

The Pathology Report
2024 Duke Pathology Annual Magazine
•
•
•
The Pathology Report
(July 1, 2023 – June 30, 2024)
Editor
Consulting
Writers
Department
Attn: Communications Strategist
Duke Medicine Circle DUMC 3712 Durham, NC, 27710
Email: pathnews@duke.edu
Phone: 919-684-3984
Dear Friends:
I am very pleased to share with you our 2024 Annual Report, which features in-depth stories about our people and showcases our department’s recent achievements and breakthroughs. This year, we’re celebrating Duke University’s Centennial, which started with a kick-off celebration on January 9th, 2024, and culminates with the graduating class in May 2025. We acknowledge this milestone with features about our department’s history and a story about one of the first Duke Blue Devil mascots, who was a Pathology resident.
Other exciting features highlight many of our team members’ advancements:
• How we’re using Artificial Intelligence (AI) to revolutionize the field of pathology and transform the ways diseases are diagnosed and treated

• How a 30-year quest to create a vaccine to treat urinary tract infections is yielding results
• How our Division of Hematopathology director has been impacting the field of lymphoma through discoveries that have led to modifications in the World Health Organization’s (WHO) classification of high-grade B-cell lymphoma
These aren’t merely success stories. They reveal our department’s continued work to provide more accurate diagnoses and better treatment plans for patients, improving their outcomes and quality of life.
We also share the phenomenal giving history and professional contributions of one of our major donors, who has lent his support to education over many years. This type of generosity empowers our people to be leaders in patient care, education, and research.
We are indebted to our alumni, faculty, staff, and trainees for your support and your important contributions. Please reach out to me if you’d like to share any stories, and I wish all of you a wonderful year.
Warm Regards,

Jiaoti Huang, MD, PhD Chairman, Department of Pathology
Duke
University School of Medicine


to Transform Pathology LEVERAGING AI
By Liz Proper Photography by STEVE CONLON

Artificial Intelligence (AI) is set to advance the field of pathology, fundamentally changing how diseases are understood, diagnosed, and treated. At the forefront of this transformation is Duke’s Department of Pathology, in collaboration with Duke Artificial Intelligence (AI) Health. Together, they have established Duke’s Artificial Intelligence and Computational Pathology Division, a pioneering initiative aimed at enhancing the accuracy, efficiency, and predictive power of diagnostic practices. This advancement hopes to provide quicker, more accurate diagnoses that can lead to earlier, life-saving interventions for patients and their loved ones.
The Department has identified priorities and started strategizing investments that will allow for the deployment of digital pathology and computational image analysis into the clinical service. The goal is to further improve diagnostic accuracy, prognostication, prediction, and ultimately personalized treatment. These advancements are designed to provide patients with treatments specifically tailored to their unique medical needs, improving outcomes and reducing the uncertainty that often accompanies medical care.
Kyle Lafata, PhD (left) and Laura Barisoni, MD (right)
Digital Pathology
Duke has made strategic investments in digital pathology, progressing from analog to digital imaging and laying the foundation for innovative uses of AI in the future. Digital pathology involves the acquisition, management, sharing, and interpretation of pathology information in a digital environment. The cornerstone of making a diagnosis is often the glass slide, which contains very thin slices of stained tissue that pathologists visualize under a microscope. Now, the glass slides
Computational Image Analysis
Digital pathology plays a pivotal role in computational image analysis, allowing for the implementation of AI algorithms to detect subtle patterns in both neoplastic and non-neoplastic diseases to improve diagnostic accuracy. AI excels in detecting “gaps” — subtle patterns or inconsistencies which can be overlooked by the human eye. These gaps can indicate early signs of disease or areas that require further investigation, making AI an invaluable tool for improving diagnostic sensitivity. By catching these early-warning signs, AI may help doctors intervene sooner, giving patients a better chance at successful treatment and recovery.
are being systematically scanned into whole slide images, which can be viewed on a computer monitor or mobile device, enabling the “anytime, anywhere” model. This digital infrastructure allows for the deployment of advanced methodologies, such as computational image analysis, which revolutionizes the way tissue damage is examined, quantified, and diagnosed. However, this requires a tremendous amount of investment in hardware, software, human intervention, and expertise necessary for implementation. Within the clinical

Leading the charge with AI and digital image analysis are co-directors of the Duke’s AI and Computational Pathology division, Carolyn Glass, MD, PhD, associate professor of Pathology, and Laura Barisoni, MD, professor of Pathology and Medicine. Several projects are conducted within the division. For example, Glass and Roarke Horstmeyer, PhD, assistant professor in Biomedical Engineering, are developing a digital polarization tool for remote diagnosis to enhance the accuracy and accessibility of specimen analysis. Meanwhile, Barisoni, Kyle Lafata, PhD, assistant professor of Radiation Oncology, and others have developed a workflow for the accurate and semi-automated assessment of kidney biopsies, which has potential to change current practices and provide patients with more precise and actionable diagnoses.
labs, “We have been thoughtful in our approach,” commented Associate Professor of Pathology Diana Cardona, MD, “growing our capabilities by leveraging immediate gains in efficiency and cost effectiveness followed by the need for remote access and flexibility during the pandemic.” These initial efforts are increasing the lab’s and pathologists’ comfort level with this shift in practice, resulting in a growing demand and interest in asking the fun question of “what next?”

Carolyn Glass, MD, PhD (left) and Roarke Horstmeyer, PhD (right)


Using AI to identify intestinal metaplasia
Currently, Duke is working on a project to recognize precancerous changes in the stomach lining, specifically focusing on a condition known as intestinal metaplasia. This condition involves the transformation of the stomach lining to resemble the intestines, which can increase the risk of developing gastric cancer. By leveraging AI, the project aims to enhance the early detection and accurate diagnosis of intestinal metaplasia, ultimately improving patient outcomes through timely interventions. Although this is in initial testing, AI has already detected about 5% of cases that pathologists missed. While AI can make mistakes, these occur less frequently than human error. As William “Will” Jeck, MD, PhD, director of Digital Pathology and Enhanced Diagnostics, noted, “The real potential lies in the collaboration between AI and pathologists.”
Jeck also co-leads the Nference project, which aims to scan nine million slides of Duke’s pathology archive. The project’s current research focuses on the development of practical implementation of AI and machine learning tools in pathology practice, supporting both diagnostic work and broader research efforts across the department. These initiatives are crucial to ensuring that AI and digital pathology enhance clinical care while maintaining regulatory and safety standards. By combining efforts, the accuracy of diagnoses can be significantly enhanced, leading to more precise treatment plans and better outcomes for patients, ultimately reducing the anxiety and uncertainty for both patients and their loved ones. This collaborative effort involves feeding large datasets into AI systems, which then learn to recognize subtle patterns indicative of disease. “It’s about giving the machine good data to work from and our ability to analyze the machine’s analysis,” said Jeck. The insights gained from these computational models are helping to refine diagnostic criteria and treatment protocols, contributing to more precise and effective medical care. What this means for those newly diagnosed is hope. It means catching cancer earlier, when it is more treatable, offering a better prognosis and greater peace of mind.
Going beyond the human eye
Computational image analysis leverages AI to identify and quantify characteristics beyond the capabilities of human vision. This approach is being championed at Duke by experts, such as Lafata and Barisoni, who is an international leader in digital nephropathology. Barisoni’s team, which includes biomedical and electrical engineers, physicists, and statisticians, uses AI to develop algorithms that accurately identify and classify kidney structures. They also apply pathomics—the study of tissue characteristics—to extract and quantify subvisual features, better characterizing kidney diseases and identifying digital biomarkers of disease progression. These technologies are currently being implemented in clinical research, with the goal of establishing robust AI-based protocols in clinical settings. The clinical deployment of these algorithms holds immense potential for improving pathologists’ performance and enhancing patient care. These efforts have the potential to directly contribute to better treatment outcomes, giving patients access to cutting-edge diagnostics.



Artificial intelligence algorithm highlights a focus of intestinal metaplasia (low-power image with AI overlay on right) missed by the original signing pathologist and three subsequent independent reviews, but agreed upon following review of the AI results. AI offers a way to provide quality control and improve diagnosis of focal findings. Intestinal metaplasia can be a sign of other important diseases, such as autoimmune gastritis or helicobacter pylori infection. It is also a risk factor for gastric cancer.
William Jeck, MD, PhD
Laura Barisoni, MD
Predictive Analysis
Predictive analysis leverages AI to examine historical patient data, helping predict disease progression and outcomes. This is particularly useful for diseases like gastrointestinal (GI) and liver disorders, where early and accurate predictions can significantly impact treatment plans. By anticipating how a disease might progress, doctors can tailor treatment plans to each patient’s needs, providing a more personalized approach that could improve the chances of successful treatment.
Personalized Medicine
Traditional medicine often relies on analyzing data across large groups of patients in clinical trials to determine the best diagnostics, prognostics, and treatments. However, what is considered optimal care on average might not be the best approach for an individual patient. Personalized medicine focuses on tailoring medical care based on a patient’s unique genetic and phenotypic characteristics. At Duke, efforts are underway to develop AI tools that can analyze these characteristics and predict how a patient’s disease will progress and respond to different treatments.
Duke is using predictive analysis to enhance patient care by anticipating disease trajectories. AI can be attentive to every case and absorb vast amounts of data during its training, allowing it to see patterns across multiple institutions. “AI has the ability to ingest an immense amount of data, including information from multiple institutions; whereas we, humans, wouldn’t be able to analyze all of that on our own,” said Jeck. This capability enables AI to provide insights that might be overlooked by human analysis alone, leading to more informed and proactive treatment decisions. For
patients, this means they can benefit from more accurate predictions about their health, allowing them to plan and make decisions. This can result in more accurate and timely treatments, potentially saving lives by catching diseases before they progress.
The use of AI in predictive analysis at Duke is exemplified by ongoing research projects that aim to refine these predictive models further. By continuously feeding new data into these AI systems, researchers are improving the accuracy and reliability of disease progression forecasts, ultimately benefiting patient care.

Professor of Pathology Rajesh Dash, MD, chair of the College of American Pathologists (CAP) Artificial Intelligence Committee, is spearheading efforts to prepare pathologists nationwide for the transformative impact of AI on personalized diagnostics, prognostics, and treatment strategies. At Duke, Dash is part of a team prototyping real-time AI diagnostics during bronchoscopy procedures, where cytology specimens are collected. His collaborators include Kamran Mahmood, MD, MPH, a pulmonologist and associate professor of Medicine, as well as Glass and Horstmeyer.
The potential for AI to enhance access to personalized medicine is immense. This approach means that treatments can be tailored specifically to each patient’s genetic makeup, improving the chances of a successful outcome and reducing the risk of adverse reactions. By integrating genetic, molecular, and clinical data, AI can help identify the most effective treatment plans for individual patients, minimizing trialand-error in medical practice and improving overall outcomes.


Rajesh Dash, MD

Clinical Deployment
Duke Pathology is at the cutting edge of integrating AI into medical practice, paving the way for groundbreaking advancements in disease diagnosis, treatment, and research. The collaborative efforts of Duke’s experts in digital image analysis, predictive analysis, personalized treatment, computational models, and diagnostic accuracy highlight the transformative potential of AI in pathology. As these technologies continue to evolve, there is a palpable excitement for the future, filled with hope for improved healthcare and support for clinicians facing the challenges of modern practice.
AI’s role at Duke includes ongoing training and validation of AI algorithms. These efforts are crucial for ensuring that AI tools meet rigorous clinical standards before widespread implementation. “It’s a process to hand automation over. Right now, we are in the step in-between. We
Improving Diagnostic Accuracy
Computer-aided diagnostics have the potential to increase accuracy, prognostication, and predictive value above and beyond current practices. Danielle Elliott Range, MD, associate professor of Pathology and vice chair of Equity, Diversity, and Inclusion, emphasizes the role of AI in advancing diagnostic accuracy in cytopathology. “Artificial intelligence has been integral to the clinical practice of cytopathology for decades. In combination with human expertise, AI is superior to either alone in diagnosing cervical lesions on Pap smears,” she said. “The use of AI in cytopathology will be key to improving diagnostics in other specimen types as well.” Advocating for the inclusion of diverse populations in AI research ensures that these technologies benefit all patients equitably.
Range is currently working on a project to design an algorithm that will assist pathologists in lowresource areas in the diagnosis and classification of thyroid tumors. By improving diagnostic accuracy in underserved areas, this project has the potential to significantly impact patient outcomes globally, offering hope to patients who might otherwise have limited access to advanced medical care. “Projects like these bring a level of medical expertise to remote parts of the world, significantly impacting global healthcare delivery,” she explained.
are teaching AI while still learning how best to do that,” said Jeck. The integration of AI into diagnostic workflows promises to reduce human error, standardize diagnoses, and ultimately improve patient outcomes. For patients and their families, this means more accurate diagnoses, quicker treatment plans, and a greater chance of positive outcomes, reducing the emotional and physical toll of prolonged medical uncertainty.
“There is robust investment and tremendous excitement in the potential of AI,” Glass shared, “but we also need to give close attention to ethics, as responsible AI is not trivial and should be taken into consideration.” With the FDA entering into this space of regulating laboratory developed tests and AI, another consideration is if burden and cost increase, will patient access decrease? Cardona weighed in, “This is something we are closely monitoring, and we are advocating for what is best for our patients, as the goal should always be to

keep our patients safe while being able to provide leading-edge, high-quality testing and diagnostic information in the least burdensome way.”
“AI will completely transform anatomic pathology; however, this transformation will probably take a very long time,” said Jeck. In similar accord, Glass shared, “Although the development of AI algorithms has become more popularized throughout leading academic centers in the world, the validation and actual clinical implementation science side of the field still remains a challenge. It will take heavy investment to move it forward.”

Danielle Elliott Range, MD
Carolyn Glass, MD, PhD

Rajesh Dash, MD (left) with residents Natalya Ramirez, MD (front) and Jarvis Williams, MD (back)

Notable AI-Related Achievements at Duke
• Strategic Partnership with Microsoft: Duke University and Duke Health have entered a five-year strategic partnership with Microsoft to support AI applications in medicine. This collaboration aims to advance healthcare delivery, champion health equity, and pioneer advanced research.
• Duke AI Health Director Appointment: Michael Pencina, PhD, has been named Duke Health’s first Chief Data Scientist. This role is designed to create a strategic direction for AI and data science at Duke Health, emphasizing both academic and clinical missions.
• Inaugural Duke Symposium on Algorithmic Equity and Fairness in Health: Duke AI Health and the Duke University School of Nursing held the inaugural Duke Symposium on Algorithmic Equity and Fairness in Health, addressing algorithmic bias in healthcare and developing methods and interventions to promote equity in health and healthcare delivery.
• Deployment of AI Tool ‘Copilot’ for Microsoft 365: Duke Health has implemented ‘Copilot’ to enhance healthcare delivery. This AI tool is designed to integrate with Microsoft 365 to improve efficiency and patient care.
• Digital Pathology Initiative at Duke University : Duke’s Department of Pathology has invested in a comprehensive digital pathology initiative to digitize all histopathology slides, allowing for AI-driven image analysis and improved diagnostic accuracy.
AI Publications by Duke’s Pathology Team
• Application of a Machine Learning Algorithm to Predict Malignancy in Thyroid Cytopathology : Led by Danielle Elliott Range, MD, this project is designed to assist pathologists in low-resource areas by using smartphone images of thyroid cytology specimens to classify thyroid nodules.
• Development of AI Tools for Kidney Disease: Laura Barisoni, MD, and her team have developed AI algorithms for the accurate and semi-automated assessment of kidney biopsies, which have the potential to revolutionize the diagnosis and management of kidney diseases.


APPROACHING
THE FINISH LINE
Dr. Soman Abraham’s Lifelong Quest for a UTI Remedy

Soman Abraham, BS, MS, PhD, has been searching for an effective treatment for urinary tract infections (UTIs) for over 40 years. His recent discovery of a unique bladder immune response focused on repair rather than eradicating bacteria is guiding his efforts to create an effective vaccine.
UTIs are one of the most common bacterial infections. They’re unique and bewildering because they tend to recur even after successful treatment, which for some patients presents a lifelong struggle. Large numbers of recurrent UTI patients — a majority of whom are women — also suffer from anxiety and depression, factors that compound the disease. The chronic pain, together with frequent voiding and associated lack of sleep, can be both physically and mentally debilitating. In many cases, a UTI recurs within six months of the first infection. Current vaccine strategies that include intramuscular injections to combat UTIs have had limited effects in reducing these recurrences.
By JAMIE BOTTA, MBA
Photography by EAMON QUEENEY
APPROACHING THE FINISH LINE

The Quest Begins
“When I began my PhD work in England in 1981, I sought to understand what was happening,” recalled Abraham. “We asked and answered several key questions over the years: Why is Escherichia coli (E. coli) the most common bacterial cause of bladder infections? What attributes of E. coli make it so pathogenic in the bladder?” Abraham found that E. coli bacteria are especially successful in infecting the bladder because they have the unique capacity to bind avidly to the bladder surface and resist the flushing action of urine. E. coli uses hair-like structures known as fimbriae to accomplish this, with an adhesive protein called FimH located at the tips of each fimbrial filament. (Figure 1). “This gives them the power to attach tightly to the bladder walls and resist the flushing action of urine. As fresh urine enters the bladder, adherent bacteria multiply in this medium, and within 20 minutes they can double in number, rapidly reaching numbers sufficient to initiate an infection,” said Abraham.
UTIs most commonly affect women, many of whom are young, healthy, and have strong immune systems. A question researchers struggled with was why these relatively healthy women experienced recurring UTIs when it would be expected that they would develop immunity against future infections after the first occurrence.

Figure 1. Electron microscopic image of a uropathogenic E.coli bacterium. Notice the hairlike filaments, called fimbriae, radiation from the bacterial surface, which mediate bacterial attachment. At the tip of each fimbrial filament is a protein called FimH which mediates attachment to the surface of bladder cells.
“The fact that healthy women kept coming back with UTIs again and again suggested some anomaly in the bladder immune system,” said Abraham.
Developing a UTI Vaccine
In spite of the questions regarding the immune system of the urinary tract, over the past three decades various researchers have attempted to develop a UTI vaccine. Many of the initial attempts have utilized a mixture of heat-killed uropathogenic bacteria as their vaccine. Abraham and few other researchers attempted a more refined approach. They theorized that a vaccine containing FimH protein might evoke antibodies that would block E.coli from binding to the bladder surface. In other words, they would prevent E.coli FimH from finding a binding partner on bladder cells. It was a similar idea to the one behind how the COVID-19 vaccine works.
In a study using mice, Abraham’s team found that vaccinating them with FimH protein evoked a strong antibody response in the circulation that offered 70% protection. This finding was in line with what other research labs had observed. However, when companies conducted human trials to test either the FimH vaccine or the vaccine comprising mixtures of uropathogenic bacteria in humans, they found that the antibody responses were weak and ineffective.
“This was very discouraging news,” recalled Abraham. “Then, we thought we’d take a different tactic — revisit what’s happening in the immune system in the bladder when UTIs occur. That’s when, after decades of searching, we finally found an answer!”
The Unique Bladder Immune Responses to Infections
To better understand the immune responses in the bladder, Abraham and his team started inducing multiple infections in their laboratory mice to mimic recurrent UTIs. They noticed a unique bladder immune response involving T cells that had been previously overlooked. Typically, there are two types of T lymphocytes recruited into infection sites: Th1 cells, which kill off pathogens as well as cells harboring pathogens, and Th2 cells, that arrive to repair tissue damaged by infection. Normally when an infection occurs, they both target the infected area. However, with UTIs, the majority arriving to the bladder were Th2 cells, which Abraham found surprising.
“It seems as though the Th2 cells involved in repair are rapidly mobilized to the bladder in large numbers, almost at the expense of the Th1, the cells that kill off bacteria,” Abraham observed. “As a result of the inadequate recruitment of Th1 cells, infectious E.coli in the bladder were not completely
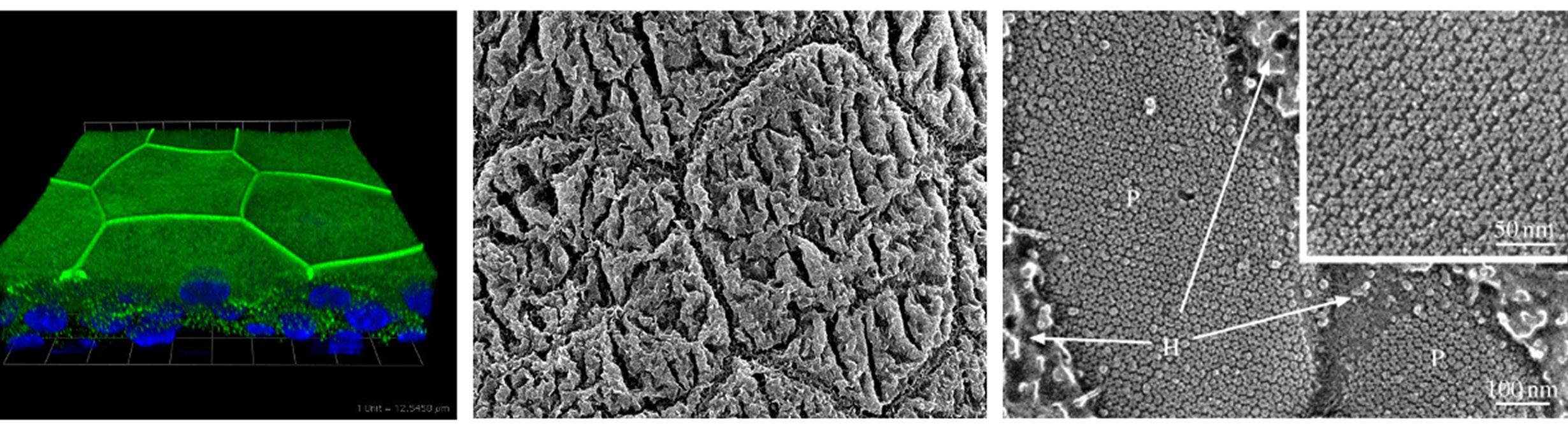
Figure 2. Microscopic images of cells lining the mouse bladder. Shown on the left is a stained cross-section of the bladder highlighting the tight junctions between adjacent cells (green) which serve as a barrier against urine. Shown in the middle is a scanning microscopic image of octagonal shaped bladder cells. On the right is a high-resolution image showing the cell surface uroplakin structures on the uroepithelium which resemble chain mail.

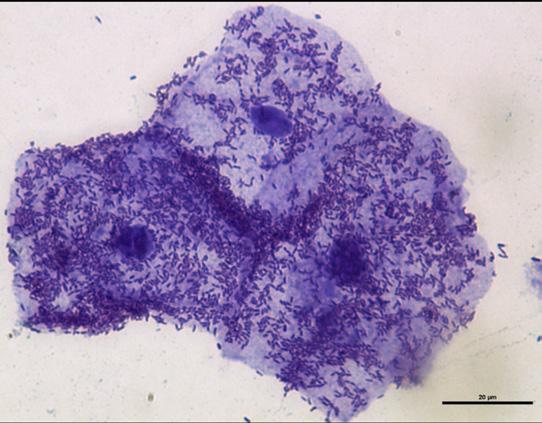

Figure 3. Scanning electron microcopy of the lining of the infected bladder. Shown above are numerous bacteria bound to the surface of the bladder. Below is a higher magnification of the same image revealing several bacteria in the process of entry into the epithelial lining of the bladder.
Figure 4. Micrograph showing uroepithelial cells shed from a patient with a UTI. Notice the large number of adherent bacteria found on the bladder cells. Shedding of epithelial cells is a powerful mechanism to reduce bacterial load in the bladder.
Figure 5. Cross-section of the mouse bladder weeks after a UTI. Notice the clumps of intracellular quiescent bacteria harboring in bladder cells (red).
cleared. In fact, pockets of residual bacteria were found to be hiding within the epithelial lining of the bladder.”
In their intracellular location, bacteria were unresponsive to antibiotics and could persist in a quiescent phase for months before re-emerging to initiate another UTI. The intracellular location of these bladder bacteria could also explain why vaccines evoking antibodies to FimH or to uropathogenic bacteria were never able to completely eliminate bladder bacteria.
The bladder is lined with unique epithelial cells that are tightly bound to one another. The surface of these cells is coated with a specialized structure resembling chain mail, composed of proteins known as uroplakins. Together, they form an impermeable barrier against urine. (Figure 2)
Abraham’s studies in mice found that when uropathogenic E. coli enter the bladder, they quickly multiply in urine and attach in large numbers to the bladder surface, some even entering the cells lining the bladder (Figure 3). In response to this invasion, the outermost layer of the epithelium undergoes widespread shedding, an action not observed in other body sites. While this remarkable response reduces the bacterial load in the bladder by up to 90% (Figure 4), it nonetheless exposes the underlying tissue to toxic components in the urine. Indeed, some of the burning sensation experienced during acute UTIs is due to salts and other harmful substances in urine coming into contact with the underlying bladder tissue.
Given the severe pathological consequences of losing the superficial bladder lining, it is not surprising that the bladder is preoccupied in repairing itself by selectively recruiting Th2 cells at the expense of Th1 cells. As a result of this disproportionate response, bladder bacteria are never completely eliminated (Figure 5), allowing them to persist to trigger another flare-up.
“With each UTI episode, the number of Th2 cells and the speed at which they arrive in the bladder increase, making the bladder more efficient at repairing itself and the lining increases in thickness,” said Abraham. “It’s like building muscle that becomes stronger and more responsive with repeated exercise. While the Th2 cell response grows more powerful with each infection, the Th1 response correspondingly weakens, predisposing the multi-infected bladder to recurrent infections.”
APPROACHING THE FINISH LINE
The Science Behind a New UTI Vaccine
These discoveries revealed a key and long overlooked role played by T cells in combatting UTIs. They also pointed to a novel target for vaccine development. In the wake of this new understanding, Abraham began forming the idea for a distinct and more efficacious UTI vaccine. He hypothesized that if one could preemptively recruit Th1 cells capable of attacking FimH-expressing E.coli into the bladder, it would not only protect the bladder from E.coli infections but also prevent the persistence of any residual bacteria. Thus, even if the bladder preferentially focused on repairing its lining during UTIs by recruiting Th2 cells, there would be sufficient numbers of Th1 already present to keep E. coli infection at bay.
Abraham and his team theorized that a vaccine formulation comprising of an adjuvant (an immune boosting agent) that selectively recruits Th1 cells combined with FimH protein could promote bacterial clearance. Since it is critical that this Th1 immune response be directed to the bladder, it would be necessary that the vaccine be delivered there. It was also expected that this vaccination strategy would induce production of circulating FimH-specific antibodies which contribute to protection, although not against intracellular bacteria.
Indeed, the Abraham team found that instilling this new vaccine formulation in the bladders of mice not only evoked a strong circulating antibody response to FimH but also, importantly, a strong Th1 response in the bladder. When these immunized mice were challenged with E.coliinduced UTIs, the mice were protected from infection. It also completely eliminated residual bacteria that normally persist in the bladder post-infection, even in mice that have experienced multiple UTIs. So, giving the vaccine formulation directly into the bladder was the key to bringing in Th1 cells that normally wouldn’t arrive to clear all the hidden bacteria.
Significant Advances
Adapting the vaccine for human use presents several additional challenges. Abraham’s team has recently overcome one key hurdle. While injecting small volumes of their novel UTI vaccine into the mouse bladder space using a catheter evoked a strong protective immune response, this approach is not feasible in human bladders, which are many times larger. Conceivably, large volumes of the vaccine (e.g. 20 mls) would be needed to have its intended effect, which is neither practical nor affordable. The relatively large volume of vaccine is required because only a small portion of the vaccine is absorbed by the bladder lining due to its impregnable nature.
So, in order to deliver adequate amounts of vaccine, frequent booster doses would be required.
“Clearly this limitation represented a significant hurdle,” said Abraham. “Recently, we found that we could overcome this hurdle by injecting small volumes of the vaccine into the bladder cavity along with an agent that temporarily breaks down the bladder barrier. Making the bladder wall leaky at sites of vaccine deposition allows for easy penetrance of all of the vaccine into the tissue.”
In April 2023, Abraham and Professor of Pathology Herman Staats, PhD, were awarded a two-year R21 grant titled “A Novel Vaccination Strategy to Curb recUTIs” from the National Institute of Allergy and Infectious Diseases. The grant enabled Abraham’s team to examine whether they could enhance their vaccine regimen by reducing the number of booster doses needed. This involved modifying the components of the vaccine and identifying additional clinical indicators of its effectiveness. The new information should facilitate the approval process from the Food and Drug Administration (FDA) for clinical studies.
“I believe there is renewed enthusiasm for vaccines, especially following the COVID-19 pandemic,” said Abraham.
Other Milestones to Meet
The R21 study is aimed at optimizing the delivery of the UTI vaccine in the bladder cavity and identifying potential markers of vaccine efficacy that can be utilized during human clinical trials. Another milestone that will facilitate early approval of a clinical study by the FDA is demonstrating the efficacy of the vaccine in a second animal species.
Abraham’s lab plans to test the efficacy of their UTI vaccine in preventing E.coli -induced bladder infections in rabbits. The rabbit bladder has many similarities to that of humans and therefore should provide valuable insights to how human bladders are likely to respond to the UTI vaccine.
A major step is securing funding for the clinical study. Abraham is pursuing two sources simultaneously. The first is the National Institutes of Health (NIH) , and the second is from industry or public-private partnerships, which is being sought with the help of Dennis Thomas, PhD, associate director of Duke’s Office for Translation & Commercialization
Approaching the Finish Line
A UTI vaccine can’t come soon enough. The adverse psychological effects of UTIs can be as debilitating as the physical pain of infection.

“I regularly receive emails and phone calls from UTI patients or their relatives inquiring about the vaccine and being part of the trial,” said Abraham. “One caller even inquired about its use for their cat’s UTI!”
UTIs, like many conditions that predominantly affect women, have long been under-studied.
“In light of the fact that there are more women in positions of power at the NIH and other research funding agencies now, there is hope that this perception will change. Indeed, officials at the NIH have recently indicated that they are especially interested in a vaccine against UTIs and that it is one of their top priorities.”
Abraham has also developed a potential new approach to treating UTI symptoms. On March 1, 2024, he published a paper with his colleagues in the journal Science Immunology that identified the likely cause of persistent pain in people with recurring UTIs, even after a round of antibiotics. The paper outlined the crosstalk between mast cells and nerves which causes chronic pain and frequent voiding, which are common symptoms for those suffering repeat UTIs. It provided a possible new approach to managing symptoms.
“In light of the fact that there are more women in positions of power at the NIH and other research funding agencies now, there is hope that this perception will change. Indeed, officials at the NIH have recently indicated that they are especially interested in a vaccine against UTIs and that it is one of their top priorities.”
Soman Abraham, BS, MS, PhD
“I feel a sense of satisfaction of coming to a point where we actually imagine a future for all this work we’ve put in,” mused Abraham. “You can see the promised land, the fruits of our labor. We haven’t reached it yet, but we can see it in the distant horizon. All these years we were working, we had no way of knowing whether we were on the right track or not. For the first time I have a feeling that maybe something will finally work out. There will be unforeseen challenges, of course, but I feel like we are closer than ever before to making a meaningful contribution for everyday people.”
For further reading
An Overgrowth of Nerve Cells Appears to Cause Lingering Symptoms After Recurrent UTIs (DukeHealth News, Feb. 21, 2024)
Direct Bladder Vaccination Halts Recurrent UTIs (BioWorld, March 12, 2021)
“Abraham Featured in TV Interview About UTI Vaccine” (www.pathology.edu, May 19, 2021)
Developing a UTI Vaccine That Expands Beyond Uro-vaxom and Uromune: Interview with Dr. Soman Abraham (www.liveutifree. com, Aug. 8, 2024)
Live UTI Free is an international community of researchers, clinicians, patients and women’s health advocates based in Europe.

A LEGACY OF EXCELLENCE
Ken H. Young’s Continuing Contributions to Hematopathology and Blood Cancer Study
KBy LIZ PROPER
en H. Young, MD, PhD, professor of pathology and director of Duke’s Division of Hematopathology, began his journey into hematopathology with a fascination for understanding diseases at the cellular and molecular levels. “The complex nature of the disease and its value to improve clinical management in patients is what attracted me to pathology,” he explained.
Photography by STEVE CONLON
Young spent his graduate career in pathology with Björn Dahlbäck, MD, who introduced him to hematology. Dahlbäck was a Swedish physician and member of the Royal Swedish Academy of Sciences. He was known for the discovery of thrombotic diseases and Factor V Leiden — a gene mutation that results in thrombophilia, which is an increased tendency to form abnormal blood clots that can block blood vessels. Young chose hematopathology as his specialty, working as a fellow with John C. Chan, MD, and Dennis D. Weisenburger, MD, known for the discovery of mantle cell lymphoma and the inauguration of the Lymphoma/Leukemia Molecular Profiling Project (LLMPP) at the University of Nebraska Medical Center.
“The significant success of LLMPP lays the foundation for the molecular classification of both B-cell and T-cell lymphoma in the world,” he said, appreciating the guidance from his mentors.
“The significant success of LLMPP lays the foundation for the molecular classification of both B-cell and T-cell lymphoma in the world.”
Ken H. Young, MD, PhD
Young’s work with the LLMPP and his fellowship training at the Howard Hughes Medical Institute, which allowed him to develop clinical and pathologic research on blood cancer, are standouts for him. To unite pathologists with similar academic interests and foster a better understanding of the molecular mechanisms of lymphoma and other blood cancers, he initiated a
Multicenter Lymphoma Consortium
This program, composed of major hematology centers in the United States and Europe, has been highly productive, leading to 92 publications in high-impact medical journals, including 38 invited review articles. “The consortium program is composed of major hematology centers in the US and Europe, and collaboration has been very productive with combined efforts,” Young noted.
Young joined Duke in 2019, where his research significantly impacts the field of lymphoma, particularly in diffuse large B-cell lymphoma (DLBCL), the most common and aggressive type of lymphoma. His work includes the development of the Visco-Young Algorithm for Practical DLBCL Classification, the impact of TP53 mutation in DLBCL in the rituximab immunotherapy era, and studies on MYC/BCL2 double expressors in DLBCL. These double expressors are associated with poor prognosis when treated with standard immunochemotherapy regimens.
“We have succeeded in the study of various therapeutic and prognostic biomarkers with important impact in the lymphoma field,” he explained. His pioneering studies contribute to modifications in the International Consensus Committee (ICC) and World Health Organization (WHO) classification of high-grade B-cell lymphoma with double hit and double expression. This work helps in providing more accurate risk stratification and better treatment plans for patients, improving their outcomes and quality of life.
In the past three years, he has focused on tumor-infiltrating normal B cells in DLBCL, inspiring the development of novel immunotherapeutic strategies for patients who have a disease that doesn’t respond to an adequate course of standard treatment. His research refines the genetic signature in subsets of DLBCL based on immune biomarker expression and tumor
microenvironment (TME) repertoire. Understanding TME’s composition is crucial for developing cancer therapies. Collaborative efforts within his consortium also have led and continue to lead to novel discoveries in rare blood cancers, such as primary brain and testicular lymphoma, which promise significant future clinical applications and novel drug development.
“Our preliminary data on primary brain and testicular lymphoma have revealed exciting novel discoveries that I envision will have significant impact on our future clinical application and novel drug development,” he said.
“The clinical and pathologic collaborations among the pathologists and hematologists with similar academic interest and passion will enhance the common academic interest.”
Ken H. Young, MD, PhD
These advancements mean that patients with these rare conditions can hope for better diagnostic tools and more effective treatments. Young’s Multicenter Lymphoma Consortium exemplifies the power of collaborative research in addressing clinical and pathologic questions. By combining the expertise of pathologists and hematologists from different centers worldwide, the consortium enhances academic pursuits and empowers medical contributions to improve diagnosis, treatment, and patient management.
“The clinical and pathologic collaborations among the pathologists and hematologists with similar academic interest and passion will enhance the common academic interest,” Young emphasized. This collaborative effort not only advances research but also fosters lifelong professional friendships and education among its members, ultimately improving patient care through shared knowledge and resources.
In January 2024, he collaborated with colleagues at various institutions to identify mutational cancer drivers and microenvironment factors for the progression of myeloma and lymphoma and to generate innovative and effective agents for cancer prevention and treatment. Their work resulted in the National Institutes of Health (NIH)/National Cancer Institute (NCI) awarding them a CAP-MGUS U54 Center Award. The award, totaling $4.65 million, is being disbursed over four years to the institutions who will share the funds. This funding reflects the strength of the Pathology Department and its robust collaboration with other institutions, which places it at the forefront of blood cancer pathologic and translational research. Based on progress made in tumor microenvironmental immune cell profiling (2024 Clinical Cancer Research), novel immunotherapeutic strategy has been developed and led to new NIH/NCI R01 funding in September 2024.
He continues to drive forward clinical practice in hematopathology and pathology research in blood cancers. His leadership in the Department of Pathology is instrumental in fostering an environment of academic excellence and innovative research. In June 2023, he assumed another leadership role when he was named as the new Research Quality Leader of the Pathology Research Quality Management Program (RQMP) and Vice Chair in the Department . In this role he is responsible for innovating and implementing best practices
in quality research, as well as with scientific integrity and accountability across Duke University. Outside of his professional life, Young enjoys hiking, badminton, basketball, cooking, and music, which provide a balance to his dedicated career in pathology.
Young envisions that large-scale clinical and pathologic studies will continue to support future research strategies and treatment algorithms. These efforts elucidate disease mechanisms, discover novel therapeutic targets, and identify prognostic biomarkers for follow-up evaluation and residual disease monitoring. Importantly, this research provides valuable resources for training and educating the next generation of physicians and pathologists.
“It’s important to train and educate our next generation of young physicians and pathologists, supporting them to be successful in their future careers,” he explained. This dedication ensures that future patients will receive care from highly trained professionals who are well-versed in the latest advancements in pathology.
Young finds his daily work highly rewarding, particularly in mentoring and supporting fellows, residents, and trainees in their careers. He takes pride in seeing successful young physicians and pathologists emerge from Duke University Medical Center, the Department of Pathology, and the hematopathology program. “We love to see more successful young physicians and pathologists coming from our Duke Medical Center, Pathology Department, and our Hematopathology Division, because they represent our future in the medical field,” he shared.
Young’s trainees speak highly of his mentorship and collaborative spirit. Now in the private sector, one of Young’s former mentees, Catherine Alexander, MD, shared, “Dr. Young has served as a role model to me throughout my hematopathology fellowship training. Not only is he prolific in terms of his research and
clinical accomplishments, but he also creates a very positive working environment. He has an infectiously enthusiastic attitude and consistently advocates for the success and wellbeing of his trainees.”
Zijun Yidan Xu-Monette, PhD, assistant professor in Duke Pathology, noted, “Dr. Young’s mentorship totally changed my career, since I had not worked on clinical aspects before the postdoctoral fellowship under his mentorship. During the postdoc job
“Dr. Young’s mentorship totally changed my career, since I had not worked on clinical aspects before the postdoctoral fellowship under his mentorship.”
Zijun Yidan Xu-Monette, PhD
interview almost fifteen years ago, Dr. Young made me realize that using my knowledge and skills in clinical researches will be meaningful and can make significant contributions to the patients.”
Beyond his dedication to mentorship, Young’s long-term goals include continuing to advance the field of hematopathology through innovative research and collaboration. He aims to further develop the Multicenter Lymphoma Consortium and explore new therapeutic targets for blood cancers. Additionally, he is committed to mentoring the next generation of pathologists, ensuring they are equipped with the knowledge and skills to push the boundaries of medical science for the future.

Notable Achievements and Honors for Ken Young
• Howard Hughes Medical Institute Fellowship
• Initiation of the Multicenter Lymphoma Consortium
• Development of the Visco-Young Algorithm for Practical DLBCL Classification
• Impact of TP53 mutation in DLBCL in the rituximab immunotherapy era, improving treatment strategies
• Studies on MYC/BCL2 double expressors in DLBCL, contributing to risk stratification and classification.
• Research on tumor-infiltrating normal B cells in DLBCL, inspiring new immunotherapies
• Refinement of genetic signature in subsets of DLBCL based on immune biomarker expression
• Discoveries in primary brain and testicular lymphoma, improving clinical applications




Historical Highlights of Duke Pathology
the Department of Pathology at Duke University has a rich history of leadership, innovation, and excellence in medical education, research, and clinical practice. Established on March 11, 1929, by founding dean Wilburt C. Davison, the department has grown under the guidance of distinguished chairmen who have left an indelible mark on the field.
Wiley D. Forbus, MD, PhD, the founding chairman, served from 1930 to 1960. Trained at Johns Hopkins University, Forbus brought excellence in anatomic pathology and practiced the Socratic method of teaching through case studies. His Friday “Round Ups” and “Pathology Conferences” were legendary. Forbus established the first medical examiner system in North Carolina and received the Gold-Headed Cane Award from the American Society for Investigative Pathology (ASIP, formerly the American Association of Pathologists) in 1975 for his contributions to pathology.
Thomas D. Kinney, MD, PhD, chairman from 1960 to 1975, was the first Duke Medical School graduate to return as a chair. He established experimental pathology and recruited outstanding faculty members. Kinney was a leader in automating clinical laboratories and developing pathology manpower. He was honored with the Thomas D. Kinney Faculty Teaching Award, reflecting his impact on medical education. Kinney received the ASIP Gold-Headed Cane Award in 1977.
Robert B. Jennings, MD, PhD, who chaired the department from 1975 to 1991, was a national and international authority on kidney and heart diseases. He performed pioneering research on acute glomerulonephritis and ischemic heart disease and recruited a world-class group of investigators to the department in the latter area. He was an early adopter of electron microscopy as a research and diagnostic tool; this remains a departmental strength. Jennings received the ASIP Gold-Headed Cane Award in 2007.
In 1991, following a stint by John D. Shelburne, MD, PhD, as interim chairman, Salvatore V. Pizzo, MD, PhD, took over
By LIZ PROPER
as chairman, spearheading the restructuring of laboratory and research activities under managed care. He consolidated diagnostic laboratories and recruited new faculty with subspecialty expertise, ensuring excellence in medical student and resident teaching. Pizzo’s research focused on the interface between blood proteins and the vessel wall.
David N. Howell, MD, PhD, served as interim chairman in 2015, followed by Jiaoti Huang, MD, PhD, who became chairman in January 2016. Huang, an expert in genitourinary pathology, has continued the department’s legacy of excellence, with active research in prostate cancer’s molecular mechanisms, biomarkers, and histological diagnosis.
“Since its founding, our department has been leading the field in research, patient care, and education. Legendary figures of pathology have worked here, and their work has transformed the field of pathology. Our department has also produced numerous leaders in pathology who work across the country. We are very proud to be associated with this storied department,” Huang said. Huang has been a pivotal leader, mentor, and scientist. As an internationally renowned surgical pathologist and prostate cancer researcher for over 20 years, Huang is a leading authority in studying molecular mechanisms, biomarkers, and novel therapeutics for prostate cancer. Huang’s research has been funded at a high level by the federal government and private foundations.
Duke Pathology resident, fellow, faculty alumnus, and adjunct professor, Fred Sanfilippo, PhD ’75, MD ’76, will receive the Gold-Headed Cane Award in 2025. Sanfilippo remarked, “This is a big deal for me because I consider this to be the ultimate award in the field of pathology. The awardees are all luminaries, and I’m not like those who have won it, typically. I’m a pathologist now, but for 20 years I wasn’t. I’m very proud to be considered in that class of company. It’s very humbling.”
The Department of Pathology at Duke remains at the forefront of medical innovation, driven by a commitment to research, education, and clinical excellence. This legacy of leadership
Forbus Kinney Jennings




and groundbreaking contributions continues to shape the future of pathology. Its chairs and their coworkers have advanced our knowledge of the pathogenesis of disease to an extraordinary degree, particularly in the crucial areas of cardiac ischemia, vascular biology, and neoplasia. At the same time, they have invariably been devoted diagnosticians and teachers, always willing to share time at the microscope and inspire the next generation of pathologists.
The Department of Pathology at Duke remains at the forefront of medical innovation, driven by a commitment to research, education, and clinical excellence. This legacy of leadership and groundbreaking contributions continues to shape the future of pathology.

Notable Achievements and Honors for Duke Pathology
• ASIP Gold-Headed Cane Award: Received by Forbus in 1975, Kinney in 1977, Jennings in 2007, and Sanfilippo in 2025, recognizing their outstanding contributions to pathology
• Thomas D. Kinney Faculty Teaching Award: Established to honor Kinney’s impact on medical education
• Establishment of the first medical examiner system in North Carolina by Wiley D. Forbus, MD, PhD
• Pioneering research in acute glomerulonephritis and ischemic heart disease by Robert B. Jennings, MD, PhD
• Innovations in experimental pathology and automation of clinical laboratories by Thomas D. Kinney, MD, PhD
• Leadership in restructuring laboratory and research activities under managed care by Salvatore V. Pizzo, MD, PhD
• In January 2024, Pathology Department Chair Jiaoti Huang, MD, PhD, and his colleagues at Duke University School of Medicine were recently awarded a $1MM Challenge Award by the Prostate Cancer Foundation for their work developing a therapeutic strategy to revolutionize the approach to managing patients who have few viable treatment options
Shelburne Pizzo
Howell Huang
The Blue Devil Med Student
A Tale of Service and Mystery
By LIZ PROPER
When not behind a 1950s microscope, Alphonse Von Schoote, a junior assistant pathology resident, could be found beneath Duke’s most coveted mask: its Blue Devil mascot , becoming the first medical student to strut its coveted cape.
“They got some orthopedic netting around his head and some long john’s from someplace, and we finally found some Duke blue dye,” said fellow med student Jerry Adamson, MD. “He was so animated that everybody in the stadium thought, wow, and they were all cheering him and applauding him.”
Adamson loved sharing stories of Von Schoote’s first game against Navy. In an unforgettable moment, Von Schoote dashed toward the Navy sideline, grabbed their live goat mascot, and began to carry it over to Duke’s side of the field. Although he managed to lift the goat, Navy fans quickly swarmed him, tossing him up and down before he escaped and collapsed on the Duke bench.
Not just a symbol of school spirit, Von Schoote also left a legacy in the medical field. After completing his Duke residency in 1958, Von Schoote’s life took a fascinating and ultimately tragic turn.
In the aftermath of WWII, he embarked on a medical mission trip to the South Pacific, where he served as a public health physician in the Truk Archipelago, now called Chuuk. His work in this remote location was marked by a deep commitment to the health and well-being of local populations, many of whom lived in areas near nuclear testing sites in the Marshall Islands.
Von Schoote’s involvement in humanitarian service caught the attention of scientists and researchers, notably Aaron Brill, a longtime ABCC (Atomic Bomb Casualty Commission) scientist, who had been interested in exploring the health effects of nuclear exposure on island populations. His fascination with Von Schoote’s work was further fueled by Von Schoote’s dedication to improving health outcomes in regions severely affected by post-war activities.
Alphonse Von Schoote
The 1950s in Chuuk were particularly challenging for local populations due to the long-term health effects from World War II activities, especially the aftermath of Operation Hailstone. The underwater wreckage from the battle, including sunken ships and aircraft, posed significant environmental hazards, such as contamination of the water and food supply from leaking fuel and munitions. These conditions contributed to a rise in health issues like skin diseases and gastrointestinal problems, making Von Schoote’s medical mission even more critical.

“They got some orthopedic netting around his head and some long john’s from someplace, and we finally found some Duke blue dye. He was so animated that everybody in the stadium thought, wow, and they were all cheering him and applauding him.”
Jerry
Adamson, MD


Von Schoote continued his medical training in pathology at several U.S. institutions and was deeply respected by his peers for his ability to blend medical expertise with a heartfelt dedication to those in need. His specific focus on parasitology and tropical medicine positioned him as a valuable asset in improving the health of island natives, who were dealing with a complex set of post-war health challenges.
Tragically, Von Schoote’s mission ended in mystery. In 1969, while attempting to replenish medical supplies, he was caught in a storm and disappeared at sea. Letters from ABCC and fellow colleagues show that his efforts in the South Pacific had not gone unnoticed. His untimely death left a gap in the field of tropical medicine and pathology, where his work was just beginning to make significant impacts. His contributions, both as the first Blue Devil and as a dedicated physician, continue to be remembered by those whose lives he touched.
Credit for uncovering these details and photography goes to Rebecca Williams of the Duke Medical Center Archives, whose research, alongside that of Aaron Brill, Rebecca Pattillo and other colleagues, has shed light on Von Schoote’s dual role as both Duke’s Blue Devil mascot and a dedicated humanitarian.
A contemporary Blue Devil mascot costume (Jack Craver Evans in 1952)
GENEROSITY IS ITS OWN REWARD
Dr. Fred Sanfilippo’s Commitment to Helping Students and Faculty
Fred Sanfilippo, PhD’75, MD’76, Duke Pathology resident, fellow, faculty alumnus, and adjunct professor, has been an internationally recognized physician-scientist and academic medicine leader for over four decades. He’s made major research contributions in immunopathology and transplantation and served as the pathology department chair at Johns Hopkins University, dean and medical center CEO at Ohio State University, and health science center CEO and health system board chair at Emory University. Throughout his career, he has recognized the help he received as a student and faculty member and is committed to return that support to others.
Sanfilippo began as an MD-PhD student at Duke in 1970, then did a residency and fellowship in pathology. He joined the faculty in 1979, and remained until 1993 as professor of pathology, immunology, and experimental surgery.
But his affinity for Duke goes beyond his education, training, and career. His wife, Janet, WC’72, MBA’80, was diagnosed with a rare ovarian germ cell cancer and treated at Duke in 1977. Thanks to the expertise of Edward Bossen, MD, and Bernard Fetter, MD, in making a rapid diagnosis, and to William “Bill” T. Creasman, MD, in developing a novel triple chemotherapy protocol, the treatment worked. Sanfilippo credits the Duke team with saving Janet’s life.
Seven years later, Duke neonatology saved their daughter, Lisa, after a very troubled delivery. Both are healthy and well, and their son, Joe, was born at Duke Hospital four years after Lisa. Janet went on to serve as associate dean for administration at Duke’s Fuqua School of Business as well as two other business schools before retiring in 2016. Lisa currently is a nurse practicing at New York University, and Joe works in healthcare as an associate partner at McKinsey.
A Supportive Student and Faculty Experience
Sanfilippo grew up in Queens, New York. After graduating high school in 1966, he received a summer research scholarship at the Max Planck Institute for Experimental Medicine in Göttingen, Germany. That scholarship experience, which he repeated the following two summers, infused him with a deep appreciation for the importance of scholarship support for students and

inspired his interest in the fields of molecular genetics and cellular biology.
As a student in the BA-MSc physics program at the University of Pennsylvania, Sanfilippo became involved in superconductivity research in the lab of subsequent Nobel laureate Alan Heeger. He was drawn to physics (and later to pathology) as fields that studied the basics of how things worked and the impact of interventions — a focus he would carry with him his entire career as a scientist and academic leader. While working on his master’s project in 1969, the idea that magnetic resonance (MR) could eventually be used to image patients sparked his interest in applying to MD-PhD programs. Of the many that accepted him, he chose Duke because of its unique curriculum, its strong Solid State Physics Department, and because it provided a
Fred and Janet Sanfilippo (front) on their wedding day with Duke Medical School classmates Bill Findley, Steve Teutsch, and Bob Lester
If you’d like to contact the Department of Pathology regarding fundraising and giving opportunities, please reach out to Emily James (812-499-1099).
funded fellowship for his entire training. Again, he saw the huge impact that financial support had on his career.
“Duke was a great fit for me,” said Sanfilippo. “I received a lot of valuable advice and support as a student and junior faculty member, which really shaped my entire career.”
He also was impressed at the collegiality of the Duke environment. Arriving as a full-fledged member of the 60’s with long hair, beard, and a “change the status quo” attitude, he was not the typical Duke medical student.
“People are often surprised to hear that I was a hippie before med school, having been to Woodstock and riding a motorcycle,” said Sanfilippo. But he was graciously accepted and rapidly became engaged in curriculum changes and other activities.
“It was an exhilarating time at Duke,” Sanfilippo said. “Duke is renowned today thanks to the legacy of innovative leaders back then who recruited great faculty and staff and supported their efforts in creating novel research, education, and clinical programs. I was very fortunate to have several mentors, and with their advice and support I changed my research focus and did my PhD in immunology, my residency in pathology, and stayed on the faculty with a primary appointment in pathology and my research lab in surgery.”
His clinical activities on the Duke faculty involved directing the Transplantation Immunogenetics Lab, the Immunopathology Lab, and the Renal-Transplant Surgical Pathology Service. His research focused on the impact of genetics on the outcomes of organ and corneal transplants in animal models, as well as large clinical data bases.
Life Beyond Duke
From 1985-87 Sanfilippo led the development of the national Scientific Registry of Transplant Recipients, which is used by the government to predict patient outcomes and monitor performance of transplant centers. The immediate and significant impact of this work increased his interests in predictive medicine, health services research, and performance improvement, which he has sustained ever since.

In 1993, he was recruited to Johns Hopkins University to create and lead an integrated model of a new pathology department from the three that existed and tasked to develop a model comprehensive transplant center. Using the tenets of predictive modeling and health services research, he tracked performance improvement of the new department across multiple parameters of research, education, clinical service, finances, and culture. The published results showed statistically significant, sustained improvement in all measures.
Subsequently, he assumed the leadership role as dean and CEO at the Ohio State University Wexner Medical Center to align the hospitals, faculty practice plans, and health sciences, which again resulted in a publication demonstrating statistically significant improvement in all measures and the development of one of the first biomedical informatics departments in the United States.
In 2007, Sanfilippo joined Emory University to lead the Woodruff Health Sciences Center and Emory Healthcare, where he made changes once more that improved organizational alignments and performance. He led a program that increased external funding for health service research more than four-fold.
Fred Sanfilippo, MD, PhD, (left), Jiaoti Huang, MD, PhD, (right) at Pathology Resident Graduation Ceremony in 2017
GENEROSITY IS ITS OWN REWARD
A Legacy of Giving to Support Students and Faculty
Over the years, Sanfilippo has been committed to supporting students and faculty in their academic and career journeys. “I’m fortunate to be able to endow scholarships for students at my high school, college, fraternity, and the medical schools at which I’ve trained and worked, and each one has particular purpose,” said Sanfilippo.
Soon after joining the Duke faculty, Dr. and Mrs. Sanfilippo became members of the Davison Club, with their support earmarked for student scholarships, and in 2001 they established a trust that includes a scholarship fund for MD-PhD students. They have gone on to support Duke with several additional gifts:
• Fred and Janet Sanfilippo Scholarship Fund (2013)
• Fred and Janet Sanfilippo Pathology Lectureship Fund (2017)
• Fred and Janet Sanfilippo Fellowship in Surgical Pathology Fund (2017)
• Fred and Janet Sanfilippo Pathology Professorship Fund (2018)
The lectureship endowment has enabled Duke Pathology to bring in high-profile speakers to cover a wide variety of topics. The Surgical Pathology Fellowship endowment has given the department an edge when competing for the best trainees, and the Pathology Professorship Fund has helped recruit an outstanding new member of the faculty, Hui-Kuan Lin, MD, PhD, who joined in May 2023.
In appreciation for their contributions, the Department created the Fred and Janet Sanfilippo Resident Research Award in 2017 to recognize a Pathology resident or fellow who distinguished themselves in research effort and ability, either from a basic science or clinical researchrelated project or publication.
Sanfilippo has stayed active with Duke, especially with the Department of Pathology. He has been a member of the Duke Health and School of Medicine Board of Visitors, and an Iron Duke golf participant in the Coach K Academy. He chairs the Duke Pathology Alumni Advisory Council, and was the resident graduation ceremony keynote speaker in 2017.
In 2016, his donation to the Association for Academic Pathology for medical students and residents to attend the annual meeting initiated the Thomas D. Kinney Scholars Program in honor of his former Duke MD-PhD Program director, dean, and pathology chair. Since its
In addition to his gifts to Duke, Sanfilippo established the following endowed programs:
• Fred and Janet Sanfilippo Physics Undergraduate Scholarship, University of Pennsylvania (2001)
• Fred and Janet Sanfilippo Pathology Research Fund, Johns Hopkins University (2001)
• Brother Peter Francis Scholarship, Archbishop Molloy High School (2014)
• Fred and Janet Sanfilippo Visiting Professor Lecture, Johns Hopkins University (2014)
• Sanfilippo Phi Phi Scholarship, AXP Fraternity (2015)
• Dr. Thomas D. Kinney Scholars Program, Association for Academic Pathology (2016)
• ASIP-Sanfilippo Visiting Lectureship, American Society for Investigative Pathology (2019)
• Fred and Janet Sanfilippo MD-MBA Scholarship, Emory University (2021)
• Fred and Janet Sanfilippo Pathology Professorship, Johns Hopkins University (pledged)
onset, hundreds of medical students and residents have applied, and more than 100 Kinney Scholar Awards have been made. His gift also started a Health Services Research and Education Grant program in 2018 for medical students and residents, with 5-10 grants awarded per year. In 2019, he endowed a junior faculty visiting professors’ program at the American Society for Investigative Pathology, to help faculty early in their careers.
Sanfilippo summarizes his giving succinctly: “Virtually all our gifts to Duke and elsewhere have been to help support the career development of students, trainees, and faculty as a small way of giving back what I was fortunate to receive.”
What Comes Next
Currently, Sanfilippo is on sabbatical to finish writing a handbook of advice for medical school faculty, which follows his previous handbook of advice for medical school chairs published recently. He has advised and mentored scores of students, faculty, and academic medicine leaders throughout his career and continues to provide help and support as needed.
He also remains involved in helping several foundations with their philanthropic efforts as a consultant and

Awards
• Duke University Medical School: Thomas Jefferson Award (1976)
• North Carolina Society of Pathologists: Wiley Forbus Award (1979)
• American Society of Transplantation: Elected President (1984)
board member. In addition to programs at Emory University and Johns Hopkins University, he’s working with colleagues at Duke, especially at the Margolis Institute for Health Policy, to expand health service research and student case competitions in health policy.
In his free time, he enjoys traveling with family and friends (especially on Duke Alumni Association trips), skiing, scuba diving, golfing, and solving difficult crossword and math puzzles.
When asked to sum up his career in just a few words, Sanfilippo says “Understanding how things work is what drives me as a scientist and leader. Academic organizations and programs are incredibly complex, and getting them to work better can significantly help the students, faculty, and patients they serve.”

• AOA National Medical Honor Society: Elected Member (1987)
• Reach for Sight Society: Physician Investigator Award (1990)
• University of Rochester: Medical Scientist Training Program Distinguished Scientist (1994)
• American Society for Investigative Pathology: Elected President (2001)
• Columbus Business First: Business Leader of the Year (2003)
• Duke University Medical Center: Distinguished Alumnus Award (2004)
• American Association for the Advancement of Science: Elected Fellow (2004)
• Columbus Technology Council: Enterprise of the Year CEO, (2004)
• National Multiple Sclerosis Society: Norman Cohn Hope Award (2005)
• Arnold P. Gold Foundation: 2005 Gold Humanism Honor Society
• American Cancer Society: John P. Minton Hero of Hope Research Champion Medal of Honor (2005)
• Emory University: MilliPub Club (2013)
• Johns Hopkins University: Distinguished Medical Alumnus Award (2017)
• Association for Academic Pathology: Distinguished Service Award (2018)
• American Society for Investigative Pathology: Gold-Headed Cane Award (2025)
The Sanfilippo family at their 50th Wedding Anniversary. Left to right: David and Lisa Herson, Janet, Fred, Olivia, Joseph, Jenny, and Lilah Sanfilippo
Janet and Fred Sanfilippo at Bhutan Eagle’s Nest in 2012
NEW FACULTY

Jeffrey L. Arnold, MD
Assistant Professor
On Jan. 8th, 2024, we welcomed Assistant Professor Jeffrey L. Arnold, MD, to our diagnostic faculty, where he primarily serves Cytopathology and Head, Neck, and Endocrine Pathology.
His professional and academic interests include the following areas:
• Undergraduate medical education (medical students) Graduate medical education (residents and fellows)
• Pathology pipeline (recruitment into the field of Pathology)
• Fine needle aspiration cytology
• Head and neck cancer
Arnold began his medical training by earning a Master of Science degree in Clinical Laboratory Science from the Medical University of South Carolina in Charleston. He obtained his Doctor of Medicine degree from the University of South Carolina School of Medicine.
He completed his Anatomic Pathology/Clinical Pathology residency at Montefiore Medical Center in New York, where he served as chief resident and received the Leo M. Davidoff Society of the Albert Einstein College of Medicine Award for Outstanding Achievement in the Teaching of Medical Students.
Arnold then travelled to Philadelphia for his two fellowships in Cytopathology and Surgical Pathology at Penn Medicine (University of Pennsylvania Health System). After completion of fellowships in 2016, he joined the faculty at Tufts Medical Center and Tufts University School of Medicine, where he received multiple teaching awards.
At Tufts Medical Center, Arnold was involved heavily in laboratory operations, administration and graduate medical education (GME) efforts. While there, he held two director titles. He also held two additional director titles at the Tufts University School of Medicine, where he served both as Pathology content director and lecturer for the first-year medical students from 2018-2023, and then ultimately as overall Pathology content director for the longitudinal preclerkship curriculum in 2023.
He has been a member of the American Society for Cytopathology since 2017, and the College of American Pathologists since 2010.

Rebecca Bacon, DVM, DACVP
Research Animal Pathology Service Director
Rebecca Bacon, DVM, DACVP, joined Duke with a dual appointment in the Department of Pathology and the Division of Laboratory Animal Resources (DLAR) at the end of December, 2023. DLAR plays a crucial role in maintaining the highest quality laboratory animal programs at Duke and serves as a valuable resource center for investigators.
Bacon provides diagnostic support for the laboratory animal colonies at Duke as well as research support via the Research Animal Pathology Service.
A North Carolina native, she graduated from North Carolina State University’s College of Veterinary Medicine.
“During veterinary school I developed a love for research pathology,” said Bacon.
Following graduation from veterinary school, Bacon worked in private practice for several years, first as an equine sports medicine and surgery intern at Piedmont Equine Practice outside of Middleburg, Virginia, and then as an associate at a mixed animal practice, Veterinary Medical Center, in Easton, Maryland.
In 2018, she joined a veterinary pathology internship at Kansas State University. The position was primarily focused on education in diagnostic anatomic and clinical pathology for cases submitted to the veterinary teaching hospital and state veterinary diagnostic lab, though she had the opportunity to participate in research on porcine reproductive and respiratory syndrome virus (PRRSV), a virus with significant economic impacts in US swine production; and in vaccine development for canine ehrlichiosis, a disease transmitted by brown dog ticks which can result in anemia, lameness, and neurologic symptoms.
In 2019, she joined a combined veterinary pathology/PhD program at Texas A&M University, completing her residency and earning board certification in veterinary anatomic pathology in 2022. She graduated from the PhD program in May 2024.
“I look forward to building on the relationships and service that my predecessor, Jeffrey Everitt, DVM, began during his tenure in this position,” said Bacon.
Jeffrey L. Arnold, MD
Rebecca Bacon, DVM, DACVP

John M. Carney, MD
Assistant Professor
On Jan. 15th, 2024, John M. Carney, MD, rejoined Duke Pathology as assistant professor of Pulmonary/Thoracic, Cardiovascular, and Autopsy Pathology.
He most recently served as assistant professor at the University of Rochester Department of Pathology and Laboratory Medicine in Rochester, New York, which he joined in 2022.
Carney attended Creighton University School of Medicine in Omaha, Nebraska, in 2013 for undergraduate medical school training. In 2017, he completed his Anatomic Pathology/Clinical Pathology residency training at Duke University, where he served as co-chief resident from 2015-2016. He followed that training with a Thoracic Pathology fellowship at Duke under the guidance of Victor Roggli, MD, Thomas Sporn, MD, and Elizabeth Pavlisko, MD, which he completed in 2018.
He remained at Duke on faculty, serving as assistant professor from 2018–2022, where he focused on Thoracic Pathology. During that time, he directed the Post-Sophomore Fellowship in Pathology, and was also involved in the Duke School of Medicine pathology course, teaching small group sessions from 2014–2022. He also served as the assistant course director from 2021–2022.
Carney’s clinical interests include non-neoplastic pulmonary pathology, with a focus on pneumoconiosis and interstitial pneumonia. He’s also interested in pleural malignancies. In addition to his clinical interests, he also enjoys teaching medical students, residents, fellows, and pathologists’ assistants.
“I look forward to getting started back in the department,” said Carney. “During my time at Duke and the University of Rochester, I have been fortunate to be involved with the Program’s Clinical Competency as well as Program Evaluation Committees. My additional interests and goals include seeking out and prioritizing opportunities to be involved within the lab, as well as the hospital/institution in general; and finding ways to be involved in state and national/international societies as they arise.” said Carney.

Rohini
Kannuswamy, MD Assistant Professor
Rohini Kannuswamy, MD joined the faculty on April 1st, 2024, as assistant professor. She primarily serves in Cytopathology, and her main areas of professional interests include fine needle aspiration cytology and gynecologic malignancies.
Kannuswamy brings a wealth of experience and knowledge in the field of cytopathology. Her academic journey began in India at Coimbatore Medical College, where she completed her medical school and residency training. In pursuit of advanced training and practice opportunities, she relocated to the United States in 2010 and completed a second residency in Pathology at the University of Missouri-Columbia.
In 2017, she moved to North Carolina to complete a surgical pathology fellowship, followed by a cytopathology fellowship, at Duke University. Post-fellowship, she practiced at LabCorp in Burlington, N.C.
“I look forward to embarking on a new phase of my career at Duke University,” said Kannuswamy. “I’m very excited for my new job that aligns more with my career aspirations and offers a multifaceted position that allows me to contribute to medical education while undertaking a challenging clinical role.”

Diana Kozman, MD Assistant Professor
On Sept. 1st, 2023, Diana Kozman, MD, joined our diagnostic Surgical Pathology faculty as an assistant professor, primarily in the areas of Gynecologic and Genitourinary Pathology. She attended the University of Cairo, Al Kasr Al Ainy School of Medicine, and served as a general practitioner in Cairo for a year after her graduation. In 2012, she moved to the United States and joined Emory Pediatric Pathology as a research intern for two years, which resulted in multiple publications. Kozman completed her Anatomic and Clinical Pathology residency at the Medical College of Georgia in Augusta, where she also served as chief resident. Following residency, she obtained fellowship training in both gynecologic and genitourinary pathology at the Cleveland Clinic.
She has multiple publications, including, but not limited to the following:
“Pediatric Right Ventricular Cardiac Steatosis Following Immunosuppressive Treatment”
“Serum Folate of Less than 7.0 ng/ ml is a Marker of Malnutrition”
• “Renal Neoplasia Occurring in Patients with PTEN Hamartoma Tumor Syndrome”
Her ongoing research projects include studies such as “Isolated PMS2 Loss in Endometrial Cancer and Mucinous Adenocarcinoma of the Prostate.”
John M. Carney, MD
Rohini Kannuswamy, MD
Diana Kozman, MD
NEW FACULTY

Mark Lee, PhD
Assistant Professor
On Feb. 1st, 2024, Mark Lee, PhD, returned to Duke as an assistant professor of Pathology. He serves in Duke’s Clinical Microbiology Laboratory, where he worked from 2019 to 2023, when he left to tend to family matters and work at Quest Diagnostics in the New Jersey/New York area.
“I’m happy to be back at Duke, and to come back to the Clinical Microbiology Lab and have the opportunity to work with Diana Alame, MD, MBE, and Lab Manager Jeanette Uzzell,” said Lee.
During his previous tenure, he had many accomplishments, including the following:
• Co-investigator of the National Institutes of Health (NIH) RADx-Underserved Population Grant Program — an initiative to reduce disparities for underserved populations who are disproportionately affected by the COVID-19 pandemic
• Expert panel member of the Infectious Disease Society of America (IDSA) COVID-19 Diagnostic Guidelines
• Co-authored over a dozen papers since 2019 while at Duke Lee’s goals include the following initiatives:
• Build sequencing infrastructure in the Clinical Microbiology Lab.
• Contribute to the department’s research and education mission.
• Continue to implement and develop clinical tests for patient care.
Duke is grateful for his return, and looks forward to supporting him in reaching his goals.

Huihua Li, MD, PhD
Assistant Professor
On July 1, 2023, Huihua Li, MD, PhD, joined Duke Pathology’s Cardiovascular and Pulmonary/ Thoracic Divisions as an assistant professor. He completed his combined Anatomic and Clinical Pathology (AP/CP) residency training at the University of WisconsinMadison, followed by a thoracic pathology fellowship at the University of Chicago. He is board certified in AP/CP.
Li obtained his Doctor of Medicine degree from the University of South China. He subsequently pursued a PhD degree in pharmacogenetics and completed his PhD training at the University of Pittsburgh. During that time, his research focused on ventilator-associated lung injury, idiopathic pulmonary fibrosis, and lung host immunity to infection, which ultimately contributed to the funding of two National Institutes of Health R01 grants.
Li’s current academic interests include immunotherapy and tumor microenvironment in mesothelioma, lung neoplasms and non-neoplastic lung diseases. In his free time, he enjoys playing basketball, hiking with family, and photography.
“Our department continues to grow with the expertise and impressive track record of our new faculty members. We’re grateful to have them join our team.”
Chair Jiaoti Huang, MD, PhD
*Includes faculty who joined in fiscal year 2024 (July 1, 2023 - June 30, 2024)
Mark Lee, PhD
Huihua Li, MD, PhD
THOMAS SPORN, MD Leaves a lasting Mark on Pulmonary Pathology
By LIZ PROPER
Photography by JAMIE BOTTA, MBA, and STEVE CONLON

For over 27 years, Duke’s Department of Pathology benefited from the contributions of Thomas Sporn, MD, particularly through his dedication to patient care and mentorship of the next generation of physicians. As an associate professor, Sporn charted a path in pulmonary care, specializing in the diagnosis of complex lung diseases. He continues this important work as an associate professor at East Carolina University, where he transitioned in 2021.
John Carney, MD, assistant professor of Pathology at Duke, who succeeded Sporn, shared, “Dr. Sporn has played a tremendous role in my career, guiding me as a trainee and as a colleague. He provided me the opportunity to put together a poster presentation early on during residency, ultimately laying the groundwork for my future interest in pulmonary pathology. I am fortunate for his mentorship and guidance. The department was made better by his presence and contributions.”
During his time at Duke, Sporn was known for his leadership, serving as chief resident in 1997 and later as the first faculty member to specialize in both forensic and pulmonary pathology. He also established the Pulmonary and Thoracic Pathology Division , a specialized section that became a cornerstone of the department. It helped to shape the department and influence peers across the medical landscape.
“One of the happiest days of my life was when I received the call that there was a position for me at Duke,” Sporn recalled. “I’m most proud of the section’s growth and academic contributions, and the opportunity to mentor fellows like Dr. Elizabeth Pavlisko and Dr. John Carney, who now continue the work we began together.”
Sporn also served as an assistant chief medical examiner for North Carolina, further demonstrating
Back row, left to right: Sergio Piña-Oviedo, MD, Victor Roggli, MD, Thomas Sporn, MD, David Howell, MD, PhD, Elizabeth Pavlisko, MD. Front row, left to right: Carolyn Glass, MD, PhD, John Carney, MD, Huihua Li, MD, PhD
THOMAS SPORN, MD
his expertise in forensic pathology. After leaving Duke in 2021, he briefly returned in 2022 to assist with onboarding new faculty members in pulmonary pathology.
Sporn’s expertise in diagnosing diseases such as pneumoconiosis and mesothelioma, often linked to occupational exposures like asbestos, has established him as a widely recognized leader in the field.
Victor Roggoli, MD, professor of pathology, mentored Sporn during his pulmonary pathology training, and said, “Thomas Sporn is a highly skilled anatomical pathologist who is very knowledgeable in all aspects of diagnostic work. His training as a pulmonologist gave him a unique perspective that is so important to optimal patient outcomes. He was always a genuine pleasure to work with and has a great sense of humor. His contributions to pulmonary research are outstanding, and we wish him continued success at ECU.”
Beyond his clinical and research accomplishments, Sporn’s influence is perhaps best seen in the careers of the fellows he mentored. One of his mentees, Elizabeth Pavlisko, MD, now director of the Anatomic Pathology and Digital Analytics (DAPDA) Laboratory and section chief of Pulmonary/Thoracic Pathology, credit him with helping to shape her professional development and inspiring her work in the field, “I consider Dr. Sporn a mentor, colleague, and friend. It is quite difficult to articulate the profound impact of Dr. Sporn’s contributions to the Department of Pathology as well as Pulmonary & Critical Care Medicine at Duke throughout his tenure at Duke. His expertise in pulmonary medicine, forensics, and thoracic pathology is a combination uncommonly found and hard to match. His presence in the department is greatly missed.”
Sporn reflected on his career journey, expressing gratitude to mentors like Roggli and colleagues such as Johnston-West Endowed Department Chair of Pathology Jiaoti Huang, MD, PhD, and Professor of Pathology David Howell, MD, for their

support throughout his time at Duke. “It was and always has been a dream of mine to work at Duke, and I’m beyond grateful for the opportunities I had there.”
As Sporn continues his career at East Carolina University, his lasting impact is evident through the fellows he trained, the research he pioneered, and the specialized pulmonary pathology section he helped build at Duke.
“It is quite difficult to articulate the profound impact of Dr. Sporn’s contributions to the Department of Pathology as well as Pulmonary & Critical Care Medicine at Duke throughout his tenure at Duke. His expertise in pulmonary medicine, forensics, and thoracic pathology is a combination uncommonly found and hard to match.”
Elizabeth Pavlisko, MD
Thomas Sporn, MD, as Chief Resident (left) and prior to retirement (right)
PETER D. ISSITT, PHD
Remembered for Advancing Transfusion Medicine
By LIZ PROPER
Professor of Pathology
Emeritus

Peter D. Issitt, PhD, passed away in July 2024, following a distinguished career that shaped both Duke University School of Medicine (Duke SOM), and the field of immunohematology. Known worldwide for his expertise in blood group serology, he was a pioneering figure in transfusion medicine, most notably through his influential publication Applied Blood Group Serology.
After joining Duke SOM, Issitt became a central figure in advancing transfusion medicine while mentoring countless students. Nick Bandarenko, MD, associate professor of Pathology, shared, “Both Dr. Issitt’s genius and legendary knowledge in immunohematology were matched by his wit and kindness. I am truly grateful to have learned from him.”
Issitt’s career began in London, where he worked with transfusion medicine leaders before moving to the US and serving at institutions like the New York Blood Center and Hoxworth Blood Center. At Duke, he was deeply admired as both a scientist and educator. David Howell, MD, PhD, professor of Pathology, reflected, “He was a gentleman scholar and my first teacher of transfusion medicine. He had an unforgettable wit and sense of humor that many warmly remember.”
His landmark text Applied Blood Group Serology became an essential resource, and his expertise in complex blood group systems such as Rh and MNS helped drive forward the science of immunohematology. Even in retirement, Issitt remained engaged with the Duke community and the broader field, regularly contributing to professional organizations such as the American Association of Blood Banks (AABB) and speaking at their Annual Meetings.
PATRICK J. BUCKLEY, MD, PHD
Retires, Named Professor Emeritus
By JAMIE BOTTA, MBA
On Feb. 2, 2024, Patrick J. Buckley, MD, PhD, retired from his position as professor of Pathology and was named professor emeritus. Buckley’s distinguished career with the department spanned 25 years, during which he served as director of Duke’s Division of Hematopathology from 1999-2014. He also served as medical director of the Hematology Laboratories for the Duke University Cancer Center and Bone Marrow Transplantation unit from 1999–2014, and of the Clinical Flow Cytometry Laboratory from 1999–2003.

“Dr. Buckley has had a career of great distinction at Duke,” said David Howell, MD, PhD. “Perhaps his most important contribution, however, has been in the area of education. His interactions with coworkers and trainees have invariably been informed by high ethical standards, professionalism, and great empathy and kindness.”
We are grateful to have had him as an integral part of the department for so many years.
Read more about his career, academic and personal history, life-long passion for cycling, and more here

Issitt’s contributions to Duke and the field of transfusion medicine continue to resonate with those influenced by his work and mentorship. His impact will be felt for many years to come.

Dr. Patrick Buckley (left) with his son, Ben.
Courtesy of FulwoodFuneralService.com
Courtesy of Patrick J. Buckley, MD, PhD
Steve Conlon
EQUITY, DIVERSITY, AND INCLUSION (EDI) COMMITTEE
Continuing our Commitment
Photography by STEVE CONLON, AVANI PENDSE, MD, PHD
Guided by the leadership of EDI Vice Chair Danielle Elliott Range, MD, our EDI Committee continues working toward its goal to create an inclusive environment for faculty, staff, and trainees with various perspectives and backgrounds. Over the past year, Range has worked with the committee to finalize a diversity strategic plan that aligns with Duke’s tripartite mission of patient care, research, and education. We would also like to recognize Anne Buckley, MD, PhD, for her contribution to the department’s EDI mission, and for being a dedicated steward of our organization.
Range has spent nearly 20 years in the education, research and practice of pathology. She works with other School of Medicine EDI leaders to advance the Moments to Movement strategic plan. As a member of the Durham and Duke communities, she sees her role as an opportunity to enhance relationships across diverse communities as they relate to pathology workforce, research, education, and clinical practice.


Department members gathered in May 2024 for the fifth EDI Committee book club meeting, where they discussed “The Night Watchman,” by Louise Erdrich. Front row, left to right: Jamie Botta, MBA, Wen-Chi Foo, MD, Karra Jones, MD, PhD. Back row, left to right: Emily Knutson, Sarah Bean, MD, David Howell, MD, PhD, Laura Hale, MD, PhD
Danielle Elliott Range, MD
Highlights of the EDI Committee’s achievements and activities
• Budget proposal for departmental EDI work with approval from Chair Jiaoti Huang, MD, PhD, making it possible to underwrite projects
• EDI Book Club has hosted five meetings since launching in June 2022, with books being purchased from the budget from a local minority-owned bookstore
• EDI resource library continues to be stocked with multiple books purchased and donated
• Underrepresented Minority (URM) mentorship in department, including virtual shadowing for undergrads and post-baccalaureate students with attendings and laboratory staff
• Attendance at numerous EDI meetings, conferences, workshops, and other events, inside and outside Duke
• Memberships in external EDI organizations, including the Association for Academic Pathology (AAPath)
• Sponsor support of Duke University’s SNMA association and annual MLK banquet
• Recruitment of speakers on EDI topics at multiple Grand Rounds
• Digital signage runs content to make us more visible to each other
• Weekly newsletter announcements to highlight EDI opportunities for department members across Duke University
• Race in medicine survey results analyzed in regard to Pathology, with plan for a custom Tableau analysis
• Inclusive representation of learners, staff and leadership on the walls of the department (photos)
• Plans for recruitment fair participation and second-look events
Notable Achievements


In October 2023, Associate Professor of Pathology Giselle Y. López, MD, PhD, received the Spark Award from the Association for Women in Science (AWIS) in recognition of her strong leadership skills and for her vocal advocacy for diversity and inclusive scientific practices.
In March 2024, Andrea Deyrup, MD, PhD, participated in a panel discussion following a presentation on “Using Race, Ethnicity, and Ancestry as Population Descriptors in Genetics and Genomics Research.” It was hosted by Duke’s Precision Genomics Collaboratory and Trinity College of Arts and Sciences. Leaders were Duke professor Charmaine Royal, PhD, and New York University professor Aravinda Chakravarti, PhD, co-chairs of the 2023 National Academies of Sciences, Engineering, and Medicine (NASEM) Report . It emphasized the importance of ensuring that genetics research benefits all groups in society and mitigates harm.
She was also named to the to The Pathologist Magazine’s Power List 2024. Deyrup was one of 20 Champions for Change awardees, selected by The Pathologist’s judging panel composed primarily of past Power Listers. Deyrup was recognized for her advocacy work to inspire pathologists to reject race-based medicine and discard outdated beliefs about biological race.
Visit our Equity, Diversity & Inclusion page to learn more.
Giselle Y. López, MD, PhD
Andrea Deyrup, MD, PhD

Ahja Buie, Autopsy Technologist
Anatomic Path Cases

FY24 141,791
Ayumi Deeny, M.H.S., PA(ASCP)CM, Pathologists’ Assistant
Cytology Cases

FY24 50,263
Doug Minot, Cytotechnologist II
Paraffin Blocks

FY24 360,881
Markece Mathis, Medical Laboratory Scientist
Laboratory Tests

FY24 12,982,717
Treasure White, Medical Laboratory Scientist, Cytogenetics
AROUND THE DEPARTMENT
Photography by Steve Conlon and Eamon Queeney
In March 2024, Duke announced 32 new Distinguished Professorships. 18 are in the School of Medicine, two of whom are members of our department:
• Hui-Kuan Lin, PhD, was named as Fred and Janet Sanfilippo Distinguished Professor
• Qianben Wang, PhD, was named as Banks Anderson, Sr. Distinguished Professor
Distinguished professorships are awarded to faculty who have demonstrated extraordinary scholarship in advancing science and improving human health. They were honored at the annual distinguished professorship event in May 2024. Read more about Lin, Wang, and the other honorees here. Read the “Duke Today” story here.
“Dr. Wang has been a leader in describing the factors influencing DNA transcription that drives cancer cell growth, particularly in prostate cancer. So I am pleased to see his work and leadership recognized by the university”
Eleanor Easley Distinguished Professor in the School of Medicine Daniel George, MD




In May 2024, the Duke School of Medicine (SOM) hosted its Spring Faculty Celebration at the Doris Duke Center at Duke Gardens, at which Pathology Professor Laura Hale, MD, PhD, received the 2024 Gordon G. Hammes Faculty Teaching Award. It recognizes continuing excellence in teaching and mentoring and exemplary commitment to the education of graduate students within basic science departments and graduate training programs in the SOM. This award is unique among faculty awards in that the recipient is selected by a committee of biomedical graduate students, not by SOM faculty or administration.
“Dr. Hale is a wonderful teacher and mentor who is truly loved by her students,” said Johnston-West Endowed Department Chair of Pathology Jiaoti Huang, MD, PhD. “What is remarkable is that she has been doing this for years and is always enthusiastic about teaching. We are very lucky to have such an outstanding mentor among us!”
Daniel George, MD, (left) and Qianben Wang, PhD, (right)
Hui-Kuan Lin, PhD
Qianben Wang, PhD
Laura Hale, MD, PhD

“The graduate faculty and students of the program are delighted that we finally have approval for this name change, as the new name more accurately reflects the nature and scope of research currently undertaken within the program.”
Soman Abraham, PhD
In May 2024, the Duke Board of Trustees approved changing the name of our PhD Graduate Program. It is now called the Graduate Program in Pathobiology and Translational Biosciences.
“The graduate faculty and students of the program are delighted that we finally have approval for this name change, as the new name more accurately reflects the nature and scope of research currently undertaken within the program,” said Director of Graduate Studies Soman Abraham, PhD.
“Besides, several of our sister Pathology Departments have already renamed their graduate programs to reflect the dynamic field of study that is undertaken in each of their programs.”
Soman Abraham, PhD
AROUND THE DEPARTMENT

Natalya Ramirez, MD (front) and Jarvis Williams, MD (back)
Co-Chief Resident Natalya Ramirez, MD, PGY-3, and Jarvis Williams, MD, PGY-1, examine a slide for sign-out in the “frozens” lab. Ramirez attended University of Texas Medical Branch John Sealy School of Medicine and her hometown is San Antonio, Texas. Williams attended Tulane University School of Medicine and is originally from Valdosta, Georgia.

Aaron Blackley, Supervisor of Immunohistochemistry/Biomarkers in the Division of Anatomic Pathology and Digital Analytics, has been with Duke Clinical Labs since 2014. His role includes overseeing the performance of immunohistochemistry and biomarker assays. He is involved in all facets of digital pathology selection, validation, and implementation. In addition to supervising technical staff, he participates in the training of residents and pathologists’ assistants for the utilization of digital assets.

Carla Smith, Clinical Technician II in the Division of Anatomic Pathology and Digital Analytics (DAPDA), who joined Duke in 1984, has been with DAPDA for 20 years. Prior to being named DAPDA, the division was called Molecular Pathology. It included Image Cytometry, where she worked as well. Smith accessions cases, processes samples, and scans slides, among other duties. She is also cross-trained in Pathology Record Control.
“I was with the labs for year, and knew Carla well,” said DUHS Talent Center Partner Leanna McKay, SHRM-CP. “She is a wonderful person and hard worker.”
“I was with the labs for year, and knew Carla well. She is a wonderful person and hard worker.”
Leanna McKay, SHRM-CP

Frances Chan locates a red cell unit for issue to a patient.
Frances Chan, an advanced medical laboratory scientist in Transfusion Services, works a four 10-hour weekend option shift and consistently serves as a weekend Person-in-Charge (PIC) on first shift. After graduating from the University of North Carolina at Chapel Hill, she completed her student rotation in the lab. She was then hired and has been employed in Transfusion Services for over 21 years.
Carla Smith
Faculty Leadership
Jiaoti Huang, MD, PhD Johnston and West Endowed Chair, Department of Pathology, Distinguished University Professor
David N. Howell, MD, PhD Sr. Vice Chair and AP&T Chair
Sarah M. Bean, MD Vice Chair of Faculty
Rex Bentley, MD Vice Chair and Director of Surgical Pathology
Diana M. Cardona, MD Vice Chair and Director, DUHS Anatomic Pathology Labs
Thomas Cummings, MD Vice Chair and Director of Residency Program
Rajesh Dash, MD Vice Chair for Pathology Informatics
Michael Datto, MD, PhD Vice Chair and Director of Clinical Pathology
Shannon J. McCall, MD Vice Chair of Translational Research
Danielle Elliott Range, MD Vice Chair of Equity, Diversity and Inclusion
Ken H. Young, MD, PhD Vice Chair for Research
Elizabeth Boswell, MD Chief, Pathology and Laboratory Medicine, Durham VA
Autopsy Pathology
Carolyn Glass, MD, PhD Associate Professor, Director
Louis R. DiBernardo, MD Assistant Professor
William Jeck, MD, PhD Assistant Professor
Laura Hale, MD, PhD Professor
Elizabeth N. Pavlisko, MD Professor
Huihua Li, MD, PhD Assistant Professor
John M. Carney, MD Assistant Professor
Shih-Hsiu “Jerry” Wang, MD, PhD Assistant Professor; Associate Director, Autopsy
Breast Pathology
Rachel Factor, MD Associate Professor, Section Head
Sarah M. Bean, MD Professor
Rex Bentley, MD Professor
Rajesh Dash, MD Professor
Cardiovascular Pathology
Carolyn Glass, MD, PhD Associate Professor, Section Head
Louis R. DiBernardo, MD Assistant Professor
John M. Carney, MD Assistant Professor
Huihua Li, MD, PhD Assistant Professor
Elizabeth N. Pavlisko, MD Professor
Cytopathology/FNA
Danielle Elliott Range, MD Associate Professor, Director, Cytopath Lab
Jeffrey Arnold, MD Assistant Professor
Sarah M. Bean, MD Professor Rajesh Dash, MD Professor
Rachel Factor, MD Associate Professor
Wen-Chi Foo, MD Associate Professor
Rohini Kannuswamy, MD Assistant Professor
Avani Pendse, MD, PhD Associate Professor
Dermatopathology
Maria Angelica Selim, MD Professor, Section Head
Jennifer Crimmins, MD Assistant Professor
Kenneth Ellington, MD Assistant Professor
Eric Morgan, MD Assistant Professor
Michelle Schneider, MB, BCh, BAO Assistant Professor
Gastrointestinal Pathology
Chanjuan Shi, MD Professor, Section Head
Diana M. Cardona, MD Associate Professor; Director, DUHS Anatomic Pathology Labs
Fengming Chen, MD, PhD Assistant Professor
Wei Chen, MD Assistant Professor
Cynthia D. Guy, MD Professor
William Jeck, MD, PhD Assistant Professor
Shannon J. McCall, MD Associate Professor
Avani Pendse, MD, PhD Associate Professor
Genitourinary Pathology
Wen-Chi Foo, MD Associate Professor, Section Head
Jiaoti Huang, MD, PhD Professor
John F. Madden, MD, PhD Associate Professor
Avani Pendse, MD, PhD Associate Professor
Gynecologic Pathology
Rex Bentley, MD Professor, Section Head
Sarah M. Bean, MD Professor
Natasha Iranzad, MD Assistant Professor
Diana Kozman, MD Assistant Professor
Head, Neck & Endocrine Pathology
Danielle Elliott Range, MD Associate Professor, Section Head
Jeffrey Arnold, MD Assistant Professor
John F. Madden, MD, PhD Associate Professor
Hematopathology
Ken H. Young, MD, PhD Professor, Section Head
Eric Carlsen, MD, PhD Assistant Professor; Director of Blood Cancer Center Lab
Luis Carrillo, MD Assistant Professor, Director, Hematopathology Lab
Elena M. Fenu, MD Assistant Professor
Natasha Iranzad, MD Assistant Professor
Anand S. Lagoo, MD, PhD Professor; Director, Flow Cytometry Lab
Jadee Neff, MD, PhD Assistant Professor; Assistant Medical Director, MPGG
Sergio Piña-Oviedo, MD Associate Professor
Wen Shuai, MD, PhD Assistant Professor, Associate Director Flow Cytometry Lab
Infectious Pathology
John F. Madden, MD, PhD Associate Professor
Liver Pathology
Cynthia D. Guy, MD Professor, Section Head
Diana M. Cardona, MD Associate Professor
Fengming Chen, MD, PhD Assistant Professor
Wei Chen, MD Assistant Professor
William Jeck, MD, PhD Assistant Professor
Shannon J. McCall, MD Associate Professor
Chanjuan Shi, MD Professor
Avani Pendse, MD, PhD Associate Professor
Neuropathology
Thomas J. Cummings, MD Professor, Section Head
Anne F. Buckley, MD, PhD Associate Professor
Karra Jones, MD, PhD Associate Professor
Yang Liu, MD, MS Assistant Professor
Giselle López, MD, PhD Associate Professor
Roger McLendon, MD Professor
Shih-Hsiu “Jerry” Wang, MD, PhD Assistant Professor; Associate Director, Autopsy
Muscle and Nerve Pathology
Karra Jones, MD, PhD Associate Professor, Section Head, Medical Director, EMICL
Anne F. Buckley, MD, PhD Associate Professor
Thomas J. Cummings, MD Professor
Shih-Hsiu “Jerry” Wang, MD, PhD Assistant Professor Ophthalmic Pathology
Thomas J. Cummings, MD Professor, Section Head
Anne F. Buckley, MD, PhD Associate Professor
Alan D. Proia, MD, PhD Professor
Shih-Hsiu “Jerry” Wang, MD, PhD Assistant Professor Pulmonary /Thoracic Pathology
Elizabeth N. Pavlisko, MD Associate Professor, Section Head; Director, DAPDA and PRC
John M. Carney, MD Assistant Professor; Associate Director, DAPDA and PRC
Carolyn Glass, MD, PhD Associate Professor
Huihua Li, MD, PhD Assistant Professor
Sergio Piña-Oviedo, MD Associate Professor
Victor Roggli, MD Professor
Renal Pathology
Laura Barisoni, MD Professor, Section Head
Anne F. Buckley, MD, PhD Associate Professor
David N. Howell, MD, PhD Professor
Soft Tissue & Bone Pathology
Diana M. Cardona, MD Associate Professor, Section Head
Wei Chen, MD Assistant Professor
William Jeck, MD, PhD Assistant Professor
Rex Bentley, MD Professor
Thomas J. Cummings, MD Professor
Undergraduate Medical Education
Andrea Deyrup, MD, PhD Professor, Director of Undergraduate Medical Education
VA Faculty
Elizabeth Boswell, MD Assistant Professor, Chief, P&LMS
Christopher Alley, MD Assistant Professor
Maureane Hoffman, MD, PhD Professor
Amy Lark, MD, PhD Adjunct Assistant Professor
Duke Regional Pathology
Michael Waugh, MD Assistant Professor, Chief and CLIA Director, DRH and Affiliated Laboratories
Maureen Bauer, MD Assistant Professor
Kenneth Ellington, MD Assistant Professor, Section Director, Blood Bank, DRH
Duke Raleigh Pathology
Rebecca Varley, MD Assistant Professor, CLIA Director, DRaH and Affiliated Laboratories
Wesley Mallinger, DO Assistant Professor, Section Director, Blood Bank, DRaH
Maggie Stoecker, MD Assistant Professor; Section Director, Hematology, DRaH
Huiwen Bill Xie, MD, PhD Assistant Professor
Research Faculty
Soman Abraham, PhD Grace Kerby Distinguished Professor; Director of PhD Program
Rebecca Bacon, DVM Assistant Professor
Laura Barisoni, MD Professor
Anne F. Buckley, MD, PhD Associate Professor
Ling Cai, PhD Assistant Professor
Dongfeng Chen, PhD Associate Professor
Ming Chen, PhD Associate Professor
Zhong Chen, PhD Assistant Professor
Donna Crenshaw, PhD Assistant Professor
Colin Duckett, PhD Professor
Laura Hale, MD, PhD Professor
Yiping He, PhD Associate Professor
Maureane Hoffman, MD, PhD Professor
Jiaoti Huang, MD, PhD Distinguished University Professor
Chelsea Landon, PhD Assistant Professor
Hui-Kuan Lin, MD, PhD Professor, Director of Prostate Cancer Research
Giselle López, MD, PhD Associate Professor
Everardo Macias, PhD Assistant Professor
Roger McLendon, MD Professor
Sara E. Miller, PhD Professor
Mikhail Nikiforov, PhD Professor
John Norton, DVM, PhD Professor
Jung Wook Park, PhD Rollie Assistant Professor of Correlative Pathology
Christopher Pirozzi, PhD Assistant Professor
Salvatore Pizzo, MD, PhD Distinguished Professor
Randall Reynolds, DVM Associate Professor
Herman Staats, PhD Professor
Mary Sunday, MD, PhD Professor
Ken H. Young, MD, PhD Professor
Qianben Wang, PhD Professor
Zijun Yidan Xu-Monette, PhD Assistant Professor
Retired from Clinical Practice
William Bradford, MD Professor
Patrick Buckley, MD, PhD Professor Emeritus
Jeffrey Everitt, DVM Professor Emeritus
Robert Jennings, MD James B. Duke Distinguished Professor Emeritus
Claudia Jones, MD Associate Professor Emeritus
Bruce Lobaugh, PhD Professor Emeritus
Barth Reller, MD Professor
Stanley Robboy, MD Professor Emeritus
John D. Shelburne, MD, PhD Professor Emeritus
Directors
Duke University Hospital Labs
Michael Datto, MD, PhD Associate Professor; Associate Vice President and Medical Director of DUHS Laboratories
Nicholas Bandarenko, MD Associate Professor; CLIA Director, Transfusion
Dongfeng Chen, PhD Associate Professor; Director, CTIL
Kristen Deak, PhD Assistant Professor; Associate Director, Molecular Pathology, Genetics and Genomics (MPGG)
Nancy Henshaw, PhD Assistant Professor; Associate Director, Clinical Microbiology
Diana Alame, MD Assistant Professor, Director, Clinical Microbiology
Mark Lee, PhD Assistant Professor; Associate Director, Clinical Microbiology
Jessica Poisson, MD Associate Professor; Associate Director, Transfusion
Catherine Rehder, PhD Associate Professor; Director, MPGG
Ludmila Francescatto, PhD Assistant Professor, Assistant Director, MPGG
Stefan Rentas, PhD Assistant Professor; Associate Director, MPGG
Sarah Rapisardo, PhD Assistant Professor, Associate Director, MPGG
Beth Shaz, MD Professor; Co-Director, Stem Cell Lab
John Toffaletti, PhD Professor; Dir., Blood Gas Lab; CHCL; CPED
Ruhan Wei, PhD Assistant Professor; Director, Clinical Chemistry
Administration
Amy Orange, BS, CFM Chief Department Administrator
Jeff Thomasson, MBA Director of Finance
Pamela Harris, MBA Director of Administrative Operations
Kelly Macklin, BS HR Director
Jamie Botta, MBA Assistant Director, Marketing & Communications
Jawanna Bell, CEAP, AS GME Coordinator, Residency/Fellowships
Michelle Johnson, MHS, PA, (ASCP), CM Program Director, PA Program
Ebony Ambrose, MBA Program Coordinator, PhD Program
Services
Brittany Harris Program Coordinator, Fellowship Program
Shannon J. McCall, MD, Director BioRepository & Precision Pathology
Sara E. Miller, PhD, Director Research EM
Shannon J. McCall, MD, Director Research Immunohistology
Steve Conlon Photopath
Visit www.pathology.duke.edu/faculty for the most current listing of department members.
40



Bernard F. Fetter, MD, was a beloved pathologist, educator, mentor, and colleague. He joined the Department of Pathology faculty in 1951, served briefly as acting chair in 1960, was promoted to professor in 1967, and became professor emeritus upon his retirement in 1991. Though a dwindling number of our current community had the pleasure of knowing him personally (he passed away in 2002), his name lives on in the department. The Bernard F. Fetter Teaching Award was established in 1992 to recognize outstanding teaching efforts by a Pathology faculty member. Fetter was a formidable, gifted, and serious pathologist — the consultant to whom trainees and peers alike always brought their

most challenging cases — but he also had a welldeveloped sense of humor that was seldom far below the surface. This is illustrated by the composite photograph at top, in which the entire department impersonated him (with masks-on-a-stick designed by Susan Reeves and Steve Conlon of PhotoPath), and the picture above, where he was caught lying down on the job with a group of students.
His teaching materials from 1951-90 are housed in Duke University Medical Center Archives here
