
5 minute read
Postoperative complications
Cataract surgery in the younger population is not without risk. Soosan Jacob, MS, FRCS, DNB reports
Paediatric cataract surgery (PCS) is challenging and needs experience and team effort to manage postoperatively. To maximise results, one should be aware of complications, age-wise distribution, difference from adults and their management.
RISK FACTORS Complications of PCS depend on aetio-pathogenesis, age at surgery and type of surgery. Generally, dense unilateral cataract is operated on between six and eight weeks of corrected gestational age and dense bilateral cataract between six and 10 weeks. Performing surgery after eight weeks in these cases causes form vision deprivation amblyopia more resistant to treatment, resulting in poorer visual outcome. Noteworthily, early surgery increases life-long risk for secondary glaucoma. Non-visual axis opacities and eyes with irreversible retinal involvement do not need surgery.
A smaller sized eye; low ocular rigidity; increased inflammation; growth changes; difficulty in examination, estimating vision,
intraocular pressure (IOP), refraction, fundus evaluation and visual rehabilitation; difficulty in applying medications, maintaining hygiene and preventing unintentional trauma, all add up and increase challenges while decreasing potential for unqualified success.
Paediatric eyes also have more vascular irides, small pupils, immature trabecular meshwork, shallow anterior chamber and small palpebral aperture with poor ocular exposure
Systemic examination, metabolic and TORCHS screening, genetic analysis and next-generation sequencing are done when indicated.
COMPLICATIONS Postoperative inflammation is stronger in children and more so in infants and in uveitic cataracts. Pupillary membrane formation, iris bombe, posterior synechiae, peripheral anterior synechiae, glaucoma, IOL pigments, pupillary capture and decentration of IOL can all occur. Steroids used to control inflammatory response can increase IOP.
Cushing’s syndrome secondary to topical steroids has been reported and is avoided by punctal occlusion following topical medications.
Cycloplegics applied to prevent posterior synechiae and a constricted tied down pupil have sometimes been associated with an increased incidence of glaucoma.
Excessive prostaglandin release from inflammation can cause darker iris pigmentation and heterochromia.
GLAUCOMA AFTER PC Glaucoma is variably reported to have an incidence between 2 and 58%, with many studies reporting a 10-to-25% risk. Exact aetiology is unknown; however, IOL implantation does not give protection. Incidence increases with longer follow-up and younger age at surgery, with greatest risk in infants with bilateral cataracts who have undergone cataract surgery at less than 1 month of age. Regular follow-up for life is needed as it may present very late.
Incidence also increases with shorter axial length, use of trypan blue, complex pathology, persistent foetal vasculature, complex surgery, occurrence of intra- or postoperative complications, residual cortex, aphakia and reinterventions.
Glaucoma in children results in optic nerve cupping, visual field defects, enlargement of cornea and globe, Haab’s striae etc. Rebound tonometry may underestimate IOP. Glaucoma is managed medically and if not responsive, with surgery, often requiring a shunt.
Posterior Capsular Opacification (PCO) is common after IOL implantation under 2 years of age because of increased tendency to inflammation and scaffold effect of anterior vitreous face and IOL. Posterior capsulectomy with anterior vitrectomy should be done up to 5-to-7 years age and for older children with developmental delays and nystagmus.
Visual axis opacification (VAO) may occur even after posterior capsulectomy due to membrane formation from increased inflammation. VAO due to lens proliferation is especially common in the first year of life. Fibrin and pigment deposition on IOL secondary to iris inflammation, if confluent, may decrease vision.
PMMA IOLs are more at risk than hydrophobic acrylic IOLs. In-the-bag IOL implantation with optic capture through a posterior capsulorhexis has been proposed to decrease this.
Anterior vitrectomy may be done prior to placement of IOL or after, through a limbal ‘under-the-IOL’ or a pars plana route. Bag-inthe-lens technique may also confer protection from VAO.
Dense amblyopia may occur secondary to stimulus deprivation preoperatively and from VAO, refractive errors, loss of accommodation, strabismus or other ocular pathology, all of which should be attempted to be treated where possible. Anisometropic amblyopia can occur with ≥1.01.5D anisohyperopia, ≥2.0D anisoastigmatism and ≥3.0-4.0D anisomyopia. Isoametropic amblyopia can occur with ≥5.0-6.0D myopia, ≥4.0-5.0D hyperopia or ≥2.0-3.0D astigmatism.
Early visual rehabilitation is needed for high hyperopic errors, even after IOL implantation, because of residual hyperopia usually intentionally left in anticipation of the myopic shift with age.
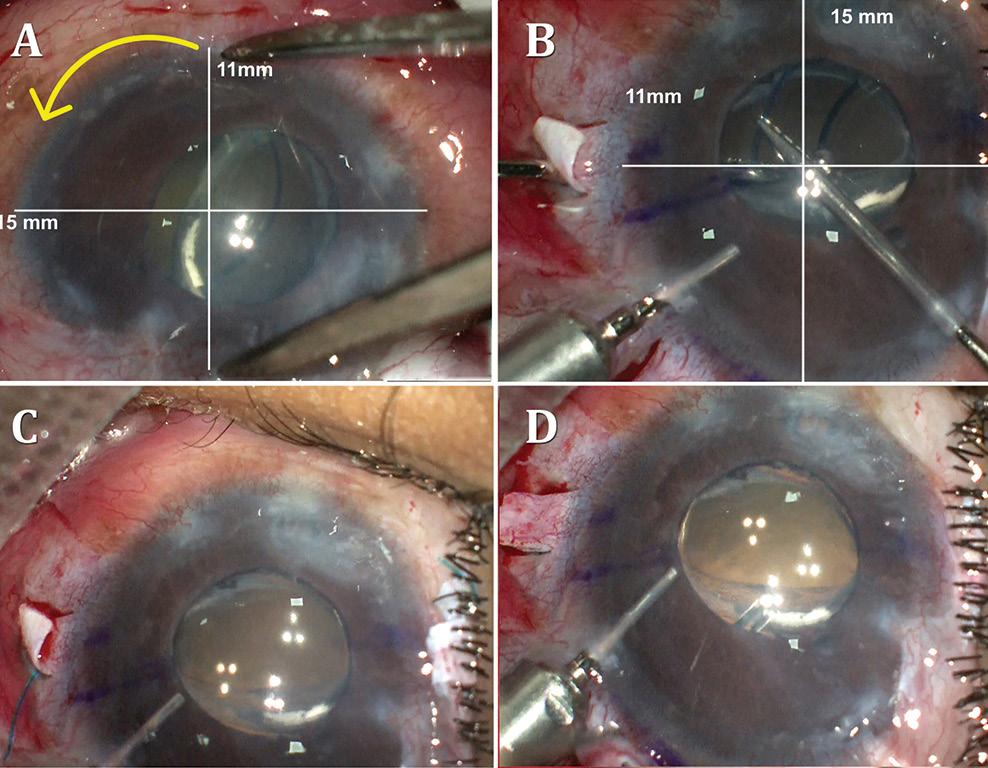
Post-paediatric cataract surgery Glaucoma: A: 3.5 years old child with cataract surgery done in infancy. Glaucoma with enlarged corneal diameter and a dislocated IOL are seen. One previous Ahmed glaucoma valve (AGV) in supero-temporal quadrant has failed to control IOP adequately; B: A second AGV plate is sutured in the infero-temporal quadrant. A closed chamber vertical translocation of haptics to glued IOL is then done sitting temporally, taking advantage of smaller vertical diameter of cornea; C: Adequate length of the externalised haptics of the IOL is seen; D: Haptics are tucked in. A well-centred IOL is seen. The AGV tube tip is positioned posterior to the iris in front of the IOL. Adequate vitrectomy is performed during IOL translocation as well as after inserting the tube tip
Suture-induced astigmatism can occur and suture management should be good.
Myopic shift with growth of eye should be treated with contact lenses, glasses, IOL exchange, piggyback IOLs or corneal refractive surgery.
Paediatric spectacles with small frames are available and preferred. Contact lenses have advantages of avoiding edge effects and loss of peripheral fields that occur with thick hyperopic spectacles as well as the aniseikonia occurring with spectacles after unilateral cataract surgery.
Occlusion therapy plays a major role in case of asymmetric visual acuity or fixation preference and is continued till around 7 years of age. Up to 6 months of age, one hour per month occlusion and till 5 years of age, six hours per day is advisable. Extensive occlusion in infancy disrupts binocularity. Prolonged occlusion resulting in reverse amblyopia in normal eye should be looked for and avoided. Strabismus and nystagmus may develop and should be treated.
RETINAL DETACHMENT Certain eyes, for example, with traumatic cataract, subluxated lens, Stickler syndrome, Marfan’s syndrome, homocystinuria, long axial length, persistent foetal vasculature, complicated or multiple surgeries etc. are at a higher risk of developing retinal detachment. As such, an overall 3% risk of retinal detachment in developmentally normal children with cataract and a 7% 20-year risk of retinal detachment has been reported. This risk increases further to 16% if associated with other ocular or systemic anomalies and even further to 23% in children with mental retardation.
ENDOPHTHALMITIS AND OTHERS Poor hygiene, posterior capsular rent, vitreous loss, unidentified vitreous wick, wound leak, poor wound closure, iris prolapse etc. are all risk factors for endophthalmitis. Other complications such as toxic anterior segment syndrome, corneal oedema, shallow AC, uveitis, hyphema, capsular block syndrome, corectopia, IOL decentration or dislocation, IOL opacification etc. can all occur in paediatric cataract surgery as well. Self-limited and self-resolving haemorrhagic retinopathy and vitreous haemorrhage has been reported in up to one-third of infants in one study. Chronic hypotony and phthisis may occur as late complications. Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com








