
15 minute read
BULLETIN Summer Été 2020
The official publication of the Canadian Orthopaedic Association Publication officielle de l’Association Canadienne d’Orthopédie
# 127
Advertisement
Publication Mail Envoi Poste-publication Convention #40026541
4060 Ste-Catherine W., Suite 620 Westmount, QC H3Z 2Z3 www.coa-aco.org
COVID-19 PANDEMIC: IMPACT ON ORTHOPAEDIC SURGERY p. 45


PANDÉMIE DE COVID-19 INCIDENCE SUR LA CHIRURGIE ORTHOPÉDIQUE p. 45
Farewell – A Message from Past CEO, Doug Thomson ...................................... 8
Félicitations aux deux gagnants de notre concours de renouvellement d’adhésion à l’ACO – c’est NOUS qui payons pour 2021! ................................... 15
Management of Proximal Humerus Fractures Debate.................................... 27
Congratulations to Our Two COA Membership Giveaway
Contest Winners – 2021 is on US!
Lexie Bilhete COA Coordinator, Membership Services & Affiliate Programs
On behalf of the COA leadership, thank you to all our members in Canada, the U.S., and abroad, for your commitment to the Association. By being a COA member, you are also contributing to national and local initiatives that Dr. Marie-Eve LeBel “Being a member of the COA has allowed me to keep connected to friends, trainees (current and former) and colleagues across our wonderful country. The COA is a very open-minded, inclusive and supportive association to all of us and I have truly enjoyed participating to different activities and meetings under their umbrella.” Dr. Marie-Eve LeBel is an Associate Professor in the Department of Surgery, Division of Orthopaedic Surgery at the Schulich School of Medicine & Dentistry at Western University, ON, since 2006. She grew up in Québec City and, following studies in physiotherapy, completed both an M.D. degree and residency in orthopaedic surgery at Laval University (QC). She then went on to pursue subspecialty training in sport medicine at the Fowler-Kennedy Sport Medicine Clinic (Western University, ON) in 2005. Dr. LeBel then worked in a community hospital in Cowansville, in Québec’s Eastern Townships for one year before being recruited to go back to an academic practice at the well-known Fowler-Kennedy Sport Medicine Clinic. In September 2012, she was recruited to join the renowned Roth|McFarlane Hand and Upper Limb Centre, specializing in the arthroscopic treatment of athletic injuries and soft tissue disorders of the shoulder. She also completed a Masters Degree in Health Professions Education at the University of Illinois at Chicago in 2014 with a special interest in simulation-based research in surgery and motor skills learning. Dr. LeBel received many research grants for the development of simulators for shoulder and knee surgery and for her work in surgical simulation research. She had the opportunity to present her research in Europe, North America and South America. “Through my COA membership, I was awarded the CFBS (CanadaFrance-Belgium-Switzerland) travelling fellowship. Myself and my co-travelling fellow were the first female Canadian CFBS fellows. I am very thankful for the COA to have allowed me to live these amazing moments and incredible experience.” support our collective community of orthopaedic surgeons, researchers, and trainees right here in Canada. Every COA member who settled their 2020 dues between February 4 – March 4 were automatically entered to win free 2021 COA membership and a randomized draw occurred in April.
Congratulations to Drs. Marie-Eve LeBel and Brad Ashman!
Dr. Brad Ashman “My COA membership has been a fantastic resource for me from medical school through to my clinical practice, enabling me to advance my knowledge and skill set, present research, network with colleagues, and stay in touch with close

friends.” Dr. Ashman graduated from the orthopaedic surgery residency program at the University of British Columbia in 2016 where he also completed his undergraduate degree and medical school training. He then moved on to a fellowship in sport medicine at the Cincinnati SportsMedicine and Orthopaedic Centre in Cincinnati, Ohio, training with a group led by Dr. Frank Noyes. After fellowship, he worked as a locum throughout BC until being offered a full-time position in Prince George, BC, in 2018. Dr. Ashman currently works alongside a group of nine orthopaedic surgeons servicing much of northern British Columbia. He also conducts outreach clinics and surgery in nearby northern communities as well.

Despite a subspecialty interest in arthroscopic and open joint preservation of the shoulder and knee, he continues to provide comprehensive orthopaedic care for patients as a general orthopaedic surgeon. “I enjoy my role as a clinical instructor for the Faculty of Medicine in the UBC Department of Orthopaedics, teaching medical students, family practice residents, and senior orthopaedic surgery residents.”
On behalf of the COA Leadership, thank you to all of our members for your ongoing participation and involvement!
(continued from page 22)
Member at Large – Executive Committee: Dr. Pascale Thibaudeau
Dr. Pascale Thibaudeau is a hip and knee reconstruction surgeon practicing in Montréal, Québec. After finishing residency at McGill University in 2012, she pursued a fellowship in adult reconstruction at the Queen Elizabeth II Health Sciences Centre in Halifax, NS. She then completed a second fellowship in knee reconstruction at the Ottawa Hospital, after which she returned to Montréal and joined her current practice at the Lakeshore General Hospital.
Dr. Thibaudeau currently serves on the Continuing Professional Development Committee of the Québec Orthopaedic Association. She is an examiner for the Royal College of Physicians and Surgeons. She had also been serving on the Standards Committee of the COA for the past three years prior to accepting her new nomination as Member-at-Large for the Executive Committee.
Memberships Committee Chair, Dr. Chad Coles
Dr. Chad Coles is an adult orthopaedic trauma surgeon practicing in Halifax, Nova Scotia. After completing residency in orthopaedic surgery at Dalhousie in 2002, he pursued an Advanced Clinical Experience in orthopaedic traumatology at Harborview Medical Centre in Seattle, Washington. He remained on staff at Harborview for an additional year, before returning to Halifax in 2004. Dr. Coles is an Associate Professor at Dalhousie University. He plays an active role in surgical education, including medical students, residents, fellows, and practicing surgeons. He has received clinical teaching awards at both the undergraduate and post-graduate level. He serves as an examiner for the Royal College of Physicians and Surgeons. Dr. Coles has a full-time academic practice in orthopaedic trauma at the Queen Elizabeth II Health Sciences Centre, which includes participation in several international, multi-centered research projects. He is on the Board of Directors of the Orthopaedic Trauma Association, serves on the Editorial Board of the Journal of Orthopaedic Trauma, and is a reviewer for Injury, and the Canadian Journal of Surgery. He has served on several COA committees, most recently on the Membership Committee, which he is now Chair.
Standards Committee Chair: Dr. Tim Daniels
Dr. Tim Daniels is Professor at University of Toronto, Head of its foot and ankle program and Chief of Orthopaedic Surgery at St. Michael’s Hospital. He manages a quaternary referral practice with an emphasis on hindfoot deformity and ankle arthritis. He serves as Associate Editor and Reviewer at prestigious journals. Other notables include Co-founder/Coordinator of the Biennial COFAS Symposia (1993 to present), Co-Founder/Past President, COFAS (2002-04), Canada’s Representative at IFFAS (2004-07), Research Chair AOFAS (2010-13), Chair/PI COFAS Ankle Arthritis Study Group (2011 to present), Member-at-Large on the AOFAS Board of Directors (2013), and Term-Chair F&A Research (2012-17 and 2020-25). He’s the recipient of the U of T Orthopaedic Chair’s Teaching Award and Jameel Ali Continuing Education Award, COA Award of Merit, the Takakura Award (2005, 2014 – for best clinical paper at IFFAS’ Triennial meetings), the Roger Mann Award (2008, 2012, 2014, 2015, 2017 – for best clinical paper at AOFAS Annual Meetings), and the COA Service to Specialty
Enrichment Award.
Practice Management Committee Chair: Dr. Mohit Bhandari
Dr. Mohit Bhandari is the Practice Management Committee Chair during his terms as President and Past President. This committee’s membership includes leadership from all of the provincial orthopaedic societies, and is prime opportunity for the COA President to engage and strategize directly with our provincial partners.
Communications Committee Chair: Dr. John Antoniou
Dr. John Antoniou is the Communications Committee Chair. Leadership of this committee by a recent Past President fosters continuity of the COA’s advocacy initiatives through our communications strategies. Dr. Antoniou served on this committee in the past both Scientific Editor and Editor in Chief of the COA Bulletin, and was President of the Association from 2018-2019.
(continued from page 34)
fixation at the end of the procedure (Figure 5.). He was placed in a custom made HKAFO orthotic instead.
The patient was strictly nonweight-bearing initially and was allowed partial weight-bearing at four months with a CT scan showing complete healing of the proximal femur and a bone scan confirming a viable femoral epiphysis. He was allowed to transition to full weight-bearing at seven months postop. Plains films showed limited avascular necrosis and femoral head collapse.

Figure 5

Unfortunately, he developed hip adduction contracture and subluxation (Figure 6.). This was then addressed with adductor tenotomy, hip arthrogram and hardware removal. Examination under fluoroscopy reveals a reducible femoral head Figure 6 with abduction (Figures 7 and 8). Therefore, the next step will require a varus derotation osteotomy (VDRO) with acetabular osteotomy to increase coverage of the femoral head. dures; however, non-negligible rates of residual symptoms, poor joint perception, and complications remain. Unsatisfactory clinical outcomes are primarily the consequence of poor, unnatural prosthetic joint biomechanics that arise from the more or less adequate execution of a suboptimal, nonphysiological surgical technique. Interestingly, recent advances in both material and design of prosthetic components, as well as precise technologically-assisted implantation, have not been game-changers. This may be due to the fact that gold
Figures 7 & 8


Meanwhile, the patient is ambulating without aids, pain-free, with a mild Trendelenburg gait and a 18mm leg length discrepancy.
Take Home Message
• Valgus-type SCFE are a completely different entity than a regular SCFE. • For SCFE in patients with bone dysplasia, obtaining CT scan is mandatory to better understand the anatomy and the displacement of the femoral epiphysis. • The risk of instability after open reduction and femoral
Personalized Joint Replacement: The End of ‘One Size Fits All’
Pascal-André Vendittoli, M.D., MSc, FRCS Hôpital Maisonneuve-Rosemont, Université de Montréal, Department of Surgery Montréal, QC
Charles Rivière, M.D., PhD 2 The MSK Lab-Imperial College London, South West London Elective Orthopaedic Centre United Kingdom


Hip and knee replacements are very successful proceshortening for SCFE should always be considered. standard techniques for implanting hip and knee components aim to implant all patients similarly (i.e. one size fits all), thus neglecting the unique joint anatomy and kinematics of each individual. Systematic techniques for joint replacement, such as the Lewinneck safe zone for THA acetabular orientation, or mechanical alignment for TKA, were originally devised
The Effect of COVID-19 Closures on Orthopaedic Sport Medicine Patients: Insights from Banff Sport Medicine
Michaela Kopka, M.D., FRCSC Laurie Hiemstra, M.D., PhD, FRCSC Julie-Anne Fritz PhD Sarah Kerslake, MSc, PT Banff Sport Medicine Foundation Banff, AB
The coronavirus (COVID-19) outbreak was first described in Wuhan, Hubei, China in December 2019, and was declared a global pandemic by the World Health Organization on March 11, 2020. In response, the Government of Canada initiated a nationwide lockdown that resulted in the cancellation of restorative orthopaedic surgeries as well as supportive healthcare services such as physiotherapy.
The Banff Sport Medicine Foundation sought to assess the impacts of COVID-19 closures on patients via questionnaires targeting two patient populations at the Banff Sport Medicine clinic: 1) Patients who had their surgeries postponed (n=269), and 2) Patients who were up to three-months postoperative (n=476).
The surveys were designed as Quality Assurance assessments, predominately using a 7-point Likert Scale for the responses. The EQ-5D was also included as a measure of generic health status.
Completed surveys were submitted by 42.8% of the postponed surgery group and 41.6% of the acute postoperative group. Descriptive statistics were used to analyze the data.
How have COVID-19 closures affected patients waiting for orthopaedic surgery?
More than 90% of patients were between the ages of 18 to 64 years (94.8%). The most common three postponed surgical procedures were anterior cruciate ligament (ACL) reconstruction, shoulder stabilization and knee arthroscopy for meniscal injury.

Effects on physical & emo
tional health • 87.8% of patients were able to stay physically active Figure 1 Feelings expressed by patients that had their surgery postponed. • 68.7% indicated the delay in surgery negatively impacted their physical health • 75.7% of patients experienced pain because of their injury during the COVID-19 closures • 51.1% indicated their pain increased, while 41.5% of patients indicated that their pain stayed the same • 41.7% stated that their symptoms increased in severity • 85.5% of feelings expressed by patients about the postponement of their surgery were negative (Figure 1)
Negative feelings described: anxious, stressed, angry, concerned, frustrated, lost, annoyed, irritable, resigned, disappointed, useless, depressed, down.
Positive feelings described: empowered, positive, motivated, grateful, happy.
Effects on the ability of patients to return to work and other activities
• 62.6% of patients indicated that postponement of their surgery has, or will, negatively affect their ability to return to work (Figure 2) • 90.4% of patients indicated there are, or will be, negative effects on their ability to return to sport and leisure activities (Figure 3)
Quotes from patients that indicated their delayed surgery will negatively affect their return to work:
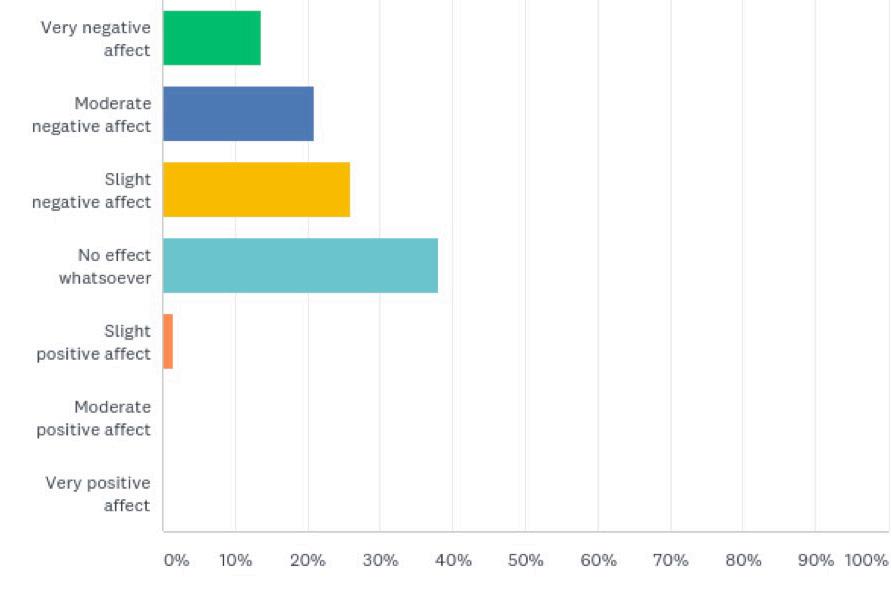
Figure 2
Survey Q. To what extent has the postponement of your surgery affected (or will affect) your ability to return to work? Please specify why in “Other”.
(continued from page 53)
Based on the EQ-5D, postoperative patients reported problems with performing their usual activities and experiencing symptoms of pain / discomfort (Table 2), while indicating their overall health state was good (Figure 9)
Table 2. EQ-5D-3L frequencies reported by dimension and level of problem reported by post-operative patients MOBILITY SELF-CARE USUAL ACTIVITIES PAIN / DISCOMFORT ANXIETY / DEPRESSION N (%) N (%) N (%) N (%) N (%)
No problems 142 (71.7) 182 (91.9) 87 (43.9) 45 (22.7) 129 (65.2)
Any problems Total
56 (28.3)
198 (100) 16 (8.1)
198 (100)
111 (56.1)
198 (100)
153 (77.3)
198 (100) 69 (34.8)
198 (100)
Figure 9
EQ-5D VAS Health State reported by postoperative patients.

Discussion
This is the first study in Canada to investigate the impact of COVID19-related health-care closures on orthopaedic sport medicine and arthroscopy patients. Patients whose restorative surgeries were postponed, as well as those in their early postoperative period (<3 months) were asked a series of questions pertaining to their physical and emotional health, barriers to recovery, and access to resources. The findings of this study revealed that, in both groups, the COVID19-related closures had an overall negative impact on physical and emotional health and resulted in significant barriers for accessing necessary care.
Patients whose surgical procedures were postponed due to COVID19 indicated that they experienced physical pain due to their injury, and nearly half (41.7%) stated that their symptoms increased as a result of the health-care closures. This finding is particularly concerning as sport medicine and arthroscopy patients are generally healthy and high-functioning individuals who form an integral part of the work force. The fact that these types of injuries result in significant physical dysfunction highlights the importance of timely and appropriate management of these patients. Another important finding was that 62.6% of postponed patients felt that delaying their surgery would have a negative effect on their ability to return to work. This underscores the impact of restorative surgeries on quality of life and the overall societal burden of disease. The majority (69.7%) of patients who were in their early postoperative period described a negative impact on their recovery as a result of the COVID19-related health-care closures. Inability to access hands-on physiotherapy was the most significant barrier reported. Despite efforts by physiotherapy clinics to offer virtual visits, only 41.4% of patients were able to access this service, and of these patients only 42.9% found them to be helpful. Postoperative rehabilitation is an essential component of a successful and timely recovery following restorative surgery. Without access to hands-on care, patients are at risk of complications including swelling, stiffness, and weakness. These complications can contribute to a prolonged recovery and, in some cases, to additional surgical interventions. Accordingly, limited access to physiotherapy (particularly during the critical, early stages of recovery) can contribute to poor outcomes and increased health-care costs 1 .
With respect to virtual orthopaedic care, this study demonstrated that although 67.8% of postoperative patients found it to be beneficial, the majority stated that it did not replace an in-person visit. This underscores the value of a hands-on assessment and in-person contact to answer patient questions and provide guidance on the course of recovery. In the setting of restorative orthopaedic surgery, virtual care may be viewed as an adjunct or alternative in select scenarios, but based on the information obtained in this survey, likely cannot replace in-person visits.
In summary, this study highlighted the significant impact of COVID19-related health-care closures on pre and postoperative sport medicine and arthroscopy orthopaedic surgery patients. The findings clearly demonstrated that restorative procedures play an important role in restoring physical and emotional health, as well as returning individuals to work and leisure activities. The study also revealed that virtual care does not adequately replace the hands-on assessments of allied care and orthopaedic specialists. As the health care system begins to reopen, it will be important to ensure that patients awaiting restorative procedures are triaged appropriately in order to reduce both the individual and societal burden of disease.
References
1. Jack K., McLean S.M., Moffett J.K., Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Manual therapy 2010;15:220-8.

