5 Simple Tips to Improve your Health if You Have Long COVID: In-Depth
1. Pay attention to your body
In my 22 years of practice dedicated to people with complex, chronic diseases, I’ve seen that people who take time to observe and chart their symptoms make the best decisions when it comes to choosing which self-management strategies to try.
• You can use a wearable tracker like a Fitbit, Oura ring, or an Apple watch.
• But you don’t need a fancy tracker or App. You can take a piece of paper (ideally in a notebook so you don’t lose it), choose the symptom area you are most interested in learning about, and start writing down what you notice every day. You can find example symptom charts in my manual Let Your Light Shine Through.
After observing one aspect of your health for 2 weeks, you are likely to notice patterns, such as what makes the symptom better or worse. This allows you to choose effective interventions.
2. Align Your Mindset with Your Goals
How we think about ourselves, our lives, and our health has powerful biological effects. People who are successful in improving their health have certain things in common
• They believe that improvement is possible. In the case of Long COVID, this belief is supported by 40 years of research on ME/CFS. Many of the same strategies tried and tested in ME are equally effective for Long COVID.
• They work to emotionally accept their circumstances no matter how dire. Paradoxically, accepting current reality is necessary to move ahead and improve health.
• They spend time each day thinking about and doing activities that elevate their mood Feelings of safety and joy decrease the brain’s ability to process pain and other symptoms related to the danger alarm system (fight/flight).
3. Pacing
Students in my courses vote “pacing” as the single most effective skill they’ve learned. ME/CFS and likely Long COVID are disorders of insufficient cellular energy. Even if you are on supplement protocols to support your energy, learning to pace is a foundational skill.
Pacing means adjusting your daily activities to match your energy envelope rather than pushing through to get the task done. It means avoiding crashes so that your body always has a bit of energy in the tank to begin rebuilding. Four essential pacing strategies include the following:
• Chunk activities into small parts and set a timer if you need to be reminded to take a break.
5 Simple Tips to Improve Your Health if You Have Long COVID 4 © Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
• Switch from cognitive to emotional to physical tasks to allow some body systems to rest and recover while other systems are engaged in completing tasks; this allows you to be more productive.
• Rest before starting task to help you complete them without crashing. Even if you’re not exhausted, rest after a task to help you refill your tank. And, for the severely ill, restorative resting each day is extremely helpful. I refer to resting as lying horizontal with eyes and ears closed so that both your body and your brain can recharge.
• Be alert for early warning signs that you’ve overdone it; this is critical. These signs are quite individual. Notice how your body tries to communicate that it’s running out of energy. Write these signs and symptoms on the list in bold letters and put it in a prominent location to remind you to STOP when you experience them.
4. Sleep
Sleep is your biggest energy and memory regenerator. Without it, you cannot activate the healing cycle. People are consistently amazed by how a few simple changes to sleep behavior help them wake more refreshed. Here are three core strategies to sleep and feel better.
• Get out of bed if you are lying awake for more than 20 minutes. This rewires your brain and reverses unconscious conditioning that connects your bed with wakeful activities.
• Get up at the same time each morning and go outside to get 10 minutes of sunlight in the first hour after dawn.
• Develop an evening practice to calm your nervous system. The most accessible practice at any time of day or night is paced breathing. Slow your exhales so that they’re longer than your inhales. Or try box breathing for which you breathe in for a certain count say four seconds, hold your breath for four seconds, breathe out for four seconds, and hold again for four seconds before breathing in. Other evidence-based tools to calm the nervous system include mindful movement, yoga nidra, meditation, and self-hypnosis. Tens of thousands of free online resources can help you easily find effective tools that appeal to you.
5. Neuroplasticity
Every thought, feeling, and action we experience changes the physical structure and function of our brains. If you understand how neuroplasticity works, you can take charge of this powerful process to rewire your brain for better health.
Anything that is caused by neuroplasticity can be reversed by a neuroplasticity-based practice. Because the brain controls every aspect of our mental and physical function—such as the release of neurotransmitters, hormones, and immune molecules learning to rewire the brain gives us considerable influence over our biology. Here’s how to get started:
5 Simple Tips to Improve Your Health if You Have Long COVID 5
© Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
• Use each awareness of a symptom, say chronic pain, as a reminder to make a choice.
• Rather than react to your symptoms in your habitual way (e.g., withdrawal, upset, and fear), decide instead to focus your attention on a thought, feeling, or activity that makes you feel good. This shifts your brain from danger mode to safety mode.
• Do things you enjoy. Neurons cannot do two things at once; therefore, if you keep your neurons busy doing enjoyable things that bring meaning, connection, and fulfilment to your life, they will be too busy to process pain and other soul-destroying symptoms.
Common Symptoms of ME/CFS and Long COVID
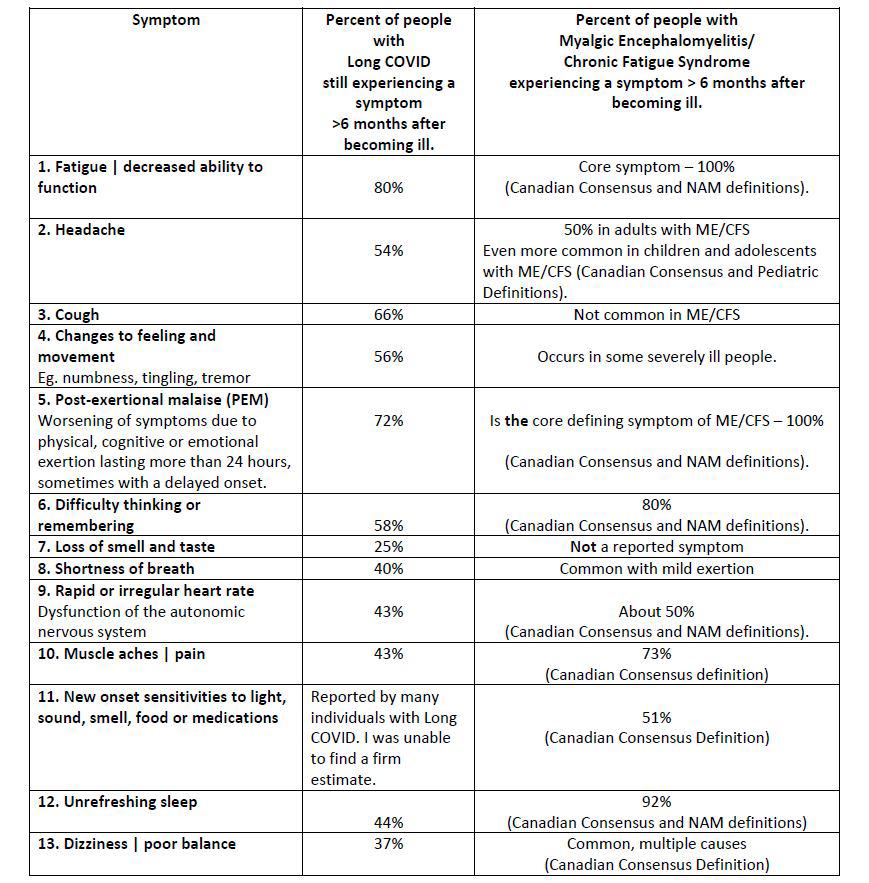
One of the most detailed studies of Long COVID symptoms was a collaboration between patients in the Body Politic patient-led research collaborative and researchers at several prestigious universities (Davis et al., 2021) This study lists the most common symptoms reported by people with Long COVID and includes many symptoms overlooked by other studies that don’t include patient partners in the research design
The table below compares the rates of the most common symptoms in Long COVID as measured by Davis et al. (2021) and those in ME/CFS as reported by the National Institute of Medicine in an exhaustive study (NAM, 2015). The rates are similar, adding to the biological evidence that these conditions are similar; it stands to reason, then, that patients with Long COVID will respond to treatments developed for ME/CFS. And in my clinical experience over the past 2 years, this is what patients report. They feel understood and at home in my groups designed for people with ME/CFS, and they benefit from the same strategies.
Look at the most common symptoms of ME/CFS and Long COVID and see if what you experience is a match. If it is, keep reading to learn more about the biology of your condition and what you can do to improve it.
5 Simple Tips to Improve Your Health if You Have Long COVID 6
© Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
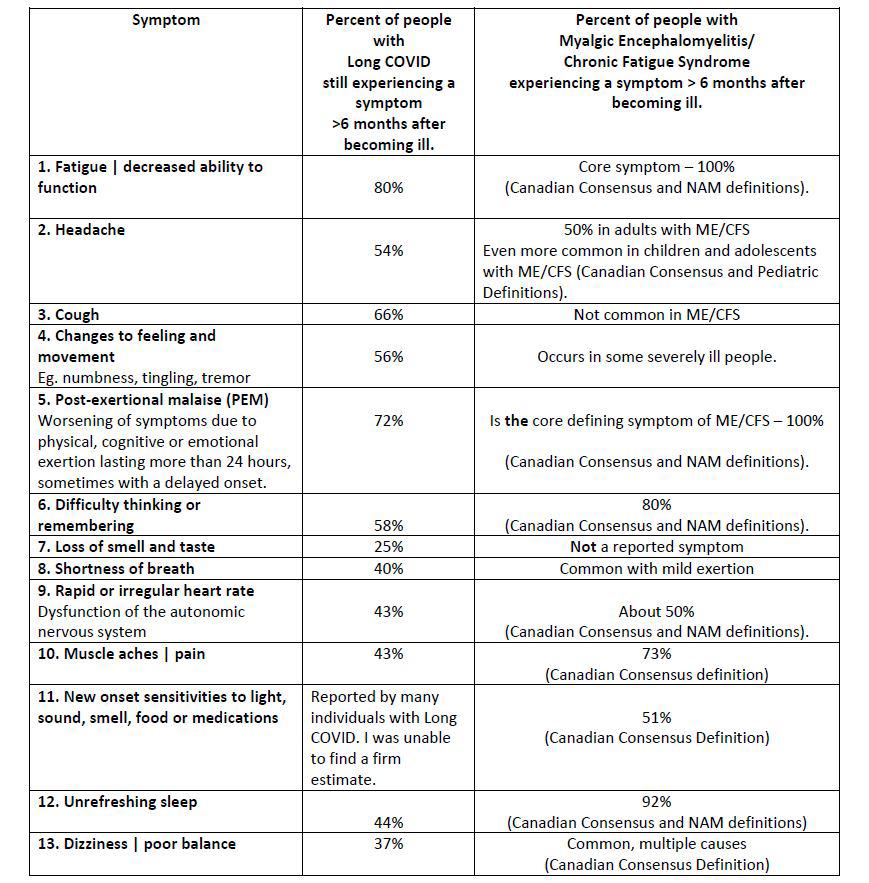
If you have five or more of these symptoms, chances are you have ME/CFS and/or Long COVID, and I can help you on the path to recovery. Based on over 30 years of personal and professional experience with ME/CFS and related conditions, I teach people with chronic, complex diseases how to identify and manage symptoms to improve health and get back to the life they love.
Improvement is the rule, not the exception
THE COURSE
5 Simple Tips to Improve Your Health if You Have Long COVID 7 ©
Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
GET
The Story Behind the 5 Simple Tips
In 1989, I became ill with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), fibromyalgia, multiple chemical sensitivities, and several comorbidities. My illnesses meant that every moment of every day was challenging. I slept for as many as 18 hours a day and still woke up unrefreshed. My brain was so fuzzy that I couldn’t do the simplest cognitive tasks. And the chronic pain sucked the joy out of life.
At that time, there were no experts. ME/CFS had been defined only the year before, and Fibromyalgia was considered suspect by many health care professionals. With no guidance, over the next 27 years, I tried everything I could afford, including off-label use of conventional drugs, extensive functional and environmental medicine testing, oodles of supplements, intravenous treatments, and experimental drugs. Although these things helped stabilize my health, they didn’t improve it enough to fully enjoy life and return to the things I loved.
Then in September 2017, I suddenly realized that my health had improved. I was waking up earlier, working more hours in the day, enjoying activities in the evenings, and going to bed later. My cognitive function improved, and sleep was more restorative. I was able to increase my physical activities without pain flares or energy crashes.
What was striking about this experience is that, at the time, I wasn’t doing any fancy protocols or taking any new supplements or new medications. I was paying close attention to selfmanagement, was trying a new diet, and had a daily neuroplasticity practice.
Encouraged, I began reading scientific literature about neuroplasticity and how it can be used to change biology and improve health. I learned that we have much more power to change our biology than I had realized. I began sharing what I was learning with my patients. And they also started improving.
I began changing the language I used with my patients. Instead of agreeing that they were unlikely to get better, I challenged their belief and used my own experience as an example. I began teaching them strategies to rewire their brains and shift their mindset. Patients, who had plateaued for years, began to improve. People began reporting better sleep; more energy and fewer crashes; less pain; less sensitivity to chemicals, light, and sound; and an improved mood and outlook.
What I Have Learned
ME/CFS and Long COVID are biomedical conditions caused by measurable changes in multiple body systems including the immune system, the cardiovascular system, the central nervous system, and many more. Self-management, also called lifestyle modification, has powerful biological effects on these systems and can help you feel better and live more fully.
What Makes Me so Optimistic?
My optimism is based on my lived experience and that of thousands of patients I’ve worked with over the past 22 years. It took me 27 years to substantially recover from my severe
5 Simple Tips to Improve Your Health if You Have Long COVID 8 ©
Stein
FRCP(C) eleanorsteinmd.ca/pathways
Dr. Eleanor
MD,
symptoms. There was a lot of trial and error and a lot of false leads. I want to try to help you learn how to improve your chronic pain much more quickly. If there’s one thing, I’d like you to take away from this story, it’s hope. Hope is a powerful thing. Hope can give you the strength to keep going when you feel like you can't. Hope can help you to see the light at the end of the tunnel. Hope can change your entire outlook on life.
If you are struggling with chronic pain and other debilitating symptoms, it is important to remember that there is always hope. Hope that you will get better. Hope that you will find a way to manage your disease. Hope that you will one day be able to live a full and healthy life again.
Here are the building blocks for a strong health foundation if you have Long COVID and ME/CFS
• Discover the Biology of Changing your Brain and Body Using Neuroplasticity, Epigenetics, and the Microbiome.
• Learn how to Use the Brain to Help Heal the Body
• Confidently Confirm Your Diagnosis
• Develop Regenerative Sleep Practices
• Manage Energy and Activity with Pacing
• Learn the Diet that Feeds, not Drains
• Implement the Secrets to Reversing Persistent Pain
• Overcome Environmental Sensitivities
• Successfully Ride the Wave of Emotions and Stress
Whether you decide to work with me or another practitioner, look for a program that helps you with the above goals. Recovery from Long COVID and/or ME/CFS requires you to consider each of these areas. Each is like a puzzle piece. To recover, you have to fit the pieces together to create a clear, beautiful image of health.
© Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
5 Simple Tips to Improve Your Health if You Have Long COVID 9
Why do Long COVID and ME/CFS have similar symptoms? The Science
There is a growing body of research showing that the underlying biology of Long COVID and ME/CFS has similarities. This is a summary of some intriguing findings.
Immune activation (inflammation) is commonly reported in both ME/CFS and Long COVID. The research suggests that immune activation lasting beyond the period of active infection plays a role in both conditions (Sukocheva et al., 2022). Inflammation is associated with many of the common symptoms. Neuroinflammation may be associated with sensitivities, vibration, brain fog, and dizziness.
Impaired mitochondrial function associated with decreased energy production is frequent research finding in ME/CFS. In Long COVID, there is indirect evidence of impaired mitochondrial function through altered balance of oxidation and reduction and low levels of antioxidants (Komaroff & Lipkin, 2021). Decreased energy production may contribute to fatigue and PEM.
Microclots Research in both ME/CFS and Long COVID suggests small blood clots exist and could be related to symptoms such as cold limbs and organ dysfunction (Kell, Laubscher, & Pretorius, 2022; Nunes, Kruger, Proal, Kell, & Pretorius, 2022).
Changes in brain function – In Long COVID, PET scan studies show evidence of a disrupted blood-brain barrier, neuroinflammation, and decreased brain metabolism. In ME/CFS there is extensive evidence of decreased blood flow to the brain and changes in brainstem connectivity. It will require studying both groups together with the same tests to see if the changes to brain function in ME/CFS and Long COVID are the same or different (Sukocheva et al., 2022). Changes in brain blood flow may explain the brain fog, vibration, sensitivities, altered sensation, and dizziness.
Changes in the microbiome (bacteria in the large bowel) have been reported in both Long COVID and ME/CFS. The organisms that live in and on us produce molecules which travel throughout the body and cause almost any symptom (Komaroff & Lipkin, 2021).
Changes to blood flow to and from the heart Dr. David Systrom from Harvard University reports insufficient blood return to the heart (preload failure) on invasive cardiopulmonary exercise testing in both ME/CFS and Long COVID (Joseph et al., 2022; Novak et al., 2022). This may be associated with fatigue, PEM, rapid and irregular heartbeat, shortness of breath, and brain fog.
© Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
5 Simple Tips to Improve Your Health if You Have Long COVID 10
References for Diagnostic Criteria of Long COVID and ME/CFS
Canadian Consensus Criteria - Carruthers, B. M., Jain, A. K., De Meirleir, K., Peterson, D. L., Klimas, N., Lerner, A. M., et al. (2003). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical working case definition diagnostic and treatment protocols - A consensus document. Journal of Chronic Fatigue Syndrome, 11(1), 7-116.
Symptoms of Long COVID - Davis, H. E., Assaf, G. S., McCorkell, L., Wei, H., Low, R. J., Re'em, Y., et al. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine, 38.
National Academy of Medicine Criteria - Institute of Medicine. (2015). Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness: The National Academies Press.
Pediatric Criteria for ME/CFS - Rowe, P. C., Underhill, R. A., Friedman, K. J., Gurwitt, A., Medow, M. S., Schwartz, M. S., et al. (2017). Myalgic encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer. Frontiers in Pediatrics, 5.
References on the Biology of Long COVID and ME/CFS
Davis, H. E., Assaf, G. S., McCorkell, L., Wei, H., Low, R. J., Re'em, Y., et al. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine, 38.
Joseph, P., Pari, R., Miller, S., Warren, A., Stovall, M. C., Squires, J., et al. (2022). Neurovascular Dysregulation and Acute Exercise Intolerance in ME/CFS: A Randomized, PlaceboControlled Trial of Pyridostigmine. Chest, 06, 06.
Kell, D. B., Laubscher, G. J., & Pretorius, E. (2022). A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications. Biochem J, 479(4), 537–559.
Komaroff, A. L., & Lipkin, W. I. (2021). Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends in Molecular Medicine, 27(9), 895–906.
Novak, P., Giannetti, M. P., Weller, E., Hamilton, M. J., Mukerji, S. S., Alabsi, H. S., et al. (2022). Network autonomic analysis of post-acute sequelae of COVID-19 and postural tachycardia syndrome. Neurol Sci, 1–12.
Nunes, J. M., Kruger, A., Proal, A., Kell, D. B., & Pretorius, E. (2022). The Occurrence of Hyperactivated Platelets and Fibrinaloid Microclots in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Pharmaceuticals, 15(8), 931.
Sukocheva, O. A., Maksoud, R., Beeraka, N. M., Madhunapantula, S. V., Sinelnikov, M., Nikolenko, V. N., et al. (2022). Analysis of post COVID-19 condition and its overlap with myalgic encephalomyelitis/chronic fatigue syndrome. Journal of Advanced Research, 40, 179–196.
© Dr. Eleanor Stein MD, FRCP(C) eleanorsteinmd.ca/pathways
5 Simple Tips to Improve Your Health if You Have Long COVID 11