Fluorescent Nanoprobe for Peritoneal Metastases
Cell Membrane ‘Blebs’ –A New Pan-Cancer Focus?
Genetic Testing, Surveillance, Preventive Interventions for Pancreatic Cancer
Scaling New Heights
Translational Research is Here. What’s the Next Horizon?
BREAKTHROUGHS IN PATIENT CARE AND CANCER DISCOVERY

FALL 2023
PUSHING FORWARD AND SCALING NEW HEIGHTS
In cancer research and treatment, progress used to be unacceptably slow. Silos stifled collaboration between laboratory researchers and clinicians. Innovations tended to languish due to lack of translation and adoption in the clinic. And above all, there was the inescapable feeling that we weren’t serving our patients to the fullest.
Thankfully, the promise of translational research is coming true. Discoveries in the laboratory are accelerating into clinical applications. Meaningful collaborations between researchers and clinicians are now the norm, and multidisciplinary patient care is increasingly informed by the latest discoveries and breakthroughs.
We are definitely scaling new heights. The challenge now is to maintain our momentum, push forward, and continue to lead the way in cancer care and research excellence.
It is my pleasure to share with you in this issue of CancerAnswers@Simmons a showcase on how the researchers and clinicians at UT Southwestern Harold C. Simmons Comprehensive Cancer Center are doing just that.
I invite you to meet our featured faculty, Toral Patel, M.D. – page 4 – a researcher and neurosurgeon who is integrating her background in biomedical engineering with her patient-centered approach to clinical care of patients with brain tumors.
On page 6, you’ll read about impactful laboratory research published in Nature by Gaudenz Danuser, Ph.D., and Andrew D. Weems, Ph.D., that holds the potential to change how computational biology is enabling the discovery of genes that drive many types of cancer.
Read how our Pancreatic Cancer Prevention Program – page 12 – is intercepting pancreatic cancer before it fully develops using a combination of medical genetics, imaging, and comprehensive surveillance for patients at risk of developing this disease.
Discover these – and many more – examples of cancer research and care at the leading edge. I hope the following pages serve as a reminder of how far we’ve come and leave us all feeling inspired and reinvigorated for the fight toward continued advancement that lies ahead.
Sincerely,
CARLOS L. ARTEAGA, M.D.
 Director, Harold C. Simmons Comprehensive Cancer Center Associate Dean of Oncology Programs
X, formerly known as Twitter: @carlosarteagamd
Director, Harold C. Simmons Comprehensive Cancer Center Associate Dean of Oncology Programs
X, formerly known as Twitter: @carlosarteagamd
Innovation in Your Inbox
Scan the QR code to receive Cancer Answers and other Simmons Cancer Center updates via email.

2 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
4 Advancing the Treatment of Brain Tumors
Researcher and neurosurgeon Toral Patel, M.D., combines interests in engineering and medicine to fuel innovative treatments for malignant and benign brain tumors.
6 Therapeutic Targeting of Septin Proteins: A New Pan-Cancer Focus?
Researchers investigate inhibition of round membrane protrusions on cancer cells called “blebs” and associated septin protein assemblies as potential treatment focus.
8 Same-Day Clinic Streamlines Acute Care
Simmons Acute Care offers convenience to patients with urgent cancer-related symptoms or side effects, providing quality acute care not always available in emergency departments.
9 Combating Uveal Melanoma with New Treatments
A multidisciplinary team of experts in this common primary intraocular malignancy offers an innovative clinical program, backed by internationally known leadership and research.
10 Fluorescent Nanoprobe Produces ‘Breakthrough’ for Peritoneal Metastases
A pH-sensitive cancer therapy discovered at Simmons Cancer Center has been fast-tracked by the U.S. Food and Drug Administration for use as a real-time surgical imaging agent.
12 Pancreatic Cancer: Catching It Before It’s Too Late
A multidisciplinary care team provides preventive care, medical genetics, and surveillance plans for patients at risk for developing pancreatic cancer.
14
Lifelong Care for Pediatric Cancer Survivors
The After Cancer Experience (ACE) Program supports pediatric cancer survivors with holistic evaluations, seamless transitioning to adult care, and documentation that follows the patient.

16 News, Honors & Awards
Simmons Cancer Center spotlights people doing great work.
3 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
FALL 2023
Advancing the Treatment of Brain Tumors

Through her studies at Johns Hopkins, Yale New Haven Hospital, and Memorial Sloan Kettering Cancer Center, Toral Patel, M.D., learned from some of the top engineers and surgeons in the world. Now, as Director of the UT Southwestern Brain Tumor Program, she’s integrating her background in biomedical engineering with a patient-centric approach to clinical care.
“I chose the field of neurosurgery because I wanted to make a difference in the lives of critically ill patients,” Dr. Patel says. “I also wanted to combine my interests in engineering and discovery with medicine. It is a privilege to be a neurosurgical oncologist. I have the unique opportunity to help patients during some of the most difficult moments in their lives and to see them through to better health.”
Integral to that approach, she says, is the unique access to clinical trials available to patients at UT Southwestern Harold C. Simmons Comprehensive Cancer Center.
“Many brain tumor patients have conditions that are not readily curable, but there are often clinical trials available at academic medical centers like
UT Southwestern,” she says. For example, a current trial for recurrent glioblastoma utilizes catheters to infuse radiation-containing nanoparticles into the tumor – made possible, in part, by Dr. Patel’s prior research.
During her neurosurgery residency at Yale, she worked on developing nanoparticles and sizing them for infusion through catheters and into the brain. That work, published by the National Academy of Sciences a decade ago, contributed to the advancement of this type of clinical translation, she says. She holds a patent titled “Highly penetrative nanocarriers for treatment of CNS disease” related to her research into how nanoparticles can be used to carry drugs directly to the site of brain tumors.
In clinical settings, Dr. Patel strives to build strong relationships with her patients through what she calls the “art of medicine.” This includes personally calling patients with test results, conferencing with family members during hospital rounds, and establishing a
4 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
As both a researcher and a neurosurgeon, Toral Patel, M.D., is uniquely experienced to offer the highest level of care for patients with malignant or benign brain tumors.
level of trust that allows the patient to be receptive to participation in clinical trials.
“I want patients to feel like they have an advocate and someone they can trust in their health care journey,” she says. “I believe that building strong relationships with patients is absolutely fundamental to providing good clinical care. These patient-physician relationships ultimately impact clinical outcomes.”
NEURO ONCOLOGY CLINIC HAS NEW LOCATION WITH SEAMLESS ACCESS TO CARE AND CLINICAL TRIALS


Bringing together the expertise of surgeons, oncologists, and radiation oncologists, the multidisciplinary Neuro Oncology Clinic located in the new Cancer Care Outpatient Building (CCOB) at UT Southwestern Harold C. Simmons Comprehensive Cancer Center provides a one-stop shop for patients, says Michael Youssef, M.D., Assistant Professor of Neurology and Internal Medicine in the Division of Hematology and Oncology. Prior to the move to the new location, patients visited several buildings to see all of their neuro oncology providers.
The new location also has a dedicated floor for clinical trials, which Dr. Youssef says is helpful in considering patients for any relevant studies when they are newly diagnosed. He points to the global trial evaluating therapies for glioblastoma known as GBM AGILE, which has historically struggled to enroll patients at the time of diagnosis.
Toral Patel, M.D., is an Associate Professor of Neurological Surgery and Director of the Brain Tumor Program at UT Southwestern. She is a member of the Peter O’Donnell Jr. Brain Institute and Simmons Cancer Center, where she is part of the Experimental Therapeutics Research Program.
Toral Patel, M.D., Director of UT Southwestern’s Brain Tumor Program, echoes Dr. Youssef’s enthusiasm about the new level of access to clinical trials and emphasis on patient care. “I think the biggest benefit of having brain tumor patients seen at UT Southwestern is that they can receive care from various subspecialists and access to clinical trials in the same location,” she says. “It is a truly patient-centric approach.”

5 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
Magnetic resonance imaging (MRI) of the brain, brain tumor.
Therapeutic Targeting of Septin Proteins: A New Pan-Cancer Focus?
Research into cell configurations uncovers vulnerability that could be leveraged to treat multiple cancer types.
Cell membrane protrusions called “blebs” could contribute to anoikis resistance in melanoma, suggesting a source to target in potential treatments of this and other cancer types. Healthy cells that detach from larger tissues typically undergo a form of this programmed cell death. But malignant cells that detach have been shown to survive and spread, forming blebs indefinitely.
In melanoma cells, blebbing attracts septin proteins, which form molecular scaffolds for active mutant NRAS and effectors. These signaling hubs activate ERK and PI3K, both well-established promoters of pro-survival pathways in cancer cells. Interestingly, inhibition of blebs or septin assembly ultimately causes cell death.
New research published in Nature by Gaudenz Danuser, Ph.D., Chair of the Lyda Hill Department of Bioinformatics and Professor of Cell Biology at UT Southwestern, suggests that septin inhibition could be part of a new therapeutic intervention strategy for melanoma as well as other cancers. Dr. Danuser co-led the study with Andrew D. Weems, Ph.D., an Instructor of Bioinformatics and researcher in the Danuser Lab.
“Our old adage in biology is that form follows function. But here, we’re flipping that concept on its head,” Dr. Danuser says. “By changing the form, we’re showing that you can change chemical processes inside the cell that control their functions.”
6 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
Discovery of a New Target
The study initially focused on Ras-transformed melanoma. Ras family mutants are found in 30%-35% of cancers, and 30% of melanomas harbor a mutation in the NRAS gene. Locked in a constitutively active state, mutant NRAS signaling results in cellular hyperproliferation and the avoidance of cell death.
Despite their clinical importance, these oncoproteins have been notoriously difficult to target – there are no selective therapies currently available for NRAS mutants.
The researchers discovered that NRAS depends on a specific subcellular architecture to operate as an efficient oncoprotein. This yields the proposal that Ras-driven pathways can be attacked by modulation of cell morphological programs that determine NRAS’ penetrance as an oncogene. While BRAFdriven melanoma cells do not rely on blebs or septins under basal conditions, they observed that these cells became strongly bleb- and septin-dependent when treated with MAPK-inhibitor therapy.
“These findings show that ‘so-called’ oncogenic mutations alone are not sufficient to drive cancer functions, but that they may depend on specific cellular configurations to do so,” Dr. Danuser says. “On the other hand, promoting these cellular configurations alone can enable cancer-generating functions in perfectly healthy cells with no mutations, which offers a fundamentally new perspective of cancer development.”
Progress Toward Clinical Trials
Unpublished preclinical work at UT Southwestern has shown that a low toxicity agricultural chemical already approved by the Environmental Protection Agency effectively targets septin-signaling hubs in mouse models of cancer.
When the researchers treated melanoma cells with a compound that inhibits septins, called forchlorfenuron (FCF), the septins could no longer scaffold Ras proteins, resulting in an inability of the cells to sustain the chemical reactions that were keeping them alive.
“FCF has been used as an agricultural chemical in the U.S. for nearly 20 years,” Dr. Weems says. “This septin-inhibiting compound and its chemical derivatives could be promising candidates for new anti-cancer therapies.”
Based on these findings, Dr. Danuser and Dr. Weems are now looking for industrial partners interested in optimizing this therapeutic avenue or collaborating to create a de novo design and test novel inhibitors.
This study was funded by grants from the National Institutes of Health (R35 GM136428) and The Welch Foundation (I-1840-20200401).
The Board of Regents of The University of Texas System has filed for a patent on the therapeutic targeting of septins and blebbing, which was based in part on data from this study. Drs. Danuser and Weems, along with Erik S. Welf, Ph.D., and Meghan K. Driscoll, Ph.D., are named as inventors.
Gaudenz Danuser, Ph.D., is Chair of the Lyda Hill Department of Bioinformatics, Director of the Cecil H. and Ida Green Center for Systems Biology, Professor of Cell Biology, and a member of the Cellular Networks in Cancer Research Program at Simmons. His research interests include causal inference in molecular pathways, machine learning of cell dynamics, and regulation of cell morphogenesis in metastasis.

Andrew Weems, Ph.D., is a Jane Coffin Childs Fellow and Research Instructor with the Lyda Hill Department of Bioinformatics at UT Southwestern in the Danuser Lab. His research interests include the regulation of the septin cytoskeleton as well as cell morphological control of signaling and its influence on cancer disease progression, cancer drug resistance, and cell fate determination.

7 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
“Our old adage in biology is that form follows function. But here, we’re flipping that concept on its head. By changing the form, we’re showing that you can change chemical processes inside the cell that control their functions.” — GAUDENZ DANUSER, PH.D.
Same-Day Clinic Streamlines Acute Care
Simplifying Access and Care
Oncology providers at the clinic can deliver various forms of treatment, in many cases alleviating a patient’s symptoms without the need for inpatient admission. More advanced services can also be scheduled as needed.
“The efficiency has been incredible. A patient may walk in that morning, come see me, and we come up with a plan – all within a few hours’ time,” Ms. Charania says.
Simmons Acute Care (SAC) offers same-day appointments for patients of UT Southwestern Harold C. Simmons Comprehensive Cancer Center who are experiencing symptoms or side effects, such as nausea or an infection, that require urgent attention but are not immediately life-threatening.
“A beneficial difference in our model is that we staff our clinic with experts in providing oncology symptom management in an outpatient context,” says Sadaf Charania, M.P.A.S., PA-C, a board-certified physician assistant at Simmons Cancer Center, who leads SAC.
The Value Proposition
Providing same-day appointments for patients builds stronger relationships with providers and drives greater adherence to the treatment plan, Ms. Charania says.

“Ultimately, we want to get these patients managed as soon as possible with a clinician who has expertise in treating that symptom,” she adds. “Another main purpose of this patient-centric initiative is to keep patients out of the Emergency Department (ED) who do not need to be there.”
From August 2020 to May 2023, SAC provided care to 3,511 patients. An analysis found that 65% of patients were discharged home, 22% were admitted to an inpatient setting for a higher level of care, and 12% were transferred to the ED. Sepsis was the most common reason for an ED transfer.
“We anticipate that the community will become more familiar with us, and more patients will seek us out directly,” Ms. Charania says. “It’s one way of helping to simplify access and care, which is a huge part of our mission at Simmons.”
8 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
Oncology experts can provide prompt specialized care not always available in emergency departments.
Sadaf Charania, M.P.A.S., PA-C, is a board-certified physician assistant at Simmons Cancer Center who leads Simmons Acute Care.
Combating Uveal Melanoma with New Treatments
Novel research, clinical initiatives aim to improve care for a rare but deadly eye cancer.

UT Southwestern Harold C. Simmons
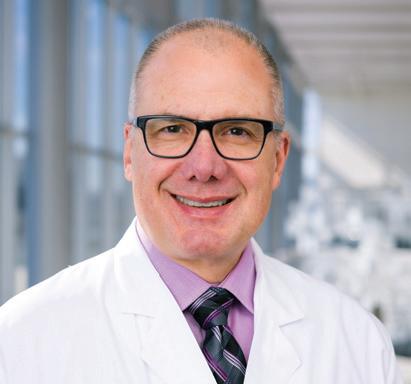
Comprehensive Cancer Center is a leader in the diagnosis and treatment of uveal melanoma, the most common primary intraocular malignancy. J. William Harbour, M.D., who was recruited to UT Southwestern as Chair and Professor of Ophthalmology in 2021, is an internationally recognized authority on uveal melanoma. His team is involved with innovative research and clinical initiatives aimed at transforming the treatment and outcomes of patients with this lifethreatening malignancy.
“Among National Cancer Institute-designated cancer centers, we are one of only a few with a dedicated multidisciplinary clinical and research program in uveal melanoma,” Dr. Harbour says. “We offer the latest standard of care and innovative clinical trials, making it as seamless as possible to deliver new treatments to our patients.”
Diagnosis and Treatment
Uveal melanoma represents approximately 5% of all melanoma diagnoses. Dr. Harbour says that patients often have questions about their diagnosis and life expectancy, which depend on a number of factors including the genetic subtype of their melanoma. Simmons Cancer Center’s unique care model facilitates seamless transition between different specialties to align with each patient’s unique treatment plan.
“Treating uveal melanoma requires a multidisciplinary approach. Treatment may include laser therapy, brachytherapy, surgery for primary disease of the eye, ongoing imaging surveillance for
multiple years to monitor for distant spread to the liver or other organs, and systemic chemotherapy. It is also important to consider participation in a clinical trial to evaluate new therapies,” explains Sanjay Chandrasekaran, M.D., Assistant Professor of Internal Medicine in the Division of Hematology and Oncology at UT Southwestern.
Advancing Clinical Trials
With many potential therapies being advanced, there are now more opportunities than ever to enroll in a clinical trial. As a pioneer in uveal melanoma research, Dr. Harbour is the Principal Investigator on several clinical trials to improve outcomes for patients with localized disease. In the adjuvant and metastatic setting, Dr. Chandrasekaran is leading trials with new systemic therapies.
“We have a range of clinical trials to enhance our ability to offer each patient the best option for them,” Dr. Harbour says. “It’s important to enroll patients in clinical trials to improve the likelihood that they will benefit from new discoveries and treatments.”
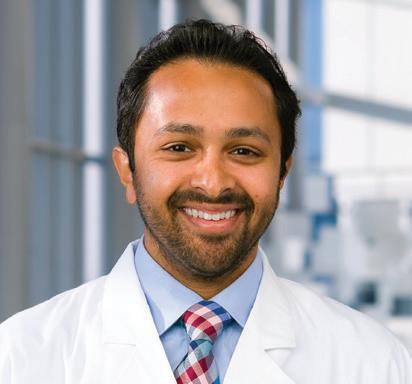
J. William Harbour, M.D., is Chair and Professor of Ophthalmology at UT Southwestern. He is a member of the Cellular Networks in Cancer Research Program at Simmons Cancer Center. His clinical and research interests focus on ocular tumors such as uveal melanoma, retinoblastoma, and lymphoma as well as the use of genomic technologies to better understand, diagnose, and treat eye cancers.
Sanjay Chandrasekaran, M.D., is Assistant Professor of Internal Medicine in the Division of Hematology and Oncology, an affiliate member of the Experimental Therapeutics Research Program at Simmons Cancer Center, and a Eugene P. Frenkel, M.D., Scholar in Clinical Medicine. He specializes in the care of patients with melanoma, advanced skin cancer, and soft tissue and bone sarcomas.
9 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
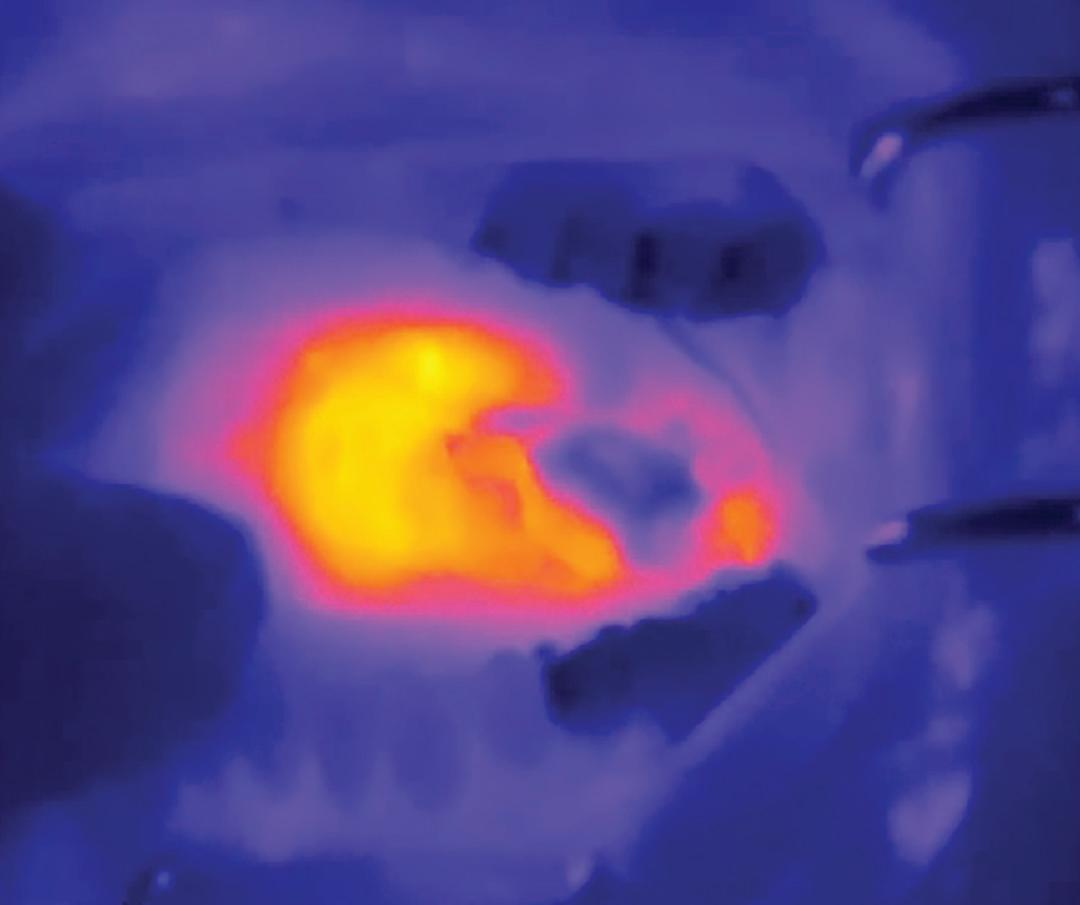
Fluorescent Nanoprobe Produces ‘Breakthrough’ for Peritoneal Metastases
Nanotechnology produces ‘glow’ effect that enhances visibility of tumor edges, allowing surgeons to remove more cancer cells than standard imaging technology.
ApH-sensitive cancer therapy discovered at UT Southwestern Harold C. Simmons Comprehensive Cancer Center has been fast-tracked by the U.S. Food and Drug Administration for use as adjunct for visualization of metastases in the peritoneal cavity.
The real-time surgical imaging agent, called the fluorescent nanoprobe, uses nanotechnology to detect acidity and make the edges of solid metastatic tumors glow during cancer surgery. The enhanced visibility
allows surgeons to remove cancer cells throughout the abdomen at 50%-60% higher rates than standard imaging technology.
The fluorescent nanoprobe technology was developed by pharmacologist and distinguished researcher Jinming Gao, Ph.D., Professor at Simmons Cancer Center and of Pharmacology, Otolaryngology – Head and Neck Surgery, and Cell Biology, and Baran Sumer, M.D., Professor of Otolaryngology – Head and Neck Surgery. It is just the third imaging agent to receive the FDA’s Breakthrough Therapy Designation.

Early data from a phase two clinical trial shows the nanoprobe identifies 10 times more metastatic cancer cells than the FDA’s minimum 5% threshold for successful detection.
“In animal models, we saw that we could detect cancers down to a half-millimeter. We didn’t necessarily expect that level of specificity in human samples, but that’s what we got. It was a very, very nice surprise,” says Dr. Sumer.
The nanoprobe is delivered through an IV about 24 hours before surgery. As the imaging agent pegsitacianine circulates through the body, it “digitizes” the acidic signals from cancer cells. The nanoprobe is switched “off” while circulating in normal pH and turns “on” when the sensors detect acidity. When switched “on,” dissociated cationic polymers attach to the cancer cells, lighting them up under near-infrared light.
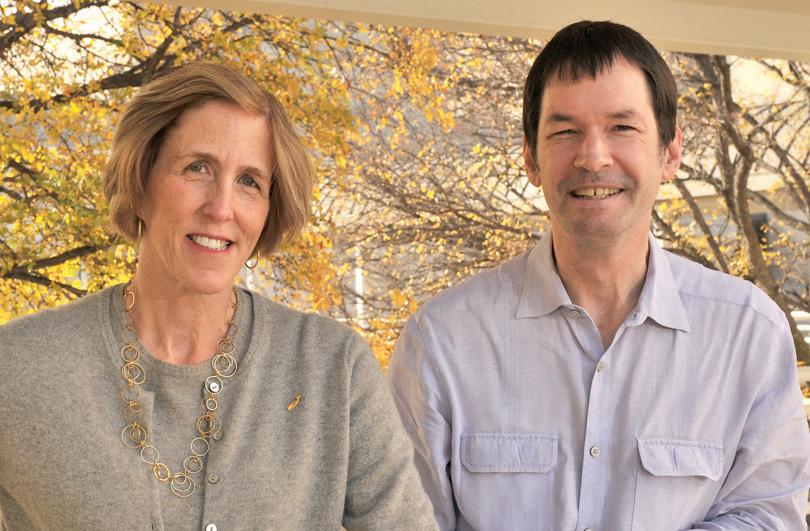
Baran Sumer, M.D., left, and Jinming Gao, Ph.D., discovered that the fluorescent nanoprobe technology detects cancers down to a halfmillimeter, performing just as well as the animal models in what Dr. Sumer called “a very, very nice surprise.”
10 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
Using an intraoperative camera, the surgeon can better visualize the glowing cells and remove them with extreme precision. Pegsitacianine is designed to light up quickly in an acidic environment and also to be compatible with cameras integrated into surgical suites, including the da Vinci robot system.
Expanding Cancer Targets in the Future
Because the nanoprobe technology targets the Warburg effect, it is tumor-agnostic and could potentially be used in other forms of cancer.
Besides an award to study peritoneal metastasis, the National Cancer Institute has awarded UT Southwestern a clinical R01 grant to study the use of the nanoprobe to locate unknown primary cancer in the head and neck. That trial is scheduled to open this year.
OncoNano Medicine Inc., a startup co-founded to commercialize the technology, has received a Small Business Innovation Research (SBIR) grant to further
develop the technology and conduct a phase three clinical trial for metastatic peritoneal tumors. Once it earns FDA approval, the trial will be held at multiple U.S. centers, including UTSW.
Next up for the nanoprobe are two adaptations of the technology being tested in human studies:
• A “nanovaccine” that trains the immune system to produce tumor-specific T cells to target the adaptor protein STING (stimulator of interferon genes) to initiate an immune response against the cancer.
• Reversing the Warburg effect to neutralize the acidic tumor environment and keep the immune system functional to eliminate cancer cells.
At UT Southwestern, Dr. Gao and Dr. Sumer are continuing to push forward with research and creating more clinical applications for the nanoprobe.
Drs. Gao and Sumer each have financial interests in OncoNano Medicine Inc., as does UT Southwestern.
Baran Sumer, M.D., is Professor of Otolaryngology – Head and Neck Surgery and Chief of the Division of Head and Neck Oncology at UT Southwestern. He specializes in head and neck cancer surgery and reconstruction. Dr. Sumer is a member of the Experimental Therapeutics Research Program at Simmons Cancer Center.

Jinming Gao, Ph.D., is a Professor at Simmons Cancer Center and of Pharmacology, Otolaryngology – Head and Neck Surgery, and Cell Biology. His lab studies the science of nanotechnology and cancer. Dr. Gao is a member of the Experimental Therapeutics Research Program at Simmons Cancer Center.

11 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
The nanoprobe is delivered through an IV about 24 hours before surgery. As the imaging agent pegsitacianine circulates through the body, it “digitizes” the acidic signals from cancer cells.
The fluorescent nanoprobe uses novel pH-sensitive nanotechnology to detect acidity and make the edges of solid metastatic tumors glow during cancer surgery.
Pancreatic Cancer: Catching It Before It’s Too Late
Highly experienced, multidisciplinary care team offers hope for patients.
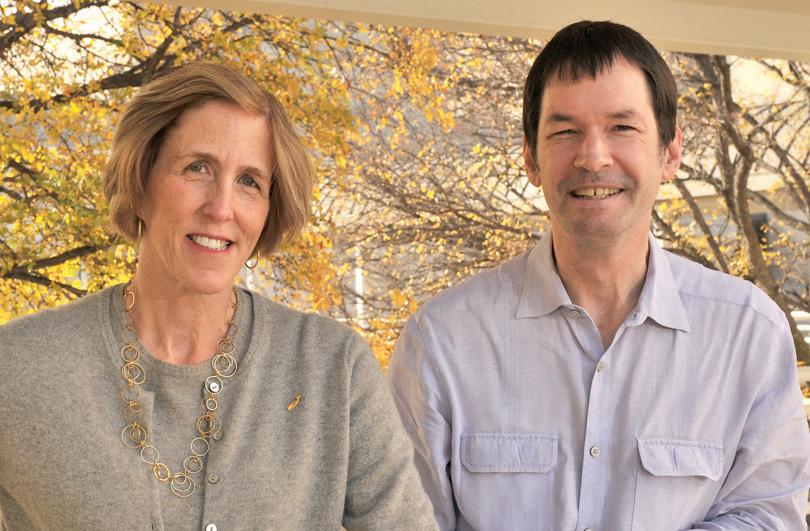
Developing better approaches to prevent pancreatic cancer is becoming increasingly urgent as incidence of the disease rises, particularly among younger patients.

“Pancreatic cancer is not like other cancers, where early detection is associated with long-term survival. Even tumors found in the early stages may be linked with a poor prognosis,” says John Mansour, M.D., Professor of Surgery in the Division of Surgical Oncology at UT Southwestern. “The aim is to identify the precancerous lesions early and remove them before they transform into cancer.”
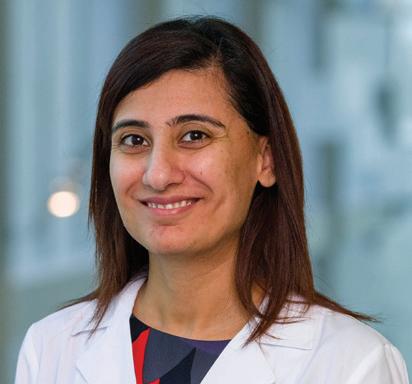
Dr. Mansour, along with Nisa Kubiliun, M.D., Associate Professor of Internal Medicine, and a team of providers, care for patients in the Pancreatic Cancer Prevention Program at UT Southwestern Harold C. Simmons Comprehensive Cancer Center. The program offers specialized care for those who have been diagnosed with a pancreatic cyst, have an inherited genetic susceptibility, or have a family history of pancreatic cancer.
Benefits of Multidisciplinary Care
A unique aspect of the program is truly multidisciplinary care, which not only offers patients the greatest level of support but also simplifies the many practical issues that arise when battling this disease.
In recent years, studies have shown that pancreatic cancer is frequently associated with inherited gene mutations (e.g., BRCA, ATM, CDKN2A), and the risk of familial disease rises exponentially with the number of first-degree relatives with pancreatic cancer. Current national guidelines recommend genetic counseling and multigene germline testing for all patients with pancreatic cancer.
12 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
“Getting a biopsy, going for appropriate scans, consulting with medical genetics, and arranging appointments with multiple experts can take a significant amount of time,” Dr. Kubiliun explains. “At Simmons, we streamline these efforts with care coordinators and patient navigators, which contributes to an efficient and patientcentered experience.”
As a result of the multidisciplinary approach, patients and their families often report feeling much more comfortable, since records and images are collected ahead of time, and all relevant practitioners work together in one place, Dr. Mansour notes.


Delivering a Distinct Care Experience
The pancreatic cancer prevention team then can create a comprehensive surveillance or treatment plan for each patient in a single visit. “With our unique surveillance approach, patients can often avoid chemotherapy and radiation entirely. If we catch it early, we can prevent the disease,” Dr. Mansour adds.
If indicated, patients in the program may be referred to Simmons Cancer Center’s Cancer Genetics Program for a comprehensive evaluation and risk assessment. Genetic testing helps to characterize risk, and genetic counseling gives families information so they understand their options. In most cases, this visit can be coordinated at the same time as their prevention appointment.
“It is often important for first-degree family members to receive genetic testing,” Dr. Mansour explains. “With the results, we can develop a personalized plan tailored to the specific genetic mutation and patient risk factors in accordance with current guidelines.”
Driving Practice Change
There is a paucity of data on optimal practice standards, particularly for individuals at high risk of developing pancreatic cancer, Dr. Mansour says. While current national guidelines recommend that diagnostic management and assessment of resectability of the cancer should involve multidisciplinary consultation at high-volume centers, the most appropriate intervals for imaging studies and the impact of comorbidities (e.g., diabetes) remain uncharacterized.
The team at UT Southwestern is collecting and analyzing data from the program, which started more than five years ago, with the aim of developing protocols that could inform practice globally in the coming years.
Looking ahead, the program’s leaders expect it to remain one of the highest-volume programs in the country that continues to pioneer unique care approaches. “Changing clinical practice is a difficult process, but we’re excited to use our local data to take on that challenge,” Dr. Kubiliun says.
John Mansour, M.D., is a Professor of Surgery, Division of Surgical Oncology, and Vice Chair of Quality in the Department of Surgery at UT Southwestern
He treats patients with malignancies of the stomach, pancreas, liver, bile duct, and other abdominal organs as well as the diverse population of sarcoma patients. Dr. Mansour is a member of the Development and Cancer Research Program at Simmons Cancer Center.
Nisa Kubiliun, M.D., is an Associate Professor of Internal Medicine at UT Southwestern and serves as Clinical Chief of the Division of Digestive and Liver Diseases. She also is the Medical Director of Endoscopy Services, where she employs advanced endoscopic techniques to treat a variety of gastrointestinal disorders and cancers. Dr. Kubiliun is a member of the Population Science and Cancer Control Research Program at Simmons Cancer Center.

13 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
Lifelong Care for Pediatric Cancer Survivors
More than 80% of children treated for cancer will survive long term. However, monitoring short- and long-term sequalae is an ongoing challenge.
“By the age of 27, nearly one in three childhood cancer survivors will develop at least one comorbidity or chronic condition, such as subsequent malignancies, heart failure, cardiomyopathy, stroke, hormone deficiencies, tumors like meningiomas, or neurological issues,” says Daniel Bowers, M.D., Professor of Pediatrics at UT Southwestern, Medical Director of Pediatric Neuro-Oncology at Children’s Health, and Medical Director of the After Cancer Experience (ACE) Program.
The ACE Program, a partnership between UT Southwestern Harold C. Simmons
Comprehensive Cancer Center and Children’s Health, aims to address the unique and substantial needs of childhood cancer survivors following completion of therapy through adulthood.

Personalized Survivorship Care
As part of its long-term follow-up care model, the ACE Program offers personalized survivorship care; holistic, evidence-supported, risk-based evaluations and assessments of support needs; smooth referrals when necessary; seamless transitioning to adult care; communication with primary care providers; and ongoing support from the ACE team even after patients transition to adult care.
Rebecca Eary, D.O., M.P.H., Assistant Professor of Family and Community Medicine at UT Southwestern, directs the Adult Survivorship Program for Simmons Cancer Center.
“We’re screening for subsequent cancers, cardiac disease, and more, plus providing referrals for integrative behavioral health and psychooncology and promoting preventive health habits,” Dr. Eary says.
Dr. Eary’s group offers a 40- to 60-minute survivorship-focused visit to discuss the patient’s risk level for long-term effects of prior cancer treatment, reduction of modifiable risks, and recommended medical tests. Screening for psychological support and special needs is also conducted at every visit.
14 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
The After Cancer Experience (ACE) Program builds a solid foundation for long-term surveillance and treatment.
The treatment summary that emerges becomes part of the patient’s record. Dr. Eary says that without this, primary care physicians would likely not have these screenings on their radar.
Continued ACE Care or Warm Handoff
Patients may elect to have just one visit, with the resulting history transferred to another primary care physician, or they may choose to continue with Dr. Eary or her colleagues as their primary care and survivorship physicians.
The ACE screening recommendations are modeled on long-term follow-up care guidelines from the Children’s Oncology Group, a National Cancer Institutesupported clinical trials group. Depending on the specifics of the patient’s cancer treatment – including type, agents, dosage, and treatment site – surveillance may prompt evidence-based screenings, such as annual echocardiograms and earlier mammography or breast MRIs, colonoscopies, or chest imaging.
Two Locations for Accessing Care
Patients can access the adult ACE survivorship clinic at two locations: UT Southwestern’s Moncrief Cancer Institute in Fort Worth or UT Southwestern’s main campus in Dallas.
Daniel Bowers, M.D., is a Professor of Pediatrics in the Division of Hematology and Oncology at UT Southwestern. He is Medical Director of Pediatric Neuro-Oncology at Children’s Health and Medical Director of the After Cancer Experience Program for childhood cancer survivors. He is a member of the Experimental Therapeutics Research Program at Simmons Cancer Center.
REPRODUCTIVE PRESERVATION TALKS START EARLY
The ACE Program provides patient education and options for fertility preservation from the beginning of treatment.
“We start our journey of discussing risks of infertility early on, even at the time of diagnosis,” says Ksenya Shliakhtsitsava, M.D., M.A.S., a pediatric oncologist and Assistant Professor of Pediatrics who leads the team’s fertility preservation efforts.
Dr. Shliakhtsitsava talks with patients about their infertility risks and options, which include harvesting and freezing eggs or sperm. For female patients, an ovary may also be frozen and banked, and for young male patients,
Rebecca Eary, D.O., M.P.H., is an Assistant Professor of Family and Community Medicine at UT Southwestern and Director of the Adult Survivorship Program. She is an affiliate member of the Population Science and Cancer Control Research Program at Simmons Cancer Center.

Ksenya Shliakhtsitsava, M.D., M.A.S., is an Assistant Professor of Pediatrics, Division of Pediatric Hematology and Oncology. She is also a Dedman Family Scholar in Clinical Care. She leads the oncofertility program at Children’s Health and is part of the survivorship team. Dr. Shliakhtsitsava is an affiliate member of the Population Science and Cancer Control Research Program at Simmons Cancer Center.

a section of testicular tissue may be frozen. Restoring fertility via reimplantation of this tissue is still considered experimental in the United States, but Dr. Shliakhtsitsava hopes to see it approved by the time current patients reach adulthood.
At Children’s Health, survivors can enroll in clinical trials through the Children’s Oncology Group, which is investigating the role of healthy habits like exercise in preventing disease. Children’s Health is also an original member of the Childhood Cancer Survivor Study expansion cohort, contributing robust data on birth defects and reproductive risks.
Through her research, Dr. Shliakhtsitsava is assessing patient knowledge of reproductive risk and designing interventions to improve patient education and access to care.
Partnering with the Simmons Cancer Center Cardio-Oncology Clinic, her team contributes its growing body of data to an ongoing translational quality improvement initiative.
“We are continually applying what we learn to systematically improve outcomes, raise cure rates, improve quality of survivorship, and provide a better overall experience for our patients and families,” she says.

15 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
UTSW, CHILDREN’S HEALTH TO LEAD MULTICENTER CLINICAL TRIAL ON VITAS
from the front lines of cancer care
UT Southwestern Harold C. Simmons
Comprehensive Cancer Center and Children’s Health will lead a national multicenter clinical trial on VITAS – Vincristine, Irinotecan, Temozolomide, and Atezolizumab in Solid Tumors – for pediatric cancer patients whose tumors have not responded to first-line treatments or have recurred.

Checkpoint inhibitor immunotherapy has made huge strides in several adult cancers, but some cancers don’t respond to checkpoint inhibitors delivered as single agents. Researchers have had some success in
combining these drugs with chemotherapies. In children, checkpoint inhibitors alone have shown little success with solid tumors.
“By enhancing immunotherapy with chemotherapy, a strategy we’ve seen succeed in clinical trials for adults with cancer, we’re hoping to see the same success in children,” says Matthew Campbell, M.D., Assistant Professor of Pediatrics in the Division of Hematology and Oncology. “What we learn from this clinical trial will help us continue to move the needle toward more children surviving these cancers.”
HONORS | MEMBERS OF HAROLD C. SIMMONS COMPREHENSIVE CANCER CENTER
ARTEAGA NAMED
AS KOMEN RESEARCH SCHOLAR
Carlos L. Arteaga, M.D., Director of the Harold C. Simmons Comprehensive Cancer Center and Associate Dean of Oncology Programs at UT Southwestern, has been named a Komen Scholar for Susan G. Komen. Dr. Arteaga is one of nine new Komen Scholars who will help guide the organization’s breast cancer research programs. He is internationally recognized for his work in laboratory-based translational research and advancing the care of breast cancer patients.
MORRISON ELECTED TO EUROPEAN MOLECULAR BIOLOGY ORGANIZATION
Stem cell biologist Sean J. Morrison, Ph.D., Howard Hughes Medical Institute Investigator and founding Director and Professor of the Children’s Medical Center Research Institute at UT Southwestern (CRI), has been elected by his peers as an associate member of the European Molecular Biology Organization (EMBO). Dr. Morrison studies the cellular and molecular mechanisms that regulate stem cell function and the role these mechanisms play in cancer. He is a member of the Development and Cancer Research Program at Simmons Cancer Center.
COLE BECOMES ASCO FELLOW


Suzanne Cole, M.D., Assistant Professor of Internal Medicine in the Division of Hematology and Oncology, has received recognition as a Fellow of the American Society of Clinical Oncology (FASCO). FASCO distinction recognizes American Society of Clinical Oncology (ASCO) members for their extraordinary volunteer service, dedication, and commitment to ASCO. Dr. Cole is the Medical Director of Community Oncology at Simmons Cancer Center and leads the Community Oncology Disease-Oriented Team. She is a member of the Experimental Therapeutics Research Program.
PAN ELECTED TO NATIONAL ACADEMY OF SCIENCES
Duojia Pan, Ph.D., has been elected to the National Academy of Sciences, one of the highest honors for American scientists. The Pan Lab investigates the molecular mechanisms of growth control and tissue homeostasis. Dr. Pan is a member of the Cellular Networks in Cancer Research Program at Simmons Cancer Center.

UT Southwestern now has 26 faculty who are members of the National Academy of Sciences, more than any other institution in Texas.

NEWS, HONORS + AWARDS
16 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
from the front lines of cancer care
ROSS PRIZE AWARDED TO TWO UTSW GENETICISTS
The Feinstein Institutes for Medical Research has selected two scientists from UT Southwestern, Helen H. Hobbs, M.D., and Jonathan C. Cohen, Ph.D., to receive the 10th annual Ross Prize in Molecular Medicine for groundbreaking research in dyslipidemias and metabolic liver disease. The duo was the first to discover the genetic cause of fatty liver disease in humans, and their ongoing work has led to a new class of cholesterol-lowering drugs.
Kidney Cancer Program Celebrates 10th Anniversary
UT Southwestern’s Kidney Cancer Program celebrated its 10-year anniversary with a faculty symposium featuring more than 60 speakers. Topics included a first-in-class drug, now FDA approved, as well as groundbreaking discoveries about the genetics of kidney cancer, invasion and metastases, tumor latency, metabolism, and rare tumor types.
“This is an important milestone for the Kidney Cancer Program, and I cannot think of a better way to celebrate it than with a symposium featuring the many faculty at UTSW whose research and contributions are advancing the care of our patients,” says James Brugarolas, M.D., Ph.D., Director of the Kidney Cancer Program and Professor of Internal Medicine.
The Kidney Cancer Program at UT Southwestern Harold C. Simmons Comprehensive Cancer Center is one of only two National Cancer Institute-designated Specialized Programs of Research Excellence (SPORE) in kidney cancer. Established in 2013, the program has become one of the largest kidney cancer efforts worldwide.
Successful Expansion at Richardson/ Plano Location
UT Southwestern Harold C. Simmons Comprehensive Cancer Center completed a multiphase project to expand and renovate infusion services at the Medical Center at Richardson/Plano location.


The yearlong project revamped the existing infusion areas to add more private rooms, community infusion space, and new fasttrack chairs.
UT Southwestern Medical Center has joined an elite Honor Roll of the nation’s top 20 hospitals recognized for delivering the highest standard of care, according to U.S. News & World Report’s Best Hospitals listings for 2023-24. Eleven UT Southwestern medical specialties are nationally ranked, including cancer. UT Southwestern Harold C. Simmons Comprehensive Cancer Center is ranked among the top 20 cancer centers in the nation at No. 19. UT Southwestern’s William P. Clements Jr. University Hospital is now ranked as the No. 1 best hospital in Texas (tied) and, for the seventh year in a row, No. 1 in Dallas-Fort Worth – the nation’s fourth-largest metro area.

The redesigned clinic not only boosts capacity but also better aligns the look and feel of the Richardson/Plano location with the Cancer Care Outpatient Building in Dallas, which opened on the main campus last November.
Simmons Cancer Center sees patients in four locations in the Dallas-Fort Worth area, including the main campus in Dallas, southwest Dallas County/RedBird, Fort Worth, and Richardson/ Plano. We offer the same National Cancer Institutedesignated comprehensive cancer care at all of our sites of service.
NEWS, HONORS + AWARDS 17 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
SIMMONS NAMED AMONG TOP 20 CANCER CENTERS IN NATION
from the front lines of cancer care
Key Research Grants
TODD AGUILERA, M.D., PH.D.
Early Response to Radiotherapy and Immunotherapy in Rectal Cancer: An Integrated Molecular, Cellular, and Spatial Approach National Cancer Institute
LARRY ANDERSON, M.D., PH.D. Multiple Myeloma Research Consortium Site Investment Grant Multiple Myeloma Research Foundation
ABD EL KAREEM AZAB, PH.D.
Recruitment of Rising Stars Cancer Prevention and Research Institute of Texas
LAURA BANASZYNSKI, PH.D.
Characterizing the Role of Novel H3.3 Interacting Proteins in Enhancer Activation
Robert A. Welch Foundation
KENNETH CHEN, M.D.
Targeting Proteasome and mTOR Pathways in ActinomycinResistant Wilms Tumors The Pablove Foundation
SUZANNE CONZEN, M.D. Fellowship (Predoc: M.E. Hofstad) Elucidating Mechanisms of Therapy Response in BRCA2 Mutant Prostate Cancers National Cancer Institute
LINDSAY COWELL, PH.D.
i-AKC: Integrated AIRR Knowledge Commons National Institute of Allergy and Infectious Diseases
GAUDENZ DANUSER, PH.D.
Computational Models of Morphology-Controlled Cell Signal Transduction
Robert A. Welch Foundation
The following list features grants awarded to Harold C. Simmons Comprehensive Cancer Center members from December 2022 to July 2023 for research that is entirely cancer-specific:
Fellowship (Postdoc: G.M. Gihana) Cell Morphological Regulation of Oncogenic Ras Signaling Howard Hughes Medical Institute
ANTHONY DAVIS, PH.D.
Evaluation of the Cellular and Molecular Responses of Lung and Liver Cells Derived from iPSCs With Varying Intrinsic Radiosensitivity to Space Radiation NASA Johnson Space Center
BENJAMIN DRAPKIN, M.D., PH.D. Circulating Tumor Cell-Derived Xenografts of Small Cell Lung Cancer via the TellDx Platform National Foundation for Cancer Research
DAVID GERBER, M.D. Establish the Accelerating Clinical Oncology Research Network – Texas, ACORN-TX to Enhance Clinical Trial Access in North and Central Texas Cancer Prevention and Research Institute of Texas
Transferring Care to Enhance Access to EarlyPhase Cancer Clinical Trials Stand Up To Cancer
GERTA HOXHAJ, PH.D.
Regulation of Cancer Cell Migration Through the Purine-Dependent Control of Serine Synthesis American Cancer Society
EMINA HUANG, M.D., M.B.A. The Role of Cancer-Associated Fibroblasts in the Pathogenesis of Hispanic EO CRC American Society of Colon and Rectal Surgeons
HUOCONG HUANG, M.D., PH.D.
Function of Mesothelial Cells in the Tumor Microenvironment of Pancreatic Ductal Adenocarcinoma National Cancer Institute
RODNEY INFANTE, M.D., PH.D. Changes in Tumor Microenvironment That Promote Cachexia Cancer Prevention and Research Institute of Texas
JENNA JEWELL, PH.D. mTORC1 Regulation by Upstream Stimuli National Institute of General Medical Sciences
Phosphorylation and Inhibition of mTORC1 by PKA
Robert A. Welch Foundation
JANE JOHNSON, PH.D.
Mechanisms Controlling the Progression of Prostate Adenocarcinoma to Neuroendocrine Cancer
U.S. Department of Defense
RALF KITTLER, PH.D., AND ESRA AKBAY, PH.D.
Development of a RUVBL1/2 Inhibitor as a Radiosensitizer and Immune Stimulator for NonSmall Cell Lung Cancer, NSCLC National Cancer Institute
MATTEO LIGORIO, M.D., PH.D. Fellowship (Postdoc: G. Pontecorvi) Shifting the Paradigm of Pancreatic Cancer
Progression: Unveiling the Role of Pancreatic Enzymes American-Italian Cancer Foundation
GLEN LISZCZAK, PH.D.
Fellowship (Predoc: M. McConville) Unexpected Mechanism Underlying Mislocalization of ThrombocytopeniaAssociated ETV6 Point Mutation National Heart, Lung, and Blood Institute
LI LIU, PH.D.
Fellowship (Postdoc: T. Wang) Heme-Targeting Agent and Immunotherapy Combinations in Renal Cell Carcinoma
U.S. Department of Defense
SIQI LIU, PH.D. Recruitment of First-Time Tenure-Track Faculty Member Cancer Prevention and Research Institute of Texas
Innate Immune Regulation of Wound Re-Epithelialization National Institute of Arthritis and Musculoskeletal and Skin Diseases
RAVIKANTH MADDIPATI, M.D. Developing a Novel Optogenetic Recombinase System to Study and Target Metastatic Cancer Cancer Prevention and Research Institute of Texas
ANANTH MADHURANTHAKAM, PH.D.
Next-Generation WholeBody MRI for Detection and Assessment of Therapy Response in Bone Lesions National Institute of Arthritis and Musculoskeletal and Skin Diseases
NEWS, HONORS + AWARDS
18 CancerAnswers@Simmons FALL 2023 UTSWMED.ORG/CANCER
from the front lines of cancer care
SUKH MAKHNOON, PH.D., M.S. Cultural Adaptation of Family Talk to Improve Family Communication in Genetics Collaborative Group of the Americas on Inherited Colorectal Cancer
RAM MANI, PH.D.
Characterization of 3D Genome Organization and Transcriptional Regulation in Prostate Cancer Cancer Prevention and Research Institute of Texas
ELISABETH MARTINEZ, PH.D.
Overcoming Jumonji KDM4A Oncogenic Function in SCLC, Small Cell Lung Cancer U.S. Department of Defense
Post-Translational Modifications
Control JARID Enzyme Activity During DNA Damage National Cancer Institute
SAMUEL MCBRAYER, PH.D.
Development and Evaluation of Lanosterol Synthase Inhibitors in Preclinical GBM Models Cancer Prevention and Research Institute of Texas
Exploiting Synthetic Lethality
With IDH Mutations for Oligodendroglioma Therapy Oligo Nation
DAVID G. MCFADDEN, M.D., PH.D. Fellowship (Postdoc: C.C. Arregui) Nutrient-Regulated Posttranslational Modifications Drive Metastasis Formation Human Frontier Science Program
Identifying Metabolic Dependencies in Hurthle Cell Carcinoma of the Thyroid National Cancer Institute
JOSHUA MENDELL, M.D., PH.D.
The Role of Long Noncoding RNA CRNDE in Normal Physiology and Cancer National Cancer Institute
Fellowship (Postdoc: M.L. Norris) Regulation and Function of Subcellular RNA Localization in Neural Crest Cells and Their Derivatives National Institute of Child Health and Human Development
SEAN MORRISON, PH.D.
Fellowship (Postdoc: H.F. Alkan) Metabolic Regulation of Immunogenicity and Metastasis Cancer Research Institute
KATHRYN O’DONNELLMENDELL, PH.D.
Fellowship (Postdoc: S. Thomas-Jardin) Immune Checkpoint Regulation by the Integrated Stress Response Pathway in Lung Cancer National Cancer Institute
The Role of Translation Initiation Factor eIF5B in Lung Cancer Pathogenesis National Cancer Institute
MICHAEL ROSEN, PH.D. Establish New Cryo-EM Core Services to Drive Cancer Research and Drug Discovery at UTSW Medical Center Cancer Prevention and Research Institute of Texas
STEPHEN SKAPEK, M.D., AND LIN XU, PH.D.
Nominating Vulnerabilities in Fusion Oncoprotein-Driven Rhabdomyosarcoma National Cancer Institute
DOUGLAS STRAND, PH.D. Interstitial Fibroblasts Drive Prostate Branching Morphogenesis National Institute of Diabetes and Digestive and Kidney Diseases
ANNA TAVAKKOLI, M.D., M.SC. Evaluation of Multi-Level Factors Associated With Post-ERCP Outcomes National Institute of Diabetes and Digestive and Kidney Diseases
LANCE TERADA, M.D. Autophagy and Tumor Endothelium Cancer Prevention and Research Institute of Texas
ROBERT TIMMERMAN, M.D. Mechanistically Dissecting Glycolysis Regulation by Lactate and Its Therapeutic Potential in Cancer National Cancer Institute
RICHARD WANG, M.D., PH.D. Regulation and Function of Viral and Endogenous Circular RNA in Cancer National Cancer Institute
TAO WANG, PH.D.
Developing Knowledge Guided Deep Learning Models to Predict the Binding between T Cell Receptors and Neoantigens for Facilitating TCR-T Therapies Cancer Prevention and Research Institute of Texas
SIHAN WU, PH.D.
Understanding the Molecular Mechanisms of Extrachromosomal DNA Segregation in Cancer Gilead Sciences
QING ZHANG, PH.D. Fellowship (Postdoc: J. Zhou) RBM39-DGAT1 Axis Is an Oncogenic Driver in Clear Cell Renal Cell Carcinoma American Association for Cancer Research
A New Histone H3 Modification Regulates Epigenetic Programming and Gene Expression in Breast Cancer National Cancer Institute
SIYUAN ZHANG, M.D., PH.D.
Understanding Anticancer Immune Responses Induced by Golden ICG During Photothermal Treatment Lyda Hill Foundation
XUEWU ZHANG, PH.D.
Structure and Regulatory Mechanism of the DeathAssociated Protein Kinase 1 Robert A. Welch Foundation
XUEWU ZHANG, PH.D.; XIAOCHEN BAI, PH.D.; AND CHUO CHEN, PH.D. Novel Regulatory Mechanisms and Agonists of STING National Cancer Institute
ZHENYU ZHONG, PH.D.
Investigating the Mechanism of NLRP3 Inflammasome Hyperactivation During Hepatocellular Carcinoma Development Cancer Prevention and Research Institute of Texas
HAO ZHU, M.D.
Understanding the Impact of Immunity on Pre-Malignant Somatic Mosaicism and Cancer Prevention Cancer Prevention and Research Institute of Texas
19 UTSWMED.ORG/CANCER FALL 2023 CancerAnswers@Simmons
NEWS, HONORS + AWARDS


5323 Harry Hines Boulevard, Dallas, TX 75390-8519 UT Southwestern is an Affirmative Action/Equal Opportunity Employer. Women, minorities, veterans, and individuals with disabilities are encouraged to apply.
you would like to refer a patient to Simmons Cancer Center, please call 214-645-HOPE (4673) or 866-460-HOPE (4673)
records
Our team welcomes the opportunity to partner with physicians in the care of patients with cancer.
REFER TO SIMMONS CANCER CENTER
with your patients,
to
If
Insurance and medical
information are requested with new patients, and we will schedule an appointment within a few days of referral. Once we have been able to schedule a time convenient for your patient, we will notify you. Refer a Patient
WHY
UT Southwestern respects the relationship you have
and we are committed
open communication throughout the course of treatment. We look forward to collaborating with referring physicians to provide the highest quality of care to your patients.


 Director, Harold C. Simmons Comprehensive Cancer Center Associate Dean of Oncology Programs
X, formerly known as Twitter: @carlosarteagamd
Director, Harold C. Simmons Comprehensive Cancer Center Associate Dean of Oncology Programs
X, formerly known as Twitter: @carlosarteagamd