Fall 2016
www.hrphysician.com
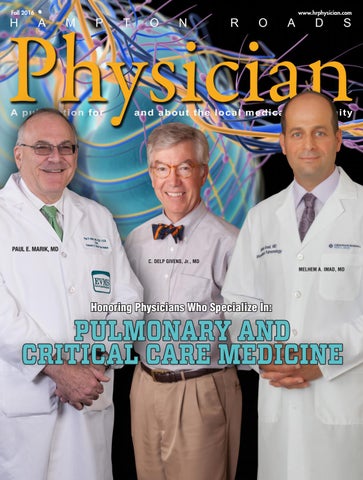
PAUL E. MARIK, MD C. DELP GIVENS, Jr., MD MELHEM A. IMAD, MD
Honoring Physicians Who Specialize In:
Patients will always remember how we make them feel. And at EVMS Medical Group we want to make them feel better. We understand that for so many patients, a trip to the doctor is stressful — especially when they’re sick or hurt, or worried about a potential diagnosis. So how can we make a positive change?
It begins with the patient experience. We are dedicating ourselves to improving quality of care across each and every point of patient contact, from the very first hello. We’re expanding the lines of communication, placing even more value on kindness and compassion. Yet it’s more than simply being nice. It’s a conscious focus on shifting our entire culture. By working together as a team, we can provide each patient with the best — and most personalized — healthcare experience. Because above all, we’re here to treat our patients well.
The knowledge to treat you better.
Learn more at EVMSMedicalGroup.com.
contents Fall 2016 VOLUME IV, ISSUE IV
12
14
44 Smart Strategies for Setting Salaries
10
45 Autologous Stem Cell Transplantation 46 Hand Therapy: Patient Education DEPARTMENTS 4 Publisher’s letter 6 Physician Advisory Board 16 Good Deeds: Shuping Wang, MD 18 Advanced Practice Providers: Jeffrey Belcher, MPA, PA-C 28 Medical Update: Accountable Care Organizations …and the next incarnation:MACRA/MIPS 48 In the News 54 Welcome to the Community 62 Awards and Accolades
FEATURES 8 Every Breath You Take…
10 C. Delp Givens, Jr., MD 12 Melhem A. Imad, MD 14 Paul E. Marik, MD
PROMOTIONAL FEATURES 20 Sports Medicine & Orthopaedic Center
26 Non-Surgical Options for Men with Prostate Cancer
34 The New Hope Center for Reproductive Medicine
32 What Medical Professionals Need to Know About Patents
16
18
38 The Canary in the Coal Mine 40 Liability Risks of Telemedicine 42 Taking the Pain Out of Knee Replacement Recovery
Taking Nominations for the Winter 2017 edition We are looking for physician leaders who specialize in
CARDIOLOGY Deadline for Nomination Submissions
Cardiology
November 24
Nomination forms are available on www.hrphysician.com (click nominate tab) or by emailing a request to holly@hrphysician.com Fall 2016 Hampton Roads Physician | 3
WELCOME TO THE Holly Barlow
Bobbie Fisher Editor
Publisher
A
s we publish this issue of Hampton Roads Physician, Fall is definitely – and finally – here. After one of the hottest and most humid summers we can remember, it’s delightful to feel that bit of chill in the air, and to take in a deep breath of autumn. Not everyone has that luxury, of course. For the millions of Americans who have respiratory difficulties, the inability to take a deep breath can be devastating. In that spirit, we devote our cover story to those physicians who care for and treat patients, no matter the etiology, who suffer from lung disease. Within pulmonary and critical care medicine – as in so many fields of medicine – there are many distinct and highly specialized areas of expertise and practice. Dr. Delp Givens, Dr. Melhem Imad and Dr. Paul Marik represent
Physician H
A
M
P
A publication for
T
O
FALL 2016 EDITION
N
R
O
A
D
S
and about the local medical community
Fall 2016 and Volume IV, Issue IV
Recognizing the achievements of the local medical community Publisher Holly Barlow Editor Bobbie Fisher Physician Advisory Board (see page 6) Magazine Layout and Design Desert Moon Graphics Published by Publishing, LLC
4 | www.hrphysician.com
three such areas: sleep medicine, Winter – Cover: Cardiology interventional pulmonology, Medical Update: Colon Cancer and critical care. It’s our great pleasure to honor them on our Spring – Cover: Ophthalmology Fall cover. Medical Update: Preventive Medicine Additionally, in this issue, Summer – Cover: Conditions of the Spine you’ll find a look at Accountable Medical Update: Geriatrics/Palliative Care Care Organizations, and articles about ophthalmology, Fall – Cover: Reconstructive Plastic Surgery orthopaedic pain management, Medical Update: Treating Obesity autologous stem cell transplantation for cancer patients, and physical therapy, among As 2016 comes to an end, the team at others. Hampton Roads Physician wants to thank As we prepare to wind down 2016, all of our readers for your support, your we’re already looking ahead to next thoughts and ideas. We hope you’ll conyear. We’ve prepared our 2017 editorial tinue to let us know what you’re thinking, calendar, and are pleased to share that and how we can better serve you. with you now. Please keep in mind that featured physicians, on our covers, are With all best wishes, chosen by our physician advisory board Holly and the team! through a nomination process.
Emeritus and Voting Board Jon M. Adleberg, MD Anthony M. Bevilacqua, DO Silvina M. Bocca, MD, PhD, HCLD Mary A Burns, MD, FACOG, FPMRS Jeffrey R. Carlson, MD Kevaghn P. Fair, DO Bryan Fox, MD Margaret Gaglione, MD, FACP Emmeline C. Gasink MD, FAAFP, CMD Jerry L. Nadler, MD, FAHA, MACP, FACE Paa-Kofi Obeng, DO Michael J Petruschak MD Richard G. Rento II, MD Michael Schwartz MD JohnM. Shutack, MD I. Phillip Snider, DO Deepak Talreja, MD, FACC, FSCAI Jyoti Upadhyay, MD, FAAP, FACS Christopher J. Walshe, MD, FACOG, FACS, FPMRS Elizabeth Yeu, MD
Contact Information 757-237-1106 holly@hrphysician.com Hampton Roads Physician is published by DocDirect Publishing, LLC, 1263 Manchester Ave., Norfolk, VA 23508 Phone: 757-237-1106. This publication may not be reproduced in part or in whole without the express written permission of DocDirect Publishing, LLC. Published four times a year, Hampton Roads Physician provides a wide variety of the most current, accurate and useful information busy doctors and health care providers want and need. Cover stories concentrate on one branch of medicine, featuring profiles of practitioners in that specialty. Featured physicians are chosen by the advisory board through a nomination process involving fellow physicians and public relations directors from local hospitals and practices. Although every precaution is taken to ensure accuracy of published materials, DocDirect Publishing, LLC cannot be held responsible for opinions expressed or facts supplied by its authors. Visit Us Online
B O A R D A D V I S O R Y P H Y S I C I A N
2016 ADVISORY BOARD
Their input will help guide the editorial content, format, and direction of the magazine. Along with our Emeritus Board, they will select our featured physicians. Alfred Abuhamad, MD Obstetrics & Gynecology Dr. Abuhamad serves as the Vice Dean for Clinical Affairs and the Mason C. Andrews Professor and Chair, Department of Obstetrics and Gynecology at EVMS. He is Board certified in Obstetrics & Gynecology and Maternal-Fetal Medicine. He is the current president of the Society of Ultrasound in Medical Education, and the National Council of Safety in Women’s Healthcare and past president of the American Institute of Ultrasound in Medicine.
O.T. Adcock, Jr., RPh, MD
Jennifer Miles-Thomas, MD, FPM-RS Urology Dr. Miles-Thomas is a urologist with The DevineJordan Center for Reconstructive Surgery and Pelvic Health-a division of Urology of Virginia, an Assistant Professor in the Department of Urology at EVMS, and the Medical Director for the Pelvic Health Center at Chesapeake Regional Medical Center. Dr. MilesThomas is Board certified and fellowship trained in urology. She is also Board certified in female pelvic medicine and reconstructive surgery.
Hesed Mugaisi, MD
Registered Pharmacist/Family Medicine Dr. Adcock is a Board certified Family Medicine physician in practice in Hampton for 32 years. He currently serves as Associate Medical Director and Service Line Chief for Primary Care and Access for Riverside Medical Group.
Dr. Mugaisi is a Board certified family medicine physician with Bon Secours Suffolk Primary Care. He acquired his bachelor of medicine and bachelor of surgery from the University of Nairobi in Nairobi, Kenya and completed his family medicine residency at Group Health Family Medicine Residency Program affiliated with University of Washington in Seattle, WA.
John W. Aldridge, MD, FAAOS
Jennifer F. Pagador, MD
Orthopaedic Surgeon Dr. Aldridge is a Board certified orthopaedic surgeon with Hampton Roads Orthopaedics & Sports Medicine. He specializes in minimally invasive muscle sparing spinal surgery and total joint replacement surgery. Dr. Aldridge practices at both the Newport News and Williamsburg office locations of HROSM. In addition to his many interests in the field of orthopaedics, he also serves as a Lieutenant Colonel in the United States Army Reserves.
Brian L. Johnson, MD
Family, Bariatric and Age Management Medicine Dr. Pagador is Medical Director of Seriously Weight Loss, LLC and Attending Physician at Revita Medical Wellness, specializing in medical weight loss and hormone optimization. Dr. Pagador is Board certified in family medicine.
Michael M. Romash, MD
Dermatology Dr. Johnson is the founder of The Virginia Dermatology & Skin Cancer Center. He is a Fellow of the American Academy of Dermatology, American College of Mohs Surgery, and the American Society of Dermatologic Surgery. His emphasis is on the treatment of skin cancer using the Mohs Micrographic surgical technique, an advanced surgical procedure for the treatment of skin cancers.
Orthopaedic Surgeon A Board certified lower extremity specialist practicing for over 30 years, Dr. Romash is a Fellow of the prestigious American Orthopaedic Association and known as a pioneer in his field. Author of numerous medical journal articles and chapters in text books about foot and ankle surgery, he has developed treatments commonly used for various heel fractures.
Mark W. McFarland, DO
Lynne A. Skaryak, MD
Orthopaedic Spine Surgery Dr. McFarland practices at the Orthopaedic & Spine Center in Newport News and is Board certified In Orthopaedic Surgery and Fellowship trained in Spine Surgery.
Thoracic Surgery Dr. Skaryak is Director of Thoracic Surgery and Co-Director of Thoracic and Lung Health at Chesapeake Regional Medical Center. She is Board certified in Thoracic Surgery.
Visit our website to see all members of the Emeritus Board: hrphysician.com 6 | www.hrphysician.com
Established in 2002 and dedicated to patient care, Dominion Pathology Laboratories, (DPL) is an independent laboratory that offers expert diagnosis on biopsies performed in healthcare facilities throughout Hampton Roads and greater Richmond.
Robert A. Frazier, Jr., M.D.
Kevaghn P. Fair, D.O.
Michael T. Ryan, D.O.
• 24 Hour Turn-Around On Routine Specimens • Board Certified Pathologists With Over 70 Years Of Combined Experience • Immediate Access To Our Physicians Whenever You Need Them • Continuous Internal Quality Control Where Second Opinions Are Routinely Provided In The Diagnosis Of Unusual, Suspicious, Or Malignant Cases. 733 Boush Street, Suite 200 • Norfolk,VA 23510 Phone 757-664-7901• Fax 757-664-9122 www.dominionpathology.com
EVERY BREATH YOU TAKE… …the somewhat dangerous evolution of pulmonary medicine
T
he lungs, wrote the second century Greek physician and philosopher Galen, had “all the properties which make for easy evacuation; for it is very soft and warm and is kept in constant motion.” He also assumed that arteries carried the purest blood to higher organs such as the brain and lungs from the left ventricle of the heart, while veins carried blood to the lesser organs such as the stomach from the right ventricle. In order for that theory to be correct, some sort of holes were needed to interconnect the ventricles, and so in the spirit of Galen’s time, he claimed he had found them. So paramount was Galen’s authority that for 1400 years, anatomists claimed to have seen these holes as well.1 Not wanting to dispute Galen when he couldn’t find those holes, Vesalius imagined that it diffused through the unbroken partition between the ventricles. When he published his 1543 8 | www.hrphysician.com
book De humini corporus fabrica, pointing out that Galen had based some of his theories on the dissection and observation of dog and monkey cadavers rather than human ones as he himself had, Vesalius was met with such opprobrium that he vowed never to write again, and lived out his life as a court physician. It took a royal intervention to save him from burning at the stake.2 It didn’t turn out as well for Michael Servetus, a colleague of Vesalius, who published that blood flowed from one ventricle to the other through the lungs, contradicting Galen’s assertion that blood “sweated” from the right ventricle to the left through invisible pores in the interventricular system. Servetus was thereafter burned atop a mound of his own books by order of John Calvin, although probably as much for his revisionist religious views as for his insult to the established theories of Galen.3
Less than a hundred years later, William Harvey had published On the Circulation of the Blood, which further described the significance of the lungs. In his Lectures on the Whole of Anatomy (1653), he said: “Pre-eminence [of the lung]: nothing is especially so necessary, neither sensation nor aliment. Life and respiration are complementary. There is nothing living which does not breathe nor anything breathing which does not live.” Further disputing Galen, Harvey concluded: “The lungs make the spirits and indicate the nourishment, wherefore more worthy than the liver if honor is judged by benefit.”4 Although he ultimately lived to see the majority of reputable anatomists acknowledge the validity of his work, Harvey himself initially experienced resistance within the medical community. In fact, he is remembered as saying, “You know very well the storm my previous
research caused. It is often better to grow wise in private at home than to publish what you have amassed with infinite labor, to stir up storms that may rob you of peace and quiet for the rest of your days.”5 Fortunately, scientists interested in the pulmonary system chose not to grow wise in private, and continued to pursue knowledge of the lungs and the circulatory system – but it would be another century and a half before scientists began to understand the physiology of respiration and the importance of oxygen. Joseph Priestly identified the presence of oxygen in air, but was unaware of its chemical and physiologic importance. Antoine Lavoisier named Priestley’s gas and defined the role of oxygen in combustion, chemical reactions, and respiration. Though probably France’s greatest chemist ever, Lavoisier lost his head to the guillotine during the French revolution.6 Fortunately, it’s much safer to practice pulmonary and critical care medicine today. These two specialties are inexorably linked. The connecting theme, of course, is that patients who are critically ill invariably have difficulty breathing for themselves, and require the assistance of a mechanical ventilator. It was the experts in lung physiology in the 20s, 30s and 40s who developed the technology that made the ventilator possible. After mechanical ventilation was introduced, it morphed into other aspects of critical care: blood pressure control, sepsis, infection, etc. The three physicians on the cover of this issue of Hampton Roads Physician represent three separate specialties that have evolved within the umbrella of pulmonary and critical care medicine: the relatively new field of sleep medicine, lung disease and the ICU. Dr. Delp Givens of Riverside Pulmonology/Sleep Center has seen the number of patients with sleep disorders skyrocket to such a degree that in 2017, he will transition his pulmonary/critical care practice to sleep medicine entirely to accommodate their needs. Dr. Melhem Imad, who practices interventional pulmonology with Bayview Physicians, Pulmonary Medicine of Virginia Beach and at Chesapeake Regional Healthcare, focuses the majority of his work caring for lung cancer patients. Dr. Paul Marik, Professor of Medicine and Chief of Pulmonary and Critical Care Medicine at Eastern Virginia Medical School, sees patients in the office and spends the bulk of his time in the ICU when he’s not authoring papers and giving lectures.
We are very pleased to honor these three physicians for their previous and future contributions to the field of pulmonary and critical care medicine. References: 1. The History of the Lungs, https://web.stanford.edu/class/history13/earlysciencelab/body/ lungspages/lung.html 2. The Martyrdom of Andreas Vesalius, http://www.ncbi.nlm.nih.gov/pubmed/2208869 3. A thousand years of pulmonary medicine: good news and bad, J. F. Murray, European Respiratory Journal 2001 17: 558-565 4. The History of the Lungs, https://web.stanford.edu/class/history13/earlysciencelab/body/ lungspages/lung.html 5. Famous Scientists: the Art of Genius 6. A thousand years of pulmonary medicine: good news and bad, J. F. Murray, European Respiratory Journal 2001 17: 558-565
Detect Lung Cancer Early with CT Lung Screening
Low-dose CT Lung Cancer Screenings—now covered by Medicare and most commercial health insurance—are saving lives for asymptomatic patients 55 years and older with a 30-pack-year smoking history. The Sentara Cancer Network provides doctors with an easy how-to guide to the required shared decision making visit, and offers patients convenient locations throughout Hampton Roads. • Chesapeake • Gloucester • Hampton
• Isle of Wight • Newport News • Norfolk
• Suffolk • Virginia Beach • Williamsburg
For more information, call 1-855-EARLY-DX (1-855-327-5939). Sentara.com/ScreenMyLungs Your community, not-for-profit health partner
Fall 2016 Hampton Roads Physician | 9
C. DELP GIVENS, JR., MD Pulmonary Medicine/Sleep Center Riverside Health System
D
elp Givens says he was accident prone as a kid. “From the time I was four or five, I was always in the hospital or the doctor’s office for one reason or other,” he says. “I’d run into something, break a bone or get a cut and need stitches. I developed a fascination with human physiology.” Luckily, he grew out of his awkward stage, but he never lost the fascination. He completed his undergraduate and medical school degrees at the University of Virginia, where he was drawn to internal medicine because “I like to analyze things, and solve problems.” Dr. Givens did his internship at Strong Memorial Hospital at the University of Rochester Medical Center. He describes his first rotation as “the intern’s nightmare. It was the
10 | www.hrphysician.com
Intensive Care Unit,” he says, “and almost nobody wants to do ICU first because the patients are so sick, and you’re not all that sure of yourself yet.” But he was paired with Dr. Richard Hyde, Chief of the Pulmonary Medicine unit, who Dr. Givens says “literally turned me on to lung pathophysiology and pulmonary diseases.” Despite the crushing schedule – working 18 hours a day, call every other night, sleeping maybe six out of every 48 hours, dealing with desperately ill patients and their families – he was exhilarated by the work of pulmonary and critical care medicine. He completed a fellowship in pulmonary and critical care at Vanderbilt University Medical Center, where he trained with Dr. Brevard Haynes, one of the first wave of sleep medicine clinicians. Dr. Givens was again fascinated – “I’d do my research
during the day,” he says, “and afterward, I’d go over to Dr. Haynes’ lab and work with his team. It wasn’t a formal part of the curriculum, but I was really interested in it.” As a result of Dr. Haynes’ mentorship, Dr. Givens was able to sit for the original American Board of Sleep Medicine exam. He is also American Board of Internal Medicine certified in Pulmonary Medicine, Clinical Care Medicine and Internal Medicine. Dr. Givens moved to Hampton Roads to begin his medical practice in 1987. “Sleep medicine was still a very young discipline in the late 1980s,” Dr. Givens explains. “There wasn’t a formal fellowship at that time. The physicians who trained in sleep usually did so as part of pulmonary or neurology fellowships, or psychiatry residencies. There weren’t that many of us.” There were so few, in fact, that his colleagues kid him about the number on his Board certificate: 214. In 1987, the only sleep center for all of Hampton Roads was at Eastern Virginia Medical School, under the direction of the renowned Dr. Catesby Ware, so Dr. Givens established the sleep center at Riverside Regional Medical Center, eliminating travel, traffic and and tunnel for residents on the Peninsula seeking help for sleep disorders. The most common of these disorders is sleep apnea syndrome – a disruption in breathing during sleep. It was an Australian respiratory doctor who invented the technology that remains the best method of treating severe sleep apnea syndrome: in 1980, Dr. Colin Sullivan perfected a means to apply positive pressure through the nasal airways to alleviate obstructed passageways – the Continuous Positive Applied Pressure machine, or CPAP – an effective medical treatment that obviated the need for tracheostomy surgeries in most cases. Sleep apnea syndrome is far more common than is generally realized, Dr. Givens says: “The number quoted most recently from epidemiology studies is 15 percent of adult men have sleep apnea, and five percent of adult women, with a further increase in incidence after menopause.”
There’s also a strong link between sleep apnea and obesity, although not as great as once thought. “The data is that about 70-75 percent of people with sleep apnea syndrome are overweight or obese,” Dr. Givens notes. “For many patients, as their obesity gets worse, their sleep apnea worsens. When they lose weight, sleep apnea improves significantly for the majority of patients. And while even significant weight loss doesn’t eliminate sleep apnea entirely for a third to a half of patients, it’s definitely a step in the right direction.” Over Dr. Givens’ career to this point, pulmonary, critical care and sleep medicine have each accounted for about a third of his practice. That will change in 2017: “The number of patients with sleep disorders has skyrocketed, and continues to,” he explains. “There are four other pulmonary and critical care physicians in our group, one of whom – Dr. Eric Weiner – also practices sleep medicine. In order to respond to our community’s growing needs, I will shift my emphasis primarily to evaluating and managing these patients.” And he’ll have an effective new modality to offer: for a certain number of patients diagnosed with obstructive sleep apnea, he is excited about the potential for Inspire upper airway stimulation therapy approved by the FDA. “It fits in the chest wall like a pacemaker,” Dr. Givens tells them. “There’s one lead that goes to the tongue muscle and one to the diaphragm, which senses when they’re about to take a breath in. It then delivers a small amount of current so that the tongue moves forward just enough to keep the airway open so they don’t snore – but more importantly, they don’t have apnea.”
Fall 2016 Hampton Roads Physician | 11
MELHEM A. IMAD, MD Chesapeake Regional Healthcare Interventional Pulmonology Bayview Physicians, Pulmonary Medicine of Virginia Beach
H
ad it not been for the fact that English medical textbooks cost less than French ones, Dr. Melhem Imad might be practicing pulmonary medicine today in France rather than the United States. Growing up in the small town of Batroun in Lebanon, he had studied both French and English, so those savings ultimately - if indirectly - resulted in him coming to America. He’d always known he’d eventually leave Lebanon: “We’ve always traveled,” he says. “It’s a common thing. There are more Lebanese outside of Lebanon than in the country. You either go to Europe or to the United States.” After graduating from the Lebanese University of Medical Sciences in Hadath, he did a rotating internship at the Lebanese University in Beirut. And in 2001, he began an internship and residency in internal medicine at New York’s Staten Island University Hospital, where he pursued a medical pathway rather than surgical. “I preferred the mystery and the problem-solving aspect of diagnosing and caring for patients,” he says. “I liked the intensity of internal medicine.” He was particularly interested in pulmonary medicine, and especially the relatively new field of interventional pulmonology. His research led him to apply for and receive a three-year fellowship for pulmonary and critical care at the University of Texas Medical Branch in Galveston. He enjoyed the curriculum at the University of Texas, but there were newer procedures in interventional pulmonology that weren’t being taught there. He spent a good deal of energy “jumping through hoops,” he says, convincing his program to let him train on elective rotations at some of the institutions that were teaching those procedures. His persistence was rewarded: he completed a four-week rotation in interventional pulmonology at the Cleveland Clinic and six-weeks at the University of Pennsylvania. By then, he had spent half of his six-year visa getting training, so he went to work, began the process of naturalization, and came to Hampton Roads to join Pulmonary Medicine of Virginia Beach. “I wanted to be on the East Coast,” he says, “because it’s closer to Europe and to Lebanon. And since I’ve always lived near the beach, I wanted that environment as well. Hampton Roads was a perfect location.” He brought with him innovative new technology and procedures. “We started doing endobronchial ultrasound, which is now a very common procedure in the hospitals,” he says, “but in 2007, no one was doing it. EBUS allows us to stage lung cancer and inflammatory diseases affecting the lungs, and lets us biopsy lymph nodes, without having to do surgery, through transbronchial needle aspiration.” Still, Dr. Imad felt his training was incomplete, and when he learned about a fellowship opportunity at Johns Hopkins in interventional pulmonology, he
12 | www.hrphysician.com
applied. He was recommended by his former colleagues at the University of Pennsylvania, and was accepted. “After three years in private practice, it meant going back into training for a full year,” he remembers. “It meant a change of lifestyle, and a change of finances.” But for a physician dedicated to perfecting his knowledge of his chosen field, it was an opportunity he couldn’t refuse. He returned to full-time employment with Pulmonary Medicine of Virginia Beach, and sees patients as an Interventional Pulmonologist at Chesapeake Regional Healthcare. He has also added the Directorships of Interventional Pulmonology and the Respiratory Department at Sentara Virginia Beach General Hospital to his resume. “Most of the work we’re doing is with lung cancer patients,” he says. “There’s been more research, especially in the area of genetic testing for lung cancer.” Recently, he explains, it’s been possible to look deeper into the genetics of tumors themselves, and the receptors on the tumors. “Certain genes that make certain tumors are susceptible to certain drugs as opposed to others. The differences in the genetics of those tumors made researchers more interested in trying to target those differences and develop drugs to target only those receptors. So lung cancer is no longer just lung cancer; it’s no longer small cell or non-small cell. It’s allow-
ing us to give more correct treatments with fewer side effects.” But, he cautions, “We’re far from perfect. And lung cancer is still the number one killer – more than breast, colon, and everything else.” Recently, approval was granted from the Cancer Institute to look for early lung cancer in people who smoked a certain amount for a certain number of years, so “we can do a yearly CT scan to look for early lung cancer while we can potentially cure it. Interventional pulmonology is responsible for advances in endoscopic procedures and other less invasive procedures to treat problems that lung cancer can cause, like putting in stents and doing laser and burning tumors inside the airway so people can breathe better.” In addition, Dr. Imad has performed procedures that can help emphysema patients breathe more easily by putting certain types of valves in their airways, or by deflating hyperinflated lungs. “Some of these have been on the horizon for a while and are being studied,” he says, “but they’re still not approved by the FDA. We’re hoping that approval comes soon.” Dr. Imad is an unrelenting advocate of smoking cessation. “We’re fighting lung cancer far better than we did years ago,” he says, “but I still see it every day. I diagnose it at least twice a week. I try to give these patients hope when I can, because there’s so much more now that we can do. But I’ll never stop trying to get people to quit smoking.”
Fall 2016 Hampton Roads Physician | 13
PAUL E. MARIK, MD Professor of Medicine and Chief of Pulmonary and Critical Care Medicine Eastern Virginia Medical School
O
n the wall of Dr. Paul Marik’s office in Hofheimer Hall is a beautifully illuminated and calligraphed rendition of the Hippocratic Oath, a gift to the graduating students of the Witwatersrand Medical School in Johannesburg, South Africa. Medical school was a foregone conclusion for Dr. Marik, from his earliest years as a student. “It was just my destiny,” he says. “There wasn’t a particular moment when I decided – I just always knew I’d go.” Students in South Africa studied six major subjects: English, Afrikaans and four other courses they could choose. “I always went for the sciences: maths, science, algebra,” Dr. Marik says. “That’s what I liked to do.” When standard vocational tests indicated the student should pursue pharmacy, it made perfect sense. But first came medical school. In South Africa, that meant six years plus an internship. At the time, South Africans had compulsory military training, so Dr. Marik served as an Army doctor during the time of the Cuban intervention in Angola. He served most of his tenure at a teaching hospital in Pretoria, but then spent three months in Angola, with a gun on his shoulder and a bucket of medicine at his side. “We looked after the local people, like a free clinic,” he explains. “We’d see as many as 200 people a day, with injuries that needed to be sewn up and infections that needed antibiotics. And we’d treat soldiers who’d been injured in battle, stabilizing them so they could fly out for treatment. It was invaluable training.” Next came residency – four years at the University of Witwatersrand, in Johannesburg. He worked in a tertiary care hospital in Soweto, caring for patients as far away as Nairobi. “It was the only hospital between Soweto and Cairo that could do dialysis,” he says, “and because testing wasn’t as advanced as it is today, we had to hone our clinical skills. We got enormous experience and exposure there.” After residency, Dr. Marik became an attending in Critical Care, and took advantage of the many opportunities the University offered for additional training. He earned a Diploma in Anesthesia in 1989, and a year later received a Bachelor of Science in Pharmacology, as well as a Diploma in Tropical Medicine and Hygiene. “I just liked learning,” he says, “and these were opportunities I couldn’t pass up.” Realizing that in South Africa, the future for academic medicine wasn’t bright, Dr. Marik decided to leave his homeland. After interviews in the US (New York City) and Canada, he chose to pursue a fellowship in critical care at the University of West London in Ontario, where he studied with Dr. William Sibbald, a noted critical care physician.
14 | www.hrphysician.com
A projected physician surplus resulted in a cutback on medical school positions, and Dr. Marik returned to the US, ultimately leaving Philadelphia to assume the role of Professor of Medicine and Chief of Pulmonary and Critical Care at EVMS. “There’s a far different atmosphere here than in Philadelphia,” he says. “There are four medical schools within miles of each other in Philly, and sixty hospitals in greater Philadelphia. Here, there’s one tertiary care facility for all the people on the southside of Hampton Roads. And because there’s such diversity in the field of pulmonary and critical care medicine, we see an enormous spectrum of pathology from all over. It’s not the same thing every day.” In fact, Dr. Marik says, even after over thirty years of practicing pulmonary and critical care medicine, he still sees conditions that he’s never seen before. “There aren’t many specialties you can say that about,” he says. “That’s why it’s so fascinating, and why there really is nothing else I’d rather do.” Dr. Marik is the author of The Handbook of Evidence-Based Critical Care. Now in its 3rd edition, the Handbook is widely used throughout the world. His scholarly contributions also include 380 peer reviewed articles and 308 lectures at national international meetings, and invited grand rounds, serving as a reviewer for a number of major medical journals, and authoring 81 book chapters. His contributions have resulted in his twice receiving the SCCM Presidential Citation for Outstanding Contributions to the Society of Critical Care Medicine. Most recently, Dr. Marik was invited to present at the National Institutes of Health on hemodynamic assessment and fluid management. He is currently working on a project that he says has the potential to be the most significant and exciting accomplishment of his entire career – an incredible claim for a physician who has been recognized throughout the world for his contributions to the field of pulmonary and critical care medicine. “Sepsis affects about 20 million people across the planet,” Dr. Marik explains. “It has a mortality rate of about 40 percent, except in the most underdeveloped countries, where the death rate is around 60 percent.” Sepsis kills nearly 250,000 thousand Americans every year. Pharmacologists and scientists have spent years and invested millions of dollars looking for a cure. Dr. Marik and his team have been doing studies, he says, “and if we’re right, we may have a novel way of managing sepsis.” He and his colleagues are in the process of finalizing their findings, and intend to publish before the end of the year. Of his estimable career, Dr. Marik says, “Being a physician is a great privilege. After thirty years, I am still excited and amazed by it.”
Fall 2016 Hampton Roads Physician | 15
GOOD DEEDS
problems haven’t been addressed. They often end up in emergency rooms until they find a clinic that will see them, but emergency rooms are not the place to treat chronic conditions. Some are so sick they need hospitalization, which for them means MCV. And so many lack funds or transportation to get there.” Many of these patients need dialysis urgently. They don’t know or don’t understand that they have a life threatening disease that might take their lives, Dr. Wang says. She tries to educate them, reviewing their lab results, diet and social habits with them and trying to teach them take proper care of themselves. Although her time at the Clinic is limited, she has many ‘regular’ patients there. “I cannot see them as often as I see my private patients,” she says, “but I see them when they come into the clinic. And when I’m not there, I am frequently in contact with OTMC providers, providing guidelines about specific treatments for each patient.” This includes medications and injections: “Olde Towne has a very strong medication program,” Dr. Wang says. “I can set up the guidance for patients to get these injections through their nurses or doctors.” It takes quite a bit of administrative time, but it’s time she has spent willingly for more than ten years. “When I first heard that the Clinic needed a kidney specialist to treat those indigent patients with no insurance, I knew I could definitely provide that kind of service to the community,” she says. “I started going a couple of hours on the first Monday of the month. Since then, my hours have increased as the need has increased. I haven’t stopped.” Dr. Wang feels strongly that physicians have a responsibility to the community in which they practice. “I feel great if I can offer something to these patients,” she says. “It doesn’t matter to me if they have no money,” she adds. “We’re all human beings and we all deserve to be treated with dignity, equally. Whatever I can do to help, I will do.” She adds, “It’s rewarding; it makes me feel so good to give something, even though I have to make time to do that – but I think it’s the right thing to do.”
Shuping Wang, MD
Peninsula Kidney Associates
D
r. Shuping Wang has practiced nephrology in the Williamsburg area since 2005. She has a special passion for geriatric care and specializes in the management of chronic kidney disease, hypertension and kidney related anemia and bone disease. A graduate of Tianjin Medical University in the People’s Republic of China, Dr. Wang continued her medical education in the United States at Pennsylvania State University Hershey Medical Center, Internship in Internal Medicine. She served her residency in Internal Medicine at the University of Virginia Health System, where she also completed a fellowship in nephrology. In addition to a full-time practice, and the Directorship of the DaVita Williamsburg Medical Center, Dr. Wang regularly volunteers her time treating patients at the Olde Towne Medical & Dental Center, which addresses the needs of Greater Williamsburg’s uninsured and medically underserved residents. “These are patients with chronic kidney disease,” she says. “They are almost without exception in bad health. Because they’ve been without insurance, their health care
16 | www.hrphysician.com
If you know physicians who are performing good deeds – great or small – who you would like to see highlighted in this publication, please submit information on our website – www.hrphysician.com – or call our editor, Bobbie Fisher, at 757.773.7550.
A surgery team just for kids. Children’s Hospital of The King’s Daughters offers the most comprehensive pediatric surgical care for children in Hampton Roads, northeastern North Carolina and Virginia’s Eastern Shore. In addition to general pediatric surgery, we offer care in five pediatric subspecialties including cardiac surgery, neurosurgery, orthopedic surgery, plastic surgery and urology. Our team also includes more than 20 pediatric anesthesiologists and dozens of OR nurses.
CHKD’s state-of-the art facilities include a new cardiac catheterization lab and cardiac operating suite at our main hospital in Norfolk and two CHKD Health and Surgery Centers in Newport News and Virginia Beach for outpatient surgery. More than 20 pediatric surgeons. More than 13,000 surgeries last year. And more than 50 years of experience in pediatric surgical care. That’s what makes CHKD more than a hospital.
Our surgeons have pioneered non-invasive techniques for the correction of chest wall abnormalities at our worldrenowned Nuss Center, and our craniofacial reconstruction program is proud to be the American home of the international charity Operation Smile. Our multidisciplinary spine team includes orthopedic and neurosurgeons and is a regional leader in spine surgery for children and adolescents.
Learn more at CHKD.org.
OUR SURGERY TEAM Cardiac Surgery Felix Tsai, MD
Neurosurgery
John Birknes, MD Joseph Dilustro, MD Gary Tye, MD
General Surgery
Frazier Frantz, MD Robert Kelly, MD Ann Kuhn, MD Michelle Lombardo, MD Margaret McGuire, MD Robert Obermeyer, MD
Orthopedics/ Sports Medicine
Marc Cardelia, MD Allison Crepeau, MD Cara Novick, MD Jeremy Saller, MD Sheldon St. Clair, MD Carl St. Remy, MD Allison Tenfelde, MD
Plastic Surgery
George Hoerr, MD Jesus (Gil B.) Inciong, MD
Urology
Charles Horton, MD Jyoti Upadhyay, MD Louis Wojcik, MD
A D VA N C E D P R A C T I C E PROVIDERS
JEFFREY BELCHER, MPA, PA-C
Pediatric Radiology Physician Assistant at Children’s Hospital of the King’s Daughters
P
eople often go into medicine as a result of growing up with a relative in the medical field. Almost as many choose the career after watching a loved one go through a serious illness. In the case of Jeffrey Belcher, it was both – and it was the same person. His mother went through the Sentara nursing program in 1984, and
he remembers her spreading her books and study materials out on the floor. “I’d sit beside her and go through anatomy with her, and it was a big influence,” he says. “From that time on, I was interested in the medical field” – so much so that he majored in biology and followed a pre-med curriculum at the University of Virginia. While working at Eastern Virginia Medical School as a Research Assistant, Mr. Belcher was encouraged by a prominent physician to explore the up and coming field of Physician Assistant. He did so, and was accepted into the Physician Assistant program at EVMS. Early into the curriculum, his mother was diagnosed with end stage renal disease, which would require multiple vascular surgeries and eventually dialysis. He wanted to learn more about renal physiology and vascular surgery, so he could better understand and help his mother. During an elective clinical rotation with a vascular surgery Physician Assistant, he found the combination of surgical skill and clinical application just what he was looking for in a future career. Upon graduation in 2005, he took a position at the UVA hospital, where he trained in Interventional Radiology, honing skills such as ultrasound guided PICC placement, CVL/ temporary dialysis catheter placement, tunneled HD catheter placement, and subcutaneous port placement. He ultimately returned to Norfolk and took a unique position working at the Children’s Hospital of the King’s Daughters in the Department of Radiology. Throughout his tenure at CHKD, he has worked diligently to develop significant working relationships with the area pediatricians and pediatric specialists. The position of pediatric radiology for a Physician Assistant is very specialized, and currently very rare. Mr. Belcher is one of only a few in the country, and may be the only one in Virginia. A typical daily schedule includes both inpatients and outpatients, their ages ranging from premature neonates to young adults. On these patients, Mr. Belcher performs fluoroscopy to evaluate the upper and lower gastrointestinal tract and urinary systems, allowing the precise placement of a variety of feeding tubes. The work is critical because of the very small window of time available, as these young patients are awake and anxious, and their parent(s) can be present as well. “It can be stressful,” he says, “so I have to bring all of my resources, clinical knowledge and experience to bear to ensure we’re getting the right number of images, using the least amount of radiation possible.” Mr. Belcher is quick to give credit to his colleagues and coworkers at CHKD. “Every day, everyone works extremely hard, to be sure every patient has the absolute best outcome,” he says. “It takes a very special skill set to work with children, let alone perform procedures on them. Our medical team brings together several caring hands to help families throughout the process. Being a part of a nationally ranked freestanding children’s hospital filled with talented medical professionals adds to that positive experience. There is no greater satisfaction than having a positive impact in a child’s life.” If you work with or know a Physician Assistant or Nurse Practitioner you’d like us to consider, please visit our website – www.hrphysician.com – or call our editor, Bobbie Fisher, at 757.773.7550.
18 | www.hrphysician.com
SPORTS MEDICINE & ORTHOPAEDIC CENTER
…expanding innovative care throughout southeastern Hampton Roads
O
n October 31, 2016, the doors will open to a new building on Discovery Drive in Chesapeake, Virginia. The building will be one of three locations of Sports Medicine & Orthopaedic Center, a venerable practice of fellowshiptrained, Board certified orthopaedists that has provided innovative, state-of-the-art care to the people of southeastern Hampton Roads since 1984. The practice began 32 years ago, when an orthopaedist named Richard Holden opened his first office in Chesapeake. Dr. Holden, now retired, was soon joined by Dr. Michael Romash and a year later by Dr. Samuel Brown. Together they built the practice that is today widely known by its initials: SMOC. At the time, they were the only fellowship trained orthopaedists in the city. “We had a clear vision of how we wanted to practice,” says Dr. Romash, SMOC’s senior physician. “We were both former military, and had both practiced in tertiary care hospitals. Our vision was to bring compassionate, tertiary level orthopaedic care to our patients.” 20 | www.hrphysician.comTodd Rauchenberger, practice administrator
Image courtesy of PF&A Design
Promotional Feature
Orthopaedic Care Just Got a New Address in Chesapeake
Image courtesy of PF&A Design
This they accomplished by a three-tiered approach that remains the practice’s mission today: • to expedite the effective diagnosis, treatment and rehabilitation of orthopaedic patients; • to implement innovative, cutting- edge technological solutions when appropriate; • to optimize individual performance in healthcare through building trust and communication between doctor and patient. In the early days of the practice, the physicians went to hospitals all throughout the region. And as they treated more and more patients, they began to see a trend. As the City of Chesapeake expanded, it was increasingly clear that they would have to expand with it to accommodate the needs of its growing population. They welcomed those opportunities, inviting only orthopaedists who matched their own qualifications of specialization and tertiary care experience to join their practice. The reputation of the practice as an exceptional and consistent provider grew as the community grew. One reason for its success has been an important philosophy of the practice, from its earliest days and continuing today – its focus on the particular needs of each patient. A patient with joint problems sees only the physician with special training in joint care. Likewise, patients with upper extremity conditions are seen by a fellowship trained surgeon in that field. Those complaining of spine issues are cared for by a spine specialist. As the region expanded, so did SMOC’s physical presence, into other sections of Chesapeake and into the rapidlygrowing area of Suffolk. Through careful planning and strategic thinking, as specific population needs were identified
in different areas of Chesapeake and Suffolk, they opened additional offices and spine centers. For a practice that has since its earliest days focused on the health and comfort of its patients, these expansions made sense: they signaled shortened wait times for appointments with providers, and less inconvenience to patients traveling to see them. Today, as SMOC celebrates the opening of its newest location on Discovery Drive, the practice consists of 13 physicians, all Board certified and all fellowship trained. Nine are orthopaedic surgeons, two are spine specialists and two are interventional pain medicine physicians. Each of the practice’s eight Physician Assistants is trained in all aspects of orthopaedic care, but each has received specialized training to support a specific orthopaedist. Rounding out the team are eight Physical and Occupational Therapists.
Innovation on Discovery Drive Among the state-of-the-art technological and surgical equipment in the new office is SMOC’s second fluoroscopy unit, complementing the one located at the Spine Center at Chesapeake. The original fluoroscopy unit has been one of the mainstays used by pain medicine physician Dr. Victor Tseng for patients in that office. With the Fluoroscopy unit, Dr. Tseng could provide injections into various parts of a patient’s body, including the spine, as well as provide procedures like radiofrequency ablation, Fall 2016 Hampton Roads Physician | 21
“We had a clear vision of how we wanted to practice,” says Dr. Romash, SMOC’s senior physician. “We were both former military, and had both practiced in tertiary care hospitals. Our vision was to bring compassionate, tertiary level orthopaedic care to our patients.”
Michael M. Romash, MD
22 | www.hrphysician.com
spinal cord stimulation, vertebroplasty and discography, among others. However, prior to the opening of the Discovery Drive location, Dr. Tseng split his time between Suffolk and the Chesapeake offices. With the acquisition of the second fluoroscopy unit, SMOC has hired an additional pain medicine physician, Dr. Michael Ingraham, there will now be a full-time pain specialist with ready access to the fluoroscopy unit every day at both locations. “We’re fortunate to have these two skilled and highly trained pain medicine physicians in Hampton Roads,” says Dr. Bryan Fox. “They are huge assets to our patients with chronic pain and nonsurgical issues.” In addition, new technology allows SMOC to offer digital radiography to all of its patients. “Digital radiography was available in some of our locations, but not all,” says Dr. David Goss. “Now we can offer it to patients in each of them.” Among the many benefits are clearer images produced more quickly, which can be populated into the electronic medical record instantaneously and easily forwarded to referring physicians and hospitals. There’s an additional bonus for patients: in addition to exposing them to less radiation, digital radiography means less time spent being filmed, with less discomfort.
“Today, with everything under one roof, clearly and conveniently marked, the space is much more efficient, and from the patient’s perspective, far more conducive to the various stages of orthopaedic care. “
David G. Goss, MD
For patients, however, one of the best features of the new location may well be its all inclusive, well-planned facility. The Wimbledon Square location was not one or two, but three buildings. Orthopaedists were in one, physical therapy in another, and SMOC’s spine and pain medicine doctors a quarter-mile down the road in yet another. “We had no room to add new providers or new equipment,” Dr. Goss says. “Orthopaedic patients are often dealing with considerable pain, and could be confused by having to shuttle back and forth between buildings to see different providers. For some, it could seem we were sending them to different providers.” Today, with everything under one roof, clearly and conveniently marked, the space is much more efficient, and from the patient’s perspective, far more conducive to the various stages of orthopaedic care. “Patients aren’t inconvenienced,” Dr. Goss adds, “so there’s a much greater sense of continuity.”
What the opening of Discovery Drive means to the community in Chesapeake “Our group is one of the busiest orthopaedics practices in the City,” says Dr. Samuel Brown. “With this new location and its many innovations, we’re able to serve more patients more quickly, and offer them the latest medical and technological advances, in a more efficient atmosphere. We’ve not just
expanded our existing services, but with the addition of another joint replacement surgeon and another pain medicine physician, we’re better able to field referrals from emergency departments, family docs and even patients themselves.”
Anticipating the future: further expansion into Suffolk SMOC has had a presence in the Belle Harbor section of Suffolk since 2012, where they serve patients from Smithfield, Newport News, Carrolton and the Western Branch of Chesapeake as well. “We’ve studied all of the populations we serve very aggressively,” says Dr. Fox, “to ensure we’re offering them what they need, where they need it. We know that North Suffolk is an area of very rapid growth, with a heavy concentration of active older adults who increasingly need joint replacements and spine care. We know the demand for orthopaedic care is growing, and we plan to be ready for those patients.” Thus, SMOC is already looking at opportunities to expand into North Suffolk, which unlike many of the surrounding cities, still has ample land mass available for development.
It’s all about being strategic and efficient So says Dr. Anthony Bevilacqua, adding, “and we’ve been very fortunate to have on our staff a capable, strategic thinker
“With this new location and its many innovations, we’re able to serve more patients more quickly, and offer them the latest medical and technological advances, in a more efficient atmosphere. “
Samuel I. Brown, MD
Fall 2016 Hampton Roads Physician | 23
“We’ve studied all of the populations we serve very aggressively,” says Dr. Fox, “to ensure we’re offering them what they need, where they need it.” like Todd Rauchenberger, who has been SMOC’s administrator for seven years. Todd has been a tremendous Bryan A. Fox, MD asset in helping us identify potential areas for growth, and in diversifying our practice.” Additionally, Dr. Bevilacqua notes, “Todd has helped us stay ahead of the multiple governmental regulations that are part of practicing medicine today.” Case in point: the acquisition of digital radiography. “The government, through the healthcare act, is forcing physicians who do x-rays to purchase and implement digital radiography,” Dr. Bevilacqua says. “On January 1st, those who haven’t been able to afford financial outlay will be penalized a percentage of receipts on
24 | www.hrphysician.com
reimbursement. Through strategically laying out what we have to do to ensure compliance with these regulations, Todd has enabled us to comply well in advance of the federal deadlines.” And that, he’s quick to note, means that SMOC physicians are able to focus on practicing orthopaedic medicine. In that vein, they have begun doing many more procedures in the office, saving their patients substantial sums of money. For instance, a hip injection in an ambulatory surgery center can cost between $500 and $800, before factoring in the physician’s time and the cost of medication; whereas SMOC is able to reduce those costs and pass on similar savings of time and money to patients for other procedures, should they choose them. Staying alert to the changing health care marketplace while continuing to provide standard-of-care service to patients in
PHYSICIANS Chesapeake Location 501 Discovery Drive Michael M. Romash, MD – Foot, ankle, reconstruction surgeon Samuel I. Brown, MD – Orthopaedic surgeon Scott E. Grabill, DO – Orthopaedic surgeon, joint replacement specialist Gordon J. Iiams, MD – Hand and upper extremity surgeon The Spine Center of Chesapeake 501 Discovery Drive David G. Goss, MD – Orthopaedic spine surgeon Richard D. Guinand, DO – Orthopaedic spine specialist Victor W. Tseng, DO – Interventional pain medicine
“We’ve been very fortunate to have on our staff a capable, strategic thinker like Todd Rauchenberger, who has been SMOC’s administrator for seven years.” Anthony M. Bevilacqua, DO
need of exceptional orthopaedic care is SMOC’s formula for a successful future. As every practicing physician and medical administrator knows, the changes taking place within healthcare today are complex, challenging the profession to adapt, and adapt quickly. The fee-for-service model is soon to be a thing of the past, and reimbursements will depend on a practice’s ability to demonstrate value. For SMOC, value has always been a guiding force. The practice’s unrelenting pursuit of the highest quality care, along with its history of visionary leadership, have ensured that SMOC will help shape – rather than be shaped by – orthopaedic care in southeastern Hampton Roads.
Suffolk Locations 150 Burnett’s Way Anthony M. Bevilacqua, DO – Orthopaedic surgeon Anthony J. Distasio, MD – Trauma surgeon, joint replacement specialist Thomas M. Bergfield, MD – Hand and upper extremity surgeon The Spine Center of Suffolk 150 Burnett’s Way Bryan A. Fox, MD – Orthopaedic spine surgeon Michael J. Ingraham, MD – Interventional Pain Medicine Belle Harbour 3920 Bridge Road, Belle Harbour Anthony M. Bevilacqua, DO – Orthopaedic surgeon Ali R. Jamali, MD – Orthopaedic surgeon
Fall 2016 Hampton Roads Physician | 25
Non-Surgical Options for Men with Prostate Cancer By Bradley Prestidge, MD, MS Regional Medical Director for Radiation Oncology Bon Secours Cancer Institute in Hampton Roads
M
en facing the diagnosis of prostate cancer have both surgical and non-surgical treatment options, depending on their stage of disease. If the cancer is believed not to have spread outside the prostate, they can undergo radical prostatectomy, removing the gland and some of the surrounding tissue, including the seminal vesicles. Most often, there are also a number of non-surgical treatment options. Four of those options involve radiation therapies:
External Beam Radiation
Image guided intensity modulated radiation therapy (IMRT or IGMRT), is an effective external beam treatment using high doses of radiation to kill prostate cancer cells. It requires a brief daily (Monday through Friday) treatment for up to nine weeks.
Brachytherapy
Brachytherapy involves placing radioactive pellets inside an organ or
tumor. There are two types of prostate brachytherapy: low dose rate (LDR) and high dose rate (HDR.) LDR brachytherapy, sometimes called “seed implants” or “permanent brachytherapy,” is an outpatient procedure for patients with cancer confined to the prostate, in which tiny radioactive seeds are permanently placed in the prostate. These seeds emit low levels of radiation for an extended period, and need not be removed after becoming inert. The patient leaves the
More Sub-Specialty Care. When you need orthopedic treatment, it’s good to know an expert with a high level of training and skill is here to care for you. Some of our orthopedic sub-specialties include: • Total joint replacement • Shoulder • Hand
• Foot & ankle • Sports medicine • Trauma
Orthopedic Specialists
757-337-3366 riversideonline.com/ortho
EXPANDED OFFICE HOURS INCLUDES SATURDAY APPOINTMENTS 26 | www.hrphysician.com
procedure with only minor safety precautions. HDR brachytherapy is not offered at all radiation facilities. The concept is similar to LDR, but instead of implanting multiple permanent seeds, a single radioactive pellet is inserted robotically through a hollow catheter or needle placed in the prostate under general anesthesia. The exact position of the pellet in each needle and the number of seconds that the pellet dwells in each position is computer driven and the entire treatment takes from 5-10 minutes to deliver. HDR prostate brachytherapy may be given as monotherapy, but is more commonly used in combination with external radiation as a “boost.” However, because of a growing interest in shorter, more hypofractionated radiation approaches, HDR brachytherapy for prostate cancer used as monotherapy is being more intensively studied. The Bon Secours Cancer Institute at DePaul is one of only eight sites in the country invited to participate in a national protocol to be implemented next year providing HDR brachytherapy in a single, stand alone treatment for early and intermediate risk prostate cancer.
Combination Therapy
Depending on the stage of prostate cancer, very often a combination of therapies is recommended – for example, five weeks of daily radiation with HDR brachytherapy as a boost, or five weeks of external radiation using LDR brachytherapy as the boost.
Stereotactic Beam Radiation Therapy
SBRT is a technologically sophisticated form of external beam radiation delivered with even greater precision and at a much higher dose per fraction than conventional external beam treatment. Multiple radiation beams, or arcs, are designed to enter the body through various angles, intersecting at the prostate. Instead of eight to nine weeks of individual daily treatments, only five are required, spread out over two weeks. It is non-invasive, does not
require general anesthesia, and results in very high cancer control rates, comparable to surgery and the other non-surgical approaches described above.
Dr. Prestidge earned his medical degree from Uniformed Services University of the Health Sciences in Bethesda, MD, and served an internship in internal medicine at David Grant USAF Medical Center at Travis Air Force Base in Fairfield, CA. He served as an active duty Air Force physician and consultant to the Surgeon General for 12 years. In addition, he completed a residency in radiation oncology at Stanford University Hospital in Stanford, CA. www.bonsecours.com
Are you looking for a satisfying career and a life outside of work? Enjoy both to the fullest at Patient First. Opportunities are available in Virginia, Maryland, Pennsylvania, and New Jersey. Open 8 am to 10 pm, 365 days a year, Patient First is the leading urgent care and primary care provider in the mid-Atlantic with over 60 locations throughout Virginia, Maryland, Pennsylvania, and New Jersey. Patient First was founded by a physician and we understand the flexibility and freedom you want in both your career and personal life. If you are ready for a career with To learn more about fantastic career opportunities at Patient First, contact Patient First, please contact us. Recruitment Coordinator Eleanor Dowdy at (804) 822-4478 or Each physician enjoys: eleanor.dowdy@patientfirst.com or • Competitive Compensation visit prcareers.patientfirst.com. • Flexible Schedules • Personalized Benefits Packages • Generous Vacation & CME Allowances • Malpractice Insurance Coverage • Team-Oriented Workplace • Career Advancement Opportunities Fall 2016 Hampton Roads Physician | 27
MEDICAL U P D A T E
Accountable Care Organizations …and the next incarnation: MACRA/MIPS “There’s a lot changing in health care.” “There are all kinds of ways to describe it.” “It’s complex.” “This is a very confusing time, and most providers don’t understand the complexities.” “It’s very complicated.” THESE ARE JUST SOME OF THE COMMENTS WE HEARD AS WE BEGAN RESEARCHING THIS ARTICLE (A TOPIC REQUESTED BY OUR PHYSICIAN ADVISORY BOARD), BOTH FROM THOSE WHOSE NAMES AND COMMENTS ARE INCLUDED BELOW AND FROM OTHERS THROUGHOUT THE COMMUNITY. OUR THANKS TO EACH OF THEM.
T
o understand MACRA/MIPS, it’s important to understand the evolution of Affordable Care Organizations. It began in 2001, with the publication of a report by the Institute of Medicine called “Crossing the Quality Chasm.” The report contained the then startling statement that: The U.S. health care delivery system does not provide consistent, high-quality medical care to all people. Americans should be able to count on receiving care that meets their needs and is based on
Richard Bikowski, MD, Eastern Virginia Medical School
28 | www.hrphysician.com
the best scientific knowledge – yet there is strong evidence that this frequently is not the case. Health care harms patients too frequently and routinely fails to deliver its potential benefits. Indeed, between the health care that we now have and the health care that we could have lies not just a gap, but a chasm.1 “The report basically said that our health system wasn’t doing a very good job,” says Richard Bikowski, MD, a family medicine physician with Eastern Virginia Medical School. Dr. Bikowski, a member of the Board of the physician-run Sentara Quality Care Network, continues, “The leaders of health care at that time said to change that, we had to do a few things.” Those “few things” included completely redesigning the way medical care was delivered in the United States. Care was no longer just about a physician delivering it, but rather became more about a team of care quality, care management; and as those practices began to evolve, there was talk about the practices getting together to work in collaboration. This was the genesis of the Patient Centered Medical Home. “An ACO is, essentially a network of patient centered medical homes and other quality minded physicians who are working together to provide care,” Dr. Bikowski says. “And whether you call it an ACO or a CIN, it’s essentially the same thing.”
In fact, the term Accountable Care Organization was prompted by Medicare, with the establishment of the Medicare Sharing Savings Program. “Medicare required that organizations set up a separate company from the health system or physician practice, an LLC at least, an entity with a legal structure and a board with specific committees – clinical, quality, etc. – that would sign a contract with CMS to participate in the MSSP program,” says Sally Hartman, Senior Vice President for Riverside Health System. “It referred to taking care of a particular population where you’re at some level of risk or have the opportunity for some kind of reward.” When the Affordable Care Act was enacted years later, it adopted the concept of the ACO and started to change the way physicians are paid: based on value, rather then volume. Under the Act, each ACO had to manage a minimum of 5,000 Medicare beneficiaries for at least three years. The ACO Medicare Savings, which began as a payment model, has morphed into a network of physicians and providers, including hospital systems, working together to give better value for the dollar: better care at lower cost. “It’s all part of the journey to value,” says Timothy Willox, MD, Chief Medical Officer with Bon Secours Medical Group.
“Right now, the payment model is feefor-service. It doesn’t reward reducing readmissions; it doesn’t reward reducing emergency department visits.” From the largest medical centers to small independent practices, tracking and reporting quality metrics has become a requirement of health care reform. For some, it has also become an overwhelming financial and administrative burden. Medicare has published more than 300 measures for physicians to report on. They
can choose the measures appropriate for their practice, but most of these measures are developed by physician expert groups like the AMA Physician Consortium on Quality Improvement. A 2015 article from Kaiser Health News, states ACOs are already becoming pervasive, but they may just be an interim step on the way to a more efficient American health care system. ACOs aren’t the end game.2 And in fact, in 2015, the US Senate overwhelmingly (98-2) passed the Medicare Access and CHIP Reauthorization Act (MACRA), repealing the Medicare Part B Sustainable Growth Rate reimbursement formula, making sweeping changes to the way Medicare pays for physician services. “Medicare is going to start tying its payments to how well physicians are doing with our patients,” Dr. Bikowski explains, “even if a physician isn’t in a network.”
Sally Hartman, Senior Vice President for Riverside Health System
MACRA created a new, pay-forperformance oriented Medicare reimbursement program called the Merit Based Incentive Payment System, or MIPS. It will base reimbursement of physicians on four categories: quality, resource use, clinical practice improvement, and meaningful technology use.
Our Women’s Pelvic Health Program is designed with You in Mind Urinary incontinence, overactive bladder symptoms, and pelvic health issues may affect your quality-of-life. Our Fellowship-trained Physicians offer comprehensive evaluation, surgical and non-surgical treatment options and will help you choose the treatment option that is best for you. Jessica M. DeLong, M.D. Kurt A. McCammon, M.D., FACS, FPM-RS Jennifer Miles-Thomas, M.D., FPM-RS Jeremy B. Tonkin, M.D. Ramon Virasoro, M.D.
Dedicated to Compassionate and Quality Care Now Accepting New Patients Appointments may be made by calling 757.457.5110 225 Clearfield Ave. | Virginia Beach, VA 23462 | www.urologyofva.net
Fall 2016 Hampton Roads Physician | 29
Small, independent physicians, whose Medicare cases represent as much as 50 percent of their practice, have bitterly complained about MACRA/MIPS. In a July 2016 column for the digital network Doximity, Niran Al-Agba, MD, wrote: Small, independent private practices are closing, increasing numbers of physicians are retiring, and fewer medical school graduates are choosing primary care. MACRA proposed reimbursement will decimate rural care as we know it. [It] will penalize 7 out of 10 small one-to-two physician practices in this country…because we will be overwhelmed complying with statistical reporting demands that do nothing to enhance the quality of care, instead of spending precious time seeing patients. Dr. Al-Agba describes a family practice physician whose Medicare payments were frozen for eight months due to a technical error. More than half of her patients were on Medicare. Without a small inheritance, her solo
Timothy Willox, MD, Chief Medical Officer with Bon Secours Medical Group
practice would have gone bankrupt. Dr. Al-Agba asks: Is this the future of medical care in this country? If we allow this MACRA atrocity to go into effect, who will be left to care for the sick, disabled, and elderly?3 It’s not an altogether unfair question, Dr. Willox says. “When you look at what physicians are being asked to do, if you don’t have a strong IT framework, a good electronic medical record system, 30 | www.hrphysician.com
and strong administrative support, you couldn’t be more at a disadvantage. If you’re an individual, or a one- or twoperson practice, it’s going to be difficult to do.” Clearly, doctors don’t want to be spending their time clicking a mouse, or checking a box. “They want to do what they do best,” Dr. Willox says. “They want to see patients, treat them and help them get better. That’s the challenge as we move into this world: how do we create efficiencies that work within the work flow, and harness the technology to enable us to remain efficient and take care of our patients.” But are things as grim as they seem to Dr. Al-Agba and other small rural practices? “There have been exceptions for certain physicians in the past,” Dr. Willox says, “and perhaps there should be a compromise in certain circumstances. If you’re a small practice in a rural, underserved area, caring for patients, I think you should be exempt. Why should you be penalized because you’re serving these people and don’t have the infrastructure to support the requirements?” Other options include joining organizations like Sentara’s Quality Care Network, which welcomes independent practices and solo practitioners to join, allowing them to reap the benefits of the network without requiring them to become part of the Sentara Health System. Likewise, Bon Secours Health System and Riverside Health System are exploring the possibility of inviting independent physicians to join their ACOs, and some of the larger medical groups are considering the possibility as well for their organizations. “We are very mindful of the physicians’ interest in maintaining their independence,” says Grace Hines, President of Sentara’s Quality Care Network (SQCN). “In fact, most of the board members who run SQCN are independent providers, and most physicians in the network itself are independent.” While there may be networks elsewhere that require exclusivity, Hines emphasizes that SQCN is not one of them. “Physicians can participate in our network, and if there’s another in this market, they can participate in that as well,” she says. “There are no
Grace Hines, President of Sentara’s Quality Care Network (SQCN)
restrictions other than a commitment to improve their quality and performance, while cutting costs effectively, and a desire to work collaboratively with all.” Still, some physicians are choosing to remain unaffiliated, willing (for the time being, at least) to absorb the penalties associated with not joining an ACO or other network. At least one specialist we spoke with reported joining an ACO and subsequently leaving it because the benefits weren’t apparent. It’s an individual choice for each individual professional and each practice. In future articles, we hope to share the experiences of area physicians, who are invited to contact our editor at 757.773.7550.
References: 1. Crossing the Quality Chasm: a New Health System for the 21st Century, report of the Committee on Quality of Health Care in America and the Institute of Medicine, July 19, 2001 2. Accountable Care Organizations, Explained, Jenny Gold, Kaiser Health News, September 14, 2015 3. How MACRA will decimate the private practice physician, Niran Al-Agba, MD, Doximity, July 20, 2016
Experience Excellence
Effective, non-surgical healing. Stem Cell or Platelet Therapy may be the answer for your patients. If their ligament strains, cartilage tears and other chronic or sports injuries haven’t healed with traditional treatments and they want to avoid surgery, call us for a consultation.
OSC PROVIDERS
We are proud to introduce
Boyd W. Haynes III, M.D.
Newport News, Virginia
Martin R. Coleman, M.D. Mark W. McFarland, D.O.
t
Orthopaedic & Spine Center
Jeffrey R. Carlson, M.D.
t
The Center for Regenerative Medicine
Robert J. Snyder, M.D.
Raj N. Sureja, M.D. Jenny L.F. Andrus, M.D. John D. Burrow, D.O. F. Cal Robinson, PsyD, MSCP
By harnessing the potential healing power of the human stem cell, OSC can effectively treat your patients for a variety of sports injuries and chronic conditions, including: arthritis, back pain, tennis elbow, rotator cuff tears, etc. To learn more, please visit our website at oscstemcell.com or call us at (757) 596-1900.
OPEN MRI CENTER
Experience Excellence at OSC.
250 Nat Turner Boulevard, Newport News, VA 23606
phone 757.596.1900 www.osc-ortho.com
WHAT MEDICAL PROFESSIONALS NEED TO KNOW ABOUT PATENTS
A
patent is a property interest granted by the federal government that permits the inventor to exclude others from using, making, selling, offering for sale, or importing the patented invention in the US for a limited time. This limited monopoly is granted in exchange for full disclosure of how to make and use the invention. The purpose of this disclosure is “to promote the Progress of Science and useful Arts.” The public benefits because it can build upon this knowledge, while the inventor benefits by the limited monopoly. A patent can be obtained for a new and useful “process, machine, manufacture, or composition of matter, or any new and useful improvement thereof.” Thus, a patent can be obtained for a new medical device, drug, biological agent, or method of treating, diagnosing, or administering medical services to a patient. The Patent Act requires the invention be new or novel, useful, and non-obvious to those skilled in the art to which the patent pertains. The patent must include a complete written description of the invention – including how to make and use it – along with any necessary drawings and a set of one or more claims that designate the metes and bounds of the inventor’s exclusionary rights. A patent can be assigned, licensed, bought, sold, or otherwise transferred in the same way as other property rights. One who, without the permission of the patent owner, makes, uses, sells, offers for sale, or imports the patented invention, may be liable for patent infringement. The remedy for infringement of a patent is a civil action in federal court. If the patent owner prevails, the infringer may be liable for damages in the form of lost profits or a reasonable royalty. The infringer may also be enjoined from further infringing activities, and may be liable for attorney’s fees. In general, there is no intent requirement 32 | www.hrphysician.com
By Matthew R. Osenga Goodman Allen Donnelly
for infringement, but if infringement is judged to be willful, the infringer may be liable for up to three times the amount of damages awarded. There are a number of potential defenses: there is no actual infringement; the patent is invalid because it fails to comply with some provision of the Patent Act; the inventor procured the patent by misstatements to or withholding information from the Patent Office.
What Should You Do? If you wish to seek a patent, keep the invention confidential until you speak to a patent attorney. The attorney can determine what parties may have rights to the invention, whether the invention may be patentable by conducting a prior art search, whether the patent would be enforceable, and whether there would be defenses to infringement. The prior art search is to see what other patents and publications exist that may disclose the invention. Finally, the attorney can also assist you with the application and drawings, as well as prosecuting the application through the Patent and Trademark Office. Next: what to do if you are accused of infringement.
Matt Osenga is a registered patent attorney with Goodman Allen Donnelly. His practice includes all aspects of patent prosecution before the US Patent & Trademark Office, as well as other aspects of patent law, including foreign patenting, patent infringement, and patent opinions. www.goodmanallen.com
That’s the JenCare Difference!
17658
Miss t he human side of medicine? JenCare Neighborhood Medical Centers is a growing medical group comprised of physician-led primary care practices that are transforming health care delivery. JenCare focuses on underserved, low-to-moderate income Medicare eligible seniors with multiple, complex conditions. With over 5,000 patients in the Tidewater area, JenCare significantly improves health outcomes with a high touch, preventive care model. OUR PHYSICIANS ENJOY: Small patient panels (<450 patients) Peer collaboration In-house medical specialists On-site diagnostics and imaging On-site prescription services Door-to-doctor transportation for patients
Our Locations
Tidewater Leadership SUSAN GIROIS MD, MPH
Medical Director Tidewater
TRAVIS INGRODI DBA, CAAMA
Network Director Tidewater
If you would like to discuss opportunities in confidence, please call:
Chevon Blue
(404) 996-7806
chevon.blue@jencaremed.com
A Portsmouth A Newport News A Virginia Beach A Norfolk
Due to space and time limitations, some services are not available at all centers.
JenCareMed.com
Promotional Feature
Dr. Robin Poe-Zeigler in her office, filled with Disney-themed gifts from patients.
THE NEW HOPE CENTER FOR REPRODUCTIVE MEDICINE … the perfect marriage of compassion and technology By: Tori Brown, New Hope Center for Reproductive Medicine Marketing Coordinator/Physician Liaison
A
ll through life we are taught to dream; to shoot for the stars and never give up on what we really, truly want in life. The hope that one day our dreams will become reality is what gets a lot of people through their day-to-day lives, and pushes them to keep going when they feel like they can’t. But what happens when you have a dream that can’t be achieved? What happens when no matter how many how-to books you read, classes you take, or effort you put in, your dream always seems a little bit too far away to grasp? That is what it feels like to struggle with infertility. The one thing you want most in the world is constantly just out of your reach. The pain and loss that infertility can cause are so great, they can take all faith of achieving the dream of parenthood away from its sufferers. But, thanks to the miracle of medicine, there is always hope: New Hope, to be exact. The New Hope Center for Reproductive Medicine, run by Medical Director and founder Dr. Robin Poe-Zeigler, is the 34 | www.hrphysician.com
light at the end of a dark tunnel for patients struggling with infertility. Founded in 1997, The New Hope Center has helped bring thousands of babies into the world through cutting-edge fertility treatments, such as in vitro fertilization, intra-uterine insemination, and embryo donation. But what is, perhaps, even more impactful for patients than the medical expertise that can be found at New Hope is the essence of the place itself. Once you’re a patient at New Hope, you become a part of the family. Every office visit feels like a trip home, where anything is possible and you are surrounded only by love and support. Dr. Robin, as she is known by all of her patients, has carefully crafted a sanctuary to help heal those who feel broken by their infertility. When patients realize that they need help getting pregnant, it can be overwhelming and very scary. Feeling the need to label yourself as “infertile” can hurt almost as badly as the
absence of a child. It’s very difficult to feel as though your body is betraying you, and taking the first step to seek the help you need can oftentimes be the most challenging. At The New Hope Center, they understand that. “These patients can be anxious, afraid and often emotional,” Dr. Robin notes, “so treating the mind as well as the body is an important component at every step in this journey.” Every staff member at The New Hope Center plays a key role in creating these miracle babies, but more importantly, they form relationships with the patients that make the intense fertility treatment process a little bit easier. Dr. Robin greets every patient with a warm hug and always remembers little details about her patients’ lives outside of their infertility struggles. She sees each one of them as an extended member of her family, and ensures that they feel that way as well. Her ideals of love, family and compassion trickle down into each and every experience these patients have at New Hope.
As the practice’s founder, Dr. Robin is the beating heart of New Hope. She says, “I believe that we have been given very specific medical knowledge and resources beyond belief. I believe these women are sent to me, and if I’m giving them a blessing, it’s only because I myself have been blessed.” Dr. Robin is happily married to her high-school sweetheart, Mark Zeigler, and is the mother of one son, Derek, who is in his junior year at The University of Virginia where he studies law. But her life has not always been so blessed. Her mother faced a two-and-a-half year battle with breast cancer, which she unfortunately lost in 1982. Watching her mother lose her fight with breast cancer inspired Dr. Robin to pursue a career in the medical field, and choose a specialty that focused on bringing new life into the world. She earned her medical degree from Eastern Virginia Medical School, during which time she was awarded a pathology externship at the University of Minnesota. She later completed a residency in obstetrics and gynecology at York Hospital in York, Pennsylvania, and returned to Hampton Roads to complete a fellowship at the Jones Institute. Upon completion of her fellowship, she returned to Minneapolis, Minnesota where she assisted in establishing a Donor Egg Program at a reputable IVF center. Despite her success in Minneapolis, she found that she was not compatible with the Minnesota climate. So, she returned to Virginia in February of 1997, and opened The New Hope Center for Reproductive Medicine, determined to establish a comprehensive center with the compassion, medical skills and technologies to offer just that: new hope to patients struggling with infertility. Located in Virginia Beach, The New Hope Center is a one-stop-shop for fertility patients. There are three distinct laboratories at New Hope that all connect to a central suite. It is a perfect mixture of what happens in each of these laboratories that allows New Hope miracles to be born.
Hormonal Assay and Immunology Lab. This satellite of LabCorp features two full-time phlebotomists. The phlebotomists, supported by two technicians, draw blood and run all hormone tests, giving Dr. Robin the ability to share results with her patients the same day – critical information when medication adjustments need to be made during an ovarian stimulation cycle. Having the ability to give same-day results also allows New Hope team members to ease patients’ anxiety about the progress of their cycles.
Andrology Lab. Two on-site andrologists do semen analyses, as well as insemination preparation in this lab. They process the semen so it’s ready for Dr. Robin to place in the patient’s uterus when she’s ovulating. “We’re available seven days a week in the andrology lab,” Dr. Robin says. “If ovulation occurs over the weekend, or on a holiday, no matter the time, we’re here for the patient. I’ve even come in on Christmas Day!”
Embryology Lab. The New Hope Embryology lab is where the real medicalmagic occurs. It is in this fully CAP certified labs that women’s eggs are retrieved and fertilized embryos are transferred. Dr. Robin’s off-site laboratory director, Lisa Ray, in conjunction with three other senior embryologists, travels to New Hope from Chicago and Charlotte on a monthly basis.
On-site embryologist Caitlin Toler analyzes embryos before incubation and transfer.
Fall 2016 Hampton Roads Physician | 35
Along with the two existing on-site embryologists, Caitlin Toler and Brittany Popp, they identify eggs; inseminate eggs with sperm; culture embryos; freeze eggs, sperm and embryos; and assist in the transfer of embryos into the patient’s uterine cavity. Biopsies of the individual embryos allow the New Hope Center staff to determine whether any genetic abnormalities exist within the embryos, well before implantation takes place. Preimplantation genetic screening, or PGS as it is more commonly known, has existed for about 10 years, but it’s evolving, and the advancements have been huge. “At first, we could identify three, then seven, then nine, then 11 – and now, we can screen the entire 23 pairs of chromosomes,” Dr. Robin says. This new technology allows her team to distinguish between chromosomally normal and abnormal embryos.
Parent of Origin Testing.
“There is no question about the commitment of my patients to undergo any process that can allow them to conceive and carry a child,” says Dr. Robin. New Hope offers several services for many different types of potential parents; each type of treatment is uniquely catered to every patients specific needs. Dr. Robin and the New Hope team cater every treatment plan and process based on what service will provide the patient with the best outcome, and what will be in their best interest financially. We offer in vitro fertilization, intrauterine insemination, embryo donation, and gestational carrier services, along with others. Our embryo donation and gestational carrier services are wonderful for patients who have trouble carrying children to term, or who are not biologically able to do so. This allows all patients, regardless of their relationship status or sexuality, to experience the joy of watching their child grow and develop.
When an embryo is revealed to have an abnormality or defect, the technology now allows Dr. Robin to identify whether it came from the egg or the sperm. “That’s an important Everyone is welcome piece of information,” she says, at the New Hope Center. “especially for women, who always Dr. Robin sees each patient seem to assume it’s their eggs that as a potential loving parent. are faulty.” This sophisticated Dr. Robin visits with a patient and her first child, born through IVF at New Hope. There is no judgment and no testing has allowed New Hope to discrimination; thus New Hope implant only chromosomally normal embryos, thereby sparing welcomes committed homosexual couples who are seeking prospective parents the heartache of many miscarriages to become parents. “My job is not to judge; my job is to and infants with major chromosomal abnormalities, lifehelp people become mothers and fathers,” she says. “I don’t threatening conditions, and early demise. discriminate against anyone. If an embryo is supposed to “We see this is a way of preventing potentially devastating implant, it’s going to implant, and I will do my best to make heartache,” Dr. Robin says. “And because the determination can that happen.” be made before implantation, there are few, if any, bioethical She employs certain modalities to help lesbian couples, one considerations.” of which involves taking eggs from one partner, adding donor sperm, and implanting the embryo into the other partner. Surgical procedures. “Both women are involved in the process, and it’s been so The New Hope Center has two fully built operating rewarding,” Dr. Robin says. rooms that connect to the Embryology Lab. Procedures Similarly, she has had a fair number of gay men seeking such as hysteroscopies are performed to diagnose and young egg donors and gestational carriers to assist them in correct problems with a woman’s uterus before embryos are having the child they long for. “At New Hope, we assist them transferred. Having these spaces on site allows patients a level in finding these essential people,” she says, asking, “Why of comfort that cannot be found at most other establishments. shouldn’t these energetic, highly-motivated men have the Instead of feeling like they are going into a new, scary and opportunity to love and nurture children?” sterilized place, they are just coming back to their comfortable New Hope welcomes patients of all types into the family, with home-away-from-home, in the trusted care of Dr. Robin. the only requirement being a desire to love and care for a child. 36 | www.hrphysician.com
The measure of success.
“We’re here to make a difference.”
Not every case can result in a pregnancy that goes to term, Dr. Robin concedes. But she emphasizes that at New Hope, “patients leave either with a healthy baby, or with a full understanding and, hopefully, with peace, about why there won’t be a child.” But there is always love, and there is always compassion.
It’s more than a motto: it’s a way of life for Dr. Robin PoeZeigler and her team at The New Hope Center for Reproductive Medicine. “We started out with seven patients in 1997,” she says, “and we have grown to thousands of patients and thousands of babies, and for that I am eternally grateful.”
Celebrating Miracles. When patients have worked so hard for their child and their little miracle is finally born, it is a huge cause for celebration. That is why, almost every year since the practice opened in 1997, Dr. Robin has hosted “Little Miracles” birthday parties. These parties serve as a gathering for the entire extended New Hope family to come together to celebrate the births of their children, re-connect with the New Hope team members who made those children possible, and give Dr. Robin the chance to experience their little ones. These events are peppered with laughter, tears of joy, and hearty celebration. The next “Little Miracles” party is particularly special to Dr. Robin and the entire New Hope team, as it will be celebrating the 20th birthday of the practice. “This is a chance for me to connect and hug all of the families that I have had the pleasure of being a part of. It is very special for me, and I think it’s special for them, too,” Dr. Robin compassionately notes. The party will be held at the Norfolk Zoo in July of 2017 on National Parents Day - July 23rd.
The New Hope Center for Reproductive Medicine 448 Viking Drive, Suite 100 Virginia Beach, VA, 23452
757-496-5370 www.thenewhopecenter.com
The New Hope team.
Fall 2016 Hampton Roads Physician | 37
The Canary in the Coal Mine By Alan L. Wagner, MD, FACS
W
hether during the 1600s when English miners searched for coal, or on some Stardate in the far distant future, the canary signals whether or not the atmosphere is safe for the people in it. The eye, and its fragile vasculature, plays the same role for the major organs of the body. Several of our articles in this column have outlined the importance of the eye, and in particular the retina, as a leading indicator regarding risk factors for major organ system compromise, morbidity, and mortality. It is appropriate – since this issue focuses on pulmonary disease – that we once again highlight the importance of recognizing and successfully intervening with Obstructive Sleep Apnea (OSA). Just as the canary needs a certain amount of oxygen to survive, the same is true of the retinal vasculature. If you also take into account the additional challenges placed by a diabetic patient’s activated immune system with the retinal endothelium and its pericytes being immune targets, the already dis-
Just as the canary needs a certain amount of oxygen to survive, the same is true of the retinal vasculature. advantaged retinal stroma is precariously close to the ischemic threshold, bringing about the complications what we know so well–macular edema, progressive capillary non-perfusion, neovascularization, vitreous cavity hemorrhage, tractional retinal detachment, and blindness. When OSA drops the dissolved serum oxygen concentration as low as one would find if you were climbing to the top of a mountain without oxygen for
38 | www.hrphysician.com
several hours a night, the complications present themselves and multiply quickly. The first article pointing to sleep apnea and its role with causing accelerated vascular disease within the eye came from our very own Eastern Virginia Medical School’s Department of Ophthalmology 30 years ago. Since then, our understanding has increased dramatically, relating both pulmonary function compromise and immunology to the eye. We now know that untreated OSA dramatically increases a patient’s risk for complications, ranging from both venous and arterial occlusion to macro vascular disease with its associated embolic phenomena. I encourage all of our colleagues to become familiar with the recommended screening parameters for all of our patients, and to make the quality-of-life assessments and appropriate physical examinations necessary to help protect patients from these preventable complications. The eye may be the canary, but the heart and the brain aren’t far behind.
Alan L. Wagner, MD, FACS founded the Wagner Macula & Retina Center in 1987. A Board certified ophthalmologist specializing in vitreoretinal surgery, Dr. Wagner received his medical degree from Vanderbilt University School of Medicine. He completed his residency in Ophthalmology at EVMS, and furthered his training as the Dyson Fellow in vitreoretinal disease and surgery at Weill Cornell University Medical Center. wagnerretina.com
Fall 2016 Hampton Roads Physician | 39
Liability Risks of Telemedicine: State Standards Among Considerations
By Dustin Shaver, Vice President of Risk Management at NORCAL Mutual Insurance Company
T
elemedicine utilization growth continues at an impressive rate. According to the FAIR Health database (the largest repository of private healthcare claims), telemedicine use in the U.S. nearly doubled between 2007 and 2015. Over half of all U.S. hospitals now use some form of telemedicine, according to the American Telemedicine Association. Telemedicine is widely credited with improving patient access, cost efficiencies and quality of care. This and increasingly favorable state and federal telemedicine legislation may explain the rapid increase in its utilization. Despite the advantages, telemedicine has liability risks, such as privacy, security, patient confidentiality, credentialing and misdiagnosis due to a lack of continuity of care. Additionally, the soft skills that may come naturally in a personal patient encounter may need to be adjusted for electronic encounters. Telemedicine providers should evaluate their “webside”
manner. For example, equipment needs to be positioned to simulate direct eye contact; active listening cues may need to be exaggerated; posture and facial expressions may need adjustment and sessions must be started and ended appropriately. Seemingly minor electronic communication strategies can significantly affect the success of a telemedicine encounter. Physicians who adopt telemedicine also have administrative considerations that may pose a challenge and liability risk. For instance, professional licensure portability and individual state mandated practice standards present major challenges. There are significant differences among state telemedicine laws and the laws are constantly changing. In the 2016 legislative session, for example, over 150 telemedicine-related bills were introduced by 44 states. The issues addressed by these bills ranged from informed consent requirements to online
Keeping your finances healthy
for over 40 years
• Internal accounting control review • Practice Administrator backup and support • Business plan development and maintenance • Full range of client bookeeping, general accounting, and tax preparation services
757.640.7190 | 150 Boush St. Suite 1100 | Norfolk, VA 23510 | mrdcpa.com 40 | www.hrphysician.com
prescribing parameters to Medicaid reimbursement. Physicians should be aware of the telemedicine laws in their own state and in the state of every patient in their telemedicine practice. Understanding the laws is paramount to understanding the medical liability risks that may be involved in the various different stages of providing telemedicine. Medical professionals providing virtual visits must work harder to reduce practice liability exposures. To help enhance patient safety and reduce risk: • Understand that individual state telemedicine practice laws vary from state to state. • Consult with your healthcare business attorney as needed. • Check your professional licensure portability to ensure that you are licensed to practice in the jurisdiction where the patient resides. • Consult with your medical practice liability insurance company to ensure that your policy covers all jurisdictions where you plan to provide services. • Be aware of online prescribing regulations that vary across jurisdictions. • Comply with all applicable privacy and security standards for the secure transmission of protected health information between patient, provider and payers. • Standardize telemedicine patient visits to help minimize the potential for error and to support good communication practices.
• Take care to ensure that the primary care physician and patient relationship is not fractured with ongoing use of telemedicine consultation. Telemedicine is an emerging practice and the rising rate of adoption by both physicians and patients is an indication of its value. As with all advancement in the field of medicine, the advantages of adopting a new way of practice should be considered carefully and risks assessed. It is important to consult with your medical professional liability insurance provider on your individual policy to ensure you are adequately covered for the scope of practice, and consult with your business attorney as needed. NORCAL Mutual has a team of risk management specialists available to consult and assist policyholders with the assessment of their practice and to help identify and address risk exposures. To learn more about managing telemedicine risk exposure, NORCAL policyholders can access the September 2016 Claims Rx entitled “Telemedicine Risk Management,” which is available through MyACCOUNT on the new MyNORCAL® mobile app. This article is reprinted with the permission of NORCAL Mutual Insurance Company. NORCAL Mutual Insurance Company. Liability Risks of Telemedicine: State Standards Among Considerations
Riverside Urology Experts Exceptional, patient-centered urological treatment is available on the Peninsula from our highly trained and skilled team. Conditions treated include: • • • • • •
Bladder, prostate and kidney cancer Urinary incontinence and infections Erectile dysfunction Kidney stones Enlarged prostates Advanced laparoscopy and robotics
Urology Specialists
Contact us at 757-847-5555 Fall 2016 Hampton Roads Physician | 41
Taking the PAIN Out of KNEE REPLACEMENT RECOVERY Innovative new modalities for managing post-surgical discomfort By Adrian T. Baddar, MD Hampton Roads Orthopaedic & Sports Medicine
E
very year in the United States, approximately 150,000 hip is wearing off and lasts a full three days. replacements are performed, and more than 350,000 knee When the knee capsule is closed, we inject the patient’s knee replacements. By contrast, the number of spinal fusions done with a fast-acting numbing medicine along with epinephrine to each year is a stunning 650,000, reflecting just how many control bleeding, and administer morphine and a strong antiAmericans suffer from a seriously aching inflammatory as well. lower back. The overwhelming majority of If this sounds like a lot of medicines in these procedures are successful, reducing or rapid succession, it’s because we’ve learned It’s well understood by substantially relieving pain and restoring the to approach all of the pathways that orthopaedic surgeons patients to comfortable, active lifestyles. produce the searing pain associated with It’s well understood by orthopaedic and patients alike this surgery without overuse of narcotics surgeons and patients alike that the pain with all of its attendant complications. that the pain that that accompanies knee replacement surgery By effectively numbing these patients, accompanies knee can be miserable. And candidly, in the preventing inflammation and reducing past, we’ve done a pretty miserable job of their sensation of pain – while keeping replacement surgery controlling it. The etiology of most of that them mobile and starting PT the same day can be miserable. pain is the work we’ve done in the bone of surgery – we’re seeing quicker recoveries itself, particularly around the area of the and more confident patients who are able periosteum. And having seen their friends and loved ones suffering to participate more fully with their therapists. – literally – with post-surgical pain, many patients have resolutely Post-surgery, patients remain on the anti-inflammatory, avoided knee replacement because of the stigma of those first days and we’ve found that IV Tylenol works just as effectively of recovery. as morphine, but without the attendant constipation and Today, fortunately, that no longer need be the case. Now the first mental sluggishness. In the past, when I saw patients the day few days are actually the easiest, because we’ve learned to control after their knee replacements, I became accustomed to often pain significantly better and more efficiently. (very) loud complaints of pain. Now when I visit, I often find It starts with the pre-surgical care: before putting patients them sleeping peacefully – or sitting up, enjoying a pain-free under, we can administer narcotic pain medicine and an antimorning. In fact, I often have to caution them that in a few inflammatory, as well as pregabalin (Lyrica) when appropriate, days, this regimen will start to wear off, and they’re going to which modifies the way they experience pain. In the case of knee experience some increasing pain – but nothing like the pain replacements, surgeons can inject a numbing medicine around the they’d feared, and nothing that can’t be easily managed. femoral nerve, best placed lower down in the quadriceps to avoid loss of motor function. Because these blocks can last as much as Dr. Baddar is a graduate of the 12 hours, patients are waking up from surgery with essentially no University of Virginia Medical School, where he completed his orthopaedic pain. And because they’ve been premedicated, they don’t require as residency. He completed a fellowship much anesthesia during the procedure itself. They wake up not only in Adult Reconstructive Surgery at pain free, but far better able to mobilize and without the groggy, the Cleveland Clinic, and is a fellow of nauseated feeling that often accompanies an “anesthesia hangover.” the American Society of Orthopaedic In addition, an injection of Exparel during the surgery, while the Surgeons. He also serves as the Medical Director for the Multi-Positional MRI joint is open, provides as much as 72 hours of pain relief. Exparel Center at Hampton Roads Orthopaedic & is a non-opioid that slowly releases bupivacaine, numbing the area Spine Center. www.hrosm.com around the bone in the surgical site. Because it takes about eight hours for maximum effectiveness, it provides relief just as the block 42 | www.hrphysician.com
NOR CAL
GR OU P
OF
COMPA NIES
MEDICAL PROFESSIONAL LIABILITY INSURANCE
VIRGINIA PHYSICIANS DESERVE
NORCAL Mutual now offers its enhanced coverage to Virginia physicians and health care professionals. NORCAL Mutual brings an A.M. Best “A” (Excellent) rating, access to award-winning Risk Solutions and CME activities, and 40 years of strength and stability.
Talk to an agent/broker about NORCAL Mutual today. NORCALMUTUAL.COM | 844.4NORCAL © 2016 NORCAL Mutual Insurance Company
Fall 2016 Hampton Roads Physician | 43nm0681
Smart Strategies for Setting Salaries
S
etting compensation levels for staffers is one of the more difficult issues that physicians face. After all, salaries typically account for a large part of a practice’s expenses. If your pay scale is low, it may drive up the rate of employee turnover. On the other hand, paying above-market rates can inflate your overhead unnecessarily. Attracting and retaining employees isn’t the only goal when setting compensation levels. They should be structured in such a way that your staff members recognize that productivity and additional effort will be rewarded. So what can you do to ensure that your compensation plans achieve these goals? Start by considering these issues.
Study Benchmark Data Pay and benefits may vary considerably from one location to another and even from one practice to another. Find out what other local physicians are paying or get wage and benefit data online to use as a benchmark when you are making compensation decisions.
Adjust for Circumstances You’ll need to adjust the benchmarks you find for a variety of circumstances. For example, consider your location. Are you in a high-cost urban/suburban area or a low-cost rural one? In addition, you should adjust for any factors specific to your practice, such as payer mix. Tailoring benchmarks to your practice’s specific circumstances will give you custom tools you can use to evaluate staff costs.
Create Incentive Plans It may make more sense from a budget perspective to offer merit or productivity bonuses to employees rather than offering an across-the-board pay raise for the whole practice. Offering incentive bonuses allows you to set specific goals. For example, if you want to reduce the number of claims that insurers reject, offer employees a monthly bonus if they can reduce rejected claims by a certain percentage, say 30 percent. Your practice can use merit bonuses to encourage staff members to acquire additional qualifications and training. It’s generally a win-win situation: Your staff member acquires additional qualifications and your practice benefits from his or her enhanced skills.
Talk to Us We can help your practice review your current compensation practices to determine where changes might be necessary and beneficial.
Serving the Bracing and Prosthetic Needs of Hampton Roads Peninsula
757-595-9800 Southside
757-673-2000 David M. Limroth, CPA
211 Bulifants Blvd. Suite B Williamsburg, VA
11747 Jefferson Ave Suite 5A Newport News, VA
7578 Hospital Dr Suite B-106 Gloucester, VA
4057 Taylor Road Suite P Chesapeake, VA
Hours: Mon – Thurs 8 am – 4:30 pm • Fri 8 am – 2 pm 44 | www.hrphysician.com
R. Paul Speece, CPA
Nicole J. Wood-Sabo, CPA, MS
Copyright 2015 by DST. All rights reserved. The general information in this publication is not intended to be nor should it be treated as tax, legal, or accounting advice. Additional issues could exist that would affect the tax treatment of a specific transaction and, therefore, taxpayers should seek advice from an independent tax advisor based on their particular circumstances before acting on any information presented. This information is not intended to be nor can it be used by any taxpayer for the purpose of avoiding tax penalties
AUTOLOGOUS STEM CELL TRANSPLANTATION for Multiple Myeloma and Relapsed Lymphoma Patients By Dean S. McGaughey, III, MD Virginia Oncology Associates
S
ome patients may be confused by the term ‘stem cell significantly improved the survival of myeloma patients, versus transplant,’ but they should be assured it’s the same standard therapy alone. methodology as the bone marrow transplant they’re Stem cell apheresis transplantation is now the standard of care familiar with. The change in the procedure, and the for patients with advanced myeloma and relapsed lymphomas. In reason for the change in terminology, is that we’re no longer addition to Hampton Roads, there are currently three centers that transplanting the bone marrow itself. For patients with relapsing offer the treatment in Virginia, making it available throughout the lymphoma and multiple myeloma, who required massive doses of Commonwealth. chemotherapy, the change has been dramatic. Prior to the year 2000, the only way to retrieve stem cells from these patients was to take them to the OR and do a bone marrow Dr. McGaughey received his medical degree harvest, which involved poking as many as three hundred holes from the University of Chicago, Pritzker School in the pelvis to extract bone marrow. Depending on the patient, of Medicine. He completed both his residency in Internal Medicine and his fellowship in recovery could take several days to weeks of back, hip and/or Hematology and Medical Oncology at Duke muscle pain with bruising. In 2000, oncologists discovered a far University Medical Center in Durham, North easier method to collect the necessary stem cells for the transplant Carolina. He is currently Director of the Stem Cell Transplant Program at Virginia Oncology that eliminates the needle sticks. Associates. www.virginiacancer.com Now we can “mobilize stem cells” by giving a moderate dose of chemo, followed by several days of neupogen, a combination that will temporarily push the stem cells out of the bone marrow into the blood stream. When blood tests reveal an adequate number of stem cells, we collect them through apheresis. We can then freeze these stem cells just as we did the THANK YOU! The doctors and staff at Allergy & Asthma Specialists extend a heartfelt thank you to all the physicians and staffs in Hampton Roads who bone marrow. We are then ready refer their patients to us for allergy and asthma health care. We never lose to do the autologous stem cell sight of the fact that your referral is accompanied with a trust in us. transplant, which involves large dose chemotherapy, followed by stem cell reinfusion. Thus, autologous transplant lets us give larger doses of chemotherapy than otherwise possible. Both internationally and locally, Dr. Gary Moss Dr. Greg Pendell Dr. Craig Koenig June Raehll Kim Pham Lisa Deafenbaugh FNP-BC NP-C PA-C the cure rate for relapsed lymphoma We make it as easy as possible on the patient and referring physician by ACCEPTING MOST INSURANCES. patients has doubled, from 20 to 40 percent with the use of transplant. Virginia Beach (757) 481-4383 • Chesapeake (757) 547-7702 • Norfolk (757) 583-4382 Stem cell transplant has also www.allergydocs.net Fall 2016 Hampton Roads Physician | 45
Hand Therapy: Patient Education
By Marcia Miller, PT, MS, CHT Tidewater Physical Therapy, Williamsburg Hand Therapy Center Clinical Director
C
hecking email on the phone. Jotting down a note. Doing a little work from home on a laptop. Hands down (pun intended), hands are among the most used parts of our patients’ bodies, and it’s easy to take them for granted and even easier for our patients to forget how often they use hands in everyday life. That is, until they develop pain. According to the Centers for Disease Control and Prevention, an estimated 52.5 million adults in the US reported being told by a doctor that they have some form of arthritis, rheumatoid arthritis, gout, lupus or fibromyalgia. Osteoarthritis is the most common arthritis causing hand problems. Today, there are a number of research-driven treatment protocols to get patients back to their active lives when their hands are impaired. Education is vital. There are several effective daily living tips patients should practice to protect their hand joints. Cell Phone Use Many modern hand injuries stem from technology related issues, namely overuse. In 2005, the American Society of Hand Therapists warned consumers there was an increased risk of hand, wrist and arm injuries from repetitive motion on small buttons and awkward wrist movements. And just think how much more dependent society is on cellphones than in 2005. Remind patients when working on a cell phone to: 1. Keep arms in front to minimize looking down. 2. Write extensive emails from computers, not phones. 3. Use a headset or speakerphone whenever possible. 4. Minimize texting when you can, or support arms, hands and phone on a briefcase or lap while texting. Talk to text is a great tool. Use it.
Take a Note Ever think about the size of the pen patients use to write notes? It matters. As patients write, they are actually putting many pounds of pressure on their hands per pinch. That multiplies as they bear down. For example, if we pinch with three pounds of force at the tip of a pen, that multiplies to 36 pounds of force at the basal joint. If patients already have pain in their hands, consider telling them to use thicker pens as they do not require as much force be applied to hold. Laptop Use It may sound obvious, but remind patients that laptops were made to be used on the lap and not on a desk or counter. That elevated position of the laptop can force the user to have their hands, wrists and upper body in an uncomfortable position that, over time, can lead to pain from inflammation in the hands and wrists. Inflammation can lead to carpal tunnel syndrome. Advise patients to modify their surface height so their wrists are neutral with their elbows at their side. Training, Stretching and Breaks Just like you wouldn’t run a marathon without training or stretching, encourage patients not to sit at a computer for eight hours straight without stretching or taking breaks. That long at a computer uses those small hand muscles in an endurance capacity. Encourage patients to stretch hourly, from the neck all the way down. Include the arms, shoulders, triceps, forearms, wrists and fingers.
Marcia Miller, PT, MS, CHT is the Clinical Director of the Tidewater Physical Therapy Williamsburg Hand Therapy Center. Learn more at www.tpti.com
46 | www.hrphysician.com
NOBODY CHOOSES TO GET CANCER... BUT YOU CAN CHOOSE HOW TO FIGHT IT. At Virginia Oncology Associates, we know each cancer is unique and so is every patient we treat. Our team of experienced physicians and staff is dedicated to providing advanced care, innovative technology and personalized treatment options. As a part of The US Oncology Network, we deliver high-quality, evidence-based care to patients close to home. Convenient locations across the southeast region of Virginia and northeastern North Carolina State-of-the-art technology, innovative treatments, and extensive research Specializing in medical oncology, gynecologic oncology, radiation oncology and hematology
Peninsula | 757-873-9400 Southside | 757-466-8683 North Carolina | 252-331-2044 VirginiaCancer.com The US Oncology Network is supported by McKesson Specialty Health. © 2016 McKesson Specialty Health. All rights reserved.
IN THE NEWS Monica Reed, BSHA, RCIS, CCCC has been honored by the Tidewater Emergency Medical Services (TEMS) Council as part of its annual recognition program. Reed, Manager of Cardiovascular Services for Bon Secours DePaul Medical Center, received the Excellence in EMS Award, also known as the R.C. Dailey Award, the top award given by the TEMS Council. Monica Reed, BSHA, RCIS, CCCC
Bon Secours DePaul Medical Center Women’s Imaging Center now has 3-D mammography technology, which allows doctors to examine breast tissue one layer at a time to inspect for any abnormalities in the tissue. During a 3-D mammogram, multiple images of the breast are acquired at different angles. Using high-powered computing, digital breast images are then converted into a stack of very thin layers or “slices.” These images can be viewed as a detailed 3-D reconstruction of the breast. One new feature on this unit is the ability to do 3-D guided biopsies. The patient can be positioned on her side or upright in a chair to have this procedure done. Barbara J. Funches, MSN, RN joined the Bon Secours Hampton Roads Health System as Vice President of Quality and Clinical Effectiveness effective August 8, 2016. She will lead performance improvement, quality, infection prevention, patient safety, patient experience, regulatory and care management across Bon Secours Hampton Roads. Barbara J. Funches, MSN, RN
Kelly Edmondson, MSN, RN, NEA-BC was recently named Administrative Director of Nursing Operations at Bon Secours Mary Immaculate Hospital. She most recently served as Administrative Director for Acute Care Services at Bon Secours Mary Immaculate.
Kelly Edmondson, MSN, RN, NEA-BC
Kathryn Funk, RN, BSN, CNRN, SCRN has been honored by the Tidewater Emergency Medical Services (TEMS) Council as part of its annual recognition program. Funk was named TEMS Nurse with Outstanding Contributions to EMS. Funk is the Neuroscience Clinical Program Coordinator for Bon Secours Maryview Medical Center and Bon Secours Health Center at Harbour View. Kathryn Funk, RN, BSN, CNRN, SCRN
48 | www.hrphysician.com
During the ninth annual Anthem LemonAid weekend, local families came together in record-setting numbers to help children fighting cancer at Children’s Hospital of The King’s Daughters, as 915 lemonade stands across Hampton Roads (and online) raised awareness for childhood cancer and an unprecedented $120,000 for the kids at CHKD. Funds will support cancer research, equipment and services to help more than 500 local children followed by CHKD’s cancer program each year.
Five-year-old River Eanes served up smiles and lemonade to Hampton police officers at a local Panera.
Chesapeake Regional Healthcare is bringing the first Mobile Mammography Unit equipped with both 2-D and 3-D Technology to Hampton Roads. The 40-foot unit will travel to communities and businesses throughout the region to offer quick appointments in a comfortable and discreet space. Most screenings will last about 20 minutes, and the units are set-up with a separate changing area and mammography room to provide the utmost privacy.
The Chesapeake Regional Health Foundation announces the appointment of four new members and one returning member to its Board of Directors, as well as its full slate of officers. Danijel Velicki, Scott Pennington, Dan Banister, and Kristi Wooten began their appointments on July 1, 2016 for terms that will last through June 2019. Dr. Harold J. Marioneaux, Jr. began his term on August 1, 2016 and his term will last through July 2019. Chesapeake Regional Healthcare introduces the SAVI SCOUT breast localization and surgical guidance system to Hampton Roads. For the first time in the region, patients who require breast conservation surgery have access to the system as an alternative to wire localization. SCOUT is an FDA-cleared device used by surgeons and radiologists to precisely locate and direct the removal of a tumor during a lumpectomy or surgical biopsy procedure. A study conducted primarily by researchers at EVMS and Sentara Healthcare may eventually improve treatments for women with advanced and metastatic breast cancer. The study demonstrates that two biomarkers, known as SIAH and EGFR, help identify resistant breast-cancer tumors and can differentiate between effective and ineffective therapies. The findings may eventually help physicians predict tumor recurrences and patient survival probabilities during firstline breast-cancer treatments. The Medical Society of Virginia has successfully launched a newly redesigned website at www.msv.org. The new site provides visitors with a more modern, richer experience using fullyoptimized mobile technology.
Dr. William Patrick Clark, Medical Oncologist with Riverside’s Cancer Specialists of Tidewater and Riverside Cancer Infusion Centers, has retired after 32 years of caring for patients in Virginia Beach. A graduate of Georgetown University School of Medicine in 1978, Dr. Clark completed his medical internship at Roger Williams General Hospital in Providence RI. Dr. Clark has been a respected William Patrick Clark, MD member of the American College of Physicians, the American Society of Clinical Oncology, the Virginia Beach Medical Society, the Medical Society of Virginia, the American Medical Association, and the Virginia Association of Hematologists and Oncologists. Riverside Health System recognizes Dr. Clark’s exceptional leadership and compassionate care toward his patients and the CST Cancer Team.
G. Richard (Rick) Jackson
G. Richard (Rick) Jackson, the System Director for the Riverside Center for Excellence in Aging and Lifelong Health, was named by Governor Terry McAuliffe to serve on the newly-formed Alzheimer’s Disease and Related Disorders Commission. The bipartisan Commission will serve as an advisory group and is an important part of state-wide efforts to assist people with Alzheimer’s and other dementias.
Fall 2016 Hampton Roads Physician | 49
IN THE NEWS Riverside Cancer Care has been selected by CMS to participate in a national oncology care model. CMS designed the five-year pilot program to support increased collaboration, information sharing and care coordination. Criteria for participation included patient navigation and coordinated referrals, data-driven continuous quality improvement, access to integrative therapies, certified EHR technology, treatment therapies consistent with nationally recognized clinical guidelines and 24/7 availability of clinicians who can access relevant medical records. Riverside Doctors’ Hospital Williamsburg was recently designated a Center of Excellence in Minimally Invasive Gynecology by the American Association of Gynecologic Laparoscopists, an international certifying body, and Surgical Review Worldwide. The honor is the result of a detailed independent study, which included surgeon training and experience, review of at least 75 qualifying procedures, observation of the gynecologic Dr. Karanvir Virk surgical suite and extensive discussion with operating room staff to ensure the highest level of knowledge and competency in caring for minimally invasive gynecologic patients. Dr. Karanvir Virk is the only certified Center of Excellence provider in minimally invasive gynecology on the Peninsula. Taffi Simone, Riverside team member Program Coordinator for Workforce Development, was recognized as a “Top Corporate Leader” for her role in HR-based leadership development programs. Within this
Weight Loss Delivered to Your Door Step Help your patients effectively lose weight and learn the skills to keep it off. Now with TPMG Tidewater Bariatrics E-Commerce site, patients can have lowcalorie foods shipped to their doorstep.
www.twb4u.com
TPMG Coastal Internal Medicine and Tidewater Bariatrics 1405 Kempsville Road Chesapeake, VA 23320
50 | www.hrphysician.com
Taffi Simone
Rebecca Mott, MHA, BSN, CHPN, CHPCA, CWS joined Sentara Hospice in the past year as its director for all Hospice branch locations.
Rebecca Mott, MHA, BSN, CHPN, CHPCA, CWS
Brian Perry, BSN, RN recently joined Sentara Home Care as director for all branch locations.
Brian Perry, BSN, RN
Michael Ware joined Virginia Eye Consultants as Practice Development Manager. He has a long background in customer service and is a native of Virginia Beach.
Michael Ware
Governor Terry McAuliffe announced that a site in Virginia Beach has been selected for a planned 120-bed Veterans Care Center. The new care center will be built in Virginia Beach’s bio health corridor on a 24-acre site off the planned extension of Nimmo Parkway and West Neck Road. Construction is scheduled to start in late 2017, and completion is expected in late 2019. The facility will feature all private rooms that will be organized into households that surround a central community center. The facility will provide comprehensive care with on-site laboratory, x-rays, physical therapy, podiatry care and other ancillary health care services similar to the other veterans care center recently announced in Northern Virginia. Virginia Eye Consultants physicians and staff members devoted two days in August to performing 50 free sight-saving eye surgeries for patients throughout Hampton Roads. The annual Looking Forward…Giving Back program is designed to help members of the community who are uninsured, underinsured or financially unable to pay for their procedure. This is the fourth year Virginia Eye Consultants has provided this service.
ACCEPTING NEW PATIENTS
(757) 842-6267 (757) 644-6819
important area, the Riverside Emerging Leaders Academy was recently ranked among the top 10 percent of programs worldwide during the annual Global Leadership Conference and Leadership Excellence and Development Awards for 2016.
mytpmg.com
Local Hospital Systems Receive Special Recognition for their collaborative efforts toward improving community health. The winning program, Healthy Communities Initiative, East Ocean View in Norfolk, is one of only five programs honored by AHA this year. The New Life Christian Center and Operation Blessing International Relief Organization were key partners in developing and supporting the initiative which grew to include partnerships with churches, community centers, the City of Norfolk, the East Ocean View Civic League, restaurants, farms, housing development organizations, universities, military bases, and other business and civic groups. Bon Secours Maryview Medical Center has received the Mission: Lifeline® Silver Receiving Quality Achievement Award for implementing specific quality improvement measures outlined by the American Heart Association for the treatment of patients who suffer severe heart attacks. Maryview has also been recognized as a recipient of Mission: Lifeline’s Silver-Plus award, which recognizes the hospital has reached an achievement score of 75 percent or greater for treating STEMI transfer patients from other facilities within 120 minutes. Bon Secours Hampton Roads Health System, part of Bon Secours Health System, Inc., has been awarded the 2016 AHA NOVA Award. Established in 1993, the AHA NOVA Award recognizes hospitals and health systems
Bon Secours Mary Immaculate Hospital has earned The Joint Commission’s Gold Seal of Approval® and the American Heart Association/ American Stroke Association’s Heart-Check mark for Advanced Certification for Primary Stroke Centers. With the certification of Bon Secours
MEDICAL PROFESSIONALS MORTGAGE Fulton Mortgage Company has designed a mortgage program to make homeownership easy and affordable for you. · A program designed for medical professionals1 including MD, DO, DDS, DMD, PHARMD and VMD · Up to 100% financing available for loan amounts up to $1.5 Million · 15 & 30-Year Fixed Rates2, as well as Adjustable Rates available · No Mortgage Insurance required · Up to 6% seller paid closing cost and prepaids allowed Call a mortgage professional, today!
844.298.8780
Lisa Cafferty NMLS #: 106796
Holly Damalas NMLS #: 758490
Matt DesRoches Marc Dugas NMLS #: 659388
NMLS #: 939171
Tom Lira
NMLS #: 284626
fultonmortgagecompany.com Fulton Bank, N.A Member FDIC. Subject to credit approval. 1 Doctorate degree required. Restrictions apply. 2Monthly payment for a $250,000 15-year term mortgage at 3.582% Annual Percentage Rate (APR) would be $1,787.21. Monthly payment for a $250,000 30-year term mortgage at 4.414% APR would be $1,248.21.
Fall 2016 Hampton Roads Physician | 51
IN THE NEWS Mary Mary Immaculate, Immaculate, Bon Bon Secours Secours Virginia Virginia is is one one of of the the largest largest stroke stroke networks networks in in the the Commonwealth Commonwealth of Virginia. Bon Bon Secours’ Secours’ pulmonary pulmonary rehabilitarehabilitation tion program program at at Maryview Maryview Medical Medical Center Center has has been been recognized recognized by by the the American American Association Association of of CardiovasCardiovascular cular and and Pulmonary Pulmonary Rehabilitation Rehabilitation (AACVPR) (AACVPR) for for its its commitment commitment to to improving improving the the quality quality of of life life by by enhancenhancing ing standards standards of of care. care. The The noninvasive noninvasive vascular vascular laboratory laboratory at at the the Bon Bon Secours Secours Vein Vein and Vascular Specialists in Chesapeake has earned three-year reaccreditation cular Specialists in Chesapeake has earned three-year reaccreditation in in vascular vascular testing testing from from the the Intersocietal Intersocietal Accreditation Accreditation Commission Commission (IAC) (IAC) in in the the areas areas of of extracranial extracranial cerebrovascular cerebrovascular testing, testing, peripheral peripheral venous venous testing and peripheral arterial testing. IAC accreditation testing and peripheral arterial testing. IAC accreditation indicates indicates the the facility facility has has undergone undergone aa thorough thorough review review of of its its operational operational and and technical technical components components by by aa panel panel of of medical medical experts experts in in the the vascular vascular testing testing field, field, according to the commission. according to the commission. Working Working Mother Mother magazine magazine recognized recognized Bon Bon Secours Secours Virginia Virginia as as one one of of the 2016 “Working Mother 100 Best Companies” for its outstanding the 2016 “Working Mother 100 Best Companies” for its outstanding leadership leadership in in creating creating progressive progressive programs programs for for its its workforce, workforce, in in the the areas of advancement of women, flexibility, child care and paid areas of advancement of women, flexibility, child care and paid parental parental leave. leave. The The 100 100 Best Best Companies Companies are are featured featured in in the the October/November October/November issue of Working Mother and on workingmother.com. issue of Working Mother and on workingmother.com.
Bon Bon Secours Secours Virginia Virginia Nurse Nurse Residency Residency Program Program at at Mary Mary Immaculate Immaculate Hospital Hospital and and the the Bon Bon Secours Secours Mary Mary Immaculate Immaculate Hospital’s Hospital’s Registered Registered Nurse Nurse Fellowship Fellowship Transitions Transitions in in Practice Practice Program Program have have achieved achieved accredaccreditation itation with with distinction distinction from from the the American American Nurses Nurses Credentialing Credentialing Center Center (ANCC). (ANCC). Bon Bon Secours Secours Mary Mary Immaculate Immaculate is is the the first first hospital hospital in in the the nation nation to to earn earn accreditation accreditation with with distinction distinction from from ANCC ANCC for for its its RN RN Fellowship Fellowship Transitions Transitions in in Practice Practice Program Program and and the the Nurse Nurse Residency Residency Program Program is is the the fourth fourth program program in in the the nation nation to to be be recognized. recognized. Bon Bon Secours Secours Mary Mary Immaculate Immaculate was was also also the the first first hospital hospital in in the the Hampton Hampton Roads Roads region region to to achieve achieve Pathway Pathway to to Excellence Excellence in in 2012, 2012, was was re-designated re-designated by by the the ANCC ANCC in in December December 2015 2015 and and received received the the national national Pathway Pathway award award in in 2013. 2013.
Chesapeake Chesapeake Regional Regional Healthcare’s Healthcare’s BariatBariatric program was recently ric program was recently accredited accredited as as aa Comprehensive Center by the American Comprehensive Center by the American College College of of Surgeons Surgeons (ACS) (ACS) Metabolic Metabolic and and Bariatric Surgery Accreditation Bariatric Surgery Accreditation and and QualQuality ity Improvement Improvement Program Program (MBSQQIP). (MBSQQIP). The surgeons involved The surgeons involved with with the the program, program, Glen Moore, MD and David Spencer, DO were both deemed Glen Moore, MD and David Spencer, DO were both deemed MBSAQIP MBSAQIP verified verified surgeons, surgeons, recognizing recognizing their their commitment commitment to to high high quality quality metametabolic and bariatric surgical care. bolic and bariatric surgical care. Chesapeake Chesapeake Regional Regional Healthcare Healthcare (CRH) (CRH) has has received received the the 2016 2016 Women’s Women’s ® ® as one of America’s Best Breast Centers. This certified Choice Award Choice Award as one of America’s Best Breast Centers. This certified designation is the only award that identifies the country’s best breast centers based on rigorous criteria that considers female patient satisfaction and clinical excellence. This is the third consecutive year CRH has received this recognition.
Jennifer Pagador, MD Diplomate, American Board of Obesity Medicine
We are a Medical Weight Loss and wellness Clinic!
We offer:
Affordable medical weight management medical skin care, products and procedures Age-Management Medicine-Bioidentical Hormone Replacement Therapy All care is supervised by both MDs and Certified Nurse Practitioners.
seriouslyweightloss.com revitamedical.com
810 Kempsville Rd. Suite 1, Virginia Beach
(757) 313-5420
52 52 || www.hrphysician.com www.hrphysician.com
Riverside Regional Medical Center was designated a Most Wired®® Hospital Hospital for 2016 by The American Hospital Association’s (AHA) Health Forum for the 12th consecutive year. The annual Most Wired survey is a leading industry barometer measuring information technology use and adoption among hospitals nationwide. The 2016 benchmarking study and survey placed a strong emphasis on telehealth, an area in which Riverside has attained a position of regional leadership during recent years. Riverside Health System has received Premier, Inc.’s 2015 Richard A. Norling Premier Alliance Excellence Award for its commitment to transforming healthcare. The annual award recognizes a Premier
member that is a leader in leveraging the collaborative power of the alliance to drive higher-quality, safer and more cost-effective healthcare. Riverside is the sole winner among Premier’s alliance of approximately 3,400 U.S. hospitals. Riverside Regional Medical Center was recently honored as a Gold Safe Sleep Champion by the Cribs for Kids® National Safe Sleep Hospital Certification Program, an organization committed to reducing infant sleep-related injuries and fatalities caused by accidental suffocation. Riverside was awarded the highest level of certification by the national organization for efforts that include a strong focus on educating new parents about safe sleep for newborns and infants in accordance with guidelines developed by the American Academy of Pediatrics. Riverside Regional Medical Center was among only 141 hospitals across the nation to receive Pathway to Excellence status re-designation from the American Nurses Credentialing Center. This action confirms the professional satisfaction of nurses at RRMC and identified the medical center as one of the best places to work within the profession. Riverside Shore Memorial Hospital was recently certified a Primary Stroke Center by DNV GL in partnership with the American Heart Association and the American Stroke Association. DNV GL evaluates hospitals’ stroke care and services by reviewing patient outcomes, care processes, care settings, and clinical records. PSC distinction recognizes programs with the highest national standards for safety and quality of stroke diagnosis, treatment and care. The Orchard, Riverside Health System’s senior adult living community in Warsaw, Virginia, has received the Bronze Commitment to Quality Award from the American Health Care Association and the National Center for Assisted Living, the second Riverside residential community to receive the distinction. Orchard residents now have access to an exercise program that offers important attributes that go beyond the well-
documented benefits of physical activity. The innovative new program is especially designed, through its emphasis on strengthening core muscles, to help older adults avoid falls.
If you have News you would like to share with our readers in the Winter 2017 edition, please contact the publisher at 757-237-1106 or email: holly@hrphysician.com Deadline for submissions is January 4th.
Get Off Your Butt It’s The Lung Cancer Awareness Month & Great American Smokeout Resource Fair Wednesday, November 16, 2016 6 – 7:30 p.m. Lifestyle Center 800 Battlefield Blvd., North, Chesapeake VA 23320 • Lung Health Screenings • Quit Kits • Talk with Physicians • Hear from a Lung Cancer Survivor • Door Prizes To register, call: 757-312-6132 or go to chesapeakeregional.com/GetOffYourButt
Fall 2016 Hampton Roads Physician | 53
WELCOME TO THE COMMUNITY
Adel Aziz, MD has joined Riverside Neurology Specialists. He received his medical degree at Tripoli University in Libya. He completed an internal medicine residency at St. Joseph’s Hospital and Medical Center in Paterson, New Jersey, as well as a neurology residency at University Hospitals Case Medical Center in Cleveland. He is fellowship trained in behavioral neurology at Mayo Clinic in Florida and Board certified by the American Board of Internal Medicine and the American Board of Neurology. Parker W. Babington, MD has joined Neurosurgical Associates. He received his BA from the University of Virginia and his medical degree from EVMS. He completed his general surgery internship and neurosurgical residency at George Washington University Hospital.
J.R. Barley, DO has joined Riverside Orthopedics and Sports Medicine. He earned his medical degree from the Philadelphia College of Osteopathic Medicine and completed a family medicine residency with Riverside Brentwood Family Medicine in affiliation with Virginia Commonwealth University. He subsequently completed fellowship training in primary care sports medicine at Wake Forest University. Dr. Barley is Board certified in both family medicine and primary care sports medicine. Lucianna Bester, MD has joined Lakeview Pediatrics & Family Medicine. She received her medical degree from Eastern Virginia Medical School, and completed her Family Medicine residency at Riverside Family Medicine.
Elen Blochin, MD, PhD has joined EVMS Dermatology. She is certified by the American Board of Anatomic and Clinical Pathology and the American Board of Pathology and Dermatology. Dr. Blochin received her medical degree from Russian State Medical School in Moscow, Russia. She completed an anatomic pathology/ clinical pathology residency at New York University Medical Center and a pediatric hematology and oncology residency at the Research Institute of Children’s Hematology and Oncology in Moscow. Dr. Blochin completed a dermatopathology fellowship at the Ackerman Academy of Dermatopatholgy in New York, as well as an oncologic surgical pathology fellowship at Memorial Sloan Kettering Cancer Center in New York.
54 | www.hrphysician.com
Rose Cummings, DO, a Board certified pediatric cardiologist, has joined Children’s Hospital of The King’s Daughters. She earned her medical degree from New York College of Osteopathic Medicine, completed her pediatric residency at Children’s Hospital at Sinai Hospital, and completed a pediatric cardiology fellowship at Children’s Healthcare of Atlanta at Emory University.
Charles Dillard, MD has joined the pediatric physical medicine and rehabilitation team at Children’s Hospital of The King’s Daughters. He earned his medical degree from VCU School of Medicine and completed his residency in physical medicine and rehabilitation at VCU, where he served as chief resident.
Afua Dodoo, DO has joined Sentara Hospital Medicine Physicians at Sentara Princess Anne Hospital. She earned her medical degree from Philadelphia College of Osteopathic Medicine and completed her residency at the University of Connecticut School of Medicine.
Mariel Focseneanu, MD is now offering pediatric and adolescent gynecologic care at Children’s Hospital of The King’s Daughters and CHKD Health System locations. She earned her medical degree from Yale School of Medicine and did her residency in obstetrics and gynecology at New York Presbyterian HospitalWeill Cornell Medical Center. She also completed a two-year fellowship in pediatric and adolescent gynecology at Washington University in St. Louis. Janine Frank, MD has joined Princess Anne Medical Associates. She received her medical degree from State University of New York at Buffalo, and completed her Internal Medicine residency at the University of Pittsburgh Medical Center.
Timothy Fusiak, DO has joined Sentara Pulmonary, Critical Care & Sleep Specialists in Norfolk. He earned his medical degree from Nova Southeastern University – College of Osteopathic Medicine. He completed his pulmonary and critical care medicine fellowship at Stony Brook University Hospital and his internal medicine residency at Jersey Shore University Medical Center.
Lori Gatzke, MD has joined Riverside Suburban Family Practice. She earned her medical degree from the Virginia Commonwealth University School of Medicine and completed VCU’s Chesterfield Family Practice Residency Program. She is certified by the American Board of Family Medicine.
Anubhi Goel, MD has joined Sentara Hospital Medicine Physicians at Sentara Virginia Beach General Hospital. She earned her medical degree from Sawai Man Singh Medical College and completed her internal medicine residency at New York Hospital Medical Center of Queens. Justin W. Griffin, MD has joined Jordan-Young Institute in Virginia Beach. He is a fellowship trained orthopaedic surgeon specializing in the latest techniques in shoulder, elbow and knee surgery, as well as treatment of sports related injuries including advanced arthroscopic, minimally invasive reconstructive techniques. Patrick Haggerty, MD joins EVMS Infectious Diseases. Dr. Haggerty received his medical degree and completed an internal medicine residency at EVMS and an infectious disease fellowship at the Medical College of Virginia. He is Board certified in infectious diseases and internal medicine. Asima Haleem, MD has joined Sentara Family Medicine Physicians in Suffolk. She earned her medical degree from Lahore Medical and Dental College. She has a special interest in women’s health services.
Edward Hanna, MD has joined Battlefield Medical Associates. He received his medical degree from Jefferson Medical College, and completed his Family Practice residency at Malcolm Grow Medical center, Andrews Air Force Base.
Jared Harrison, DO has joined Riverside Norge Internal Medicine and Pediatrics. After undergraduate studies at the University of Richmond, Dr. Harrison earned his medical degree at Edward Via College of Osteopathic Medicine. He completed a residency in family medicine and osteopathic manipulative treatment at Penn State Health St. Joseph. He is certified by the American Osteopathic Board of Family Physicians.
?
Are You an Independent Physician
We can help you stay that way!
Christopher L. Graff JD, CPBC
John G. Corley, III, MBA, CPBC
We provide full service consulting, tax an accounting services and have been serving the needs of the Hampton Roads medical community for nearly 40 years. Find out how you can remain independent, or become independent and grow your practice!
The Medical Management Consulting Group, Inc. Your medical practice CFO’s
757-473-9226 Visit our website at www.mmcgonline.com
154 Newtown Road, Suite B-4 Virginia Beach, VA 23462 Fall 2016 Hampton Roads Physician | 55
WELCOME TO THE COMMUNITY
Bert Holmes, MD has joined Patient Choice Oceana a division of Bon Secours Hampton Roads Health System. He received his medical degree from Meharry Medical College in Nashville, Tennessee, where he also completed his internal medicine residency.
Steven Hospodar, MD has joined Riverside Orthopedics in Gloucester. After earning his medical degree from the Medical College of Virginia, Dr. Hospodar completed internships in general and orthopedic surgery, as well as an orthopedic surgery residency, at Wilford Hall USAF Medical Center in San Antonio, Texas. He is Board certified in orthopedic surgery and sports medicine Marybeth S. Hughes, MD joins EVMS Medical Group as Chief of EVMS Surgical Oncology. She received her medical degree and completed her surgery residency at EVMS before completing her surgical oncology fellowship at the National Cancer Institute NIH, in Bethesda, MD. Dr. Hughes is certified by and a fellow in the America College of Surgeons, an advanced trauma life support instructor and a DaVinci Robotic Consult Surgeon.
Stephen Hunley, MD has joined Sentara Cardiology Specialists in Williamsburg. Dr. Hunley earned his medical degree from the University of Kentucky College of Medicine. He completed his interventional cardiology fellowship at Virginia Commonwealth University, his cardiology fellowship at East Carolina University College of Medicine and his internal medicine residency at the University of Kentucky College of Medicine. Luke Kohan, MD has joined Sentara Cardiology Specialists in Norfolk. He earned his medical degree from State University of New York, Upstate Medical University. He completed his cardiovascular medicine/interventional cardiology fellowship at the University of Virginia and his internal medicine residency at Wake Forest Baptist Medical Center.
Elizabeth Jenkins, MD joins EVMS Endocrine & Metabolic Disorders. She received her medical degree from the University of Virginia, School of Medicine. She completed her internal medicine residency at the School of Medicine & Dentistry, University of Rochester, and an endocrinology fellowship at the University of Maryland School of Medicine in Baltimore. She is Board certified in internal medicine and endocrinology, diabetes & metabolism.
HAND THERAPY Tendonitis and Bursitis: Trigger Finger, DeQuervain’s Overuse Injuries: Tennis Elbow/Golfer’s Elbow Post-trauma and Reconstructive Surgeries Sport Injuries • Arthritis • Custom Splints
flixr tpti.com Williamsburg | First Colonial | Red Mill | Gloucester | John Rolfe 56 | www.hrphysician.com
Kent Lam, MD joins Dr. Joseph Han in EVMS Ear, Nose & Throat Surgeons after completing his fellowship in rhinology and anterior skull base surgery at the University of Texas Health & Science Center in Houston. Dr. Lam received his medical degree from Georgetown University School of Medicine in Washington, DC and an otolaryngology residency at Northwestern University Feinberg School of Medicine in Chicago, Illinois. He is Board certified in OtolaryngologyHead and Neck Surgery. Donna Lawson, DO has joined Sentara Hospital Medicine Physicians team at Sentara Princess Anne Hospital. She earned her medical degree from Virginia College of Osteopathic Medicine and completed her residency at Lewis Gale Hospital Montgomery.
Steven J. Lewis, MD MPH joins EVMS Portsmouth Family Medicine after completing his Family Medicine residency and serving his final year as an Academic Chief Resident at EVMS. Dr. Lewis received his medical degree and masters in public health from the University of Virginia School of Medicine in Charlottesville, Virginia. He is Board certified in Family Medicine.
Raffaele Marchigiani, MD has joined Sentara Surgery Specialists at Sentara Leigh Hospital. He earned his medical degree from American University of Antiqua College of Medicine. He completed his cardiothoracic surgery fellowship at the University of Iowa Hospitals and Clinics and completed his residency at St. Luke’s University/Temple University.
Margaret McGuire, MD has joined Children’s Hospital of The King’s Daughters’ pediatric surgery team. She earned her medical degree at Jefferson Medical College of Thomas Jefferson University, completed a surgical residency at the University of Massachusetts, and was a surgical research fellow at Boston Children’s Hospital. She is certified by the American Board of Surgery in general surgery and critical care. Akin Ojo-Carons, MD has joined Urology of Virginia. He completed his medical degree from Albert Einstein College of Medicine, Yeshiva University, New York and completed his surgical internship and urology residency training at Northshore-LIJ Health system, Smith Institute for Urology. He completed a fellowship in female pelvic medicine and reconstructive surgery training in Woodbury, MN.
Talent, Skill, Compassion. Riverside’s team of cardiovascular and thoracic surgeons welcomes Dr. Rozales A. Swanson. Fellowship trained and board certified, Dr. Swanson is a highly skilled surgeon with special expertise in: • •
Ventricular assist device implantation Mitral valve repair and replacement
Heart & Vascular
757-394-9800
Rozales A. Swanson, M.D.
riversideonline.com/talent Fall 2016 Hampton Roads Physician | 57
WELCOME TO THE COMMUNITY
Mary Ojo-Carons, MD has joined Monarch Women’s Wellness and Lakeview Obstetrics & Gynecology. She received her medical degree from Georgetown University School of Medicine, and completed her Obstetrics & Gynecology residency at The Mount Sinai School of Medicine Hospital.
Olusegun Olusesi, MD, an electrophysiologist, has joined the Sentara Cardiology Specialists team. He earned his medical degree from the University of North Carolina. He completed his cardiology fellowship at Washington University at St. Louis/ Barnes-Jewish Hospital and completed his internal medicine residency at Yale School of Medicine.
• Custom compounding for individualized care • Medications for: skin care, hospice needs, pain management, hormone replacement therapy & more... • Superior facilities and staffing • Special dosage forms such as ointments, creams, gels, injections, suspensions, etc.
We Moved!
4001 Virginia Beach Blvd., Suite 110 Virginia Beach, VA 23452 (757)934-0533 Toll Free: (877) 873-9564 Fax: (757) 228-3991 Other locations include: Jamestown, NY • Erie, PA Houston, TX • Greenville, SC
58 | www.hrphysician.com
Kerry Prewitt, MD has joined Sentara Cardiology Specialists in Williamsburg. He earned his medical degree from Emory University School of Medicine. He completed his interventional cardiology fellowship at Johns Hopkins Medical Institution, his cardiology fellowship at Walter Reed Army Medical Center and his internal medicine residency at Fitzsimons Army Medical Center. Animesh Rathore, MD has joined Sentara Vascular Specialists in Norfolk. He earned his medical degree from Grant Medical College. He completed a vascular and endovascular fellowship at Mayo Clinic, a pediatric surgery fellowship at Yale New Haven Hospital, a general surgery residency at the University of Nebraska and a general surgery residency at Harlem Hospital Center. Adam Sagarwala, DO has joined Riverside Vascular Specialists in Newport News. He earned his medical degree at Texas College of Osteopathic Medicine, and served his internship at St. Barnabas Hospital in New Jersey. He completed his residency at Doctors’ Hospital Ohio Health, and a fellowship at Newark Beth Israel Hospital Medical Center. He is Board certified. Lauren E. Salmon, DO has joined Riverside Cancer Specialists of Tidewater in Suffolk and Virginia Beach. After earning her medical degree from the Virginia College of Osteopathic Medicine in Blacksburg, she completed an internal medicine residency at Christiana Care Hospital in Newark, DE. She also completed fellowship training in hematology and oncology at East Carolina University in Greenville. Dr. Salmon is Board certified in internal medicine and Board eligible in hematology and medical oncology.
Manuela Schuksz, MD has joined the Sentara Vascular Specialists team in Hampton. She earned her medical degree from the University of California and completed her vascular surgery residency at the University of Massachusetts. Tammis Seipel, MD has joined Virginia Beach Internal Medicine. She received her medical degree from Ross University School of Medicine, and completed her Internal Medicine residency at Eastern Virginia Medical School. Minal Shah, MD has joined Sentara Hospital Medicine Physicians at Sentara Leigh Hospital. She earned her medical degree from Baylor College of Medicine and completed her residency at Baylor College of Medicine. Elias Siraj, MD joins EVMS Medical group as Chief, EVMS Endocrine & Metabolic Disorders, EVMS Strelitz Institute. Dr. Siraj received his medical degree from Addis Ababa University, School of Medicine, Ethiopia. He completed an internal medicine residency and a fellowship in endocrinology at the Cleveland Clinic /Foundation in Cleveland, OH. He is Board certified in internal medicine and endocrinology, diabetes & metabolism. John Sloboda, MD has joined Riverside Orthopedic Specialists in total hip/knee replacement and hip preservation. He earned his medical degree from Case Western Reserve University in Cleveland. He completed an orthopedic surgery residency at Madigan Army Medical Center at Fort Lewis in Tacoma, Washington, and a total joint fellowship with Carilion Clinic in affiliation with Virginia Tech School of Medicine. He is Board certified in Orthopaedic Surgery and Orthopaedic Sports Medicine.
Tequilla Pryor-Hunter, MD has joined Lakeview Pediatrics. She received her medical degree from the Medical College of Georgia, and completed her Pediatrics residency at the Children’s Hospital of The King’s Daughters.
Raman Unnikrishnan, MD has joined Urology of Virginia. He earned his medical degree from the University of Kentucky. After an internship in general surgery, he completed his residency in urology at the Glickman Urological and Kidney Institute at the Cleveland Clinic in Cleveland Ohio.
WHAT YOU’VE BUILT
IS WORTH PROTECTING.
MassMutual’s disability income insurance products help you protect your income in the event you become too ill or injured to work. And if you own a medical practice with two or more qualifying staff or professionals, you may be eligible for: • Unisex rates • Portable coverage • Rate discount • Non-cancellable, guaranteed continuable coverage to age 65 provided premiums are paid on time • Own occupation rider* Please contact me today to learn more! Robert P. Burke, CLU®, ChFC®, AEP General Agent MassMutual Commonwealth 222 Central Park Avenue, Suite 1100 Virginia Beach, VA 23462 757-490-9041 robertburke@financialguide.com www.massmutual.com/commonwealth LIFE INSURANCE + RETIREMENT/401(K) PLAN SERVICES + DISABILITY INCOME INSURANCE LONG TERM CARE INSURANCE + ANNUITIES
MassMutual Financial Group refers to Massachusetts Mutual Life Insurance Co. (MassMutual), its affiliated companies and sales representatives. Local sales agencies are not subsidiaries of MassMutual or its affiliated companies. *Available at additional cost; not available in CA. Insurance products are issued by MassMutual, Springfield, MA 01111, and its subsidiaries, C.M. Life Insurance Company and MML Bay State Life Insurance Company, Enfield, CT 06082. CRN201806-172248
Fall 2016 Hampton Roads Physician | 59
WELCOME TO THE COMMUNITY
Katharine M. Van Slyke, DO has joined TPMG Coastal Internal Medicine and Tidewater Bariatrics. She earned her Doctor of Osteopathic Medicine degree from Philadelphia College of Osteopathic Medicine, where she also completed an internship and residency in Internal Medicine. She did her residency at EVMS, and is certified by the American Osteopathic Board of Internal Medicine. Erin Vipler, MD has joined Sentara Hospital Medicine Physicians at Sentara Virginia Beach General Hospital. She earned her medical degree from the University of Miami Miller School of Medicine and completed her internal medicine residency at The George Washington University.
Cara A. Watts, MD has joined Riverside Ear, Nose and Throat Physicians and Surgeons in Newport News. After her undergraduate studies at Yale University, Dr. Watts earned her medical degree at the University of Virginia School of Medicine. She completed an Otolaryngology - Head and Neck surgery residency with the University of Illinois at Chicago Medical Center.
Candace Wise, DO has joined Riverside Family Care and Internal Medicine in Williamsburg. She earned her medical degree from the West Virginia School of Osteopathic Medicine and completed the Shenandoah Valley Family Practice Residency Program affiliated with the Medical College of Virginia at VCU.
Alfloyd Woodard, MD has joined Sentara Hospital Medicine Physicians at Sentara Princess Anne Hospital. He earned his medical degree from Virginia Commonwealth University and completed his internal medicine residency at Christiana Care Health System.
We would like to welcome your new physicians, NPs and PAs Please contact us at 757-237-1106 or email: holly@hrphysician.com Deadline for submissions for the Winter edition is January 4
Welcome NPs and PAs
Amber Achensinski, PA Sentara Cardiology Specialists team at Sentara Leigh Hospital.
Beatrice Clayton, MSN, CRNP Sentara Hospital Medicine Physicians at Sentara CarePlex Hospital.
Casey Dashiell, PA Sentara Cardiology Specialists at Sentara Leigh Hospital.
Holly Griffith, PA Sentara Orthopaedic Trauma Specialists.
Christina Hunley, PA-C Sentara Cardiology Specialists.
Letitia Juday, PA Sentara Cardiology Specialists.
Jeffrey Padgett, PA-C Sentara Urgent Care.
Grace Pagtakhan, NP Sentara Family Medicine Physicians
Brittany Ptachick, NP Sentara Family Medicine Physicians.
60 | www.hrphysician.com
Paula Figgs, PA-C Neil Donovan, PA-C Sentara Vascular Specialists Sentara Urgent Care in Williamsburg.
Amanda Kubin, PA-C Sentara Neurology Specialists.
Kimberly Maigi, FNP-C Riverside Primary Care Center.
Michelle Gideon, MSN, FNP-C Sentara Vascular Specialists
Kristin Grabill, PA-C Sentara Family Medicine Physicians.
Thomas McDonald, PA Amanda Murphy, PA Sentara Pulmonary, Critical Sentara Neurosurgery Specialists. Care & Sleep Specialists.
Stephanie Sarfan, PA Robert Surprenant, PA-C Taylor Watrous, Sentara Cardiology Sentara Hospital Medicine PA-C Sentara Urgent Care. Specialists. Physicians at Sentara Norfolk General Hospital.
Francine Wright, DNP Sentara Hospital Medicine Physicians at Sentara Norfolk General Hospital.
LAKE TAYLOR DELIVERS AWARD-WINNING RESPIRATORY CARE
NOW I CAN... TAKE THE FAST LANE.
Regional leader in pulmonary rehabilitation and therapies, Lake Taylor Transitional Care Hospital has been recognized by both the AARC and AHCA/NCAL with national awards for quality in the area of respiratory care. Our ventilator weaning success rate, three times the national average, has resulted in families and providers relying on Lake Taylor as a resource for referrals from across the nation. L O N G T E R M A C U T E C A R E H O SPITA L | SKI L LE D NURSI N G | L ON G -T E R M C A R E
The Future of Health Care for a World in Transition
TM
Centrally located in Hampton Roads
For more information, visit LakeTaylor.org today or call 757-461-5001, ext. 475. 757.461.5001 ex t. 475 | www.laketaylor.org | 1309 Kempsville Road | Norfolk, VA 23502
Fall 2016 Hampton Roads Physician | 61
Awards Accolades
Celebrating the Accomplishments of Those Who have Received Major Honors
A book co-written by Alfred Abuhamad, MD, Mason C. Andrews Chair in Obstetrics and Gynecology, Professor and Chair of EVMS Obstetrics and Gynecology, and Vice Dean for Clinical Affairs, was recognized by the British Medical Association (BMA) awards ceremony. The organization named A Practical Guide to Fetal Echocardiography: Normal and Abnormal Hearts its Medical Book of the Year.
Jessica Churchill, a fourth-year medical student at Eastern Virginia Medical School, was recently honored by the Medical Society of Virginia for her service as a Medical Student. The award was given to physicians and medical students in the Commonwealth for their selfless services to others, impact to the health of the population served and commitment to health care excellence at Medical Societyâ&#x20AC;&#x2122;s 12th annual Salute to Service Award at its Annual Physicians Gala.
Richard Conran, MD, PhD, JD, EVMS Professor and Chair of Pathology and Anatomy, has received a key award from the Association of Pathology Chairs (APC). Dr. Conran was selected to receive the Michele Raible Distinguished Teaching Award, which honors pathology educators who demonstrate a range of contributions at the local, regional and national levels in undergraduate medical education. The award was presented at the APC annual meeting in July. Dr. Conran came to EVMS in 2013 following a career in the US Army.
Your ideas are yours.
Protect them.
Our clients trust Goodman Allen Donnelly with their credentialing matters, Board of Medicine complaints, internal audits and litigation matters. Let us help you with your broader legal needs. Our Intellectual Property team can help you protect your important contributions to the medical field. From medical devices to biopharmaceuticals, we are equipped to secure and defend your rights.
Matthew R. Osenga RICHMOND 804.346.0600
62 | www.hrphysician.com
Dr. Elizabeth Yeu received a Top Forty Under 40 award from Inside Business. She is a corneal, cataract and refractive surgery specialist at Virginia Eye Consultants.
Learn more about our Intellectual Property team at www.goodmanallen.com.
Charles M. Allen CHARLOTTESVILLE 434.817.2180
Martha A. Weis NORFOLK 757.625.1400
501 Discovery Drive, Chesapeake
NOW OPEN
Meet Your Chesapeake Team
SCHEDULE AN APPOINTMENT TODAY 757-547-5145 smoc-pt.com | Chesapeake | Suffolk | BelleHarbour
ORTHOPAEDIC CARE | SPINE CARE | PHYSICAL THERAPY | INTERVENTIONAL PAIN MEDICINE Back Row (Left to right): Richard D. Guinand, DO, Deniz O. Goss, PA-C, Timothy S. Winkler, PA-C, Lena Sifen, PA-C, Stephen Warwick, PA-C, Scott Clingan, MSHS, PA-C, Victor Tseng, DO Front Row: Samuel I. Brown, MD, Michael M. Romash, MD, Gordan J. Iiams, MD, David G. Goss, MD, FAAOS, Scott E. Grabill, DO, A. Jamali, MD, FACS
S AY “ Y ES” TO
LIFE WITHOUT LIMITS
READ TRUE STORIES FROM OUR PATIENTS AT SMOC-PT.COM
Bon Secours Surgical Specialists:
WHY SEND YOUR PATIENTS ANYWHERE ELSE? Better outcomes. Greater satisfaction. Thatâ&#x20AC;&#x2122;s why more physicians are referring their patients to Bon Secours Surgical Specialists. Our surgical teams are some of the most experienced in the region and are led by expert surgeons who are breaking new ground in state-of-the-art minimally invasive surgery, using laparoscopic and robotic surgical techniques. Our surgical specialists lead the way across a wide array of specialties including general surgery, bariatric, colorectal, and surgical oncology. With seven offices across Hampton Roads, your patients will have convenient access to the innovative, compassionate surgical care they need and deserveâ&#x20AC;&#x201D; with less pain, shorter recovery and improved outcomes.
To learn more, visit BonSecours.com/surgicalspecialists DePaul
Maryview
Mary Immaculate
757-278-2220
757-483-3030
757-947-3170
Elizabeth Barrett, MD, FACS general & bariatric surgery
Joseph Frenkel, MD, FACS, FASCRS colon & rectal surgery
Gregory Adams, MD, FACS general & bariatric surgery
Jeffrey Riblet, MD, FACS general surgery
Anthony Terracina, MD, FACS bariatric surgery
Pete Williams, MD, FACS general & robotic surgery
Charles Ives, MD, FACS general & breast surgery
Yassar Youssef, MD, FACS general & robotic surgery
Chong Lee, MD, FACS, FASCRS colon & rectal surgery