SSM Health’s support brings asthma supplies into public schools across Oklahoma
 By LISA EISENHAUER
By LISA EISENHAUER
SSM Health St. Anthony Hospital in Oklahoma City is making it possible for a nonprofit organization to put asthma inhalers in every public school in the Sooner State.
The hospital, part of St. Louis-based SSM Health, is giving $192,568 through a grant and in-kind donations to the Brendon McLarty Memorial Foundation. The foundation is using the gifts to provide Oklahoma’s 539 public school districts with at least one inhaler and related supplies for every school, about 1,600 in all.
Continued
Ministry care providers support call-to-action to counter epidemic of loneliness
By LISA EISENHAUER
Dr. Venkata Dalai sees the evidence among patients of what the U.S. surgeon general spotlights in a recent advisory called “Our Epidemic of Loneliness and Isolation.”

A psychiatrist on staff at Mercy Hospital Fort Smith in Northwest Arkansas, part of Chesterfield, Missouribased Mercy, Dalai says that for some patients the biggest need is for a social support structure.
“I feel helpless sometimes because the problem is not depression, the problem is not anxiety,” he says. “The problem is
Bon Secours St. Francis in South Carolina equips barbers, stylists to talk health with customers
 By JULIE MINDA
By JULIE MINDA
The topics of conversation have been shifting a bit lately at the UpTown Barber Shop near Greenville, South Carolina.
Much more so than in the past, UpTown owner and master barber Timothy “Dreze” Shell and his clients have been talking about heart health, blood pressure, healthy living and mental health.
Shell has been initiating such conversations with clients since earlier this year when he and nearly 20 other Greenville-
area barbers and stylists accepted Bon Secours St. Francis Health System’s invitation to join its “Beauty and Barbershop Talk” program. Through the program — which is aimed at hair stylists with a predominantly minority clientele — a nurse educator taught the group why and how to discuss health topics with their patrons as well as how to help the patrons take their blood pressure. The group learned to assist clients in seeking care if they need it.
Shell says he’s glad the program has
Continued
Eldercare facility leaders attuned to shrinking pool of qualified candidates for administrator posts
By JULIE MINDA
The same types of factors that have been constricting the job candidate pool for frontline positions in eldercare also have shrunk the number of prospects for top administrator roles.
In recent years, exigencies of the COVID19 pandemic have accelerated the departure of workers from the labor pool: Baby Boomers have been retiring in large numbers, burnt out workers have joined the “Great Resignation” out of the labor market or at least into different roles, and too few newcomers are repopulating the pipeline.
Ministry eldercare leaders say they are watching these trends especially closely when it comes to the pipeline of candidates for top administrator positions in continuum-of-care facilities.
They say they are continually seeking new ways to identify prospective candidates who are the right fit for ministry leadership and to illustrate to these prospects the many rewards of being a leader in the Catholic health ministry.
“It’s truly a calling to care for the aged — it’s a vocation and a ministry. It is challenging but also rewarding work,” says
ABOUT
increases the risk of premature death by 26%
Lacking social connection can increase the RISK FOR PREMATURE DEATH as much as smoking up to 15 cigarettes a day.
Social isolation among older adults alone accounts for an estimated $6.7 BILLION in excess Medicare spending annually, largely due to increased hospital and nursing facility spending.
Chronic loneliness and social isolation can increase the RISK OF DEVELOPING DEMENTIA by approximately 50% in older adults.
Source: “Our Epidemic of Loneliness and Isolation,”
“ Lights, camera,
Continued on 6
ethics 5 Executive changes 7 Garden feeds those in need 3
Loneliness
HALF of U.S. adults report experiencing loneliness, with some of the highest rates among young adults.
U.S. Surgeon
healing
the
General’s advisory on the
effects of social connection and community, 2023
It’s truly a calling to care for the aged — it’s a vocation and a ministry. It is challenging but also rewarding work. But there are not always enough people to fill these positions. We’re all vying for the same group of people.”
— Sr. M. Peter Lillian Di Maria
on 2
Children carry backpacks with gifts provided by the Brendon McLarty Memorial Foundation. The nonprofit is focused on asthma education and awareness. It is using funding from SSM Health St. Anthony Hospital in Oklahoma City to get free asthma supplies into the state’s public schools.
on 4
Brandy McMahand leads a ‘Beauty and Barbershop Talk’ program at Corte Tropical Dominican Salon & Barbershop in Mauldin, South Carolina. McMahand, a nurse and case manager for the Healthy Outcomes Program at Bon Secours St. Francis Health System, has been leading free sessions on the basics of heart health and other healthy living topics for barbers and stylists in the Greenville, South Carolina, area. This is one of those groups.
Continued
on
Dalai AN EPIDEMIC OF LONELINESS JUNE 15, 2023 VOLUME 39, NUMBER 10 PERIODICAL RATE PUBLICATION
8
Asthma supplies
From page 1
Jen Blair, the foundation’s executive director, says Oklahoma will be the first state in the nation to have asthma inhalers in every public school. Blair credits SSM Health St. Anthony’s support for propelling the work of the foundation “in ways that we dreamed of but weren’t sure was actually going to happen.”
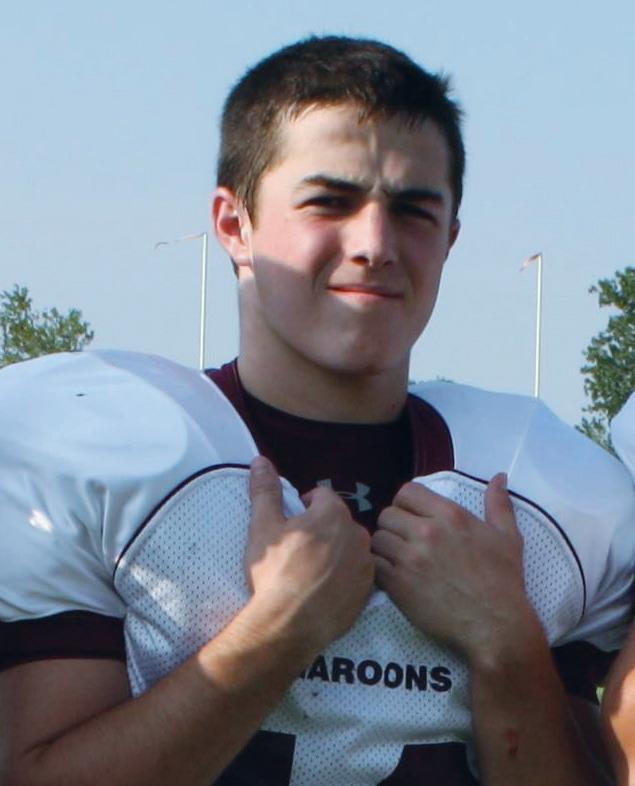
Tragedy spurs action
The Brendon McLarty Memorial Foundation is named for a 16-year-old who died after an asthma attack in 2012. Blair is the first cousin of Brendon’s mother, Lori McClarty, though she says they are closer than most sisters and she considered Brendon her nephew.

On the day of his fatal attack, the last day of school in his sophomore year, Brendon was home alone after football practice. During the attack, he was without oxygen for about 20 minutes. He died three days later at a hospital in Oklahoma City.
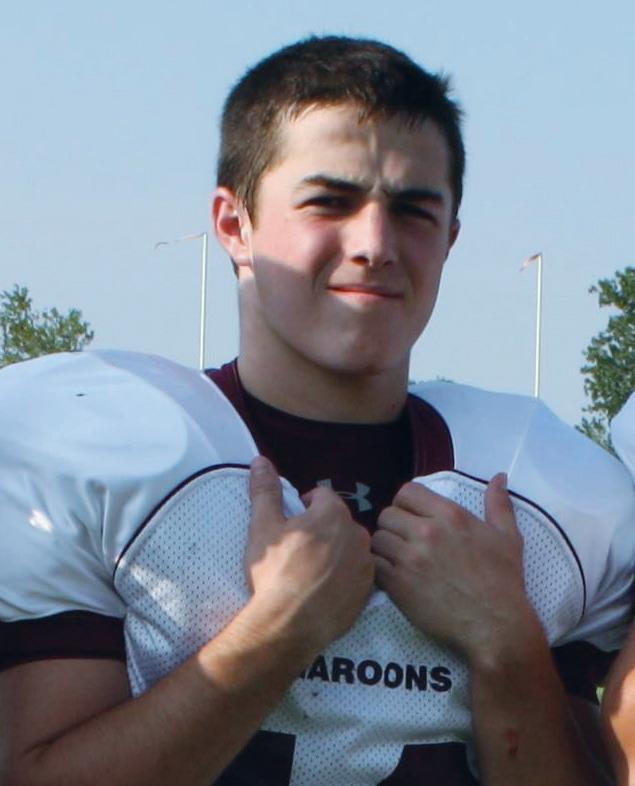
“Obviously it was just a horrific tragedy for our family,” Blair says. “He was so young.”
In hopes of helping other children with asthma and their families, Brendon’s family set up the nonprofit memorial foundation. Its goal is to fight the disease through education and awareness.
Putting inhalers within reach
The Centers for Disease Control and Prevention calls asthma a chronic disease that requires ongoing medical management. It afflicts about 6 million U.S. children ages 17 and under. About 16% of Black children have asthma as do about 7% of white children. The federal agency reports that because of better asthma treatments and care, the number of fatal attacks, missed school days and hospital stays are down.
Andrew Ochs, regional vice president of mission integration for SSM Health Oklahoma, says increasing access to health care was one of the community needs identified in SSM Health St. Anthony’s assessment. Ochs says that by supporting the work of the Brendon McLarty Memorial Foundation, the hospital is helping to meet that need by putting asthma supplies within reach of more people.
He says the system sees the inhaler distribution as a step toward increasing access to education, too, “because kiddos aren’t having to miss school and parents aren’t having to take time off of work to come and deliver an inhaler or take a kiddo home or, God forbid, a kiddo ends up having to go to the emergency room because she or he doesn’t have access to their inhaler.” Ochs was one of CHA’s 2022 Tomorrow’s Leaders.
In addition, Ochs says SSM Health St. Anthony sees part of its mission to be meeting the needs of people in the rural areas of the state so that they can stay there and thrive, as did its founding congregation, the Sisters of St. Francis of Maryville. The order later reunited with its original congregation, becoming the Franciscan Sisters of Mary.
By supporting distribution of the inhalers and related asthma supplies well beyond its own urban and suburban service area, Ochs says the hospital is ensuring that rural children with asthma aren’t overlooked. He says SSM Health St. Anthony is hopeful that the state eventually will step in to take over funding the asthma supplies in schools.
Ochs says that working with established community groups such as the Brendon McLarty Memorial Foundation helps SSM Health accomplish its community healthrelated work. Those groups, he says, bring expertise and passion to their efforts. Mean-
Asthma causes wheezing, difficulty breathing and coughing.
Asthma in children
Source: Centers for Disease Control and Prevention
About 6 million children, or 1 in 12, in the U.S. ages 17 and younger have asthma.
16% of Black children and 7% of white children have asthma.
Every year, 1 in 6 children with asthma visits an emergency department.
Measurable success
To date, the inhalers and related supplies — such as disposable spacers that direct the flow of the medication — are in about half of Oklahoma’s schools. Blair says the foundation is hopeful of getting them in all public schools by the end of the next school year.
In addition to the purchase of inhalers, the grant from SSM Health St. Anthony has enabled the foundation to upgrade its software so it can track the distribution and use of the inhalers. In the school year that just ended, Blair says the inhalers were used at least 1,500 times and in 83% of cases, the students involved were able to return to class.
Every year, about 1 in 20 children with asthma is hospitalized for the disease.
More than half of children with asthma had at least one attack in 2016.
age and use of the inhalers. Each inhaler can provide about 200 puffs.
The first school district to get the inhalers was Perry Public Schools, a rural district in Northern Oklahoma where Brendon was a student. By the time COVID-19 hit in early 2020, the foundation had provided inhalers to 11 districts, but the pandemic put a halt to the distribution.
Blair says the foundation got a boost when a man who works for the Oklahoma State Department of Education contacted the nonprofit and asked how he could help. The man previously had been a coach and once lost a player to an asthma attack. That connection led to the department’s endorsement of the inhaler project. “At that point, it really took off,” Blair says.
The foundation references SSM Health as its “premier sponsor.” And support has flowed both ways. The foundation donates proceeds from its own fundraising events — including an annual baseball tournament — for a Brendon McLarty Memorial Asthma Fund overseen by the St. Anthony Hospital Foundation. The fund pays for asthma supplies for families in need of them.
Of SSM Health’s support for the inhaler distribution to schools, Blair says: “It’s definitely expanded our program in more ways than we could have ever imagined.”
leisenhauer@chausa.org
while, having their projects co-branded with SSM Health adds credibility to their work, he says.
“We’re more than happy to help in that regard,” Ochs says.
Supplies and training
Before the foundation started supplying inhalers to schools, it advocated for Oklahoma lawmakers to pass a law making it legal for schools to have the prescription medication on site. The lawmakers passed the law unanimously and it was signed by Gov. Kevin Stitt in 2019. The American Lung Association says 17 states now have either laws or guidelines allowing schools to stock quick-relief medication for students with asthma.
In Oklahoma, schools can keep up to two inhalers in secure locations. In addition, the school nurse or another employee must undergo training on the proper stor-
The department worked with the foundation to get the word out among districts about the free inhalers and to offer training on the use of the inhalers by video in a session that lasts about 40 minutes. At some schools, Blair says, the training is offered to everyone on staff on professional development days.
Diversity & Disparities Networking Zoom Call June 29 | 1 – 2 p.m. ET
Faith Community Nurse Networking Zoom Call
July 25 | 1 – 2 p.m. ET
Catholic Ethics for Health
Vice President Communications and Marketing Brian P. Reardon

Editor Lisa Eisenhauer leisenhauer@chausa.org
314-253-3437
Associate Editor Julie Minda jminda@chausa.org
314-253-3412
Graphic Design
Norma Klingsick
Advertising ads@chausa.org 314-253-3477
Catholic Health World (ISSN 8756-4068) is published semimonthly, except monthly in January, April, July and October and copyrighted © by the Catholic Health Association of the United States. POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@ chausa.org. Periodicals postage rate is paid at St. Louis and additional mailing offices. Annual subscription rates: CHA members free, others $29 and foreign $29. Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA. Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
© Catholic Health Association of the United States, June 15, 2023
Care Leaders Virtual Program Tuesdays Sept. 5 – Oct. 17 | 1 – 3 p.m. ET Mission in Long-Term Care Networking Zoom Call (Members only) Sept. 6 | 1 – 2 p.m. ET Deans of Catholic Colleges of Nursing Networking Zoom Call Oct. 3 | 1 – 2 p.m. ET United Against Human Trafficking Networking Zoom Call Oct. 4 | Noon – 1 p.m. ET Community Benefit 101: The Nuts and Bolts of Planning and Reporting Community Benefits Virtual Program Oct. 24 – 26 | 2 – 5 p.m. ET each day Upcoming Events from The Catholic Health Association chausa.org/calendar
Blair Ochs
Brendon McLarty of Perry, Oklahoma, died after an asthma attack at the age of 16. He had just come home from football practice on the last day of school his sophomore year.
2 CATHOLIC HEALTH WORLD June 15, 2023
Andrew Ochs says that working with established community groups such as the Brendon McLarty Memorial Foundation helps SSM Health accomplish its community health-related work. Those groups, he says, bring expertise and passion to their efforts.
Garden at HSHS Wisconsin hospital grows fresh food for those in need
By LAIGHA ANDERSON

HSHS St. Joseph’s Hospital is tackling hunger head on, by growing food in a garden for the community.
For the past 10 years, the hospital in Chippewa Falls, Wisconsin, has been providing fresh food to local food pantries in its service area through a volunteer-tended garden. The garden produces hundreds of pounds of food per week during the planting and harvesting season, which starts in mid-May.

“God provides the sunshine, we provide the water and security,” said Roger Elliot, who coordinates the hospital’s garden program.
The garden took root after the 2010 census. That census revealed that in Chippewa County and the surrounding area the hospital serves about 14% of people lived at or below the poverty line and as many as one-tenth of the population of about 100,000 were food insecure.

“We looked at the report and said there is like 40 acres of vacant land behind the hospital. If we could do garden space, we could grow food, provide those who are hunger challenged space to grow their own food,” explained Elliot.
The hospital already was undertaking a massive renovation project that included work on the hospital’s healing garden.
The vacant 40 acres became the site of 24 garden plots, each 12 feet wide by 24 feet long. The HSHS St. Joseph’s Hospital Foun-
“We looked at the report and said there is like 40 acres of vacant land behind the hospital. If we could do garden space, we could grow food, provide those who are hunger challenged space to grow their own food.”
— Roger Elliot
FOUNDATIONS
of CATHOLIC HEALTH CARE LEADERSHIP
AVAILABLE ON- DEMAND AND LIVE
Leaders in Catholic health care recognize the crucial importance of formation in ensuring the Catholic identity of our ministries. In response to member needs, CHA is offering Foundations On-Demand as a sister program to Foundations Live.
Foundations On-Demand

ALWAYS AVAILABLE
The program is ideal for those who have difficulty getting away from their work to attend a scheduled program. A local dialogue partner supports On-Demand participants as they work at their own pace.
Foundations Live
JAN. 30 — MARCH 21, 2024
Foundations Live is an interactive eight-week (virtual) program. Engage in meaningful dialogue with ministry colleagues from your system and across the country.
dation provided the money to pay for the work needed to create the plots. The plots have an irrigation system, so volunteers do not need to haul water into the garden.
Deterring intruders
It was slow going at first. Elliot said the garden initially was not fenced in. And being in a deer-heavy part of the state, that meant the wildlife was helping itself to the plants. The open nature of the site also allowed for vandals to disturb the garden. At one point, someone drove a car through. In total, the garden produced less than 200 pounds of food in 2013.
There was a fix for both problems, though — a fence with a locked gate that now surrounds the garden. Over the next nine years, the garden produced more than 11 tons of food for local food pantries and food kitchens.
When the concept of the garden originally took shape, the hope was that families in need would claim a plot for a small fee that would be put into the upkeep. While that remains an option, and scholarships can cover the $20 garden fee, the hospital has found that the best use of the garden is to open the plots to volunteer gardeners. Those growers pay a $35 fee and then donate their crops to food pantries. The fees are reinvested in the garden, with some of the money used to buy new tools and the rest kept in a fund for use as needed.
Volunteers are able to drop off their harvest at the hospital, where staff take the food to nearby food kitchens and food pantries. Which of the places gets the food depends on whether they are open on the day of the donation and how much they can take.
Trial and error
One of the volunteers at the garden is Cathy Lombard. She said she has always
had a love of gardening.
The first year Lombard gardened one plot, but she enjoyed it and increased her growing space. At one point she tended as many as seven plots. For now, she’s gardening five.
She said there has been some trial and error over the years. Once chipmunks dug into her plots. However, she quickly discovered that chipmunks don’t like Irish Spring soap. Putting some soap into the holes kept the critters away.
She has experimented with the foods she has grown and donated, learning that those who receive the foods can be quite adventurous in what they enjoy. One year she attempted to grow kidney beans only to find that the summer heat made them too bitter.
‘A nice service’
Lombard and the other growers aren’t the garden’s only volunteers. Years ago, a Boy Scout built a shed for the garden as a part of his Eagle Scout project. The shed allows tools and other gardening supplies to be kept on site. The shed is accessible with the same key that is used to get inside the garden fence. The scout raised money to build the shed and used what was left over to buy tools so no one has to bring their own to the garden.
The garden has grown to include a small apple orchard. A local group prunes the trees. Two Honeycrisp trees are recent additions. Two beehives in the garden pollinate the plants to increase sustainability.
Lombard pointed out that, given the high incidence of food insecurity in and around Chippewa Falls, it is likely that she and the other gardeners are growing food for some of their friends and neighbors.
“It is a nice service to provide to the community, so they have fresh vegetables,” Lombard said.

Questions?
Email formation@chausa.org or call 800-230-7823
LEARN MORE AT CHAUSA.ORG/FOUNDATIONS
Over nine years, the community garden at HSHS St. Joseph’s Hospital has produced more than 11 tons of fruits and vegetables. Volunteer gardeners donate their harvests to local food banks for giveaway to people who are food insecure.
The community garden at HSHS St. Joseph’s Hospital in Chippewa Falls, Wisconsin, has 24 plots that are tended by either families who are food insecure or volunteer gardeners. The site also has a small apple orchard and two beehives.
June 15, 2023 CATHOLIC HEALTH WORLD 3 Elliot
Loneliness epidemic
From page 1
feeling isolated or living alone, and lack of people to talk to or share something.”
Other mental health care providers as well as social service coordinators across the Catholic health ministry say they, too, see many patients who are lonely or socially isolated as well as indications that the prevalence of those experiences is increasing. They voice support for Surgeon General Dr. Vivek Murthy’s appeal for a national response.
Harm to individuals, society
Murthy issued his call-to-action May 3 in an 82-page advisory. He says studies have found that half of the nation’s adults reported experiencing loneliness even before the COVID-19 pandemic cut many people off from family, friends and support systems.
“Loneliness is far more than just a bad feeling — it harms both individual and societal health,” Murthy writes.
He says being socially disconnected increases the risk of cardiovascular disease, dementia, stroke, depression, anxiety and premature death. He adds that the harmful effects of a society that lacks social connection “can be felt in our schools, workplaces, and civic organizations, where performance, productivity, and engagement are diminished.”
Murthy’s advisory says countering the epidemic of loneliness and isolation will require “reimagining the structures, policies, and programs that shape a community to best support the development of healthy relationships.” Some of the responses he calls for are public, such as investing in libraries and green spaces, and others are personal, such as reaching out to neighbors and setting phones aside when dining with others.
The advisory has a page of ideas for health workers, health systems and insurers. Those ideas include:
Explicitly acknowledge social connection as a priority for health.
Provide health professionals with formal training and continuing education on the health and medical relevance of social connection and risks associated with social disconnection.

Provide adequate reimbursement for time spent assessing and addressing concerns about social disconnection and incorporate these measurements into value-based payment models.
Bold action needed
Mekhala Merchant, a licensed clinical psychologist with Loyola Medicine and an associate professor in the Department of Psychiatry and Behavioral Neurosciences at Stritch School of Medicine at Loyola University Chicago, calls the advisory a good
start to draw attention to the worsening trends of loneliness and isolation.
Merchant says some of the findings cited in the advisory that stood out to her were that the rate of loneliness among young adults ticked up every year from 1976 through 2019, that only 16% of Americans feel connected to their local communities and that 30% live alone.
The findings make a compelling argument, she says, that loneliness should be addressed across society, including by health care providers. “I do think that for an advisory to have impact we have to make bold claims about the changes we expect from the health system,” Merchant says.
She points out that Loyola Medicine already has processes in place, such as screenings, to identify mental or spiritual distress in patients. Loyola Medicine, part of Trinity Health, also has social workers, psychologists and chaplains on staff to provide care and connections to community services.
“Our mission statement is ‘Treating the human spirit,’” she notes. “I believe we are very focused and committed to understanding the psychosocial needs of any of the patients that we’re treating in any of our medical specialties.”
Suffering alone
Dr. Katherine Johnson, interim chair of psychiatry at Loyola Medicine, says she and her colleagues have seen spikes in cases of depression and anxiety in recent years that are in large part consequences of social disconnection.
In fact, she says, many people suffering mental illness believe they are alone in their misery. “I have so many patients tell me, ‘Everybody else seems to be doing OK,’” she says. “And I’m like, ‘No, I’m here to tell you they’re not.’”
Johnson agrees that the surgeon general presents what could be a good start to a conversation about Americans’ disconnection and to addressing isolation and loneliness — which she calls “modifiable risk factors” for mental and physical ailments.
The next step, she says, is to follow through with funding. “The government, in particular, is going to have to put their money where their advisory is,” she adds.
She cites, for example, the advisory’s call for training and continuing education for health care professionals on the health impacts of isolation and loneliness as an action that comes with costs. Another is its call for insurance coverage of the time that care providers spend assessing and addressing social disconnection.
Offering connections

Joshua Primeaux is director of social services for the mental and behavioral health department at Our Lady of the Lake


Regional Medical Center in Baton Rouge, Louisiana. He helps make social connections for patients who show signs of isolation, such as linking elderly people to community programs that offer group activities.
Primeaux says that the system Our Lady of the Lake is part of, Franciscan Missionaries of Our Lady Health System, has prioritized assessing and addressing the social determinants of health among patients. Care providers and social workers have access to a platform called Pathways to refer patients to community agencies that can help meet underlying needs that fuel mental distress, such as hunger or homelessness.
Even so, Primeaux says he’s not sure that all patients follow up on those referrals or that the agencies can meet the demand for assistance. “We can provide the information, but are they actually going to get the resources?” he wonders. “I’m not very confident of that.”
Primeaux says many patients, especially the elderly, are in need of family support to see that their social needs are met.
Stressing social structure
Dalai, the Mercy psychiatrist, agrees that family is often the missing link for disconnected patients and for those suffering mental health crises.
Dalai recalls recently nudging a patient with treatment-resistant depression to contact his estranged parents. The patient did and later told Dalai that he hugged his parents, dined with them and enjoyed his best time ever.
substance use disorders and loss, such as from a failed marriage or through diminished health.
Weatherill says the various behavioral therapies he and his colleagues employ all have a socialization component. In addition, the care providers educate their patients on the importance of being around other people.
“It is emphasized every day on our unit,” he says. “Even if a person has some social anxiety and doesn’t feel comfortable yet attending a group, it’s talking to staff or talking to other patients one on one.”
However, staying connected to other people once they are on their own is a challenge for many patients, Weatherill admits. “I wish I could write a prescription for social support and it would be that easy,” he says. “Many people just don’t have it.”
‘Why didn’t this happen before?’
Susan LaMonica is a nurse practitioner with Hospital Sisters Health System Medical Group in Effingham, Illinois, who specializes in mental health. She’s seeing an upsurge in requests for care amid a shortage of providers.


Right now, new patients have to wait 2½ months for an appointment with her. Some of her patients drive almost two hours to get to her office.
LaMonica says the pandemic undoubtedly created conditions that left more people feeling alone and isolated. Among her recent patients, many said their biggest complaint was being lonely. “Patients didn’t get to see their family during the pandemic. Many took the precautions pretty seriously,” LaMonica says. “They would FaceTime and stuff, but they really missed that in-person connection with them.”
— Dr. Jay Weatherill
“I think the touching, the feeling and the hugging and the physical presence definitely makes a huge difference,” Dalai says. “So whenever I interview my patients the first time, I always stress the social structure because that plays a very big role in treating the mental health disorders.”
Dr. Jay Weatherill is a psychiatrist who practices at Avera Behavioral Health Hospital in Sioux Falls, South Dakota, and primarily treats adult inpatients. He says social isolation is often a precipitating factor identified among patients with depression or anxiety. He calls it is as big of a contributing factor to those conditions as
CHRISTUS Health renames children’s hospital in San Antonio
The Children’s Hospital of San Antonio got a new name in April: CHRISTUS Children’s.
The hospital is part of Irving, Texasbased CHRISTUS Health. The health system said the new name reflects the hospital’s expansion into a network of freestanding emergency centers, specialty, maternal and pediatric clinics as well as outpatient rehabilitation centers located throughout San Antonio and nearby New Braunfels, Texas.
In a press release about the renaming, CHRISTUS said the change is part of a transformation of the hospital’s main campus that will include adding colorful murals and other visual elements to create a sense of cohesion between all of the buildings.

In the fiscal year that began July 1, the CHRISTUS Children’s network has tallied 6,000 children and maternal inpatients; just
under 5,000 surgeries and 105,000 emergency department visits; and more than 180,000 children and expectant mothers as patients at the network’s more than 50 outpatient specialty clinics in 15 locations.
CHRISTUS Health President and Chief Executive Ernie Sadau said: “CHRISTUS Children’s has a bright future ahead with plans for growth into new communities, new providers, and new services.”
Amid the stress and grief the pandemic created, LaMonica says the crisis has brought some beneficial changes. It has reduced the stigma around mental health care and focused national attention on the need for social connection. That attention, she suspects, is what prompted the surgeon general’s advisory.
“I think honestly the biggest thing that struck me is why didn’t this happen before?” she says “You know, why are we in 2023 just talking about loneliness? But I guess it took the pandemic to really bring it to the forefront.”
leisenhauer@chausa.org
Weatherill
Primeaux
“I wish I could write a prescription for social support and it would be that easy. Many people just don’t have it.”
YOU TO THE FRIENDS OF THE ASSEMBLY
LaMonica
THANK
is
from: Silver Friends
Friend HealthTrust Performance Group
University Chicago Mercy Housing Ziegler
Assembly 2023
made possible in part by generous support
Platinum
Loyola
Design plans show how colorful accents will be added to the newly renamed CHRISTUS Children’s hospital in San Antonio. The changes are part of a wider plan to add color and other visual elements to create a sense of cohesion between the hospital and its network of facilities.
4 CATHOLIC HEALTH WORLD June 15, 2023
Johnson
Lights, camera, ethics: CommonSpirit program makes movies the stars of discussions
By LISA EISENHAUER
Before the start of each session of “Ethics on the Big Screen,” Leslie Kuhnel wonders if participants will be searching for tissues before the evening is over.
Kuhnel, vice president — ethics and theology for CHI Health, the Midwest Division of CommonSpirit Health, has seen the tears flow as program participants watch emotionally charged films and hear panel discussions on sensitive topics such as race-based disparities in health care outcomes, living with mental illness, losing a loved one to dementia and facing the experience of homelessness.
The Ethics on the Big Screen education series has been hosted by the CHI Health Ethics Center in Omaha, Nebraska, for almost 20 years. Each session offers health care professionals the opportunity to explore the lived experiences of a particular patient population through a format of film, didactic learning, small-group discussion and expert panel presentations — often including a first-person perspective from a patient or family members. Participants can earn continuing education credits and attend sessions in person or virtually over Zoom.
personal experiences takes the stage to delve more deeply into the topic. Recent sessions have included medical students and other learners from CHI Health’s academic partners, presenting basic information on the topic area of that session.
My Beautiful Broken Brain, the documentary shown in May, explores the struggles of a woman who has to relearn to speak, read and write after suffering a stroke at the age of 34. Kuhnel says the discussion that followed focused on “autonomy, personhood and decisionmaking challenges” for patients recovering from a life-changing acquired brain injury such as a stroke. The panel included a mother who works as a care manager in the rehab medicine setting

and who shared her family’s story following her son’s brain injury.
Aftershock, a documentary about how racial and gender bias factor into poor maternal health outcomes and high rates of maternal death among Black women, screened at the January session.


Doctors and midwives participating in the panel discussion talked about how to address racial inequities in maternal health care including by improving access to prenatal care for members of high-risk groups and by making conscious efforts to counteract the impact of systemic racism and unconscious bias within this population in particular.
Also on the panel was Lynnette Zepeda, who shared her own story about the com-

munication gaps that she experienced as a Black woman and how the initial treatment she got for an ectopic pregnancy made her feel like “a slab of meat on a tray.”
Said Zepeda: “No one would tell me what was going on. They were getting ready to do surgery on me (and) I didn’t know what they were going to do and I don’t know what the outcome would have been.”
But just before the procedure was to start, the lead physician came into the room and explained to Zepeda what was happening and why. The same doctor was at her bedside when she awoke after the procedure. The doctor, she said, “made me feel like a human being and heard me.”
Kuhnel says first-person stories such as Zepeda’s are a powerful part of the participation experience at Ethics on the Big Screen sessions.
Kuhnel generally uses documentaries rather than feature films to anchor the discussion topics. “With more and more powerful stories being told through documentary films, we have the opportunity to dive deeply into a wide variety of ethics questions in health care,” she says.
leisenhauer@chausa.org
The program’s reach had been primarily local with a small regional following throughout the Midwest Division. But thanks to technology developments resulting from the COVID-19 response and a new partnership with a local Omaha arts organization, that has changed.
Ethics on the Big Screen used the arts organization’s theater for its spring event, during which the documentary My Beautiful Broken Brain was shown and discussed. The session was live-streamed for the virtual audience. With the technological advancements, Kuhnel says, “We can offer a high-quality learning experience no matter where our colleagues are located.”
With expanded promotion throughout CommonSpirit, the spring installment drew almost 130 participants from across the health system’s 24-state footprint.
The program uses documentaries to help health care workers “recognize how social stigma and our own biases impact patient care, and how can we be better prepared to care for our patients with compassion and respect for their unique stories and experiences,” Kuhnel says.
Each three-hour session starts with Kuhnel introducing the ethics topic. Following the film screening, attendees break into small groups for in-person or virtual chats about the topic. After that, a panel of health care professionals and people with related
MEDICAID COVERAGE TOOLKIT AVAILABLE NOW.
DOWNLOAD
TALKING POINTS
Crafted for staff to guide patients through the process, including how to update their information
Designed to co-brand or rebrand to align with your system’s guidelines
The documentary My Beautiful Broken Brain, about a woman’s recovery from a stroke she suffered at 34, was the focus of discussion during the ‘Ethics on the Big Screen’ session in May.
Kuhnel
AT CHAUSA.ORG/MEDICAID
PROTECT WHAT’S PRECIOUS.
MESSAGING
The documentary Aftershock, which looks at how racial and gender bias affect maternal health care, was the topic of discussion earlier this year.
CLEAR
TO USE
Featuring direct paths to helpful information and state Medicaid agencies READY
June 15, 2023 CATHOLIC HEALTH WORLD 5
Eldercare administrators
From page 1
Sr. M. Peter Lillian Di Maria, O CARM. “But there are not always enough people to fill these positions. We’re all vying for the same group of people.”
Sr. Di Maria is a member of the leadership team of the Carmelite Sisters for the Aged and Infirm, a congregation that sponsors, cosponsors and serves at more than a dozen eldercare campuses in Florida, Illinois, Iowa, Kentucky, Massachusetts, New York, Ohio, Pennsylvania and Ireland. She also directs the congregation’s Avila Institute of Gerontology.

She says eldercare facilities are looking for people with a desire and passion to guide the care of the elderly and who have the skill set to do so effectively. “When we find those people, they are a treasure!”
Sr. Di Maria says.
Post-traumatic stress disorder
Jenna Kellerman is director of workforce strategy and development for LeadingAge, an organization representing nonprofit aging services providers. She says it is common in nursing homes for residents and staff to be very close — almost like family — since they spend so much time together. So, when COVID-19 took lives and impaired the health and wellness of residents and staff, the impacts hit administrators very hard.
Kellerman notes that many administrators took on additional roles to fill the gap of vacant positions. Some administrators even slept at the facilities they oversaw. The degree of many administrators’ personal investment made the pandemic especially daunting for them. Research is showing that staff who were on the front lines of COVID19, such as aging services professionals, are at risk for post-traumatic stress disorder due to the trauma they experienced working during the pandemic, Kellerman says. She adds this is contributing to retirements and resignations.
Sr. Di Maria says that stress among health care workers — including administrators — was a problem before 2020 but the extreme pressures brought on by the pandemic greatly increased burnout.

She adds that many of the people who have departed from such roles in the ministry were part of the first generation of laity to be formed alongside men and women religious.
Heavily recruited
Kevin Law is director of talent acquisition for Trinity Health Senior Communities, which has 24 senior living and health care campuses in Connecticut, Indiana, Iowa, Massachusetts, Michigan and North Carolina. He says recent dramatic

Studies show staffing shortages, pressures remain in eldercare, including for administrators
Research is bearing out that considerable staffing challenges continue for eldercare systems and facilities, and this includes when it comes to top leadership at those organizations.
shifts in the eldercare job market also are due to job candidates having many choices, with the same skill sets prized in many settings. Many job seekers are opting for gig economy work, he adds. Sr. Di Maria notes many also want a better work-life balance, remote work and reduced hours — perks often unavailable in long-term care administrator roles.
Laura Campbell, Benedictine senior vice president for people development, says given such pressures, there is a “shrinking market” of candidates, including for these positions. She says candidates qualified to apply for such positions are heavily recruited.
Kathleen Murray, Benedictine director of workforce solutions, adds that the pipeline issues are compounded because of recent shifts in eldercare: Since such organizations are adding assisted living options to campuses, administrators must be certified to run not only nursing homes but also assisted living sites. Benedictine has more than 30 communities across Illinois, Minnesota, Missouri, North Dakota and Wisconsin.
Allison Q. Salopeck, president and chief executive of Jennings, says anticipating vacancies in administrator roles “is a topic we always have to pay attention to.” Jennings has four campuses in Ohio.


Leader cultivation
Especially given the dynamics of the eldercare job market, Law says it is ideal to build the pipeline to the top administrator positions from within an organization.
Salopeck agrees. She says: “We need to always ensure we’re cultivating the type of leadership in our organizations” that will build a solid pool of people who have a love of serving elders, alignment with the Catholic health mission and the capability to guide the organization in achieving that mission.
To do this at Trinity Health Senior Communities, Law says that organization
focuses on understanding what it is about the culture that makes people want to stay and then investing in and bolstering those areas. The organization also pays constant attention to succession planning. And it remains in communication with all staff about their job satisfaction, so it can quickly identify issues that could spark an exodus. It addresses problem areas right away, Law says.
All the ministry eldercare leaders who spoke to Catholic Health World say their organizations are very intentional about keeping an eye out for mission-minded staff with leadership potential. The organizations have — or are in the process of developing — formal programs to help those staff build up leadership capabilities so they can advance if they wish to. The programs include formation in the organizations’ spiritual heritage. Jennings’ program is “Reach”; Trinity Health Senior Communities, “Emerge”; and the Carmelites, “Roots of Caring.”
Many of these organizations also have developed mentorship programs to give budding executives support.

LeadingAge offers multiple programs for people aspiring to executive positions in eldercare. It is developing a fellowship to increase diversity in eldercare administration.
Selling eldercare
The eldercare organizations also work to develop the external pipeline, including by countering misconceptions about working in eldercare and building awareness of the positives of a career in that field. LeadingAge’s Kellerman says such education of the public is needed because longterm care is not generally seen as an on-theradar, highly desirable career path, in part because of U.S. society’s focus on youth over old age.
Salopeck says Jennings has established programming to expose students from high school up to the many types of job opportunities at continuum-of-care sites.
She notes that Jennings is fortunate to be in a state where multiple top universities have developed curriculum and programming around long-term care career preparation. Jennings takes part in internship and administrator-in-training partnerships with the universities. Those programs have steered multiple people with an interest in eldercare administration to Jennings. Other executives say their systems have forged similarly effective educational partnerships. Some say they are looking to expand the partnerships significantly.
Law says beyond those educational partnerships, Trinity Health Senior Communities is working on other ways of building awareness of and interest in ministry eldercare roles. The organization is attuned to how it and its leadership are interacting with the community.

“We don’t just sit back, we need to be constantly innovating our processes,” Law says. “This includes projecting our values and culture to the market and making sure we have a strong employment brand.”
He says the organization uses its mar-
According to a poll the LeadingAge nonprofit conducted among its membership of eldercare sites in February and March, 64% of the nearly 900 respondents said the workforce crisis had not improved since LeadingAge last queried on the subject in June 2022.
That same poll found 92% of nursing home respondents and nearly 70% of assisted living respondents report significant or severe workforce shortages.
In the poll 78% of respondents said staff were leaving eldercare for better pay; 53% said they were leaving for better schedules; and 73% said staff were leaving because of burnout.
An analysis of Bureau of Labor Statistics data by the American Health Care Association and National Center for Assisted Living showed that nursing homes have lost 210,000 employees over the course of the pandemic. The AHCA/NCAL released this analysis in January.
In that reporting, AHCA/NCAL said that at the current rate of hiring, nursing homes would not return to pre-pandemic staffing levels until 2027.
McKnights Long-Term Care News found in its 2022 Mood of the Market survey that about 52% of long-term care facility administrators had considered leaving their jobs in the three months prior to the survey.
According to March 2022 reporting in Skilled Nursing News, in a survey the publication conducted, 58.6% of respondents said they expected the administrator hiring climate to get harder. About 32.5% of respondents said hiring administrators has been increasingly challenging because there are not enough qualified applicants. The total respondent count for the survey was 116 operators of small, midsized and large nursing homes.
In the same survey, 65.2% of respondents said they expected administrator retention to get harder. More than 48% of those surveyed said retention had gotten harder due to pandemic-related burnout and current operating challenges.
keting and social media to tell the stories of the important work that goes on at Trinity Health Senior Communities. It also encourages employees and executives to be ambassadors for the system’s sites. Those relationships between the informal ambassadors and people in the community can be leveraged to attract candidates into the pipeline to top positions.
Murray too says it’s vital that people outside the organization know the powerful work going on inside facility doors. “Our faith-based work is definitely a selling point for us,” she says. “People join and stay for the right reasons and it’s a beautiful culture and people do purpose-driven work here.”
Sr. Di Maria says if more people were aware of the life-changing vocations available to them in long-term care, “they’d be banging down the doors to work here.” jminda@chausa.org
Graduates of the Larry Minnix Leadership Academy gather onstage at the LeadingAge 2022 annual meeting in Denver. The Leadership Academy from the LeadingAge eldercare association aims to develop the capacities and competencies of aging services professionals by tapping into their natural talents and authentic leadership styles. Programs like these can help prepare people to enter the pipeline to executive positions in eldercare facilities. Minnix is the chief executive of LeadingAge.
Kellerman
Sr. Di Maria
Law
Campbell
Trinity Health Talent Acquisition Partner Shawn Hewitt speaks with Johani Morillo at a hiring event at Saint Mary Home in West Hartford, Connecticut, in May. Effective recruitment is key to addressing growing concerns about maintaining a stream of strong candidates for top positions in eldercare, say ministry eldercare leaders. Saint Mary Home is part of Trinity Health Senior Communities.
6 CATHOLIC HEALTH WORLD June 15, 2023
Murray
PRESIDENTS/CEOS
Jonathan Brouk to president of Our Lady of the Lake Children’s Health in Baton Rouge, Louisiana, from interim president. The facility is part of Franciscan Missionaries of Our Lady Health System.
Eric Young, chief operating officer of Bon Secours Memorial Regional Medical Center, to interim president of Bon Secours Memorial Regional Medical Center in Mechanicsville, Virginia, and Rappahannock General Hospital in Kilmarnock, Virginia. He replaces Leigh Sewell, who has departed as president.

ADMINISTRATIVE CHANGES
Veronica Scott-Fulton to chief nurse executive of Bon Secours Mercy Health.

Sheri Shapiro to CommonSpirit Health senior executive vice president and chief strategy officer.

Organizations within CHRISTUS Health have made these changes: Anna Gore to chief nursing officer of CHRISTUS Santa Rosa Hospital — San Marcos in Texas; and David Karchut to vice president of mission integration at CHRISTUS St. Michael Health System in Texarkana, Texas.
Tracey Smithson to chief nursing officer for St. Dominic Hospital of Jackson, Mississippi, part of Franciscan Missionaries of Our Lady Health System.

HONOR
The American Society of Business Publications Editors’ ASBPE Educational Foundation has honored Health Progress, CHA’s journal, with its Journalism That
CommonSpirit
Matters Award. The award recognized lead writer Sally J. Altman and the Before Ferguson Beyond Ferguson team for the third installment of a series on racial and health disparities. The American Society of Business Publications Editors first presented the award in 2009. It goes to journalists whose articles have brought about change within their industries. Below, Health Progress Editor Betsy Taylor accepts the award from Paul J. Heney, the foundation’s president.
ACQUISITION
On May 1, CommonSpirit Health acquired Steward Health Care’s five Utah hospitals and affiliated outpatient facilities. The
hospitals and clinics will be managed under CommonSpirit’s Centura Health.
CommonSpirit said in a release that the acquisition marks the return of faith-based health care to the region. In 1875, the Sisters of the Holy Cross established the health care ministry that later would become Steward.
CommonSpirit said “in a tribute to their Catholic heritage, the hospitals and clinics have been renamed in honor of the Sisters of the Holy Cross.”
The hospital name changes: Davis Hospital and Medical Center of Layton to Holy Cross Hospital — Davis Jordan Valley Medical Center of West Jordan to Holy Cross Hospital — Jordan Valley
Jordan Valley Medical Center-West Valley Campus of West Valley City to Holy Cross Hospital — Jordan Valley West Mountain Point Medical Center of Lehi to Holy Cross Hospital — Mountain Point Salt Lake Regional Medical Center of Salt Lake City to Holy Cross Hospital — Salt Lake
Steward Medical Group, the physician group, to Holy Cross Medical Group

CHRISTUS in talks to acquire New Mexico medical center
Irving, Texas-based CHRISTUS Health is in talks to acquire Gerald Champion Regional Medical Center, a 98-bed New Mexico hospital. The organizations have signed a nonbinding letter of intent and are in exclusive negotiations on the acquisition. CHRISTUS and Gerald Champion Regional are aiming to reach a final agreement this summer.
CHRISTUS is a nonprofit ministry system with 43 hospitals in Texas, Louisiana and New Mexico and 17 in Chile, Colombia and Mexico. It has more than 45,000 staff and more than 15,000 physicians. Gerald Champion Regional is in rural Alamogordo in South Central New Mexico. It is an independent, nonprofit community hospital with a Level III trauma center, 33 medicalsurgical specialties and a network of primary and specialty clinics. It has a staff of about 1,000 and contracts with about 160 providers.
CHRISTUS St. Vincent Regional Medical Center is in Santa Fe, New Mexico, which is more than 200 miles north of Alamogordo.
According to a press release on the negotiations, CHRISTUS and Gerald Champion Regional are focused in their talks on elevating the Alamogordo hospital’s mission to serve the community, leveraging the strength of CHRISTUS’ network, investing in capital improvements, expanding recruitment and retention efforts and bolstering clinical capabilities.
Norm Arnold, Gerald Champion Regional board chair, said in the release that amid health care industry changes, “rural community hospitals like ours (are) facing the strongest headwinds.” The hospital’s Chief Executive Jim Heckert said the best way to honor the hospital’s 74-year legacy is “to ensure we have the resources and financial support to care for our community well into the future.”
Specifics on the deal were unavailable as Catholic Health World went to press.
gala raises $2 million


San Francisco Mayor London Breed, right, listens as Wright Lassiter III, chief executive officer of CommonSpirit Health, addresses attendees at the CommonSpirit Health Foundation’s Humankindness Gala. The event held May 18 at City Hall in San Francisco raised almost $2 million to support behavioral health initiatives across CommonSpirit Health. About 350 people attended. The gala was chaired by foundation board members Jed York, chief executive of the San Francisco 49ers, and Kristi Yamaguchi, professional ice skater, Olympian and founder of Kristi Yamaguchi’s Always Dream. Sr. Mary Haddad, RSM, CHA president and chief executive officer, provided a blessing. CommonSpirit will use the funds to help reduce stigma related to mental health, depression and addiction; provide improved access to mental health care for people who are in crisis and seeking care in emergency departments; and implement proactive mental health screening to support people before their mental health concerns worsen to crisis level.
CHA seeks candidates for the position of senior director, theology & sponsorship.
The Catholic health ministry is the largest group of nonprofit health care providers in the nation. It is comprised of more than 600 hospitals and 1,600 long-term care and other health facilities. To ensure vital sponsorship and a vibrant future for the Catholic health ministry, CHA advocates with Congress, the administration, federal agencies and influential policy organizations to ensure that the nation’s health systems provide quality and affordable care across the continuum of health care delivery.
This position serves as a primary resource to sponsors of Catholic health care as they guide their sponsored works, transition to new forms of sponsorship, and come together as a sponsor community. Responsibilities include developing, implementing and evaluating programs, services and products designed to support sponsor groups and bishops; working in cooperation with other service areas within CHA; and providing research, education and formation for evolving forms of sponsorship and governance. Some travel is required.
CHA seeks candidates with:
A minimum of three years of experience in Catholic ministry governance and three-plus years of experience working in canonical sponsorship.
Experience and ability to understand and work collaboratively with church leaders.
Experience in nonprofit, corporate
matters.
Demonstrated expertise in fostering a strong sense of Catholic identity and as it applies to ministry.
Understanding of Catholic theology and canon law as it applies to Catholic health ministry.
Experience with Catholic health care systems and with CHA.
Demonstrated expertise in effective communications and presentations.
Proven leadership experience in management or supervision.
This position requires a Ph.D. and/or master’s degree in theology, canon law or health care, or a combination of these.
Interested parties should direct resumes to the attention of:
Cara Brouder
Senior Director, Human Resources
Catholic Health Association HR@chausa.org
CHA offers a competitive salary and a comprehensive benefits package.
To view a more detailed posting for this position, visit the careers page on chausa.org.
JOB
SENIOR DIRECTOR, THEOLOGY & SPONSORSHIP
Scott-Fulton
POSTING:
KEEPING
UP
Brouk Shapiro Karchut Smithson
March 1, 2022 CATHOLIC HEALTH WORLD 7 June 15, 2023
David Carson
Barbershop program
From page 1
given him inspiration and resources to help his customers take better care of their health. “For a lot of guys in today’s time, life is really stressful, and their blood pressure can go up,” he says. “These guys go through a lot but not all of them go to the doctor. Now, in the comfortable setting of my shop, we can talk about this.”
From reflection to action
Brandy McMahand is a nurse and case manager for Bon Secours St. Francis Health System’s Healthy Outcomes Program. She says the impetus for the Beauty and Barbershop Talk program came after the May 2020 killing of a Black man, George Floyd, by a white police officer. The unrest following that death prompted reflection and discussion about race relations nationwide.
McMahand says Bon Secours St. Francis Health System President Matt Caldwell initiated conversations about how the twohospital subsystem could better address inequities, including around race.

Several ideas rose to the top: building up the pipeline of people of color seeking health care jobs, helping people to manage chronic conditions and advocate for themselves in the health system, and engaging a council of clergy from minority communities in surfacing top health concerns.
McMahand and Sean Dogan, a pastor who is Bon Secours St. Francis community health director, have been guiding the work in these areas.
To pursue the goal of helping people manage chronic illness, they initiated a partnership with the American Heart Association. That organization already had begun developing the barbershop program’s basics but did not yet have a health system partner to roll it out. Bon Secours St. Francis and the association agreed to together launch the program with Greenville barbers and stylists.

Dogan says the two partners agreed to address through program content some of the conditions that rank highest as concerns on Greenville community health needs assessments. These include heart disease and stroke, which often are caused by hypertension. McMahand notes that nationwide these conditions impact more than half of Black adults and are among the leading causes of death for Black people.
‘Trusted place’
McMahand says the Beauty and Barbershop Talk initiative addresses “how to talk about chronic conditions in the AfricanAmerican community.” She says a goal is to reach people of color who may be reticent to interact directly with the health system. They may be avoiding health care providers because they do not trust them or because they do not want to talk about potentially concerning health conditions. Instead of waiting for people of color to come into the health system, this program aims to connect with them “in a trusted place.”
McMahand says the barbershop and hair salon “are places where African Americans spend several hours at a time and share their lives. They get close to their stylists.” She mentions that while other health care providers have worked with barbershops to spread health information in the past, this is the first time Bon Secours St. Francis has done this.
To launch the program, about a year ago McMahand approached barbershops and hair salons in communities with a large population of African Americans. She explained the program and asked them to join.
Those barbers and stylists who accepted her offer took a free class she led about four
months ago. She used curriculum developed with the American Heart Association to provide the group with basic information about heart health, blood pressure, sodium and other healthy lifestyle topics. She taught them to use blood pressure cuffs and to interpret the results on a chart. She told them about where they can refer people who need care but who do not have a
health care provider, including Bon Secours St. Francis. She provided them with complementary blood pressure cuffs and a binder with basic health information. The American Heart Association had donated some of these materials to the group.
McMahand remains a go-to contact for the group and periodically visits to see if the barbers and stylists have any questions or needs.
Opening up dialogue
McMahand says hypertension and other heart conditions can be silent killers, because they can strike when people have had no symptoms. That’s why it’s good, she says, that the Beauty and Barbershop Talk program is opening up dialogue and also placing resources right in the shops. This way people can take action right away — by taking the blood pressure screening in the shop — instead of having to take the time to make an appointment with a health care provider.
She says the program is too new to have statistically reliable results documented. Anecdotally she has heard from numerous participating barbers that people are welcoming the conversation on healthy living. The clients are agreeing to measure their blood pressure. There have been multiple instances of barbershop and salon customers receiving worrisome results from the blood pressure readings in the shops.
McMahand has learned of some customers then seeking out and receiving followup care. They’ve gotten help managing their high blood pressure or other surfaced health condition.
Shell at UpTown says this has been the case for several of his customers. He notes that he and his clientele also now feel comfortable talking about other health concerns more openly. As a result of such conversations a shop customer sought help for depression. Customers have thanked Shell for helping them get the care they need.
Bon Secours St. Francis already is expanding the barbershop program. McMahand in mid-May trained a new group of barbers and stylists for the program — that group has clientele who are predominantly Hispanic.
Bon Secours St. Francis is helping a Bon Secours Mercy Health campus in Richmond, Virginia, to evaluate the program for possible launch there.
Dogan is encouraged to see Beauty and Barbershop Talks spread. He says the program “is important because it’s actually an opportunity for people to take control of their health and not wait until something happens” to get care.
He says, “if it’s important to do self-care and pamper yourself at the salon, why not look wonderful on the outside and be wonderful on the inside too?”
jminda@chausa.org
AWARDS

For innovative programming that changes lives
LIFETIME ACHIEVEMENT AWARD
For a lifetime of contributions
SISTER CAROL KEEHAN AWARD
For boldly championing society’s most vulnerable

SISTER CONCILIA MORAN AWARD
For demonstrated creativity and breakthrough thinking

TOMORROW’S LEADERS HONOREES
Honoring young people who will guide our ministry in the future
Dzenan Berberovic, MA, CFRE, Chief Philanthropy Officer, Avera Health, Sioux Falls, South Dakota
Brian Li, System Director, Community Health Strategic Initiatives, CommonSpirit Health, San Francisco, California
John R. Albright, Jr., Director of Home Care and Georgia Infirmary, St. Joseph’s/Candler Health System, Inc., Savannah, Georgia
Jessica Darnell, MSN, RN, CENP, Vice President Nursing and Chief Nursing Officer, Ascension Saint Thomas Hospital Midtown, Nashville, Tennessee
Elliott Bedford, PhD, Director, Ethics Integration, Ascension St. Vincent, Indianapolis, Indiana; Ascension Via Christi, Wichita, Kansas
John Kohler, Sr., MD, MBA, Southern Illinois Regional Chief Medical Officer, Medical Group President, SSM Health, Saint Louis, Missouri
Zachary Melick, Director of Business Transformation, PeaceHealth, Vancouver, Washington
Tyler Limbaugh, Regional Integration Officer, Ascension Florida and Gulf Coast, Jacksonville, Florida
Lauren King, Senior Director, Talent Strategy and Innovation, HR, Ascension, Saint Louis, Missouri
Ratish Kumar Mohan, Biomedical Engineer, Hospital Sisters Health System, Springfield, Illinois

2 2 3
Recognizing Extraordinary Contributions to the Catholic Health Ministry VIRTUAL ASSEMBLY 2023 CHAUSA.ORG/ASSEMBLY A TIME TO CONNECT
McMahand Dogan
8 CATHOLIC HEALTH WORLD June 15, 2023
Timothy “Dreze” Shell, left, trims a customer at his business, UpTown Barber Shop near Greenville, South Carolina. Through a program from Bon Secours St. Francis Health System, he educates clients about healthy living, including when it comes to heart health.
Rod Hochman, MD President and Chief Executive Officer Providence St. Joseph Health, Renton, Washington
Sr. Linda Werthman, RSM Past Member of Trinity Health Board, Trinity Health, Livonia, Michigan
Sr. Catherine O’Connor, CSB, PhD Congregational Leadership Team of Brigidine Sisters and Covenant Health Board, Covenant Health, Tewksbury, Massachusetts
ACHIEVEMENT CITATION
The Mercy COVID Care @ Home SMS (Short Message Service) Spiritual Care Program
 By LISA EISENHAUER
By LISA EISENHAUER

 By JULIE MINDA
By JULIE MINDA