3 minute read
FEATURE
from December 2020
by Cedar Post
Photo Courtesy of Sharon Bistodeau
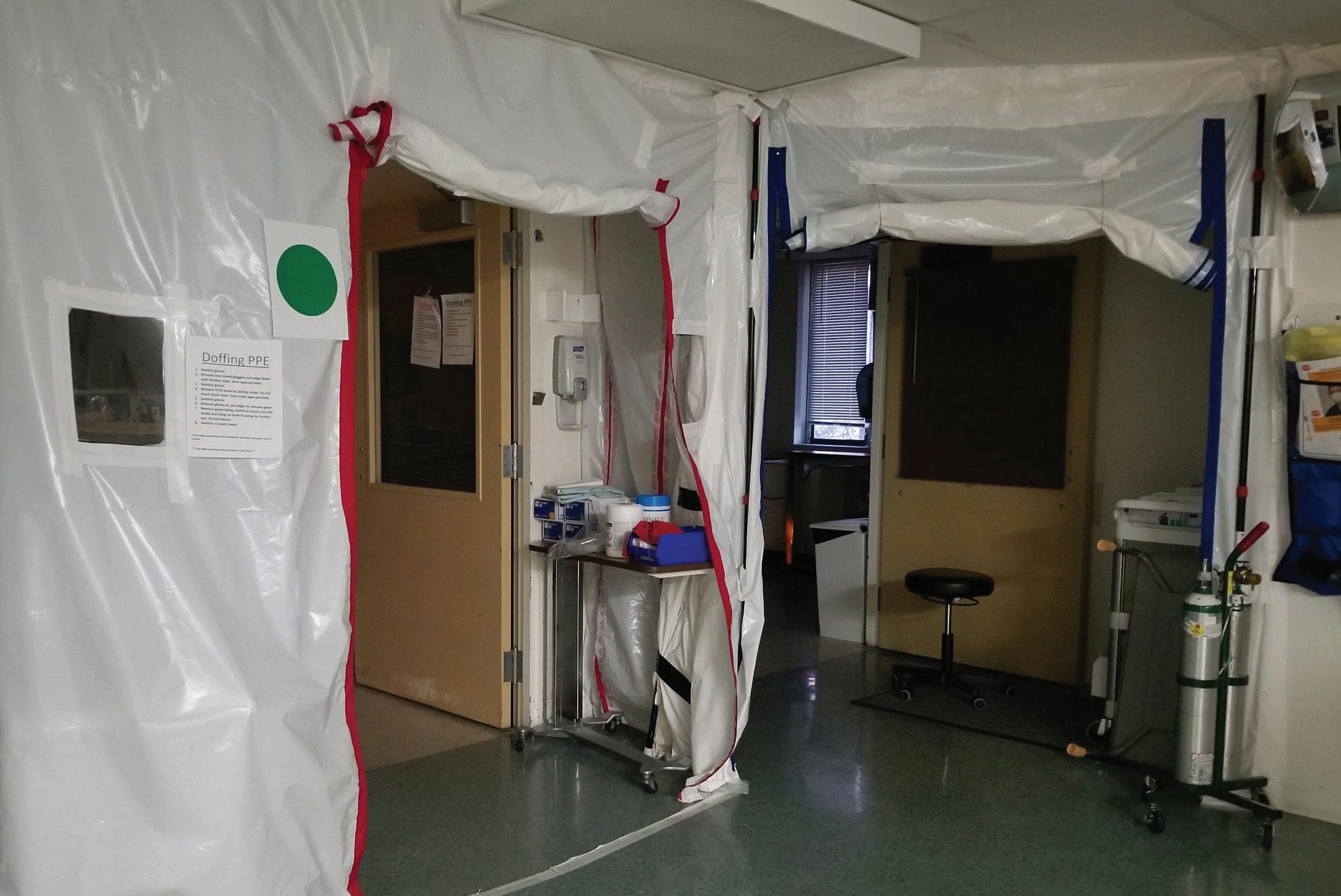
Above: Tents are set up inside the COVID sanctioned area in the Intensive Coronary Care Unit of Bonner General Health as precaution.
Advertisement
Washington, said that his day to day intensive aftercare of COVID patients is time consuming. He stays busy treating the patients’ other health concerns that couple with the virus such as Acute Respiratory Distress Syndrome and pneumonia. He explained that it is a process to enter the room of a COVID patient and the team has to have a plan and suit up in protective gear such as a PAPR (Powered Air Purifying Respirator). Many hospitals, including Deaconess, have altered the airflow of COVID patients’ rooms so that contaminated air does not circulate through the rest of the hospital when the door is opened. May contracted COVID and experienced all the common flu-like symptoms except for a fever. He observed that not developing a fever was a trend in most of the COVID patients he treated. May had to quarantine for 10 days and could only go back to work after being symptom free for a full 48 hours. With practice in conducting COVID tests, May found that tests are not always reliable since, “People that contract COVID can test positive kind of on and off for a while and so it would make the test erroneous.” he said.
Dealing with COVID patients has been a learning experience for nurses and physicians across the nation. For May, becoming more familiar with ventilators, machines that help breathe for patients, was a critical learning curve. “It’s difficult to optimize the vent settings...” May said, “[and] find the happy place that best oxygenates the patient and there’s a type of different style to protect their lungs.” In some cases, even if putting a patient on a ventilator is the only method of care that will keep them alive, it is a struggle for their body to keep up with the stress of their treatment changing.
In Bonners Ferry, community member Tracey Koch practices nursing at the Kootenai Tribal Clinic. “It’s been a real challenge, as far as the clinic is concerned, to really make sure that we’re available for everyone and that people have access to care,” she said, “but yet we have to think about the big picture and keep everybody safe.” The clinic has had to undergo a lot of procedural changes to make the facility safer such as letting only a certain number of patients into the building at a time. They also engage in “telemedicine” where patients can seek help over the phone to minimize the amount of people coming to the clinic in person.
Nursing Supervisor, Sharon Bistodeau, has devoted 28 years of her life to working at Bonner General Hospital in the ER, ICU, and anywhere else she is needed. As a smaller hospital, Bonner General is staffed according to a 25 bed hospital so they do not have an abundance of extra hands. There has been a nationwide shortage of nurses for years, and more so now than ever because the intensity in hospitals because of COVID is too much for some nurses to stay in the practice. But not for Bistodeau.
Caring for COVID patients is more time and resource consuming. “There is a whole plethora of people that take care of one patient,” Bistodeau said. Because the disease is so contagious, nurses who care for COVID patients have to be isolated to the COVID pods--the area sanctioned specifically for the










