
BY DR. JOEL “GATOR” WARSH
Author of Parenting at Your Child’s Pace @DrJoelGator


BY DR. JOEL “GATOR” WARSH
Author of Parenting at Your Child’s Pace @DrJoelGator
Introduction
Overview of Gut Health: Importance of gut health for overall well-being.
Purpose of the Guide: Empower families with knowledge and practical strategies.
Chapter 1: Understanding the Gut
Basic Anatomy: Quick overview of the gastrointestinal system.
The Gut Microbiome: What it is and why it matters.
How Gut Health Affects the Body: Impact on immunity, mood, and more.
Development of the Gut Microbiome: From infancy to adolescence.
Common Gut Issues in Children: Symptoms and when to seek help.
The Role of Nutrition: How diet influences children’s gut health.
Chapter 3: Nutritional Foundations
Key Nutrients for Gut Health: Fiber, probiotics, and prebiotics.
Balanced Diet for a Healthy Gut: Food groups and their benefits.
Foods to Avoid: How certain foods can disrupt gut health.
Chapter 4: Probiotics and Prebiotics
Understanding Probiotics: Strains, benefits, and sources.
The Power of Prebiotics: Foods that fuel a healthy microbiome.
Incorporating Fermented Foods: Recipes and serving ideas.
Chapter 5: Meal Planning and Recipes
Creating a Gut-Healthy Meal Plan: Tips for balanced meals.
Family-Friendly Recipes: Breakfast, lunch, dinner, and snacks.
Adapting Recipes for Sensitive Stomachs: Gluten-free and dairy-free options.
Chapter 6: Lifestyle Factors
Stress and the Gut: How stress affects gut health and ways to mitigate it.
Importance of Sleep: Connecting good sleep and gut health.
Exercise and Gut Health: How physical activity benefits the microbiome.
Common Symptoms and What They Mean: Bloating, constipation, diarrhea.
When to Consult a Health Professional: Guidelines for seeking help.
Supplements and Medications: Safe use of supplements for gut health.
Conclusion
Maintaining Gut Health Long-Term: Strategies for sustained well-being.
Empowering Kids: Teaching children about gut health.
Resources and Further Reading: Books, websites, and experts.
Appendices
Glossary of Terms: Definitions of key concepts.
FAQ Section: Answers to common questions.
Checklists and Charts: Tools for monitoring diet and symptoms.
Gut health is fundamental to overall wellbeing, influencing everything from our digestion to our immune system, mood, and even chronic disease risk. As a holistic doctor, I view gut health as essential not just for managing symptoms but for fostering a vibrant, holistic health lifestyle.


This guide is crafted to empower families with the knowledge and practical strategies needed to nurture their gut health. It’s designed to be accessible, providing clear guidance on how to support gut health through diet, lifestyle changes, and more.
The gastrointestinal system includes the entire tract from the mouth to the anus, encompassed by organs such as the stomach, intestines, liver, and pancreas. These organs work in concert to digest food, absorb nutrients, and expel waste. Here’s a more detailed look at the anatomy of the gastrointestinal (GI) tract:
The digestive process begins in the mouth. Saliva, containing enzymes like amylase, starts the breakdown of carbohydrates. The act of chewing physically breaks down food, making it easier to digest further down the tract.
This muscular tube connects the throat (pharynx) to the stomach. Swallowed food moves down the esophagus via a series of muscular contractions known as peristalsis. A sphincter at the end of the esophagus opens to allow food into the stomach and closes to prevent stomach acids from coming back up.
The stomach is a sac-like organ that holds food while it mixes with gastric juices. These juices contain hydrochloric acid and digestive enzymes that break down protein. The stomach lining also produces mucus to protect itself from being digested by its own acids and enzymes.
The longest part of the GI tract, the small intestine is where most digestion and nutrient absorption occur. It is divided into three parts: the duodenum, jejunum, and ileum. The duodenum receives bile and pancreatic juice, which help digest fats, proteins, and carbohydrates. Nutrients are absorbed through the walls of the small intestine into the bloodstream.
The large intestine absorbs water and salts from the material that has not been digested as food, turning it into solid waste. The colon hosts a large number of bacteria that play a crucial role in the gut microbiome, influencing digestion, immunity, and even mental health.
The rectum stores feces until they are expelled from the body through the anus. The control of this expulsion is helped by the anal sphincters.
Liver: Produces bile that helps digest fats and also processes nutrients absorbed from the small intestine.
Gallbladder: Stores and concentrates bile from the liver, releasing it into the small intestine to aid in digestion.
Pancreas: Produces digestive enzymes and bicarbonate, which are delivered to the small intestine to aid in the digestion and neutralization of stomach acid.
This detailed overview provides a foundational understanding of each part of the gut and its role in the digestive process. Understanding the structure and function of these components is crucial for grasping how the digestive system works holistically to maintain health.

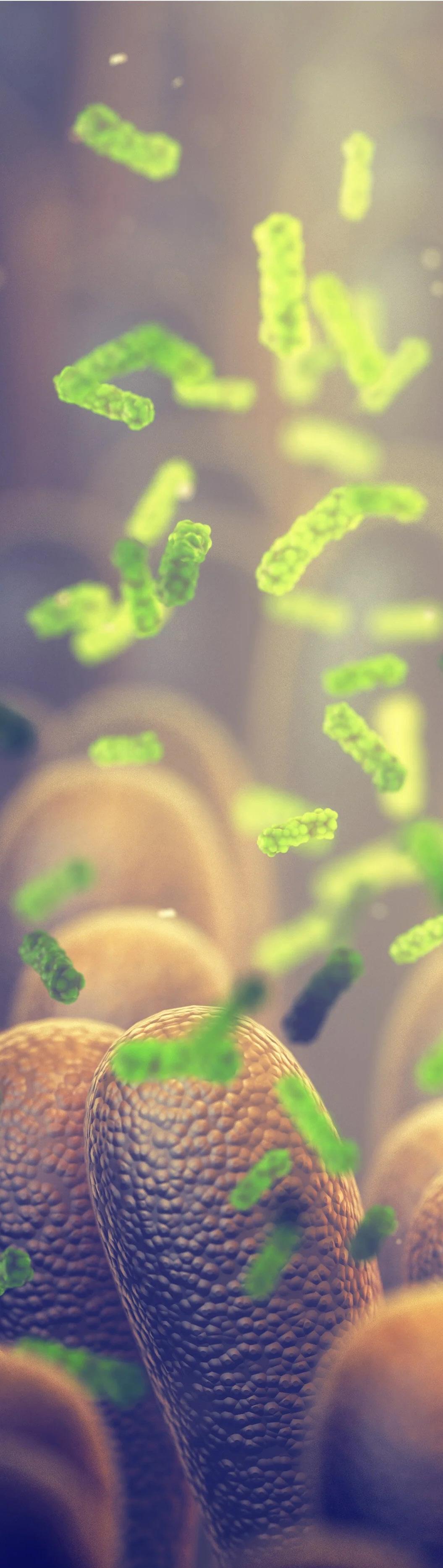
Our gut hosts a complex community of over 100 trillion microbial cells, vital for digestive and immune function. The diversity and balance of this microbiome are crucial for optimal health. Disruptions in this balance can lead to numerous health issues, highlighting the need for a balanced diet and healthy lifestyle.
The gut microbiome refers to the trillions of bacteria, viruses, fungi, and other microorganisms living in the digestive tracts. In children, the gut microbiome plays a crucial role in digestion, the development of the immune system, and even affects brain function and behavior.
The establishment of the gut microbiome begins at birth. Babies born vaginally acquire their initial microbiota from their mother’s birth canal, while those born via cesarean section are more likely to have a gut microbiome similar to their mother’s skin microbiota. Breastfeeding also significantly influences the microbiome’s development by providing beneficial bacteria and prebiotics that promote the growth of healthy bacteria.
The gut microbiome is crucial in educating and regulating the immune system. A diverse gut microbiome can protect children from autoimmune diseases like asthma and allergies by promoting a balance between pro-inflammatory and antiinflammatory responses. Disruptions in the microbiome early in life, such as those caused by antibiotics or a lack of exposure to diverse environments, may predispose children to these conditions.
The gut microbiome helps break down dietary fibers and complex carbohydrates that the human body cannot digest alone, producing shortchain fatty acids (SCFAs) like butyrate, propionate, and acetate. These SCFAs are vital for gut health, serving as energy sources for intestinal cells and contributing to metabolic health. In children, an optimal gut microbiome can improve nutrient absorption and energy balance.
Emerging research suggests a connection between the gut microbiome and the central nervous system, often referred to as the “gut-brain axis”. This relationship means that changes in the gut microbiota can affect a child’s brain development and behavior. For instance, certain probiotics have shown potential in reducing symptoms of anxiety and depression in adolescents.
To support a healthy gut microbiome in children:
Promote a diverse diet: Eating a variety of foods, especially high-fiber fruits, vegetables, and whole grains, can help maintain a diverse microbiome.
Encourage regular physical activity: Physical activity can help increase the diversity of the microbiome.
Limit unnecessary antibiotics: While sometimes necessary, antibiotics can disrupt the microbiome. Use them only when prescribed by a healthcare provider.
Consider probiotics: In some cases, probiotics may help maintain or restore gut health, especially after antibiotic use.
The gut microbiome is a vital component of health that begins to develop at birth and evolves throughout childhood. Understanding its role and maintaining its balance can help optimize immune function, digestion, and even mental health in children.
From birth, children’s gut microbiomes begin to develop. Factors like delivery method (C-section vs. vaginal birth), breastfeeding, and early diet all play significant roles. By age 3, the microbiome stabilizes but continues to evolve into adolescence.
The initial colonization of the gut microbiome starts at birth. Vaginal delivery exposes the newborn to maternal vaginal and fecal microbes, which begin to colonize the infant’s gut. This exposure is thought to be beneficial for the development of the child’s immune system and metabolic processes. Conversely, infants born via cesarean section often have a gut microbiome that initially resembles the skin microbiota, which can differ significantly from those of vaginally delivered babies in terms of bacterial diversity and composition. Studies have shown that cesarean-delivered infants may have a delayed colonization of certain beneficial bacteria like Bacteroides, which are important for immune system development.
Breastfeeding plays a pivotal role in shaping the gut microbiome. Breast milk is not only a source of nutrition but also contains beneficial bacteria and a rich supply of oligosaccharides that serve as prebiotics, feeding the beneficial bacteria in the baby’s gut. This helps to establish a microbiome that can protect against pathogens and supports the development of the immune system. Formula-fed infants, on the other hand, tend to have a different microbiome composition, often with increased levels of Firmicutes and a lower presence of Bifidobacteria.

As infants transition to solid foods, their gut microbiome begins to change significantly. The introduction of new nutrients and food types encourages the growth of a more diverse array of microbial species. Proteins, fats, and complex carbohydrates from solids diversify the microbial ecosystem, reducing the dominance of milkoriented microbes like lactobacilli and increasing the abundance of microbes capable of processing the complex carbohydrates and fibers typical of a solid diet.
By age 3, a child’s gut microbiome largely resembles that of an adult in terms of its composition and diversity, indicating a stabilization phase. However, this does not mean the microbiome becomes static. It continues to evolve and respond to dietary changes, health status, antibiotic use, and environmental factors throughout childhood and into adolescence. This dynamic change can influence everything from nutrient metabolism to immune function and even behavioral aspects through the gut-brain axis.
Entering adolescence, the gut microbiome can be impacted by many new factors. Changes in diet, increased stress, hormonal changes, and lifestyle choices (like exercise and sleep patterns) can all influence the composition and health of the gut microbiome. Adolescents with a diverse and balanced gut microbiome tend to have better health outcomes, illustrating the importance of maintaining a healthy diet and lifestyle during these formative years.

Understanding the development and evolution of the gut microbiome from birth through adolescence underscores the importance of early-life exposures and interventions that can promote a healthy microbiome. These include choosing natural childbirth when possible, breastfeeding, carefully timing the introduction of solid foods, and maintaining a balanced diet rich in fibers, fruits, and vegetables. Such practices are crucial for fostering a robust and resilient microbiome, which in turn supports overall health and disease prevention.
Children may experience various gut-related issues such as colic, reflux, constipation, and diarrhea. Recognizing these symptoms early and understanding when to seek professional help are critical steps for parents.

Colic is characterized by prolonged periods of excessive, inconsolable crying in a healthy infant, typically beginning a few weeks after birth and often improving by three to four months of age. The exact cause of colic is unknown, but it is believed to be partly related to the immaturity of the gut and the baby’s adaptation to its environment outside the womb. The crying episodes often occur in the late afternoon or evening, and although they are distressing, they are usually not a sign of a serious health issue. Management strategies might include soothing techniques, dietary changes for the mother if breastfeeding (like avoiding caffeine or spicy foods), or switching formulas under the guidance of a healthcare provider.
Gastroesophageal reflux (GER) is common in infants and involves the contents of the stomach coming back up into the esophagus. While it can be messy and might cause discomfort, it’s generally considered normal if the baby is otherwise healthy and growing well. Symptoms include spitting up after meals, irritability during or after feeds, and sometimes cough or hiccupping. In most cases, GER resolves on its own by the time the child is one year old. Simple measures such as feeding smaller, more frequent meals and keeping the infant upright after feeding can help. However, if the reflux is accompanied by weight loss, refusal to eat, or respiratory issues, it might be gastroesophageal reflux disease (GERD), which requires medical evaluation.

Constipation in children often presents as infrequent bowel movements, difficulty passing stools, or painful defecation. It can be caused by the transition to solid foods, inadequate fiber or fluid intake, or during potty training or other times of stress. Parents can usually manage mild constipation with dietary modifications, such as increasing water and fiber intake through fruits, vegetables, and whole grains. Regular physical activity also helps stimulate intestinal activity. However, persistent constipation may need a pediatrician’s assessment to rule out underlying conditions and to discuss other treatments such as laxatives designed for children.
Diarrhea is characterized by frequent, loose, or watery stools and can be caused by infections (viral, bacterial, or parasitic), intolerance to certain foods, antibiotics, or other medications. It’s especially important to monitor hydration in children with diarrhea, as they are more susceptible to dehydration. Treatment generally focuses on maintaining hydration, possibly with oral rehydration solutions. Dietary adjustments, such as providing bland, easy-to-digest foods, can also help. Persistent or severe diarrhea warrants a visit to the doctor to determine the cause and to prevent complications like dehydration.
For all these conditions, understanding the symptoms and their severity is crucial. Mild cases often resolve with home care strategies, but there are signs that should prompt a visit to a pediatrician:
• Symptoms persist longer than a few days or worsen.
• The child appears to be in pain or discomfort.
• There are changes in growth, feeding, or general behavior.
• There are additional symptoms like fever, vomiting, blood in the stool, or signs of dehydration (such as reduced urination, dry mouth, or lethargy).
Early recognition and intervention can prevent complications, alleviate discomfort, and provide parents with peace of mind as their children grow and develop. Understanding these common gut-related issues helps parents prepare for and effectively manage potential digestive disturbances in their children.


Nutrition is pivotal in shaping children’s gut health. A diverse diet rich in whole foods supports a healthy microbiome, providing the foundation for lifelong health.
Nutrition is fundamental to health for several compelling reasons, impacting everything from physical growth and immune function to mental well-being and chronic disease prevention. Here’s why nutrition is so crucial:
Nutrition provides the essential nutrients necessary for the body to function. These include macronutrients like carbohydrates, proteins, and fats, which supply energy and are vital for growth, repair, and maintenance of body tissues. Micronutrients, including vitamins and minerals, support numerous biochemical processes; for example, calcium is essential for bone health, while vitamin C supports immune function.
A well-nourished body has a stronger immune system. Nutrients such as vitamin D, vitamin C, zinc, and selenium play critical roles in immune health, helping to maintain the function of the immune cells and protect against infections and diseases. Conversely, nutrient deficiencies can impair immune responses and increase susceptibility to illness.
From infancy through adolescence, nutrition is crucial for healthy growth and development. Proper nutrition ensures that children reach their developmental milestones, supporting everything from the physical growth of bones and muscles to cognitive development and learning abilities.
Adequate nutrition can help prevent a variety of diseases. For example, a diet rich in fruits, vegetables, and whole grains, with limited processed foods and saturated fats, can reduce the risk of chronic conditions such as heart disease, diabetes, and obesity. Diets high in fiber can improve digestive health and prevent conditions like colorectal cancer and inflammatory bowel disease.
Balanced nutrition helps maintain a healthy body weight, which is crucial in preventing obesity-related diseases such as type 2 diabetes, heart disease, and certain types of cancer. Proper nutrition involves not just the quality of food but also portion control and the balance of energy intake and expenditure.
Emerging research shows a strong link between diet and mental health. The gut-brain axis, which connects the gastrointestinal tract and the brain, illustrates how gut health influenced by diet can affect mood and mental health. Nutrients like omega-3 fatty acids, vitamins, and minerals play roles in brain function and are associated with a lower risk of depression and cognitive decline.
The digestive system relies on a balanced diet to function effectively. Fiber, for instance, aids in bowel regularity and helps manage blood sugar levels. Enzymes, vitamins, and minerals facilitate the breakdown of food, ensuring that the body can absorb and utilize nutrients effectively.
Good nutrition not only extends life expectancy but also improves the quality of life. It enhances physical capabilities and performance, increases energy levels, and improves mood, allowing individuals to engage more fully in daily activities and enjoy a higher quality of life.
In summary, nutrition is foundational to all aspects of health. It influences our physical condition, how we feel, and our ability to lead an active, enjoyable life. Proper nutrition is key to prevention, recovery, and optimal living, underscoring the importance of making informed dietary choices throughout life.


• Fiber: Essential for digestive health and regularity.
• Probiotics: Live beneficial bacteria that support gut and immune health.
• Prebiotics: Non-digestible fibers that fuel healthy bacteria.
A balanced diet includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. These foods provide the nutrients necessary for a thriving gut microbiome.
A balanced diet rich in whole foods provides essential nutrients that nurture the gut microbiome and the entire body. For children, this involves a variety of food groups including:


These are high in fibers, vitamins, and minerals that are essential for maintaining a healthy gut. The fiber acts as a prebiotic, feeding beneficial gut bacteria, which helps them flourish and diversify. Brightly colored fruits and vegetables also contain antioxidants and phytochemicals that reduce inflammation and support gut lining health.
Foods such as oats, quinoa, brown rice, and whole wheat contain non-digestible carbohydrates that reach the colon intact and help to stimulate the growth of beneficial bacteria. These fibers also aid in digestion and prevent constipation, which can be a common issue in children.



Adequate protein intake from varied sources like lean meats, fish, beans, and nuts is crucial for the growth and repair of tissues and can influence the composition of the gut microbiota. It’s important to choose lean proteins and to vary sources to include plantbased options, which bring their own set of nutrients and fibers.
Yogurt, kefir, sauerkraut, and miso contain live cultures that can enhance the diversity of the microbiome. These foods introduce beneficial bacteria directly into the gut and can help balance the microbial environment.
Fats are essential for brain development and the absorption of fat-soluble vitamins. Sources like avocados, olive oil, and fatty fish (which provide omega-3 fatty acids) are beneficial for reducing inflammation and supporting the health of the gut lining.
While a diverse diet is essential, there are specific nutritional considerations that can particularly impact gut health in children:
• Adequate Fiber Intake: Children often consume less fiber than recommended. Encouraging a variety of fiberrich foods helps maintain regular bowel movements and supports a healthy gut microbiome.
• Limiting Processed Foods: High intakes of processed foods, sugars, and saturated fats can negatively affect gut health by promoting the growth of harmful bacteria and reducing microbial diversity. These diets can also lead to inflammation and increased permeability of the gut lining (leaky gut), which may contribute to various health issues.
• Hydration: Adequate water intake is essential for digestive health, helping to dissolve nutrients and fibers for easier digestion and to maintain regular bowel movements.

The dietary habits established in childhood can influence gut health well into adulthood. Early education about nutrition and involving children in meal preparation can foster healthy eating habits. Regular family meals can also promote more balanced eating behaviors and provide opportunities for parents to model healthy eating.


Understanding and implementing these nutritional fundamentals can have a profound impact on a child’s current and future gut health, overall development, and well-being. Nutrition not only supports the physical aspects of gut function but also plays a crucial role in cognitive and emotional health through the gut-brain axis. Thus, nurturing the gut microbiome through thoughtful nutrition is a vital strategy for fostering lifelong health.

Probiotics are beneficial bacteria that help maintain the health of the gut microbiome. They can be found in supplements and fermented foods like yogurt, kefir, and sauerkraut.
Prebiotics are fibers that the body cannot digest. They help feed the beneficial bacteria in the gut. Foods rich in prebiotics include garlic, onions, bananas, and asparagus.
Fermented foods are a great way to boost the probiotic content of the diet. This section includes recipes and tips for incorporating these foods into daily meals.

Probiotics are live microorganisms, often referred to as “good” or “beneficial” bacteria, because they help maintain the health of the gut microbiome. These microorganisms can enhance gastrointestinal health, boost the immune system, and even potentially improve mental health outcomes.
Besides supplements, natural sources of probiotics include a variety of fermented foods. Yogurt and kefir are perhaps the most well-known, rich in lactobacilli that can help balance the gut flora. Other sources include sauerkraut, which is fermented cabbage, and offers a wide range of bacteria beneficial to the gut. Kombucha, a fermented tea, and kimchi, a Korean dish made from fermented vegetables, are also excellent sources.
Probiotics play a role in digesting food, destroying disease-causing cells, and producing vitamins. Numerous studies have shown that probiotics are effective in treating diarrhea, irritable bowel syndrome, and certain intestinal infections. They may also help with conditions such as eczema and urinary tract infections.
When selecting probiotic foods or supplements, it’s important to look for the types of bacteria involved—commonly Bifidobacteria and Lactobacilli—and their concentrations, often listed in colony-forming units (CFUs). The effectiveness of probiotics can depend on the strains and the dosage, so consider these factors when incorporating them into your diet.

Prebiotics are non-digestible fibers that act as food for probiotics. By feeding and maintaining healthy colonies of probiotics, prebiotics help improve gut health, enhance digestion, and boost immune function.
• Sources of Prebiotics: While garlic and onions are wellknown prebiotic-rich foods, other sources include bananas, asparagus, leeks, chicory root, and Jerusalem artichokes. Whole grains like barley and oats also contain valuable prebiotic fibers that help nourish gut bacteria.
• Health Benefits: Prebiotics are particularly beneficial in promoting the growth of beneficial bacteria in the gut, which can enhance nutrient absorption, help with digestion, and improve metabolic health. They have also been linked to improved sleep and reduced stress.
• Incorporating Prebiotics: To maximize the benefits, include a variety of prebiotic-rich foods in your diet. This not only helps maintain a healthy gut microbiome but also ensures that the body receives a mix of fibers, which can aid in regular bowel movements and gut health.

Fermented foods are not just flavorful additions to the diet; they’re also excellent for enhancing the probiotic content of your meals, which supports gut health and overall wellness.
• Benefits of Fermented Foods: These foods undergo a process of lactofermentation, where natural bacteria feed on the sugar and starch in the food, creating lactic acid. This process preserves the food and creates beneficial enzymes, b-vitamins, Omega-3 fatty acids, and various strains of probiotics.
• Common Fermented Foods: Beyond yogurt and sauerkraut, consider adding miso, tempeh, and natto (fermented soybean products) to your diet. These not only provide depth and flavor but also are rich in both probiotics and proteins.
• Recipes and Tips: Start by incorporating small amounts of fermented foods into your daily diet. For example, add sauerkraut to a sandwich or salad, drink a small glass of kombucha, or use miso paste in soups and marinades. As your palate adjusts, you can increase the quantity and variety of fermented foods you consume.
• Homemade Fermentation: Consider making your own fermented foods as a cost-effective way to enjoy these benefits. Simple recipes like homemade yogurt, kefir, and fermented vegetables can be made with just a few ingredients and basic kitchen tools.
By understanding and utilizing probiotics, prebiotics, and fermented foods, you can significantly enhance your gut health, which in turn supports overall health and well-being. This approach not only adds diversity to your diet but also leverages the natural synergy between these components to optimize gut flora and boost immune function.
To support a healthy gut, meal planning is essential. This involves balancing macronutrients and incorporating a variety of foods that promote microbial diversity. Here, we’ll provide strategies for planning meals throughout the week that are both nutritious and appealing to all family members.
This section includes recipes designed to support gut health for every meal:

Smoothies with probiotic yogurt, oats, and berries.

Quinoa salad with mixed greens, prebioticrich vegetables, and a probiotic dressing.

Grilled chicken or tofu with a side of fermented kimchi and steamed vegetables.

Homemade kefir popsicles or hummus with carrot sticks.
Creating a gut-healthy meal plan involves incorporating a diverse range of foods that promote a balanced microbiome. Here are ten family-friendly recipes designed to support gut health for every meal, making them both nutritious and appealing to all family members.
These recipes are designed to be easy to prepare, delicious, and full of ingredients that support a healthy gut, making them perfect for the whole family to enjoy while benefiting their overall health.
BREAKFAST

INGREDIENTS
1 cup probiotic yogurt
½ cup mixed berries (blueberries, strawberries)
1 banana
1 tablespoon flaxseeds
½ cup almond milk
INSTRUCTIONS
Blend all ingredients until smooth. Serve chilled for a refreshing, gut-friendly start to the day.
INGREDIENTS
1 cup rolled oats
2 tablespoons chia seeds
2 cups almond milk
1 tablespoon maple syrup
½ teaspoon vanilla extract
INSTRUCTIONS
Combine all ingredients in a jar and let sit overnight. Serve with a topping of banana slices and a sprinkle of cinnamon.

INGREDIENTS
1 cup cooked quinoa
2 cups mixed greens (spinach, arugula)
½ cup chopped carrots
¼ cup sliced red onions
2 tablespoons olive oil
1 tablespoon apple cider vinegar
INSTRUCTIONS
Toss all ingredients together. Serve with a probiotic yogurt dressing.
INGREDIENTS
2 tablespoons olive oil
1 chopped onion
Sauté onions and garlic in olive oil until translucent. Add carrots, potatoes, and broth. Simmer until vegetables are tender. Blend if desired and season. LUNCH
2 minced garlic cloves
2 sliced carrots
2 diced potatoes
4 cups vegetable broth
salt and pepper to taste

INGREDIENTS
4 chicken breasts
Salt Pepper
1 cup kimchi
1 tablespoon sesame oil
Steamed broccoli
INSTRUCTIONS
Season chicken with salt and pepper, grill until cooked. Serve with kimchi and a side of steamed broccoli drizzled with sesame oil
INGREDIENTS
1 block firm tofu, diced
2 cups mixed vegetables (bell peppers, zucchini)
½ cup fermented vegetables
2 tablespoons soy sauce
1 tablespoon ginger, minced
INSTRUCTIONS
Stir-fry tofu and fresh vegetables with ginger until crisp-tender. Add fermented vegetables and soy sauce. Stir well and serve.

INGREDIENTS
2 cups plain kefir
1 cup mixed berry puree
1 tablespoon honey
INSTRUCTIONS
Mix kefir, berry puree, and honey. Pour into popsicle molds and freeze until solid.
INGREDIENTS
1 can chickpeas
2 tablespoons tahini
1 lemon juiced
2 minced garlic cloves
Olive oil
Carrot sticks
INSTRUCTIONS
Blend chickpeas, tahini, lemon juice, and garlic in a food processor. While blending, slowly add olive oil until smooth. Serve with carrot sticks.

INGREDIENTS
4 apples, cored
¼ cup walnuts
¼ cup raisins
½ teaspoon cinnamon
1 cup vanilla yogurt
INSTRUCTIONS
Stuff apples with walnuts, raisins, and cinnamon. Bake at 350°F for 25 minutes. Serve warm with yogurt.
INGREDIENTS
1 cup vanilla yogurt
½ cup chia seeds
1 cup mixed berries
1 tablespoon honey
Layer yogurt, chia seeds soaked in almond milk, berries, and a drizzle of honey in glasses.
When managing food sensitivities, it’s important to adapt recipes to accommodate dietary restrictions while still ensuring that meals are nutritious and enjoyable for everyone. This section focuses on gluten-free and dairy-free alternatives, providing strategies for creating gut-friendly meals that help avoid discomfort for those with sensitive stomachs.
Gluten, a protein found in wheat, barley, and rye, can cause digestive issues for individuals with celiac disease or gluten sensitivity. Here are some tips for adapting recipes to be gluten-free:
• Flour Alternatives: Replace wheat flour with glutenfree flours such as almond flour, rice flour, coconut flour, or a gluten-free all-purpose blend. These alternatives work well for baking and thickening sauces.
• Grains: Opt for naturally gluten-free grains like quinoa, buckwheat, and millet. These can be used in salads, as sides, or as bases for dishes that traditionally use pasta or couscous.
• Breading and Binding: Use gluten-free breadcrumbs or crushed gluten-free cereal for coatings. For binding in recipes like meatballs or burgers, consider gluten-free oats or cooked quinoa.
Dairy can be problematic for those with lactose intolerance or a milk protein allergy. Here are some ways to adapt recipes to be dairy-free:
• Milk Alternatives: Substitute cow’s milk with plantbased milks such as almond milk, coconut milk, oat milk, or soy milk. These alternatives can generally be used in a 1:1 ratio in recipes.
• Butter Alternatives: Use plant-based butters or oils such as coconut oil, olive oil, or avocado oil for cooking and baking.


Here are a few practical adaptations to make popular family recipes gluten-free and dairy-free:
• Pancakes: Use a gluten-free flour blend and almond milk to make the batter. Serve with dairy-free chocolate chips or fresh berries for added flavor without dairy.
• Creamy Soups: Create creaminess with coconut milk or blended cashews instead of dairy cream. Use glutenfree stock and thicken with a slurry of cornstarch and water.
• Lasagna: Use gluten-free lasagna noodles or Spaghetti Squash, layer with dairy-free ricotta made from tofu, and use nutritional yeast to add a cheesy flavor without actual cheese.
• Mac and Cheese: Prepare with gluten-free pasta and a sauce made from dairy-free cheese and nutritional yeast. Add creaminess with a touch of coconut milk.
• Desserts: Bake cookies using gluten-free oat flour and dairy-free dark chocolate. Sweeten with natural sugars like coconut sugar for a healthier option.
Adapting recipes for sensitive stomachs doesn’t have to mean sacrificing flavor or enjoyment. By incorporating gluten-free and dairy-free alternatives, families can enjoy a wide variety of delicious, gut-friendly meals that cater to everyone’s health needs and preferences. These adaptations not only prevent discomfort but also ensure that meals remain balanced and satisfying.

Chronic stress can significantly impact gut health by altering gut bacteria and increasing inflammation. Here, we provide techniques for managing stress in family settings, such as mindfulness, yoga, and family therapy, emphasizing their importance in maintaining gut health.
Quality sleep is crucial for gut health. This section discusses the bidirectional relationship between sleep and the gut, offering tips for establishing healthy sleep routines for children and adults alike.
Physical activity can enhance gut health by increasing gut motility and promoting a healthy microbiome. This part includes simple and enjoyable family-oriented exercises that support digestive health.

• Mindfulness and Meditation: These practices help calm the mind and reduce stress by focusing on the present moment. Simple guided meditations or mindfulness exercises can be done together as a family, even if just for a few minutes daily.
• Yoga: Incorporating yoga into your family routine can provide both physical and mental benefits. Yoga helps in reducing stress, improving flexibility, and enhancing digestion. Family yoga sessions can be a fun and engaging way to benefit everyone’s gut health.
• Family Therapy: Sometimes, professional help in managing family dynamics and stress can be invaluable. Family therapy provides tools and strategies to improve communication, solve conflicts, and reduce stress within the home environment.
Quality sleep plays a vital role in maintaining gut health. The relationship between sleep and the gut is bidirectional; not only can poor gut health affect sleep quality, but inadequate sleep can lead to gastrointestinal issues and imbalances in gut bacteria.
• Consistent Sleep Schedule: Maintaining a regular sleep schedule helps regulate the body’s internal clock and can improve sleep quality. This is important for both children and adults.
• Bedtime Rituals: Establishing calming bedtime rituals, such as reading, taking a warm bath, or listening to soothing music, can help signal the body that it’s time to wind down.
• Environment: Create a sleep-conducive environment that is dark, quiet, and cool. Consider using blackout curtains, white noise machines, and comfortable bedding to enhance sleep quality.

Physical activity is beneficial for gut health in several ways. It can enhance gut motility, which helps prevent constipation and promotes regular bowel movements. Exercise also helps in managing stress and can indirectly support a healthy microbiome.
FAMILY-ORIENTED EXERCISES TO SUPPORT DIGESTIVE HEALTH:
• Walking or Hiking: A simple walk after dinner or a weekend hike can help with digestion and is an excellent activity for all family members.
• Cycling: Whether it’s a leisurely bike ride around the neighborhood or a more vigorous cycling class, this activity can be both fun and beneficial for gut health.
• Team Sports: Engaging in team sports like soccer, basketball, or baseball can be a fun way to get the whole family moving and support gut health through vigorous exercise.
By integrating stress management techniques, ensuring adequate sleep, and maintaining regular physical activity, families can support their gut health effectively. These strategies not only improve digestive function but also enhance overall well-being and quality of life for all family members.
We discuss how to recognize and understand common gut symptoms like bloating, constipation, and diarrhea, providing clear guidance on when these may be signs of more serious conditions.
This section outlines the scenarios in which consulting a healthcare provider is advisable. It includes a checklist of symptoms and signs that necessitate professional evaluation.
While focusing on natural and dietary approaches, we also explore when supplements or medications might be appropriate. Safe usage and the importance of professional guidance are stressed, especially for probiotics, fiber supplements, and digestive enzymes.
Understanding and recognizing common gut symptoms are key to managing digestive health effectively. This section explores how to interpret symptoms like bloating, constipation, and diarrhea and provides insights into when these symptoms might indicate a more serious condition.
• What it is: A feeling of fullness or swelling in the abdomen, often uncomfortable or painful.
• Common causes: Overeating, consuming highfiber foods quickly, or intolerance to certain foods such as dairy or gluten.
• When to worry: If bloating is persistent, accompanied by symptoms like weight loss, severe pain, or changes in your stool, it may indicate a more serious condition like irritable bowel syndrome (IBS), celiac disease, or even ovarian cancer.

• What it is: Fewer than three bowel movements per week, often accompanied by hard, dry stools that are difficult to pass.
• Common causes: Lack of fiber, inadequate hydration, inactivity, or certain medications.
• When to worry: If constipation is new, severe, persists for several weeks, or is accompanied by pain, blood in the stool, or weight loss, it’s important to seek medical advice as these could be signs of bowel obstruction or colon cancer.
• What it is: Frequent, loose, or watery bowel movements.
• Common causes: Infections, food intolerances, medications, or chronic digestive conditions like Crohn’s disease or ulcerative colitis.
• When to worry: If diarrhea lasts more than a few days, leads to dehydration, or is accompanied by fever, blood in the stool, or severe pain, medical attention is necessary.

Knowing when to consult a healthcare provider can help in addressing digestive issues before they become more serious. This section provides a checklist of symptoms and signs that necessitate professional evaluation.
• Persistent Symptoms: Any digestive symptoms that last more than a few weeks.
• Painful Symptoms: Severe or recurring pain in the abdomen.
• Changes in Bowel Movements: Significant changes in the frequency, consistency, or appearance of stools, especially if accompanied by blood.
• Weight Loss: Unexplained weight loss along with digestive symptoms.
• Fatigue: Persistent tiredness or fatigue that doesn’t go away with rest.
• Additional Symptoms: Night sweats, fever, or anemia.

While natural and dietary approaches are foundational, there are situations where supplements or medications are appropriate and beneficial. This section discusses when and how to safely use these interventions under professional guidance.
• Use: Can help restore and maintain a healthy balance of gut bacteria, beneficial for conditions like antibiotic-associated diarrhea and IBS.
• Guidance: Choose supplements with evidencebased strains and doses. Consult a healthcare provider for recommendations specific to your needs.
• Use: Useful for managing constipation and maintaining regularity, especially if dietary fiber intake is insufficient.
• Guidance: Start with a low dose and gradually increase to avoid gas and bloating. Ensure adequate water intake.
• Use: Can aid in the digestion of certain nutrients like fats, proteins, and carbohydrates, helpful for people with enzyme deficiencies or conditions like pancreatitis.
• Guidance: Use under the supervision of a healthcare provider to determine the correct type and dosage.
• Always consult with a healthcare provider before starting any new supplement or medication, especially if you have underlying health conditions or are taking other medications.
• Monitor for any adverse reactions or interactions with other treatments.
Understanding these aspects of gut health — recognizing symptoms, knowing when to seek help, and responsibly using supplements and medications — can significantly improve management and outcomes for gastrointestinal issues.
Sustaining gut health is a lifelong journey. This concluding section provides strategies for continued gut health maintenance, emphasizing regular health check-ups, continual education, and adaptation of diet and lifestyle as the family grows and changes.
Teaching children about gut health from a young age fosters lifelong healthy habits. We provide tips for making learning about gut health fun and interactive, such as garden-based learning where kids can grow their prebiotic-rich foods.
• “Gut: The Inside Story of Our Body’s Most Underrated Organ” by Giulia Enders - Provides a fascinating insight into the digestive system and its importance to our overall health.
• “The Microbiome Solution: A Radical New Way to Heal Your Body from the Inside Out” by Dr. Robynne ChutkanFocuses on how to nurture your microbiome for optimal health.
• “The Good Gut: Taking Control of Your Weight, Your Mood, and Your Long-term Health” by Justin and Erica Sonnenburg - Explores the connection between the gut microbiome and various aspects of health.
• Gut Microbiota for Health - Offers up-to-date information on gut microbiota research and its implications for health (link).
• American Gastroenterological Association - Provides resources and patient education materials on gastrointestinal health (link).
• The International Foundation for Gastrointestinal Disorders - Features comprehensive resources on managing various gastrointestinal disorders (link).
• Dr. Mark Hyman - Known for his work on functional medicine, particularly relating to inflammation and gut health.
• Dr. David Perlmutter - Neurologist and author specializing in topics related to the connection between neurological health and nutrition.
• Dr. Rob Knight - Professor and co-founder of the American Gut Project, specializing in microbiome research.
• Microbiome: The community of microorganisms (such as bacteria, fungi, and viruses) that inhabit a particular environment, especially the human body.
• Probiotics: Live bacteria and yeasts that are good for your health, especially your digestive system.
• Prebiotics: Compounds in food that induce the growth or activity of beneficial microorganisms such as bacteria and fungi.
• Fermentation: A metabolic process that produces chemical changes in organic substrates through the action of enzymes, producing energy and creating probiotics.
Q1: WHAT ARE THE SIGNS OF AN UNHEALTHY GUT?
A1: Signs may include upset stomach, high sugar diet, unintentional weight changes, sleep disturbances, skin irritation, and autoimmune conditions.
Q2: HOW CAN I IMPROVE MY GUT HEALTH NATURALLY?
A2: Eat a diverse range of foods, include plenty of fiber, add fermented foods to your diet, limit artificial sweeteners, and manage stress.
Q3: ARE PROBIOTICS SAFE FOR CHILDREN?
A3: Yes, probiotics are generally safe for children, but it’s important to choose strains and products specifically designed for children and seek advice from a healthcare provider.
Q4: HOW OFTEN SHOULD I CHANGE MY DIET TO BENEFIT MY GUT HEALTH?
A4: Instead of frequent drastic changes, aim for consistent, long-term habits that include a variety of nutrients to support a healthy microbiome.
• Daily Food and Symptom Diary: Helps track what you eat and any symptoms you experience, to identify food sensitivities or triggers.
• Gut Health Progress Chart: Monitor improvements in symptoms or general well-being over time.
• Prebiotic and Probiotic Foods Checklist: A handy guide to ensure a balance of beneficial foods in your diet.