
FACULTY
AND STUDENTS
PUT PUBLIC HEALTH INTO PRACTICE


FACULTY
PUT PUBLIC HEALTH INTO PRACTICE
NICOLE BAYNE, MPH ’21, AND SUKHMANI KAUR, MPH ’24, ARE WORKING ON RESEARCH INVOLVING HOUSEHOLD CLEANING TECHNIQUES AND INDOOR AIR QUALITY.


The Applied Practice Experience (APEx) helps students gain an on-the-ground understanding of health systems and communities, allows them to explore the area of public health they are most passionate about, and provides an opportunity to apply what they have learned in the classroom to make an impact on public health at community, national, or global levels.
To ensure students of all backgrounds have the financial flexibility to pursue the APEx that is most meaningful to them, consider making a gift to Columbia Mailman today.
Make your gift today at publichealth.columbia.edu/give or contact Laura Sobel at ls3875@cumc.columbia.edu to discuss the power of leadership giving.
View the digital version at publichealth.columbia.edu/ CPHmagazine.
DEAN
Linda P. Fried, MD, MPH
ASSOCIATE DEAN AND CHIEF COMMUNICATIONS OFFICER
Vanita Gowda, MPA
EDITOR IN CHIEF
Dana Points
ART DIRECTOR
John Herr
EDITORIAL DIRECTOR
Tim Paul
COPY EDITOR
Emmalee C. Torisk
As part of our commitment to environmental stewardship, this issue is printed by The Standard Group on Rolland Enviro™ 100% recycled paper.
© 2024 Columbia University
CONNECT WITH US Alumni:
msphalum@cumc.columbia.edu publichealth.columbia.edu/alumni
SUPPORT US Development:
msphgive@cumc.columbia.edu publichealth.columbia.edu/give
WORK WITH US Career Services:
msphocs@cumc.columbia.edu publichealth.columbia.edu/careers
LEARN WITH US Admissions:
ph-admit@columbia.edu publichealth.columbia.edu/apply
2024–2025 EDITION



COLUMNS FEATURES
In her last year as dean, Linda P. Fried, MD, MPH, discusses public health past and future with alumna Perri Peltz, MPH ’84.
16 Community at the Center
In the heart of New York City, the School offers community research and training experiences unlike any other. By Dana Points
22
Faculty and students are working hard to communicate about public health in the most effective ways. By Christina Hernandez Sherwood
28
Lead, arsenic, and other metals are all around us, with important health effects. By Caroline Wilke
As the School’s Program on Forced Migration and Health has its 25th anniversary, the need for its leadership has never been greater. By Jim Morrison
36
With a new professorship and Child Health Center for Learning and Development, the School is doubling down on children’s health. By Paula Derrow

After 16 years as dean of the wonderful Columbia University Mailman School of Public Health, I plan to conclude my service in June 2025 and focus on my role as a faculty member and director of the Robert N. Butler Columbia Aging Center. It has been my privilege to lead this remarkable institution and to help advance our community’s shared mission to build a healthy and just world.
I feel honored to have played a role in our School’s trailblazing history. For more than a century, the School has educated public health leaders, conducted groundbreaking science, and developed innovative solutions to protect and improve population health. Today, Columbia Mailman School leads in taking on the most pressing global public health challenges, including health inequities, the climate crisis, environmental threats to health, emerging infectious diseases, violence, the need for healthy longevity, and much more.
Since its founding, our School has been deeply intertwined with and dedicated to population health in New York City and the greater region. Over the years, hundreds of our graduates have gone to work for our city’s agencies and initiatives; two School deans have also served as commissioner of health of the city; and our faculty, staff, and students have conducted research, served on commissions, implemented programs, and more, throughout the city. Our latest endeavor, the Community Health Equity Collaborative, profiled in our cover story (page 16), will further strengthen our partnerships and contributions in Northern Manhattan and across our beloved city.
Telling our School’s stories through this magazine is always a highlight of my year.
One of the magazine’s goals is to engage our amazing network of alumni, donors, and friends who create meaningful change around the world. Thank you for your continued support of our School. And to all of our alumni, faculty, staff, and students: I am grateful for the opportunity to have been a part of your professional journey and our School’s significant contributions to the public’s health.
Wishing you good health,

Dean Linda P. Fried, MD, MPH

EXPOSOMICS, WHICH ANALYZES DATA FROM ENVIRONMENTAL EXPOSURES— PHYSICAL, CHEMICAL, BIOLOGICAL, AND PSYCHOSOCIAL—WILL TRANSFORM PUBLIC HEALTH MUCH AS GENOMICS HAS REVOLUTIONIZED MEDICINE. And the new Columbia Mailman Center for Innovative Exposomics promises to be a major player in the space. “Our genes don’t provide a complete picture of disease risk. Health is also shaped by what we eat and do, our experiences, and where we live and work,” says the new Center’s director Gary Miller, PhD, vice dean for research strategy and innovation and professor of Environmental Health Sciences. The exposome is the compilation of these factors.
The Center’s team, drawn from across the Columbia University scientific community, is driving discovery and innovation through the development of new methods and workflows to measure complex exposures in blood and other biological samples. Miller and colleagues are leading an
arm of a global study using exposomics to examine determinants of cancer in people of African descent. Other investigators are studying cancer, liver disease, Alzheimer’s disease, and Parkinson’s disease. (Miller was also recently asked to lead the new NEXUS [Network for Exposomics in the U.S.] Coordinating Center at Columbia University, with more than $7 million in National Institutes of Health funding.)
The Center for Innovative Exposomics partners with the Biomarkers Core Laboratory of the Irving Institute for Clinical Translational Research, the Columbia Precision Medicine Initiative, and the Data Science Institute. With links to the European Human Exposome Network, France Exposome, and the Expanse Project, the Center promises to be an international intellectual hub, connecting academia, industry, and government, to share information about this rapidly evolving field.

Epidemiology
trailblazer
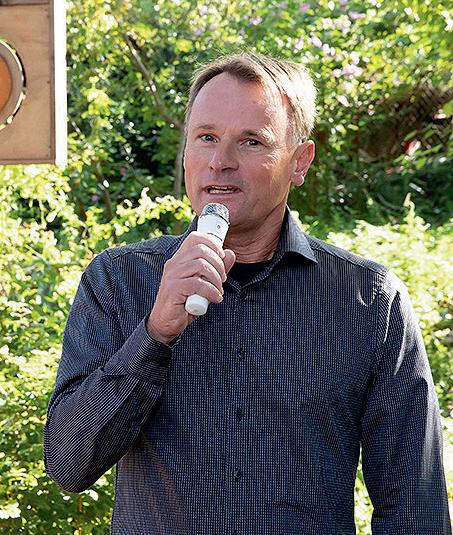
W. Ian Lipkin, MD, marks 40 years in research and 50 in medicine.
Lipkin’s 40th Anniversary
Leading scientists from around the world convened last spring to celebrate the extraordinary career and transformative scientific work of W. Ian Lipkin, MD, the John Snow Professor of Epidemiology and the founding director of the Center for Infection and Immunity (CII). The daylong symposium marked Lipkin’s 40th year in research. Panelists, most of whom have collaborated with Lipkin for decades, highlighted Lipkin’s significant accomplishments, including the fact that he spearheaded the development of the technology of pathogen discovery used worldwide, which he has used to identify more than 1,500 viruses and advance science on serious outbreaks including West Nile virus, SARS, Zika, MERS, and SARS-CoV-2.
Recognition for Public Service
Diana Hernández, PhD, associate professor of Sociomedical Sciences, and Parisa Tehranifar, DrPH ’04, associate professor of Epidemiology, were inducted into the Academy of Community and Public Service.
Medical Center Award to Smith Gilbert Smith, administrative director at CII, received the Columbia University Irving Medical Center Baton Award, recognizing team players who contribute to the medical center’s success.
Llanos at the White House
Adana A.M. Llanos, PhD, MPH, associate professor of Epidemiology, was an invited participant at the 2024 White House Minority Health Forum.
5 Faculty Among Top 1,000
Dean Linda P. Fried, MD, MPH, and four Columbia Mailman School colleagues are among the Best 1,000 Female Scientists in the World, as rated by Research.com. Elaine L. Larson, PhD, RN; Regina M. Santella, PhD; Frederica P. Perera, MPH ’76, DrPH ’82, PhD ’12; and Melanie Wall, PhD, all made the list.
Weissman Wins Award
Myrna Weissman, PhD, the Diane Goldman Kemper Family Professor of Epidemiology and Psychiatry, is the recipient of the Women in Medicine Legacy Foundation’s Alma Dea Morani Award, which recognizes a woman who has furthered the practice of medicine and made significant contributions outside medicine.
Fullilove and Rosner on PBS
Robert Fullilove, EdD, and David Rosner, PhD, MPH, professors of Sociomedical Sciences, were featured in The Invisible Shield, a PBS documentary examining public health’s role in improving lives.
THANKS IN GREAT PART TO THE FIELD OF PUBLIC HEALTH, LIFE EXPECTANCY HAS ROUGHLY DOUBLED SINCE 1900. By 2050, the number of people aged 80 or older is expected to triple. Society now faces the challenge of optimizing our longer lives by extending our “healthspan”—years of life lived free of disease and disability. Dean Linda P. Fried, MD, MPH, has long been a leading researcher and advocate for healthy aging; now she is leading CHAI, the Columbia University Irving Medical Center Healthy Aging Initiative, a medical center-wide steering committee defining a new vision for aging research at Columbia. This spring, its Healthspan Extension Summit brought together 300 researchers and guests from across the medical center and beyond to present findings in basic science, clinical medicine, and public health.
Allison E. Aiello, PhD ’03, of the Robert N. Butler Columbia Aging Center led a discussion examining the need to translate basic science insights from animal models to humans. The Columbia Aging Center’s Alan Cohen, PhD, said animal models are important but cautioned that mice with short lifespans are substantially different
from humans. CUIMC clinicians presented findings on disrupted sleep, which disproportionally affects older people. Representatives from neurology, nursing, pulmonology, and cardiology also shared findings. Columbia Mailman’s Thalia Porteny, PhD, spoke to the effect that social determinants of health have on aging, while Katherine Keyes, PhD ’06, MPH ’10, pointed to spikes in suicide and binge drinking among older adults.
Daniel Belsky, PhD—a co-lead on the symposium planning committee with Gregory Alexander, PhD, RN, of Nursing, and Caitlin Hawke, associate director of programming at the Columbia Aging Center—added that scientists need to both “translate up from the basic sciences, but also translate back down,” to make sure mechanisms identified in the lab are present in communities of people.
Katrina Armstrong, CEO of CUIMC, concluded the plenary by announcing that CHAI would immediately launch $240,000 in pilot funds to foster new collaborations. “I feel a sense of optimism coming from the people in this room, but also an incredible sense of urgency,” she said. “We need to get this work done.”
HEATHER KRASNA, PhD, EdM, ASSOCIATE DEAN OF CAREER SERVICES, TOOK A CLOSE LOOK AT SALARY DIFFERENCES BETWEEN PUBLIC- AND PRIVATE-SECTOR JOBS AND PUBLISHED RESULTS IN THE AMERICAN JOURNAL OF PUBLIC HEALTH Thirty of 44 occupations paid at least 5 percent less in government than the private sector, with 10 occupations paying 20 percent to 46.9 percent less. To develop a sustainable public health workforce, health departments must consider adjusting salary or using creative incentives such as student loan repayment for hard-to-fill roles.
A NEW INITIATIVE AT COLUMBIA MAILMAN SCHOOL WILL INVEST IN PUBLIC HEALTH SOLUTIONS FOR THE SURGING MENTAL HEALTH CRISIS—for example, examining how changes to the physical and social environment affect mental health. Called SPIRIT (Social Psychiatry: Innovation in Research, Implementation, and Training) and led by Katherine Keyes, PhD ’06, MPH ’10, the effort will explore the root causes of the rise of mental health problems, including social determinants of health. Fifty participating faculty come from across Columbia University Irving Medical Center and explore factors giving rise to mental illness, such as the emotional stress of climate change, social media and other new technologies, as well as what is driving poor outcomes in populations like Black and LGBTQ+ communities.
Other efforts will examine how brain development, stress response, and loneliness each play a role. Researchers will also examine possible solutions. These include school- and community-based prevention programs, economic and social policy, crisis support, and stigma reduction. SPIRIT also offers pilot funding and mentoring to scholars to further expand the research and keep the scholarship and collaboration going long term.
The Heilbrunn Department of Population and Family Health welcomes a new department head this fall. Thoai D. Ngo, PhD, MHS, is an internationally recognized scientist working at the intersections of global public health, population dynamics, gender equality, and sustainable development. He comes to the School from the Population Council, where as vice president for social and behavioral science research he led a global team of interdisciplinary scientists with expertise in climate science, demography, epidemiology, economics, public health, and sociology. Before that, Ngo was the vice president and senior director of research at Innovation for Poverty Action, directing a team of 500 research staff in conducting over 250 impact evaluations of programs and policies to address global poverty in 18 countries.
Ngo is also the founding director of the Girl Innovation, Research and Learning (GIRL) Center, a globally recognized hub for research on adolescents. He received a PhD in epidemiology and population health from the London School of Hygiene and Tropical Medicine and his Master of Health Science in global epidemiology and disease control from Johns Hopkins Bloomberg School of Public Health.


AS THE CLIMATE WARMS, SWATHS OF PERMAFROST ARE THAWING. ARCTIC PERMAFROST STRETCHES ACROSS Alaska, Scandinavia, Russia, Iceland, and Canada and is a reservoir of microbes, including bacteria, viruses, and fungi. With little known about these potentially infectious agents, the School’s Center for Infection and Immunity (CII) was invited to visit Fort Wainwright, Alaska, and the U.S. Army Corps of Engineers’ Permafrost Tunnel Research Facility. J. Kenneth Wickiser, PhD, the administrative director of the Global Alliance for Preventing Pandemics (GAPP) at CII, was one of a handful of civilians present as advisors in February when Army Corps of Engineers members extracted samples for research to detect pathogens in permafrost. “Melting of permafrost will trigger the release of pathogens not seen for thousands and thousands of years,” says Wickiser, an associate professor of Population and Family Health. “Most of our work out of CII and GAPP is in temperate or tropical climates. But we will be working in other climates, and these are the places likeliest to be subject to climate change. A significant number of people are living on top of or exposed to permafrost.”
Researchers inside the U.S. Army Corps of Engineers permafrost tunnel, which is held at around 25° F, prepare to take samples.
The Army Corps of Engineers will send ice core and permafrost samples to CII to assess for viral and bacterial pathogens, and CII will direct further sampling from areas where there is currently no melting but where permafrost is expected to melt in the future. “The goal is to get ahead of this,” says Wickiser, and tests invented at CII, VirCapSeq-VERT and BacCapSeq, will enable CII to do so. “The tools we have here are great in that they assess all pathogens simultaneously. So you don’t have to know exactly what you are looking for to find it.”
The same innovative tests are also helping CII interrogate wastewater at the U.S. Air Force Academy. Like permafrost, wastewater can contain a massive biological load, and looking for harmful pathogens can be like seeking a needle in a haystack. But CII’s tests enable the noninvasive detection of pathogens circulating in a community of hundreds of students housed in close quarters. “COVID-19, measles, mpox, adenovirus ... our technology finds everything all at once,” says Wickiser. With new uses for CII’s tests arising frequently, there is seemingly no end to the potential for these breakthrough technologies.

TWO STUDIES BY ROBBIE M. PARKS, PhD, ASSISTANT PROFESSOR OF ENVIRONMENTAL HEALTH SCIENCES, POINT TO HOW CLIMATE CHANGE MAY WORSEN HEALTH EFFECTS DUE TO HEAT EXPOSURE. Parks and fellow researchers found that temperature spikes due to climate change led to a marked increase in the number of hospital visits for alcohol-related disorders, including alcohol poisoning, alcohol-induced sleep disorders, and alcohol withdrawal in New York state. The higher the temperature, the more hospital visits. Higher temperatures also resulted in more hospital visits for disorders related to cannabis, cocaine, opioids, and sedatives, but only up to a
point—possibly because above a certain temperature people are less likely to go outside. The findings could inform policy on proactive assistance of alcoholand substance-vulnerable communities during periods of elevated temperatures, which stand to become increasingly common due to climate change.
In a separate study, Parks and fellow researchers also determined that an estimated 1.8 million incarcerated people in the United States—primarily in Florida and Texas—are exposed to a dangerous combination of heat and humidity, on average experiencing 100 days of such conditions each year. In recent decades, the number of
dangerous humid heat days in carceral facilities has increased, with those in the South experiencing the most rapid warming. (The Starr County Jail in Rio Grande City, Texas, averaged 126 days of dangerous humid heat per year.) Exposure can lead to heat stroke and kidney disease from chronic dehydration, among other health issues. “Dangerous heat impacting incarcerated people has been largely ignored, in part due to perceptions that their physical suffering is justified,” says Parks. “Laws mandating safe temperature ranges could mitigate the problem.” Forty-four states do not require air conditioning for inmates.
OpenAI’s GPT-4 can accurately interpret types of cells important for the analysis of single-cell RNA sequencing with high consistency equivalent to the performance of human experts doing time-consuming manual annotation, Biostatistics researchers reported in Nature Methods.
The researchers assessed GPT-4’s performance across 10 datasets covering five species and hundreds of tissue and cell types, including both normal and cancer samples. GPT-4 matched manual analyses in more than 75 percent of cell types in most studies and was notably faster.
“The process of manually annotating cell types for single cells can take weeks to months,” says study author Wenpin Hou, PhD, assistant professor of Biostatistics. “GPT-4 can transition the process from manual to a semior even fully automated procedure and be cost-efficient and seamless.” The researchers have developed GPTCelltype software to facilitate the automated annotation of cell types using GPT-4. While GPT-4 surpasses current methods, there are limitations. “But fine-tuning GPT-4 could further improve performance,” Hou says.
AMERICANS LIVING IN PUBLIC HOUSING SUPPORTED BY THE U.S. DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT (HUD) have significantly lower blood lead levels than comparable populations, likely due to tighter enforcement of residential lead paint laws in HUD buildings, reports a new Columbia Mailman School study.
HUD provides affordable housing assistance to nearly 5 million families. The new study is the first to examine blood lead levels (BLLs) by federal housing assistance status. People with HUD assistance had 11.4 percent lower blood lead levels than a comparable waitlist group. They also had 40 percent lower odds of having a risky BLL. No protective effect was seen for housing choice vouchers. (HUD enforces more stringent lead controls in public housing units versus voucher-eligible units.) The link between housing assistance and BLLs was weaker for non-Hispanic Black and Mexican American participants than for non-Hispanic Whites, possibly due to exposure to other lead sources, such as contaminated drinking water and pollution.
“Lead exposure is a major health risk at any level,” says senior author Ami Zota, ScD, associate professor of Environmental Health Sciences. Elevated BLLs in adults are linked with high blood pressure, cardiovascular disease, and kidney problems. Even low levels of exposure among children have been associated with neurocognitive impairment, poor school performance, behavioral problems, and criminality later in life. Approximately 3 million children currently live in public housing.
24% 35% 53%
INCREASE IN NUMBER OF FULL-TIME FACULTY SINCE 2014
PROPORTION OF FULL-TIME FACULTY WHO ARE PEOPLE OF COLOR, A HISTORIC HIGH
PERCENTAGE OF TENURED FACULTY WHO ARE WOMEN

Reducing Cancer Risk Residing in a more walkable neighborhood protects against obesity-related cancers in women, report researchers in Epidemiology. They studied 14,274 women for more than 20 years and found that those in neighborhoods with higher walkability levels, as measured by average destination accessibility and population density, had a lower risk of postmenopausal breast cancer. Moderate protective associations were also found for endometrial cancer, ovarian cancer, and multiple myeloma. 28% EIGHT 25
People with cognitively stimulating occupations between ages 30 and 70 had a lower risk of mild cognitive impairment (MCI) and dementia after age 70, finds a new study reported in Neurology The study is the first to connect cognitively stimulating occupations and reduced risk for MCI and dementia with objective assessments rather than subjective evaluations.
The researchers looked at occupations such as teacher, salesperson, nurse and caregiver, office cleaner, civil engineer, and mechanic. The group with low occupational cognitive demands had a 37 percent higher risk of dementia compared to the group with high occupational cognitive demands. “Our study highlights the importance of mentally challenging job tasks to maintain cognitive functioning,” says Vegard Skirbekk, PhD, former professor in the Heilbrunn Department of Population and Family Health and the Robert N. Butler Columbia Aging Center, who initiated the project. The next step will be to pinpoint the specific occupational cognitive demands that are most advantageous for healthy aging.
Researchers at Columbia Mailman School and the New York City Department of Health and Mental Hygiene have found that a stunning 30 percent of New York City residents experience energy insecurity, meaning they are unable to pay household energy bills, are in debt due to energy bills, have received a shutoff notice, or have shown other signs they are unable to meet their household energy needs due to cost. Residents with indicators of energy insecurity had higher odds of respiratory, mental health, and cardiovascular conditions and electric medical device dependence than residents with no indicators, the researchers reported in Health Affairs.
More than 1 in 4 New York City residents experienced indoor temperatures that were too cold (30 percent) or too hot (28 percent). Twenty-one percent had difficulty paying utility bills. Of those, a majority were in debt for energy costs. Three percent of residents experienced service shutoffs for heat, electricity, or gas. Black non-Latino and Latino residents, renters, recent immigrants, and households with children all experienced significantly higher levels of energy insecurity than their counterparts, notes study senior author Diana Hernández, PhD, associate professor of Sociomedical Sciences.

OLDER ADULTS WITH ATTENTION-DEFICIT/HYPERACTIVITY DISORDER (ADHD) HAVE A HIGHER CAR CRASH RISK THAN OTHER OLDER ADULTS, finds a study that tracked more than 2,800 drivers aged 65 to 79 with in-vehicle devices for more than three years. The researchers linked ADHD to a 74 percent increased risk of crashes, a 102 percent increased risk in self-reported traffic tickets, and a 7 percent increase in the risk of hard braking events.
About 8 percent of adults are known to have ADHD. “ADHD could affect driving safety in different ways,” says Guohua Li, MD, DrPH, professor of Epidemiology. Inattention might result in a driver failing to notice a vehicle coming from the side, while impulsive tendencies could lead to speeding or cause a driver to cut in when it might be safer not to do so. Enhanced screening, diagnosis, and clinical management of ADHD in older adults might help counter driving issues, as could limiting use of in-vehicle media, such as the ability to make phone calls while driving.
96% 66 24%
NUMBER OF COUNTRIES REPRESENTED IN STUDENT BODY
LIKELIHOOD A GRADUATE IS EMPLOYED OR CONTINUING THEIR EDUCATION WITHIN SIX MONTHS OF GRADUATION
PROPORTION OF STUDENTS WHO ARE UNDERREPRESENTED MINORITIES
report that the average liter of bottled water contains 240,000 detectable plastic fragments—a far greater number than previous estimates.
MAKING POLICE THE PRIMARY SOLUTION FOR INTIMATE PARTNER VIOLENCE (IPV) MAY HARM SURVIVORS, according to a new study that is the first to review the consequences of IPV policing in the U.S. IPV, which includes physical and sexual violence, psychological abuse, and other forms of coercion between current or former partners, impacts more than 40 percent of people in the U.S. The country has long maintained a police-centric response to IPV, despite growing calls for reform; there is mixed evidence that arrest reduces subsequent victimization and studies have documented an association between mandatory arrest laws and risk of survivor arrest.
The researchers analyzed scholarly articles about IPV published over 40 years. “More research is needed, but we know the current approach is ineffective and damaging,” says Seth Prins, PhD ’16, assistant professor of Epidemiology and Sociomedical Sciences. The study noted greater negative effects for Black survivors, as well as a lack of research into some consequences of IPV policing, such as police violence against survivors, reduced help-seeking, survivor arrest, or child protective services involvement.
There is a growing unmet need for treatment for cannabis use disorder (CUD), yet treatment has actually decreased since 2004, particularly in states with medical cannabis dispensaries. “We found that specialty treatment for cannabis use disorder remained very low and decreased in states with dispensary provisions, even among people reporting pastyear CUD, which is an indicator of treatment need,” says Pia Mauro, PhD, assistant professor of Epidemiology. CUD has negative health and social consequences yet there are no pharmacological treatments approved by the Food and Drug Administration. While cannabis use in the U.S. remains illegal at the federal level, 38 states and the District of Columbia have medical cannabis laws, and 24 states and the district have recreational cannabis laws. “Few people needing CUD treatment in our study perceived a need for treatment,” Mauro observes. In other studies, cannabis laws have been associated with lower cannabis-related perceived harms.
“We urgently need to target efforts in support of people with CUD, particularly in states with dispensaries. This includes training providers to increase screening and discussions about cannabis use,” says Mauro.
500+ 18% 419
PROPORTION OF STUDENTS WHO ARE FIRST-GENERATION COLLEGE GRADS
NUMBER OF CAREER COUNSELING APPOINTMENTS WITH ALUMNI COMPLETED BY THE OFFICE OF CAREER SERVICES LAST YEAR
NUMBER OF CLASSES OFFERED DURING THE 2023–2024 ACADEMIC YEAR
Dean Linda P. Fried, MD, MPH, has led Columbia Mailman School of Public Health to become one of the world’s top institutions for public health education and science. Through 16 years, thousands of students, and one global pandemic, her leadership has ensured that students go out into the world prepared to innovate and take charge to address society’s most persistent and urgent public health challenges. As she prepares to step down at the end of the 2024–2025 school year, Fried talks with alumna and Board of Advisors member Perri Peltz, MPH ’84, about what’s needed and what’s next for public health.

Thank you, Dean Linda Fried, for your visionary leadership. Take us back to when you started. How did you see this school then?
The school that I had the privilege to join 16 years ago had amazing people and was ready to rise to a whole new level. There was deep commitment to the public and the public good, and enough expertise to cover the leading edge of so many issues. My role has been in part to better support people’s success, to ensure the School has the institutional goals and capabilities and the bench staff to tackle the very complex issues that we were intent on tackling.
As somebody who had experience with the School back in 1984 when I was a master’s student and then when I returned as a doctoral student, I’ve seen the evolution. How did you take on the enormity of what you have been able to accomplish?
I was excited to come to an institution of such deep commitment and to lead in building the fabric of an institution that could support its mission: to bring scientific knowledge to the problems that threaten people’s health. And then to build the science, to understand how to keep people healthy. That commitment was there.
My approach to leadership is to help enable an institution to be great. It requires building the substance from the bottom up rather than the image from the top down, so that you can actually deliver on what the future needs.
When I met you, Linda, maybe 15 years ago. I remember thinking that you were looking at this school in a very big way. You spoke about systems. You used the word interdisciplinary. What were you thinking, and have you accomplished that?
It was clear to me that the challenges of the 21st Century are ones where no one discipline is sufficient to understand them or to solve them. The causes are complex and multifactorial. Let’s take really any health problem, whether it’s what causes a pandemic or what causes people to develop heart disease or stroke. Science has unveiled that there are many factors that have to come together in a perfect storm to end up with those outcomes, and you need multiple disciplines to understand the truth.
It’s never one thing that causes ill health, and it’s never one thing that creates health. You need to have multiple disciplines working together from different points of expertise to say, well, how do we solve this effectively? In 2008, it was clear to me that there was no academic institution that had yet taken those learnings about the necessity of interdisciplinary thinking and intentionally built the range of sciences needed to solve these challenges effectively. We had to figure that out. And we had to transform from very strong disciplinary expertise—not scuttle that, not throw it out, but expand capabilities—and unite disciplines to solve complex problems. My 16 years here has been dedicated to laying that foundation; to have successful interdisciplinary science be the norm. The great news is we have accomplished it.
When I walked out of that meeting, I thought to myself, doesn’t she know that academia doesn’t do this? Honestly, I didn’t think that there was a chance that you could accomplish what you were talking about. Of course, at the time, I didn’t know you. How is this school different now?
It looks very different. That’s not all due to me. It is due to our ability to come together as an institution and ask: What will the future demand of a great school of public health, a great science institution, an educational institution, committed to building a better future of health? We interrogated that together and came to a shared agreement that interdisciplinary science and knowledge had to be at the core. That has required many levels of change. Over a number of years, we went through formal processes to identify the issues that we should confront that are threatening our health and decide whether they required interdisciplinary solutions, scientifically and educationally.
Linda P. Fried, MD, MPH, becomes dean of the School. A national leader in the field of geriatric health and epidemiology, she is the first woman in the position.
The Biostatistics Epidemiology Summer Training Diversity Program (BEST) for students from underrepresented backgrounds begins. In subsequent years, it is joined by other “pathway” programs to bring historically marginalized groups into the public health field.
A strategic planning process identifies critical issues for public health in the 21st century.
Dean Fried is instrumental in launching Columbia University’s first global center in Europe.
Professors Quarraisha Abdool Karim, MS ’88, PhD, and Salim S. Abdool Karim, MS ’88, MD, PhD, publish a study in the journal Science finding that tenofovir gel is effective in preventing HIV transmission in women.
The School establishes the Climate and Health Program.
The revamped MPH Core Curriculum debuts, providing a rigorous program of interdisciplinary training in public health science and leadership. The Center for Injury Science and Prevention, a CDC-funded Injury Control Research Center, is founded.
Columbia Mailman School and the Columbia Journalism School take responsibility for leading Age Boom Academy, a summer boot camp for journalists on aging issues.
The University creates the Robert N. Butler Columbia Aging Center, an endowed, universitywide, interdisciplinary research and policy center housed within the School.
Sidney and Helaine Lerner establish the Lerner Center for Public Health Promotion and corresponding endowed professorship in public health promotion.
The Incarceration and Public Health Action Network is developed to examine mass incarceration through a public health lens and incorporate criminal justice reform into public health education.
The Master of Healthcare Administration (MHA), offered through the Department of Health Policy and Management, gives students intensive training in leadership and management along with a broad introduction to public health, health policy, and healthcare systems.

ICAP at Columbia begins providing technical assistance for the Population-based HIV Impact Assessment (PHIA) Project to capture the state of the epidemic in the most affected countries.
President Barack Obama cites the School’s research at a White House meeting to shine a light on the link between climate and health.
The first cohort of Tow Scholars is announced. Supported by the Tow Foundation, the program fosters research by mid-career faculty.
Researchers at the School’s Center for Infection and Immunity (CII) report that chronic fatigue syndrome is a physical illness, rather than a psychological disorder.
The Symposium on Preventing Childhood Obesity brings together researchers across disciplines.
An international roster of experts gathers in Shanghai to address aging in China and around the world at the Columbia-Fudan Global Summit on Aging and Health.
Fried receives the Inserm International Prize, a scientific award given each year by the French National Institute of Health and Medical Research, the French equivalent of the U.S. National Institutes of Health.

The Global Consortium on Climate and Health Education (GCCHE), a network of health professions schools and programs, launches.
The School partners with Barnard College to offer a 4+1 program that allows undergraduates to earn an MPH a year after they graduate with a BA. Similar programs follow with other schools.
David Rosner, PhD, MPH, and Gerald Markowitz, PhD, give testimony in a landmark case in which paint manufacturers are found responsible for lead contamination in California. Toxic Docs, a repository of documents related to toxic exposures, launches.
The Yusuf Hamied Fellowship Program, supported by the celebrated Indian scientist and pioneering business leader, catalyzes collaborations between researchers at Columbia Mailman School and their counterparts in India.
Experts from across the School pioneer testing techniques and therapies for COVID-19, conduct modeling to forecast spread, and offer technical assistance worldwide. Faculty and students support community awareness and vaccine programs.
Students, faculty, and staff create the FORWARD (Fighting Oppression, Racism and White Supremacy through Action, Research and Discourse) initiative, one in a series of efforts to promote inclusive and equitable education in the field of public health..
Here’s a key example. In 2008, climate change and its effects on health rose in our analysis to one of the top issues that will threaten health in this century. We know that climate change is causing extremes of heat, changes in hurricanes, flooding, drought, a whole set of natural disasters, wildfires. It’s causing food insecurity and water insecurity. And all of those are threatening human health and threatening human survival and creating, in many parts of the world, refugees. And I didn’t even mention the rise in infectious diseases in areas that never saw them before, like malaria, because of a warming climate. There is no one discipline that can address all those consequences. All of these require teams of people handling these different problems.
Working together as teams, we went on to build the governance to support interdisciplinary work. Will faculty be promoted for interdisciplinary work? Will they have interdisciplinary centers to work in that will bring these teams together? We’ve built the governance to support success in interdisciplinary science. We have recruited 130 new faculty in my time as dean, in large part to bring the expertise to tackle the issues of our collective future.
In your letter to the School community sharing that you would be concluding your service as dean, you write, “We have accomplished so much together, but our ambitious community knows there is more to be done.” What is on the horizon?
Public health was responsible for adding 25 of our increased 30 years of life expectancy over the last century. Now, public health needs to take the lead in ensuring those additional years are healthy. There is an opportunity for the United States to invest in a new vision of public health focused on healthy longevity for everyone. There are many dimensions where public health needs to rise and to redefine the role of the public health system, so as to deliver conditions that enable people in every community in this country to be healthy. And there are many other challenges. Why are cancers rising in young people? How do we eliminate the number four cause of death around the world, which is air pollution? Health is a human right. Public health has shown that prevention works. And it is public health’s responsibility to deliver the vast majority of health to the public.
Is there anything else that keeps you up at night in terms of public health?
The threat of loneliness is a huge threat. It is a consequence of many forces which are new to human beings, like social media, disinformation and misinformation, the pandemic exacerbating disconnection from other human beings. Young people and old people, especially, feel isolated and lonely. And then on top of that, loneliness is shredding our ability to come together to solve issues that we can only solve together. If we want to solve loneliness, by definition, we need to do it together.
Drug addiction and substance use are other issues where we need collective action, both to care for people who are addicted, but also to tackle the factors that are driving people to addiction. No one approach can solve this alone.
As you are talking about things that have kept you up at night, I recall that at some of the deepest, darkest moments—the COVID-19 pandemic being one—you have seemed calm. You said to me at the time that this had to do with your deep faith in the School and your love of the School. What is it that you love about it?
I love walking in the door every morning. I am surrounded by people who are committed to creating knowledge as a basis for a better world and empowering all sectors of society to accomplish that. It’s inspiring to be surrounded by people who are committed to the public good; who are spending their lives dedicated to improving well-being and elevating human society. How can that not be inspiring?
When I talk to people on your staff about what makes you such an incredible leader, it’s not related to public health specifically; it’s leadership skills. You have been a student of leadership. What have you learned?
MY COLLEAGUES AND I HAVE BEEN ABOUT CHANGE FOR THE GOOD SINCE I’VE BEEN AT THE SCHOOL, AND WE HAVE ACCOMPLISHED TRANSFORMATION TOGETHER.
I was persuaded to study leadership out of necessity many years ago. I observed that principled and effective leadership matters. I was confronted by the need to see if there was a skill set I could learn because I’m a physician, I’m a scientist, but neither of those calling cards come with training in leadership skills.
What I’ve learned over the years is that there is a whole set of skills that can be applied at any stage of leadership, and that some of what you need to do is to create a vision of what the future demands—that is aspirational, and that, hopefully, will unite people and inspire them to work together. And then it’s your responsibility as a leader to make that aspiration clear and to make it achievable and to make every person feel they can be part of it, and they won’t fall off the boat that’s going there.
What is next for Dean Linda Fried?
Well, I understand I’ve earned a sabbatical, which I will take. But I’m excited to come back to the faculty and continue to lead the Robert N. Butler Columbia Aging Center, a university-wide center dedicated to the idea that we can create a third demographic dividend, where societies and people flourish because of longevity, not despite it.
What wonderful news that you will be returning. Linda, as we conclude is there one message that you would like to share with the Columbia community?
I’ll give you two. One is that change is more than possible. People say that longstanding institutions cannot change. And particularly that universities don’t change. I very proudly can say that my colleagues and I have been about change for the good since I’ve been at the School, and we have accomplished transformation together.
The other message is something I am obsessed with, which is that public health is an exemplar of public goods. For capitalism to survive there are essential components that we must make sure are strong because everyone gains from them and no one profits from them. Public health requires collective investment to prevent disease, disability, and injury—which accounts for seventy percent of our overall health. And when we make adequate investment in public health at the science level, at the practice and policy level, all people have the opportunity to flourish and all sectors of society do better.
We’re going to end with a Linda Fried Fun Fact. I have learned that you have a black belt in Aikido. Has that training informed the way in which you work?
I trained in Aikido for many years; it’s deeply part of who I am. Aikido is a nonviolent Japanese self-defense art in which you learn that you don’t have to be big and muscular to lead. You can lead change, if attacked, by joining with the attacker and redirecting aggression toward a shared end while protecting the attacker from getting hurt. It’s possible to do that in almost any situation, to turn situations of conflict to better ends and mutual benefit. And that is the foundation of how I think about leadership.
The School hosts the inaugural Data Science for Public Health Summit, convening public health leaders to consider the many dimensions of data science in public health.
Faculty, with researchers across the University, launch the Columbia Scientific Union for the Reduction of Gun Violence (SURGE).
A team led by Dean Fried synthesizes evidence on the aging-related pathophysiology underpinning the clinical presentation of frailty. The findings appear in the inaugural issue of the journal Nature Aging
CII launches the Global Alliance for Preventing Pandemics (GAPP) to establish sustainable infrastructure for infectious disease discovery, surveillance, diagnostics, and response through global capacity building.
As the School celebrates its centennial, Dean Fried leads a visioning exercise to chart a course for the coming decades.
Dean Fried co-chairs a commission that publishes the National Academy of Medicine Global Roadmap for Healthy Longevity.
Dean Fried receives the Insignia of the Chevalier of the Légion d’Honneur, France’s highest order of merit, recognizing her positive impact on France and on a global level.
The School announces the recipients of eight Dean’s Centennial Grand Challenges grants for interdisciplinary research projects that address some of the 21st century’s biggest public health challenges.

The Food Systems and Public Health certificate program launches to train students in the role that food plays in public health.
Columbia Mailman ranks third in the nation for NIH Prime Awards to schools of public health, with a gain of 61 percent since 2018.
The School co-organizes the inaugural Global First Ladies Academy, hosting eight first ladies from African nations and U.S. first lady Dr. Jill Biden.

The Columbia Mailman Center for Innovative Exposomics launches to bring sophisticated environmental analysis to open new avenues for prevention and treatments.
Professor Katherine Keyes, PhD ’06, MPH ’10, leads the newly created SPIRIT (Social Psychiatry: Innovation in Research, Implementation, and Training) initiative to catalyze collaboration to address the mental health crisis.


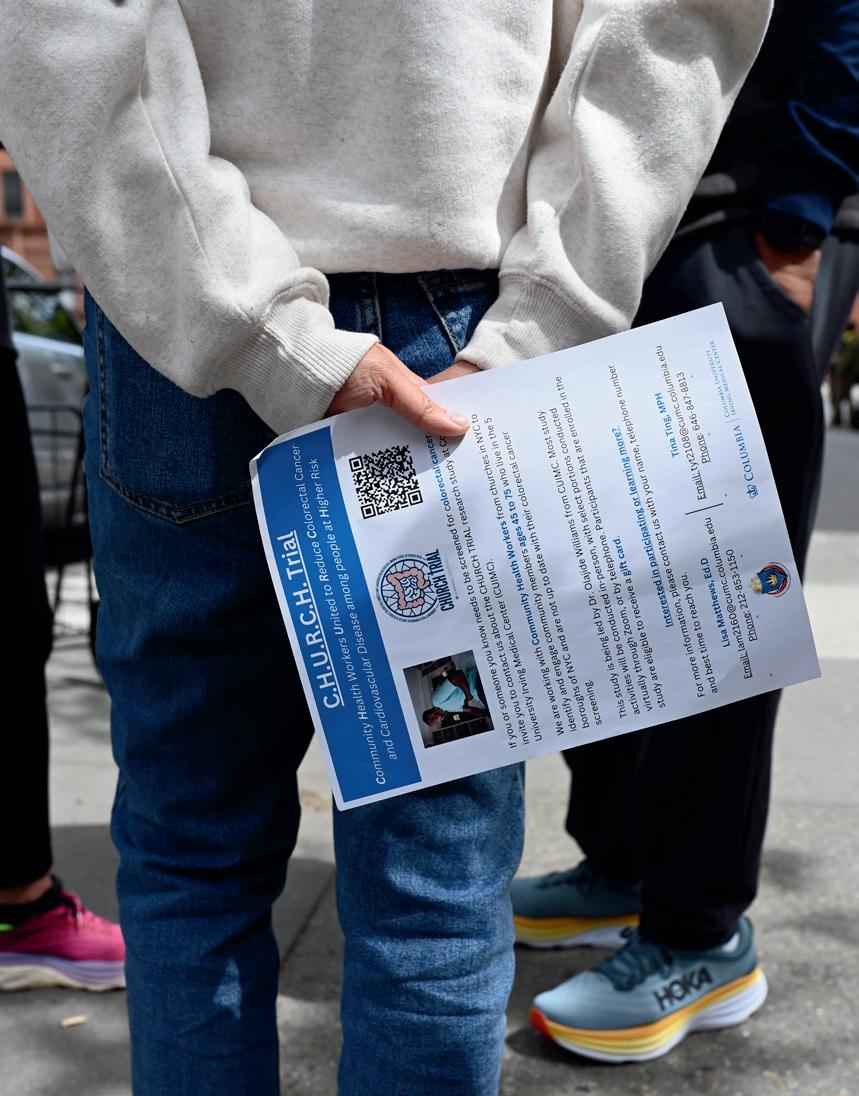
SCENES IN THE CITY From top left: Student Hersh Pareek, MPH ’25, doing outreach for the CHURCH study in Harlem; Bermarys Santos Pimentel examines her family’s air purifier in the Bronx; ICAP outreach assistant Ramiah Fennell; students Sarahy Martinez, MPH ’25, and Lilly Krupp, MPH ’25, at God’s Love We Deliver; Harlem community member Ilean Taylor and student Tobechi Dimkpa ’25, at Convent Avenue Baptist Church; South Bronx Unite is the School’s partner on air pollution research; the ICAP mobile van in the community; Nicole Bayne, MPH ’21, project manager, and Sukhmani Kaur, MPH ’24, research assistant, work on indoor air quality research; Convent Avenue Baptist Church Deaconess Marie Taylor, a CHURCH trial outreach volunteer; Markus Hilpert, PhD, leads air pollution research; a flyer for the CHURCH trial; Kaur and Bayne with Marileidy Pimentel at her home; Mychal Johnson, cofounder of South Bronx Unite; tobacco ads in Harlem have been a focus of research by Sociomedical Sciences Assistant Professor Daniel P. Giovenco, PhD, MPH








Faculty, staff, and students from Columbia Mailman School are working with New York City neighborhood residents to shed new
light on persistent public health challenges.
By Dana Points
COLUMBIA MAILMAN SCHOOL ALREADY HAD A CENTURY-LONG HISTORY OF DEVELOPING RESEARCH PARTNERSHIPS, facilitating student practica, and collaborating to improve public health in Northern Manhattan. Then COVID-19 hit. When the School’s leaders saw how longstanding health inequities fueled the pandemic’s devastating effect on the neighborhood, they knew they had to do more. And so, in 2021, under the guidance of Dean Linda P. Fried, MD, MPH, the School began to lay the groundwork for a Community Health Equity Collaborative (CHEC), launched in 2024, that would build new academic-community partnerships, accelerating efforts to decrease health inequities and improving the health of neighboring communities. Today, Columbia Mailman School is doing more than ever to reach out to those who live in the community and to its churches, nonprofit organizations, religious institutions, and advocacy groups.
In the field of public health, two or three decades ago, the norm was that experts communicated to the public when there was certainty. “That model said, ‘I don’t want to create stress about health risks, particularly environmental ones, until I know there is sufficient data,’” says Mary Beth Terry, PhD ’99, a professor of Epidemiology and Environmental Health Sciences


who has been at Columbia Mailman School for 25 years, first as a PhD student and then as a faculty member.
Today, community organizations are increasingly partners from the ground up. “Ideas are first discussed with community advisory boards to get their input on whether a project is worthwhile,” says Terry. “The ‘deficit’ model of communication has been replaced with a ‘dialogue’ model. The deficit model is linear. The dialog model is a circle: You still have scientists with disciplinary expertise, but you also have community members who have their own expertise, and policymakers. And we acknowledge that science evolves constantly so we have to communicate on an ongoing basis.”
You can see that circle in action in a collaborative effort underway between the School’s scientists and activists in

laboration that used monitors to document traffic related to the opening of a grocery warehouse. “We were able to highlight the environmental impacts of the new facility on the community,” says Markus Hilpert, PhD, associate professor of Environmental Health Sciences and one of the project’s leads. The findings were published in peer-reviewed journals and disseminated to community members through outreach events. The research has helped South Bronx Unite fight land use and transportation policies that would increase traffic in the community.
The researchers’ latest effort, funded through the New York State Department of Environmental Conservation, has more than tripled the number of sensors of the previous project, allowing for more detailed analyses as they measure, minute by minute, levels of particulate matter, carbon mon-


the South Bronx. The South Bronx experiences heavy truck traffic, and air pollution has had a devastating effect on the health of its residents, most of whom are low-income people of color. The area has one of the nation’s highest rates of asthma, with 1 in 4 children affected. The Mott Haven neighborhood is often referred to as “Asthma Alley.”
A research project organized by environmental justice group South Bronx Unite and environmental health scientists at Columbia Mailman School has installed 25 air pollution monitors in strategic locations throughout Mott Haven and nearby Port Morris, with a control monitor in the affluent, tree-filled western Bronx neighborhood of Riverdale, which has fewer industrial sources of particulate matter.
This research is driven by the community’s needs and designed to answer its questions. It is modeled on an earlier col-
oxide, ozone, and other substances. An anemometer, which measures wind speed, helps pinpoint air pollution sources.
Community-generated research ultimately cycles back to community organizations, which advocate for policy changes that foster health. Peer-reviewed research conducted with Columbia Mailman School scientists helped a coalition of advocacy groups co-led by South Bronx Unite to successfully lobby for New York state’s cumulative impacts law, which is designed to prevent the approval and reissuing of permits for actions that would increase inequitable pollution burdens on disadvantaged communities.
Terry is leading another air pollution research project in Washington Heights and the Bronx that is looking at indoor air quality. The team equipped families with HEPA air purifiers and measured inflammatory biomarkers for chronic disease.



They also provided the families with “green” cleaning products and an educational video about environmental and lifestyle risk factors and chronic disease risk reduction strategies. Families such as Marileidy Pimentel, Juan Santos, and their daughter Bermarys, who live in the Bronx, aren’t in the dark as study participants—they’ve been asked for their feedback as the project has unfolded. “Despite 30 years of research, chronic diseases were not reduced across all groups,” says Terry. “So our old model of communicating with communities didn’t work. Now this idea of having community involvement in lots of projects versus only special projects is becoming the norm. The National Cancer Institute now requires scientists to understand what is relevant to the community and how to have an ongoing dissemination of information related to the cancer burden there. And funders increasingly emphasize how the work being done reduces health disparities, versus only reducing disease risk.”
Connecting with the community includes forging partnerships with nonprofits that have deep roots in specific populations. Nour Makarem, PhD, assistant professor of Epidemiology, is leading a first-of-its-kind Food Is Medicine clinical trial in New York City in partnership with the nonprofit God’s Love We Deliver (GLWD). The trial began enrolling participants in August, with a focus on recruiting in Harlem and Washington Heights. A conversation between Makarem and Kelly V. Naranjo, MS, manager of research and evaluation at GLWD, was the impetus for the project and other nonprofits have since signed on.
The study’s goal is to help determine how to enhance the effectiveness of medically tailored meals (provided by GLWD) among people who have multiple risk factors for heart disease, such as Type 2 diabetes and high blood pressure. Among those with more severe disease, who qualify for medically tailored meals, the research is examining whether
supplementing meal delivery with a culturally relevant heart health curriculum will result in improved diet quality and better blood sugar and blood pressure metrics. “We have joined with Ryan Health, a community healthcare provider, and partnered with the nonprofit Harvest Home Farmer’s Market to implement community-centered nutrition education, including cooking demonstrations and fresh produce bags,” Makarem says. Among a second group of people who have less severe disease and don’t currently qualify for meals, the study is examining whether introducing the special meals earlier in the course of disease might forestall problems and, if so, what “dose” of meals is most impactful and cost effective. The American Heart Association is funding the research.
“A really big piece of community-engaged research is having your finger on the pulse of what is important to people, what works, and what doesn’t,” says Makarem. Students involved in the study are learning this firsthand. They began volunteering with GLWD in the weeks leading up to the study and engaging with the communities they would be recruiting from by screening for diabetes and high blood pressure at neighborhood health fairs. Now, they are recruiting patients and administering questionnaires to the 200 residents who will participate in the study, scheduling them for program appointments, and keeping them engaged for eight months.
Along the way, students get a firm understanding of community-engaged and community-led research, and the hurdles that researchers face. “The students are great at working with participants in different neighborhoods, from different backgrounds. They are learning how to implement contextual interventions and how we are in ongoing conversation with the community as the study progresses,” Makarem says.
The Food Is Medicine study is hardly the only current research that engages students with community members. The
CHURCH trial (CHURCH stands for Community Health workers United to Reduce Colorectal cancer and cardiovascular disease among people at Higher risk) focuses on colorectal cancer awareness in collaboration with Black churches in Harlem and the Bronx. It is a National Institutes of Health–funded research study based at Columbia University Irving Medical Center. CHURCH partners with community health workers from the churches to engage New York City residents aged 45 and older who are not up to date with colorectal cancer screening. It’s just one of the projects spearheaded by the Columbia Center for Community Health, which is co-led by Robert E. Fullilove, EdD, associate dean for community and minority affairs and professor of Clinical Sociomedical Sci-

MPH ’25—to recruit study participants. Kim has found community-based research to be a valuable learning opportunity. “Sometimes in an academic environment you fall into being told things.You learn about a health issue, but hardly do you experience or talk to people dealing directly with it. Being part of community-based research has been meaningful in that regard. I learn in class, but then I see something out in the community, and I can connect the two.”
Much of the current research was already under way when, as a natural outgrowth of its work on health equity and justice,


ences at Columbia Mailman School, and Olajide A. Williams, MD, MS ’04, professor of Neurology and vice dean of community health at the Columbia University Vagelos College of Physicians and Surgeons.
CHURCH draws many of its research assistants from Columbia Mailman School’s student population. “Working in the community is often interdisciplinary, cross-School, student-involved work, and it takes place in New York City— all things that make Columbia Mailman School a truly distinctive place to study,” notes Kathleen J. Sikkema, PhD, chair and Stephen Smith professor of Sociomedical Sciences. Valerie Kim, MPH ’25 (in center photo, above), joined as a research assistant earlier this year. She attends health fairs and church events, where she works alongside community members—and fellow students such as Tobechi Dimkpa, MPH ’25, and Hersh Pareek,
Columbia Mailman School announced that it was launching CHEC, housed in the Dean’s Office, with the goal of continuing and expanding innovative partnerships with Northern Manhattan communities to address complex underlying causes of health inequities and better improve health.
Faculty members Kelli Hall, PhD ’10, an associate professor of Population and Family Health, and Alwyn T. Cohall, MD, professor of Public Health and Pediatrics at Columbia University Irving Medical Center and Columbia Mailman School, led an extensive project to plan the new effort and identified more than 50 active community partnerships already run by departments, individual faculty members, administrative offices, and student groups. ICAP at Columbia was rolling through Harlem and the Bronx with a mobile clinic, evaluating whether using mobile health units to deliver

Air pollution is a focus of research and advocacy in the South Bronx.


integrated health services for people with opioid use disorder could improve HIV and substance use treatment and prevention. And for close to a decade, Daniel P. Giovenco, PhD, MPH, an assistant professor of Sociomedical Sciences, had been examining how minority communities are disproportionately targeted with ads for the deadliest tobacco products and looking at the link between tobacco use and neighborhood characteristics, such as tobacco retailer density, local tobacco control policies, and exposure to product advertising.
But while the breadth of the School’s partnerships was strong, “as meaningful as the School’s public health work has been to date, it has not been enough to fully offset the structural and societal issues that create disparities in the opportunity for health,” says Fried. “Addressing the underlying causes of health inequities in Upper Manhattan and the U.S. as a whole is a complex challenge that requires new solutions and partnerships between community, academic, and other organizations.” This School-wide centralization of CHEC within the Dean’s Office will ensure that collaboration with partners across departments and centers is coordinated to support outcomes.
CHEC is designed to be a true collaboration with the community, with neighborhood members receiving training on community-based participatory research (to enhance their capacity to collaborate with academic researchers) and community leaders helping the School’s faculty and staff to set goals and design service-learning projects for students that would foster learning in real-world settings. “This office is a lever we can use to dislodge health inequity and create conditions to foster health equity, while also creating a model of how academia can engage with the community respectfully,” says Ana Jimenez-Bautista, who was named executive director of CHEC in September and will fully assume her new role in 2025.
Successful public health interventions will likely require integration or consideration of many of the disciplines rep-
resented at Columbia University—from architecture to engineering to medicine. CHEC will provide the University with an umbrella for cross-discipline initiatives that can be guided by Columbia Mailman’s deep history and experience in New York City community engagement. The CHEC office will work with community members to jointly identify health priorities and the opportunities for successful intervention, with support of academic data science capabilities and implementation science. Three examples of interdisciplinary areas CHEC might focus on are trauma (which has a significant intergenerational impact on mental and physical health); support for formerly incarcerated individuals (including health support but also education, housing, and jobs); and neighborhood conditions such as pollution and food insecurity.
Jimenez-Bautista, who has worked in Northern Manhattan since 1989 and had roles at Columbia Mailman School for a decade, feels the time is right for the School to engage more deeply and cohesively with these long-standing challenges. “Thanks to Dr. Bob Fullilove and others like Dr. Williams, community-based participatory research has blossomed. We have talent and the interest from many of the faculty here in community-based research.” The School already has a 25-year history of partnership with WE ACT, the West Harlem environmental action coalition that has explored environmentally driven causes of poor health. But more can be done, and students are eager to participate. Says Jimenez-Bautista, “The students are coming in with more interest in prevention, in starting upstream of many of the health problems we are seeing, and engaging the common person in active participation. There are more robust student organizations at the School working on community engagement. I’ve seen a qualitative change since the pandemic—if you say, let’s talk about community, there are immediately ten students who raise their hand. That wasn’t always the case.”
Dana Points, the editor of this magazine, lives in Harlem.

A science storytelling class with Columbia Journalism School. A Health Policy and Management panel featuring the aide who spearheaded President Biden’s COVID-19 messaging. A contest to encourage creative communication strategies for public health professionals. These are just a few of the ways students and faculty are getting the word out about public health.
By Christina Hernandez Sherwood
Illustration by David Cooper
There is no denying it:
Today’s information landscape is punctuated by an increased mistrust of science, a partisan political climate, and a cacophony of social media voices. Public health experts must shout—strategically— in order to be heard.
This has led to expanded interest in a skill that Columbia Mailman School has long emphasized: public health communication—that is, the act of conveying public health information not only to peers, but also to society at large.
Public health professionals are realizing they need to change the way they think about this key skill. “Public health is largely invisible until there's a crisis. When the crisis recedes, the public health workforce fades into the background,” says Michael Sparer, JD, PhD, chair of Health Policy and Management. “We haven’t effectively communicated how public health makes life better for all of us, all of the time.”
Over the last year, faculty members have contributed to mainstream media outlets in growing numbers, publishing a host of articles and opinion pieces on a range of public health topics. The School’s public health professionals have long worked to effectively translate their research into practical lessons and health policy suggestions, Sparer says. But the onslaught of mis-
information surrounding the pandemic has amplified interest in communicating effectively. “More researchers are figuring out how to reach audiences that are not going to pick up the New England Journal of Medicine, but who might watch Fox News,” says Sparer. The School’s Communications office has seen a significant uptick in news articles and faculty op-eds published in top-tier mainstream outlets, notes Vanita Gowda, MPA, associate dean and chief communications officer. “Our School is a leading media source due in part to our educational focus on health communication. But our location in New York City—a media hub—and our faculty’s efforts to make public health knowledge and evidence as widely accessible as possible are also critical,” she says.
The interest in health communication also inspired a new class: When longtime friends Julie Herbstman, PhD, professor of Environmental Health Sciences and director of the Columbia Center for Children’s Environmental Health, and Duy Linh Tu, dean of academic affairs and professor of professional practice at Columbia Journalism School, shared a meal a few years ago, the conversation soon turned to work. While chatting about their respective challenges— Tu as a science journalist in a rapidly evolving field and Herbstman as a researcher trying to communicate her science without formal training in communication—they realized they could help each other. “There is a perception that scientists and journalists have an adversarial relationship,” Herbstman says. “It doesn’t need to be that way. We need each other, but we don’t work together very well.”
Spurred by (now former) Columbia University Provost Mary C. Boyce’s call for interdisciplinary course proposals, Herbstman and Tu, who met as undergraduates at Tufts University, began to develop a class that would, Herbstman says, “bridge the gap between scientific research and the distribution of important health information to the public.” The course, The Scientist and the Storyteller, demystifies public health research and journalism, emphasizing that the two can share the same goal: to bring science to the public.
During sessions in the Columbia Journalism School “World Room” where the Pulitzer Prizes are announced each spring, Herbstman and Tu helped a cohort of students (those studying public health and those with a journalism focus) to understand the differences, and similarities, in the two fields. “What is the role of an editor versus the role of a peer reviewer?” Herbstman says. “How is grant writing different from pitching in a journalistic setting?”
Herbstman, who explained the life cycle of a research study for the students in the class, says the biggest difference between the fields is the time frame in which they work. “Journalists call me and they need information by this afternoon,” Herbstman says. “But from an idea to a research paper can be five-plus
Over the last year, Columbia Mailman School faculty have taken on a remarkable range of topics and written for a wider audience than ever.
Read excerpts from their work.
years. How do you make that newsworthy today?”
“Losing your first tooth is a rite of passage for many children. But what if we never talked to them about this normal part of childhood? ... Imagine if, instead of rewarding children with a dollar bill, our silence and stigma led them to hide this experience out of embarrassment. ... This lack of knowledge, insufficient support, and feeling of shame are exactly what many people experience when it comes to periods.”
MARNI SOMMER, DrPH ’08, MSN, RN, professor of Sociomedical Sciences, and co-author Joanne Armstrong, MD, MPH, in Fortune

By the end of the course, each student had written a journalistic story about a scientific article, working with editors from Scientific American and Forbes to polish the pieces as if for publication. Herbstman says she hopes the course inspires future public health professionals to work with journalists to communicate their research. “Otherwise, the impact of our work is limited to the handful of people who are on PubMed,” a massive database of scientific literature.
Herbstman talked about the course as a member of a panel on bridging the gap between scientific information and public understanding held as part of the Health Policy
and Management Healthcare Conference last April, another sign of the School’s vigorous interest in this topic. Moderated by Robert Shepardson, senior lecturer in Health Policy and Management and co-founder of the advertising agency SS+K, the session also featured Kevin Munoz, assistant press secretary at the White House.
During the panel, Munoz emphasized how today’s “deeply fragmented media environment” called for meeting people where they are to communicate valuable health information. “You need to be in the tabloids. You need to be
“Graduates of for-profit institutions … are not achieving the same labor market outcomes as their counterparts from more traditional colleges and universities [even though] their institutions were held to the same academic accreditation standards. With this in mind, the next time your admissions or hiring committee excludes or scoffs at applicants with online degrees, think twice.”
ROXANNE RUSSELL, PhD, adjunct assistant professor of Health Policy and Management, in Inside Higher Ed

on TikTok, Instagram. All of these are going to play a role in how you communicate about public health issues,” he said.
For a long time, many public health professionals believed sharing their work meant talking about their scientific findings with graphs, data, and statistics, but without interpretation. “They would assume that public health information could speak for itself,” says Gina Wingood, ScD, MPH, the Sidney and Helaine Lerner Professor of Public Health Promotion in Sociomedical Sciences, director of the Lerner Center for
“If you were to go to buy a $1 chocolate bar but were told it would actually cost $6, you would probably complain about the $5 difference and refuse to pay it. But if you were buying an airline ticket priced at $250 that turned out to cost $255, you would be more likely to proceed. This illustrates the widespread and influential phenomenon of ‘mental accounting,’ which helps explain why individuals, institutions, and societies perceive the value of money as relative to its origin and purpose.”
KAI RUGGERI, PhD, professor of Health Policy and Management, in the Financial Times

“The
implications of climate change on HIV health outcomes have not historically been made obvious, but as an international development community, we are beginning to see the range of risk behaviors associated with climate change impacts, especially among women. We have a responsibility to establish programming that reflects what we know.”
ANDREA LOW, MD, PhD, adjunct assistant professor of Epidemiology in ICAP, in The Hill

Public Health Promotion, and director of the Health Communications Certificate. But if the COVID-19 pandemic left public health professionals with one lesson about communication, Wingood says, it’s that the public needs help interpreting scientific findings (not to mention parsing jargon).
An example of COVID-19 communication done right: the wildly successful Dear Pandemic, a social media campaign co-founded by Sandra Albrecht, PhD, assistant professor of Epidemiology, to combat misinformation about COVID-19. Albrecht was part of an interdisciplinary team of researchers and clinicians who took to Facebook, Twitter, and Instagram in the early days of the pandemic to deliver factual information in nonpartisan, accessible language for the public.
A winning formula for public health communications, Wingood says, includes using messages from trusted messengers that address social determinants of health, appeal to the reader’s emotions, and include visuals that tell the story— and reaching out across a diverse array of communication channels. For instance, she says, information for older adults could use compelling narratives directly from older adults. “There’s no monolithic audience who’s going to respond in the same way,” Wingood says. “Public health messages need to be framed for diverse audiences. Health literacy is another underestimated problem. Messages should use nontechnical language and aim to motivate a single action rather than a lifestyle change. Health literacy is a cornerstone of messages
On a sense of purpose
“Research shows that having more sense of purpose in life, and of control over one’s life and health (a so-called internal locus of control), are associated with better physical health, including less disease, pain, strokes, dementia, and Alzheimer’s. Yet, while many people find such purpose through reliance on faith and traditional religions … it can consist of social and political ideals as well.”

created by the Lerner Center’s founder, the late Sid Lerner, an advertising-industry legend.
Columbia Mailman School students practice designing compelling health messages by competing in the Lerner Center’s annual Health Messaging for Justice competition, which challenges students to create products that reduce stigma, enhance social justice, and counteract racism. This year’s submissions spanned communication products ranging from a documentary on transforming spaces for accessibility, to a “get to know you” card game for new sexual partners.
The student competitors, who came from across departments, were scored on messaging, creativity, design, and dissemination strategy, topics frequently covered in their coursework, Wingood says. The winning submission came from Jazmyne Bullock, Courtney George, Ugomma Korie, and
On racism in drug policy
“At face value, New York’s Good Samaritan law seems like an important step towards harm reduction; however, upon closer examination, it simply masks an ongoing mandate to criminalize drug users.”
JOHN PAMPLIN II, MPH ’14, PhD ’20, assistant professor of Epidemiology, on Thirteen.org

Megan Spinella (all ’25); their submission, Health, Happiness, and Life: A Guide for Expectant Black Mothers in NYC, is a free podcast that melds personal stories with expert interviews. The student winners “were excellent at integrating issues of health literacy and tailoring their podcast to the audience of African American women,” Wingood says.
Students can study health communications in single courses or through the Health Communication Certificate, where they learn about mobile health, email marketing, data visualization, and infographics, and how to tackle misinformation. Graduates of the program, which offers extensive exposure to health communications experts across New York City, have gone on to careers in city and national health departments, in the media, and at the Centers for Disease Control and Prevention, as well as at digital communication agencies, healthcare companies, and nonprofits.
Health communication courses include the long-running Writing for Publication in Health Policy and Management, which was recently taught by Maria Smilios, author of The Black Angels: The Untold Story of the Nurses Who Helped Cure Tuberculosis. Every full-time Health Policy and Management student takes a professional development course called PIVOT that helps them learn to communicate about their work through mock interviews and simulated conversations. “Everybody’s searching for different ways of communicating with different audiences,” says Sparer. “There’s much greater attention being paid now, among academics, to how to more effectively reach the consumers you want to reach.”
Christina Hernandez Sherwood specializes in journalistic storytelling. See more at christinahernandezsherwood.com. Additional reporting by Neha Kumar, MHA ’24.

Metals are at once essential and unavoidable in our environment. Now a growing body of research at Columbia Mailman School is uncovering their health risks— and exploring state-of-the-art antidotes for overload.
By Carolyn Wilke

Present in the Earth’s crust since our planet formed, metals are everywhere. They occur in soils and rocky ores. They circulate in the water we drink and the air we breathe. Our food—from vegetables to grains to fish—carries metals too. Our daily activities expose us to metals, in our surroundings and in commercial products. (A new study at the School even found metals in tampons.)
“These are really important environmental exposures,” says Ana Navas-Acien, MD, PhD, MPH, Leon Hess Chair and Professor of Environmental Health Sciences. And with its myriad biological interactions, the metallome— the array of metals in our bodies— is crucial to human health.
Many metals are essential for life, such as potassium, calcium, and magnesium. Others, including copper, zinc, and iron, are required in small amounts. As parts of proteins and enzymes, these metals enable the chemical reactions that keep us alive.
But the body’s relationships with some of these substances can sour if they are present at too high a concentration. Meanwhile, other metals and metalloids are toxic at even low levels. These elements—lead, cadmium, mercury, and arsenic—can wreak havoc on cells and tissues.
Human activities, such as mining or burning fossil fuels, can liberate metals, including toxic ones. As chemical lookalikes of essential metals, harmful metals can interfere with biological processes. For instance, lead mimics calcium while cadmium imitates zinc. “That’s one of the key ways in which they induce toxicity,” Navas-Acien says.
Metal exposures contribute to manifold health problems. Some metals can cause skin, bladder, or lung cancer. Others play a role in heart disease and diabetes. And some, like lead, are potent neurotoxins. Ten years ago, when lead poisoned the water supply for Flint, Michigan, David Rosner, PhD, MPH, the Ronald H. Lauterstein Professor of Sociomedical Sciences and professor of history, helped bring a spotlight to the situation, writing about the crisis and placing it in a long history of lead contamination from paint and gasoline.
Today, researchers at the School continue to push metals research forward with interdisciplinary work that weaves together strategies from chemical analysis to community partnerships. They are bringing to light exposures from everyday sources, such as water and cannabis. They are tracing the connections between metal exposures and health impacts on individuals and populations. And they’re exploring approaches that could remove metals from the body to improve health and treat disease.
MANY INSIGHTS INTO THE HEALTH EFFECTS OF METAL EXPOSURES HAVE FLOWED FROM LONG-TERM ONGOING PARTNERSHIPS BETWEEN RESEARCHERS AT THE SCHOOL AND INDIGENOUS COMMUNITIES. Tribal groups are often faced with elevated concentrations of metals in their drinking water and environment. Meanwhile, Indigenous people in the United States shoulder a greater burden of heart disease than the general population. Since the late 1980s, the Strong Heart Study has investigated heart disease, including its mortality and risk factors, by following thousands of tribal members across several states.
Through work with the Strong Heart Study beginning more than 15 years ago, Columbia Mailman School researchers have uncovered links between arsenic exposure and heart disease and between multiple metals and lung disease, as well as certain brain conditions and cancers. Scientists at the School have also unveiled how exposure pathways and the body’s metabolism contribute to disease risk, revealing that interventions—from public health to precision medicine—will need to consider environmental exposures, Navas-Acien says.
In its decades-long history, the Strong Heart Study has emphasized community ownership of data and community input into the research, as well as connections—through workshops and visits—between tribal groups and researchers. Columbia Mailman School researchers followed its model when they developed new projects such as the Strong Heart Water Study, which began in 2015. Working with tribal members, the collaboration investigated the efficacy of water filters in reduc-
ing arsenic exposures in a Northern Great Plains American Indian nation.
The project, which recently finished, saw a 47 percent decrease in arsenic levels in individuals’ urine after a two-year period with use of a mobile health program and a drinking water filter. But not all the lessons were scientific. Navas-Acien recalls wanting to work quickly to achieve water quality improvements. “I learned hard lessons that, as a scientist, you need to be very respectful of the timing, the process,” she says. “You need to listen.” Science has been slow to recognize the depth of knowledge that rural and Indigenous communities carry. With community feedback, the team altered their experimental approach—favoring a comparison between two groups that both installed water filters but received different types of instruction during the intervention rather than a typical scientific approach using a control group. The tribe had raised concerns about a control group potentially drinking more contaminated water during the study. Navas-Acien’s experience with these communities—their deep interest, grasp of scientific topics, and feedback—has underscored how much she and other researchers can learn from them. “It’s very humbling.”
New directions prompted by findings from the Strong Heart Study have seeded a partnership between researchers across schools at Columbia University and Missouri Breaks, a research organization focused on tribal communities. Beginning in 2022, the Columbia University Northern Plains Partnership for the Superfund Research Program has been searching for environmental health solutions to harmful metals in drinking water sources near abandoned uranium mines and Superfund sites. “There’s a huge team of us trying to understand how water consumption, specifically arsenic and uranium [in the water], leads to cardiometabolic diseases such as heart disease and diabetes,” says Tiffany Sanchez, PhD, assistant professor of Environmental Health Sciences. And with the possibility of new or renewed mining activity in the Northern Plains, some tribes have approached the researchers to measure metal levels in waterways and learn about potential increases in metals contamination.
BUT WATER IS FAR FROM THE ONLY WAY IN WHICH PEOPLE TAKE IN METALS, and researchers at the School have uncovered other metal exposures that have received less attention. In 2021, Sanchez was walking around New York City noticing how many new cannabis shops had cropped up and thinking about how someone needed to figure out what was in these products. After all, the cannabis plant is known to guzzle up metals that are present in water, soil, and chemical treatments as it grows. “I realized it should be me—I should be doing that research,” she says. Her realization kicked off work digging through publicly available data collected between 2005 and 2018 on thousands of people in the United States. Sanchez
Ana Navas-Acien, MD, PhD, MPH, who joined the School in 2016, has been named Leon Hess Professor and Chair of Environmental Health Sciences. Announcing the appointment, Dean Linda P. Fried, MD, MPH, said: “Ana has distinguished herself as an exemplary and internationally renowned scholar and educator, a champion of environmental justice, and a thoughtful colleague and caring mentor.”
Navas-Acien has published more than 350 peer-reviewed publications and leads multiple National Institutes of Health–funded projects and centers. In addition to the Strong Heart Study and the Columbia University Northern Plains Partnership for the Superfund Research Program, she is principal investigator of the VapeScan Study in collaboration with colleagues at the Vagelos College of Physicians and Surgeons and the Chronic Kidney Disease of uncertain origin (CKDu) CURE Consortium. She has served on numerous committees with the National Academies of Sciences, Engineering, and Medicine, and in 2023, was appointed by President Joseph Biden to the National Cancer Advisory Board. From 2013 through 2023, she was the founding editor in chief of Current Environmental Health Reports, now a top environmental health journal.
Navas-Acien is faculty director of the Program to Inspire and Mentor Undergraduates in Environmental Health Science Research (PrIMER) and received the 2019 Dean’s Excellence in Mentoring Award at Columbia Mailman. She is also a member of the Herbert Irving Comprehensive Cancer Center and an associate member of the Earth Institute. She co-chairs the Columbia Climate School postdoctoral program, helping to ensure a future of strong scholars taking on some of science’s most pressing issues.
and her team combined data on cannabis usage with measurements of the levels of five metals in blood and urine.
People who reported using marijuana had elevated levels of cadmium and lead in their blood and urine as compared with people who didn’t use the drug. “This is the first study of metals in marijuana users,” says Katlyn McGraw, PhD, a postdoc in Environmental Health Sciences who is the lead author on this work. As a federally illegal drug, cannabis was covered by a patchwork of different rules across different states. Such evidence points to a need for federal regulation and more stringent guidelines on contaminants in cannabis products, she says. Sanchez’s team now plans to look for links between metals in cannabis and risk factors for heart and lung disease.
WHEN CERTAIN METALS, SUCH AS LEAD AND CADMIUM, ENTER THE BODY, THEY CAN LODGE THEMSELVES IN THE BONE, WHERE THEY CAN LINGER FOR DECADES, DISPLACING CALCIUM. Columbia Mailman School researchers wondered if metals could be removed from the body to improve health. They’ve revived an idea that first gained traction in the 1950s—infusing metal-grabbing molecules into people to pry toxic metals from the body so that they can be excreted in urine.
The tactic, called chelation therapy, has shown that it could help some people who had had heart attacks to live longer, but the benefit was inconsistent across studies.
Analytical chemist Kathrin Schilling, PhD, Navas-Acien, and others won a 2023 Precision Medicine Pilot Grant from Columbia’s Irving Institute for Clinical and Translational Research to explore the approach. In one pilot study, 20 people above the age of 70 with diabetes received weekly infusions of ethylenediaminetetraacetic acid, or EDTA, over the course of a year. Based on patients’ blood and urine samples, the team saw that the molecule was successful at clawing metals out of the body. EDTA removes metals—harmful and essential alike—of a particular charge. So, the researchers gave a supplement to replenish needed metals, such as calcium.
Many of the study participants saw health improvements, Schilling says. Some of these patients had limb ischemia—a condition that hampers blood flow to the limbs, creating a risk of losing fingers, toes, or a limb—and were expecting to have an amputation. “Most of them didn’t have to go through with the amputation.” That suggests that EDTA can remove the calcium from plaques in the veins, restoring blood flow. Based on chemical signatures of the metals, the researchers can clue in to where in the body the EDTA treatments strip metals from. A second study investigated the potential for chelation therapy to remove metals from younger people. In ten volunteers aged 25 to 40 who received three infusions, the team studied the relationship between EDTA dose and the amount and types of metals removed. The study found that low doses were effective at removing lead. These findings can help clinicians tailor the dose of EDTA to remove lead while preserving other elements.
Metal-removing infusions to prevent disease may take time to reach the clinic. But in the meantime, reducing metals exposures can improve health. Columbia Mailman School researchers documented a decrease in blood lead levels of Indigenous people in Arizona, Oklahoma, North Dakota, and South Dakota over ten years. Over the decade, those same people showed decreases in systolic blood pressure. The improvement was similar to what could be achieved by taking blood pressure medication, starting an exercise regimen, or decreasing salt intake, says recent graduate Wil Lieberman-Cribbin, PhD ’24, who led the work while pursuing his PhD, working with Anne Nigra, PhD ’20, an assistant professor. “There’s a really immediate benefit of lowering the amount of metals in the environment or in the body.” Seeing those benefits is motivating to Columbia Mailman School researchers, who will continue uncovering the sources and health impacts of metals so that consumers and policymakers alike can take steps to reduce exposures to these ubiquitous contaminants.
Carolyn Wilke is a science writer and editor in Chicago. She covers chemistry, Earth science, and more for curious readers old and young in The New York Times, National Geographic, and more.


Columbia Mailman School has long worked to help communities faced with humanitarian crises. Today, with wars raging across the planet and millions of people displaced by economic upheaval and climate crisis, the School is rising to new challenges for global public health. By Jim Morrison
FOR CLAIRE GREENE, PhD, MPH, THE MEMORY OF THE GROUP OF VENEZUELAN PEOPLE THAT SHE MET IN A MIGRANT SHELTER IN COLOMBIA LAST SPRING LINGERED LONG AFTER SHE RETURNED TO COLUMBIA MAILMAN SCHOOL, where she is an assistant professor in the Heilbrunn Department of Population and Family Health. Eleven adults traveling with children had journeyed hundreds of miles from Venezuela to Peru, mostly on foot. They arrived with only a few bags of belongings. In Peru, one member fell ill but could not get care. So, like so many migrants today, they kept moving, backtracking to Colombia, which they had left a year earlier. They expected to gain access to emergency care there, because migrants had access to it, but they lacked legal status and getting it takes time and has barriers. “The devastation and the frustration,” Greene recalls. “They were making huge decisions about where their family was living, uprooting again only to find they were basically back where they started and not sure where to go next. It left me feeling really sad.”
Greene, who teaches in the School’s Program on Forced Migration and Health, has examined how to bring mental healthcare to those fleeing upheaval since 2010. Her work has been complicated in recent years by a change: Migrants today are constantly in transit—often for years—while awaiting asylum, which has heightened the effect on their mental health. An estimated 22 percent of people in conflict-affected communities have a mental health problem, triple the usual rate. “It’s a population that has unique risks for mental health problems, but is also underserved despite the fact that they’re in greater need of supports,” she says.
As the School’s Program on Forced Migration and Health celebrates its 25th anniversary, the challenges for those forced to flee are increasing in number and complexity. Migration has more than doubled since 1990. The climate crisis is driving migration as populations depart from places that are too hot, too dry, or too wet. Or conflict may cause migrants to move, and drought, flooding, cyclones, or heat exacerbate their plight. In Kenya and Bangladesh, where
The number of people displaced by persecution, conflict, violence, human rights violations, or events seriously disturbing public order almost doubled.
the government says 1 in 7 will be displaced, migrants are pushed into areas already endangered by climate change. “It’s a double whammy for populations that have been displaced primarily, in the first instance, by conflict, but are now being housed in places that are at the edge of climate insecurity,” says Monette Zard, former director of the Program on Forced Migration and Health and now a professor in the program. Researchers like Greene are stretching to find fresh solutions in hot spots like Central America, Eastern Europe, Africa, and the Middle East.
Conflicts, too, have multiplied. In 2024, there were 56 conflicts worldwide, the most since World War II, according to the Global Peace Index. In 2022 alone, the United Nations documented 3,931 verified instances of denial of humanitarian access to children living in conflict zones, with the highest figures verified in the Occupied Palestinian Territory, Yemen, Afghanistan, and Mali.
Providing health support to migrants was a driving mission when the Program on Forced Migration and Health was founded during a humanitarian crisis coming out of the Rwandan genocide. Three Columbia Mailman School leaders were pioneers in creating the field of humanitarian health: James McCarthy, PhD, then-director of the Heilbrunn Center for Population and Family Health; Allan Rosenfield, MD, then-dean of the School; and Ron Waldman, MD, MPH, the program’s founding director.
“At the time that the idea for this program was being developed in the late 1990s, the humanitarian sector, and particularly the health sector within it, had really neared its lowest point,” recalls Waldman. A civil war in Somalia created nearly half a million refugees in the 1990s. The violence in Rwanda in 1994 led to half a million people fleeing to camps in the Democratic Republic of Congo, where cholera killed 45,000 people in weeks. “It was the disaster following the disaster,” Waldman says. “The [need for] humanitarian intervention was as bad as it could get.”
One of the School’s first initiatives was to participate in an evaluation of the Sphere standards, an effort started
5.8 million in need of international protection
6 million Palestine refugees under UN Relief and Works Agency mandate
6.9 million asylum-seekers
31.6 million refugees under UNHCR’s mandate
68.3 million internally displaced people
SOURCE: UNHCR Global Trends 2023
in 1997 to craft and maintain minimum guidelines for humanitarian response. The standards spelled out the need to provide water, showers, communal places, sleeping areas, an infirmary, and dedicated space for counseling. In 2006, the School also pioneered the Reproductive Health Access, Information, and Services in Emergencies (RAISE) initiative at Columbia Mailman School. RAISE and its partners catalyzed changes in how sexual and reproductive health was addressed in humanitarian settings and were among the first to focus on improving access to contraception and abortion.
Sara Casey, DrPH ’16, now the director of RAISE, began working with the program as a student two decades ago. “When we started, family planning methods were not available in many of the places in which we worked, especially sub-Saharan Africa,” she says. “People had outdated training. They didn’t have supplies. Postabortion care, if a woman had an unsafe abortion, was very difficult to get.” Casey says the focus, now that larger organizations have programs in place, is to expand into smaller, women-led local groups. “They’re there before the crisis happens, during, and after,” she says. “We’ve been trying to find better ways to amplify their voices and help them get into the rooms where the humanitarian community makes decisions.”
Over the years, researchers like Greene have come to use health systems as a delivery path for services through a “whole of person” approach that looks at not only mental and physical health, but also at their circumstances and opportunities for things like employment. “What goes into making someone healthy is multifaceted,” says Zard. “It’s about water. It’s about education. The social determinants of health are critical to whether someone can live a healthy life. Health is an entry point to talking about a wide variety of things that we know are critical to well-being.”
With the number of displaced people growing and the length of displacement increasingly measured in decades, integrating services to help rebuild lives is an evolving challenge. Greene says a minimum of 1 in 5 people affected by a humanitarian emergency will need mental health services.
But many stay only a few days in a shelter, not enough time to get care from a psychologist or other provider. “There’s almost nothing there for those who are in transit,” she says. “Many of the migrants we interview say this is the first time that they’ve even talked about this with anyone.”
Getting them care means exploring new intervention ideas, coordinating with providers, and collecting more data. One new approach has been to give migrants a fanny pack with basic mental health information including a card with contact information so they can tap into services along their route. The self-care kits include a cellphone bag, basic hygiene products, and stress management cards with tips.
Greene has begun a project based in Mexico at the United States and Guatemalan borders to recruit up to 300 migrants to follow over 18 months to understand how their health and health needs evolve, particularly where mental disorders are concerned. Notes Zard, “We need to figure out how we change service delivery so that we are meeting their needs—both the fact that they’re moving, but also that particular needs may arise out of that movement.”
The Program on Forced Migration and Health is not the only team at Columbia Mailman School focused on global crises. As global conflicts rise, so do complex health crises. In Ukraine, ICAP at Columbia University is working with the Ukrainian Center for Public Health in a program funded by the Centers for Disease Control and Prevention. ICAP, as a global health leader that combines innovative research with collaborative technical assistance, is ideally positioned to help implement an antimicrobial resistance (AMR) project to combat infections that no longer respond to available antibiotics. In conflict settings, AMR rates increase, especially among wounded military patients. They suffer trau-
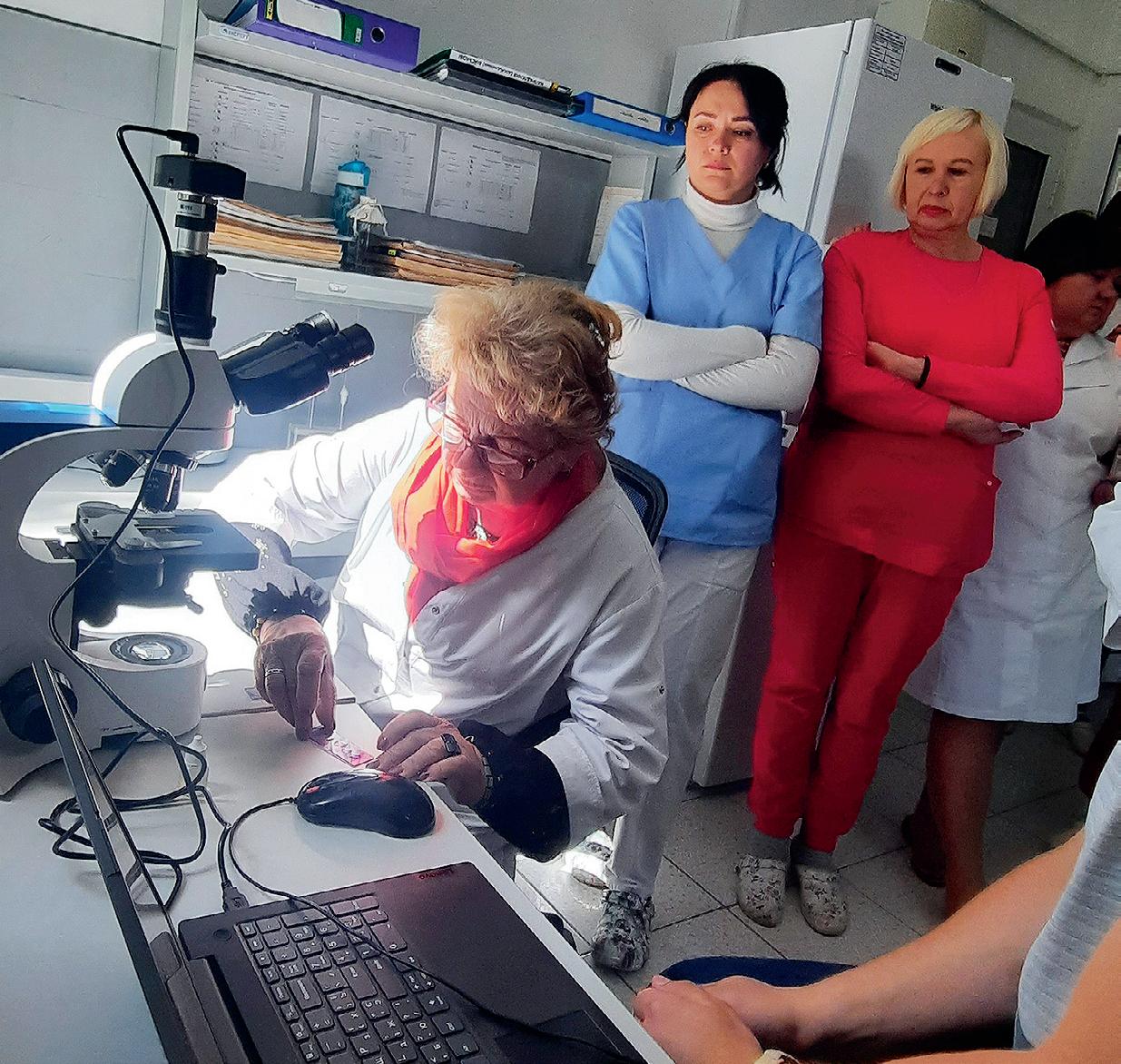
matic wounds and surgeries under conditions that give rise to infection. Then they are evacuated to several healthcare settings over weeks, providing opportunities for antimicrobial-resistant organisms to spread.
AMR causes more deaths globally than HIV or malaria, according to the World Health Organization, which calls it a top ten public health threat. In Ukraine, one of the most concerning AMR infections is Klebsiella pneumoniae. Rapid identification of resistant infections such as this one is key to getting ahead of an outbreak. “A big focus of our work has been improving diagnostic capacity,” says Andrea Howard, MD, director of ICAP’s Clinical and Laboratory Unit.
The hospitals may receive more than 50 wounded people at a time, and identifying infections as soon as possible is a challenge. ICAP began working with healthcare facilities in the Ternopil, Khmelnytskyi, and Vinnytsia regions to procure laboratory equipment and supplies, and to train local workers in how to make the best use of equipment that identifies pathogens within minutes. ICAP has also helped to establish multidisciplinary teams at the hospitals, including a laboratorian, a clinician, an infection prevention and control specialist, an epidemiologist, and a clinical pharmacist.
Sarah Legare, MPH, CPHQ, ICAP’s regional AMR advisor, and Oksana Dereviankina, MD, MBA, ICAP country representative in Ukraine, visited hospitals in the program in January to examine how they’re using new equipment, adjusting their workflows, and isolating patients who may be carrying resistant organisms. There has been progress. The hospitals have developed infection prevention and control committees, standardized lab procedures, and increased collaboration. For Legare, walking the wards is a window into the human reality of her work. “To see these men with their injuries in wheelchairs and on crutches and understand a little bit of what they’ve been through has been personally meaningful to me. We hope it will be impactful, not only for Ukraine, but for Europe, and even globally, to understand and mitigate the risks that AMR is posing right now.”
Zard says the conditions worldwide today are reminiscent of the circumstances that led to the founding of the Program on Forced Migration and Health. “We are in an era that is really troubling as a humanitarian,” she says. “What we thought was the minimum that was required of humanity—that we should not starve populations, that we should not bomb health facilities, that healthcare workers and patients should be protected—all seems to be in play right now. And that, for me, is a profound challenge to everything we hold dear about humanitarian work.”
Jim Morrison has written for The Washington Post, Wired, and The New York Times. He is a contributing writer for Smithsonian.com.

Columbia Mailman School has a storied history of protecting the youngest and most vulnerable.
Now, with the launch of the Child Health Center for Learning and Development, the stars are aligned to tackle this generation’s most daunting challenges.
By Paula Derrow

mental toxicants. (Her groundbreaking research showed that chlorpyrifos, first developed as a nerve gas by Germany in the 1930s and then used as a pesticide, is associated with brain and behavioral change in children and youth. It helped lead to a ban on the chemical’s use in 2021.)
As a perinatal epidemiologist with training in psychiatric epidemiology, Rauh has focused on the neurodevelopment of children, who are particularly vulnerable to physical, environmental, and social stressors in their environment. She has been a faculty member at Columbia Mailman School since 1984; in April, she was named the Jane and Alan Batkin Professor in Child Health and Well-Being. As the community of children in CCCEH birth cohort studies matured, she turned her attention to the well-being of older children and youth in the School’s Washington Heights neighborhood. The time was right to focus on older children. In the listening tour, she says, “One thing that came up again and again is that, while there have been many excellent programs for very young children in the community, school-age children and adolescents continue to have unmet health and developmental needs, many of which were exacerbated during the COVID-19 pandemic.”
Not that research wasn’t being done. “There are amazing things going on in every department related to children’s health at Columbia Mailman School and throughout the University—including research exploring the effects of environmental stressors, climate change, and the impact of gun violence,” says Rauh. “But we could be doing more to integrate and build on these efforts.”
IN THE SUMMER OF 2023, VIRGINIA RAUH, ScD, EMBARKED ON A LISTENING TOUR, ASKING FACULTY AT COLUMBIA MAILMAN SCHOOL, AT THE VAGELOS COLLEGE OF PHYSICIANS AND SURGEONS, AND ACROSS THE UNIVERSITY ABOUT THEIR WORK IN THE AREA OF CHILD AND ADOLESCENT HEALTH. The purpose was to identify research and service-related gaps—community health needs that were not being adequately addressed. For more than 20 years, as deputy director of the Columbia Center for Children’s Environmental Health (CCCEH), Rauh had been putting children at the center of her work, studying the effects of prenatal and early childhood exposure to environ-
For years, Rauh and Danielle Kassow, PhD, director of programs in the Heilbrunn Department of Population and Family Health, had talked about creating a center that would focus more broadly on the health and development of schoolage children. “The idea is to bring together researchers and practitioners at Columbia in child and adolescent psychiatry, pediatrics, and public health to work together synergistically to solve ongoing health, developmental and learning problems experienced by school-age children” Rauh explains.
Now, that dream has become a reality. Thanks to a generous endowment from Alan R. and Jane Batkin to fund a professorship, the School has launched the new Child Health Center for Learning and Development, with Rauh as its inaugural director. Alan R. Batkin (chair emeritus of Columbia Mailman School’s Board of Advisors) and Jane Batkin (a retired child psychologist) are longtime advocates for children’s health. The couple was keenly interested in the teaching and community training that Rauh and Kassow were doing that
focused on the effects of childhood trauma on growth and development. “We teach a course on adverse childhood experiences. Alan and Jane have been directly engaged and visited to hear our students’ presentations,” reports Kassow. The Batkins’ extraordinary generosity ensures that the School will be able to continue to invest in children’s health.
Given the powerhouse talents already focused on children’s health at Columbia Mailman School and throughout the University, “having a center that pulls together people doing this research and service was a no-brainer,” says Rauh. “We aim to reach children where they spend a great deal of time— in schools in Washington Heights, Inwood, Harlem, and the Bronx. We are planning is to develop a corps of MPH students from different departments to work in the schools with existing providers and educational professionals.”
Among their goals: to bring the data management and analytics skills of public health experts to help evaluate the effectiveness of the various programs. “If children are missing a lot of school because of asthma flare-ups, for instance, our students could could monitor and assess family engagement with the asthma management techniques the children are being taught in school clinics, to try to reduce school absences and increase children’s capacity to manage their symptoms,” Rauh explains. The MPH students would get credit for doing public health science teaching and other after-school health-related activities with children and youth. “We would then measure the impact of our work—on dropout rates, truancy rates, or the children’s academic performance,” she says. “We would also like to compare health outcomes of children in schools that have on-site clinics with schools that don’t have them,” she says. “Do children who have access to school clinics end up in the emergency department less? Do they see their pediatrician more regularly?”
Kassow is excited about sending students out into the living laboratory of New York City to partner with organizations like Fresh Youth Initiatives, which serves many immigrant and first-generation youth in the area. One scenario she imagines: “Our students could assess the impact of their programs, and collaborate on ways to make programs stronger.”
The new Center will complement an array of Columbia Mailman School’s existing programs and renowned experts, all laser focused on giving children a chance to grow up in a safer, less toxic world. One of those researchers is Sonali Rajan, EdD, a professor at both Columbia Mailman School and Teachers College. She is also the first president of the new Research Society for the Prevention of Firearm-Related Harms, which evaluates evidence-based practices for preventing firearm-related injuries and deaths.
Since 2020, firearms have been the No. 1 cause of death among U.S. children. But even before guns sat at the top of the list of threats to children, gun violence and injury prevention were a primary focus for Charles Branas, PhD, Gelman Professor of Epidemiology and chair of Epidemiology. “What we’re doing is very much in line with the new Center’s mission, which includes studying the effects of adverse childhood experiences and trauma,” says Branas. Along with his work leading the Centers for Disease Control
“ONE THING CAME UP AGAIN AND AGAIN: SCHOOL-AGE KIDS AND ADOLESCENTS HAD UNMET NEEDS.”
—RAUH

and Prevention (CDC)–funded Columbia Center for Injury Science and Prevention, which, for more than a decade, has been tackling issues such as child safety seats, the nation’s opioid crisis, alcohol misuse, and now gun violence, Branas wants nothing more than to “solve the problems that seem intractable; it’s what so many of us go into public health for—to focus on issues where we can do the greatest good.”
Gun violence is one of those intractable problems, and moving the needle isn’t easy. “Because of politics, our country hasn’t even vaguely invested the amount of money in solving this problem compared with, say, reducing infectious disease in kids,” Branas says. “When I started out as a junior researcher, I was told not to use the f-word in my papers—I’m talking about ‘firearm.’” But thanks, in part, to the work of Branas and nearly three dozen faculty across various schools at the University who are part of the Columbia Scientific Union for the Reduction of Gun Violence (SURGE), there has been some progress. This past June, U.S. Surgeon General Vivek Murthy, MD, declared gun violence a public health crisis.

New streams of funding from the CDC and the National Institutes of Health are enabling Branas and his team to look at the effectiveness of various types of gun violence prevention strategies in schools, whether metal detectors, educational programs, or arming teachers. “Too often, we focus on reacting to gun violence instead of looking at how well preventive tactics work,” he says. “Right now, for instance, states are actively arming teachers, but we haven’t thought through the implications of that.” Branas is also studying the role of school nurses in gun violence prevention, and how well social and emotional learning programs work.
One finding has already been transformational: “Improving housing and expanding green spaces in under-resourced communities not only makes people feel better and healthier, but it also reduces gun violence,” says Branas. “When you have vacant lots and abandoned housing, that increases the opportunity to store illegal guns. Our research shows that improving those spaces reduces that problem and empowers the community to interrupt the cycle of violence,” says Branas. “That’s the most basic kind of public health.”
Just as crucial to the future of our children: the groundbreaking research on the effects of air pollution, pesticides, and other toxic chemicals on fetuses, infants, and children spearheaded by Frederica (Ricky) Perera, MPH ’76, DrPH ’82, PhD ’12, professor of Environmental Health Sciences. Perera is founder of CCCEH at Columbia Mailman School, where she served as director from 1998 to 2019. “Long be-
fore the Center was launched, I was studying environmental toxicants and cancer in adults; then I found that the same molecular markers of exposure to carcinogens were present in newborns. It was clear that we needed to learn more about toxic exposures in the womb.”
The Center began by studying air pollutants. Then Robin Whyatt, DrPH, now professor emeritus, and Rauh brought a focus on pesticides. “The current director, Julie Herbstman, [MSc, PhD], was interested in chemicals in flame retardants and endocrine disruptors like PCBs,” Perera says. The mission grew organically, “and the work just took off,” she adds. The Center is following over 1,000 mothers and children to learn about long-term effects of early environmental exposures. “We’re seeing children of the children—it’s a multigenerational study,” Perera says.
More recently, as director of CCCEH’s Translational Research Program, Perera has focused on the ways fossil emissions and climate-driven exposures affect kids’ cognition, behavior, academic success, and ability to contribute in life. “We’re interested in the benefits of environmental and climate policies for children,” she says. Between Zoom meetings during the COVID-19 pandemic, Perera wrote the book Children’s Health and the Peril of Climate Change At the moment, she is focused on how policies that curb fossil fuel emissions and CO 2 impact the health of children. “Right now, we’re studying how policies to electrify vehicles and reduce power plant emissions benefit children, as well as how New York City’s congestion pricing plan [slated to be implemented in January 2025] might benefit economically vulnerable children, especially.”
Like Rauh and Branas, she is happy that more attention is being paid to children, early exposures, and their development, as well as to the economic disparities that put so many vulnerable kids at risk. “One thing I write about in my book is that we can’t just say we’ve done the deal if we’ve brought down emissions; we need social programs integrated with environmental programs. That means giving kids access to good nutrition, preventive healthcare, and top-notch education. That’s why what Ginny [Rauh] is doing now—focusing on school-age kids in schools—is so important.”
With the endowment from Jane and Alan R. Batkin and the new Child Health Center for Learning and Development, Rauh is adding to the work already being done across Columbia Mailman School. “I see this as a great opportunity to pull together the different parts of my own life’s work, alongside the work of Charles Branas and Sonali Rajan on gun violence and trauma and kids; and of Ricky Perera and Julie Herbstman on children and climate change,” says Rauh. “The new Center provides a scaffolding for us to build on. It’s all coming together.”
Paula Derrow covers health, psychology, and social change for a wide variety of outlets, including universities and nonprofits.

IT TOOK TWO TRIES, BUT TOCHI IROKU-MALIZE FINALLY GOT THE ADMISSIONS OFFICE AT COLUMBIA MAILMAN SCHOOL TO SIT UP AND TAKE NOTICE OF HER. “I just want to let you know that in the future, I will be well known for the work I do internationally,” she wrote in her personal statement when she applied to the School. “And so the choice is, will I say that I’m an alumnus of Columbia, or of another organization?”
It was a fitting pronouncement from someone like Iroku-Malize, the oldest daughter of a surgeon and a nurse practitioner who had big plans to become a leader in the healthcare field. Iroku-Malize had earned her medical degree at the University of Nigeria and had moved back to New York City, where she was born and spent most of her childhood, when she applied to get her MPH. “Lo and behold,” she says with a chuckle about her boldness, “I was accepted.”
In 1998, she started on the Health Policy and Management track. At that time, policymakers and insurance companies had turned to health maintenance organizations to try to make healthcare more efficient. Iroku-Malize recalls learning about that shift from her professors and how it was designed to make primary care doctors gatekeepers. The hardship this created stuck with her and still informs the advocacy work she does today as senior vice president of family medicine at Northwell Health and past president of the American Academy of Family Physicians. “The system is broken and puts a tremendous burden on primary care doctors,” she says. “We need to do better.”
Iroku-Malize set out on her personal path to become a primary care doctor in 1999 after being accepted into the family medicine residency program at Southside Hospital on Long Island (now South Shore University Hospital, part of Northwell Health). She became chief resident and

Dvora Joseph Davey, MPH ’03, PhD
Dvora Joseph Davey became frustrated while working in Mozambique early in her career. Her job was to increase HIV prevention and treatment, but one-third of her U.S.-based funding was tied to abstinence education and another third focused on partner fidelity, with just the last third for promoting condom use. “It seemed so ridiculous to me that you would be telling sex workers, or any population, that you have to abstain from sex and remain faithful,” she says. “It was the opposite of what I had learned at Columbia Mailman School, which was to focus on evidence-based interventions.”
Joseph Davey soon left the post to return to school for a PhD in epidemiology. Today, she lives in Cape Town and works as an epidemiology research associate professor at the David Geffen School of Medicine and Fielding School of Public Health at UCLA, where she not only does research but also helps bring about policy changes that are backed up by science. In 2022, thanks to her work with colleagues evaluating interventions to increase the use of HIV-prevention drugs, South Africa became
By Nancy Averett
stayed on after graduation to help start a hospital medicine program. Soon she was director of that program, using her MPH training to think about conflict resolution, create a strategic business plan, and figure out metrics to see if the program was successful.
She wasn’t quite finished with her MPH, taking a leave and not returning until 2007 after she had added another role at the hospital: associate director, then director, of the family medicine residency program. Returning to Columbia Mailman School, she discovered that the School had innovated, using the flipped classroom and team-based learning, two changes that informed her when she helped Northwell Health create its medical school in 2008. She is the inaugural chair and professor of family medicine at the school. “I was always a go-getter,” she says of all the different roles she has juggled. “And that’s what I was trying to tell the admissions committee in my letter, like, ‘Yeah, listen, I plan on doing some things.’”
one of the first countries to publish guidelines on using PrEP to prevent HIV acquisition and vertical transmission of HIV from pregnant and breastfeeding women to their infants.
Joseph Davey’s interest in such work goes back to her time at Columbia Mailman School. Under the tutelage of maternal health giant Professor Deborah Maine, PhD, Joseph Davey helped evaluate UNICEF programs that were part of the School’s Averting Maternal Death and Disability Program, which Maine started. Then-Dean Allan Rosenfield, MD, another champion of maternal health and HIV prevention, was a big influence. “Allan and Deborah were key in making us realize the importance of reaching women with contraception and safe obstetric options,” she says.
After graduation, she went to Rwanda to study couples where one partner was HIV positive and the other wasn’t, to assist in preventing transmission and help pregnant women to get antiretrovirals. She went on to several nongovernmental organizations before getting a doctorate. “I've always been passionate about working with pregnant women and making sure women can access contraception so they can get pregnant when they want to—all harkening back to my days at Columbia Mailman School. It really stayed with me,” she says. Coming full circle, Joseph Davey joined the School’s Board of Advisors in 2024.

Chinwe Onyekere, MPH ’02
Chinwe Onyekere focused on history and public health while earning her Sociomedical Sciences MPH. Her thesis examined the intersection of bebop, Harlem, and heroin, chronicling how public policies, infrastructure, and other factors made a once-healthy neighborhood vulnerable to the drug epidemic.
“I still remember the course, A History of Public Health Decline in Harlem with Professor Bob Fullilove,” she says. “It just opened my lens. It was incredible. And then Professor Beverly Watkins took us on a Harlem walking tour that brought to life how the built environment can affect health outcomes.”
Onyekere still views public health through a historic lens, and hasn’t forgotten her professors’ other lessons, such as the importance of addressing the social determinants of health and “understanding how community has the solutions.” She has applied those lessons again and again—from elevating how disparities of care and quality are interrelated while at the Robert Wood Johnson Foundation, to working as executive director of

Lourdes
Rodríguez, DrPH ’04
When Lourdes Rodríguez came to the School in 1999, university security guards warned students not to cross over to the east side of Broadway. “I had already crossed Broadway,” Rodríguez says, “and the people on the other side looked more like me than the guards did.”
Immersing herself in communities experiencing difficult conditions was the reason Rodríguez had come to the School. The Puerto Rico native chose the Sociomedical Sciences track because it offered her an interdisciplinary learning space that made room for inquiry with the community. Still, she nearly quit the MPH program after she began working on a National Institutes of Health–funded research project, asking family members to corroborate data reported by research participants who were experiencing their first break of psychosis and struggling with substance use. Family members wanted to share their sadness and fear to make meaning of the moment, but the research design did not allow for that. It was disheartening. “But the chair said to me, ‘What do you need?
Health Leads New York, an initiative at Harlem Hospital where providers can prescribe resources like job training or food access to patients, with volunteers connecting patients to resources.
She later brought those ideas to Main Line Health’s Lankenau Medical Center in Pennsylvania. Onyekere was born in the hospital and grew up in adjacent West Philly, which has consistently poor health outcomes. She created a half-acre farm on hospital grounds to provide fresh food to patients—eventually getting to meet first lady Michelle Obama. “I have chills just thinking about it,” Onyekere recalls. While at Lankenau, Onyekere also co-founded the health equity nonprofit Together for West Philadelphia.
Today, as a program officer at Vanguard’s Strong Start for Kids, she takes a community participatory grantmaking approach to funding early-childhood initiatives such as helping residents start a neighborhood literacy program and bringing a mobile preschool to children attending home-based child care. While residents of West Philly and Harlem have struggled for a long time, their return to health will only happen if the community drives the recovery. “At Columbia Mailman School, I learned to understand the history of a place and then leverage that to do things differently in a way that centers the community. That was a major take-home message for me.”
Because we’ve lost too many Latinas, and you can’t go.’ I said, ‘I need to do research grounded in community.’” This opened the door for her to join the Northern Manhattan Community Voices Collaborative, funded by the W.K. Kellogg Foundation. There, she cut her teeth on developing community-university partnerships. After graduation, she co-directed the Urbanism and the Built Environment track, a groundbreaking program that looked at how city planning could help or hinder public health. This served her well when she joined the New York State Health Foundation in 2012. In 2016, she left for the University of Texas at Austin where she built a community-based research unit before working in public health philanthropy. In 2022, she became CEO of the David Rockefeller Fund, where she is changing the “transactional” model of awarding grants and receiving reports to building deeper relationships. “I want us to work together, rather than in parallel,” she says. It’s a fitting focus for someone at the forefront of community-based public health, and one that is now ingrained in every MPH student. Today, the School’s orientation includes a neighborhood walk that, yes, has students crossing Broadway.
Journalist Nancy Averett covers public health from Cincinnati.Ohio.
IN THE PAST ACADEMIC YEAR, eight master’s students collaborated with faculty, staff, and community leaders on projects to promote racial equity through the School’s FORWARD Fellows program, a paid training experience for students focused on racial justice and health equity. (A four-year-old School-wide initiative, FORWARD is short for Fighting Oppression, Racism and White supremacy through Action, Research, and Discourse.)
The Second Annual Equity Showcase in the spring of 2024 featured a student poster session about their projects. Rose Monet Little, MPH ’24, and Joelle Mentis, MPH ’24, worked on enhancing content about vulnerability to structural racism in Sociomedical Sciences courses. Brandon Christophe, MHA ’24, and Moza Mendes, MPH ’24, facilitated student partnerships with community organizations that address health disparities as part of a Health Policy and Management consulting course. Janelle Micaela S. Panganiban,
THE GLOBAL FIRST LADIES ACADEMY convened for a second time to hear from Columbia Mailman School leaders as part of a partnership with the Global First Ladies Alliance. Over three days, with simultaneous translation services in several languages, presentations by experts in public health and executive leadership sparked lively discussion among 14 first ladies and former first ladies from countries in Africa, South America, and the Caribbean, as well as their advisors. The Alliance was co-founded in 2009 by Cora Neumann, MPH ’23, a member of the School’s Board of Advisors.
Workshops and roundtable discussions focused on interdisciplinary strategies to improve public health and well-being. Facilitators included Wafaa El-Sadr, MD, MPH, MHA, director of ICAP and Columbia World Projects, and Michael Sparer, JD, PhD, chair of Health Policy and Management. First ladies also learned from one another: Fatima Maada Bio, first lady of the Republic of Sierra, spoke about her successful campaign to end childhood marriage in her country, which had been signed into law only days earlier. Mellisa Santokhi-Seenacherry, first lady of Suriname, discussed her work to improve mental health among women and girls.
“Learning from other first ladies has been so valuable, I am so grateful I came,” said Leticia Ocampos, first lady of Paraguay.
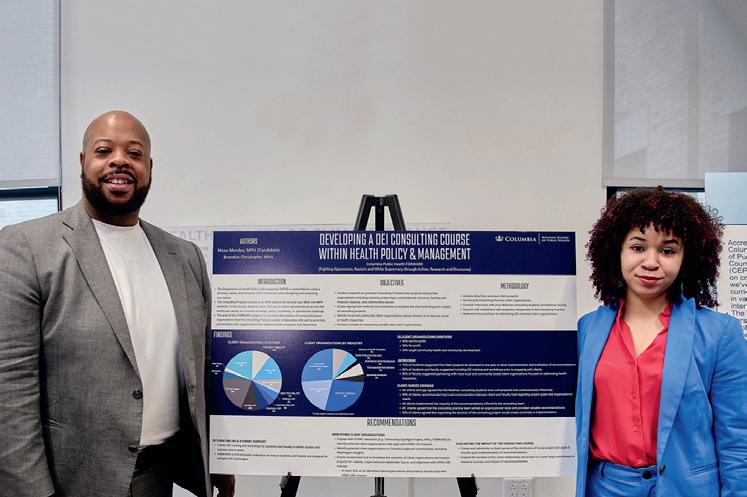
Christophe and
presented a poster summarizing their health equity project in May.
MPH ’24, and Folashade Wilson, MPH ’24, produced a series of short films highlighting community organizations in Washington Heights through the School’s Digital Learning Studio. And Olamide Fagbamiye, MPH ’24, and Caroline O’Connor, MPH ’24, proposed curricular changes in a leadership course to bolster community engagement.
The fellowship program gives students valuable professional experience working on team-based projects. Yvonne Ortiz, MEd, associate dean of inclusive excellence, who moderated a panel discussion with students at the showcase, emphasizes that the equity goals pursued by the fellows align with the goals of the field of public health—“to create healthy communities that are successful and work for everyone,” she says.
The newest group of fellows is now hard at work. Says Christophe, “The sky is the limit on what you can accomplish through this program.”
Books by Campus Authors / Three new works by our faculty bring public health to the page
BUILDING THE WORLDS THAT KILL US (Columbia University Press)
David Rosner, PhD, MPH, Ronald H. Lauterstein Professor of Sociomedical Sciences, and Gerald Markowitz, PhD, adjunct professor of Sociomedical Sciences, explore U.S. history through the lens of death and disease and explain how deep inequities determine health disparities among populations.
WINNING WITH DATA SCIENCE (Columbia Business School Publishing)
Howard Steven Friedman, adjunct professor of Health Policy and Management, co-authored this comprehensive guide to data science with data scientist Akshay Swaminathan. The book walks readers through each step of managing a data science project, with a focus on how readers can collaborate productively and efficiently with data science teams.
HEALTH CARE LAW AND POLICY: ACRONYMS AND TERMS (American Health Law Association)

First daughter of Iraq Sara Rashid and first lady of Angola Ana Dias Lourenço at the conference. Says Dias Lourenço, “There is no other forum like this in the world.”


Editor Ari J. Markenson, JD, MPH ’98, adjunct assistant professor of Health Policy and Management, says he got the idea for this book on his first day at Columbia Mailman School. “At orientation, we were given a packet of terms and acronyms and told by the time we were done with our program, we should know them or the School hasn’t really done its job. I never forgot how useful it was.”







Highlights from the program, clockwise from center: Rayna Patel from the University of North Carolina at Chapel Hill studied use of SNAP nutrition benefits with New York Common Pantry; Ermelinda Calderon from the University of Chicago discussed her research; the University of Pittsburgh’s Matthew Tang presented his research at the Centers for Disease Control and Prevention; Vaughn-Regan Bledsoe from Duke University and classmates in an Environmental Health Sciences course; program leaders Michael Joseph, PhD, MPH, vice dean of education and Troy Hoffman, MPA, director of educational initiatives and of the Summer Public Health Scholars Program (far left) with most of the SPHSP class of 2024; students visited Inwood Farm to learn more about the Lenape people of New York and a health disparities framework for public health; scholars sorted and packaged food for the Washington Heights community at West Side Campaign Against Hunger.
Columbia Mailman School’s Summer Public Health Scholars Program brings together undergraduates from across the country to explore public health and biomedical sciences careers—and have a little fun along the way. The 2024 class of 30 scholars came from 25 colleges and universities. The rigorous program includes public health courses; hands-on field experience; seminars with public health leaders; and mentoring by faculty members—all within a diverse, economically disadvantaged urban environment—to ensure students’ exposure to the breadth and importance of public health as a career option.

“Working alongside my APEx site, the AfriChild Centre, was a once-in-a-lifetime opportunity to collaborate with experts on the ground in Uganda. Without the funding I received, contributing toward this mission would not have been possible.”

Blessing James, MPH ’24
“My practicum with the Undocumented Women’s Fund allowed me to put my coursework into action to help respond to the needs of marginalized women in New York City. I chose this experience because it was a small grassroots organization, and I’m grateful I could work through this practicum with financial support.”
Brittany Markarian, MPH
’23
A gift to Columbia Mailman School supports our students’ hands-on APEx learning experiences, allowing them to collaborate with grassroots organizations that may have limited resources but make maximum impact in their communities. Your generosity empowers students to apply their classroom learnings to address real-world public health challenges, fulfilling Columbia Mailman’s mission to build a healthy, just world. Make your gift today at publichealth.columbia.edu/give or contact Laura Sobel at ls3875@cumc.columbia.edu to discuss the power of leadership giving.
