7 minute read
Navigating the Pandemic
Innovation
The COVID-19 pandemic put enormous strain on the hospital, physician group, staff, and ancillary groups. Our shared UI Health COVID-19 journey has taught us the importance of collaboration, dynamic surge and staffing models as well as the need to use technology to extend our specialists across a larger inpatient census.
Continuing On The Front Lines
The entire ID faculty continued to be engaged in the response to COVID-19. Dr. Susan Bleasdale, as director of infection control, and chief quality officer for UI Health, with the assistance of Dr. Scott Borgetti, assistant director of infection control, continues to lead the medical center at large on policy changes to the evolving pandemic. While the routines in the medical center continue, they have worked tirelessly behind the scenes to keep up with changes in infection control guidelines and treatment practices.
Dr. Susan Bleasdale continued to be a key consultant to the Illinois Department of Public Health (IDPH) and continued to work with university leadership providing guidance on how to keep campus activities open and safe.
The city's Strike Team response to outbreaks in homeless shelters, long term care facilities and other congregate settings in collaboration with the College of Nursing was led by Dr. Stockton Mayer. Dr. Mayer’s team was awarded a new contract with Chicago Department of Public Health (CDPH) that will expand testing and vaccination beyond COVID-19. The University will serve as a community-based outbreak response team, investigating outbreaks of influenza, legionella, candida auris, and other pathogens.
Dr. Scott Borgetti helped develop and implement the clinical program for COVID-19 outpatient management, which continues to evolve as new treatments come on line, and provides guidance to the treatment team.
In addition to providing clinical, organizational and policy leadership, infectious diseases faculty continued to move the coronavirus research agenda forward.

Dr. Richard Novak, chief of the division of infectious diseases, became an investigator for the Coronavirus Prevention Network and leads the ongoing Moderna COVID vaccine trial, and the Janssen Ensemble vaccine trial. Dr. Novak collaborated with OB/GYN and pediatrics on the Momivax study to understand vaccine effects on both pregnant women and their newborn children.
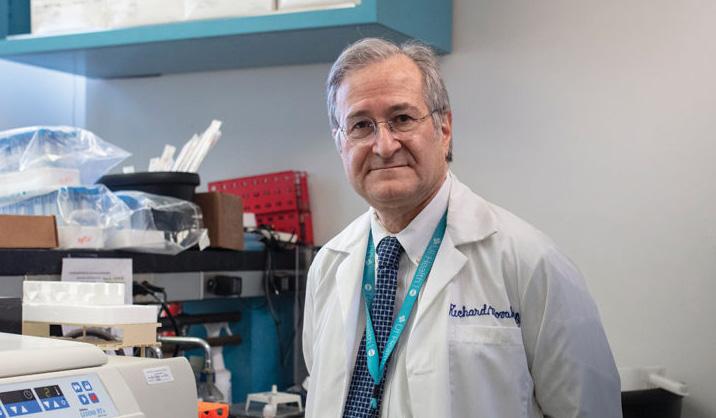
Dr. Borgetti leads the CPAT study of vaccine booster doses in organ transplant recipients. All members of the ID faculty as well as fellows contribute to the research effort, evaluating study participants and conducting study visits. Any time not committed to clinical work or committees are devoted to these research efforts. Dr. Novak was honored this year by the dean with a Distinguished Service Award. Drs. Novak, Bleasdale, and Jerry Krishnan were honored by the University of Illinois President with the Presidential Medallion award.
Post Covid Clinic
In June 2021, a new Post-COVID Clinic began seeing patients at the University Village Primary & Specialty Care Clinic and the Outpatient Care Center. The multidisciplinary clinic for COVID-19 long haulers, patients who previously had COVID-19 and still experience long-lasting symptoms, brought together a variety of specialties — primary care, pulmonology, nephrology, neurology, immunology, and rheumatology. Unique to the clinic is the critical role of the patient care navigator who coordinates a patient’s care across specialists and assists with activities like appointment scheduling. Our physicians are dedicated to helping patients manage their chronic symptoms as a result of COVID-19.
Nephrology Care
The Division of Nephrology faced unique challenges posed by the Omicron surge. Not only was there an increased demand for in-patient dialysis services due to the influx of critically ill patients, but the division faced critical staffing shortages. Working closely with hospital leadership and Infection Control, Dr. Claudia Lora (medical director of the Dialysis Unit) and Mary Ann Medina, RN (director of Patient Care Services for Dialysis) addressed these challenges by coordinating a successful multidisciplinary effort which included nephrology faculty, fellows, as well as dialysis technicians and nurses.
Coping With Covid
The COVID-19 pandemic offered numerous challenges which required the Division of Gastroenterology and Hepatology staff to adapt the way we provide patient care and also the way we interact with each other. One of the highlights of the calendar year was the fellows graduation, which takes place every June and typically includes a celebratory dinner and speeches. In 2020, the division resorted to a backup plan by Zoom meeting, which was still sentimental but understandably muted.
This past June saw the return of an in-person ceremony for graduating fellows Mitali Agarwal, Najib Nassani, and Dino Melitas. Using masks, socially distanced seating and boxed meals, we were able to combine appropriate precautions (at the cusp of the onset of the Delta variant), with a shared space which allowed us to more properly celebrate the accomplishments of our departing trainees.
ADVANCED PRACTICE PROVIDERS (APP)
During a time of unprecedented change in the world around us, the DOM APP’s have met this change with professionalism and resilience. In the face of the pandemic, our APP’s have stepped up to meet the issues facing all providers, from extending your clinic practice, staffing the vaccine clinics, moving to telehealth and rounding on the inpatient medicine teams. We had another year of growth, as we continued to add APP’s to the DOM to expand clinical practice and develop new programs.
MONKEY POX AND COVID-19
In the midst of one pandemic, the Outbreak Response Team, co-led by Stockton Mayer, assistant professor in the UIC College of Medicine and UIC Nursing assistant professor Rebecca Singer coordinated a mass vaccination event that provided nearly 1,200 people with monkeypox vaccinations at UIC in August 2022.
Through a partnership with Rush University and UIC, a team of 90 people was formed, many of whom were volunteering their time.
The Outbreak Response Team is an extension of the COVID Rapid Response Team, which was formed to provide testing and vaccinations in high-risk and underserved parts of Chicago.
2021 FELLOW OF THE YEAR - PULMONARY MEDICINE
The Fellow of the Year personifies the core values of UI Health: Compassion, Accountability, Respect, and Excellence. These physicians put their patients first in all encounters and consistently contribute to the delivery of world class patient care.
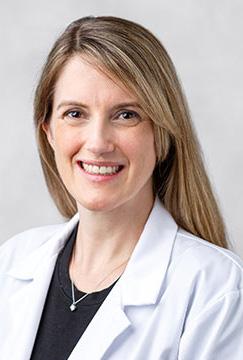
Dr. Christen Vagts is the ultimate example of what it means to live up to our clinical mission in everyday work. Dr. Vagts spent several weeks directly caring for our sickest COVID-19 patients. During the most difficult and grueling clinical work, she served on the front line in an environment that posed significant risk to our providers. She cared for patients with this lifethreatening illness — one we did not fully understand, had limited ability to treat, and at the time, very limited PPE — with leadership and excellence. She took on extra clinical obligations, and because of her leadership we were able to deliver the highest levels of patient care and provider safety.
Dr. Vagts is an exemplary fellow who has demonstrated a high degree of passion for her work, including a dedication to her dual roles as educator and clinician. She has the promise of a remarkable career going forward.
EVEN DURING A PANDEMIC, ”HARVEY” CONTINUES TEACHING UIC MEDICAL STUDENTS
Over the last 31 years, Dr. George Kondos, professor and interim head in the Department of Medicine, has taught thousands of first-year University of Illinois Chicago medical students how to perform the cardiovascular physical exam using a highly advanced simulator who goes by the name Harvey.
Dr. Kondos typically conducts the teaching sessions inperson, but with COVID-19, these in-person teaching sessions needed to be converted to virtual teaching sessions. This was not an easy task since heart sounds and other subtle physical exam findings need to be displayed so students would understand the difference between a normal patient and a patient with one of the various cardiac diseases.
Harvey is a lifesize manikin able to simulate 50 different cardiovascular diseases through heart sounds and lifelike pulses in the neck and chest. It serves as a simulator for students to be able to hear sounds mimicking various diseases and feel the pulse that would correspond to these diseases.
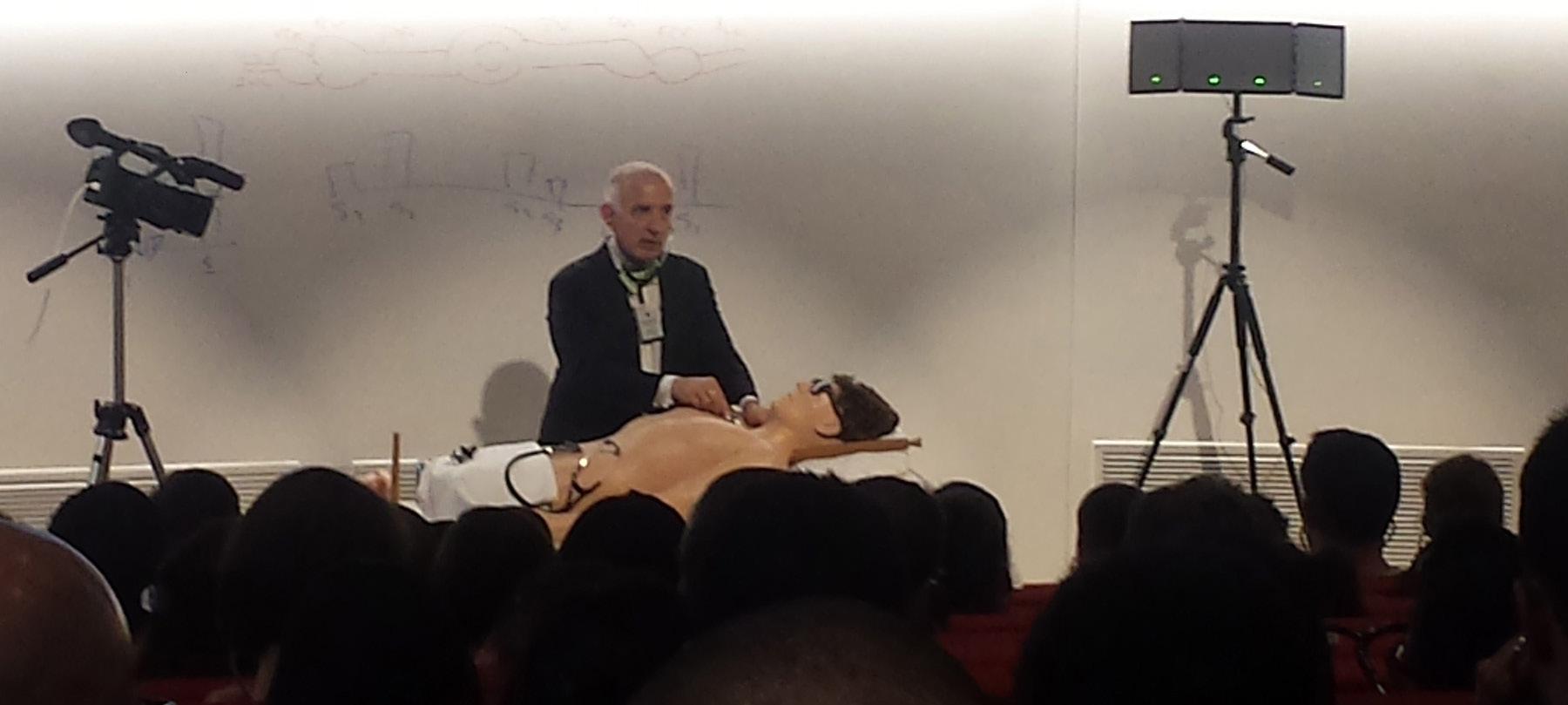
“You can give 20 common heart sounds and murmurs to primary care physicians and they’ll get about 10% of them correct, and that’s because they’ve never been really taught how to listen to the heart sounds,” said Kondos.
Comparing Harvey to airplane simulators that have taught pilots how to react to events in the air from the safety of the ground, Dr. Kondos said Harvey is used to train young doctors how to assess and treat a patient by simulating conditions a new doctor would confront bedside with a patient.
Normally, Harvey would join Dr. Kondos as he traveled to the College of Medicine’s Peoria, Rockford and UIC campuses, where he would teach more than 300 students yearly. Prior to the pandemic when he would have had to drive to each of the campuses, he would give the same lessons independently to the students on each of the campuses. He previously conducted the sessions surrounded by the students, who would break out into small groups.
Since COVID-19 forced teaching to go virtual, Harvey, which was developed by UIC College of Medicine Class of ’61 alum Michael Gordon, also has was forced to do its teaching online.
“Obviously COVID made a little bit of a problem for us, but we converted it from an actual in-person course to an online course,” said Kondos. “I ran them through the normal physical and gave them findings of the abnormal physical exam.”
Kondos used Harvey to simultaneously teach more than 300 students — 182 in Chicago, 55 in Rockford and 66 students in Peoria — who took part in an online cardiology plenary course introducing them to the cardiac exam.
He did this by using various examples that students could see virtually; for example, he used cotton swabs to dramatize the strength of the carotid pulse by laying the stick of the swab flat across Harvey’s neck as the pulse sent the stick and swab tip moving up and down along with the sound of the pulse.
“Even though you don’t have the actual patient here, you can simulate to students what they are actually seeing and hearing and can show students various examples of disease states,” Kondos said. “We all recognize simulators are no substitute for a real patient. However, if you can’t make the diagnosis on a simulator you probably would miss the diagnosis on a real patient.”
One of the benefits that happened with them having to go online is that it allowed it to become more manageable.
“Many times these class sizes are so big that everybody can’t really see everything and these are subtle kinds of things that you’re showing,” Kondos said. “So with Harvey, it’s actually helped because here the students can see, they can hear — probably better than they can in a large group — and you can engage them in discussion.”