
29 minute read
CPD CENTRE
Answer the questions online at www.dentalcommunity.com.au To retrieve your FREE Dental Community Login, Call (02) 9929 1900 or email joseph@dentist.com.au
cad | CAM
READ ME FOR CPD
3D printing dentures - Part 1: Choosing a printer
By Terry Whitty
Having a look at the recent statistics for edentulism in Australia and other places in the world, you would think that the demand for dentures is on the decline. However, things could not be further from the truth. In a nutshell, as far as Australia goes, roughly 1 in 10 adults 45 years and over and 1 in 5 adults 65 years and older are edentulous. While there has been a decline in edentulism over the past decade, there are other factors in to play here including an ageing population, increases in life expectancy and population growth to name a few. Couple with the shortage of skilled dental technicians, especially for removable prosthetics and Houston... we have a problem. This is exactly why people are now pushing the digital denture barrow down your street and it’s no surprise it has been on the boil for many years as digital technology continues to permeate all areas of dentistry.
A simple overview of the workflow encompasses scanning either intraorally or on a bench-top scanner and taking records, digital design using CAD software packages and then manufacturing the digital dentures.
For manufacturing, there are essentially two methods currently favoured - namely milling or 3D printing. And you can also do a combination of both as well as incorporating “carded” teeth and there are other options and hybrids as well.
26 eLABORATE July/August 2022
READ THE ARTICLES AND ANSWER THE QUESTIONS ONLINE
ceramic | TECHNIQUES
READ ME FOR CPD
Expectations met: hybrid abutment crown made of zirconium oxide with vestibular cut-back
When fabricating a hybrid abutment crown, the choice of material plays an important role. The framework material should provide high stability as well as having translucent properties and a tooth-like appearance. The author describes why he prefers NexxZr T Multi (Sagemax) zirconia and how he deals with the clash between high aesthetics and economic requirements
By Mark Bultmann, Master Dental Technician
Clinical work by Dr med. dent. Katharina de Buhr
Meeting expectations is part of the routine in the dental laboratory, but the challenge comes up again and again. Every patient has concrete expectations for the outcome that are driven by individual desires and specific needs. Working together with the dental practice, as dental technicians we are obliged to satisfy these expectations. In implant prosthetics we are responsible for effectively realising implant dentistry therapy with an aesthetic restoration. A delicate task for all ambitious dental technicians. To prevent excessive pressure due to placing too many demands on ourselves, we need to rely on tested processes and premium materials.
Patient case
The osseointegrated implant in position 14 required fitting with an all-ceramic crown. In theory, this can be covered in the digital workflow; increasingly, we receive the dataset from the intraoral scanner. In this case, a conventional impression was taken. The master model was digitised with the scanbody and the data uploaded into the CAD software. The decision about the type of restoration was made in agreement with the dental practice. We fabricate almost exclusively all-ceramic abutments. One-part and two-part abutments are differentiated.1-3 In this case, a hybrid abutment crown (two-part) was fabricated. The all-ceramic CAD/CAM crown was cemented onto a titanium bonding base. In contrast to the one-part zirconia abutment, the contact surface with the implant is made of titanium. This eliminates the danger of material wear caused by direct contact between zirconia on metal. Released titanium particles could lead to negative aesthetic effects on the gingiva (titanium tattooing). The hybrid abutments also have a comparably high strength or fracture load because the titanium bonding bases increase the stability.4,5
Framework fabrication
Amonolithic crown was constructed taking into account the functional criteria. A cut-back was created in the vestibular area. It is often possible to achieve a natural aesthetic without veneering with multi-layer zirconia. However, to meet the high aesthetic expectations in this case, vestibular veneering was required.
After construction, the abutment crown was milled from NexxZr T Multi (Sagemax). This multi-layer zirconia combines two generations of zirconia (3Y-TZP and 5Y-TZP). This results in a high flexural strength (1170 MPa) in the cervical region that is associated with high incisal translucency. Unlike some other multi-layer zirconia, NexxZr T Multi has a smooth colour and translucency gradient and is free of visible layers. As a result, the restorations appear very natural and in many situations monolithic implementation without aesthetic compromises is possible. To be able to optimally utilise the colour gradient when nesting, ensure that the crown is correctly positioned in the milling blank. Morphological details are touched up after the milling. Caution: Zirconia is a “delicate petal” - particularly in the white chalk-like state (before sintering) - and it must be handled with care. Do not use laboratory turbines or steam!
34 eLABORATE July/August 2022
Question 1. DLP technology uses... a. A DMD device comprising of micro mirrors. b. Laser tracing. c. An LCD screen and LED array. d. An incandescent light bulb.
Question 2. One major advantage of printing dentures over milling is... a. No need for a pressure vessel. b. You can print multiple parts at the same time. c. Parts can be printed in 1 minute. d. No need to post cure any parts.
Question 3. Most 3D printing resins for dentures are... a. Nylon-based b. Polypropylene c. Photopolymers d. PMMA
Question 4. In Australia, the demand for dentures is... a. On the decline b On the rise c. Stable d. Not relevant anymore due to fluoride
Question 5. Very good printable denture base materials... a. Will never be available. b. Are 10 years away. c. Are 5 years away. d. Are now available. Question 6. In this case the impression was... a. Digital from an Intra Oral Scanner b. CBCT c. Conventional d. Compound
Question 7. With multilayered zirconia, high aesthetics is often achievable... a. Only with pre-sintered staining. b. Without veneering porcelains. c. With the addition of titanium oxides. d. None of the above.
Question 8. To correctly achieve the colour gradient when milling... a. Always insert the disk upside down. b. Always insert the disk right side up. c. Position the restoration in the disk nesting software correctly. d. Position the restoration sideways.
Question 9. To conceal the titanium base... a. Use a light blocker. b. Use zinc oxide cement. c. Use cyanoacrylate. d. It’s not necessary to conceal the titanium base.
Question 10. In this case, the titanium base was adhered to the crown using... a. Superglue b. Ivoclar Multilink Hybrid Abutment c. PVA adhesive d. Elmer’s glue all
Play your cards right. Play your cards right.



Medentika® MPS Multi Platform System Medentika® MPS Multi Platform System NE & MG SERIES Compatible with Neoss® & MegaGen NE & MG SERIES Implant Systems Compatible with Neoss® & MegaGen Implant Systems
Contact your Straumann Group Solutions Specialist to claim your free trial Contact your Straumann Group Solutions Specialist to claim your free trial
Straumann Pty Ltd/Straumann New Zealand Limited
93 Cook Street, Port Melbourne VIC 3207, Australia AU Toll Free 1800 660 330 | NZ Toll Free 0800 408 370 Email customerservice.au@straumann.com www.straumann.com.au www.straumann.co.nz Straumann Pty Ltd/Straumann New Zealand Limited 93 Cook Street, Port Melbourne VIC 3207, Australia AU Toll Free 1800 660 330 | NZ Toll Free 0800 408 370 Email customerservice.au@straumann.com ©Institut Straumann AG, 2021. All rights reserved. Straumann www.straumann.com.au ® and/or other trademarks and logos from Straumann® mentioned herein are the trademarks or registered trademarks of Straumann Holding AG and/or its affiliates.www.straumann.co.nz

3D printing dentures - Part 1: Choosing a printer

By Terry Whitty
Having a look at the recent statistics for edentulism in Australia and other places in the world, you would think that the demand for dentures is on the decline. However, things could not be further from the truth. In a nutshell, as far as Australia goes, roughly 1 in 10 adults 45 years and over and 1 in 5 adults 65 years and older are edentulous. While there has been a decline in edentulism over the past decade, there are other factors in to play here including an ageing population, increases in life expectancy and population growth to name a few. Couple with the shortage of skilled dental technicians, especially for removable prosthetics and Houston... we have a problem. This is exactly why people are now pushing the digital denture barrow down your street and it’s no surprise it has been on the boil for many years as digital technology continues to permeate all areas of dentistry.
A simple overview of the workflow encompasses scanning either intraorally or on a bench-top scanner and taking records, digital design using CAD software packages and then manufacturing the digital dentures.
For manufacturing, there are essentially two methods currently favoured - namely milling or 3D printing. And you can also do a combination of both as well as incorporating “carded” teeth and there are other options and hybrids as well.
Additive or subtractive?

What is best? Up until a year or so ago, I would have always said milling is the way to go and it still gives you premium results as it works with materials we already know and have used for years, namely PMMA. However, it does have limitations, for example, one mill can only mill one denture at a time,regardless of the size of the mill, be it base or teeth or a combination of both and some denture bases cannot be milled due to geometry limitations. It’s also quite a time-consuming process and let’s face it, milling equipment is a fairly hefty invest- Figure 1. Printed dentures. ment in both dollar terms and time spent learning the procedures. I’d love to say every digital manufacturing procedure like this was plug and play but It’s just not. Although it’s usually very good and reliable, you can get a curve ball you may well just want go back to pack and press.
With 3D printing, in comparison, the manufacturing of dentures is a lot easier and less expensive to get into and the learning curve is a little easier than with milling. You can print multiple parts at a time, for example, multiple denture bases or multiple sets of teeth. You can print any geometry so that patient with the huge anterior tissue undercut can be printed exactly. You have a choice of many materials and more and more materials are coming to market as the demand is growing. I will say the perfect 3D printable denture base material is not here yet, but things have improved so much in the last couple of years that it’s now very feasible to create a good denture with 3D printing. Figure 2. General vat polymerisation 3D printer parts.





Figure 6. ASIGA MAX UV printer.
Figure 9. UNIZ NBEE high speed MSLA printer. Figure 7. ASIGA PRO 4K printer.
Figure 10. NextDent 5100 printer. Figure 8. Formlabs Form 3 printer.
Figure 11. Ackuretta SOL printer.

Of course, we will always be comparing 3D printed dentures with the materials we know, like PMMA, but if you look a little past that comparison, you’ll find it a great addition and a fantastic way to start your digital journey.
Printer selection
Selecting a 3D printer for dentures can be confronting and difficult to the uninitiated. The main reason for this is that every manufacturer will tell you that their product is the best. They have glossy brochures, amazing websites and throw crazy numbers and statistics at you, 4K, 6K, 8K, 10-200µm layers, etc, all of which actually means nothing unless understood in context.
The internet is awash with 3D printers, especially the temptingly cheap ones that promise the world and if you want to have a dabble, by all means buy one and print some chess pieces and the like. However, once you start relying on it as an option for professional manufacturing for dentistry, you’ll most likely be sadly disappointed and look around for something better.
For polymer printing, the standard process involved uses a vat of photo polymerising resin where a light source underneath cures layers of the object being printed one at a time, gradually building up the shape. A build platform moves up in small increments, usually 50 or 100 microns, until the object is printed.








Figure 12. cara Print 4.0 from Kulzer. Figure 13. UNIZ SLASH 2 PRO. Figure 14. Pro S from SprintRay.
There are 3 main technologies: 1. SLA - Stereo Lithography; 2. DLP - Digital Light Projection; and 3. MSLA - Masked Stereo Lithography.
Essentially, the technologies are the same except for the light source. Whereas SLA uses a laser bounced off a mirror, DLP uses an ingenious array of micro mirrors to process and project a light source while MSLA uses LED lights and an LCD screen in a similar way to how an LED TV works.
Light sources
Comparing the light technologies, SLA tends to be quite a slow process as the laser has to “draw” each layer to be printed, whereas DLP and MSLA expose the entire layer all at once. So if speed is important, SLA may not be your best choice.
MSLA can print quite quickly and as mentioned, uses an LCD screen that is directly under the build platform. The formation of resin layers creates quite a lot of heat, the LCD screen therefore must be able to withstand quite high temperatures and this is why they are often cooled with fans. Some manufacturers even use liquid cooling, not unlike the cooling system to cool engines in automobiles. Eventually they fail and need to be replaced, but this a known consumable part. TABLE 1. STL File Support for 3rd Printer Manufacturer Technology Support party resins MAX UV ASIGA DLP Yes Yes PRO 4K ASIGA DLP Yes Yes Form 3 Formlabs SLA Yes No SOL Ackuretta MSLA Yes Limited Pro S SprintRay DLP Yes Limited NextDent 5100 Next Dent DLP Yes No NBEE UNIZ MSLA Yes Yes SLASH 2 PLUS UNIZ MSLA Yes Yes cara Print 4.0 Kulzer DLP Yes No
DLP can also print quite quickly but there is no contact with sensitive parts, so the heat generated potentially does not damage anything. It’s also a very reliable technology.
Other consumable parts to be aware of are resin tanks, these hold the resin and incorporate a special non-stick film within. This film wears out over time and needs to be replaced. Often you can trace misprints to the wear of this film but because it’s incredibly difficult to assess this by eye, a system that monitors it for you and advises when replacement is required is best. Of course, the resin is a consumable, but we will cover biocompatible denture resins in an upcoming article.
Accuracy
Many people ask the same question, “how accurate is the printer” and to answer that in detail, see Dental 3D printing: Is it accurate and precise? (eLABORATE Volume 18, Number 04, Jul/Aug 2021) where I have written an entire article on that subject. Always look beyond the quoted “build resolution” figure as there is way more to it than that. Suffice to say, all the quality printers available for dentistry these days show good dimensional accuracy - and possibly more importantly repeatability - and can be used to print denture bases and teeth. However, as with a lot of things in life, generally you will get what you pay for so if a printer appears to be an absolute bargain, there will be a reason why - you will sacrifice something.
PRINT MODELS IN 5 MINUTES PRINT MODELS IN 5 MINUTES
• High Efficiency Liquid Cooling• High Efficiency Liquid Cooling • Patented Micro Stereo Film• Patented Micro Stereo Film • High Power Light Source• High Power Light Source • Resin Temperature Control System• Resin Temperature Control System • Closed Loop Motor Control• Closed Loop Motor Control • Full Software Suite • Full Software Suite • Large Variety Of Dental Resins Available• Large Variety Of Dental Resins Available • Easy To Use• Easy To Use • Compact Free Standing• Compact Free Standing

Scan the QR code to see six models Scan the QR code to see six models printed in 5 minutes on the amazing printed in 5 minutes on the amazing
NBEE 3D Printer from UNIZ NBEE 3D Printer from UNIZ
Contact us today and we will show you how to integrate Contact us today and we will show you how to integrate 3D Printing into your Laboratory 3D Printing into your Laboratory 1300 878 336 1300 878 336

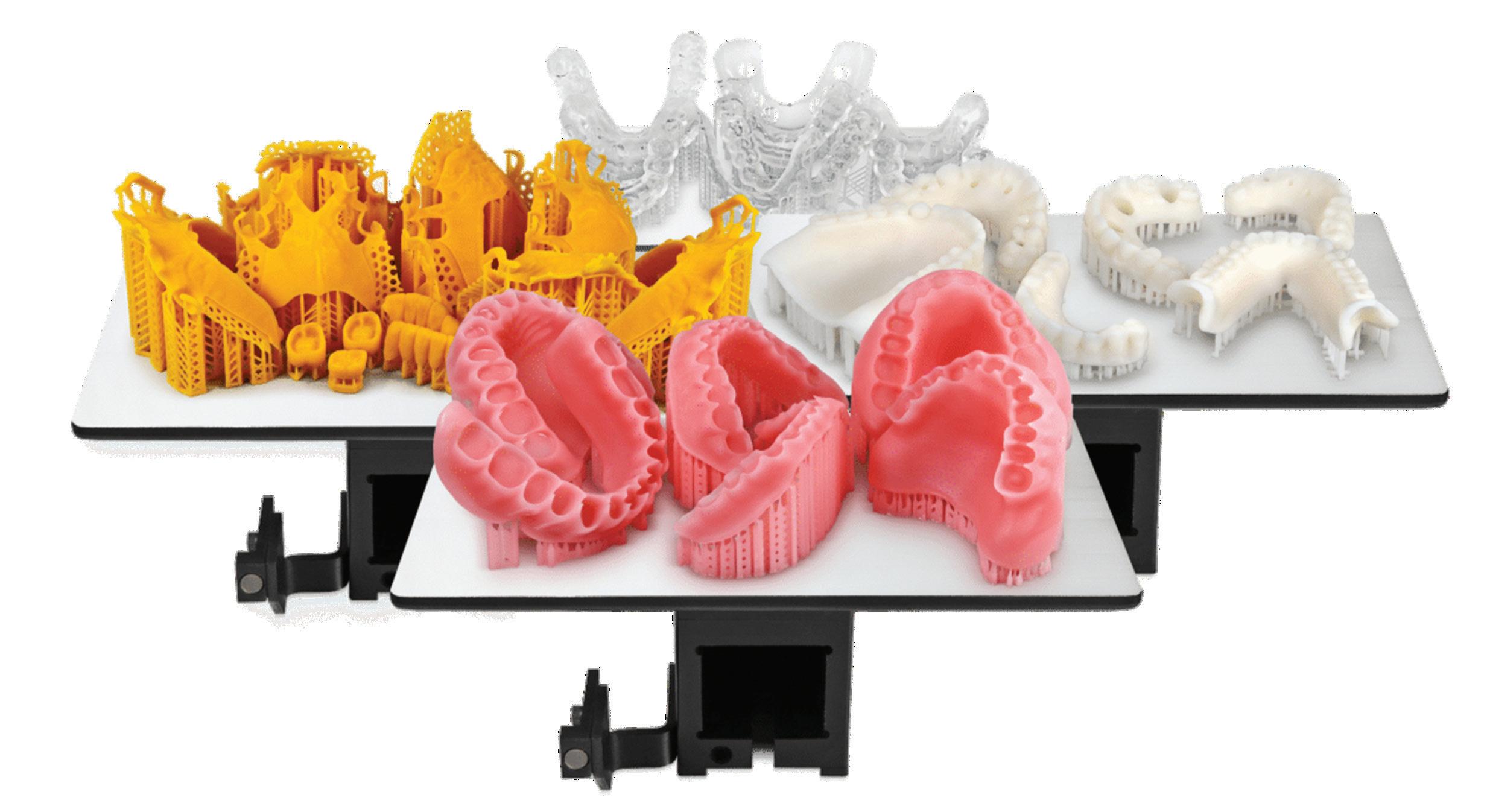

Figure 15. The applications for 3D printing in dentistry continue to expand as new materials safe for in-mouth use are released.
Materials
One really important feature of 3D printers for dentures is the ability to print materials from different manufacturers. Some printers lock you in to their resins and you cannot print 3rd party resins. Now of course, that’s a smart thing to do from one perspective; it’s like saying “use our resin and our printer and everything will be fine”. And it will usually be fine until a new breakthrough material comes to market or prices increase. What if you want to start printing new Brand X super supreme denture material?
The alternative is getting a “do all” printer, one that can print any material regardless of whether it is available now or in the future. These printers allow you to tweak any setting of the printer so you can match the parameters needed to print the desired resin. This is a good thing and allows a lot of flexibility so you must really consider this as a “must have” feature in my opinion for denture printing.
Track record
Last but not least, you have to look at the track record of the company behind the printer. Has the manufacturer been around for a while or are they a startup yet to secure its future. What is their service and support like? Do they have local agents and service centres near you (that can repair the product in Australia) and is after sales training available both online and by remote support. This is very important for digital dental technology, especially when you want to dive in to something new.
Table 1 shows a comparison of a selection of current locally available 3D printers suitable for denture manufacturing.
About the author
Terence Whitty is a well-known dental technology key opinion leader and lectures nationally and internationally on a variety of dental technology and material science subjects. He is the founder and owner of Fabdent, a busy dental laboratory in Sydney specialising in high tech manufacturing. Using the latest advances in intra- and extra-oral scanning, CAD/ CAM, milling, grinding and 3D printing, most specialties are covered including ortho, fixed and removable prosthetics, computerised implant planning and guidance, TMD, sleep appliances and paediatrics.
READ ME FOR CPD
Expectations met: hybrid abutment crown made of zirconium oxide with vestibular cut-back
When fabricating a hybrid abutment crown, the choice of material plays an important role. The framework material should provide high stability as well as having translucent properties and a tooth-like appearance. The author describes why he prefers NexxZr T Multi (Sagemax) zirconia and how he deals with the clash between high aesthetics and economic requirements
By Mark Bultmann, Master Dental Technician
Clinical work by Dr med. dent. Katharina de Buhr
Meeting expectations is part of the routine in the dental laboratory, but the challenge comes up again and again. Every patient has concrete expectations for the outcome that are driven by individual desires and specific needs. Working together with the dental practice, as dental technicians we are obliged to satisfy these expectations. In implant prosthetics we are responsible for effectively realising implant dentistry therapy with an aesthetic restoration. A delicate task for all ambitious dental technicians. To prevent excessive pressure due to placing too many demands on ourselves, we need to rely on tested processes and premium materials.
Patient case
The osseointegrated implant in position 14 required fitting with an all-ceramic crown. In theory, this can be covered in the digital workflow; increasingly, we receive the dataset from the intraoral scanner. In this case, a conventional impression was taken. The master model was digitised with the scanbody and the data uploaded into the CAD software. The decision about the type of restoration was made in agreement with the dental practice. We fabricate almost exclusively all-ceramic abutments. One-part and two-part abutments are differentiated.1-3 In this case, a hybrid abutment crown (two-part) was fabricated. The all-ceramic CAD/CAM crown was cemented onto a titanium bonding base. In contrast to the one-part zirconia abutment, the contact surface with the implant is made of titanium. This eliminates the danger of material wear caused by direct contact between zirconia on metal. Released titanium particles could lead to negative aesthetic effects on the gingiva (titanium tattooing). The hybrid abutments also have a comparably high strength or fracture load because the titanium bonding bases increase the stability.4,5
Framework fabrication
Amonolithic crown was constructed taking into account the functional criteria. A cut-back was created in the vestibular area. It is often possible to achieve a natural aesthetic without veneering with multi-layer zirconia. However, to meet the high aesthetic expectations in this case, vestibular veneering was required.
After construction, the abutment crown was milled from NexxZr T Multi (Sagemax). This multi-layer zirconia combines two generations of zirconia (3Y-TZP and 5Y-TZP). This results in a high flexural strength (1170 MPa) in the cervical region that is associated with high incisal translucency. Unlike some other multi-layer zirconia, NexxZr T Multi has a smooth colour and translucency gradient and is free of visible layers. As a result, the restorations appear very natural and in many situations monolithic implementation without aesthetic compromises is possible. To be able to optimally utilise the colour gradient when nesting, ensure that the crown is correctly positioned in the milling blank. Morphological details are touched up after the milling. Caution: Zirconia is a “delicate petal” - particularly in the white chalk-like state (before sintering) - and it must be handled with care. Do not use laboratory turbines or steam!

Figure 1. Milled hybrid abutment crown (NexxZr T Multi, Sagemax).
Figures 3 and 4. Opaquing the adhesive surfaces (screw channel) with a light blocker (LightBlock) to conceal the titanium base.

Figure 2 Manual finishing; here, removing the fissures with a square cutter.


To conceal the titanium base, the crown is coated inside the screw channel with a light blocker (LightBlock, Briegel Dental). This opaque liquid prevents the titanium base showing through without negatively affecting the translucency of the zirconia. During sintering, the liquid diffuses into the zirconia and masks the titanium base.
Completing the abutment crown
The sintered crown (NexxZr T Multi) showed the usual good fit and after sintering, had wonderful optics and a smooth colour gradient. The vestibular veneering (ZI-CT, Creation) was performed in five steps. For the first firing - Frame Shade bonding agent - the veneering surface was coated with a high-fusing, fluorescing ceramic material. The second firing is similar to the wash firing. Using the sprinkle technique, fluorescing shoulder material was sprinkled onto the framework. This produces a slightly roughened or glazed surface that creates vivid colours and supports the bond between the zirconia and the veneering ceramic. For the dentine firing, the crown was coated with the dentine and enamel materials. Because NexxZr T Multi has a tooth-like colour already, only a thin veneer layer is necessary. This step was followed by a corrective firing and, after working the surface texture, by the final glaze firing.
Cementation of the titanium base and insertion
Cementing a crown to the titanium base requires a reliable protocol because the bond determines the long-term success. Blasting and conditioning of the titanium base and the zirconia adhesive surface and cementation with the luting composite (Multilink Hybrid Abutment, Ivoclar) were performed according to the information from the manufacturer. Thorough removal of residual composite near the cementation joint followed manual polishing of the basal parts. A certain micro-roughness is recommended in the transmucosal area to encourage the growth of the gingiva while at the same time counteracting the deposition of plaque.3 A final check on the model confirms the fit and correct adjustment of the proximal contact surfaces. The restoration was sent to the practice and screwed occlusally into the patient’s mouth.

Figure 5a. Immediately after the sintering: Wonderful aesthetic properties with a smooth colour and translucency gradient. Figure 5b. Familiar precise fit of a restoration made from NexxZr T zirconia.





Figure 6a and b. Preparation of the surface for the vestibular veneering: “Sprinkle technique” - sprinkling of fluorescing shoulder material for a vivid internal colour. Figure 7. Veneering completed and finalised after working the surface texture.
Conclusion
The exceptionally natural appearance of the light optics of the hybrid abutment crown is confirmed intraorally. The restoration appears warm and vibrant from the inside out. The titanium base is completely concealed; nevertheless, the crown has a beautiful translucency. In theory, NexxZr T Multi and its colour and translucency gradient allow the fabrication of monolithic restorations. Because the esthetic demands in this case were high, vestibular thin-layer veneering was carried out. The functional surfaces remain monolithic, which provides a high level of protection against chipping. The expectations of the patient were met in full. The implant dentistry therapy is successfully completed. At the same time, this efficient method of fabrication is in accord with the economic requirements of the dental laboratory.
References
1. Gehrke P, Dhom G, Brunner J, Wolf D, Degidi M, Piattelli A. Zirconium implant abutments: fracture strength and influence of cyclic loading on retaining-screw loosening. Quintessence Int 2006; 37:19–26 2. Gehrke P, Johannson D, Fischer C, Stawarczyk B, Beuer F. In vitro fatigue and fracture resistance of one- and two- piece CAD/CAM zirconia implant abutments. Int J Oral Maxillofac Implants 2015; 30:546–554. 3. Gehrke P, Kaiser W, Fischer C. Comparative analysis of surface topography of custom of CAD/CAM zircona abutments by means of optical profilometry. In progress. 4. Stimmelmayr M, Sagerer S, Erdelt K, Beuer F. In vitro fatigue and fracture strength testing of one-piece zirconia implant abutments and zirconia implant abutments connected to titanium cores. Int J Oral Maxillofac Implants 2013; 28:488–493. 5. Yilmaz B, Salaita LG, Seidt JD, McGlumphy EA, Clelland NL. Load to failure of different zirconia abutments for an internal hexagon implant. J Prosthet Dent 2015; 114:373–377.

Figure 8. Cementation of the hybrid abutment crown onto the titanium base.

Figure 10. Hybrid abutment crown cemented on the titanium base, prepared for screwing into the patient’s mouth. Figure 9. Fit check on the model.

Figure 11. Restoration after being screwed onto the implant at position 14.

About the author
Mark Bultmann is a master dental technician and owner of Via Denta GmbH, a dental laboratory founded in March 2006 in Germany. He believes in taking a holistic approach to patient care and designing restorations based on comprehensive scientific backing and research.
Dr med. dent. Katharina de Buhr studied dentistry at the University of Ulm. She currently works in her own private dental practice Zahnwerk Westerstede in Westerstede, Germany.
For more info, contact Impulsedent Australia on 1300-303-638 or (07) 3200-4750 or visit www.impulsedent.com.au.
NexxZr+ Multi multilayer zirconia
Sagemax NexxZr T Multi is the latest generation multilayer zirconia (3Y-TZP cervical, 5Y-TZP incisal). The combination of the very high flexural strength (1170 MPa cervical, 630 MPa incisal) and the smooth gradient of colour and translucency makes the difference. This combination offers optimal conditions for the fabricat- ion of monolithic or anatomically reduced single-tooth and bridge restorations.
Choosing a thermoforming machine
By Peter Herring, Adv Dip Dent Tech, ACCDP
Whether you are new to thermoforming or an experienced user, today’s market gives you plenty of choice of equipment. There are options of pressure forming, vacuum forming, automation, attachments, a wide range of price points and so on.
When choosing a thermoforming machine, it’s tempting to start with comparing the machinery or fitting to a budget but in my opinion, the best starting point is with the question “What do I want to use the machine for now and into the anticipated future”. Finding the best thermoforming unit to answer this question will set you on a path for success in the longer term.
So, what do you want to make?
Mouthguards, splints, impression trays, base plates, temporary crowns and bridges, orthodontic appliances, snore guards, bleach trays, temporary dentures, surgical guides and more, the applications for dental thermoforming are expansive and engages a wide range of skill levels and equipment needs. As examples, a surgery which wants to add the simple capability of in-house whitening trays, retainers, mouthguards and the occasional splint will need a machine that can be easily operated by multiple staff with minimal training and would be best served by an automatic rapid vacuum unit. An orthodontic practice producing quantities of retainers and aligners on 3D printed models may prefer a “plug and play” automatic pressure unit. While a production laboratory might use both a rapid vacuum unit and a pressure unit to take advantage of each machines’ strengths.
So when considering which machine to purchase, it’s important to choose the unit that is best suited to produce the appliances that you want to make now and also to try and predict what you may wish to produce in the future.
Pressure or vacuum?
Both pressure and vacuum thermoforming units broadly achieve the same result but each has unique characteristics that predispose them to suit different use cases and environments.

With Erkopress - automatic pressure forming - the material is “pushed” onto the model in a closed chamber. If the forming pressure is high enough, there are always good results. With Erkoform - automatic rapid vacuum - the material is “pulled” onto the model and accessible during the forming process. Rapid (sudden) vacuum gives results clinically equivalent to pressure.

Pressure machines operate either from an external compressed air supply or via an inbuilt compressor, operating at pressures of up 6 atmospheres.
With pressure, there is the advantage of very high thermoforming power but with the disadvantage that more attention to model quality and blocking out procedures is required. The model is not accessible during the forming process and a clean supply of compressed air may be required. These machines are the “universal” thermoforming machines and can be used to make any appliance. They are most often used by commercial dental laboratories that have good facilities for high quality model production and well trained operators and for orthodontic surgeries where the machines with inbuilt air compressors provide a “plug and play” automatic pressure solution.
Pressure machines are recommended for use by more experienced operators and are especially good for orthodontic bracket transfer appliances, retainers/aligners on printed models and essential for techniques that involve self cure acrylics.
Automatic rapid vacuum machines are widely used in both labs and surgeries. Requiring no external air supply, they operate by accumulating a vacuum in an internal reservoir using a self-contained vacuum pump. When the heating cycle is complete, the automatic forming process brings the foil to the model and the stored vacuum is released, thereby forming the foil rapidly downwards over the model. It is this rapid forming process that allows the creation of the detail and fit which is clinically the equivalent to pressure forming. The rapid vacuum machines have the advantage of requiring no compressed
About the author
air supply, are quiet, easy-to-use and leave the model accessible during the forming process. Access to the model allows the use of optional articulator type attachments which make it possible to add the bite into a splint or mouthguard at the same time as thermoforming is taking place.
The less aggressive nature of these machines can make appliances, in particular hard retainers and splints, more passive and comfortable for patients to wear. Model quality is less particular than with the pressure units.
These machines are preferred for general production of bleach trays, splints (with articulator type attachment), laminated “Playsafe” type mouthguards, custom trays, orthodontic retainers, etc. The automatic operation and ease of use makes these machines more suitable for use by a variety of dental office staff.
Peter Herring is a dental technician, prosthetist and a regular contributor to eLABORATE. He is the Australasian and Indonesian distributor for Erkodent products and spends his time between offices in Perth and Bali. He also operates a busy Australian lab dedicated to thermoformed appliances. He can be contacted at pjh@erkodent.com.au or for general enquires, call Freecall 1800-242-634.



