
7 minute read
In the beginning: Interview with professor emerita Judy Holt
By Linda Hulton
Hired in 1981, Judy Holt quickly proved to be a dynamic faculty member who was instrumental in shaping the JMU nursing program for the first 20 years. She provided a level of clinical expertise that enabled and inspired over 1500 nursing students to achieve excellence. Holt considers her greatest accomplishment to be the legacy of her students.
Advertisement

Maureen Chambers receives nursing program’s first pin from President Ronald Carrier as Dean Marcia Dake looks on.
Tell me about your memories of the start-up of the JMU nursing program.
During the 1960-70s, JMU started exploring the idea of developing some pre-nursing courses in conjunction with the Rockingham Memorial Hospital’s nursing program. That program was highly respected in the community and the administrators wanted to support the RMH nursing students by preparing them in the prerequisite science courses so the students could eventually go on to finish their Bachelor of Science degrees in nursing if they desired. During the 1970s, many of the hospital diploma nursing programs were closing. Rockingham Memorial Hospital’s nursing program opened in 1912 and closed in 1977. JMU’s President Dr. Carrier was always a great supporter of a nursing program at JMU and he began a State Council on Higher Education for Virginia (SCHEV) proposal in 1972. There was initially some opposition to the proposal locally with concerns about the expense of a new nursing program and concerns about the ongoing recruitment of nurses to staff the healthcare systems in the Shenandoah Valley. There was a strong feeling that students may not stay in the Valley, but continue their careers elsewhere. Finally, SCHEV approved the proposal in 1979 and Dr. Marcia Dake was hired as the first department head. The first nursing class of 21 students was admitted in 1980 with four nursing faculty supporting the new program.
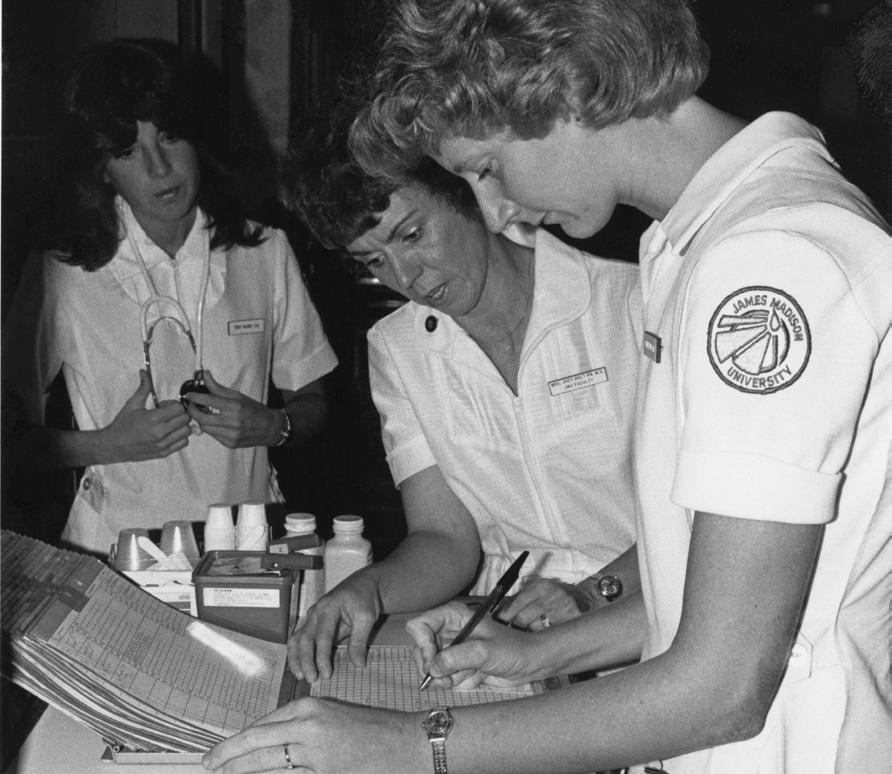
Judith Holt (center) supervises students nurses Terry Mooney (left) and Sharon Liskey as they enter information on a patient’s chart.
What were some of the challenges you faced in the early days of the program?
The applications from students was overwhelming and the faculty had a difficult time choosing which of the outstanding students to admit to the new program. It was a painful process and many parents complained to the Board of Visitors about the selection process. The writing of the curriculum and preparing for the immense challenges of acquiring clinical sites in the community was a challenge. We also had the overwhelming job of recruiting and selecting faculty in a time when they would choose to take a salary that was much less than they could make working in the hospitals as a nurse. In the end, three nursing colleagues developed the curriculum and arranged for all the student clinicals over one summer. Most of us did not have any teaching experience, but we were expert clinicians. I remember as a clinical instructor, I would have seven to nine students on a floor and was responsible for 12 to 18 patients on any particular day. Finally, in the summer of 1982, we wrote the accreditation papers to be submitted to the National League for Nursing (NLN).
Once the program was up and running and we had received accreditation, President Carrier was sent on sabbatical and another university administrator was in charge of the budget. Nursing has always been expensive due to the number of faculty required in the clinical arena to supervise students. Some of the Board of Visitors were questioning the financial viability of the program and were also concerned that the nursing graduates were moving on to bigger medical centers like Duke and Johns Hopkins and not staying in the Valley. When President Carrier got word of this, he came out of sabbatical and we had a big meeting. Parents, students and patients began to write letters to the Board of Visitors and the local hospital administrators to show support of the program – and it was saved.
What do you remember about Dr. Marcia Dake, JMU Nursing’s first Department Chair?
Marcia was a champion for the program, but a real taskmaster. She was tried-and-true to the program and respected the opinions of the faculty that were hired. She had a lot on her back due to the negativity of the early days of the program and she had to spend a lot of time convincing the administrators about the need for financial resources for the program. But, she had a kind heart. I remember that day that I interviewed, my babysitter fell through. She said it was okay to bring along my 5-year-old son who sat in my lap during the entire interview.

A tradition of jumping in Newman Lake in full uniform to celebrate the end of classes was short lived.
What do you remember about Dr. Vida Huber who came after Dr. Dake retired?
Vida and I lived in the same neighborhood and our children were such good friends. We had collaborated on many projects previously while she was on faculty at Eastern Mennonite University. Her Mennonite background gave her a deep heart for service. The Institute for Innovation in Health and Human Services (IIHHS) began as an idea in the nursing department and then she made it a reality when she became Associate Dean.

Vida Huber, JMU Nursing Department Head 1988-1999
What major changes took place on campus while you were a professor at JMU?
The nursing department moved to four different locations. Originally, we had the top floor of Wilson Hall. They had to take down walls between classrooms to make a nursing lab. They couldn’t get the equipment up through the elevator, so they used a crane to hoist the hospital beds up to the top floor.
Those were also the years when the nursing students would jump into Newman Lake after the capping ceremony. Then, we moved to WinePrice which was the original dorm of the RMH School of Nursing. It was like the “ghost” of nursing past. The bottom floor was a learning lab for child development and the College of Education. Some of the children of the nursing professors were there as a day care center. We finally had a few more floors to expand our growing nursing program and properly equipped labs.
Then, we moved to CISAT. We had wonderful roomy labs and large spaces including an alternative therapy lab that included massage beds, aromatherapy, etc.
What kinds of opportunities do you remember having during the early days of the program?
Well, we were so new that we could try anything. As faculty, we had to go into the clinical settings and be really comfortable in any area. We had to educate the physicians on how to work with nursing students. Back in the early days, the nurses and the students had to give up their chairs when a physician entered the nursing station. I remember one physician who disrespected a student in front of a patient and family. I had to report him to the administration and he was reprimanded. Later, we came to an understanding and actually became friends. But, I had to demonstrate to these young students that we were into a new era of nursing and rudeness and disrespect would not be tolerated.
What do you see as your greatest accomplishments during your time at JMU?

Buildings and grounds crews use a crane to remove nursing equipment from the third floor of Willson Hall.
I guess I’ve always been a renaissance woman. Clinical expertise has always been at my roots. I spent four years in the Navy and practiced trauma nursing/ICU in four different countries. At JMU, I was able to be tenured without a PhD. I opted to stay clinically focused with a Family Nurse Practitioner (FNP) degree from the University of Virginia and an International Nursing Certificate from George Mason University. I’ve won numerous teaching awards and developed innovative nursing curriculum. My teaching was always informed by my “boots on the ground” clinical experiences for 16 years. I took care of Roy Rogers out in California after he had a heart attack.
I’ve always taken advantage of opportunities in faculty development and I learned to love transcultural and holistic nursing through the lens of working with interdisciplinary colleagues. I’ve done a lot of really fun stuff! I worked with the HIV/AIDS network that started in Harrisonburg in the 1980s and then did some HIV/AIDS research in Hong Kong during a sabbatical in the spring of 1994. Staying active in the holistic community prompted opportunities for more holistic nursing research with massage/ acupuncture and therapeutic touch and I brought these methodologies into the fundamentals lab.
Most importantly, my accomplishments have been the legacy of my students. I’ve taught over 1500 students over my 20 years in teaching. This is a small-town legacy of those students and the gifts they brought to healthcare all over the local community, states and internationally. Many of those students have now returned to faculty positions.
I practice the yin/yang balance with holistic body techniques and conventional medicine. I brought students along with me in this journey. I always challenge students to acquire the balance. Technology came along and I would still encourage touch, being present, going into the room to talk to the patient before looking at the equipment, labs, or numbers.

President Rose presents Holt with Distinguished Faculty Award in 1997.

Student nurse Karen Williams practices using a syringe.










