
5 minute read
University of Illinois at Urbana-Champaign Develops Interactive Mixed Reality Software for Sepsis Diagnosis
Virtual and Augmented reality helps train medical professionals
SPONSORED BY THE UNIVERSITY OF ILLINOIS AT URBANA-CHAMPAIGN
It's rare to find someone in America who's life has not been impacted by sepsis, whether themselves or a loved one. Michelle Osborne, an employee of the University of Illinois, recalls her father passing away from sepsis in 2012: “The symptoms progressed so quickly that it was difficult for doctors to determine he had it until it was too late.” The same year in Central Illinois, 5-year-old Gabby Galbo died from sepsis from an undetected tick bite, prompting her parents to fight for legislation to develop evidence-based protocol for early recognition and treatment in statewide hospitals. “Gabby’s Law” was signed into effect by Governor Bruce Rauner in 2016 and has been followed by legislation in Ohio and Wisconsin. While sepsis can affect anyone, the very young and very old are often most at risk. In deployed field hospitals, soldiers with abdominal trauma and significant tissue loss are at greater risk of developing sepsis, according to an article published by BMJ Military Health in 2013. Collaboration efforts have led to a 16% decrease in mortality-associated sepsis since 2013 according to the CDC, yet the disease remains notoriously difficult to identify and treat quickly.

Student’s view of Interactive Mixed Reality Trainer during simulation performed in summer 2019, showing the 360-degree video recording component. The simulated patient is a 35-year-old female complaining of fever after a recent surgery.
The CDC estimates that at least 1.7 million adults in the United States annually develop sepsis, which is the body’s response to an infection. Sepsis can be difficult to diagnose and is often fatal if not treated in a timely manner. Out of those 1.7 million adults, nearly 270,000 die from sepsis: that’s nearly one out of every three patients who die in a hospital. Symptoms are ambiguous and can include a fever and chills, shortness of breath, and high heart rate, progressing to cognitive impairment and organ shutdown. To improve sepsis outcomes, a new Interactive Mixed Reality (IMR) training tool has been developed by OSF HealthCare and the University of Illinois at Urbana-Champaign. IMR encompasses both virtual and augmented reality (VR and AR), merging real and virtual worlds to produce new learning environments. This tool makes it easier for healthcare providers to diagnose by directing them through sepsis prevention protocol with a 360-degree video recording and annotation, proving the efficacy of new simulated environments in training novice medical professionals.
“Simulation technologies such as virtual and augmented reality are becoming more common in medical training,” said T. Kesh Kesavadas, Director of the Health Care Engineering Systems Center (HCESC) at the University of Illinois. VR and AR are a major focus of HCESC, a research center that fosters collaboration between engineers and physicians. Other areas of focus for HCESC are surgical robotics, health data analytics, and smart health. Kesavadas states, “Our center is at the forefront of developing these technologies as well as software that makes it possible for faculty without programming skills to create IMR scenarios.”

The sepsis IMR trainer features four components: an introduction to the scenario, direction through a patient evaluation, directions on administering protocol to a patient in septic shock, and suggestion of additional tests to perform on the patient.
HCESC’s goal is that increasing usability of VR and AR technologies for instructors will make them more widespread in training novice medical professionals and improving existing healthcare processes. These technologies allow students to practice techniques more thoroughly prior to practicing on a simulated or actual patient but are not easy to create; lack of effective software for instructors to easily develop VR curriculum content is a hurdle that HCESC is working diligently to overcome.
In partnership with OSF HealthCare, HCESC has created a software platform that simplifies the creation of IMR. The sepsis protocol training referenced above is comprised of three parts: an integrated, 360-degree video recording of a clinical encounter to provide firstperson perspective, rich annotated content, and an assessment questionnaire. “An important part of simulation is including real-world parameters: patient physiology, emotions, and clinical team behaviors all contribute to how successful an encounter might be. Our software platform allows instructors to easily include all these parameters,” Kesavadas said.
“OSF HealthCare is testing VR as a replacement for traditional simulation training for nurses. VR-based software has made this training accessible to nurses in a timely manner at their workstation,” added John Vozenilek, M.D., Vice President and Chief Medical Officer for Innovation and Digital Health at Jump Trading Simulation and Education Center at OSF HealthCare. “We are planning to develop a comprehensive set of curriculum for nursing staff and other health professionals using the new IMR technology.”
HCESC’s sepsis prevention education scenario demonstrates the potential of enhancing simulated medical training by accelerating clinical exposure for novice students. “We conducted an IRB-approved study with 28 novice students to evaluate its efficacy, and proudly concluded that our IMR software is a usable technology,” Kesavadas said. The participants provided feedback by answering demographics, NASA-TLX, and system usability scale questionnaires. “It’s a step towards improving VR-based education content development.”
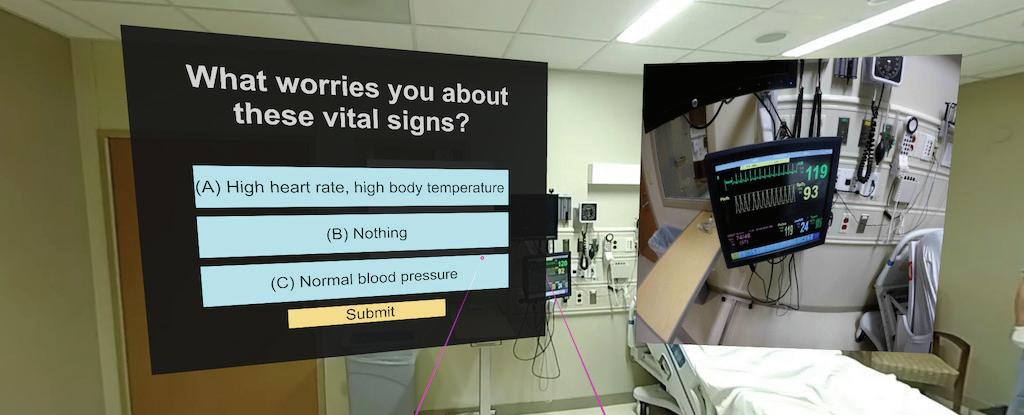
The sepsis IMR trainer displays questions about patient statistics to direct a student through determining if sepsis is present. The inset on the right is a zoomed-in reading of the patient’s heart rate and body temperature readings.
The Health Care Engineering Systems Center at the University of Illinois is a research center housed under the Grainger College of Engineering, with a focus on fostering collaboration between engineers and physicians to improve healthcare technologies and patient outcomes such as sepsis recovery. Simulation technology using VR and AR is a huge focus of HCESC, especially as its use becomes more viable as an educational tool in hospitals such as the OSF HealthCare system. A large part of HCESC’s mission is collaboration: their partnership with Jump Simulation Center provides training on the latest mannequin-based simulators and virtual reality tools to meet the needs of the new Carle Illinois College of Medicine and other medical and allied health organizations in central Illinois. Their partnership with OSF HealthCare in Peoria, Jump ARCHES, provides direct access and competitive grants for engineers and clinicians of every discipline to work together and solve healthcare problems. Over the last four years, this endowment has provided $3 million to affiliates at the University of Illinois at Urbana-Champaign, University of Illinois College of Medicine in Peoria, and OSF HealthCare systems. In 2019, the partnership was expanded to foster further collaboration between investigators in areas beyond engineering, such as applied health sciences and veteran’s affairs at the University of Illinois.
While sepsis remains difficult to diagnose and may rapidly turn fatal, the University of Illinois is hoping that this Interactive Mixed Reality technology will prompt healthcare providers to ask the right questions and perform the correct assessments quickly. The portable nature of IMR sepsis training allows for quick and easy adoption, ultimately benefitting patients from large hospital complexes to deployed field hospitals with limited resources. Osborne adds, “This technology may have saved my father’s life had doctors been using it in 2012, but I’m hopeful that it can save countless lives as HCESC moves forward with it in the future.”










