










We’re excited to share our first newsletter of 2024 with you. Dementia Connections will offer quarterly newsletters this year, and we’ll occasionally share additional articles at DementiaConnections.org.
For this issue we’re trialling a flip book style newsletter that is reminiscent of our magazine roots. Short on time? You can also quickly access some of the articles on our website but you’ll miss out on some terrific extras. We’d love your feedback - have a look at the flipbook and let us know what style of newsletter you prefer.
With spring arriving soon, we invited Green Care Farms to share about how they empower people living with dementia to get outside and learned from Root in Nature about the many benefits of sensory plants. We’ve also connected with experts from across Canada (and one from the US) to report on innovations in dementia care, new pathways toward finding a cure, and to share valuable insights borne of lived experience from two care partners.
Did you know all past issues of Dementia Connections magazine are now available for free? Thanks to our friends at Rare Dementia Support and Nipissing University Library for hosting the open access digital collection.
Do you have a story to share? Dementia Connections reports on research news, amplifies voices of lived experience and shares expert advice. Get in touch to talk about sharing your story in our Summer newsletter.

Enjoy spring!
 Carolyn Brandly, Editor
Carolyn Brandly, Editor


Writer and campaigner Nicci Gerrard set out to explore the illness we still struggle to speak about after her own father's death from dementia. What Dementia Teaches Us About Love (Penguin) is a hopeful inquiry into the nature of self and what it is to be human.
Dementia teaches us what we value in our lives. When someone has lost the social markers of value and can no longer connect their inner world with their outer world, we can learn to accompany them, to hold them as eminently precious and loveable, and in doing so we grow our capacity to love.
Dementia teaches us how to express what is inexpressible. Spending time with people with dementia can help us rediscover ways to be present in every miraculous moment. We can relearn how to connect deeply, to join hands, to sing, to dance, to hold the gaze of someone who can no longer speak, and perhaps even how to contemplate the reality our own impending death.
Dementia teaches us that we are made of more than our memories.
People with dementia live with courage, stoicism, and joy even as they lose connection with former versions of themselves. Spending time with people with dementia can help us face and overcome our own terror of loss of self. Talking with people who are living with dementia can help us recognize the indelibility of our shared humanity.
Alzheimer’s Disease International has launched the 2024 Attitudes Towards Dementia global survey, giving you the opportunity to join thousands of others and help build theworld’s largest international surveyon prevailing attitudes and stigma towards dementia.
Tools for Caring are a series of free, short videos that provide practical advice for family caregivers through the expertise of Positive Psychology Specialist, Josephine Tite.
Each episode offers a different tool caregivers can implement into their lives to increase hope and life satisfaction while reducing caregiver burnout.

Understanding the unique needs and experiences of diverse communities is a key step in improving the quality of life for people with dementia and their caregivers. Don’t miss this interesting read from the Alzheimer Society of Canada. Read

In Canada, more than 650,000 people have dementia and the numbers are sharply increasing. Over the next 30 years, we anticipate the number of people living with dementia in Canada will grow by 187%.
 ByCanadianCoalitionforSeniors’MentalHealth
ByCanadianCoalitionforSeniors’MentalHealth
Intense emotions, less interest in daily activities, trouble sleeping – most people living with dementia will experience changes in mood or behaviour that are unique to their context and background.
It’s important to understand that changed memory, thinking, moods or behaviours are not deliberate and they are not always a problem. In fact, these expressions are often an attempt to communicate discomfort and distress when the person with dementia has difficulty expressing their needs or making sense of their environment.
By paying close attention to patterns of moods or behaviours and exploring root causes of behaviour with compassion and curiosity, we can identify and meet the unspoken needs of people living with dementia. If changes in mood or behaviour do become concerning, there are evidence-informed approaches that can help.
Powered by the Canadian Coalition for Seniors’ Mental Health, the Behaviours in Dementia Toolkit is a brand-new online library of over 230 free resources filled with practical and evidence-informed approaches to navigate dementia-related changes in mood and behaviour.
The goal of the Toolkit is to help care partners and health care providers better understand these changes, compassionately respond to moods and behaviours, and ultimately support people with dementia to live well.
In the Toolkit library you can search for online resources including videos, guides and courses that can help build understanding, improve communication, and support well-being.
Health care providers will also find tools to support assessment, documentation and staff training, along with information handouts for patients.


There’s a lot to explore in the Behaviours in Dementia Toolkit. Below are a selection of 5 resources and resource collections to get you started:
1. Understanding behaviours in dementia pamphlet: This pamphlet includes a symptom checklist, highlights factors that may increase behaviours in dementia, and shares an overview of steps you can take to support someone experiencing dementia related mood and behaviour change.
2. A series of infographics that provide resources specific to different types of dementia, a variety of equity perspectives and unique care contexts. Some topics include young onset dementia, lewy body dementia, self-care essentials for care partners, resources for first responders and resources for personal support workers.
The Toolkit also includes links to multilingual resources available in 52+ languages!
3. Behaviour or mood specific resources: These resources are available in a variety of formats including tip sheets, web pages, videos, training courses and evidence summaries. Find different collections at the links below:
Anger
Desire to move
Eating habits
Fear or worry
Hygiene
Sadness
Sleep
Social interactions
Thoughts, beliefs, or perception
Other
4. Resources with approaches to support with medication: There are several resources available to health care providers on assessment and treatment algorithms, medication guidelines and appropriate prescribing and deprescribing techniques.
Video and audio recordings can be accessed to learn how to implement deprescribing algorithms and appropriately use medication in the treatment of behavioral and psychological symptoms of dementia.
5. Resources with approaches to support without medication: Many resources highlight ways to increase meaningful engagement with people living with dementia to support their quality of life, personal goals and help reinforce aspects of their identity.
Remember that needs change over time and what works one day may not work the next. Stay flexible and be creative. With support, people experiencing behaviours in dementia can lead active and fulfilling lives.

Explore the Behaviours in Dementia Toolkit at BehavioursInDementia.ca for practical and evidence-informed resources today!

The Canadian Coalition for Seniors' Mental Health (CCSMH) is the only Canadian not-for-profit organization focused solely on supporting older adults' mental health through information, resources, professional development and clinical guidelines.
Find no-cost, evidence informed resources for health care providers and for older adults at CCSMH.ca.




Empoweringpeoplewithdementia togetoutside.
byGreenCareFarmsGreen Care Farms is Canada’s first care farm dedicated to people living with dementia. Located on a half-acre plot on Andrews Farm Market and Winery in Milton, Ontario, the program engages participants in a variety of purpose-driven therapeutic outdoor activities like planting, watering, and harvesting fresh produce.
Care farming is a type of therapeutic programming that combines horticultural and agricultural activities with care services. Research has shown many benefits for people with dementia, such as increased physical activity, enhanced social interaction and a renewed sense of purpose. The concept of care farming originates in Europe and is widespread there yet care farming related to dementia remains relatively new and unknown in Canada.

At Green Care Farms, members can reap the rewards of their work by taking home a bounty of fresh produce each week. Members can also feel good about making a positive contribution to their community as the surplus produce is donated to the local food bank.
Theprogramalsooffersadayof respitetocarepartnersandfamilies, somethingthatRebekah Churchyard,theCEOandFounderof GreenCareFarms,personallyknows issoimportant.
Respite programs support busy caregivers by enabling them to spend time away from providing care to their loved one and to focus on themselves, even for just a few hours. Respite programs reduce caregiver burnout as well as the number of nonemergency hospital visits.
“By providing our members with fun and purposeful activity and their family members with respite, we are reducing healthcare provider burden and maintaining higher quality of life at home,” says Churchyard. This type of support can help people with dementia live longer supported at home.
Churchyard, a Social Worker and Psychotherapist specializing in geriatrics and dementia care, was inspired to start Green Care Farms after her grandfather Ron, a Christmas tree farmer, was diagnosed with early-onset frontotemporal dementia. She witnessed the challenges her family faced to find support and outdoor programs for him to safely continue to do the meaningful work he loved. As his dementia progressed, opportunities for him to be safely outside decreased.
Without stimulation and adequate support at home, people with dementia deteriorate more quickly, and caregivers’ health and mental health is often also significantly impacted. “The caregiving demand on my grandmother became unbearable, and no one was happy with him being locked inside all day,” Churchyard shared. “My grandparents lived in a rural area and I witnessed their struggle to find support and appropriate programming.”
Other than Green Care Farms, there are no targeted programs for people with dementia to be active outdoors in Canada, and waitlists for adult day programs in Ontario can be years long. This is especially challenging for people whose lives and careers revolved around the outdoors before their dementia diagnosis, and for their caregivers who need regular support and respite that can be hard to find due to healthcare system capacities and shortages.

At Green Care Farms our vision is “A care farm in every community in Canada”. We want people with dementia across Canada to be able to access a Green Care Farm locally which is why we will soon be offering a series of workshops on how to start your own care farm.
We aim to inform, help, and inspire other passionate individuals to replicate our model in their community. The workshop will be free of charge and we will capture feedback from the participants to inform our future Green Care Farms services.
We hope you will join us to learn more about creating farm experiences rooted in purpose and belonging that empower people living with dementia all across Canada.

Want to learn more about starting your own care farm? Email hello@carefarmscanada.com to join in the upcoming virtual workshop series ideal for community groups, farmers and local professionals supporting older adults.

Green Care Farms serves people of any age living with a cognitive impairment who would enjoy working on a farm. This year we will also be supporting group outings for retirement and long-term care homes as well as congregate living settings. Learn more about our work at CareFarmsCanada.com.
More from Green Care Farms in our Live Well article archive: Nature As Medicine.



Socialdeterminantsofhealth affectingdegreeoforaccessto potentialriskfactorchange
Incomeandsocialstatus
Employmentandworking conditions
Educationandliteracy
Earlychildhooddevelopment
Physicalenvironmentsand housing
Socialsupports
Accesstohealthservices
Biologyandgenetics
Gender Culture
Race,racismandracialization
Disabilityandableism
It is estimated that in 2020 there were 10,800 people of Indigenous ancestry living with dementia in Canada. By 2050, we can expect this number to increase by 273% to 40,300.
AlzheimerSocietyofCanada,2024

For the past 30-40 years, Alzheimer’s disease research has been dominated by a proposal called the “amyloid hypothesis”.
According to this hypothesis, Alzheimer’s disease is caused by a protein in the brain called beta-amyloid which clumps into small aggregates that are toxic to brain cells, ultimately killing them and leading to the symptoms of dementia as these brain cells die.
Also according to this hypothesis, beta-amyloid is an abnormal protein that is not supposed to be in the brain, but is abnormally produced for reasons that are not fully understood.
Regrettably, almost all drugs developed to block the production of beta-amyloid and its aggregation have failed to help treat the disease.
Recently, there has been some limited success with two therapeutics, one called lecanemab, the other called donanemab, which bind to beta-amyloid clumps and which seem to have some effectiveness in treating the disease.
The partial success of these two agents supports the notion that beta-amyloid probably plays an important role in the progression of Alzheimer’s disease, but that the amyloid hypothesis is not sufficient to explain the full cause of Alzheimer’s.
In short, the amyloid hypothesis is part of the answer, but isn’t the whole answer.
In the search for additional or alternative explanations for Alzheimer’s, many other suggestions and hypotheses have been put forth.
These include proposals that Alzheimer’s arises from slow infections of the brain, inflammation of the brain, damage to brain cell membranes, too much copper (or zinc, or iron) in the brain, and so on – the list is long with many different and varied suggestions.
One of the emerging leading hypotheses is that Alzheimer’s is caused by malfunctioning of the immune system within the brain, which in turn leads to inflammation in the brain with subsequent brain damage.
In our lab, we are studying this brain immune system malfunctioning hypothesis. Using state of the art computer modelling methods, we have been simulating the behaviour of betaamyloid when it is near a brain cell. These simulations predict that the beta-amyloid protein initially sticks to the surface of a brain cell and then part of the protein then wiggles through the brain cell’s membrane, rupturing it and causing the cell to die.
We also noticed that beta-amyloid protein does the exact same thing to bacterial cells. Additional extensive computer modelling also suggested that beta-amyloid is in fact a normally occurring protein in the brain and functions as a type of molecule called a “cytokine”, where cytokines are messengers that carry information between immune cells in the brain.
One of the emerging leading hypotheses is that Alzheimer’s is caused by malfunctioning of the immune system within the brain, which in turn leads to inflammation in the brain with subsequent brain damage.
-Dr.DonaldWeaverBased upon these computer simulations, backed up by experiments using brain cells, we have devised a new theory of Alzheimer’s disease: following a variety of stimuli, including brain infections, trauma, or even depression, beta-amyloid is released as a cytokine which is trying to protect the brain. As part of its protection duties, beta-amyloid searches for bacteria in the brain, primed to kill the bacteria should any be detected.
However, in a horrible case of mistaken identity, beta-amyloid gets confused and misrecognizes normal brain cells as bacteria, leading to the death of these brain cells.
In this way, Alzheimer’s disease emerges as a disorder of the brain’s immune system, which occurs because beta-amyloid, while trying to defend the brain, cannot differentiate between bacteria and brain cells, culminating in the accidental death of brain cells.
We are now exploiting this new and interesting theory of Alzheimer’s disease in an attempt to identify potential new drugs for the treatment of this chronic, progressive brain disease.
The brain is the most complex organ in the human body, and arguably, Alzheimer’s is one of the most complicated diseases of the brain. We need new and innovative ways of looking at this disease in our attempt to devise new therapies.
The notion that Alzheimer’s occurs because beta-amyloid, as an important contributor to the brain’s immune system, gets confused and mistakes brain cells for bacteria is a new way to look at this challenging disease.
Time and additional research will tell us if this theory is right or wrong, but when it comes to Alzheimer’s, all new knowledge is useful.
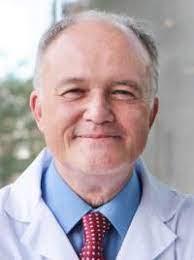

Dr. Weaver is a Senior Scientist at the Krembil Research Institute at the University Health Network. He is a professor of Chemistry, Medicine and Pharmaceutical Science at the University of Toronto and a neurologist at the Toronto Western Hospital.
Dr. Weaver is also the Krembil Chair in Drug Discovery for Alzheimer’s Disease, Chief Medical Officer of Treventis Corporation, and is the former President of Epilepsy Canada.
Find more Research Updates in our Live Well article archive.
Didyouknow?
Most dementia care is organized for people in their 70s and 80s. But there is a growing group of people developing young-onset dementia in their 40s, 50s and early 60s—or even earlier.


Boosthydrationthroughan irresistiblecandy.
byJellyDrops
Jelly Drops are an innovative sugar-free treat, made of 95% water with added electrolytes, designed to increase fluid intake among people with dementia and others who struggle to stay hydrated.
Dehydration can have serious impacts for people living with dementia who may be unable to recognize or communicate that they are thirsty due to changes in signalling within the brain. Dehydration can impact cognitive function resulting in increased confusion, may increase the risk of falls or urinary tract infections and can make medication less effective.
English inventor Lewis Hornby was inspired to create water candy after his grandma Pat, who had dementia, was struggling to hydrate. After successful launches in the UK and US, Jelly Drops are now available in Canada.
With an eye-catching colorful design and shape, the tasty bite-sized treats have a solid, yet smooth, texture that encourages independent hydration in those who may otherwise require assistance to drink.
My momma has trouble with becoming dehydrated easily. It makes her dizzy and prone to falling. She loves Jelly drops. She calls them a treat.
It makes me happy to see her happy. Such a small thing makes a huge difference.
-SharleeTreloar,Toronto
Jelly drops come in six fruity flavors: orange, lemon, blackcurrant, strawberry, raspberry and peach. They are not recommended for those with swallowing difficulties or suspected swallowing difficulties. Consult a speech and language therapist if you have any concerns before use.
Jelly Drops offer a sweet solution to avoid dehydration.
MoreInformation
Learn more at JellyDrops.ca



Aguidetosensorygardenplants& theirtherapeuticbenefits.
Sensory gardens are transformative spaces that engage all five senses, offering a unique blend of therapeutic benefits. These carefully curated landscapes are more than just visually appealing; they serve as natural sanctuaries for relaxation, cognitive stimulation, and sensory exploration.
Designed to be inclusive and interactive, sensory gardens provide a soothing environment that caters to individuals with various conditions, such as autism, Alzheimer's disease, and anxiety disorders, enhancing their emotional well-being and sensory processing abilities.
The benefits of sensory gardens extend beyond their beauty. They are a source of comfort and healing, promoting stress reduction and relaxation through gentle engagement with nature. For individuals with cognitive challenges, these gardens stimulate memory and cognitive function, offering a peaceful retreat that evokes memories and encourages reminiscence.
Physical health is also enhanced as these gardens motivate visitors to engage in physical activity, improving motor skills and coordination.
Sensory gardens also serve as educational platforms, enriching users' knowledge about plants, wildlife, and the environment, while fostering social interaction and community engagement.

Plants that are visually stimulating:

Sunflowers stand tall, their large, bright blooms following the sun, symbolizing nature's vibrancy. They're a source of joy and a visual anchor in gardens.
Black Eyed Susans, with their golden-yellow petals and dark centers, bring a dynamic visual appeal and invite pollinators, enhancing the garden's liveliness.
Japanese Maples are visually striking, offering serene beauty with their intricate leaves and stunning fall colors, perfect for tranquil retreats and adaptable to smaller spaces.
Plants that offer pleasant aromas:
Rosemary's robust scent is linked to memory enhancement, making it an asset for cognitive health in garden settings.

Mock Orange, with its sweet, citrus-like aroma, blooms in late spring, enriching gardens with its delightful fragrance.
Lavender is famed for its calming scent, contributing to a peaceful garden environment and aiding relaxation.
Plants that are great for tactile engagement:
Lamb's Ear is beloved for its soft, velvety leaves, offering a comforting touch.
Moss provides a unique, soft texture underfoot or at hand, promoting a sense of connection with nature.
Aloe Vera intrigues with its succulent leaves filled with soothing gel, combining visual interest with a tactile experience.


Plants that encourage auditory stimulation:
Bamboo creates calming music as the wind moves through its leaves and stems, offering auditory stimulation.

Ornamental Grasses whisper as they sway, adding a gentle, relaxing sound to the sensory garden.
Plants that have wonderful flavour:
Basil offers a fresh, aromatic flavor, enhancing culinary dishes and garden experiences. Mint brings a cool, refreshing taste to foods and drinks, adding a burst of freshness.
Woodland Strawberries delight with their sweet, aromatic flavor, thriving in shaded areas and encouraging garden exploration through taste.

Discover more sensory plant examples in a complimentary lesson from Root in Nature's online course: Introduction to Therapeutic Horticulture. Sign up here.

Root in Nature strengthens human health by connecting people with plants and nature through therapeutic horticulture, while serving as a training hub and professional growth platform for practitioners in the field..
By 2050 1 in 4 people with dementia will be of Asian origin. That is a 785% increase from 2020. Didyouknow?


Acarepartner‘sreflectionsalong ajourneywithFTD.
byDanielleBarrette-Marcuccio
I’ve often quoted that the journey of caring for someone with Frontotemporal dementia (FTD) is not for the faint of heart. I truly believe that caring for someone living with FTD is a personal choice, one you make early on, which hopefully, can sustain you.
My journey began when my husband John was diagnosed with Behaviour-Variant Frontotemporal dementia (bvFTD) in September of 2015, at the age of 61. It took us a long time to get a diagnosis, years in fact, but we were fortunate, we ended up, at the Memory Disorder Clinic at Elizabeth Bruyere Hospital in Ottawa with a remarkable neurologist, Dr. Andrew Frank.
I think that at first, we were mostly shocked at the diagnosis. My initial reaction was to find out as much as I could about this type of dementia to address the fear and anxiety I was feeling.My husband’s family, who lived five hours away, were quite upset at the diagnosis as was our daughter Stephanie who was living in Toronto at the time.
Stephanie started coming home more frequently as she was very close to her father. She truly was heartbroken at his diagnosis and fearful of losing him. Her primary coping strategy was to not think about the longer term but to just focus on the dayto-day connections.
This meant she made many more Facetime calls, frequent trips home and started focusing her energies on caring for her father.
When John was diagnosed, I was still working as an executive. I started to readjust my schedule to accommodate Dementia groups/meetings and medical follow up to gain some support and ensure that we were doing all we could to address his dementia. John was on medical leave for close to 18 months and would ‘retire’ officially, in 2016 as did I. My original plan was to work as a consultant and had registered a business “Future Transitions Management”, but I quickly realised I had to forego that plan as I would need to focus on caring for John.
From the start, my approach has been that we live life to the fullest and make the days count. We joined a gym, John began participating in day programs and observational research, we began meeting other young onset couples for support, recreational, and social activities.
I also learned, following a couple of ER visits, that John could develop delirium that rendered him unable to function and/or walk if he got dehydrated or had an infection. This journey with FTD has ongoing issues, challenges, and changes you must learn to adapt to.
The more I learned and connected with others living with FTD, the better and more empowered I felt. At the same time, I recognized how many caregivers have little knowledge on what this journey entails or how to navigate it, so I started doing advocacy work, helped set up focus groups and established a couple of Facebook groups, one national FTD group (275 members) and one, local Young Onset Dementia group (52 families).

I felt I should share or leverage what I was learning and build a community. I was surprised at how little research and/or focus FTD has here in Canada in comparison to the US. It also provided me with a purpose and a way to channel my energies.
In 2020, when Covid hit, John’s father passed away in April and his mother subsequently got placed into long-term care following a dementia diagnosis. I tried, remotely, to support his sisters who had to cope with everything, the funeral, placement, and sale of the family home the same year.
Everything shut down, all doors, programs, literally, closed, social outings all ended. I cancelled all PSWs who were coming into the home for the next 2 years. Our daughter started working remotely in Ottawa during the pandemic to provide me with some back-up, which created a lot of stress and anxiety for her but also meant she shifted her entire life to support her father.
John’s FTD progressed during this period compounded by limited social interaction. I tried to get him involved in online programming, some physical activity, set up a treadmill and we went for walks, which helped my stress levels. But he stumbled during one walk in 2020, barely making it back to the car. I was alarmed when his depth perception started to fail, particularly on the stairs, I thought he might stumble and fall. I devised interim and longer-term solutions to address this (i.e. tape on shower stairs, installing a chair lift).
Then when John experienced his first seizure in May 2021, I literally thought the worst. He went to the ER, which dramatically changed our journey with FTD.
His neurologist counselled us to look at antiseizure medications, should there be a recurrence. Six months later, he had another seizure. In addition, he was now having trouble swallowing and started to walk with a shuffle.
Once on anti-seizure meds, John experienced, 2-3 times a week, “mini seizures” that required ongoing monitoring and changes to medication for the next 8-9 months. It took us through to the summer of 2022 to stabilize his medication and seizures. This was emotionally draining and created ongoing anxiety and stress for both my daughter and me.
If this wasn’t challenging enough, I lost my brother during this period, in April 2021, to Covid. He was our family’s rock, everyone leaned on him, particularly my mother during the Pandemic. This loss knocked the wind out of our family’s sails.
I’ve discovered that love can sustain you and that support can sometimes come from unexpected people and places. I recognize that those that can, do and those that can’t ought not to be judged.
-DanielleBarrette-MarcuccioI know that having limited contact with family and friends, particularly during Covid, created feelings of isolation and loneliness.
I found that being ‘mindful’ about my daily activities and interactions with John, focusing on all that was present, fun, and joyful was uplifting. Given that my husband was now wheelchair-bound, we installed a vertical platform lift to enable us to take walks outside, as well as manage outdoor visits with family and friends.
In 2020, an estimated 61.8% of persons living with dementia in Canada were female. By 2050, the Landmark Study projects that over 1 million women will be living with dementia in Canada. Women are doubly affected by dementia (almost 2:1 dementia cases and >50% of caregivers). Didyouknow?
TheManyFacesofDementiainCanada.AlzheimerSocietyofCanada,2024.
Now that we have the flexibility of more social contact and connections, including celebrating John’s 70th birthday in October 2023, I feel there’s much more love and support surrounding us.

I’ve learned so much in this journey, not just about FTD. I’ve learned about the kindness of strangers keeping an eye on my spouse so he doesn’t wander, a company that honours a credit that my husband is not able to confirm, a doctor who calls you within hours when John was in the ER.
I’ve also learned to be patient and kind with myself, not to chastise myself when I can’t get something done or my house is in disarray. I’ve discovered that love can sustain you and that support can sometimes come from unexpected people and places. I recognize that those that can, do and those that can’t ought not to be judged.
I say this frequently, I feel blessed to be on this journey. To have family supporting us every step of the way. I feel blessed to have a husband who is so good-natured and offers me daily smiles and although he can no longer speak and must face multiple daily challenges, he holds onto my hand tightly and I feel the love in my heart. I can honestly say that I’ve never loved my husband more “for better or for worse”.


Making medical decisions to support a person living with dementia can sometimes feel like reaching a busy intersection with many forks in the road. How can we choose the direction that best reflects the wishes and goals of the person with dementia?
As a full-time emergency room (ER) physician I know that establishing goals of care helps care partners, families, and people living with dementia to better understand care choices and to feel confident when making medical decisions on behalf of a person with dementia.
Planning for peace of mind begins with understanding which of the three fundamental goals of medical care will best honour the wishes of the person living with dementia.
1) Full Treatment - Primary goal is to stay alive. All medical interventions available to treat new or pre-existing conditions are requested. Care that is focused on keeping someone alive is OK.
2) Some but Not All - Primary goal is to protect and maintain quality of life. Medical interventions are chosen on a case-by-case basis depending on the person's recent quality of life. Care that is focused on prolonging life may or may not be OK depending on the situation and how the person's quality of life would be affected with or without it.
When a person no longer wants CPR (cardiopulmonary resuscitation) they will be in this goal of care group (or comfort care) and not in Full Treatment.
3) Comfort - Primary goal is to prevent suffering and provide comfort. Any care intervention, including medications, procedures, surgery, testing, trips to ER or stays in hospital, should have the underlying intention to first provide comfort.
The person should not receive care that is meant to keep them alive as the main reason for care.
Although conversations about medical care can be uncomfortable, planning goals of care well ahead of a pressure-filled visit to the ER will offer you considerable peace of mind should a life changing decision be required.
Key questions to discuss or think through when planning goals of care:
What fundamental values has the person with dementia held throughout their life?
What does quality of life mean to the person with dementia?
What is their current quality of life?
What level of medical screening or intervention is acceptable?
When will goals of care be reassessed?
Wherever possible, people with dementia should be included in conversations to establish goals of care. Decisions about goals of care should be shared among family members so they are not a surprise at the time of a medical event.
While conversations about medical goals of care can feel heavy, the peace of mind and confidence these conversations can provide is well worth the effort.


Dr. Brittany Lamb is a board-certified emergency medicine attending physician with over 12 years of health care experience. Dr. Lamb supports care partners to become confident medical decision makers through her free Facebook Community and her online course – Make Your Plan with Dr. Lamb. Learn more about her work at BLambMD.com.
More from Dr. Lamb in our Live Well article archive: Ten Tips to Make an ER Visit Less Stressful.
By 2030, almost 1 million Canadians will live with dementia. Its impact is and will continue to be felt across all borders, sectors and cultures. We need to increase awareness of the diversity of who develops dementia in Canada.

