Official Publication of the Florida College of Emergency Physicians A Chapter of the American College of Emergency Physicians
Introducing
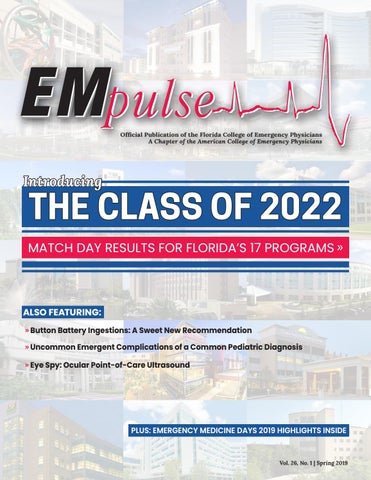
THE CLASS OF 2022
MATCH DAY RESULTS FOR FLORIDA’S 17 PROGRAMS »
ALSO FEATURING: » Button Battery Ingestions: A Sweet New Recommendation » Uncommon Emergent Complications of a Common Pediatric Diagnosis » Eye Spy: Ocular Point-of-Care Ultrasound
PLUS: EMERGENCY MEDICINE DAYS 2019 HIGHLIGHTS INSIDE
EMpulse Spring 2019
Vol. 26, No. 1 | Spring 2019
1
Join TeamHealth Emergency Departments in Central Florida Advent Health in Orlando, Florida, has served the central Florida community for more than 50 years. Comprised of 10 Advent Health emergency facilities spanning across four central Florida counties, the system ranges from quaternary care to community-based medicine, including an established emergency medicine residency program and two dedicated pediatric emergency departments. In fall 2019, Advent Health will open two additional free-standing emergency departments and a dedicated pediatric emergency department to better serve our Florida community. TeamHealth has a mission to deliver compassionate care to the central Florida community and build a supportive team and environment for our physicians and advanced practice clinicians.
TeamHealth offers: Generous sign-on bonus
Comprehensive benefits package
Relocation incentives
CME allowance
Highly competitive compensation
teamhealth.com/join
Contact Lisa Murray at 865.244.7643 or Lisa_Murray@teamhealth.com
Spring 2019 | Volume 26, Issue 1
Table of Contents
Florida College of Emergency Physicians
FCEP COMMITTEE REPORTS
4 A Letter to Readers
Beth Brunner, MBA, CAE
5 FCEP President’s Message
J. Adrian Tyndall, MD, MPH, FACEP
6 Gov’t Affairs: EM Days 2019 Damian Caraballo, MD, FACEP
12 Pediatric Committee
John Misdary, MD, FACEP & Todd Wylie, MD
13 Membership & Professional Development
René Mack, MD, RDMS, FACEP
8 ACEP President's Message
14 EMRAF
9 Medical Economics
16 Medical Student Committee
Vidor Friedman, MD, FACEP
Daniel Brennan, MD, FACEP
Misty Coello, MD, PGY-1 Kimberly Herard
FCEP Executive Committee President
J. Adrian Tyndall, MD, MPH, FACEP
President-Elect
Kristin McCabe-Kline, MD, FACEP, FAAEM, ACHE
Vice President
Sanjay Pattani, MD, MHSA, FACEP
Secretary-Treasurer
Damian Caraballo, MD, FACEP
10 EMS/Trauma
Immediate Past-President
Christine Van Dillen, MD, FACEP
Joel Stern, MD, FACEP, FAAEM
Executive Director
COLUMNS & FEATURES
8 Daunting Diagnosis
Karen Estrine, DO, FACEP, FAAEM
17 Updates on the Opioid Crisis
Compiled by Samantha League, MA
18 Meet the Class of 2022
Florida’s EM Residency Programs
20 Residency Program Updates
Florida’s EM Residency Programs
30 Resident Case Report: Uncommon Emergent Complications of a Common Pediatric Diagnosis Thomas Ruffin Jr., MD, FAAP, PGY-6 & Carolyn Lyon, MD
Beth Brunner, MBA, CAE
32 Ultrasound Zoom: Eye Spy: Ocular Point-of-Care Ultrasound
Kelsey Wolfe, MD, PGY-2 & Leila Posaw, MD, MPH
36 Poison Control: Button
Battery Ingestions: A Sweet New Recommendation
Kristen C. Lee, PharmD, BCBS & Madison Schwartz, PharmD
38 Membership Spotlight: Dr. Sanjay Pattani
René Mack, MD, RDMS, FACEP & Shayne Gue, MD
UPCOMING DEADLINES: Summer 2019
3717 S. Conway Road Orlando, Florida 32812 t: 407-281-7396 • 800-766-6335 f: 407-281-4407 www.emlrc.org
• Ad insertion orders due: May 17 • Ad design/payment due: May 31 • Articles due: June 3
Fall 2019
• Ad insertion orders due: July 26 • Ad design/payment due: Aug. 16 • Articles due: Aug. 16
EMpulse is always accepting articles, case reports and advertisements. Find our advertising kit at emlrc.org/empulse and contact Dr. Karen Estrine at karenestrine@hotmail.com or Samantha League at sleague@emlrc.org for article guidelines. EMpulse Spring 2019
EMpulse Editorial Board Editor-in-Chief
Karen Estrine, DO, FACEP, FAAEM karenestrine@hotmail.com
Managing & Design Editor Samantha League, MA sleague@emlrc.org
www.emlrc.org/empulse
Published by:
Johnson Press of America, Inc. 800 N. Court St. Pontiac, IL 61764 t: 815-844-5161 | f: 815-842-1349 www.jpapontiac.com All advertisements in EMpulse are printed as received from advertisers. The Florida College of Emergency Physicians does not endorse any products or services, except those in its Preferred Vendor Partnership. FCEP receives and distributes employment opportunities but does not review, recommend or endorse any individuals, groups or hospitals that respond to these advertisements. Opinions stated within articles are solely those of the writers and do not necessarily reflect those of the EMpulse staff, the Florida College of Emergency Physicians and our advertisers/sponsors. 3
A Letter to Readers
By Beth Brunner, MBA, CAE Executive Director of the Florida College of Emergency Physicians
Dear FCEP members, As a membership organization heavily involved in advocacy, it is our duty to follow events unfolding in the political sphere. FCEP has always taken the stance of advocating for patients and emergency physicians, regardless of political party affiliations. As the current political climate continues to polarize, it is our duty as highly-educated professionals to rise above divisive rhetoric and focus solely on advocating for the best health policy. It has been brought to our attention that recent EMpulse articles have been too politically-charged and divisive. This is not the intention of EMpulse Magazine or FCEP, and we apologize
for publishing this type of content. EMpulse Magazine is a platform in which FCEP members can express their thoughts and opinions on emergency care-related issues, and we greatly value this type of content. We also recognize that FCEP members are entitled to their own views and opinions, which is why our policy on page 3 states: “opinions stated within articles are solely those of the writers and do not necessarily reflect those of the EMpulse staff, the Florida College of Emergency Physicians and our advertisers/sponsors.” In effort to move forward with po-
sitioning ourselves as a respected scientific journal and member-benefit magazine, we would like to reaffirm our commitment to advocating for patients and emergency physicians regardless of party affiliation, and to publishing content that promotes and stems from evidence-based arguments. As always, we appreciate and value your feedback. You are welcome to reach out to the FCEP executive committee (found on page 3); our editor-in-chief, Dr. Karen Estrine, at karenestrine@hotmail.com; or our managing & design editor, Samantha League, at sleague@emlrc.org. ■
NOT COLLECTING WHAT YOU SHOULD?
Our industry-first Revenue Calculator immediately identifies missing practice revenue!
REVCALCULATOR.COM FOUNDED BY ED PHYSICIANS | PROPRIETARY BILLING AND REPORTING SOFTWARE | UP TO 30% MORE REVENUE 4
EMpulse Spring 2019
COMMITTEE REPORTS
FCEP President’s Message By J. Adrian Tyndall, MD, MPH, FACEP FCEP President • Interim Dean of UF College of Medicine
When I moved to Florida, my first meeting experience with the Florida College of Emergency Physicians was Emergency Medicine Days in 2007. This highlight and emphasis on advocacy has always been, in my opinion, what sets FCEP apart from other chapters that I know of. March 11-13, 2019 was no different, except that it represented the 30th year FCEP has hosted Emergency Medicine Days in Tallahassee. This year, over 50 physicians, residents and medical students travelled to Tallahassee to learn about issues impacting emergency physicians across the state and the patients they serve. This was an opportunity to have conversations with dozens of legislators and legislative aides and visit with state government officials, all in effort to focus on bills and policies that could have a lasting impact on the health care delivery system in Florida. In today’s environment, the importance of advocacy cannot be understated. Emergency physicians have the unique experience of truly being on the front lines of patient care, at
NEXT MEETINGS: FCEP Committee Meetings May 22, 2019 9:00 am-4:00 pm EMLRC in Orlando, FL Joint FEMF/FCEP Board Meeting May 23, 2019 9:00 am-1:00 pm EMLRC in Orlando, FL Look for call-in #s in FCEP’s enews
EMNews Now
Are you receiving our enews on Wednesday mornings? Sign up now!
“
Emergency physicians have the unique experience of truly being on the front lines of patient care, at an interface that few others see in the health system... We need to be able to tell these stories to policymakers so that the legislative process, in the end, benefits and does not harm our citizens.
an interface that few others see in the health system. We see the issues impacting vulnerable populations and the outcomes when access to care is inhibited. We need to be able to tell these stories to policymakers so that the legislative process, in the end, benefits and does not harm our citizens. This is a powerful and privileged platform, and one of the greatest benefits the College provides to its members and emergency physicians across the state. We are truly the voice for emergency physicians in Florida and there are still many opportunities to get involved in organized emergency
medicine at FCEP. For example, at our quarterly Board of Directors meeting on March 12, I announced that there are five open board seats and 10 Councillor positions available to represent FCEP at ACEP’s Scientific Assembly and annual meeting. Now is the time to become involve in organized emergency medicine. As you read this edition of EMpulse, be sure to read the perspectives of medical students and residents who experienced advocacy for the first time. While the legislative process has progressed well beyond the reports contained in their updates, the core of what we do and what we advocate for remains. The process and the need for advocacy remains. This was, again, another successful year in supporting the mission of the College. I must thank our committee chairs and FCEP staff for a job well done. For those who did not attend, you missed an impactful time for emergency medicine. The more of us that attend, the greater impact we will have. Plan to attend next year, will you? ■
CALL FOR COUNCILLORS & BOARD MEMBERS: FCEP Board of Directors serve a 3-year term and are eligible to serve a maximum of two terms. We have 5 seats open for election in August. FCEP Councillors serve a 2-year term and represent FCEP at ACEP’s Annual Council meetings. Of our 21 slots, 10 are still open. There is no limit on how many terms a Councillor can serve.
EMpulse Spring 2019
To qualify, you must be: a) a member of FCEP b) actively involved in the chapter as evidenced by committee membership and/or attendance at the Board of Directors meetings HOW TO APPLY: Submit your letter of interest to Executive Director Beth Brunner at bbrunner@emlrc.org by April 17, 2019.
5
COMMITTEE REPORTS
Government Affairs: EM Days 2019 By Damian Caraballo, MD, FACEP Government Affairs Committee Chair • FCEP Secretary-Treasurer
March 11-13, 2019 marked the 30th annual Emergency Medicine Days: FCEP’s advocacy conference in Tallahassee. Similar to an ED shift, what was initially thought to be a “quiet” legislative session quickly descended into chaos for the House of Medicine, as House Speaker Oliva and the House Leadership unleashed a host of bills aimed at “disrupting” the delivery of medicine. Among the bills filed this session include:
• a bill which would allow pharma-
cists to test/diagnose strep and influenza in the pharmacy, while also adjusting patient prescriptions without the writing physician’s permission (HB 111 & SB 300); • independent autonomy for nurse practitioners and PA’s (who are now contemplating changing their name from physician assistants, given the sea-change in non-physician autonomy movements around the country) (HB 821); • a bill allowing law enforcement and psychologists to initiate involuntary holds to clinically sober and competent patients if they demonstrate a lack of control due to their chronic substance abuse disorder (HB 313), and • a bill which would apply a fee-schedule cap to all physicians in Florida at a price ceiling of 200% of Medicare (HB 1317 & SB 1790). Other bills include reinstituting malpractice caps, finding a PIP solution which did not squeeze out EMTALA providers, and continued funding and treatment for the opioid crisis. Needless to say, FCEP worked hard this session to play defense and kill bills which would further undermine quality emergency care in Florida. For those in attendance, this legislative session marked an eye-opening view at the hostility many lawmakers have towards current physicians and hospitals as healthcare costs continue 6
BILLS TO WATCH THIS SESSION: HB 1317 (Burton) & SB 1790 (Perry): DOH Adopt Statewide Fee Schedules for Services AGAINST
HB 111 (Plasencia) & SB 300 (Brandes): Testing & Treatment of Influenza and Streptococcus AGAINST
HB 313 (Gottlieb): Marchman Act AGAINST
SB 896 (Brandes) & HB 733 (Grall): Motor Vehicle Insurance (PIP Repeal) AGAINST
SB 528 (Rouson): Mental Health & Substance Use Disorders SUPPORT
HB 307 (Silvers) & SB 360 (Rouson): Insurance Parity for Mental Health & SUD SUPPORT
SB 418 (Simpson): Essential Health Benefits Under Health Insurance Policies & Contracts AGAINST
to skyrocket. Emergency physicians are erroneously being blamed for costs associated with emergency care, such as facility fees, out-of-network costs and high-deductibles. It’s our job to educate lawmakers on the true value of emergency physicians, given that we see more acute care patients than any other specialty and treat the highest number of uninsured and Medicaid patients in the state, without any regard to their ability to pay. As healthcare costs become a bigger portion of state and national budgets, we must work hard to prove our value as leaders in the healthcare field. This comes by forming relationships with our legislators during events such as EM Days. Fortunately, through years of hard work and fostering relationships, we appear to have enough backstops to halt many of these poorly written bills (we’ll have a better idea towards the end of session in May). Still, even if we manage to defeat bad bills this year, we know many will return in similar forms next year. It’s our hope that those in attendance, especially younger physicians and residents, EMpulse Spring 2019
HB 821 (Pigman): Advanced Practice of Registered Nurses AGAINST
now realize the uphill battle we face in protecting physician independence. As FMA President Dr. Corey Howard told FCEP members during his lecture, the House of Medicine needs to band together to find proper solutions to the crises facing modern healthcare. We need to find innovative ways to expand access and provide higher quality care, while standing up for physician rights to improve doctor-patient autonomy in an environment where every insurer, administrator, conglomerate company and even legislator is now trying to dictate how to provide healthcare. Next year’s EM Days will be in January 2020. It’s up to us to take back the practice of medicine and work together to improve emergency medicine—and the practice of medicine in general—in the upcoming years. FCEP Government Affairs strongly encourages you to join us in mapping out the future of our medical practice by joining us in advocacy efforts. Please contact us to find out how you can get involved in improving the practice of emergency medicine in Florida. ■
EMpulse Spring 2019
7
COMMITTEE REPORTS
ACEP President’s Message By Vidor Friedman MD, FACEP ACEP President • FCEP Past-President
While I was prepared before becoming ACEP President to spend half the year on the road advocating for our specialty, the reality has still been daunting. It is truly amazing to witness how far we have evolved in EM. However, our obligations under EMTALA make our profession very vulnerable to cuts in reimbursement. My role is to express upon everyone that we are the ones actually taking care of patients—not the ones to attack—but it is becoming more and more difficult. Let me show you how I do this with a recap of a recent week in my life. On Monday night, I flew to D.C. The following day, ACEP staff and I had meetings on the Hill all day, focused on members of the Senate HELP committee and the Price Transparency Work Group (PTWG). Clearly, the focus is on “surprise bills” and out-of-network (OON) billing. We also had several meetings on Wednesday, including one with the House Minority Health Legislative Aide, and I had a separate meeting with Congressman Soto (D-FL), an old friend who is now on the E&C committee in the House. The insurers have succeeded in get the jargon “surprise bills” into com-
mon language, yet hardly a soul up there even understands out-of-network billing. While in general we were well received, there was definitely push back. Once again the insurers have succeeded, in part, in controlling the narrative and have painted physicians as being the unreasonable ones in the equation. There are currently three different solutions being bandied about on the Hill: rate setting, bundled payments and arbitration. The first two would be disasters for EM. Unfortunately, the insurer’s answer is always connected to raising premiums. Politically, the powers that be do not want to be seen increasing health care costs. We need to be creative and resourceful to combat these tactics. In addition to our work within ACEP, there is also an ad-hoc group of EM groups that is working independently, albeit collaboratively, with ACEP on this issue. There has been a great deal of work going on behind the scenes, and that work is ongoing. Thursday, Dr. Bill Jaquis, Sandy Schnieder and I flew to Chicago to meet with American Society of Anesthesiologists (ASA) leadership. We had
good discussions ranging from OON billing and sedation to physician mental health and burnout. I believe that we will be able to work collaboratively with them on a number of initiatives. Friday, Brad Gruehn and I flew to New Orleans for an event for Senator Bill Cassidy, a leader within the PTWG. We were able to spend a fair amount of time with the senator and his senior staff. I think it was a very useful couple of days. Once again, the focus was on OON billing, and the senator seems to be cautiously supportive of arbitration as a solution. A big shout out to our D.C. staff who are working above and beyond on this issue. The level of intensity and the amount of work is beyond anything I have seen in over a decade of involvement at the federal level, and I think this level of activity will be going on at least till June, perhaps longer. I also managed to work in a few media interviews regarding gun violence, our electric scooter PSA and a reporter for Modern Healthcare doing a series of articles on emergency medicine. I also managed to approve multiple staff requests and committee objectives... just another week in the life. ■
Daunting Diagnosis: Q By Karen Estrine, DO, FACEP, FAAEM Editor-in-Chief
A 52 year-old female presents with left-sided facial droop since 2013 that was diagnosed as sequela of Bell’s Palsy. Upon initial diagnosis 6 years ago, head CT was “negative” for pathology. The patient had no resolution of her symptoms with acyclovir and steroids. Over time, the patient developed headaches, gait instability, left-sided hearing loss and memory loss. Upon re-evaluation years later, brain CT and subsequently brain MRI were preformed. The MRI of the patient is shown. What is her diagnosis?
8
EMpulse Spring 2019
CONTINUE ON PAGE 24 »
COMMITTEE REPORTS
Medical Economics By Daniel Brennan, MD, FACEP Medical Economics Committee Chair
OIR: HUMANA OUT-OFNETWORK UNDERPAYMENTS
FCEP met with the Office of Insurance Regulation (OIR) on January 17 regarding the continued violation of the balance billing legislation by Humana. With a new administration and new OIR staff, we thought it would be helpful to show them the ongoing prevailing practice of HUM to pay outof-network (OON) claims at less than statutorily required. We emphasized this is a pervasive business practice, now documented in two consecutive years by two different EM billing companies representing many affected groups, and that the legislation gave OIR the enforcement power to intercede. OIR promised to investigate and respond; subsequent follow-ups have not yet resulted any action on OIR’s part.
BCBSFL: LEVEL 4/5 LOW ACUITY DX DENIALS
Conversations among EDPMA, FCEP and BCBSFL yielded little in the BCBSFL denials 99284/99285 level claims with “low acuity” diagnoses. BCBS had little understanding of EM billing and of their own policy, initial-
ly stating new admissions would be denied (not knowing the EM professional claims do not denote that information). In any event, they insist this is not a denial, merely a code edit, and that it is not denying of coverage, just denial of 99284/5 payment. Similarly, we do not agree with their representation that this is not a violation of prudent layperson laws. Some groups have noted a recent downtick in BCBSFL denials of 99284/5 claims (previously as high as 8%; now 1-2%), so it will be interesting to see if this is a non-published reversal of their “reimbursement change” or if the denials will increase.
LEGISLATIVE UPDATES
We expect a host of issues to be active this session, revolving around scope of practice (ARNP/pharmacy), telemedicine, opioids and insurance. Many of these impact FCEP medical economics, and our government affairs and medical economics committees work well together with our lobbyist, Toni Large, to represent all emergency physicians’ interests throughout (and before) session. If you did not attend, we highly encourage you to donate to the PAC to assist in our efforts. PIP
repeal is being proposed again, despite the data in 2017 showing minimal savings and data last year showing it would increase insurance costs. Regardless, PIP as a no fault plan pays promptly and fairly, so we will be pushing for a EM medical pay protection in any PIP repeal plan.
MEDICAID MANAGED CARE
AHCA recently represented that all Medicaid Managed Care plans (MMA plans) should now be paying all contracted providers Medicare rates for pediatric patients (<21 yo). At EM Days 2019, Shevan Harris from AHCA was much less definitive in her comments, indicating “if savings existed” they would be used to provide enhanced provider payments to “specialists” caring for pediatric MMA patients.
PAYMENT REFORM SUMMIT
Congratulations to Medical Economics co-chair Dr. Jordan Celeste on a fantastic conference February 7-8. The conference highlighted evolving EM payment issues and featured nationally recognized experts. It is truly a conference any EM practice leader would benefit from. ■
PAYMENT REFORM SUMMIT 2019 COST-EFFECTIVE CARE IN A RISK-BASED WORLD
Scan to see all photos
EMpulse Spring 2019
9
COMMITTEE REPORTS
EMS/Trauma
By Christine Van Dillen, MD, FACEP EMS/Trauma Committee Chair
Emergency medical services around the state continue to fight Influenza, battling with high call volumes and the havoc it leaves behind. The week of December 22 was when the Centers for Disease Control (CDC) reported that influenza was widespread across the state, but it wasn’t until February 23 that influenza was considered widespread across the entire U.S. The CDC expects flu activity to remain elevated for a number of weeks. Florida temperatures are rising, and so are outdoor activity levels and heat-related illness incidents. Emergency medical personnel can educate and assist their community on how to prepare for these upcoming hot summer days. Initiate proper hydration days before any outdoor event, stay cool and hydrated during an outdoor event, use evaporative cooling (mists) to help cool off and take frequent breaks. Here comes the heat!
FAEMSMD UPDATE
January 24, 2019 was our last meeting. We started by congratulating Dr. Joe Nelson on his 14 years of service to Florida as State Medical Director. He has dedicated his life to EMS and remains active as a medical director and emergency physician. Thank you, Dr. Nelson! Dr. Ken Scheppke presented numerous goals he foresees for EMS in Florida as he steps into his role as State Medical Director. We discussed the strengths of FAEMSMD, which included the potential for an annual dataset, ability to establish standards of care, and significant source of expertise to advise legislators and policymakers. Dr. Scheppke is also very passionate about ending the opiate crisis that continues to attack Florida and the U.S. as a whole. His proposed state10
wide initiatives include:
• Educate EMS, nurses and physicians
• Follow data with EMSTARS and heat mapping
• Develop database of legitimate treatment centers
• Centralized addiction stabilization facility • Project Leave Behind
For questions or resources on how you can help end the opiate crisis, please contact Amanda Muller, DCF Overdose Prevention Coordinator, at Amanda.Muller@myFLfamilies.com. Dr. Scheppke presented a review of innovative strategies on out-of-hospital cardiac arrest (OHCA) care. These included heads up CPR, focusing on compressions rather than medications, devices that assist in CPR (thoracic pump), dispatch-led CPR, bystander CPR, resuscitations centers, hypothermia post arrest, ETCO2 as a marker of viability, CPR as a bridge to the catheterization lab, data collection, and establishment of best practices. ROSC Rates Proposed Statewide Initiatives:
• Pre-Hospital Initiatives • Post Resuscitation Initiatives • Data Monitoring for CQI • Quarterly Resuscitation Symposium
CARES
The Cardiac Arrest Registry to Enhance Survival (CARES) was established as a collaborative effort by the CDC and Emory University to create an efficient system to collect and report cardiac arrest. CARES is a secure HIPPA internet application that tracks cardiac arrests from 911 dispatch, EMS and hospital outcomes. CARES provides a uniform data collection EMpulse Spring 2019
tool that measures cardiac arrest and ROSC rates following the Utstein template for cardiac arrest. EMS agencies and hospitals will have the ability to measure their performance, which will help them identify inefficiencies and potential areas of improvement. Hospitals and EMS agencies are actively signing up with 6 million Floridians covered to date. DCF has a new CARES Coordinator, Mr. Thomas DiBernardo, who can be reached at Thomas.DiBernardo@flhealth.gov.
HURRICANE REVIEW
Dr. Scheppke led a panel discussion on Lessons Learned During Hurricane Michael Response and Recovery. Panelists included Edward Badamo, MBA, paramedic, who is the Operations Manager at American Medical Response Orlando; Brad Elias, MD, who is the Patient Movement Director at Florida Department of Health; Chief Michael Ragone from the Office of Emergency Management at American Medical Response; and John Wilgis, MBA, RRT, who is the Director of Emergency Management Services at the Florida Hospital Association. ■
The Future of EMS We’re thrilled to introduce next year’s EMS fellows: ORANGE COUNTY Dr. Amy Souers UNIVERSITY OF FLORIDA Drs. Alicia Buck and Alison Leung UNIV. OF SOUTH FLORIDA Dr. Andrew Smith
CLINCON THE PREMIER EMS CONFERENCE
& BILL SHEARER ALS/BLS COMPETITION
July 17-19, 2019
DoubleTree by Hilton—Universal Studios Orlando, FL
WEDNESDAY AGENDA:
THURSDAY AGENDA:
FRIDAY AGENDA:
LECTURES & SKILLS
LECTURES & SKILLS
LECTURES & SKILLS
Sal Silvestri Key Note: How Ultrasound Can Help Save Lives
Richard Slevinski Key Note: The Future of EMS Kenneth Scheppke, MD
Javier Rosario, MD, FAAEM & Leoh León, MD
ECG Case Studies: Lessons that Can Save Lives
Sports Medicine Emergencies in EMS
John O’Brien, MD, FACEP
Seth Smith, MD & Jason Zaremski, MD
On the Flip Side: Position Ventilation in Transport
Skills Lab: The Pregnant Patient: OB Complications & Abnormal Deliveries Ayanna Walker, MD & Christine Van Dillen, MD, FACEP
Skills Lab: Ultrasound Jason Jones, MD
EVENTS Opening Ceremony: 12:30 pm
Jon C. Inkrott, RRT, RRT-ACCS
Tips & Tricks for Blue & Barely Breathing Baby Christina Bailey, RRT, NPS & Danielle Nelski, BSN, RN, C-NPT
Should We Push Dose (Pressors) Out The Door?
Holly Ringhauser, DO
Are You Ready for Tachycardia? Bob Page, M.Ed., NRP, CCP, NCEE
How EMS can Use Telehealth for Addiction Care Chief Richard Ellis & Lauren Young, LCSW
TBI & ICP: the Pressure is On
David Olvera NRP, FP-C, CMTE
Identifying & Treating PTSD, Depression & Suicide in Emergency Medicine & First Responders
New HazMat Medical Protocols for Florida
Todd Husty, DO, FACEP
Ventricular Antiarrhythmatics: Ideal Selection Ivan Rios, EMT-P, CC-P
State EMS Awards Ceremony
Maternal & Neonatal Emergencies: Managing the Maladies of Pre-Hospital Care Danielle Nelski, BSN, RN, C-NPT, Rachel Hinkle, MS, RNC-OB, C-EFM
Ketamine Use in Airway Management Ivan Rios, EMT-P, CC-P & Justin Krantz, EMT-P, CCEMT-P
emlrc.org/clincon
Advanced Hemorrhage Control
Bob Page, M.Ed., NRP, CCP, NCEE
Exhibit Hall Reception
Find the full schedule & register online at
EMS to ED Hand-off: Touchdown or Fumble? Victor Quinones, M.S., PA-C, EMT-P & Raymond Hilton, MMSc, PA-C
“You Want Us to Transport What?” Concepts in Mechanical Circulatory Support Made Easy Ryan Dale, MSN, RN, CFRN, EMT-P
EVENTS ALS/BLS Preliminaries (closed to public) EMpulse Spring 2019
Richard Stilp PM, RN, MA, FPEM
Air Medical Advance Airway & Ventilation Carlos Tavarez, RN, EMT-P
Not If, but When…How to Plan for the Unknown Gary Schindele, FF/EMT & Juan Atan, MS, EMT-P
Skills Lab: Advance Airway & Ventilation Sonny Weishaupt, FF/PMD
Skills Lab: Extrication Richard Stilp PM, RN, MA, FPEM
EVENTS ALS/BLS Competition Finals (open to public) ALS/BLS Competition Awards Ceremony Totally 80’s Social 11
COMMITTEE REPORTS
Pediatric Committee By John Misdary, MD, FACEP Pediatric Committee Co-Chair
EDUCATION
Since 2014, the Pediatric Committee’s efforts have largely been oriented towards education. This has not changed for 2019, and the committee has two exciting educational opportunities lined up for the coming months. First, members of the committee will be putting on a pediatric emergency medicine (PEM) workshop at the 2019 Emerald Coast Conference (formerly Southeast ACEP Section Conference) in Destin, FL on June 3-6, 2019. The PEM workshop is part of the pre-conference and is scheduled for June 2 from 1:00-5:00 pm. This immersive three-hour program will focus on neonatal emergencies, and includes an update on the latest neonatal resuscitation guidelines and hands-on practice with high-fidelity simulators. Second, following the success of the 2017 and 2018 Symposium by the Sea PEM workshops, Pediatric Committee members will be conducting another PEM workshop at Symposium by the
By Todd Wylie, MD Pediatric Committee Co-Chair
Sea 2019. This PEM workshop will focus on pediatric trauma. A sincere “thank you!” to Dr. Shiva Kalidindi and Dr. John Misdary for organizing both programs.
FLORIDA PEDREADY
The Pediatric Committee is very excited to be participating in the Florida PEDReady collaborative. To understand Florida PEDReady, a little background is necessary. In 2013, multiple national organizations—including the U.S. Health Resources & Services Administration (HRSA), national EMSC, ACEP, AAP and Emergency Nursing Association (ENA)—launched an ongoing quality improvement initiative to ensure pediatric readiness in emergency departments around the country. A product of this initiative includes the recently published guidelines, “Pediatric Readiness in the Emergency Department,”1 which Dr. Madeline Joseph introduced in the last edition of EMpulse.
Want pediatric news delivered to your inbox? Subscribe to the FL PEDReady Pe2arl: an enewsletter dedicated to pediatric emergency education, advances, research & literature
SCAN TO SUBSCRIBE or visit bit.ly/FLpearl
12
EMpulse Spring 2019
In Florida, the state EMSC has identified the initiative as Florida PEDReady and has partnered with EMLRC to host the Florida PEDReady website. The FCEP Pediatric Committee will primarily serve as a content resource for the website, help identify educational opportunities, and assist in the production of the Florida PEDReady Pe2arl of the Week (Pediatric Emergency Education, Advances, Resources and Literature). Please visit the website at emlrc.org/flpedready for more information and many valuable resources, and sign up for the Pe2arl of the Week newsletter, debuting very soon. ■
REFERENCES
1. Remick K, Gausche-Hill M, Joseph MM, Brown K, Snow SK, Wright JL; AAP Committee on Pediatric Emergency Medicine and Section on Surgery; ACEP Pediatric Emergency Medicine Committee; ENA Pediatric Committee. Pediatric Readiness in the Emergency Department. Pediatrics. 2018 Nov; 142: e20182459. Access at bit.ly/ pedsguidelines2018.
COMMITTEE REPORTS
Membership & Professional Development By René Mack, MD, RDMS, FACEP MPD Committee Co-Chair
Congratulations to all of the medical students whose countless hours of dedication to their craft and passion crested on March 15 with Match Day 2019. For the 2019 NRMP Match, 2,488 PGY-1 EM positions were offered nationwide and 98.8% were filled at the conclusion of the Match. This is compared to the 2015 NRMP Match offering 1,821 PGY-1 EM positions nationwide with a 99.6% fill rate. There are many inferences and conclusions that can be drawn from the results of the Match, and one of them is that the field of emergency medicine is growing... quickly! If you are a practicing (or retired) emergency physician, your voice is needed to help mentor and facilitate the transfer of knowledge to the upcoming generation of healthcare leaders. Please contact the FCEP office for information on how to join our Medical Student Mentorship Program. As we celebrate and welcome this new group of physi-
Emergency Medicine on the Seas Updates in Emergency Medicine
CME Cruise
February 22-29, 2020
7 night Eastern Caribbean Cruise Norwegian Breakaway Ǧ Port Canaveral, FL For more information, visit
EMOnTheSeas.com
cians, we must also stay vigilant in protecting ourselves and each other from the many seen and unseen burdens of our chosen and beloved profession. Over the years, increased attention—and rightfully so—has been brought to wellness and burnout within our profession. These are buzz words that essentially speak to various methods of protecting your mental health and ensuring your continued professional success. As such, ACEP Wellness Week is April 7-13, 2019 and has numerous activities aimed at providing tools for navigating these sometimes turbid waters. By the time you receive this issue of EMpulse, the week will have already passed, but the sentiment of the celebration is long lasting. The basic premise is to take the time to enjoy the non-clinical activities that give you joy. Have you enjoyed personal (alone) time today? Have you spent uninterrupted time with friends/family this week? Have you exercised/meditated in the past week? If your answer to any of these questions is “no,” please strongly consider implementing at least one of these activities into your regular self-care routine. Unfortunately, the rise of wellness events correlates with the increase of physician suicides over the past 10 years. Physician suicide takes the life of approximately 400 doctors each year, which equates to more than 1 per day; comparatively, this is more than double the suicide rate of the general U.S. population. In February 2019, I learned that a fellow Florida EM physician, Dr. Shawn Prakash, took his life. He was a respected member of our community and his death brings so many questions and a sense of loss that is at times difficult to explain. I, and those who knew Shawn, mourn him and contemplate the circumstances that led to him taking his life. If you are having any concerns with any myriad of stressors (personal, clinical, financial, etc.) or have contemplated suicide, please, ask for help. If you notice that a colleague is struggling, please, reach out. We deserve the best from each other. FCEP and ACEP are dedicated to promoting and supporting our mental health and have various methods of assistance available for distribution and easy implementation. You can find more information on various wellness strategies on ACEP’s website. Our next committee meeting will take place at the FCEP office on May 22, 2019. I hope to see you there, or at least speak with you on the conference line. Take care of yourselves, and each other. ■
EMpulse Spring 2019
13
COMMITTEE REPORTS
EMRAF President’s Message By Misty Coello, MD, PGY-1 EMRAF President • FCEP Board Member
By the time you are reading this, Emergency Medicine Days 2019 has come and gone. This year we had more than five programs represented, included residents, fellows, program directors, and even fourth-year students who came to Tallahassee during Match Week (many of whom found out they matched into EM!). However, our plans and goals are far from finished. It was at EM Days, working among EM leaders, that my eyes were opened to the truth of medicine and politics. We come every year to advocate for our specialty, for patients and their safety. However, we are not on the forefront and vanguard of medicine; we are just reactive to the changes happening around us, solely advocating for whether we agree or not, and for whether those changes are safe for patients. It is for that reason that I not only encourage you to support and participate in these events, but myself and the EMRAF committee have established that
“
It was at EM Days, working among EM leaders, that my eyes were opened to the truth of medicine and politics... we are not on the forefront and vanguard of medicine; we are just reactive to the changes happening around us, solely advocating for whether we agree or not, and for whether those changes are safe for patients.
there is a need. I am proud to announce that we will be expanding EMRAF, and one of our goals is to create an advocacy executive position. If you are interested, please email me. Congratulations to the now 17 programs on matching the incoming Class of 2022! Florida has seen and continues to see our field expand. It is for that reason that we will be cre-
by the
ating a platform where all residents can communicate and learn about incoming opportunities. Our goal in EMRAF continues to be to empower residents in the field of emergency medicine. Another goal is to create more events for residents to participate in during Symposium by the Sea. We are currently in the discussion of creating an ultrasound competition. If you or any of your ultrasound directors are interested in participating, please reach out to me at the email above. We are looking for any type of involvement, from teams participating in the competition, volunteers, and individuals willing to be part of the planning committee or judges. Residents, if there are any topics or aspects within residency or emergency medicine that you would like EMRAF to address or engage, or if you interested in any of the positions mentioned, please contact me at mistycoello@gmail.com. ■
201 9
August 1-4, 2019 | Boca Raton, FL BOOK YOUR HOTEL ROOM: Boca Raton Resort & Club, A Waldorf Astoria Hotel 501 East Camino Real, Boca Raton, FL 33432 Room Rate: Starting at $190/night* Parking: $20/day valet Reservations: 1-888-543-1277 Group/Event Name: Symposium by the Sea
REGISTRATION OPENS THIS MONTH • www.emlrc.org/sbs 14
EMpulse Spring 2019
PHYSICIAN AND LEADERSHIP OPPORTUNITIES NORTH FLORIDA ■ Gulf Coast Medical Center Panama City
■ Sacred Heart Hospital Pensacola
■ Indian River Medical Center Vero Beach
CENTRAL FLORIDA ■ Oak Hill Hospital Brooksville
■ Citrus Memorial Hospital Inverness
■ Ocala Regional Medical Center Ocala
LEADERSHIP OPPORTUNIITES
■ Largo Medical Center Tampa Bay
■ Temple Terrace Free Standing ED
■ Northwest Medical Center Ft. Lauderdale
Tampa
■ Tampa Community Hospital Tampa
■ Medical Center of Trinity Tampa Bay
■ Lawnwood Regional Medical Center Ft. Pierce
■ Plantation General Hospital Ft. Lauderdale
■ Millenia ER
■ Doral Freestanding ER
■ Osceola Regional Medical Center
■ Kendall Town and Country Free Standing ED
Orlando
Miami
■ Oviedo Medical Center
■ Raulerson Hospital
■ Central Florida Regional ER
■ JFK Medical Center
Orlando Sanford
Okeechobee
Orlando
Regional Medical Director and Staff Brandon and Brooksville
■ Broward Health Medical Center Ft. Lauderdale
Miami
Miami
■ Millenia ER
■ Brandon Regional Hospital and Oak HIll Hospital
■ Baptist Hospital of Miami
Orlando
Orlando
PEDIATRIC EMERGENCY MEDICINE OPPORTINITIES
SOUTH FLORIDA
■ Baldwin Park ER Orlando
■ Baldwin Park ER
■ Osceola Regional Medical Center Orlando
■ Gulf Coast Medical Center Panama City
■ Palms West Hospital Wellington
West Palm Beach
■ Brandon Regional Riverview Freestanding ED Tampa Bay
COAST-TO-COAST FULL-TIME, PART-TIME AND PER DIEM OPPORTUNITIES FOR MORE INFORMATION, CONTACT: 877.226.6059 success@evhc.net
ASK ABOUT OUR EMBASSADOR TRAVEL TEAM OPPORTUNITIES
COMMITTEE REPORTS
Medical Student Committee By Kimberly Herard, MD Candidate, FAU Class of 2020 Medical Student Committee Secretary-Editor
As emergency medicine rapidly grows into an important medical specialty, EM Days in Tallahassee is an important opportunity to participate in the advocacy needed to protect patients in the ED, emergency physicians and emergency medicine as a whole. Emergency physicians provide 67% of healthcare to the medically uninsured and 50% of care to Medicaid and CHIP pediatric patients. Emergency medical care is expensive, and it’s difficult to cover costs because many patients do not have insurance and limitations on physician reimbursements do exist. EM Days is therefore a unique and powerful conference put in place to help support and protect emergency physicians and the millions of patients they serve. The many policies being discussed and voted on by Florida legislators will impact emergency physicians now and all of us students not yet in the workforce. Therefore, students all over Florida decided to join physicians at the state Capitol to help support and strengthen the discussions and advocating done to protect patients and the emergency physicians that serve them. Medical students attending the conference in Tallahassee had the opportunity to learn about a variety of relevant topics within emergency medicine. Topics discussed include opioid addiction, prescription drug monitoring, and Medicaid management—all of which greatly affect patients and emergency physicians in the ED. During the conference, students also had the exciting opportunity to see advocacy at work: by accompanying physicians on legislative visits!
16
“
As we hope to join the EM workforce in the future, it is important to be aware of legislation that will impact our future care of patients. It is also important to know that positive change is possible as long as we remain an important piece of the discussion.
One important bill that was discussed and supported by FCEP was “Insurance Coverage Parity for Mental Health and Substance Use Disorders.” This legislation is extremely important considering the current opioid epidemic: it will ensure that insurance covers the cost of substance use and mental health treatment. Medical student and EM Days attendee Tori Ehrhardt says, “the most impactful activity I participated in was attending a legislative visit discussing the expansion of the IDEA Exchange program in Miami,
FL. The opioid epidemic is a very personal topic for me and affects so many patients seen in the ED, as well as their loved ones. This program is an initiative that improves the health outcomes of those afflicted with substance use disorder and connects them to resources in the community designed to help them overcome their addiction.” Medical student participation in EM Days is extremely important. As we hope to join the EM workforce in the future, it is important to be aware of legislation that will impact our future care of patients. It is also important to know that positive change is possible as long as we remain an important piece of the discussion. Nicolas Ramsay, Medical Student Council Chair, says, “(Advocacy is) very important because changes in legislation will only occur if we point out the areas that need improvement. If physicians don’t advocate for the patients and for physicians, then legislation will cater to the groups that are advocating for themselves.” ■
FIU medical students at EM Days 2019. From left: Rishi Rane, M3; Jovans Lorquet, M3; Hannah Gordon, M4; Ilya Luschitsky, M3; Tori Ehrhardt, M2; Dr. Todd Slesinger, Aventura Program Director; Nicolas Ramsay, M3. EMpulse Spring 2019
UPDATES ON THE OPIOID CRISIS: FCEP Endorses MAT Induction in the ED as Best Practice On March 12, 2019, FCEP’s Board of Directors officially endorsed the initiation of medication-assisted treatment (MAT) in the ED for opioid use disorder (OUD) patients as a best practice, and strongly encourages physicians to obtain their X-waiver to better facilitate outpatient treatment. MAT induction in the ED allows emergency physicians to begin treatment while care management staff coordinate next steps to connect the patient with community treatment providers. This is especially critical when patients seeking help present during evenings and weekends when treatment providers’ intake hours are unavailable. Thus, a short duration prescription for buprenorphine is needed. While administering buprenorphine in the hospital or ED requires no special training or waiver, federal law currently requires physicians to obtain a DEA X-waiver to prescribe buprenorphine for outpatient addiction treatment. Physicians need 8 hours of online training, which covers pharmacology, the induction process for the drug and information about best practices. Modifying this cumbersome requirement is a priority for ACEP leadership, but until then, emergency physicians can take this course for free online. Demystifying addiction treatment goes a long way. The history of medicine is, in part, the history of physicians stretching the scope of their practice to answer the pressing needs of their times. We are in a culture shift—addiction treatment has not historically been part of emergency medicine care; however, like with any cultural change, emergency physicians can be the drivers of care for these patients outside of the ED, on the hospital wards and in the community. Normalizing this care in the ED will produce more willing and capable hospitalists, primary care doctors and outpatient care delivery systems for patients suffering with OUD. ■
CURRENTLY IN FLORIDA: Only
1,575
of
51,582
actively practicing physicians1
are X-waivered to treat OUD with buprenorphine Learn about how to apply for your DEA X-waiver here3
2
3%
Read a 2-page summary about how medications for OUD save lives4
EMS RESOURCES: All About Narcan (Naloxone)6 Locate a Naloxone Distribution Site7 Prescribe to Prevent: Naloxone Resources8 Harm Reduction Resources9 Contact Amanda Muller, DCF Overdose Prevention Coordinator, for more information & resources: amanda.muller@myFLfamilies.com
REFERENCES & LINKS 1. 2018 Physician Workforce Annual Report. Florida Department of Health. November 2018. Access at: www.floridahealth.gov/provider-and-partner-resources/ community-health-workers/ physician-workforce-development-and-recruitment/2018DOHPhysicianWorkforceReport-FINALDRAFT.pdf 2. Buprenorphine Practitioner Locator. SAMHSA. Access at: www.samhsa.gov/medication-assisted-treatment/practitioner-program-data/ treatment-practitioner-locator 3. Apply for a Practitioner Waiver. SAMHSA. https://www.samhsa. gov/medication-assisted-treatment/buprenorphine-waiver-management/apply-for-practitioner-waiver 4. Medications for Opioid Use Disorder Save Lives. National Academies of Sciences, Engineering & Medicine. March 20, 2019. Access at: nationalacademies.org/hmd/ reports/2019/medications-for-opioid-use-disorder-save-lives
Get Your X-Waiver—for Free Online
5. 8 Hour Online MAT Waiver Training. PCSS. Access at: learning. pcssnow.org/p/onlinematwaiver
Offered by: The Providers Clinical Support System (PCSS) is a coalition funded by the Substance Abuse & Mental Health Services Administration (SAMHSA) and led by the American Academy of Addiction Psychiatry (AAAP).5
Are you working on the opioid crisis? Interested in getting started? Let FCEP know by contacting sleague@emlrc.org.
ACCESS COURSE
EMpulse Spring 2019
6. www.narcan.com 7. Naloxone Locator. Access at: isavefl. com/locator.shtml 8. Prescribe to Prevent. Access at: prescribetoprevent.org 9. Harm Reduction Coalition. Access at: harmreduction.org
17
Congratulations to the
CLASS OF
2022 MATCH DAY 2019 RESULTS »
Brock Clark
Edward Via College
Zack Albaugh
Georgetown Univ.
Emily Clark
Oakland Univ.
Michael Hughes
William Daly
Univ. of Central Florida
Jyotirmoy Das
Univ. of Kansas–Wichita
Anthony DeRenzi
Univ. of Washington
James Lee
Univ. of Texas at Houston
USF Health
Marcos Marugan-Wyatt
Univ. of Oklahoma
USF Health
Univ. of Oklahoma
Jayden Miller
Louisiana State Univ.
A.T. Still Univ.
Andrew Nicholas
Orlando Health Bryce Bergeron
FSU–Daytona Beach
Greg Black
Bobby Butera
FSU at Sarasota Memorial Thomas Cox
Alexandria “Nykole” Griddine Brad Hamlin
Alexander Sterling
Brody Hingst
Univ. of South Carolina
Courtney James Mayo Clinic
Connor Karr
East Carolina Univ.
Lindsay Maguire Virginia Tech
Sophia Meziani
William Carey Univ.
Univ. of Central Florida
West Virginia School of Medicine
Mary Roberts
Michigan State Univ., Grand Rapids
Washington Univ. in St. Louis
Augusta Univ.
Darrell Ray
Kevin Raymond
Medical Univ. of South Carolina
Marshall Univ.
Jean Laubinger
James Neumeister Jonathan Rebik Jacob Ruzicka
Lake Erie College
Joshua Lehman
Talia Cola
Univ. of Illinois
Liberty Univ.
UF Jacksonville Chelsea Allen
Edward Via College
Liberty Univ.
Lake Erie College
Courtney Verboncoeur
Kendall Regional Medical Center Andrew Adams
Lincoln Memorial Univ.
St. George’s Univ.
Geoffrey Wade
Andrew Allen
St. George’s Univ.
Univ. of Minnesota
Melanie Worley
Ma Lovely Batasin (Maria)
Ohio Univ.
INAGURAL CLASS
William Carey Univ.
Caitlin Blackwell
Nneka Azih
Morehouse School of Medicine
Grant Barker Univ. of Miami
Richard Courtney
Nova Southeastern Univ.
Thomas Frauenhofer Alabama College
Francisco Gironza Michigan State Univ.
Kasondra Hartman
Augusta Univ.
Geisinger Commonwealth
Medical Univ. of South Carolina
East Carolina Univ.
Touro Univ. Nevada
Florida International Univ.
Nicolas Ellis
John Hurley
Florida International Univ.
Evelyn Ramirez
Florida Atlantic University
East Carolina Univ.
Pooja Sarin
Elizabeth Calhoun FSU
St. George’s Univ.
Lake Erie College
Univ. of Iowa
Medical College of Wisconsin
St. George’s Univ.
Midwestern Univ.
Eastern Virginia Medical School
Brown Univ.
Florida International Univ.
Alex Tymkowicz
Sean Ellis
Mani Hashemi Tyson Jackson
Spencer Greaves
Semir Karic
Katriin Kivilo
Jessica Ramos
Charles Updegrove
Rebecca Mendelsohn
Glen Malaret Hernandez
Alberto Romero
William Waite
Thomas Peterson
Amar Mittapalli
Ronya Silmi
Ali Syed
Collin Smith
Andrew Warren
Univ. of Puerto Rico Ross Univ.
Lake Erie College
Edward Via College, Auburn
Univ. of South Carolina
Stony Brook Univ.
Thomas Jefferson Univ.
Nova Southeastern Univ.
St. George’s Univ.
Jessica Wanthal
Yehuda “Hudi” Wenger
Sackler School of Medicine 18
UCF/HCA at North Florida Regional
UCF/HCA at Ocala Health
Michael Turchiaro
EMpulse Spring 2019
Kelly Wright
Mercer Univ.
Temple Univ.
Augusta Univ.
Parker Young
Lake Erie College
Aventura
Mount Sinai Florida International Univ.
Hannah Kim
UCF/HCA of Greater Orlando
Chase Hemphill
Leeran Baraness
Morgan Jensen
Jared Culp
David Nguyen
Midwestern Univ. Arizona
Thomas Jefferson Univ.
Ben-Gurion Univ. of the Negev
Nova Southeastern Univ.
John Choi
Univ. of Pikeville
Fayez Ajib
Nova Southeastern Univ.
Hannah Gordon
Palm Beach Consortium Des Moines Univ. Touro Univ.
USF Health
Edward Via College
Univ. of Virginia
Edward Via College
Florida International Univ.
Meharry Medical College
Philadelphia College
Univ. of Central Florida
Florida International Univ.
Georgetown University
St. George’s Univ.
Pacific Northwest Univ.
A.T. Still Univ. Kirksville
San Juan Bautista School of Medicine
Nova Southeastern Univ.
Univ. of Southern California
Gideon Logan
Jeremy Mayfield Parth Patel
Fernando Rivera Alvarez Mark Rivera-Morales
Ponce Health Sciences Univ.
Roger Sliney UF Gainesville
Jesse Wu
Univ. of Texas Medical Branch, Galveston
Jackson Memorial Hospital
Chia-Yuan Lee
Amir Hashemi
Grethel Miro
Jiodany Perez
Stefani Sorensen Paige Swalley
Dennis James
Osiris Johnson
Nathaniel Pearl
Benjamin Pirotte Kenneth Roberts Univ. of Miami
AdventHealth East Orlando
Trung Tran
Wayne State Univ.
Nicolas Ulloa
Yuchen Duan
Ross Univ.
Florida International Univ.
Richard Winters
Saleh Hasan
Univ. of Oklahoma
Northeast Ohio Medical Univ.
Ricardo Hernandez
Andrea Alvarado
San Juan Bautista School of Medicine
HCA West at Brandon Regional
Robert Barry
Michigan State Univ.
Touro Univ. Nevada
Anna Culhane
West Virginia School of Medicine
Lake Erie College
New York Medical College Stony Brook Univ. Univ. of Wisconsin
Ponce Health Sciences Univ.
Bryce Hoer
Annie Au
Tyler Mills
Dasha Dewberry
Joseph Ray
Justin Harris
Nicole Tobin Lam Tran
HCA West at Oak Hill Hospital Nicholas Bencomo St. George’s Univ. Dhiaa Daoud Ross Univ. Arun Malhotra St. Matthew’s Univ. Kyle Meggison Touro Univ. Joel Miller Philadelphia College Juan Diego Rondon St. George’s Univ.
UF Gainesville Manuel Borobia
Florida Atlantic Univ.
Carlos Garcia-Rodriguez
A.T. Still University
John “JP” Baker
Sebastian Gil
Ross Univ.
Graham Clifford
Univ. of Arizona
Jonathan Hill
Univ. of Virginia
Univ. of North Carolina
USF Health
Jordan Johnson
Philadelphia College
American Univ. of Beirut
Michael Buchko
Jordan Markel
University of Florida
Yuya Burkhart
Itnia Mustafid Pramanik
Eastern Virginia Medical School
Catherine Cantrell
Nushin Nataneli
Sarah Jabre
Lake Erie College
Warren Linnerooth
Univ. of Central Florida
Jennifer Okungbowa-Ikponmwosa
USF Health
Univ. of Wisconson Oakland Univ.
Oswald “Oz” Perkins
Univ. of Virginia
Bryan Hyman
USF Health
Ross University USF Health
David Kuai
Christian Padgett
Nova Southeastern Univ.
Michigan State Univ.
Meharry Medical College
Univ. of Science, Arts & Tech
USF Health
Lake Erie College
Miguel Ribe
Univ. of Eastern Virginia
Max Rippe
Univ. of Tennessee, Memphis
Cameron Shoraka
Univ. of Texas, Houston
Melissa Velazquez New York Univ.
Joseph Zakaria
Univ. of California, Irvine
Tiffany Pleasant Wesley Priddy
Jared Senvisky
Northeast Ohio Medical Univ.
Lawrence Seymour
Cecilio Padron
Kishan Nayan Patel
USF Health
Univ. of Illinois
Matthew Lindgren Texas Tech Univ.
Jonathan Liu
Kevin Rivera-Rodriguez
Univ. of Central Florida
Calixto Antonio Romero III
Ross Univ.
Ponce Health Sciences Univ.
Medical College of Wisconsin
American Univ. of the Caribbean
Univ. of Missouri-Columbia
Alabama College
Michael Weaver
Chelsea Crose
Jacinto Fernandez UF Health Shikerria Green
NY Institute of Technology
Wright State Univ.
Philip Plevek
Bradley Collins
Travis Weber
EMpulse Spring 2019
Nykia Porter
Zachary Stanton
Univ. of Mississippi
Brian Szczucki
East Tennessee State Univ.
Lake Erie College
USF Health
Pooja Mysore
Andrew Smith Nina Xue
Univ. of Vermont 19
Introducing
FLORIDA’S NEWEST
EMERGENCY MEDICINE RESIDENCY PROGRAMS HCA West at Brandon Regional (new!) By Rashmi Jadhav, MD, PGY-1
The Brandon Regional Hospital EM Residency Program is well into its inaugural year and we have hit the ground running! The year has been filled with many fun events, noteworthy accomplishments by residents, and steadfast dedication from faculty in molding this program and each of its 15 residents into strong physicians. In conjunction with the Oak Hill Hospital EM Residency Program, we kicked off our first month with an intense, hands-on boot camp. This consisted of high-yield lectures, hands-on simulations for ultrasound, venous access, airway management, resuscitation and much more. This initial month of residency rapidly projected us into the EM mindset. Along with prepping for the in-training exam through weekly conferences, practicing for oral boards and hosting resident-run lectures, we also began the “Save of the Month” to highlight commendable medical management by our residents. Our conferences have been steered by residents and truly cater to our needs as we progress through our training.
staple of emergency medicine, we are fortunate to have ultrasound-fellowship-trained Dr. Eric Kalivoda leading the ultrasound program. We’re also elated to have Dr. Nicholas Governatori on as core faculty, who has advanced training in medical education and has been an invaluable asset as we navigate through clinical and educational aspects of residency. In fact, all of our faculty have been strong advocates of research and continued education. Their enthusiasm and support led Dr. Caroline Trippel, PGY-1 to publish a case study titled “Rupturing Thoracic Aortic Aneurysm” in EM Resident Magazine. Additionally, Brandon Regional Hospital competed in the EMRA Quiz Bowl hosted by CORD in Seattle, WA this March. We are very excited about the
As bedside ultrasound has become the
20
EMpulse Spring 2019
accomplishments of our residents and program thus far. Along with hard work comes some time to play and have fun. We recently had an exciting Wellness Day that featured an energetic day of laser tag. Our faculty certainly stress the importance of wellness, and there was no better time than after the in-training exam. As we progress into the second year of our program, we eagerly await the entrance of our next class of interns. We were pleased to meet so many exceptional candidates who shared such a sincere passion for emergency medicine. We look forward to welcoming 15 new residents into our rapidly progressing residency program. ■
17 EM
FSU at Sarasota (new!) By Kelly P. O’Keefe, MD, FACEP Program Director
Greetings from Sarasota Memorial & the FSU COM EM Residency program! All is going well as we eagerly anticipate the start of our program in July. I would like to take this opportunity to introduce our core clinical faculty. We were quite fortunate to be able to fill a number of faculty positions with existing members of the group, while bringing in outstanding physician educators from other locations as well. Dr. Sarah Temple is the Associate Program Director and ably assists me in the overall management of the residency. Our Research Director, Dr. Sagar Galwankar, has an international reputation, and will undoubtedly make many major contributions here. Dr. Ashley Grant heads our excellent emergency ultrasound instruction. Simulation training is enthusiastically led by Dr. Rose Goncalves and Dr. Steve Kamm, who will also lead our wellness initiatives. Dr. Wes Ruffin is our very capable Director for Emergency Pediatrics training. Dr. Ryan
RESIDENCY PROGRAMS Snitowsky will educate our lucky residents in all aspects of CQI & Patient Safety. Dr. Marshall Frank is our EMS Director, and Dr. Tamas Peredy will share his expertise as our Director of Toxicology. Dr. Julio Arrieta, an FSU COM alumnus, is our Medical Student Clerkship Director. Finally, Dr. Joel Gerber, CEO of our physician group, and Dr. Reuben Holland, our Medical Director, will handle Leadership Development, instruction in the business of EM, and medical-legal aspects. I am very happy to announce that our Hospital Foundation recently made a generous donation of $400,000 to the residency for the development of our simulation center. This will get us off to a great start! Finally, I would like to recognize Dr. Holland for his tireless efforts in the benefit of our ED and hospital. As a result, he is Sarasota Memorial’s Physician of the Year. ■
HCA West at Oak Hill (new!)
Our growth has included developing a simulation center, planning an ED expansion, hiring two more faculty members and so much more. We are also working on a variety of projects including sepsis treatment protocols, EMS practices across the country and interesting case reports. We also
JACKSONVILLE • UF, Jacksonville GAINESVILLE • UF, Gainesville • UCF/HCA at North Florida Regional OCALA • UCF/HCA at Ocala Health
Central Florida: BROOKSVILLE • HCA West at Oak Hill Hospital TAMPA • HCA West at Brandon Regional • USF Health ORLANDO • Orlando Health • AdventHealth East Orlando • UCF/HCA of Greater Orlando
By Jonathan Yaghoubian, DO, MS & Corey Cole, DO, PGY-1s We are excited to be the inaugural class at Oak Hill Hospital’s new EM program. The hospital has been very welcoming as we successfully navigate through our first year. As the first class of a brand new program, we can say that we have experienced a variety of emotions ranging from excitement to fear, but know our attendings and staff have our backs.
North Florida:
recently participated in an “intubation rodeo” for the local EMS services. Our program director, Dr. Alfredo Tirado, has been an integral part of building our program and our success. His background in ultrasound as well as his involvement in launching other programs has been a great asset to our growth. We greatly appreciate all of his hard work. As our first year wraps up, it will be exciting to see how our program continues to be shaped. Transitioning from interns to seniors will be a big step, but our faculty will always be there for us. ■ EMpulse Spring 2019
SARASOTA • FSU at Sarasota
South Florida: PORT ST. LUCIE • Palm Beach Consortium at St. Lucie BOYNTON BEACH • FAU Charles E. Schmidt COM MIAMI • Aventura Hospital • Jackson Memorial Hospital • Kendall Regional Medical Center • Mount Sinai 21
CENTRAL FLORIDA
UCF/HCA of Greater Orlando By Andrew Hanna, MD, PGY-2 & Amber Mirajkar, MD, PGY-1
We are proud to announce that we have reached continued accreditation by ACGME. These past few months, we saw many great medical students both interviewing and rotating through our program. We look forward to welcoming our new members. In ED leadership news, we welcomed Dr. David Lane as Director of the ED. He comes from MedStar Georgetown University Hospital in Washington, D.C., and we are very excited to work with and learn from him. We are also happy to announce the promotions of Dr. David Lebowitz to Program Director and Dr. Tracy MacIntosh to Associate Program Director. Although we are sad to be losing the senior and inaugural class, our PGY-3s have bright futures ahead of them. Drs. Leoh Leon and Aman-
da Webb will be staying with us as fellows in ultrasound and research, respectively. Drs. Amninder Singh and Adam Benzing will be pursuing EMS fellowships at UT San Antonio. Dr. Abhishek Roka will also be going to UT San Antonio to complete a fellowship in combined ultrasound/global health. Dr. Nicholas Kramer will be joining the Envision Healthcare Ambassador Team, and Dr. Rolando Cabrera will be with TeamHealth in West Palm Beach. Congratulations to all of our PGY-3s! With burnout rates unfortunately high in emergency medicine, we try to incorporate wellness frequently. Whether it be a Women in Emergency Medicine dinner or bowling after the in-service exam, mental health and relaxation is an important part of being a well-rounded physician. Since medicine is a team sport, we also
coordinate wellness activities such as painting and innertubing with other specialties. In the realm of research, our residents continue to thrive, and we are excited to have multiple residents and faculty accepted to speak at SAEM. Our PGY3s and PGY-2s will have six abstracts and three didactic presentations with topics ranging from gender differences in subarachnoid hemorrhage and prehospital sepsis to double sequential defibrillation. We look forward to representing Florida at the conference. On behalf of all members of our residency program, we hope everyone is having a wonderful start to the new year. We are grateful for the opportunity to serve and learn from the community of Central Florida and advance the field of emergency medicine. â&#x2013;
EMERGENCY MEDICINE HOSPITALIST URGENT CARE
A Holistic Approach to Revenue Cycle Management: Physician Education MIPS/Managed Care Business Intelligence Dedicated Support
Ask us about a Free Analysis Gottlieb Half Pg Ad.indd 1
3/4/19 11:04 AM
CENTRAL FLORIDA
Orlando Health
By Laura Cook, MD & Anne Shaughnessy, MD, PGY-2s In March, we took time to celebrate the life of Dr. Sal Silvestri with the annual Salvatore Silvestri Memorial Ballgame, attended by residents, faculty, staff and many alumni. We continue striving to #LivelikeSal and remember how Dr. Silvestri’s love and passion for emergency medicine shaped ORMC during his memorable time as program director. Match Day came and went, and we cannot wait to welcome our new intern class. We had a great interview season and enjoyed meeting so many wonderful candidates along the way. ORMC EM participated in the annual Quality Retreat in March, and it was exciting to see research presented from all PGY classes as well as many of our fellows. Congratulations to our
new Chief Residents, Drs. Laura Cook, Brian Guetschow and Margaret Stutsman, and our Chief Quality officers, Drs. Mitch Barneck, John Kennedy and Katie Pearson. Additionally, we are happy to announce that four of our incredible seniors will be pursuing fellowship this year. Dr. Amy Souers will stay with ORMC as an EMS fellow, and Drs. Steven Ritchey and Lisa Cook as ORMC ultrasound fellows. Dr. Dallas Joiner will start her critical care fellowship in Miami and we wish her the best of luck! In April, we have several residents and fellows participating in and presenting research at the CORD Academic Assembly in Seattle. We hope to see some of our fellow EM Floridians there! ■
AdventHealth East Orlando
By Shannon Armistead, DO, PGY-2 Greetings from AdventHealth East Orlando, formerly Florida Hospital. In January, we underwent a name change to signify our part in the greater whole of the Adventist Hospital System. Confusing as it was for some, the change in name did not lessen the quality of our care. As a residency, we came together to celebrate the collective efforts of the academic year thus far during the holiday season and cherished the opportunity to thank our hardworking faculty and clinical attendings for all they do when guiding us through our educational journey. The early months of 2019 heralded the rapidly approaching “rank list” sea-
son and the excitement that comes with planning for our next class. After rigorous hours of study and multiple review lectures with more Rosh questions than we thought possible, the in-training exam is complete for another year. We then participated in our Annual Program Evaluation in hopes of continued evolution and effort in improving each part of our residency experience. Congratulations to all of our matched residents! Our interns are transitioning into “taking over” some of the educational responsibilities during shift sign out and conference as our seniors edge closer to graduation. ■
EMpulse Spring 2019
USF Health
By Matthew Beattie, MD, PGY-2
Spring is an exciting time of the year! Most of our seniors have jobs lined up and are ready to step out on their own in July. As one group prepares to move on, we get the opportunity to welcome another. Match Day has come and passed and we are excited for our new group of interns to join us. One of the big events this spring was EM Days in Tallahassee. For those of you who have never attended, I encourage you to get involved next year or plan on attending the ACEP Leadership and Advocacy Conference this May. We worked alongside Florida’s leaders in emergency medicine to fight for issues that are currently being discussed in legislative session. Right now, there are bills that would allow pharmacists to take on the role of clinicians in order to diagnose flu and strep, and to make medication changes to “simple” conditions. There are bills trying to cap physician reimbursement at 200% of Medicare, and there are bills that would allow insurance companies to offer plans that do not include emergency care in their benefits. We spoke face-to-face with legislators about why these bills would be harmful to our patients if they were to pass. In addition, now that there are 17 residency programs approved in Florida, we discussed in the EMRAF meeting the possibility of setting up a more organized board structure. Start thinking of how you might like to get involved and contact Dr. Misty Coello, EMRAF President, at mistycoello@gmail.com. We get to work in the best specialty in medicine. Stay positive and keep doing your best! ■
23
SOUTH FLORIDA
Palm Beach Consortium at St. Lucie
Florida Atlantic University
By Blaire Laughlin, DO, PGY-3
By Jeff Klein, MD, PYG-2
First and foremost, I am proud to announce that the FAU Emergency Medicine core faculty have been awarded a $950,000 grant to further fund their prospective cohort study investigating primary and recurrent head bleeds in elderly patients on antiplatelets and anticoagulants. This not only represents the first major grant for clinical research awarded to our emergency medicine program, but also to all other residencies affiliated with FAU including internal medicine, general surgery, neurology and psychiatry. This project is expected to be completed June 2021. A special thank you to all core faculty for their hard work! Over these past three months, we have had the pleasure of hosting several noteworthy Grand Rounds speakers. The list of speakers includes Dr. Ken Butler from the University of Maryland who spoke on “The Trauma Patient in a Non Trauma Center;” Dr.
Neeraja Kairam from Goryeb Children’s Hospital who lectured on “Risk Management in the Pediatric ED;” and Dr. Richard Amini from the University of Arizona speaking on the “Top Ten Ultrasounds for the Community EM Doc.” Our academic experiences over this timeframe have been further enhanced through our monthly simulation cases coordinated by our simulation director, Dr. Patrick Hughes. These cases have included thrombotic thrombocytopenic purpura, iron overdose and cyanide toxicity. Although a dynamic and engaging curriculum is always part of our program, our monthly wellness activities continue to promote mental health and have included miniature golf, a day at the beach, and a food tour of the famous Atlantic Avenue in Delray Beach. In closing, congratulations to everyone for making it through the inservice exam and interview season! ■
Daunting Diagnosis: A « CONTINUED FROM PAGE 8
This MRI shows a 5x6x6cm encapsulated mass with extension into the left middle cranial fossa, suggestive of a giant facial nerve schwannoma. The patient’s symptoms mimicked Bells Palsy, but in fact, her diagnosis was much more ominous. The patient was subsequently treated by ENT
24
and Neurosurgery for which she underwent a craniotomy with left neck exploration and resection of the tumor. In cases with persistent, progressive symptoms such as this case, further exploration with labs and imaging is warranted. ■
EMpulse Spring 2019
Match results are in! We are excited to welcome the class of 2022: John Choi, Chase Hemphill, Morgan Jensen, David Nguyen, Nicole Tobin and Lam Tran. Our current residents recently came together to volunteer at the Treasure Coast Marathon. Upcoming events include Residents Day Out and SimWARS. In March, St. Lucie hosted the South Florida Emergency Medicine Grand Rounds at Nova Southeastern. Special thanks to guest speaker Alexis LaPietra DO, FACEP, FAEEM for her lecture on “Alternatives to opioids for pain management in the ED.” Dr. Michael Gulenay, PGY-3 is currently doing an anesthesia elective to continue expanding the use of US for nerve blocks and pain management. As we prepare to say goodbye to our PGY-4 class, we are looking forward to their last lecture series as inspired by Randy Pausch. We’d also like to extend a special thank you to our Chief Resident, Jessica Chambers. ■
SOUTH FLORIDA
Kendall Regional Medical Center By Stefan Jensen MD, PGY-3
It has been a season of change and joy here at Kendall Regional. We invite you to join us in celebrating the birth of Aaron Scott Napier, son of Dr. Andrew Napier, PGY-2, and Mila Bora Moreno, daughter of Dr. Moises Moreno, EUS Director. In addition, Chief Resident Dr. Pavel Antonov got married to Dr. Francisca Valenzuela on January 19, 2019. We would also like to welcome our new Program Director, Dr. Emilio Volz. We thank Dr. Kevin King for his incredible contributions to our program and for laying a solid foundation from which we can move forward. We wish him well in his future endeavors. As the second half of the year is upon us, we are very much focused on making sure our third-year residents
are prepared to take on the additional responsibilities of attending emergency physicians. We are very excited to prepare for our futures at wide-ranging clinical practices in Florida, Texas, Arizona, Pennsylvania and elsewhere. In three short years, we have seen Kendall expand from a community ED into a fully-staffed academic department. We welcome students from all over the country and assist in the training of our hospital’s internal medicine, transitional year and anesthesia residents. It has been an honor to be present at this dramatic expansion of the program. Growing into our clinical practice during these changes has been a tremendous learning opportunity that we will take with us through the rest of our career as physicians. ■
By EM Residency Staff
Our PGY-2 class and faculty members attended the annual AAEM conference this March in Las Vegas. We enjoyed supporting our many students, residents and faculty who presented their research at this great conference. Having finished a grueling but exciting recruitment season, we were excited
By Michael Cecilia, DO, PGY-3
This past winter was an extremely exciting time for our residency. We are excited to announce the opening of our long awaited, new state-ofthe-art emergency department and accompanying surgical tower. Our new 34,000 sq. ft. department boasts 56 private treatment rooms, dedicated lab and CT in the ED, and some of the best views of Biscayne Bay in the entire city! In addition, Mount Sinai was proud to host the Miami Beach Resuscitative TEE Workshop on February 16, 2019. We would like to thank our Ultrasound Director, Dr. Mark Newberry, for his continued efforts in growing our residency’s ultrasound program. In other news, we are pleased to announce that our ED Chairman, Dr. David Farcy, was honored by the Miami Beach Chamber of Commerce during its annual Heroes Breakfast. Dr. Farcy was presented with an award in recognition of his significant contributions to maintaining and improving the quality of prehospital medical care and disaster medicine in Miami Beach.
Jackson Memorial Hospital We have survived Miami winter so far! There were a few days in the 50s, but we managed to pull through and eagerly await the beautiful spring weather of South Florida.
Mount Sinai Medical Center
to learn which talented individuals will be joining us. We are also preparing for the class of 2019’s graduation. We have an amazing group of residents and will be sad to see them go. Six residents are heading into fellowships in toxicology, palliative care, EMS, neurocritical care and hyperbarics. The remaining 10 residents are heading into a mix of academic and community careers throughout the country. We are excited to see them head off and start their careers as colleagues in EM, but not ready to have them leave quite yet. ■ EMpulse Spring 2019
Lastly, we are very excited with the number of events coming up this spring. We are looking forward to taking part in the eighth Annual FLAAEM Scientific Assembly on May 10-11, 2019, which will be held right here in Miami Beach. We are also excited to announce that South Florida Wilderness Medicine will be holding its second annual Advanced Wilderness Life Support Course at Mount Sinai on April 12-14, 2019. ■
25
SOUTH FLORIDA
Aventura Hospital & Medical Center By Scarlet Benson, MD Assistant Clinical Professor
We had a very successful interview season and look forward to welcoming a new intern class! We had 1,000 applicants and completed 120 interviews. We were also recently approved to increase our incoming class to 12 residents. Our faculty continue to impress with their academic achievements:
• Assistant program director Dr.
Andy Pennardt published an article in 2018 titled, “The Emergence and Evolution of the Journal of Special Operations Medicine: An Interview with Publisher Michelle Landers”
• Ultrasound director Dr. Huy Tran
co-wrote an article published this year in CJEM titled, “The diagnostic accuracy of a point-of-care ultrasound protocol for shock etiology: A systematic review & meta-analysis”
• Simulation director Dr. Jessica
Cook delivered an MCI drill as a course at the IMSH simulation conference in late January in San Antonio, TX. She also co-presented
a course called “Evaluation made simple: checklists, global rating scales, milestones and competencies” with former Yale colleagues at the same conference for the second year running
• Program director Dr. Todd
Slesinger published two articles in November 2018: “Intra-Arrest Induction of Hypothermia via Large-Volume Ice-Cold Saline for Sudden Cardiac Arrest: The New York City Project Hypothermia Experience” and “Urban and Rural Emergency Department Performance on National Quality Metrics for Sepsis Care in the United States”
The residents have also been highly successful in their own endeavors:
• Dr. Jenny Reyes presented her
poster, “Overcompensated ventriculoperitoneal shunt resulting in subdural hematoma and subarachnoid hemorrhage,” at the FOMA poster presentation at Nova in February with the supervision of
research director Dr. Erin Marra
• Dr. Reyes and co-resident Dr.
Ahmed Amer also had a photo submission accepted for presentation at AAEM in March entitled, “Right ventricular perforation presenting as chest pain in the ED”
• Dr. Mitali Mehta presented her
poster, “Not every red leg is cellulitis: a case of calcinosis cuties of the lower extremity,” at the Nova poster competition in November, and her photo, “I don’t know how they got in there: a case of multiple magnet ingestion,” was featured at the AAEM competition in March in collaboration with Dr. Thomas Yang
• Dr. Mehta also published a Stat-
Pearls article on the Parkland Formula in January, and was appointed the EMRA Medical Education Committee Vice President
Congratulations to our faculty and residents. Keep up the good work. ■
Life AFTER
Residency 2019 SAVE THE DATE: SEPTEMBER 2019 www.emlrc.org/lar 26
EMpulse Spring 2019
NORTH FLORIDA
UF Health: Gainesville
GLOBAL
By Michael Chami, MD, PGY-2
We have fully transitioned into a full residency class with 14 spots per training year. Our intern class is fun, hungry to excel and learn the ropes. Our residency program has begun integrating community EM rotations at our freestanding EDs, which has been a categorical hit. We have also begun partnering with nearby hospitals to facilitate the rollout of EDie and look forward to further reducing redundant testing and smoothing our patients’ transitions between hospitals. We are proud of our graduating senior residents including those who are off to fellowship: Dr. Joshua Altman will be doing Sports Medicine at UF, Dr. Nicole Hardy will be doing pediatric EM at UNC, Dr. Alicia Buck will be doing EMS, and Dr. Travis Murphy will be doing citical care medicine at UF. We were also excited to start our new
International Emergency Medicine Fellowship, founded by our very own Dr. Torben Becker! The Cardiac Arrest Research Team celebrated its first birthday after a productive year with presentations at NAEMSP, AHA, SCCM, ACEP and SAEM. A study evaluating the use of xenon gas for neuroprotection following cardiac arrest will be starting soon as part of a larger clinical trial in partnership with other institutions nationwide. Other projects range from a study evaluating the use of perfluorocarbon emulsions in a pig model of cardiac arrest, to looking at trends in Cardiac Arrest litigation in partnership with UF’s law school. We eagerly await meeting our next class of 2022! ■
Emergency Medicine Fellowship Opportunity
Global Fellowship Program
• Clinical sites in Haiti & Ghana • All travel expenses paid for
Learn more at: bit.ly/uf-global
UCF/HCA at North Florida Regional By Ryan Luevanos, MD, PGY-2
Everyone here at the North Florida EM Residency program is blown away by how our successful second year has flown by! Our amazing attendings and PGY-2’s all agree that our incoming interns have been performing phenomenally and could not be any prouder of them. I am also honored to work alongside my PGY-2 colleagues, who all share a lifelong passion for teaching and mentoring our hardworking interns, medical students and all other staff members who work alongside us. Our program continues to function as a cohesive and collegial group as we all train to not only become community leaders in the emergency department, but also in academia and policy. We have two motivated residents serving as chairs of nation-
al committees at CORD and we are beyond excited for what they have to offer. Our attendings will be going full-force to SAEM in Las Vegas, NV to support our new incoming chiefs and presenting residents, so stay tuned for a podium presentation of our program’s research on opioid prescription reduction. In addition, we have been getting numerous research projects off the ground and published that we all continue to be very proud of. I value how our amazing program directors and attendings strive to ensure that we continue to live balanced lives between pursuing our passions, working our shifts and having fun outside of work. As I type this, we just got back from one of our favorite new traditions, which is our biannual wellness EMpulse Spring 2019
days. The latest one was an intense day of paintball with not only all our resident classes, but also our attendings! It was once again a huge success, and we cannot wait to continue this tradition in the years to come. We’re excited to see what our program’s upcoming third year has in store for us, as we will at last have three full classes of bright, motivated and personable residents eager to train into some of the best physicians ready to serve beyond residency. We are excited to reconnect and meet with all the other programs at SAEM and ACEP 2019, and we continue to wish you all the best of success in this upcoming 2019-20 academic year! ■ 27
Thank You Donors The success of our advocacy efforts is dependent upon generous donations to FCEP's political action committees (PCs). Thank you to those who donated in December 2018-February 2019. Zaza Atanelov David Ball Jacqueline Barnes Michael Borunda Jerry Thomas Brooks Corrine Bullock Carlos Cao Jordan Celeste Julio De Pena Batista Alex Doerffler Steven Eccher Stephen Feilinger Jennifer Fredericks Brian Hartfelder Brooke Hensley Rory Hession Ebony Hunter Jorge Infante Stanley Janasiewicz Steven B Kailes Frederick Keroff Gary Lai Dakota Lane John Patrick Michael McCann Anna McClain Pamela Miller Craig Mitchell Mary Schmieder Donna Schutzman-Bober Wayne Stark Robert B Tober Jon Van Heertum Juan Felipe Villegas Christina Wilson Jason Wilson
HOW TO DONATE TO FCEP’S PCS: Text “FCEPPC” to “41444” Donate online at: emlrc.org/fcep-pac-donations Mail a check to FCEP at: 3717 S. Conway Road Orlando, FL 32812 28
NORTH FLORIDA
UCF/HCA at Ocala Health By Caroline Smith, MD, PGY-1 & Vir Singh, MD, PGY-2
We are looking forward to continued growth and improvement of our program in the coming months. Ocala Regional Medical Center opened the first phase of this emergency department expansion in March, with completion of the full expansion anticipated in the third quarter of this year. Ocala Health also broke ground on a new freestanding ED in February, which will be completed by the end of 2019, expanding the clinical experience of residents. In addition to the physical expansion of Ocala Regional, the clinical services continue to expand. Ocala Regional is now a comprehensive stroke center thanks to the arrival of two neurointerventionalists and implementation of new institutional protocols for stroke patients. We are excited to improve outcomes for our stroke patients by providing timely interventions in our hospital. As a new residency program, our curriculum continues to evolve and
improve. We are working on adding a dental rotation in conjunction with FreeDOM Clinic, which provides free dental, optical and medical care to underserved patients. Also, our EMS educational experience expanded with the upcoming addition of flight medicine to the rotation. Research within the residency program continues to grow with the arrival of Ocala Regional’s new research coordinator, Dr. Cristobal Cintron. Congratulations to Dr. Jason Lippert, PGY-2 who recently published a case report on bilateral luxatio erecta. More publications will soon follow as residents continue to work on research projects, quality improvement projects and case reports. Congratulations also to Dr. Vir Singh, PGY-2, who was selected for participation in the 2020 class of EMRA Leadership Academy. The program is proud to have a resident participate in leadership within EMRA and excited to benefit from this leadership training. ■
UF Health: Jacksonville By Corey Dye, MD, PGY-2
UFHCOM Jacksonville sends its best wishes to all emergency candidates who participated in match this year. Congratulations to our simulation team (Drs. Steven Chadwick, Cory Clugston, Kim Papa and Corey Dye) that took first place at the SAEM Southeast Regional Conference in February in Greenville, SC! Our second years enjoyed an amazing retreat weekend in Greenville, coupled with some friendly clinical competition and came out victorious. In other good news, a distinguished and beloved faculty member who had EMpulse Spring 2019
recently fallen severely ill, requiring ECMO in the ICU, is making great strides with recovery. We all send you our best wishes for a continued and expedient return to better health. Our senior class is entering the home stretch of residency training with only a few months left to go. We wish you all the very best of luck! We also would like to thank outgoing chiefs, Drs. Landon Lichtman, Francis Behan and Davis Lester, for their hard work this past year and welcome our incoming chiefs, Drs. Kim Papa, Cory Clugston and Sean McAlister, into their new roles. ■
Join tens of thousands of providers across the country working together to catch patients before they fall. Learn how Collective is helping care teams collaborate at: collectivemedicaltech.com/florida-collaborative-care/
RESIDENT CASE REPORT
Uncommon Emergent Complications of a Common Pediatric Diagnosis By Thomas Ruffin Jr., MD, FAAP, PGY-6 Pediatric Emergency Medicine Fellow at Arnold Palmer Hospital for Children, Orlando Health
ABSTRACT
Children present a unique challenge to the emergency physician in diagnosing rare but potentially fatal complications of routine diagnoses. It can be easy to overlook subtle signs and symptoms unless you are aware of these medical emergencies and approach each patient with a high degree of suspicion. Acute otitis media is a condition commonly treated in the pediatric emergency department. Complications arising from acute otitis media have become much less common in the era of widespread antibiotic use. Gradenigo syndrome and dural venous sinus thrombosis are rare but serious potential complications.
CASE DESCRIPTION
A nine-year-old boy presents to the ED complaining of headache, left-sided facial pain, blurry vision, diplopia and vomiting. He had previously been seen on two other occasions by his primary doctor for drainage from the left ear and had been prescribed Cefdinir and Oflaxacin otic drops. He denies fever, cough or rhinorrhea. He is an otherwise healthy, fully immunized child.
There is no mastoid bone tenderness to palpation or erythema. The patient has no sinus tenderness to palpation and there is no oropharyngeal erythema or exudate. His neck is supple and there is no meningismus. The remainder of his exam, including neurological findings, is normal. His lab work is unremarkable. The CT head reveals bilateral mastoid air cell opacification and inflammatory changes of the petrous bone on the left. An MRI of the brain with and without contrast demonstrates apical petrositis and dural venous sinus thrombosis of the left sigmoid sinus with caudal extension into the jugular vein. The patient was admitted to the Pediatric Intensive Care Unit. Neurosurgery was consulted and recommended Fig. 1: MRI image from case.
MRA, MRV and a lumbar puncture. He was treated with Ceftriaxone and Vancomycin pending CSF culture results. Due to concern for increased intracranial pressure secondary to venous sinus thrombosis, he was started on Diamox and Lovenox. A hypercoagulability workup was negative. He had bilateral myringotomy tubes placed by Otolaryngology and was continued on Ofloxacin otic drops. CSF cultures were negative and bilateral ear cultures grew Group A Strep. The patient was discharged home on Cefuroxime and Lovenox. At time of discharge, his headache and emesis had resolved but he only had mild improvement of his diplopia and no change of his left esotropia. He returned to the ED nine days later with complaints of worsening persistent headache and vomiting. He had papilledema on fundoscopic exam. A repeat MRI/MRV revealed no acute abnormality, patency of the venous sinuses, and internal jugular vein. A lumbar puncture was performed, which revealed extremely high opening pressures that required placement of a lumboperitoneal shunt. He was discharged home on Cefdinir and Lovenox. At the time of discharge, he had complete resolution of his headache, emesis, diplopia and abducens nerve palsy.
Physical exam shows a well-appearing boy in no acute distress. Vital signs are normal. He is alert and oriented. Pupils are 3 mm bilaterally and reactive. There is mild lateral gaze palsy and esotropia on the left. The remainder of the cranial nerves are intact. There is no papilledema. The right tympanic membrane demonstrates chronic changes and the left tympanic membrane cannot be visualized due to purulent drainage. 30
By Carolyn Lyon, MD Pediatric Emergency Medicine Physician at Arnold Palmer Hospital for Children, Orlando Health
DISCUSSION
The diagnosis of Gradenigo syndrome was made on the basis of the patientâ&#x20AC;&#x2122;s history and clinical exam findings of suppurative acute otitis media, facial pain in the trigeminal nerve distribution, and diplopia EMpulse Spring 2019
from an ipsilateral abducen’s nerve palsy.13 The patient’s CT demonstrated petrous apicitis consistent with Gradenigo syndrome. The MRI/MRV additionally revealed a dural venous sinus thrombosis of the left sigmoid sinus with caudal extension into the jugular vein. The time interval between the onset of acute otitis media and the manifestation of cranial nerve dysfunction varies between 1 week and 2-3 months.9 The clinical presentation can be initially subtle and difficult to diagnose. The neurological manifestations of Gradenigo syndrome are attributed to the proximity of cranial nerves to the petrous apex.9, 11 The trigeminal nerve ganglion and abducens nerve are the two most common cranial nerve deficits. They are the most susceptible to an adjacent inflammatory reaction as they are only separated from the petrous apex by a thin layer of dura matter.11 Facial sensory dysfunction and retrobulbar pain is secondary to irritation of the trigeminal nerve. Lateral rectus palsy and subsequent diplopia result from inflammation involving the abducens nerve.11 Dural venous sinus thrombosis can
REFERENCES
1. Suzich KL, Adelson S, Choi CS. An Interesting Case of Gradenigo Syndrome. J Binocul Vis Ocul Motil. 2019 Jan 7:1-2. doi: 10.1080/2576117X.2018.1540909. [Epub ahead of print] PubMed PMID: 30615575. 2. Taklalsingh N, Falcone F, Velayudhan V. Gradenigo’s Syndrome in a Patient with Chronic Suppurative Otitis Media, Petrous Apicitis, and Meningitis. Am J Case Rep. 2017 Sep 28;18:1039-1043. PubMed PMID: 28955030; PubMed Central PMCID: PMC5629926. 3. Vitale M, Amrit M, Arora R, Lata J. Gradenigo’s syndrome: A common infection with uncommon consequences. Am J Emerg Med. 2017 Sep;35(9):1388.e1-1388.e2. doi: 10.1016/j.ajem.2017.07.020. Epub 2017 Jul 5. PubMed PMID: 28720403. 4. Jensen PV, Hansen MS, Møller MN, Saunte JP. The Forgotten Syndrome? Four Cases of Gradenigo’s Syndrome and a Review of the Literature. Strabismus. 2016;24(1):217. doi: 10.3109/09273972.2015.1130067. Epub 2016 Mar 16. Review. PubMed PMID: 26979620. 5. Janjua N, Bajalan M, Potter S, Whitney A, Sipaul F. Multidisciplinary care of a paediatric patient with Gradenigo’s syn-
be septic or aseptic in origin. A septic origin is due to an infection causing thrombophlebitis whereas an aseptic etiology is secondary to hypercoagulable conditions, trauma or iatrogenic causes.8 Middle ear infections cause venous sinus thrombosis by direct spread or via the emissary veins.8 The most common presenting symptoms are headache, otalgia and fever.9 Thrombosis of the dural venous sinuses can lead to increased intracranial pressure due to the obstruction of venous outflow with subsequent venous engorgement and potentially impaired cerebrospinal fluid absorption. Patients may therefore present with severe headache, vomiting, ocular palsies, visual changes, papilledema and lethargy. CT scan is the imaging of choice to evaluate for petrous apicitis due to its sensitivity and low false positive rate.11 MRI and MR Venography is the preferred imaging for suspected thrombophlebitis as CT scan has up to a 40% false negative rate for lateral sinus thrombosis.9 Treatment of Gradenigo syndrome is typically with intravenous antibiotics. Otolaryngology should be consulted
drome. BMJ Case Rep. 2016 Feb 25;2016. pii: bcr2015214337. doi: 10.1136/bcr-2015214337. PubMed PMID: 26917799; PubMed Central PMCID: PMC4769448. 6. Zanoletti E, Cazzador D, Faccioli C, Sari M, Bovo R, Martini A. Intracranial venous sinus thrombosis as a complication of otitis media in children: Critical review of diagnosis and management. Int J Pediatr Otorhinolaryngol. 2015 Dec;79(12):2398403. doi: 10.1016/j.ijporl.2015.10.059. Epub 2015 Nov 5. PubMed PMID: 26590005. 7. Wong BY, Hickman S, Richards M, Jassar P, Wilson T. Management of paediatric otogenic cerebral venous sinus thrombosis: a systematic review. Clin Otolaryngol. 2015 Dec;40(6):704-14. doi: 10.1111/coa.12504. Review. PubMed PMID: 26769686. 8. Balasubramanian A, Mohamad I, Sidek D. Extensive dural sinus thrombosis and bilateral lateral rectus palsy as an uncommon complication of chronic suppurative otitis media. BMJ Case Rep. 2013 Jan 25;2013. pii: bcr2012007414. doi: 10.1136/bcr-2012-007414. PubMed PMID: 23355565; PubMed Central PMCID: PMC3603784. 9. Scardapane A, Del Torto M, Nozzi M, Elio
EMpulse Spring 2019
early as surgical intervention is warranted if patients fail medical therapy, have cranial nerve palsies, or develop an abscess. Initial surgical management is often insertion of tympanostomy tubes.3 More recent studies have demonstrated the safety and efficacy of conservative otological surgery and anticoagulant therapy for treatment of sinus venous thrombosis. 6,7,9,12 As reported in prior studies, medical therapy with antibiotics and anticoagulants generally achieves complete resolution of symptoms of Gradenigo syndrome with associated sinus venous thrombosis.9 Our patient returned to the children’s ED after nine days with signs and symptoms suggestive of worsening increased intracranial pressure. The elevated opening pressures on lumbar puncture but normal MRI/MRV findings were surprising and suggestive of benign intracranial hypertension. In conclusion, otological complaints are common in the pediatric ED. These rare but potentially fatal complications must be considered in our differential diagnosis. A high index of suspicion can lead to early recognition and treatment. ■
C, Breda L, Chiarelli F. Gradenigo’s syndrome with lateral venous sinus thrombosis: successful conservative treatment. Eur J Pediatr. 2010 Apr;169(4):437-40. doi: 10.1007/s00431-009-1047-4. Epub 2009 Aug 21. PubMed PMID: 19697060. 10. Burston BJ, Pretorius PM, Ramsden JD. Gradenigo’s syndrome: successful conservative treatment in adult and paediatric patients. J Laryngol Otol. 2005 Apr;119(4):325-9. PubMed PMID: 15949093. 11. Sherman SC, Buchanan A. Gradenigo syndrome: a case report and review of a rare complication of otitis media. J Emerg Med. 2004 Oct;27(3):253-6. PubMed PMID: 15388211. 12. Stam J, De Bruijn SF, DeVeber G. Anticoagulation for cerebral sinus thrombosis. Cochrane Database Syst Rev. 2002;(4):CD002005. Review. Update in: Cochrane Database Syst Rev. 2011;(8):CD002005. PubMed PMID: 12519565. 13. Motamed M, Kalan A. Gradenigo’s syndrome. Postgrad Med J. 2000 Sep;76(899):559-60. Review. PubMed PMID: 10964120; PubMed Central PMCID: PMC1741722
31
THE ULTRASOUND ZOOM
Eye Spy Ocular Point-of-Care Ultrasound
As an emergency physician, I see a lot of patients with complaints of eye pain, eye trauma, vision changes and, of course, a lot of patients with headaches. Acute ocular emergencies carry high risk and warrant prompt diagnosis and management. However, I often face difficulties in performing a conventional physical exam on a swollen, closed and painful eye, and a good funduscopic examination in a well-lit, chaotic department can be near impossible. This is when point-of-care ultrasound (POCUS) of the eye is extremely helpful. Ocular POCUS is simple, rapid, non-invasive and amenable to dynamic assessment. Using POCUS, we can “rule-in” many abnormalities including retinal detachment, posterior vitreous detachment, lens dislocation, vitreous hemorrhage and increased intracranial pressure (ICP). In my busy emergency department, using POCUS to supplement my clinical exam has not only helped me manage ocular emergencies quickly, but has also increased my patient satisfaction scores and my patient throughput time.
COMMON OCULAR COMPLAINTS
Common ocular complaints that can be managed with POCUS can be divided into three basic subsets: (a) painless changes in vision, (b) headache and (c) ocular trauma (Fig. 1). Painless Changes in Vision If my patient presents with spon32
By Kelsey Wolfe, MD, PGY-2 Jackson Memorial Hospital
Edited by Leila Posaw, MD, MPH Emergency Ultrasound Director, Jackson Memorial Hospital
Fig. 1: Common ocular complaints and potential diagnoses that can be diagnosed with ocular POCUS Painless Changes in Vision
Headache
Ocular Trauma
» » »
taneous, painless, monocular vision loss, I am faced with a broad list of differential diagnoses: retinal detachment (RD), vitreous hemorrhage (VH), posterior vitreous detachment (PVD), central retinal artery/vein occlusion and Amaurosis Fugax. In recent years, several case reports have highlighted the use of POCUS in the diagnosis of central retinal artery obstruction (absence of flow on color Doppler [Fig. 2], absence of bidirectional flow in the central vessels on spectral Doppler, edematous optic nerve, hyperechoic emboli) and Amaurosis Fugax (fresh thrombus and complete occlusion of the common carotid artery). However, for us emergency physicians, I find POCUS most useful in the diagnosis of RD, PVD and VH. EMpulse Spring 2019
Retinal Detachment Vitreous Hemorrhage Vitreous Detachment Central Retinal Artery Occlusion
Increased Intracanial Pressure
Lens Dislocation Foreign Body Retrobulbar Hematoma Globe Rupture
Retinal detachment occurs as a result of separation of the retina from the underlying layer and comes in three flavors: rhegmatogenous RD due to retinal tears, exudative RD due to subretinal exudates and tractional RD due to vitreoretinal traction. On POCUS, RD always appears as a funnel-shaped echogenic membrane attached to the optic nerve head posteriorly and to the oro serrata anteriorly. On a dynamic scan (with the patient moving their eyes side-to-side, also called oculokinetic echography), the detached retina will undulate like a “sheet in the wind” (Fig. 3). If the RD involves the macula (mac off), it is “too late” for this macula and the patient needs urgent follow up. However, if the RD does not involve the macula (mac on), the patient should be seen by ophthalmology as
soon as possible, as this macula can be saved. On POCUS, the macula is located directly in the visual axis, lateral to the optic nerve. Vitreous hemorrhage occurs when blood extravasates into the vitreous chamber. On POCUS, VH appears as hyperechoic material in the normally anechoic vitreous chamber. On dynamic scanning, this material tumbles like “clothes in a drier” (Fig. 4). Vitreous detachment occurs when the vitreous membrane separates from the retina. On POCUS, VD appears as an undulating echogenic free-floating membrane, described as “swaying seaweed” (Fig. 5).
Fig. 2: Absence of flow in the central retinal vessels4
Optic nerve edema not caused by increased ICP is called pseudopapilledema. This can be due to optic disc drusen (calcified optic disc which caused a bright signal with a clean shadow) or due to unilateral nerve inflammation, caused by optic neuritis, syphilis, lupus or sarcoidosis.
Fig. 3: Retinal detachment4
Ocular Trauma Trauma to the face can result in eye injuries: retrobulbar hematoma, foreign bodies, lens dislocation, globe rupture, VH, RD and elevated ICP. All can be evaluated with POCUS. (Caution: examination of globe rupture with POCUS is controversial, as ocular pressure may cause further loss of vitreous fluid.)
Headache If my patient presents with a headache and I suspect increased intracranial pressure (ICP), POCUS is an excellent method to evaluate for papilledema (swelling of the optic nerve head). This is especially useful in patients with Idiopathic Intracranial Hypertension or pseudotumor cerebrii. Several recent articles have described POCUS in the diagnosis, management and follow-up of patients with this condition.
thought to represent increased ICP. The grey zone is 5–6 mm, in which case visualization of optic disc elevation and/or the crescent sign confirms the diagnosis (Fig. 6).
Fig. 4: Vitreous hemorrhage
4
With POCUS, papilledema is visualized as optic disc elevation into the vitreous chamber, increased optic nerve sheath diameter (ONSD), and as fluid around the optic nerve, which may appear as a crescent or doughnut sign. A normal ONSD is less than 5 mm, and a diameter of more than 6 mm is
Bleeding and edema around the orbit can lead to a retrobulbar hematoma, which on POCUS is visualized as a mixed-echogenic collection behind the globe. Missed diagnosis can lead to pressure necrosis of the optic nerve and blindness. Trauma can cause lens dislocation, which on POCUS appears as a lentiform structure that moves
CONTINUE ON PAGE 34 »
Eye Spy.To.Go.
• Cut along the border of the table below. • Fold in the middle. • Stick in your wallet. Reference on-the-go.
Find this table online at emlrc.org/ultrasoundzoom
Courtesy of authors Leila Posaw, MD, MPH and Kelsey Wolfe, MD, PGY-2
Ocular Point-of-Care Ultrasound Step 1
Step 2
Step 3
Step 4
EMpulse Spring 2019
Step 5
Step 6
33
Fig. 6: Right and left eyes of a patient with headache and dilated ONSD. Images by Dr. Kristina Jacomino
Fig. 5: Vitreous detachment4
Fig. 7: Lens dislocation4
Fig. 8: Ocular anatomy, showing the anterior chamber (red), lens (green), vitreous chamber (blue) and optic nerve (yellow).5
ÂŤ CONTINUED FROM PAGE 33 independently of intended oculokinetic movements in the anterior or posterior chamber (Fig. 7). Globe rupture is a surgical emergency. POCUS findings include a deformed globe, with chamber collapse and decreased ocular fluid. If you must ultrasound this, then experts advise copious amounts of cold gel and no pressure is to be applied on the open globe.
Fig. 9: Normal transverse, sagittal views and measurement of the optic nerve sheath diameter. Images by Dr. Kelsey Wolfe
POCUS is more sensitive than CT for detecting intraocular foreign bodies, especially if the FB is radiolucent. All FBs are bright and echogenic. Metal/ glass produce reverberations and wood produces posterior acoustic shadowing, which can assist detection by POCUS.
CONTINUE ON PAGE 35 Âť
Ocular Point-of-Care Ultrasound Lens dislocation
34
Headache & dilated ONSD
Vitreous detachment
Vitreous hemorrhage
EMpulse Spring 2019
Retinal detachment
Absence of flow in central retinal vessels
HOW TO
Ultrasound the Eye Prior to scanning, familiarity with ocular anatomy and the corresponding sono-anatomy is recommended. See Fig. 8 for review.
Probe and Positioning
Fig. 10: Step-by-Step Guide
Step 1:
Lay the patient back and ask them to close their eyes.
• The patient should be in a supine or reclined position with eyes closed.
• The high frequency linear probe (12-4 MHz)
is recommended. While some may prefer the high frequency endocavitary probe (9-3 MHz), it is more awkward to hold and position.
• The probe should be stabilized, with the operator’s 5th finger placed on the patient’s forehead or nose.
Step 2:
Apply a small amount of sterile ultrasound gel to the upper eyelid.
• Some operators prefer placing a generous
amount of sterile gel directly on the closed eyelid while others prefer placing a transparent, adhesive patch on the closed eyelid, and then placing sterile gel on top of the patch.
• Each eye is scanned in the transverse plane
(probe marker to the nose) and in the sagittal plane (probe marker to the forehead) (Fig. 9). The standard probe marker position for the transverse views of both eyes is medial/nasal.
Step 3:
Cover the eye with a transparent adhesive film. Smooth out any air bubbles or wrinkles to minimize artifact.
• Each eye is first scanned with the patient looking straight ahead, and then with the patient looking from side to side (oculokinetic echography).
• While RD can be visualized on low gain, the
gain is increased to better visualize PVD and VH.
Step 4:
Place a liberal amount of sterile ultrasound gel on the film.
• ONSD is measured 3 mm behind the optic disc. The ONSD is measured twice for each eye (transverse and sagittal planes) and these are averaged to get the final number. ■
Step 5:
REFERENCES & SUGGESTED READING
Place a linear probe on the ultrasound gel. Fan through the entire globe in both transverse and sagittal planes, visualizing the entire anterior and posterior chambers.
2. Adhikari, Srikar R. “Section Links.” ACEP Clinical Policy on Opioid Prescribing. www.acep.org/sonoguide/smparts_ocular.html
Step 6:
1. Lorente-Ramos, Rosa M., et al. “US of the Eye Made Easy: A Comprehensive How-to Review with Ophthalmoscopic Correlation.” RadioGraphics, vol. 32, no. 5, 2012, doi:10.1148/rg.325115105
3. Avila, Jacob. “Optic Nerve Sheath Diameter.” 5 Minute Sono, 25 Mar. 2016, 5minsono.com/onsd 4. The POCUS Atlas. www.thepocusatlas.com/ocular 5. Left image licensed under Creative Commons Attribution 3.0 via Wikimedia Commons. “Three Internal chambers of the Eye” by Artwork by Holly Fischer. https://wolframsyndrome.dom.wustl.edu/diabetes-and-optic-atrophy
To measure the ONSD, obtain a still image with the lens and optic nerve in view (plane which transects the nerve at its greatest diameter). Measure ONSD 3 mm behind the optic disc in the axis of the nerve. Average sagittal and transverse measurements.
Model: Austin Maddy EMpulse Spring 2019
35
POISON CONTROL
BUTTON BATTERY INGESTIONS:
A SWEET NEW RECOMMENDATION Disc batteries, or “button” batteries, are frequently found in the household and electronic devices. Button batteries are typically composed of an outer metal coating, which has a positive and negative pole, and an interior compartment containing an electrolyte, typically manganese dioxide, zinc-air, silver oxide or lithium.1 The 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System contains 3,649 single substance disc battery ingestions, including four fatalities—all of which were pediatric patients under the age of five.2 The injury caused by button batteries is primarily attributed to the generation of an electric current that hydrolyzes tissue fluids at the battery’s negative pole, producing hydroxide. Other factors contributing to injury are the leakage of battery contents (typically hydroxide) and physical pressure of the battery on the tissue against which it is lodged. The “3 Ns” mnemonic—negative, narrow and necrotic—refers to the negative pole, which is the narrower end of the button battery on lateral radiograph and causes the most necrotic injury.1 Button batteries impacted in the esophagus are known for their abil-
REFERENCES 1. Litovitz T, Whitaker N, Clark L, White
NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010 Jun;125(6):1168-77.
2. Gummin DD, Mowry JB, Spyker DA,
Brooks DE, Fraser MO, Banner W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017 Dec;55(10):1072-1252.
36
ity to cause serious local damage in as little as 2 hours, making prompt evaluation of location and removal paramount in management. Button batteries can also cause serious mucosal damage when lodged in the stomach or in the intestine.3, 4 Risk factors associated with gastric mucosal damage include age <4 years, the ingestion of two or more batteries or magnet co-ingestion, batteries ≥ 20 mm (hearing aid batteries are assumed to be < 12 mm) or in place for ≥ 48 h, an unknown time of battery ingestion, or the presence of symptoms.3 Of note, lithium-containing button batteries have a higher capacitance and thus ability to generate more current, producing greater hydroxide compared to other button batteries.1 Due to the risk of immediate damage and delayed complications, confirmation of location and assessment of need for removal are critical. When button battery ingestion is known or suspected, patients should not receive anything by mouth due to a possible need for endoscopic removal. However, prior to emergency department evaluation and radiographic localization of ingested batteries, honey may be administered orally to coat the battery and reduce local generation of hydroxide.6 This
3. Ríos G, Rodríguez L, Lucero Y, Miquel
I, Arancibia ME, Alliende F. Endoscopic Findings Associated With Button Battery Ingestion in Children: Do We Need to Change the Protocol for Managing Gastric Location? Pediatr Emerg Care. 2018 Jan 23.
4. Elmalik K, Patel RV, Gabra H. Lapa-
roscopic management of intestinal obstruction and perforation of Meckel’s diverticulum by a button battery. J Ped Surg Case Reports. 2013;1:117–119. EMpulse Spring 2019
Kristen C. Lee, PharmD, BCPS Clinical Toxicology, EM Fellow Madison Schwartz, PharmD Clinical Toxicology, EM Fellow
may be completed at home or in the health care facility. Criteria for use of honey include all of the following: patient should be >12 months old, able to swallow, the button battery ingestion was within the last 12 hours, and honey is immediately available (i.e., seeking medical care at an emergency department should not be delayed to obtain honey). The dose is 10 mL (2 teaspoons) of honey by mouth every 10 minutes, up to 6 times. Commercial honey is preferred to avoid potential exposure to plant toxins in natural honey products. As an alternative to honey, sucralfate liquid may be administered following radiographic confirmation of battery location, while awaiting endoscopy.6 The dose is 10 mL of the 1 g/10 mL suspension administered orally, every 10 minutes, for up to 3 doses. Administration of sucralfate liquid prior to radiographic visualization is not recommended given its potential for radiopacity. ■ FPICN toxicologists are available 24 hours a day at 1-800-222-1222 to assist emergency physicians in the treatment of all toxic exposures, including triage and management of button battery ingestions.
5. Jatana KR, Rhoades K, Milkovich S,
Jacobs IN. Basic mechanism of button battery ingestion injuries and novel mitigation strategies after diagnosis and removal. Laryngoscope. 2017 Jun;127(6):1276-1282.
6. Anfang RR, Jatana KR, Linn RL, Road-
es K, Fry J, Jacobs IN: pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope. 2018 Jun 11; Epub ahead of print.
APP Advanced Practice Provider
Skills Camp May 2-3, 2019 EMLRC in Orlando, FL
Approved for AMA PRA Category 1 Creditsâ&#x201E;˘ and nursing contact hours Price: $350 Registration Closes April 24, 2019 Target audience: nurse practitioners, physician assistants, primary care physicians, urgent care center physicians & allied health professionals seeking a refresh on their emergency medicine knowledge
DAY 1 TOPICS:
DAY 2 TOPICS:
By Dr. Caroline Molins
By Dr. Hector Rivera
Arthrocentesis
Pediatric Non-Traumatic Surgical Emergencies
Pediatric Review MIPS
Transfusions
Brief Resolved Unexplained Event
Caring for Opioid Use Disorder Patients
ABG
Skills: Tips & Tricks of Plain Films
Lunch: EM Jeopardy
Skills: IO Lab
By Dr. Carmen Martinez By Dr. Miguel Acevedo By Dr. Todd Haber By Dr. Vincent Valente
By Dr. Andrew Gibson By Dr. Aaron Wohl
Dr. Michael Lozano Various faculty
Skills: Foreign Body Removal Lab Various faculty
Register Now
Skills: ECG Interpretation By Dr. Jose Rubero
www.emlrc.org/appsc
Schedule subject to change. EMpulse Spring 2019
37
Membership Spotlight
Get to know fellow FCEP members through Q&A's, beginning with FCEP's Executive Board. By René Mack, MD, RDMS, FACEP & Shayne Gue, MD
Meet Your Exec-Board:
Sanjay Pattani, MD, MHSA, FACEP Vice President Q What sparked your interest in joining
FCEP’s Board of Directors and how did you first become involved?
A When I came to Orlando, many of my
colleagues I worked with were part of FCEP. Once I attended my first EM Days, I was hooked. When we work side-by-side in the ER, we share our patient care experiences and clinical knowledge. However, in Tallahassee, I saw yet another way I could learn with and from my colleagues in a non-clinical way. Our FCEP Board is one of the strongest in the nation. Since that time, and with every opportunity, I look forward to our collaboration and how we advocate for our members, our patients, and ultimately our specialty. The FCEP Board is a prime example of how professional growth in emergency medicine can be achieved outside the clinical realm.
Q How has being in emergency
medicine changed the way you think about leadership, and how will you apply those skills while serving on the board?
A In my opinion, emergency medicine
physicians are the most dynamic and organized physicians who truly have the most to offer health care systems in regards to intellectual capital and innovation. Our ability to problem-solve and create solutions make us all significant leaders on every shift. Board membership is the catalyst I use to reach out to our statewide network of ER leaders. Over the past five years, I have learned from my fellow board members in many different areas, ranging from
38
public policy, tort reform and clinical best practices. My leadership and communication skills allow me to articulate FCEP issues and positions in a non-threatening, collaborative fashion.
“
In my opinion, emergency medicine physicians are the most dynamic and organized physicians who truly have the most to offer health care systems in regards to intellectual capital and innovation.
to manage a work/life balance. I learned from many seasoned leaders that spending time with your family and taking enough “personal” time is important. I may be a little old school, but I firmly believe in quality family time, where my four sons cannot play on their iPads or Xbox, and my wife and I cannot check email or texts. As hard as this is, we must do our best to minimize distractions and enjoy the precious moments in our lives. When my kids mature, I may have more time to dedicate towards additional professional growth and responsibility. I also try to reciprocate and support my colleagues in their careers and times of need. Q Where can we find you on your days
off?
A If I’m not at Orange Theory or the Q What is your biggest goal to ac-
complish during your tenure on the board?
A I’m not sure if I have a major objec-
tive other than continuing to promote the evolution of our practice and advocating for our patients. I do hope to recognize and develop our young leaders, and continuously provide support long after my tenure on the board.
Q Physician wellness is an important
priority within the EM community. How do you make it a priority not only to yourself but within your institution?
A With EM being among the leading
burnout specialties, it is important EMpulse Spring 2019
gym, or chaperoning one of my four sons to their sporting events, you can most definitely find us on the lake wake surfing, boarding and tubing!
Q What’s your favorite tip for an EM
resident or medical student interested in emergency medicine?
A Continue to challenge yourself. Al-
ways carry a healthy sense of paranoia while at work. Never let your guard down—your nursing team and your patients need you to always be at your best. Maintain trust, transparency and open communication. You have the ability to make a difference in so many ways. And your potential is limitless. ■
NOW HIRING
EMERGENCY PHYSICIANS IN DAYTONA BEACH AREA
L O R T N O C R U YO . . . E L U D E H SC
LB YIVTEH E
OCEAN
Join EMPros in Sunny Central Florida!
• Private EM group staffing 5 hospitals in Daytona Beach Florida Area
• Employee Option with Full Benefits or Independent Contractor • Flexible Scheduling
• Comradery with Fellow Physicians
FOR MORE INFORMATION, VISIT EMPROSONLINE.COM OR FACEBOOK.COM/EMERGENCYMEDICINEPROFESSIONALS
Corporate Partners
The success of the Florida Emergency Medicine Foundation (FEMF)/Emergency Medicine Learning & Resource Center (EMLRC) is due in large part to our corporate partners who provide annual sponsorship support for our educational programs and events. Thank you to our corporate partners for believing in our mission and helping us provide lifesaving education for lifesavers.
3717 S. Conway Road, Orlando, FL 32812 www.emlrc.org/fcep | (800) 766-6335
Meet Our
EM Innovators
EM Champion
EM Advocates
BECOME A PARTNER Are you interested in becoming a corporate partner? View our various opportunities at emlrc.org/becomeapartner or by scanning now. 40
EMpulse Spring 2019
Non-Profit Org. U.S. POSTAGE PAID Pontiac, Illinois PERMIT NO. 592
EM Dignitary