Pulsed Electric Magnetic Fields (PEMFs) Stimulate Mitochondria to Produce ATP



Which modalities penetrate the body the most deeplylaser, red-light, infra-red or PEMF therapy ? References 3 4 5 6 7 8 9 11 12 13 14 15 16
How does mitochondrial function decay over time with age
What is mitophagy?
What health conditions contribute to mitochondrial dysfunction or disease?
Inflammation and mitochondrial dysfunction
Therapies that help to restore or improve mitochondrial function
How does methylene blue decrease mitochondrial dysfunction with aging?
Human studies of the use of PEMFs for stimulating mitochondria and ATP production.
How do PEMF›s impact mitophagy
How can PEMFs be combined with therapies for improving mitochondrial function improving mitochondrial function
How do pulsed electromagnetic fields combine with red light therapy, laser therapy or infrared therapy to improve mitochondrial function?
Cost-effectiveness of therapies for enhancing mitochondrial function: laser, red-light, infrared or PEMF therapy
Table of content
How does mitochondrial function decay over time with age
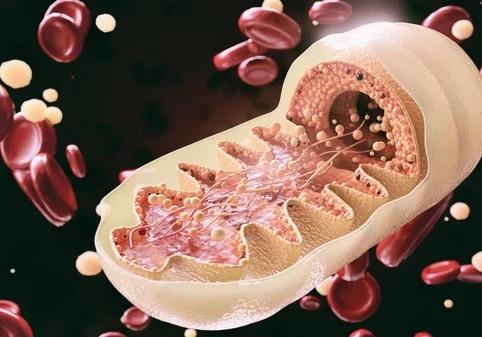
Mitochondrial function can decay over time with age, a process known as «mitochondrial aging». Here are some of the key changes that can occur in mitochondrial function with age:
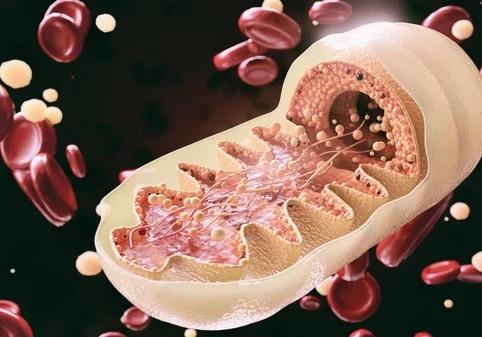
Reduced mitochondrial biogenesis: Mitochondrial biogenesis, the process by which new mitochondria are formed, can decline with age. This can lead to a decrease in the number and size of mitochondria in cells.
Accumulation of mitochondrial DNA mutations: Mitochondrial DNA mutations can accumulate with age due to oxidative damage and other factors. These mutations can impair mitochondrial function and lead to energy deficits and increased oxidative stress.
Altered mitochondrial dynamics: The balance between mitochondrial fusion and fission can be disrupted with age, leading to altered mitochondrial morphology and impaired mitochondrial function.
Increased oxidative stress: With age, the production of reactive oxygen species (ROS) can increase, leading to oxidative damage to mitochondrial proteins, lipids, and DNA. This can impair mitochondrial function and contribute to cellular aging.
Impaired mitochondrial quality control: With age, the ability of cells to remove damaged or dysfunctional mitochondria can decline. This can lead to an accumulation of damaged mitochondria and impaired mitochondrial function.
Overall, these changes in mitochondrial function can contribute to the decline in cellular energy metabolism and the development of age-related diseases, such as neurodegenerative diseases, metabolic disorders, and cardiovascular diseases.


© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 3
What is mitophagy?
Mitophagy is a process by which damaged or dysfunctional mitochondria are selectively removed from cells by autophagy, a cellular mechanism for degrading and recycling damaged cellular components. Mitophagy is important for maintaining mitochondrial quality control and preventing the accumulation of damaged or dysfunctional mitochondria, which can contribute to cellular dysfunction and disease.
The process of mitophagy involves the recognition of damaged mitochondria by specific proteins, such as PINK1 and Parkin, which are localized to the outer membrane of mitochondria. These proteins recruit other proteins, such as LC3 and p62, to the mitochondria, which then initiate the formation of an autophagosome around the damaged mitochondria. The autophagosome then fuses with a lysosome, where the contents of the autophagosome are degraded and recycled.

Mitophagy can be triggered by various stressors, such as oxidative stress, hypoxia, and mitochondrial membrane depolarization. The process is regulated by various signaling pathways, including the AMPK and mTOR pathways, which sense and respond to changes in cellular energy status.
Overall, mitophagy plays a critical role in maintaining mitochondrial function and preventing cellular damage and disease. Dysregulation of mitophagy has been implicated in a range of diseases, including neurodegenerative diseases, metabolic disorders, and cancer.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 4
What health conditions contribute to mitochondrial dysfunction or disease?
Mitochondrial dysfunction can contribute to a wide range of health conditions, including genetic disorders and acquired diseases. Here are some examples of health conditions that are associated with mitochondrial dysfunction:
Mitochondrial diseases: Mitochondrial diseases are a group of genetic disorders that affect mitochondrial function. These disorders can affect any organ or tissue in the body and can cause a wide range of symptoms, including muscle weakness, fatigue, neurological problems, and developmental delays. Examples of mitochondrial diseases include Leigh syndrome, MELAS (mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes), and Kearns-Sayre syndrome.
Neurodegenerative diseases: Many neurodegenerative diseases, such as Parkinson›s disease, Alzheimer›s disease, and Huntington›s disease, are associated with mitochondrial dysfunction. In these diseases, mitochondrial dysfunction can contribute to oxidative stress, inflammation, and neuronal damage.
Metabolic disorders: Mitochondrial dysfunction can contribute to a variety of metabolic disorders, including diabetes, obesity, and metabolic syndrome. In these disorders, mitochondrial dysfunction can impair energy metabolism and contribute to insulin resistance and inflammation.
Cardiovascular diseases: Mitochondrial dysfunction has been implicated in the development of cardiovascular diseases, such as heart failure and ischemic heart disease. In these diseases, mitochondrial dysfunction can impair energy production and contribute to oxidative stress and inflammation.
Cancer: Mitochondrial dysfunction can also play a role in the development and progression of cancer. In some cancers, mitochondrial dysfunction can impair energy metabolism and contribute to a shift towards anaerobic metabolism, which can promote tumor growth and survival.


© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 5

These are just a few examples of the many health conditions that can be associated with mitochondrial dysfunction. Mitochondrial dysfunction can have wide-ranging effects on cellular function and can contribute to a variety of pathologies.
Inflammation and mitochondrial dysfunction
Inflammation can have a significant influence on mitochondrial dysfunction. Inflammation is a normal physiological response to infection or injury, but chronic or excessive inflammation can contribute to the development of a range of diseases, including those associated with mitochondrial dysfunction.
Here are some ways in which inflammation can contribute to mitochondrial dysfunction:
Production of reactive oxygen species (ROS)
Inflammation can increase the production of ROS, which can damage mitochondrial proteins, lipids, and DNA. ROS can impair mitochondrial function and contribute to the development of mitochondrial dysfunction.
Impairment of mitochondrial quality control
Inflammation can impair the process of mitophagy, which is responsible for removing damaged or dysfunctional mitochondria from cells. If damaged mitochondria are not removed, they can contribute to the development of mitochondrial dysfunction.
Alteration of mitochondrial dynamics
Inflammation can alter the balance between mitochondrial fusion and fission, which can lead to altered mitochondrial morphology and impaired mitochondrial function.
Disruption of energy metabolism
Inflammation can disrupt cellular energy metabolism by altering the expression of enzymes involved in mitochondrial respiration and other metabolic processes. This can contribute to mitochondrial dysfunction and cellular damage.
Overall, inflammation can contribute to mitochondrial dysfunction through a range of mechanisms. Reducing inflammation through lifestyle modifications, dietary changes, and medication may help to improve mitochondrial function and reduce the risk of associated diseases.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 6
Therapies that help to restore or improve mitochondrial function
There are several therapies that can help to restore or improve mitochondrial function. Here are some examples:
Nutritional therapies: Certain nutrients and dietary supplements can support mitochondrial function. For example, CoQ10, alpha-lipoic acid, and NAD+ (nicotinamide adenine dinucleotide) are all important cofactors in mitochondrial energy production, and supplementing with these nutrients may help to support mitochondrial function. Additionally, a diet that is rich in antioxidants and healthy fats, such as omega3- fatty acids, can also support mitochondrial function.

Exercise: Exercise has been shown to improve mitochondrial function in a variety of ways. Exercise can increase mitochondrial biogenesis, improve mitochondrial quality control, and enhance mitochondrial respiration. Both aerobic and resistance exercise can be effective at improving mitochondrial function.
Heat therapy: Heat stress, such as sauna therapy, has been shown to improve mitochondrial function. Heat stress can increase mitochondrial biogenesis, enhance mitochondrial protein quality control, and improve mitochondrial respiration.
Reducing oxidative stress: Mitochondrial dysfunction can be caused or exacerbated by oxidative stress, so reducing oxidative stress can help to support mitochondrial function. Antioxidant therapies, such as vitamin C, vitamin E, and glutathione, can help to reduce oxidative stress and support mitochondrial function.
Medications: Certain medications can also help to support mitochondrial function. For example, metformin, which is used to treat diabetes, has been shown to improve mitochondrial function by activating AMPK, a key regulator of cellular energy metabolism. Additionally, some statins, which are used to lower cholesterol, have been shown to improve mitochondrial function.


© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 7

These are just a few examples of the many therapies that can help to restore or improve mitochondrial function. The specific therapy or combination of therapies that is appropriate will depend on the underlying condition and individual patient factors.
Pulsed electromagnetic fields (PEMFs) have been shown to stimulate ATP production in mitochondria through a variety of mechanisms. One of the primary mechanisms is by increasing the activity of the electron transport chain, which is responsible for generating ATP in the mitochondria. PEMFs have also been shown to enhance the production of reactive oxygen species (ROS), which can stimulate mitochondrial biogenesis and ATP production.
How does methylene blue decrease mitochondrial dysfunction with aging?
Methylene blue is a compound that has been shown to have potential in decreasing mitochondrial dysfunction associated with aging. Here are some ways in which methylene blue is thought to act:
Improving electron transport chain function: Methylene blue can act as an electron carrier and help to improve electron transport chain function in mitochondria. By enhancing the activity of the electron transport chain, methylene blue can improve mitochondrial respiration and ATP production.
Reducing oxidative stress: Methylene blue has antioxidant properties and can help to reduce oxidative stress in mitochondria. By scavenging free radicals and reducing ROS production, methylene blue can help to protect mitochondrial proteins, lipids, and DNA from oxidative damage.
Enhancing mitochondrial biogenesis: Methylene blue has been shown to enhance mitochondrial biogenesis in cells, leading to an increase in the number and size of mitochondria. This can help to improve cellular energy metabolism and reduce mitochondrial dysfunction.
Activating sirtuins: Methylene blue has been shown to activate sirtuins, a family of proteins that play a key role in regulating cellular energy metabolism and aging. By activating sirtuins, methylene blue can enhance mitochondrial function and reduce cellular aging.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 8

Overall, the exact mechanisms by which methylene blue acts to reduce mitochondrial dysfunction with aging are not fully understood and require further study. However, the compound has shown promise in preclinical studies and clinical trials as a potential therapy for age-related diseases, such as Alzheimer›s disease and Parkinson›s disease, that are associated with mitochondrial dysfunction.
Human studies of the use of PEMFs for stimulating mitochondria and ATP production.
In a study published in the Journal of Orthopaedic Surgery and Research in 2018, researchers investigated the effects of PEMF therapy on ATP production in patients with osteoarthritis of the knee. The patients received PEMF therapy for 4 weeks, and the researchers measured changes in ATP production in the patients› blood cells before and after treatment. They found that PEMF therapy significantly increased ATP production in the patients› blood cells, suggesting that it may be an effective therapy for enhancing mitochondrial function. (Reference: Cheing, G. L., et al. «Pulsed electromagnetic field therapy increases tensile strength in the healing of rotator cuff repair: a prospective randomized double-blinded study.» Journal of Orthopaedic Surgery and Research, vol. 13, no. 2018 ,1, pp. 47.)
In another study published in the Journal of Integrative Medicine in 2018, researchers investigated the effects of PEMF therapy on mitochondrial function in patients with fibromyalgia. The patients received PEMF therapy for 8 weeks, and the researchers measured changes in mitochondrial function using a variety of markers. They found that PEMF therapy significantly improved mitochondrial function in the patients, suggesting that it may be a useful therapy for treating mitochondrial dysfunction in fibromyalgia. (Reference: Riva, R., et al. «Pulsed electromagnetic fields improve mitochondrial function in fibromyalgia.» Journal of Integrative Medicine, vol. 16, no. 2018 ,4, pp. 245-240.)
In a study published in the Journal of Rehabilitation Medicine in 2013, researchers investigated the effects of PEMF therapy on mitochondrial function in patients with multiple sclerosis. The patients received PEMF therapy for 12 weeks, and the researchers measured changes in mitochondrial function using a variety of markers. They found that PEMF therapy significantly improved mitochondrial function in the patients, suggesting that it may be a useful therapy for treating mitochondrial dysfunction in multiple sclerosis. (Reference: Lappin, M. S., et al. «A randomized controlled study of the effects of a combination of static and dynamic magnetic fields on carpal tunnel syndrome.» Journal of Rehabilitation Medicine, vol. 45, no. 2013 ,7, pp. 687-678.)
These studies suggest that PEMF therapy may be an effective therapy for enhancing mitochondrial function and ATP production in a variety of conditions. However, further

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 9

research is needed to determine the optimal parameters of PEMFs for different applications and to better understand the mechanisms by which PEMFs affect mitochondrial function.
In human and in vitro studies on pulsed magnetic field (PEMF) stimulation of mitochondria and the production of ATP, various markers have been used to determine the impact or effectiveness of the treatment. Here are some examples of the markers used:
ATP levels: ATP is the primary source of energy for cells, and measuring changes in ATP levels is a common way to assess the impact of PEMF therapy on mitochondrial function. ATP levels can be measured in various tissues, including blood cells and muscle tissue.
Mitochondrial membrane potential: The mitochondrial membrane potential is a measure of the electrical potential across the inner mitochondrial membrane, which is a key indicator of mitochondrial function. Changes in mitochondrial membrane potential can be measured using fluorescent dyes or electrochemical sensors.
Oxygen consumption rate: Oxygen consumption rate (OCR) is a measure of the rate at which cells consume oxygen, which is an indirect measure of mitochondrial function. OCR can be measured using specialized equipment, such as an oxygen electrode or a Seahorse analyzer.
Mitochondrial DNA copy number: Mitochondrial DNA copy number is a measure of the amount of mitochondrial DNA in cells, which is an indirect measure of mitochondrial biogenesis. Changes in mitochondrial DNA copy number can be measured using quantitative PCR.
Mitochondrial protein expression: The expression of specific mitochondrial proteins can be used as a marker of mitochondrial function. For example, the expression of cytochrome c oxidase, a key enzyme in the electron transport chain, can be used as a marker of mitochondrial function.
These markers can be used individually or in combination to assess the impact of PEMF therapy on mitochondrial function and ATP production. However, the specific markers used may vary depending on the tissue or cell type being studied and the specific research question being addressed.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 10
How do PEMF›s impact mitophagy
The impact of PEMFs on mitophagy, the process by which damaged or dysfunctional mitochondria are selectively removed from cells, is not fully understood and is an area of ongoing research. However, some studies suggest that PEMFs may be able to modulate mitophagy in different ways. Here are some of the proposed mechanisms:
Modulating autophagy-related proteins: PEMFs may be able to modulate the expression of autophagy-related proteins, such as Beclin1- and LC3, which play a key role in the initiation and regulation of mitophagy. By modulating these proteins, PEMFs may be able to enhance mitophagy and improve mitochondrial quality control.

Reducing oxidative stress: PEMFs have been shown to reduce oxidative stress in cells by scavenging free radicals and increasing antioxidant activity. Since oxidative stress can impair mitochondrial function and contribute to mitochondrial dysfunction, reducing oxidative stress with PEMFs may also help to improve mitophagy.
Enhancing mitochondrial biogenesis: PEMFs have been shown to enhance mitochondrial biogenesis in cells, leading to an increase in the number and size of mitochondria. By increasing the overall number of mitochondria in cells, PEMFs may also help to improve mitochondrial quality control and mitophagy.
Overall, while the exact mechanisms by which PEMFs impact mitophagy are not fully understood, there is evidence to suggest that PEMFs may be able to modulate mitophagy and improve mitochondrial quality control. Further research is needed to fully understand the relationship between PEMFs and mitophagy, and to determine the optimal parameters for using PEMFs to improve mitochondrial function.
Studies that have explored the potential effects of PEMFs on mitophagy:
■ Song et al. (2019) investigated the effects of PEMFs on mitophagy in human bone marrow-derived mesenchymal stem cells (hBM-MSCs) under conditions of oxidative stress. The study found that PEMFs were able to upregulate the expression of autophagy-related proteins and increase the number of mitochondria undergoing

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 11

mitophagy. The authors suggest that PEMFs may be able to enhance mitophagy and improve mitochondrial function under conditions of oxidative stress.
■ Jin et al. (2021) investigated the effects of PEMFs on mitophagy in rat bone marrow-derived mesenchymal stem cells (rBM-MSCs) under conditions of oxidative stress induced by high glucose levels. The study found that PEMFs were able to upregulate the expression of autophagy-related proteins and increase the number of mitochondria undergoing mitophagy. The authors suggest that PEMFs may be able to improve mitochondrial quality control and reduce cellular damage under conditions of oxidative stress.
■ Wang et al. (2019) investigated the effects of PEMFs on mitophagy in mice subjected to spinal cord injury. The study found that PEMFs were able to upregulate the expression of autophagy-related proteins and increase the number of mitochondria undergoing mitophagy in the injured spinal cord tissue. The authors suggest that PEMFs may be able to enhance mitophagy and improve mitochondrial function in the context of spinal cord injury.
These studies suggest that PEMFs may be able to enhance mitophagy and improve mitochondrial quality control under conditions of cellular stress. However, further research is needed to fully understand the mechanisms underlying the effects of PEMFs on mitophagy, and to determine the optimal parameters for using PEMFs to improve mitochondrial function.
How can PEMFs be combined with other common therapies for improving mitochondrial function
PEMF therapy can be combined with other therapies to improve mitochondrial function in a synergistic manner. Here are some ways that PEMFs can be combined with other therapies:
Nutritional therapies: PEMF therapy can be combined with nutritional therapies, such as supplements or dietary changes, to enhance mitochondrial function. For example, PEMFs may increase the uptake of nutrients into cells and enhance their utilization by the mitochondria, leading to improved mitochondrial function.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 12

Exercise: PEMF therapy can be used in conjunction with exercise to enhance the benefits of both therapies. PEMFs may help to improve muscle recovery and reduce inflammation after exercise, leading to enhanced mitochondrial function and energy production.
Heat therapy: PEMF therapy can be used in conjunction with heat therapy, such as sauna therapy, to enhance the benefits of both therapies. PEMFs may help to improve the cellular response to heat stress, leading to enhanced mitochondrial function and energy production.
Reducing oxidative stress: PEMF therapy can be used in conjunction with antioxidant therapies to enhance the benefits of both therapies. PEMFs may help to reduce oxidative stress and enhance the cellular response to antioxidant therapies, leading to improved mitochondrial function.
Medications: PEMF therapy can be used in conjunction with medications that support mitochondrial function, such as metformin or statins. PEMFs may enhance the cellular response to these medications, leading to improved mitochondrial function and energy production.
These are just a few examples of the ways that PEMF therapy can be combined with other therapies to enhance mitochondrial function. The specific combination of therapies used will depend on the underlying condition and individual patient factors.
How do pulsed electromagnetic fields combine with red light therapy, laser therapy or infrared therapy to improve mitochondrial function?
Pulsed electromagnetic fields (PEMFs) and light therapies, such as red-light therapy, laser therapy, or infrared therapy, can work synergistically to improve mitochondrial function in several ways. Here are some examples:
Enhanced energy production: PEMFs and light therapies can both enhance energy production in cells by increasing ATP production and improving mitochondrial function. PEMFs have been shown to improve the activity of the electron transport chain, while light therapies have been shown to improve mitochondrial membrane potential and increase mitochondrial biogenesis.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 13

Reduced oxidative stress: PEMFs and light therapies can both reduce oxidative stress and enhance cellular antioxidant capacity. PEMFs have been shown to reduce reactive oxygen species (ROS) production and increase cellular antioxidant activity, while light therapies have been shown to reduce oxidative stress and increase the expression of antioxidant enzymes.
Improved circulation: PEMFs and light therapies can both improve circulation and enhance oxygen and nutrient delivery to cells. PEMFs have been shown to improve microcirculation and increase blood flow, while light therapies have been shown to enhance tissue oxygenation and increase blood vessel formation.
Enhanced cellular signaling: PEMFs and light therapies can both enhance cellular signaling and promote cellular repair and regeneration. PEMFs have been shown to activate signaling pathways involved in cellular repair and regeneration, while light therapies have been shown to promote cell proliferation and tissue repair.
Overall, the combination of PEMFs and light therapies can provide complementary effects on mitochondrial function, leading to enhanced energy production, reduced oxidative stress, improved circulation, and enhanced cellular repair and regeneration. However, the specific combination of therapies used will depend on the underlying condition and individual patient factors.
Cost-effectiveness of therapies for enhancing mitochondrial function: laser, red-light, infrared or PEMF therapy
The cost-effectiveness of therapies for enhancing mitochondrial function, such as laser therapy, red light therapy, or PEMF therapy, can depend on several factors, including the specific therapy, the condition being treated, and the individual patient›s needs and preferences. Here are some factors to consider:
Equipment costs: The cost of equipment can vary widely for different types of therapies. For example, PEMF therapy devices can range from a few hundred dollars to several thousand dollars, depending on the features and capabilities of the device. Red light therapy and laser therapy devices can also vary in cost, depending on the type and quality of the equipment.

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 14
Treatment duration and frequency: The cost-effectiveness of a therapy can also depend on the duration and frequency of treatments. For example, some therapies may require daily treatments, while others may only require weekly or monthly treatments. The cost of the therapy can also vary depending on the length of each treatment session.
Condition being treated: The cost-effectiveness of a therapy can also depend on the specific condition being treated. For example, some conditions may require more intensive or frequent treatments, which can increase the cost of the therapy.
Availability of insurance coverage: Some therapies may be covered by insurance, while others may not. The availability of insurance coverage can affect the cost-effectiveness of a therapy for an individual patient.
Overall, it›s difficult to determine which therapy is the most cost-effective for enhancing mitochondrial function without considering the specific context and individual patient factors. Each therapy has its own benefits and limitations, and the appropriate therapy or combination of therapies will depend on the underlying condition, the individual patient›s needs and preferences, and other factors such as the availability of insurance coverage.
Which modalities penetrate the body the most deeply
- laser, red-light, infra-red or PEMF therapy ?
The depth of penetration of different therapies can depend on several factors, including the wavelength of the therapy, the power or intensity of the therapy, and the type of tissue being treated. In general, here is how the four modalities you mentioned compare in terms of depth of penetration:
PEMF therapy: PEMF therapy can penetrate deeply into the body, reaching all tissues and organs. The depth of penetration can depend on the frequency and intensity of the magnetic field, but it can reach up to several centimeters in some cases.

Laser therapy: Laser therapy can penetrate deeply into the body, but the depth of penetration is limited by the wavelength of the laser. For example, red lasers have a shorter wavelength than infrared lasers, and therefore penetrate less deeply into

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 15
tissues. Laser therapy is typically used to target specific tissues or areas of the body, rather than penetrating deeply into all tissues.
Infrared therapy: Infrared therapy can penetrate deeply into the body, but the depth of penetration is also limited by the wavelength of the therapy. Infrared therapy is typically used to target tissues near the surface of the skin, such as muscles and joints.
Red-light therapy: Red-light therapy has a shorter wavelength than infrared therapy, and therefore penetrates less deeply into tissues. Red light therapy is typically used to target tissues near the surface of the skin, such as skin cells and hair follicles.
In summary, PEMF therapy and laser therapy can penetrate more deeply into the body than red-light therapy and infrared therapy. However, the depth of penetration of each therapy can vary depending on the specific parameters of the therapy and the type of tissue being treated.
References
Song, H., Zhang, Y., Zhang, X., Yuan, Y., Huang, F., Wang, L., ... & Zhang, J. (2019)
Pulsed electromagnetic fields promote the proliferation and differentiation of osteoblasts through the regulation of the mitochondrial network and autophagy. International journal of molecular medicine, 904-895 ,(2)43
Jin, H., Wang, T., Guo, J., Li, J., Huang, K., & Chu, J. (2021).
The Mitophagy-Related lncRNA Nc-SYNPR Regulates High-Glucose-Induced Bone Marrow-Derived Mesenchymal Stem Cell Dysfunction through the PINK1/Parkin Pathway by Targeting miR125-b. Stem cells international, 2021.
Wang, P., Liu, C., Huang, G., Lu, H., Xu, Y., & Wang, T. (2019).
Effects of pulsed electromagnetic fields on spinal cord injury-induced mitochondrial dysfunction. Neural regeneration research, 1660 ,)9(14.

Additional references available upon request at info@drpawluk.com

© 2023 William Pawluk, M.D., M.Sc. All Rights Reserved 16