20 minute read
Complete Denture Aesthetics Revisited in the Digital Age
AUTHOR
Steven J. Sadowsky, DDS, is professor in the department of preventive and restorative dentistry at the University of the Pacific, Arthur A. Dugoni School of Dentistry. He is a diplomate of the American Board of Prosthodontists and sits on the editorial review boards of the Journal of Prosthetic Dentistry, the International Journal of Oral and Maxillofacial Implants and the International Journal of Prosthodontics. He is the abstract editor of the International Journal of Prosthodontics and has been appointed to the editorial council of the Journal of Prosthetic Dentistry. Conflict of Interest Disclosure: None reported.
Advertisement
ABSTRACT
Background: The objective of this review is to elucidate the principles of complete denture aesthetics and establish a rationale for a digital workflow for chairside arrangement of artificial teeth.
Types of studies reviewed: Articles were culled on the topic of complete denture aesthetics and the digital fabrication of complete dentures. These included systematic and literature review articles as well as clinical, descriptive and in vitro studies that range from 1958 to 2020 using PubMed and Web of Science databases.
Results: Biometric measurements have been illuminated over the last 60 years, serving as a basis for analogue and digital denture aesthetics. However, a number of studies have shown that individual arrangement of the anterior teeth is essential to capture asymmetry and balance in the setup. This review highlights that customization of the smile is optimally done chairside with patient feedback. A proof of concept was identified from the literature to incorporate a wax try-in in the digital workflow.
Practical implications: Given the heightened value placed on aesthetics in dentistry, a review of complete denture aesthetics will enhance the clinician’s skillset, and incorporating a chairside try-in in the digital workflow will lead to more authentic prostheses.
Key words: Complete denture aesthetics, biometrics, digital dentures
——————————
A digital approach to fabricating complete dentures has offered clinicians a more efficient fabrication process enlisting computer-aided design and computer-aided manufacturing (CAD/ CAM) technology for milled and printed dentures. [1,2] The advent of 3D facial scanning (3DFS) and designing technology has facilitated a virtual clinical evaluation of the aesthetic denture setup. [3] There are notable advantages to using a digital approach with 3DFS. The 3D libraries for teeth are quite exhaustive with 3,500 denture teeth and 380 tooth mould libraries available, including wellknown companies such as Myerson, Vita, Shofu, Candulor, Kulzer and Dentsply. You can download any library with an exocad serial number and a valid email address. A permanent exocad DentalCAD license with a currently active upgrade contract or an exocad DentalCAD/ ChairsideCAD/exoplan Flex License is needed. A virtual teeth setup permits efficient adjustments of midline, tooth size and position and generalized adjustments to the facial appearance and occlusal plane. In addition, the virtual setup is digitally stored, reducing the time and cost of replacement. However, there are several drawbacks to this technology. While stereophotogrammetric systems demonstrate accuracy and reliability in the collection of 3D facial scans, their cost, size and complexity make them unsuitable for most clinical practices. Further improvements in their technical specifications are also needed. For example, the alignment of the neutral smile and cheek retractor scans depend on the stability of the forehead as a reference. In patients with excessive facial grooves, this region can deform when smiling, hindering an accurate registration. Other errors have been reported due to movement during the scan, salivary flow and facial hair as well as the differences in technology used by each scanner. [3,4] Moreover, multiple factors are best evaluated chairside. The measurement of the vertical dimension of occlusion, centric relation and closest speaking space requires an animated patient and will impact function and phonetics. [5]
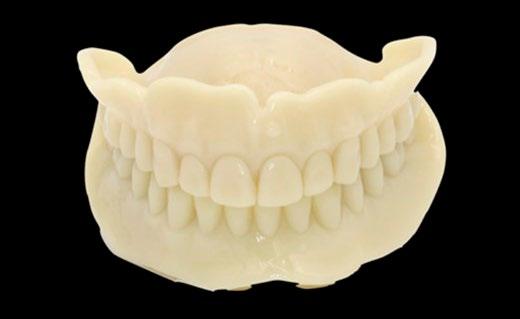
Virtual changes in the anterior tooth setup offer the patient only a semblance of the final aesthetic arrangement of teeth. A monolithic analogue (monoblock) denture try-in is limited in its utility for individualization and assessing patient satisfaction (FIGURES 1). The importance of showing the patient a midline change, correction of canted incisal plane, impact of a colored gingival matrix display, aesthetic effect of rotation of lateral incisors and opening up of incisal embrasures all are critical. The ability to test out changes in real time chairside is critical to an aesthetic and phonetic evaluation. The need for an inperson adjustable denture try-in within the digital workflow has clearly been established.
Using computer-engineered complete denture (CECD), a systematic review assessed patient satisfaction using digital libraries and a virtual try-in. [6] They concluded that 25% of patients were dissatisfied with the overall outcome and 15% were unhappy with the aesthetics. Their recommendation was the addition of a trial placement option for CECDs could result in improved clinical outcome, reducing the incidence of other complications such as occlusal vertical dimension, centric relation, tooth arrangement and aesthetics, improving patient satisfaction and reducing remake of the dentures.
Proof of Concept To Offer the Clinician an Adjustable Analogue Try-in in the Digital Workflow
While a number of authors [7–9] have reported on rapid prototyping (RP) complete dentures, Chen et al. [10] have quantitatively evaluated a wax pattern of a maxillary complete denture using a plaster cast and CAD software to program a 3D wax printer (ProJet CPX 3500, 3D Systems, Rock Hill, S.C.). There was no significant difference between the 3D printed group and the analogue group for measurements of deviation between the denture tissue surface and the plaster cast. This research has offered the prospect of an accurate, adjustable waxed base from a Standard Tessellation Language (STL) file (FIGURE 2A) to place on individual RP denture teeth from a second STL file (FIGURE 2B). When position changes are made chairside, the corrections can be scanned to digitize the new denture’s cameo surface and artificial teeth. [11] This can then be used for a CAD/ CAM application as well. [12,13] Given the premium on an attractive smile and its link to success as well as heightened patient expectations, a review of complete denture aesthetics will underscore the importance of a chairside try-in appointment in the digital workflow to enhance a customized setup.
Individualizing a Patient’s Smile
Nature and enduring art are thematically based in balance and asymmetry. Balance creates the appearance of symmetry and sets up a dynamic tension and vitality that mimics all that is alive. In the natural dentition, symmetry in the anterior sextant is found only in 10% to 14% of subjects (FIGURE 3). [14] The mouth should be a subset of the face. It should also have a midline that separates two non-mirror-like images within the outline of the lips. Lombardi called this dynamic unity and applied it to the prosthetic arrangement of anterior teeth. [15] Frush and Fisher coined the term “dynesthetic” to reflect the power and vitality of a smile when it is customized to reflect the patient’s individuality, considering sex (gender), personality and age. [16]
The attribution of gender in an anterior setup is not simply to reflect whether the patient is a male or female. In fact, neither experts in dentistry nor laypeople were able to identify a sexual dimorphism from photographs of a smile when the lips were covered. [17,18] Instead, the use of lapping of the lateral incisors and rounding of the incisal edge reveal a softness (FIGURE 4), while a frontal display of lateral incisors and a flat incisal edge confers a boldness, based on a gestalt of the patient (FIGURE 5). Similarly, a delicate or a vigorous personality can be depicted by a mesial or vertical axial inclination of the cuspids. Finally, age is the fourth dimension of a tooth setup which is reflected in a linear wear of the incisal edge over the life of the individual. Males and females show similar rates of tooth wear. Maxillary central incisors wear 1 mm by the age of 70, while the mandibular central incisors wear 1.5 mm. [19] Incorporating time related changes in the incisal length bestows an authenticity to the smile (FIGURE 6).
Biometric Guides
Biometric guides have been suggested for selecting the width of the maxillary central incisor (CW). The ratio of the interpupillary distance (IPD) and CW in a pre-extraction smiling photograph can be implemented when measuring the patient’s IPD to establish the CW (FIGURES 7). When an archival photograph is not available, the appropriate maxillary anterior tooth size can be estimated by anthropometric measurements. Cesario and Latta [20] found a reliable correlation between the interpupillary distance divided by 6.6 for CW (FIGURE 8A). Using the inner canthal distance multiplied by a geometric proportion of 0.618 divided by 2 has also been found to be a reliable predictor for CW (FIGURE 8B). [21] The bizygomatic width divided by 16 has been suggested to be predictive of the CW, although correlation coefficients have been found to be low for this face:tooth ratio. [22] However, a recent systematic review indicated that the combined width of the maxillary central incisors can be forecast by multiplying the interalar distance (IAD) by 70%. [23] In this same study, neither the IAD or the inner canthal distance were reliable guides to predict intercuspid distance. The golden proportion (1.618 to 1) also has not been proven to be predictive between perceived maxillary anterior teeth widths. [24] Moreover, in only 25% of patients with a natural dentition is the CW in golden proportion to the mandibular incisor width. [25] Regarding the ratio of incisal length to mesial/distal length of the maxillary central incisor, anthropometric measurements have been found to be predictive. Giddon et al. [26] reported a significant correlation in the ratio of the left fourth digit and the right second digit of the hand. Finally, facial height is both a functional and an aesthetic consideration and has been correlated to the width of four fingers (FIGURE 9). [27] Facial shape has often been ascribed to sexual dimorphism and the impact of testosterone or estrogen but has also been shown to correlate to the second:fourth digit ratio. [28] The link between facial form and tooth mold has long been a focus of complete denture practitioners.
Mold
Mavroskoufis and Ritchie [29] evaluated Williams’ “law of harmony” that says facial form can predict a square, tapering or ovoid tooth form. The results of their investigation invalidated this method of mold selection because more than two-thirds of the subjects showed a dissimilarity between face and maxillary central incisor form. A corroborating study using AutoCAD software also found no significant tooth mold/facial form association and noted that the ovoid tooth form was most prevalent and the square tooth form was least common. [30] Perhaps, more importantly, when the width/height ratio of the maxillary central incisor is 85%, it is considered to be optimally aesthetic. [31]
Arrangement
The placement of the maxillary central incisors is of paramount importance. If they are well positioned, all other teeth will be more nearly correct. They also dictate the midline. A parallel discrepancy of the dental midline with the facial midline of 2 mm or more is likely to be noticed by laypeople and reduce attractiveness (FIGURE 10). When the dental midline is canted in relation to the facial midline, it creates an even more uncomfortable visual tension and discrepancies of 10% were viewed as unaesthetic by 40% of laypeople. [32] Use of floss to bisect the face will facilitate a coincident midline. Using landmarks such as the labial frenum, nasopalatine papilla and midpalatal suture has been identified as reliable in 70% of subjects, but the range of those outside this percent was as much as 5.5 mm from the facial midline. [33] This limits an assessment without a try-in. The ultimate position of the maxillary central incisors is dependent on phonetic and aesthetic determinants. The incisal edge of the central incisor should contact the vermillion border of the lower lip when enunciating fricative (F) sounds. [34] Appropriate buccolingual position of the maxillary central incisors is essential to create a natural lip drape, as the middle third of the tooth is mainly responsible for scaffolding the upper lip. This assumes that in the impression phase a natural contour is developed in the labial flange region. There is also an aesthetic benefit of rotational and positional variance between the maxillary central incisors, which enhances the appearance of vitality by different light reflections and produces natural asymmetry. [16] The length discrepancy between the maxillary central and lateral incisor seen in a patient at age 30 may be eclipsed by age 70 because of wear. The display of the maxillary central incisors in respect to the lip at rest also changes with age. A young man or woman displays 2 mm to 3 mm of incisal edge below the lip, respectively, and an aged individual may have incisal edges up to 2 mm above the lip at rest. [35] This is due to increased perioral flaccidity, genetics and sunlight exposure. The maxillary lateral incisors show more variation in form and position than any other tooth. Rotation, pitch, forward/backward placement and axial deviation can be used to create dynamic unity. [16] By rotating the lateral incisors, the incisal embrasure is increased, which lends individuality and a figure ground interplay with light and shadow (FIGURE 11). The speaking line is another assessment of the proper display of the lateral incisors, which should be partially visible during speech (FIGURE 12). [36]
The maxillary cuspids are the transition teeth between the anterior and posterior setup. Their distal slope should not be visible in the frontal plane, as the incisal edge points to the central fossa of the posterior quadrant. The cervical aspect is everted in a typical canine eminence and the incisal edge is slightly tucked in. A vertical axial inclination would depict a more vigorous personality (FIGURE 13), while a mesial inclination reflects a softer affect. The cuspid should be abraded at the tip in an aging patient. The cuspids complete the anterior sextant and the incisal edges should follow the envelope of the smiling lower lip, whether arcuate or straight (FIGURES 14). Looking into a mirror with the patient allows the clinician to visualize the perceived setup, which is different from the observer’s view.
Confirmation of Position of Maxillary and Mandibular Anterior Teeth
There is a gradual shift in the display of the maxillary and mandibular anterior teeth with age; the exception is patients with Class II malocclusions. [37] Patients aged 30 display approximately 0.5 mm of the mandibular incisors at rest. This changes by age 60 with about 3 mm of the mandibular anterior teeth visible and no display of the maxillary sextant. [38] Thus, with age, the natural appearance of the mandibular anterior teeth becomes more crucial. Because of their similarity in size and shape, the mandibular incisors must be varied in their axial orientation to appear realistic. Plastic artificial teeth can also be stained on the incisal edge to add reality to wear faceting (FIGURE 15). Once the mandibular anterior teeth are set in wax, a phonetic confirmation of their correct position can be confirmed by articulating sibilant (S) sounds. Seventyfive percent of the population produces a sibilant sound by approximating the maxillary and mandibular anterior teeth to within 1 mm. [39] The anterior teeth should also approximate an end-to-end position when the patient says “judge.” Of all sounds, sibilants induce the most superior positioning of the mandible to the maxilla and are considered the “closest speaking space.” [5] When the vertical dimension of occlusion encroaches on the vertical dimension of rest, the teeth will contact. This becomes a functional impediment but also affects facial aesthetics with a strained appearance.
The incisal/occlusal plane and buccal corridor are also aesthetic factors. When the plane is canted in respect to the interpupillary line, it is a distraction from facial harmony. This relationship can be disclosed simply when the clinician extends the patient’s commissures with the forefingers in a parallel plane with the interpupillary line so that the anterior and posterior planes can be visualized (FIGURE 16). Anteriorly, aesthetic considerations should define the occlusal plane; posteriorly, the tongue, retromolar pad and Stenson’s duct have been used as landmarks. Using the ala-tragus line (Camper’s line) to establish the occlusal plane is also well documented, and Nayar et al. [40] found that the inferior border of the tragus to the ala is parallel to the occlusal plane in most dentate subjects. The buccal corridor will affect the attractiveness of a smile. As the amount of buccal corridor display was increased (FIGURE 17A), smiling images were scored less appealing by the evaluators (FIGURE 17A). [41] Conversely, when there is an absence of the buccal corridor, there is a loss of perspective and realism (FIGURE 17B). [42]
The Gingival Matrix or Visible Denture Base
Interdental papilla should follow the following precepts: It should be convex and self-cleansing. The shape of the papilla should be a complementary factor in age interpretation with more recession seen in older patients. Diastemas between the anterior teeth and posterior teeth must be V-shaped to shed food. When completing the waxup, flossing interproximally eliminates wax between teeth that otherwise would be processed, resulting in a compromise of the individuality of the setup. The gingival margin of the central incisors must be leveled or slightly coronal to the cuspids and leveled or slightly apical to the lateral incisors. When the base is visible, characterization will add authenticity. [43] This completes the refinement of a prosthodontic service that merges physiologic and psychologic comfort. [44]
Conclusion
Biometric guides for placement of artificial teeth for complete-denture patients are useful to create harmony and proportion in the anterior setup. However, the dynamism that can be reflected in personalizing a patient’s smile is the result of careful chairside arrangement of individual teeth following the tenets of balance and asymmetry published over 60 years ago. The literature elucidating complete denture aesthetics has had the longest half-life of relevance compared to any other discipline in dentistry. This remains true in the wake of the digital revolution.
REFERENCES
1. Masri G, Mortada R, Ounsi H, et al. Adaptation of complete denture base fabricated by conventional, milling and 3D printing techniques: An in vitro study. J Contemp Dent Pract 2020 Apr 1;21(4):367–71.
2. Anadioti E, Musharbash L, Blatz MB, Papavasiliou G, Kamposiora P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020 Nov 27;20(1):343. doi: 10.1186/s12903-020-01328-8.
3. Hassan B, Greven M, Wismeijer D. Integrating 3D facial scanning in a digital workflow to CAD/CAM design and fabricate complete dentures for immediate total mouth rehabilitation. J Adv Prosthodont 2017 Oct;9(5):381–386. doi: 10.4047/ jap.2017.9.5.381. Epub 2017 Oct 16.
4. Amornvit P, Sanohkan S. The accuracy of digital face scans obtained from 3D scanners: An in vitro study. Int J Environ Res Public Health 2019 Dec 12;16(24):5061. doi: 10.3390/ ijerph16245061.
5. Pound E. Let /S/ be your guide. J Prosthet Dent 1977 Nov;38(5):482–9. doi: 10.1016/0022-3913(77)90022-1.
6. Kattadiyil MT, AlHelal A, Goodacre BJ. Clinical complications and quality assessments with computer-engineered complete dentures: A systematic review. J Prosthet Dent 2017 Jun;117(6):721–728. doi: 10.1016/j.prosdent.2016.12.006. Epub 2017 Feb 20.
7. Wang C, Shi YF, Xie PJ, Wu JH. Accuracy of digital complete dentures: A systematic review of in vitro studies. J Prosthet Dent 2021 Feb;125(2):249–256. doi: 10.1016/j. prosdent.2020.01.004. Epub 2020 Feb 27.
8. Kalberer N, Mehl A, Schimmel M, Muller F, Srinivasan M. CAD-CAM milled versus protyped (3D printed) complete dentures: An in vitro evaluation of trueness. J Prosthet Dent 2019 Apr;121(4):637–643. doi: 10.1016/j.prosdent.2018.09.001. Epub 2019 Jan 31.
9. Alharbi N, Wismeijer D, Osman RB. Additive manufacturing techniques in prosthodontics: Where do we currently stand? A critical review. Int J Prosthodont Sep–Oct 2017;30(5):474–484. doi: 10.11607/ijp.5079. Epub 2017 Jul 27.
10. Chen H, Wang H, Lv P, Wang Y, Sun Y. Quantitative evaluation of tissue surface adaption of CAD-Designed and 3D printed wax pattern of maxillary complete denture. Biomed Res Int 2015;2015:453968. doi: 10.1155/2015/453968. Epub 2015 Oct 25.
11. Lee SY, Kim H, Lee D, Park C. Modified digital workflow for artificial tooth exchange in a complete denture: A digital technique. J Prosthet Dent 2020 Feb;123(2):236–238. doi: 10.1016/j. prosdent.2019.03.007. Epub 2019 May 16.
12. Steinmassl O, Dumfahrt H, Grunert I, Steinmassl PA. CAD/ CAM produces dentures with improved fit. Clin Oral Investig 2018 Nov;22(8):2829–2835. doi: 10.1007/s00784-018-2369-2. Epub 2018 Feb 22.
13. Srinivasan M, Kalberer N, Naharro M, Marchand L, Lee H, Müller F. CAD-CAM milled dentures: The Geneva protocols for digital dentures. J Prosthet Dent 2020 Jan;123(1):27–37. doi: 10.1016/j.prosdent.2018.12.008. Epub 2019 May 10.
14. Mavroskoufis F, Ritchie GM. Variation in size and form between left and right maxillary central incisor teeth. J Prosthet Dent 1980 Mar;43(3):254–7. doi: 10.1016/0022-3913(80)90398-4.
15. Lombardi RE. The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent 1973 Apr;29(4):358–82. doi: 10.1016/s0022-3913(73)80013-7.
16. Jameson WS. Dynesthetic and dentogenic concept revisited. J Esthet Restor Dent 2002;14(3):139–48. doi: 10.1111/j.1708- 8240.2002.tb00514.x.
17. Radlanski RJ, Renz H, Hopfenmuller W. Sexual dimorphism in teeth? Clinical relevance. Clin Oral Investig 2012 Apr;16(2):395– 9. doi: 10.1007/s00784-011-0537-8. Epub 2011 Mar 10.
18. Ferreira Jasse F, Vilhena Correa J, Ferreira Santos da Cruz A, et al. Assessment of the ability to relate anterior tooth form and arrangement to gender. J Prosthodont 2012 Jun;21(4):279–82. doi: 10.1111/j.1532-849X.2011.00822.x. Epub 2012 Feb 19.
19. Ray DS, Wiemann AH, Patel PB, et al. Estimation of the rate of tooth wear in permanent incisors: A cross-sectional digital radiographic study. J Oral Rehabil 2015 Jun;42(6):460–6. doi: 10.1111/joor.12288. Epub 2015 Mar 10.
20. Cesario VA, Latta Jr. GH. Relationship between the mesialdistal width of the maxillary central incisor and the interpupillary distance. J Prosthet Dent 1984 Nov;52(5):641–3. doi: 10.1016/0022- 3913(84)90133-1.
21. Abdullah MA. Inner canthal distance and geometric progression as a predictor of maxillary central incisor width. J Prosthet Dent 2002 Jul;88(1):16–20.
22. Radia S, Sherriff M, McDonald F, Naini FB. Relationship between maxillary central incisor proportions and facial proportions. J Prosthet Dent 2016 Jun;115(6):741–8. doi: 10.1016/j.prosdent.2015.10.019. Epub 2016 Jan 13.
23. Liao P, Fan Y, Nathanson D. Evaluation of maxillary anterior teeth width: A systematic review. J Prosthet Dent 2019;122(3):275–81.e7. doi.org/10.1016/j. prosdent.2018.10.015.
24. Mahshid M, Khoshvaghti A, Varshosaz M N, Vallaei N. Evaluation of “golden proportion” in individuals with an esthetic smile. J Esthet Restor Dent 2004;16(3):185–92; discussion 193. doi: 10.1111/j.1708-8240.2004.tb00032.x.
25. Preston JD. The golden proportion revisited. J Esthet Dent 1993;5(6):247–51. doi: 10.1111/j.1708-8240.1993. tb00788.x.
26. Giddon DB, Bibko J, Anderson NK. Second to fourth digit ratio relation to anterior tooth morphology. J Dent Res 2006;85(Spec Iss A): Abstract #0760 (www.dentalresearch.org).
27. Ladda R, Bhandari AJ, Kasat VO, Angadi GS. A new technique to determine vertical dimension of occlusion from anthropometric measurements of the fingers. Indian J Dent Res May–Jun 2013;24(3):316–20. doi: 10.4103/0970-9290.117993.
28. Fink B, Grammer K, Mitteroeker P, Gunz P, Schaefee K, et al. Second to fourth digit ratio and face shape. Proc Biol Sci 2005 Oct 7;272(1576):1995–2001. doi: 10.1098/rspb.2005.3179.
29. Mavroskoufis F, Ritchie GM. The face-form as a guide for the selection of maxillary central incisors. J Prosthet Dent 1980 May;43(5):501–5. doi: 10.1016/0022-3913(80)90319-4.
30. Mehndiratta A, Bembalagi M, Patil R. Evaluating the association of tooth form of maxillary central incisors with face shape using AutoCAD software: A descriptive study. J Prosthodont 2019 Feb;28(2):e469–e472. doi: 10.1111/jopr.12707. Epub 2017 Dec 27.
31. Álvarez-Álvarez L, Orozco-Varo A, Arroyo-Cruz G, Jiménez- Castellanos E. Width/length ratio in maxillary anterior teeth. Comparative study of esthetic preferences among professionals and laypersons. J Prosthodont 2019 Apr;28(4):416–420. doi: 10.1111/jopr.12642. Epub 2017 May 17.
32. Shyagali TR, Chandralekha B, Bhayya DP, Kumar S, Balasubramanyam G. Are ratings of dentofacial attractiveness influenced by dentofacial midline discrepancies? Aust Orthod J 2008 Nov;24(2):91–5.
33. Latta Jr GH. The midline and its relation to anatomic landmarks in the edentulous patient. J Prosthet Dent 1988 Jun;59(6):681–3. doi: 10.1016/0022-3913(88)90382-4.
34. McCord JF, Firestone HJ, Grant AA. Phonetic determinants of tooth placement in complete dentures. Quintessence Int 1994 May;25(5):341–5.
35. Fisher RD. Personalized restorations vs. plates. J Prosthet Dent 1973;30(4 Pt 2):513–4.
36. Murrell GA. Complete denture esthetics. Dent Clin North Am 1989 Apr;33(2):145–55.
37. Khan F, Abbas M. The mean visible labial length of maxillary and mandibular anterior teeth at rest. J Coll Physicians Surg Pak 2014 Dec;24:(12):931–4.
38. Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent 1978 May;39(5):502–4. doi: 10.1016/s0022- 3913(78)80179-6.
39. Engelmeier RL. Complete denture esthetics. Dent Clin North Am 1996 Jan;40(1):71–84.
40. Nayar S, Bhuminathan S, Bhat WM, Mahadevan R. Relationship between occlusal plane and ala-tragus line in dentate individuals: A clinical pilot study. J Pharm Bioallied Sci 2015 Apr;7(Suppl 1):S95–7. doi: 10.4103/0975-7406.155822.
41. Tikku T, Khanna R, Maurya RP, Ahmad N. Role of buccal corridor in smile esthetics and its correlation with underlying skeletal and dental structures. Indian J Dent Res Mar–Apr 2012;23(2):187–94. doi: 10.4103/0970-9290.100424.
42. Oshagh M, Zarif NH, Bahramnia F. Evaluation of the effect of buccal corridor size on smile attractiveness. Eur J Esthet Dent Winter 2010;5(4):370–80.
43. Pattanaik S, Pattanaik B. Characterization of a denture base using autopolymerized pour-type denture basin resin and acrylic stain. J Prosthodont Res 2013 Apr;57(2):145–6. doi: 10.1016/j. jpor.2012.08.007. Epub 2013 Feb 27.
44. Frush JP, Fisher RD. The dynesthetic interpretation of the dentogenic concept. J Prosthet Dent 1958;8:558–81. doi. org/10.1016/0022-3913(58)90043-X.









