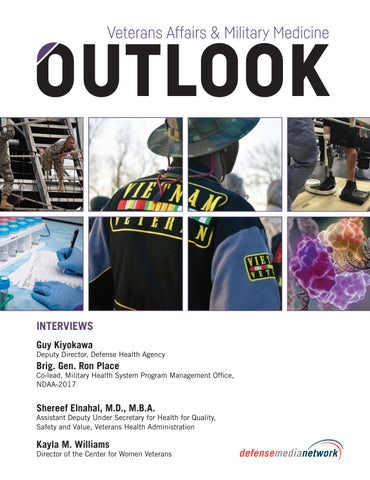
INTERVIEWS Guy Kiyokawa
Deputy Director, Defense Health Agency
Brig. Gen. Ron Place
Co-lead, Military Health System Program Management Office, NDAA-2017
Shereef Elnahal, M.D., M.B.A.
Assistant Deputy Under Secretary for Health for Quality, Safety and Value, Veterans Health Administration
Kayla M. Williams
Director of the Center for Women Veterans
2017 SPRING EDITION
HEALTHCARE INNOVATION Starts Here.
DSS delivers integrated best-of-breed and custom health information technology solutions into the VA’s EHR Platform, with the technical and service integration expertise that comes from more than 25 years of industry-leading innovation. Our breakthrough technologies improve efficiencies for clinical and administrative users, and increase Veterans’ access to care, satisfaction, and performance outcomes. For more information about how DSS supports Veteran care, visit www.dssinc.com.
Don’t miss upcoming editions of
Sign up or update your information to assure your continued complimentary subscription and delivery.
It’s easy, just go to
www.VAMilMedOutlook.com/subscribe
“To care for him who shall have borne the battle and for his widow and his orphan...” Abraham Lincoln
Veterans go above and beyond
count on us for value-added
the call of duty to defend
programs that help you manage
America’s freedoms. At 3M, we
patient-centered care. 3M care
believe it’s only right that we do the same for them. That’s why
pathways include: • Surgical safety
our care pathways are designed
• Device reprocessing
around world-class science.
• Vascular access management
And why, with 3M, science is
• Critical tube management
only the beginning. You can also
• Skin & wound management
To learn more about our care pathways and other 3M Health Care solutions, contact: 3M Health Care Helpline at 1-800-228-3957, or visit www.3M.com/healthcare © 3M 2017. All rights reserved. 3M is a trademark of 3M Company.
Proudly supports all of your dental, medical, and supply needs. Supporting your supply needs through the following contracts: DLA ECAT Dental Program SPM2DE-14-D-7469 DLA ECAT Lab Contract SPE2DE-15-D-0007 DLA Medical/Surgical DAPA Holder SP0200-96-H-5014
FEDERAL SUPPLY SCHEDULES: Pharmaceuticals and Drugs (Anesthetics) V797P-2280D Dental Equipment and Supplies V797P-3160M
HENRY SCHEIN, INC. IS A PROUD FEDERAL SUPPLY SCHEDULE DISTRIBUTOR FOR: KaVo Dental Equipment V797P-3218M Kerr V797D-30021 Imaging Sciences Dental Equipment V797P-3235M Pelton & Crane Contract V797P-3241M Busse Hospital Disposables—Medical Equipment and Supplies V797P-4488B
PDI V797D-40290
To Order: 1.800.851.0400 8am–6pm (et ) To Fax: 1.877.350.7890 24 Hours
www.henryschein.com/sm 16FD3700
16FD3700 Fed Ad.indd 1
3/17/17 10:17 AM
Where you earn your MPH online degree
TABLE OF CONTENTS
makes a difference.
INTERVIEWS Kiyokawa, 6 Guy Deputy Director, Defense Health Agency Brig. Gen. Ron Place,
Co-lead, Military Health System Program Management Office, NDAA-2017 By Chuck Oldham
Elnahal, M.D., M.B.A. 28 Shereef Assistant Deputy Under Secretary for Health
for Quality, Safety and Value, Veterans Health Administration, Department of Veterans Affairs By Rhonda Carpenter
M. Williams 62 Kayla Director of the Center for Women Veterans
Earn your master of public health degree from the health sciences university which created whole person healthcare.
By Chuck Oldham
FEATURES
A.T. Still University’s CEPH-accredited MPH online degree prepares graduates to make a difference.
VA’S GENOMIC MEDICINE SERVICE: 16 THE Bringing Genes into Clinical Care By Craig Collins
22 GERIATRICS By J.R. Wilson
Help lead the future of healthcare.
MEDICINE 34 PRECISION The VA and DOD Are Helping to Lead Nothing
mph.atsu.edu
Less Than the Transformation of American Medicine. By Craig Collins
CENTURY ORTHOPEDICS 40 21st By Craig Collins A.T. Still University’s College of Graduate Health Studies offers online degrees in:
46 By J.R. Wilson
HOSPITALISTS
Doctor of Education in Health Professions Doctor of Health Administration Doctor of Health Sciences Master of Health Administration Master of Public Health Master of Public Health-Dental Emphasis Master of Science in Kinesiology
THE U.S. ARMY MEDICAL SERVICE CORPS:
52 100 Years of Support for Military Medicine By Craig Collins
Research: THE OBESITY EPIDEMIC 56 VA By Craig Collins Research: WOMEN’S HEALTH 66 VA By Craig Collins www.defensemedianetwork.com
3
Experience Proven Versatility
Published by Faircount Media Group 701 North West Shore Blvd. Tampa, FL 33609 Tel: 813.639.1900 www.defensemedianetwork.com www.faircount.com EDITORIAL Editor in Chief: Chuck Oldham Managing Editor: Ana E. Lopez Editor: Rhonda Carpenter Contributing Writers: Rhonda Carpenter, Craig Collins, Chuck Oldham, J.R. Wilson DESIGN AND PRODUCTION Art Director: Robin K. McDowall Designer: Daniel Mrgan Designer: Kenia Perez-Ayala Ad Traffic Manager: Rebecca Laborde ADVERTISING Ad Sales Manager: K en Meyer Account Executives: Lorri Brown, Tanya Hensch, Bonnie Schneider, Geoffrey Weiss OPERATIONS AND ADMINISTRATION Chief Operating Officer: Lawrence Roberts VP, Business Development: Robin Jobson Business Development: Damion Harte Financial Controller: Robert John Thorne Chief Information Officer: John Madden Business Analytics Manager: Colin Davidson FAIRCOUNT MEDIA GROUP Publisher: Ross Jobson
©Copyright Faircount LLC. All rights reserved. Reproduction of editorial content in whole or in part without written permission is prohibited. Faircount LLC does not assume responsibility for the advertisements, nor any representation made therein, nor the quality or deliverability of the products themselves. Reproduction of articles and photographs, in whole or in part, contained herein is prohibited without expressed written consent of the publisher, with the exception of reprinting for news media use. Printed in the United States of America.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
GUY KIYOKAWA
Deputy Director, Defense Health Agency
BRIG. GEN. RON PLACE
Co-lead, Military Health System Program Management Office, NDAA-2017
By Chuck Oldham
n GUY KIYOKAWA is the deputy director of the Defense Health Agency (DHA), Defense Health Headquarters, Falls Church, Virginia. During Kiyokawa’s 29-year career in the U.S. Army, he demonstrated visionary leadership across a spectrum of experience, from aeromedical evacuation pilot to health facility engineering and management to health care administration. Kiyokawa ascended to the rank of colonel and retired from the Army in 2015. Prior to joining the senior executive service, Kiyokawa served as the chief of staff of the DHA, where he played a pivotal role in the planning and implementation of Military Health System (MHS) governance reforms, particularly in the area of shared services, serving as the Army’s liaison officer to the MHS Governance Implementation Planning and Transition teams. Moreover, with the creation of the DHA, he drew upon his decades of experience leading people and organizations though large-scale change, including the TRICARE Management Activity, medical clinics, medical centers, and health facilities. He served as executive assistant to the Army surgeon general and is a diplomate in the American College of Healthcare Executives. Kiyokawa was born and raised in Honolulu, Hawaii. He holds a master’s in health administration from Baylor University and a Bachelor of Science in civil engineering from the University of Southern California. He graduated from the U.S. Army War College, where he completed the War College Fellowship with the Department of Veterans Affairs in Washington, D.C. 6
■■ Guy Kiyokawa, Deputy Director, Defense Health Agency.
www.defensemedianetwork.com
U.S. ARMY PHOTO BY MONICA KING
GUY KIYOKAWA, DEPUTY DIRECTOR, DEFENSE HEALTH AGENCY
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
BRIG. GEN. RON PLACE CO-LEAD, MILITARY HEALTH SYSTEM PROGRAM MANAGEMENT OFFICE, NDAA-2017
U.S. ARMY PHOTO
n BRIG. GEN. RON PLACE graduated from the University of South Dakota cum laude with a degree in Chemistry and was commissioned a second lieutenant as a Distinguished Military Graduate of the ROTC program. A member of Alpha Omega Alpha medical honor society, he graduated from Creighton University School of Medicine, receiving a Doctor of Medicine degree cum laude. Place completed his general surgery internship and residency training at Madigan Army Medical Center (MAMC), where he received the Major General Floyd L. Wergeland Award as Madigan’s Outstanding Graduating Resident and was also selected as the Teaching Resident of the Year. Place is a graduate of the Command and General Staff Officer Course, the National War College, is board certified in both general surgery and colorectal surgery, and the author of more than 40 peer-reviewed articles and book chapters. His awards include the Distinguished Service Medal, Legion of Merit with three oak leaf clusters, Bronze Star Medal with oak leaf cluster, the Presidential Unit Citation, Combat Action Badge, Combat Medic Badge, Flight Surgeon’s Badge, Army Surgeon General’s “A” Designator for clinical excellence, the Order of Military Medical Merit, the Army Staff Identification Badge, and others.
n Veterans Affairs & Military Medicine Outlook: Under the 2017 National Defense Authorization Act (NDAA) there are going to be upward of 400 military treatment facilities (MTFs) formerly under the individual services that are going to fall under Defense Health Agency (DHA) authority. How big a task do you see it will be to make this transition? Guy Kiyokawa: How big is this [task] going to be? The bottom line is that Gen. Place being a clinician and a sitting commander of a region in the Army Medical Command and my position as deputy director of the DHA from an administrative standpoint, the leadership felt that they wanted both perspectives to lead this effort for the statute, which is really comprised of 40 sections. But Subtitle 7, or the Title 7 of the statute, focuses on nine sections that talk about reforming TRICARE in the Military Health System, and specific to the military treatment facilities is Section 702, which essentially says that on 1 Oct. 2018, the director of the Defense Health Agency is going to be responsible for the administration of each MTF. We’re going to make a transition from the three services and the DHA because the DHA currently administers and manages Walter Reed and Fort Belvoir MTFs, but the four groups [are] kind of coming together to figure out
www.defensemedianetwork.com
■■ Brig. Gen. Ron Place, Co-lead, Military Health System Program
Management Office, NDAA-2017.
how to move the administration and management of each MTF to the DHA’s authority in those specified areas that are listed. So it’s budgetary, information technology, and so on. But I think the other big challenge that we are currently working through is ensuring that as we do that, that we don’t forget the whole reason why we’re here, which is to support the warfighter from a medical perspective. So there is going to be a fine balancing act. And I think that adds to the complexity and back to your question on how big of a transition is this going to be. Brig. Gen. Ron Place: If I could just add one other point to that. The NDAA, even Title 7 of the NDAA, has 40 sections. And each of them could be answered individually. And we could probably get a good answer. But if they are integrated, if the people who are doing the work on each of the different sections can be integrated together, then we believe that there are good synergies that can come from that. And based on that synergy, we believe that we’re going to get a better product. So it’s a two-fold thing. Yes, it’s complex. Yes, there is a lot to do. But in addition to just answering each of the issues that come with the law, how can you get a strategic vision to see what can we do to make the entire Military Health System that much better of a system. 7
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Leaders from the service medical departments and the Defense Health Agency (DHA) met Jan. 13, 2016, with beneficiary groups to discuss
several initiatives to improve health care delivery. Pictured are (center left) Guy Kiyokawa, DHA deputy director, and (center right) Brig. Gen. John M. Cho, deputy chief of staff for support, U.S. Army Medical Command.
8
it for 400 houses. So we’re talking about 400 military treatment facilities. Instead of being your local hospital in downtown America, we’re talking about [being] on every continent across the world in 18 different time zones, and tens of thousands of deployed personnel around the world. So the scope and scale is really what I’m trying to get across. The scope and scale of the transformation is the second part of it, just because that it’s so huge of a challenge that we’re facing. As far as the Integrated Health Delivery Systems, I understand it was supposed to be based on partnerships between civilian health systems and the Department of Veterans Affairs (VA) and the MTFs. But are there enough civilian and VA facilities that are co-located or in close proximity to MTFs or those areas where you need the service or is that not necessary? I mean do you have that in some places and
www.defensemedianetwork.com
MHS PHOTO
Have you identified yet what you think the biggest 800-pound gorillas in the room are going to be, what the greatest challenges are going to be? Kiyokawa: If you read the language even beyond Title 7, there are probably about eight or nine sections that keep coming back to why we’re here, which is: What are our medical readiness requirements? And while we’ve done a great job in the last 16 years of fighting a prolonged conflict and just have unprecedented results from battlefield medicine, the challenge is how do we take those lessons and apply them to the way we do business back in garrison, so to speak. Place: The scale of the system that has to transform is extraordinary. So when people talk about challenges to making some transitions, I mean, think if you have some sort of do-it-yourself project that you want to do at your house and that’s a one-person thing. But imagine if you had to do
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ “We’ve put the right people at the right place with the right training for the right mission.”
not in others, but overall the end result is that you have a better system for everyone? Kiyokawa: Right, the law does lend to that. In fact, Section 706 talks about those partnerships. We’ve already been working with the VA and local civilian entities. But we tend to do it at local levels. I think what the law is trying to encourage us to do is do it more from an enterprise perspective. So, for example, the law talks a lot about trauma care. And there are a lot of good lessons learned from the 16 years of war that can be shared with the civilian sector, and vice versa, there are trauma centers throughout the United States that we could potentially leverage through these partnerships. But the real question for us to further define is what are those skill sets that we need to prepare for the next conflicts, and then, more importantly, where should we center those capabilities within our MTFs? And then it gets to your question – is that location the right location where we can also partner with both civilian and VA facilities to provide the right capacity or, I’m sorry, the right demand of cases that are required to maintain those types of skill sets? So I think we’re kind of looking at it from a different perspective, not just are those VA or civilian organizations nearby our MTFs. It’s more from the approach: Where do we want to center that training at specific MTFs, of which then the ability to partner with those other two entities is available. Place: And then secondarily to that the law also describes how the ability of veteran patients or civilian patients to be seen within the existing military treatment facilities, is also authorized. So if you look back 15 years, if you look at the skill set within our military treatment facilities, that combat casualty care part of it, was not a significant component, just because there weren’t a lot of combat casualties anywhere. So that wasn’t really an innate skill set that most people – not all, but most people – had within our organization. But now that we have been at war for 15 years it is. It’s a comprehensive skill set that many, if not most, of our clinical staff have. So if they have that capability and if the community, by having some sort of collaboration with veterans or achieving American College of Surgeons trauma status or a level 1 trauma center, a level 2 trauma center, or perhaps even level 3 trauma center, is there a way that we can maintain those skill sets within the existing military treatment facilities that we have and/or can that process also be some way of enabling that community within which that military treatment facility sits – is it a good partner for the community that way as well.
www.defensemedianetwork.com
So it provides good training within the hospital system or the military staff and does it still give back to the community by doing that. The sections of the law actually offer that. So we see it as another way of facilitating that partnership between the entire military community there and the civilian community within which they sit. I can remember writing stories talking about military physicians working in civilian trauma centers to get the benefit of that experience. And it seems like everything has flipped around now, because military surgeons and physicians have had so much experience that they have something to give back to the civilian community. It seems like that’s what you’re describing to some extent. Place: I’ve been an Army general surgeon for almost 30 years. And in the late 1990s, early 2000s, I maintained the skill set within that subspecialty pretty well, but the Army still had a requirement for me to be a deployable trauma surgeon. And I just wasn’t getting that. So the Army allowed me on my own time to do moonlighting; to work as a surgeon on my off time within a level 2 trauma system. But because of that, I felt very comfortable with my trauma skills because I worked there. Well, I deployed soon after 9/11 in support of special operations forces as a combat general surgeon, as a de facto trauma surgeon. And because I had that skill set from my own time, I felt comfortable deploying. After being a deployed general surgeon multiple times, I felt even more comfortable. In fact, when I would go back then to the place that I was moonlighting at, I felt more comfortable than some of the other surgeons who were there, because my experience was so completely based on that combat experience. So you’re right; we’ve flipped the paradigm. Here’s the thing though. If things go as we’d like them to and we’re not doing combat operations, that means that our clinical staff is not getting that experience. Well, woe to us if we go back to “gosh, if only we had maintained that skill set.” So the whole idea is not to have a drop off in that skill set. How can we continue to keep it at a really high level in a time of lessened or hopefully no combat operations? Could you describe the vision for the new Joint Trauma System? Place: What we’ve learned is that by communicating we can do things better and, in fact, we have military models of this already. If you look at our safety centers, they are great 9
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Vice Adm. Raquel Bono, Defense Health Agency director, spoke in February at the annual Healthcare Information and Management Systems
Society (HIMSS) Conference in Orlando, Florida, on DHA’s role in support of military medicine and partnerships with the American medicine industry.
10
using the information that was started by military clinicians almost immediately after the start of the war and it’s formatting that process. So not only are we continuing to get those lessons out, but we’re able to do it faster so that ultimate outcomes, the ultimate recipients of that trauma care have the best outcome possible. I wanted to ask about another part of the act. As I understand it, it requires standardization of tactical combat casualty care training. Obviously battlefield medicine has expanded and grown and become better by leaps and bounds as the last couple of decades has passed. But it seems like there are different standards and emphases at the moment. Do you think that because of the act there will now be sort of a tiered set of standards and competencies that will apply across all the services and commands? Place: I think by anyone’s measure the performance of the Military Health System and particular combat casualty care of the Military Health System over the last 15 or so years has
www.defensemedianetwork.com
DEFENSE HEALTH AGENCY FACEBOOK PAGE
examples. So if you talk about a whole concept, and aviation is one of those, but you have to look at it from every single factor that goes into it, so to do that you look at how do you reference your initial information. So the Joint Trauma System will have a trauma care reference body. And then the establishment of standards of care, and then, like any learning organization, how do you do rapid reviews? How do you review? How do you update those standards of care? And then, based on the questions that you have, you say, “Well, maybe we should do some research on this as well.” So then it talks about prioritizing and coordinating both clinical and quite frankly bench trauma research. So then if you have that reference body and standards of care in research, then how do you take all that together? So whether it’s clinical lessons or research lessons or bench lessons or whatever they are, how do you then take those lessons learned and put them back into clinical practice, which then impacts that trauma care reference body, which then impacts the updating of the standards of care. It’s a big circle. And the Joint Trauma System is
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
been extraordinary. If you look at survivability rates they are the best ever. If you look at died-of-wounds rates, they are the lowest ever, which of course, is a good thing. But the fact is that we’ve been a learning organization. We’ve put the right people at the right place with the right training for the right mission. The establishment of the Joint Trauma Education and Training Directorate really ties all this process together. And perhaps we weren’t as organized about that particular specific as we could have been. But at its core what the section really requires is standardized combat casualty care instruction, and then it can get into some of the specifics of those disparate mission sets that we talked about. So the whole idea is to build comprehensive trauma registries looking at the types of education that we’re using, looking at our outcome measures, and are they the right quality outcome measures, and do we have the right metrics that go with them. And if we do all that right, it’s going to give us insight into that whole trauma system, which then allows us to say, “OK, for this particular competency or this particular mission set, what do we need for competencies, what do we need for standards, and what level of training. Do we need doctoral level people? Do we need physician assistants? Do we need medics? Do we need enhanced medics?” It gets the right person with the right skill set with the right mission. I may have danced around your question and I hope I didn’t. I think that answers it pretty well. But I suppose that is sort of a moving target. It’s something that you’re trying to work out at the moment, right? Place: So, having a whole group of them I think is important. The whole idea of mission command is that the particular person who is involved in the mission understands the big picture and understands where they fit into it, and they are empowered with decision-making to be able to handle all of those things. If we can understand those sorts of big picture things as health care practitioners within mission command, then we will have by and large the right person with the right training and the right skill set for the right mission. That’s the way I see it. Going back to the MTFs, as far as having three different services and DHA involved … how many differences are there now with respect to procedures, administration, and medical practices that you’ll have to standardize? Kiyokawa: I think right now the differences are based on the fact that the service medical departments, which, oh by the way, report to their service [line] leadership, have developed rules and procedures that are dictated by their particular service, so to speak. So while health care is consistent and we’ve done a good job at doing that I think this language provides us kind of the opportunity to take it to the next level. And once again I’ll reiterate what I said in the last question – that sometimes people think that standardization is good across the board. And it’s not a one size fits all. I think what we’re trying to do is mitigate
www.defensemedianetwork.com
HAMILTON-T1 Transport ventilation for armed forces •
Performance of a full-featured ICU ventilator
•
For use in helicopters, airplanes, ambulances, ships, combat support hospitals, and battalion aid stations
•
Advanced ventilation modes including automated ventilation using ASV®
•
Independence from compressed air
•
Over 9 hours of battery operating time
•
NATO stock number NSN 6515-01-648-5814
www.hamilton-medical.com/HAMILTON-T1military
11 HAMILTON-T1-military-advert-jsom-en-ELO20160712N.00.indd 1
14.07.2016 16:20:49
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ The Soldier Specialty Care Clinic (SSCC), a more than 23,000-square-foot addition to the Guthrie Ambulatory Health Care Clinic at Fort
Drum, New York, is home to the traumatic brain injury clinic and occupational therapy department. “Co-locating all traumatic brain injury care and occupational therapy assets on Fort Drum here at the Soldier Specialty Care Clinic is a significant step in improving access for the community,” said Brig. Gen. Ronald J. Place, assistant surgeon general for force projection, at the ribbon-cutting ceremony, April 21, 2016. Pictured are (from left) Place; David Stoehr, Health Facility Planning Agency; Maj. James Curlee Jr., U.S. Army Corps of Engineers, New York District; Col. John McMurray, U.S. Army Medical Department Activity, Fort Drum commander; Brig. Gen. Paul Bontrager, 10th Mountain Division (LI) and Fort Drum acting senior commander; and Lt. Col. James Goetschius, Health Facility Planning Agency.
12
change for us because we’re going to have to standardize the way we do business in order to leverage the EHR as it is laid out. Is MHS Genesis a popular system among civilian doctors and hospitals today? Kiyokawa: MHS Genesis is based on a Cerner product. What’s really interesting, and we’ve been talking to many other civilian health care organizations that have used it, is that it’s not just an electronic health record, but it’s potentially a way to leverage process improvement and standardization throughout an enterprise. So while the original intent was to get to the next generation of electronic health record, we believe that there are many other opportunities
www.defensemedianetwork.com
PHOTO BY CHUCK YANG
any unwanted variation because, as you know, health care is local. It’s dependent upon the geography. It’s dependent upon the demographics. It’s also dependent upon, in some cases, where you have smaller MTFs – what is available outside the gate, so to speak – through any partnerships or the TRICARE contract. So I think that there is some difference out there. I think we’re going to continue to build on some of the things that we’ve already done. MHS Genesis, our new EHR [electronic health records] that just got kicked off in the Pacific Northwest, is a way that we are already using to standardize workflows because, unlike old-time previous electronic health records in the DOD [Department of Defense], this is off the shelf. And it’s a big
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
MILITARY HEALTH SYSTEM AND DEFENSE HEALTH AGENCY IMAGE
to standardize the way we do business. And oh, by the way, it is not just within our MTFs, because MHS Genesis eventually will migrate to operational platforms, too, so we have a true longitudinal medical record. We just kicked that off in the Pacific Northwest within the last several months. And it’s going to take us a few years to get it across the enterprise. Place: Most people forget how similar the three different service medical departments actually are. This electronic health record required a standardization of what we would call workflow processes. In other words, if you’re going to get admitted to the hospital, that’s a workflow process. If you’re going to schedule someone for the operating room, that’s a workflow process. There are hundreds and hundreds and hundreds of workflow processes that go [into it] whenever you have a standardized electronic health record. And we’ve already worked through all those things. And what we found was, while there were some slight variations in the way that each of us did [things] – by each I mean the Air Force, the Navy, and the Army, and then within the Defense Health Agency here in the National Capital Region, the Walter Reed and Fort Belvoir community hospital – what we found is, while there is some slight variation in those workflow processes, they were essentially the same. And so then coming together and say, “Yeah, we’re going to agree to this workflow process,” that’s already been done. So is there more work to be done to bring the three service MTFs into the same sort of [workflow process]? Absolutely. Yes, there is more. But I don’t want anyone thinking that … these are completely different health care systems, because they were not, they are not, and they will just get closer together based on our work together on this 2017 NDAA. Could you describe the responsibilities of the four new deputy assistant directors that are specified in the legislation? Kiyokawa: I think the key is that one of the positions is an assistant director position. And Congress is very specific in not only who that position reported to, which would be the director, but also what qualifications that individual will have. So it was very, very specific. And I think the key is not just that position. It’s also then the four deputy assistant director positions under that; one having to do with information technology, under financial operations, health care operations, and medical affairs. And I’d like to begin with the last one, medical affairs. It is one of the few that in the language gets very specific regarding individual responsibilities. And I think things like patient safety and infection control and some of the quality things are going to be just building upon some of the great work that has already been accomplished in developing the HRO [high reliability organization] concept across the MHS, because that was focused on patient safety and quality. So that would build upon that.
www.defensemedianetwork.com
The financial management position: It aligns then to what [Section] 702 says the director is responsible for. All the dollars used to run the MTFs flows through the assistant secretary of defense for health affairs. So we’re just going to have to figure out the policies and procedures necessary in order to manage it. That’s what that position would focus on. The fourth position is health care operations, and that’s going to get at the heart of what it’s going to take to administer each of these MTFs, which are, as we said earlier, going to make this big transition from aligning to the services and now aligning to a single agency. As far as aligning with a single agency, do you anticipate that DHA is going to have to grow in order to take on some of these new responsibilities? Kiyokawa: So that’s the million-dollar question, because I think, without a doubt one of the clear intents of working under a single agency is that there will be efficiencies. And if you look at Section 702 in the reports to Congress that we need to provide the first section says, “Tell us how you’re going to do it.” And then the next three sections tell us, in order, where there is duplication, then where are there efficiencies, and the last piece is, tell us what the reductions are. So that is very specific in telling us whether or not we’re going to get bigger or smaller as a Military Health System. Now your question was specific to the DHA. So without a doubt, we’re working through right now with the services what are those very, very specific functions that do need to move to the DHA along with the necessary resources in order to administer and manage the MTFs. And I think that’s the ongoing work that we are conducting right now. I believe that the deadline for implementing that change of the MTFs is October 2018, is that right? Kiyokawa: Correct, so as I mentioned, the first of October 2018. But this is important: We have an implementation plan due to Congress on the first of March of next year. So what 13
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ “… we definitely see telemedicine and other new technologies as really being an important part of the future way health systems provide access to care.”
we’re working through right now is trying to define those functions and specific tasks and looking to the department to help us itemize those items to resources so that we can get into the planning and programming and budgeting cycle to ensure that we can move those things in a timely fashion in order to meet that 1 October date. Well, pretty much one of the last things and one of the big ones is what are the major changes that TRICARE enrollees are going to see under this new NDAA? Kiyokawa: So what’s interesting is that it doesn’t go without notice is that [Section] 701, the very first section, is about the TRICARE program. And I believe we recognize TRICARE has been going on for 20-plus years, and we’ve kind of run it in the same way over the years. And over a period of time, it became its own system, rightfully so, because there are so many beneficiaries out there that are not near an MTF. And I think what this does, and it’s not just 701, there are many other sections, it starts to build on some of the things that we’ve already started to do within the Military Health System as it relates to this TRICARE program really being reformed … So I think the creation of the Defense Health Agency was a big first step in trying to get at the three things that you’ll see throughout all the language – accountability for access, quality, and patient safety. And when we say access, access to care is not just access but also the patient’s experience. So one of the big things in the law in 701 is really combining our options. We currently have a Prime, Extra and Standard option, and what they’ve come back and said is eliminate the Standard and Extra and instead create something called TRICARE Select. That’s based more on a PPO model, and it’s going to simplify TRICARE and it also introduces cost-sharing but in a very “grandfathered way,” because the cost-sharing is kind of more the fee structures that haven’t changed in the last 20 years. I think for the most part it’s going to impact those coming on active duty after Jan. 1 of next year. So it’s going to be more of a downstream impact to people and not so much on the individuals that are currently within the program. So TRICARE Select becomes a big part of it. There are many other areas that are really kind of focusing around the patient and making things easier
14
for the beneficiaries. For example, implementing a standard process for specialty care so you don’t need that prior authorization that we currently have in our system. Also, a big push on urgent-care clinics within our MTFs, but also based on the pilot that we have ongoing eliminating any pre-approvals to utilize those urgent-care clinics out in the community. And then we’ve already started a lot of good efforts focusing on primary care with nurse advice lines, secure messaging, and things of that nature. So this continues that ability to do that. There [are] also things in there about leveraging telemedicine. And I’m sure Gen. Place can talk more about that. But we definitely see telemedicine and other new technologies as really being an important part of the future way health systems provide access to care. And leveraging off of telemedicine I believe I know the Army and the other two services have been looking at implementing telemedicine as a force enabler down range in the operational world. Something that has struck me, discussing this with you two, is that it seems like while I’ve looked at this as being a whole series of challenges, it seems you identify a lot of opportunity in this as far as trying to create synergies. Place: Yeah, you’re absolutely right. If you look at the law and you look at the individual sections, you see it as tasks to do. If you look at the whole law and think of the big picture, you see it’s really a strategic opportunity to transform the Military Health System from the way it is today to the way that we wish it could be to both facilitate readiness of the armed forces, and by readiness of the armed forces I mean medically ready forces, healthy forces as well as a ready medical force, a medical force that is ready to do everything it is asked to do combined with an Integrated Health Delivery System. So yes, there are tasks that have to be done. In fact, Mr. Kiyokawa mentioned just the one deadline that you asked him about, which is the movement of the MTFs. But there are literally dozens of dates in there that are requirements to have done. And it would be easy to get lost in this forest for those trees. But we collectively, as the co-leaders of this program, see this as a strategic opportunity to make the Military Health System the best health system that it could possibly be.
www.defensemedianetwork.com
At Optum, we’re dedicated to helping military service members, veterans and their families receive the care they deserve. As a health services and innovation company, we’ve made it our mission to increase access to quality care and improve patient outcomes. Through a streamlined network and modernized infrastructure, we can better serve those who serve us. That’s how well gets done. optum.com/MilitaryandVeterans
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
THE VA’S GENOMIC MEDICINE SERVICE: Bringing Genes into Clinical Care
n THE VETERANS HEALTH ADMINISTRATION (VHA) began its pioneering work in genomic medicine in the mid-1990s, with investigators discovering links between genetic mutations and several diseases and disorders. So the VHA was ready, when the international scientific collaboration known as the Human Genome Project had at last identified and mapped the entirety of the human genome in 2003, to assume a leadership role in the ensuing surge in genomics research. When it established its Genomic Medicine Program in 2006, the VHA charted a course to continue and expand this leadership role. From the outset, because it’s also the nation’s largest integrated health care system, serving 8.76 million patients annually, VHA also wanted to emphasize the rapid 16
transfer of genomic discoveries into clinical decision-making – to use emerging genomic technologies to personalize medicine for veterans. The advisory committee that established the Genomic Medicine Program made this a clear goal in its charter: “using genetic information to optimize clinical care of veterans, and enhance the study and development of diagnostic tests and treatments for diseases of particular relevance to veterans.” As Laurence Meyer, M.D., Ph.D., VHA’s national director of Genomic Medicine and chief of Specialty Care Services, pointed out, genetics as a medical specialty grew out of pediatric care. In the 1980s, it was almost certain that a clinical genetics program would be based in a hospital’s pediatrics
www.defensemedianetwork.com
VA PHOTO
By Craig Collins
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
wing, focusing on hereditary diseases in children. Meyer himself, a former fellow in pediatric genetics, brought his knowledge of the field to the VHA and helped to establish the Genomic Medicine Service (GMS) – the clinical arm of the VHA’s Genomic Medicine Program – in 2011. As knowledge of genomics has advanced, Meyer said, it’s become increasingly clear that many adult-onset diseases and disorders can be linked to genetic information. “About half of all clinical genetics is done in adult-care settings,” he said, “dealing with adult-onset diseases.” Adult clinical genetics most often involves cancer, said Meyer, but also involves neurological disease, cardiovascular disease, and endocrine disorders. The desire to apply genetic information to health care in the VHA presented a few challenges: Though genomic medicine is a rapidly expanding field, its number of trained professionals has yet to catch up to the scope of the veterans’ health care system, which comprises more than 1,700 sites of care nationwide. Also, because the VHA practices patient-centered care, it considers veterans equal partners in medical decision-making. Personalizing medicine for these veterans means ensuring they have all the knowledge they need to understand and act on their health care needs and preferences. One of the GMS’ first tasks, then, was to determine how it would maximize the reach of genetic information – and the ability of trained professionals to help interpret that information for veteran patients. It established a process for credentialing and providing privileges to telehealth providers who could consult with patients at the Department of Veterans Affairs (VA) sites across the country. The service hired its first VA clinic genetic counselor in January 2011; within weeks, it had signed its first Memorandum of Understanding (MOU) to provide telegenetic services at a remote VA clinic, and promptly launched the effort to negotiate MOUs with each of the system’s 21 Veterans Integrated Service Networks (VISNs). Since those early efforts, the GMS has been off and running: From its hub of operations within the VA Salt Lake City Health Care System, its professionals have provided about 10,000 consultations so far to veteran patients and their families.
■■ OPPOSITE: A lab worker examines DNA samples. The VA’s Million
Veteran Program is now the world’s largest database of genomic information, with more than 500,000 volunteer veterans enrolled as of August 2016. Researchers believe the information contained in the database could hold the key to preventing and treating diseases. ABOVE: Like a watch wrapped around a wrist, a special enzyme encircles the double helix to repair a broken strand of DNA. Without molecules that can mend such breaks, cells can malfunction, die, or become cancerous.
NIH PHOTO
WHAT ARE GENETIC SERVICES?
Almost all disease is a result of the interaction between genes and the environment. Heredity can have a direct or contributing influence on health, and genetic mutations can directly cause congenital disease or disorders. Certain genes can make a person more susceptible to disease, such as cancer or heart disease. The molecular composition of individual genes may also influence how responsive a person is to drug treatments and chemotherapies. Because medical genetics is a relatively young field, VA’s Genomic Medicine Service was built to extend its reach throughout the veterans’ health system. Clinical geneticists,
www.defensemedianetwork.com
like Meyer, are physicians with a broad scope of practice encompassing risk assessment, diagnosis, treatment, and referral. The adult medicine practice in the VHA, Meyer said, typically involves a physician – an oncologist, gastroenterologist, surgeon, or women’s clinic provider, for example – working closely with a genetic counselor: a health care professional with a master’s-level degree, trained in educating patients about their options regarding genetic services. “Genetic counselors are not medical providers,” Meyer said, “and they don’t diagnose, but they work with medical providers and do a lot of legwork in providing genetic care.” 17
The non-invasive Answer when the Question is BLADDER CANCER Cxbladder Triage, Detect and Monitor genomic tests for the detection and management of bladder cancer • Superior performance to other urine based tests • Portability for testing in out patient settings • Cxbladder Triage, Detect and Monitor — Optimized genomic tests with high sensitivity and specificity, and a Negative Predictive Value > 97%
• Improved compliance as a result of less invasive testing • Accurate early detection results in reduced costs, fewer invasive procedures and better patient outcomes • Cxbladder – FSS Contract # V797D-60660
www.cxbladder.com or call 1-855-292-5237
Efficiency Through Standardization
EVIS EXERA III Universal Platform Standardization with Olympus enables streamlined asset management and logistics, simplified staff training and biomed support, cost savings, backward compatibility, full-service and financing contract options. The EVIS EXERA III Universal Platform is the industry’s only Universal Platform to support numerous clinical disciplines from general surgery to endoscopy to urology with 100+ rigid and flexible scopes. The modular design of the Universal Platform provides an economical upgrade path from 2D to 3D. Olympus America Inc. Registered Trademark of Olympus or its affiliates. I www.medical.olympusamerica.com I OAIES0417AD22059
RHODA BAER, NATIONAL INSTITUTE OF ARTHRITIS AND MUSCULOSKELETAL AND SKIN DISEASES, NATIONAL INSTITUTES OF HEALTH
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
At a VHA facility that collaborates with the GMS, for example, an oncologist may refer a patient with a diagnosis or family history of cancer to a genetic counselor at the GMS. The patient, from a medical center or outpatient clinic, would then consult with the genetic counselor via one or more 90-minute videoconferences, during which they would discuss the role genetics might play in determining risk for cancer, the course of the disease, and/or the patient’s susceptibility to treatment. “We encourage the veteran to bring family members if they wish to come,” said Meyer. “Prior to the visit, the medical record is reviewed and we try to collect a more full family history to find out what their options are.” About half these discussions, Meyer said, result in the patient and the counselor deciding together that a genetic test is appropriate – though this decision, ultimately, is up to the patient. Currently, there are about 6,000 genetic tests that can be performed on blood samples, Meyer said, and the
www.defensemedianetwork.com
■■ James Balow Jr., M.S., biologist, inserts a GeneChip into the
GeneChip™ Fluidics Station to analyze RNA from patient samples in order to identify genes that are differently expressed between patients with autoinflammatory diseases and controls.
counselor and the patient will make an informed decision about which is most suitable. In many cases, GMS counselors consult directly with providers as well. Genetic testing, said Meyer, “is not just for diagnosis. It can actually guide therapy in cases. It can provide prediction for a patient, or it can provide suggested intervention, such as screening or more aggressive treatment of dyslipidemia or blood pressure. There are things we can do that can affect the outcome of an individual veteran to benefit their health.” One available test, for example, is designed to identify Lynch syndrome, a group of inherited mutations that indicate 19
YOUR NEXT STEP IN NURSING: DOCTOR. The University of Maryland School of Nursing Doctor of Nursing Practice program offers you a variety of options: post-BSN and post-master’s with 8 specialties post-master’s without a specialty Earn your Doctor of Nursing Practice to become an advanced practice registered nurse, and you’ll have full practice authority throughout the Department of Veterans Affairs. We also offer these nationally top-ranked programs: Bachelor of Science in Nursing Master of Science in 3 specialty areas PhD
LEARN MORE: nursing.umaryland.edu/academics
Because B. Braun
Clinicians are protected. Patients are safe. The environment is healthy. We’re proud to serve those who serve us. © 2017. B. Braun Medical Inc., Bethlehem PA. All rights reserved. 4/17
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
a high risk of colon cancer, as well as several other cancers. A positive test for Lynch syndrome would set in motion another round of decision-making, among the patient, provider, and genetic counselor: If the patient doesn’t already have a cancer diagnosis, the positive result can indicate whether to have frequent follow-up screenings. If the patient has been diagnosed with colon cancer, Meyer said, a positive test can help determine the course of treatment. “One of the exciting things about genetics,” he said, “is that for more than a few of these conditions now – if we know somebody, for example, has colon cancer associated with Lynch syndrome, one of the most common causes – they are specifically susceptible to certain kinds of chemotherapy. So we would recommend one of the new immunotherapies, maybe the PD-1 blockade that has a much higher incidence of success. Patients with prostate cancer who have one of the common breast cancer syndrome genes, BRCA2 … are more susceptible to a class of agents called the PARP inhibitors [a substance that blocks an enzyme in cells].” Knowing whether a case of colon cancer is connected to Lynch syndrome has proven so important to the outcome of cases, in fact, that the GMS has helped to implement a protocol so that every veteran with colorectal cancer will have the tumor processed for screening. The protocol may ultimately identify dozens of people annually with Lynch syndrome – who will then benefit from this emerging knowledge about the best treatments available for cancers with this specific genetic cause.
PHOTO BY STEVEN M SKURSKI (AMC)
THE GMS AND THE BIGGER PICTURE
Though it’s only a few years old, the GMS has proven so valuable to patients and providers throughout the veterans’ health system that it’s looking to expand its expertise to additional hubs nationwide; a growing number of VA medical centers provide on-site clinical genetic consultation, making it possible that the capacity to reach more patients and providers throughout the system could be boosted considerably. In addition to its core mission of providing genetic services to veterans and their health care providers, the GMS is involved in efforts to shape and guide the integration of telegenomics and genomic testing into clinical care throughout the VHA. It works closely with the VA’s Office of Research and Development (ORD) to bring the most up-to-date information about genomics into clinical care within the veterans’ health system – and sometimes to work with VA researchers on clinical research projects. “We’re just kicking off a program called PRIME Care [PRecision medicine in MEntal health Care], where we’ll be using a pharmacogenomics test to really see if it has clinical utility in the treatment of psychiatric disease,
www.defensemedianetwork.com
■■ U.S. Army Edgewood Chemical Biological Center researchers
have developed a means for Department of Defense labs across the globe to quickly obtain a genomic analysis of unknown biological samples.
specifically depression, in veterans,” Meyer said. “These tests are heavily marketed, but the evidence that they actually improve the care and outcome of patients is not strong. So we’re trying to set up a multicenter study in the VA, and we expect to be enrolling patients in just a few weeks.” The GMS works constantly to expand the knowledge base both within and beyond the community of medical geneticists and genetic counselors. It has led or helped to coordinate several nationwide education programs among providers: streaming video seminars, for example, on the evaluation of colon cancer syndromes and polyps; one-day on-site conferences; or training modules available through the VHA’s employee education system. The service is involved in several patient education initiatives, providing veterans and their families with their own knowledge bases – and preparing them to make future decisions about care. Because the emerging field of medical genetics has already proven so significant within the VHA, improving outcomes for many veteran patients and providing them with the information they need to make informed decisions about medical care, Meyer considers it an obligation to get this information to as many as possible. “As a whole, this genetic community tends to share this information extensively – and obviously, as members of the federal government, we share whatever information we’ve generated. But we also draw from academic institutions and the National Cancer Institute. We’re all trying to up everyone’s game.” 21
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
GERIATRICS By J.R. Wilson
n THE DEPARTMENT OF VETERANS AFFAIRS (VA) has had a strong focus on geriatrics, identifying and dealing with age-related health issues among the nation’s veterans, for decades, but changing social attitudes have had as great – if not a greater – impact on VA health care services than demographics. In the 1970s, the largest veteran population in U.S. history – the millions who fought in World War II – began reaching their mid-60s, followed a decade later by a smaller Korean War cohort and a decade after that by the Vietnam War generation. Each successive group had a greater reliance on and willingness to take advantage of VA health care services. By the time of the first Gulf War, new veterans were far more likely to call on VA health care. That trend has increased significantly since the turn of the century with the third-largest veterans group the VA has faced, although one that, for the most part, will not be needing geriatric care until the 2040s. “In the 1970s, the leadership realized the VA would be facing an aging population that would be increasing more rapidly than the rest of the nation and began developing GRECCs [Geriatric Research Education and Clinical Centers],” Dr. Richard M. Allman, chief consultant for VA’s Geriatrics & Extended Care Services, told Veterans Affairs & Military Medicine Outlook. “Now we have 10,000 baby boomers a day turning 65, but the VA rate has been even greater. “The GRECCs look at how we should be caring for older adults, educating the next generation of providers on these issues, and developing new models of care that will allow us to optimally advance the health and well-being of this age group. As a result, the VA has developed models of care for the rest of the nation.” One program that has grown over the past 50 years is home-based primary care for veterans who have trouble getting to clinics. Whenever possible, the VA has created home-based primary care teams – social workers, mental health providers, 22
etc. – to provide care to veterans who can’t reach a clinic. “Our data suggest for high-risk, older individuals, this is a way to prevent emergency room situations,” he said. “Medicare is now testing this concept, but on any given day, the VA has 30,000 veterans reached through home-based primary care.” Since the first GRECC was created around 1975, the VA has established 20 such centers around the continental United States, more than half of them east of the Mississippi. Although Congress authorized up to 25 in 1995, Allman said the budget has
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ On March 29, 2016, Vietnam veterans joined together at the Lexington
VA PHOTO BY MEGAN MOLONEY
VA Medical Center in Kentucky for a flag-raising ceremony to commemorate the 50th anniversary of the Vietnam War. The Department of Veterans Affairs estimates there are more than 7 million living Vietnam veterans.
www.defensemedianetwork.com
focused on expanding access to outpatient, primary care, and mental health services and “trying to do more with less.” He was the founding director of one of the last to be created – the Birmingham/Atlanta GRECC in 2000 – but said there currently are no plans to expand the number of centers. That will place a growing burden on the existing 20 GRECCs, the outpatient, home-based primary care, and other VA services and facilities already in place as the number of veterans aged 65 and over grows from 4 million out of the 9 million currently enrolled to an estimated 4.5 million in the next two decades. “The group that will really be depending on the VA in the next 20 to 30 years will be our aging Vietnam cohort. In 2014, we had 743,000 veterans age 85 or above enrolled in the VA. By 2035, that will be 1.2 million,” he said. “The group over 75 currently is 1.988 million enrolled; between now and 2035, we’re projecting 2.865 million enrolled in that age group. And that’s the group that really needs a lot of care, as long-term services and support increase dramatically at that age. “The big driver for the number of enrollees and utilization is age-related problems as you get older. The average younger or middle-aged person might go to the doctor once or twice a year, while older patients may go three or four times. There also is a shift in the proportion of our veterans who are high priority. In 2014, only 5.27 percent of veterans 85 and older were service-connected high priority, but as the Vietnam era cohort ages, we expect nearly one-third of those over 65 will be in that category.” That is a dramatic shift in demand on VA geriatric services, one that will force the VA to seek out alternative forms of care. “Because of the specialized programs developed after 9/11, more veterans are coming to the VA than in the past,” Allman noted. “The law currently requires the VA to pay for nursing home care for [older veterans], so we’re working very hard [to] honor their preferences for sites of care. Most prefer to stay at home as long as possible, so it is very important for us to optimize geriatric care through home- and community-based services so they can avoid unnecessary nursing home admissions where possible. “In 1900, the average life expectancy was only 42 years; now, it is mid-70s to 80s, so there has been a dramatic extension of life and the number who need these geriatric services has increased. Nearly 60 percent of U.S. citizens live to be 50 or older, and 60 to 70 percent can expect to be in a nursing home at some point, for an average of up to two years. The VA is working hard to plan for this and to have the components in place to meet the challenge of having veterans 23
More Reasons
Why You Should Standardize with Exergen TA Thermometers Exergen TAT-5000S Connected Models are now Available on Leading Vital Signs Monitors for EHR Data Integration
GE Healthcare VC150, V100, Corometrics
Exergen’s Value Proposition: • Improve Patient Outcomes - Exergen has MORE THAN 60 PUBLISHED STUDIES SUPPORTING ACCURACY FROM PREEMIES TO GERIATRICS IN ALL AREAS OF CARE. Unlike other thermometers, the Exergen TemporalScanner does not come into contact with mucous membranes, thus greatly reducing the risk of cross contamination. Additionally, full instrument sheaths, protecting the entire thermometer, can be utilized for all levels of cross-contamination protection. • Improve Patient Safety - Exergen has no probe covers that can break, as often occurs with oral thermometers. With a lifetime warranty, your thermometers can be replaced whenever necessary at no charge. Exergen also has less environmental issues than other thermometer methods, increasing reliability of readings. • Reduce Costs - Exergen doesn’t require expensive probe covers, and with a LIFETIME WARRANTY, COST SAVINGS OF UP TO 90% OVER OTHER THERMOMETRY METHODS can be achieved. Other thermometers can cost hundreds of dollars per year for probe covers and repairs. Exergen TA thermometers cost $0 per year.
Philips SureSigns VS4
Capsule SmartLinx Vitals Plus
• Increase Efficiencies - Exergen’s non-invasive temperature collection can be utilized on virtually any patient situation, therefore ONE THERMOMETER CAN BE UTILIZED THROUGHOUT THE FACILITY. Also, Exergen upgraded the thermometer casing to reduce or eliminate stress micro cracks that can allow harsh chemical cleaners to penetrate the material and cause fractures. • Attractive Payback - Elimination of probe covers and repair costs, and easily affordable acquisition costs results in LESS THAN ONE YEAR PAYBACK for standardizing with Exergen TA thermometers.
TemporalScanner™
Exergen Corporation 400 Pleasant Street Watertown, MA 02472
For more information, please call 617-923-9900 x6234, email: medical@exergen.com, web: www.exergen.com/tat5000s
ZOE 740Select
Schiller Diagnostic Station DS20
VA PHOTO BY REYNALDO LEAL
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
dispersed across the nation, including some in highly rural places.” In addition to veterans living longer and the numbers who served in Vietnam in the 1960s and ’70s and in Southwest Asia since 9/11 creating new bubbles, attitudes toward utilizing service-related benefits have changed dramatically since “the Greatest Generation” went to war in the 1940s. And the VA has had to adjust, as well. “In general, World War II veterans tended to be very independent,” Allman acknowledged, with a large percentage never calling on the VA for health care. “And we’re a different VA than we were in the 1960s, ’70s, ’80s, and ’90s – and hopefully are getting better every day, although we’ll never get it perfect. In geriatrics and the challenges aging veterans have, the VA has a unique continuum of care and cohort of services not available from any other health system I’m aware of. “When veterans are eligible for Medicare after age 65, there is a decrease in demand for VA services, except for areas Medicare doesn’t cover, such as adult day care. Veterans can get those from the VA. After age 80, the number of veterans seeking VA support begins to go up because of the utilization of unique VA services not available through Medicare.” Because it is not just the nation’s veterans who are aging in record numbers, but the population as a whole, the VA is working with other agencies – especially the Department of Health and Human Services (HHS) – to develop and implement services to meet the nation’s overall needs in geriatric medicine. “With the Veteran-Directed Care program, we work in partnership with HHS’ network of providers in the Aging and Disability Network to enhance access to home- and community-based services,” he said. “Many veterans would prefer not to have an agency provider come in and help care for them; they would rather have a neighbor or friend do that. So the Veteran-Directed [Care] program
www.defensemedianetwork.com
■■ A Korean War veteran at a Veterans Day 2014 celebration. The population overall – not
just veterans – is aging in record numbers. The VA is partnering with other agencies like the Department of Health and Human Services to develop and implement services to meet the nation’s overall needs in geriatric medicine.
provides them with a budget that would allow them to stay at home and pay for their own caregivers. We will try to extend that to all medical centers during the next three years. “The GRECCs also have worked closely with centers founded by the NIH [National Institutes of Health] and academic affiliates focusing on aging adults in general and on basic science research, minority health disparities, Alzheimer’s, and Parkinson’s. The GRECCs frequently provide leadership for these NIH-funded centers in finding new treatments for aging individuals, identifying the underlying causes of age-related diseases, and new approaches that might allow us to prevent those going forward.” The VA also is working with the Geriatrics Workforce Enhancement Program (GWEP), administered by HHS’ Health Resources and Services Administration (HRSA), which is working to increase the number of doctors and other health care professionals
trained to care for the nation’s growing older population. “In the past five years or so, our GRECCs developed clinical demonstrations of care, such as helping individuals transition from hospital to home; currently, 20 to 30 percent are readmitted within 30 days, but we believe we can reduce that,” Allman said. “We also developed a hospital and home model where people who show up at an ER with some problems are offered the option of having hospital-level care provided at home. That is lower-cost and often more acceptable to veterans and their families.” Exchanges of information on geriatric care also take place on the international level, with the VA taking part in discussions with its Canadian counterpart and with South Korea in recent years. Another demographic change the VA is working to address is the rapid increase in the number of female veterans, especially since 9/11. 25
Z NE
therma
TM
CONTINUOUS THERMAL THERAPY TM
Caring For Our Veterans is the American Thing to do When You Support VSF, you support: H Housing For Homeless Veterans H Outreach Services & Aid For Veterans of All Conflicts H Benefits For Hospitalized Veterans H Service Officer Program To Assist Families H and many other organizations.
You can donate directly to VSF at:
H www.vsf-usa.org H
or by signing up with the CFC # 11324 â„¢ MILITARY, VETERANS & PATRIOTIC SERVICE ORGANIZATIONS OF AMERICA
VSF is a 501(c)(3) charity to which donations are deductible to the donor.
VHA PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
“Women’s health has been an important issue for the VA for a number of years and we’ve been working to enhance that at our centers, but there is more to be done. The average age of female veterans is about 55 now, so they will be moving into the age 65-plus group in about a decade. Statistically, at that age, women are more likely than men to have problems dealing with day-to-day living, but live longer than men. Roughly 70 percent of nursing home residents are women,” Allman said. “With the aging of the U.S. population, the number over age 65 will double in the next 20 years, but there will be fewer available caregivers. Twenty years ago, there were 30 for each older adult; now it’s 10, and in 20 years it will be four because there are fewer children and they are more likely to be working full time. Our female veterans are less likely to be married and have a spouse or children to care for them, so the need for long-term services and support [is] likely to increase dramatically and there have been reports [that] they are more likely to have service-connected issues.” As with anyone trying to predict the future in a world that changes more rapidly in a single year than it once did in a decade, the VA is uncertain what facilities and health care providers it will need to meet the requirements of an aging veterans population in the decades to come. In President Barack Obama’s budget for the VA – $182.3 billion – one of the largest allocations is $8.588 billion for long-term services and support, which represents only a portion of what will be spent on geriatric care. It also reflects some of the dramatic changes the VA has faced since 2009: • 365,000 VA workers were employed in FY 16, up about 88,000 since 2009 roughly 9 million veterans were • enrolled in VA health care at the end of FY 16, compared to 7.8 million in FY 09 about 58 million VA medical • appointments were scheduled in FY 16, a 6 percent increase in two years • more than 542,000 veterans were rated as 100 percent disabled at the
www.defensemedianetwork.com
end of FY 16, more than double the 265,000 in 2009. “We are looking carefully at current data and needs projections, including a study we hope to have available in FY 18 that will give us an idea on projected needs and resources and how we can best meet future needs, including adapting or changing policies. My guess is we will at least need what we now have in VA-owned and -operated facilities, but there certainly will be more veterans likely needing nursing home admissions if we don’t grow our home- and community-based services. If we do, we may be able to reduce the number of nursing home admissions for our aging veterans. But we don’t have any definitive answers today,” Allman concluded. “In terms of clinic and hospital care, we need to optimize health and wellness services to prevent disease and disability and prolong a healthy, active life among our veterans, avoiding hospitalization whenever possible and helping people make the right decisions for optimal health, including avoiding unnecessary tests and procedures. In the next 10 to 15 years, we will continue to optimize disease prevention and health promotion efforts and slow the rate of rise we otherwise might expect. But we will need more doctors.”
■■ The first Geriatric Research, Education
and Clinical Center (GRECC) was established around 1975. Today, there are 20 centers around the continental United States, providing focused care for aging veterans.
27
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
SHEREEF ELNAHAL, M.D., M.B.A. Assistant Deputy Under Secretary for Health for Quality, Safety and Value, Veterans Health Administration, Department of Veterans Affairs By Rhonda Carpenter n DR. SHEREEF ELNAHAL is the assistant deputy under secretary for Health for Quality, Safety, and Value at the U.S. Department of Veterans Affairs (VA). He was initially appointed to the VA as a White House Fellow in 2015, and in that capacity, founded the Diffusion of Excellence Initiative, the major initiative meeting the under secretary’s priority of establishing consistency in clinical and administrative best practices. He has authored many publications on health care quality, operations management, and patient safety. Elnahal co-developed a published methodology that doubled clinic efficiency in the Johns Hopkins Pancreas Multidisciplinary Cancer Clinic, cutting patient wait times by half. As an operations consultant for Wright-Patterson Air Force Base, Ohio, and Pittsburgh VA hospitals, he expanded on that work to improve care access for veterans and active-duty service members. He was a fellow in the Armstrong Institute for Patient Safety and Quality, and served as chair of the House Staff Patient Safety and Quality Council at Hopkins. Elnahal served on advisory boards for two firms focused on patient education and clinical operations. He also co-founded the Baltimore chapter of The Triple Helix, a 501(c)(3) nonprofit that publishes an internationally circulated journal on science in society. His civic contributions earned him the 2015 National Quality Scholar Award from the American College of Medical Quality. Elnahal received a dual-degree M.D. and M.B.A. with distinction from Harvard University. He also graduated summa cum laude with a B.A. in biophysics from Johns Hopkins University. Veterans Affairs & Military Medicine Outlook: Could you briefly explain what the Diffusion of Excellence Initiative is and how is it helping veterans receive their health care? Dr. Shereef Elnahal: The Diffusion of Excellence Initiative was commissioned two years ago by Secretary David Shulkin, M.D. [then the Veterans Health Administration (VHA) under secretary], to achieve consistency across the entire VA hospital system. The easiest way to describe the way in which 28
■■ Dr. Shereef Elnahal, assistant deputy under secretary for Health for
Quality, Safety, and Value, Veterans Health Administration, at the U.S. Department of Veterans Affairs.
the initiative has been resonating with veterans is to think about their social networks. Many have friends all over the country as a result of their service. For example, a veteran receiving care in one part of the country visits a friend or a family member receiving care at a VA health care facility elsewhere in the nation. He or she
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
hears about an amazing practice, sees the way a clinic is set up, learns about a model of care, or witnesses great customer service, and wonders: “Why isn’t this service offered at the VA I normally visit? Why isn’t it available and consistent for veterans across the country?” This is the consistency in service and practice our initiative is trying to achieve. It’s about finding excellence wherever it exists in VA, diffusing it across the system, and making it a standard part of what VA does for veterans.
VA PHOTOS BY KATE VIGGIANO
Thank you for including those examples as you went along. Can you tell us how it was developed? This all started in October 2015, when I launched the initiative at Dr. Shulkin’s direction. Just about six weeks before that, when I first entered the VA as a White House Fellow, Dr. Shulkin outlined his five priorities for transformation of VHA. One of those priorities was achieving consistency in best practices. I started with a solicitation through a VA social media platform called “VA Poll” with a simple request for all frontline employees to submit an example of projects they led that have made changes for veterans that supported one of Dr. Shulkin’s other four priorities. These priorities included access to care; employee engagement; care coordination across care delivered both within the VA and in the community; and restoring veterans’ trust and enhancing the veteran’s experience through highquality care. We made an open-ended solicitation for projects that could be completed within six to 12 months that had made tangible improvements in care or enabled very high performance in one of those priority areas, and asked for submissions. I expected to get, maybe, a few dozen examples of people making changes. We got over 300 submissions in the first solicitation. I did not expect this level of interest among employees. So one of the principles we have developed is empowering frontline employees who are doing the work every day and interfacing with veterans every day to propose, or at least tell us about, changes they have already made to improve the veteran’s experience. We’ve built upon the tremendous level of interest we received ever since. Are the solicitations ongoing or was this just a kickstarter that then propelled toward the initiative? Since the initiative’s start, we’ve had tremendous success in driving adoption of best practices. By now, we’ve had more than 450 examples of replication projects to support a discrete set of best practices. We had no choice but to continue the effort. We are now in our third round of solicitations. We are about to announce our semi-finalists for the third round. We have developed a set of 26 best practices thus far that we’ve endorsed to be spread nationally across VHA. And we’ve built a structure for internal operations within VA Central Office to be able to do this well.
www.defensemedianetwork.com
■■ Dr. Shereef Elnahal speaking at the Diffusion of Excellence
Planning Summit, March 2016.
More importantly, we’ve provided tools to and received endorsements from lay experts and leaders throughout the VHA system, so that these projects are being picked up within the system every single day. The way I know they’re being picked up is through a tool called the “Diffusion Hub,” which every single person in the system interested in best practices uses to start a project, and to replicate others, in their hospitals. We’re seeing a tremendous level of engagement and, as a result, have continued with three rounds of solicitations. Every six months there will be a new one. Research has shown that it takes an average of 17 years for evidence-based practices to find their way into everyday care. Is the Diffusion of Excellence speeding that adoption, and if so, how? Yes, and we are trying to reduce that time frame from 17 years to just one year. The way we’re doing that is by setting up an infrastructure that allows for effective communication channels. It gives teams in the field the right tools to hear about great work that is being done in clinical care and to be able to actually start projects to replicate that great work. So again back to the program’s basics: The Diffusion Hub and our system of governance and our operating model are helping. It’s not just technology. We bring people together every six months for what we call a planning summit, where innovators of best practices interact directly with people who are replicating them. The way we get to that point is through an event we call the “VA Shark Tank,” where finalists from throughout VHA pitch the value of their work to medical center directors across the country. Instead of rich people and personalities, you have executives in hospitals making decisions about what projects they 29
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
30
■■ A soldier working in the Fort Drum, New York, pharmacy. In
one successful best practice, in Madison, Wisconsin, clinical pharmacists worked alongside primary care teams, taking the lead to discuss medication needs with patients and freeing up primary care doctors’ schedules to see patients with medical needs.
platform people can easily use, and pick up these projects on their own. That’s how we are getting these projects scaled and available to as many places as possible in the system. You just stated the words I was going to ask about. What is the Gold Status best practice? Does that relate back to the 15 or 20 of the sharks, if you will? It does. Gold Status best practices are what we end up with after our solicitation rounds go through the complete process. Let me describe to you how the process goes. The very first thing we do when we receive a submission is to send that submission to peer employees across the system who would be able to comment on it. For example, one of our Gold Status best practices was to develop group therapy sessions led by chaplains for veterans with moral injuries [people who have undergone events that transgress deeply held moral beliefs and expectations] that had led to PTSD [post-traumatic stress disorder]. Normally, a veteran with a moral injury will go to a psychologist or psychiatrist for medical intervention and counseling. This is an innovative way of helping veterans coping with moral injuries to deal with
www.defensemedianetwork.com
U.S. ARMY PHOTO
would like to bid on. And their bids aren’t money directly. They offer resource allocation within their own facilities to be able to get projects completed. That comes in the form of people, time, funding to implement technology, space, and equipment purchasing. So, it ultimately does come down to money. But the way we are getting the bids, and the form of the bids, are in terms of resources and resource commitments medical center directors are making across the country. At the end of that event, we end up having 20 finalists and multiple bids for those projects in different places. And we ultimately narrow it down to between 10 and 15 projects we consider Gold Status, and at the end of the planning summits, people are going back to their facilities ready to go to replicate the project. Because we have this tool [the Diffusion Hub] that has all the projects on it, replication is not just limited to the people who come to this summit. We end up getting a tremendous amount of what we call organic engagement – people picking up projects on their own because they are hearing about them. And because everybody’s contact information is on this electronic platform, people can easily reach out to the facilities where these projects originated. So that is another way in which we’re seeing a tremendous proliferation. People are more easily able to do that because we intensively project manage the initial round of replications. These are where the “sharks” have chosen someone to own the project. And we provide project management support and extensively document these experiences so we can put a toolkit on this
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
their illness by bringing chaplains into the mix and getting groups of veterans together to counsel each other, as well as to develop a more spiritual approach to veterans’ treatment. This practice went to other chaplains across VA that are available to us to evaluate these submissions. We asked a simple question: “Would this work at your facility and do you think it’s a valuable project for veterans?” So, that input is the first round of evaluation. If those evaluations are positive, we send the submission to subject-matter experts for a second round. Now we have VHA’s chief of chaplains and mental health professionals who have national leadership roles and are known for their expertise looking at these projects. That’s the second round of evaluation. We then bring it to the Shark Tank, where we have essentially a market-based mechanism for medical center directors, who know their priorities and know what their problems are in their facilities, to bid on these projects. So we then have that level of evaluation and endorsement. Finally, the practice goes to medical centers and VA leadership at the senior level nationally to pick final Gold Status best practices. They assess the project’s alignment with organizational priorities and whether they want to put their names behind these projects. That is the final hurdle before we say that these are the sets of projects we are determining to have Gold Status. And what Gold Status means is that we would like to see these projects replicated in as many facilities as possible, if not in every site of care throughout the VA system. What are some examples of nonclinical best practices? I think you just touched on that. Yes, that’s one of them. Another one I really like is a project that involves VA employees who don’t normally interface with veterans because of the nature of the work they do. People who process claims and those who are involved in logistics and getting supplies where they need to go are just a couple of examples of that type of employee. There is now an organized program enabling those employees to be able to follow a veteran through their experience in the VA. They take a day off from work and are assigned a veteran who volunteers for this program. They get to talk with the veteran throughout their VA experience and sit with them in waiting rooms. If the veteran is comfortable, they can even sit in on the appointments – obviously with the veteran’s consent. They get to really understand what a veteran goes through when they interface with the VA and, of course, they can ask the veteran about their service to better understand the great people we serve every day. We have the best patients in the world, but it’s not necessarily apparent to every employee if they don’t interface with our patients and our veterans. This project allows them to experience firsthand what our mission really is. The analogy I like to make is to NASA, where a reporter famously asked a custodian who was cleaning the floors in one of NASA’s buildings, “What are you here doing right
www.defensemedianetwork.com
now?” And that employee answered, “I’m helping to put a man on the moon.” That is the mentality that we want to have in terms of increasing our employees’ engagement with the mission. And this is just one example of a project that has been really successful in doing that. I would classify it as administrative, because it’s not directly related to clinical care. But it’s something that is very important and something we’re trying to spread to as many places as possible. So, if I were a VA employee working at a medical facility specifically, I could submit a best practice for consideration and I think you said that would go through the hub? Yes, any employee in the system can submit something. We ask that their immediate supervisors are aware of their submissions so that if the employee is asked to be on the Shark Tank and asked to come to planning summits, their supervisors would be aware. Last fall, you and Dr. Carolyn Clancy, who is the VHA deputy under secretary for Health for Organizational Excellence, testified before the Senate Committee on Veterans’ Affairs about the initiative. Can you tell us briefly what some of those responses were? We received a tremendous level of interest from senators. In fact, after the hearing, a number of them on both sides of the aisle, both Democrats and Republicans, issued press releases about specific projects that were going on at facilities in their states. So we had a lot of positive feedback in that hearing about our model. We had two frontline employees come testify with us. It was not just Dr. Clancy and myself. One of them, Dr. Kimberly Garner, associate director for Education and Evaluation for Veterans Integrated Service Network [VISN] 16, had started a project in Little Rock, in which she brought groups of veterans together to tell them about a really important factor in their care planning called advanced directives. This is an effort that allows everybody on the care team to know what a veteran’s preferences are for care at the end of his or her life. Bringing that level of control was something this employee found so important that she, on her own volition and her own time, set up this program. It got great results because the number of advanced directives filed at that site is quite high. So that’s just one example. She was there testifying with us. Another person who was with us was Scott Bryant. He was an innovation specialist in Chicopee, Ohio, and had created a number of projects that helped veterans not so much with their care, but with the job skills they needed to go into the private sector and be successful in getting a job. These employees proved that VHA is not just a health system. We serve so many other needs veterans have and really support the whole veteran in our mission. The [senators] really appreciated it. They got to speak directly with frontline employees who highlighted the great work they were doing. And again, we know they were clearly happy with 31
TAKE YOUR NEXT STEP
UNIVERSITY OF UTAH COLLEGE OF NURSING You know what it means to serve. We want to help. Our programs will help take your career to the next level. • Online RN-BS • Doctor of Nursing Practice (Post-BS to DNP) programs: · Adult/Geron Acute Care NP
· Neonatal NP
· Adult/Geron Primary Care NP
· Family NP
· Psychiatric/Mental Health NP
· Midwifery
· Women’s Health NP • Doctor of Nursing Practice (Post-MS to DNP): · Organizational Leadership NP Distance options available. The VA offers scholarships for VA nurses seeking advanced degrees. Search: National Nursing Education Initiative APPLY NOW or get in touch to find out if one of our programs can fit your needs.
NURSING.UTAH.EDU | 801.581.3414
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
what they saw because they sent press releases immediately after this hearing, which we appreciated at the VA. But we know it was because they were convinced that these projects were helping veterans in ways that were tangible and meaningful.
VA PHOTO
Where do you see the initiative in five years or 10 years? My goal would be for this not to be considered its own separate initiative in five years, but rather embedded into the work we do every single day. The idea that we need to find what we’re doing well and spread it to other places should come naturally. We don’t want Diffusion of Excellence to be its own project or initiative. We want it to be a normal part of what the VA does every single day. So we’re starting to do that. We now have a pack of performance standards designed to support best practices baked into the performance plans of some of our senior leaders in the organization, including medical center directors and directors of our networks who preside over many VA facilities. Both facility and network directors are responsible for contributing and reapplying best practices at their own sites. That’s the first step in really getting this embedded into what networks and facilities do on a regular basis. Is there anything I haven’t asked that you would like to add? I just want to give you a sense of the impact that is possible with this type of approach. One of our really successful best practices involves clinical pharmacists embedded in some primary care teams. These are professionals who know a lot about medication, dosing, and regimens, including optimizing what medications veterans should take to the veteran’s needs and capabilities. The exact schedule for medication will depend on the whole veteran and what they can do practically. These professionals are so good at this specific aspect of their care that they’re better than physicians at making these very
www.defensemedianetwork.com
■■ VA Eastern Colorado Health Care System (ECHCS) Director Sallie Houser-Hanfelder,
American Federation of Government Employees Local 2241 President Bernard Humbles, and White House Fellow Dr. Shereef Elnahal observe medical support assistant scheduling training at the ECHCS as part of the VA’s second national “Access Stand Down” one-day event, Feb 27, 2016.
specific decisions in many cases. So in Madison, Wisconsin, frontline clinical pharmacists who set up a model to be able to do this convinced doctors on their care team they should transfer appointments that were made specifically to discuss medication issues to the pharmacists’ schedules. So essentially what the primary care doctors do now is to look at their schedules in advance and transfer those appointments to a clinical pharmacist. Ultimately, this was ingrained into the operations of the clinic to the extent that when a patient first called to schedule an appointment, a decision would be made about whether this was a medication issue or if it required the input of a physician. Pharmacists were able to see those patients up front. As a result, the physician’s schedule was freed up from 28 percent of their appointments. That’s 28 percent of the primary care doctor’s appointments that could be safely transferred to a pharmacist. Those patients got superior care for that specific medication issue. And primary care doctors could see more
patients for problems that only a physician could address. So the idea not only improved the quality of care for veterans in terms of their medication management, but also improved access overall for primary care about 28 percent. That can be scaled across the whole system. VA does about 58 million appointments a year in total, with a subset of those being primary care appointments. You’re talking about tens if not hundreds of thousands of additional appointments we could offer across the whole system if we were able to apply this model everywhere. That’s what we’re working on. The Diffusion of Excellence Initiative is really about impact on a mass scale, reaching hundreds of thousands of veterans as a result of the work of just one or several employees in the workplace. If we’re able to establish this model and make it successful in a sustainable way every year, we’re talking about having an impact on the care of millions of veterans. That is the vision and hope we have for this initiative. 33
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
PRECISION MEDICINE The VA and DOD Are Helping to Lead Nothing Less Than the Transformation of American Medicine. By Craig Collins
n IN 2015, WHEN PRESIDENT BARACK OBAMA announced the sweeping federal research effort known as the Precision Medicine Initiative (PMI), many Americans had never heard the term “precision medicine” before – but it was far from a new concept. The agency in charge of the PMI, the National Institutes of Health (NIH), defines precision medicine as “an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment and lifestyle for each person” – which sounds like a pretty conventional idea: Practicing medicine tailored to a patient’s individual needs is more effective than applying the “one-size-fits-all” approach. An obvious example would be giving blood transfusions matched to a patient’s blood type, rather than from randomly selected donors. But such examples of precision medicine are fairly limited. The launch of the PMI was in part an acknowledgement that recent technological advances in our abilities to both decode genetic information and to compile and analyze vast quantities of data have moved medical science to the threshold of an exciting new era, beyond which precision medicine will become the rule, rather than the exception. By the time the PMI had been established, precision medicine work was already well underway in the Military Health System and the Veterans Health Administration. In fact, one of the reasons the NIH was able to set such an ambitious goal for its own research – a plan to study a group (cohort) of at least a million volunteers from around the country – was because it had established a cooperative relationship with the Department of Veterans Affairs (VA), which was already four years into the largest study ever of this kind: the Million Veteran Program (MVP). By August 2016, more than 500,000 veterans had volunteered to provide genetic, military service, lifestyle, and health information to the largest database of its kind in the world, an integrated health and genomic database tied to the nation’s largest health care system. Several studies of the MVP cohort are already underway, examining the role genes play in cardiovascular risk, substance abuse, metabolic disorders, Gulf War illness, kidney disease, and 34
age-related macular degeneration. Investigators in these studies will examine genetic and other data from anonymous blood and tissues samples, donated by veteran volunteer participants in VA studies and stored at the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC) in Boston. With NIH in the lead, the PMI will use the experience gained by the MVP’s architects in putting together its own cohort, biobanks, secure data sets, and computer networks. MVP volunteers will be invited to enroll in the PMI, offering the national initiative a leg up in building its own cohort. Likewise, precision medicine had been a focus of study within Department of Defense (DOD) research institutions for years by the time the federal PMI was established. According to Terry Rauch, Ph.D., the acting deputy assistant secretary of Defense for Health Readiness Policy and Oversight, “There are probably about 300 studies we have going on within DOD in the area of genomics, health care and medicine.” TARGETING CANCER TREATMENT
The PMI is, essentially, an effort to gain better insights into the biological, environmental, and behavioral influences on diseases that have so far eluded a proven means of prevention or treatment. The most obvious example of this type of disease is cancer, which explains why expanding precision medicine in the area of cancer research is one of the initiative’s short-term goals, and why the Cancer Moonshot, a $1.8 billion effort to accelerate cancer research, had been funded by Congress in December 2016. The new program is led by the National Cancer Institute (NCI), one of the National Institutes of Health. This may be precision medicine’s most exciting nearterm promise: its potential to transform the way cancer is prevented, diagnosed, and treated. Nearly a third of MVP enrollees have reported a cancer diagnosis, offering researchers a resource for exploration and analysis. Military
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Then-President Barack Obama delivers remarks at the White House during the unveiling of the Precision Medicine Initiative highlighting
OFFICIAL WHITE HOUSE PHOTO BY PETE SOUZA
his 2016 budget request investments to improve health and treat disease through precision medicine, Jan. 30, 2015. Obama explained that precision medicine is “delivering the right treatments, at the right time, every time to the right person.” At right is a DNA model.
and veteran cancer expertise – in the Murtha Cancer Center at the Walter Reed National Military Medical Center in Bethesda, Maryland; in The American Genome Center (TAGC) at the Uniformed Services University of the Health Sciences (USU); and throughout the portfolio of more than 260 ongoing cancer studies among VA researchers – make the DOD and VA uniquely qualified to help lead these efforts. For more than 25 years, blood serum from service members has been collected and stored at the DOD Serum Repository in Silver Spring, Maryland, an effort that began as a means of enabling infectious disease research. A team led by Army Col. Craig Shriver, M.D., director of the Murtha Cancer Center, is at work on a longitudinal study of samples donated over time. Shriver’s team, Rauch said, can create a kind of molecular timeline to track changes in a person’s blood. “We can go into the serum repository,” Rauch said, “and pull a service member’s serum from before they were diagnosed with cancer, at the point they were diagnosed, and then at different periods of time post-diagnosis. And in that serum analysis, we can look for different protein signatures, and through that
www.defensemedianetwork.com
exploratory protein analysis, try to find signatures or markers to help us diagnose cancer earlier and track how well service members are recovering from their cancer treatments. We can look for serum markers in previous tests that indicate cancer recurrence.” DOD is now evaluating the first set of those serum samples through testing at the Pacific Northwest National Laboratory, a premier protein analysis center. Another initiative prompted by the Cancer Moonshot is the APOLLO (Applied Proteogenomics Organizational Learning and Outcomes) program. Developed by the Murtha Cancer Center in collaboration with the NCI, USU, and the VA, APOLLO will tap into the remarkable array of tools available among these partners, classifying tumors (with an initial focus on lung tumors, to be followed by gynecologic, prostate, breast, and other malignancies) not only by genetic changes, but by levels of certain proteins. APOLLO is the only program of its type in the world to perform molecular analyses of every possible gene mutation and protein expression identifiable at high-throughout scales. The data generated will be analyzed in conjunction with NCI and outside experts, and
35
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Researchers prepare biological specimens. Much of today’s cancer research is influenced by the increasing focus on precision medicine, a
will predictably result in new insights into the biology of various cancers, as well as new cancer treatment targets that can be evaluated in clinical trials. These data ultimately will be shared with other researchers through NCI’s Genomic Data Commons programs. Michael Kelley, M.D., VA’s national program director for oncology and a professor at the Duke University School of Medicine, said the APOLLO program’s ability to track protein expression, in addition to genes, is one of its most exciting elements: “There’s some information that tells us, in terms of prognosis, that looking at proteins may be better than looking at just genes alone. We can look at all the genes, all 23 or 24 thousand of them, and it’s not that expensive and it doesn’t take that long. For proteins, it’s much more complex.” The driving purpose of APOLLO is to move genetic discoveries from the lab to clinics – and the VA took a historic 36
step toward doing that last year, when Kelley established its Precision Oncology Program. The program makes genetic testing available to VA cancer patients for whom testing may help determine either a course of treatment or a prognosis. Precision oncology is such a new field that there haven’t been many drugs or chemotherapies developed to target tumors with specific mutations, but as studies continue to fuel new discoveries, the VA’s Precision Oncology Platform is positioned to put these new drugs and therapies to use for every VA cancer patient. “That’s really the core paradigm of what we’re working on with precision oncology,” said Kelley. “There are other aspects to it – in terms of prognosis, simply helping us understand the patient’s tumor better. And that can give us better information about what to expect for an individual patient, in addition to helping guide us in terms of treatment decisions.”
www.defensemedianetwork.com
NIH PHOTO
patient-centric approach that emphasizes genetic analysis to identify health risks and optimal treatment strategies for each individual.
Online Degrees
Define Yourself
with a degree from IWU
SOME PROGRAMS ARE ALSO OFFERED
Onsite EDUCATION CENTERS IN
INDIANA OHIO KENTUCKY •
DISCOUNT available to active duty, national guard, reserves, spouses and veterans*
•
MILITARY CREDITS ACCEPTED
•
Choose from over 90 DEGREE PROGRAMS Not all programs are offered at onsite locations. *Some restrictions apply.
CHAPTER 33 YELLOW RIBBON PROGRAM
indwes.edu 866.498.4968
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ In this image from a genetically
BEYOND CANCER
Because every cancer begins with a genetic mutation, its relationship to the concept of precision medicine is obvious, but the data that can be used to personalize medicine – for cancer as well as other diseases – includes a patient’s history, lifestyle, and environmental factors. One of the first studies of the MVP cohort is looking at the complex interrelation of risk factors for cardiovascular disease, including family history, ethnicity, age, diet, alcohol consumption, and physical activity. Another recently launched VA study, PRIME Care (PRecision Medicine in Mental Health), will be centered at the Philadelphia VA and led by David Oslin, M.D., director of the regional (VISN 4) Mental Illness Research, Education and Clinical Center. The purpose of the study – which is scheduled to begin the recruitment phase in 38
summer 2017 – is to determine the best way of using genomic information to better treat depression in veterans. A common metabolic pathway for some antidepressant medications, Oslin explained, is an enzymatic reaction in the liver known as the cytochrome P450 system, and there’s a known genetic variation in that system that makes some drugs less effective for patients who carry it. “They would end up metabolizing a particular drug in a very different way,” said Oslin, “than people with a normal expression of that gene.” The way antidepressants are prescribed today doesn’t account for such differences, and the purpose of PRIME Care, said Oslin, will be to lay the groundwork for genetic tests and lab work that can help prescribers match drugs and dosages to patients. One commonly administered drug, sertraline (Zoloft®), is usually dosed at around 100 milligrams. “But some people do fine on 50 or 75,” Oslin said, “and some
need to be at 200. Is that because of differences in genetics? We have no idea … and that’s why we’re doing the trial.” The DOD recently launched a partnership with the National Collegiate Athletic Association (NCAA) to study and prevent concussion. Known as the CARE (Concussion Assessment, Research and Education) Consortium, the effort builds on findings of the landmark Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS), which revealed genes and biomarkers that associated with risks for post-traumatic stress disorder (PTSD), suicide, and persistent postconcussive symptoms related to traumatic brain injury. Each of the military service academies belongs to the NCAA, Rauch explained, and every Army and Air Force cadet has been enrolled in the CARE Consortium, which will establish baseline blood and serum assessments. In the event of a head injury, a participant will enter into a more defined protocol to track any changes in blood work or brain images that might have occurred after the brain injury. “We’re looking now at trying to determine certain proteins and certain genes,” Rauch said, “that may be active or shut down as a result of head injury in the natural recovery from concussion.” The Army STARRS study is one of several to reveal a correlation between PTSD and cardiovascular disease – a condition recognized since the Civil War, when doctors documented a condition among combat veterans known as “soldier’s heart.” A recent partnership formed by the National Heart, Lung, and Blood Institute and USU is aimed at exploring the findings of the
www.defensemedianetwork.com
NIH IMAGE
engineered mouse model, lung cancer driven by the KRAS o ncogene shows up in purple. As a key driver in many types of cancer– such as colon, pancreatic, and lung cancers – the KRAS gene makes a promising target for new cancer therapies.
VHA PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Army STARRS study further using one of the most powerful investigative tools available to DOD and VA researchers: the TAGC at USU, one of only four academic whole-genome sequencing centers in the United States, and the only one within the federal system. The goal of the new Collaborative Health Initiative Research Program (CHIRP) is to explore the genomic relationship between PTSD and cardiovascular disease. “There actually may well be a very powerful genetic basis to this association,” said Art Kellermann, M.D., M.P.H., dean of USU’s F. Edward Hébert School of Medicine. “The genes that are involved and activated by PTSD may turn out to be many of the same genes involved in risk factors for cardiovascular disease.” The ability to sequence a genome, however, is only part of the equation; the ability to detect and understand correlations among the millions of genes sequenced during a study by the TAGC is enabled by extraordinary computing power. This explains why the VA recently partnered with the Department of Energy, where 32 of the fastest 500 supercomputers in the world reside, to comb through data from the MVP cohort. At USU, the work of analysis and interpretation is done by an installation known as the Bioinformatics Core. Kellermann looks forward to being able to produce actionable clinical data through the CHIRP program for Army STARRS participants. “We’re currently standing up that capability,” he said. “If it turns out you have a heightened risk of coronary artery disease, we want to be able to get in touch and work with you to help prevent the heart attack you might otherwise be facing a few years down the road. That’s where the power and ultimate utility of precision medicine will come from.” Another USU-led precision medicine initiative, the Surgical Critical Care Initiative (SC2i), is designed to study biomarkers associated with wound infection. “If we can develop a biology-based approach that looks
www.defensemedianetwork.com
■■ As part of the 2016 Nationwide Access Stand Down event, the William Jennings Bryan Dorn
VA Medical Center, Columbia, South Carolina, hosted an informational open house offering information ranging from improvements to patient care and nursing services to veterans benefits in general, Feb. 27.
at inflammatory biomarkers, exudate from the wound, quantitative cultures, and a number of other factors using machine learning,” said Kellermann, “we’ll have a much higher rate of accuracy and competence for decisionmaking on wound closure. We’ll give better care to soldiers, it will cost less money, and we’ll have better outcomes.” The combination of capabilities emerging in the VA, the Military Health System, and the federal government have ushered in a new era of discovery. “We’re able to do things we would only have dreamed about doing a few years ago.” One of the most exciting frontiers in precision medicine is the potential for generating exact genetic copies of tissues that might be used to model treatments for individual patients. The first successful attempt to do this, using induced pluripotent stem cells (iPS; cells that can be modified to grow into any kind of tissue desired), was in 2006. “With iPS cells,” Kellermann said, “you could program cells with a genetic biochemical makeup to grow into tissues, and test them for drugs or treatments,
and know exactly what’s going to happen before you expose a patient to that. And we’re actually doing some really cool work in bio-printing here where we’ll be developing an artificial gut or artificial lung in order to do that kind of testing.” Bio-printing copies of a person’s tissues for testing drugs may sound far out – but it’s around the corner, Kellermann said, and, like the other innovations introduced by precision medicine, it promises to bring optimum care to warfighters and veterans. “At the same time, the discoveries are going to benefit civilian medicine in the United States and around the world, very much like advances in combat and battlefield care have advanced civilian trauma surgery,” he said. “We’re working closely with Walter Reed, NIH, our colleagues at the VA, and military hospitals around the country – a health care system with millions of beneficiaries, a global reach, and a diverse population of people who represent all the different groups that make America great. It’s exciting to think of what we can do with this.” 39
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
21st CENTURY ORTHOPEDICS By Craig Collins
n ORTHOPEDICS – THE MEDICAL SPECIALTY FOCUSING on injuries and diseases of the musculoskeletal system – is an area of particular concern for the military and veteran medical communities. Whether in training or in combat, warfighters typically walk or run long distances over rough terrain, often carrying gear that can weigh more than 100 pounds. They jump out of aircraft. They sit for long periods in cramped spaces. Research by both the departments of Defense (DOD) and Veterans Affairs (VA) indicates that service members have a greater risk of musculoskeletal injury, particularly to vulnerable load-bearing areas such as the hips, knees, ankles, and spine. Recent work by the VA’s War Related Illness and Injury Study Center has produced several eye-opening findings, including: • Basic training installations average six to 12 injuries per month for every 100 recruits. • Army garrisons average 10 to 12 injuries per month for every 100 soldiers, with 80 to 90 percent of limited-duty days related to physical training. • 51 percent of Army soldiers in one study were injured in a six-month period, a rate of 142 injuries annually per 100 soldiers. • Among soldiers deployed to Afghanistan, 45 percent were injured within 12 months, the most common sites of injury being the lower back, knee, and shoulder. Eight percent of these injuries occurred in physical training, rather than in combat. Given such numbers, it isn’t surprising that osteoarthritis – the degenerative disease often associated with injury or prolonged “wear and tear” of joints – is the second-most common reason soldiers are discharged from the Army. Osteoarthritis is the leading cause of disability in the United States, and 1 in 4 veterans (25.6 percent) suffers from the disease, compared to 1 in 5 civilians. 40
Given the significance of these injuries among active-duty service members, and of the consequent degenerative diseases that can lead to debilitating pain among veterans, orthopedics has been a vital focus for investigators, particularly at the VA, where clinicians are charged with treating these conditions post-deployment. For active-duty service members and veterans alike, these technological breakthroughs offer exciting glimpses of a future that involves more mobility, less pain, and a better quality of life for those with musculoskeletal problems. REGENERATIVE MEDICINE
Most often, joint pain is caused by the degradation of cartilage, the smooth rubber-like tissue that pads the junctions of bones. As cartilage wears down, bones rub against each other, causing stiffness and pain. This is true for the long bones of the limbs as well as the vertebrae of the spine, which are cushioned by cartilaginous disks. A 2012 Army study found degenerative disc disease (DDD) to be a significant problem among active-duty service members: Between 2001 and 2010, nearly 132,000 active-duty personnel were diagnosed with DDD. Standard treatments for DDD today include spinal fusion – fixing two or more vertebrae together, which decreases pain but also reduces mobility – and disk replacement surgery, in which the cartilage is removed and replaced with an artificial disk made of metal and/or plastic. Harvey Smith, M.D., a spinal surgeon at the Philadelphia Corporal Michael J. Crescenz VA Medical Center and assistant professor of orthopedic surgery at the University of Pennsylvania, pointed out that while prosthetic disks have generally performed well, “all mechanical replacement devices involve inherent concerns about wearing out over time.”
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ LEFT: A patient wears a
LEFT: COURTESY DEPARTMENT OF VETERANS AFFAIRS; SALT LAKE CITY HEALTH CARE SYSTEM RIGHT: COURTESY OF VA SALT LAKE CITY HEALTH CARE SYSTEM
prosthetic limb connected to the post of a POP (percutaneous osseointegrated prosthesis) implant. The post is attached to an internal stem that is implanted into a patient’s residual bone. RIGHT: A POP device features a titanium rod that is surgically implanted into the bottom of the femur. The post then serves as a connection to an artificial leg.
With his co-investigator, VA researcher Robert Mauck, Ph.D., Smith is at work on a series of studies designed to create a new kind of replacement: a biologic intervertebral disk, produced from living tissue, that they’ve grown in a lab before transplanting it successfully in rats, rabbits, and most recently goats, whose vertebrae more closely resemble those of humans. Smith’s disk is made of two parts: an artificial nucleus pulposus, the soft inner ring of the disk, made of a special hydrogel, and the hard outer annulus fibrosus, made of a biodegradable polyester. Both of these components are seeded with stem cells. “Once it’s implanted,” Smith said, “it’s designed to grow on its own. Our ultimate goal is that after a certain period – and this could take years – it’ll all be living tissue. The materials we initially use as carriers for the cells will be, over time, replaced by the body.” It’s still early, but the results so far are encouraging, Smith said; the animals are walking around and behaving normally after the surgery. Smith and Mauck are moving the study into
www.defensemedianetwork.com
a second stage, implanting the biologic disks in up to 72 goats and evaluating the results. The day when humans receive bioengineered disk transplants, Smith cautioned, is a long way off – but in the meantime, he and his team are learning more about the individual parts of the intervertebral disk and about how to get engineered tissue to integrate into surrounding bone. “I think there will be a lot of offshoots from this,” he said, “as we’re learning things that have applications to other areas in orthopedics, both in the spine and elsewhere.” The approach used by Smith and Mauck is on the leading edge of translational research, a field broadly known as “regenerative medicine”: replacing, engineering, or regenerating cells or tissues to restore or establish normal function. But tissue engineering is only one way in which cells might be regenerated; there are known methods for stimulating the body’s own repair mechanisms. Daniel Clegg, M.D., chief of rheumatology at the VA Salt Lake City Health Care System and professor at the University of Utah School of Medicine, recently launched a pilot project to investigate the effectiveness of one of these methods: ultrasonic therapy, which has been proven to generate bone and cartilage growth. Clegg’s pilot trial will evaluate how effective a commercial device used to help heal fractures may be in treating osteoarthritis of the knee – either slowing the progression of cartilage degeneration or stimulating the growth of new cartilage 41
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
in the knee joint. Participants in the study, which is still in the recruitment phase, will sit with the device attached to their knee by an elastic cuff – “The whole thing looks a lot like a wristwatch, actually,” Clegg said – for daily intervals of 20 minutes. Half these participants will have a working device, applying low-intensity ultrasonic waves to their knee cartilage, and the other half will have a non-working “placebo” device. “We have two primary outcome measures,” Clegg said. “One is pain relief, and the other is slower cartilage degeneration. We’d be delighted to have regeneration, but we’d also be pleased if we could demonstrate that it simply took longer to develop osteoarthritis.” BETTER METHODS, BETTER MODELS
Mechanical joint replacements, of course, can work well for many patients – and they’re working better for an increasing number of people, thanks to refinements in both materials and methods. At the VA Center for Limb Loss and MoBility (CLIMB) in Seattle, investigators are re-evaluating a surgical procedure that had previously fallen out of favor: total ankle replacement. As Bruce Sangeorzan, M.D., CLIMB’s director, explained, the balland-socket prostheses introduced in the 1970s “just didn’t last. They loosened. They caused pain.” While a better understanding of materials has led to great improvements, many patients with osteoarthritis of the ankle continue to opt for ankle fusion – fixing the ankle joint so that the bones eventually grow together and immobilize the joint – instead of replacement. Ankle fusion works fine for many patients, said Sangeorzan. “When you’re walking down the hallway in shoes, no one knows you have an ankle fusion,” he said. “But if you walk barefoot, or if you walk on a hill, or down stairs, it becomes more obvious that the ankle is fused.” A few years ago, Sangeorzan and colleagues at CLIMB launched a pilot study comparing outcomes for fusion and replacement, the first prospective comparative study of its kind. Patients with ankle replacements are reporting better outcomes, overall, than those who’ve undergone ankle fusion – but Sangeorzan cautions that it’s still early. “Ankle replacement is an operation that’s intended to last for 20 years,” he said. “So we want to follow them longer. But in the short term, the ankle replacements are more than holding their own.” Investigators at CLIMB have developed an array of technologies that allow them to model the form and function of human limbs. William Ledoux, Ph.D., has developed a biplane fluoroscope that allows his team to examine, in real time, X-ray images of lower limb bones in motion from two different perspectives. Ledoux, Sangeorzan, and Patrick Aubin, Ph.D., have developed a dynamic robotic gait simulator, a machine that examines the movement of feet – either prosthetic models or donated cadaverous feet – through every conceivable angle and rotation, in a series of studies
www.defensemedianetwork.com
that can help inform the development of new interventions: orthotics, prosthetics, or surgeries. “The advantage to using a prosthetic foot or a cadaver is that you can deploy sensors that are much more invasive than you could on a living subject,” said Aubin. “Maybe you’re interested in the movement of the joint, or in measuring pressure loading. You can actually place a sensor inside that joint and measure it.” Cadaverous feet, not surprisingly, involve a number of limitations for researchers. The amount and variety of studies Aubin and his colleagues will be able to conduct on the simulator are set to increase significantly, as they implement one of the newest pieces of equipment: a 3-D printer capable of producing models of all the different tissues of the foot – skin, bone, tendon, fat, and others – in a single build. CLIMB investigators can scan the feet of people with toe arthritis, for example, and program that scan into the 3-D printer. “We usually get a replica of the foot that’s pretty good,” he said. “It’s soft and squishy where it needs to be, like a regular foot, and has bones and joints in the other places. And then we can use those 3-D printed feet to carry out our experiments. So if we’re interested in comparing different surgeries, we can print the same foot twice.” Aubin emphasized that he sees developments such as the 3-D-printed foot as means of researching mobilityrelated diseases and interventions, not ends. He likens the 3-D-printed foot to a crash-test dummy. “We’re not proposing that patients with foot problems should be going to their doctors and getting scans and 3-D printouts of their feet,” he said. “We’re building a platform to help answer some of these clinical questions.” BONE AND METAL: A NEW ERA FOR PROSTHESES
In Salt Lake City, at the Bone and Joint Research Lab (BJRL) in the George E. Wahlen VA Medical Center, a team led by principal investigator Sarina Sinclair, Ph.D., has been working on a platform of its own – and over the last two years, a team of surgeons led by Drs. Erik Kubiak and Jayant Agarwal have been attempting to prove its worth in collaboration with DJO Surgical, located in Austin, Texas. The name for the project – the percutaneous osseointegrated prosthesis (POP) implant – is a mouthful, but the concept is simple: It’s a metal stem and post, attached directly to the long bone of the leg, that protrudes through the skin and provides a point of attachment for a prosthetic leg. Anyone who wears a traditional stump-and-socket prosthetic will understand how different the design is. “The current socket systems,” said Sinclair, “are like a hard shell worn on the outside of the skin. And there are a number of complications associated with those. Even the most highly functioning patient will tell you it doesn’t fit well. It’s constraining. They can’t wear it all day. It can be very uncomfortable. They’re constantly having to adjust it. The closest thing 43
JOIN AMSUS exists to advance federal medicine. Modern advances IN federal medicine that HAVE resulted in the finest & healthiest military forces in history are not accidental. They are shaped through the associations & research publications supported by
AMSUS’ continued existence depends on membership. Join AMSUS so we can continue to support you & advance federal medicine.
amsus.org/membership
DATE SAVE THE
126th Annual
Meeting
28 Nov - 1 Dec 2017 | National Harbor, MD amsusmeetings.org | #AMSUS2017
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ U.S. Army privates negotiate the “Victory Tower” at Fort Jackson, South Carolina. Victory Tower is a military obstacle course designed to
U.S. ARMY PHOTO BY STAFF SGT. TEDDY WADE
build confidence in new Army recruits. According to the War Related Illness and Injury Study Center, basic training installations average six to 12 injuries per month for every 100 recruits.
I can compare it to is having to adjust your socks and shoes every hour or so. There’s constantly something you’re dealing with when you’re wearing a socket.” The POP system Sinclair and colleagues are investigating involves two parts: The stem, or the “endoprosthetic” part of the implant attached directly to the bone, is made of a biocompatible porous metal, specially made for orthopedic implants, that is designed to allow for the ingrowth of bone tissue and blood vessel formation. The stem is designed to become a part of the patient’s body. The post – the “exo-prosthetic” bridge to the outside world – attaches to the stem, and the artificial leg is attached to this post. “It can take about five seconds to click the leg on and off,” Sinclair said. After years of development and testing in animal models at the Salt Lake City BJRL, under the direction of VA scientist Roy Bloebaum, Ph.D., an FDA-approved early feasibility study with human subjects – the first of its kind in the United States – kicked off in December 2015, as the first two of what would become 10 total veteran participants underwent surgery to have the stem attached. The 10 participants have several things in common: Their legs were amputated above the knee (the POP implant for the trial is specifically for attachment to the femur). Each of their amputations was performed after trauma to the leg, not as a consequence of infection, vascular disease, or diabetic complications.
www.defensemedianetwork.com
The team allows four to six weeks, Sinclair said, before the post is attached. “And about 24 hours later we attach their leg to their post.” The first subjects in the POP pilot were up and walking in February 2016, and by the end of April 2017, all 10 veteran participants had been fitted and were moving around on their prostheses. “All of our patients to date have returned to independent walking within four to six weeks,” said Sinclair. Sinclair said that researchers at the Salt Lake City VA and the University of Utah are working on POP applications for other anatomical sites: “We’re currently designing a platform for the upper limb,” she said, “and we’re interested in developing one for below the knee.” Sinclair foresees a day when a POP platform could become even more seamlessly a part of the human body, connected to something like the neuroprosthetic technology being developed at the Louis Stokes Cleveland VA Medical Center and Case Western Reserve University: an artificial leg that can be clicked directly onto the POP, and plugged directly into, or perhaps even wirelessly connected to, the wearer’s motor cortex. This day – when people with limb-loss or mobility problems could potentially move as effortlessly and painlessly through their days as everyone else in the world – may be closer than most people imagine, thanks to the work of VA researchers. 45
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
HOSPITALISTS
n THERE HAS BEEN A GRADUAL CHANGE in medical care underway at America’s hospitals – and especially the Department of Veterans Affairs (VA) – since the turn of the century. It’s called “hospital medicine”: a discipline in which physicians, called “hospitalists,” are full time on staff, organized around a site of care (the hospital), rather than an organ (such as cardiology), a disease (i.e., oncology), or a patient’s age (pediatrics, geriatrics). Hospitalists have no private practice and only see acutecare patients while they are hospitalized. When working at teaching hospitals, they also are responsible for teaching, oversight of residents, and research. At both teaching and non-teaching hospitals, they are heavily involved in executive leadership involving the delivery of hospital-based care. 46
“Hospitalist is a relatively young specialty. It really started about 15 years ago, maybe a few as long as 20 years ago. The care given by hospitalists is often better and means patients are discharged in better shape and earlier than otherwise,” according to Laurence J. Meyer, M.D., Ph.D., national director of Genomic Medicine and chief of Specialty Care Services for the VA. “It’s very common for hospitalists to be a core of the teaching service for medical students and residents, usually internal medicine, or others rotating through as part of their specialty programs. They often direct the entire residency program in internal medicine – that’s more common than not. Research is a core foundation of the VA – and we really need to look at our patterns of care. Because of our national
www.defensemedianetwork.com
SAN FRANCISCO VA HEALTH CARE SYSTEM PHOTO
By J.R. Wilson
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
scope and high volume, we are well positioned to do that and bring our hospitalists into that.” Dr. Kathryn Fletcher, chair of the VA’s Hospital Medicine Field Advisory Committee, agreed: “A hospitalist in the VA isn’t all that different from hospitalists elsewhere. We take care of hospitalized patients, mostly with medical problems. Our work really revolves around admitting those patients to the hospital, diagnosing and treating them, then transiting them back home. In general, hospitalists also tend to be pretty involved in committee work at the VA hospitals where they work, such as utilization and management, bed flow, things that help the hospital function more efficiently and safely. “While the education mission is not a requirement for hospitalists, what we’re seeing around the country is a lot of hospitalists are stepping into major leadership roles in education in addition to just supervising residents in our clinical work. At VA facilities where there is a teaching service, we have relationships similar to what we have with nurses because we have more contact hours. From a supervisory standpoint, I think that is a very good situation for the team.” The VA currently operates 170 medical centers nationwide, of which 140 are teaching hospitals. The 30 smallest centers usually do not have graduate medical education (GME) physician resident programs and would not meet the Association of American Medical Colleges definition of a teaching hospital. However, due to the Veterans’ Access, Choice, and Accountability Act GME expansion, most small VA medical centers are on their way to having GME programs in the coming years. While hospitalists at both generally devote their time to caring for general medical patients, those at smaller facilities – where a specialist may not always be available in house – may be called upon to care for all medical patients, including those with heart problems, diabetes, or pneumonia. “In those with academic affiliations, hospitalists are used to supervise residents taking care of hospitalized patients and serve as an outlet valve for busy times in the hospital, taking care of patients the residents don’t have time to see. That allows for fluctuations in the number of patients being taken care of,” she explained. “For VAs that don’t have residents, the hospitalists will be the primary way patients are cared for in the hospital. So as the VA expands its use of hospitalists, we’re seeing [the use of hospitalists in] under-covered services expanding. “Where residents were supervised by people who were not hospitalists, more and more are now using hospitalists as part
■■ OPPOSITE: A medical team at the San Francisco VA Health Care
System. Although still a relatively small percentage of physicians working within the Department of Veterans Affairs system, the use of hospitalists by the V A is extensive and growing.
www.defensemedianetwork.com
of a movement to pull specialists away from supervising residents in the care of acute medical patients. Another realm where hospital medicine is increasing in the VA is looking for more people who are dedicated to caring for patients at night – we call them nocturnists. Hiring staff physicians to do that is less expensive than hiring people as sort of moonlighters, so we’re finding more and more hospitalists doing that.”
■■ “Hospital medicine is really a clinical specialty, but doesn’t require special training beyond your regular residency. It can include research and education, depending on where you practice and your job definition. I have colleagues who don’t teach or do research, but they are still hospitalists. There are others, including myself, who use VA funding to do research applicable to the in-patient setting.”
Overall, Fletcher and Meyer estimate at least 70 percent of VA hospital patients are treated by hospitalists. Hospital medicine is very facility dependent, which creates a lot of leeway to develop as local needs dictate. While there is a VA list server hospitalists use to communicate with each other and share information, there is no national directive on how to use hospitalists within the VA. There is no national program director, as emergency medicine and some others have, but Fletcher said there has been some talk about it as hospitalists become a bigger group. “We are staff doctors, but we don’t do outpatient work, so a technical definition would be someone who does the majority of their clinical work in facility. We’re not primary care – we only take care of people who are sick and hospitalized. So the primary difference between us and other general internal medicine doctors is we don’t do outpatient care,” she said. “Hospital medicine is really a clinical specialty, but doesn’t require special training beyond your regular residency. It can include research and education, depending on where you practice and your job definition. I have colleagues who don’t teach or do research, but they are still hospitalists. There are 47
LET NOTHING STOP YOU ™
For Pain
For Anxiety
For Depression
For Insomnia
Fast, Safe and Proven Effective Relief Without Drugs Alpha-Stim provides fast, safe and proven effective relief without drugs. It can be used alone, along with other therapies or as an adjunct to medication (without the risk of drug interactions). There are no serious adverse effects, no risk of addiction, and more than 100 research studies over 35 years that prove the effectiveness of this low level electrical prescription brain therapy. “In the wartime theaters of both Iraq and Afghanistan… Alpha-Stim CES was the single most effective form of treatment our Combat Stress Control Teams were able to provide for Service Members in our care.” COL (Ret) Kathy T. Platoni, PsyD Co-editor, Healing War Trauma: A Handbook of Creative Approaches (2013)
HELP IS HERE.
Call 1-800-FOR-PAIN or 940-328-0788 for government/veteran pricing or visit www.Alpha-Stim.com to learn more and see clinical data. Alpha-Stim and the Alpha-Stim logo are registered trademarks, and LET NOTHING STOP YOU is a trademark of Electromedical Products International, Inc. © 2017 Electromedical Products International, Inc. All rights reserved. Read a full disclosure of the minor and self-limiting risks here: alpha-stim.com/risk.
The College of Allied Health and Nursing at Minnesota State University, Mankato promotes health and wellness through real-world experiences in state-of-the-art facilities. We prepare professionals who serve as strong partners in improving the wellbeing of people and families in our communities, our region and our world. Our School of Nursing prepares nurses who understand the importance of family and society in the healthcare setting. We offer bachelor’s, master’s, and doctoral degrees— and a fully online RN Baccalaureate Completion program!
NEW! Fill a critical need in the health-care industry and help people lead healthier lives with an online master’s degree in Wellness Coaching and Disease Prevention!
Learn more at ahn.mnsu.edu! A member of the Minnesota State system and an Affirmative Action/Equal Opportunity University. This document is available in alternative format to individuals with disabilities by calling the College of Allied Health and Nursing at 507-389-6981 (V), 800-627-3529 or 711 (MRS/TTY).
VA PHOTO BY JEFF BOWEN
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
others, including myself, who use VA funding to do research applicable to the in-patient setting.” While still a relatively small percentage of physicians working within the VA system, the use of hospitalists by the VA is extensive and growing. “It’s hard for primary care doctors to continue to have efficient [private] practices if they split their time between their clinics and a hospital. When you’re taking care of patients in the hospital, it takes you away from your clinic and makes access more difficult for your primary care patients. It’s really an efficiency of access issue – the arrival of hospitalists has made it easier to have a vibrant outpatient practice and works out well on many levels,” Fletcher explained. The VA operates the nation’s largest health care system of hospitals, clinics, home- and community-based care, and, increasingly, telemedicine and remote patient-monitoring services. While hospitalists currently are involved only with hospitalized patients – typically not those requiring specialists, such as cardiologists or oncologists – Fletcher said their role may evolve along with advanced medical care delivery technologies and practices now being developed. “Right now, because we are facilitycentric and dedicated to taking care of people in the hospital, we are neither affected by nor affect telemedicine nor home-based primary care. I can imagine applications as these things become more prominent; for example, there are hospitals that have tele-ICUs [tele-intensive care units], with doctors watching monitors and EKGs [electrocardiograms] and using video to look at patients who are not in the hospital, although I don’t know if that is being done by the VA at this time,” she said. “Some VA facilities have a program called ‘hospital at home,’ for patients in the ER who meet certain criteria and may be sent home with nursing support. Is there a role for hospitalists in that? Potentially. Hospitalists being based at a specific facility will continue to be the
www.defensemedianetwork.com
■■ Hospitalists are physicians whose primary professional
focus is the general medical care of hospitalized patients. Their role may include the teaching of medical students, residents, and fellows; research; and involvement in practice guideline, quality assurance, and protocol development.
49
Online Masters Masters of of Science Science Programs Programs Orofacial Pain Medicine and Pain Medicine | Geriatric Dentistry
The Herman Ostrow School of Dentistry of USC offers online master’s programs designed for highly motivated dental professionals who currently have full-time clinical employment in either private practice or academia. Programs involve video lectures, live video conferences regarding patient cases, short visits to the USC campus and the preparation of a research article. For more information: (213) 740-9158 ofpom@usc.edu
http://dentistry.usc.edu/programs/online-programs/
When your dedication to wellness grows...
Offering Master’s and Doctoral Programs for Registered Nurses Specialties offered: • • • •
Certified Nurse-Midwife Family Nurse Practitioner Women’s Health Care NP Psychiatric-Mental Health NP
Complete coursework online with only 1-3 brief visits to campus.
frontier.edu/military
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
majority of the job, but can we participate in more creative treatments for patients outside the hospital who still have hospitalist needs? Yes, but I don’t think it’s happening right now.” Hospitalist is not a specialty on which medical students, interns, and residents focus. As with all medical doctors, after medical school they choose an area of medicine in which to perform as an intern for one year, then two more years as a resident. From there, they can do a fellowship in some specialty or become a primary care doctor or become a hospitalist. There are some hospitalist fellowships that offer more clinical experience, but Fletcher said most are focused on giving the new doctors a better set of research or quality improvement tools. For those choosing the hospitalist route, the vast majority complete their residencies in internal medicine, making them eligible for board certification in hospital medicine, although that is not a requirement. Hospitalists also are not required to be educators or researchers, although the former is becoming a major part of the job at VA hospitals affiliated with medical schools. About 70 percent of all U.S. physicians have rotated through the VA hospital system as either medical students or residents, and hospitalists are considered integral to that part of the mission. That also serves as the VA’s chief recruitment tool; according to Fletcher, the majority of VA hospitalists are recruited straight out of residency (although not necessarily residencies at VA hospitals). How hospitalists are employed will change as the demographics of the veteran population change – including an aging “bubble” of Vietnam era vets (see “Geriatrics” on page 22), more female veterans, and higher incidents of PTSD (post-traumatic stress disorder) and TBI (traumatic brain injury), the latter two both largely from Operation Iraqi Freedom (OIF) and Operation Enduring Freedom-Afghanistan (OEF). “The preponderance of hospitalists in the VA are internal medicine physicians; we deal with a lot of chronic diseases – many in the same person. And we have a higher proportion of patients with PTSD, TBI, and spinal cord injuries. However, you don’t see a lot of the new veterans in a VA hospital setting. They may still be in military hospitals or, if recovered, may not need to still be in a hospital. So our outpatient counterparts are more likely to see Gulf War veterans, while we’re taking care of older World War II, Korea, and Vietnam veterans,” Fletcher said. “It’s fascinating to take care of each generation of veterans in the VA, who do have some things in common, but there are a lot of individual variations, as well. The Vietnam generation has taught us a lot about PTSD care while we’re taking care of their medical problems, in a way the World War II generation did not because many of them never got that diagnosis. As we see more and more Vietnam era veterans hospitalized with medical problems,
www.defensemedianetwork.com
■■ In an age in which the majority of doctors seem to be specialists, it is interesting to note the growth of a new cadre of general internal medicine practitioners with no private practices nor commitments outside the hospitals at which they work.
it gives us the opportunity – and challenge – to care for them in a way that is sensitive to their mental health issues, which will be very helpful when the OEF/OIF generation begins coming in.” Hospitalist may be a term with which most VA – and non-VA – patients are unfamiliar, but, increasingly, the odds are the doctor caring for a hospitalized medical patient either is a hospitalist or, in a teaching hospital, being supervised by one. Given its size and unique patient population, how and where VA hospitalists are used is likely to evolve more quickly – and perhaps in different ways – than for their civilian counterparts. In an age in which the majority of doctors seem to be specialists, it is interesting to note the growth of a new cadre of general internal medicine practitioners with no private practices nor commitments outside the hospitals at which they work. That also applies to their roles as medical researchers, increasing involvement in the supervision of teaching hospital residents and in the operations of their hospitals – both academic and non-teaching. “Hospitalists take our roles as patient safety experts and advocates very seriously, beyond our clinical mission. Even in non-teaching hospitals, hospitalists are very active in working on patient safety issues, root-cause analyses used to understand the reasons for any adverse events that occur. Hospitalists are often the go-to physicians for those sorts of roles, both in the VA and outside,” Fletcher concluded. “Because we are facility based, we feel a special commitment to those facilities and an intimate understanding of the issues there. So we can help leadership understand what solutions are needed and feasible. That’s an important part of our role. And because we spend so much time in the hospitals, we may be more facile at coordination with the nurses, who feel they can come to us because we are around so much and we have good working relationships with them. That helps us better plan what patients need on a day-to-day basis and as they are getting ready to go home.” 51
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
THE U.S. ARMY MEDICAL SERVICE CORPS: 100 Years of Support for Military Medicine
n EVERY YEAR ON JUNE 30, as with most birthday parties, cake is served when officers of the U.S. Army Medical Service Corps (MSC) celebrate the founding of their organization. But an MSC birthday party is different from most: Traditionally, the cake is cut with a sword, a reminder that the officers of the MSC, while performing the most diverse range of duties of any corps within the U.S. Army Medical Department (AMEDD), are soldiers, members of a profession of arms. At MSC birthday celebrations, the cake-cutting sword is usually wielded by both the most senior officer in
52
attendance – a symbol of the honor and respect paid by MSC officers to their most experienced and senior leaders – and the most junior officer, signifying the MSC’s commitment to fostering and developing the talent that will renew the Corps for generations to come. 2017 marks the 100th birthday of the MSC, though its origins can be traced back to the Revolutionary War, when the Continental Army found itself with neither a coordinated medical supply system nor even basic management practices that could relieve the military’s medical professionals
www.defensemedianetwork.com
LIBRARY OF CONGRESS PHOTO
By Craig Collins
U.S. ARMY MEDICAL DEPARTMENT, OFFICE OF MEDICAL HISTORY
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
– physicians, nurses, dentists, and veterinarians – from logistical and administrative duties that hindered patient care. Battle-wound casualty rates were high in the War for Independence, primarily because of bad logistics: The functions of evacuating and treating wounded soldiers were integrated into line commands, whose main focus was winning battles. For decades, the new U.S. Army struggled to integrate administrative and logistical support for its medical professionals, but the Civil War was a grim wake-up call. More than 2,700 Union soldiers were killed or wounded in the first major battle of the war, the First Battle of Bull Run, and many stretcher-bearers fled along with the Army’s panicked retreat, leaving the wounded behind. Some wounded soldiers remained on the battlefield for days. President Abraham Lincoln acted decisively to reverse these early failures, installing William A. Hammond as surgeon general of the Army. Hammond’s reforms included better transport of the wounded from the battlefield – he placed this function under the direct command of a medical corps, with its own drivers and bearers. The new system of combat casualty care and evacuation was designed by Maj. Jonathan Letterman, who borrowed from the principles of “triage” developed by Napoleon’s physician, Baron Dominique-Jean Larrey. At division and corps headquarters, Letterman established mobile field hospitals, connected to each other and to the battlefield by a transport system also innovated by Larrey: horse-drawn “flying ambulances,” manned by early versions of medics and corpsmen. Under Letterman’s system, Union mortality rates dropped significantly in the Army of the Potomac, and Congress adopted it as the official procedure for intake and treatment of battlefield casualties. The Ambulance Corps was created by law for all Union armies through the Ambulance Corps Act of 1864. The Civil War’s new casualty and evacuation doctrine, which continues to this day, also added specialties to the Army’s medical department that refined its expertise: medical logistics, pharmacy, administration, recordkeeping, and statistical reporting grew in importance. The addition of dedicated, trained, and qualified medical support personnel to help coordinate care and handle the transport of the sick and wounded, however, proved insufficient during the nation’s first expeditionary war: the SpanishAmerican War of 1898. While a swift and decisive American victory, the war resulted in 932 service members dying from war wounds, and more than 5,400 dying from diseases, such as malaria and yellow fever, in the tropical jungles of Cuba and the Philippines. The challenges faced by these support personnel overseas, in unfamiliar environments, prompted a further round of study and reform. When Maj. Gen. William Gorgas became Army surgeon general in 1914, he examined the ways in which
www.defensemedianetwork.com
■■ OPPOSITE: An American Zouave ambulance crew demonstrating removal of wounded soldiers from the field during the American Civil War. ABOVE: Medical Director of the Army of the Potomac Maj. Jonathan Letterman (second from left) with his staff. He developed a system of combat casualty care that became known as the “Letterman System.”
the French and British militaries had relieved military physicians from administrative and other non-medical burdens. Gorgas began to assemble a “Sanitary Corps” of administrative and scientific specialists to aid and support the U.S. military medical team. By the time the United States had entered World War I, the War Department had issued orders for this corps to consist of up to 1,000 officers and 3,905 enlisted personnel, representing specialties from accounting to nutrition. The corps rapidly expanded to include 3,000 officers during the war. Gorgas’ Sanitary Corps, in its structure and function, is the clearest predecessor of today’s MSC. In his 1997 history of the MSC, Col. Richard Ginn (Ret.) wrote: “Indeed, today’s MSC is almost a mirror image of its precursor.” For this reason, the date the Sanitary Corps was established – June 30, 1917 – is considered to be the MSC’s official date of birth. Meanwhile, the automobile had helped to revolutionize the evacuation and transport of wounded combatants. In 1917, the same year the Sanitary Corps was formed, the Army created the Ambulance Service. In the trench warfare of World War I, U.S. medical teams adopted a system similar to that already employed by the British, who staged Casualty Clearing Stations (CCSs) several miles behind the front lines: Non-physicians treated casualties in the trenches and prepared them for transport to front-line first-aid stations, which fed field hospitals staffed by surgeons, anesthetists, and nurses. Both the Sanitary Corps and the Ambulance Corps were formed as temporary wartime elements, and both were demobilized after the armistice. It didn’t take long for the
53
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
Medical Department to feel the loss of this expertise, however, and leaders of the Army’s medical establishment began to lobby for a permanent corps for administrative and scientific specialty officers to support Army medicine. The Medical Administrative Corps (MAC) was established in June 1920. Some functions of the Sanitary Corps were absorbed by the new MAC, while others were placed in the Army’s Reserve component.
logistical issues of World War II varied as widely as its theaters of operation, from the cities of Europe to the deserts of Africa to the jungles of the Pacific tropics. The growing ranks of the MAC freed physicians for patient care and occupied an expanding diversity of positions. By war’s end, the MAC comprised 22,000 officers, whose work had proved essential to the Allied victory: Medical logistics and administrative officers
helped plan and execute medical supply missions that were carried out on a global industrial scale. Scientific officers of the MAC – sanitary engineers, bacteriologists, biochemists, serologists, parasitologists, nutritionists, and medical photographers, among others – helped to develop the military’s preventive medicine program and proved crucial to the battle against diseases, particularly malaria, among warfighters. Another medical support function to grow in significance during World War II was the role of pharmacist. In July 1943, President Franklin Roosevelt signed legislation establishing the Pharmacy Corps as a component of the regular Army. The United States emerged from World War II a world power and the Army Medical Department with an expanded suite of responsibilities. There was no longer any question that the department needed a permanent corps of administrative and scientific specialty officers. On the recommendation of Army Surgeon General Maj. Gen. Norman T. Kirk, Congress agreed to consolidate the medical support expertise of the Sanitary Corps, Medical Administrative Corps, and Pharmacy Corps into a single Medical Service Corps. The Army MSC was established by law on Aug. 4, 1947, and consisted of four operational sections:
THE MODERN MSC
U.S. ARMY MEDICAL DEPARTMENT, OFFICE OF MEDICAL HISTORY IMAGES
The MAC survived the Great Depression with fewer than 100 officers, but World War II soon demanded much from its experts. The medical and
■■ TOP: A class of Medical Service Corps
officers learns how to properly strap a patient and litter on an H-13 helicopter, October 1954. RIGHT: Scientific officers of the Medical Administrative Corps, one of the forerunners to the Medical Service Corps, helped to develop the military’s preventive medicine program, and proved crucial to the battle against diseases, particularly malaria, among service members.
54
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Army Maj. Lance Olsen, left, and Army Sgt. Frisco Cleary sort out medications in the pharmacy tent during Beyond the Horizon 2016 in San
ARMY PHOTO BY SPC. KELSON BROOKS
Pedro, Guatemala, May 16, 2016. Olsen and Cleary are assigned to the 396th Combat Support Hospital Company. On Aug. 4, 1947, the Army Medical Service Corps was established and consisted of four operational areas: pharmacy, supply, and administration; medical allied sciences; sanitary engineering; and optometry. Today, pharmacists may be assigned to an Army medical center, community hospital, troop medical clinic, or in a field environment located in the United States or overseas.
pharmacy, supply, and administration; medical allied sciences; sanitary engineering; and optometry. The United States’ standing as the leading world power bestowed an expanding set of global responsibilities on the Army Medical Department, including the support of peacetime medical care for active and retired service members and a growing research and development effort. The roles demanded of administrative and scientific officers in the MSC continued to grow in scope and sophistication. The Korean conflict would further evolve the expertise within the MSC. The most obvious advancement in the field was the development of an aeromedical evacuation (aerovac) doctrine. MSC aviators were assigned to the first helicopter evacuation detachment in Korea. The successes of MSC’s helicopter pilots led to the development of the Army’s firstgeneral utility helicopter, the UH-1 Iroquois, or “Huey.” Aerovac became routine in the Vietnam conflict; in 1969, the peak year for air evacuation, 200,000 casualties were transported by helicopter. Behavioral intervention and other social support became increasingly important in the latter 20th century, particularly during and after the Vietnam and Gulf wars, when many service members were found to be suffering from post-traumatic
www.defensemedianetwork.com
stress. The MSC’s expertise has expanded to include clinical and counseling psychologists, and social workers – degreed and licensed professionals capable of helping service members make personal and psychological adjustments both during and after service. Like the rest of the U.S. military, which began its first round of Base Realignment and Closure in 1988, the MSC has undergone several reorganization and streamlining initiatives in the 1990s and early 2000s, but its core mission remains the same. Today’s MSC provides administrative, clinical, scientific, planning, programming, and leadership expertise for every Army Medical Department effort. In wartime, its officers maintain the Army’s medical capability through its field commands. Its 9,500 officers provide expertise in 26 specialty areas. On June 30, 2017, when they gather at AMEDD Headquarters, Fort Sam Houston, Texas, many of these professionals – the health services administrators, biochemists, entomologists, podiatrists, audiologists, social workers, helicopter pilots, and many others – will celebrate one hundred years of service in support of U.S. military medicine. Varied as they are, the officers of the U.S. Army Medical Service Corps remain united, more capable than ever of leading the Medical Department’s crucial role in national defense.
55
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA Research: THE OBESITY EPIDEMIC By Craig Collins n AMERICANS HAVE HEARD PLENTY ABOUT the “obesity epidemic” over the past decade or so, and in that time the problem has worsened. In fact, the word “epidemic” seems hardly severe enough to describe the public health crisis confronting U.S. adults, and particularly veterans. In 2015, the Department of Veterans Affairs (VA) estimated that 78 percent of veterans – nearly four out of five – was either overweight or obese. Among these, nearly 165,000 veterans who received health care from the VA had a body mass index of more than 40, indicating a serious condition known as morbid obesity. Obesity is a risk factor for diabetes (about 25 percent of veterans are diabetic), heart disease, stroke, and some types of cancer. It’s also a much more complex health issue to address than many diseases, because it involves a combination of causes and contributing factors including genetics, behavior, and social and environmental factors. VA researchers and clinicians recognize the seriousness of the obesity epidemic among veterans, and are at work on numerous interventions and studies aimed at helping veterans achieve and maintain a healthy weight. Some VA research on obesity examines the basic biological processes of weight gain and weight loss. In January 2016, for example, researchers at the VA San Diego Healthcare System and the University of California-San Diego found that as fat cells develop, they change the types of nutrients they metabolize (process) to produce fat and energy. The findings may lead the way toward a better understanding of how fat cell metabolism may differ among patients with obesity and/or diabetes – and toward new treatments for these conditions. RISKS AND BARRIERS TO TREATMENT
Cellular biology is only one factor, however, in determining a person’s risk for overweight or obesity, and VA investigators are busy developing a clearer picture of those risks among veterans – for example, a service member’s risk for weight gain increases as soon as he or she separates from the military. In a 2015 study using data from the Department of Defense’s Millennium Cohort Study, a team led by Alyson Littman, M.P.H., Ph.D., found that discharged service members were 56
significantly less physically active than those who were not, with greater declines among those who had been discharged more recently (two years ago or earlier); among those who served longer (14 to 25 years); and those who had deployed with combat exposure. Littman, an investigator with the VA’s Seattle Epidemiologic Research and Information Center (ERIC) and associate professor of epidemiology at the University of Washington, has also been involved in a pair of recent studies examining weight gain among veterans with lower-limb loss. The studies found, perhaps unsurprisingly, a greater tendency for weight gain among amputees, with the greatest weight gain occurring among those whose legs had been amputated proximally to the knee joint. These studies launched further investigations, beginning with surveys of veterans with limb loss in the Northwest region to discover likely barriers to physical activity for them. The most commonly related barriers, Littman said, were resource related – “lacking resources to obtain adapted prosthesis or sports prosthesis or wheelchair, join a gym, get to activities or events, so transportation.” Physical pain – associated with an ill-fitting prosthesis, back or joint pain, or phantom limb pain – was a close second. In follow-up interviews, Littman and colleagues took a deeper look at the differences between active and less active veterans who had comparable limb losses. They discovered several key factors: Veterans who viewed exercise as a part of their routine, an activity that gave each day an anchor and a sense of purpose, were more active. “Another major facilitator for some – and a barrier for others – was social support,” Littman said. “We found that veterans really appreciated friends, family, and also clinicians, such as physical therapists, who had very high expectations for them and provided some accountability, who saw what their potential was and pushed them to get there.” The most prominent and comprehensive of the VA’s weightloss programs is MOVE! An evidence-based weight management and health promotion program, MOVE! is available to veterans throughout the Veterans Health Administration (VHA): Veterans who receive care in VHA facilities are screened for obesity, referred to weight management services,
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Gunnery Sgt. Rhonda Jackson, assistant operations chief for Marine Corps Air Facility Quantico, Virginia, does an exercise called “shakers”
PHOTO BY LANCE CPL. SHANDRA DYESS
during a maximum group fitness class. The VA’s weight management and health promotion program, MOVE!, encourages healthy eating and physical activity and is customizable based on a veteran’s needs.
and enrolled in a MOVE! program that encourages healthy eating and physical activity while meeting their individual needs. Because these needs vary widely, MOVE! is designed to be customized. Some programs last four weeks; some last four months. Some are delivered in group or in-person coaching sessions, and some deliver coaching through oneon-one telephone calls, in-home messaging services, or a mobile app, MOVE! Coach, that allows veterans to manage their weight on their own. Veteran engagement in the MOVE! program also varies widely throughout VHA facilities, and researchers are discovering additional vulnerabilities to obesity among those
www.defensemedianetwork.com
who use the program. Katherine Hoerster, M.P.H., Ph.D., an investigator at the VA Center of Innovation for VeteranCentered and Value-Driven Care in Seattle and assistant professor at the University of Washington’s Department of Psychiatry and Behavioral Sciences, was among a group of researchers who recently reported poorer outcomes among veterans with post-traumatic stress disorder (PTSD) who were enrolled in VA’s national MOVE! program. “That was despite equivalent or in some cases greater participation in MOVE!,” said Hoerster. “It wasn’t attributed to lower engagement in the program.” Additional research by Hoerster and others has shown that psychiatric conditions 57
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
such as PTSD and depression are barriers to physical activity and healthy eating – and that PTSD involves its own idiosyncratic barriers. “For example,” she said, “safety-related concerns are a really prominent symptom of PTSD. And it’s shown in the literature that those fears about safety get in the way of being active.”
WILLIAM SALLETTE, TRIPLER ARMY MEDICAL CENTER
STUDYING TREATMENTS AND INTERVENTIONS
Hoerster has piloted a variant of the program, MOVE!+UP, designed specifically for veterans with PTSD. In addition to educational components common to most weight-loss programs, such as gauging portion sizes and behavior tracking, the program teaches basic anxiety management skills. There’s also an emphasis on social engagement in group settings, Hoerster said, to counter the tendency of people with PTSD to become socially isolated. The program is led by a peer support counselor who is in recovery from PTSD, and the entire MOVE!+UP intervention is implemented over a period of four months: weekly group meetings that include a group walk in the community, followed up by telephone coaching sessions with the counselor. Hoerster is currently studying the effectiveness of the MOVE!+UP model. In Seattle, after gathering data and interviewing veterans, Littman has piloted a MOVE! variant aimed at meeting the specific needs of veterans with lower-limb loss, and is currently working on the problem of how to scale such a program up to include a larger number of participants. Another investigator to evaluate the effectiveness of MOVE! and other weight-loss interventions among veterans is Laura Damschroder, M.P.H., M.S., with the VA Ann Arbor Center for Clinical Management Research. Her studies of the MOVE! program have generally focused on comparing a conventional program to both group and telephone variants involving a team of multidisciplinary coaches. Figuring out what works and what doesn’t is challenging, said Damschroder, because of the variables involved. “Our results include a mix of people,” she said, “some of whom had 16 sessions … and also some who only showed up to the orientation session. Most of the people who enroll in these programs, on average, are on a weight-gain trajectory. So even if we’re just getting that trajectory to flatten out, that’s an achievement.” Generally, Damschroder found supportive, interactive groups and consistent attendance to be positively correlated with good outcomes – data measurements that included height, weight, and waist measurements; blood pressure; demographics; cholesterol and glucose; comorbidities; and self-reported satisfaction. “The telephone lifestyle coaching program seemed to be a very successful program,” she said. “Like the in-person program, it had the same coach over time – and a coach who was not just didactic, but who worked with veterans on their own goals. So being patient centric is very important.” Obesity and related disorders were one of several critical areas of interest recently targeted by the VA’s Office of Health
www.defensemedianetwork.com
■■ Betchie Curran, cardiology health technician, Tripler Army
Medical Center, Hawaii, discusses the day’s treatment in the cardiac rehabilitation program with a cardiac rehabilitation patient. The program is different for every patient, but it focuses on strengthening, nutrition, and fitness. Obesity puts people at a higher risk for heart disease, stroke, diabetes, and some types of cancer.
Services Research and Development (HSR&D), through its CREATE (Collaborative Research to Enhance and Advance Transformation and Excellence) initiative. CREATEs are groups of related studies, each aimed at discovering more about a particular health services issue. Damschroder is one of several investigators evaluating prevention strategies in the Transforming Prevention into Action CREATE, and the program she and her colleagues are designing, Stay Strong, is an intervention aimed at encouraging physical activity among Afghanistan and Iraq veterans. The basic plan for the Stay Strong intervention, said Damschroder, is to give each participant a Fitbit® activity tracker and a Bluetooth®-enabled scale, to help correlate activity levels and data to weight loss or gain. Damschroder’s group will compare outcomes between two groups: those 59
DNP MSN BSN Completion
Receive Your FREE Copy of the Upcoming Edition of
Ferris State University Online Nursing Degrees
• Flexible Programming •G old level rating for being Veteran friendly 2015 and 2016 •9 5% courses taught by full time expert faculty engaged in research and practice • Student-centered Curriculum Please visit www.ferris.edu/HTMLS/colleges/alliedhe/ Nursing/homepage.htm for more information
SIGN UP HERE vamilmedoutlook.com/#subscribe
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
simply given the Fitbit tracker and the scale, and those who, in addition, receive personalized goals and messages – both instructional and inspirational – via the Fitbit app. Damschroder plans to begin recruiting participants in summer 2017. DIET AND SURGERY
A key factor in obesity and related disease, of course, is what people eat, and diet has been a focus of several VA-funded studies. A team led by William Yancy, M.D., M.P.H., a research scientist and physician at the Durham VA Medical Center and associate professor of medicine at Duke University, recently discovered that obese patients who are allowed to choose their own diet plans lost less weight than those who were assigned a diet to follow. “Providing a choice of diets to follow,” Yancy concluded, “does not enhance and may actually hinder weight loss.” VA investigators are discovering that a bit of direction and encouragement also can help sustain weight loss – an even more difficult task, for many, than initiating weight loss. In February 2017, a team led by Corrine Voils, Ph.D., a research scientist at the William S. Middleton Memorial Veterans Hospital and visiting professor at the University of Wisconsin School of Medicine and Public Health, reported on their study of a weight-loss maintenance program among VA primary care patients who, overall, lost an average of 16 pounds as part of a structured 16-week weight-loss program. One group was left alone, while the other received regular coaching from dieticians in biweekly face-to-face meetings that transitioned to phone calls every two months. After a total of 42 weeks, the patients in Voils’ study who received coaching were left alone for an additional 14 weeks – and then all participants, those who had received the coaching and those who hadn’t, were weighed again. Those who’d received sustained coaching had regained an average of 1.5 pounds – but those who hadn’t been coached gained back an average of 5 pounds. Voils is launching a VA-funded pilot to adapt her coaching intervention, this time to promote weight-loss maintenance among patients following bariatric surgery – a procedure that’s been proven one of the most effective interventions for reducing weight. A body with longstanding obesity typically defends itself against weight loss by reducing the metabolic rate – but this metabolic effect isn’t seen after bariatric surgery, which permanently alters the digestive tract. It’s long been known that bariatric surgery can lead to dramatic weight loss, but – until recently – not much was known about how surgery patients fared over the longer term. In August 2016, a team led by Matt Maciejewski, Ph.D., a research scientist at the Durham VA Medical
www.defensemedianetwork.com
Center and professor at Duke University School of Medicine, reported on outcomes for patients who had undergone bariatric surgery a decade earlier. In the first part of the study, Maciejewski’s team compared weight loss among 1,800 veteran patients who had undergone a gastric bypass – the most common bariatric procedure, in which the stomach is reduced in size and attached directly to the lower small intestine – to 5,300 obese veterans who’d had no weight-loss surgery or formal weight-loss treatment. After a year, bypass patients had lost 31 percent of their body weight, compared to 1 percent for the non-surgical group. A decade later, the researchers compared the weight information they had on 564 of the surgical patients. All but 19 of them had kept their weight off. Overall, the surgical group’s weight loss was 21 percent higher than the non-surgical group. A second phase of the study compared different surgical outcomes, and found that gastric bypass was far more effective, in both the short and long terms, than two other procedures: gastric banding and sleeve gastrectomy. Yancy, who was part of Maciejewski’s team, described the investigation as “a pretty impactful study, because it’s one of the first times we’ve had really long-term data on weight effects of bariatric surgery – and it’s one of the better studies in terms of having complete data, because the patients were within the VA system, and so we were able to follow them and get complete outcome data.” Maciejewski is now putting together a study of this same cohort, funded by the National Institutes of Health, that will look at long-term mental health outcomes. “There’s been non-VA work that has shown that alcohol misuse, opioid misuse, and depression are impacted by bariatric surgery,” said Maciejewski. “But there haven’t been VA studies to examine that in veterans yet. So we’re beginning this study to fill those gaps.” Expanding the focus of obesity research to include mental health conditions associated with weight-loss surgery is an acknowledgement that obesity is a complex and multifaceted public health problem, requiring variety and flexibility among those who work to help veterans maintain a healthy weight and lifestyle. To Hoerster, this realization is one of the most encouraging things about working in the field today: VA’s prevention programs increasingly adopt a whole-health perspective that doesn’t focus merely on weight. “A weight-loss program is key, of course,” Hoerster said, “but getting veterans to really ponder how to live in a way that improves their overall health is a really important movement we see happening. I’m really excited to continue to do that work, especially because, as we’ve continued to refine our intervention, a large part of what has shaped those changes has been the veteran voice and perspective.” 61
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
INTERVIEW
KAYLA M. WILLIAMS Director of the Center for Women Veterans By Chuck Oldham
What functions does the Center for Women Veterans perform? [The] CWV was established by law in 1994; our congressionally mandated functions include advising the secretary [of the Department of Veterans Affairs] and other senior leaders on policies, programs, and legislation affecting women veterans; conducting outreach to and promoting the use of VA benefits by women veterans; disseminating information and serving as a resource center; publicizing the results of 62
■■ Kayla M. Williams, director of the Center for Women Veterans.
significant medical research; and supporting the independent VA Advisory Committee on Women Veterans. Our mission is to monitor and coordinate VA’s administration of health care and benefits services, and programs for women veterans; serve as an advocate for a cultural transformation [both within VA and in the general public] in recognizing the service and contributions of women veterans and women in the military; and raise awareness of the responsibility to treat women veterans with dignity and respect.
www.defensemedianetwork.com
PHOTO COURTESY KAYLA WILLIAMS
n KAYLA M. WILLIAMS is the director of the Center for Women Veterans at the Department of Veterans Affairs (VA), where she is responsible for monitoring and coordinating VA’s administration of health care, benefits, and programs for women veterans; serving as an advocate for increased recognition of the service and contributions of women veterans and service members; and raising awareness of the responsibility to treat women veterans with dignity and respect. Prior to coming to VA, Williams spent eight years at the RAND Corporation and five years enlisted in the U.S. Army, including a yearlong Operation Iraqi Freedom deployment with the 101st Airborne Division. Williams earned a B.A. in English literature from Bowling Green State University and an M.A. in international relations from American University. She is a former member of VA Advisory Committee on Women Veterans, a 2013 White House Woman Veteran Champion of Change, and a 2015 Lincoln Award recipient. Williams is the author of Love My Rifle More Than You: Young and Female in the U.S. Army and Plenty of Time When We Get Home: Love and Recovery in the Aftermath of War, both published by W.W. Norton. Veterans Affairs & Military Medicine Outlook: Why is a Center for Women Veterans (CWV) important to veterans and to the nation? Kayla M. Williams: The Center for Women Veterans and our sister office, the Center for Minority Veterans, are important in ensuring the unique or disproportionate needs of minority groups are met. All those who have served our nation honorably deserve the same access to care and benefits.
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ Celebrating the women veterans whose courage and sacrifice help demonstrate equality on Women’s Equality Day, Aug. 26, 2016. The
PHOTO BY LANCE CPL. ALEJANDRO SIERRAS
Department of Veterans Affairs estimates there are approximately 2 million living women veterans today.
As a combat veteran, what elements of your service experience did you find to be in contrast to the public’s perception of women in combat? I took part in the initial invasion of Iraq in 2003 as part of the 101st Airborne Division (Air Assault). When we came home in 2004, it became clear that the public had no understanding of how women were serving overseas: Some people asked if I was even allowed to carry a gun as a woman, while others asked if I were in the infantry [which, at that time, was still barred]. Today, public awareness has increased significantly – most Americans today are likely aware that since 9/11, women troops have been prisoners of war and have been injured and killed in combat. What do you think the public most needs to learn about women service members and veterans? How strong and resilient we are; what tremendous assets we are to our communities. Compared to our male counterparts,
www.defensemedianetwork.com
women veterans are more likely to have college degrees and to work in management or professional occupations; we have significantly higher average household incomes than women who have never served. We return to our communities with leadership and technical skills and a high propensity to serve in new ways through volunteering and other forms of civic engagement. Unfortunately, media coverage often focuses exclusively on the challenges we face, such as higher rates of sexual trauma, homelessness, and suicide than our civilian peers. While those are very real issues, they do not represent the totality of our experience. In your book Plenty of Time When We Get Home, you write about women veterans and post-traumatic stress disorder, and mention that many seem to cope with their experiences in combat differently than male veterans. What are some of the ways that women service members and veterans differ in how they deal with the wounds of war? 63
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ U.S. Army Spc. Amanda Vasquez, with Headquarters and Headquarters Troop, 3rd Heavy Brigade Combat Team, 1st Cavalry Division,
renders a salute during the presentation of the colors at “Fight Night for Heroes,” the first-ever mixed martial arts fights held at Forward Operating Base Marez, Iraq, in 2009. Today, women are one of the fastest-growing subgroups among the veteran population, according to the CWV.
When you wrote your books, some military occupational specialties were not yet open to females. What are your thoughts on how that has changed? 64
The final barriers to women’s military service have finally fallen, and we now have female infantrymen and Ranger School graduates. It’s been incredibly rewarding to see the honorable service of millions of women validated by this progress. How have your personal experiences, and the experiences of female soldiers you served with, affected how you perceive the issues and needs of women veterans and how you perform your job? My personal experiences, both in the military and as a veteran, have given me a great deal of passion for the VA mission to serve those “who shall have borne the battle” and their families and survivors. At the same time, the eight and a half years I spent at the RAND Corporation doing research and analysis grounds me in the need to ensure that programs and services are evidence based and effective. Both my life and the data show that VA can be an important part of a
www.defensemedianetwork.com
PHOTO BY SENIOR AIRMAN KAMAILE CHAN
Anecdotally, I’ve heard that women are more likely to have talked about their experiences – a documentary filmmaker once told me that many of the male veterans she’d interviewed had shown tremendous emotion and told her they had never told anyone what they’d been through before, while the women had stronger social ties and had obviously talked about their experiences with one another. Research shows that women in general use both health care and mental health care at higher rates, so we seem more likely to seek help. Men and women veterans should know that VA can help, including through counseling at vet centers, which are predominantly staffed by other veterans. In fact, 25 percent of vet center employees are women veterans who have served in a war zone!
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
successful transition after the military, so I’m very dedicated to ensuring women veterans are aware of the benefits they have earned – and that VA serves them effectively and sensitively when they come to us.
VA PHOTOS BY ROBERT TURTIL
How have your husband’s experiences with his wound and treatment influenced your view of veterans’ issues or suggested how the system could be improved? We’ve seen tremendous improvement in the systems and services available since Brian was injured in 2003. When he was released from Walter Reed [National Military Medical Center], there were no warrior transition units like there are today; another major improvement has been the development of the Integrated Disability Evaluation System. Case management and integration of caregivers into planning are other positive developments. One of my biggest concerns is that the public will forget about the commitment we have made to those who served our nation as the conflicts overseas wind down or get less media attention. What advice would you give to a female recruit? The advice I’ve traditionally given to women considering military service is to cry in the bathroom, avoid dating anyone in the workplace, and seek to advance your career by working hard to accomplish the mission. Now, I’d also encourage them to seek a mentor. Overall, I think it’s decent advice for anyone entering the workforce.
www.defensemedianetwork.com
■■ TOP: On March 21, 2013, the VA Central Office Federal Women’s
Program, the Center for Women Veterans (CWV), and the Women’s Health Services office presented a Women’s History Month Roundtable titled, “Women Veterans Make History.” ABOVE: Iraq and Afghanistan veteran and Army National Guard soldier Sgt. LuWanda Knuckles and her son, Zavian. Knuckles is the Kentucky Department of Veterans Affairs’ women veterans coordinator. CWV Director Kayla M. Williams says, “... 25 percent of vet center employees are women veterans who have served in a war zone.”
65
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
VA Research: WOMEN’S HEALTH By Craig Collins
n THE POST-9/11 ERA HAS SEEN AN UNPRECEDENTED surge in the number of American women veterans: The Department of Veterans Affairs (VA) estimates there are about 2 million living women veterans today. By 2018, these women will account for 10 percent of all veterans, making women the fastest-growing segment of the veteran population. The nation’s largest integrated health care system, the Veterans Health Administration (VHA), wasn’t built with women in mind – and understandably so, as women veterans, until the 21st century, demanded such a small portion of VA resources. But the radical change in demographics has demanded an equally dramatic change in philosophy: VA leaders, health care providers, and research scientists are in the midst of a historic transformation, discovering data and anecdotal information that will help describe the specific health care needs of a diverse, complex, and growing population of female veterans, and then creating or adapting policy and programs to meet these needs. In 2005, the VA held its first women’s health agenda-setting conference, focusing broadly on biomedical, clinical, rehabilitation, and health services research. It’s difficult to convey how significant the increase in women’s health research by VA investigators has been over the past decade. Elizabeth Yano, Ph.D., M.S.P.H., is director of the Center for the Study of Healthcare Innovation, Implementation and Policy in the VA’s Office of Health Services Research & Development (HSR&D), and an adjunct professor of health policy and management at the University of California-Los Angeles. In the 66
first five years after that 2005 conference, Yano said, there was more research published on women veterans than in the previous 25 years. “And since then,” she said, “the amount of research related to women veterans’ health has more than doubled again.” In 2010, under the leadership of Yano and VA investigators Susan Frayne, M.D., M.P.H., and Alison Hamilton, Ph.D., M.P.H., the HSR&D created the Women’s Health Research Network and its Practice-based Research Network (PBRN), an initiative aimed at including more women in VA studies, expanding research on women veterans, sharpening the VHA’s focus on their health needs, and improving their care and health. Some recent women’s health studies have been coordinated under initiatives aimed at addressing high-priority issues. One of the projects of the VA’s Collaborative Health Research to Enhance and Advance Transformation and Excellence (CREATE) initiative, for example, is led by Yano and includes five funded projects aimed at understanding how to improve access to comprehensive care, retention of women veterans, and quality of care for women veterans. Last year, Hamilton and other investigators at the VA Greater Los Angeles Healthcare System launched a trio of investigations under the Quality Enhancement Research Initiative (QUERI), an initiative aimed at rapidly implementing and evaluating evidence-based improvements in routine care. The Enhancing Mental and Physical Health of Women through Engagement and Retention (EMPOWER) QUERI, Yano said, “is basically using patient-engagement methods to help women
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
■■ With more women than ever before serving inthe military, there is an urgent need to address the many issues that these women will face
VA PHOTO BY ROBERT TURTIL
when they end their service. In July 2011, the VA held its first-ever National Training Summit for Women Veterans. Nearly 700 attendees – women veterans,servicew omen, and advocates from across the country – came together to collaborate and discuss issues facing women veterans and women service members.
participate in redesigning their care.” EMPOWER has three areas of focus: cardiovascular risk reduction, diabetes care, and treatment for anxiety and depression. How do VA researchers decide on such areas of emphasis? Through careful studies of women veterans. According to Yano, EMPOWER’s three areas of focus evolved from previous studies that found shortfalls in care for women veterans. An inaugural PBRN study, led by Rachel Kimerling, Ph.D., a psychologist and researcher for the National Center for PTSD and the VA HSR&D Center for Innovation to Implementation at the VA Palo Alto Health Care System in California, discovered that women veterans generally had a strong preference for receiving mental health services that were designed specifically for women and delivered in a
www.defensemedianetwork.com
primary-care setting. The EMPOWER QUERI is also evaluating a diabetes prevention program tailored to fit the lifestyle of women veterans who might otherwise decline to attend: “That one was going to enroll about 40 women,” said Yano, and they ended up with almost 120, because of the demand for some of their online opportunities and ways to accommodate women’s schedules – if they were, say, caregivers for children or older adults.” The most important thing to remember about today’s research in women’s health, Yano said, is that several post-9/11 initiatives have driven and supported a broader spectrum of inquiry and a more comprehensive research agenda. “It used to be that 69 percent of VA research on women’s health was related to PTSD [post-traumatic stress disorder] or mental 67
N
O
R
T
H
W
E
S
T
E
R
N
U
N
I
V
E
R
S
I
T
Y
The Time is Now. Take the Lead. Graduate Programs in Healthcare Quality and Patient Safety
PROGRAM DIRECTORS: Kevin Weiss, MD, MPH Professor of Clinical Medicine Feinberg School of Medicine Northwestern University Senior Vice President Institutional Accreditation Accreditation Council for Graduate Medical Education (ACGME)
MASTER OF SCIENCE
FACULTY DEVELOPMENT
CERTIFICATE PROGRAM
• 2-year program
• 12-month program
• 12-month program
Designed for clinical and non-clinical professionals currently working in
Designed for faculty who
Designed for the healthcare professional who wants to
healthcare who want to focus their career development on improving healthcare delivery systems
Donna Woods, EdM, PhD Associate Professor Center for Healthcare Studies Feinberg School of Medicine Northwestern University
wish to develop the educational tools, methods and curricular approaches for integrating quality and safety into the medical education curriculum
acquire a comprehensive overview of healthcare quality and patient safety
“Medical Errors Now Third Leading Cause of Death in U.S.�
All programs are part-time and do not require Chicago residence.
— BMJ Quality & Safety
www.northwestern.edu/quality-safety
312.503.5533
MastersIHS@northwestern.edu
The Hampton University Proton Therapy Institute Easing Human Misery and Saving Lives
You’ve heard the phrases before: as comfortable as possible; as normal as possible; as effective as possible. At Hampton University Proton Therapy Institute (HUPTI), we don’t want you to live a good life considering you have cancer; we want you to live a good life, period, and be free of what others define as possible. Cancer is killing people at an alarming rate all across our country. It is now the leading cause of death in 22 states, behind heart disease. Those states are Alaska, Arizona, California, Colorado, Delaware, Idaho, Kansas, Kentucky, Maine, Massachusetts, Minnesota, Montana, Nebraska, New Hampshire, New Mexico, North Carolina, Oregon, Vermont, Virginia, Washington, West Virginia, and Wisconsin.
The men and women whose lives were saved by this lifesaving technology are as passionate about the treatment as those who work at the facility each and every day. Dr. William R. Harvey, a true humanitarian, led the efforts of HUPTI becoming the world’s largest, free-standing proton therapy institute which has been treating patients since August 2010.
“As a patient treatment facility as well as a research and education center, HUPTI builds upon Hampton’s legacy of knowledge and innovation. HUPTI doctors and researchers are further developing the science of proton therapy and remain at the vanguard of the fight against cancer into the future. HUPTI is a catalyst for new scientific discoveries and increasingly accurate, advanced care for cancer patients,� Harvey said.
The Hampton University Proton Therapy Institute
The latest statistics released by the American Cancer Society’s annual report confirms that cancer cases will significantly outpace the population growth in many states. The Hampton University Proton Therapy Institute (HUPTI) is uniquely poised to make a difference.
HUPTI treats a broad variety of cancers including, but not limited to some
of the most technically challenging cases of prostate cancer, breast cancer, lung Easing Human Misery and Saving Lives cancer, cancers of the brain and spine, head and neck, GI; and pediatric. The proton therapy used at HUPTI continues to be an innovative and effective
The men and women whose lives were saved by this lifesaving technology You’ve nonsurgical, heard thenoninvasive phrases before: as comfortable as advantages possible;include: as normal as cancer treatment. It’s primary are as passionate about the treatment as those who work at the facility each and possible; as effective as possible. At Hampton University Proton Therapy Institute everyUniversity day. (HUPTI), we don’t want you to live a good life considering you have cancer; weHampton has one of only
want you to live a good
life, period, and be free of what others define as possible.17 proton centers in the U.S. Dr. William R. Harvey, a true humanitarian, led the efforts of HUPTI leaving healthy cells unharmed
becoming the world’s largest, free-standing proton therapy institute which has Cancer is killing people at an alarming rate all across our country. It is now the today for apatients consultation at 877.251.6838 2010. been treating since August leading cause of death
in 22 states, behind heart disease. Those states are Alaska,Call us each appointment being 20 to 30 minutes per dayKansas, for one toKentucky, nine weeks. Maine, Arizona, California, Colorado, Delaware, Idaho, “As a patient treatment facility as well as a research and education center, Massachusetts, Minnesota, Montana, Nebraska, New Hampshire, New Mexico, HUPTI builds upon Hampton’s legacy of knowledge and innovation. HUPTI North Carolina, Oregon, Vermont, Virginia, Washington, West Virginia, and doctors and researchers are further developing the science of proton therapy Wisconsin. and remain at the vanguard of the fight against cancer into the future. HUPTI is The latest statistics released by the American Cancer Society’s annual report confirms that cancer cases will significantly outpace the population growth in many states. The Hampton University Proton Therapy Institute (HUPTI) is uniquely poised to make a difference.
The proton therapy used at HUPTI continues to be an innovative and effective nonsurgical, noninvasive cancer treatment. It’s primary advantages include: Successfully treating children
Dr. W. R. Harvey, President &
without harsh side effects Visionary behind HUPTI
Targeted radiation can reduce side effects & discomfort
a catalyst for new scientific discoveries and increasingly accurate, advanced care for cancer patients,� Harvey said.
HUPTI treats a broad variety of cancers including, but not limited to some of the most technically challenging cases of prostate cancer, breast cancer, lung cancer, cancers of the brain and spine, head and neck, GI; and pediatric. World Renowned Oncologists
Our staff provides support &
Live Your Life &
compassion to our patients Let Us Fight Your Cancer Hampton University has one of only
17 proton centerstherapy in the U.S. institute hampton university proton
leaving healthy cells unharmed
hampton, virginia 23666 Call us today for a consultation at 877.251.6838 40 enterprise parkway, each appointment being 20 to 30 minutes per day for one to nine weeks. 757-251-6800 - www.hamptonproton.org
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
health. And while that’s still an important area of study, we have a really healthy portfolio in reproductive health, postdeployment health, primary care, and prevention.”
PHOTO BY DAVID E. GILLEPSIE
REPRODUCTIVE HEALTH AND COMMUNITY CARE
The demographic change occurring among U.S. veterans doesn’t simply mean there are more women veterans. VA studies reveal that the percentage of women veterans in rural areas has more than doubled since the first Gulf War – and that as the male veteran population continues to age, most women veterans fall into younger age groups. This has compelled the VHA to transform itself into a health care system that provides – or, more accurately, pays for – communitybased perinatal care to pregnant women and mothers with newborn babies. Of course, very little is known about the reproductive health needs of women veterans, because – until recently – nobody has launched a comprehensive study of those needs. For the past several years, one of the leading VA investigators in the field has been Kristin Mattocks, Ph.D., M.P.H., associate chief of staff for research at the VA Central Western Massachusetts Healthcare System and an associate professor at the University of Massachusetts Medical School. “Much of our work with women veterans,” said Mattocks, “is just figuring out the challenges they’re having in getting and coordinating care.” In 2010, Mattocks and colleagues published a study that showed pregnant Iraq and Afghanistan veterans carried a higher burden of mental health conditions such as anxiety, depression, and PTSD. But because women didn’t receive pregnancy care at VHA facilities, little was known about their care or their health outcomes. About a year and a half ago – at a time when the number of women delivering babies using VHA benefits had doubled in the previous five years – a team led by Mattocks launched the VA’s first-ever study of female veterans during pregnancy and following childbirth. Known as the COMFORT (Center for Maternal and Infant Outcomes Research in Translation) study, the three-year, 15-site investigation will inform the VA’s ongoing efforts to improve prenatal and postpartum care coordination and follow-through for women enrolled in the VHA. “We’re about a year and a half into it,” said Mattocks. “We’ve interviewed about 250 women veterans during the pregnancy period, and 125 who have already delivered. And we’re learning a lot about veteran mothers and their babies.” One of the programs already in place to increase access to specialty care for veterans in rural areas and medically underserved areas is the VA’s SCAN-ECHO (Specialty Care Access Network-Extension for Community Healthcare Outcomes) program, which has driven several programs throughout the VHA. One of them, part of the Women’s Health CREATE, is led by Donna Washington, M.D., M.P.H., of the VA Greater
www.defensemedianetwork.com
■■ Capt. Ebony Todd, legal adviser at Fort Campbell, Kentucky,
discusses her pregnancy with Capt. (Dr.) David Tillman, Blanchfield Army Community Hospital OB-GYN provider, Jan. 30, 2017. She is an advocate for regular well-women screenings.
Los Angeles Healthcare System, who is evaluating a program of tele-support and education for women’s health care at community-based outpatient clinics (CBOCs). “There are fewer designated women health providers out in those CBOCs,” explained Yano. “So a lot of women end up wanting to drive all the way to the VA medical center and bypass the nearby clinics, just to get to that designated women’s health provider.” The program being evaluated by Washington’s team involves a centralized gynecologist who provides support and education to CBOC providers, in order to improve women veterans’ access to local care. The VA, said Mattocks, is at a tipping point when it comes to caring for women veterans. “It’s a time of transition,” she said, “when we’re really figuring out what care needs to stay in house and what care needs to go to the community – and along with that, the issues of coordinating care between the two. Probably the best example of that is pregnancy, because we just don’t do much of it in house, and there’s so much we don’t know. For example, do women come back [to] the VA when they’re done being pregnant? It’s not something we used to spend much time thinking about.” MENTAL HEALTH CARE AND SUICIDE PREVENTION
Mattocks began her investigations into the mental health burdens of pregnant veterans because these burdens had already been well established by the Women Veterans Cohort Study (WVCS) – a landmark study of Iraq and Afghanistan veterans, launched in 2007, that recently received another round of funding through 2018. Among the WVCS’ findings: Women veterans suffer depression at twice the rate as male 69
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
veterans, and female veterans have greater anxiety and difficulty readjusting to civilian life than men. • 20 percent – 1 in 5 – women veterans have been victims of military sexual trauma (MST). The VHA has been screening all veterans, male and female, for MST since 2002, and its prevalence has been monitored annually for more than a decade. Among women receiving VHA care, 1 in 4 have reported being a victim of MST. While the rate of PTSD is about the same among male and female veterans, other VA studies have shown that the number of women veterans with PTSD tripled from 1999 to 2009. A report last year from the VA’s Office of Suicide Prevention also showed alarming rates of increase in suicide by women veterans: The age-adjusted rate of suicide among female veterans has increased 85.2 percent since 2001, compared to 30.5 percent among male veterans. Perhaps the report’s most shocking discovery: For women veterans aged 18 to 29, the risk of suicide is 12 times the rate of non-veteran women. Clearly, gender-tailored interventions are necessary to support the mental health of female veterans – and VA investigators are working to build the evidence
base for those interventions. The common-sense notion that mental health conditions contribute to suicide is an important consideration for women veterans, explained Kimerling: “In studies of veterans, we find that the risk for suicide posed by mental health conditions is substantially stronger for women than men,” she said. “So a diagnosis of depression increases your risk for suicide to a much greater extent if you’re female than if you’re male.” Kimerling is investigating ways the VA can tailor women veterans’ mental health services to post-deployment problems by looking at the variables that may be especially important for women – PTSD, MST, intimate partner violence, depression, and anxiety, for example. Kimerling and colleagues have found MST to be a significant contributor to homelessness for women veterans, and just last year reported that MST was, by itself, apart from any associated mental health conditions, a significant contributor to suicide risk. Such research is already translating into practice: Because Congress has mandated free medical care for all MST-related conditions, Kimerling said, “We know we’re reaching the people at high risk of suicide with those mental health services. And we’ve said: ‘Well,
We’re making
women's health a priority
MASTER OF SCIENCE IN NURSING:
WOMEN’S HEALTH NURSE PRACTITIONER PROGRAM
Carlow.edu/nursing 70
www.defensemedianetwork.com
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
maybe now we can really do a better job of linking MSTrelated services with suicide-related services’ – which is one of the actions that VA took as a result of the data.” This cross-linkage of MST- and suicide-related services is evidence of VHA’s responsiveness to the results that researchers like Kimerling provide – but the worsening suicide problem has made Kimerling turn the focus of her future work on investigating ways of getting women veterans to engage in care. “I’ll be looking at veteran preferences for care,” she said, “and talking to veterans to make sure we aren’t just setting these services up and saying: ‘OK, here you go,’ but also presenting them in a way that will make it easy to get care, and make people want to engage. We continue to see people who have experienced MST who didn’t know they could walk into a VA and receive care for free. It’s important to let people know treatment is available.”
VA/ROBERT TURTIL
RESEARCH INTO PRACTICE
It’s important to emphasize, as Kimerling does, the direct relationship between the data and information VA investigators discover and the care and services provided at VHA facilities. Mattocks’ discoveries about mental health conditions among pregnant woman veterans led, in part, to a VA policy requiring every VHA site to have a maternity care coordinator to track pregnant women veterans
www.defensemedianetwork.com
■■ The Washington DCVeterans Affairs Medical Center’s Winterhaven Homeless V eterans Stand Down 2015 event saw record numbers of homeless, at-risk,and underemployed v eterans. More than 700 men and women veterans attended the 21st annual Winterhaven Homeless V eterans Stand Down toreceive assistance with health care, benefits, counseling, employment, managing finances, a nd housing.
and maintain communication between the VHA and the non-VA provider. Sally Haskell, M.D., M.S., is a researcher, clinician, and one of the architects of women’s health care delivery across the VHA. She’s VA deputy chief consultant for women’s health services, VA director of comprehensive women’s health care, and also the lead investigator for both phases of the WVCS. The study itself, Haskell said, has contributed to the launch of new programs related to women veterans’ health care. One recent example: the Mini-Residency in Musculoskeletal Care, a three-day training course for women’s health providers. Some of the earliest investigations published in the WVCS, said Haskell, involved the prevalence of musculoskeletal conditions or diagnoses among women returning from deployment. “It turned out that women had higher rates of musculoskeletal conditions, and slightly higher rates of chronic pain, than men,” Haskell said. “So the musculoskeletal miniresidency trains the primary care providers and updates their skills in managing musculoskeletal conditions. It deals 71
ALL PROGRAMS ARE ONLINE. LOYOLA UNIVERSITY NEW ORLEANS IS A YELLOW RIBBON PROGRAM PARTICIPANT.
DEGREES OFFERED: Ranked among the top 50 Online Graduate Nursing Programs for 5 years and among the top 20 Online Graduate Nursing Programs for Veterans for 2016 by U.S. News & World Report.
1. Doctor of Nursing Practice • MSN to DNP for Executive Leadership and Nurse Practitioner • BSN to DNP for Family Nurse Practitioner 2. Master of Science in Nursing a. Students with a non-nursing bachelor’s degree may apply into the MSN program through the BLEND (Bridge) option • Nursing Leadership • Family Nurse Practitioner • Nurse Educator 3 RN to Bachelor’s of Science in Nursing
For more information, call (504)-865-3124, or toll free at (800)488-657, email nursing@loyno.edu, or visit us online at loyno.edu/nursing.
LOYOLA UNIVERSITY NEW ORLEANS SCHOOL OF NURSING GREAT OPPORTUNITIES FOR VETERANS AT LOYOLA UNIVERSITY NEW ORLEANS— A YELLOW RIBBON COMMUNITY JESUIT EDUCATION WITH A FOCUS ON INNOVATIVE LEADERSHIP AND CLINICAL EXPERIENCE. ALL PROGRAMS REQUIRE RN LICENSURE. CCNE ACCREDITED.
BATTLE CREEK VA MEDICAL CENTER FLICKR PHOTO
V E TE R AN S AFFAI R S & M I LITARY M E D I CI N E O UTLO O K
with things that occur in both men and women, but focuses on those that are more common in women, like knee and hip injuries, and shoulder injuries.” A more broadly offered mini-residency, in place since 2009, updates provider skills to address women’s health issues more generally. “It’s a fantastic program, and we’ve actually trained over 3,000 women’s health providers through this program,” Haskell said. “It’s really our biggest effort in terms of improving access, training up the VA workforce to ensure that we have enough people actually trained to be designated women’s health providers.” Haskell said the work of VA researchers has been influential in implementing an overall policy that’s transforming women’s health care. Research by Yano and others, for example, has led to substantial changes in primary care, making the experience less fragmented and easier to access. “In our policy, we established that all women should really be offered assignment to what we call a designated women’s health provider,” said Haskell. “We now have designated women’s health providers in every health care system, and at almost every site of care.” Studies have since established that the overall quality of gender-specific health care delivered by these providers is better, compared to other providers. Several policies have also been rolled out, Haskell said, to address the discomfort women veterans have expressed, in interviews with investigators, about a lack of privacy in health care settings. While this work is most visible at the facilities level – privacy curtains in exam rooms, private inpatient rooms, and bathrooms set aside for women, Haskell said it’s really about “transforming a whole health care system that was really set up for men. Now, with this very rapid increase in the population of women, we’ve just had a lot of work to do to bring everybody up to speed.” The speed and effectiveness with which that work is progressing, said Yano, has to do with the unusual level
www.defensemedianetwork.com
of collaboration throughout the VHA. “All the research informing women veterans’ health care is done in partnership with the frontline providers, with women veterans themselves, and with policymakers. It’s very unusual to have this kind of multilevel engagement. I think that’s why we’re able to have the impact that we are: We’ve transformed the literature. And we’re transforming care for women veterans.”
■■ A patient receives physical therapy care
at the Battle Creek VA Medical Center, February 2016. One Women Veterans Cohort Study (WVCS) follow-on program – a three-day training course for women’s health providers called the Mini-Residency in Musculoskeletal Care – revealed the prevalence of musculoskeletal conditions or diagnoses among women returning from deployment.
73