technology Services Group, Marketing & Communications ADDITIONAL INTERNATIONAL, NATIONAL, STATE, REGIONAL & LOCAL AWARDS AffiliateoftheYearAwardfromtheNationalAssociationofClinical NurseSpecialists Donna Bond - Monica Coles - Cindy Ward - Phyllis Whitehead CRMH Clinical Nurse Specialists FellowoftheAmericanAcademyofNursingAward Phyllis Whitehead CRMH Clinical Nurse Specialist, Carilion Ethics Continued next page



Page 24 Within REACH ADDITIONAL INTERNATIONAL, NATIONAL, STATE, REGIONAL & LOCAL AWARDS continued 202140Under40AwardedbyTheRoanokerMagazine Katie Martin CRMH NICU 202240Under40AwardedbyTheRoanokerMagazine Suzanne Tyler Carilion Infection Control MedicalHeroAwardfromtheAmericanRedCross Alicia McAllister-Daniels CRMH Pediatric Services MagnetNurseoftheYearAwardinEmpiricalOutcomesfromANCC Ellen Harvey CRMH Clinical Nurse Specialist PresidentialCitationfromtheSocietyofCriticalCareMedicine Ellen Harvey CRMH Clinical Nurse Specialist YearoftheNurseAwardfromtheVirginiaNursesFoundation Jonathan Philips CFMH ICU *Red highlighted names = nursing staff
Introducing the Virtual Healthcare Hot Topics Journal Club!

Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC Research Council Unit Outreach Subcommittee
The Unit Outreach Subcommittee of the Research Council has started a virtual journal club to provide an opportunity to read and discuss issues of concern in healthcare. The journal club is open to any employee The most exciting thing about the Healthcare Hot Topics Journal Club is that it is virtual! Using the Teams platform will allow participants to post their comments and opinions when it is convenient for them.
A new discussion will be started every one to two months. There will be a channel for each new topic with the article posted in the Files section. Discussion questions for the article will be located in the Wiki. A separate tab will give access to the evaluation form. Please complete the evaluation to let us know your opinion about the journal club and what future topics you’d like to discuss.
Participation in a journal club can be used to fulfill the Research criteria for RN 2. The subcommittee will discuss ways journal club participation could be added to RN 3 and 4 criteria and make recommendations to the CAP Committee.
Questions? Contact: Cindy Ward - Clinical Nurse Specialist email: cwward@carilionclinic.org phone: 540-224-2508

Page 25 Practical Applications of Nursing Inquiry
Whitehead, P. June, 2022. CDC Chronic Pain Guidelines: What you need to know. Virginia Association of Clinical Nurse Specialists Annual Virtual Conference. (Invited Speaker)
Whitehead, P. June 2022. Moral Distress & ECMO. Ethical Considerations & Moral Distress Within ECMO. Extracorporeal Life Support Organization Virtual, Quarterly Meeting. (Invited Speaker)
Ramsey, K. August 2022. The Evolution of Surfactant Therapy: Helping Babies Breathe. Annual Respiratory Nursing Society & Interprofessional Collaboration. Roanoke, VA
Bond, D. August 2022. Vaping is Better than Smoking. Annual Respiratory Nursing Society & Interprofessional Collaboration. Roanoke, VA
Lucas, A. August 2022. Life After Sepsis. Annual Respiratory Nursing Society & Interprofessional Collaboration. Roanoke, VA
Hubbard, S., O’Conner, K., Brogan, T., Harvey, E., Lockhart, R. October 14, 2022. Nursing Work Related Anxiety in the ICU and Aromatherapy: A Randomized, Blinded, Placebo-Controlled Trial. Ochsner’s 14th Annual Evidence-Based Practice/ Nursing Research Conference: Achieving Health Equity: Advancement and Opportunities in Nursing. New Orleans, LA.

Beels, S., Martin, M. June 2022. Improving Long Term Follow-up Compliance Post-Vascular Surgery in a Regional Care Center. Society of Vascular Surgery (SVS) Conference, Boston, MA
Gerow, R., Altice, N., Wu, Y., Muthukattil, R., Carter, K. September 2022. Early Cardiac Rehabilitation to Reduce Heart Failure Readmissions. Journal of Cardiopulmonary Rehabilitation and Prevention 2022, (42), 324-330.
Ward, C., Mitchell, T. September 2022. Reducing Nurse Burnout When Caring for Patients with Substance Use Disorder. Nursing2022, 52, (9), 36-40.
Reiter, L., Taylor, O., Jatta, M., Plaster, S., J. Cannon, McDaniel, B., Anglin, M., Harvey, E. September 2022. Reducing External Ventricular Drain Associated Ventriculitis: An Improvement Project in a Level 1 Trauma Center. American Journal of Infection Control, https://doi.org/10.1016/j.ajic.2022.08.029
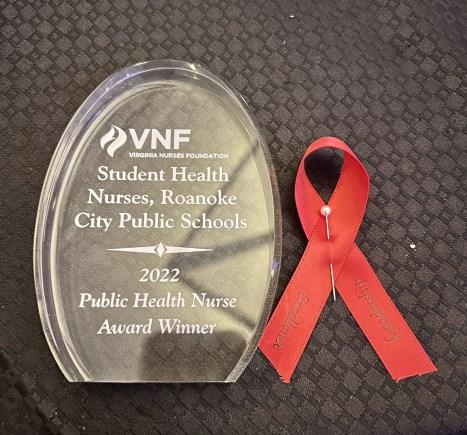
Roanoke City Public School Nurses. September 10, 2022. Virginia Nurses Foundation Award WinnerPublic Health Category
Amber Sawyer, BSN, RN. September 10, 2022. Virginia Nurses Foundation Award FinalistLeadership Category.
Margaret Perry, MSN, RN-BC. October 2022. TEACH Educator Mentorship Award.
Tanya Trevilian, MSN, RN, CCRN, CPN. October 2022. Selected to participate in the Pediatric Pandemic Network Scholars Program.
Ottilia Lewis, RN & the CRMH Trauma Survivors Network Program. October 2022. Received a $1,000 grant from the American Trauma Society (ATS).
Ariel Dooley, MSN, RN, NPD-BC - October 2022, Achieved her certification in Nursing Professional Development from ANCC.
Whitehead, P, Gamaluddin, S., DeWitt, S., Stewart, C., Kim, K. July 5, 2022. Global Perspectives in Cancer Care: Religion, Spirituality and Cultural Diversity in Health and Healing. Silberman M and Berger A, eds. Holistic Care of the Cancer Patients, United States: Identifying Unique Aspects of Palliative Care (pp. 33-44), New York, NY: Oxford University Press.
Liddle, D. July 2022. Effects of Labor Support Education on Nursing Knowledge, Confidence, and Cesarean Rates. Journal of Obstetric, Gynecologic and Neonatal Nursing 51(4), Supplement, S54.

Page 26 Within REACH
July 2022 - December 2022 (& past presentations not noted prior to this edition)



Page 27 Practical Applications of Nursing Inquiry Basic Research for the Healthcare Professional NR-CE333L *Additional classes have been added for 2023* Go to our hub on Inside Carilion for additions to our Nursing Research Classes schedule for 2023. https://insidecarilion.org/hub/nursing-research-evidence-based-practice/ all-activity/nursing-research-classes CLASSES & EVENTS 2023 January 12, 2023 - 3:00-7:00pm February 16, 2023 - 1:00-5:00pm March 16, 2023 - 1:00-5:00pm April 20, 2023 - 8:00am-12:00pm June 22, 2023 - 1:00-5:00pm August 17, 2023 - 8:00am-12:00pm October 19, 2023 - 1:00-5:00pm December 21, 2023 - 8:00am-12:00pm *All classes and events will be virtual at this time.
40 Under 40

Sarah Henshaw, MSN, RN Senior Director

CRMH CVI Medicine

(takenfromarticleinTheRoanokerbyLizLong)
Sarah Henshaw began her career as a nursing assistant in CCU, becoming an ICU bedside nurse before being promoted to a preceptor in 2014, then unit director in 2018 and now as senior director as of 2021. She currently oversees four inpatient units, one outpatient and five procedural areas in the Cardiovascular Institute at Carilion Roanoke Memorial Hospital. She was a recipient for the 2016 Human Touch Awards and a 2017 ANA Leadership Excellence Award Finalist. Henshaw is also a certified fitness instructor since 2017 and teaches atFerguson Fitness; she enjoys teaching others how to become stronger and improve their health through exercise. Her enthusiasm has led her to complete the Charlottesville Women’s Four Miler in support of breast cancer and volunteer at IRONMAN; she also volunteers at the American Heart Association and at the Rescue Mission with her kids. “I am always looking for ways that I can volunteer at our local food banks or community outreaches. Most importantly, I purposefully look for opportunities that my children can also volunteer alongside me. I hope one day they look back and realize the impact they had with all the little things we did together. I hope they grow into compassionate adults that never lose their desire to contribute to the greater good of others.”
From the Nomination: “Sarah Henshaw is a single mom raising two wonderful kids! Not only is she raising them on her own but she is leading by example and gets them involved in their community. Henshaw makes it look so effortless when in reality I always wonder how she shows up and makes it happen for everyone. She gives 110% in everything she does. She has been an ICU nurse since 2006 and hasn't stopped there. … She has a contagious laugh and a big heart to serve others in her day-to-day life. When she isn't busy saving lives, she's a fitness instructor at a local gym and enjoys teaching others how to move their body. … The challenges she has overcome and the lives she has touched. She started as a nursing assistant, became a bedside nurse, was promoted to a preceptor, then a unit director and is currently a senior director. She's a team-player, a wealth of knowledge, and an incredibly humble person. I'm surprised she hasn't been nominated sooner!"
How does your passion impact our community?
Henshaw: “My time spent as a bedside ICU nurse, specializing in cardiac care taught me the importance of physical health. I have always been very active myself, but my experience has given me a true passion for the health of others. Caring for the patient quickly turned into helping others avoid the need for extensive medical care. I took a role at Ferguson Fitness as an instructor several years ago, and I lead group exercise classes each week. I am always looking for ways that I can volunteer at our local food banks or community outreaches. Most importantly, I purposefully look for opportunities that my children can also volunteer alongside me. I hope one day they look back and realize the impact they had with all the little things we did together. I hope they grow into compassionate adults that never lose their desire to contribute to the greater good of others.”
40 Under 40

Brandon Jones, MSN, RN System Patient Experience Manager Carilion Clinic
 (takenfromarticleinTheRoanokerbyLizLong)
(takenfromarticleinTheRoanokerbyLizLong)
A nurse for 17 years, Brandon Jones has experience in critical care and emergency medicine both at the bedside and in various leadership positions. He served as one of the directors for Carilion Roanoke Memorial Hospital's level one trauma center; he has served as adjunct clinical nursing faculty for VWCC since 2018 and was appointed to the Virginia Board of Nursing by Governor Northam in 2019. He is currently a member of the American Nurses Association and Virginia Nurses Association, serves as chair of the Committee of the Joint Boards of Nursing and Medicine and was elected by his Board of Nursing colleagues to serve as President in 2022. He and his wife Erin, a pediatric emergency RN, recently started a new podcast, “Real Nurses, Real Talk,” where they share unique perspectives and insights into the industry. “Caring for others is my calling ... Three words can summarize much of my work caring for both the community and fellow caregivers: Heal, Empower and Inspire. … Through healing, empowering and inspiring nursing students, future nurses are better equipped to provide safe, high-quality, compassionate care. Compassion changes everything, and I will continue to advocate fiercely for patient-centered care and to improve the human experience in healthcare.”
From the Nomination: “Brandon [Jones] envisions a world where hospitals are a beacon of healing for the communities they serve. A place where patients receive safe, compassionate, quality care in every moment and where the caregivers are respected, cared for, and get an actual lunch break. Jones is an enthusiastic patient experience warrior for Carilion Clinic, although his “official” job is serving as the System Patient Experience Manager. …Throughout his career, Jones’ work within the patient experience arena has not gone unnoticed. He frequently presents at local, regional, and national conferences speaking on topics such as patient experience, human experience, purpose-driven healthcare and purpose-driven nursing. … During his time in the Emergency Department, Jones advocated for and pioneered creating a Patient/Family Advisory Council (PFAC). This PFAC was a way to better connect the Emergency Department with the community they serve. Because of the strong foundation created by Jones, the ED PFAC continues today. Additionally, Jones is active in his local church. He helps lead the college LifeGroup, The Bridge, which is a community of young adults. He also serves as a Deacon, serving the congregation when needed. Jones’ passion for improving the human experience is immediately evident for anyone who interacts with him. He has been instrumental in helping to develop the patient-centered culture for Carilion Clinic. … On one of his recent evaluations from students, one student noted: ‘Brandon Jones is an amazing clinical instructor that brings out the best in everyone he leads. His passion in his work is genuine and inspiring. He helps the group understand and dig for a bigger picture with their assigned patients and encourages independent thinking and learning from the concepts. Brandon is the nurse I dream to be and more.’ This is a great summary of what sets Brandon apart through his overwhelming passion.”
How does your passion impact our community?
“Caring for others is my calling, and I am passionate about improving the human experience in healthcare. Three words can summarize much of my work caring for both the community and fellow caregivers; Heal, Empower and Inspire. The community we serve is benefited through healing, empowering, and inspiring caregivers.





















































Page 28 Within REACH
“
The World is a book, and those who do not travel read only a page.” – Saint Augustine Palm
United Kingdom Lake Buena Vista
Williamsburg
Natl. Harbor, MD Greenville
Nottingham Anaheim Aurora


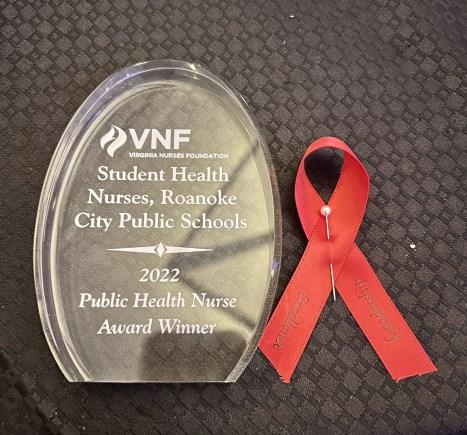




Page 29 Practical Applications of Nursing Inquiry VirginiaNurse’sFoundationAward Finalists&Winners Finalists: • Amber Sawyer - Practice Supervisor - Pediatric Hem/Onc Category - Patient Safety • Roanoke City Student Health Nurses Category - Public Health Winners: • Roanoke City Student Health Nurses Category - Public Health HonorableMention: • Brooke Hickman - CRMH 11W Unit Director • Russell Beggarly - CRMH 8M ICU Unit Director • Annie Phillips - CRMH 10W Med-Surg - Unit Director Nominations: • Kristy Massey - CRMH CSICU Unit Director








Campus 2023 NURSING CONFERENCE INFORMATION NTI 2023 Philadelphia: May 22-24, Preconferences May 21 Virtual: June 12-14
Carilion Clinic Roanoke






 Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS - CRMH Clinical Nurse Specialist
Donna Bond, DNP, RN, CCNS, AE-C, CTTS, FCNS - CRMH Clinical Nurse Specialist







































 (takenfromarticleinTheRoanokerbyLizLong)
(takenfromarticleinTheRoanokerbyLizLong)