Association of Ménière disease with human leukocyte antigen in Taiwanese population
KTP-laser assisted endoscopic management of glomus tympanicum tumors: A case series
Endoscopic medialization middle turbinoplasty in endoscopic sinus surgery




































































Association of Ménière disease with human leukocyte antigen in Taiwanese population
KTP-laser assisted endoscopic management of glomus tympanicum tumors: A case series
Endoscopic medialization middle turbinoplasty in endoscopic sinus surgery



































































Jean Abitbol, MD
Jason L. Acevedo, MD, MAJ, MC, USA
Jack B. Anon, MD
Gregorio Babighian, MD
Peter C. Belafsky, MD, PhD
Bruce Benjamin, MD
Gerald S. Berke, MD
Michael J. Brenner, MD
Kenneth H. Brookler, MD
Karen H. Calhoun, MD
Steven B. Cannady, MD
Ricardo Carrau, MD
Swapna Chandran, MD
Chien Chen, MD
Dewey A. Christmas, MD
Nicolle T. Clements, MS
Daniel H. Coelho, MD, FACS
David M. Cognetti, MD
James V. Crawford, MD
David H. Darrow, MD, DDS
Rima Abraham DeFatta, MD
Robert J. DeFatta, MD, PhD
Hamilton Dixon, MD
Paul J. Donald, MD, FRCS
Mainak Dutta, MS, FACS
Russell A. Faust, PhD, MD
Ramón E. Figueroa, MD, FACR
Charles N. Ford, MD
Paul Frake, MD
Marvin P. Fried, MD
Richard R. Gacek, MD
Andrea Gallo, MD
Frank Gannon, MD
Emilio Garcia-Ibanez, MD
Soha Ghossani, MD
William P. R. Gibson, MD
David Goldenberg, MD
Jerome C. Goldstein, MD
Richard L. Goode, MD
Samuel Gubbels, MD
Reena Gupta, MD
Joseph Haddad Jr., MD
Missak Haigentz, MD
Christopher J. Hartnick, MD
Mary Hawkshaw, RN, BSN, CORLN
Garett D. Herzon, MD
Thomas Higgins, MD, MSPH
Jun Steve Hou, MD
John W. House, MD
Glenn Isaacson, MD
Steven F. Isenberg, MD
Stephanie A. Joe, MD
Shruti S. Joglekar, MBBS
Raleigh O. Jones, Jr., MD
Petros D. Karkos, MD, AFRCS, PhD, MPhil
David Kennedy, MD
Seungwon Kim, MD
Robert Koenigsberg, DO
Karen M. Kost, MD, FRCSC
Stilianos E. Kountakis, MD, PhD
John Krouse, MD
Ronald B. Kuppersmith, MD, MBA, FACS
Rande H. Lazar, MD
Robert S. Lebovics, MD, FACS
Keat-Jin Lee, MD
Donald A. Leopold, MD
Steve K. Lewis, BSc, MBBS, MRCS
Daqing Li, MD
Robert R. Lorenz, MD
John M. Luckhurst, MS, CCC-A
Valerie Lund, FRCS
Karen Lyons, MD
A.A.S. Rifat Mannan, MD
Alexander Manteghi, DO
Richard Mattes, PhD
Brian McGovern, ScD
William A. McIntosh, MD
Brian J. McKinnon, MD
Oleg A. Melnikov, MD
Albert L. Merati, MD, FACS
Joseph P. Mirante, MD, MBA, FACS
Ron B. Mitchell, MD
Steven Ross Mobley, MD
Jaime Eaglin Moore, MD
Thomas Murry, PhD
Ashli K. O’Rourke, MD
Ryan F. Osborne, MD, FACS
J. David Osguthorpe, MD
Robert H. Ossoff, DMD, MD
Enrique Palacios, MD, FACR
Michael M. Paparella, MD
Kourosh Parham, MD, PhD
Arthur S. Patchefsky, MD
Meghan Pavlick, AuD
Spencer C. Payne, MD
Kevin D. Pereira, MD, MS (ORL)
Nicolay Popnikolov, MD, PhD
Didier Portmann, MD
Gregory N. Postma, MD
Matthew J. Provenzano, MD
Hassan H. Ramadan, MD, FACS
Richard T. Ramsden, FRCS
Gabor Repassy, MD, PhD
Dale H. Rice, MD
Ernesto Ried, MD
Alessandra Rinaldo, MD, FRSM
Joshua D. Rosenberg, MD
Allan Maier Rubin, MD, PhD, FACS
John S. Rubin, MD, FACS, FRCS
Amy L. Rutt, DO
Anthony Sclafani, MD, FACS
Raja R. Seethala, MD
Jamie Segel, MD
Moncef Sellami, MD
Michael Setzen, MD, FACS, FAAP
Douglas M. Sidle, MD
Herbert Silverstein, MD
Jeffrey P. Simons, MD
Raj Sindwani, MD, FACS, FRCS
Aristides Sismanis, MD, FACS
William H. Slattery III, MD
Libby Smith, DO
Jessica Somerville, MD
Thomas C. Spalla, MD
Matthew Spector, MD
Paul M. Spring, MD
Brendan C. Stack, Jr., MD, FACS
James A. Stankiewicz, MD
Jun-Ichi Suzuki, MD
David Thompson, MD
Lester D.R. Thompson, MD, FASCP
Helga Toriello, PhD, FACMG
Ozlem E. Tulunay-Ugur, MD
Galdino Valvassori, MD
Emre Vural, MD
Donald T. Weed, MD, FACS
Neil Weir, FRCS
Kenneth R. Whittemore, MD
David F. Wilson, MD
Ian M. Windmill, PhD
Ian J. Witterick, MD,MSc, FRCSC
Richard J. Wong, MD
Naoaki Yanagihara, MD
Eiji Yanagisawa, MD, FACS
Ken Yanagisawa, MD, FACS
Anthony Yonkers, MD
Mark Zacharek, MD
Joseph Zenga, MD
Liang Zhou, MD
Dysphagia
Peter C. Belafsky, MD, PhD
Gregory N. Postma, MD
Facial Plastic Surgery
Anthony P. Sclafani, MD, FACS
Geriatric Otolaryngology
Kourosh Parham, MD, PhD, FACS
Karen M. Kost, MD, FRCSC
Head and Neck
Ryan F. Osborne, MD, FACS
Paul J. Donald, MD, FRCS
Reena Gupta, MD
Imaging
Enrique Palacios, MD, FACR
Ramón E. Figueroa, MD, FACR
Laryngoscopic
Robert T. Sataloff, MD, DMA, FACS
Otoscopic
John W. House, MD
Brian J. McKinnon, MD
Pathology
Lester D.R. Thompson, MD, FASCP
Pediatric Otolaryngology
Rande H. Lazar, MD
Rhinoscopic
Eiji Yanagisawa, MD, FACS
Dewey A. Christmas, MD
Joseph P. Mirante, MD, MBA, FACS
Ken Yanagisawa, MD, FACS
Special Topics
Robert T. Sataloff, MD, DMA, FACS
Thyroid and Parathyroid
David Goldenberg, MD
A randomized, controlled trial comparing balloon dilation with ongoing medical therapy as treatment for persistent Eustachian tube dysfunction reported zero complications and significant symptom improvement through 12 months for patients treated with the XprESS™ ENT Dilation System.1
dilation SUPERIOR to medical management
1 Meyer TA, O’Malley E, Schlosser RJ, et al. A randomized controlled trial of balloon dilation as a treatment for persistent Eustachian tube dysfunction with 1-year follow-up. Otol Neurotol. 2018. DOI: 10.1097/
MAO.0000000000001853
INDICATIONS FOR USE: To access and treat the maxillary ostia/ethmoid infundibula in patients 2 years and older, and frontal ostia/recesses and sphenoid sinus ostia in patients 12 years and older using a transnasal approach. The bony sinus outflow tracts are remodeled by balloon displacement of adjacent bone and paranasal sinus structures. To dilate the cartilaginous portion of the Eustachian tube for treating persistent Eustachian tube dysfunction in patients 18 years and older using a transnasal approach.
Please see Instructions for Use (IFU) for a complete listing of warnings, precautions, and adverse events as well as cleaning, sterilizing and care for surgical instruments.

CAUTION: Federal (USA) law restricts these devices to sale by or on the order of a physician.
ENTELLUS MEDICAL and XPRESS are trademarks of Entellus Medical, Inc.
DURABLE symptom improvement through 12 months
Editor-in-Chief Robert T. Sataloff, MD, DMA, FACS 219 N. Broad St., 10th Fl., Philadelphia, PA 19107 entjournal@phillyent.com Ph: 215-732-6100
Managing Editor Linda Zinn
Manuscript Editors Martin Stevenson and Wayne Kuznar
Associate Editor, Reader Engagement Megan Combs
Creative Director Eric Collander
Customer Service/Subscriptions www.entjournal.com/subscribe Ph: 888-244-5310 email: VendomeHM@emailpsa.com
Reuse Permissions Copyright Clearance Center info@copyright.com Ph: 978-750-8400 Fax: 978-646-8600
Chief Executive Officer Jane Butler
Chief Marketing Officer Dan Melore
Vice President, Finance Bill Newberry
Vice President, Custom Media Jennifer Turney
Director, Circulation Rachel Beneventi
ENT-Ear, Nose & Throat Journal (ISSN: Print 0145-5613, Online 1942-7522) is published 9 times per year in Jan/Feb, Mar, Apr/May, June, July, Aug, Sept, Oct/ Nov and Dec, by Vendome Group, LLC, 237 West 35th Street, 16th Floor, New York, NY 10001-1905.
©2018 by Vendome Group, LLC. All rights reserved. No part of ENT-Ear, Nose & Throat Journal may be reproduced, distributed, transmitted, displayed, published, or broadcast in any form or in any media without prior written permission of the publisher. To request permission to reuse this content in any form, including distribution in education, professional, or promotional contexts or to reproduce material in new works, please contact the Copyright Clearance Center at info@ copyright.com or 978.750.8400.
EDITORIAL: The opinions expressed in the editorial and advertising material in this issue of ENT-Ear, Nose & Throat Journal are those of the authors and advertisers and do not necessarily reflect the opinions or recommendations of the publisher, editors, or the staff of Vendome Group, LLC. ENT-Ear, Nose & Throat Journal is indexed in MEDLINE/PubMed and Current Contents/Clinical Medicine and Science Citation Index Expanded. Editorial offices are located at 812 Huron Rd., Suite 450, Cleveland, OH 44115. Manuscripts should be submitted online at www.editorialmanager.com/entjournal. Instructions for Authors are available at www.entjournal.com

SUBSCRIPTIONS: For questions about a subscription or to subscribe, please contact us by phone: 888-244-5310; or email: VendomeHM@emailpsa.com Individual subscriptions, U.S. and possessions: 1 year $225, 2 years $394; International: 1 year $279, 2 years $488; Single copies $28; outside the U.S., $40.
POSTMASTER: send address changes to Ear, Nose & Throat Journal, PO Box 11404 Newark, NJ 07101-4014.
Now there’s a better way to provide saline washes. The HydroCleanse™ Sinus Wash Delivery System from Medtronic combines pressurized sinus irrigation with builtin suction capability for a more efficient procedure. Disposable and easy to use, it allows you to irrigate the sinuses while limiting pooling and effluent discharge.
§ Disposable and easy to use
§ 360° fan spray
§ Pressurized saline irrigation
§ Built-in suction capability
§ Choice of angled catheter tips

HydroCleanse™ Sinus Wash Delivery System
IMPROVE THE SALINE WASH EXPERIENCE. CHOOSE HYDROCLEANSE.
Rx only. Refer to product instruction manual/package insert for instructions, warnings, precautions and contraindications.
For further information, please call Medtronic ENT at 800.874.5797 or consult Medtronic’s website at www.medtronicent.com
396 Association of Ménière disease with human leukocyte antigen in Taiwanese population
Kai-Chieh Chan, MD; Che-Ming Wu, MD; Wan-Ling Ho, MD, PhD; Ping-Chin Lai, MD, PhD
399 KTP-laser–assisted endoscopic management of glomus tympanicum tumors: A case series
Julia E. Noel, MD; Hamed Sajjadi, MD
404 Endoscopic medialization middle turbinoplasty in endoscopic sinus surgery
Elie Rebeiz, MD, FACS; Mihaela Smith, PA
413 Evaluation of bendable surgical suction devices made of shape-memory alloy for the endonasal transsphenoid removal of pituitary tumors
Ronny Grunert, PhD; Sandra Klietz, BEng; Paul A. Gardner, MD; Juan C. Fernandez-Miranda, MD; Carl H. Snyderman, MD, MBA
E1 Diagnosis and treatment of laryngopharyngeal reflux: Use of empirical lansoprazole
Aysegul Batioglu-Karaaltin, MD; Omer Develioglu, MD; Umur Akiner, MD; Mehmet Kulekci, MD
E7 An unusual presentation of papillary thyroid carcinoma in a pediatric patient: A case report
Matthew G. Cravens, BS, BA; Tyson J. Nielsen, MD; Erynne A. Faucett, MD; Audrey B. Erman, MD
E11 Red ear syndrome: Perspectives for the otolaryngologist
Sheldon P. Hersh, MD; Joshua N. Hersh, MD
E15 A fistulating oropharyngeal lesion
Richard Heyes, MBChB (Hons), MRCS DO–HNS; Courtney M. Tomblinson, MD; David G. Lott, MD
E18 Destructive lesion of the temporomandibular joint: A case of tophaceous pseudogout
Jessica B. Howell, MD; Yula A. Indeyeva, MD; Stephanie E. Ambrose, MD; Evan R. Reiter, MD
E21 Effects of acidic and nonacidic reflux on the eustachian tube: An animal experiment
Erbil Kilic, MD; Mustafa Gerek, MD; Omer Karakoc, MD; Mehmet Gamsizkan, MD
E28 Aggressive fibromatosis of the parotid gland
Vishaal Patel, MD; Virginia Falvello, MD; Marion Hughes, MD; Barry Schaitkin, MD
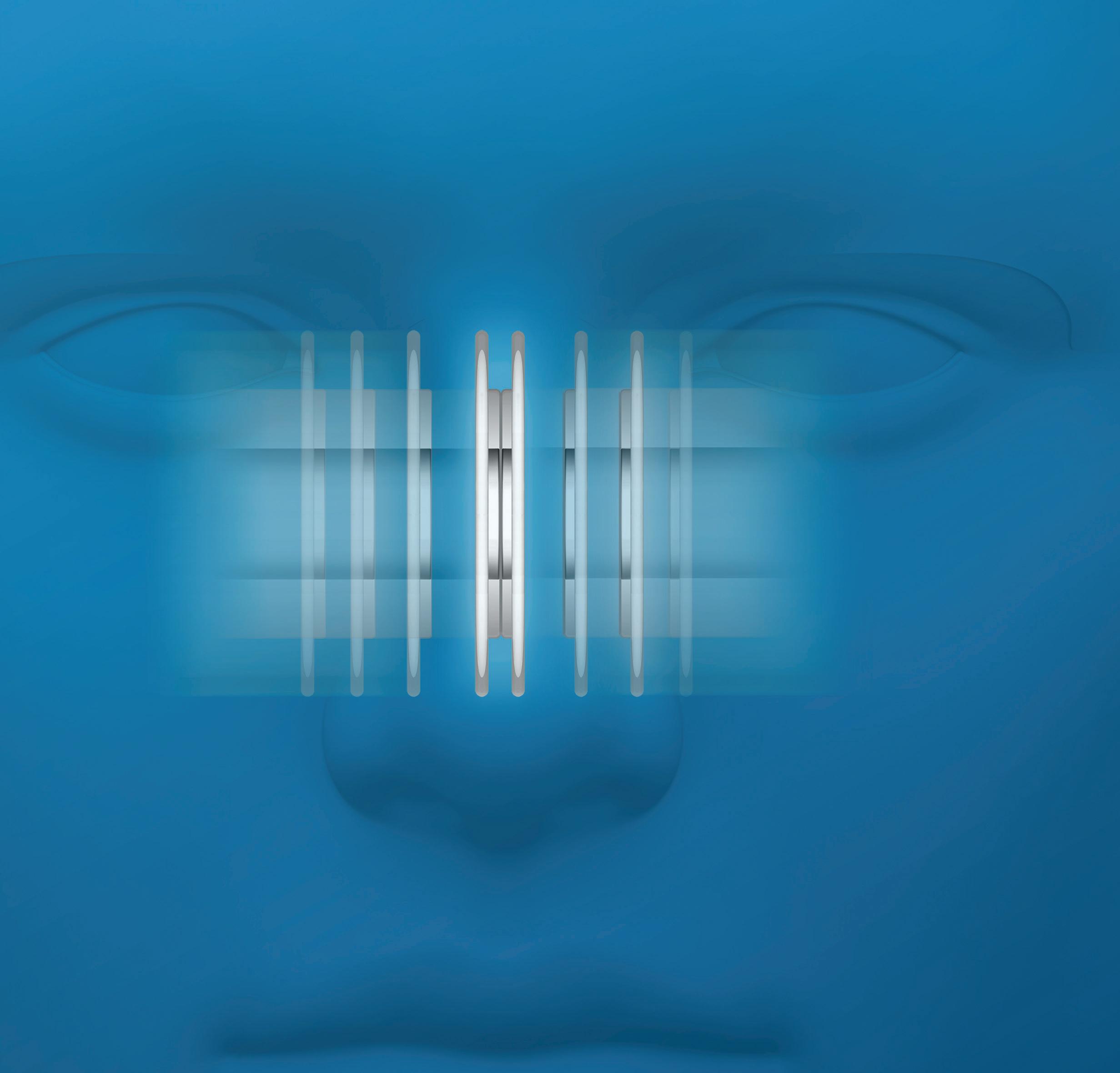
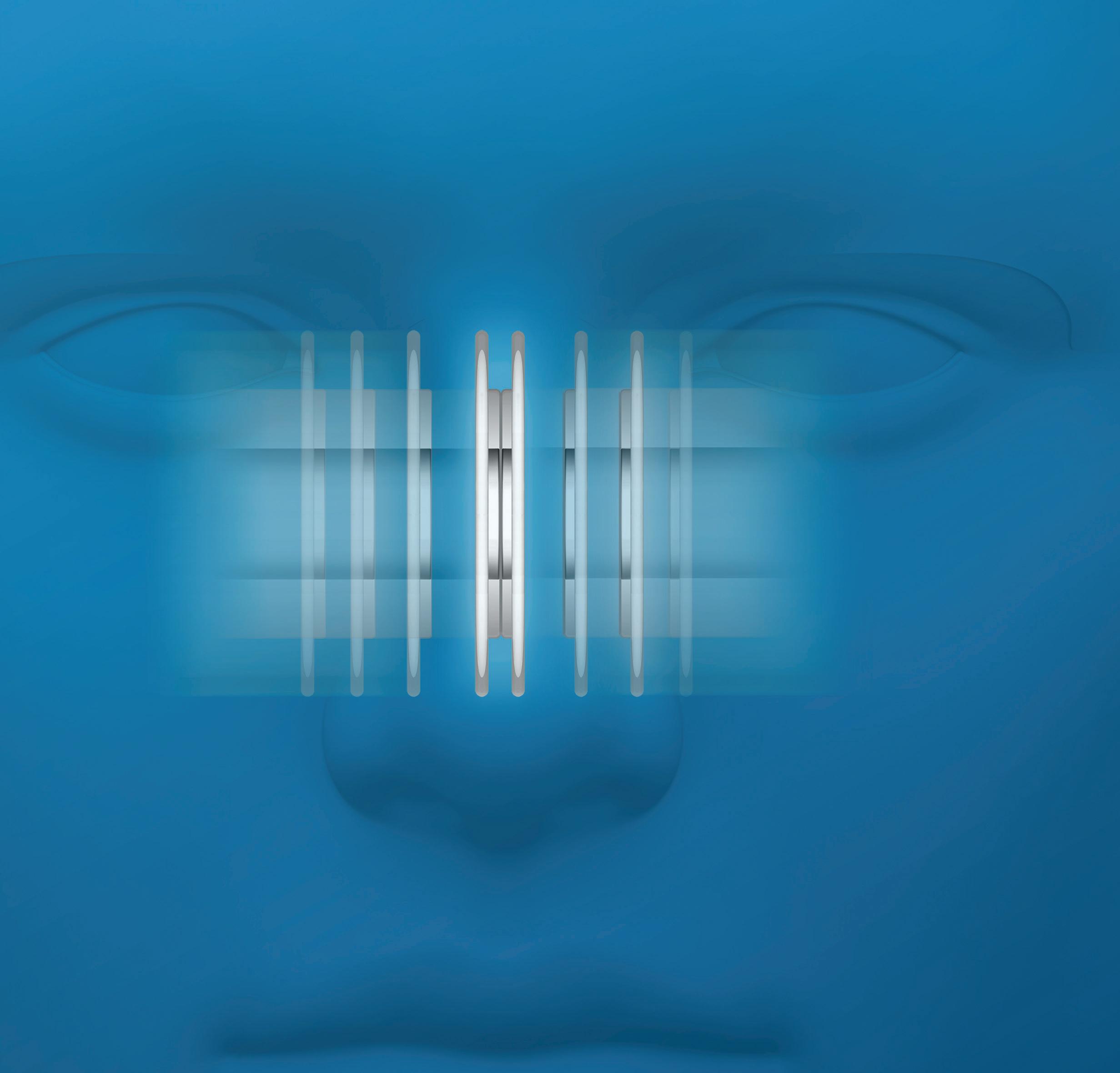
Partnership between Medtronic and surgeons like you, working together to advance navigation technology and protect patients — over 20 years strong — has resulted in some of the most advanced ENT technology available.
You can continue to trust navigation surgical solutions from Medtronic, such as the StealthStation™ ENT, to increase your operative efficiency and precision. Let’s advance further, together.

Rx only. Refer to product instruction manual/package insert for instructions, warnings, precautions and contraindications.
For further information, please call Medtronic ENT at 800.874.5797 or consult Medtronic’s website at www.medtronicent.com
Ear, Nose & Throat Journal's website is easy to navigate and provides readers with more editorial content each month than ever before. Access to everything on the site is free of charge to physicians and allied ENT professionals. To take advantage of all our site has to offer, go to www.entjournal. com and click on the “Registration” link. Once you have filled out the brief registration form, you will have full access. Explore and enjoy!
Diagnosis and treatment of laryngopharyngeal reflux: Use of empirical lansoprazole
Aysegul Batioglu-Karaaltin, MD; Omer Develioglu, MD; Umur Akiner, MD; Mehmet Kulekci, MD
The objective of this study was to evaluate the effectiveness of empirical medical treatment in patients with laryngopharyngeal reflux (LPR) disease by scoring the findings and symptoms. Hence, 122 patients were examined at the voice laboratory with a laryngovideostroboscopic device, and all results were recorded for further evaluation. Patients were treated with lansoprazole twice a day. All patients....
An unusual presentation of papillary thyroid carcinoma in a pediatric patient: A case report
Matthew G. Cravens, BS, BA; Tyson J. Nielsen, MD; Erynne A. Faucett, MD; Audrey B. Erman, MD
Cystic neck masses in the pediatric population are common but rarely concerning for malignancy. Given this typically benign nature, they are frequently managed conservatively. Here we present an unusual case of a waxing and waning cystic neck mass in a pediatric patient. After surgical removal, the mass was found to be metastatic papillary thyroid cancer. This is a unique presentation in....
Red ear syndrome: Perspectives for the otolaryngologist
Sheldon P. Hersh, MD; Joshua N. Hersh, MD
Red ear syndrome (RES) is an unusual, often unrecognized condition that has rarely been reported in the otolaryngology literature despite the presence of symptoms and associated disorders of relevance to the otolaryngologist. When present, RES may have diagnostic value when uncertainties arise in cases of sinus headache and referred otalgia. Despite the appearance of a distinctive red ear, as well as symptoms and....
A fistulating oropharyngeal lesion
Richard Heyes, MBChB (Hons), MRCS DO–HNS;
Courtney M. Tomblinson, MD; David G. Lott, MD
Post-transplant lymphoproliferative disorder (PTLD) is a unifying term for a spectrum of lymphoid expansion entities brought about by immunosuppression. It can present throughout the head and neck, and tonsillar involvement is not limited to children. We report the case of a 67-yearold woman who developed odynophagia associated with putrid halitosis 4 months after she had undergone renal....
Destructive lesion of the temporomandibular joint: A case of tophaceous pseudogout
Jessica B. Howell, MD; Yula A. Indeyeva, MD; Stephanie E. Ambrose, MD; Evan R. Reiter, MD
Tophaceous pseudogout of the temporomandibular joint is a rare entity that clinically and radiographically mimics neoplastic or infectious conditions. Diagnosis requires histopathologic examination. Given the rarity of this condition, there is a paucity of information pertaining to the surgical approach, reconstructive options, and postoperative outcomes....
Effects of acidic and nonacidic reflux on the eustachian tube: An animal experiment
Erbil Kilic, MD; Mustafa Gerek, MD; Omer Karakoc, MD; Mehmet Gamsizkan, MD
We investigated the effects of pepsin/hydrochloric acid and bile acids on eustachian tube function and eustachian tube mucosa in 40 Sprague-Dawley rats. The animals were randomly assigned to groups of 10: one group received pepsin/ hydrochloric acid (pepsin/HCl group), another received human bile (human bile group), a third received a mixture of pepsin/HCl and human bile (combination group), and the fourth received isotonic saline solution (control group)....
Aggressive fibromatosis of the parotid gland
Vishaal Patel, MD; Virginia Falvello, MD; Marion Hughes, MD; Barry Schaitkin, MD
Extra-abdominal fibromatosis (EAF) is a rare, locally aggressive tumor that originates in fascial structures. It accounts for less than 0.3% of all tumors diagnosed. Head and neck tumors account for only 7% of those, and only a few cases occurring in the parotid gland have been previously reported. We describe the case of a 34-year-old woman who presented with a painful parotid mass. She was found to have an EAF of her right parotid gland....
Otoscopic Clinic: Stapes footplate defect as a source of CSF leak and otogenic meningitis in a patient with a cochlear implant
Maria Vartanyan, MD; Fiona Hill, MBBS; Kumiko Orimoto, MD, PhD; Stephen O’Leary, PhD, FRACS, FAHMS




The addition of the Multi-Hz test to the GSI TympStar Pro™ clinical middle ear analyzer provides audiologists the tools needed to confidently identify resonance frequency of the middle ear system. This powerful test can be completed five times faster than its predecessor and takes as little as 13 seconds. Multi-Hz offers the efficiency and accuracy needed to assess pathologies in the middle ear system.





The GSI TympStar Pro now has a dedicated test type to identify a patulous eustachian tube. The capability to store measurements from four test conditions and an adjustable time base makes the Patulous ET test a reliable, flexible, and customizable option to meet the needs of every facility’s protocol.

Visit www.grason-stadler.com to learn more about all the features of the TympStar Pro and explore the entire line of GSI products.



The root cause of physician burnout cannot be solved with resilience efforts
Physician burnout has become a hot topic in the popular press. It seems that a day doesn’t pass without seeing an email, editorial, or published research article on the topic, and this is good. Burnout in medicine is real and has been proven to lead to detrimental effects on the physicians who are affected, their colleagues, and even their patients and their patients’ clinical outcomes. It has been shown to start in medical school and affects about 50% of physicians at any given time regardless of career phase, practice setting, income, or gender.
Professional burnout is a constellation of three factors that manifest mostly in people who work in the human services industries: emotional exhaustion, depersonalization, and reduced sense of professional accomplishment. Emotional exhaustion presents with chronic feelings like one is at the end of his/her rope and has no more to give on an emotional level. Over time, this can lead to depersonalization, which is the frightening tendency to treat those people around us as objects. The reduced sense of professional accomplishment that results is associated with adverse psychological consequences such as depression and anxiety; and burnout may even play a role in the rising rate of physician suicide.
While physician burnout surely has been present in some individuals across the profession for decades, the corporatization of medicine that began in the early 1990s has levied a heavier toll on physicians in recent years. The burnout problem can be traced largely to loss of physician autonomy and marginalization of physicians in the decision making within our practices.
The exponential rise in healthcare administrative burden, challenges of the electronic medical record, external practice regulations, financial pressures, and increased focus on outcomes have created a recipe for burnout in the physician workforce. The problem is real and has become recognized at the highest ranks in medicine in the United States. The good news is that recognition and awareness of critical problems generally leads to change.
Initial efforts targeting the problem were directed at physician resilience: sleep hygiene, exercise, mindfulness/meditation, taking vacation, and avoidance of unhealthy coping strategies such as alcohol misuse. While in no way diminishing the role that these efforts
play in everyone’s life, they just don’t get to the root of the problem.
With expanded pressure to address the issue, there has been great growth in wellness programs available to clinicians at most large health systems. These are valuable as they can serve as a toolbox for individual wellness and often offer an opportunity for interaction with peers regarding the topic. Such programs also serve as an important platform to initiate institutional changes around physician work, workflow, documentation support, electronic record optimization, and over- interpretation of federal regulation, for example.
More change is needed. The National Academy of Medicine has launched the Action Collaborative on Clinician Well-Being and Resilience. Hopefully, this will set the stage for national policy changes to protect and promote our physician workforce collectively. Physicians need to fight the notion that we are simply “providers,” which is a word I detest. We are at the core of every element of restoring and promoting health for our patients. We are not a cog in the corporate healthcare wheel, and we need to stand together for our patients and ourselves.
As physicians, we need to find a way to unite, lest we be left to wallow with the destiny of our profession at the hands of healthcare administrators. Only through the preservation of our profession can the problem of burnout be mitigated meaningfully.
Michael M. Johns III, MD Director, USC Voice Center Division Director, Laryngology Professor, USC Caruso Department of Otolaryngology— Head and Neck Surgery University of Southern California Los AngelesOur amazing mentor, Eiji Yanagisawa, was an Olympics-caliber gymnast as a young man. Because of an injury sustained in a gymnastic competition, Eiji’s future turned to a career in medicine. He eventually trained as an otolaryngologist at Yale University School of Medicine under Dr. John Kirchner. Dr. Yanagisawa was destined to become probably the most outstanding and well-known otolaryngologist trained at this institution. He remained in New Haven in private practice but became an important influence in the training of Yale ENT residents for more than 50 years.
Dr. Christmas’s association with Dr. Yanagisawa started in the 1960s when Dr. Christmas was fortunate enough to have him as his most important teacher. It was standard procedure for Dr. Yanagisawa and his residents to document every case seen and every operation performed with 35-mm slides or 16-mm movies. In the 1960s, he was a prominent otologist of the highest caliber, and he was able to bring the best, i.e., Hal Schuknecht and Jim Sheehy, to Yale to teach.
Working as a resident with Dr. Yanagisawa involved long days and unending nights with a very patient instructor who had a great desire to teach and an intense desire to photo-document everything.
In 1975, Dr. Yanagisawa coupled a home Magnavox video recorder with a flexible fiberoptic scope to perform fiberoptic videolaryngoscopy (figure 1, A). He made a presentation of “Photography and Videotaping of Microsurgery of the Larynx” at the 1977 AAO–HNS annual meeting, and his photo-documentation career was off to the races.


Because of a friendship formed in Dubrovnik, Yugoslavia (now Croatia), Dr. Yanagisawa was instrumental in bringing Dr. Heinz Stammberger to Yale in 1984 to present one of the first courses on functional endoscopic sinus surgery in the United States. In the 1990s, Dr. Yanagisawa converted to a true rhinologist with the introduction of powered endoscopic sinus surgery. He participated in several instruction courses
Continued on page 393
 Jérôme R. Lechien, PhD, MS; Camille Finck, MD, PhD
Jérôme R. Lechien, PhD, MS; Camille Finck, MD, PhD
A 38-year-old male singer was referred to the Department of Laryngology and Voice Rehabilitation with a few months’ history of hemoptysis and dysphonia. His medical history included a human immunodeficiency virus infection and several episodes of depression. His voice was dysphonic (1/3), breathy (1/3), and asthenic (2/3), and videolaryngostroboscopy revealed bilateral multiple vocal fold telangiectasias without visible hemorrhage or polyp (figure 1). Nasal telangiectasias also have been visualized with telangiectasias in the pharyngolaryngeal area. The patient complained of limited maximal phonation time (MPT: 9.5s); and acoustic measurements revealed a fundamental frequency (F0) of 201 Hz.
Frequency and intensity ranges were 164 to 415 Hz and 59 to 90 dB, respectively. A surgical procedure was performed with a KTP laser 532nm. The patient’s voice improved gradually during the follow-up period without recurrence (figure 2). After 18 months, his
voice was perceptually normalized, and voice measures were considerably improved (F0: 155 Hz; MPT: 18.2 s; frequency: 110 to 440 Hz; and intensity: 53 to 95 dB).
Laryngeal telengiectasia involving the vocal folds is an uncommon presentation of Rendu-Osler-Weber; only one case has been described.1 This condition is known to cause hemorrhages, which are often difficult to control given the vascular wall fragility. It is extremely rare to diagnose Rendu-Osler-Weber syndrome based on a vocal disorder. Early diagnosis and adequate treatment are needed to control the impact of the disease on voice quality, especially in voice professionals. Follow-up is crucial given the high risk of recurrence.1,2

1. Chang J, Yung KC. Dysphonia and vocal fold telangiectasia in hereditary hemorrhagic telangiectasia. Ann Otol Rhinol Laryngol 2014;123(11):769-70.
From the Laboratory of Phonetics, Faculty of Psychology, Research Institute for Language Sciences and Technology (Dr. Lechien and Dr. Finck); the Laboratory of Anatomy and Cell Biology, Faculty of Medicine, Research Institute for Health Sciences and Technology (Dr. Lechien), University of Mons, Mons, Belgium; and the Department of Otolaryngology and Head and Neck Surgery, CHU de Liège, Liège, Belgium (Dr. Finck).
Vikas Malhotra, MBBS, MS(ENT), DNB; Nikhil Arora, MBBS, MS(ENT), DNB; Pankhuri Mittal, MBBS, MS(ENT), DNB
A 16-year-old female patient presented with a huge neck swelling that had been present since she was 2 years of age. On examination, the swelling was found to measure approximately 20 × 15 cm. The swelling was mostly solid with cystic areas in between, and it was hanging down to the upper chest with the overlying skin stretched and discolored (figure 1).

After considering all the differentials of cystic neck swelling, such as lymphangioma, cavernous hemangioma, branchial cleft cyst, and teratoma, we decided to perform fine-needle aspiration cytology, which revealed benign cystic swelling with the possibility of lymphangioma. Contrast-enhanced computed tomography (CT) showed a huge lesion reaching superiorly to the
From the Department of ENT and Head and Neck Surgery, Maulana Azad Medical College, New Delhi, India.
patient’s skull base and inferiorly to the suprasternal notch. The lesion involved the parapharyngeal space, with attenuation of the great vessels (figure 2).
As expected, sclerotherapy with multiple injections of bleomycin to the swelling produced no response because of the lesion’s size. Because of the risk of the patient’s developing airway obstruction if the swelling expanded farther, she was taken to surgery for excision via a transcervical approach without a mandibulotomy. The gross specimen after removal weighed 1.42 kg and measured 20 × 15 × 9 cm in its largest dimensions (figure 3). Histopathology of the specimen was consistent with lymphangioma. To the best of our knowledge, this is the world’s largest neck lymphangioma ever removed in toto with minimal access. The patient was allowed to eat and drink orally within 24 hours, and she could speak normally almost immediately. She remained free of the disease at her 2-year follow-up.

Lymphangiomas usually result from sequestration or obstruction of developing lymph vessels. The clinical effects with which these patients present depends on their relationship with vital structures, although most patients present with a painless lump and no other symptoms.
The management of such lesions is still a matter of great debate. Various treatment modalities are available, including sclerotherapy, cryotherapy, excision, radiotherapy, and embolization. Complete surgical excision is traditionally considered the treatment of choice,1,2 although sclerotherapy also has been considered appropriate. 3 If the planes are well defined, surgical excision remains the treatment of choice.
Treatment selection should be based on the size, depth, and location of the lesion, as well as potential morbidity and surgical complications. In our case, we initially tried sclerotherapy because lymphangiomas generally are infiltrating in nature, making surgical excision difficult, but it was not effective. Considering the possibility of airway obstruction and death with such a large swelling, we decided to perform surgical excision despite the vital structures involved.
In our case, the transcervical surgical approach without mandibulotomy was significant, demonstrating that huge lesions can be removed without mandibulotomy and with minimal access, thereby avoiding postoperative feeding and speech difficulties and leading to faster recovery. Because such lesions have a propensity for recurrence, our patient remains on a rigorous monthly follow-up. Early detection of lymphangiomas is essential for better management.
1. Riechelmann H, Muehlfay G, Keck T, et al. Total, subtotal, and partial surgical removal of cervicofacial lymphangiomas. Arch Otolaryngol Head Neck Surg 1999;125(6):643–8.
2. Mandel L. Parotid area lymphangioma in an adult: Case report. J Oral Maxillofac Surg 2004;62(10):1320–3.

A 57-year-old man with a multinodular goiter and hyperthyroidism presented with progressive hoarseness and dysphagia of 2 months’ duration. Flexible laryngoscopy revealed a nodular appearance of the soft palate, uvula, epiglottis, arytenoids, and vocal folds. The patient was started on omeprazole 20 mg twice daily and scheduled for a barium swallow study.
On the patient’s return a week later, he reported a persistent globus sensation. Because of the appearance of his oropharynx and supraglottis after a negative swallow study (figure), he underwent a biopsy of his polypoid-appearing uvula. Pathology returned as a benign polypoid mucosa containing deposits consistent with amyloid, but with negative Congo red staining for amyloidosis.
Two months later, the patient underwent a total thyroidectomy for his multinodular goiter. Pathology of the thyroid specimen was positive for nodular hyperplasia without amyloid deposits. Six months after his initial presentation, he underwent esophagoscopy with gastroenterology for persistent dysphagia despite removal of his thyroid goiter. Biopsy of an esophageal specimen showed amyloid deposits with negative Congo red staining. The patient was referred to hematology/ oncology, where he underwent a bone marrow aspirate of his iliac crest. He was subsequently diagnosed with and began treatment for systemic amyloidosis.

While common conditions are more likely to result in hoarseness and dysphagia, amyloidosis is a rare but possible diagnosis. Laryngeal amyloidosis presents earlier than nonlaryngeal amyloidosis because of its anatomic location, but any polyposis of the airway should raise suspicion.1 Because our patient’s biopsies were consistently negative for Congo red stain, it was important to have a hematology/oncology evaluation to
rule out other causes of abnormal protein deposition, such as multiple myeloma.
Amyloid deposition often does not demonstrate diagnostic staining, and electron microscopy may be necessary to confirm a diagnosis.2 Physicians should refrain from making diagnoses of more common etiology until biopsy has been performed in these cases. A thorough workup with subsequent identification of abnormal physical exam findings is important in patients with a seemingly obvious yet complicated presentation.
References
1. Simpson GT 2nd, Strong MS, Skinner M, Cohen AS. Localized amyloidosis of the head and neck and upper aerodigestive and lower respiratory tracts. Ann Otol Rhinol Laryngol 1984;93(4 Pt 1):374-9.
2. Goodman TF Jr., Abele DC, West CS Jr. Electron microscopy in the diagnosis of amyloidosis. Arch Dermatol 1972;106(3):393-7.
From the Department of Otolaryngology–Head and Neck Surgery, West Virginia University School of Medicine, Morgantown. Previous presentation: This article has been edited and adapted from its presentation as a poster at the 2018 American Broncho-Esophagological Association Annual Meeting; April 19, 2018; National Harbor, Maryland.
A 75-year-old woman presented with a 4-month history of nasal congestion, right facial pain, and headaches. She had been given antibiotics by her family physician for suspected sinusitis. Her pain improved, but the congestion persisted. She also noticed a metallic taste and began to spit up thick, green secretions. Her medical history was significant for hypothyroidism, hypertension, dyslipidemia, and Paget disease. Her medications included levothyroxine, lisinopril, atorvastatin, propranolol, calcium, vitamin D, and alendronate. Endoscopic examination revealed thick secretions in the nasopharynx and mucopurulence from the right middle meatus. Computed tomography of the sinuses revealed complete opacification of the right maxillary sinuses, with evident “double densities;” magnetic resonance imaging (MRI) was subsequently performed, which corroborated the diagnosis of fungal sinusitis (figure 1).

The patient underwent right-sided, limited functional endoscopic sinus surgery in our outpatient clinic, including uncinectomy, wide maxillary antrostomy, and removal of fungal debris. An anterior ethmoidectomy also was performed to complete the opening of the
ostiomeatal complex (figure 2). A large-caliber, shortcurve suction device was used to effectively aspirate the fungal debris, after sending specimens for fungal and bacterial cultures, as well as histopathology.
Surgical treatment of this elderly patient’s fungal sinusitis could have been performed either in the operating room under general anesthesia, in the operating room with intravenous sedation, or under local anesthesia in the outpatient department. The decision to proceed with a particular approach must be based on several factors, starting with a comprehensive discussion of the options with the patient. The potential advantages and disadvantages of each option, as well as the patient’s comorbidities, medications, and anatomy must all be considered in guiding the final decision.
Technologic advances have facilitated a shift from the operating room to the office, as evidenced by the fact that in the United States in 2009, at least 12 million outpatient procedures were performed.1 Potential advantages include saving operating room time, avoiding general anesthesia, reduced cost, scheduling convenience, and a quicker recovery for the patient.2-5
From the Department of Otolaryngology–Head and Neck Surgery (Dr. Kost, Dr. Tewfik, and Dr. AlSuliman), and the Voice and Dysphagia Laboratory (Dr. Kost), McGill University, Montreal, Canada; the Department of Surgery, Division of Otolaryngology–Head and Neck Surgery, UCONN Health, Farmington, Ct. (Dr. Parham); and the Department of Otolaryngology–Head and Neck Surgery, King Fahad Medical City, Riyadh, KSA (Dr. AlSuliman),
Figure 2. Photo shows uncinectomy, wide maxillary antrostomy, and removal of fungal debris.
Dr. Yanagisawa has published approximately 375 original articles, 79 book chapters, and 4 otolaryngology books (figure 1, C). He has produced more than 75 movies and instructional videotapes. He has made more than 200 presentations at ENT meetings.
It is interesting that despite the logarithmic increase in office-based procedures, there are few safety-related guidelines regarding patient selection, vital sign monitoring,2,5 and equipment requirements, such as the presence of a crash cart. Risks are often specialty-specific. In sinus surgery, although bleeding may be an issue, the lack of volatile agents and use of local anesthesia tend to improve the visual field. In addition, feedback from the patient helps to prevent orbital and/or skull base complications, since these structures are sensitive and painful. In laryngology, much of the risk is airway-related.
In summary, office-based procedures in the elderly, particularly the frail and those at risk for cognitive decline, offer a potentially attractive alternative to surgery under general anesthesia. In the absence of established guidelines, sound judgement and careful consideration of both patient- and office-related factors are critical in optimizing patient outcomes and safety.
References
2. Yung KC, Courey MS. The effect of office-based flexible endoscopic surgery on hemodynamic stability. Laryngoscope 2010;120(11):2231-6
3. Bove MJ, Jabbour N, Krishna P, et al. Operating room versus office-based injection laryngoplasty: A comparative analysis of reimbursement. Laryngoscope 2007:117(2):226-330.
4. Cho S, Arya N, Swan K, et al. Unsedated transnasal endoscopy: A Canadian experience in daily practice. Can J Gastroenterol 2008;22(3):243-6.

5. Morrison MP, O’Rourke A, Dion GR, et al. Hemodynamic changes during otolaryngological office-based flexible endoscopic procedures. Ann Otol Rhinol Laryngol 2012;121(11):714-18
Dr. Yanagisawa’s proudest accomplishments were probably his intense involvement in the training of more than 100 ENT residents in the Yale program and his becoming an American citizen (figure 1, D).

The many residents and educators who worked on Dr. Yanagisawa’s many projects, writings, and videos will remember his favorite workshop—his entire home basement—which seemed to store as much information as the National Archives or Library of Congress. Many hours were spent by all to finish projects in that famous basement.
During the more than 50 years of Dr. Yanagisawa’s remarkable teaching accomplishments, there was a “power behind the throne,” his remarkable wife, June. She was always at his side to help when needed and encourage him to proceed. June never complained of the intense work, travel, and teaching schedule (figure 2, A).
Dr. Yanagisawa has been editor of the Rhinoscopic Clinic since its inception in 1993 to the present. We have been fortunate to have been part of his Rhinoscopic Clinic team for many years (figure 2, B). He is a true educator, an outstanding otolaryngologist, and a master of ENT photo and video documentation (figure 2, C). Most importantly, he has been our mentor and friend. Fortunately, gymnastics’ loss many years ago (figure 2, D) became otolaryngology’s gain! Thank you, Eiji! You will always be our mentor! (figure 3)
We wish to thank Linda Zinn for her tireless effort and long-standing friendship over the many years we have worked together. Her expertise and true professionalism are why the Rhinoscopic Clinic has been such a success. We wish her good health and a long, happy retirement!
Laryngopharyngeal reflux (LPR) is an extraesophageal phenomenon that affects the larynx and is encountered frequently by otolaryngologists. Symptoms such as persistent cough, throat clearing, globus sensation, and dysphonia are reported by patients who
experience LPR. A survey performed by the American Broncho-Esophagological Association reported that the signs of LPR on laryngoscopy include vocal fold erythema, posterior commissure hypertrophy, arytenoid erythema, and arytenoid edema.1 Additionally, the
From the Department of Otolaryngology–Head and Neck Surgery, Philadelphia College of Osteopathic Medicine, Philadelphia (Dr. Weinsheim); the Department of Otolaryngology–Head and Neck Surgery, Drexel University College of Medicine, Philadelphia (Dr. Weinsheim and Dr. Sataloff); and student, Philadelphia College of Osteopathic Medicine (Ms. Lesser).

same survey found that flexible fiberoptic laryngoscopy was the test of choice to diagnose LPR, with a dual pH probe with impedance testing as a valuable adjunct.1 Many other symptoms and signs have been reported.2

Treatment of this condition may include a proton pump inhibitor (PPI) with or without concurrent H2 blocker therapy. In 2012, a study by Koufman and Johnston found that the addition of alkaline drinking water (pH 8.8) instantly denatured pepsin, in addition to acting as an acid buffer.3 However, potentially harmful side effects of alkaline water include nausea, vomiting, hand tremor, and confusion.
We report a potential danger to patients who have LPR and use alkaline water as an adjunct treatment. A 65-year-old man presented to our laryngology office for follow-up regarding his LPR and vocal fold granuloma. After initiation of PPI daily, an H2 blocker before bedtime, a low-acid diet, and alkaline water, the patient was found to have a decrease in his reflux finding score from 11 to 6, and his granuloma resolved without surgery.
Rather than purchasing bottled alkaline water, the patient chose to use concentrated alkaline drops obtained over the Internet, which can be added to drinking water to raise the pH to a level that denatures pepsin. The patient reported that there was an accidental spill of the alkaline drops while he was carrying the product in his pocket. Unfortunately, they came in direct contact with his skin and caused a third-degree burn that required serial debridement at a burn facility (figure). This was an unforeseen consequence of recommending the consumption of alkaline water.
We present this case as a warning to otolaryngologists and our patients. Drops used to constitute homemade alkaline water can cause a caustic injury if they are at full strength (not diluted in water) and contact skin. Patients should be cautioned to screw the top on tightly and avoid carrying the drops in a pocket adjacent to skin.
1. Book DT, Rhee JS, Toohill RJ, Smith TL. Perspectives in laryngopharyngeal reflux: An international survey. Laryngoscope 2002;112(8 Pt 1):1399-1406.
2. Sataloff RT, Castell DO, Katz PO, et al. Reflux and other gastroenterologic conditions that may affect the voice. In: Sataloff RT. Professional Voice: The Science and Art of Clinical Care. 4th ed. San Diego: Plural Publishing, Inc.; 2017:907-97.
3. Koufman JA, Johnston N. Potential benefits of pH 8.8 alkaline drinking water as an adjunct in the treatment of reflux disease. Ann Otol Rhinol Laryngol 2012;121(7):431-4.
Abstract
The etiology of Ménière disease (MD) is multifactorial; genetic factors seem to play an important role. The associations between MD and human leukocyte antigen (HLA) status have been studied previously in several populations and have shown that the HLA alleles imparting susceptibility varied. In the present study, we explored HLA status in Taiwanese patients with definitive MD. HLA was typed via polymerase chain reaction, sequence-specific oligonucleotide genotyping in 35 patients with MD diagnosed using the criteria of the American Academy of Otolaryngology–Head and Neck Surgery and 70 unrelated healthy controls. HLA allele association tests were used to evaluate differences in allelic frequencies between the patients and controls. The allelic frequency of HLA-A*11 was significantly greater in MD patients than in controls (52.9 vs. 31.4%, odds ratio: 2.45, 95% confidence interval: 1.4 to 4.4, p = 0.004, p corrected = 0.03). Thus, A*11 may be a useful HLA biomarker in Taiwanese patients with MD. Further larger-scale studies are required.
Introduction
Prosper Ménière first described Ménière disease (MD) in 1861.1 MD is characterized by intermittent episodes
From the Division of Otology, Department of Otolaryngology (Dr. Chan and Dr. Wu), the Graduate institute of Clinical Medical Science (Dr. Chan), and the Department of Nephrology, Kidney Institute (Dr. Lai), Chang Gung Memorial Hospital, Linkou, Taiwan; the College of Medicine, Chang Gung University, Taoyuan, Taiwan (Dr. Chan, Dr. Wu, and Dr. Lai); the Department of Pediatrics, Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan (Dr. Ho); the Fu Jen School of Medicine, Catholic University, New Taipei City, Taiwan (Dr. Ho); and the China Medical University Hospital, Kidney Institute, Taichung, Taiwan (Dr. Lai).
Corresponding author: Ping-Chin Lai, MD, PhD, Department of Nephrology, Kidney Institute, Chang Gung Memorial Hospital, College of Medicine, Chang Gung University, No.5, Fuxing St., Guishan Dist., Taoyuan City 333, Taiwan. Email: georgepclai@gmail.com
Funding/support: This work was funded by Research Grant CMRPG381101 from Chang Gung Memorial Hospital, Linkou, Taiwan.
of vertigo, fluctuating hearing loss, tinnitus, and aural pressure.1 MD is the second most common cause of vertigo in the United States, with the prevalence being approximately 200 per 100,000 (0.2% of the population).2 The pathogenesis may feature disturbance of cochlear fluid homeostasis and/or endolymphatic hydrops of the membranous labyrinth.3
MD may have a multifactorial etiology featuring both a genetic predisposition and environmental factors.4,5 Various etiologies have been suggested, including infection, allergy, an endocrine disturbance, a sympathetic vasomotor disturbance, psychosomatic factors, and disorders of the immune system.6 Most cases of MD are sporadic; a minority of patients have a relevant family history featuring autosomal-dominant MD inheritance.7 In 1979, McCabe introduced the concept of autoimmune inner ear disease, 8 as MD was thought to be associated with such autoimmunity as evidenced by the response to steroid therapy of some MD patients with elevated levels of circulating immune complexes, especially during the active phase.8-10
Relationships between the human leukocyte antigen (HLA) complex and MD have been extensively investigated; however, the candidate HLA genes have varied worldwide (table 1). For example, HLA-Cw7 was more common in British patients,11 DRB1*1602 in Japanese patients,12 and DRB1*09 served as a protective genetic marker in a Beijing Han population.13 Mediterranean patients with bilateral MD are often of HLA DRB1*1101 status.14 In Korean patients with MD, the frequencies of Cw*0303 and Cw*0602 were significantly greater and those of B44 and Cw*0102 were significantly less compared with controls.15
Recently, Dabiri et al found that the HLA-Cw*04 and HLA-Cw*16 alleles were significantly elevated in Iranian patients with both definitive and probable MD.16 However, any such association in Taiwanese patients with MD has not yet been investigated. Therefore, we explored
whether an HLA marker was associated with MD in such a population.
Ethical considerations. All patients gave written informed consent as mandated by the Declaration of Helsinki. The Institutional Review Board of Chang Gung Memorial Hospital and National Taiwan University Hospital approved the study.
Reference Population HLA class I HLA class II
Xenellis et al11
Koyama et al12
Meng et al13
British Cw*7
Japanese DRB1*1602
Northern Chinese DRB1*09
Lopez-Egcamez et al14 Mediterranean DRB1*1101
Yeo et al15
Southern Korean Cw*0303
Cw*0602
B*44
Cw*0162
Dabiri et al16
Present study
Patients. For this case-control study performed between December 2009 and December 2013, DNA samples were obtained from 35 unrelated patients with definitive MD (experimental group) while 70 healthy controls were enrolled at Chang Gung Memorial Hospital, Linkou. All patients with MD were diagnosed using the MD criteria of the American Academy of Otolaryngology–Head and Neck Surgery (AAO–HNS).17 These criteria were two or more definitive spontaneous episodes of vertigo ≥20 minutes in duration; audiometrically documented hearing loss on at least one occasion; tinnitus or aural fullness in the treated ear; and exclusion of other causes such as otosyphilis or acoustic neuroma.
Iranian Cw*04
Cw*16
Taiwanese A*11
Key: HLA = human leukocyte antigen.
All statistical analysis was performed with the aid of the Statistical Package for the Social Sciences software v. 17.0.
DNA extraction and genotyping. Peripheral blood samples (10 ml) from all patients and controls were collected into tubes containing ethylenediamine tetraacetic acid. The buffy coats were lysed and genomic DNA isolated using proteinase K and a QIAamp blood kit (Qiagen; Hilden, Germany) according to the manufacturer's instructions. The HLA-A, B, Cw, DRB1, and DQ loci were typed by polymerase chain reaction amplification followed by sequence-specific oligonucleotide probing. The amplified sequences were hybridized to arrays of immobilized probes.
Statistical analysis. Allele frequency (AF) was calculated using the following formula:
AF (%) = (n/2 N) × 100, where n = the number of subjects with a particular allele and N = the total number of individuals.
Differences in HLA allele frequencies between MD patients and controls were compared using the chi-square or Fisher exact test, as appropriate. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were also calculated. The Bonferroni method was used to derive corrected p values ( p corrected: pc); a difference was considered significant when the pc value was <0.05.
The clinical features of the study group are shown in table 2. We studied 35 adult Taiwanese patients (21 women and 14 men) with a mean age of 53.9 ± 13.6 years and a definitive MD diagnosis. The age at onset was 49.4 ± 12.7 years. Unilateral lesions were present in 33 patients and bilateral lesions in 2 patients. Most lesions (62.9%) were left sided. In terms of hearing status, 19 patients (54.3%) had a hearing loss of 25 to 40 dB, 12 (34.3%) had a loss of >40 to 70 dB, and 4 (11.4%) had a loss >70 dB. The hearing losses of the less affected ears of the 2 patients with bilateral MD were both <25 dB.
The caloric test was run on 32 patients, of whom 22 had evidence of canal paralysis (R/L = 8/14) and 10 did not. Furthermore, the extent of functional disability as reported by the self-administered AAO–HNS instrument was level I in 2 patients, level II in 5, level III in 10, level IV in 10, level V in 3, and level VI in 1. Four patients could not select sentences defining their conditions.
A total of 8 HLA-A, 13 HLA-B, 9 HLA-Cw, 12 HLADRB1, and 6 HLA-DQ alleles were typed. The prevalence of HLA-A*11 was significantly greater in MD patients compared with controls (37/70 [52.9%] vs. 44/140 [31.4%], OR: 2.45, 95% CI: 1.4 to 4.4, p = 0.004, pc = 0.03). No other allele frequency differed significantly between the groups (data available in table form upon request from the corresponding author).
being the natural ligand for the inhibitory KIR3DL2 receptor.18 Several epitopes recognized by cytotoxic T lymphocytes are HLA-A11–restricted.
Infections and immune conditions associated with HLA-A11 expression have been investigated; these include familial otosclerosis, pulmonary tuberculosis, leprosy, cytomegalovirus infection with epilepsy, osteosarcoma, antidepressant-induced hepatitis, steroid-responsive nephrotic syndrome, and diffuse panbronchiolitis.19-26 It has been proposed that immunologic responses are initiated under certain conditions by general or unique HLA determinants in susceptible A11 carriers.27
The presence of certain HLA antigens renders patients susceptible to MD; ethnic differences in HLA-associated genes may partially explain the variations in MD incidence among populations. However, HLA genetic differences are not the only relevant factors. Contributions made by unidentified genetic, multigenetic, environmental, and infectious factors also must be considered. In addition, patients of the same ethnicity living in different regions may vary in terms of the MD- associated HLA gene. For example, HLA-B54 and HLA-A11 were positively associated with diffuse panbronchiolitis in Northern and Southern Chinese, respectively.26 Therefore, it is reasonable that DRB1*09 should be protective in a Beijing Han population (Northern Chinese) with MD but that A*11 should increase MD susceptibility in a Taiwanese population (East-Southern Chinese).
In this case-control study, we found that A11 was strongly associated with definitive MD in ethnic Chinese living in Taiwan. This HLA marker has never been reported in other MD populations. Various autoimmune diseases, including MD, are associated with particular HLA class I and/or class II alleles. British,11 Korean,14 Iranian,16 and (now) Taiwanese studies have revealed that HLA class I antigens are associated with MD. However, HLA class II antigens were associated with MD in Japanese,12 Northern Chinese13 (a Beijing Han population), and Mediterranean MD patients.15 Therefore, ethnic differences in such associations are in play. The differential distributions of relevant HLA class I or II loci may yield insights into the immune reaction or inflammatory response associated with MD.
A*11, an HLA class I molecule, is encoded between the HLA-A and HLA-B loci on chromosome 6p21.3 and has long been known to exert specific biologic functions,
The effects of genetic predisposition and geographic background on MD development in various ethnic Chinese groups require further study. We found a positive association between HLA-A*11 and MD in ethnic Chinese of Taiwan, which is unlike what has been noted in other populations. We suggest that the HLA class I antigen may play an immunologic role in MD pathogenesis in Taiwanese patients. Our sample size was relatively small and our study, thus, underpowered. Further larger scale population studies are required to confirm our findings.
This study was supported by grants from CMRPG381101 from Chang Gung Memorial Hospital, Linkou, Taiwan.
1. Ménière P. Maladies de l'oreille interne offrant des symptômes de la congestion cérébral apoplectiforme. Gaz Med de Paris 1861;16:88.
2. Wladislabosky-Waserman P, Facer GW, Mokri B, Kurland LT. Ménière’s disease: A 30-year epidemiologic and clinical study in Rochester, Mn, 1951-1980. Laryngoscope 1984;94(8):1098–102.
3. Hallpike CS, Cairns H. Observations on the pathology of Ménière’s syndrome: (Section of Otology). Proc R Soc Med 1938;31(11):1317-36.
Abstract
Endoscopic technology is widely used in rhinology and anterior skull base surgery, but it has been less quickly incorporated into otologic practice. The design of the instrumentation forces surgeons to work one-handed and limits depth perception. Nevertheless, endoscopy also offers wide fields of view and access to spaces that are typically difficult to visualize. Its advantages have broadened the type and extent of operations that can be performed via the ear canal. We describe a method of endoscopic resection of glomus tympanicum tumors in 5 adults who had undergone endoscopic or endoscopyassisted resection. A successful resection was achieved in all patients—exclusively via the ear canal in 4 of them. A KTP laser was used to address the tumor’s vascular supply. Attachment of a neonatal feeding tube to the endoscope for use as a suction catheter obviated the need to repeatedly switch instruments while using the laser. At a minimum of 12 months of follow-up, all patients were free of recurrence. Postoperative audiometry detected no significant adverse hearing outcomes in any patient. We conclude that the minimally invasive endoscopic transcanal approach is a feasible technique for addressing middle ear tumors. We have also developed a method that allows surgeons constant use of the KTP laser to resect a glomus tympanicum tumor.
Introduction
Since its introduction to otologic practice in the 1960s,1 endoscopic instrumentation has become increasingly popular in the management of middle ear diseases. Proponents of the endoscopic technique favor the wide surgical view it provides, its minimally invasive nature, and the opportunity it provides to maneuver into spaces that are typically difficult to visualize. Fur-
From the Department of Otolaryngology–Head and Neck Surgery, Stanford University School of Medicine, Stanford, Calif.
Corresponding author: Julia E. Noel, MD, Department of Otolaryngology–Head and Neck Surgery, Stanford University School of Medicine, 801 Welch Rd., Stanford, CA 94035. Email: jtomlin2@stanford.edu
thermore, adding high-definition imaging to the procedure has transformed the applications of endoscopic surgery, making it a viable and comparable alternative to traditional microscopic techniques.
While endoscopy is ubiquitous in sinus surgery, its incorporation into clinical otologic practice has been more gradual. The design of the instrumentation forces surgeons to work one-handed and limits depth perception. The diameter of the endoscope often can preclude fine manipulations through the ear canal, and the endoscope poses a risk of thermal injury to the canal skin. Endoscopy is not routinely introduced during training, since excellent outcomes are being achieved with traditional microscopic techniques.
Endoscopic surgery has been applied to a number of otologic operations, including tympanoplasty, ossiculoplasty, stapedotomy, cholesteatoma surgery, and cochlear implantation.2-6 However, few authors have described the application of this technique to address middle ear lesions, including glomus tympanicum tumors.7 Glomus tympanicum tumors are the most common of the benign middle ear lesions.8
Middle ear paragangliomas are slowly growing, benign vascular lesions that arise from the tympanic plexus on the cochlear promontory.8 They have historically been addressed via a microscopic approach through either the canal or a postauricular incision.9 Transcanal endoscopic ear surgery offers a novel and often more conservative approach to the middle ear and temporal bone. It provides surgeons with a wide field of illumination and more complete visualization of the lesion.
We describe the excision of glomus tympanicum tumors via an endoscopic transcanal technique in 5 patients. Tumor excision was assisted by KTP laser treatment and a novel smoke-management system.
Patients. During 2015 and 2016, the senior author (H.S.) operated on 5 patients—3 men and 2 women, aged 38 to 77 years (table)—who had a glomus tympanicum tumor (figure 1). Preoperatively, all patients
underwent either computed tomography (CT) of the temporal bone or magnetic resonance imaging (MRI) of the skull base. In 4 patients, imaging demonstrated the presence of a Fisch type A tumor that was limited to the middle ear cleft; the remaining patient had a Fisch type B tumor that diffusely involved the tympanomastoid complex. Preoperative audiometry also was obtained in all cases.
Surgical methods. All operations were performed with general anesthesia. A 3.0-m (length: 14 cm) and a 2.7-m (18 cm) Hopkins 0 ° telescope was used for surgical excision, followed by use of a 3.0-m 30 ° Hopkins endoscope for inspection and confirmation of complete removal. A high-definition camera head and monitor facilitated image projection. The light intensity was set no higher than 60% to avoid thermal injury to the canal and middle ear structures.
The ear was prepped and draped sterilely; it was not necessary to shave the postauricular hair. Infiltration with 2% lidocaine with 1:100,000 epinephrine was performed at the vascular strip and inferior canal until blanching was seen at the tympanic membrane. The radial canal incisions were made at 12 and 4 o’clock to ensure adequate exposure of the lesion on the promontory in the anterior inferior quadrant. A tympanomeatal flap was raised, and the tumor was exposed (figure 2, A). The middle ear was inspected, and the extent of the lesion noted. A KTP laser (Iridex; Mountain View, Calif.) was used on the ultrapulse setting at 4 W to address the base of the lesion where the vascular supply was evident (figure 2, B).

It is critical to consider the location of the lesion in relation to the ossicles and tympanomeatal flap, both of which are prone to injury during this step. A 3.5-Fr neonatal feeding tube was affixed to the 2.7-mm endoscope with a Steri-Strip to allow for simultaneous
visualization and suctioning (figure 3).
Once the vessels had been adequately addressed, the lesion was grasped with a cupped forceps and gently avulsed from the promontory. Cottonoid pledgets soaked in epinephrine were applied to halt any additional bleeding, which was minimal. Inspection was performed with the 30 ° endoscope to ensure that no other lesion or abnormal pathology was present. Several pieces of Gelfoam soaked in ofloxacin were placed in the middle ear to support the tympanic membrane.
The tympanomeatal flap was unrolled from the anterior canal and replaced in its preoperative position. The canal was filled with Tisseel, and a dry cotton ball was placed in the concha.
All procedures were completed on an outpatient basis with limited blood loss (≤25 ml). There were no intraor postoperative complications. In 4 cases, total resection was achieved endoscopically without the need for a postauricular incision. For the patient with the Fisch type B tumor, we had to use a combined endoscopic and postauricular approach because of the extent of disease.
During a follow-up of 12 to 38 months, all patients exhibited clear middle ears with no evidence of tumor on endoscopic otoscopy. There was no significant change from preoperative baseline in pure-tone average or speech discrimination score in any patient.
Endoscopic instrumentation has facilitated the evaluation of previously challenging spaces and expanded the types and extent of procedures that can be performed via an exclusively transcanal approach. Its surgical application has been described in a number of pathologies, most notably cholesteatoma, tympanic membrane perforation, ossicular chain disruption/ fixation, and cochlear implantation.2,4,5,10,11 Surgical outcomes are fundamental to the comparison between endoscopic and microscopic ear surgery.
Perhaps the best-described application for endoscopic ear surgery has been cholesteatoma removal. With regard to disease eradication, a systematic review by Presutti et al found a comparable rate of residual and recurrent cholesteatoma between cases treated entirely endoscopically or with endoscopic assistance (9.3%) and cases treated with classic microscopic surgery.12 In other studies, the incidence of residual cholesteatoma


discovered on endoscopy after microscope-only tympanomastoidectomy has ranged between 17 and 31%.13-15
In a study directly comparing the two techniques in 59 pediatric ears, Marchioni et al found that endoscopic visualization facilitated a lower rate of residual and recurrent cholesteatoma (19.3 and 12.9%, respectively) than did microscopic canal-wall-up mastoidectomy (34.4 and 17.2%, respectively).3 Additionally, the ossicular chain was preserved in 42% of the endoscopic cases, compared with only 10% of the microscopic cases. The mean improvement in pre- and postoperative pure-tone averages was similar in the two groups. Marchioni et al first reported the application of endoscopic instrumentation to middle ear tumors in 2013.16 They described the resection of paragangliomas, carcinoid tumors, and osteomas from the middle ear. In the absence of significant contraindications, surgical removal is the most effective treatment for these lesions. Stereotactic radiosurgery or just simple observation may be appropriate for patients who are not amenable to or who are at too high a risk for general anesthesia.9,17 For smaller tumors limited to the mesotympanum, a transcanal microscopic procedure has traditionally been employed. However, larger lesions that extend into the protympanum or hypotympanum may require a postauricular approach.18 As reported by Killeen et al, the endoscope provides superior visualization of these spaces and may, in some instances, allow surgeons to avoid an incision.19
One of the challenges reported with endoscopic ear surgery that is particularly pertinent to these tumors is that surgeons must operate with only one hand, which in this specific context limits their ability to suction blood and smoke during dissection. We have proposed a solution to this, which involves the attachment of a neonatal 3.5-Fr feeding tube to the endoscope with a Steri-Strip. This has obviated the need to exchange instruments frequently, it has improved visibility, and it has shortened operative time. Furthermore, although limited by a lack of depth perception, endoscopic approaches do afford a wider view that can often facilitate resection while avoiding a postauricular incision.
In our series, 3 of the 5 tumors that had extended into the protympanum were visualized entirely and removed safely. Clearly, an endoscopic approach is not appropriate for larger tumors, and discretion must be used to determine the appropriateness of technique in each case.
In conclusion, surgical resection is the preferred treatment for paragangliomas. In our study, total resection was successful in all 5 patients who underwent endoscopic or endoscopy-assisted resection of their paraganglioma. We observed no evidence of recurrence

on follow-up. The treatment of paragangliomas of the middle ear is but one illustration of the expanding application of endoscopic instrumentation in otology.
References
1. Mer SB, Derbyshire AJ, Brushenko A, Pontarelli DA. Fiberoptic endotoscopes for examining the middle ear. Arch Otolaryngol 1967;85(4):387-93.
2. Alicandri-Ciufelli M, Marchioni D, Kakehata S, et al. Endoscopic management of attic cholesteatoma: Long-term results. Otolaryngol Clin North Am 2016;49(5):1265-70.
3. Marchioni D, Soloperto D, Rubini A, et al. Endoscopic exclusive transcanal approach to the tympanic cavity cholesteatoma in pediatric patients: Our experience. Int J Pediatr Otorhinolaryngol 2015;79(3):316-22.
4. Hunter JB, O’Connell BP, Rivas A. Endoscopic techniques in tympanoplasty and stapes surgery. Curr Opin Otolaryngol Head Neck Surg 2016;24(5):388-94.
5. Orhan KS, Polat B, Çelik M, et al. Endoscopic-assisted cochlear implantation: A case series. J Int Adv Otol 2016;12(3):337-40.
6. Yong M, Mijovic T, Lea J. Endoscopic ear surgery in Canada: A cross-sectional study. J Otolaryngol Head Neck Surg 2016;45:4.
7. Isaacson B, Nogueira JF. Endoscopic management of middle ear and temporal bone lesions. Otolaryngol Clin North Am 2016;49(5):1205-14.
8. Carlson ML, Sweeney AD, Pelosi S, et al. Glomus tympanicum: A review of 115 cases over 4 decades. Otolaryngol Neck Surg 2015;152(1):136-42.
9. Sweeney AD, Carlson ML, Wanna GB, Bennett ML. Glomus tympanicum tumors. Otolaryngol Clin North Am 2015; 48(2):293-304.
10. Kiringoda R, Kozin ED, Lee DJ. Outcomes in endoscopic ear surgery. Otolaryngol Clin North Am 2016;49(5):1271-90.
11. Marchioni D, Alicandri-Ciufelli M, Molteni G, et al. Endoscopic tympanoplasty in patients with attic retraction pockets. Laryngoscope 2010;120(9):1847-55.
12. Presutti L, Gioacchini FM, Alicandri-Ciufelli M, et al. Results of endoscopic middle ear surgery for cholesteatoma treatment: A systematic review. Acta Otorhinolaryngol Ital 2014;34(3):153-7.
13. Good GM, Isaacson G. Otoendoscopy for improved pediatric cholesteatoma removal. Ann Otol Rhinol Laryngol 1999;108(9):893-6.
14. Sarcu D, Isaacson G. Long-term results of endoscopically assisted pediatric cholesteatoma surgery. Otolaryngol Head Neck Surg 2016;154(3):535-9.
15. Farahani F, Shariatpanahi E, Jahanshahi J, Poorolajal J. Diagnostic performance of endoscopic and microscopic procedures for identifying different middle ear structures and remaining disease in patients with chronic otitis media: A prospective cohort study. PLoS One 2015;10(7):e0132890.
16. Marchioni D, Alicandri-Ciufelli M, Gioacchini FM, et al. Transcanal endoscopic treatment of benign middle ear neoplasms. Eur Arch Otorhinolaryngol 2013;270(12):2997-3004.
17. Semaan MT, Megerian CA. Current assessment and management of glomus tumors. Curr Opin Otolaryngol Head Neck Surg 2008;16(5):420-6.
18. Alaani A, Chavda SV, Irving RM. The crucial role of imaging in determining the approach to glomus tympanicum tumours. Eur Arch Otorhinolaryngol 2009;266(6):827-31.
19. Killeen DE, Wick CC, Hunter JB, et al. Endoscopic management of middle ear paragangliomas: A case series. Otol Neurotol 2017;38(3):408-15.
Continued from page 398
4. Arweiler DJ, Jahnke K, Grosse-Wilde H. Ménière’s disease as an autosome dominant hereditary disease [in German]. Laryngorhinootologie 1995;74(8):512-5.
5. Fung K, Xie Y, Hall SF, et al. Genetic basis of familial Ménière’s disease. J Otolaryngol 2002;31(1):1-4.
6. Wassef M. Pathology of the ear. Ann Pathol 2009;29(4):347-60.
7. Morrison AW, Mowbray JF, Williamson R, et al. On genetic and environmental factors in Ménière’s disease. Am J Otol 1994;15(1):35-9.
8. McCabe BF. Autoimmune sensorineural hearing loss. 1979. Ann Otol Rhinol Laryngol 2004;113(7):526-30.
9. Brookes GB. Circulating immune complexes in Ménière’s disease. Arch Otolaryngol Head Neck Surg 1986;112(5):536-40.
10. Derebery MJ, Rao VS, Siglock TJ, et al. Ménière’s disease: An immune complex-mediated illness? Laryngoscope 1991;101(3):225-9.
11. Xenellis J, Morrison AW, McClowskey D, Festenstein H. HLA antigens in the pathogenesis of Ménière’s disease. J Laryngol Otol 1986;100(1):21–4.
12. Koyama S, Mitsuishi Y, Bibee K, et al. HLA associations with Ménière’s disease. Acta Otolaryngol 1993;113(5):575–8.
13. Meng X, Lian N, Yang Z, et al. An association study of histocompatibility leukocyte antigen-class II with Ménière’s disease [in Chinese]. Zhonghua Er Bi Yan Hou Ke Za Zhi 2001;36(1):25-7.
14. Lopez-Escamez JA, Vilchez JR, Soto-Varela A, et al. HLADRB1*1101 allele may be associated with bilateral Ménière’s disease in southern European population. Otol Neurotol 2007;28(7):891-5.
15. Yeo SW, Park SN, Jeon EJ, et al. Influence of human leukocyte antigen in the pathogenesis of Ménière’s disease in the South Korean population. Acta Otolaryngol 2002;122(8):851-6.
16. Dabiri S, Ghadimi F, Firouzifar M, et al. HLA-Cw allele frequency in definite Ménière’s disease compared to probable Meniere’s disease and healthy controls in an Iranian sample. Iran J Otorhinolaryngol 2016;28(87):262–6.
17. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg 1995;113(3):181-5.
18. Pende D, Biassoni R, Cantoni C, et al. The natural killer cell receptor specific for HLA-A allotypes: A novel member of the p58/p70 family of inhibitory receptors that is characterized by three immunoglobulin-like domains and is expressed as a 140kD disulphide-linked dimer. J Exp Med 1996;184(2):505–18.
19. Gregoriadis S, Zervas J, Varletzidis E, et al. HLA antigens and otosclerosis. A possible new genetic factor. Arch Otolaryngol 1982;108(12):769–71.
20. Xu XP, Li SB, Wang CY, Li QH. Study on the association of HLA with pulmonary tuberculosis. Immunol Invest 1986;15(4):327–32.
21. Kim SJ, Choi IH, Dahlberg S, et al. HLA and leprosy in Koreans. Tissue Antigens 1987;29(3):146–53.
22. Iannetti P, Morellini M, Raucci U, Cappellacci S. HLA antigens, epilepsy and cytomegalovirus infection. Brain Dev 1988;10(4):256–8.
23. Barona P, Sierrasesúmaga L, Antillón F, Villa-Elízaga I. Study of HLA antigens in patients with osteosarcoma. Hum Hered 1993;43(5):311–4.
24. Berson A, Fréneaux E, Larrey D, et al. Possible role of HLA in hepatotoxicity. An exploratory study in 71 patients with druginduced idiosyncratic hepatitis. J Hepatol 1994;20(3):336–42.
25. Cheung W, Ren EC, Chan SH, et al. Increased HLA- A*11 in Chinese children with steroid-responsive nephrotic syndrome. Pediatr Nephrol 2002;17(3):212-6.
26. Chen Y, Kang J, Wu M, et al. Differential association between HLA and diffuse panbronchiolitis in Northern and Southern Chinese. Intern Med 2012;51(3):271-6.
27. Makhadatze NJ, Sanches-Llamozas P, Franco MT, Layrisse Z. Strong association between major histocompatibility complex class I antigens and immune aberrations among healthy Venezuelans. Hum Immunol 1995;42(3):189–94.

Abstract
Recurrence of sinonasal disease can be caused by many factors, including lateralization of the middle turbinate as a complication of endoscopic sinus surgery (ESS). Different ESS procedures have been tried to prevent this complication. We conducted a prospective study to determine if medialization is an effective means of lateralizing the middle turbinate. Our study population was made up of 142 adults who underwent ESS from July 2013 through December 2014. A total of 235 sides were operated on; the middle turbinate was medialized in 90 patients (145 sides) and not medialized in 52 patients (90 sides). Follow-up ranged from 6 to 12 months. At 3 months postoperatively, the middle turbinate position was satisfactory on 210 sides (89%) and remained lateralized on the other 25 (11%). Among the latter, the turbinate obstructed the middle meatus in 16 patients and did not obstruct it in 9 patients. The 16 patients with obstruction required revision in the form of either a partial or complete turbinectomy, depending on the severity of the scarring. No complications were associated with middle turbinate medialization. We conclude that medialization middle turbinoplasty is an effective solution to a problem faced by many sinus surgeons. It is safe, quick, and easy to perform, and it is associated with minimal morbidity without adding to cost. It provides postoperative access to the ethmoid sinuses for debridement, and it reduces the risk of middle meatal stricture.
Introduction
One of the primary aims of endoscopic sinus surgery (ESS) is to enlarge the sinus ostia to facilitate sinus drainage and aeration and thereby prevent future sinus infections. However, lateral synechia formation between the middle turbinate and the lateral nasal wall is
From the Department of Otolaryngology–Head and Neck Surgery, Tufts Medical Center, Boston.
Corresponding author: Elie Rebeiz, MD, FACS, Department of Otolaryngology–Head and Neck Surgery, Tufts University School of Medicine, Tufts Medical Center, 800 Washington St., Box 850, Boston, MA 02111. Email: erebeiz@tuftsmedicalcenter.org
a well-documented complication of ESS, having been reported in 1 to 43% of cases.1,2
Several factors contribute to lateralization of the middle turbinate with or without synechia formation: (1) trauma to the lateral mucosal surface of the middle turbinate, (2) resection of the horizontal portion of the basal lamella, (3) improper manipulation of the middle turbinate resulting in a floppy turbinate, (4) severe polyposis surrounding the middle turbinate, (5) postoperative swelling, (6) inadequate postoperative debridement, and (7) improper packing of the nasal airway after surgery.3
Scar tissue formation (1) can lead to outflow tract obstruction from the ethmoid, frontal, and maxillary cavities, (2) prevents adequate sinus debridement after surgery, (3) results in poor drainage and aeration, and (4) possibly leads to the need for revision surgery.
In 1999, Bolger et al published a short communication entitled, “A Targeted Problem and Its Solution,” in which they described their technique for creating a controlled synechia between the middle turbinate and the nasal septum to prevent lateralization of the middle turbinate.3 Since then, many modifications have been described to address the issue of middle turbinate lateralization and synechia formation with the lateral wall.4-11 These include partial turbinectomy, middle turbinate suture conchopexy, and the placement of septal flaps, metal clips, bioabsorbable implants, and middle meatal spacers.
In this article, we describe our experience with the middle turbinate medialization technique described by Bolger et al3 on a cohort of patients undergoing ESS, and we compare our findings with those of a control group.
Patients. Our study population was made up of 142 adults—70 men and 72 women (mean age: 52.3 yr)— who had not responded to medical therapy for chronic rhinosinusitis and who had subsequently undergone ESS (table 1). Chronic rhinosinusitis was defined as a symptomatic inflammation of the sinuses for at least 3 months. Patients with previous ESS, a concha bullosa,
For the treatment of AOMT in pediatric patients due to S. aureus, S. pneumoniae, H. influenzae, M. catarrhalis, and P. aeruginosa.
The first and only antibiotic/steroid combination ear drop in single-dose vials
• Manufactured using blow-fill-seal technology— each vial is formed, filled, and sealed in a continuous, automated, sterile operation2,3

• Technology minimizes human intervention in the fill/finish process3

• Single-use vials contain 1 premeasured dose each—dose BID/7 days4












• No drop counting. No mixing or shaking required4



• Demonstrated efficacy and safety in 2 clinical trials1,5 Order
OTOVEL® (ciprofloxacin and fluocinolone acetonide) is indicated for the treatment of acute otitis media with tympanostomy tubes (AOMT) in pediatric patients (aged 6 months and older) due to S. aureus, S. pneumoniae, H. influenzae, M. catarrhalis, and P. aeruginosa.
Contraindications
OTOVEL is contraindicated in:





• Patients with known hypersensitivity to fluocinolone acetonide or other corticosteroids, ciprofloxacin or other quinolones, or to any other component of OTOVEL.
• Viral infections of the external ear canal, including varicella and herpes simplex infections and fungal otic infections.
The following Warnings and Precautions have been associated with OTOVEL: hypersensitivity reactions, potential for microbial overgrowth with prolonged use, and continued or recurrent otorrhea.
The most common adverse reactions are otorrhea, excessive granulation tissue, ear infection, ear pruritis, tympanic membrane disorder, auricular swelling, and balance disorder. For additional Important Safety Information, please see Brief Summary of Prescribing Information on adjacent page, and full Prescribing Information available at www.otovel.com.
References: 1. Otovel [package insert]. Atlanta, GA: Arbor Pharmaceuticals, LLC. 2016. 2. Data on file. Arbor Pharmaceuticals, LLC. 3. Guidance for industry: sterile drug products produced by aseptic processing—current good manufacturing practice. Food and Drug Administration. https://www.fda.gov/downloads/Drugs/Guidances/ucm070342.pdf. Published September 2004. Accessed March 15, 2018. 4. Orange Book: Approved drug products with therapeutic equivalence evaluations. US Food and Drug Administration. https://www.accessdata.fda.gov/scripts/ cder/ob/default.cfm. Updated May 17, 2013. Accessed July 15, 2016. 5. Spektor Z, Pumarola P, Ismail K, et al. Efficacy and safety of ciprofloxacin plus fluocinolone in otitis media with tympanostomy tubes in pediatric patients: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg 2017;143(4):341-349.
Otovel is a registered trademark of Laboratorios Salvat, S.A. with the US Patent and Trademark Office and under license by Arbor Pharmaceuticals, LLC. Trademarks are the property of their
OTOVEL® (ciprofloxacin and fluocinolone acetonide) otic solution
Brief Summary of Prescribing Information
1 INDICATIONS AND USAGE
OTOVEL is indicated for the treatment of acute otitis media with tympanostomy tubes (AOMT) in pediatric patients (aged 6 months and older) due to Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Pseudomonas aeruginosa
2 DOSAGE AND ADMINISTRATION
• OTOVEL is for otic use only. It is not for ophthalmic use, or for injection.
The recommended dosage regimen is as follows:
• Instill the contents of one single-dose vial 0.25 mL into the affected ear canal twice daily (approximately every 12 hours) for 7 days. Use this dosing for patients aged 6 months of age and older.
• Warm the solution by holding the vial in the hand for 1 to 2 minutes. This is to avoid dizziness, which may result from the instillation of a cold solution into the ear canal.
• The patient should lie with the affected ear upward, and then instill the medication.
• Pump the tragus 4 times by pushing inward to facilitate penetration of the medication into the middle ear.
• Maintain this position for 1 minute. Repeat, if necessary, for the opposite ear [see Instructions for Use]
3 DOSAGE FORMS AND STRENGTHS
Otic Solution: Each single-dose vial of OTOVEL (ciprofloxacin 0.3 % and fluocinolone acetonide 0.025 %) delivers 0.25 mL of solution equivalent to ciprofloxacin 0.75 mg and fluocinolone acetonide 0.0625 mg.
4 CONTRAINDICATIONS
OTOVEL is contraindicated in:
• Patients with known hypersensitivity to fluocinolone acetonide or other corticosteroids, ciprofloxacin or other quinolones, or to any other components of OTOVEL.
• Viral infections of the external ear canal, including varicella and herpes simplex infections and fungal otic infections.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
OTOVEL should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity. Serious and occasionally fatal hypersensitivity (anaphylactic) reactions, some following the first dose, have been reported in patients receiving systemic quinolones. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, angioedema (including laryngeal, pharyngeal or facial edema), airway obstruction, dyspnea, urticaria and itching. Serious acute hypersensitivity reactions may require immediate emergency treatment.
5.2 Potential for Microbial Overgrowth with Prolonged Use
Prolonged use of OTOVEL may result in overgrowth of non-susceptible bacteria and fungi. If the infection is not improved after one week of treatment, cultures should be obtained to guide further treatment. If such infections occur, discontinue use and institute alternative therapy.
5.3 Continued or Recurrent Otorrhea
If otorrhea persists after a full course of therapy, or if two or more episodes of otorrhea occur within 6 months, further evaluation is recommended to exclude an underlying condition such as cholesteatoma, foreign body, or a tumor.
6 ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling: Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials, 224 patients with AOMT were treated with OTOVEL for a median duration of 7 days. All the patients received at least one dose of OTOVEL. There were 220 patients who received at least one dose of ciprofloxacin (CIPRO) and 213 patients received at least one dose of fluocinolone acetonide (FLUO). The most common adverse reactions that occurred in 1 or more patients are as follows:
1Selected adverse reactions that occurred in ≥ 1 patient in the OTOVEL group derived from all reported adverse events that could be related to the study drug or the drug class.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ciprofloxacin and fluocinolone acetonide otic solution, 0.3% / 0.025% outside the US. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
• Immune system disorders: allergic reaction.
• Infections and infestations: candidiasis.
• Nervous system disorders: dysgeusia, paresthesia (tingling in ears), dizziness, headache.
• Ear and labyrinth disorders: ear discomfort, hypoacusis, tinnitus, ear congestion.
• Vascular disorders: flushing.
• Skin and subcutaneous tissue disorders: skin exfoliation.
• Injury, poisoning and procedural complications: device occlusion (tympanostomy tube obstruction).
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy Risk Summary
OTOVEL is negligibly absorbed following otic administration and maternal use is not expected to result in fetal exposure to ciprofloxacin and fluocinolone acetonide (12.3)].
8.2 Lactation Risk Summary
OTOVEL is negligibly absorbed by the mother following otic administration and breastfeeding is not expected to result in exposure of the infant to ciprofloxacin and fluocinolone acetonide.
8.4 Pediatric Use
OTOVEL has been studied in patients as young as 6 months in adequate and wellcontrolled clinical trials. No major differences in safety and effectiveness have been observed between adult and pediatric patients.
8.5 Geriatric Use
Clinical studies of OTOVEL did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
10 OVERDOSAGE
Due to the characteristics of this preparation, no toxic effects are to be expected with an otic overdose of OTOVEL.
Distributed by: Arbor Pharmaceuticals, LLC Atlanta, GA 30328
Under license of Laboratorios SALVAT, S.A.
OTOVEL is a registered trademark of Laboratorios SALVAT, S.A.
U.S. Patent No: 8,932,610
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
For more detailed information, see the full prescribing information for Otovel at www.otovel.com or contact Arbor Pharmaceuticals, LLC at 1-866-516-4950.
environmental allergies, asthma, and aspirin intolerance were included in the study. We did not include any patients who were younger than 18 years, who were lost to follow-up, and who had simultaneous inferior turbinate surgery, septoplasty, or other nasal surgery.
The diagnosis of chronic rhinosinusitis, the presence of unilateral or bilateral sinusitis, and the indications for surgery were confirmed by computed tomography and endoscopic examination in all patients. The most common symptoms were nasal congestion (91% of cases), headache (53%), postnasal drip (35%), nasal discharge (32%), and olfactory disturbance (8%).
Before December 2013, surgeons at our institution did not perform medialization turbinoplasty consistently. Of the 142 patients in this study, 52 had undergone ESS from July through December 2013; none had undergone turbinoplasty. Their ESS records were reviewed retrospectively, and these patients served as our control group. Of the 52 controls, 38 underwent a bilateral procedure and 14 a unilateral procedure, for a total of 90 operated sides.
Our turbinoplasty group originally included 94 patients. They were operated on from January though December 2014. Their ESS was performed bilaterally in 70 patients and unilaterally in 24 patients, for a total of 164 sides. Four of the 94 patients were lost to follow-up, leaving us with a cohort of 90 patients (156 sides). In addition, turbinoplasty was not performed in another 11 sides because the turbinate was partially or completely absent as a result of previous surgery or other causes such as excessive scarring where it was deemed necessary to resect the middle turbinate. This resulted in a total of 145 turbinoplasty sides.
Surgical technique. At our hospital, ESS begins with packing of the involved side of the nose and middle meatus with oxymetazoline packs for a few minutes. The packs are then removed, and lidocaine 1% with epinephrine 1:200,000 is injected into the uncinate process and root of the middle turbinate. In some cases, injection of epinephrine is not performed—for example, when a patient is hypertensive and/or older than 70 years or when the anesthesiologist requests that it not be done.
Before the initiation of the actual sinus surgery, a small upbiting Thrubite forceps is used to remove 2 to 3 mm of mucosa from the medial surface of the middle turbinate and the adjacent nasal septum (figure 1). Sinus packs are then placed lateral to the middle turbinate. If a microdebrider is used, then the mucosal surfaces are denuded in the same location with the blade of the microdebrider. The middle turbinate is immediately pushed medially with a Freer elevator, which allows the raw surfaces to come into contact with each other; the elevator is held in position for 5 to 10 seconds.
During the remainder of the procedure, we try not to manipulate the middle turbinate but to keep it medialized. When a concha bullosa is present, its medial portion is resected along with the opposing 3 mm of the nasal septal mucosa. During the rest of the procedure, we try to keep the middle turbinate medialized.

The uncinate process is then identified and medialized with a Cottle elevator, and an uncinectomy is performed with a straight Thrubite forceps. The surgery is then performed, and the sinuses are opened as indicated by the patient’s disease. In general, middle turbinate medialization takes only a few seconds. It is typically performed at the beginning of the procedure, but it can be performed at any time during surgery.
At the conclusion of the ESS, Merocel packs are inserted in the middle meatus and allowed to expand via irrigation, thus maintaining the middle turbinate in a medialized position and allowing it to come into contact with the nasal septum. The packs are removed in the office 4 to 5 days later. Patients are administered an antibiotic while the packs are in place.
Postoperative outcomes and measures. Our primary outcomes measures were the postoperative endoscopic position of the middle turbinate and the presence or
absence of lateral synechia formation. Postoperative endoscopic examinations were performed on all patients. Postoperative visits and endoscopic examinations were done at 5 days, 2 weeks, 3 weeks, 3 months, and 6 months after ESS. Both groups were followed for 6 to 12 months.


At each postoperative visit, patients were assessed for middle turbinate positioning, synechia formation, the ease of debriding the sinus cavities, and recurrence of symptoms. The position of the middle turbinate was classified as either medial (touching the nasal septum), neutral (midway between the septum and lateral wall), or lateral (touching the lateral wall or preventing adequate visualization of the middle meatus). Symptoms or the lack thereof, including any changes in sense of smell, were recorded.
Ethical considerations. The study protocol was approved by the Institutional Review Board of the Tufts University School of Medicine.
Of the 146 patients in the entire study before the loss of the 4 patients to follow-up, 114 (78%) reported significant improvement after surgery and 21 (14%) reported some improvement.
In the final study population, the position of the middle turbinate was satisfactory (i.e., in the medial or neutral position) on 210 sides (89%) and relateralized on 25 (11%). In 9 of those 25 sides, the middle turbinate lateralized without an obstruction of the middle meatus or a recurrence of symptoms; in the other 16 cases, the middle turbinate lateralized and did cause obstruction or opacification of the middle meatus, and these cases warranted a partial or complete revision turbinectomy, depending on the severity of the scarring.
At the 3-month follow-up, the rate of middle turbinate medialization was significantly higher in the turbinoplasty group than in the nonturbinoplasty group—68 vs. 19% (p < 0.001) (table 2). In the turbinoplasty group, 99 sides demonstrated middle turbinate
medialization that featured a well-defined synechia between the septum and the middle turbinate (figure 2).
The rate of lateral displacement with synechia formation was just slightly higher in nonturbinoplasty group—13 vs. 9% (p = 0.29) (table 2).
Complications were observed in 5 patients. They included postoperative bleeding in 3, a cerebrospinal fluid (CSF) leak in 1, and periorbital ecchymosis in 1. The bleeding was controlled with packing in 2 patients and with surgical cautery of the septal branch of the sphenopalatine artery in the other. The CSF leak was repaired immediately with a septal flap. The patient with periorbital ecchymosis did not exhibit any ocular findings or visual changes. None of the complications was attributable to middle turbinate medialization. There were no cases of vision loss, diplopia, or orbital hematoma. We also found that sense of smell was not adversely altered after middle turbinate medialization, a finding that was previously reported by Dutton and Hinton.12
Many surgical techniques have been described that address the issue of middle turbinate lateralization and synechia formation with the lateral wall. No consensus has been reached on a single standard procedure because the various techniques all have their benefits and disadvantages.
LaMear et al advocated partial resection of the middle turbinate.13 However, that can still result in synechia formation and lateralization of the superior portion of the turbinate. Furthermore, the middle turbinate serves as an important anatomic landmark and is believed to improve nasal humidification, so we prefer to preserve it when possible. Thornton’s technique of suture conchopexy has had a high success rate in preventing middle turbinate lateralization.10 However, this





technique is time consuming and, in our experience, it can be difficult to perform.
Finally, the use of bioresorbable implants (e.g., Silastic sheets) and middle meatal spacers has been reported to reduce the risk of middle turbinate medialization.1 However, our technique avoids the extra cost of these stents. Moreover, our technique results in less patient discomfort during removal of these materials.
Creating a synechia by denuding the medial aspect of the middle turbinate and the nasal septum is a safe, quick, simple, and effective means of preventing lateralization. Placing nonabsorbable packing lateral to the middle turbinate for 3 or 4 days can effectively stabilize the middle turbinate. It can also prevent a “floppy” turbinate, and it is well tolerated by patients.
It is important to point out that a patent sinus cavity and a lack of synechiae do not always correlate with control of symptoms. Conversely, a well-lateralized middle turbinate and a patent meatus do not always ensure a favorable outcome. In 2015, Chen et al 2 described their comparison of postoperative endoscopic findings and Lund-Mackay scores14 between a middle turbinate suture group and a control group; they found no statistically significant difference between the two groups. This is possibly because many other factors play a role in controlling symptoms and preventing further sinus infections. These factors include an incomplete surgery, patient compliance, proper postoperative cleaning of the sinus cavities, and control of environmental, food, and aspirin allergies in addition to many other factors.
In 1999, Ramadan found that the most common cause of treatment failure was the presence of residual air cells and adhesions in the ethmoid sinus area (30.7% of failures).15 Other causes included maxillary sinus ostium stenosis (27%), frontal sinus ostium stenosis (25%), and a middle meatal antrostomy separate from the natural ostium with recirculation phenomena (15%).
The technique we describe provides for adequate medial positioning of the middle turbinate. Further studies need to be completed to better assess the correlation between (1) middle turbinate lateralization and the recurrence of symptoms and (2) the need for revision ESS. However, we found that medialization of the middle turbinate allowed for easy debridement and good visualization of the maxillary, ethmoid, sphenoid, and frontal sinus meatus postoperatively. This technique also provides good access for obtaining postoperative cultures if needed. We also found no correlation between middle turbinate medialization and olfactory disturbance.
In conclusion, synechia formation after ESS is a common complication that can lead to lateralization of the middle turbinate and obstruction of the middle meatus. This results in difficulty visualizing and properly
debriding the sinus cavities postoperatively, which can possibly result in recurrent disease.
Medialization turbinoplasty is a simple and effective technique that is an effective solution to a problem many sinus surgeons face. It is safe, quick, and easy to perform, and it does not add to the cost or morbidity of the surgery. It provides adequate access to the ethmoid sinuses postoperatively for debridement, and it reduces the risk of middle meatal narrowing.
In our study, medialization of the middle turbinate performed in patients undergoing ESS resulted in a significantly higher rate of medialization and wide access to the middle meatus in patients who underwent turbinoplasty. We observed no complications associated with the procedure. We conclude that medialization middle turbinoplasty is effective in providing wide access after ESS while reducing the risk of middle meatal stricture.
1. Lee JY, Lee SW. Preventing lateral synechia formation after endoscopic sinus surgery with a Silastic sheet. Arch Otolaryngol Head Neck Surg 2007;133(8):776-9.
2. Chen W, Wang Y, Bi Y, Chen W. Turbinate-septal suture for middle turbinate medialization: A prospective randomized trial. Laryngoscope 2015;125(1):33-5.
3. Bolger WE, Kuhn FA, Kennedy DW. Middle turbinate stabilization after functional endoscopic sinus surgery: The controlled synechiae technique. Laryngoscope 1999;109(11):1852-3.
4. Shrime MG, Tabaee A, Hsu AK, et al. Synechia formation after endoscopic sinus surgery and middle turbinate medialization with and without FloSeal. Am J Rhinol 2007;21(2):174-9.
5. Miller RS, Steward DL, Tami TA, et al. The clinical effects of hyaluronic acid ester nasal dressing (MeroGel) on intranasal wound healing after functional endoscopic sinus surgery. Otolaryngol Head Neck Surg 2003;128(6):862-9.
6. Chandra RK, Kern RC. Advantages and disadvantages of topical packing in endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg 2004;12(1):21-6.
7. Friedman M, Landsberg R, Tanyeri H. Middle turbinate medialization and preservation in endoscopic sinus surgery. Otolaryngol Head Neck Surg 2000;123(1 Pt 1):76-80.
8. Lindemann J, Keck T, Rettinger G. Septal-turbinate suture in endonasal sinus surgery. Rhinology 2002;40(2):92-4.
9. Moukarzel N, Nehmé A, Mansour S, et al. Middle turbinate medialization technique in functional endoscopic sinus surgery. J Otolaryngol 2000;29(3):144-7.
10. Thornton RS. Middle turbinate stabilization technique in endoscopic sinus surgery. Arch Otolaryngol Head Neck Surg 1996;122(8):869-72.
11. Hewitt KM, Orlandi RR. Suture medialization of the middle turbinates during endoscopic sinus surgery. Ear Nose Throat J 2008;87(12):E11.
12. Dutton JM, Hinton MJ. Middle turbinate suture conchopexy during endoscopic sinus surgery does not impair olfaction. Am J Rhinol Allergy 2011;25(2):125-7.
13. LaMear WR, Davis WE, Templer JW, et al. Partial endoscopic middle turbinectomy augmenting functional endoscopic sinus surgery. Otolaryngol Head Neck Surg 1992;107(3):382-9.
14. Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology 1993;31(4):183-4.
15. Ramadan HH. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope 1999;109(1):27-9.
CIPRODEX® Otic is the #1 prescribed antibiotic eardrop of ENTs and pediatricians.1



It has been prescribed for AOE and AOMT since 2003, with more than 30 million prescriptions filled.1,2
AOE, acute otitis externa; AOMT, acute otitis media with tympanostomy tubes. Not an actual patient.
INDICATIONS AND USAGE
CIPRODEX® Otic is indicated for the treatment of infections caused by susceptible isolates of the designated microorganisms in:
• Acute Otitis Media (AOM) in pediatric patients (age ≥ 6 months) with tympanostomy tubes due to Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Pseudomonas aeruginosa
• Acute Otitis Externa (AOE) in pediatric (age ≥ 6 months), adult and elderly patients due to Staphylococcus aureus and Pseudomonas aeruginosa
DOSAGE
• CIPRODEX® Otic is for otic use only, and not for ophthalmic use, or for injection.
• The recommended dosage is four drops into the affected ear twice daily for seven days.
• CIPRODEX® Otic is contraindicated in patients with a history of hypersensitivity to ciprofloxacin, to other quinolones, or to any of the components in this medication.
• Use of this product is contraindicated in viral infections of the external canal including herpes simplex infections and fungal otic infections.
Hypersensitivity Reactions: CIPRODEX® Otic should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity. Serious and occasionally fatal hypersensitivity (anaphylactic) reactions, some following the first dose, have been reported in patients receiving systemic quinolones.
Potential for Microbial Overgrowth with Prolonged Use: Prolonged use of CIPRODEX® Otic may result in overgrowth of nonsusceptible bacteria and fungi. If the infection is not improved after one week of treatment, cultures should be obtained to guide further treatment. If such infections occur, discontinue use and institute alternative therapy.
Continued or Recurrent Otorrhea: If otorrhea persists after a full course of therapy, or if two or more episodes occur within six months, further evaluation is recommended to exclude an underlying condition such as cholesteatoma, foreign body, or a tumor.
The most commonly reported adverse reactions in clinical trials were:
• AOM pediatric patients with tympanostomy tubes: ear discomfort (3.0%), ear pain (2.3%), ear residue (0.5%), irritability (0.5%) and taste perversion (0.5%).
• AOE patients: ear pruritus (1.5%), ear debris (0.6%), superimposed ear infection (0.6%), ear congestion (0.4%), ear pain (0.4%) and erythema (0.4%).
Please see Brief Summary of Prescribing Information on adjacent page.
For additional information refer to the full prescribing information.
1 INDICATIONS AND USAGE
CIPRODEX® is indicated for the treatment of infections caused by susceptible isolates of the designated microorganisms in the specific conditions listed below:
• Acute Otitis Media in pediatric patients (age 6 months and older) with tympanostomy tubes due to Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Pseudomonas aeruginosa
• Acute Otitis Externa in pediatric (age 6 months and older), adult and elderly patients due to Staphylococcus aureus and Pseudomonas aeruginosa
4 CONTRAINDICATIONS
• CIPRODEX is contraindicated in patients with a history of hypersensitivity to ciprofloxacin, to other quinolones, or to any of the components in this medication.
• Use of this product is contraindicated in viral infections of the external canal including herpes simplex infections and fungal otic infections.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
CIPRODEX should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity. Serious and occasionally fatal hypersensitivity (anaphylactic) reactions, some following the first dose, have been reported in patients receiving systemic quinolones. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, angioedema (including laryngeal, pharyngeal or facial edema), airway obstruction, dyspnea, urticaria and itching.
5.2 Potential for Microbial Overgrowth with Prolonged Use
Prolonged use of CIPRODEX may result in overgrowth of non-susceptible, bacteria and fungi. If the infection is not improved after one week of treatment, cultures should be obtained to guide further treatment. If such infections occur, discontinue use and institute alternative therapy.
5.3 Continued or Recurrent Otorrhea
If otorrhea persists after a full course of therapy, or if two or more episodes of otorrhea occur within six months, further evaluation is recommended to exclude an underlying condition such as cholesteatoma, foreign body, or a tumor.
6 ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
• Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
• Potential for Microbial Overgrowth with Prolonged Use [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In Phases II and III clinical trials, a total of 937 patients were treated with CIPRODEX. This included 400 patients with acute otitis media with tympanostomy tubes and 537 patients with acute otitis externa. The reported adverse reactions are listed below:
Acute Otitis Media in Pediatric Patients with Tympanostomy Tubes
The following adverse reactions occurred in 0.5% or moreof the patients with non-intact tympanic membranes.
Adverse Reactions Incidence (N=400)
Ear discomfort 3.0%
Ear pain 2.3%
Ear precipitate (residue) 0.5%
Irritability 0.5%
Taste Perversion 0.5%
The following adverse reactions were each reported in a single patient: tympanostomy tube blockage; ear pruritus; tinnitus; oral moniliasis; crying; dizziness; and erythema.
Acute Otitis Externa
The following adverse reactions occurred in 0.4% or more of the patients with intact tympanic membranes.
Adverse Reactions Incidence (N=537)
Ear pruritus 1.5%
Ear debris 0.6%
Superimposed ear infection 0.6%
Ear congestion 0.4%
Ear pain 0.4%
Erythema 0.4%
The following adverse reactions were each reported in a single patient: ear discomfort; decreased hearing; and ear disorder (tingling).
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of CIPRODEX®. Because these reactions are reported voluntarily from a population of unknown size it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions include: auricular swelling, headache, hypersensitivity, otorrhea, skin exfoliation, rash erythematous, and vomiting.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects. Pregnancy Category C:
No adequate and well controlled studies with CIPRODEX have been performed in pregnant women. Caution should be exercised when CIPRODEX is used by a pregnant woman.
Animal reproduction studies have not been conducted with CIPRODEX.
Reproduction studies with ciprofloxacin have been performed in rats and mice using oral doses of up to 100 mg/kg and IV doses up to 30 mg/kg and have revealed no evidence of harm to the fetus. In rabbits, ciprofloxacin (30 and 100 mg/kg orally) produced gastrointestinal disturbances resulting in maternal weight loss and an increased incidence of abortion, but no teratogenicity was observed at either dose. After intravenous administration of doses up to 20 mg/kg, no maternal toxicity was produced in the rabbit, and no embryotoxicity or teratogenicity was observed.
Corticosteroids are generally teratogenic in laboratory animals when administered systemically at relatively low dosage levels. The more potent corticosteroids have been shown to be teratogenic after dermal application in laboratory animals.
8.3 Nursing Mothers
Ciprofloxacin and corticosteroids, as a class, appear in milk following oral administration. Dexamethasone in breast milk could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical otic administration of ciprofloxacin or dexamethasone could result in sufficient systemic absorption to produce detectable quantities in human milk. Because of the potential for unwanted effects in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and efficacy of CIPRODEX have been established in pediatric patients 6 months and older (937 patients) in adequate and well-controlled clinical trials. No clinically relevant changes in hearing function were observed in 69 pediatric patients (age 4 to 12 years) treated with CIPRODEX and tested for audiometric parameters.
10 OVERDOSAGE
Due to the characteristics of this preparation, no toxic effects are to be expected with an otic overdose of this product.
Distributed by: Alcon Laboratories, Inc. Fort Worth, TX 76134 USA
U.S. Pat.: www.alconpatents.com
CIPRODEX® is a registered trademark of Bayer Intellectual Property GmbH, licensed to Alcon by Bayer Intellectual Property GmbH.
©2003, 2004, 2008, 2009, 2015 Novartis Revised: December 2015 W9012314-1115
Ronny Grunert, PhD; Sandra Klietz, BEng; Paul A. Gardner, MD; Juan C. Fernandez-Miranda, MD; Carl H. Snyderman, MD,
Abstract
In minimally invasive surgeries, it can be difficult to reach desired anatomic areas with rigid instruments, especially when obstacles are present in the surgical corridor (e.g., during transnasal pituitary surgery). We developed a new kind of suction device constructed of the shape-memory alloy Nitinol (nickel titanium), which is adaptable to a patient’s specific anatomy. Use of this device minimizes surgical risks by allowing physicians to use an endonasal transsphenoid approach. The suction device, which is equipped with a cannula made of the shape-memory alloy, was planned and manufactured with three different handpiece designs. Experienced pituitary surgeons tested the prototypes in human cadaver skulls and rated the devices on specific questionnaires. The results of their evaluation indicate that this device is a suitable tool for improving the surgical procedure. Its potential benefits include a more effective surgery and reductions in the risk of injury, the duration of surgery, and costs.
From the Department of Medical Engineering, Fraunhofer Institute for Machine Tools and Forming Technology, Dresden, Germany, and the Department of Neurosurgery, University of Leipzig Faculty of Medicine, Leipzig, Germany (Dr. Grunert); the Department of Biomedical Engineering, West Saxon University of Applied Sciences, Zwickau, Germany (Mrs. Klietz); the Department of Neurological Surgery, University of Pittsburgh Medical Center (UPMC), Pittsburgh (Dr. Gardner); and the Center for Cranial Base Surgery, UPMC Presbyterian Hospital, Pittsburgh (Dr. FernandezMiranda and Dr. Snyderman). The study described in this article was conducted at UPMC.
Corresponding author: Ronny Grunert, PhD, Department of Medical Engineering, Fraunhofer Institute for Machine Tools and Forming Technology, Nöthnitzer Straße 44, 01187 Dresden, Germany. Email: ronny.grunert@iwu.fraunhofer.de
Funding/support: The authors received grants from The Fraunhofer Society of Munich, Germany, for this research.
MBAIntroduction
Surgeons need a high degree of skill and precision when operating in small areas during neurosurgery to remove a pituitary tumor via the endonasal transsphenoid approach. Currently, the standard surgical approach is through the nostril and nasal cavity to the pituitary gland behind the sphenoid sinus.1-3 However, this path is a long, narrow corridor that is limited by bone and soft-tissue structures. This surgery traditionally requires the use of scissors, bone rongeurs, and coagulation instruments. Various rigid angled suction devices also are used to dissect and aspirate pituitary tumor tissue to achieve a complete excision.
Avoidance of excessive force is required to prevent complications such as injury to delicate blood vessels (ischemia or hemorrhage), the dural lining over the brain (cerebrospinal fluid leak), cranial nerves (vision loss or diplopia), and the posterior part of the pituitary gland (diabetes insipidus). Factors that contribute to such injuries include the use of instruments that are not well suited for the task and the forceful use of instruments to access an area beyond the reach of standard instruments.
The use of a limited array of rigid suction devices results in numerous exchanges of instruments, with attempts to use other angled instruments that are less effective than our new approach with a bendable suction. This results in surgical inefficiency, as well as increasing operating time and its attendant costs. Several disadvantages are recognized with the use of standard rigid suction devices:
• They are not adaptable to a patient’s individual anatomy.
• The risk of surgical injury is increased with the use of inadequate instrumentation.
• The surgical field needs to be extended to allow for access.
• The limited surgical field requires the use of multiple angled suction devices.
• Limited access results in incomplete tumor resection, which increases the risk of recurrence and need for radiation therapy.
• Modification of existing suction methods by bending them is difficult, and it narrows the diameter of the cannula.
• Bent suctions are difficult to restore to their original shape, and they require more frequent replacement.
We developed a new surgical suction device that surgeons can bend into any desired shape. With this device, it should be possible to achieve better access to all areas of the surgical field and improve the safety and efficiency of surgery.
Material properties. One of the promising materials tested for the manufacture of medical devices is the shape-memory alloy (SMA). This material is already being used for stents, needles, and braces, and it is suitable for surgical instruments such as suction devices.4
A cannula manufactured with an SMA can be adapted to a patient’s anatomy simply by bending it by hand during surgery. One particular SMA material is Nitinol (nickel titanium), which we used to develop our bendable suction device.5
Ergonomics. Ergonomics is important in the development of a suction handpiece. The user should be able to handle the device for a long period of time without experiencing any discomfort such as clenching of the hand or arm and fatigue and pressure marks from weight of the device. It should lie in the hand comfortably and allow for precise control in any position.
In close collaboration, surgeons, product designers, and engineers, with the aid of computer-aided design (CAD) software, worked to create three different models of a new suction handpiece, designated type 2, type 3, and type 4 (figure 1). These models give the user a choice of the most comfortable fit. The design of the handpiece must take into account its connection to the suction unit. The new suction device must be usable with all common aspirators to enable worldwide application.
One suction device is the ATMOS Record 55 DDS (ATMOS Medizin Technik; Lenzkirch, Germany). Its connection adapter for the cannula has a diameter of 6 mm. The CAD software allows developers to make rapid changes in design based on improvements suggested by surgeons.

Production process. The suction handpieces are made of the titanium alloy Ti6AI4V and are manufactured by a process called generative laser melting (figure 2). To ensure that the suction device can be bent by the surgeon in any desired shape according to patient-specific anatomy, an SMA was used for the suction cannula. The cannula reverts to its original shape after it is activated by heat during autoclaving. Two different inner diameters were considered: 2 and 3 mm. The handpieces are finished with a coating of black carbon to reduce light reflection during surgery (figure 3).
Autoclave test. A test was performed to confirm that a bent suction cannula would revert to it original straight shape. The cannula was heated at 120 °C (248°F) for 20 minutes. The test was performed a total of 20 times.
Evaluation questionnaire. The suction devices were rated by pituitary surgeons via a questionnaire. The surgeons provided their opinions on bendability, surgical access, and ergonomics. A 5-point scale with direct and closed-ended questions was used to categorize responses. Scores ranged from –2 (not at all) to +2 (very good). Each question pertained to only a single issue, and the questions were short, simple, direct, and comprehensible.
Overall, seven questions were asked—one technical question related to the device’s return to its initial straight form after heating, and six clinical questions related to its use during surgery:
• Can the suction be bent in every desired shape?
• What is the force required to bend the suction?
• Is it possible to reach the pituitary?
• Is the diameter wide enough to remove tissue?
• How is the handling/ergonomics?
• How is the handpiece design?
• Is it possible to achieve the straight shape when the suction is heated?
Additional comments were also solicited. Suggestions for improvement were considered in the design of subsequent prototypes and implemented in the 3-D CAD model of the handpiece. To provide a realistic simulation of pituitary surgery via the endonasal transsphenoid approach, fresh-frozen and fixed human cadaver skulls were used. Three surgeons from the University of Pittsburgh Medical Center (UPMC) tested the device and completed the evaluation questionnaire.
Preparation process. Current suction cannulas can be prepared in two ways: manually and mechanically. In the manual preparation process, the device is cleaned with ultrasound, a flexible brush similar to a pipe cleaner, and disinfectant solutions and water. The disinfectants must be aldehyde-free, phenol-free, and quaternary-ammonium-cation–free to avoid fixation of residuals and disturbance. The mechanical process begins with brush cleaning. This is followed by alkaline and thermal disinfection via a single-chamber disinfection device without ultrasound.
After cleaning, the devices are inspected for damage, checked for function, sterilized with steam at 134°C (273°F) for at least 5 minutes, and then packaged.6,7 To minimize the risk of unintentional transfer of difficult-to-diagnose prions (false-folded proteins that are responsible for the fatal Creutzfeldt-Jakob disease), steam sterilization at 134°C for at least 18 minutes is recommended.8,9

Ethical considerations. All procedures that contributed to this work were performed in compliance with the ethical standards expressed in relevant national and institutional guidelines on human experimentation (UPMC) and in accordance with the 1975 Declaration of Helsinki as revised in 2008.
We developed three functional prototypes of this new type of suction device. In all, the bendable suction devices left a positive impression on the UPMC surgeons. After each cadaver experiment, the handpiece design was revised with the 3-D CAD program and manufactured with the laser-beam melting machine, based on the surgeons’ recommendations.

We were able to straighten each bent cannula after every autoclave procedure. No changes in the coating were detected.
The surgeons rated the ability to bend the suction device in every desired form as very good, although they recommended modification of some ergonomic features, such as the position of the suction hole.
First prototype. After the round of tests with the first prototype, the surgeons noted that the handpieces were too slim, and they recommended that they be widened by about 5 mm. They also said that the first 4 cm of the suction cannula near the handpiece should be rigid to avoid undesired bending and that the connection between the cannula and handpiece must be stable. They
also recommended that the balance point of the suction device be located at the air-control hole and not at the cannula connection to the suction unit.
The surgeons also commented favorably that they were able to reach all areas of the surgical field and, again, that they could bend the suction cannula in any desired shape.
Second prototype (revised first prototype). For the development of the second prototype, suction devices with an inner diameter of 2 and 3 mm were manufactured. For the second round of tests, the surgeons evaluated wider suction devices: one with an inner diameter of 2 mm and the other with a 3-mm inner diameter. Both devices were equipped with a rigid proximal cannula segment of 40 mm. The 3-mm diameter device was good for drilling, but its cannula was too difficult to bend. The proximal lengthening of the cannula for 40 mm was rated as too long and needed to be shorter (20 mm for future prototypes).
The position of the air-control hole made the device unwieldy because it was set more toward the direction of the connection to the suction unit. The instrument’s center of mass needs to be considered. The wider suction devices were comfortable to use except for the type 3 device, which required further widening of the supporting surface. The surgeons said the diameter of the type 3 device was too small for drilling and the proximal part of the cannula (near the handpiece) was too flexible.
Third prototype (revised second prototype). Improvements for the third prototype included the production of three wider handpieces with inner diameters of 2 and 3 mm, and the application of the surgeons’ proposals. The length of the suction tube is 150 mm.
Based on the testing surgeons’ proposals, we were able to design a comfortable handpiece. Their evaluations affirmed that a bendable suction device is suitable for endonasal pituitary surgery. A working length of 150 mm is adequate, and all surgical fields can be reached. The ergonomics of the type 4 handpiece were rated as very good, and this type now serves as the primary design.
The use of a bendable suction device made of an SMA reduces the need for multiple rigid suction devices and shortens surgical time, which in turn reduces costs. Moreover, the ability to bend the device means that less tissue and bone must be removed to achieve surgical access, which improves efficiency and reduces the risk of major complications secondary to unnecessary dissection.
Because surgical risk is lower, less experienced surgeons can operate more safely and effectively and achieve a more thorough tumor dissection. The bendable suction device is suitable not only for endonasal transsphenoid pituitary surgery, but it also has wide applications to other surgical procedures such as endoscopic sinus surgery and some neurosurgical procedures.
After each autoclaving procedure, the cannula can be straightened and then adapted again for the next patient.
The bendable suction cannula will be developed further. For the next phase in that development, manufacturing and testing of next-generation prototypes will continue to be based on testing by and feedback from surgeons at UPMC.
In conclusion, the SMA Nitinol allows surgeons to bend a suction cannula in any desired form to adapt it to a patient’s individual anatomy. With a well-designed handpiece and the ability to choose from among different cannula diameters, surgeons can extend the application of this device to meet multiple needs. This device obviates the need to use different rigid suction devices, which results in economy of time and cost. Because the risk of life-threatening injury is reduced, less experienced surgeons can perform critical operations in a safer and more effective manner. These suction devices offer patients and surgeons the promise of optimal surgical outcomes.
1. Burton CM, Nemergut EC. Anesthetic and critical care management of patients undergoing pituitary surgery. Front Horm Res 2006;34:236-55.
2. Frank G, Pasquini E, Farneti G, et al. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology 2006;83(3-4):240-8.
3. Jho HD, Alfieri A. Endoscopic endonasal pituitary surgery: Evolution of surgical technique and equipment in 150 operations. Minim Invasive Neurosurg 2001;44(1):1-12.
4. Mantovani D. Shape memory alloys: Properties and biomedical applications. The Journal of the Minerals, Metals & Materials Society 2000;52(10):36-44.
5. Desai S, Bidanda B, Bártolo P. Metallic and ceramic biomaterials: Current and future developments. In: Bártolo P, Bidanda B, eds. Bio-Materials and Prototyping Applications in Medicine. Boston: Springer; 2008:1-14.
6. Axmann S. Keimreduktion auf Flächen und Medizinprodukten. In: Schulz-Stübner S, ed. Repetitorium Krankenhaushygiene und hygienebeauftragter Arzt. Berlin, Heidelberg: Springer; 2013:109-31.
7. Schulz-Stübner S, ed. Repetitorium Krankenhaushygiene und hygienebeauftragter Arzt. Berlin, Heidelberg: Springer; 2013.
8. Gibbs CJ Jr., Asher DM, Kobrine A, et al. Transmission of Creutzfeldt-Jakob disease to a chimpanzee by electrodes contaminated during neurosurgery. J Neurol Neurosurg Psychiatry 1994;57(6):757-8.
9. Rutala WA, Weber DJ. Creutzfeldt-Jakob disease: Recommendations for disinfection and sterilization. Clin Infect Dis 2001;32(9):1348-56.
Y our peers wanted to share an update since adding a FYZICAL Balance Center to their ENT practice:

“This is the single best thing we’ve ever done in our practice. We can’t comprehend why an otolaryngologist would not do this. It’s a no-brainer and it’s taking our profession by storm."

ü We're seeing 40 - 4 5 patients per day for balanc e therapy only.
ü Our hearing aid sales have increased 59%.
ü Our total patient visits are up 15% for new patients and 5% for return patients.
ü Our allergy / immunotherapy population has grown 20% since joining.
"We
*Limited seating and only open to those with open territories* Discover more at www.BusinessofBalance.com
"We can't stress enough how amazing of an opportunity this really is. You will grow every part of your practice through this vehicle."
couldn’t be more excited about our future. Get in touch with FYZICAL. You absolutely, positively, 100% need to see for your own eyes what this can do for your practice before it’s too late.”
Tuscaloosa ENT Group

