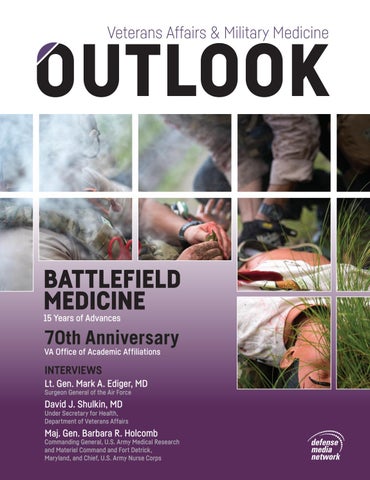
BATTLEFIELD MEDICINE 15 Years of Advances
70th Anniversary VA Office of Academic Affiliations
INTERVIEWS Lt. Gen. Mark A. Ediger, MD Surgeon General of the Air Force
David J. Shulkin, MD
Under Secretary for Health, Department of Veterans Affairs
Maj. Gen. Barbara R. Holcomb
Commanding General, U.S. Army Medical Research and Materiel Command and Fort Detrick, Maryland, and Chief, U.S. Army Nurse Corps
ENHANCED SAFETY DURING HAZARDOUS DRUG HANDLING Now Available through the Federal Supply Schedule
Equashield’s Closed System Transfer Device is designed to prevent exposure to hazardous drugs and reduce overall risk of exposure. Hazardous drugs have been clinically shown to contribute to a higher rate of both acute and serious health risks, including birth defects, spontaneous abortions, malformations of fetus, infertility, leukemia or other cancer1. However, protection is within reach as Equashield’s industry leading Closed System Drug Transfer Device (CSTD) is available for safe compounding and administration of hazardous chemotherapy drugs. Protect yourself and your staff by using a CSTD clinically shown to eliminate surface contamination and adhering to the upcoming USP 800 recommendations2,3. CSTDs should now be a part of your safe handling practice in addition to gloving, gowning and other PPE requirements for both Pharmacy and Nursing departments. Get compliant with Equashield. 1. NIOSH Alert 2004 – Published by the CDC 2. Clark, Bernadette A. and Sessink, Paul JM. “Use of a closed system drug-transfer device eliminates surface contamination with antineoplastic agents” -Cleveland Clinic Study. Journal of Oncology Pharmacy Practice. 2013Jun;19(2):99-104. 3. US Pharmacopeia General Chapter <800> Hazardous Drugs- Handling in Healthcare Settings
FSS contract number: V797D-50561
WWW.EQUASHIELD.COM
Safe. Simple. Closed.
855-378-2744
Upgrade to the
The TRUE METRIX® portfolio* achieves a level of performance driven by science, research and technological advancements.
High-quality protective screen Alternating time and date
Featuring
Event tagging
The system automatically detects, analyzes and corrects variables in each blood sample to ensure proven accuracy and confidence in results.
Elegant, black, soft-touch
Proven Accuracy
Large display and digits for easy reading
The TRUE METRIX® System exceeds the more stringent minimum ISO 15197:2013 performance requirements.1
Test strip release button
With TRUE METRIX – ®
Accuracy is Confidence
Easy-to-use test strip port
Features: • No coding • Tiny 0.5 microliter sample size • As fast as 4 seconds • Stores 500 results • Data management • Download capabilities
* TRUE METRIX® is intended for selfmonitoring blood glucose only and not for multiple patient use. Only TRUE METRIX® PRO is intended for multiple patient use.
BEFORE MEAL AFTER MEAL EXERCISE
EVENT TAGGING
Easy-to-use TRUE METRIX® with advanced event tags empowers users to make the connection between personal lifestyle and results. Providing this information helps users make informed choices to actively manage diabetes.
SICK MEDICATION
OTHER
For product information go to: www.trividiahealth.com For product orders call: (800) 342-7226 ext. 4129 NICO-3821 © 09/16 Trividia Health, Inc. TRUE METRIX, TRIPLE SENSE TECHNOLOGY and the Trividia Health logo are trademarks of Trividia Health, Inc. 1. Data on file.
Full Spectrum Infection Control Solutions The world’s fastest autoclave from Start to Sterile. ■
STATIM 2000 G4 cycles times: 6 min. unwrapped – 14 min. wrapped
■
STATIM 5000 G4 cycle times: 9 min. unwrapped – 17.5 min. wrapped
■
A large 3.5” high-resolution touchscreen offers a vivid display of messages and current cycle information all with extraordinary clarity.
■
Uses fresh steam distilled water with every cycle.
■
Dri-Tec drying system for fast dry loads.
BRAVO™ The BRAVO is a fractionated vacuum sterilizer that incorporates both pre-vac (to remove air) and post-vac (to ensure a dry load every time) cycles to ensure the perfect steam penetration for any load. ■
The BRAVO 17V, with a 17 liter chamber, has a large vacuum pump and employs total cycle times, including drying, starting at just 19 minutes.
■
The BRAVO 17V is one of the fastest chamber autoclaves on the market.
■
The BRAVO 17V comes standard with 5 sterilization trays, increasing load capacity and office efficiency.
■
The BRAVO 21V, with a 21 liter chamber, is a larger chamber autoclave allowing the sterilization of a 14” cassette. The BRAVO 21V has a top filling port as well as a front mounted master drain port, and an integrated USB port for data logging. The BRAVO 21V continues to employ total cycle times, including drying, starting at just 23 minutes.
SANAO™ Easy on the hand, SciCan’s SANAO handpieces are ergonomic wonders. ■
■
■
HPS (Hygiene Protection System) - SciCan is known as “your infection control specialist” in the dental industry, and the SANAO line incorporates its Hygiene Protection System, an internal resin to help prevent material and debris from collecting inside the handpiece. Ergonomic - The SANAO line of handpieces has been engineered ergonomically, to reduce hand stress, offer optimal comfort in the hand, and provide maximum control in the oral cavity.
HYDRIM® G4 Instrument cleaning has never been faster or smarter. ■
The HYDRIM C61w G4 has a 6 full size cassette capacity, the largest of its kind, allowing offices to turnover 120 instruments in 35 minutes. Start to dry.
■
The HYDRIM L110w G4 has a 10 full size cassette capacity, the largest of its kind, allowing offices to turnover 2500 instruments in a 10 hour day.
■
The time saved by automated washing compared to ultrasonic cleaning is approximately 1 hour of labor for every nine procedural set-ups.
Power - With a motor that produces up to 3.5 Ncm of torque, procedures will take less time, the preparations will be more precise, making the dentist more efficient overall.
OPTIM ® 33TB ONE-STEP Disinfectant cleaner: A revolutionary disinfectant with all the upsides and none of the downsides. ■
Fast contact time
■
1 minute bactericidal and virucidal claim
Federal Supply Schedules
■
30 second sanitizer
Dental Equipment & Supplies
V797D-30276
Medical Equipment & Supplies
V797D-40024
SciCan, Inc. Corporate Office
800-572-1211
HYDRIM, OPTIM and STATIM are registered trademarks and BRAVO, SANAO and Your Infection Control Specialist are trademarks of SciCan Ltd.
STATIM® G4
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ U.S. Marines with Task Force Koa Moana
16.2 undergo the practical application portion of the Combat Lifesaver course on USNS Sacagawea (T-AKE 2), May 24, 2016.
TABLE OF CONTENTS INTERVIEWS
10 David J. Shulkin, MD 30 Lt. Gen. Mark A. Ediger, MD 53 Maj. Gen. Barbara R. Holcomb
Under Secretary for Health, Department of Veterans Affairs
Surgeon General of the Air Force
U.S. MARINE CORPS IMAGERY BY MCIPAC COMBAT CAMERA LANCE CPL. JESUS MCCLOUD
Commanding General, U.S. Army Medical Research and Materiel Command and Fort Detrick, Maryland, and Chief, U.S. Army Nurse Corps
FEATURES
22 Battlefield Medicine: 15 Years of Advances 40 Disaster Response and Emergency Preparedness 62 Developments in Army Medical Imaging 68 AMSUS: Tying Together the Military Health System and Others By J.R. Wilson
By J.R. Wilson
By Scott R. Gourley
By J.R. Wilson
www.defensemedianetwork.com
5
© 2016 Optum, Inc.
HEALTHIER IS HERE At Optum, we believe that veterans, members of the military and their families have earned the best service in health care. As a health services and innovation company, we power modern health care by combining data and analytics with technology and expertise across the entire health spectrum. It’s the transformative power of this data science that can make both mental and physical health care more timely, streamlined and effective — unlocking new opportunities to improve access and outcomes for those who give their all. optum.com/government
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA PHOTO BY ROBERT TURTIL
â&#x2013; â&#x2013; Overnight Jan. 25-26, 2015, the annual Point-in-Time (PIT) Homeless Count was held in Baltimore. During the last week of January, the Department of Veterans Affairs, Housing and Urban Development, and local agencies across the country conduct PIT Counts to get a statistically reliable, unduplicated count of sheltered and unsheltered homeless veterans, individuals, and families in the United States.
83 The Path to Excellence 92
VA Office of Academic Affiliations Celebrates Its 70th Anniversary By Chuck Oldham
By Carolyn M. Clancy, MD Deputy Under Secretary for Health for Organizational Excellence, Veterans Health Administration
96 VA Research: Genomic Medicine 102 VA Research: Auditory Vestibular Research 113 VA Research: Homelessness Research: Improving Equity and Reducing in Health Care 122 VADisparities Opioid Use Disorder and Transforming Pain Management in the VA 128 Addressing By Craig Collins
By Craig Collins
By Craig Collins
By Craig Collins
By Gail Gourley
138 Pharmacy Automation in the VA By Gail Gourley
www.defensemedianetwork.com
7
Proud to serve those who serve US FoodsŽ has played a supporting role in delivering foodservice products and value-added services to the U.S. Department of Veterans Affairs and military medical facilities across the nation since 1996. We understand the challenges that foodservice operators face and are able to offer foodservice expertise, customized solutions and a full array of products for every operational budget. We have the dedicated people and resources to help foodservice directors achieve the highest levels of quality, efficiency and satisfaction in their operations. We share your commitment. We share your passion. We share your calling. Questions, comments or setting up a new account, please contact: Fabian Sriwardene, Director Veterans Affairs and Government | Email: Fabian.Sriwardene@usfoods.com | Office: 703-387-3209 Š2016 US Foods, Inc. 06-2016 NAT-2016062408
Published by Faircount Media Group 701 North West Shore Blvd. Tampa, FL 33609 Tel: 813.639.1900 www.defensemedianetwork.com www.faircount.com EDITORIAL Editor in Chief: Chuck Oldham Managing Editor: Ana E. Lopez Editor: Rhonda Carpenter Contributing Writers: Carolyn M. Clancy, MD, Craig Collins Gail Gourley, Scott R. Gourley, J.R. Wilson DESIGN AND PRODUCTION Art Director: Robin K. McDowall Designer: Daniel Mrgan Ad Traffic Manager: Rebecca Laborde ADVERTISING Ad Sales Manager: Ken Meyer Account Executives: Lorri Brown Bonnie Schneider, Geoffrey Weiss
Proudly Supporting Our Veterans and The Red, White and Blue Inspired by Veterans and aging/disabled Americans, Harmar’s driving purpose is to make lives easier. Harmar creates Lifts for Life - Made in the USA. Harmar proudly supports Veterans and the VA through our FSS contract and has provided vehicle lifts, stair lifts and porch lifts for more than 50,000 Veterans over the past 7 years.
OPERATIONS AND ADMINISTRATION Chief Operating Officer: Lawrence Roberts VP, Business Development: Robin Jobson Business Development: Damion Harte Financial Controller: Robert John Thorne Chief Information Officer: John Madden Business Analytics Manager: Colin Davidson FAIRCOUNT MEDIA GROUP Publisher: Ross Jobson
©Copyright Faircount LLC. All rights reserved. Reproduction of editorial content in whole or in part without written permission is prohibited. Faircount LLC does not assume responsibility for the advertisements, nor any representation made therein, nor the quality or deliverability of the products themselves. Reproduction of articles and photographs, in whole or in part, contained herein is prohibited without expressed written consent of the publisher, with the exception of reprinting for news media use. Printed in the United States of America.
Learn about Harmar’s new Stars -N- Stripes Platform Lift at
www.harmar.com/heroes
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
DAVID J. SHULKIN, MD Under Secretary for Health, Department of Veterans Affairs By Chuck Oldham
n THE HONORABLE DAVID J. SHULKIN, MD, is under secretary for health for the United States Department of Veterans Affairs. As the chief executive of the Veterans Health Administration (VHA), Shulkin leads the nation’s largest integrated health care system, with more than 1,700 sites of care serving 8.76 million veterans each year. The VHA is also the nation’s largest provider of graduate medical education and major contributor of medical research. Shulkin oversees the system that employs more than 300,000 people. Prior to being nominated by President Barack Obama and being confirmed by the United States Senate as under secretary for health, Shulkin served in numerous chief executive roles, including serving as president at Morristown Medical Center, Goryeb Children’s Hospital, and Atlantic Rehabilitation Institute, and the Atlantic Health System Accountable Care Organization. Shulkin also previously served as president and CEO of Beth Israel Medical Center in New York City. He has held numerous physician leadership roles including the chief medical officer of the University of Pennsylvania Health System, the Hospital of the University of Pennsylvania, Temple University Hospital, and the Medical College of Pennsylvania Hospital. Shulkin has also held academic positions including the chairman of medicine and vice dean at Drexel University School of Medicine. As an entrepreneur, Shulkin founded and served as the chairman and CEO of DoctorQuality, one of the first consumer-oriented sources of information for quality and safety in health care. Shulkin is a board-certified internist, a fellow of the American College of Physicians. He received his medical degree from the Medical College of Pennsylvania, his internship at Yale University School of Medicine, and a residency and fellowship in general medicine at the University of Pittsburgh Presbyterian Medical Center. He received advanced training in outcomes research and economics as a Robert Wood Johnson Foundation Clinical Scholar at the University of Pennsylvania. 10
Over the course of his career, Shulkin has been named as one of the “Top 100 Physician Leaders of Hospitals and Health Systems” by Becker’s Hospital Review and one of the “50 Most Inf luential Physician Executives and Leaders” by Modern Healthcare and Modern Physician. He has also previously been named one of the “One Hundred Most Inf luential People in American Healthcare” by Modern Healthcare. Veterans Affairs & Military Medicine Outlook: Coming into the Department of Veterans Affairs (VA) from the private sector, have you seen opportunities to implement some private-sector health care best practices? If that is the case, are there also areas where those private-sector models just don’t seem to apply? David J. Shulkin, MD: Yeah, I certainly have. I’ve spent my career really running private-sector organizations. So I couldn’t help but come in with a private-sector perspective on health care. While there are many unique things about the VA, so much of what we do we share similarities with what’s going on in the private sector. And as you know, what is happening in the private sector is all of the old assumptions about how health care is delivered and ways of doing things are being challenged. And we’ve never seen, never been in a time where there has been so much change happening in health care, both in the way that we pay for health care [and] the expectations of consumers, and how we’re using new technologies. So my message coming into VA has been that we have to be looking at the changes that are happening in the private sector because we have to be changing just like they’re changing. So we’ve taken many of the challenges that we’re having in the VA and looked at how the private sector is looking at it. Some of them are very applicable and others don’t fit quite as well, but I think there’s never been a time where we’ve been more open to sharing what we’re doing with the private sector and learning from what the private sector does well. www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
good type of care that’s being delivered on a daily basis hundreds of thousands of times a day across the country. People aren’t open to hearing from you when they think that you’re not addressing the crisis. They’re not open to hearing the full picture of all the amazing things that are happening in VA. So it’s been a challenge to adequately and accurately represent the scope of activities, and really what we do on a daily basis, because so much attention’s been focused on the negative or on the crisis aspects. One of the challenges that has resulted from that has been the morale of our workforce, who is demoralized by seeing how much negative attention has been put on the VA over the past couple of years. And that’s resulted in us seeing a decrease in applications for people wanting to come to work for the VA. So at the very time that we need to be attracting the best and the brightest and filling all of our spots, we’re actually seeing a decrease in applications related to this morale issue.
VA PHOTO
■■ VA Under Secretary for Health David J. Shulkin, MD.
What do you consider the biggest challenges at the moment that you’ve had to face? Well, I think there are really a couple. The first is that our biggest challenge is to regain the trust and confidence of veterans and the American public in what VA is doing. And having gone through this crisis, which began in VA in April 2014, we clearly lost a lot of that trust and confidence. And if you’re going to be a health care organization, one of the key ingredients, in fact what I call our currency since we don’t operate in a financial forprofit sense, our currency is really the trust and confidence of those we serve. So that’s really been our biggest challenge: to show people that we are being responsive and doing everything that we can to address the health care needs of veterans. And that’s how we’re going to regain trust. One of the challenges is that when you’re going through a crisis like VA has gone through, it’s been very hard to get the word out about the unbelievably
www.defensemedianetwork.com
We certainly have written stories about the quality of the health care in the VA. Whatever the issues may be with keeping up with appointments and wait times or what have you, once the person is being taken care of, it’s the best care anywhere, practically. You can’t do better, really. Well, I think that every health care organization should strive to do better, and we’re no different. We have many, many areas where we are seeking to improve our performance. Even in areas where it is good, we’re looking to make it even better. So it’s not that we’re a system that is perfect. We’re far from that. But we are doing and should be proud of many, many parts of our health care system that are doing extraordinary things. Even in the area of access and wait times, I will put our wait times up against the leading health care centers anywhere in the country, and I think that we perform as well or better in terms of access. What I think is challenging is that there are parts of the country where it just is very, very hard to hire health care professionals – parts of the country that are very rural where we don’t train medical students and where we don’t have medical schools. And getting people to move to those parts of the country and to come to work for us is very, very challenging. No other health care system has the scope of responsibilities that the VA does, which is to deliver care to every part of this country where veterans live. And therefore, the standard that we’re being held to is really one that doesn’t compare well with any other private-sector organization. That’s a good point. More than a year ago when you were sworn in, you had some priorities you put forward that you wanted to address. Where have you found success in advancing those priorities? 11
Did you know the Department of Veterans Affairs has issued a national policy to provide any veteran with spinal cord injury (SCI) who meets the physical qualifications access to ReWalk exoskeleton technology?
What is ReWalk? ReWalk is a robotic exoskeleton medical device that enables individuals with spinal cord injury (SCI) to stand and walk. The ReWalk system is cleared by the FDA for home and community use. For a free screening and information on evaluation and training with ReWalk, please contact your local VA Hospital or VA Rehabilitation Center. You may also contact ReWalk directly at: www.rewalk.com/contact or by phone at 508-251-1154 Ext. 741 At ReWalk, our mission is to fundamentally change the Quality of Life for individuals with lower limb disability through the creation and development of market leading robotic technologies.
www.rewalk.com â&#x20AC;&#x153;With ReWalk, I leave my disability behind in the chair.â&#x20AC;?
Rtd. Army Specialist Gene L. - Spinal Cord Injury in 2001 - ReWalker since 2013
Facebook.com/Rewalk @ReWalk_Robotics
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA PHOTO BY EUGENE RUSSELL
■■ Shulkin uses telehealth technology from his office in Washington, D.C., to see patient Larry Bayless at the West Palm Beach VA Medical Center.
Well you’re right. Before I came in – because I wanted to come in and have a clear sense of direction from the first day I started – I had established five priorities for VA. And I had done that really as a private citizen looking at as much information as I could gather from reading about VA and talking to people. But I thought once I got in and I learned more, I’d probably change some of those priorities and give myself that flexibility. But as it turned out, I didn’t change a word of them. The five priorities that I set out with, really, I believe, just as much today, 15 months into the job – they are the right five priorities for VA to
www.defensemedianetwork.com
be focused on. So we’re working all of them. They are: improving access and wait times; improving the engagement of our employees; implementing best practices so that we act in a consistent way across the country as a national health system; and developing a high-performance network to work with our community partners as well as internal VA operations. And the fifth is to regain the trust and confidence of veterans and the American public. So in each of those areas, I believe that we’re making significant progress, some faster than others. But in each of them, I think that they are beginning to transform the way 13
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
that VA is viewed both internally and externally as we are making progress in each of these areas. And I think that they’re all interlinked and critically vital to becoming the type of health care organization that people expect from us and that we want for ourselves. You mentioned that you had put together these priorities before you actually were sworn in. Were there any surprises for you when you were on the inside versus when you were looking from the outside in? I think the biggest surprise was the type of care that VA delivers and how different it is than what you see in the private sector. And the way I would explain that is, and I really hadn’t understood this until I got on the inside … the comprehensiveness of the care given in the VA system so that it’s not just focusing on the physical health needs of its patients. But it actually is a model that is much more holistic, that looks at not only the physical but the psychological and the social and the economic aspects of being human that allows you to create well-being for veterans. So it includes things like support for caregivers and transportation support. It includes things like if you don’t have a home, providing a home – you know, addressing the issue of homelessness. It provides things like clothing, and
recommendation when they issued their final report. But it certainly was considered. And we had a chance to talk to them and address that issue. I think that what I clearly said is that that would be the worst decision for veterans. And I think that the commission members ultimately agreed with that. The reason why I said that this would be a horrible outcome for veterans was precisely because the more that I understood and got a chance to experience it myself, the VA health care system is doing things that frankly don’t exist in the private sector. So if you were to take away that type of health care system for veterans, you frankly can’t replace all those services in the private sector. So therefore you’re just going to stop doing important things that matter to the health and well-being of veterans. And we made a commitment to those who stepped up to serve for this country that we were going to take care of them and provide them with what they needed for the rest of their lives. And that’s the commitment that we take seriously. In fact, it’s our only mission in the Veterans Health Administration. And if you don’t have an organization [that] has that mission, veterans are clearly not going to get what they deserve. So yes, I feel very strongly about that. Now, at the same time, what I said to the commission is VA doesn’t need to be doing all the things that the private
■■ We made a commitment to those who stepped up to serve for this country that we were going to take care of them and provide them with what they needed for the rest of their lives. And that’s the commitment that we take seriously. our adaptive sports programs, so that if you have a spinal cord injury or an amputation, it’s not just addressing those physical needs but it’s actually giving you joy back in your life and creating a purpose. So that definition of health is very different than the definition that most private-sector health care organizations use. And that model of care and supporting that model of care really was the biggest surprise for me. That plays into another question I wanted to ask. I know some of the people serving on the Commission on Care had recommended shutting down VA medical centers and outpatient services and moving veterans to get their medical care in the private sector. And you said this wouldn’t be a good idea. You touched on that a little bit already in your answer, but I wondered if you could expand on that. … What the Commission on Care did was they had a healthy debate, as the commission was charged to do. And that probably included all ends of the spectrum of what are the choices that could be taken. One choice clearly would be to shut down the VA and privatize health care. I think that the commission did not come up with that 14
sector is doing well or in some cases even doing better. So what we’ve come up with in my high-performance network plan is to come up with what is the best thing for veterans. And that is to support – have full support for – those services that are unique in the VA health care system that the VA does better for veterans, and utilize and work closely in a seamless way with community health care providers that are doing things that they do better for veterans. So when you put the veteran in the center and you really just answer one question – “What’s the best thing for the veteran?” – then you come up with the right answer, I believe: the idealized system that works seamlessly between the community and the VA. I think in the end, now that you look back and now you see how the whole thing played out, that group who surfaced their ideas did everybody a service because I always think you’re better when you get all the candor and the ideas out on the table and you have a chance to have a healthy debate and look at data and support whether the solution fits with what the data says. And in this case, that’s what happened – that generated a very healthy debate about whether privatization of the VA was a good thing or a bad thing. And ultimately, the commission members did reach consensus on recommendations. I think there were three
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Shulkin speaks at the Diffusion of Excellence Planning Summit in March 2016. VA employees and leaders participated in the summit to co-
create plans to adapt innovations and practices with demonstrated results in specific VA facilities so that they can be diffused throughout the system to more rapidly serve veterans and their families.
VA PHOTO BY KATE VIGGIANO
of the commissioners that withheld their final vote on this. But they still had 12 that did support it. And I think that those recommendations, which now have been sent to the president, and the president will be issuing a statement on Sept. 6 [President Barack Obama issued his statement on the findings of the Commission on Care on Sept. 1, 2016], were important in being able to provide recommendations that ultimately can have benefit to veterans and, frankly, to the Veterans Health Administration as well. How is the Veterans Choice Program progressing? Do you think you can resolve the issues with it in a timely manner in working with Congress? What are the difficulties in implementing it quickly? Well, the Veterans Choice Program was introduced with the idea that it wanted to be part of helping improve access to health care for veterans. And I think that it has been successful in doing that. I think that one of the unintended results of it was that it turned out to be a very complex program to implement. So as we’ve learned about the program, we’ve identified ways to be able to make the program simpler and work better for veterans. And we actually submitted a proposal on how to make revisions to the Veterans Choice plan that would make it work better. We submitted it to Congress at the end of October of 2015. And we’ve been waiting for Congress to provide legislative changes that would allow us to implement that plan. Many of those recommendations are incorporated in what’s called the Veterans First legislation, which right now has a version before the Senate and a version before the House. And we are waiting to see whether Congress will be able to act and support legislative changes that would make this program work better for us. In the meantime, we had done a number of revisions to the contract, I believe 42 in total, in order to make incremental improvements to the way that the Choice Program works so that it begins to be more
www.defensemedianetwork.com
responsive to veterans’ needs. And we are seeing some positive movement in the number of appointments that we’re able to schedule for veterans through the Veterans Choice Program. So I think we’re moving in the right direction. But ultimately, we think that in order to make the program truly work better that we are going to have to have legislative action from Congress. On a more personal level, I understand you take time out once a month to simply work as a physician in the system. Could you tell me a little bit about that – how you came to want to do that and where and when it happens? Well I, No. 1, view myself as a physician, and secondly as an administrator. The reason why I do what I do every day is to be able to help people. And if I lose connection with my primary motivation about why I go to work every day, which is to help people, I would lose something personally, and I think I would be less effective at what I do. I have always, as a chief executive, always seen patients in any of the settings that I’ve worked in or had the privilege to lead. And I do that for a number of reasons, but primarily so that I can feel connected to the primary mission and I can understand what similar people who work in the health system are experiencing – whether the administrative systems that we put in place and the clinical systems that we put in place are actually working or not. And it grounds me with our customer. It allows me to interact with veterans and to hear how they’re doing and hear how we’re doing for them. So I actually do this in two ways. I see patients as an internist in the Manhattan VA in New York City. And there I primarily serve in our walk-in clinic so that anybody … who needs to see a doctor, I will see that day when I am there. And it gives me a broad overview of the types of services that we provide in the Manhattan VA Medical Center. And more recently, I’ve started to practice internal medicine in Grants Pass, Oregon. Now I don’t even know where that is. But I see patients in Oregon 15
You’ve Served Us. Now Let Us Serve You. UHS developed the Patriot Support Program network of treatment centers, support staff and medical professionals to meet the needs of active duty members of the military, veterans and their families. Patriot Support Centers of Excellence help individuals cope with the emotional and psychological effects of military service, deployment and combat. Specialty inpatient, partial hospitalization, outpatient and residential treatment services include: H Chemical dependency H Post-traumatic stress H Eating disorders H Military sexual trauma
H Complex trauma H Behavioral pain management H Specialized women’s services
Want to learn more? Visit www.patriotsupportprogram.com 1-888-505-1475
As a leading provider of behavioral health services through TRICARE®, we continually enhance programs to ensure military personnel and their families receive exceptional support and care. Our Centers of Excellence include: Brynn Marr Hospital - Jacksonville, NC Cedar Hills Hospital - Portland, OR Cedar Springs Hospital - Colorado Springs, CO Chris Kyle Patriots Hospital - Anchorage, AK Cumberland Hall Hospital - Hopkinsville, KY El Paso Behavioral Health System - El Paso, TX Emerald Coast Behavioral Hospital - Panama City, FL Laurel Ridge Treatment Center - San Antonio, TX Lincoln Trail Behavioral Health System - Radcliff, KY Poplar Springs Hospital - Petersburg, VA Salt Lake Behavioral Health - Salt Lake City, UT Stonington Institute - North Stonington, CT UBH Denton - Denton, TX Valley Hospital - Phoenix, AZ
Our focus is providing services and support to help you achieve your personal success.
TRICARE® is a registered trademark of the Department of Defense, Defense Health Agency. All rights reserved. The Department of Defense, Defense Health Agency did not select or approve this advertiser and does not endorse and is not responsible for the views or statements contained in this advertisement. 160731
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ The reason why I do what I do every day is to be able to help people. And if I lose connection with my primary motivation about why I go to work every day, which is to help people, I would lose something personally, and I think I would be less effective at what I do.
from my office here in Washington, D.C., using tele primary care, where the staff in Oregon support me, and I actually see the patients right here overlooking the White House. And I can listen to their hearts and lungs, I can look in their eyes and ears and in their throat, I can have my staff in Oregon do parts of the physical examination that I’m not physically able to. And it’s been a terrific experience for me to work with a rural clinic that doesn’t usually have access to physicians all the time and for me to get to talk to and take care of veterans who are out in that part of the country. So it’s expanded my view of how to use technology. And both having time to see patients in person and do this via telehealth has really given me a much better perspective on the types of things that we’re trying to do across the VA health care system. It sounds like in addition to informing your role it’s personally rewarding to you as well. Oh, absolutely, it is. It is. But I think beyond that, it makes me better and more effective as a leader. It allows me, I think, to also understand what it means to be practicing in the VA system, because I’m one of the thousands of clinicians that are doing that every day. Yearly, we usually do something with VA research. And this year one of the stories we’re covering is genomics. Could you update us on how the Million Veteran Program is coming along and explain why it is such an important initiative? So the Million Veteran Program was actually started years ago. I think that’s the thing that I’m most proud of, that people in the VA had the foresight to start a program like this, because today it is now the largest database of genomic materials in the country. And that puts VA in a tremendous leadership position to be able to do research and discovery in ways that, frankly, no other organization in the country can do. So the concept was to collect the blood samples and then do genomic sequencing on a million veterans and be able to tie that to the VA’s long-standing electronic medical record of over 25 years. And now you have a very unique source of information
www.defensemedianetwork.com
in which to tie genomics to very detailed clinical data and do research that will benefit other veterans. And currently right now we have nine major research projects underway. I think the big landmark for us was actually last month, where, in Atlanta, the president announced that we just had gone over the 500,000th veteran enrollee in the program. I actually had a chance to meet No. 500,000 in person in Atlanta. And this is really the halfway point of us reaching that million figure. But already we’re able … to utilize this database in incredible ways. We tied this very much to a couple of other important initiatives. One is the vice president’s Moonshot initiative to be able to find new ways and discoveries to treat cancer. And in doing that we’re able to leverage the Million Veteran Program not only to help other veterans but really to help all Americans and to accelerate our work and understanding of how to treat cancer in a better way. But we’re also now working much more with other federal organizations. So the Department of Defense has just signed on as a partner in the Million Veteran Program. So now we can not only enroll veterans, but we can enroll active military service members. The NIH [National Institutes of Health] and VA are working together on the NIH’s Precision Medicine Initiative so they can learn from what we’ve done in the Million Veteran Program. And we’re also working now with the National Cancer Institute, FDA [the Food and Drug Administration], the Department of Energy, and other federal agencies all to work together to advance our knowledge in how to care for both cancer as well as other genomic-related research programs. So I think that this program has really allowed VA to be central to helping the federal government in general and other programs around the country to know how to direct a program in genomics. And it’s going to be very important for the way that we deliver health care in the future, because this is clearly where health care is going. Just one final thing on this: VA has really worked hard in the last couple of years to open itself up to doing strategic partnerships with outside organizations, whether they are federal programs or even companies around the country or organizations around the country. Whoever is able to provide help to make us take better care of veterans, we want to be partnering with. So out of the Million Veteran Program, we partnered with IBM Watson, which is providing 10,000 analyses of these gene sequences so that we can help patients who have cancer to be able to get the individualized care – the personalized treatment – quicker and better than if we were doing this alone. And so it’s these types of strategic partnerships and advances in technology that allow us to assure ourselves that we’re providing veterans with the very best health care that you can in this country. 17
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Battlefield Medicine: 15 Years of Advances n BATTLEFIELD MEDICINE MADE UNPRECEDENTED strides during Operation Iraqi Freedom and Operation Enduring Freedom-Afghanistan, resulting in the lowest killed-inaction statistics in the history of warfare. But the wars in Southwest Asia also marked the spread of a different type of warfare – insurgencies and terrorism perpetrated by nonnation states – and expanded the definition of “battlefield” far beyond what it had been for thousands of years. Today’s battlefield may be a traditional one of clashing national armies or a combination of non-uniformed armies, insurgents, and terrorists (as with the ongoing fight against the Islamic State of Iraq and the Levant), or a nightclub, train station, or other non-military facility – situations and settings in which thousands of civilians 22
have been killed or injured since the turn of the century. It also extends to the U.S. Coast Guard’s law enforcement mission at sea against smugglers, pirates, and terrorists. Since 9/11, “battlefield medicine” has grown beyond the Army medic or Navy corpsman treating wounded warfighters in a foreign conflict. It now includes treating the sick or wounded aboard a smuggler’s boat seized at sea by the Coast Guard, National Guard medics treating the survivors of a natural or man-made domestic disaster, or Marines helping in the fight to contain Ebola or Zika. Those various contingencies have incorporated many of the advances made in on-site, first responder medical care in whatever battlespace or environment may be involved. Those include the latest developments related to traumatic brain
www.defensemedianetwork.com
U.S. AIR FORCE PHOTO BY STAFF SGT. RYAN CALLAGHAN
By J.R. Wilson
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ OPPOSITE: U.S. Air Force Senior Airman
U.S. ARMY PHOTO BY SGT. DALLAS WALKER
Michael Triana, left, 347th Operations Support Squadron independent duty medical technician-paramedic, addresses injuries on a simulated patient during a Tactical Combat Casualty Care (TCCC) course on Sept. 22, 2016, in Okeechobee, Florida. TCCC is the standard for combat medical procedures for all U.S. armed services, and courses such as this test and reinforce participants’ lifesaving medical skills while they are in high-stress combat scenarios. RIGHT: U.S. Army and Air Force medics rush a casualty into the emergency room of the theater hospital at Balad Air Base during military operations in Iraq in 2005. The positioning of emergency and traumatic care doctors and surgeons far forward in combat theater hospitals has increased the survivability of warfighters.
injury (TBI), eye injuries, bleeding wounds, loss of limbs, facial injuries, spinal cord injuries, etc. In 2011, Tactical Combat Casualty Care (TCCC) – a set of doctrines and procedures that had been under development and limited implementation for nearly two decades – was made the standard for combat medical procedures for all U.S. armed services. TCCC procedures and subsequent changes ordered by the Department of Defense’s (DOD) top medical authorities include: • Before any aid is rendered, both medics and, if possible, the wounded return enemy fire in an effort to prevent additional casualties. • Next, the medic – or, if able and without a medic immediately available, the wounded – use an aggressive approach to control bleeding through Combat Application Tourniquets (CATs) and hemostatic agents. Such “damage control” is intended to keep the wounded warfighter alive during the “golden hour” until being seen by a doctor. • Soldiers in cold climates, such as the Afghan mountains, also now carry Hypothermia Prevention and Management Kits – chemically heated blankets and hoods. • The fielding of small CT medical imaging machines to battlespace hospitals ended a previous mandate that front-line surgeons conduct invasive exploratory surgeries to find shrapnel embedded in the limbs of soldiers wounded by explosive blasts, such as improvised explosive devices (IEDs). By replacing surgery with noninvasive imaging, the risk of fatal complications has been greatly reduced. • Specialized teams of vascular trauma surgeons also were deployed to in-theater hospitals after data collected in the DOD Trauma Registry, which tracks treatments given to wounded warfighters once they reach field
www.defensemedianetwork.com
hospitals, showed a much higher rate of injuries to veins and arteries in Southwest Asia than in previous wars. • Since 2005, field hospitals also have employed continuous venovenous hemofiltration, a short-term emergency dialysis treatment reducing the incidence of pulmonary edema and respiratory failure among burn victims, many of whom previously had been given too much saline fluid during resuscitation. By 2011 and nearly a decade of constant combat in Southwest Asia, every warfighter was receiving advanced first aid training, and the materials needed for emergency treatment were added to the basic kit, elevating every soldier and Marine to a level roughly equivalent to a Vietnam-era medic. While not scheduled for completion until 2017, the new generation of medics is being trained to the level of civilian emergency medical technicians (EMTs), with the ability to communicate directly, in real time, with doctors who can provide guidance until the wounded warrior can be treated by field doctors. Unlike the rear guard MASH (Mobile Army Surgical Hospital) units of Korea and Vietnam, emergency and traumatic care doctors and surgeons advanced to the front lines, making care that previously could have taken hours or even days to reach available within the golden hour after being wounded. Once stabilized, the wounded now are immediately airlifted to the nearest permanent military hospital or hospital ship, then on to major medical care facilities, such as Landstuhl Regional Medical Center near Ramstein Air Base, Germany – often within 24 hours of being injured – and finally to the United States and the most advanced medical care available at facilities such as the Walter Reed National Military Medical Center in Bethesda, Maryland, and the Army Institute of Surgical Research Burn Center at Brooke Army Medical Center in San Antonio, Texas. 23
THEY GAVE 100% SERVING OUR COUNTRY. WE’LL HELP THEM HEAL WITH CLINICALLY PROVEN PRODUCTS.1-6 EpiFix® and AmnioFix® are amnion/chorion membrane allografts that enhance healing, modulate inflammation, and reduce scarring in acute and chronic wounds. • Demonstrated 90%+ healing rates in three DFU randomized clinical studies, two comparative studies, and a crossover study; 90%+ remained healed after 9-12 months1,2,4,5,6 • Contain essential wound healing growth factors • Stored at ambient conditions for up to 5 years
Ask about EpiFix and AmnioFix www.mimedx.com
866.477.4219
1. Zelen CM, et al. Int Wound J. 2013 Oct;10(5):502-7. 2. Zelen CM. J Wound Care. 2013 Jul;22(7):347-8,350-1. 3. Zelen CM, et al. Wound Medicine. 2014 Feb;4:1-4. 4. Zelen CM, et al. Int Wound J. 2014 Apr;11(2):122-8. 5. Zelen CM, et al. Int Wound J. 2015 Dec;12(6):724-32. 6. Zelen CM, et al. Int Wound J. 2015 Dec 23. doi: 10.1111/iwj.12566. Patents and patents pending see: www.mimedx.com/patents. AmnioFix®, EpiFix®, and MiMedx® are registered trademarks of MiMedx Group, Inc. 1775 West Oak Commons Court NE, Marietta, GA 30062 ©2016 MiMedx Group, Inc. All Rights Reserved. www.mimedx.com SB274.003
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Several ophthalmologists assigned to the 332nd Expeditionary
PHOTO BY STAFF SGT. JULIE SHOWALTER
Medical Operations Squadron operate on a trauma patient who sustained extensive eye injuries during combat operations in Iraq. The increased number of traumatic eye injuries sustained in Southwest Asia has resulted in the majority of the Defense Department’s vision research funding being directed toward battlefield eye trauma treatment, diagnosis, surgical approaches, TBIrelated vision impairment, and other combat injuries.
Vastly improved personal body armor dramatically reduced penetrating wounds to the torso, but the head, arms, and legs remained subject to blast and bullet injuries. The latter led to the highest percentage of amputations among U.S. military wounded since the Civil War, but the escalating levels of care available, from the moment of injury, meant many who would have died in the field in previous wars survived, often with seriously damaged limbs saved, others eligible for technologically advanced prosthetics. In the case of lower-limb prosthetics, some claim they are better than the legs with which they were born. Advances in injury prevention, plus early diagnosis and treatment of those who were wounded, including “invisible” trauma to the brain, have saved the lives and quality of life of thousands of servicemen and women since 9/11. Those advances were carried over to post-service care through the Department of Veterans Affairs (VA) and into civilian medicine, as well. But while warfighter protective gear has saved lives, the changing nature of combat and enemy tactics have also increased injuries – and resulting medical research and care. Since 9/11, the majority of DOD vision research funding has gone toward battlefield eye trauma treatment, diagnosis, surgical approaches, TBI-related vision impairment, and other combat injuries. While the vast majority of reported eye injuries are listed as mild or superficial, the wars in Southwest Asia also saw an increase in serious retinal, optic nerve, and burn injuries to the eye, with blast-related eye injuries leaving thousands of warfighters at a high risk of eventual blindness. Those and
www.defensemedianetwork.com
other blast injuries require immediate action in the field if the wounded warrior is to reach advanced medical care in a condition conducive to saving a limb, hearing, sight, etc. “It’s not unusual for doctors at Walter Reed and Landstuhl to spend hours trying to rebuild an eyeball that was severely damaged. There are no civilian injuries that come close to what we are facing on today’s battlefield from blast injuries. Ophthalmologists called to active service and deployed to Iraq or Afghanistan say they had never seen, in private practice, what they had to deal with there,” according to Tom Zampieri, a Vietnam-era Army medic and, after returning to college, an Army National Guard flight surgeon. Today, blinded in a non-military-related accident, he is director of government relations for the Blinded Veterans Association. “In the past, people with such horrific injuries never would have made it off the battlefield alive. Today they do, and we have to figure out how to put a private’s face back together and often restore vision. An Air Force surgeon on his third combat deployment told me the magnitude of facial injuries from this war is unbelievable. [In the first decade alone], surgeons in Afghanistan said, about 16 percent of all wounded evacuated to Landstuhl had some form of eye trauma.” Zampieri said deployment-related trauma research is directed toward tissue, cornea, and retina repair, with the hope some ongoing research into neural systems will help down the road. Also some years away from possible application will be the result of current research into tissue regeneration, such as regrowing parts of the retina or growing a new cornea using stem cells. Programs at the U.S. Army’s Telemedicine & Advanced Technology Research Center (TATRC) are focusing on a wide range of battlefield and post-evacuation solutions to meet operational gaps in theater health services regarding vision, field medical robotics, biomedical technologies, sleep deprivation, nutrition and hydration, and more. In March 2016, TATRC’s Operational Telemedicine Lab partnered with the Marine Corps Warfighting Lab (MCWL) to conduct experiments in battlefield medical situational awareness and combat casualty care during the Rim of the Pacific (RIMPAC) 2016 exercise in Hawaii and Southern California. MCWL inserted a forward surgical unit, a maneuvering shock trauma squad, and a shock trauma squad operating within an aircraft into the Southern California urban terrain operations. TATRC support included six TEMPUS Pro™ physiological monitors, integrated into the Navy’s experimental 25
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A TEMPUS Pro device, which enables a patient’s vital signs and
Distributed Tactical Communications Systems (DTCS), allowing forward resuscitative care teams, on the ground and airborne, to transmit vital signs and other medical data over tactical communication systems to higher echelons of care to ensure situational awareness, get assistance, and prepare for the arrival of casualties. All that is part of what MCWL calls the “Medical Common Operating Picture,” designed to provide future commanders and medical officers with real-time patient status during transit, the status and location of medical units and supplies, and disease tracking. TATRC and MCWL plan to continue this partnership at least through 2018, working to integrate ultra-wideband medical sensors and other en route care wireless medical capabilities, capture and transmit electronic point-of-care medical data with DTCS, and integrate medical data into the Tactical Cloud. Joint collaborative cooperation, experimentation, and development between TATRC and MCWL is essential to the success of future joint operations, according to the Corps. Through leveraging partnerships and innovations, the Army and Marine Corps can ensure that they are ready to provide the best possible care for the casualties of future wars. Although the Air Force is not normally thought of as providing battlefield medical care, aside from long-distance patient transport, it, too, has benefitted from technological advances. The Critical Care Air Transport Team (CCATT), for example, provides C-130-based flying ambulance services and emergency medical care, when and where needed. 26
According to the Air Force, that includes the only longdistance extracorporeal membrane oxygenation (ECMO) machine in the world to provide cardiac and respiratory care. Almost all U.S. Coast Guard cutters involved in potentially hazardous missions have basic first aid, emergency medical technicians, and corpsmen aboard. Not many smallboat stations have a corpsman, but every effort is made to have at least one EMT on each crew that does smallboat or boarding missions operating from a cutter, in case something arises that requires more than basic medical training. “That’s as much to protect our own people as it is those with whom we interact in the maritime environment, having some immediate capability to triage or at least start them toward more advanced medical help if the situation requires it,” Capt. Daniel Deptula, Coast Guard chief of Contingency Preparedness and Exercise Policy, explained. “If advanced-level care is required, we would work to get that individual to the proper medical facility as quickly as possible. “But we don’t have the capability for large numbers of personnel handing medical care. They do have a more advanced medical capability – and it’s not easy to get that EMT certification – but they aren’t doing higher-level care. So we also always have a Coast Guard flight surgeon available by phone to have a connection to advanced capability to give our folks in the field direction until they can reach a hospital. Sometimes we also have U.S. Navy doctors involved in that role.” For the first few years of OIF/OEF, many serious injuries to the brain, eyesight, and hearing went under-reported – and untreated – on the battlefield, especially when caused by IEDs or other explosions that resulted in more visible, often life-threatening, wounds. Army medical officials estimate as many as 29 percent of all those wounded in combat also suffered eye injuries, for example, before the military mandated the use of ballistic glasses, which had been issued to deployed troops but often not used. Those findings spurred more intensive medical safety training of warfighters prior to deployment and the inclusion of components in the standard kit, such as coagulant bandages designed to stop or at least reduce bleeding, and the CATs. A new Burn Resuscitation Decision Support System helped combat medical personnel determine the ideal amount of IV fluid to give a patient 48 hours after a severe burn. The Army also instituted a TBI management strategy mandating medical attention within 24 hours of a suspect incident (such as an IED causing those in an otherwise protected vehicle to be tossed around inside the hull) and medical clearance before being allowed to return to duty.
www.defensemedianetwork.com
PHOTO BY CPL. SCOTT REEL
other medical data to be transmitted from the battlefield to higher echelons of care, undergoes operational testing aboard Camp Pendleton, California, over two days of trials in January 2014.
U.S. AIR NATIONAL GUARD PHOTO BY STAFF SGT. ALLAN EASON
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
U.S. AIR FORCE PHOTO/SENIOR AIRMAN NICOLE SIKORSKI
■■ ABOVE: Tech. Sgt. Eddie Colon, left, and Lt. Col. Patrick
Johannes, both assigned to the 10th Expeditionary Aeromedical Evacuation Flight and both members of a Critical Care Air Transport Team (CCATT), discuss a patient’s care in flight on July 4, 2014. RIGHT: A first responder retrieves gauze from a first aid kit to treat a simulated wound during a TCCC course on Aug. 5, 2015. Among the standard items in kits issued to warfighters are Combat Application Tourniquets as well as coagulant bandages designed to stop or reduce bleeding.
Unfortunately, TBI symptoms may not manifest for months or even years after the original injury. Research by Duke University’s School of Medicine and the VA has found soldiers close to explosions in combat may experience brain injuries without showing any symptoms. Despite an increase in research and treatment protocols, brain trauma remains a mystery. It is believed to be a trigger for post-traumatic stress disorder (PTSD), but any exact relationship remains unclear. A 2015 study by Royal Navy surgeons and the University of Birmingham of U.K. soldiers who survived “unsurvivable” injuries in Southwest Asia found the level of injury severity in which half of casualties would be expected to survive had nearly doubled between 2003 and 2013. According to the study, 572 casualties survived injuries the U.K. National Health Service (NHS) classified as “life-threatening” and 38 survived what NHS termed “unsurvivable” wounds. “This study is the most detailed analysis of combat casualties ever released on either side of the Atlantic and is the
www.defensemedianetwork.com
first to definitively prove that the huge efforts to advance and improve the care of our wounded have been enormously effective,” Lt. Cmdr. Jowan Penn-Barwell, a Royal Navy surgeon, told the London Telegraph. Even so, there remain many gaps in the treatment available to wounded warfighters in the field. While a number of government agencies, universities, and private-industry labs are working to address most of those, many are looking to the Defense Advanced Research Projects Agency (DARPA) for major future advances. Known for its pursuit of technologies 27
Proudly supports all of your dental, medical, and supply needs. Supporting your supply needs through the following contracts: DLA ECAT Dental Program SPM2DE-14-D-7469 DLA ECAT Lab Contract SPE2DE-15-D-0007 DLA Medical/Surgical DAPA Holder SP0200-96-H-5014
FEDERAL SUPPLY SCHEDULES: Pharmaceuticals and Drugs (Anesthetics) V797P-2280D Dental Equipment and Supplies V797P-3160M
HENRY SCHEIN, INC. IS A PROUD FEDERAL SUPPLY SCHEDULE DISTRIBUTOR FOR: KaVo Dental Equipment V797P-3218M Kerr V797D-30021 Imaging Sciences Dental Equipment V797P-3235M Pelton & Crane Contract V797P-3241M Busse Hospital Disposablesâ&#x20AC;&#x201D;Medical Equipment and Supplies V797P-4488B
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Defense Advanced Research Projects Agency Director Dr. Arati Prabhakar speaks with reporters during DARPA Demo Day 2016 at the
DOD PHOTO BY MARINE CORPS SGT. DREW TECH
Pentagon on May 11, 2016, to give the Defense Department community an up-close look at the agency’s portfolio of innovative technologies and military systems. Among DARPA’s current research endeavors are the Pharmacy on Demand and Biologically-derived Medicines on Demand initiatives of its Battlefield Medicine program, which aims to close current capability gaps in combat zones of the future.
and capabilities considered on the far edge of science, DARPA has established a Battlefield Medicine program to close current capability gaps in future combat zones. According to the program’s director, Dr. Tyler McQuade, DARPA is pursuing two integrated research thrusts – the Pharmacy on Demand (PoD) and Biologically-derived Medicines on Demand (Bio-MOD) initiatives. Together, they are seeking to develop miniaturized device platforms and techniques that can produce multiple small-molecule active pharmaceutical ingredients (APIs) and therapeutic proteins on site in response to specific battlefield threats and medical needs as they arise. “The PoD research is aimed at developing and demonstrating the capability to manufacture multiple APIs of varying chemical complexity using shelf-stable precursors, while the Bio-MOD research is focused on developing novel, flexible methodologies for genetic engineering and modification of microbial strains, mammalian cell lines, and cellfree systems to synthesize multiple protein-based therapeutics,” he explained. “As a proof of concept, both PoD and
www.defensemedianetwork.com
Bio-MOD efforts will seek to develop platforms for manufacturing single-dose levels of FDA-approved APIs and biologics and demonstrate high purity, efficacy, and potency in short timeframes. “[In so doing], Battlefield Medicine will leverage continuous flow approaches that will, if successful, pave the path forward for enabling distributed, on-demand medicine manufacturing capabilities in battlefield and other austere environments. Additionally, the platform would have built-in flexibility to produce multiple types of therapeutics through its modular reaction design. The ultimate vision for Battlefield Medicine is to enable effective small-batch pharmaceutical production that obviates the need for individual drug stockpiling, cold storage, and complex logistics.” The treatment of wounded warfighters in the field and at first-level battlefield medical facilities in 2016 is so far advanced over late 20th century capabilities it could be seen as science fiction-cum-fact. But what researchers expect to be fielding in 2026 could make even those advances pale by comparison. 29
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
Lt. Gen. Mark A. Ediger, MD Surgeon General of the Air Force By Scott R. Gourley
n LT. GEN. MARK A. EDIGER, MD, is the surgeon general of the Air Force, Headquarters U.S. Air Force, Washington, D.C. Ediger serves as functional manager of the U.S. Air Force Medical Service. In this capacity, he advises the Secretary of the Air Force and Air Force Chief of Staff, as well as the Assistant Secretary of Defense for Health Affairs on matters pertaining to the medical aspects of the air expeditionary force and the health of Air Force people. Ediger has authority to commit resources worldwide for the Air Force Medical Service, to make decisions affecting the delivery of medical services, and to develop plans, programs, and procedures to support worldwide medical service missions. He exercises direction, guidance, and technical management of a $5.9 billion, 44,000-person integrated health care delivery system serving 2.6 million beneficiaries at 75 military treatment facilities worldwide. Prior to his current assignment, Ediger served as deputy surgeon general, Headquarters U.S. Air Force, Washington, D.C. Ediger is from Springfield, Missouri. He entered the Air Force in 1985 and has served as the aerospace medicine consultant to the Air Force surgeon general, commanded two medical groups, and served as command surgeon for three major commands. He deployed in support of operations Iraqi Freedom, Enduring Freedom, and Southern Watch.
Veterans Affairs & Military Medicine Outlook: What is the Air Force surgeon general’s role and in what ways, if any, does it differ from the other armed forces surgeons general? Lt. Gen. Mark A. Ediger, MD: In Air Force Medicine, we have three primary roles. The first one is to support the Air Force operations and the operations of the joint team. Our second primary role is to sustain a ready medical force deployable and prepared to support joint operations anywhere in the world. Then our third primary purpose is to provide high-quality, safe medical care. My job as the Air Force surgeon general is to ensure that our medical professionals in our hospitals and clinics and at our deployed sites have what they need and are prepared to meet those three primary roles. 30
Now, my role differs a bit from that of my Army and Navy counterparts in that I am not in command of our medical forces. In the Air Force mission, it has always been the case that our medical force is under the command and control of operational commanders. In most cases, that’s a wing commander. That works well for our mission and continues to work well for us today. I am an officer on the Chief of Staff of the Air Force’s staff. Then at each of our major commands, we have a command surgeon. I work in close coordination with the major command surgeons to ensure that our medical force is developed, ready, and has all the resources required to successfully support the mission. Can you talk about the kinds of Air Force medical teams that you have out there and how many you have deployed? Certainly. Our types of teams fall into two main categories. One category includes the medical teams that perform on the ground. We call them ground assemblages. This consists of our squadron medical elements. These are squadron flight surgeons and their technicians. They deploy with Air Force flying units and special operational units to ensure they have the medical support they need. Then also, our ground assemblages consist primarily of our field hospital, which we call the Expeditionary Medical Support [EMEDS] system. That is our version of a field hospital. It’s [modular] and it can be deployed and established in a number of different configurations, which makes it flexible to meet the mission. Those are our ground assemblages. Within that EMEDS system, there are component teams that can be broken out and deployed separately. The most common is the Mobile Field Surgical Team [MFST], which is a verymuch-in-demand asset in today’s U.S. military operations. Then we have Aeromedical Evacuation Teams. As you might expect, their role is to provide something we call en route care. That is the movement of patients, some of whom may be trauma victims from combat trauma. Others may be patients with disease. They are prepared to move patients with whatever the condition may be and get them to a source for definitive care. In an aeromedical evacuation, we have the standard aeromedical evacuation crew,
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Lt. Gen. Mark A. Ediger, MD, surgeon general of the U.S. Air Force.
U.S. AIR FORCE PHOTO
Registry]. Data goes into that system from all of the trauma patients we treat in our deployed sites and includes data in regard to the outcomes for those service members all the way back through their definitive care in a U.S. medical center and their rehabilitative care. That has produced a lot of opportunities for research and has produced a number of significant changes and gains in the way we handle trauma victims. The research based on those lessons learned and that trauma registry have led to multiple publications in U.S. and international medical journals and have led to significant changes and improvements in the standard of care for trauma victims in trauma centers around the world. An example I can cite for you is how we do fluid and blood product resuscitation of trauma victims. The things we learned from our experience supporting combat operations in Iraq and Afghanistan fundamentally changed the way trauma patients are now resuscitated in emergency rooms and trauma theaters through the use of fluid and blood products. And it’s made a real difference in terms of improving the outcome for those patients. Another example would be our management of burn patients. The data that was captured from the combat operations highlighted some excellent opportunities to improve the outcomes for patients with serious burns. Those have become standards in the fluid resuscitation of burn patients now. which consists of nurses and technicians, specially trained to provide care in flight. We also have Critical Care Aeromedical Transport Teams. These are specialty teams with critical-care specialists, who can move patients who require critical-care support during transport. They are trained and equipped to move patients long distances as required. Then for the more tactical environment where we have critical-care patients that need to be moved within a deployed theater, perhaps even from the point of injury, we have Tactical Critical Care Evacuation Teams. These teams, as the name implies, can provide critical-care support before the patient reaches their initial hospital to start the continuum of critical care needed for a patient with a significant combat injury. How have the operational lessons learned allowed these teams to operate farther forward? The operational lessons learned that we’ve gained via the Joint Trauma System is one of the major advances that came about during the wars in Iraq and Afghanistan. The Joint Trauma System operates a database called the Joint [Theater] Trauma Registry [now the Department of Defense Trauma
www.defensemedianetwork.com
What kinds of stresses are placed on Air Force medical personnel due to operating farther forward as well as the change in emphasis toward stabilization and rapid evacuation of wounded rather than treatment in more elaborate field hospitals, as in the past? The opportunity that presents itself now to improve outcomes for trauma victims, as you stated, requires initial stabilization and then movement within a relatively short time window to a medical center for definitive care. The experience has shown that this improves outcomes. So, in order to be able to do that and to fully leverage the opportunities to provide advanced care in a forward field setting, our teams need to be prepared to provide advanced care in a field hospital and even in a pre-hospital environment. That means we’re deploying teams with more advanced capability than we have ever in our history. And that’s true for Army, Navy, and Air Force as well. That requires that our teams go forward with the techniques, and the technology, and the equipment to be able to provide advanced care – and sustain the readiness to do so. The other thing that imposes demands on our medical teams with current combat operations is that the nature of the counterterrorism combat operations really requires that we have agility and 31
AMSUS, a non-profit, membership-based organization, was created: “for the purpose of advancing the knowledge of military surgery, medicine, and sanitation in the medical departments of the Army, the Navy, and the Marine-Hospital Service of the United States and of the militia of the different States, and to increase the efficiency of the different services by mutual association and the consideration of matters pertaining to the medico-military service of the United States in peace and in war.” – AMSUS Congressional Charter 1903
AMSUS continues this mission today, and also represents all healthcare disciplines affiliated with: • Federal Health Agencies • Department of Veterans Affairs • International Military Medicine
amsus.org
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Ediger (middle) and Chief Master Sgt. Jason E. Pace, chief, Medical Enlisted Force (right) examine dental equipment at the 48th Dental
U.S. AIR FORCE PHOTO BY AIRMAN ELI CHEVALIER
Squadron dental lab at Royal Air Force Lakenheath, England, July 25, 2016. Ediger and Pace visited many of the 48th Medical Group’s facilities during their tour to engage with airmen.
the ability to be somewhat mobile in terms of our surgical stabilization capability. To apply the advanced intervention techniques and to apply the lessons we’ve learned from the research using the Joint Trauma Registry, our teams need to be able to be agile and to move about, but have equipment that is a small enough equipment package that it can be moved readily and set up in a building of opportunity. In support of counterterrorism operations, we’ve found that the surgical teams and the critical-care teams need to be able to operate outside the hospital environment often in a location that was never built or designed to be used for medical care. That’s requiring a lot of innovation and ingenuity and a lot of training and a lot of insight as we equip the teams. Can you highlight any developments either involving en route care or innovations on the battlefield that bring a special sense of organizational pride? The establishment of the Critical Care [Air] Transport Teams in the late 1990s has enabled us to move trauma victims much more quickly than we were able to do
www.defensemedianetwork.com
historically. That’s had a dramatic effect on improvement on the outcomes. But we know that there are further opportunities to enhance our capability in terms of what kind of inventions and what kind of monitoring we can apply in the in-flight environment. So we continuously are performing research in terms of new ways to apply technology in the in-flight environment and aeromedical evacuation and new ways to be able to continue with the stabilization process during movement. We know the nature of U.S. military operations are such that it is becoming increasingly likely on occasions that we will move patients a significant distance who have yet to be treated in a hospital. We know we need to have as much capability as possible in flight to continue the stabilization. So we have research right now on systems that will help our teams do that. Examples of these would be systems that use equipment, including microprocessors capable of using computer logic, to help with trend analysis in flight on vital signs, to actually have autonomous adjustment of ventilator settings in flight, and also to apply some diagnostic techniques in flight, such 33
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Staff Sgt. Michael Garrett, with the 59th Training Group, briefs Ediger and Pace during their tour of the Medical Readiness Training (MRT)
Center on Joint Base San Antonio, Camp Bullis, Texas, May 5, 2016. The MRT provides initial, sustainment, and future medical training on its 128-acre training site.
34
get to a hospital. Of course, the new electronic health record that the Department of Defense is acquiring now will include the capability to capture and transfer data as well. Are there differences between Air Force deployable or expeditionary facilities and those of the other services? There are. As in Air Force medicine, we’re part of a joint team, obviously. In Iraq and Afghanistan and in the operations today, we’ve got a strong track record of operating well as a joint team. What we bring to the joint team tends to be a ground medical capability that is more agile and … can be moved with relatively little airlift, can be established quickly,
www.defensemedianetwork.com
U.S. AIR FORCE PHOTO
as ultrasounds, that would enable us to detect conditions that may need intervention while in flight. These are just a few of the innovations that are being researched right now. This is being done in partnerships with trauma centers where we have Air Force trauma specialists embedded and then being prototyped for use in operational settings. We’ve also implemented an electronic health record in aeromedical evacuation. That’s helping us in terms of more fully capturing data in terms of the status of our patients and the interventions we provide and then being able to transfer that data into the patient’s electronic health record when they
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
and be able to provide emergency room and surgical stabilization capability within hours of arrival. Our field hospitals are not large in capacity. Our largest bed capacity in a field hospital is the EMEDS+25. That’s a 25-bed hospital. We have a smaller version that’s just a 10-bed hospital. The Army and Navy have much larger field hospitals with a greater bed capacity that require more time to move and be established. So what we bring to the joint team is the ability to get in quickly and rapidly establish emergency care and surgical stabilization. You’ve served in the past with Air Force Special Operations Command (AFSOC). What special training, skills, or standards pertain to special operations medical airmen? I first came to AFSOC in the aftermath of the engagement in Mogadishu [Somalia] that became part of the Black Hawk Down story. That was a time when special operations medicine was learning some things that have now translated into the conventional force. That was about the importance of controlling hemorrhage at the point of injury and the opportunity to save lives by doing that. During my initial tour in AFSOC, Army, Navy, and Air Force special operations medics were working together to develop the techniques to control hemorrhage in a tactical environment. That begins with the operators providing care to each other or potentially to themselves in order to immediately control hemorrhage and then for the special operations medics to provide a hemorrhage control and resuscitation in the tactical environment. That led to the creation of something called Tactical Combat Casualty Care. That proved to be a very successful concept that has become the foundation and the basis for training every military member and every deploying military medic. Tactical Combat Casualty Care is now fundamental to how we prepare soldiers, sailors, airmen, and Marines to go forward and be prepared to care for each other immediately to improve the opportunity to survive a serious wound. That all started with a special operations experience that our military had in Mogadishu. Those lessons were captured. And so today’s special operations medics are a very, very capable force. Because of the nature of the mission they support being a very small but agile combat force, they have to be small, efficient, and agile as well. So some of the changes we made to our conventional capability to support the ongoing counterterrorism operations today really came from special operations. Our conventional force also, of course, has to be ready for a large-scale combat operation because we know that is always something for which we must maintain our readiness. So special operations medical forces really focus on the agile support in an austere environment almost exclusively, whereas our conventional forces bridge between large-scale
www.defensemedianetwork.com
counterterrorism operations and then a major, more conventional combat operation. Can you talk just a bit more about the ongoing requirement to maintain medical readiness for deployment? Yes, when I came in the Air Force, the range of medical specialties we would deploy in military medicine was pretty narrow. For example, when I came in the Air Force 30 years ago, we did not think we would deploy a vascular surgeon or a neurosurgeon, or even a burn surgeon. But over time, our medical professionals have developed the capability to take advanced techniques into the field environment. That means we’ve got a lot more capability in a field hospital than we once had. That means that we need to keep the medical professionals that make up that advanced capability in practice day to day at home station in the hospitals where they are assigned that will sustain that readiness to provide the kind of complex care they provide in a combat field hospital. And that creates some new requirements for us. The population that we serve, who are primarily active-duty members and their families, tends to be a relatively, young, healthy population [that does] not typically need the kind of complex care those professionals are able to provide. We’ve found that we need to actually reach out and establish partnerships with trauma centers and academic medical institutions and with the Veterans Administration so that our surgical sub-specialists, our general surgeons, our orthopedic surgeons, and our critical-care specialists get the volume and the mix of complex care that they need to sustain their skills. So we’ve found that we’ve evolved the practice of our surgical and our critical-care specialists such that they practice in our hospitals, but they also practice in partner institutions where there are more trauma patients or more patients with complex medical conditions. The agreements we’ve established with the Veterans Administration have been very helpful in that by virtue of receiving referrals from the Veterans Administration, we are able to provide great care to veterans in our hospitals and at the same time help keep our deployable medical teams current through a more diverse practice. We continue to work to increase the number of our agreements. We currently have over 60 agreements with Veterans Administration hospitals to provide specialty care. And we continue to build that number. That’s an endeavor that is underway. We have a concept that we published last year that describes the principles. We have a multi-phased action plan right now that is in progress. A significant part of that action plan is investing in the development of our medical professionals so that they are trained and knowledgeable in how to continuously improve how we provide care and also to have the strong communication and the focus on identification of risk early. 35
Modernizing VistA to Support Veteransâ&#x20AC;&#x2122; Heatlhcare For more than 20 years, VA has benefited from our technical and service integration expertise to modernize the legacy system into a robust platform with hundreds of Best-of-Suite, Best-of-Breed, custom applications and integrated components. These components provide a fast path to healthcare breakthroughs that improve Veteransâ&#x20AC;&#x2122; access to care, satisfaction and performance outcomes.
dssinc.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Ediger attended battlefield acupuncture training taught by Dr. Richard Niemtzow, director of the Air Force Acupuncture Center on Joint Base
U.S. AIR FORCE PHOTO/MATTHEW EICHIE
Andrews, on April 1, 2016. Battlefield acupuncture is a rapid technique using tiny acupuncture needles inserted into the ears that directly modify the way the central nervous system processes pain so as to reduce pain significantly in more than 80 percent of patients. The technique was developed by Niemtzow in 2001.
In addition to deployment readiness, where are the challenges in delivering safe and quality medical care to Air Force personnel and their families? Every health system has as its primary focus the assurance that the care we provide is best quality and as safe as we can possibly make it. That is not easily done. It requires continued focus and attention. Last year, in Air Force Medicine, we reviewed our performance as a health system. While our performance was good and compared favorably with other health systems, we felt like we could be better. We decided to apply our commitment to safe, high-quality care in a new way. It’s called Trusted Care. Under Trusted Care, we’re seeking to gain the highest possible reliability as a health care system. It is a new way of applying our commitment. Primarily, it’s a new approach to leading and developing a culture within Air Force Medicine, in which we have a laser focus on recognizing potential risk and then mitigating that risk before it turns into something that could reach a patient or even harm a patient. That requires that as a team, every member of the team in Air Force Medicine has a duty and a responsibility day to day to be alert for things that could pose risk to a patient and then to communicate about that risk and then participating in the actions to ensure that risk does not turn into
www.defensemedianetwork.com
something that could harm a patient. That’s what I mean by a culture focused on risk. We also need a culture that takes a systems approach to engineering safety into our operations. That engineering includes our processes by which we provide care. It also includes things like the sustainment, maintenance, and design of our equipment. And the purpose of that engineering is to catch errors before they reach a patient. We know that anything that involves human activity – such as provision of health care, flying aircraft, working on a construction site – those are all human endeavors, and so errors will occur. That’s just the nature of human activity. We’ve found that in our culture, we need to acknowledge the fact, even though we don’t like to do so, that we will sometimes make errors. So we need to engineer our processes, and our equipment, and our facilities so that we have safety measures in place that will catch errors before they reach a patient. The third important imperative that we must meet in this effort is to apply standards and use standards within our provision of care. Standards will help us be more consistent in terms of our approach and will allow us to also operate a military health system in which our staff moves from assignment to assignment, or even deploys, and they are all accustomed 37
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
to practicing under the same standards. So those standards translate into the deployed environment, but they’re also consistent from one Air Force hospital to another and from one Air Force clinic to another. Are those some of your biggest challenges today or are there any others you can point to? I think Trusted Care and moving forward with the cultural change in Air Force Medicine to continue to provide safer care is one of our biggest challenges. The other challenge that I would say is one of our biggest challenges is sustaining our readiness as a medical force. As I described earlier, we have a highly capable medical force that we ask to go into austere and difficult environments and to provide advanced care. Keeping that force ready day to day and prepared to go where they may need to go and to be able to provide the best quality care in any environment is a big challenge. And it’s really why we exist in uniform in military medicine. In your February 2016 Senate testimony, you briefly mentioned some of the strategies to meet future needs of the Air Force and joint team. Can you talk briefly about how you see military medical care evolving in the future? I think as we think about what our future operating concept would be in military medicine and in Air Force Medicine, in particular, there are six primary things that we believe will be encompassed in that future concept. The first is our casualty care in the future will need to be increasingly agile and more capable. By more capable, I mean more capable in terms of taking advanced intervention techniques into the field hospital, but then also all the way to the point of injury and putting them in the hands of the medics who are forward deployed with the operational force. No. 2 would be a continued emphasis on enhancing the ability of the airmen to perform day to day. Our airmen are being asked to perform in a complex array of mission capabilities and in a constantly changing threat environment. We are asking more and more of airmen in terms of their ability to perform and adapt and innovate in that performance. No. 3 would be provision of high-quality, safe specialty care that meets the needs of our patients in terms of operational medicine as well as more traditional clinical medicine, but also sustaining a ready medical force by doing so. No. 4 would be precise prevention-focused primary care. This is state-of-the-art primary care for airmen and their families to help them live a long, healthy life. No. 5 would be the integration of health data across the entire continuum of a member’s service and across the entire continuum of their health care, from the point they first fall under military medicine’s responsibility all the way through their care in the Veterans Administration following service
www.defensemedianetwork.com
■■ The agreements we’ve established with the Veterans Administration have been very helpful in that by virtue of receiving referrals from the Veterans Administration, we are able to provide great care to veterans in our hospitals and at the same time help keep our deployable medical teams current through a more diverse practice. or within our system following service – integrated data available across the entire continuum. Then the sixth is global health. That is our ability to support the U.S. strategies by working as an international partner and engaging in global health imperatives around the world, whether that’s humanitarian assistance, capacity building, or partnerships with a foreign military service to increase their capability. Those are the six primary things that fall within our future operating concept we believe in Air Force Medicine. Currently, today, we have four primary focus areas where we have actions in progress right now that support that future operating concept and build us toward that destination. The first of our focus areas is full-spectrum readiness and keeping the medical team clinically current and ready across the spectrum of the missions we support. The second is integrated operations support. That is reaching beyond the walls of our clinics and hospitals into the operational units to provide health-oriented and performance-oriented support that is tailored to the mission. The third is the Air Force Medical Home. That is really our instrument by which we have teams that provide primary care. That’s prevention oriented and provides coordinated care for complex chronic conditions. Then the fourth focus area for us is Trusted Care – that renewed commitment to high-quality safe care. Do you have any other takeaway messages you would care to share? We, in Air Force Medicine, in military medicine, are the beneficiaries of strong support from the taxpayers of the United States, from the Congress, and from our leadership in the Department of Defense and the services. We value and appreciate that support. We understand that we provide care for probably the most special patient population anywhere. We take that obligation very seriously. I’m privileged to be the surgeon general for an extraordinary group of medical professionals in Air Force Medicine. We appreciate everybody’s support. I personally appreciate the great work by the men and women of Air Force Medicine. And I’m privileged to be their surgeon general. 39
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
Disaster Response and Emergency Preparedness n TRAINING BOTH DOMESTIC AND FOREIGN civil defense and first responder organizations and active uniformed services to prepare for and respond to natural and man-made disasters, including major disease outbreaks, has become a significant part of the mission for the U.S. Army, Navy, Air Force, Marine Corps, Coast Guard, National Guard, and reserves. Every operational military unit receives medical training as part of its individual and unit qualifications. If personnel are being deployed to a known hazardous health environment, more advanced training and equipment are provided that typically are not available to all units. Officials say they are working to increase response capabilities in such environments in the future, not just with small numbers of personnel but also to be able to operate on a sustained basis. Looking at the equipment and training needed to support that effort is an ongoing initiative. Each uniformed service shares best practices with the others as well as with non-military agencies, such as the Centers for Disease Control and Prevention (CDC), the Department of Health and Human Services (HHS), the Department of Homeland Security (DHS), the Federal Emergency Management Administration (FEMA), etc. “DOD [the Department of Defense] doesn’t really work unilaterally with state and local officials domestically nor with other countries, although the COCOM [combatant commander] with that geographic responsibility will have some security and human assistance agreements they may work through that country’s military or ministry of health, for both pre- and post-disaster. But most of the time, DOD deals with another U.S. federal agency as part of a coordinated response,” according to Thomas LaCrosse, director of Defense Support of Civil Authorities (DSCA) in the Office of the Assistant Secretary of Defense for Homeland Defense and Global Security. Many routine FEMA requests for DOD help with a domestic disaster can be approved by the COCOM, which 40
www.defensemedianetwork.com
U.S. ARMY NATIONAL GUARD PHOTO BY SGT. HEIDI KROLL
By J.R. Wilson
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
■■ OPPOSITE: Members of FEMA’s Massachusetts Task Force 1 Urban
U.S. ARMY PHOTO BY SGT. JESIAH DIXON
Search and Rescue, an airman from the Royal Canadian Air Force, and an airman from the New York Air National Guard lift a sked containing a simulated casualty during Vigilant Guard 2016 at Camp Ethan Allen Training Site, Jericho, Vermont, on July 29, 2016. Vigilant Guard is a national-level emergency response exercise, sponsored by the National Guard and NORTHCOM, which provides National Guard units an opportunity to improve cooperation and relationships with regional civilian, military, and federal partners in preparation for emergencies and catastrophic events. RIGHT: Civil Affairs soldiers and security forces from 10 allied and partner nations receive training from Dana Chivers, an adviser to U.S. European Command (EUCOM) for USAID and the Office of U.S. Foreign Disaster Assistance (OFDA), on humanitarian aid and disaster response during Exercise Immediate Response 16. Preparing for and responding to natural and man-made disasters has become an important part of the mission for the U.S. military.
usually is U.S. Northern Command (NORTHCOM) for the continental United States, Puerto Rico, and the U.S. Virgin Islands, and U.S. Pacific Command (PACOM) for those in the Pacific. More complex requests require authorization from the Office of the Secretary of Defense (OSD), which could be the secretary, an OSD specialist, or a service secretary, the decision on whom is made by OSD subject-matter experts. All FEMA requests receive fiscal and legal reviews before assistance is approved. Foreign disaster relief typically falls into two categories, LaCrosse said: “Steady State Humanitarian Assistance – Helping other countries with their ability to prepare for disasters, so when we have to go there, we have a partner or what we already have done there has made that country more capable of handling everything on their own. The Philippines typically falls into the latter, for example. “Standard Disaster Relief – Tied very closely to USAID’s [U.S. Agency for International Development] Office of Foreign Disaster Assistance, which typically calls on DOD assistance for about 10 percent of the international disasters it tracks. “For the first half of 2016, we received 48 requests for domestic assistance – 19 from FEMA, six from HHS, and nine from the National Interagency Fire Center, plus about a dozen from other sources, such as the political conventions, UN events, even the Rio Summer Olympics. Not every domestic emergency or disaster will require a DOD response.” While little specialized individual or unit training is required for domestic or international military disaster response efforts – which involve the same equipment and tasks used in their regular missions – it has become an increasingly important part of international training exercises, according to John Trigilio, director of Humanitarian Assistance and Response Operations in the Office of the Assistant Secretary of Defense for Special Operations and Low Intensity Conflict. “More and more military exercises include a humanitarian element, taking unique capabilities we have ‘off the
www.defensemedianetwork.com
shelf.’ Those often are done in cooperation with USAID and [the Department of] State,” he said. “OHDACA [Overseas Humanitarian, Disaster, and Civic Aid] also funds humanitarian anti-mine activities out of my office.” Training with and of civilian first responders and response to an actual domestic disaster are among the few exceptions to the Posse Comitatus Act of 1878, which added to the U.S. Code provisions prohibiting the use of the Army for domestic law enforcement. The U.S. Air Force was added to the prohibition in 1956. While the Navy and Marine Corps are not specifically named in the law due to their status as maritime forces, the Department of the Navy has implemented internal regulations essentially applying Posse Comitatus to both services. Air and Army National Guard units, considered to be state militias, are exempt. So is the U.S. Coast Guard, an armed uniformed service under DHS (except when called to duty as a wartime component of the Navy). In August 2016, DOD published a three-volume manual detailing the legal and regulatory conditions under which U.S. military capabilities can be used during domestic civilian emergencies. The manual identifies six standing Execute Orders (EXORDs) authorizing DOD support to civilian authorities, relevant presidential directives, and a host of other instructions, regulations, statutes, and directives that limit or expand military domestic involvement. Despite more than a century of legal restrictions, the manual describes a wide range of areas in which the military has been granted a domestic mission, including: search and rescue, explosive ordnance disposal, response to chemical, biological, radiological, and nuclear (CBRN) incidents, pandemics, acts of terrorism, mass migration emergencies, civil disturbances, and support to National Special Security 41
OWN THE FUTURE™
PRACTICE PLANMECA
Discover ProMax 3D Mid ®
PLANMECA
CBCT Ultra-Low Dose™ Technology Without Reduction in Image Quality*
Planmeca ProMax® 3D Mid, an all-in-one imaging solution, includes 2D and 3D modalities, versatile and selectable volume sizes and the Planmeca Ultra-Low Dose™ protocol. Integrate Planmeca Romexis® open-architecture software for optimal workflow and treatment planning.
certified
Ø20x17cm Ultra-Low Dose with Airway Visualization
Ultra Low Dose
For more information please contact Planmeca at 1-855-245-2908 or visit us on the web at www.planmecausa.com *According to “Dosimetry of Orthodontic Diagnostic FOVs Using Low Dose CBCT Protocol” by JB Ludlow and J Koivisto. For a copy of this study, please contact Planmeca USA.
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
■■ Sailors assigned to the Fleet Activities Sasebo branch medical clinic emergency medical team care for a Sasebo city firefighter during an
PHOTO BY PETTY OFFICER 1ST CLASS JOSHUA WAHL
annual national disaster prevention drill at Camp Ainoura. Commander, U.S. Naval Forces Japan Regional Fire Department, and Commander, Fleet Activities Sasebo Emergency Medical Team participation is part of a mutual aid agreement for disaster preparedness and disaster relief operations between the city and base fire departments.
Events (such as political conventions) and national and international sporting events (i.e., the Olympics, World Series, and Super Bowl). The 2012 Defense Strategic Guidance designated DSCA as a primary DOD mission. The Unified Command Plan assigned DSCA as a core mission of NORTHCOM and PACOM. In each case, the designated DOD component does not initiate a response nor act independently, but works closely with FEMA, the CDC, Homeland Security, and state and local authorities. The department’s work with FEMA includes development of all-hazards, pre-scripted mission assignments (PSMAs), which translate civilian support requirements into military tasks to expedite the request-for-assistance process. Although more are in development, there are 28 all-hazards PSMAs for DOD support, more than 30 PSMAs for the Army Corps of Engineers (USACE), and six PSMAs for National Guard support. U.S. NAVY/MARINE CORPS
An important aspect of U.S. military response to overseas disasters is its participation in a variety of annual training exercises throughout the world. One such exercise was conducted on Sept. 1, 2016, by elements of the U.S. Navy from its base at Sasebo, on the Japanese island of Kyushu, and U.S.
www.defensemedianetwork.com
Marine Corps personnel from the USS Bonhomme Richard Expeditionary Strike Group operating near Okinawa. Two MV-22 Ospreys flew medical personnel to Sasebo from the Strike Group and evacuated a simulated patient from a remote island during the annual drill at the Japanese Ground Self-Defense Force’s Camp Ainoura. “Launching from a sea-base to Sasebo for this drill demonstrates the dynamic capability of the U.S. Navy-U.S. Marine Corps team to assist Japanese civilian populations and work alongside our Japanese self defense force counterparts in the event of a disaster,” Capt. Robert Hall, deputy commander of Amphibious Force 7th Fleet, said. At Camp Ainoura, Marines from Combat Logistics Battalion 31 off loaded a Tactical Water Purification System, which would provide an important capability in disaster response. While Fleet Activities Sasebo participates in the drill each year, providing medical and firefighting services to demonstrate the Navy’s commitment to assisting the city in the event of a real emergency, this was the first time that capability was brought from afloat to further assist the simulated disaster relief effort. U.S. ARMY
One of NORTHCOM’s assets for domestic disaster response is the Air Forces Northern National Security 43
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
■■ Soldiers with the 172nd Hazard Response Company from Fort
Emergency Preparedness Directorate, which will take charge during a major national emergency, whether natural or man-made – and especially anything involving radiological materials. Through the directorate, NORTHCOM is mandated by Congress to address 15 National Planning Scenarios, including creation of several classified “concept plans,” such as DSCA. In August 2016, NORTHCOM’s Joint Task Force Civil Support (JTF-CS) participated in Exercise Sudden Response 16 at Fort Hood, Texas. Several JTF-CS units established and operated mass casualty decontamination lines in response to simulated nuclear fallout. Sudden Response was the most recent integration training exercise for DOD’s Defense Chemical, Biological, Radiological, Nuclear Response Force (DCRF), a scalable capability able to deploy within 24 hours to support local, state, tribal, and federal agencies in the event of a large-scale CBRN incident. “Conducting a large-scale exercise like this really helps us to be prepared so that when we have masses, we’re not overwhelmed and we can provide the care and assistance that’s needed,” Capt. Melissa Moorehouse, commander of the 172nd Hazard Response Company, said of the exercise, which also involved more than 200 civilians playing the role of nuclear disaster survivors. “(The role players) are a great enhancement to training because it allows us to relate to real-world scenarios [and] really helps put it into perspective for us.” Overseas exercises provide U.S. and foreign militaries and civilian responders similar opportunities to hone their skills. For example, in February 2016, the U.S. Army Reserve’s 773rd Civil Support Team, members of the Slovenian army, and a team from Spain’s Unidad Militar de Emergencias conducted a weeklong CBRN exercise: Ocean Response. The joint response team trained in disaster scenarios staged at U.S. facilities in Baumholder and Miesau, Germany, before concluding the exercise at the U.S. Rhine Ordnance Barracks. In January 2016, NORTHCOM’s Army component – Army North (5th Army) – deployed its Defense Coordinating Officer/Element (DCO/E) for the Southeastern United States to North Carolina for a 44
Certification Exercise (CERTEX) in which it trained to assist local, state, and federal civilian authorities responding to a simulated Category Four hurricane that had devastated several areas along North Carolina’s coast. The exercise closely mimicked real-world events Army North will face in FEMA’s Region IV – North Carolina, South Carolina, Georgia, Florida, Mississippi, Tennessee, Kentucky, and Alabama – with Army North and more than 50 personnel from nine states focusing on being DOD’s on-site observer and coordinator in a multiagency, civilian-led emergency operations center. It also was designed to further develop the relationship between FEMA and state emergency preparedness liaison officers (EPLOs) assigned to Region IV’s eight states. “As natural disasters or man-made disasters become more complex and resources get constrained, we need to come together as a collaborative group effort to provide the support necessary,” noted Col. Jonathan Simmons, Alabama EPLO. In a simultaneous effort less than a mile from the DCO/E exercise, Army North’s Task Force (TF) 51 took a more hands-on field approach, serving as the forward command post for Joint Forces Land Component Command (JFLCCForward). As with the CERTEX, coordination with civilian officials was a critical component of the TF-51 exercise. “This type of exercise allows us to build solid relationships with local, state, and federal agencies and to better coordinate efforts,” said Maj. David Briten, a TF-51 liaison and future operations planner. U.S. AIR FORCE
In domestic disaster response, the Air Force – typically through the Air National Guard and Air Force Reserve – provides airlift, evacuation, and fire suppression capabilities. The regular Air Force provides similar capabilities for overseas disaster relief missions. Special operations airmen can be dropped into a disaster zone anywhere on Earth within hours to set up and operate emergency airfields. “The USAF could provide a plane with a mixed crew – Air Guard, active duty, Reserve – but fly as a single crew. As soon as they get 12 miles off the U.S. coast, that crew becomes a Title 10 asset, even if they were a Guard asset when they took off. So the Air Force is much more agile as to
www.defensemedianetwork.com
U.S. ARMY PHOTO BY SGT. MARCUS FLOYD, 13TH PUBLIC AFFAIRS DETACHMENT
Riley, Kansas, run a decontamination site Aug. 25, 2016, at Fort Hood, Texas, during Exercise Sudden Response 16. The weeklong exercise was a key training event for the 172nd Hazard Response Company and various other units within Joint Task Force Civil Support, a rapidly deployable force of more than 5,000 service members from across the country who are specially trained and equipped to provide life-saving assistance in the event of chemical, biological, radiological, or nuclear disasters in the United States.
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
■■ Coast Guard Marine Safety Unit Huntington Western River Flood
Punt Team gets locals to safety near Clendenin, West Virginia, on June 24, 2016. The team was assisting the West Virginia State Emergency Operations Center by providing disaster and relief assistance in response to widespread flooding.
what duty status their personnel are in, with the Air Guard floating almost seamlessly between being a state and a federal responder,” LaCrosse explained. Just as DOD works closely with and at the direction of FEMA in most domestic missions, it coordinates overseas disaster response efforts with USAID, which in FY 2015 responded to 49 crises in 45 countries (not all of which involved DOD assistance), a light year compared to the average of 65 disasters in 50 nations. U.S. COAST GUARD
U.S. COAST GUARD PHOTO
The Coast Guard generally is seen by the public as a safety and counter-smuggling agency. But it also is the seventhlargest naval force in the world and called upon by the State Department for the vast majority of training missions involving foreign navies. That has been expanded to include emergency preparedness. The Coast Guard also is called into both domestic and foreign disaster response efforts – from humanitarian aid to earthquake and hurricane response to maritime oil spills, etc. – as well as search and rescue (SAR), at-sea ship collisions, and rescue operations. Those do not always involve the on-site use of Coast Guard equipment and personnel, but may be limited to technical advice to other countries. “From a preparedness perspective, from the national to local levels, we participate in all kinds of missions. We take part in about 500 exercises each year, from tabletop exercises practicing communications and coordination at the headquarters level to the actual deployment of ships and aircraft,” Capt. Daniel Deptula, Coast Guard chief of Contingency Preparedness and Exercise Policy, explained. “Contingency response, in and of itself, can almost be looked at as a mission, although it may be part of any of our 11 missions. But that environment can be unique, and having the skills and capability to not only operate but be a leader is critical to the Coast Guard. “In preparing our medical response – whether mass rescue, hurricane, or earthquake contingency planning – we consider the human impact in terms of health and safety. We may not have all the resources needed to handle those, but we work out plans with our interagency partners to do so. The Coast Guard is unique in that we have many training and evolving relationships with all maritime nations friendly to the U.S.” In actual domestic disaster response operations, the Coast Guard provides some personnel with basic medical training, but the majority of medical care would be
www.defensemedianetwork.com
45
MDX4500 TeleAudiology System
Remote Diagnostic & Fitting Instrumentation
QUASAR
Certified
The MDX4500 TeleAudiology Station comes equipped with Interacoustics proven audiology solutions including: • The Equinox2.0 Audiometer and Real Ear Measurement System for complete and accurate audiometric testing and
hirp® LS verification
• The Titan Tympanometer for
screening and clinical testing
• The Viot Video Otoscope for effective cerumen
management and diagnosis of abnormalities.
All of these devices work seamlessly together. Read more at interacoustics-us.com
VA contract number V797P-43488
*Image view of practitioner conducting a test
ABR/OAE
Balance Assessment
Fitting Systems
Middle Ear Analyzers
Audiometers
Interacoustics is a world leading diagnostic solutions provider in the fields of hearing and balance assessment. We help the professional audiologic world reach new milestones through continuous developments and a constant focus on integration and direct customer value. Interacoustics USA
10393 West 70th Street
Eden Prairie, MN 55344
T +1-800 947 6334
info@interacoustics-us.com
THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
■■ South Carolina National Guardsmen plan
U.S. ARMY NATIONAL GUARD PHOTO BY SGT. BRIAN CALHOUN, 108TH PUBLIC AFFAIRS DETACHMENT
evacuation support as a part of Hurricane Matthew response efforts. Hurricane Matthew peaked as a Category 4 hurricane in the Caribbean and was projected to pass over the Southeastern United States, including the South Carolina coast. Approximately 1,400 South Carolina National Guard soldiers and airmen were activated Oct. 4, 2016, to support coastal evacuations after Gov. Nikki Haley declared a state of emergency.
handled by other agencies. More direct basic care often is provided on an emergency basis during foreign disaster relief missions, especially in the early days. “Those are challenging environments to provide that kind of support, using first responder training. But we work with USAID’s Office of Foreign Disaster Assistance and the State Department to provide whatever we are best capable of doing, such as helicopter evacuations,” Deptula said. An area of growing concern is identifying and treating victims of some of the most virulent diseases of modern times – HIV, Ebola, Zika – and protecting U.S. responders from those plagues. That applies both to foreign emergency support efforts as well as day-to-day contact with maritime lawbreakers or those in need of rescue at sea. “We provide basic awareness and training to all Coast Guard employees and take our cue from other parts of the government, such as CDC and HHS, to have the proper level of awareness and follow their guidelines on seeking medical care if the symptoms are seen,” Deptula added. “Some of our special strike teams have responded in the past to anthrax situations and have some capability to respond in support of other viral diseases, such as Ebola, in terms of moving patients to higher level care. We are expanding our capabilities to do that on a larger scale with personal protection equipment and methods of patient transport using our boats and aircraft, but right now only have limited capability.” NATIONAL GUARD AND RESERVES
Army and Air Force Guard units, in their roles as state militias, frequently are among the earliest responders to major emergencies in their own or neighboring states (at the request of the other state’s governor). The most visible of those are forest fires, storms, earthquakes, and riots, in which they work with other local, state, and federal agencies to end the emergency, evacuate victims, and provide first-contact medical care. “The National Guard serves as a critical state resource in disaster responses and can provide much-needed
www.defensemedianetwork.com
capabilities to state governors very quickly. The majority of National Guard support in disaster responses is performed at the direction of a state governor and in a State Active Duty status as a state militia,” Robert G. Salesses, deputy assistant secretary of defense for Homeland Defense Integration and Defense Support of Civil Authorities, told a House Subcommittee on Emergency Preparedness, Response, and Communications in June 2015. More than 365,000 members of the Army, Navy, Marine Corps, and Air Force reserves, living in thousands of communities across the nation, also are on call for domestic disaster and emergency response missions. For example, the Army Reserve provides a significant portion of the Army’s disaster response effort, including mortuary affairs (75 percent), quartermaster (65 percent), medical (59 percent), transportation (44 percent), and engineer (31 percent) capabilities. DOD relies heavily on the Guard for response to a nuclear accident, attack, or terrorist “dirty bomb.” The CBRN Response Enterprise, involving almost 17,000 military personnel, currently comprises 57 National Guard Weapons of Mass Destruction Civil Support Teams, 17 National Guard CBRN Enhanced Response Force Packages, 10 National Guard Homeland Response Forces, one DCRF, and two Command and Control CBRN Response Elements. “DOD is better prepared to … assist civil authorities in the aftermath of a catastrophic incident than at any other time in our nation’s history. DOD is prepared, when directed by the president or the secretary of defense, to provide, as part of the federal government’s support of state and local emergency assistance efforts, capabilities and resources to save lives, sustain lives, and protect property and public health and safety,” Salesses told lawmakers. 47
INTRODUCING VETERANS AFFAIRS & MILITARY MEDICINE
THE YEAR IN
VETERANs AffAIRs
THE YEAR IN
VETERANS AFFAIRS
& Military Medicine
& Military Medicine
veterans’
behavioral health
ImprovIng post-Combat Care interviews:
sen. Lindsey graham, r-s.C. U.s. army vice Chief of staff gen. peter Chiarelli SPECIAL SECTION: VA Research
features:
special operations medicine
INTERVIEWS
army medical research and materiel Command
VA Secretary Robert A. McDonald VA Under Secretary for Health David J. Shulkin VHA Chief Nursing Officer Donna Gage
2009-2010 Edition
2015-2016 Edition
coverF.indd 1
10/12/09 6:22 PM
C e l e br at i ng t h e 6 0t h A n n i v e r sa ry of Vet e r a ns Day
THE YEAR IN
VETERANs AffAIRs
THE YEAR IN
VETERANs AffAIRs
& Military Medicine
& Military Medicine 2008-2009 Edition
OUTLOOK
2014-2015 Edition
THE YEAR IN
VETERANs AffAIRs
SUBSCRIBE FOR FREE AT: WWW.VAMILMEDOUTLOOK.COM/ SUBSCRIBE
NEW NAME TWICE A YEAR
THE YEAR IN
VETERANs AffAIRs
& Military Medicine
2007-2008 Edition
2013-2014 Edition
cover final.indd 1
10/30/07 3:55:49 PM
ion
rs ai e ff cin dit
3E 01
-2 12 20
a di ns Me raary e t lit Ve i AR
E
TH
IN
YE
&
M
Veterans’ Jobs Forecast
Prosthetics: A Step Ahead Global Medic 2012
THE YEAR IN
Veterans affairs
& Military Medicine 2011-2012 Edition
cover w spine
THE YEAR IN
VETERANs AffAIRs
& Military Medicine 2010-2011 Edition
SUPPORTING OUR VETERANS •
10/22/04
5:20 PM
Page 1
VETERANS SUPPORTING OUR
A 7 5 T H A N N I V E R S A R Y P U B L I C AT I O N A FA I R C O U N T P U B L I C AT I O N
FORMERLY THE YEAR IN VETERANS AFFAIRS & MILITARY MEDICINE
& Military Medicine
A 75th Anniversary Publication
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
Maj. Gen. Barbara R. Holcomb
U.S. ARMY PHOTO
Commanding General, U.S. Army Medical Research and Materiel Command and Fort Detrick, Maryland, and Chief, U.S. Army Nurse Corps
n MAJ. GEN. BARBARA R. HOLCOMB is a 1987 Distinguished Military Graduate of Seattle University Army ROTC where she earned a Bachelor of Science degree in nursing. She earned a master’s degree in nursing administration from the University of Kansas, a master’s level certification in emergency and disaster management from American Military University, and a master’s in military strategic studies from the U.S. Army War College, Carlisle, Pennsylvania. Holcomb’s military education includes the AMEDD Officer Basic Course, AMEDD Officer Advanced Course, Faculty Development Course, Combined Arms Services and Staff School, resident Command and General Staff College, AMEDD Executive Skills Course, Interagency Institute for Federal Health Care Executives, Medical Strategic Leadership Program, Army War College, Army Strategic Leader Basic, Intermediate and Advanced courses, and CAPSTONE. Her previous assignments include Clinical Staff Nurse, Post Anesthesia Care Unit and Department of Emergency Medicine, Madigan Army Medical Center; EMT Section, 47th Combat Support Hospital, Fort Lewis, Washington, and deployment to Desert Shield/Desert Storm; Staff Nurse and Clinical Head Nurse, Mixed Med/Surg Ward and Head Nurse, Troop Medical Clinic and 111th MI Brigade Family Clinic, Fort Huachuca, Arizona; Officer Basic Course Nurse Advisor, Department of Nursing Science and Commander, A/187th Medical Battalion, Fort Sam Houston, Texas; Chief Nurse, Department of Outlying Health Clinics, 67th CSH/Wuerzburg MEDDAC, Germany; Medical Detachment Commander (Provisional), Camp Able Sentry, Macedonia; Chief Nurse/XO, 14th CSH, Fort Benning, Georgia; Commander, Special Troops Battalion; Chief, Base Transformation Office, U.S. Army Garrison, Fort Sam Houston, Texas; Chief, Ambulatory Nursing, Brooke Army Medical Center; Chief, Nursing Administration, Carl R. Darnall Army Medical Center and Commander, 21st CSH, Fort Hood, Texas; Commander, Medical Task Force 21, Operations Iraqi Freedom and New Dawn; Chief, Army Nurse Corps Branch at Human Resources Command, Fort Knox, Kentucky; Commander, Landstuhl Regional Medical Center, Landstuhl, Germany; Command Surgeon, FORSCOM HQs, Fort Bragg, North Carolina; Army Action Officer for
www.defensemedianetwork.com
■■ Maj. Gen. Barbara R. Holcomb, commanding general, U.S.
Army Medical Research and Materiel Command and Fort Detrick, Maryland, and chief, U.S. Army Nurse Corps.
the Military Health System Review; Commanding General, Regional Health Command-Central (Provisional), Fort Sam Houston, Texas; and prior to becoming Commanding General, Medical Research Materiel Command and Fort Detrick, she served as the Deputy Commanding General for 53
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Operations, U.S. Army Medical Command. She was designated as Chief, Army Nurse Corps on Nov. 2, 2015. Holcomb’s awards and decorations include the Distinguished Service Medal (1OLC), Legion of Merit (2OLC), Bronze Star, Meritorious Service Medal (5OLC), Army Commendation Medal (3OLC), Army Achievement Medal (1OLC), National Defense Service Ribbon, Iraq Campaign Medal (2 campaign stars), Kosovo Campaign Medal, NATO Service Ribbon (Kosovo), Southwest Asia Service Medal (3 campaign stars), Kuwait Liberation Medal (Saudi Arabia and Kuwait), the Meritorious Unit Commendation Ribbon (1OLC), and the Expert Field Medical Badge. She is a member of the Order of Military Medical Merit.
our nurses to become completely dependent on machines and technology.
Veterans Affairs & Military Medicine Outlook: What made you want to make your career in Army Medicine? Maj. Gen. Barbara R. Holcomb: I initially had no intention of making Army Medicine a career. I worked in the Military Science Department as a clerk typist for my workstudy program. At the end of my freshman year, I realized the grants and scholarships I received for the first year didn’t cover all of the subsequent years. I applied for and received a
Is the Army still projecting a nursing shortage? How is the Army competing with civilian employers in recruiting and retaining skilled medical personnel? Overall, the Army has military nurses, civilian nurses (government employees), and contracted nurses. The Army Nurse Corps includes both active and Reserve component nurses. We have some shortages in some specific areas but not a shortage overall. Certified registered nurse anesthetists
What would remain familiar? What aspects of care endure? The need for care and compassion has not changed. The ability to use our senses – hearing, touch, smell, visual – and to communicate what we are doing and why with both the patient and the family is still keenly important. Many of the principles of healing haven’t changed; patient’s attitudes, understanding of their situation, rest, nutrition, mobility, involvement in their own care, including the family in their care, are all things that would be familiar.
■■ The need for care and compassion has not changed. The ability to use our senses – hearing, touch, smell, visual – and to communicate what we are doing and why with both the patient and the family is still keenly important. three-year ROTC nursing scholarship between my freshman and sophomore year of college. I saw it as a way to help pay for my school and I was drawn to the military customs and traditions I observed working in the department. About two years into my first assignment at Madigan Army Medical Center, in Tacoma, Washington, I was returning to my work area, having been pulled to help cover the ICU that night. The sun was coming up, the mountain was out (Mount Rainier) and I got a sense of peace and realization that I loved what I was doing and wanted to continue doing it. After that, I always said I would stay as long as I was enjoying it and felt like I could still contribute. This year marks 115 years of the Army Nurse Corps. What would most impress a nurse from more than a century ago about the nurses of today? I think understanding the levels of technology; the medications available and the ability of nurses to make decisions are all so much different today. We’ve learned so much about health, the disease process, and human responses even since I first became a nurse. I believe the collaborative teamwork we have within the military between providers, nurses, physical therapy, respiratory therapy, [and] nutrition care, among others, is probably much different. We have many more options, and the risk is that we must take care to not allow 54
(CRNA), psychiatric nurse practitioners, and OB-GYN nurses are examples of shortage areas. We use precision recruiting to focus on those specific areas and have some recruiting and retention tools that are very effective in filling active-duty vacancies. Our civilian workforce is on average 49 years old, so we will see nurses retire in the near future who have been in our military health care system for many years. We are challenged to compete with the [Department of Veterans Affairs] as it typically pays a higher salary rate. Some areas of the country are easier to hire than others. It requires a continuous effort to ensure we have the right skill mix and staff numbers on hand. We balance our military nurses with our civilians and contractors to ensure appropriate staffing, but more importantly to ensure our military nursing staff has the ability to maintain their skills to provide care in a deployed, austere environment. Every day is an opportunity to hone our skills as we care for patients and their families. For many, the reward of caring for America’s sons and daughters, the opportunities to grow professionally, and the ability to make a difference is enough to retain our nurses. What kinds of opportunities for continuing education and advancement in their field do Army nurses have today?
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Soldiers display the various uniforms of Army nurses from World War II through the modern era during the Army Nurse Corps 115th
U.S. ARMY PHOTO BY MARCY SANCHEZ
anniversary celebration at William Beaumont Army Medical Center, El Paso, Texas, Feb. 2, 2016. On Feb. 2, 1901, Congress established the Army Nurse Corps as a professional element of nursing professionals within U.S. Army Medicine with the Army Reorganization Act of 1901. While technology has advanced and medical knowledge has increased in the 115 years since the Army Nurse Corps was established, “The need for care and compassion has not changed,” Holcomb noted.
Army nurses have many opportunities to advance and grow throughout their time in the military. All Army nurses come into the Army with a Bachelor of Science in nursing. A new nurse, usually a second lieutenant, will start out by being a staff nurse and within 18 months to two years can advance to be a team leader on their shift, precepting other nurses and teaching their newer staff members. They can select a specialty area, such as the ICU, ER, OB-GYN, psychiatry, public health, or operating room, and attend a 12- to 16-week course that teaches the skills of that specialty. They can also obtain a master’s degree in a variety of areas such as administration, informatics, education, or as a clinical nurse specialist, or a doctorate in nursing practice (DNP) and become an advanced practice nurse in
www.defensemedianetwork.com
anesthesia, psychiatric nurse practitioner, family nurse practitioner, or a nurse midwife. They can also become a nurse scientist by earning a PhD. These opportunities are part of the Long Term Health Education and Training program where the military pays for the education and the officer incurs an obligation to stay in the military. There are many other leadership opportunities throughout their career that include becoming the clinical nurse officer in charge (CNOIC), supervisor of an inpatient section, deputy commander for inpatient services, chief nursing officer, all within a hospital setting. Outside the hospital, there are opportunities to work directly with our soldiers in brigade combat teams, work in our forward surgical teams and Combat Support Hospitals in field environments and deployed settings, or to support combat operations, natural 55
NEW TO YOUR DoD TREATMENT FACILITY
ella® AND EContra® EZ, TWO EMERGENCY CONTRACEPTIVE OPTIONS Now available on the FSS ®
ulipristal acetate tablet 30 mg www.ellanow.com/hcp.html
Rx Required
• The only FDA-approved oral emergency contraceptive for use up to five days after unprotected sex or a known contraceptive failure.1,2 • The first and only oral emergency contraceptive that has been shown to delay ovulation when luteinizing hormone (LH) is still rising.3,4
ORDER TODAY MCKESSON NDC# 50102-911-01
ORDER#
3470556
Now available on DAPA • The cost-saving alternative to Plan B One-Step.® • Afaxys®’ first over-the-counter emergency contraceptive, effective for up to three days after unprotected sex or a known contraceptive failure.
(Levonorgestrel) Tablet, 1.5 mg
www.econtraez.com/hcp.php
OTC
ORDER TODAY CARDINAL NDC# 50102-111-12 ABC NDC# 50102-111-12
ORDER#
5062591
ORDER#
10157388
For more information, visit afaxys.com/DOD
The Experts in Emergency Contraception IMPORTANT SAFETY INFORMATION FOR ella ® ella® Important Safety Information5 The most common side effects of ella (ulipristal acetate) tablets include headache (18%), abdominal pain (12%), nausea (12%), dysmenorrhea (9%), fatigue (6%), and dizziness (5%). ella is contraindicated in women with a known or suspected pregnancy, and should not replace a regular method of contraception. ella is not indicated for termination of an existing pregnancy. Women who become pregnant or complain of lower abdominal pain after taking ella should be evaluated for ectopic pregnancy. ella may alter the next expected menses. If menses is delayed beyond 1 week, pregnancy should be ruled out. ella is not recommended for use in breastfeeding women. A rapid return of fertility is likely following treatment with ella; therefore, a reliable barrier method of contraception should be used with subsequent acts of intercourse in that same menstrual cycle. Because ella and the progestin component of hormonal contraceptives both bind to the progesterone receptor, using them together could reduce their contraceptive effectiveness. After using ella, if a woman wishes to use hormonal contraception, she should do so no sooner than 5 days after intake of ella. Repeated use of ella within the same menstrual cycle is not recommended. Drugs or herbal products that induce CYP3A4 decrease the effectiveness of ella. ella does not protect against sexually transmitted infection (STI) or human immunodeficiency virus (HIV). References: 1. Glasier A, Cameron S, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomized non-inferiority trial and meta analysis. The Lancet Lancet. 2010; 375: 555–562. 2. Moreau C, Trussel J. Results from pooled Phase III studies of ulipristal acetate for emergency contraception. Contraception. 2012; 86: 673–680. 3. Brache V, Cochon L, et al. Immediate pre-ovulatory administration of 30 mg ulipristal acetate significantly delays follicular rupture. Human Reproduction. 2010; 25: 2256–2263. 4. Gemzell-Danielsson K, Berger C, Lalitkumar PGL. Emergency contraception – mechanisms of action. Contraception. 2012; 87: 300–308. 5. ella® prescribing information. Charleston, SC: Afaxys, Inc. 2015 © 2016 Afaxys, Inc. Charleston, SC. All rights reserved. APH-154-0816 August 2016
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
disasters, or humanitarian missions. There are also opportunities to work as a staff officer, in recruiting, as an ROTC nurse counselor, as a commander, or in other nontraditional nursing roles such as a congressional liaison or on the Army staff. You served in a Combat Support Hospital during Operation Desert Storm, and then later commanded one in Iraq in 2010. How different was your experience and what perspective did you gain? Both experiences were very rewarding, both personally and professionally, but very different from each other. During Desert Shield/Desert Storm, we had no idea how long we’d be deployed. We spent most of our time in locations that had no base support, so we provided our own security, established our own life support areas, and ate a lot of MREs and T-rations. We lived in GP Medium tents, with a cot and sleeping bag. We took the MUST hospital (Medical Unit, Self-contained, Transportable) with us and while in the Saudi Arabian desert, we were issued and trained on the DEPMEDS (Deployable Medical System) hospital. We arrived in October and provided care for soldiers injured in training, illnesses, and accidents. Communication was very limited. We drove three hours to a phone bank and were allowed 15 minutes to make phone calls once in the first three months. We wrote letters home and it was weeks before receiving mail back. In March, we joined a 604-vehicle convoy into Iraq, driving for two and a half days in the back of 5-ton trucks. We set up our hospital (47th Combat Support Hospital) during the night and the next day received casualties, most of whom were Iraqi soldiers and civilians. Many of them had received injuries two to three days prior. The experience was a test of resilience, tolerance, and stamina. The biggest challenge was in not knowing what was happening in theater or how long we’d be there. In 2010, we deployed the 21st Combat Support Hospital to Iraq, to a known location for a known length of time. We covered three separate locations, but were on established bases with many of the comforts of home: indoor plumbing, showers, containerized housing with beds and well-stocked dining facilities. I could Skype every night with my husband. Our hospitals were mostly in hardened buildings, although with the drawdown to Operation New Dawn, we moved out of one fixed location back into DEPMEDS so we could transfer the fixed location over to the Iraqi air force. The medical equipment was more modern and we had ready access to medical supplies and medical evacuation. As the commander, I had a very good understanding of the situation on the ground. The biggest challenge was making good decisions that were right for each location and the constant worry about getting everyone home safely. How much of an effect have modern technologies in body armor had on combat casualty care as well as long-term care?
www.defensemedianetwork.com
■■ It’s easy to prepare for the injuries and illnesses from the last war, but we rarely fight the same war twice. There are many diseases we had not expected, Ebola and Zika for example, and some we haven’t yet discovered. Each corner of the world has something different that we may or may not know about or for which we do not have protective measures in place. The use of body armor during the recent conflicts is a very significant contributor to the high survival rate of injured warfighters, including those who suffer from mild traumatic brain injury (mTBI). Despite an increase in the severity of injuries suffered by our service members in Iraq and Afghanistan, because of modern body armor’s ability to protect against penetrating wounds, we’ve seen a sharp decrease in the fatality rate. In addition, the modern combat helmet helps protect against penetrating injuries and provides some protection against impact. Adding to this protection, sensors have been included in the helmet and body armor to act as additional indicators for exposure to potentially concussive events and risk for TBI. These sensors can assist medical personnel in the assessment and analysis of concussive events allowing for diagnostic support and better treatment in the critical early period after the event. What are some of the key technologies, such as hemostatic agents, that have affected military medicine? The injuries sustained by warfighters today are often severe, destructive, and complex, and can affect the service member for the rest of their lives. For example, a blast injury from an IED [improvised explosive device] can lead to multiple injuries, including burns, amputations, nerve damage, and TBI. Some of the latest technologies influencing military medicine come from lessons learned in past wars with, of course, an eye on the future of combat operations. We have been working on several exciting new technologies. Of particular note is the development of junctional tourniquets, which are focal pressure tourniquet devices used to stop blood flow by compressing blood vessels at – or proximal to – a junctional injury. We’re talking about injuries such as pelvic fractures and high leg injuries; injuries that are commonly caused by improvised explosive device blasts, and that can result in massive hemorrhage if not addressed immediately. The SAM® junctional tourniquet was cleared for use by the U.S. Food and Drug Administration in 2013 for groin area use. It was also later cleared for use in the armpit area and for pelvic binding as well. The Combat Ready Clamp (CRoC®) is another 57
CorMatrix® Extracellular Matrix (ECM®) CorMatrix devices have been implanted in over 145,000 procedures including vascular repairs and cardiac device envelopes CorMatrix CanGaroo®
The CorMatrix CanGaroo device envelope secures cardiac implantable electronic devices and promotes a healthy, neo-vascularized tissue pocket.
CorMatrix Vascular Repair is a non-synthetic, natural material that remodels into healthy, functional tissue. CorMatrix ECM for Vascular Repair
CorMatrix has partnered with LGS [SDVOSB] to make these and other implantable devices available to the Veterans Health Administration. Contact Chris Lovell at 850.684.1867 or email: chris@lovellgov.com.
Veterans Administration Supply Schedule (FSS): #V797D-50450 General Services Administration (GSA): #V797D-50450 Defense Logistics Agnecy (DLA): #SP0200-16-H-0011 MK-1260-01/Rev.A ©2016 CorMatrix Cardiovascular, Inc. All rights reserved.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
U.S. ARMY PHOTO BY SPC. CAITLYN BYRNE, 27TH PUBLIC AFFAIRS DETACHMENT
■■ An Army lab reconnaissance team for Joint Forces CommandUnited Assistance, comprising members of the Centers for Disease Control and Prevention, U.S. soldiers, and members of the Armed Forces of Liberia, walk down the flight line at the Roberts International Airport, Monrovia, Liberia, Dec. 4, 2014, on their way to survey and assess potential sites for a new Army medical laboratory in Greenville, Sinoe County, Liberia. Carefully developed and rigorously implemented Force Health Protection guidelines that help ensure troop readiness translated into a very small number of service members presenting with malaria symptoms during Operation United Assistance.
type of junctional tourniquet, which differs from the others in that it has a vise-like compression disk that creates direct bilateral pressure in any chosen spot. Ultimately, this helps stop blood flow and thereby stops massive bleeding that might otherwise claim a life. What’s particularly exciting about the CRoC is it can be assembled and applied in less than a minute. In the realm of hemostatic dressings, a variety of hemostatic agents have been incorporated into gauze and bandage products to aid in hemorrhage management. These products include the HemCon® Bandage and QuikClot Combat Gauze®. The use of products such as these is important, given that hemorrhage accounts for 50 percent of all combat fatalities. In conjunction with direct pressure, hemostatic dressings have proven invaluable for treating severe hemorrhage in soldiers injured during operations in Iraq and Afghanistan. The next technology is the resuscitative endovascular balloon occlusion of the aorta – or REBOA – which is a technique that stops severe bleeding in trauma patients by deploying a flexible, balloon-tipped catheter up through the femoral artery and into the aorta before it is ultimately inflated. This method stops blood flow beyond the balloon, but also to the lower part of the body. As such, REBOA use is only temporary, and is used as a bridge to get the severely injured patient to more definitive care. To be clear, the REBOA is not yet available for general-use situations, but rather only in certain special operations settings. Another example is the Miniature Field Deployable System for Rapid TBI Assessment, and it serves as a portable electroencephalography [EEG] device. It quantifies and analyzes the brain’s electrical activity patterns unique to traumatic brain injuries. This in turn aids in the early, rapid, effective, and objective assessment of TBI severity and also helps determine the need for possible medical imaging. One such device, the Ahead ® 100, which received clearance from the Food and Drug Administration in November 2014, is a headbandshaped device that measures a patient’s EEG signals, or brain electrical activity. The results are then interpreted by a clinician for diagnosis. How has Force Health Protection (FHP) changed medical care during your career? Focus on Force Health Protection has always been essential in preventing illness and injuries that jeopardize
www.defensemedianetwork.com
missions. With the recent emphasis that the secretary of defense and the chief of staff of the Army have placed on troop readiness, FHP has taken on greater importance. As a result, we’re seeing our armed forces in a higher state of medical readiness and suffering from fewer illnesses that compromise our service members’ ability to complete their missions. Take malaria prevention, as an example. In 2003, 225 Marines deployed to Liberia. Within a month, about 20 percent of the Marines were evacuated due to malaria. Contrast this with Operation United Assistance in 2014-2015. Over 2,500 service members deployed to West Africa in support of the U.S. response to the Ebola outbreak, and yet only five service members presented with malaria symptoms. Carefully developed FHP guidelines and rigorous oversight of their implementation resulted in a nearly complete prevention of malarial infection, which in turn resulted in greater mission effectiveness. How much has jointness come into play over the years within military medicine? The Army is more active, mobile, and geographically dispersed than we have been in the past, and more likely to work in joint operations or partnerships with other governmental agencies and nations. We’ve found that working in joint environments at the tactical and operational level helps to advance collaboration, leading to innovative medical research and development to improve military community health and save lives on and off the battlefield. Most of our graduate medical education programs and advanced practice nursing programs are open to all services and it’s very common to work with medical personnel from our sister services. The Base Realignment and Closure 59
Don’t miss upcoming editions of
Sign up or update your information to assure your continued complimentary subscription and delivery.
It’s easy, just go to
www.VAMilMedOutlook.com/subscribe
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Maj. Gen. Barbara R. Holcomb assumes command of the U.S. Army Medical Research and Materiel Command and Fort Detrick from Maj.
PHOTO BY MELISSA MYERS, USAMRMC PUBLIC AFFAIRS
Gen. Brian C. Lein in an outdoor ceremony on Fort Detrick’s Blue and Gray Field, July 28, 2016.
(BRAC) initiative in 2005 directed that all enlisted medical training for the Army, Navy, and Air Force be conducted at Fort Sam Houston, Texas. While there are some unique requirements for each service on their warfighting platforms, the basic medical knowledge and skills are very similar and we continue to work toward collaboration in our training environment. One of the best examples of jointness, from my perspective, was my experience as the commander of Landstuhl Regional Medical Center (LRMC) in 2012. While it is an Army command, we had large numbers of Air Force and Navy staff members, and even some Marines. Everyone worked together and focused on the mission of taking care of casualties flown in from Iraq and Afghanistan as well as the military beneficiaries in Europe. When you walked into a ward, with everyone in scrubs, you could not tell who was in which service, except by the color of their T-shirt, and it didn’t matter to patients. We continue to work toward that same sense of team and camaraderie in several of our other large medical facilities where we have multiple services providing patient care.
www.defensemedianetwork.com
What do you see as the greatest future challenges for protecting and ensuring the health and welfare of soldiers? Preparing for the unknown is always the biggest challenge. We live in a volatile, uncertain, chaotic, and ambiguous environment. It’s easy to prepare for the injuries and illnesses from the last war, but we rarely fight the same war twice. There are many diseases we had not expected, Ebola and Zika for example, and some we haven’t yet discovered. Each corner of the world has something different that we may or may not know about or for which we do not have protective measures in place. There are weapon technologies that continue to evolve, so we have to understand the effects on the human body and brain of those technologies. Some of the most exciting things about the Medical Research and Materiel Command are the scientific research efforts being done to develop vaccines, laboratory testing procedures, and other physical protective measures in anticipation of the unknowns. We also have to continue to refine existing measures to meet the changing technologies and environments in which our service members fight and serve. 61
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Developments in Army Medical Imaging By Scott R. Gourley
62
(CT); magnetic resonance imaging (MRI); and digital breast imaging. COMPUTER TOMOGRAPHY
One of the significant imaging enhancements over the last few years has been the movement of “CT scan” technology “further forward” in tactical Army operations. “We have placed CTs in Level III hospitals in theater, which is the Combat Surgical Hospital [CSH],” Moaveni said. “At that level, the CT is used to do things like help remove any foreign objects out of the body or to identify bleeding.” Moaveni observed that the initial deployment of CTs to these tactical settings was driven in part by the anticipation of “imminent conflict” early in the first decade of the 21st century. “Initially, MEDCOM [U.S. Army Medical Command] had invested in some old CTs – version one,” he said. “And when the need for a better CT was identified, we were tasked with upgrading those units. Our initial concern was to find a CT that not only is superior to what we had but also is more rugged. Because you’re talking about multiple computers and a 2-ton wheel rotating around an axis with a 300-pound X-ray tube sitting on it. To take that piece of equipment and haul it 6,000 miles and drop it into the theater meant that we went through learning pains in regards to ruggedizing these machines. “So we did a lot of hard work behind the scenes to make sure that what we put out there would survive,” he added. “It was the first time. There were a lot of unknowns. And we did suffer some setbacks. But, because of the fact that our base was strong, and we had done our calculations and homework, we were rapidly able to overcome the setbacks in theater.” Those early machines, now approximately a dozen years old, are also candidates for technology upgrade.
www.defensemedianetwork.com
PHOTO BY JOHN BROOKS, U.S. ARMY
n U.S. ARMY MEDICAL CARE IS AN INCREDIBLY dynamic environment, replete with the acquisition and fielding of new capabilities in parallel with the upgrade and enhancement of existing systems. One of the critical players in this process is the U.S. Army Medical Materiel Agency (USAMMA). Headquartered at Fort Detrick, Maryland, USAMMA has the mission “To develop, tailor, deliver, and sustain medical materiel capabilities and data in order to build and enable health readiness.” A leading participant in fulfillment of USAMMA’s mission is the Integrated Clinical Systems (ICS) Project Management Office, which executes a patient-centric, “system of systems” approach to ensure timely delivery of affordable, sustainable, interoperable, and information assurance compliant capabilities in support of clinical requirements for fixed and deployed military treatment facilities. Specific office responsibilities include managing picture archiving and communication systems (PACS), imaging, and teleradiology program initiatives; executing the Technology Assessment and Requirements Analysis program; and managing information assurance requirements for designated medical devices. The medical imaging arena provides several representative examples of how USAMMA is working to acquire and field optimized diagnostic tools for service members and their families. Additionally, these Army efforts also serve to provide a glimpse of similar medical materiel activities taking place across the armed services. According to Siamack Moaveni, USAMMA senior biomedical engineer in the ICS Project Management Office, Army patients are the beneficiaries of a number of imaging enhancements that have been introduced over the past several years. Moreover, many of those capabilities are currently undergoing continuing upgrades or new enhancements designed to further improve medical outcomes. Moaveni pointed to representative medical imaging enhancements in three areas: computer tomography
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ General Leonard Wood Army Community Hospital (GLWACH) hosted an unveiling to celebrate the acquisition of a new CT scanning system,
which is the most sophisticated CT scanner in Army Medicine. Pictured left to right are USAMMA’s Product Manager for Clinical Technologies Jimmy Bisenieks; GLWACH Commander Col. (Dr.) Peter Nielsen; USAMMA senior biomedical engineer Mack Moaveni; and GLWACH’s Chief of Radiology Lt. Col. (Dr.) Shahin Nassirkhani.
“Luckily, this time we believe we have some time,” he stated. “So we’re going to take our time to make sure that the next generation of CTs going to the theater are going to be superior to what we had – and, by the way, what we had is still state of the art for some settings.” Moaveni said that one of the most recent advances in CT scan technology is a program dubbed Computed Tomography Radiation Dose Reduction Software. “It’s not just software,” he explained. “It’s a combination of software and hardware. Computer tomography, which is a CT scanner, is a diagnostic tool that generates X-rays. And X-rays are ionizing radiation. That means that they can cause cancer in your body if you have prolonged exposure to them. That prolonged exposure can also burn your skin or your anatomy.” He continued, “Because of the fact that the CT is a trauma tool, it is used at times when there are a lot of
www.defensemedianetwork.com
unknowns within the patient’s body – shrapnel, foreign objects, things that are not supposed to be there. And they don’t know how deep these objects are within the body. While traditional X-ray can reveal these objects, it doesn’t give any information with regard to their location. However, the CT scanner, because of the fact that it is a three-dimensional image, can pinpoint exactly how deep the objects are within the body. “CT is a very common ‘go-to’ tool that all radiologists and all clinicians would like to use,” he added. “But when this becomes a chronic thing as far as exposure to ionizing radiation, then they have to do something with regard to somehow reducing the amount of radiation for the patient.” However, in most situations, higher radiation levels were used to provide the clearest possible pictures of the patient’s anatomy or injury. Moaveni said that the key to providing 63
World Leading Medical Imaging Solutions • Radiology • Surgery • Hybrid OR
Accurate Medical Imaging for the Digital Era
With over 45 years developing and manufacturing innovative display solutions designed for mission critical applications, EIZO is one of the leading healthcare brands worldwide.
(800) 800-5202 | (562) 431-5011
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ The Army’s new CT scanning system’s Single Energy Metal Artifact Reduction algorithm capability reduces metal streak artifact (shown in
PHOTO BY JOHN BROOKS, U.S. ARMY
the left image, corrected on the right) increasingly seen in patients with prosthetic devices.
clear images at lower radiation levels was the “removal of noise” from the CT image. “In order to remove the noise, they had to go into elaborate mathematical calculations and devise new algorithms,” he said. “And at the same time, they had to correlate the use of those algorithms with the reduction of the voltage of the CT scanners to make sure that the pictures are clear at the same time that the dosages are reduced. There is a relationship between reducing the dose, reducing the X-ray, and getting a clear picture. The concepts work together in something called the dose reduction solution to make sure that the patient doesn’t receive too much dose, and at the same time the radiologists have a clear image to diagnose from.” He said that the Army began to buy the first noisereduction solutions “around 2006,” but quickly added, “However, because of the fact that we have 30 to 40 of these systems, and we couldn’t replace all of them at the same time, we decided to negotiate with the vendors to see if they could implement that solution as an upgrade to our old systems. Some were capable of that. Some were not. That was because of the age of the CTs. Those that they couldn’t upgrade was because … that version of the CT platform was too old. However, some we were able to upgrade. And within perhaps a year we replaced those that were too old with a new platform that had the dose reduction capability.
www.defensemedianetwork.com
“Of course, during 2006-2007, when we did this, the dose reduction solution was anywhere between 15 to 35 percent [reduction]. Today, dose reduction for the CT is close to 85 to 90 percent, which is just like an X-ray, instead of the traditional CT. And we are trying every day to align ourselves to take advantage of these large dose reduction technologies,” he said. Recently the Army also began fielding some of the world’s most advanced new CT technology at Brooke Army Medical Center (Fort Sam Houston, Texas) and General Leonard Wood Army Community Hospital (Fort Leonard Wood, Missouri). “Those CTs can image the heart in one rotation,” Moaveni stated. “That means the X-ray machine doesn’t have to stay on for a long amount of time to overexpose the patient.” Said another way, the new CT systems are able to produce a 3-D image of the entire heart in less than one heartbeat. The new design uses a wider detector that allows the system to capture complete images of organs, such as the heart, in one scan rather than multiple scans that have to be “stitched together” electronically. “Dose reduction consists of three parts,” Moaveni summarized. “The first is the software algorithms that control how the data is captured from the detectors and processed. Second, it has the capability of communicating with the hardware in the X-ray, including the generator’s release of the voltage. The third part is timing. We have found out that the wider the 65
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ An “injured” soldier is prepared by providers with the Kandahar Airfield Role 3 Hospital to receive a magnetic resonance imagery (MRI)
scan during a mass casualty exercise Feb. 14, 2014. Recent advances in MRI involving magnet coil strength have decreased the amount of time it takes to image the anatomy.
MAGNETIC RESONANCE IMAGING
Another critical imaging technology is magnetic resonance imaging (MRI). Although not used for trauma cases, MRI is an exceptional tool for soft tissue diagnostics. Moaveni said that recent MRI advances have focused on increases in the magnet coil strength. “We have magnets that have field strengths up to 15 tesla and we have magnets with field strength of .2 tesla,” he began. “But the standard today is a 1.5 tesla MRI. However, while the 1.5 tesla MRI could be adequate for imaging the abdomen, the liver, the lungs, muscles, joints, and cartilage, it takes time for imaging neurons, for the brain, to a point where radiologists can see the minute connections between the different centers of the brain. “They found out that when they doubled the strength of the magnet – to go from 1.5 to 3 tesla – the speed of the images improved. Previously a patient had to stay in a 1.5 tesla MRI for 45 minutes to get their liver imaged and they had to stay for about two hours to get the neurons imaged in their head. But with the 3 tesla MRI, this time was decreased,” he said. 66
“So that’s what’s behind the increase of field strength from 1.5 to 3 tesla,” he added. “However, as I said, we have magnets that operate on .2, which can image a liver in about three hours. And we have magnets that are 15 tesla, but it’s usually used for research. It’s very targeted – in case they want to see a certain part of the anatomy. But it’s not good for routine imaging.” DIGITAL BREAST IMAGING
While changing military demographics might lead some to expect an increased need for breast imaging, Moaveni said that the actual number of breast imaging locations has remained fairly constant. However, he quickly added that the recent introduction of new digital breast imaging technologies has expanded patient opportunities by decreasing the time required for imaging. “We introduced digital mammography in the Army a little later than the rest of the world,” he acknowledged, “because we wanted to make sure that the digital machines were ready for our patients. In the past, the older, traditional film screen had an infinite number of elements or pixels. By contrast, digital screens have a finite number. It’s a lot. But it’s also a lot less than the film screen. So, when the number of detector
www.defensemedianetwork.com
U.S. ARMY PHOTO BY CAPT. ANDREW COCHRAN
detector, the less dose to the patient. So the advancements in CT dose reduction since 2006 have been tremendous.”
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ U.S. Air Force Tech. Sgt. Lakiesha Toney, assistant NCO-in-charge, Breast Imaging, examines an image taken with digital equipment in the
Wilford Hall Medical Center Mammography Clinic, Feb. 18, 2010. Though the Army embraced digital mammography later than the Air Force and others – opting to delay slightly its adoption of digital breast imaging to ensure the technology could match traditional mammography capabilities – it has employed digital imaging for the past five years.
U.S. AIR FORCE PHOTO BY SENIOR AIRMAN JOSIE KEMP
elements decreased, your image quality decreased. And we wanted to keep the mammogram as sharp as possible. But now that digital mammography is at the point where it is very, very clear, we have employed digital mammography for the past five years.” He said that another advantage of the digital technology involved “tomography.” “That allows for a 3-D image of a discovered tumor,” he offered. “In the past, the traditional mammogram machine took one or two pictures that the radiologist studied. But now, with tomosynthesis capability, the mammography machine takes as many as 20 pictures from different angles. So when the computer looks at these images, it can construct a 3-D image that gives the radiologist a better sense of the size and shape of the possible tumor.” SUPPORTING TECHNOLOGIES
Along with these representative technology efforts, USAMMA representatives are also involved in a range of supporting imagery projects. As one example, several radiology PACS have been purchased and fielded over the past two years throughout the former Southern and Western Regional Health Commands. Fielding to the Northern region is currently in progress (estimated completion by January 2017). Each new system
www.defensemedianetwork.com
enhances radiologist performance, provides new advanced 3-D imaging capabilities, and helps to streamline workflow. In another example, the joint Army/Navy Enterprise Clinical Imaging Archive (ECIA) has gone live in two Defense Health Agency data centers and represents the first federated long-term radiology imaging archive. The archive consolidates seven-plus antiquated archives into two primary locations, federates Army and Navy radiology images, and will tie into the forthcoming Cerner® Electronic Medical Record. Ultimately, this makes historical images more accessible to providers to help expedite diagnosis times. Looking toward the future, Moaveni anticipates that imaging technologies will increasingly integrate spectroscopy technology. “Spectroscopy is a type of imaging that not only shows you the shape of the object but also the material that it’s made of,” he said. “For example, right now the CTs, by having dual energy, can determine if a deposit at your joint is calcium or uric acid. It uses the spectrum of shades of gray to determine the material. And I think pretty soon … we’re going to be able to distinguish between a lot of other materials as well. “So it’s going towards a comprehensive way of diagnosis,” he concluded. “And I suspect it will be different from what we look at in radiology today.” 67
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
AMSUS: Tying Together the Military Health System and Others By J.R. Wilson
n FOUNDED IN 1891 AND CHARTERED BY CONGRESS in 1903 as the Association of Military Surgeons of the United States, AMSUS later retained the acronym but officially renamed the organization The Society of Federal Health Professionals to reflect its wider reach and concerns in the 20th century. Although 2016 marks the 125th anniversary of AMSUS as a permanent organization, its unofficial roots can be traced back to 1863 and formation of the Confederate Association of Army and Navy Surgeons. Both groups shared a common concern: how to retain and disseminate the medical knowledge and lessons learned in combat both during and between wars, as was the case in 1891, and help facilitate and spread dramatic changes and advances – medical, technical, operational, and philosophical. An organization like AMSUS had to be created to document and preserve the perishable medical knowledge gained in war as well as in natural disasters and epidemics. “There was a need to gather and maintain some of the lessons learned from previous wars on how to treat battlefield injuries so we don’t have to learn the same lessons over and over again,” said Cmdr. John Class, USN (Ret.), AMSUS deputy executive director and a former Medical Service Corps health care administrator. “Because of the time frame [between wars], a lot of the physicians involved in previous combat care were retiring or dying and that knowledge base was getting lost. And once you lose those with experience, then the next generation of physicians has to learn the same lessons all over again.” From the beginning, AMSUS was set apart from other medical organizations by taking no advocacy role on any of those topics, but providing U.S. federal health care providers – both military and civilian – medical and pharmaceutical companies, state emergency health care providers, and, more recently, the international military medicine community with open forums to report new discoveries, discuss changes in emergency medicine, and exchange ideas and information. “We’re more platform than activist,” Class said. “I don’t think there is any other medical meeting that brings all these agencies together in one place or a journal that has all the 68
different disciplines and agencies and partnerships together in one place. Through our annual meeting and the journal, we provide others the opportunity to gather and share information. “For instance, in Military Medicine, we publish a lot of supplemental issues on specific topics, such as women in combat. It’s a place where you have a number of different DOD [Department of Defense] and VA [Department of Veterans Affairs] authors of different articles and studies compiled in one place, making their own recommendations that both DOD and the VA can use to determine future issues and where they are going.” At the same time as its founding, AMSUS began publishing the monthly Military Medicine journal and holding an Annual Continuing Education Meeting, both designed to build a new system of medical networks and provide forums for interservice and interdisciplinary exchanges, free from competitive or organizational “stovepipe” restrictions. Its members and beneficiaries of these efforts include DOD, the VA, and the U.S. Public Health Service (PHS). “We are a historical vessel, helping keep alive the traditions of the military. We support them through our awards ceremonies; we support fellowship between federal agencies that not only increases the satisfaction of being a health care professional, but I believe helps smooth the operations of organizations with others by providing professional social relationships in an environment where they are not separated by competition,” said AMSUS Executive Director and former Navy Surgeon General Vice Adm. Michael Cowan. “We help advance the knowledge of military medicine – and the realm we advance is readiness, which is totally unique in the federal environment. And, finally, but very importantly, we are the most prestigious recognizer of excellence. The AMSUS awards are the only accredited, recognized awards in military medicine.” In 1953, AMSUS assisted in the creation of the Sustaining Members (SM), comprising private-sector companies doing business with components of federal health. Representatives from the approximately 100 SM companies meet quarterly to interact with and learn from federal officials – and
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
SPECIAL ISSUE
■■ LEFT AND BELOW LEFT: AMSUS’ Military Medicine journal is peerreviewed and indexed, and has been published continually for 125 years.
International Journal of AMSUS
GUEST EDITORS
Patricia A. Deuster Stephanie J. Van Arsdale Bradley C. Nindl
ALL IMAGES COURTESY OF AMSUS
SPECIAL ISSUE - MAY 2016 Supplement to Military Medicine Volume 181, Number 5
www.defensemedianetwork.com
JANUARY 2016
SUPPLEMENT TO VOL 181, NO 1
each other – on topics of interest to their industries. Those include management consultants, pharma, and manufacturers of both durable and disposable medical goods. “We have almost no history on how that started. The evidence indicates that somehow people got together from industry – pharma, manufacturing, consumable and durable medical goods, etc. – and said they wanted to meet from time to time as an industry to develop networks, relationships, and mutual understanding,” Cowan said. “They wanted acquisition and policy officials and leaders of military service medical elements [to] meet with them – not to try to sell anything to them but to exchange information. They needed a 501(c)(3) umbrella, so AMSUS became that for them – about 100 companies, mostly sales execs, who meet on a quarterly basis under the sanction of AMSUS.” SM is not part of the Annual Continuing Education Meeting program and only a few AMSUS staff attend their meetings. However, SM companies get first shot at exhibit booths at the AMSUS meetings. Very few SM personnel would be eligible for AMSUS membership, which requires having served as a medical professional in a federal medical department. To be part of SM, companies have to be voted in by the existing members. “We think AMSUS provides a service to our target audience – the military – who have so many ethical and regulatory restrictions that make it difficult to deal with their partners in the industry sector. So, once again, we provide a platform for them to come together, so long as they are not buying or selling. And we think that is a tremendous benefit to the government. So do the companies involved,” Cowan added. The importance of industry to medical research and development requires strong communications with those who know the needs of military and federal medical services. “Otherwise, industry doesn’t know where to put their R&D. So in recent years, a partnership between the agencies and industry has grown so they can use scarce dollars the best way they can, giving each group an understanding of their operations,” Class explained. “They represent all areas of industry, medical equipment and supplies, medical consulting, direct patient care, insurance, etc., so you have all elements of health care represented, working toward the overall goal of helping care for the patients. “When the SM meets and talks to different agencies, they’re not there to sell a product but to make sure the process of getting their products out there is beneficial to everyone and satisfies each requirement. Sometimes government will say they have to put some rule in place, not realizing that would make it impossible for industry to provide a solution. So that 69
Proud to serve the people who serve.
3M Infection Prevention Solutions
3M Critical and Chronic Care Solutions
Whatever your role in helping prevent hospital acquired infections in your facility, we’re here to help you influence lasting change, with the goal of reducing the HAI rate to zero. You battle HAI risks in the OR, ICU, waiting room and everywhere in between. We offer the broadest array of solutions in the fight against hospital acquired infections.
Proven, innovative 3M solutions that help prevent and treat critical and chronic conditions across the care continuum. Whether you’re a patient or helping to care for one, critical and chronic care conditions can be tricky to manage. We’ll help you simplify it. Our extensive line of trusted products helps simplify and improve skin health and the treatment of wounds, both acute and chronic.
To learn more about these and other solutions from 3M Health Care, contact the 3M Health Care Helpline at 1-800-228-3957, or visit www.3m.com/healthcare ©3M 2016 2015 All AllRights RightsReserved. Reserved.3M 3Misisaatrademark trademarkof of3M 3MCompany Company. ©3M
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A professional panel discussion at the AMSUS Annual Continuing Education Meeting. The annual meeting is a unique and important
gathering for federal health professionals.
exchange really makes that group click, helping each other bring out all these points. “Things change in government all the time. The health care industry is always dealing with change, not only government rules and regulations, but technology changes in health care itself. Sometimes government is a little slower at adopting new developments than private health care. So there will always be a place for the SM to help deal with that constant change through communication between industry and government.” For example, an AMSUS meeting might include a four-hour discussion, attended by senior leadership from DOD, VA, PHS, and all the military services, on high-reliability organizations. “This is a cultural change to how hospitals are run right now, but is necessary to drive the error rates out of the practice of medicine. So to take military health care to the next level, including VA and PHS, they come to AMSUS to have a major interagency discussion, at both the worker and policymaker levels, about high-reliability organization,” Cowan said.
www.defensemedianetwork.com
“These topics also are published in Military Medicine, so the dialogue and culturalization of new ideas, such as amputation over saving a partially functional leg, is facilitated. If you want someone to understand something, tell them seven different ways seven different times. So we are one of the ways, a very important one, that allows progress.” Another operation that has benefitted from AMSUS as a platform for information exchange and discussion is the Military Health System (MHS) strategic planning process. MHS 2020 engaged national and international health care experts to envision the practice and delivery of health care in the year 2020. The health futures group’s mission was to synthesize future health care directions and integrate military health functions, ranging from individual fitness to war zone operations, including IT and electronic health records. “Again, we provide a platform for information to be gathered in one place and easily accessed. When you look at some of the benefits of our membership, we’re one of the only organizations out there that is going to provide appropriate information, education, repositories applicable to a number of 71
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ The show floor at a recent AMSUS Annual Continuing Education Meeting, an important forum where federal health care professionals, medical and pharmaceutical companies, state emergency health care providers, and international military medicine professionals can exchange knowledge, ideas, and techniques.
government agencies, both U.S. and international, such as DOD, the Public Health Service, international medical care organizations, etc.,” Class said. “When we start to look at where health care is going within the U.S., within the DOD, VA, etc., we are a single location platform for that information and partnership opportunities within the profession and with industry. It’s one thing to get everyone together in a meeting, but if you don’t have a place for all that information to be housed and accessed, you have to start over and over again. So DOD may examine what’s of interest to them in particular, but we also provide information for a host of other groups.” While AMSUS has maintained the same basic approach to aiding the military medical community since its founding, it also has evolved along with medicine, warfare, and society, starting with its membership. “Originally, I’m sure they were primarily physicians, but as the health care profession began to expand and specialties were formed and a lot more non-physician providers [nurse practitioners, technicians, etc.] began to become more involved, our membership started to change along with that,” Class said. “Overall, our membership base has moved in the same direction as health care. We have a lot of researchers, in particular, and we have a lot of industry involvement through our sustainment group. “And as the U.S. has become more involved with global issues, our membership has started to reflect that as well. Because of our overall general mission of gathering information and keeping it all in one place, it interests a lot of groups, including our international partners. The goal of not 72
repeating lessons learned also extends to other nations; the U.S. shares medical information with everybody as much as possible.” As new agencies and organizations were created, such as the VA and PHS, they also were folded into the AMSUS membership. “What I’ve seen start to really grow is international involvement. A couple of years ago we had 35 countries represented at our meeting, which is a terrific way to share information and build relationships. Last year, a lot of our international groups gave presentations on how they have responded to Ebola; the world was divvied up, with different countries having responsibility for different geographic areas,” he added. “This was a great opportunity for those countries to describe how they set up and what they did in their different areas. Watching that sharing of information and how representatives reacted to what other nations were doing was great. And I’ve seen that evolve, I think, into one of the biggest changes that has occurred.” Despite all those expansions and changes, the majority of AMSUS members still come from the U.S. military, although the uniformed PHS has maintained the highest rate of retention and activity. “We also appeal to a subset in the VA – those in surgical or rehab-intensive fields, especially those who tend to have prior military service themselves. The VA writ large is mostly an academic or training hospital and we don’t play in the minds of most of those people. And we don’t try to. Our subject matter is those issues that revolve around medical support for deployed and combat forces,” Cowan said. “That’s still a pretty wide swath, going all the way from fitness and resilience – both psychological and physical – preventive medicine, the maintenance of healthy families, keeping the force fit and healthy on and off the battlefield – all of which are just as important as medevac and all the other things we think of as combat medicine. Battlefield medicine doesn’t start and stop at the edge of combat; it extends on to those who have served and retired.” Nevertheless, cultural and administrative changes within the military have restricted uniformed membership. For
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ AMSUS Annual Continuing Education Meetings allow colleagues of different services and federal organizations to exchange ideas and information.
example, Cowan noted that until the early years of the 21st century, a young medical officer entering the military would be advised by his or her commander to join a professional organization in the officer’s specialty – and AMSUS. However, the interpretation of rules on ethical conflicts of interest has become so restrictive, no commander today would even consider telling a young officer to join a private membership organization. That has not prevented them from benefitting from the constantly updated database AMSUS maintains, because the association has always made the information it gathers freely available to anyone who needs it. Large turnouts at the annual meetings also helped offset any loss of
www.defensemedianetwork.com
new membership income. But with the government now restricting travel to and attendance at such events, the organization is evolving once again. “Even as AMSUS continues to provide platforms looking at the use of new technologies, the way we deliver those platforms will need to change. But our overall mission of providing platforms remains the same and will not go away. We just need to keep getting better at it,” Class acknowledged. “We’re here to communicate [information] as best we can, using the best – and most economically feasible – ways to do that. But there is so much information out there now and so many places people go to look for it, it can be hard to pinpoint just where we need to go. 73
NOW YOU HAVE A CHOICE!
0.5 mL each
1/2 SECOND SPRAY is all it takes!
SPrAY KIT – MUlTIPlE USE UNIT DOSE – PATIENT SAFETY An Innovative Non-Aerosol Unit Dose Topical Anesthetic Spray • • • • •
• • •
Meets Joint Commission Standard for the most ready-to-administer form available* Fast onset • Short duration Virtually no systemic absorption Utilizes bar code medication administration (BCMA) to accommodate point-of-care scanning Virtually eliminates adverse events resulting from preventable medication errors, ensuring the “5 Rights” are met: √ Right Drug √ Right Patient √ Right Dose √ Right Route √ Right Time Single unit-of-use packaging eliminates the potential for cross-contamination Increases billing accuracy and improves supply chain costs Recyclable
ONLINE MSSW ONLINE & DSW DSW Programs Programs & MSSW Certifi Certificate MSSW available in trauma available as well well as as veterinary as social work, work, school, social & gerontology gerontology & Accepting applications applications Accepting for 2017 for 2017 @ www.csw.utk.edu www.csw.utk.edu @
20% Benzocaine Oral Anesthetic • Eliminates pain and discomfort • Fast onset (within 30 seconds) • Short duration (15 minutes) • Safe – available over the counter • Best value among topical anesthetic sprays • Great Wild Cherry flavor!
20% Benzocaine for fast, temporary relief of occasional minor irritation and pain associated with: • Canker sores • Minor dental procedures • Minor injury of the mouth and gums • Minor irritation of the mouth and gums caused by dentures or orthodontic appliances
FAST ONSET AND SHORT DURATION Spray
Anesthetizes within 30 seconds and lasts approximately 15 minutes.
SAFE Trusted by medical and dental professionals for over 40 years.
FOUR GREAT FlAvORS Extension Tubes
LLC
• Wild Cherry • Piña Colada
• Mint • Watermelon
To place an order or for more information, please contact your supplier or call us direct at 1-800-238-8542, M-F: 8:00 a.m. – 4:30 p.m. ET. www.beutlich.com *Joint Commission Standard: MM.05.01.11, EP4 HurriCaine® and HurriCaine ONE® are registered trademarks of Beutlich® Pharmaceuticals, LLC. VADA 708 0815
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ One of the speakers at the AMSUS 2014 Continuing Education Meeting Dec. 2, 2014, at the Walter E. Washington Convention Center.
“In the past few years, we’ve really started to use some social media a bit more to get people to look at things every day. We have a Facebook page where we put all kinds of information to let people know about new journal articles or things happening within DOD or the VA they should be aware of. As that evolves, we will have to evolve with it. Within the next 10 or 15 years, most things will not be in print anymore and we’ll have to look at how to deal with that. Meetings also are changing and as technology allows it to become more economically feasible to live-stream things, we will look at that, too.” From an idea that sprang up in the midst of the bloodiest conflict in American history to an organization created during a period of peace, from state National Guard surgeons general to combat physicians to a wider membership that includes civilian and non-physician health care providers, AMSUS has evolved with the times. And it will continue to do so in the decades to come. “AMSUS today is best described as a communications platform for federal health professionals. Our annual meeting is where leadership has its only real opportunity to have fellowship and communication with each other – military, VA, etc. – in an open environment where they are not competing with each other. And where physicians from other nations also can come together to build relationships with one another,” Cowan concluded. “So it’s not just those in the trenches learning about the latest and greatest in military medicine – blood products, non-opioid pain treatments, health information technology, global health, etc. There is an education component, fellowship component, networking components, and health system recognition awards.”
www.defensemedianetwork.com
75
From an original VA Nursing Academy to a leading, nationally recognized VA Academic Partnership American Association of Colleges of Nursing
2015 Exemplary Academic-Practice Partnership Award •
VANAP– Undergraduate
•
Veterans CAN!
•
VANAP– Graduate Education
•
VA National Quality Scholars
– Mental Health Nurse Practitioner Program
•
Caring for America’s Heroes
– MHNP Residency
Dean Doreen C. Harper, PhD, RN, FAAN serves on The Department of Veterans Affairs National Academic Affiliations Council
Proud Member of the Joining Forces Initiative
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ President Harry S Truman promotes Gen. Omar Bradley to five-star rank, Sept. 22, 1950. Truman appointed Bradley the administrator of the
Veterans Administration on Aug. 15, 1945, and the VA’s Office of Academic Affiliations was established under the general’s leadership.
VA Office of Academic Affiliations Celebrates Its 70th Anniversary U.S. MARINE CORPS PHOTO BY LANCE CPL. JACOB D. BARBER
By Chuck Oldham n THIS YEAR, THE DEPARTMENT of Veterans Affairs (VA) is celebrating 70 years of partnership with American medical and health professional schools. It’s fair to say that the VA would be unrecognizable today without the hundreds of thousands of health professionals that have trained and worked there in a relationship that has benefited everyone involved, a true win-win for everyone. “We are extremely proud of the long-standing, close relationships built over the past 70 years among VA and academic institutions across the country,” said VA Secretary Robert A. McDonald. “These partnerships strengthen VA’s
www.defensemedianetwork.com
health care system, and provide high quality training for the nation’s health care workforce. We cannot do what we do without them.” The origins of the Office of Academic Affiliations (OAA) might be said to begin on Aug. 15, 1945, the day after World War II ended, when President Harry S Truman appointed Gen. Omar Bradley administrator of the Veterans Administration (now the Department of Veterans Affairs). Six months later, the number of veterans had swelled from 6,680,000 to 13,490,000, and was expected to increase to 20,000,000 over the next year and a half. 83
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Clearly this would be a great challenge to the VA, which responded in three ways. First, the VA invested $400 million in building 72 new veterans hospitals. Second, it created the Department of Medicine and Surgery (DMS), the forerunner of the Veterans Health Administration, within VA. The third response presented the biggest challenge: staffing the DMS and each of those hospitals with a well-trained health care work force and qualified medical personnel. Even before the end of World War II, the VA was struggling to find enough qualified physicians and health care professionals to take care of its patient load. One solution would be to draw more doctors from the private sector, but the American Medical Association (AMA) was against a full-time workforce of government doctors, and had even refused to allow full-time VA doctors membership in the organization. The VA’s newly appointed chief medical officer, Maj. Gen. Paul Hawley, MD, appealed directly to the AMA, addressing the House of Delegates. “I have been asked frequently what was the greatest advance in medicine between World War I and World War II which had accounted for the great reduction in the case fatality rate among the wounded in World War II,” Hawley told the delegates. “I was expected to say plasma or whole blood, sulfonamides, penicillin. I know these certainly played a great part; but, from very close association with the wounded, I am quite sure in my own mind that the greatest advance between the two world wars was the better education of doctors. There is no substitute for a good doctor. “Now I come this afternoon to present for your consideration the greatest single problem that has ever faced American medicine, and perhaps one of the greatest problems ever in the history of medicine,” Hawley continued. “This is to give a very high standard of medical care to approximately 20 million men.” Hawley went on in his speech to propose affiliating VA hospitals with medical schools, creating resident and teaching fellowships at VA hospitals, and creating a VA hospital-based research program. The result has been a seven-decade success story for the VA, its veteran patients, for institutions of American medical education, and for their students. “Through this historic collaboration, VA has become the largest single provider of medical training in the country, where more than 40,000 residents and 20,000 medical students receive clinical training each year,” said Darrell G. Kirch, president and CEO of the Association of American Medical Colleges. Today, VA conducts the largest education and training programs for health professionals in the United States. More than 70 percent of all doctors in the United States have received training in the VA health care system. The VA invests more than $900 million annually to provide clinical education and training programs in collaboration with more than 1,800 colleges and universities. These include 135 of 144 84
allopathic medical schools and 30 of 33 osteopathic medical schools. More than 120,000 interns, residents, fellows, and students in more than 40 clinical health professions are trained annually in the VA system, among them more than 10,000 graduate medical education (GME) positions training more than 40,000 physicians annually. “VA benefits enormously from its relationship with its partners in the medical academic community. We are able to do the work we do because of this synergistic relationship,” said VA Under Secretary for Health David J. Shulkin, MD. “We have the benefit of the top medical professionals being produced by leading academic institutions. In turn, the medical community and patients around the country benefit from VA innovations – innovations such as the implantable cardiac pacemaker; the nicotine patch to help smokers quit; liver transplants and electronic medical records. We are both proud and grateful for these relationships.” Karen Sanders, MD, Deputy Chief Academic Affiliations Officer at the OAA, and Stuart Gilman, MD, MPH, the OAA’s director of Advanced Fellowships and Professional Development, took the time to speak to Veterans Affairs & Military Medicine Outlook in a telephone interview about the origins of the Office of Academic Affiliations, its programs today, and where it is headed in the future.
Veterans Affairs & Military Medicine Outlook: Can you set the scene as far as the scope of the problem post-World War II? What had changed for the VA following World War II and why did this have to be dealt with? Stuart Gilman, MD, MPH: I actually suggest you think back earlier, to the thirties, because there were some things there that had important political framing. During the Depression, the federal government created bonus payments for World War I veterans to help ease the poverty and unemployment of many veterans. But the political compromise for that bonus payment was one where they basically gave the veterans bonds payable in the future, which wasn’t helpful to people who needed the money now. So that led to a massive protest and the creation of what was called the Bonus Army. It started with a small number of people rumbling out of Portland, or someplace like that in Oregon, driving across the country, gathering people as they went across. So the aftermath of the Bonus Army was that there was a lot of pressure, I think – political pressure – to be sure that America did it right as the demobilization from World War II proceeded. I believe there were two problems that they were solving as they were solving this challenge of the hundreds of thousands of acute care wounded personnel who were going to be coming back to the United States from their combat injuries. One was how to set up a medical system that could take care of their needs. The other was how to set up a medical system that the public would have faith in, and veterans would have faith in, and not feel like they were getting poor www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ OAA Deputy Chief Academic Affiliations
Officer Karen Sanders, MD.
PHOTO COURTESY OF KAREN SANDERS, MD
the political side of the transformation that was necessary for VA, because there was a lot of legislative relief that needed to happen for the academic affiliations to be successful. The principal one of those was the creation of Title 38, which is the human resources mechanism that was created for VA to allow relatively fluid movement of physicians to and from the VA. It allowed part-time employment, and it eliminated the need for onerous civil service processing to hire physicians, that sort of thing. Hawley and Bradley threatened to resign if Congress and the president wouldn’t support Title 38, because they didn’t think they could run the health system under the prior Title 5 civil service structure.
quality care or government care. So the academic affiliations also helped address that problem, because people largely had faith in the quality of the doctors and institutions of their local academic health centers. And the VA could say to the veterans and their families and to Congress that the veterans are getting cared for by the best physicians in these communities at the same time as they were having it happen within the construct of this expanding VA system. Gen. Omar Bradley was recruited, forced really, I think, to come take over VA. He brought with him Maj. Gen. Paul Hawley, and Hawley recruited an academic surgeon named Paul Magnuson, who was very well established in academic medicine. Hawley himself was not. He was a military guy. He was an Army guy, and he needed an insider in academic medicine. And that’s where Paul Magnuson came in. There are also other people who are very involved, such as Bernard Baruch, the New York financier, who was very important in
www.defensemedianetwork.com
Dr. Sanders, how important are these relationships to the VA today as far as it being able to operate and fulfill its obligations to veterans? Karen Sanders, MD: These relationships are essential to VA conducting its business in today’s world. I think people don’t realize that 70 percent of all of our VA physicians have faculty appointments at a nearby medical school, which means that they are held to academic standards of promotion, tenure, scholarship, and research. So that ensures VA of the quality of our physician workforce, in a way we are able to recruit most of these really fine physicians because of our affiliations with academic centers. I believe that the quality of the physician workforce in VA would be much degraded without the academic affiliations. But that’s only one component of why these are essential relationships. So we have the recruitment of our academic physician workforce. We have the trainee relationship, so that by affiliating with academic centers we participate in thousands of unique educational programs in all the specialties of medicine. And that brings trainees, a continuous stream of new young health professionals into our buildings, to learn how to take care of veterans. That is our huge workforce pipeline for the next generation of our health professionals. I’m basically a former trainee. Many of my colleagues are former trainees. We ended up working for VA because we were exposed to VA during 85
N
O
R
T
H
W
E
S
T
E
R
N
U
N
I
V
E
R
S
I
T
Y
The Time is Now. Take the Lead. Graduate Programs in Healthcare Quality and Patient Safety
PROGRAM DIRECTORS: Kevin Weiss, MD, MPH Professor of Clinical Medicine Feinberg School of Medicine Northwestern University Senior Vice President Institutional Accreditation Accreditation Council for Graduate Medical Education (ACGME) Donna Woods, EdM, PhD Associate Professor Center for Healthcare Studies Feinberg School of Medicine Northwestern University
MASTER OF SCIENCE
FACULTY DEVELOPMENT
CERTIFICATE PROGRAM
• 2-year program
• 12-month program
• 12-month program
Designed for clinical and non-clinical professionals
Designed for faculty who wish to develop the educa-
Designed for the healthcare professional who wants to
currently working in healthcare who want to focus their career development on improving healthcare delivery systems
tional tools, methods and curricular approaches for integrating quality and safety into the medical education curriculum
acquire a comprehensive overview of healthcare quality and patient safety
“Medical Errors Now Third Leading Cause of Death in U.S.”
All programs are part-time and do not require Chicago residence.
— BMJ Quality & Safety
www.northwestern.edu/quality-safety
312.503.5533
MastersIHS@northwestern.edu
Expand your career and become a leader in public health Improve and impact the health of communities
Consider one of the following options: •
Online Master of Public Health
•
Certificate in Public Health Fundamentals and Principles
•
Certificate in Public Health Surveillance and Preparedness
•
Certificate in Global Health Studies
All programs offer affordable, flexible, part-time study with no on campus requirements.
Call 518-402-0361 or visit www.albany.edu/sph/online for more information.
ADVANCING HEALTH LOCALLY AND AROUND THE WORLD
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
our training programs, and we got to know and love the system and our patients. So I think those two are huge reasons – both the recruitment of staff and then the future workforce pipeline. I think the third thing is our research mission. I don’t think we could have the intramural research program that we do have in VA without the significant academic affiliations. I don’t think we’d have access to the expertise, equipment, and laboratories without this totally synergistic research relationship. Stuart Gilman, MD, MPH: I think that’s exactly right … because you can’t have a research program without an academic infrastructure. That’s what academic institutions do. So the faculty for our academic mission are also frequently the investigators in the research mission. There is a huge amount of interaction. And VA is an unusual federal agency in that we have an intramural research program. VA’s research money is awarded in grants to the VA researchers. Unlike NIH [the National Institutes of Health], which awards money to people at universities, the VA awards it only within the VA. So the only way for people to do research on VA funding is if they are within the VA. And the research stays within the VA. The resources for the research and all that are within the VA. The Department of Defense [DOD] has a huge extramural program for military medicine research, meaning they’ll give grants to universities and academic centers, but not necessarily within the DOD. VA uses our research mission to strengthen directly our clinical and educational missions. These are highly interactive positive feedback loops between the three principal missions, with education and research clearly being there to advance the clinical mission. The research resources stay within the VA system and serve to strengthen VA’s clinical and education missions. What about the students, the interns, the future health professionals? How do they benefit from this? Stuart Gilman, MD, MPH: If the VA health system were to disappear, one of the things that would create a massive vacuum would be this learning environment for 120,000 health professionals each year, because the other academic settings are saturated already with trainees. One of the things the students get out of it and that America gets out of this is that we have the capacity, again through that synergy, where by having the education mission we can provide more and better veterans’ health care. We’re also expanding the capacity of the general health workforce in the U.S. In terms of other things that the trainees get out of this, for instance VA was on the forefront of electronic medical records. We were the place where a generation of physicians got exposed to the use of electric health records before they became widely employed in nongovernment hospitals, so that they already had exposure and experience. And in many cases, they were demanding the use of electronic health records
www.defensemedianetwork.com
■■ One of the things the students get out of it and that America gets out of this is that we have the capacity, again through that synergy, where by having the education mission we can provide more and better veterans’ health care.
in their private-practice settings because they saw the power for quality of care and improved communication and patient safety that a system like the VA’s brings to health care. So I think VA has had a massive impact on really pretty subtle things like that awareness and acceptance of electronic health records. Dr. Sanders, could you describe the range of different health professionals that benefit from those academic relationships with the VA? Karen Sanders, MD: Every year, for the last bunch of years, we’ve had over 120,000 trainees that are part of our VA system and learning in our VA system. That includes learners that are there for just a month versus people that may stay a whole year in VA. But a range of health professions – I think we usually say over 40 health professions – train and learn in VA. And that’s everything from nursing and physicians to dentists and podiatrists and optometrists, and of course the mental health professionals like psychologists, social workers, chaplains, and licensed mental health counselors. So a huge number of professions train in VA. We have a huge role to play in education of the health professions workforce in the country. And these people, we don’t recruit all of them, obviously. Probably only a fraction of them come to work for VA. But when they go out and practice, all of a sudden they know about veterans. They know about veteran illnesses and injuries. They are quite capable of taking care of veterans in their private practices. And they spent a bit of time with us. So I think it’s good for both the VA and the nation. Can you talk a little bit about the VA mental health education expansion initiative? I know it’s been talked about as being a challenge trying to recruit and retain all the people that will be necessary to deal with those issues. Karen Sanders, MD: Yes. I think we’ve had four completed years of our mental health education expansion. And this year we are just putting out another RFP for the fifth cycle of our mental health expansion. We target specific mental health disciplines. And we have, I think, success in terms of hundreds of new trainees coming through the VA system. Every year we have hundreds of psychology trainees that train in VA. So psychologists are the No. 1 directly paid trainee discipline. And we pay over 600 psychologists a 87
Ranked Top 30 Online Graduate Nursing Program
Offering Master’s and Doctoral Programs for Registered Nurses
Specialties offered:
frontier.edu/military
• • • •
Certified Nurse-Midwife Family Nurse Practitioner Women’s Health Care NP Psychiatric-Mental Health NP
Complete coursework online with only 1-3 brief visits to campus.
Calling All Active Duty and Reserve Dentists! If you plan to open a private practice once you’ve retired from the military, or if you’re a Reservist with a private practice, give back to your fellow service members by joining the TRICARE Retiree Dental Program (TRDP) and/or Veterans Affairs Dental Insurance Program (VADIP) networks. > Build your practice with access to over 1.5 million members enrolled in these programs. > Receive direct and timely payments. > Get access to easy-to-use online tools to save time. Delta Dental is proud to administer the TRDP and VADIP. Visit us at trdp.org/dentists and deltadentalvadip.org/dentists for more information about joining our networks!
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ OAA Director of Advanced Fellowships and Professional Development Stuart Gilman, MD, MPH.
PHOTO COURTESY OF STUART GILMAN, MD, MPH
year. A lot of the problem actually with the mental health workforce issues ends up not being the number of trainees that we train but the hiring process itself. It takes a lot of time. It’s still a kind of sequential step process. I know that there are a lot of people hard at work in trying to make our hiring processes better in VA. What sort of impact have these partnerships had on U.S. health care in general? Stuart Gilman, MD, MPH: In the initial step, it’s by helping expand the workforce, as we’ve talked about, which is a pretty darned good start. But beyond that, the VA’s academic mission has led to the development of a wide variety of clinical care advances that are in U.S. health care. So keeping focused just on education, fields like geriatrics might not exist as a medical profession specialty had it not been for significant VA support, in part through the research investments, but also in part through significant educational investments where VA decided to focus on education of people to pursue care in geriatrics before these became recognized as medical specialties. There are a number of other fields that have the same story. We can look at addiction psychiatry, palliative care, clinical informatics, recently addiction medicine, recently traumatic brain injury, and others that don’t roll off the top of my head, as recognized medical specialties by the American Board of Medical Specialties. VA had a significant role in helping create the critical mass of practitioners and researchers who would pursue these fields and helped then to create them. Fields like patient safety and health care quality are areas where the VA has made significant contributions to the development of these professions, and helped elevate the practice throughout the nation, not just in the VA. Karen Sanders, MD: I think a current example is nurse practitioner residents. The standard in the community is that nurse practitioners, after they finish their master’s training, are functional providers already. And we in VA have said no, we actually believe that a nurse practitioner graduate needs an additional year of training to become fully functional. We created these nurse practitioner residents that are now catching on in the private sector. I think we’ve influenced all the key nursing organizations to agree with us that this is a valuable additional year and perhaps a nurse practitioner coming out of their degree program is not sufficiently ready to assume a practice role. Stuart Gilman, MD, MPH: Karen’s discussion is an example of other kinds of interactions. We talk a lot about our interactions with academics, meaning schools of nursing and medicine, etc. But another very important sphere that we interact with on these academic issues is with professional
www.defensemedianetwork.com
organizations that set standards for certification and quality in each of these fields we work with. And our office has a lot of relationships with professional organizations and is in ongoing dialogue with them about these kinds of issues that influence both VA and the nation. When did the VA Nursing Academy Partnership program begin, and how many partnerships are involved today? Karen Sanders, MD: The VA Nursing Academy Partnership program began in the academic year 2007-2008. It began as a five-year pilot that was then renewed. So there are now a total of 24 partnerships, some at the undergraduate level and some at the graduate level. When we speak of the undergraduate level, we mean baccalaureate-prepared nurses. And when we speak of the graduate level, we’re pretty much talking about nurse practitioner master’s-level trainees. What do you see as being challenges in the future, and what are the initiatives you have to meet them? 89
University of Pennsylvania
School of Social Policy & Practice
Doctorate in Clinical Social Work
Preparing Leaders in Social Work Practice
“The hybrid DSW program is flexible, rigorous, and intellectually stimulating. I was able to pursue my doctoral studies while serving on active duty in the United States Air Force.” - Kenneth Marfilius, DSW Class of 2018
“SP2’s commitment to advancing the field of Military Social Work is clear, and has already provided me with exciting academic and professional opportunities!” - Crystal Shelton, DSW Class of 2018
Earn a doctorate in just three years, from wherever you are. www.sp2.upenn.edu/dsw
dswcoord@sp2.upenn.edu
215.573.7133
Honored to serve
UCLA Operation Mend now provides family-focused treatment for TBI and PTSD Our renowned surgical and medical program serving active-duty service members and veterans has expanded to provide comprehensive psychological health and social support for both wounded warriors and their family members. Eligible participants will receive the personalized “wraparound” care for which UCLA Operation Mend is known; all at no cost.
To learn more, call 310-267-2110 or visit operationmend.ucla.edu
Operation Mend is a proud member of Warrior Care Network
LAW/VAMM
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
PHOTO BY REYNALDO LEAL/U.S. DEPARTMENT OF VETERANS AFFAIRS
■■ VA Secretary Robert A. McDonald talks to residents at the intensive care unit at the Bronx VA Medical Center in New York. Every year, approximately 120,000 trainees work and learn in the VA system.
Karen Sanders, MD: I think one of the most interesting things we’re currently involved with is the new VA GME expansion. That was legislated under the Choice Act two years ago. This was a requirement from Congress that allows VA to increase up to 1,500 new GME positions over five years. And the interesting thing about what Congress did is that they challenged VA to put these GME positions into rural and underserved VAs and communities. They basically said, “We don’t want you to be doing GME as usual. We want you to look for small VAs in rural communities that maybe never had participated in GME before. And we want you to go out and build programs in those areas because we know that when you build GME in a small community, those graduates will likely stay there and improve the workforce for both VA and those smaller communities.” So Congress set out this really tough job for us, I would say, over five years. We are finding that it is going to take more than five years to do this. But we find it incredibly exciting to be participating in this new GME expansion, because we really feel that this expansion has such a public health mission to it. It really is to try to address the physician maldistribution in the United States. It helps VA, but it also helps all those smaller communities out there that don’t have doctors, or have rural doctors that are retiring and they can’t find anybody else to come practice there. So this is a very “feel good” initiative for VA. It’s hard. It’s required in our office to create a lot of new kinds of partnerships, like the osteopathic community program, family medicine community program, teaching health centers under HRSA [Health Resources and Services Administration] – a lot of new kinds of graduate medical education partners. But we also feel that, if we’re successful at this, and we hope we will be, this will be quite an important step forward for both VA and the smaller communities out there. I understand that the overall program is in collaboration with 135 of 144 allopathic medical schools and 30 of 33 osteopathic medical schools. How many VA facilities do
www.defensemedianetwork.com
these students practice in or learn in? I’m not quite clear on how that works. Karen Sanders, MD: Well, let me answer that question with a little bit of a caveat. The partnerships are fluid things. We can query the database today and I could give you a number, and I could query the database tomorrow and I would give you a different number. Let’s put it this way: Probably almost 120 VAs out there have a significant GME component or have some trainees of some type. In fact, most VAs have trainees of some type. But not all of them have medical students or residents. It’s still over 100 VAs out there that have medical students or residents. But the number changes because there are elective experiences and there are students that go to other VAs, not their home VA. So it’s kind of fluid day by day. For this expansion initiative, we’ve targeted about 30 smaller VAs that have little to no GME currently. So we call them the complexity level two or three VAs. Those are the smaller VAs primarily in small communities, rural VAs. And those are the VAs we’re targeting for this Choice Act GME expansion. Stuart Gilman, MD, MPH: And when Karen is talking about 100 to 120 VA medical centers, remember that these medical centers often have multiple locations. They may have more than one hospital campus within them. They may have multiple community-based outpatient clinics. So the numbers of actual VA locations where the trainees are will be more than the number of medical centers that we have them attributed to. 91
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
The Path to Excellence By Carolyn M. Clancy, MD Deputy Under Secretary for Health for Organizational Excellence, Veterans Health Administration
We are what we repeatedly do. Excellence, then, is not an act, but a habit. – Aristotle
92
■■ VHA Deputy Under Secretary for Health for Organizational
Excellence Carolyn M. Clancy, MD.
ASSESSING AND IMPROVING QUALITY AND SAFETY
While it’s no surprise that new learning is essential to improving health care quality and safety, few may realize
www.defensemedianetwork.com
VA PHOTO
n WHAT DOES “EXCELLENCE” MEAN WITH REGARD to veterans’ health care? How is it operationalized on a daily basis at Department of Veterans Affairs (VA) facilities nationwide? As suggested by the Aristotle quote, excellence is a way of being, and going about one’s work. Within the context of Veterans Health Administration (VHA) care, it is the continuous striving toward the highest quality care for veterans. Today, at facilities nationwide, VHA staff are using best practices, repeatable processes, clinical practice guidelines, highreliability training, and many other learning methods in our ongoing effort to ensure veterans receive the best care anywhere, anytime they seek our help. Excellence is also a dynamic concept, one that implies an ongoing quest toward the optimum state. For example, while veterans’ access to health care has improved significantly since 2014 (with nearly 97 percent of appointments now completed within 30 days of the veteran’s preferred date), our ultimate goal is for every veteran to get the care they need, as soon as they need it. Using predictive analytics, survey instruments, ongoing data collection, and other tools (many developed with veterans’ input), VHA staff are continually and systematically working toward this goal. In December 2015, VHA brought together these capabilities and resources under a single directorate: the Office of Organizational Excellence (OE). Our new office is charged with coordinating the vital components of veterans’ care that focus upon: • Assessing and improving quality and safety; • Helping the field assess performance on key measures; • Disseminating best practices; • Promoting health equity; and • Addressing the critical issues that assure public trust and integrity. In short, OE is the engine that drives quality, safety, and integrity throughout the VA health care system.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Through the VA Quality of Care website, interested parties can find
out how different Veterans Health Administration (VHA) facilities have rated in a variety of areas according to the Strategic Analytics for Improvement and Learning (SAIL) Value Model.
that VHA leads the way in training. Last year on these pages, VA’s Clinical Team Training (CTT) program was featured in the article “Creating High-reliability Health Care for Veterans.” To recap, CTT is a yearlong initiative comprising didactic training and the implementation of a project aimed at improving teamwork, communications, team decisionmaking, and patient safety. One of the characteristics that distinguishes CTT from other learning methods is its sustainability: CTT deepens learning through repeated training sessions that ultimately lead to culture change. In the year since the article’s publication, CTT (now part of OE) has been used by additional multidisciplinary teams across the VHA enterprise. In 2016, more than 23 unique training events were conducted nationwide. This training included the development and implementation of a standardized handoff protocol between levels of care when transporting patients from the operating room to surgical intensive care and post-anesthesia care (Memphis); implementation of a standardized safety briefing and two checklists for dialysis (Pittsburgh); and improving patient flow and access for unscheduled (or walk-in) patients (Las Cruces). Additionally, facility-wide CTT implementation at the Truman VA Medical Center (VAMC) in Columbia, Missouri, has led to a number of team-based innovations. One of the most significant innovations, “4Med,” occurred on the inpatient Medical Surgical unit. Here, physicians began using a checklist, following medical rounds, to lead daily briefings for all nursing staff at the nurse’s station. These short briefings, averaging six minutes in duration, provide an opportunity for face-to-face communication, questions, and verbal clarifications about items in each veteran’s plan of care. In the first six months of the checklist implementation, more than 214 physician-led briefings (aka “huddles”) were held. The Truman VA’s use of this training is a significant step toward improving physician/nurse communications, fostering teamwork, and most importantly, enhancing the safety culture. Another key area where VA has led the way in health care quality is through clinical practice guidelines (CPGs). These guidelines are intended to improve care by reducing variation in practice, systemizing best practices, reducing errors, and ensuring consistent quality. Through VHA’s EvidenceBased Working Group, which is also a part of the OE directorate, VA collaborates with the Department of Defense (DOD) and other professional organizations to develop CPGs in six areas: chronic disease in primary care, mental health, military-related, pain, rehabilitation, and women’s health. In addition to reviewing the latest research evidence on a given topic, the Evidence-Based Practice Program conducts
www.defensemedianetwork.com
veteran/patient focus groups. Generally speaking, these focus groups are a sample of active duty, military dependents, veterans, and family members. Participants are asked about personal experiences and questions are framed to help elicit what works, doesn’t work, and what isn’t being addressed in dealing with a particular health care issue. This input/feedback is utilized in developing “key questions,” which in turn guide a literature review and resulting evidence. Over the past year, for example, the Working Group has been revising its 2010 CPG on chronic opioid therapy. As part of the revision process, findings from a focus group in Washington, D.C., were combined with input from an individual stakeholder meeting with the family of a Marine whose death was reportedly related to mixed drug toxicity, including opiates. The input from both groups was consistent and led to identification of seven overarching themes: • Encourage shared decision making; • Identify individual risk/benefit and modify treatment accordingly; • Involve family caregivers according to patient preference; • Educate patient and family on treatment plan with alternative options and monitoring; • Ensure continuity of care across and within health care systems; • Organize treatment that encourages patient adherence and participation; and • Continue pain management transformation. As this article goes to press, the revised CPG, VA/DOD Management of Long Term Opioid Therapy, is in the final production stages and scheduled to be released in December 2016. HELPING THE FIELD ASSESS PERFORMANCE ON KEY MEASURES
The realignment of functions under OE means VHA can further strengthen support to the field, and, in turn, 93
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ VA staff at the spring 2016 Diffusion of
Excellence Planning Summit.
of facilities demonstrated meaningful improvements. DISSEMINATING BEST PRACTICES
94
PROMOTING HEALTH EQUITY
Excellence also means assuring access and the highestquality health care for veteran population groups who have systematically experienced greater social and/or economic obstacles to health based upon factors such as race/ethnicity, gender, sexual orientation, socioeconomic status, and mental health, as well as military era or period of service or cognitive, sensory, or physical disability. Through the Office of Health Equity (OHE), also part of OE, VHA supports and participates in a wide range of efforts to ensure high-quality care for veterans in these population groups. These efforts include novel technologies to reduce gender disparities in cardiovascular disease; acupuncture for veterans with posttraumatic stress disorder (PTSD) and pain; maternity management for women veterans in rural areas; and decision aid management for elderly heart failure patients with cognitive impairment.
www.defensemedianetwork.com
VA PHOTO
veterans. An example of such support is the SAIL (Strategic Analytics for Improvement and Learning) Value Model, a web-based balanced scorecard that measures, evaluates, and benchmarks quality and efficiency at every VAMC on a quarterly basis. SAIL assesses 27 quality measures in areas such as death rate, complications, and patient satisfaction, as well as overall efficiency at individual VAMCs. These metrics include all those used by the private sector as well as some that are unique to VA. The reports and tools within SAIL enable executives and managers to examine a wide breadth of existing measures. Expert consultation is routinely provided both on-site and virtually to help staff better understand data, identify opportunities, and achieve improvement in priority areas. For example, when frontline staff at the Buffalo VAMC realized, from the facility’s SAIL scores, that help was needed for improvement, they reached out to OE for expert consultation. Following hard work by facility leaders and frontline staff to improve clinical care and processes within the system, the VAMC slowly began making improvements. Over time, the facility has seen significant improvements in many key quality areas and they continue to monitor progress in SAIL reports today. (To see the SAIL scorecard table, visit the VA Quality of Care website www.va.gov/qualityofcare, under the left-hand tab “How Does Your VA Measure Up?”) We’ve also incorporated an explicit focus on SAIL metrics into the performance plans of all medical center and network directors. Beginning in 2015, these plans included a comparison of performance at the end of the fiscal year to performance with the prior year using a statistical improvement index (each facility is evaluated based on its own, respective improvement). Notably, in FY 2016, 82 percent
On average, it can take as long as 17 years before evidence-based research is put into clinical practice. Diffusing and implementing new practices across the board in large health care systems such as VA (with more than 1,700 sites of care and 300,000+ employees) is inherently challenging. To speed adoption system-wide, VHA’s Office of Strategic Integration and OE have combined forces on a new initiative, called the Diffusion of Excellence. Through this initiative, VHA is working with frontline VHA employees to identify and then disseminate best practices (both clinical and administrative) throughout the entire system. Our goal is simple: achieving a standardization of practices that deliver positive outcomes for veterans and their families system-wide. Since the fall of 2015, the initiative has generated more than 3,000 ongoing implementations of best practices in 70 facilities. In addition to disseminating best practices, Diffusion of Excellence furthers both employee engagement and veteran outreach. Through the initiative’s Innovators Network, frontline employees co-design new practices with veterans and other stakeholders. The result is veteran-centric best practices developed by the front line, for the front line.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Clancy, then-interim under secretary for
health for the VA, and VA Secretary Robert A. McDonald testify before the Senate Committee on Veterans Affairs on the state of VA health care on Sept. 9, 2014, at the Hart Senate Office Building in Washington, D.C. Since 2014, VHA has made significant progress in addressing reported issues of veteran access to care.
Additionally, OHE works closely with VA Research to shape and focus new studies aimed at reducing disparities in care, a collaboration that is discussed elsewhere in this publication under “VA Research: Improving Equity and Reducing Disparities in Health Care.”
VA/ROBERT TURTIL
ASSURING PUBLIC TRUST AND INTEGRITY
Shortly after becoming VA secretary in 2014, Robert McDonald told an Institute of Medicine audience how – in the wake of the access crisis – VA had “perhaps its greatest opportunity to enhance care for veterans in its history.” In the two years since Secretary McDonald took office, VHA has used these and other challenges as springboards for taking deeper looks “within” to examine our processes. For example, we’ve taken a proactive role with regard to access. In 2014, we invited The Joint Commission (the independent, not-for-profit organization that accredits and certifies nearly 21,000 U.S. health care organizations and programs) to make unannounced visits to all VAMCs. These on-the-ground assessments showed that our facilities were making significant progress and working diligently to understand the causes underlying access. Since then, our path toward excellence has continued, and we’ve worked to more precisely frame what access means in the context of veterans’ health care. As noted at the beginning of this article, nearly 97 percent of appointments are completed within 30 days of the veteran’s preferred date. Our “true north” goal for access, however, directly ref lects veterans’ reported experiences. Using a subset of items from the widely used Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey, our goal is a composite of the percentage of veterans who report that in the past six months they always or are usually able to: obtain care that is needed right away, obtain care for routine needs, and obtain primary and specialty care. At this writing, we have seen steady improvements across the system, and additional improvement efforts continue.
www.defensemedianetwork.com
In a similar manner, we are using the opportunity presented by VHA’s inclusion on the Government Accountability Office (GAO) “high-risk list” to take a closer look at our internal processes. Our objective is not to get off the list per se, but to ensure VHA is providing veterans with timely, cost-effective, safe, and high-quality health care, and to eliminate performance barriers and ensure the work itself is simpler for the dedicated employees who serve veterans. In August, we submitted a response to GAO that outlined our approach to addressing five issue areas identified, and summarized progress to date. Notably, employee engagement has been critical to this effort, both in formulating the VHA’s response and in moving forward to address the five high-risk issues. As of this writing, an internal task force is being formed to directly solicit employee insights and perspectives on the five high-risk issues and how they affect daily work. CONCLUSION
As demonstrated above, VA’s path to excellence is an ongoing journey that continually invites key stakeholders to come along: veterans and their families as well as frontline staff at VHA facilities nationwide. Over time, we hope to evolve OE as a VHA-wide clearinghouse for the resources, tools, and expertise that help make “excellence” habit, and ensure the highest quality care for veterans. 95
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA Research: Genomic Medicine By Craig Collins n YEARS BEFORE THE INTERNATIONAL Human Genome Project determined the sequence of chemical base pairs that make up human DNA, researchers at the Department of Veterans Affairs (VA) were pioneers in this new line of inquiry, uncovering links between specific genes – the segments of DNA that form the molecular units of heredity – and particular diseases or disorders. Beginning in the mid1990s, investigators at the VA’s Puget Sound Health Care System made a series of discoveries linking genetic mutations to Werner’s syndrome (a rare hereditary disease that causes premature aging and death), schizophrenia, and a rare form of dementia. This 1998 discovery offered a potential target for the treatment of Alzheimer’s disease. When the 13-year effort to map the entirety of the human organism’s hereditary material – the genome – was finalized in 2003, it sparked an explosion in genomics research, and the VA, with several successful investigations already completed and more underway, assumed a leading role in this new era. In 2006, to advance knowledge of how genes affect health and to examine the potential for emerging genomic technologies to personalize medicine for veterans, the agency formally established its Genomic Medicine Program. The first steps in launching the program included the establishment of a distinguished 13-member Genomic Medicine Program Advisory Committee (GMPAC) to lay the groundwork and chart a course for investigation. Meanwhile, the Veterans Health Administration (VHA) broadened its network of laboratories conducting genomics research; at the Washington, D.C. VA Medical Center, for example, investigators began looking into genetic changes in cancers that might predict responses to chemotherapy and guide patient care. Genomic research promises to change the field of medicine completely, offering evidence-based and personalized approaches to prevention, diagnosis, and treatment. A significant portion of genomics research today is devoted to the field of pharmacogenomics, or studies of how individual genes determine a person’s reaction to certain drugs or immunotherapies. Genetic studies are generally of two types: candidate gene studies, in which researchers focus on associations 96
between pre-specified genetic variations and disease states, or genome-wide association studies (GWAS), which scan the entire genomes of a large sample of people for common genetic variations, and, with the help of super-fast computers, discover which genes turn up in one group (i.e., people with diabetes) and not another. Sumitra Muralidhar, PhD, director for the Million Veteran Program (MVP), in the VHA’s Office of Research and Development, pointed out that several things need to be in place before a useful GWAS can be implemented, including a large sample of genetic material, the infrastructure necessary to store and examine it, and powerful informatics and computational tools to compare hundreds of thousands to millions of variants. The VHA is, in many respects, the ideal venue for genomics research. It’s the nation’s largest integrated health care delivery system, providing care to about 8.8 million veteran patients; it uses one of the world’s most sophisticated electronic medical record systems; many of its investigators are also esteemed faculty members at the nation’s finest research universities; and its professionals are committed to personalizing medicine to the greatest extent possible. The sheer number of patient volunteers has allowed the VA to launch some of the world’s largest genomics studies. In 2009, a VA-funded research team, including Muralidhar, began investigating the genetic basis of schizophrenia and bipolar disorder, which together affect some 170,000 VA patients. Researchers in this GWAS are scanning DNA from upward of 29,000 veterans (~9,000 with either illness and at least 20,000 controls without either illness) in search of gene variants found in those with mental illness. VA’s research in the genetics of schizophrenia has led scientists to discover genes that weren’t on anyone’s radar a few years ago. The ability to compare the genomes of such a large cohort, along with the data contained in individual medical records, offers nothing less than an opportunity to revolutionize the way medicine is practiced, said Muralidhar. “Now you’re looking at large numbers of people who did and did not develop an illness,” she said. “And you can better pinpoint the causes of it, genetic as well as lifestyle and environmental factors. You can include all these in a study.”
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ ABOVE: DNA samples from veterans at the Million Veteran Program
(MVP) biorepository in Boston, Massachusetts. The MVP is an ambitious initiative to build a comprehensive database including genetic, military service, lifestyle, and health information from 1 million veteran participants. RIGHT: Dr. Don Humphries, with the VA Boston Healthcare System, helps manage VA’s Million Veteran Program.
The questions such a large genomic cohort can help to answer – Why does a treatment work well for some people, and not others? Why are some people at greater risk for this disease? How might we prevent certain diseases in the first place? – are relatively simple. But being able to answer them definitively, using genomic and other data, will do nothing less than revolutionize medicine.
VA PHOTOS BY FRANK CURRAN
THE MILLION VETERAN PROGRAM
To date, Muralidhar said, most genetic studies have had disappointing results, simply because they weren’t able to compare DNA from sufficient numbers of people with and without the disease to get a definitive answer, and a result that could be replicated by other studies. For the VA, whose investigators also study complex, multivariable disorders like
www.defensemedianetwork.com
post-traumatic stress disorder (PTSD) and the cluster of medically unexplained symptoms known collectively as Gulf War Syndrome, this has been a severely limiting circumstance. The strength and validity of GWAS findings, obviously, increase in direct proportion to the amount of genetic material sampled. In 2011, the VA launched its landmark initiative to harness the full potential of the data contained within its health care system: the Million Veteran Program (MVP). 97
■■ ABOVE: Research coordinators from the Million Veteran Program,
VA PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
The MVP is an ambitious initiative to build a comprehensive database including genetic, military service, lifestyle, and health information from 1 million veteran participants. By the summer of 2016, the program had signed on its 500,000th volunteer, on pace to enroll its millionth veteran by 2020, making it one of the largest databases of its kind in the world: an integrated health and genomic database tied to a health care system, with the largest representation of minorities of any genomic cohort in the United States. At its core, MVP is a massive data mining effort, confronted with several unique challenges: recruiting participants on a massive scale; keeping this data protected without impeding the efforts of researchers to access it; and applying 98
the computing power needed to squeeze hidden information and associations from such a vast amount of data. Blood and tissue samples from MVP participants are collected and stored at the Core Laboratory at the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC) within the Boston VA facility. Here, hundreds of thousands of DNA samples, taken from veterans taking part in MVP as well as clinical trials through the VA’s Cooperative Studies Program, are stored in a biorepository that will someday house millions of samples in an enormous freezer – sorted, stored, and retrieved by a sophisticated robotics system. When a veteran enrolls as an MVP participant, a study number is assigned; each participant becomes an anonymous blood vial with a history attached to it. Anonymity over the lifetime of a participant is enabled by the MVP’s computer network, the Genomic Information System for Integrative Science (GenISIS). All data collected, for example from
www.defensemedianetwork.com
PHOTO BY DERRICK MORIN, MVP, BOSTON
Central Western Massachusetts VA, explain the program to a veteran during an outreach event. LEFT: Army veteran Michael Owen Smith, from Montgomery, Alabama, was the 500,000th enrollee in the MVP. He is pictured here with Drs. Michael Gaziano and John Concato of the MVP.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A veteran research participant signs informed consent documents
associated with participation in MVP.
the survey or from the electronic medical record, are also assigned a code. Anonymity is only part of the problem confronting the people who handle this data: In hunting for disease-linked genes in a GWAS, researchers are looking for molecular changes in the chemical bases that make up the DNA sequence – variations called single nucleotide polymorphisms (SNPs). There are millions of SNPs among the 3 billion chemical base pairs that make up human DNA, and finding the critical ones is a challenge, to say the least. Each sample taken in at the MAVERIC lab undergoes a scan for about 765,000 SNPs of known significance, and some samples undergo closer scrutiny: a complete sequencing of the exome, the relatively small portion of the DNA that encodes for the building of proteins. Though more costly than a scan, exome sequencing is efficient: While it makes up less than 2 percent of the genome, the exome is believed to contain the majority of disease-related SNPs. An even smaller number of MVP samples have undergone or will undergo a sequencing of the entire genome, a procedure that costs around $2,000 per sample. This deep-level analysis is typically conducted on selected sets of samples: people over 95 years of age who are exceptionally healthy, for example, or those diagnosed with a particular disease or disorder. It’s difficult to imagine the artificial intelligence capable of finding commonalities among the billions of SNPs involved in studies of these groups. In a single study, Muralidhar said, “You’re talking about tens of thousands of cases, and other tens of thousands of controls, and to do that computation you need very high computing capacity.” This capacity is still being developed. “Right now, we may have 25 to 50 researchers accessing the system at the same time,” said Muralidhar. “But imagine down the road, when we have hundreds or even thousands of researchers who’ve been approved and are accessing at the same time. We’re still trying to determine the capabilities and processes we’ll need to clean and curate all this data.”
VA PHOTO
A NEW ERA OF GENETIC STUDY
The MVP allows teams of researchers to conduct investigations by combining secure data from GenISIS with the electronic health record data contained in another network, the VA Informatics and Computing Infrastructure (VINCI), and searching for the differences – genetic and otherwise – among those who have a certain disease and those who don’t. While the infrastructure and capabilities are still being developed to support large numbers of intensive genomic studies, several investigative teams
www.defensemedianetwork.com
have already begun to study parts of the MVP cohort. VA researchers Joel Gelernter, MD, and Murray Stein, MD, for example, recently launched a GWAS of PTSD. About 18 percent of the veterans enrolled in the MVP so far have a reported diagnosis of PTSD, and when enrollment reaches the 1 million mark, this will provide the research team with 180,000 veterans to study. For starters, Gelernter and Stein will focus on comparing 10,000 veterans with PTSD to a control population of 10,000. PTSD is a difficult disorder to study. Its diagnosis isn’t as clear-cut or easily substantiated as something like diabetes or cancer, and the team expects to find several genetic variants that are relevant for all cases of PTSD – but combining genetic information with health- and service-related data allows investigators to narrow their focus to cases of combatrelated PTSD. If Gelernter and Stein’s team can find evidence about genes in combat-related stress, drugs might be developed to target the underlying biology of the disease. In the past year, several additional studies of the MVP cohort have been funded, including: • A study of the genes that influence how obesity and lipid levels contribute to cardiovascular risk, and of whether these genetic factors differ among African-Americans and Hispanics. Farooq Amin, MD, and Peter Wilson, MD, at the Atlanta VA Medical Center, along with Kelly Cho, PhD, at the Boston VA Healthcare System, will lead the study. • An examination of the genetic risk factors for chronic use of alcohol, tobacco, and opioids – and the dangerous use of all three together – led by Daniel Federman, MD, and Amy Justice, MD, PhD, at the VA Connecticut Healthcare System, and Henry Kranzler, MD, at the Philadelphia VA Medical Center. • An investigation by Adriana Hung, MD, at the VA Tennessee Valley Healthcare System, of how genes affect the risk and progression of kidney disease and hypertension, including the different responses among diabetic patients (who often develop kidney problems) to the drug metformin, based on their genetic profile. • A study, involving five VA regions and two universities, exploring the role of genetics in metabolic conditions 99
The non-invasive Answer when the Question is BLADDER CANCER Cxbladder Triage, Detect and Monitor genomic tests for the detection and management of bladder cancer • Superior performance to all other urine based tests • Portability for testing in out patient settings • Cxbladder Triage, Detect and Monitor — Optimized genomic tests with high sensitivity and specificity, and a Negative Predictive Value > 97%
• Improved compliance as a result of less invasive testing • Accurate early detection results in reduced costs, fewer invasive procedures and better patient outcomes • Cxbladder – FSS Contract # V797D-60660
www.cxbladder.com or call 1-855-292-5237
Clinically, they’re all low risk Biologically, they’re not
PSA 6.2 6 Gleason Score Onco type DX® GPS 11 Identified for
ACTIVE SURVEILLANCE
Refine risk stratification Define treatment choices
Genomic Health, Oncotype DX, and Oncotype IQ are trademarks of Genomic Health, Inc. © 2016 Genomic Health, Inc. All rights reserved. GHI40000_0716
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Since President Barack Obama launched the Precision Medicine
Initiative (PMI) in January 2015, the administration has made significant progress in advancing its goals of ushering in a new era of medicine that delivers the right treatment at the right time to the right person. The development of the infrastructure and informatics necessary to make MVP work have helped pave the way for programs like PMI.
– obesity, diabetes, and abnormal lipid levels – as drivers of heart disease. Philip Tsao, PhD, at the VA Palo Alto Health Care System and Kyong-Mi Chang, MD, at the Philadelphia VA Medical Center will lead this team of investigators. • A study evaluating the potential genetic risk factors for Gulf War Illness (GWI), and to examine the interaction between genetic variants and Gulf War environmental exposures and susceptibility to GWI. The investigation will compare 7,500 veterans with GWI to 7,500 controls. • An investigation of the genes that may make people susceptible to age-related macular degeneration (AMD), a retinal disorder that affects about 10 percent of older Americans. The MVP has enrolled more than 64,000 African-American veterans in this study, enabling researchers to identify susceptibility genes among a diverse population and to support an independent evaluation of susceptibility genes that have already been identified by other studies.
VA PHOTO/ROBERT TURTIL
THE FUTURE OF PERSONALIZED MEDICINE
The MVP, and the effort to develop the infrastructure and informatics necessary to make it work, have laid the groundwork for expanded initiatives that will combine the resources of different agencies to make personalized precision medicine possible for the nation. VA and the Department of Defense (DOD) have signed an agreement to open up MVP enrollment to active-duty service members before they transition to the VA. This activity will begin with DOD’s Millennium Cohort Study members. “You can imagine how powerful and rich that resource will be,” Muralidhar said. “It will allow investigators to learn about their health and illness, throughout their lives. We’ll be able to better predict things, when people are younger, and maybe even prevent certain illnesses. It will be a great contribution.” In his State of the Union address in January 2015, President Barack Obama announced the Precision Medicine Initiative (PMI), an effort to gain better insights into the biological, environmental, and behavioral influences on diseases, such as cancer and Alzheimer’s disease, that have thus far eluded a proven means of prevention or treatment. As part of this initiative, the National Institutes of Health (NIH) will build a national cohort, with a biobank, secure data sets, and computer networks. VA has signed an interagency agreement with the NIH, and will invite veteran volunteers to enroll
www.defensemedianetwork.com
in the PMI cohort as well. Likewise, the MVP is playing an important role in the National Cancer Moonshot initiative, introduced by Vice President Joe Biden in early 2016. Precision medicine’s greatest promise may be its potential to transform the way cancer is prevented, diagnosed, and treated. Nearly a third of the MVP enrollees have reported a cancer diagnosis, offering researchers a resource for exploration and analysis. To help in these analyses, said Muralidhar, VA has signed an agreement with the Department of Energy to make use of the expertise and large supercomputing capacity and computing expertise at several of the agency’s national laboratories, including Oak Ridge, Sandia, Livermore, Los Alamos, and Argonne. “This will allow us to conduct data analysis at a scale that is currently not possible within the VA, and it will also allow us to make the cohort data more broadly available to larger numbers of researchers in the country, across federal agencies and universities.” The ultimate goal of the MVP and PMI, of course, will be to take what’s learned from these large-scale genomic studies and use that knowledge to optimize treatments for diseases – or to prevent them entirely. It’s possible that the practice of medicine could be completely different in the span of a decade or two, and it will all have been made possible, Muralidhar said, by the altruism and patriotism of American veterans who paved the way by volunteering for the MVP. “They’ve served their country once,” she said. “And they look at this as a second opportunity to serve.” When the MVP launched its focus groups and sent out early rounds of surveys to gauge the interest of veterans, more than 70 percent said they would participate. “If you visit our website (www.research.va.gov/mvp), you’ll see quotes by many of the veterans about why they’ve chosen to participate and serve again. It’s heartwarming to see their willingness to volunteer – for the benefit of not only their brothers and sisters, but of our entire nation.” 101
NCRAR PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A research subject localizes sounds coming from an array of speakers in a specially designed anechoic (without echo) chamber.
102
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA Research: Auditory Vestibular Research By Craig Collins n AMONG AMERICAN VETERANS, THE MOST common serviceoriented disabilities are hearing-related problems, including tinnitus: the hearing of sound (often described as a ringing, buzzing, or hissing) when no external sound is present. In 2013, 1.1 million veterans received compensation for tinnitus, and more than 850,000 for hearing loss. Department of Veterans Affairs (VA) research is aimed at discovering the best practices for preventing, diagnosing, and treating hearing loss, tinnitus, and vestibular (balance and spatial orientation) problems. VA investigators study the most common cause of hearing loss – aging – but also devote considerable resources to other origins including infections, allergies, noise or blast exposure, and heredity. Much of VA’s research into auditory and vestibular issues is coordinated and carried out through the work of the National Center for Rehabilitative Auditory Research (NCRAR) at the Portland, Oregon VA Medical Center (VAMC). NCRAR researchers train and mentor new scientists, disseminate information to clinicians who assess and treat veterans, and provide educational resources to veterans and community members. NCRAR’s research program, led by Patrick Feeney, PhD, features a unique focus on auditory and vestibular dysfunction and on translating research findings into practice. The program is varied and multidisciplinary, including investigations into the basic biophysiology of the auditory and vestibular systems; the effects of age; the pathways of specific pathologies or disorders; and the effectiveness of specific evaluation and rehabilitation strategies. Tinnitus, Feeney pointed out, disproportionately affects veterans because of the greater likelihood that they’ve been exposed to loud noise. VA researchers have studied the condition for decades. James Henry, PhD, an NCRAR investigator, was recently awarded the highest honor given to researchers by the VA’s Rehabilitation Research and Development Service (RR&D) – the 2016 Paul B. Magnuson Award – for his development of an incremental treatment approach called Progressive Tinnitus Management (PTM). Developed after years of clinical trials, PTM establishes five levels of assessment and intervention that escalate with the intensity and severity of the tinnitus. The condition can range from mildly irritating (which might involve basic education in managing the condition) to severe (which would typically involve more
www.defensemedianetwork.com
intensive approaches such as sound therapy, or cognitive behavioral therapy) to completely debilitating (requiring specialized one-on-one services). PTM continues to be adopted as the program of choice in both VA and Department of Defense (DOD) hearing clinics. Meanwhile, Henry’s team is engaged in a study of the effectiveness of different types of sound-generating devices for tinnitus management, as well as a longitudinal study of the relationship between noise exposure and tinnitus – a study that might yield insight the military could use to design and modify job categories and prevent the exposures that lead to tinnitus. Another NCRAR team, led by Robert Folmer, PhD, recently completed its investigation of a treatment for chronic tinnitus, known as transcranial magnetic stimulation (TMS). An FDA-approved treatment for depression, TMS is a method of stimulating brain tissue with a magnetic field. Folmer’s team found that TMS reduced the severity of tinnitus for more than half of the participants in the treatment group throughout the six-month duration of the study. Tinnitus isn’t the only effect of blast exposure on the auditory system; research led by Marjorie Leek, PhD, and Frederick Gallun, PhD, has shown that those exposed to high-intensity blasts are more likely to experience problems with central auditory processing, or the delivery of sound information from the inner ear to the brain’s auditory cortex. Blast-related problems in neural connections, they hypothesize, may be responsible for difficulties processing rapid sequences of sounds and in understanding speech in a noisy environment. This was a significant finding: Standard hearing tests, which focus on the ear and don’t evaluate neural connections, had indicated normal hearing in many veterans who had complained of hearing difficulties in noise. The team also established that these processing deficits were long-term, lingering years after veterans’ exposure to blasts. Another investigator looking at the effects of blast exposure is Melissa Papesh, PhD, AuD, who is building on previous NCRAR studies suggesting that people who have been exposed to blasts may have a difficult time understanding speech when competing noise is coming from a different location. Papesh and Gallun are both in the early stages of exploring rehabilitation options for blast-exposed veterans with auditory processing disorders. 103
Serving America’s Military & Veterans Since Desert Shield
Why You Should Standardize with
Exergen TA Thermometers Exergen’s Value Proposition: • Improve Patient Outcomes - Exergen has MORE THAN 60 PUBLISHED STUDIES SUPPORTING ACCURACY FROM PREEMIES TO GERIATRICS IN ALL AREAS OF CARE. Unlike other thermometers, the Exergen Temporal Scanner does not come into contact with mucous membranes, thus greatly reducing the risk of cross contamination. Additionally, full instrument sheaths, protecting the entire thermometer, can be utilized for all levels of cross-contamination protection. • Improve Patient Safety - Exergen has no probe covers that can break, as often occurs with oral thermometers. With a lifetime warranty, your thermometers can be replaced whenever necessary at no charge. Exergen also has less environmental issues than other thermometer methods, increasing reliability of readings. • Reduce Costs - Exergen doesn’t require expensive probe covers, and with a LIFETIME WARRANTY, COST SAVINGS OF UP TO 90% OVER OTHER THERMOMETRY METHODS can be achieved. Other thermometers can cost more than $100 per year each for probe covers and repairs. Exergen TA thermometers cost $0 per year. • Increase Efficiencies - Exergen’s non-invasive temperature collection can be utilized on virtually any patient situation, therefore ONE THERMOMETER CAN BE UTILIZED THROUGHOUT THE FACILITY. Also, Exergen upgraded the thermometer casing to reduce or eliminate stress micro cracks that can allow harsh chemical cleaners to penetrate the material and cause fractures • Attractive Payback - Elimination of probe covers and repair costs, and easily affordable acquisition costs results in LESS THAN ONE YEAR PAYBACK for standardizing with Exergen TA thermometers. Add up these values and you’ll want to standardize with:
TemporalScanner™
For more information, please call 617-923-9900 x6234, email: medical@exergen.com, or visit: www.exergen.com
Exergen Corporation 400 Pleasant Street Watertown, MA 02472
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
NCRAR PHOTO
■■ Human electrophysiology testing using an electrode cap, as shown, can help to measure how speech sounds are coded by the brain.
Age and hearing loss are also known factors in auditory processing, and several NCRAR researchers are examining the ways in which they affect hearing, both at the functional and physiological levels: Michelle Molis, PhD, recently reported on the effects of hearing loss and aging on word recognition, and Curtis Billings, PhD, is at work measuring the brain waves of veterans in response to noise and speech. “He’s finding that in older listeners, there’s an effect in brain activity that’s different from younger listeners,” said Feeney. “These give us an objective measure of the brain function of these individuals, and establish a link to the deficits they have in their perceptions of speech and noise.” Sometimes hearing loss isn’t directly attributable to age, but to external factors whose incidence may increase with age. Dawn Konrad-Martin, PhD, and Marilyn Dille, PhD, have spent several years collaborating on investigations related to two factors known to be associated with hearing loss: diabetes and medications. It’s long been known that people with diabetes have higher rates of hearing loss, though it’s not yet known exactly why. Because about 1 out of every 4 U.S. veterans has diabetes, NCRAR studies of these associations have focused on discovering linkages that could reveal new avenues for intervention. A study published in the spring of 2016, for example, revealed that diabetes is associated with slower neural conduction to the auditory cortex – to a much higher degree than age alone – and that this damage occurs early in the diabetes disease process. Dille and Konrad-Martin also lead NCRAR efforts to investigate the problem of ototoxicity, a line of investigation first established by Stephen Fausti, former NCRAR director. Simply put, ototoxicity is the tendency of some drugs, such as antibiotics, diuretics, antiseptics, and chemotherapeutic agents, to literally poison the ear – particularly the cochlea or auditory nerve – and cause hearing loss. NCRAR researchers have developed a small handheld device, the OtoID, that will allow an individual to monitor his or her hearing before each dose of the damaging drug is administered; Feeney uses the example of a cancer patient in a treatment unit receiving an IV drip of cisplatin, a known ototoxin. OtoID, which is patented by the VA, can send a message directly to the audiologist after the test is completed, offering real-time updates and improving the odds of preserving a patient’s hearing function while effectively treating their cancer. In 2014, a team led by Konrad-Martin and Dille also published a “Proposed Comprehensive Ototoxicity Monitoring Program for VA Healthcare (COMP-VA),” a plan for implementing a monitoring regimen throughout all levels of VA health care. Dille is spearheading the next steps to be taken in gathering the data and forming the
www.defensemedianetwork.com
partnerships needed to go agency-wide with this initiative, which has the potential to mitigate hearing loss for tens of thousands of veterans. Konrad-Martin was among the first researchers to investigate a new and emerging area of study in the field of audiology: “hidden hearing loss,” or, simply speaking, a form of hearing impairment that can’t be measured by a conventional audiogram. Hidden hearing loss may be associated with the function of the eighth cranial (vestibulocochlear) nerve, which transmits sound information from the inner ear to the brain. Konrad-Martin, who has demonstrated age-related deficits in the “first wave” of activity transmitted from the eighth nerve to the brain (the auditory brainstem response, or ABR), has helped to guide the work of another NCRAR researcher, Naomi Bramhall, PhD, who recently discovered significant differences in the ABR of veterans with a history of loud noise exposure. “And over long periods of time, being exposed to loud noise,” said Feeney, “we think there could be an effect on more complicated signals. Maybe you hear tones okay, but you might have a deficit in hearing a more complex signal, requiring more of those eighth nerve fibers to respond – say, speech. A lot of this right now is theory. And work like the kind Naomi and Dawn are doing is on the forefront of trying to uncover what actually is going on with humans.” In his own laboratory, Feeney focuses much of his work on tests that can help measure how the inner ear receives and processes more complicated auditory information. One study, which he’s doing in collaboration with Douglas Keefe, PhD, of the Boys Town National Research Hospital in Omaha and Lisa Hunter, PhD, of the Cincinnati Children’s Hospital Medical Center, is examining the ability of a more versatile test battery: wideband acoustic immittance (WAI), which evaluates the middle ear’s response over a broad range of frequencies and ear canal pressures. 105
VA PHOTOS
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ LEFT: A subject conducts a self-test using the NCRAR-developed OtoID device. The hand-held tool enables users to monitor their hearing before taking doses of ototoxic drugs, and the device can relay those test results to their audiologists. RIGHT: U.S. Rep. Phil Roe, R-Tenn., watches as Dr. Ashley Clark demonstrates a new test of inner ear balance function on Owen Murnane, PhD, during a visit with the staff of the Auditory Vestibular Research Enhancement Award Program. Murnane, along with AVREAP Director Faith Akin, PhD, has been studying how exposure to loud noise affects the vestibular system.
Feeney is also at work studying the potential of a wideband test of otoacoustic emissions (OAE), the sounds that travel back out of the ear canal after an auditory signal has been received. “We want to include that as part of a test battery for veterans,” said Feeney, “because the otoacoustic emission test tells how the outer hair cells are functioning, and if you have damage to the outer hair cells you typically have hearing loss. Unfortunately, most veterans, and most adults in general, never have that tested as part of a hearing test.” Wideband OAE tests can also help evaluate patients for ototoxicity, allowing clinicians to evaluative middle ear and hair cell function together. Feeney and his colleagues are proposing a study to test them at higher frequencies than are traditionally evaluated – extended high frequencies, as they’re known. “The goal here,” Feeney said, “is to try to have the most sensitive test of ototoxicity that we can, and one that doesn’t have the false positives, due to middle ear dysfunction, that we might encounter from time to time on certain patients.” THE AUDITORY VESTIBULAR RESEARCH ENHANCEMENT AWARD PROGRAM (AVREAP)
NCRAR’s work is complemented by the work of the AVREAP, headquartered at the Mountain Home, Tennessee VAMC. The program, conducted through five distinct laboratories, aims to improve the quality of life for veterans with hearing and balance disorders. The AVREAP’s director, Faith Akin, PhD, also leads the program’s Vestibular/Balance Research Program, which explores problems – and the potential for solutions – associated with the inner ear’s vestibular organs. For the last 15 years, she and her AVREAP colleague Owen Murnane, PhD, 106
have been studying the question of what happens to the vestibular system when people are exposed to loud noises. “We’d seen patients in the VA who reported ongoing balance problems following blast exposures from as long ago as the Korean Conflict,” Akin said. “It just didn’t fit with what we knew about the vestibular system and how it recovers from damage, and there were no human studies on the effect of noise on the vestibular system.” Akin and Murnane helped drive the body of research that zeroed in on the otolith organs, the gravity sensors of the inner ear. In fish and amphibians, otoliths are the organs of hearing, but it wasn’t proven until the 1990s that otoliths in mammals also responded to sound. During that same time period, investigators in Australia developed a method to record a sound-evoked otolith response from the neck muscles of humans. Akin and Murnane’s work refined this response as a functional evaluation of otolith organs in humans, and, in later studies, discovered a correlation between the soundevoked otolith response and noise-induced hearing loss. They were among the first investigators to demonstrate a link between noise exposure and damage to the inner-ear balance system. More recently, they’ve extended this work to patients with dizziness following mild traumatic brain injury (TBI) and have observed a similar link. Akin and colleagues recently launched a new study designed to comprehensively measure the effect of loud noise on all five organs of the vestibular system – the three semicircular canals, which are sensitive to rotations of the head, and the two otoliths that sense gravity and linear acceleration – in animals and humans. “One of the things that’s been disturbing about the dizziness related to head injury or blast exposure,” she said, “is that it can last for a long time, sometimes years. Typically inner-ear
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
balance-related symptoms resolve in weeks to months.” Having a clearer sense of how loud noise affects all of the balance organs, and how each organ recovers from noise exposure, may one day help clinicians figure out ways to help patients improve their balance after a head injury or blast exposure. Though nearly everyone with hearing loss can be helped with hearing aids, only about 1 in 5 people use them, and their reasons for not using them vary widely. AVREAP’s Audiologic Rehabilitation Laboratory is directed by Sherri Smith, AuD, PhD, who studies rehabilitation strategies specific to veterans with hearing loss. Much of her work is devoted to exploring ways to make existing interventions more effective and increasing their appeal to veterans. One such study, currently underway, is evaluating the effectiveness of using a “test box,” a small, sound-treated enclosure that allows accurate measurements of a hearing aid, to determine the level ■■ Even though hearing aids can help nearly anyone with hearing loss, many people with of sound in a person’s ear when the hearing loss don’t wear them. AVREAP researchers are evaluating ways to make the use of such hearing aid is worn. Smith is comparing aids more effective and appealing for veterans. outcomes for veterans whose hearing aids are fitted and verified using this approach – which doesn’t require veterans to leave their impairs the exchange of information; it can lead to lonelihomes – to outcomes for veterans who have their hearing aids ness, isolation, dependence, and frustration – and most of fitted and verified by in-person visits to VA hearing clinics, this can be easily avoided with the use of hearing aids and which are busy and often far from where many veterans live. other interventions. “If the data show that this method is an effective way to fit It’s not the treatments that are lacking in the fight against a hearing aid accurately,” Smith said, “it will give us a way hearing loss among veterans. The most successful interto meet the needs of the veteran and save them a face-to- ventions simply require early recognition and rehabilitaface visit.” tion, but unfortunately, as with many chronic health condiSmith is also evaluating an experimental technology for tions, relatively few people with hearing loss seek treatment reducing background noise – the ambient sound one might immediately, if at all. 80 percent of hearing-impaired adults encounter in a crowded restaurant, or at a sporting event – fail to treat their hearing loss in the first five to 10 years after that often deters many people from using hearing aids. The its detection. study is comparing two hearing aids programs: one with It’s one thing to know this – and another thing to know standard programming, and the other programmed with why, and to be able to do something about it. NCRAR’s an experimental noise reduction algorithm. “If there’s a dif- associate director, Gabrielle Saunders, PhD, is leading ference between the programs,” Smith said, “it might help an effort to examine the most changeable of variables people who are highly intolerant of background noise get influencing hearing health care behaviors: the attitudes more benefit from their hearing aids while wearing them and beliefs of veterans with hearing loss. The findings in noise.” of Saunders’ group may help to guide the development of Studies like this one may ultimately help grow the per- strategies that will lead more hearing-impaired veterans to centage of veterans who choose to wear hearing aids. Health seek intervention, to reduce the secondary negative effects researchers refer to this choice as a “health behavior,” and of hearing loss, and ultimately, as they’re better able to VA’s auditory investigators understand that people’s health communicate and understand speech, to improve their behaviors directly affect their quality of life. Hearing loss quality of life.
www.defensemedianetwork.com
107
Don’t miss upcoming editions of
Sign up or update your information to assure your continued complimentary subscription and delivery.
It’s easy, just go to
www.VAMilMedOutlook.com/subscribe
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A veteran smiles for a group photo with Veterans Affairs personnel and volunteers at the Washington, D.C. VA Medical Center’s 21st annual Winterhaven Homeless Veterans Stand Down on Jan. 24, 2015. More than 700 homeless and at-risk veterans, including a number of female veterans, attended the event to receive one-on-one assistance with health care, benefits, employment, and housing. Homelessness disproportionately affects veterans, and the VA is working on several fronts to bring an end to the issue.
VA Research: Homelessness VA/ROBERT TURTIL
By Craig Collins
n ABOUT 7 PERCENT OF AMERICANS OVERALL are veterans – but veterans account for about 11 percent of the nation’s homeless population. Because it’s a problem that
www.defensemedianetwork.com
disproportionately affects veterans, the Department of Veterans Affairs (VA) attacks homelessness on several fronts: VA medical and dental providers examine and 113
■■ Then-VA Secretary Eric K. Shinseki presents the VA’s five-year plan to end homelessness among veterans during an address to VA officials, other government representatives, and private-sector homeless outreach organizers at the VA National Summit Ending Homelessness among Veterans on Nov. 3, 2009, in Washington, D.C. The plan included the establishment of the National Center on Homelessness among Veterans.
114
treat homeless veterans at dozens of locations around the country. Trained staff at the National Call Center for Homeless Veterans offer counseling and referral services to link veterans and their families to the services they need. The oldest federal health care program for veterans, the Domiciliary Care Program, was established by post-Civil War legislation, and continues to provide care and rehabilitation in residential settings on VA medical center grounds. In 2009, former VA Secretary Eric Shinseki and President Barack Obama announced the ambitious goal to end homelessness among veterans. The U.S. Interagency Council on Homelessness, representing 19 federal agencies, drafted the first-ever national strategy to end homelessness. In order to promote recovery-oriented care for homeless or atrisk veterans, the VA established its National Center on Homelessness among Veterans. The center works with community partners, university affiliates, and VA researchers across the country to analyze policy; develop and implement programs; educate and disseminate information about the problem of veteran homelessness; and conduct research. Over the past eight years, more than 85,000 housing vouchers have been distributed through the HUD-VA Supportive Housing (HUD-VASH) program, a collaboration with the Department of Housing and Urban Development to provide rental subsidy and support services to help veterans and their families sustain permanent housing. The results so far have been encouraging: According to HUD’s 2015 Point-in-Time (PIT) count, a snapshot of homelessness on a given night in America, veteran homelessness has declined by 36 percent since 2010. But much work remains to be done: The 2015 PIT count reported more than 47,700 veterans were homeless on a given night. VA homelessness researchers conduct population-based research that examines risk factors for veteran homelessness and how to prevent it, as well as program-specific investigations aimed at improving housing and health outcomes for veterans. Many of these studies are conducted with support from VA’s Health Services Research and Development Service (HSR&D). Soon after it had been established, the National Center on Homelessness among
www.defensemedianetwork.com
DOD PHOTO BY ARMY SGT. 1ST CLASS MICHAEL J. CARDEN
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Pictured from left in 2013 are Simha Reddy, MD, social worker
VA PHOTO
Megan Krampitz, and registered nurse Brian Hopps, members of a VA H-PACT team that was providing health care and related services to veterans on the streets of Seattle, Washington.
Veterans partnered with HSR&D to launch the VA Homelessness Health Services Research Initiative, which funded studies aimed at implementing best practices and improving outcomes for homeless and at-risk veterans participating in four VA programs: Housing First: Throughout the United States, the traditional approach to subsidized housing has strings attached: People are promoted into more stable, longer-term housing options after they find work or complete addiction or mental health treatment programs. This approach has worked well for some, but not so well for others, and in 2012, based on a mounting evidence base, the VA joined a growing list of U.S. and international government agencies in formally adopting a different approach, known as Housing First. Housing First’s underlying philosophy stands the traditional approach on its head: It proposes that people have a better chance of moving forward on issues of recovery and employment after they’ve established permanent access to housing. Through the HUD-VASH program, housing vouchers are unconditional, and VA support services are offered in conjunction with – and not contingent upon – this housing. Studies of the Housing First approach have revealed better long-term housing outcomes for participants, as well as better health care outcomes – fewer emergency room visits and more outpatient care visits. VA-supported housing isn’t just about putting a roof over veterans’ heads; it involves case management by a social worker and referrals for health and social services. As Stefan Kertesz, MD, a primary care physician and homeless health researcher at the Birmingham (Alabama) VA Medical Center (VAMC), points out: “Housing First is a major change of clinical philosophy and a giant logistic change at the same time. The clinical philosophy takes housing and treats it as a human right instead of a reward for doing well. And that can be uncomfortable and difficult. The logistic challenge is that a medical center may have hundreds or thousands of rental vouchers that need to be redeemed in the community as fast as possible. And that necessarily involves dealing with money, geography, and bureaucracy.” In short, VA caseworkers are
www.defensemedianetwork.com
called upon not only to resolve clinical and psychological issues, but also to solve logistical problems involving real estate, rental contracts, bill payment, clothing, and furniture. Housing First involves intense staffing requirements. To discover the best practices among VA centers – what factors contribute most to the success of the Housing First approach, given these challenges – Kertesz and colleagues designed a study called Homeless Solutions in a VA Environment (H-SOLVE). To begin with, Kertesz’s group found significant variations in the way the approach was implemented across eight different VAMCs. The group also discovered that providers who had been tasked with finding housing as a first priority often felt their case management duties were being neglected in favor of the logistical problems, and that in some cases this led to turnover and burnout. H-SOLVE, a study based entirely on interviews with VA personnel, revealed the importance both of frontline providers – who, in the more successful implementations of Housing First, are skilled and assertive in forging new relationships to secure housing, often with outside parties – and VAMC leadership, which Kertesz’s team evaluated using a scientific model known as the Organizational Transformation Model. Successful integration of the Housing First approach across VA service lines, Kertesz said, usually requires collaborative working groups, with strong support and investment from the center’s senior-most leadership – integration among working groups, and from top to bottom. “It’s not enough,” he said, “for committed social workers in the homeless service program to dedicate themselves to this task. They’re going to require collaboration and assistance from a vehicle fleet, from the information technology people, from the psychology or mental health service, from the emergency department, and others.” Homeless Veterans Patient Aligned Care Teams (H-PACT): In 2010, the Veterans Health Administration (VHA) began implementing the PACT model of care, a patient-centered, team-based approach to providing and managing primary care over a veteran’s lifetime. A year later, the VA piloted the H-PACT, tailored specifically to meet the needs of homeless veterans by addressing the many barriers to care these patients encounter. Before he became director of the VA’s National Center on Homelessness among Veterans, Tom O’Toole, MD, directed the H-PACT program, which he said differs from traditional care models in several different ways: • Open access. Because their circumstances create difficulties in making and keeping appointments, H-PACT patients can take advantage of on-demand care, with walk-in appointments available at participating locations. 115
Caring For Our Veterans is the American Thing to do When You Support VSF, you support: H Housing For Homeless Veterans H Outreach Services & Aid For Veterans of All Conflicts H Benefits For Hospitalized Veterans H Service Officer Program To Assist Families H and many other organizations.
You can donate directly to VSF at:
H www.vsf-usa.org H
or by signing up with the CFC # 11324 â&#x201E;¢ MILITARY, VETERANS & PATRIOTIC SERVICE ORGANIZATIONS OF AMERICA
VSF is a 501(c)(3) charity to which donations are deductible to the donor. VSFAd_VAMM16.indd 1
2016-10-12 1:52 PM
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
• Wrap-around, integrated services. When possible, H-PACTs avoid referrals by offering a suite of services, in addition to medical care, in one place. “Seventy percent of our clinics have food available on-site,” said O’Toole. “Most have clothes pantries. Transportation is made available to and from the clinic. You can walk down the hall and talk to somebody about getting housing, or about getting food stamps.” To the extent possible, H-PACT clinics are one-stop shops. • Holistic case management. Similarly, H-PACT services focus on outcomes in the community beyond the clinic, in housing and community services. • A specialized skill set. H-PACT providers need to both understand which services are available and necessary for homeless patients and how to engage veterans in those services. The H-PACT model has three main objectives: to engage homeless veterans in care, to address unmet health needs, and to facilitate the delivery of services that will help patients find permanent housing. The model, O’Toole said, “takes the best of PACT and builds on it ... the idea is to really engage these high-risk veterans into care, stabilize them both socially and clinically, and then be able to transition them into a PACT team as they become more medically and socially stabilized.” The H-PACT model has proliferated swiftly: There are 60 active sites throughout the United States, and O’Toole and colleagues are launching new studies and tracking results as more are established. “We’re literally building the plane as we’re learning to fly it,” he said. O’Toole’s study, Aligning Resources to Care for Homeless Veterans (ARCH), is actually a series of studies funded through the VA Homelessness Health Services Research Initiative. ARCH studies have compared outcomes of the H-PACT and traditional PACT models, along with comparisons of four different variations of the H-PACT model. So far, these studies have demonstrated that H-PACT patients, overall, had fewer emergency room visits and hospitalizations and were more engaged in ambulatory care services. In addition, compared to traditional PACT care for veterans, H-PACT care costs about $10,000 less per homeless veteran per year.
www.defensemedianetwork.com
The H-PACT, O’Toole said, “has been a pretty good program. And it’s been nice to have the funding available to design this research and create the evidence base as we’re pushing a new model of care through the VA.” Addiction Housing Case Management (AHCM): The leader of this study, Andrew Saxon, MD, is a psychiatrist in the VA Puget Sound Health Care System and director of the VA Center of Excellence in Substance Abuse Treatment and Education (CESATE). The AHCM study, Saxon said, grew out of an earlier investigation of more than 700 veterans who were entering addiction treatment. A secondary analysis of their health records revealed that among this group, veterans who were homeless had worse substance abuse outcomes. “They also utilized more in-patient and emergency services,” Saxon said, “and were generally a sicker population.” Saxon then launched the AHCM study, aimed at improving outcomes for homeless veterans entering addiction treatment: Among 181 homeless veterans in Seattle, Washington, Saxon’s team randomly assigned some who were being treated for addiction – the experimental group – to an addiction/ housing case manager who would simultaneously address the issues of homelessness and substance abuse. The experimental intervention was based on an evidence-based model known as assertive community treatment (ACT), designed to overcome the chaotic circumstances that often prevent patients with chronic mental illness from receiving services. In ACT, a caseworker is expeditionary when necessary. Rather than wait for clients to arrive, he or she ventures out into the community to find clients and connect them with services – with a psychiatrist or social worker or physician, for example. Saxon’s control group, also veterans receiving addiction treatment, attended a weekly drop-in housing group led by two accomplished social workers. The AHCM was designed to evaluate whether AHCM resulted in earlier transition into housing and/or more stable housing among veterans entering addiction treatment, and Saxon’s team learned that it didn’t appreciably improve housing outcomes. “What we found,” he said, “was that about two-thirds of the participants, regardless of experimental condition, ended up housed at the end of a year. But onethird didn’t end up housed.” Saxon’s team had early difficulties finding a sizeable population; the study was designed for an era when substance abuse treatment might have been a requirement for housing. When the VA adopted Housing First as its approach, it delinked housing and addiction treatment, and many potential participants had no incentive to join the AHCM study. Another unexpected discovery was that the adapted AHCM 117
VA PHOTO
■■ Stephen Iadeluca, center, a veteran who suffered a work-related injury that eventually led to homelessness, turned to the VA and benefited from the H-PACT model of care – an approach established by Tom O’Toole, MD, right.
■■ Missy Frazier, a VA nurse, provides a basic health screening to a local homeless veteran in Reading, Pennsylvania, during a Military Veterans Stand Down at GoggleWorks Center for the Arts, a three-day event to provide essential services to homeless veterans in the Reading area. VA homelessness researchers examine risk factors for veteran homelessness, how to prevent it, and ways to improve housing and health outcomes for veterans.
118
approach applied resources that many potential participants viewed as simply too overwhelming, given their already difficult lives. The AHCM study is a good illustration of how difficult it can be to isolate variables in such a perplexing social context. The study doesn’t prove that AHCM doesn’t work; it simply showed that it didn’t work given the complexities of this group. Further explorations of the differences between participants who did and didn’t end up in housing at the end of the year may reveal more about the complex relationship between homelessness and addiction. Re-Engage: About a decade ago, VA researchers discovered that veterans with severe mental illnesses such as schizophrenia or bipolar disorder were at higher risk for homelessness and “unforeseen mortality” – deaths despite little or no time spent in inpatient care over the previous year. On the heels of these findings, the VA developed the Re-Engage program: Using an algorithm to identify at-risk veterans, caseworkers were given a list of veterans in the surrounding community and a toolkit of resources – an informational web portal, a brief training session via conference call, and the availability of a technical assistance hotline – that could be used to find them and bring them back into the VA health care system. After the program had been established, a team led by Amy Kilbourne, PhD, MPH, director of the VA’s Quality Enhancement Research Initiative (QUERI) examined outcomes among close to 5,000 veterans with severe mental illness who had been lost to care. The team’s findings were striking: 72 percent were successfully returned to care, and among those who returned, there was a sixfold decrease in unforeseen mortality. In other words, homeless veterans with severe mental illness who were returned to care through Re-Engage were six times more likely to survive. With HSR&D funding, Kilbourne’s team then designed a study to test whether Re-Engage outcomes could be further improved by an enhanced implementation strategy, the facilitation model. In addition to the resources available to caseworkers in the original program, the facilitation model involved weekly collaboration with a trained facilitator, a mental health professional with knowledge of Re-Engage, and the VA organization. In the enhanced program, the facilitator and frontline provider worked closely together to overcome barriers to implementing Re-Engage, both on the patient side and the institutional side – making sure clients and colleagues alike were aware of the program’s benefits. Kilbourne’s study compared the standard and enhanced strategies at randomized VA sites. “We
www.defensemedianetwork.com
PHOTO BY SPC. DAVID THOMPSON
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Individuals who took part in the 2013 count of Portland, Oregon area homeless gather outside of the Portland VAMC’s Community Resource
VA PHOTO BY KELLI D. FOESCH
& Referral Center, which serves homeless veterans, or those at risk of becoming homeless, with access to care and benefits. During the last week of January, the VA, the U.S. Department of Housing and Urban Development, and local agencies across the country conduct Point-in-Time (PIT) counts to get a statistically reliable, unduplicated count of sheltered and unsheltered homeless veterans, individuals, and families in the United States. While much progress has been made to eradicate veteran homelessness, the 2015 PIT count of 47,700 veterans homeless on a given night means there is still work to be done.
found that more providers implement Re-Engage if they’re receiving facilitation,” Kilbourne said, “versus providers who only received the standard toolkit. So the additional support and training with facilitation got more providers to implement Re-Engage.” Her team is still examining patient-level outcomes among the veterans who took part at the test sites, but the study has already had an effect, Kilbourne said: “We showed that this facilitation program works, and subsequent to that, the VA mental health operators, our clinical leadership in VA, have adopted the facilitation model and are using the facilitation model to continue to run the Re-Engage program.” The enhanced approach is now the approach to implementing Re-Engage, and is tracked as a national program in the
www.defensemedianetwork.com
VHA’s performance measures system, the Strategic Analytics for Improvement and Learning (SAIL) database. Changing the way one of the largest integrated health care systems in the world delivers services to the tens of thousands of veterans who struggle to find and maintain housing is a colossal undertaking. Kertesz compares it to “turning around the Queen Mary.” But as VA researchers work to learn more about the problem of veteran homelessness and to extend the reach and capabilities of the professionals who work with homeless veterans, there’s plenty of reason to hope the number of homeless veterans will continue to decline – and that more of those veterans who do find themselves homeless, for whatever reason, will receive the care and services they need. 119
Phoeni An exoskeleton to enhance possibilities
Features:
SuitX has developed the Phoenix exoskeleton; the world's lightest and most advanced exoskeleton designed to help people with mobility disorders to be upright and mobile in the clinic, at home, and in the workplace. Phoenix is only powered at the hips; with unpowered knee joints which would allow support during stance and ground clearance while walking. This minimal and intelligent design allows for organic and non-robotic gait, agility, light weight, comfort, affordability and robustness.
A modular exoskeleton that allows the user to independently put on and remove each piece. Weighs only 12.25kg (27 lbs), affording greater agility. On a single charge, Phoenix can last 4 hours of continuous use or 8 hours intermittently. Phoenix is adjustable for different size users and can easily be configured to fit individual conditions. The intuitive interface is designed for users to control standing up, sitting down and walking. Phoenix modular design provides the ability to put on the suit independently while sitting in a wheelchair. An Android app allows for tuning the device parameters and collection and storage of user data.
Phoenix is composed of a hip exoskeleton and two orthotic legs. Custom made orthotic legs work to create comfort and agility. Universal orthotic legs are designed to fit a wide range of users.
Phoenix is an investigational device, and is limited by federal (or United States) law to investigational use.
MA An exoskeleton to enhance capabilities Logistical and support operations have the ability to influence the planning and execution of all aspects of warfare. MAX is designed to enhance capabilities and avoid injuries of skilled personnel.
MAX (Modular Agile eXoskeleton) is a versatile exoskeleton that can allow its wearer to complete shoulder, lower back, and leg intensive tasks with reduced injury risk while remaining comfortable enough to wear all day. MAX is composed of three exoskeleton modules: BACKX, ARMX, and KNEEX. Applications: logistics, construction sites, shipbuilding , material handling , distribution centers, storage, maintenance, foundries, factories, assembly operations, airports and palletizing facilities. All SuitX products intelligently engage when you need them, and donâ&#x20AC;&#x2122;t impede you otherwise. Ascending and descending stairs and ladders, driving, and biking are completely unimpeded.
www.suitx.com Emeryville, California
Armx ARMX is an arm exoskeleton that augments its wearer by reducing forces at the shoulder complex, enabling the wearer to perform above the head tasks for longer durations and with less effort.
BAckX BACKX is a novel trunk support exoskeleton that reduces the forces and torques on a wearerâ&#x20AC;&#x2122;s lower back region (L5/S1 disc) by an average of 60% while stooping, lifting objects, bending or reaching.
KneeX KNEEX is a leg exoskeleton that allows the wearer to squat repeatedly or for prolonged periods of time by reducing the forces on the knee joint and the quadricep muscles.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA Research: Improving Equity and Reducing Disparities in Health Care By Craig Collins n WHEN THE DEPARTMENT OF VETERANS AFFAIRS (VA) released its Strategic Plan for FY 2014-2020, it noted that the veteran population overall – 21.8 million, according to the 2014 U.S. Census – was undergoing dramatic demographic changes. The majority of veterans today is predominantly male and white, with the largest cohort having served during the Vietnam War. But over the next 25 years, as Gulf War veterans overtake Vietnam veterans as the largest group, the percentage of white male veterans is set to decline by nearly 48 percent. Meanwhile, the percentage of several other groups – women, African-Americans, Hispanics, and other nonwhite veterans – will increase. By 2040, women will be nearly 20 percent of the veteran population, and 34 percent of all veterans will be nonwhite. American veterans, then, are increasingly from populations the federal government – including the VA, the Department of Health and Human Services, and other health-related agencies – considers to be “potentially vulnerable patient populations.” Veterans from these groups are at risk for receiving lower-quality medical care, or for having worse medical outcomes, than patients from the majority. A higher percentage of nonwhite adults, for example, suffers from at least one of seven chronic conditions – asthma, cancer, heart disease, diabetes, high blood pressure, obesity, or depression. In 2001, the Institute of Medicine (now the National Academy of Medicine) released a framework outlining six aims for the nation’s 21st century health care system: Medical care, the report stated, should be safe, effective, patient-centered, timely, efficient, and equitable, meaning “Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.” The VA aims to minimize disparities – significant differences, either in health status or in the quality of health care 122
– among vulnerable patient populations, both in the delivery of care and in a robust research program conducted on a vast number of fronts: • The Cooperative Studies Program Epidemiology Center, founded in 1997 on the campus of the Durham, North Carolina VA Medical Center, conducts population studies investigating sources of disparities in health care and health outcomes among veterans. • The Center for Health Equity Research and Promotion (CHERP) was established in 2001 as a national Center of Excellence focused on detecting, understanding, and reducing disparities in health and health care in vulnerable populations. Co-located at the VA Pittsburgh Healthcare System and the Philadelphia VA Medical Center, CHERP promotes equity by conducting research, partnering with VA clinicians and policy stakeholders, and training and mentoring beginning researchers – fellows, medical students, and residents. • The Health Equity and Rural Outreach Innovation Center (HEROIC) in Charleston, South Carolina, began in 2004 as a targeted research initiative, focused on rural health outcomes, equity, and obstacles to care. In 2013, HEROIC became a VA Center of Innovation (COIN), focused on advancing the implementation of evidencebased interventions and developing innovative research methodologies for health equity data. • VA has a long-standing and extensive research portfolio and network of investigators nationwide, focused on addressing health disparities among veterans. There are no simple explanations for differences in health or the quality of care between groups, but the good news is that, as the nation’s largest health care system, the VA offers a unique opportunity to study the many applicable variables and to develop and evaluate patient-centered and culturally sensitive ways to deliver care.
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A tribal veteran speaks with Lourdes E. “Alfie” Alvarados-Ramos, director of the Washington State Department of Veterans Affairs, at the
VA PHOTO BY BRET BOWERS
6th Veterans Training Summit, held April 17-18, 2015, at the Swinomish Conference Center in Anacortes, Washington. The objective of these summits is to invite tribal leaders, tribal veterans, tribal veterans representatives, tribal health directors, as well as other federal and state partners who work with American Indians and Alaska Natives for services and benefits to collaborate, educate, and network to better serve this population. While white males make up the majority of veterans today, by 2040, women will constitute nearly 20 percent of the veteran population and 34 percent of all veterans will be nonwhite. The Department of Veterans Affairs is already working to address disparities in health outcomes among minority groups, with the ultimate goal of providing equitable care to all patients regardless of gender, ethnicity, socioeconomic status, or geographic location.
In 2006, a group of VA researchers led by Amy Kilbourne, PhD, and including CHERP’s director, Michael Fine, MD, MSc, published a conceptual framework in which it outlined three phases of health disparities research: detection, understanding, and reduction/elimination. Detection means acquiring the knowledge that disparities exist – knowledge typically discovered through epidemiological studies of large patient populations. The second phase of research, aimed at understanding why these disparities exist, is more complex. “The explanation,” said Fine, who is also an attending physician in the VA Pittsburgh Healthcare System, “is usually multifactorial. Some factors can be at the patient level – based on patient beliefs, or patient biology, or on differences in demographic characteristics.” Other factors, Fine said, may be provider related: “Do they harbor some type of implicit or explicit bias? How do they communicate with one group of patients versus another group of patients?” A third category of institutional factors could exist at the level of the medical center, or the health care system
www.defensemedianetwork.com
itself, ingrained in policies or practices. And finally, a host of social and environmental factors, existing completely outside of the health care system, may be at work. Third-generation studies evaluate strategies or interventions aimed at reducing or eliminating disparities. “So what can we do,” said Fine, “once we’ve detected a disparity and understand its root causes, to eliminate a disparity between a vulnerable and a non-vulnerable population? The goal of our center – and the goal of most people invested in health equity research – is to move the continuum from first- to second- to third-generation work, to ultimately make a difference and reduce health disparities.” THE CONCEPTUAL MODEL IN ACTION
A good example of one who has moved the continuum of research in this way is Said Ibrahim, MD, co-director of CHERP and a physician at the Corporal Michael J. Crescenz VA Medical Center in Philadelphia. Ibrahim’s research, 123
Automated needle retraction effectively
reduces the risk
of needlestick
injuries
Activated VanishPoint ® syringes require less disposal space than other safety syringes & prevent disposal-related injuries.
VISIT RETRACTABLE.COM TO LEARN MORE ABOUT OUR
OTHER AVAILABLE SAFETY PRODUCTS
VanishPoint ® Blood Collection Set
VanishPoint ® Blood Collection Tube Holder
VanishPoint ® IV Catheter
Patient Safe ® Syringe
NEW
EasyPoint ™ Retractable Needle
N E E D L E S T I C K P R E V E N T I O N T H AT M E E T S Y O U R N E E D S
P : 9 7 2 . 2 9 4 .17 7 0 • F : 9 7 2 . 2 9 4 . 4 4 0 0 To l l F r e e : 1. 8 8 8 .7 0 3 .10 10 r t i s e r v i c e @ va n i s h p o i n t . c o m 511 L o b o L a n e • L i t t l e E l m , Tex a s 7 5 0 6 8 • U S A
VA PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ LEFT: CHERP co-director Said Ibrahim, MD, MPH, right, a staff physician at the Cpl. Michael J. Crescenz VA Medical Center (CMC VAMC)
in Philadelphia, Pennsylvania, and professor of medicine at the University of Pennsylvania’s Perelman School of Medicine, shown here with Daniel Hendee, CMC VAMC medical center director, has long focused his research on health equity and disparities, particularly in the area of osteoarthritis care. One of Ibrahim’s studies is the first-ever third-generation intervention trial to reduce a well-documented disparity. RIGHT: Ibrahim’s third-generation intervention trial found that educating minority patients, particularly African-American veterans, about the risks and benefits of hip or knee replacement procedures increased their likelihood of undergoing the surgery by nearly 85 percent.
funded continuously by the VA and the National Institutes of Health for the past 15 years, has focused particularly on racial disparities in the use of knee and hip replacement surgery in the management of advanced osteoarthritis – procedures that are on the rise nationally as the American population ages and the incidence of osteoarthritis increases. When Ibrahim’s team examined knee and hip replacement utilization nationwide, they found that minority patients, and particularly African-American veterans, were significantly less likely than non-minority veterans to undergo the procedures when they needed them. The team’s second-generation studies were designed to discover why this disparity existed. They yielded a surprising result. Ibrahim examined several issues and was able to eliminate them one by one: Though joint replacements are elective procedures, among the most expensive funded through U.S. health care plans, the motivations weren’t financial. “Obviously insurance is not a problem in the VA, because everybody is insured,” Ibrahim said, “and in fact, outside of the VA, the majority of these procedures are paid for by Medicare.” Ibrahim also looked into whether there was a difference in how orthopedic surgeons treated African-American patients, and discovered that this wasn’t a significant issue, either; VA surgeons would generally operate on anyone who elected to undergo the procedure. “We didn’t find any bias on the part of physicians in terms of the treatment recommendation,” Ibrahim said. What remained to be studied were the patients. “We found that minority patients, both at the VA as well as outside of the VA, are significantly less willing to try knee or hip replacement, compared to non-minority patients,” said Ibrahim,
www.defensemedianetwork.com
“and we found out that part of the reason is that there is actually a lot of misinformation about the risks and the benefits of the treatment. Minority patients don’t have enough information about the complications from the treatment. They tend to exaggerate it, and they don’t actually have a whole lot of family or friends who have had the procedure, compared to white patients.” Ibrahim’s next study was the first-ever third-generation intervention trial to reduce a well-documented disparity. “We educated minority patients, before they actually saw the orthopedic surgeon about knee or hip problems,” Ibrahim said. “And what we found, to our surprise, was that educating minority patients about the risks and benefits of hip or knee replacement increases their likelihood of undergoing the surgery by almost 85 percent.” Ibrahim’s findings are to be published soon in the journal JAMA Surgery. It’s worth asking why, given the time, attention, and resources paid to health disparities by researchers from the VA and other agencies, it’s taken so long for a third-generation trial to succeed in reducing a health care disparity. The answer lies in the complexity of the problems investigated. Ibrahim’s findings, for example, raised several more questions that could have been investigated. Why, for example, did minority patients tend to exaggerate the negative complications of joint replacement surgery? Where did the misinformation come from? But Ibrahim was able to apply Occam’s razor, designing an intervention aimed at the most easily addressed problem – the information gap that seemed to be the primary reason for minority patients’ unwillingness to undergo joint replacement. Teasing apart the variables contributing to health disparities among racial and ethnic minorities isn’t easy, particularly 125
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Leslie Hausmann, PhD, a core investigator at CHERP in Pittsburgh,
when they deal with patient-provider relationships or institutional practices and policies. Somnath Saha, MD, a researcher and physician at the Portland VA Medical Center, has spent the past 10 years studying the issue of “cultural competence,” which has become a catchall term describing one’s ability to interact effectively with people of different backgrounds. In order to determine whether interventions – training programs to develop cultural competence – could be designed to reduce disparities, Saha first had to do two things: come up with a useful and distinct definition of the term, and develop a valid means of measuring it. Saha’s research team surveyed 800 primary care doctors across the country and, after analyzing the responses, developed six distinct scales that could be used to measure cultural competence. The team used those scales to examine differences among HIV care providers and, in 2013, reported that providers who scored higher in cultural competence delivered more equitable care among white and nonwhite patients – most of whom were African-American. A second study, among VA patients with diabetes, found that among the six concepts evaluated, the one that had the greatest impact on racial disparities was “valuing diverse perspectives,” a scale that Saha said measured a provider’s openness to hearing about a patient’s values and health beliefs. “Among people who scored high on that scale,” Saha said, “their white and black patients basically did the same. But black patients rated them much lower than white patients when they scored low on that scale.” For Saha’s team, the next question that needs to be answered is: What do providers who score high on this scale actually do differently when they’re with patients? What does open-mindedness look like? They recently launched a study in which they’ll observe VA physicians who score high and low on that scale, and compare what they actually do and say when they’re with patients. “The study is called ‘Opening the Black Box of Cultural Competence,’” Saha said. “We want to find out what’s in the box that translates into better care.” Another issue that’s been studied by VA researchers is perceived and unconscious biases in the health care system. Leslie Hausmann, PhD, a core investigator at CHERP in Pittsburgh, investigates how different types of discrimination and bias can affect a VA patient’s health care experience and his or her health status. Her research has demonstrated that perceived discrimination is negatively associated with outcomes such as patient-provider communication, trust in physicians, health status, and utilization of preventive health care services in patients with common medical conditions, including osteoarthritis, diabetes, heart disease, and hypertension. In 126
a 2015 study, she also reported that unconscious racial bias among providers is associated with poorer psychosocial outcomes for individuals with spinal cord injury. In 2014, Hausmann, in partnership with the VA’s Office of Health Equity (OHE), piloted a curriculum for a training program aimed at raising awareness of unconscious bias among providers. The curriculum was pilot-tested at three different VA facilities. “It was an innovative project,” Hausmann said, “that brought a lot of people across the VA together to focus [on] how unconscious biases permeate our interactions with each other and with patients – and strategies to try to make patient care experience as positive as possible, no matter who the patients are.” The goal of the curriculum wasn’t necessarily to eliminate biases, but to encourage providers’ understanding that biases are real and can affect interactions with patients. “This was one of the first efforts to systematically evaluate a curriculum to train providers to understand the presence of unconscious bias,” said Hausmann, “and how it can play out in their interactions with each other and with their patients.” In addition to exploring how patient-provider relationships affect disparities, other researchers are examining a multitude of additional factors such as patient preferences, health care beliefs, health care system issues, and social context. This research has informed the development of initiatives to reduce disparities, including novel storytelling models to improve patient engagement and self-management of chronic diseases such as hypertension as well as interventions that target veteran behavior and experience through multifaceted approaches sometimes including family, peers, and social networks. Some of the most difficult variables to account for in health disparities research, said Fine, involve social determinants of health – factors outside the health care setting. “I think we’re really becoming much more aware of the fact that within the health care system, there are only so many things we can do,” he said. “And unless we get beyond the health care system and understand where patients live and what factors influence them during the 99 percent of the time they’re outside
www.defensemedianetwork.com
PHOTO BY BILL GEORGE
Pennsylvania, has found through her research that perceived discrimination can negatively affect a patient’s health care experience and his or her health status.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ This graphic, developed in part by the VA’s Office of Health Equity
(OHE), illustrates the difference between equality and equity in health care. Since its establishment in 2012, the OHE has supported the VHA’s vision to provide appropriate individualized health care to each veteran in a way that eliminates disparate health outcomes and assures health equity.
the health care system, it’s going to be very difficult to make meaningful change.” For example, rural Americans, compared to their urban counterparts, confront several obstacles – long distances to VA facilities, lack of specialty and urgent care within rural VA clinics, and shortages of providers – to quality care. These circumstances can adversely affect the health of rural veterans, who typically report lower health-related quality of life than urban veterans. Leonard Egede, MD, director of HEROIC in Charleston, recently studied an intervention designed to overcome the difficulty older rural patients often have in accessing mental health care professionals from where they live. “We did eight sessions of behavioral intervention by video phone,” Egede said, “and we found that, compared to a face-to-face visit, it was just as good. That’s the first large study to show you can actually provide care for rural veterans using video teleconferencing.” The study of more than 200 veterans was reported in The Lancet in July 2015. Egede is now at work on a study to evaluate, among veteran and non-veteran patients alike, the effectiveness of telemedicine in the treatment of Type 2 diabetes.
VA IMAGE
RESEARCH INTO PRACTICE
The establishment of the VA’s OHE in 2012 was intended to invigorate the work of CHERP and HEROIC investigators, and other health care researchers throughout the VA, to measure progress, chart the path forward, and translate research into health care practices and policies. OHE is also charged to champion efforts to address health disparities through education, training, communications, programs, projects, and initiatives that combine efforts and break down silos in the organization. One of the first achievements of the OHE, led by Uchenna Uchendu, MD, was to develop and publish the “Health Equity Action Plan,” a strategic roadmap for reducing health disparities throughout the VA health care system and position VA as a leader in this area.
www.defensemedianetwork.com
In 2015, the OHE announced and funded a new initiative and identified a core investigator through the VA’s Quality Enhancement Research Initiative (QUERI). The project is designed to establish a clear link between VA researchers, clinical practice, and operations specific to addressing health care disparities. The Partnered Evaluation Initiative is led jointly by Uchendu and by Donna Washington, MD, MPH, an investigator at the VA’s Center for the Study of Healthcare Innovation, Implementation and Policy (CSHIIP) in Los Angeles, California. While the work done thus far by VA investigators has revealed many disparities among VA patients and done much to advance our understanding of them, Washington said the knowledge base remains incomplete: “So often there may be a lack of information about some of the smaller racial and ethnic groups,” she said, “or there may be particular conditions that haven’t been examined. So what we’re doing here at the Partnered Evaluation Center is systematically using VA data to describe where the disparities are in health and health care for vulnerable populations.” According to Uchendu, the Partnered Evaluation Initiative’s three basic goals are to: • assess current gaps in morbidity and mortality for conditions among vulnerable veteran populations; • examine trends in quality of care across the conditions observed in these populations; and • assess how new models of care, such as telemedicine, affect health and health care disparities. The linkage between the Partnered Evaluation Center and the OHE, Washington said, will push data with a clinical orientation to an office well positioned to act on it. Work supported by the initiative can then be used to inform policy, education, resource allocation, operations, and practice. “We hope to produce actionable data that all stakeholders can use to address disparities,” Uchendu said. It should be pointed out that the connection between health disparities research and clinical practice isn’t new at the VA; for one thing, it already exists organically, as many researchers, including Fine, Ibrahim, Saha, Egede, and Washington, are practicing VA physicians who see patients regularly. The idea behind the Partnered Evaluation Initiative is to create a higher-level engagement between research and clinical operations – and ultimately, to bring department-wide change that will provide the same level of highquality care and improve health for all veterans, regardless of demographics. 127
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Addressing Opioid Use Disorder and Transforming Pain Management in the VA By Gail Gourley
n OVER THE LAST SEVERAL YEARS, the health care community, the federal government, and the media have focused enormous attention on the epidemic of overdose deaths from opioids – including prescription opioid pain relievers and heroin – in the United States. According to the Centers for Disease Control and Prevention (CDC), more people died from overdoses in 2014 than any year on record, with more than 60 percent of those involving an opioid and half of those involving a prescription opioid. The vast topic of pain management is inherent in addressing the opioid problem, and the Department of Veterans Affairs (VA) has concentrated significant effort to develop systemwide approaches to both transforming pain care in the VA 128
and in preventing and treating opioid use disorder (OUD) among veterans. In addition to the alarming rates of overdose deaths, chronic pain as a major public health problem has also gained increased attention. “Approximately 30 percent of the U.S. adult population have some kind of chronic pain, and it’s much higher in the VA – 50 to 60 percent,” according to Rollin M. Gallagher, MD, MPH, national program director for pain management for the VA and clinical professor of psychiatry and anesthesiology at the University of Pennsylvania. The VA has seen a huge influx of patients from recent wars who were exposed to extreme battlefield environments. In addition to experiencing severe musculoskeletal injuries,
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ OPPOSITE: With opioid-related overdose on the rise, the
VA PHOTO BY ROBERT TURTIL
LIBRARY OF CONGRESS PHOTO BY HENRY ULKE
Department of Veterans Affairs is taking steps to protect veterans by conducting research and implementing an opioid safety initiative to reduce and/or better manage opioid use. LEFT: A Civil War soldier displays a battle wound to his arm. The problem of wounded service members managing pain with opioids and subsequently becoming addicted has a long history. ABOVE: A Vietnam veteran salutes during Veterans Day events at the Vietnam War Memorial in Washington, D.C. The VA sees patients dealing with chronic pain that can stem from a range of things, including blast injuries sustained in recent conflicts or conditions associated with aging.
Gallagher explained, veterans have survived blast injuries due to advanced far-forward emergency medicine care, but now return with traumatic limb and facial injuries as well as nerve damage and traumatic brain injury. All these injuries cause pain, which can be compounded by psychological effects of battlefield exposure and post-traumatic stress disorder (PTSD). And, Gallagher said, “We have Vietnam veterans who are developing all the diseases of aging that cause pain. A whole confluence of things make the challenge even more daunting in the VA system.” And that complex challenge involves not just pain management, but also opioids and OUD. “The risk of opioid use disorder is a growing problem in the VA over the same period of time that it has been for the larger U.S. population,” said Karen Drexler, MD, acting national mental health program director for addictive disorders in the VA and associate professor of psychiatry at Emory University. “There are similar factors contributing to that as well as some that are unique to veterans. People with post-traumatic stress disorder are at increased risk for developing substance use disorders (SUD), and we know from our own internal VA data that that is certainly true among veterans as well.” An historical perspective helps to explain the context and precipitating factors of the current epidemic. “Opioid use disorder in the United States has a long history,” said Drexler. “The first epidemic in this country was in the late 1800s, and like with the current epidemic, it was multi-factorial.”
www.defensemedianetwork.com
Among those factors, Drexler said, was an accelerated development of new chemistry technology, which allowed isolation of the active ingredient from the opium poppy to develop new medicines like morphine. Injured Civil War soldiers were able to survive what previously would have been fatal injuries by enhanced surgical techniques and improved pain control, but some became addicted to the morphine. “But another development,” Drexler continued, “was that the opioids were included in patent medicines and were widely promoted for treating all kinds of pain – headaches, non-life-threatening types of painful conditions. So by the late 1800s, it was a huge problem that many in mainstream society were addicted. Congress felt compelled to act upon it, and passed the first laws restricting access to opioids, cocaine, and other potentially addicting substances.” Other major opioid epidemics included the late 1950s and 1960s epidemic that involved heroin, Drexler said, “that made the headlines because of the life-threatening nature of this addiction – that people were dying of overdose. That led to the development of methadone as an effective and lifesaving medication for treating opioid use disorder.” The 1980s saw changes in thinking about pain management, with advances in cancer treatment and end-of-life care and emphasis on compassion and pain relief. With success in using opioids in those situations, which are closely monitored settings, Drexler said, “doctors began to feel more comfortable prescribing opioids. And then there were a few reports published in the medical literature suggesting that you could provide opioids safely for non-cancer, non-end-of-life care, and 129
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ During Prescription Opioid and Heroin Epidemic Awareness Week, Sept. 18-24, 2016, VA Secretary Robert A. McDonald took part in a
that patients would not develop addiction or other adverse events. Those were highly promoted. Doctors were told, ‘You just need to screen folks to make sure they don’t have a substance use disorder, and if they don’t, you can use opioids safely and effectively to treat all kinds of pain.’ And we did.” Gallagher noted, “The other forces that were sort of pushing our society towards using opioids were the increased recognition that pain is disabling and the costs of pain to employers and to the country in terms of disability, but also the fact that the medical system was not really allowing providers the time, nor training them with the skills, to manage pain.” Consequently, he continued, “With little time to do comprehensive evaluations, and with little training in terms of how to treat pain except with a pill as documented by the Institute of Medicine (IOM) in its 2011 study, ‘Pain in America,’ and the recently published National Pain Strategy, patients and doctors naturally went to that solution and continued that … so you ended up with a whole spectrum of people taking higher doses, which led to the problems of overdose and addiction.” Additionally, Gallagher explained, access was minimal to treatments that could substitute for use of medications, 130
like the psychosocial intervention of cognitive behavioral therapy (CBT), or complementary and alternative medicine treatments, like acupuncture, that are effective for pain. “So doctors didn’t know how to start those [treatments], how to get them paid for, and then in due course went to opioids and other pills more exclusively as their treatment of choice,” he said. So in that context, said Drexler, “Sales of opioid pain medicines increased dramatically starting in the early 1990s, and by 2012, the CDC recognized that that increase in sales was also followed by a parallel increase in the number of opioid overdose deaths and in the number of patients seeking treatment for an opioid use disorder. All of these had more than quadrupled over that period of time. “That got everyone’s attention, and particularly here in the VA, we became concerned about veterans who were receiving opioid pain medicines and also who were at risk for opioid use disorder,” she said. In a broad response to that concern, the VA is addressing pain management and tackling OUD with multiple efforts focused on prevention, treatment, and ongoing research. Prevention begins early in the process as patients present with pain. “That’s where the real action is, that I think is
www.defensemedianetwork.com
VA PHOTO
roundtable discussion on efforts to assist veterans suffering from opioid use disorder.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Acupuncture is an alternative method of pain management that
has received increased attention from the VA, which has worked with the Department of Defense to train health care providers in battlefield acupuncture.
very exciting for the VA,” said Gallagher. “Not only have we worked closely with HHS [Department of Health and Human Services] on developing the National Pain Strategy, where they call out the VA’s approach, but we’ve also in the VA been able to institute some very rigorous training programs to skill-up our workforce and offer additional alternative treatments for pain when it starts, or when it first comes up in the VA system with a veteran.” These are training programs like for acupuncture, Gallagher explained, and this training is one example of several education programs that the VA and the Department of Defense (DOD) work jointly on to improve pain management in both organizations. “We’ve trained, with the DOD, over 2,400 providers in battlefield acupuncture across the system,” he said. “But more importantly in terms of sustainment, we’ve trained over 100 medical acupuncturists who are now faculty in their facilities across the system, who are trained now to train every provider – nurse practitioner, PA [physician assistant], or physician – that wants training in battlefield acupuncture and [to] be able to use it as a frontline treatment right in the clinic and not wait until after the pain has gone on too long or after pills haven’t worked or after they’re already exposed to opioids.” Other examples of therapies emphasized in the primary care setting as an alternative to opioids include CBT, exercise, physical therapy, yoga, and meditation. Gallagher said those kinds of treatments make a difference long-term in chronic pain and may prevent exposure to opioids in the beginning. Another example of the VA’s response is its Opioid Safety Initiative (OSI), piloted in 2012 and rolled out nationwide in 2013. “Since that time, we have had tremendous success in reducing the risk of opioid use disorder among veterans by improving pain management and reducing unsafe opioid prescribing,” said Drexler. As evidence of the effect of the multiple VA efforts, Drexler provided the following comparison figures: From 2011 to 2014, the number of “CMS Part B” [Medicare] enrollees using opioids for non-cancer, non-palliative care increased by 22 percent. In the VA, opioid utilization over that same time period decreased by 7 percent, even with an increase in the VA patient population. The OSI includes multiple components focusing on education for patients and care providers as well as monitoring opioid prescribing safety practices with mechanisms for feedback and support. For example, “Recognizing the risks of opioids long-term, we developed a policy that every veteran who’s going to be considered for long-term opioid therapy [more than three months and not for palliative or cancer care] undergoes a signature informed consent procedure
www.defensemedianetwork.com
where they’ll actually go through a whole educational program about pain itself, all the different treatment approaches for pain and particularly going over the risks of opioids,” explained Gallagher. Other components of the OSI utilize software tools “to help providers know when they may be over-relying on a certain type of treatment like opioids, and then giving them individual support and instruction through academic detailing, which is monitoring care, feeding back outcomes of that care to the providers, and then providing instruction and support,” Gallagher said. “That really helps them change their prescribing behaviors as well as learn new ways of managing pain.” But Gallagher pointed out that pain is a symptom in some serious chronic conditions that require not just alternative approaches but also skillful use of medications. “Opioids are part of a toolbox and providers need training, and we’re doing that right now across the whole system to train all of our providers in safe opioid prescribing, to treat pain in many different ways and avoid over-exposure to opioids,” he said. In addition to pain management education, Drexler pointed to another prevention effort. “We have been increasing our screening [for SUD] by teaching primary care providers and others who are managing pain about opioid use disorder, its risk factors, how to recognize signs and symptoms, and how to make appropriate referrals for treatment of opioid use disorder,” she said. This is in conjunction with integrating onto the primary care team mental health professionals, who can assist with making a diagnosis of OUD if appropriate and with bringing addiction medicine into pain management. In addition to prevention strategies and education to reduce the risk of OUD, Drexler said another of their targeted efforts in the VA is to increase access to medicationassisted treatment for those diagnosed with OUD. “We follow the VA/DOD clinical practice guidelines, which were just updated in 2015 based on systematic reviews of the evidence using the well-respected GRADE methodology for Continued on page 137 131
TO HELP REVERSE AN OPIOID OVERDOSE Concentrated The only 4 mg intranasal dose of naloxone approved by the FDA Needle-free Designed for intranasal delivery and rapid absorption Ready-to-use No assembly or special training required* Not a substitute for emergency medical care. Repeated doses may be necessary.
*Administer in accordance with the Instructions for Use
INDICATIONS NARCAN® (naloxone hydrochloride) Nasal Spray is an opioid antagonist indicated for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression. NARCAN® Nasal Spray is intended for immediate administration as emergency therapy in settings where opioids may be present. NARCAN® Nasal Spray is not a substitute for emergency medical care.
NARCAN® Nasal Spray: Fast. Strong. Proven. In an overdose emergency, the first response is critical. Caregivers, family members and first responders can’t always be sure of the opioid involved, but they can be prepared with NARCAN® (naloxone HCl) Nasal Spray. Special interest pricing is available for Veterans Affairs groups and the Department of Defense.
To order NARCAN® Nasal Spray, visit www.narcan.com IMPORTANT SAFETY INFORMATION NARCAN® Nasal Spray is contraindicated in patients known to be hypersensitive to naloxone hydrochloride. Seek emergency medical assistance immediately after initial use, keeping the patient under continued surveillance. Risk of Recurrent Respiratory and CNS Depression: Due to the duration of action of naloxone relative to the opioid, keep the patient under continued surveillance and administer repeat doses of naloxone using a new nasal spray with each dose, as necessary, while awaiting emergency medical assistance. Risk of Limited Efficacy with Partial Agonists or Mixed Agonists/Antagonists: Reversal of respiratory depression caused by partial agonists or mixed agonists/antagonists, such as buprenorphine and pentazocine, may be incomplete. Larger or repeat doses may be required. Precipitation of Severe Opioid Withdrawal: Use in patients who are opioid dependent may precipitate opioid withdrawal characterized by body aches, diarrhea, increased heart rate (tachycardia), fever, runny nose, sneezing, goose bumps (piloerection), sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated and may be characterized by convulsions, excessive crying, and hyperactive reflexes. Monitor for the development of opioid withdrawal. Risk of Cardiovascular (CV) Effects: Abrupt postoperative reversal of opioid depression may result in adverse CV effects. These events have primarily occurred in patients who had pre-existing CV disorders or received other drugs that may have similar adverse CV effects. Monitor these patients closely in an appropriate healthcare setting after use of naloxone hydrochloride. The following adverse reactions were observed in a NARCAN® Nasal Spray clinical study: increased blood pressure, musculoskeletal pain, headache, nasal dryness, nasal edema, nasal congestion, and nasal inflammation. See Instructions for Use and full Prescribing Information in the use of this product. To report SUSPECTED ADVERSE REACTIONS, contact Adapt Pharma, Inc. at 1-844-4NARCAN (1-844-462-7226) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. Please see a Brief Summary of Prescribing Information on the following page. © 2016 ADAPT Pharma, Inc. NARCAN® is a registered trademark licensed to ADAPT Pharma Operations Limited. Adapt Pharma, Inc. Radnor, PA NAR4-100-16
BRIEF SUMMARY OF PRESCRIBING INFORMATION FOR NARCANÂŽ (naloxone hydrochloride) NASAL SPRAY INDICATIONS AND USAGE NARCAN Nasal Spray is indicated for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression. NARCAN Nasal Spray is intended for immediate administration as emergency therapy in settings where opioids may be present. NARCAN Nasal Spray is not a substitute for emergency medical care. WARNINGS AND PRECAUTIONS Risk of Recurrent Respiratory and Central Nervous System Depression The duration of action of most opioids may exceed that of NARCAN Nasal Spray resulting in a return of respiratory and/or central nervous system depression after an initial improvement in symptoms. Therefore, it is necessary to seek emergency medical assistance immediately after administration of the first dose of NARCAN Nasal Spray and to keep the patient under continued surveillance. Administer additional doses of NARCAN Nasal Spray if the patient is not adequately responding or responds and then relapses back into respiratory depression, as necessary. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance. Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists Reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete. Larger or repeat doses of naloxone hydrochloride may be required to antagonize buprenorphine because the latter has a long duration of action due to its slow rate of binding and subsequent slow dissociation from the opioid receptor. Buprenorphine antagonism is characterized by a gradual onset of the reversal effects and a decreased duration of action of the normally prolonged respiratory depression. Precipitation of Severe Opioid Withdrawal The use of NARCAN Nasal Spray in patients who are opioiddependent may precipitate opioid withdrawal characterized by the following signs and symptoms: body aches, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated and may include the following signs and symptoms convulsions, excessive crying, and hyperactive reflexes. Monitor the patient for the development of the signs and symptoms of opioid withdrawal. Abrupt postoperative reversal of opioid depression after using naloxone hydrochloride may result in nausea, vomiting, sweating, tremulousness, tachycardia, hypotension, hypertension, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. These events have primarily occurred in patients who had pre-existing cardiovascular disorders or received other drugs that may have similar adverse cardiovascular effects.
Although a direct cause and effect relationship has not been established, after use of naloxone hydrochloride, monitor patients with pre-existing cardiac disease or patients who have received medications with potential adverse cardiovascular effects for hypotension, ventricular tachycardia or fibrillation, and pulmonary edema in an appropriate healthcare setting. It has been suggested that the pathogenesis of pulmonary edema associated with the use of naloxone hydrochloride is similar to neurogenic pulmonary edema, i.e., a centrally mediated massive catecholamine response leading to a dramatic shift of blood volume into the pulmonary vascular bed resulting in increased hydrostatic pressures. There may be clinical settings, particularly the postpartum period in neonates with known or suspected exposure to maternal opioid use, where it is preferable to avoid the abrupt precipitation of opioid withdrawal symptoms. In these settings, consider use of an alternative, naloxone-containing product that can be titrated to effect and, where applicable, dosed according to weight. ADVERSE REACTIONS Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to the rates in the clinical studies of another drug and may not reflect the rates observed in practice. In a pharmacokinetic study of 30 healthy adult volunteers exposed to one spray of NARCAN Nasal Spray in one nostril or two sprays of NARCAN Nasal Spray, one in each nostril, the most common adverse reactions were: increased blood pressure, musculoskeletal pain, headache, nasal dryness, nasal edema, nasal congestion, and nasal inflammation. The following adverse reactions have been identified primarily during post-approval use of naloxone hydrochloride in the post-operative setting. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: Hypotension, hypertension, ventricular tachycardia and fibrillation, dyspnea, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. Excessive doses of naloxone hydrochloride in post-operative patients have resulted in significant reversal of analgesia, and have caused agitation. Abrupt reversal of opioid effects in persons who were physically dependent on opioids has precipitated an acute withdrawal syndrome. Signs and symptoms have included: body aches, fever, sweating, runny nose, sneezing, piloerection, yawning, weakness, shivering or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, tachycardia. In the neonate, opioid withdrawal signs and symptoms also included convulsions, excessive crying, and hyperactive reflexes. USE IN SPECIFIC POPULATIONS Pregnancy The limited available data on naloxone use in pregnant women are not sufficient to inform a drug-associated risk. In animal
reproduction studies, no embryotoxic or teratogenic effects were observed in mice and rats treated with naloxone hydrochloride during the period of organogenesis at doses equivalent to 6-times and 12-times, respectively, a human dose of 8 mg/ day (two NARCAN Nasal Sprays) based on body surface area comparison. Naloxone hydrochloride crosses the placenta, and may precipitate withdrawal in the fetus, as well as in the opioiddependent. The fetus should be evaluated for signs of distress after NARCAN Nasal Spray is used. Careful monitoring is needed until the fetus and mother are stabilized. Lactation There is no information regarding the presence of naloxone in human milk, or the effects of naloxone on the breastfed infant or on milk production. Studies in nursing mothers have shown that naloxone does not affect prolactin or oxytocin hormone levels. Naloxone is minimally orally bioavailable. Pediatric Use The safety and effectiveness of NARCAN Nasal Spray has been established in pediatric patients for known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression. Use of naloxone hydrochloride in pediatric patients is supported by evidence from adequate and well-controlled studies of naloxone hydrochloride in adults with additional data from 15 clinical studies (controlled and uncontrolled) in which neonates and pediatric patients received parenteral naloxone hydrochloride in doses ranging from 0.005 mg/kg to 0.01 mg/kg. Safety and effectiveness are also supported by use of other naloxone hydrochloride products in the post-marketing setting, as well as data available in the medical literature and clinical practice guidelines. NARCAN Nasal Spray may be administered to pediatric patients of all ages. Absorption of naloxone hydrochloride following intranasal administration in pediatric patients may be erratic or delayed. Even when the opiate intoxicated pediatric patient responds appropriately to naloxone hydrochloride, he/she must be carefully monitored for at least 24 hours, as a relapse may occur as naloxone hydrochloride is metabolized. In opioid dependent pediatric patients, (including neonates), administration of naloxone hydrochloride may result in an abrupt and complete reversal of opioid effects, precipitating an acute opioid withdrawal syndrome. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be lifethreatening, if not recognized, and should be treated according to protocols developed by neonatology experts. In settings such as in neonates with known or suspected exposure to maternal opioid use, where it may be preferable to avoid the abrupt precipitation of opioid withdrawal symptoms, consider use of an alternate naloxone-containing product that can be dosed according to weight and titrated to effect. Also, in situations where the primary concern is for infants at risk for opioid overdose, consider whether the availability of alternate naloxone containing products may be better suited than NARCAN Nasal Spray.
Geriatric Use Geriatric patients have a greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. Therefore, the systemic exposure of naloxone hydrochloride can be higher in these patients. Clinical studies of naloxone hydrochloride did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. PATIENT COUNSELING INFORMATION Advise the patient and family members or caregivers to read the FDA-approved patient labeling (Patient Information and Instructions for Use). Recognition of Opioid Overdose Inform patients and their family members or caregivers about how to recognize the signs and symptoms of an opioid overdose such as the following: • Extreme somnolence - inability to awaken a patient verbally or upon a firm sternal rub. • Respiratory depression - this can range from slow or shallow respiration to no respiration in a patient who is unarousable. • Other signs and symptoms that may accompany somnolence and respiratory depression include the following: - Mosis. - Bradycardia and/or hypotension. Risk of Recurrent Respiratory and Central Nervous System Depression Instruct patients and their family members or caregivers that, since the duration of action of most opioids may exceed that of NARCAN Nasal Spray, they must seek immediate emergency medical assistance after the first dose of NARCAN Nasal Spray and keep the patient under continued surveillance. Limited Efficacy for/with Partial Agonists or Mixed Agonist/ Antagonists Instruct patients and their family members or caregivers that the reversal of respiratory depression caused by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and may require higher doses of naloxone hydrochloride or repeated administration of NARCAN Nasal Spray, using a new nasal spray each. Precipitation of Severe Opioid Withdrawal Instruct patients and their family members or caregivers that the use of NARCAN Nasal Spray in patients who are opioid dependent may precipitate opioid withdrawal.
For more information, visit www.narcan.com
© 2016 ADAPT Pharma, Inc. NARCAN® is a registered trademark licensed to ADAPT Pharma Operations Limited. Adapt Pharma, Inc. Radnor, PA NAR4-100-16
AMC RESOURCE GUIDE
k O O l t u O
U.S. ARMY C ORPS OF EN GINEERS
d Coast Guar
2015-2016 EDITION
CI A L S PER IO N S T A OPE ITIO 017 ED 2016-2
r in he Yea
N
BUILDING S The 25th Anniversary of
SERVING THE
NATION AND TH
TRONG
E ARMED FO
DESERT SHIELD DESERT STORM
RCES
Coas t Guard
YD .IELACORMMM U.S AN TER
Av iAtion Cent
enni Al
interview with . Commandant Adm Paul Zukunf t
MA
1991-2016
Arctic Challenges
BAT T MEDICLIEFIELD NE
2016-2017 EDITI ON
cues Greatest Air Res
INTERV
AARnnSiveOrsaCry M th 10
Lt. Gen.
an Osterm seph L. . Gen. Jo . Scot t der Maj W Comman Sgt. Maj. John Regiment C SO and ider • MAR C Comm arine Ra t Group • MARSO r D. Huntley, M Raider Suppor tions School te e ra • Col. Pe D. Duke, Marin ine Special Ope n ar mander • Col. Jo t A. Bourne, M TH Com et SOCNOR • Col. Br z, . Met
–
–
IEW: INTERV
Rear Ad
m. Kerry
15 Years
of Adva nces
70 th An VA Of fic n e of Acad iver s a r em
$5.95
0
ANN 16 5 US CDN $5.9
74470
80773
IEWS
ic Af filia
Mark Surgeon General A . Ediger, of the Ai r Force David J. Under Se Shulkin, MD cretar y Departm fo ent of Ve r Health, terans Af fairs M
65
aj. Gen. B
tions
y
MD
arbara
Comman din R. Hol and Mate g General, U. S. Army comb riel Comm Medical Marylan Research d, and Ch and and Fort Detri ief, U.S. Army Nu ck, rse Corp s
5
M
The Year in Special Operations I The Year in Veterans Affairs & Military Medicine Desert Shield Desert Storm 25th Anniversary I U.S. Coast Guard Outlook U.S. Army Corps of Engineers: Building Strong® I AMC Resource Guide Check Out Our Free Online Magazine Library
www.defensemedianetwork.com/defense-and-military-online-magazines
®
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Continued from page 131 ■■ The VA’s FY 16 funding for pain relevant research is $31 million.
The more than 100 projects this funding supports include studies ranging from the mechanism of pain itself to opioid use and how to prevent it.
reviewing the literature and developing recommendations based on evidence,” said Drexler. “And that guideline recommends for opioid use disorder medication-assisted treatment using either buprenorphine/naloxone [which is] also known by the brand name Suboxone, methadone provided through a federally regulated opioid treatment program (OTP), or extended release injectable naltrexone.” The good news for veterans, Drexler said, is that the medications that can be prescribed – buprenorphine and injectable naltrexone – are available through the VA national formulary. For methadone treatment, the VA has 32 OTPs at facilities nationwide, but many veterans also receive treatment in non-VA community OTPs. Even with increased demand for treatment, Drexler said currently approximately 34 percent of veterans diagnosed with OUD receive medication-assisted treatment, up from about 26 percent when the effort began. Research is another essential component in focusing on pain and OUD. “We have a very robust team research enterprise,” Gallagher said, regarding VA research on these topics. Funding for pain relevant research for FY 2016 is approximately $31 million supporting more than 100 projects, with an additional $20 million for SUD research. “There’s an overlap, too, because some of our pain research is about opioids. So it’s a nice confluence of efforts,” he said. Projects include studies ranging from the mechanism of pain itself to opioid use and how to prevent it with interventions such as a combination of CBT and meditation, for example. The research leads to opportunities for trials to develop new treatments, with implementation research – where a new approach based on a clinical trial can be evaluated not only by research evaluation instruments, but also by its effect on patients’ clinical behavior in a facility setting – being an important part of the portfolio. Regarding SUD research, Drexler said, “Areas where we can learn more, and we’re actively researching, are things like preventing overdose death through our opioid Overdose Education and Naloxone Distribution program (OEND).” A component of the OSI, the OEND distributes naloxone rescue kits to VA facilities and families and trains them in their use to reverse opioid overdose. “We have distributed over 35,000 naloxone rescue kits,” said Drexler, adding that they have at least 173 reports of rescues nationwide in a voluntary reporting system. There are many challenges in providing the necessary care to veterans with pain or SUDs. “One of the biggest challenges for us in SUD treatment is getting that treatment out to veterans, particularly in rural areas and at small clinics,” said Drexler. Gallagher agreed, noting that it’s crucial to have the ability to utilize technology to reach veterans “who may be distant or
www.defensemedianetwork.com
have trouble getting to the hospital because of their injuries, pain, or disabilities. So we’re working on telemedicine, telehealth, e-consultation, all sorts of ways of doing these things. “For example,” he said, “we do have cognitive behavioral therapy for pain that can be done over the telephone. And we’ve done research to show that actually works. So access to our multi-modal integrative care is one big challenge in making sure that we have those kinds of assets available to our patients.” Another challenge is rehabilitation, “and getting patients who are very complex the kind of intensity of care that they need to really get back to a quality of life and functioning that they desire,” said Gallagher. “We’ve been very successful in the VA in developing CARF [Commission on Accreditation of Rehabilitation Facilities] accredited rehabilitation programs for chronic pain. We’ve gone from two in 2010 to over 20 currently, and a couple more are in development across the country. These facilities care for more complex patients including some of those with substance use disorders as well as pain, but others with just severe, chronic, disabling pain.” Some are inpatient programs and others are domiciliary with patients coming in for intensive treatment during the day, and, Gallagher said, are very successful at getting people back to functioning again. But, Gallagher summarized, “I think the big challenge we have, like the nation, is a large number of patients on opioids who may need to be tapered from their opioids to lower doses, or off the medications, and get on to a more comprehensive self-management and integrated team management approach to their pain care. And that’s always a challenge because it’s hard work, particularly for those who have substance use disorder.” With the significant challenges and broad scope of combating the serious problem of OUD, the VA has already seen positive effects from its efforts, and continues those efforts on multiple fronts. 137
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Pharmacy Automation in the VA n IN A HEALTH CARE STRUCTURE AS LARGE and complex as that of the Department of Veterans Affairs (VA), with more than 1,700 sites of care and serving more than 9 million enrollees, numerous systems work together to deliver care to veterans. The VA Pharmacy Benefits Management Services is one of those crucial elements. Within that system, pharmacy automation is the integration of the physical processes – like medication vials moving along a conveyer belt in the VA’s mail-order pharmacies – with complex and detailed information technology. It is sometimes visible to patients and sometimes behind the scenes, and constantly evolves with changing technologies and veterans’ needs. And those processes, whether in inpatient or outpatient settings, ultimately result in increased 138
patient safety, reduced cost due to pilferage, detection of diversion, and the enhanced ability of pharmacists to provide patient care. “VA pharmacy services started using automation back in the 1980s, so it does have a long history and it has certainly come a long way,” said Lynn Sanders, PharmD, associate chief consultant, Clinical Informatics for Pharmacy Benefits Management at the VA. Because of the complexities and differences in size and type of facilities, including large, complex medical centers, community-based outpatient clinics, and other ancillary care services, Sanders said the VA utilizes a variety of automation technologies to prepare and deliver medications to patients.
www.defensemedianetwork.com
VA PHOTO
By Gail Gourley
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ OPPOSITE: Bottles of prescription
PHOTO BY SHAWN JAMES, HVAMC MEDIA SECTION
medication move along a conveyor belt at the Department of Veterans Affairs’ Consolidated Mail Outpatient Pharmacy facility in North Charleston, South Carolina. RIGHT: In this 2002 photo, Jeffery Dubea, LVN, ensures veteran Willie R. Hutcherson receives the correct medication in the correct dose at the correct time by using a hand-held scanner to read Hutcherson’s barcoded identification wristband. The VA was an early adopter of barcode medication administration, one example of pharmacy automation.
It could be a simple automated system like a pill counter with associated information technology, including inventory management and patient safety features. Or, Sanders said, “There may be something very complex, such as treating a patient with chemotherapy and all of the algorithms and processes that are involved in that, as well as IV robotics. In some cases, we’re looking at inventory systems or point-of-care systems for the patient to be used by nursing. There’s a preponderance of different approaches you can use, and we do tailor the systems that we have in practice based on the needs of the particular [facility] and the populations they serve.” Regardless of the system utilized, Sanders said, “All of them must comply with the VA standards and regulations and they have to be able to communicate with the VistA [Veterans Health Information Systems and Technology Architecture] system, our VA electronic health records system, through our standardized interfaces.” There are many examples of how automation augments safety. “One of the first advances with automation, and VA was certainly involved with that, was barcode medication administration, where the packaging of the medication with a barcode had to match the patient’s barcode identity bracelet,” Sanders said. “I think that was one of the most significant advances in health care in terms of patient safety for medication use in the inpatient area.” Automated dispensing cabinets with drawers containing patients’ individual medication orders provide another example. When the nurse goes to that dispensing cabinet for a particular patient’s medication, Sanders said, only the drawer that has the specific medication ordered for that patient will open. “They wouldn’t be able to open the drawer for another medication and thereby give the wrong medication to the patient or engage in undetectable medication diversion,” she said. IV smart pumps also enhance safety. The pharmacy works with nursing to program the dosage and administration rate
www.defensemedianetwork.com
of intravenous medications into the pump, Sanders said, avoiding the medication being administered at the wrong dose or the wrong rate because it’s linked to the product identification that’s in the pump. Safety features are also built into the system and linked to patients’ electronic health records to include warnings about potential adverse drug interactions, medication allergies, drug recalls, or unsafe dosages. “In VA, we’ve been working and have technologies now with our systems called the Medication Order Check Healthcare Application, or MOCHA,” said Sanders. Within that system, for example, “we have safeguards that if the dosage ordered is too high, an alert will trigger to the prescriber as well as to the pharmacist to intervene on the processing of that order.” The technology includes inventory management, Sanders said, “So you know that you actually have the drug there. If the drug is short, the pharmacy will automatically get an alert that we’re low on this inventory and signal to reorder the medication and to restock the cart, so that we don’t get to the point where the nurse looks at the drawer and there’s nothing in there. … You’re not having delays in therapy because the medication is not available.” Pharmacy automation improves workflow and efficiency, Sanders said, because “back in the day, pharmacists and technicians did the counting and pouring, which took up considerable time. Preparing these orders with automation, now our pharmacists have more time to spend in patient care, especially our clinical pharmacists. We’re fortunate in VA that we have clinical pharmacy specialists who can act as providers, prescribing medication and managing patients’ care. By having these technologies, we 139
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ A VA pharmacist checks an automated dispensing cabinet. Such
VA PHOTO
automation technology has greatly improved the accuracy and speed of filling prescriptions.
can free up pharmacists’ time so they can perform more of these clinical care capabilities that are so important, especially to our veterans.” Because VA pharmacy automation utilizes industry standards, communication compatibility exists with the Department of Defense and other non-VA health care systems. VA is currently working on technology to incorporate additional standards and data-sharing and interoperability systems to improve these communications. Additionally, the VA has developed tools to share data with states’ prescription drug monitoring programs, an important aspect in addressing potential opioid or other drug overdoses. With those technologies, Sanders said, “we can share data about patients’ medication use regarding controlled substances with participating states and give the prescribers and the clinicians in the state, as well as the VA, more information on how to better manage the patient and reduce the potential for misuse as a result.” Sanders identified several project areas they’re working on to advance VA pharmacy automation capabilities and meet veterans’ needs. Projects include enhancing the barcode medication administration system and improving the inpatient automated dispensing equipment interface to better utilize commercial technologies. The VA has a number of other key VistA software development projects that will improve the ability to use automated technologies. For example, Park a Prescription, OneVA Pharmacy, and InBound ePrescribing will expand the ability to dispense medications to better meet the needs of veterans. Also, said Sanders, “We’re particularly looking at some specialty areas for pharmacy medication management in the area of women’s health and teratogenic drugs to reduce the risk to female patients of exposure to certain medications.” Other efforts are directed toward hepatitis, diabetes, and anticoagulation treatment, “areas where in the VA population, in particular, we have a significant need to address and be able to provide them additional services,” said Sanders. Additional endeavors include: increasing rural access to medications with telehealth solutions; allowing the VA system to process veterans’ prescriptions from non-VA providers; and developing a mobile app for prescription refills. “When veterans come into the VA system after their military career, they typically stay in our system for decades,” Sanders summarized. “It’s a very unique situation that you don’t see in the private sector, and often our pharmacists have very long-term relationships with our veterans. We know they have unique needs … and we’re constantly working on thinking of ways to better meet those specific needs.”
www.defensemedianetwork.com
Another way in which VA pharmacy automation benefits veterans is through its mail-order pharmacy service. “The VA is a unique environment where we can invest in automation throughout the health care scheme that relates to pharmacy, and it’s all under one umbrella,” said Ken Siehr, RPh, national director of the VA’s Consolidated Mail Outpatient Pharmacy (CMOP). That umbrella includes CMOP, a centrally managed, automated outpatient mailorder pharmacy system for veterans who choose to receive their prescriptions by mail. “In the 1950s, VA became the first organization in the country to mail prescriptions to patients,” explained Siehr. “At that time, the mailing was done from local medical center pharmacies.” Initial consolidation of that service in the mid1970s led to progressive increases in centralization and automation over the next several decades. The seven current CMOP locations were established in 1999, and were consolidated under one leadership structure in 2005. A distinct quality of CMOP that is a major departure from commercial mail-order pharmacies is that it’s an integrated part of the whole VA pharmacy automation system, and in fact, extends those features into the mail-order process, improving continuity of care and providing additional safety and convenience for veterans. Siehr explained that in the private sector, the pharmacy automation systems can be completely separate for inpatient and outpatient venues as well as nursing homes and mail-order pharmacies, with separate decision support mechanisms. “We’re unique in VA in that those can all be combined and integrated much more closely than they are in the private sector,” he said. Additionally, the VA mail-order system works differently than its private-sector counterparts. “If you or your loved ones get prescriptions from a mail-order pharmacy in the private sector, your physician communicates directly with the mail-order pharmacy,” explained Siehr. “The mail-order pharmacy has its own automation system to track that individual prescription. So they input that prescription into their automation system and then they use their automated equipment to fulfill that 141
X-RAY CASSETTE COVERS
PROUD VETERAN SUPPLIER GSA CONTRACT # V797P3239M
TOUGH, DURABLE, DISPOSABLE EASY PLACEMENT AND REMOVAL SAVES TIME PROTECTION OF YOUR EXTREMELY EXPENSIVE CASSETTES FROM BLOOD AND BODILY FLUIDS ALL STANDARD CASSETTE SIZES & ANY CUSTOM SIZES TO FIT YOUR APPLICATION
SEE IT FOR YOURSELF!
FREE SAMPLES AND DEMONSTRTION VIDEO AT RADMANRADIOLOGICAL.COM
GSA CATALOG #J69502 #J69522DR X-RAY CASSETTE COVERS
CURRENTLY USED BY HUNDREDS OF AMERICAS’ LEADING HOSPITALS
PHONE: 757 4306710 FAX: 855 7236262 TOLL FREE: 18664522624 RADMANRADIOLOGICAL@YAHOO.COM
WWW.RADMANRADIOLOGICAL.COM
Serve on the frontlines as a leader in healthcare Advance your career as a leader in healthcare with a degree or certificate from Pacific University. Our healthcare administration and leadership programs pair rigorous academics with flexible schedules. Study online or in evening and weekend courses in programs designed for working professionals. Bachelor of Health Science in Healthcare Management Master of Healthcare Administration Graduate Certificate in Healthcare Compliance
“Treat each patient as you would want your family treated.”
Graduate Certificate in Gerontology 1-800-933-9308 | gradadmissions@pacificu.edu | pacificu.edu/HAL
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ VA Secretary Robert A. McDonald speaks with pharmacy supervisor Brad Smith during his visit at the Charlotte Community Based Outpatient
VA PHOTO
Clinic in North Carolina. Pharmacy automation improves workflow and efficiency, which enables pharmacists to spend less time manually filling prescriptions and more time on managing their patients’ care.
prescription and send it to you. So you are a direct customer of that mail-order pharmacy.” But if you then go to a brick-and-mortar pharmacy, they have a different profile, Siehr continued. “They may not have the same drug profile that the mail-order pharmacy has. The mail-order pharmacy only knows about those prescriptions you sent to them; [the non-mail-order pharmacy] only knows about those prescriptions that you sent to [them]. No one has a complete picture of your medication therapy. In VA, we realized that problem and fixed it.” A key difference is that the VA’s CMOP system is designed for the veteran to have a single point of pharmacy care, and that point is the medical center pharmacy. “If the veteran doesn’t know CMOP exists, that’s a good thing, because we want the veteran to have one point of
www.defensemedianetwork.com
pharmacy care, not multiple points of pharmacy care like they have in the private sector,” Siehr said. So the process, Siehr continued, is that when a veteran visits a VA facility for outpatient treatment, the provider enters prescription information into the VA’s electronic medical record. That prescription is electronically transmitted to the local medical center or clinic pharmacy, where it is reviewed in combination with the patient’s electronic medical record information, including medical history and other prescribed medications. That differs in the private sector, where each individual entity has only the potentially fragmented information that it was provided. “The local VA pharmacy processes that prescription on the front end,” said Siehr. “‘Is everything right for this patient? Is the drug at the right dose? Are there any interactions with 143
VA PHOTO BY VICTORIA DILLON
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
other medications?’ – all those sorts of things. Once they’ve done that review, that prescription information is put into an electronic queue, assuming that patient wants it mailed. Then, every night, the queue of those prescriptions from every medical center across the country is sent to the CMOP core system database. “From there, we have seven CMOP facilities across the country, actual physical plants, that receive that prescription information from the medical centers, fulfill that prescription – in other words, put the pills in the bottle – and then mail the prescriptions or send them via commercial carrier to the veteran,” Siehr said, noting that once CMOP receives those prescriptions, the standard is that they enter the delivery system in 48 hours or less. According to Siehr, CMOP fills 80 percent of all the outpatient prescriptions that are prescribed for VA patients. That equates to about 119 million prescriptions this fiscal year; more than 460,000 prescriptions each work day are placed in 310,000 packages, some containing multiple medications, and into the delivery system. That’s about 82 million packages a year, said Siehr, so CMOP employs a mail consolidator who processes most of the packages into the United States Postal Service’s Parcel Select Lightweight option. Utilizing the consolidator cuts delivery time and saves about $26 million annually over the cost of First-Class Mail ®. Veterans with a My HealtheVet account, the VA’s online personal health record, can track the package along the delivery process. After the prescription information is reviewed and entered into the system, CMOP automation takes over regarding patient safety. Siehr asserted that the automated process is safer and has error rates much lower than a manual system. “It is all 144
done electronically, primarily with barcode reads and RFID [radio-frequency identification] tags that are in the conveyance systems that we use in CMOP,” he said. “All of those electronic checks and balances make our system extremely safe – greater than Six Sigma [a measure of quality with extremely low error rates] safe. “All of our systems are geared to that effect – that the right veteran gets the drug that was prescribed in the quantity prescribed in a timely manner,” he said. “We pay a lot of attention because there’s no room for error.” As with the rest of the VA pharmacy automation system, in addition to safety features, the CMOP provides pharmacists at local sites opportunities to fulfill more clinical functions. “From a VA pharmacy-wide perspective, I call CMOP ‘the innovation that changed pharmacy,’ because before CMOP, all those 119 million prescriptions were filled at each local site,” Siehr said. Now, with CMOP filling those, pharmacists can “get involved in opioid safety or antibiotic resistance … or do more direct patient care.” Siehr noted that for the eighth consecutive year, the VA mail-order pharmacy received an “Among the Best” ranking from market research company J.D. Power and Associates, one of only two organizations to receive this designation, and for six of the last eight years, received the highest customer satisfaction score for all mail-order pharmacy organizations surveyed. Although CMOP services have a positive impact on veterans by ensuring their prescriptions are correct and delivered in a timely manner, Siehr said, “I don’t necessarily want the veterans to know I exist. I want them to think that their pharmacy care is provided by their local pharmacy, because that’s the face of pharmacy to that veteran. … There should only be one.”
www.defensemedianetwork.com
VA PHOTO
■■ LEFT: The CMOP in North Charleston, South Carolina, is one of seven CMOP facilities across the country. Altogether, the system fills 80 percent of all outpatient prescriptions prescribed for VA patients. ABOVE: VA Secretary Robert A. McDonald (center) and medical adviser Dr. Baligh Yehia (right) tour the Northeast Consolidated Mail Outpatient Pharmacy with facility director Chris Conisha (background). According to Ken Siehr, national director of CMOP, the system’s automated process is safer and has error rates much lower than a manual system.