TOGETHER, WE WILL RADICALLY ADVANCE RESEARCH INTO



TOGETHER, WE WILL RADICALLY ADVANCE RESEARCH INTO

The Epilepsy Research Institute’s purpose is to leverage the extraordinary advances in epilepsy research over the past few years by radically transforming the research ecosystem.
Over the last year, the Institute has demonstrated the benefits of collaboration. The addition of new members and the emergence of integrated conversations, together with changes in the funder and policy landscape, offer new opportunities for us to continue to develop and promote our collaborative purpose.
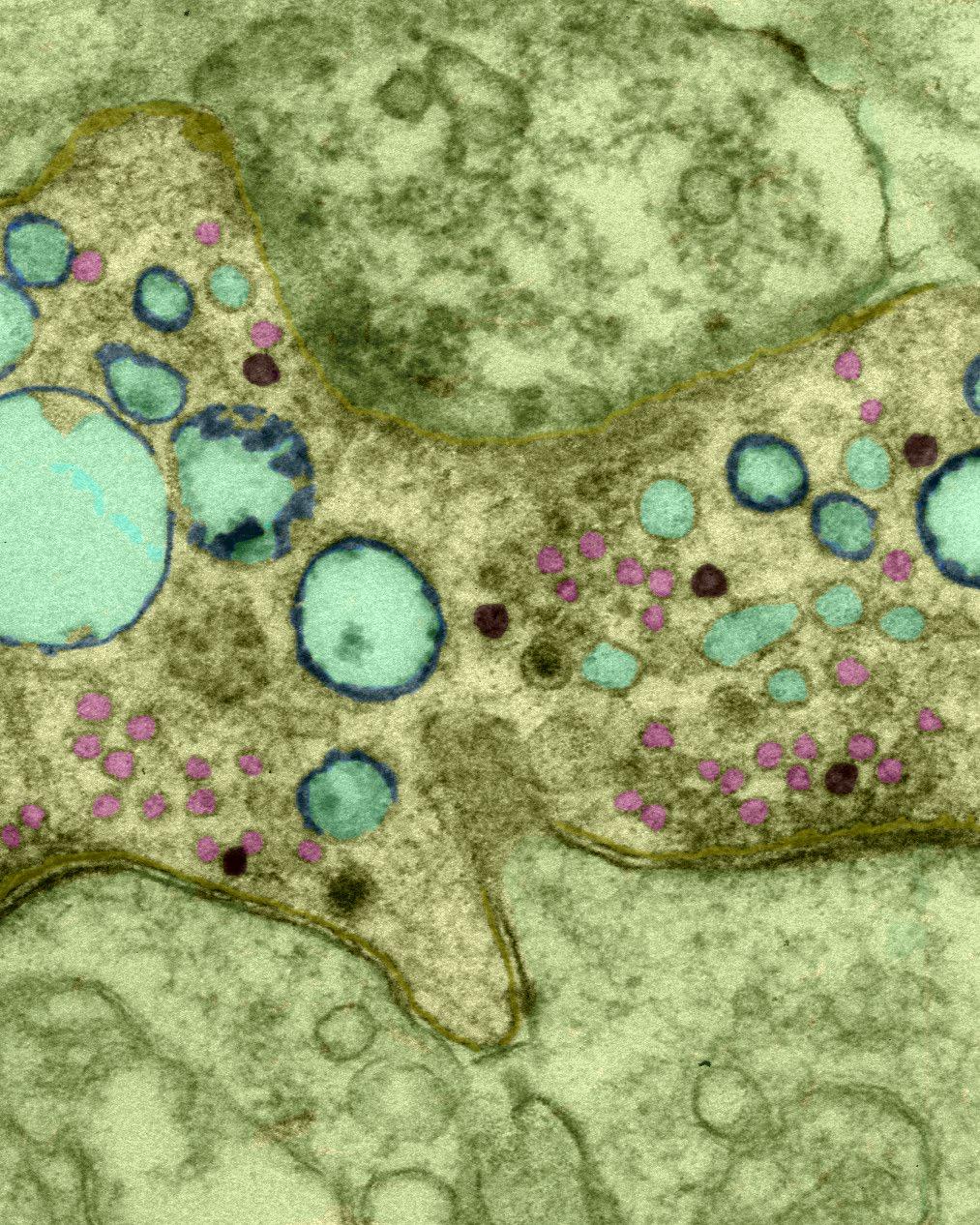
Breakthroughs in genetics, imaging and pharmacology have opened new pathways for understanding this complex condition, potentially transforming the lives of many who live with epilepsy.
There is also a growing recognition that epilepsy is not just a neurological disorder, but a complex condition that interacts with various other health issues. From mental health to cardiovascular diseases, epilepsy’s wide-reaching impact is becoming clearer to us all.
This holistic understanding offers the Institute the opportunity to foster new collaborations across different fields of medicine, leading to more integrated and comprehensive care for patients.
This roadmap demonstrates the exciting work the Institute has undertaken in the last year. Through this work we have brought together neurologists, geneticists, engineers, data scientists, and pharmacologists to explore where new ideas and opportunities are likely to emerge with this greater collaboration.
I am excited by the ambition of this document and look forward to working with all our stakeholders to deliver tangible benefits for those living with a diagnosis of epilepsy.
John Williams Epilepsy Research Institute Chief Scientific Officer
To radically advance research into epilepsy
INTEGRITY
We are open and transparent about all aspects of our work and employ the utmost candour in our focus to ‘radically advance research into epilepsy’.
COLLABORATIVE
We appreciate that it is only by working together we will achieve our vision of ‘a life free from epilepsy’. Our teamwork and partnerships reflect our integrity, professional approach and trustworthiness.
HONEST
We expect a high standard of excellence, supporting the best science with our systematic and rigorous approach to all of our work.
INNOVATIVE
We are courageous and ambitious to enable groundbreaking research and welcome innovative and creative ideas.
DIVERSITY & INCLUSION
We are respectful of all the people working with, and for us, including people living with epilepsy, researchers, collaborators and our supporters, fostering teams across diverse cultures and backgrounds and valuing their views and input.

Achieving Institute status in 2023 means that we are ideally placed to strengthen the epilepsy research ecosystem by driving investment and developing partnerships and collaborations between academia, the NHS, industry, funders, policy makers, politicians, and people living with epilepsy.
Our research roadmap will radically transform the epilepsy research ecosystem and offer hope to all who are living with epilepsy, as well as those in their wider social networks.
To advance research, the Institute will:
Facilitate UK and wider global conversation that will radically change the research agenda for epilepsy and related neurological disorders
Encourage inward investment into the area and increase the likelihood of effective progress towards better prevention, diagnosis, treatment and care for people living with epilepsy
Facilitate collaborations that will ultimately lead to the development of new diagnostics, treatments, technology and innovations for people with, and at risk of developing, epilepsy
Support, facilitate and encourage multiple site collegiates to bid for appropriate funding pots as described in this document
Understand the impact of the comorbidities experienced by people living with epilepsy and drawing on expertise and insights that are emerging from epilepsy adjacent research fields e.g. dementia, mental health to ensure that we are taking a whole person/syndrome approach
Harness enabling technologies, ensure research and clinical data is widely available to researchers, foster collaborations and attract early career researchers
Address inequalities by ensuring equitable access to opportunities to participate in research studies, access innovative clinical trials and ensure the very best clinical care is central to our advocacy
Ensure the voices of the one in 100 people affected by epilepsy are heard and acted upon
Crucially, through all of the above we will ensure people affected by epilepsy are at the heart of all research and able to shape the design and delivery of studies, to ensure we remain focused and on track.


As a first step to becoming the Epilepsy Research Institute, we identified the research priorities that matter most by engaging with a broad spectrum of stakeholders, including people with epilepsy, their families and carers, those bereaved by epilepsy, clinicians, health and social care professionals, and representatives from patient organisations.
Using the well-established James Lind Alliance methodology, we facilitated a national dialogue that brought together these diverse voices. This once-in-ageneration process culminated in October 2022, when we collated and ranked the Top Ten research priorities for epilepsy, reflecting the unified voice of the epilepsy community. These priorities have now served as the foundation of our work.
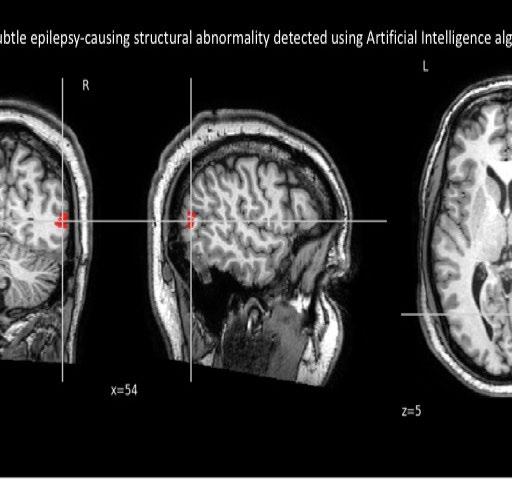
Priorities identified covered a broad range of topics, ranging from epilepsy-related deaths, the underlying mechanisms of epilepsy, to personalised medicine and brain health. This created opportunities to bring together researchers drawn from across fundamental neuroscience research, clinical research and novel methodologies, and included big data and Artificial
Intelligence (AI). (See Appendix A)
Gaining Institute status has empowered us to focus solely on working with our partners to design our operational structure and start to develop collaborations to enable us to translate these community generated research priorities into a robust roadmap that will shape our future work, bring hope to the wider community and help the Institute to radically transform the research ecosystem and deliver innovative solutions as it develops its overarching strategic plan.
To achieve this, our research activities are underpinned by the following six key themes:
Neurodevelopment
Advanced Therapeutics & Disease Modification
Mortality, Morbidity & Risk
Reproduction & Hormones
Enabling Technologies
Capability Building.
Each theme is led by three co-leads, who are supported by a task force comprising pre-eminent scientists and clinicians, future research leaders, industry partners and members of the Shape Network. Membership includes influential professionals drawn from both the UK and wider international connections.
Working collaboratively within this agreed framework, the theme co-leads and task force members have developed their own individual sub-strategies outlining their purpose, ambition, and key priorities for research in their own domain.
All of these six sub-strategies are at the core of the Institute’s overall strategy for the next five years as
Figure 1
described in this document.
Taken forward the six core themes will deliver effective collaborations that attract investment and lead to:
diagnosis
Effective prevention
Better treatments
We believe, once implemented, this will not only transform the research and translational landscape for epilepsy in the UK and globally but will most importantly address the research priorities of those living with the condition. (See Figure 1).
Radically transforming the epilepsy research ecosystem
Impactful collaboration

Under the leadership of our Programme Director, Professor Tony Marson, our underpinning research themes were developed.
To provide more context, the following text provides a summary of the purpose and key ambition in each of the six research themes. The importance of the research in each of these themes is reinforced through the powerful case studies provided alongside each section.





The Neurodevelopment theme aims to drive novel multidisciplinary research into the causes of epilepsy and its lifelong relationships with neurodevelopmental conditions, accelerating the development of interventions and improving quality of life for all affected.
To understand the causes and underlying biology of neurodevelopmental forms of epilepsy and use this knowledge to develop early interventions and precision therapies to improve quality of life.
To characterise the relationship between epilepsy and brain development, learning and behaviour and use this knowledge to improve brain health.
Clinical Co-Lead
Professor Sameer Zuberi
University of Glasgow

Basic Science Co-Lead
Professor Juan Burrone
King’s College London

Early Career Co-Lead
Dr Felix Chan
University of Birmingham
For many families, navigating a diagnosis of epilepsy is a journey filled with uncertainty, hope, and resilience. Here, Christophe shares the emotional and medical journey of his son’s epilepsy, and his hopes for future research.
In February 2022 our son, then three years old, began complaining of an itchy eye. Concerned, we took him to the eye clinic and although he was given the all-clear, his symptoms persisted. Just two days later, we received a call from his nursery to say that he had experienced a seizure.
After a series of tests, he was diagnosed with epilepsy. At first, I did not fully take in the gravity of this. I had heard of epilepsy but couldn’t imagine the impact it could have on a person’s life. My son’s initial diagnosis was a benign childhood form of epilepsy which we were told he would grow out of. We started him on the anti-seizure medication Clobazam and hoped his symptoms would stabilise and eventually disappear.
After that initial diagnosis, his condition deteriorated at a frightening pace. Despite multiple medications, his seizures worsened and it quickly became clear that his epilepsy was far more complex and harder to control than initially thought. By March 2022, his condition had worsened so much that he began to lose his speech. We were eventually transferred to Oxford John Radcliffe hospital, for specialist neurological care. Within 24hours our son was in the Intensive Care Unit.
After a week, we were transferred to the Bristol Royal Children’s Hospital for further assessment. Throughout this time, our son remained very unstable requiring continuous emergency medical intervention as doctors performed every available test, culminating in a Stereo EEG, hoping to pinpoint the source of the seizures. Unfortunately, this was unsuccessful. We then tried the ketogenic diet, which, combined with a careful medication balance gave us enough stability to be able to bring him home.
A later attempt to reduce his medication landed him back in the hospital, but it also led to an effective balance of medications that, from November 2022, controlled his seizures. However, the looming question of when the seizures would return was a daunting prospect hanging over us.

In February 2023, we received a breakthrough — the team identified the brain abnormality causing his seizures. Our son underwent brain surgery and six months later we began the process of weaning him off his medications. Unfortunately, after tapering his first drug, our son’s seizures re-emerged after an 18-month absence. We’ve had to re-introduce his medications and are now adjusting to a different future than we had hoped.
Epilepsy has had a profound impact on my son’s life. He has spent a significant amount of time in various hospitals, enduring numerous medical interventions. Even once his condition stabilised, the heavy mix of anti-seizure medication has significantly affected his ability to focus, as well as his speech, mood and levels of fatigue. These side effects impact every aspect of his daily life, from his education and social interactions to his emotional wellbeing and communication.
“Through my son’s journey, it has become clear how epilepsy can hinder a child’s development, particularly in critical areas like speech and motor skills.”
Beyond the seizures themselves, the medications he takes have a significant effect on his cognition and ability to keep up in school. Research into the relationship between epilepsy, anti-seizure medication and neurodevelopment is crucial, not only to better understand these impacts but also to create tools and resources that can help parents, carers, and educators support children affected by epilepsy and any neurodevelopment delays they may experience.
I hope that with further research, we can develop more treatment options for difficult-to-treat forms of epilepsy — ones that minimise the detrimental impact on quality of life and support better integration into society. I also hope for a deeper understanding of the various types of epilepsy, allowing for faster, more accurate diagnoses.
AIM
The Advanced Therapeutics & Disease Modification theme aims to facilitate and enable the development of innovative therapies and interventions across the translational pipeline for the treatment and prevention of epilepsy.
AMBITIONS
To develop a translational research framework to identify and test new treatments for epilepsies with high unmet need, spanning basic discovery to clinical trials.
To identify treatments that prevent the development of and/or reduce the severity of epilepsy.
To develop productive links with industry and regulators to speed the translation of candidate therapeutics.
THEME

Clinical Co-Lead
Professor Michael Johnson
Imperial College London

Basic Science Co-Lead
Professor Gabriele Lignani
UCL Queen Square
Institute of Neurology
Early Career Co-Lead
Dr Gareth Morris
University of Manchester/UCL
Malcolm, 69, has lived with focal epilepsy since he was two years old. His condition developed after contracting meningitis, which damaged areas of his temporal lobe and led to lifelong epilepsy. In this article, Malcolm shares his story, and the role research has played.
When I was younger, I experienced around four seizures a month, mostly as I was falling asleep. I was prescribed Phenobarbitone and Phenytoin common medications to treat epilepsy at the time.
“Epilepsy affected both my social skills and learning development, and the impact of this became more obvious to me later in life.”
In primary school, the staff were aware of my epilepsy and made sure that I understood what was being taught. My learning development improved during those years but this progress was quickly undone when I moved to a much larger secondary school. No one knew about my epilepsy, and I struggled to keep up.
My epilepsy had a significant impact on my attention span and my memory. Without the same support that I received in primary school, I fell behind my peers to the extent that I failed all my exams and my school leaving report was far from complimentary.
Throughout this period, I also found it difficult to make friends. It became easier in my teenage years as my cognitive ability improved and I developed learning strategies to improve my social skills. However, looking back I believe epilepsy affected my cognitive development. Even now, I sometimes struggle to find the right words and don’t have the detailed recall of specific events that my peers seem to.
It wasn’t until 2016, when my seizures started to increase to around seven a month that I was referred to a

neurologist for the first time. Over the next few years, my medication was changed from Phenobarbitone and Phenytoin to Levetiracetam and Lamotrigine, which are more widely used today. This change made a huge difference – I felt less drowsy, had more energy, and my seizures became less frequent and shorter in duration, compared to 25 years ago.
For the first time, I was introduced to support groups, where I could share my story and connect with people like me, who live with epilepsy. In 2019, this started my journey with Epilepsy Action, and I soon became a research volunteer and subsequently found the Epilepsy Research Institute and its Shape Network. Both organisations have had a significant impact on my life. They connected me with people who understand my journey, and just as importantly, they gave me a platform to help shape epilepsy research.
“I am really heartened to see the number of studies being carried out and the consequent progress in epilepsy research over the years.”
I feel privileged to be able to contribute to this important work, as a member of the Shape Network.
My own journey demonstrates why research into Advanced Therapeutics and Disease Modification is so important. The development of new and improved anti-seizure medication has greatly improved my quality of life and further research has the potential to make a real difference for others living with refractory epilepsy.
AIM
The Mortality, Morbidity & Risk theme aims to accelerate research through multidisciplinary approaches to identify risk factors, reduce morbidity and prevent epilepsy-related deaths.
To prevent all avoidable epilepsy related deaths.
To identify pathways and mechanisms that can be targeted to prevent Sudden Unexpected Death in Epilepsy (SUDEP).
To identify and stratify people with epilepsy to reduce their risk of mortality and/or morbidity.
To understand the bi-directional relationships between epilepsy and other mind-brain health conditions, using this to inform treatments and improve quality of life for people with epilepsy across the lifespan.
To understand the comorbidity of complex genetic and acquired epilepsies.


University of Oxford
University of Manchester/UCL
University of Warwick
Murray and his wife Emma have been raising funds for epilepsy research since the sudden death of their daughter, Lara, 10 years ago. Here, Murray shares their story and what they’ve learnt from their experience.
Our daughter Lara was born 32 years ago. When she came home from hospital after a few days all seemed fine. However, soon afterwards, we started to notice that she would occasionally ‘flinch’ in a strange way - putting her arms, feet and hands straight out. We got concerned at this and went to see the GP and after a few weeks, Lara was finally put on the EEG machine where she ‘flinched’ again a number of times.
Lara was immediately put on medication with the instruction that we should ‘double the dose’ if Lara continued to fit. Emma believed the medication was actually not helping and she wanted to do something rather than nothing. She turned to homeopathy despite my misgivings (I was science trained and sceptical about such therapies), but the seizures actually stopped soon after a short course of homeopathy and Lara later came off drugs altogether.
For around six years thereafter Lara appeared not to suffer from any seizures at all and she developed well. Until one afternoon when Lara (now aged 8) suddenly collapsed in her room. Immediately she was placed on medication which proved pretty effective. She was also showing signs of puberty, and it seemed that this early puberty had somehow triggered the re-start of seizures.
Soon after Lara took her GCSEs, we were told she could no longer remain on the drug to ‘side effects’, as she was now of childbearing age. This change in medication was apparently necessary but regrettable. It was the start of what I would call a “suck it and see” journey to try to find the right drug replacement. During this period, she would have several seizures. More than once, she woke up with a black eye from her fall and would be taken to hospital for a check-up. She told us that having epilepsy was like living in a bubble… she would never know when she might wake up in a strange place.
On 7 June 2014 she was 22, Lara had a fun weekend out clubbing, celebrating her birthday with friends. The

following week, on Monday 16 June Emma went up to her flat to find her lying across her bed and not breathing. Emma called an ambulance and I started CPR. Paramedics took over and then a doctor arrived. They came out and told me her heart had been re-started and gave me praise for doing a good job.
In the next 24 hours in hospital it was clear to the doctors that her brain had ‘coned’ and tests confirmed it. As we received this news the doctor asked whether we would consider, knowing Lara’s views, making her organs available for transplant. We agreed there and then - it was a whirlwind of form filling, grief, regret and soul-searching.
What did we learn from Lara’s struggles in her 22 short years and what could we have done differently?
“There needs to be more knowledge and a greater understanding of what epilepsy is and how dangerous it can be.”
Epilepsy is debilitating – even when seizures are relatively infrequent. They can hold back development, cramp lifestyle and activities, cause depression and social exclusion and seizures are, let’s face it, downright dangerous for all manner of reasons.
Early diagnosis is definitely important as is, I would suggest, the need for a wearable device or implant to monitor seizure patterns and raise alarm when necessary. Seizure diaries that patients are asked to keep are, I believe, variable in quality and validity. Good quality data harvested from technology must be obtained and shared to support research.
A trial and error process of medication is one way to go, and may work for some, but I sense that we need to find a route to greater pharmacological accuracy and focus. Will artificial intelligence offer any assistance? The ultimate goal of course has to be the total control or elimination of seizures if possible. High quality research and research collaboration is key – and that is where the Epilepsy Research Institute comes in.
The Reproduction & Hormones theme aims to advance and accelerate research into the study of reproductive health and hormones in epilepsy across the lifespan, working across the translational pipeline to deliver impactful patient benefit.
To inform the development of safer anti-seizure medicines for people with epilepsy who wish to have families.
To enable reproductive decision-making for men and women with epilepsy by expanding translational research to build evidence-based risk information and how to deliver this.
To find ways to reduce international rates of children born with intellectual disabilities and congenital abnormalities related to the use of anti-seizure medications.
To decrease the rates of deaths in people with epilepsy in their reproductive years.
To overcome the failure to treat seizures influenced by hormonal changes and the associated risks (e.g. mental health).
To mitigate the impact of epilepsy and anti-seizure medication on male and female reproductive hormones throughout the lifespan.



University of Manchester
After developing epilepsy in adulthood, Anna became a supporter of epilepsy research going on to become a Founding Funder of the Epilepsy Research Institute. Anna is specifically interested on the effect of hormones on her seizures. Here, she shares more on her experience of living with epilepsy and why research into reproduction and hormones is important.
I found out I had epilepsy aged 31 when I woke up in the A & E department, with no memory of how I got there. I had my first seizure earlier that day at 5.00 am when I was feeding my 6-month-old daughter at home. The last thing I remember was collapsing onto the kitchen floor.
When I was first diagnosed with epilepsy I was in complete denial. Complete denial!
“An epilepsy diagnosis for me was shocking and frightening. I knew nothing about the condition other than how horrible it looked when you saw someone having a seizure.”
Living with epilepsy has been challenging! We live in the countryside which is not a great plan for someone who perpetually loses their driving licence. The transportation links are very limited with an hourly bus to the local town. Why stay, you may ask? Well moving is difficult; the children go to the local school and our friends and support network are here.
After my diagnosis, I soon realised that I wanted to do something. I am very lucky that my seizures are controlled by medication but a third of people who live with epilepsy have no means of controlling their seizures, this severely impacts their lives. Research can help develop lifechanging innovations for people living with epilepsy, but sadly, such research has been hampered by chronic underfunding. The Epilepsy Research Institute is an amazing organisation, and I feel very privileged to be involved as a Founding Funder.

My seizures are linked to fluctuations in my hormone levels ¬ a condition called catamenial epilepsy. This effects one in every three women living with epilepsy and impacts on them throughout their life, from menstruation to post menopause. Little is known about the link between hormones and seizures and the effects of epilepsy mediation on your unborn child and the risk of seizures during pregnancy.
As well as the effect my hormones have had on my epilepsy, the condition has also impacted my reproductive health. I faced an awful dilemma during my three pregnancies; do I continue taking my epilepsy medication at the risk of my child being born with a birth defect or developmental problems or, do I stop taking my medication at the risk of having seizures and harming my unborn child.It was a dilemma that even medical practitioners could not help with.
“This is an awful predicament for any pregnant woman and is why I think research into reproduction & hormones is incredibly important.”
I hope research and clinical trials can find a cure for catamenial epilepsy. We know research into the causes of epilepsy, clinical trials, new and improved drugs, will transform the lives of people living with epilepsy. I hope with increased funding, the Epilepsy Research Institute’s aim will come true, and we will all live a life free from epilepsy.
The Enabling Technologies theme aims to leverage technologies and foster collaborations to enhance innovation and accelerate impact for patient benefit in ways that extend beyond the existing research and clinical landscape.
To ensure that every person with epilepsy can benefit from currently available research and clinical technologies.
To establish a world-leading environment for the rapid translation of promising technological advances towards direct applications in epilepsy.
To create a frictionless research landscape in the UK for developing novel technologies that address urgent priorities in epilepsy.
Clinical Co-Lead
Professor Mark Richardson
University College London

Data Co-Lead
Professor John Terry
University of Birmingham

Early Career Co-Lead
Dr Richard Rosch King’s College London
Following surgery to remove a brain tumour, Dominique’s life took an unexpected turn—she started having seizures, marking the beginning of her epilepsy journey. In this blog, Dominique opens up about her experiences and the role of the Vagus Nerve Stimulator (VNS) in managing her seizures.
Before epilepsy, I lived a full and active life. Shortly after my son was born, I began experiencing worsening headaches. My GP initially thought that it was due to stress, but the reality was far more serious — a large tumour the size of an orange had developed in my brain. I had to undergo surgery immediately, which took place in May 2015.
While the surgery was successful in removing the tumour, it resulted in me being in an induced coma for three days. It was also the beginning of my epilepsy journey.
Initially, I was prescribed an anti-seizure medication called Keppra. As well as experiencing side effects, finding the right dosage was challenging. Despite increasing the dose, I was still experiencing drop seizures, absence seizures and tonic-clonic seizures. Just when we thought we had found a medication and dosage that worked, the seizures would increase, and my dosage had to be adjusted again. The hardest part was never knowing when the seizures were coming, which made them very dangerous as I often injured myself. I broke my feet twice, had ligament damage, and sprained my wrist. I’ve had drop seizures more times than I can count.
It was in 2022 when my neurologist first told me about Vagus Nerve Stimulation (VNS) — a treatment where a small device, like a pacemaker, is implanted and connected to the left vagus nerve in the neck. This device sends mild pulses of electrical energy to the brain to help regulate abnormal activity that causes seizures. There’s also a magnet that can send an extra pulse when you feel a seizure coming on.
I’ve had my VNS for two years now. At first, it didn’t impact my daily life much — except for one unusual side effect. My voice began to change whenever the stimulator would

activate. It wasn’t painful, just an odd sensation. As the frequency increased, my voice changed even more. While it does sound different now, it’s something I’ve grown accustomed to and I don’t mind it anymore.
Before the VNS, my seizures were longer, and the aftereffects often left me feeling disoriented and exhausted. Since getting the implant, my seizures have become shorter, and I tend to recover more quickly—except for the tonic-clonic seizures, which I don’t have as often. My quality of life has improved, but it’s still early in my treatment. It’s only been two years, so I’m hopeful for even more progress. I’m also on new medication, as it’s a lot of trial and error to find the right balance. Everybody responds differently, so it takes time to see what works best for me.
This journey has shown me just how important epilepsy research is. With so many different types of epilepsy, finding the right treatment can often feel like a frustrating process of trial and error. Every individual’s needs are unique, and it’s crucial that we keep pushing for more targeted, effective therapies.
“The world of medicine is always evolving, and with that, our understanding of epilepsy and how to treat it should keep pace.”
I truly hope that in the future, it becomes easier to identify and treat epilepsy as early as possible. I also hope that more people become aware of life-changing treatment options like VNS. It has had a significant impact on my own life and could do the same for so many others. To everyone involved in epilepsy research—thank you for the incredible work you’re doing. Your efforts make a world of difference to people like me, and your support means everything!
The Capacity Building theme aims to transform the epilepsy research ecosystem in the UK and internationally through informed, strategic interventions to elevate and expand multidisciplinary networks, generate opportunities and foster a progressive and inclusive research culture.
To elevate and expand research into epilepsy to ensure a thriving, inclusive environment that attracts and retains the brightest minds.
To facilitate access to equipment and expertise to reduce barriers to epilepsy research.
To support students and early-career researchers working in epilepsy research with practical training/learning opportunities and mentorship.
To facilitate collaborative multidisciplinary research networks within the UK and worldwide, including with industry, funders, NHS, healthcare providers, policymakers and people living with/ affected by epilepsy.
To increase the visibility of epilepsy research – through campaigns, policy-facing work, patient and public engagement, and celebrating achievements.

Basic Science Co-Lead
Professor Torsten Baldeweg
UCL Great Ormond Street
Institute of Child Health

Clinical Co-Lead
Dr Sukhvir Wright
Aston University

Early Career Co-Lead
Dr James Mitchell
The Walton Centre
NHS Foundation Trust
Dr Abbie Fearon is an Epilepsy Research Institute trustee, Shape Network member and has worked in the field of cancer research for over 10 years. Abbie was diagnosed with epilepsy in 2020 so wanted to get involved in epilepsy research, given her background. Here, Abbie shares more on her journey, the importance of research and why we need to build capacity in epilepsy.
I was about thirteen when I started experiencing the symptoms that I now know to be associated with epilepsy, but I was only diagnosed recently. I would experience severe headaches alongside a strange smell. These episodes continued a few times a year, until I had my first convulsive seizure in 2020. It was then that I was first diagnosed with epilepsy.
Luckily, my epilepsy is now under control and I’m seizure free as I’ve been responsive to medication. But not everybody is as fortunate as I am.
“That’s why we urgently need more research into
epilepsy,
so that
we can understand the mechanisms behind the condition and find new treatments.”
I have an interest in epilepsy research because I live with the condition but also because I have a background in research. I completed a PhD in tumour biology, which was sponsored by Cancer Research UK, and I have worked in academia as a research scientist for many years, mainly in cancer research. More recently, when I left academia, I worked for the National Cancer Research Institute (NCRI) and now work for the National Institute for Health and Care Research (NIHR) as Cancer Portfolio Lead.
Through my own experiences of working in cancer research, I’ve seen how important patient and public involvement is for ensuring the right research is done and that the patient perspective is considered. Being an Epilepsy Research Institute Shape Network member has involved taking part in different funding panels, as well

as other exciting opportunities such as the priority setting partnership.
I’m also proud to be a trustee for the Epilepsy Research Institute. The formation of the Institute is significant for the epilepsy research space, as there’s so much to be uncovered about the condition and that can only happen through collaboration. Collaborations between scientists and clinicians and people affected by epilepsy, but also between funders. Everybody working together will enable us to find treatments more easily and faster.
An important part of collaborative working is capacity building, which I feel passionately about in research. It’s great to see that it is a focus of the Institute’s research programme and is one of their six research themes.
Capacity building means not only encouraging the next generation of researchers into the field but also retaining them, as this can often be difficult. The other element of capacity building is helping to build momentum by collaborating with researchers from different fields, whose expertise can be utilised in epilepsy research. For example, there may be techniques and knowledge in the cancer research field that could be applicable in epilepsy research.
“If
multiple disciplines work together, we can advance the field much more quickly.”
There are so many exciting possibilities in epilepsy research where we can really begin to understand the basic biology of epilepsy. I hope we can use this to find more treatment options so that we can help people live well with epilepsy.
We are extremely grateful to Christophe, Malcolm, the Westons, Anna, Dominique and Abbie for sharing their powerful stories which highlight the importance of research for them and the one in 100 people living with epilepsy.







Our roadmap is designed to unlock the transformative power of research and thereby enable us to make significant advances in our ability to diagnose, treat and prevent epilepsy.
We are seeking to radically change how we do research by bringing together world class research communities and unlocking the knowledge barriers that have historically slowed progress in the sector.
Building on our progress to date and the longer-term ambition in each of our six themes we are confident we will achieve a systemic shift in research outcomes. Accelerating research in this way will enable people living with epilepsy to maximise their independence and live more fulfilled lives, which is central to the Institute’s work.
We look forward to continuing to develop and strengthen our networks to maximise our impact. With us all working together in ever greater collaboration we will transform how society views epilepsy and energise the research efforts that will bring benefit to the one in 100 living with epilepsy and their families. We hope you will join us on our journey.
Following the nationwide engagement programme we funded and led, the UK Epilepsy Priority Setting Partnership (PSP) announced the Top Ten priorities for research into epilepsy in October 2022. These priorities were established by the UK epilepsy community including people living with and affected by epilepsy, healthcare professionals and patient groups.
The Top Ten include a broad range of topics, from epilepsy-related deaths, the underlying mechanisms of epilepsy, personalised medicine and brain health. These topics span fundamental neuroscience research, clinical research and novel methodologies, including big data and AI.

What are the causes and contributing factors of epilepsy-related deaths, including Sudden Unexpected Death in Epilepsy (SUDEP), and how can these deaths be prevented?
What underlying mechanisms cause epilepsy in children and in adults?
What impact do epilepsy, seizures and anti-seizure medication (ASMs) have on brain health – including cognition, memory, learning, behaviour and mental health?
How does epilepsy and epilepsy treatment impact neurodevelopment, and can this be managed or prevented?
How can targeted, personalised medicine, such as gene therapy, be used to treat and/or prevent epilepsy?
How can tools, devices and biological markers be used to accurately predict and prevent seizures and the onset of epilepsy?
How do hormonal changes in women throughout the lifespan (puberty, pregnancy, menopause) impact epilepsy, and how can this impact be addressed?
How can quality of life be improved for people with epilepsy, their families and carers, including those bereaved by epilepsy?
What causes drug-resistant (refractory) epilepsy, and how can it be best treated
How can big data analysis, through artificial intelligence (Al) and machine learning, aid the diagnosis and management of epilepsy?