2 minute read
Femtosecond laser can
Promising technique
Femtosecond laser can aid with improving vision in keratoconus cases. Dermot McGrath reports
Stromal lenticule addition keratoplasty (SLAK) is a promising new technique that has shown good safety and efficacy in early trials in improving the corneal shape and vision in patients with keratoconus, according to Mario Nubile MD, PhD.
“It is a very promising era in keratoplasty with the introduction of lenticule implantation procedures such as SLAK. The concept is to provide a less invasive surgical technique as compared to standard keratoplasty, with novel approaches to treat keratoconus and corneal ectasia now possible,” he said at the 11th EuCornea Congress.
Explaining the concept in more detail, Dr Nubile, Excellence Eye Research Centre (Directed by Prof. L. Mastropasqua) at the University Gabriele d’ Annunzio of Chieti Pescara, Italy, said that the original idea was to try to make use of extracted stromal lenticules deriving from SMILE® refractive surgery. In theory, the lenticules could be used to insert tissue into a pathological cornea in order to obtain an effect and potentially treat conditions such as keratoconus, ectasia and certain corneal dystrophies. To date tissues from Eye Bank corneas suitable for transplantation, can be used in Europe.
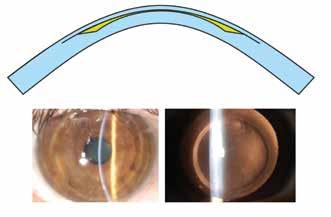
“The concept of SLAK is reliant on implanting a negative meniscus shaped lenticule that is thinner in the centre and thicker in the periphery with the aim to reshape and stabilise the cornea in eyes with progressive keratoconus (Figure). The basic idea is to implant lenticules intrastromally to improve the geometrical quality of pathological corneas affected by keratoconus and ectactic disorders,” he said.
After successful proof-of-concept studies, the technique was then successfully tested in 10 cases of advanced keratoconus. The lenticules were implanted in a pocket created by femtosecond laser at a depth of approximately 150 microns in the anterior stroma.
“The extended follow-up results up to 24 months showed very stable results in terms of keratometry, anterior corneal asphericity in the central 8.0mm zone, and corneal volume. The visual and refractive outcomes were also encouraging with improved uncorrected and best-corrected visual acuity and a reduction in mean spherical equivalent,” said Dr Nubile.
Vector analysis of the refractive astigmatism showed a mean reduction of 45%. More recent optical coherence tomography (OCT) studies have shown the extent of epithelial and stromal remodelling following SLAK, said Dr Nubile.
“We showed that intrastromal lenticules implanted in SLAK promotes corneal reshaping characterised by central flattening and both stromal thickening and epithelial thickness restoration. From a clinical point of view, this is important because the increase of the corneal stromal thickness allows us to perform cross-linking in progressive diseases when the cornea is very thin,” he said.
Likewise, SLAK may also benefit keratoconus patients who are contact lens intolerant and could potentially avoid the need for invasive graft surgery.
Another exciting possibility in the future is to use decellularised lenticules as a transplantable bio-scaffold with native-like stromal architecture and chemistry for specific ocular pathologies, concluded Dr Nubile. Mario Nubile: m.nubile@unich.it
Top: Schematic drawing of the negative meniscus lenticule implanted intrastromally. Bottom: Slit lamp and transillumination view of the cornea after SLAK Courtesy of Mario Nubile MD, PhD
ECCTR is a project funded by the ESCRS with initial support from the EU
European Union
Web-Based Registry
The aim of the project is to build a common assessment methodology and establish an EU web-based registry and network for academics, health professionals and authorities to assess and verify the safety quality and effi cacy of corneal transplantation.








