Vision statement guides CHA’s development of next strategic plan
By JULIE MINDA
CHA is creating its next strategic plan, and it is using its new vision statement as a guide for that process.
The vision statement that CHA unveiled at the virtual Catholic Health Assembly in June is: “We Will Empower Bold Change to Elevate Human Flourishing.”
The association developed the vision statement through engagement with the board, CHA members, staff and other stakeholders. Now, the association is undertaking an extensive process to build ministry consensus around the statement’s meaning and then to apply that understanding as it sets forth its fiscal year 2025 to 2027 strategic plan.
CHA will present that plan to the board for approval at a May meeting. If the plan is approved, CHA will roll it out at the June
Continued on 3
Doctor relishes new role steering Providence toward environmental sustainability
 By KATHLEEN NELSON
By KATHLEEN NELSON
Providence St. Joseph Health has set an ambitious goal: to be carbon negative by 2030. Helping to steer its course is Dr. Brian Chesebro, who recently joined Providence’s national advocacy and social responsibility division as medical director of environmental stewardship.
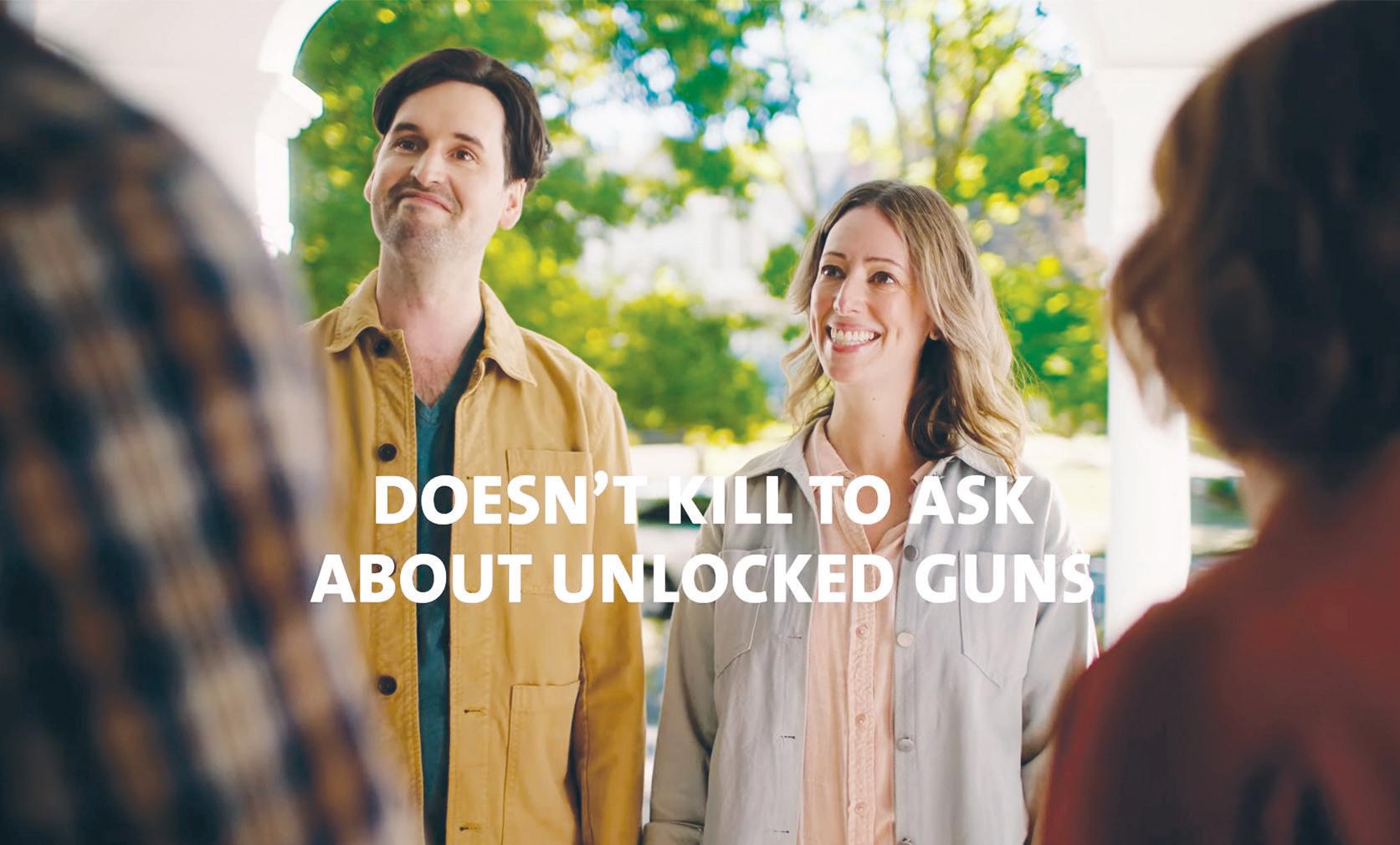
GUN VIOLENCE: ‘A PUBLIC HEALTH CRISIS’

Trinity Health backs campaign that urges parents to ask about unlocked guns
By JULIE MINDA
During pediatric patient visits, clinicians at some Trinity Health Mid-Atlantic facilities are advising parents to inquire about unsecured firearms before their children go to visit a friend or relative.
The office visit discussions are part of a broader campaign that Trinity Health Mid-Atlantic began at the start of this year called “Doesn’t Kill to Ask.” Through those conversations, plus public service announcements, news releases, social media posts, newsletters and other means, the region and its facilities hope to normalize discussions about gun safety so that parents can feel comfortable asking about firearms when their kids are visiting friends and family.
Continued on 4
Hundreds gather for gun violence summit hosted by St. Louis archdiocese
By VALERIE SCHREMP HAHN
SHREWSBURY, Mo. — After the shooting death of 9-yearold Evelyn Dieckhaus along with two other students and three adults at a school in Nashville, Tennessee, in March, members of her grandparents’ parish more than 350 miles away in Washington, Missouri, gathered to pray.

“People showed up in great numbers, not really knowing what to say,” said Fr. Mike Boehm, then the pastor of the parish, St. Francis Borgia. “It was really a time for our church to be seen as a beacon of hope.”
Fr. Boehm was among those who called for the Catholic Church to become a beacon of hope — and action — during a
Continued on 5
CHI Saint Joseph Health pioneers virtual nursing technology
 By DALE SINGER
By DALE SINGER
Patients at Saint Joseph Hospital in Lexington, Kentucky, are getting some of their care from nurse Corey Ross, even though he’s working from hundreds of miles away.
Chesebro
Chesebro will help transform Providence’s clinical delivery of care by reducing pollution through mitigation, developing resilient systems and advocating for planet-safe policies and decisions.
An anesthesiologist by training, his personal struggle and journey have helped put Providence on its climate-friendly path. “In a way, it is my mental health therapy,” he says. “This job and this work saved me.”
Continued on 8
Ross is part of a pioneering effort at Saint Joseph known as virtually integrated care, in which nurses on the floor are joined electronically by nurses whose presence is activated with a simple tap on a wallmounted screen. Hospital officials say the system helps address the nationwide nursing shortage and extend the capabilities of nurses.
“It’s about putting together new models that add technology to help the nurses at the bedside,” says Kathleen Sanford, executive vice president, chief nursing officer, for CommonSpirit Health, which selected
NICU boutique 2 Executive changes 6 Researching All of Us 2
Bastiaan Slabbers/NurPhoto via AP David Carson/St. Louis Post-Dispatch via AP
Students from Philadelphia-area schools join others to protest violence and to demand a safer world. The march was in the Northwest section of Philadelphia in 2022. Trinity Health Mid-Atlantic, which has a catchment area that includes Philadelphia, has a campaign underway on gun safety.
Students gather in a parking lot near St. Louis’ Central Visual and Performing Arts High School after a shooting there last fall. The Archdiocese of St. Louis convened a firearms summit this summer focused on how to reverse the tide of gun violence. Health care workers were among those who spoke out.
SEASON OF CREATION
Decorating with a repurpose. PAGE 3 Check out CHA's resources. PAGE 8 Continued on 6 SEPTEMBER 1, 2023 VOLUME 39, NUMBER 14 PERIODICAL RATE PUBLICATION
Virtual nurse Corey Ross joins via video a discussion with other care team members at Saint Joseph Hospital in Lexington, Kentucky. The hospital’s virtually integrated care program is helping address staffing challenges while adding a registered nurse working remotely to the hospital care team, which includes a bedside nurse and a patient care assistant.
Essentia Health helps sign people up for national All of Us research program
By VALERIE SCHREMP HAHN
A clinic that is part of Essentia Health St. Joseph’s Medical Center in Brainerd, Minnesota, in July hosted workers with All of Us, a program led by the National Institutes of Health to build one of the most diverse health databases in history.
The workers met with potential participants in the research program that is aiming to enroll more than 1 million people. So far, the program has more than 685,000 participants nationally. Essentia, St. Joseph’s parent system, has helped sign up more than 4,000.
People who sign up are asked to share various kinds of information about themselves over time. They may get an in-person appointment, where research staff takes basic physical measurements, does a blood draw, and collects urine and saliva samples. If a participant agrees, researchers then perform full genetic sequencing on the samples through genotyping and whole genome sequencing. Participants get to see genetic results, such as genetic ancestry and health-related DNA traits. They also learn if they may be more sensitive to certain medications.
The samples collected are sent to the biobank at the Mayo Clinic in Rochester, Minnesota, part of their collection of biospecimens used for research.
All of Us began enrolling participants in 2017. Essentia Health joined the effort in 2018. “Participants want to join to learn more about themselves, but also help the
future generations, if you will, to learn more within health research,” said Krystal Klicka, a research and evaluation specialist with Essentia Health.
Reaching underrepresented groups
All of Us aims to include people who historically have been underrepresented in health research, including racial and ethnic minorities, sexual and gender minorities, and rural residents. St. Joseph’s service area in and around Brainerd, 125 miles northwest of Minneapolis, is classified as rural, as is 84% of Essentia’s overall footprint in Minnesota, North Dakota and Wisconsin. Essentia can connect All of Us with that population.

If residents aren’t able to come in physically or don’t have the technology to participate, researchers offer at-home saliva and measuring kits as well as iPads to sign in and answer questions online.
All of Us researchers follow up with occasional surveys, but participants can choose how much they would like to participate.
The program is for those 18 and up, and anyone can participate and sign up on their own, not just through their health system. “Otherwise, just a little bit of your time is really all you’re giving to this program,” said Klicka.
Getting involved
Essentia has used different methods to help sign people up over the years, including community health events and inquiries through MyChart.
“Some people are hesitant, but once we explain it to them, most of them are happy to join,” said Nathan Mukai, a research project coordinator for Essentia and communications lead for All of Us. “We have many participants that have been really eager to join in and contribute.”
The program is free for participants. The information collected for research is kept confidential and secure and is not tied back to a particular person’s name or address, according to the National Institutes of Health. Patients can choose not to receive certain information. They also get to decide whether to discuss any findings with their doctor.
Saint Peter’s children’s hospital offers necessities for NICU babies, toys for siblings
The Children’s Hospital at Saint Peter’s University Hospital in New Brunswick, New Jersey, has opened the Bless U Baby Boutique, a shop stocked with donated gifts and other items for parents whose babies have been admitted to the hospital’s neonatal intensive care unit.
Located across from the NICU, the shop is filled with new toys, books, outfits, hats, blankets and personal care items. All the items are given to parents free of charge. The boutique also gives every family a set of rosary beads.
Parents with other children at home can shop for a toy to bring home to the baby’s sibling. The intent is to help those siblings realize their importance in their growing family.
All items can be gift wrapped.
Catholic Health World (ISSN 87564068) is published semimonthly, except monthly in January, April, July and October and copyrighted © by the Catholic Health Association of the United States. POSTMASTER: Address all subscription orders, inquiries, address changes, etc., to CHA Service Center, 4455 Woodson Road, St. Louis, MO 63134-3797; phone: 800-230-7823; email: servicecenter@chausa.org.
Periodicals postage rate is paid at St. Louis and additional mailing offices.
Annual subscription rates: CHA members free, others $29 and foreign $29. Opinions, quotes and views appearing in Catholic Health World do not necessarily reflect those of CHA and do not represent an endorsement by CHA.
Acceptance of advertising for publication does not constitute approval or endorsement by the publication or CHA. All advertising is subject to review before acceptance.
Vice President Communications and Marketing
Brian P. Reardon
Editor Lisa Eisenhauer leisenhauer@chausa.org
314-253-3437
Associate Editor Julie Minda jminda@chausa.org
314-253-3412
Associate Editor Valerie
Schremp Hahn
vhahn@chausa.org
314-253-3410
Graphic Design
Norma Klingsick
Advertising ads@chausa.org
314-253-3477
Essentia, which includes five Catholic hospitals, is part of the program through the Essentia Institute of Rural Health. Other hospitals may work with the All of Us program’s communications and engagement partners, such as the American Academy of Family Physicians and the Black Greek Letter Consortium, to tell people about All of Us and sign them up.
The National Institutes of Health says more than 4,000 projects in the works now are using data from the program, and group information is available in a public database. The agency, part of the Department of Health and Human Services, says researchers have used All of Us data to find 118 previously unknown genetic variants that could cause health problems; link birthplace to cancer risk in Hispanic communities; and learn that lesbian, gay and bisexual cancer survivors reported a lower mental and social quality of life than heterosexual cancer survivors.
“Being able to learn just from our communities and other communities, it can definitely improve the health within our community, which trickles down to our health care system,” said Klicka.
For more information on All of Us, visit allofus.nih.gov.
vhahn@chausa.org
The idea for the boutique came from Dolly Allen, director of adult emergency services at Saint Peter’s University Hospital, while she was in her previous role as nurse manager of the hospital’s NICU. She explained in a press release, “Families with a baby in the NICU are often caught off guard by their baby’s early arrival. This has left them little to no time to shop for those essential items needed to care for their baby at home.
“Our NICU families experience varying emotions and challenges while we are caring for their baby in the NICU, which sometimes can be for a few days or several months. In our Bless U Baby Boutique, families can feel a sense of normalcy as they select items for their baby while thinking about the day they get to take them home.”
She noted that some families may be in financial need, and the boutique will help them get some of the items they require.
Information on donating to the NICU or the Bless U Baby Boutique is available at saintpetershcs.com/DonateNICU.
Catholic Ethics for Health Care Leaders Virtual Program Tuesdays Sept. 5 – Oct. 17 | 1 – 3 p.m. ET Mission in Long-Term Care Networking Zoom Call (Members only) Sept. 6 | 1 – 2 p.m. ET Emerging Topics in Catholic Health Care Ethics: Telemedicine or Touch in the Physician-Patient Relationship Sept. 6| 1 – 1:45 p.m. ET United Against Human Trafficking Networking Zoom Call Oct. 4 | Noon – 1 p.m. ET Community Benefit 101: The Nuts and Bolts of Planning and Reporting Community Benefits Virtual Program Oct. 24 – 26 | 2 – 5 p.m. ET each day Mission Leader Seminar Virtual Program Tuesdays Nov. 7 – 28 | 1 – 2:30 p.m. ET Upcoming
from The Catholic Health Association We Will Empower Bold Change to Elevate Human Flourishing. SM chausa.org/calendar © Catholic Health Association of the United States, Sept. 1, 2023
Events
many been
An animated video encouraging Americans to take part in the All of Us initiative being led by the National Institutes of Health is among the resources on the program available at joinallofus.org.
2 CATHOLIC HEALTH WORLD September 1, 2023
FROM WASTE TO WHIMSY
DECORATOR’S DESIGNS ARE TRANSFORMATIONAL
Mobiles made of crumbled tissue paper and vaccine vial caps that resemble vivid sea creatures dangle from the ceiling. Cutouts of themed letters of the alphabet — “B” for bee, “C” for caterpillar, “F” for fox — stream in a colorful array across a wall of cabinets. A small plastic dinosaur stands at the ready in a bright yellow cap and vest for crossing guard duty.
SEASON OF CREATION

The décor is part of a back-to-school motif dreamed up by Spanish interpreter Brenda Serna to add whimsy to the pediatric space at SSM Health Dean Medical Group’s clinic on the west side of Madison, Wisconsin.

Serna freshens up her designs often, reflecting holidays and changes of season. Some of her past indoor wonderlands have included paper clouds polkadotted with colorful leftover “COVID-19 vaccinated” stickers; lantern-like hangings made from upcycled plastic bottles; and delicate origami butterflies, some of them

Vision statement
From page 1
2024 Catholic Health Assembly in San Diego.
Sr. Mary Haddad, RSM, CHA’s president and CEO, said the association developed the new vision statement because of the impact “challenging and changing times — particularly with COVID — have had on our members and Catholic health care in the U.S.”
Sr. Mary said CHA’s board recognized that “as we continue to serve in dynamic ways, we must constantly reassess how we approach our work.” She said the board decided in 2022 that a new vision statement was necessary to guide CHA into the future and serve as a compass for its next strategic plan.
Articulation
Katie Hurley, CHA vice president, general counsel and compliance officer, said CHA’s board decided at the start of fiscal year 2023 to postpone its regular work of developing the next three-year strategic plan and focus instead on articulating a vision statement that could guide CHA’s strategy going forward. Then-CHA Board Chair Laura Kaiser headed a special committee to shepherd the statement creation. Kaiser is SSM Health president and CEO. Working with consultant Tenfold Health, that committee gathered the input of hundreds of association stakeholders in various venues and formats, then used that input to develop the statement. Using feedback the board provided in the spring, the spe-
alighting on blossoms cut from the soft wrappers that once covered eco-friendly bamboo bath tissue. The dinosaur is a regular and popular prop, with a wardrobe
cial committee refined the elements of the vision to finalize a concise but impactful statement.
Hurley said, “The board’s energy and alignment throughout the process and its unwavering affirmation of the final vision statement have put the board in a great position going into the strategic planning work that it will undertake.”
Roadmap
CHA Chief Operating and Finance Officer Loren Chandler said CHA staff, under the direction of the association’s executive committee, are helping the board to define in a comprehensive way what the three main pillars of the vision state ment mean. Those pillars are “we will,” “empower bold change” and “ele vate human flour ishing.” Working closely with the board, CHA staff will then help to apply those definitions to the strategic plan.
The association will engage member affinity groups, such as ministry CEOs, in this process. “We are taking our time to develop a strong founda tion,” Chandler said.
As it is developing the strategic plan, CHA also will be determining what its vision roadmap will be. The roadmap will be a projection of what success will look like by 2035 as the vision is pursued and what
Serna coordinates to match the theme of the décor.
She looks to nature for her inspiration and to her surroundings for her material
types of milestones the association will hit along the way.
Amy Ballance, CHA chief of staff, added, “Once the foundation is set with clearly identified strategic goals that support our vision, we can begin the engaging work of setting new priorities and work plans to achieve those goals.”

Broad themes
While CHA is early in the process of defining the terms of the vision, setting forth the vision roadmap and building out the strategic plan, some themes are likely to emerge throughout the process, said Diarmuid Rooney, CHA vice president, sponsorship and mission services.
When it comes to the “we will” aspect of the work, the strategic plan is likely to reflect that CHA is pursuing work in community, and therefore will be seeking to build new and expanded partnerships that enable the ministry to achieve change. Such partnerships will involve community organizations, government agencies, religious congregations and Catholic Church leadership.
When it comes to empowering bold change, the strategic plan will seek ways to bring about systemic shifts that further the ministry’s vision for health care that cre-
— leaves, twigs, cat food boxes, used office paper, plastic parts from spent medical supplies and other cast-off whatnots. “It’s nice to just be able to reuse stuff, to repurpose it,” says Serna, who has worked for SSM Health for 21 years.
She started brightening the main reception area near her ground-level office in the multispecialty clinic with her vibrant creations several years ago. It wasn’t until the COVID-19 pandemic that she thought to add some colorful touches to the pediatrics section on an upper floor as a surprise for the harried staff there.



She first festooned the space with paper flowers. “I did it at the end of the day so by the next morning, when they came in, they were so happy because it was colorful and fresh,” she recalls.
That was three years ago, and Serna continues to use the space as a backdrop for the works of art she has taught herself to make, sometimes with a little help from YouTube videos.
Of the many off-hours she devotes to piecing her designs together, Serna says: “It’s an activity that my brain enjoys.”
She admits that she also enjoys it when her creations delight someone. “I like the smiles,” she says.
ates and sustains a strong, healthy national community. Such a health system will recognize health care as a human right. The ministry’s work under this pillar will aim to ensure equitable access to essential health services across people’s lifespans, with special attention to the needs of low-income and vulnerable people.
And when it comes to elevating human flourishing, the strategic plan will emphasize the common good and whole-person care. The plan will reflect that people’s health and well-being are intertwined with the health and well-being of the broader community, with health care an essential element contributing to the common good. The plan will recognize that for human flourishing, health care must be seen in the context of social determinants of health including education, employment and a safe environment.
Shared goals
Ballance said there is much excitement within the ministry for the new vision statement and the opportunities to apply it to CHA’s strategic work moving forward.
She said members of the ministry “will be able to use those strategic priorities to guide their organizations’ strategic goals.”
“Imagine the impact we can make in our communities if most of our members took on the challenge of bold change, connected their organizations’ priorities with CHA’s broader strategic plan and collectively worked together to achieve those shared goals,” Ballance said. “Talk about bold change!”
jminda@chausa.org
September 1, 2023 CATHOLIC HEALTH WORLD 3
Serna
Brenda Serna adds a colorful alphabet to the pediatrics space at an SSM Health Dean Medical Group clinic in Madison, Wisconsin. Serna began decorating the space, often repurposing cast-off material, during the pandemic with her playful creations. She changes the décor several times a year.
Doesn’t Kill to Ask
From page 1
“Up until now there’s been a stigma attached to people asking about” guns in other people’s homes, says James Woodward, president and CEO of Trinity Health Mid-Atlantic.

“But we’re showing how people can raise the question in a nonpolitical, nonjudgmental way.”
He adds that gun violence “is a public health crisis, and the data shows that gun violence is a leading cause of death in kids. Our hope is that this campaign will spread. If we can save even just one child, it will be well worth it.”
Interwoven issues
The Doesn’t Kill to Ask campaign is from Hospitals United, a collaboration of nearly 200 health systems and hospitals across the U.S., including Trinity Health and others in the ministry. Trinity Health Mid-Atlantic signed on to the firearm awareness campaign because it is in a region with a high rate of gun violence.
Trinity Health Mid-Atlantic includes four hospitals and their affiliated networks: Mercy Fitzgerald Hospital in Darby, Pennsylvania; Nazareth Hospital in Philadelphia; Saint Francis Hospital in Wilmington, Delaware; and St. Mary Medical Center in Langhorne, Pennsylvania. The facilities serve a region that spans parts of Delaware, Pennsylvania and New Jersey.
St. Mary, which is leading the system’s Doesn’t Kill to Ask campaign, is one of the
few Level II trauma centers in a service area that includes parts of Philadelphia. That city, and others in Trinity Health MidAtlantic’s catchment area, have seen rising rates of gun deaths in recent years. The city of Philadelphia reported 2,263 shooting victims last year, of which 217 were younger than 18. That compares with 1,294 shooting victims in 2015; 81 of them were younger than 18.
“Philadelphia is infamous for gun violence now, and we’re seeing that many of the victims are children of color — innocent victims,” says Woodward. He notes that community health needs assessments that Trinity Health Mid-Atlantic hospitals and other facilities in the region have produced consistently show alarming rates of mental health concerns, substance abuse and gun violence. He says these are interwoven issues that have proven intractable.
Dr. Quoc Thai Vu, a general surgeon who practices at St. Mary’s trauma center, says he and his fellow clinicians see the fallout as they tend to gunshot victims of all ages. He says many firearm tragedies are “highly preventable,” particularly when it comes to children. “Often, if the adults in the household had safely secured their firearms, then the kids would not have acquired and used them,” Vu says.

Guard down
When it signed on to the Doesn’t Kill to Ask campaign, Trinity Health Mid-Atlantic got access to a tool kit and customizable materials it could use to spread the message.
In addition to sharing the messages through various media outreach efforts, Trinity Health Mid-Atlantic facilities provided the campaign’s talking points on gun safety to the clinicians who would be speaking with parents in pediatrician visits. Doctors, nurses and physician assistants are among those clinic staff who raise the topic with parents.
Woodward notes that clinicians are encouraged to speak realistically with their patients’ parents about the topic, including acknowledging that conversations about gun safety can be awkward. He says the messages generally have been well received so far.
Adam Garber is executive director of CeaseFire PA, a nonprofit organization that educates about and advocates for gun safety. CeaseFire has partnered with Trinity Health Mid-Atlantic on gun violence prevention efforts in the past and now supports the region’s newest campaign. Garber says a challenge in the past has been that many people see gun-related issues in black-andwhite terms: people are for guns or against guns. People can put their emotional guard up when talking about guns because of this dichotomy. What is promising about the Doesn’t Kill to Ask campaign, says Garber, is that it focuses not on the legality or morality of guns but on responsible gun ownership.
Hospitals United shares tips for checking on gun safety
On its website, the collaborative group Hospitals United offers tips for asking potentially awkward questions about whether guns are properly secured. Parents can:

Say their doctor recommends they ask about gun safety.
Note that other parents also are asking about this.
Include gun safety when asking about other potential threats, such as an accessible pool, harmful allergens or inappropriate media.
Ask friend groups on social media about their take on posing gun safety questions.
Say they heard an expert on television suggesting such questions be asked.
The website, hospitalsunited.com, also includes blog posts on the topic from Northwell Health in New York. Northwell helped originate the campaign. The blog posts cover some of the social nuances around the gun safety topic, ways people can overcome the stigma of talking about it and proper ways for people to secure their firearms.
The physician, Vu, adds that having the awareness discussion with family members is an important aspect of the campaign. He notes that the most effective way to prevent gun violence involving children is to make safety and prevention the responsibility of the entire family. With everyone in a household ensuring that guns are safely secured, there’s less risk of children getting ahold of those weapons, he says.
Toward a national narrative

Woodward notes that this campaign is the latest in a series of efforts to promote gun safety. In the past Trinity Health MidAtlantic has partnered with groups such as local Rotary Clubs to host clinicians from Trinity Health hospitals to speak on the impact of gun violence. And Trinity Health hospitals also have joined with local police departments to provide community members with free gun locks and trigger locks.
Woodward says these efforts as well as the latest campaign could have far-reaching impacts, since gun violence is so prevalent in parts of Trinity Health Mid-Atlantic’s service area. “Our community and our colleagues are really affected,” Woodward says.
“We hope that the more we talk about prevention, the more awareness there will be. This should become a national narrative.
“We hope this movement grows. We have a big tent, and all are welcome,” he adds.
jminda@chausa.org
— James Woodward
Gun violence “is a public health crisis, and the data shows that gun violence is a leading cause of death in kids. Our hope is that this campaign will spread. If we can save even just one child, it will be well worth it.”
The “Doesn’t Kill to Ask” campaign, led by Northwell Health, created a short video acknowledging the social awkwardness, along with the importance, of broaching the topic of gun safety with the parents of children’s playmates. Trinity Health Mid-Atlantic is among the health systems that are taking part in the Doesn’t Kill to Ask campaign. This video can be seen at northwell.edu/lock-guns.
Woodward
Vu Garber 2015 2016 2017 2018 2019 2020 2021 2022 2,500 2,000 1,500 1,000 500 0 81 (10 fatal) 1,294 1,340 1,263 1,449 1,470 2,260 2,337 2,263 100 (15 fatal) 98 (18 fatal) 119 (17 fatal) 119 (15 fatal) 197 (27 fatal) 212 (34 fatal) 217 (30 fatal) Source: City of Philadelphia younger than 18 Philadelphia gun
victims 4 CATHOLIC HEALTH WORLD September 1, 2023
Trinity Health Mid-Atlantic and other participants in a campaign to combat gun violence got access to graphics promoting gun safety strategies.
violence
Addressing gun violence
From page 1
daylong summit to address gun violence convened by the Archdiocese of St. Louis. About 350 people gathered for the July 29 event, called “Addressing Gun Violence: Promoting a Culture of Life.”

The summit featured several speakers and panelists, including Fr. Boehm, who discussed the impact of gun violence. After a lunch break, participants met in workshops on topics such as ministering to survivors and advocating for sensible gun legislation.
“As a church committed to the value of life, we need to address these issues with our Christian Catholic perspective,” St. Louis Archbishop Mitchell T. Rozanski told the crowd. He is the liaison between the United States Conference of Catholic Bishops and the CHA Board of Trustees.
Archbishop Rozanski noted that the bishops conference has spoken pointedly about gun violence, including sending a letter to Congress calling for action after the mass shooting at Uvalde, Texas, in 2022 that took the lives of 19 children and two teachers. “We cannot stand by without living our faith and addressing the issue of gun violence,” he said.
A widespread problem
Dr. Alexander Garza, chief community health officer for SSM Health, pointed out that in 2021 there were more than 48,000 firearm-related deaths in the United States, with 134 people dying each day. Over the past 10 years, the death rate due to firearms has increased by almost 40% nationwide, according to Garza, citing data from the Centers for Disease Control and Prevention. The firearm death rate in Missouri is among the highest 10 in the nation, he said. In the counties that make up the St. Louis archdiocese, 57% of firearm deaths are homicides, compared to 44% across Missouri, he said.

The other gun deaths are suicides.
Most of the gun violence victims in Missouri — 85% — are male, with Black Missourians 17 times more likely than those who are white to die by firearm homicide, he said. Of people who take their own lives by gun, they are 1.9 times more likely to be white than Black and 6.6 times more likely to be men than women, he said.
logical ethics and health care ethics at Saint Louis University, and before that, he was a police officer and correctional officer. When the family moved to Ireland, his daughter stayed in St. Louis with friends to finish her senior year at a St. Louis high school.
He recounted the day last October when he and his wife got a text from her saying her school was under lockdown because of gunfire. A former student was on a rampage, killing a teacher and a student.
“My daughter had to step over this student’s body to escape,” he said, showing a slide with a photo of 15-year-old Alexandria Bell. Central Visual and Performing Arts High School where the shooting took place shares a campus with the school Winright’s daughter attended, Collegiate School of Medicine and Bioscience.
the Bureau of Alcohol, Tobacco, Firearms and Explosives. He lives near the St. Louis school where the shooting took place and responded immediately. As he looked for the shooter, he evacuated students. It was strange to see both innocence and terror in their faces, he said.
“One tall, sweet kid, through a face full of tears, said ‘Thank you. Thank you so much.’
So we reassured him,” McGrath said. “It was clear that this young man had spent an unacceptable amount of time wondering if that was his last day. And I mean that absolutely in the most literal way you can think.”
While his passion for justice is inextricably linked to his faith, McGrath said he and his colleagues in law enforcement see “unacceptable levels of human violence.” He said they agree that their related stress and mental fatigue has been long lasting.
Empowering responders, survivors
Kyle Dooley, a former police officer, spoke about the five members of his family, including his father and grandfather, who died by suicide with a handgun. He now trains police officers on how to respond to people experiencing a mental health crisis in his work with the National Alliance on Mental Illness St. Louis. The group has trained more than 7,000 police officers in the St. Louis region.
“I have realized that I touch more lives today than I ever touched as a police officer arresting people and putting them into our criminal justice system,” he said.
Atif Mahr shared that in the months following the fatal drive-by shooting of his 19-year-old daughter, Isis Mahr, he relied on the help and support of his parish family and his faith in God. Two men were charged in the shooting, but the primary witness died. In July, less than two weeks before the summit, the charges were dropped.
Mahr’s daughter wanted to be a nurse. After her death, he started a foundation in his daughter’s name to mentor youth who would like to become nurses.
Garza hopes people see that the issues surrounding deaths and injuries from firearms are complex, he said. “They’re not just a law enforcement problem,” he noted. “They’re not just a public health problem. It’s all of our problem.”
A school shooting hits home
Tobias Winright is a professor of moral theology at St. Patrick’s Pontifical University in Maynooth, Ireland. Before that, he served as an associate professor of theo-
85% of homicides involve a gun
The decision to move to Ireland was difficult, but the gun issue factored into it, Winright said. He pointed out that Ireland is a “very Catholic” country, with about 50 to 70 gun deaths a year.
At the summit, he reviewed the long history of nonviolence taught by the Catholic Church, which he said stresses that lethal force must be used in moderation. “Rights are always accompanied with responsibilities,” he said.
Michael McGrath is a special agent with
Black Missourians are 17 times more likely than their white counterparts to die by firearm homicide — and 9.5 times more likely than Hispanics.
Men are 4.7 times more likely than women to die by firearm homicide. More than half of the victims are ages 15-34.
62% of gun deaths among children and teens result from interpersonal violence.
“To walk with the spirit of God teaches me to be a blessing to my community, to say, ‘Hey, I need to forgive, move on, so I can continue to live in a godly manner,’” Mahr said. “And whatever God has planned, it will bring her justice.”
Lori Beck, a trauma nurse specialist with St. Louis Children’s Hospital, spoke about her 28 years of taking care of kids injured or killed by firearms. “It takes a toll,” she said. “I remember faces. I remember their stories. I very clearly remember the sounds of grieving families.”
When she first started at the hospital, she and her colleagues took care of three to five firearm injuries a year. Now, it’s more than two gunshot wounds a week, something they handle with the same frequency as simple surgeries like appendectomies.
61% of suicides involve a gun
90% of gun suicide attempts are fatal. White Missourians are 1.9 times more likely than their Black counterparts to die from firearm suicide — and 2.6 times more likely than Hispanics.
Men are 6.6 times more likely than women to die of gun suicides.
Source: Centers for Disease Control and Prevention statistics, 2018-2021
A few years ago, Children’s and St. Louisbased BJC HealthCare began giving away gun locks. They since have handed out about 30,000 in all. Preliminary data shows that the number of intentional firearm injuries seen since at Children’s has remained about the same, but unintentional injuries are down by half, she said.
Looking out at the crowd, she said: “This gives me so much hope. I do know I want to be part of the solution.”
vhahn@chausa.org
University of Iowa to acquire Mercy Iowa City; Catholic provider has filed for bankruptcy
Mercy Iowa City has signed a letter of intent with the University of Iowa for the university to acquire Mercy’s facilities.
In a related move, the Iowa Catholic hospital has filed to reorganize under Chapter 11 of the U.S. Bankruptcy Code. In a press release, Mercy leadership said plans call for Mercy to seek court approval of a sale process, with the university serving as the “stalking horse bidder.” The goal will be to transition the hospital and its employees to a new owner and operator.
Under this plan, the university will acquire substantially all the operating facilities and key assets of Mercy, preserving the continuity of care for patients and continuing opportunities for physicians and employees, the hospital said.
According to the bankruptcy filing, the university plans to pay $20 million for the purchase. The 194-bed Mercy Iowa City hospital and clinics remain open during this process.
Tom Clancy, chairman of the board and
CEO of Mercy Iowa City, said in a release that “Mercy Iowa City believes this plan is the best path forward to preserve our hospital operations.”
Mark E. Toney, Mercy Iowa City chief restructuring officer, said in the release that “the recent actions of one of our largest creditors has significantly and negatively impacted the hospital and resulted in this bankruptcy filing. The board and management moved rapidly to secure a partner to maintain health care in our community.”
According to the release, Mercy Iowa City has filed a motion with the bankruptcy court to use its cash and investments to fund operations. Mercy also has asked the court to allow the hospital to be able to pay employees their wages and benefits. According to information from Mercy, the hope is that the sale process will be completed by about mid-October.
Mercy Iowa City has a medical staff of 250 physicians, and it has 1,350 employees. It was founded by the Sisters of Mercy in 1873.
Firearm violence in Missouri
“We cannot stand by without living our faith and addressing the issue of gun violence.”
— Archbishop Mitchell T. Rozanski
St. Louis Archbishop Mitchell T. Rozanski listens from among a crowd of about 350 people who attended the firearms summit led by the archdiocese at the Cardinal Rigali Center in Shrewsbury, Missouri. The archbishop and many other speakers called for the Catholic Church to take a lead role in finding ways to address gun violence.
Garza
September 1, 2023 CATHOLIC HEALTH WORLD 5
Valerie Schremp Hahn/@CHA
PRESIDENTS/CEOS
Dr. Richard R. Vath plans to retire in June as president and CEO of Franciscan Missionaries of Our Lady Health System of Baton Rouge, Louisiana, a position he has held since 2019. He has worked as a physician and in health care administration for more than 40 years. FMOLHS has secured executive search firm WittKieffer and has formed a committee to select his successor.
Avera Health has made these changes:
Doug Ekeren is transitioning out of the position of regional president and CEO of Avera
Virtual nursing
From page 1
Saint Joseph as a pilot site. Saint Joseph is within CHI Saint Joseph Health, part of CommonSpirit Health.
CommonSpirit Health is one of several systems in the Catholic health care ministry using virtual technology to enhance their inpatient nursing care. For example, Providence St. Joseph Health and Trinity Health have created teams with nurses joining through telehealth to give bedside care providers more time for hands-on care. The same is true for Intermountain Health, a system that includes Catholic hospitals that were once the separate SCL Health system.
At Saint Joseph, Melissa Bennett, chief operating officer/chief nursing executive of CHI Saint Joseph Health, Kentucky, explains the simplicity of the system the hospital is piloting. “If I’m a bedside person, I walk into the room, I can call the virtual nurse. I simply tap the screen,” she says.
The screen tap sends an audible alarm to the virtual nurse. That virtual nurse, for privacy, will come on verbally and introduce himself or herself, and then ask permission to come on to the screen.
“Nurses utilize the virtual nurse. Patients and family utilize the virtual nurse. Physicians utilize the virtual nurse, technical staff pharmacy, care management,” Bennett says. “Everyone has the ability to tap into that virtual nurse.”
For Ross and other virtual nurses, the technology provides innovative, more efficient ways to use their skills and their time. “I get many, many calls throughout the day from patients and their families, and it’s great because that’s what we’re here for,” he says.
COVID and the nursing shortage
The virtual nursing idea, Sanford says, goes back to 2008, as part of the long-term plan of Catholic Health Initiatives, the system that along with Dignity Health merged in 2019 to form CommonSpirit Health. Its timeline projected that by 2020 virtual nursing would be a part of the system’s acute care. In 2011 a white paper forecast how virtual nursing could play a major role in the future, and in 2016 the system got a patent. Then came the COVID-19 pandemic and the nursing shortage. Sanford says CommonSpirit realized that “we had better get started on new models. The thought was that with this shortage, we needed to do

Queen of Peace Hospital of Mitchell, South Dakota, in the next year. He will continue as regional president and CEO of the Avera Sacred Heart region that includes the Yankton, South Dakota, hospital and surrounding facilities. Dr. Hilary Rockwell, who was chief medical officer at Avera Queen of Peace, succeeds Ekeren as regional president and CEO of that facility.
John Emery to president of Bon Secours Memorial Regional Medical Center of Mechanicsville, Virginia, and Bon Secours Rappahannock General Hospital of Kilmar-

nock, Virginia. He was president of Bon Secours Southside Medical Center in Petersburg, Virginia, and Bon Secours Southern Virginia Medical Center in Emporia, Virginia.
Claudio Ferraro to president of Ascension Via Christi St. Joseph of Wichita, Kansas, from Ascension Medical Group Via Christi chief operating officer. Ferraro replaces Robyn Chadwick, who retired Aug. 31.


Russell J. Woolley to president and CEO of CHI Mercy Health in Roseburg, Oregon,
effective Oct. 2. He succeeds Kelly Morgan, who has retired. Woolley was vice president and chief operating officer of Virginia Mason Franciscan Health’s St. Francis Hospital in Federal Way, Washington. The facility is part of CommonSpirit Health.


ADMINISTRATIVE CHANGES
CommonSpirit Health and one of its facilities have made these changes: Lilicia Bailey to senior executive vice president and chief people officer. Dr. Charlie Abraham to chief medical officer, Dignity Health — St. Bernardine Medical Center San Bernardino, California. Ardel Guillamas Avelino to vice president and chief operating officer of Dignity Health — St. Mary Medical Center in Long Beach, California.
Catherine Codispoti to senior vice president and chief people officer of Mercy of Chesterfield, Missouri, beginning Dec. 1. Corinne R. Francis to Trinity Health executive vice president and chief mission integration officer, effective Oct. 23.




only to transitioning from floor nurse to virtual nurse but to an atmosphere in Kentucky that varies from that in her former job in Zimbabwe. She learned quickly how to handle the differences.
“Initially, I thought it’s all about just sitting on the screen and just talking to your patients. And I wanted to do much of the physical work on the floor,” Kujinga says. “But when I got into it, I realized there’s a lot of work, because I have to talk to doctors, I have to talk to nurses, I have to talk to therapists, I have to talk to my managers — every problem that needs to be solved.
“You have to know everything. So that’s how different it was for me. There’s a lot that I learned. And there’s a lot of help that I gave my colleagues and my patients.”
something totally different and take advantage of the new technologies that were emerging. So we did.”
Bennett says Saint Joseph started virtually integrated care with a small set of patients in December 2022 and quickly expanded, in terms of both the rooms involved and the focus of the program itself.
“When we first went live, we were really focused on making sure we had a good connection, and that the image was clear, and that they could hear everything,” Bennett says. “Then the question became: Is this going to work?”
That question was quickly answered. “If I took this away from the providers, they would be distraught,” Bennett says. “The providers recognized how valuable it is to have that point person who’s helping to connect all the dots.”
Anthony A. Houston, CEO of CHI Saint Joseph Health, Kentucky, says the combination of in-person and on-screen attention has worked well.
“What you find is people really enjoy the experience,” he notes. “And when we talk to our caregivers, they’re also enjoying the experience a lot. We’re
touching the patients in a way that we just couldn’t touch them before. It’s really powerful and exciting.”
Virtually from the start
From the nursing point of view, Ross says that expanding the treatment team virtually helps both him and his patients, even though he works remotely.
“When we do our admissions, we make sure to explain what our role is in the plan of care, because I feel like it comforts them,” he says.
Ross says virtual nurses tell patients: “We’re here at all times to answer any questions you might have. If you have any concerns that you might need to be conveyed to a doctor, I can call and contact the doctor any time. I can go through your medications with you to let you know more if you have questions about those. And then I can review the doctor’s notes.”
Ross credits his in-person experience in several units of the hospital, before he moved to northern Indiana, with helping him become comfortable and be successful working virtually, especially in a time when nurses aren’t always easy to find.
“It’s different than floor nursing, I will say that. The time management aspect of it is just as critical, because we have larger patient loads than the typical floor nurse might have,” he says. “We start working towards discharge from the time they’re admitted. So we need to identify those barriers. Does that patient need things at home? Do they have a place to go when they leave the hospital? How are they going to get there? Just identifying patient needs right off the bat is something we’re able to take hands on.”
Nurse Tendai Kujinga had to adjust not

And for patients, Kujinga says: “Most of them were like, ‘Oh wow, this is really cool. I like this because I can just talk to somebody.’”
Expanding screens
The virtual nurse software used at Saint Joseph is a proprietary system. The system also provides virtual admission, discharge and transfer nursing services. It is used now in other CommonSpirit facilities and it is headed to more, with plans for virtual nursing in all CommonSpirit markets by the end of this year.
The expansion, Sanford says, will not leave traditional best medical practices behind.
“We are never not going to be hands-on in nursing because people who come to the hospital are sick enough to need handson,” Sanford says. “This is just an addition to our team.”
And it’s a good one, she says, based on patient surveys and evaluations, which have shown improvements in areas such as communication and discharge information.
Sanford expects the next generation of nurses to be well-versed in virtual processes and other advances, both current ones and those on the horizon. “We have partnerships with a couple of different universities who are just now beginning to teach their students that they will be going into a different environment,” she says.
And in that environment, Bennett adds, the real benefits to the nursing staff are easy to spot.
She says: “What we hear from our nurses is this: I have the ability to go home at the end of the day and feel joy — joy that I was able to meet the needs of my patients, because I know that I’ve got that extra support virtually to help make sure everything is connected.”

KEEPING UP
Ha'Jra Winn, a monitor tech-health unit coordinator and a nurse extern with Saint Joseph Hospital in Lexington, Kentucky, works closely with other members of the virtually integrated care team to ensure patients are connected with both the virtual nurse and bedside caregivers. Saint Joseph is a pilot site for the program that will expand by the end of the year across CommonSpirit Health. Sanford
Bennett
Houston
Kujinga
Rockwell Woolley Codispoti Ferraro Abraham Chadwick Avelino
“I get many, many calls throughout the day from patients and their families, and it’s great because that’s what we’re here for.”
6 CATHOLIC HEALTH WORLD September 1, 2023
— Virtual nurse Corey Ross
PeaceHealth partners with Y to develop wellness programming



The Eugene, Oregon, Family YMCA and PeaceHealth are collaborating in a 10-year contract to develop a suite of combined educational, wellness and health programming for youth, adults and families at a center planned to open in December.
The $1.25 million PeaceHealth partnership includes the naming of the new Y’s health and wellness center, which will be called the PeaceHealth Wellness Center.
The decade-long medical partnership begins when the new Y opens in December.
“A key strategic goal for PeaceHealth is to continue to expand wellness services into our communities,” Susan Blane, director of community health for PeaceHealth Oregon, said in a press release announcing the partnership. “The Y is a perfect partner to accomplish this. Early preventative care is necessary to combat disease and illness that can have devastating results. PeaceHealth is looking forward to supporting the Y in creating healthy habits that will last a lifetime.”
The Y and PeaceHealth plan to assign measurable goals to joint community wellness programs, preventative medicine and medical screenings easily administered and assessed in a nonclinical environment.


Health Calls




Goal development will focus on common, chronic, preventable disease processes and the elimination of health risks. These programs will be managed by a committee comprising Y and PeaceHealth leaders.
Dignity Health — St. Rose Dominican builds fifth neighborhood hospital

Dignity Health — St. Rose Dominican Hospitals broke ground Aug. 10 on a new neighborhood hospital in the Centennial Hills community in Las Vegas.
The 24,000-square-foot facility on two floors will include 10 inpatient beds and eight emergency exam rooms, including a dedicated triage room. There are four existing Dignity Health Neighborhood Hospital campuses. The neighborhood hospitals are built and operated through a partnership with Emerus Holdings. Dignity Health runs three acute care hospitals in the Las Vegas valley. St. Rose Dominican is part of CommonSpirit Health.
CHRISTUS Spohn Hospital triples size of emergency department
CHRISTUS Spohn Hospital Corpus Christi — South in Texas has expanded its emergency department to nearly 19,000 square feet, more than triple its original size.
The hospital now has 27 dedicated emergency bays and rooms, focusing on privacy for patients and their families. The emergency department was also revamped to provide a comprehensive range of medical services, from advanced radiology and diagnostics to a stat lab that speeds test results, expediting the diagnosis and treatment process.
St. Vincent celebrates 125 years in Billings, Montana St. Vincent Healthcare in Billings, Montana, kicked off a yearlong anniversary on Aug. 7, 125 years after the first cornerstone was laid for what would become the city’s first hospital.
St. Vincent Healthcare, now part of Intermountain Health, was founded by the Sisters of Charity of Leavenworth at the request of the city’s first mayor and first Catholic priest. At the time, it was known as St. Vincent Hospital.
St. Vincent has been recognized as an innovator for advancements in heart, stroke, neurological and cancer care. It includes the region’s first pediatric intensive care unit, which includes the only pediatric surgery program serving eastern Montana, northern Wyoming and the western Dakotas, according to the hospital. Caregivers celebrated on Aug. 7, and the year will include several special events to share St. Vincent’s history and vision for the next 125 years, including a benefit, displays, lectures, and a closing celebration and Mass in August 2024.
Pickleball complex opens at Avera campus; public welcome

Avera Health has opened the largest dedicated pickleball complex in South Dakota at the Avera on Louise Health Campus in southwest Sioux Falls.
The Linda Erickson Pickleball Complex includes 12 regula tion size courts, as well as a large parking lot and public restroom for players. The public is welcome to use the courts, free of charge. Member ships will be available on four of the outdoor courts to give players the opportunity to reserve courts.
“Generous community members made this project possible through their philanthropic support,” Dzenan Berberovic, Avera chief philanthropy officer, said in an announcement about the project. “Families who enjoy the sport collaborated with us on this project, and this new complex is the exciting result. We are grateful for their generous support.”
IN BRIEF
Bringing together thought leaders to discuss a more just and healthy society Visit chausa.org/podcast Health Calls Catholic Health Association of the United States SUBSCRIBE TO CHA’S OFFICIAL PODCAST Health Call Health Care Ethics and Artifi...
March 1, 2022 CATHOLIC HEALTH WORLD 7 September 1, 2023
Members of PeaceHealth Oregon’s Community Health team join others to check out progress on a YMCA set to open in December in Eugene. The PeaceHealth Wellness Center is part of the project.
CHA offers resources to enhance Season of Creation celebration
SEASON OF CREATION
CHA has gathered a collection of resources in celebration of Season of Creation 2023.
The annual ecumenical celebration of prayer and action to protect the Earth takes place from Sept. 1 — the World Day of Prayer for Creation — to Oct. 4 — the Feast of St. Francis of Assisi. The theme for this year’s Season of Creation is “Let Justice and Peace Flow.” The symbol for the celebration is a river.
The event’s website notes: “Prophet Amos cries out: ‘But let justice roll on like a river, righteousness like a never-failing stream!’ (Amos 5:24) and so we are called to join the river of justice and peace, to
take up climate and ecological justice, and to speak out with and for communities most impacted by climate injustice and the loss of biodiversity.” The website is seasonofcreation.org.
In his World Day of Prayer for the Care of Creation, Pope Francis reiterates these themes and urges action. He asks that everyone “transform our hearts, our lifestyles, and the public policies ruling our societies.”
CHA’s resources for Season of Creation include reflections, prayers and links to coverage of environmental sustainability efforts across the Catholic health care ministry that can help respond to Pope Francis’ call in his World Day of Prayer message to “join hands and take bold steps” to heal the Earth.
Season of Creation 2023 Let Justice and Peace Flow
In 2019, Providence Oregon named Dr. Brian Chesebro its first medical director of environmental stewardship. Since then, the system’s facilities in Oregon have decreased greenhouse gas emissions from anesthesia by 96% and reduced overall carbon emissions by 11.5%. The change has saved the system $2 million annually on the cost of anesthesia.
Chesebro
From page 1
True to his (Bitter)roots
Raised on a ranch in Montana’s Bitterroot Valley, Chesebro loved rock climbing, skiing and backpacking with friends and family. His father conducted research in virology at the National Institutes of Health Rocky Mountain Laboratories in Hamilton.
“My whole life was built around the environment,” says Chesebro. “I was simultaneously exposed to environmental stewards and the world of science and biomedical research.”
Yet he didn’t envision his love of the great outdoors shaping his career path when he graduated from The Johns Hopkins University School of Medicine in 2003 or when he completed his residency in anesthesiology and perioperative care at the University of California, San Francisco, in 2008. The next year, he joined the Oregon Anesthesia Group, which provides services to three Providence hospitals. Starting in 2015, he served concurrently with the anesthesia group and as Providence’s medical director of anesthesiology and perioperative quality.
Eco-despair
Living through wildfires, flooding and other extreme weather wrought from climate change took a toll on his spirit and led in 2016 to behavioral health struggles known as solastalgia. “I call it eco-despair, and I had a severe case,” he says. “I think it’s an underappreciated and underrecognized mental health challenge we face as a species as we try to make sense of climate change.”
Seeking guidance, Chesebro turned to the “Hopes and Aspirations for Providence Ministries” document written by the founding Sisters of Providence when they established the health system’s public juridic person, Providence Ministries. The document encourages the ministry to be “good stewards of all we have been given for this ministry — our people, our resources, and our Earth.”
The message inspired Chesebro to take a personal inventory of his own carbon footprint. He assessed and modified his home energy use, transportation and diet. But he also realized that he could have a larger impact professionally by changing his choice of anesthesia.
According to the international coalition Health Care Without Harm, the health care industry’s climate footprint is equivalent to 4.4% of global net emissions. If the health sector was a country, it would be the fifth-largest emitter on the planet. Anesthesia contributes to the sector’s emis-
sion of greenhouse gases. By choosing the anesthetic sevoflurane over desflurane, Chesebro says clinicians can reduce their carbon footprint by 90% and save money without compromising safety and efficacy for patients.
Spreading the word
A self-described data geek, Chesebro has shared his personal research and findings regarding sevoflurane with his colleagues to encourage them to switch anesthetics. He also has shared his message nationwide, again with the Hopes and Aspirations document as his touchstone.
“The sisters specifically called out environmental stewardship and expected Providence to be modeled so that others can learn from us,” he says. “It’s part of the mission that we’re constantly reaching out and helping others.”
In 2019, Providence Oregon named Chesebro its first medical director of envi-
ronmental stewardship. Since then, the system’s facilities in Oregon have decreased greenhouse gas emissions from anesthesia by 96% and reduced overall carbon emissions by 11.5%. The change has saved the system $2 million annually on the cost of anesthesia.

Chesebro later applied his data-driven approach to environmental stewardship throughout Providence’s Oregon facilities, extending it to nonclinical areas. For example, he helped Providence Willamette Falls Medical Center in Oregon City source 100% renewable electricity.
He also helped design and implement the WE ACT Scorecard that each Providence hospital receives every month. The scorecard tracks resource use, cost and carbon emissions categorized by the scorecard’s acronym: Waste, Energy and water, Agriculture and food, Chemicals and Transportation.
His new systemwide role is under the
umbrella of Providence’s advocacy and social responsibility department. Though he has narrowed his responsibility to clinical innovations, his reach extends throughout the seven states that Providence serves. The system hopes that achieving its goal of being carbon negative by 2030 also results in annual savings of $100 million.
Beyond mitigation
To this point, Chesebro says, much of the work has focused on mitigation strategies. More opportunities lie ahead in improving the system’s environmental resilience. For example, Providence hospitals, lacking HVAC upgrades, “struggled to keep the outdoor air distinct from the indoor” during wildfires in 2020 and 2021, Chesebro says. Conversely, with new insulated windows and a reflective skin on the outside, Providence St. Vincent Medical Center stayed cool enough for patients during a heat dome in Portland in 2021.
“Our infrastructure was not designed for the climate we’re experiencing,” he says. “We need to think critically and prepare so our doors can stay open and we can remain a safety anchor. We know that when our vulnerable struggle, they often come to a haven, like a hospital, for protection.”
Chesebro performs the bulk of his environmental stewardship duties from home, which gives him time to see his three children off to school in the morning.
— Brian Chesebro
“I’m in position to help them navigate their early adolescence,” he says. “And working from home is better for the environment. I love it. It’s a very full life.”
Meanwhile, Chesebro continues to provide clinical care in Providence Portland Medical Center’s operating rooms two days a week. He says he thinks it’s important for those steering the system toward environmental sustainability to be connected to the practice of health care.
“We need to maintain contact to keep a strong sense of what we do in a hospital and how these changes really work,” he says. “We can spend a lot of time writing papers, but our ultimate goal is to translate those ideas into action.”
>> The Season of Creation resources are available at chausa.org/soc.
Dr. Brian Chesebro is an anesthesiologist who has worked to convince others to join him in switching to the use of an anesthetic that has a smaller carbon footprint. Chesebro this year became the first medical director of environmental stewardship for Providence St. Joseph Health.
“Our infrastructure was not designed for the climate we’re experiencing. We need to think critically and prepare so our doors can stay open and we can remain a safety anchor.”
8 CATHOLIC HEALTH WORLD September 1, 2023

 By KATHLEEN NELSON
By KATHLEEN NELSON


 By DALE SINGER
By DALE SINGER