Harvard Public Health Review
Fall 2011
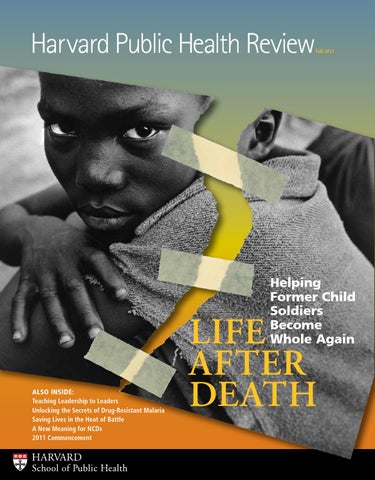
Helping Former Child Soldiers Become Whole Again
Also Inside: Teaching Leadership to Leaders Unlocking the Secrets of Drug-Resistant Malaria Saving Lives in the Heat of Battle A New Meaning for NCDs 2011 Commencement
HARVARD
School of Public Health
Life after Death
Dean’s Message
A Broader View of Global Security
T
he year 2001 saw not only the horrors of 9/11 and the anthrax attacks, but also the establishment of the UN Commission on Human Security. In its report to the General Assembly, the commission wrote that human security “means protecting people from critical and pervasive threats and situations, building on their strengths and aspirations. It also means creating systems that give people the building blocks of survival, dignity, and livelihood.” In a world of rapid global change, that is the timeless mission of public health. Indeed, during the past decade, the health agenda has moved from the exclusive domain of medical and public health practitioners to take center stage among many different groups of experts as they address some of the most pressing issues of our time. We now understand that: • Good health is not just the result of economic development—it is one of the conditions for economic development to occur at all. Much of why some nations develop faster than others is that their people enjoy better health.
2
Harvard Public Health Review
The absence of good health, generated by the slow-burning persistence of huge inequities around the world, is one of the major causes of global insecurity. This issue of the Review offers a number of stories demonstrating Harvard School of Public Health’s broader sense of what constitutes global health security. The cover story on Theresa Betancourt, who for nearly two decades has worked with children traumatized by war, illustrates how HSPH researchers are trying to help promote resilience and healing in these young people. The School’s National Preparedness Leadership Initiative, co-led by Lenny Marcus and David Gergen, demonstrates that enlightened leadership in times of disaster is a quality that can actually be taught. Other stories on HSPH’s impact on malaria, military medicine, TB, and health inequities underscore how health is at the heart of global security.
The absence of good health, generated by the slow-burning persistence of huge inequities around the world, is one of the major causes of global insecurity. The injustice represented by the millions of unnecessary deaths from preventable causes breeds social discontent that may eventually lead to resentment and extremism. It is by improving health, addressing fundamental inequities, and preventing threats to well-being that we in public health can be leaders in bringing about true global security.
Julio Frenk Dean of the Faculty and T & G Angelopoulos Professor of Public Health and International Development, Harvard School of Public Health
Kent Dayton/HSPH
• Good health is key for national security and economic stability. Infectious disease pandemics can potentially kill thousands, disable millions, and disrupt entire economies. Investments in epidemiologic surveillance and response are crucial to controlling threats—whether natural or man-made.
• Good health underlies democratic governance and the realization of human rights. A comprehensive definition of health security includes access to health care as well as protection against the economic consequences of disease—so that no one goes broke for getting sick.
Harvard Public Health Review
Fall 2011
18 Life after Death Theresa Betancourt has made it her mission to understand resilience and healing in former child soldiers and war-affected youth. 2 Dean’s Message Also in this Issue A broader view of global security 14 4 Frontlines 14 Teaching Leadership to 10 Philanthropic Impact Leaders 45 Alumni News Helping seasoned professionals handle unprecedented disasters 47 Faculty News 26 Unlocking the Secrets of Drug Resistance in Malaria Parasites New gene search tool opens “endless possibilities”
26
29 A Public Health Perspective for Physicians Commonwealth Fellows 32 Returning Home A plan to thwart killer TB 36 Saving Lives in the Heat of Battle Delivering military medicine in Afghanistan 40 Looking Back, Looking Ahead Commencement 2011
Image Credits: Cover, 14-year-old child soldier from Sierra Leone ©Stuart Freedman/ PANOS; This page top and center, Kent Dayton/HSPH; below, Comstock/Getty Images
42 Strengthening Health Systems to Address “New Challenge Diseases” Reframing the familiar public health acronym “NCD”
47 Bookshelf 48 In Memoriam 49 Continuing Professional Education Calendar
Clarification The Spring/Summer 2011 issue of the Review included an article by HSPH professor emeritus Bernard Lown, “Waging Peace, Saving Lives,” which described Lown’s lessons and observations as an antinuclear activist. A photo caption incorrectly identified Lown as the “founder of Physicians for the Prevention of Nuclear War.” In fact, Lown was the co-founder of International Physicians for the Prevention of Nuclear War, along with American physicians Herb Abrams, Eric Chivian, and Jim Muller, and with Soviet physicians Evgueni Chazov, Leonid Ilyin, and Mikhail Kuzin. In addition, the article states that IPPNW was founded in 1981; the correct year is 1980.
front lines
Listen Up: Kids Get Fewer Ear Infections in Smoke-Free Homes
I
Attorney General SPEAKS ON YOUTH VIOLENCE AT HSPH U.S. Attorney General Eric Holder advocated a public health approach to addressing youth violence at a May 6 Forum webcast. The event was moderated by Jay Winsten, Frank Stanton Director of the Center for Health Communication at HSPH. Watch
n the first study to show the public health benefits to children of the increase in smoke-free homes across the U.S., researchers from HSPH and Ireland’s Research Institute for a Tobacco Free Society quantified a decline over the last 13 years in middle ear infections among children. The study attributes the drop—which reverses a long-term upward trend—to the rise in U.S. households that have adopted voluntary no-smoking rules: from 45 percent in 1993 to 86 percent in 2006. Lead author Hillel Alpert, research scientist in HSPH’s
online at http://hsph.me/holder-forum.
Organized chaos: tracking cellular crowds
pull as they migrate through the human body—even while they’re moving cooperatively in the same intended direction. A new study by HSPH and the Institute for Bioengineering of Catalonia found that cell groups migrating toward a task—say, healing a wound, creating an embryo, or forming a malignant tumor—are far less orderly than once thought. Understanding how and why cells behave as they do in large groups may lead to ways to control or interrupt diseases such as cancer that
Department of Society, Human Development, and Health, says that if parents avoid smoking at home, they can “protect their children from [ear infections], the most common cause of visits to physicians and hospitals for medical care.” A seminal paper published by the School’s Dimitrios Trichopoulos in 1981 was among the first to establish a link between secondhand smoke and lung cancer.
involve abnormal cell migration.
Learn More Online Visit the Review Online at http://hsph.me/frontlines for links to press releases, news reports, videos, and the original research studies behind these stories.
4
Harvard Public Health Review
Clockwise from top: Kent Dayton/HSPH; Ebby May/Getty Images; Shaw Nielsen, illustration
Like racers jostling for position, groups of cells push and
The Heat is On A new study by researchers at HSPH and Johns Hopkins Bloomberg School of Public Health looked at how heat waves—predicted to increase in number and intensity with global climate change—may affect city dwellers. Currently, according to American Red Cross statistics, heat waves cause more deaths than all other weather events combined. (In just one week in 1995, a summer heat wave in Chicago caused nearly 700 excess deaths.) The HSPH/ Johns Hopkins research, led by Francesca Dominici, HSPH professor of biostatistics and associate dean for information technology, estimated that in the years 2081–2100, Chicago could see 166 to 2,217 additional deaths annually—“a profound impact,” according to Dominici.
Clinton and Sebelius Visit HSPH-affiliated Clinics in Tanzania
H
SPH faculty are engaged in various research and training initiatives in Tanzania, with the ultimate aim of improving maternal and child health and reducing the risk of infectious diseases such as HIV, TB, and malaria. On June 12, 2011, U.S. Secretary of State Hillary Rodham Clinton visited the Buguruni Health Center in Tanzania. That facility, associated with HSPH, offers reproductive and child health services. U.S. Secretary of Health and Human Services Kathleen Sebelius attended the opening of the Mnazi Mmoja Center for Excellence in HIV Care and Education in Dar Es Salaam, Tanzania, on July 22. The Center, for which HSPH Dean Julio Frenk helped lay the foundation stone earlier this year, provides a general outpatient clinic with services for family planning, reproductive and child health, HIV care and treatment, and tuberculosis care. It also serves as a site for training in HIV management to develop nationally recognized leaders in the field, and to conduct research to advance knowledge related to management of HIV/AIDS. Funding for the Center comes from the United States via the School’s President’s Emergency Plan for AIDS Relief (PEPFAR) program in Tanzania, the U.S. Department of Health and Human Services, and an agreement with Management Development for Health (MDH), an independent organization in Tanzania established with support from HSPH, that aims to sustain and expand existing public health service programs.
Women’s Height Declining in Developing Countries U.S. Department of State
Over the last 40 years, adult women’s height in economically deprived countries has either declined or stalled. The findings come from a new HSPH study that tracked this key indicator of the health and wellbeing of a population, and a predictor of children’s chances for survival. The declines are thought to reflect poor nutrition, exposure to infections, and other environmental factors that may stunt or hamper children’s growth. The study, whose lead author was S.V. Subramanian, HSPH professor of population health and geography, tracked women’s height in 54 countries between 1994 and 2008.
Fall 2011
5
front lines Seeing Patients through the Lens of Impoverished Lives Day after day, the medical histories of the young patients Nadine Burke, MPH ’02, treated at her clinic in San Francisco’s impoverished Bayview-Hunters Point neighborhood followed strikingly similar patterns. Childhoods marred by stress and trauma were followed
Study Reveals Racial Differences in Stress Levels
A
n HSPH team led by research fellow
Michelle Sternthal found that African-Americans
by a host of adult physical ailments such as asthma, scabies, and weight
and U.S.-born Hispanics
problems. As described in a March 21 profile in The New Yorker, Burke
suffer higher stress levels
realized one day, after treating a teenage mother: “What if [the patient’s]
than whites and foreign-
anxiety wasn’t merely an emotional side effect of her difficult life, but the
born Hispanics—and that
central issue affecting her health?” Today, the Bayview Child Health Center addresses the physiological effects of patients’ childhood traumas—and Burke hopes to eventually develop a protocol much like those that doctors use for treating patients with cancer and other diseases.
this stress contributes to these groups’ frequently poorer health compared to whites. The investigators studied 3,000+ Chicago blacks, whites, and Hispanics ages 18 and older. According to senior author David R. Williams, HSPH’s Florence and Laura Norman Professor of Public Health, “This study underscores the importance of safety-net programs—unemployment benefits, cash assistance,
Governor Patrick Describes Next Phase of Health Care Reform
housing, child care, and transportation benefits
Massachusetts Governor Deval Patrick spoke about the next phase
to low-income working
of Massachusetts health care reform—controlling costs and improv-
families—to promote the
ing quality—at an April 28 Forum event. The governor’s speech was
economic well-being and
Professor of the Practice of Public Health. Watch online at http://hsph.me/patrick-forum.
6
Harvard Public Health Review
the health of families faced with high levels of stress.”
Ned Brown/HSPH
followed by an expert panel moderated by John McDonough, HSPH
Offthe Cuff
W “
Bill Hanage, Associate Professor of Epidemiology
hy are we seeing so many deadly new forms of E. coli in our food?
Bacteria are a bit like a Mr. Potato Head®. You have the core DNA—which is the potato—and then onto
that are stuck all kinds of other genes that help it adapt to its niche. In bacteria, the promiscuous interchange of genes is happening all the time, so new combinations constantly emerge. And our globalized food chain helps new combinations of genes to reach and colonize new niches. People often say, ‘Bacteria are a primitive life-form.’ No, they’re not. They’ve been around longer than we have and they’ll be around after we leave. It’s estimated that the number of bacterial cells on the planet is five times 1030—that’s a 5 followed by 30 zeroes. To
put that in context, that’s more than the number of stars in the known universe. So in terms of our knowledge of bacteria, we haven’t scraped the tip of the iceberg, not even the thin sheen of ice melt in the midday sun on the top of the iceberg. We’ve seen maybe the top few layers of molecules about to evaporate. Causing foodborne disease is not the primary function of E. coli. It’s just that we tend to notice that quality in them. We’re humans, Kent Dayton/HSPH
we’re self-centered, and what happens to us is the most important thing in the world. Learn More Online
”
Visit the Review Online at http://hsph.me/frontlines for links to press releases, news reports, videos, and the original research studies behind these stories.
Fall 2011
7
front lines
Why IS Health Care Reform So Elusive? Interview with John McDonough Q: W hat are the biggest myths and misconceptions about the Patient Protection and Affordable Care Act? A: A significant number of people believe that there are death panels in the law. And many believe that when the big expansions and the individual mandate take effect in 2014, they are going to have to give up their employer-sponsored insurance and buy individual coverage on their own. Both assumptions are absolutely untrue. John McDonough, HSPH Professor of the Practice of Public Health, was a senior adviser on the U.S. Senate committee responsible for developing
Q: H ow does American public opinion break down on health care reform? A: A bout half of the public—mainly Republicans—says that the law should either be completely repealed or substantially repealed. About half—mainly Democrats—says the law should be kept as is or strengthened.
the Patient Protection and Affordable
Q: Does that suggest Americans have different core beliefs about the issue?
Care Act, the landmark health care
A: There is a broad shared sense—actually, bipartisan—that we spend much more on health care services than we would need to if we had an efficient, effective health care system. The difference is how to do that. For example, Democrats wanted to reduce Medicare spending by $450 billion over ten years and use those proceeds to pay for expanding coverage to the uninsured. Republicans don’t mind cutting Medicare by $450 billion—but they wanted to use the money for tax cuts. It’s not an argument over facts or data. It’s an argument, fundamentally, over values.
reform plan that President Barack Obama signed into law in March 2010. A former Massachusetts state legislator and executive director of the advocacy group Health Care for All, McDonough recently spoke with the Review about the revolutionary
Q: How did health care spending spin out of control?
Security Act of 1935 and the Medicare
A: If you go back to before the 1980s and look internationally at health spending as a percentage of gross national product, you find that the United States is expensive—but bunched among the leading nations. Not until the early 1980s did we become an outlier. We took off and grew at a much faster clip than all of the other industrialized countries. A: That may be because, in the 1980s, the U.S. embraced with gusto this ethos that market competition would fix our health care system. At the state and federal levels, we abandoned different kinds of regulation and instead embraced “competition.” The idea was that it would drive down costs and create better value. But it didn’t.
and Medicaid Act of 1965. His new book is Inside National Health Reform. See page 47 for more information.
8
Harvard Public Health Review
Kent Dayton/HSPH
law, which he compares to the Social
An early draft of the bill that would become the Patient Protection and Affordable Care Act.
Q: In your mind, what’s the best health care system in the world? A: My best of all possible worlds is something like the French system. In terms of public satisfaction, the French are near the top. They spend only about 10 percent of their national income on health care services—very reasonable, by international standards. It’s one of the most effective and efficient and high-quality systems in the world. Everybody is covered. There is complete choice of providers. And even though France spends a lot less money per person than we do, they have more physicians, more hospitals, and more hospital beds per capita. Like many other national health care systems that work, the French system is coherent and cohesive in terms of its financing, workforce planning, access to care, and accountability. All those parts work together toward the common goal of delivering quality health care. Q: How will we pay for the new national law? A: The law gets paid mostly through two buckets. One bucket is ten years of changes in the Medicare program, which is going to generate about $450 billion in savings to the Federal Treasury. For example, the hospital industry agreed to give up $155 billion in revenue that they would otherwise obtain from the Medicare program—they figured that if insurance coverage went up in the U.S., they would eventually recoup the loss. Same deal with the home health industry and others. The other bucket is new “ … in the 1980s, the U.S. taxes and assessments on higher-income individuals, new fees on pharembraced with gusto this ethos maceutical companies and medical device makers, and a fee on insurance companies. that market competition would Q: What’s an especially effective provision in the new law?
REUTERS/Larry Downing
A: One of my favorite provisions in the law is a 10 percent tax on the use of indoor tanning services. When Senate Majority Leader Harry Reid brought out his version of the bill, initially there was no indoor tanning tax. Instead, there was a tax on elective cosmetic surgery that became known as the “Bo-Tax.” It was met with shrieks of anger from many consumers—particularly women—who felt that it was discriminatory, as well as strong opposition from the American Society of Dermatologists. Q: In the final version, the “Bo-Tax” was removed. At the last minute, the Senate substituted a tax on indoor tanning services. In recent years, we’ve seen an explosion in skin cancer diagnoses such as melanoma, especially among women between the ages of 15 and 35. From a public health standpoint, that’s one of the most defensible measures in the law. Thea Singer is a Boston-based science journalist and author.
fix our health care system. At the state and federal levels, we abandoned different kinds of regulation and instead embraced ‘competition.’ The idea was that it would drive down costs and create better value. But it didn’t.” Learn More Online Visit the Review Online at http://hsph.me/frontlines for links to press releases, news reports, videos, and the original research studies behind these stories.
Fall 2011
9
philanthropic impact
A Challenge We Face Together This fall, nearly 500 new students enter HSPH. They come from 44 different countries and 40 U.S. states. Many of them arrive having already accomplished extraordinary things in their careers. They are physicians, professors, scientists, policy analysts, research assistants, medical residents, teachers, and others who see public health as the best way they can make a difference in the world. What better way to welcome them than with the words of Dr. Lakshmi Nayana Vootakuru, who, as student speaker at commencement in May, sent the departing class off with these thoughts: Ellie Starr Public health is about re-imagining this society, to one where education, health, and opportunity are plentiful and access to services is available to those who need it most and can ask for it least. Yes, in this most scientific of fields, firmly rooted in epidemiology and biostatistics, the most salient feature to me is…imagination. Because that is where transformation begins. …Henry David Thoreau said, “This world is but a canvas to our imaginations.” May your imagination give you the vision to create a hundred new realities in every corner of the globe and every frontier of public health.
Imagining a healthier world is a challenge we face together. To everyone who has risen to this challenge—and especially those who have supported our students and contributed to our ambitious goal of tripling financial aid over the next two years—thank you. I can imagine no better way to make a difference than helping committed people whose driving ambition is to make the world a better, safer, more just, and healthier place.
Ellie Starr, Vice Dean for External Relations
Safety Test: Gates Foundation Supports Clinical Trial for Childbirth Checklist
O
f the estimated 130 million births each year around the world, 4 million babies die in the first 28 days of life. Nearly 350,000 of those births result in the mother’s death, 99 percent of them in developing countries. An innovative childbirth safety checklist—a single sheet providing core guidelines to improve safety and health care quality around the time of birth—could have a dramatic impact on making birth safer for mothers and children around the world. Thanks to a $14.1 million, four-year grant from the Bill & Melinda Gates Foundation, HSPH researchers will test the effectiveness of the World Health Organization (WHO) Safe Childbirth Checklist in reducing deaths and improving outcomes for mothers and infants in 120 hospitals in northern India. A team led by Atul Gawande, associate professor of health policy and management at HSPH and a surgeon at Brigham and Women’s Hospital, and co-principal investigator Jonathan Spector, research associate in health policy and management at HSPH and a neonatologist at Massachusetts General Hospital, worked between 2008 and 2010 with the WHO Departments of
10
Harvard Public Health Review
Patient Safety, Reproductive Health and Research, and Maternal, Newborn, Child and Adolescent Health to develop the checklist. The list is expected to be released later this year. The same team will now conduct a clinical trial in areas of extreme poverty in northern India to evaluate the checklist’s impact. Based on a review of existing protocols and produced in consultation with frontline health workers and policymakers around the globe, the list focuses on the biggest killers of mothers and newborns, such as bleeding, infection, high blood pressure, and asphyxia. The childbirth checklist program is modeled after a similar safe-surgery program pioneered by Gawande that reduced surgery-related deaths and complications by more than onethird at eight pilot sites worldwide. “Checklists can be an important tool for health workers, because the documents help organize both the time and resources needed to save the lives of women and newborns during birth,” says France Donnay, Senior Program Officer for Maternal Health at the Gates Foundation. “The Bill & Melinda Gates Foundation is pleased to be a part of this effort.”
Kent Dayton/HSPH
Student speaker Lakshmi Nayana Vootakuru
CIFF Grant Supports New Health Leadership Development Program
H
arvard School of Public Health and Harvard Kennedy School of Government (HKS) will launch a unique ministerial health leadership development program next year in collaboration with the Children’s Investment Fund Foundation (CIFF). Designed for ministerial-level leaders mainly from low- and middle-income countries, the program aims to promote health as a cornerstone of economic development, strengthen political leadership in health, and improve health system performance in the ministers’ own countries. The initiative will place special emphasis on innovations in maternal and child health.
day session that covers progress made and lessons learned. CIFF, a philanthropic organization dedicated to improving the lives of children living in poverty in developing countries, is supporting the program with a two-phase, seven-year grant. The grant awarded for the first phase is $4.01 million. The initial cohort of leaders will give priority to countries in sub-Saharan Africa and India, and in future years the program could expand to include leaders from other regions. Serving as the program’s executive director is Michael Sinclair, former Senior Vice President at the Henry J. Kaiser Family Foundation and head of the Foundation’s South Learning from Africa program. In that role he overDistinguished Peers saw key priorities including health An intensive week-long introducleadership development, child health, tory session for participants will maternal mortality, and HIV/AIDS. open the program next June at HKS. Housed within the new Division Customized to address circumof Policy Translation and Leadership stances specific to each participating Development (PTLD) at HSPH, country, the program will focus on the program will carry out one of topics including leadership for transDean Frenk’s priorities: the translaformation, health and development tion of scientific knowledge into priority setting, political strategy, effective policies and actions. “I am and financing. Distinguished former profoundly grateful to CIFF for its ministers and other high-level govern- support of this effort, which will ment leaders will contribute, adding help fulfill one of my goals as dean an interactive “peer learning” dimenby enabling the School to convene sion to the program. HSPH and HKS current global health leaders to drafaculty, along with local institutions, matically improve the health of their will provide in-country technical citizens,” says Dean Frenk. Jamie and leadership support following the Cooper-Hohn, president and CEO Harvard session to assist leaders in of CIFF, says that the foundation’s implementing health systems improve- partnership in this effort “reflects ments. A year after the program, the our appreciation that the policies, ministers will reconvene for a threeprograms, and resources put in place and allocated by government leaders
are key determinants of progress toward reducing the disproportionately high levels of child mortality and morbidity in these regions.” CooperHohn is an alumna of the Kennedy School as well as a member of the HSPH Board of Dean’s Advisors. Improving Health Systems
“This program hopes to provide a strategic framework aimed at substantially improving the health systems of multiple countries. It provides a bridge to exchange key information between global policy scientists, experienced ministerial policy advisers, and senior decision makers from countries engaged in a transformational process,” notes Division director Robert Blendon, a faculty member with joint appointments in the HSPH Department of Health Policy and Management and at HKS. As a joint project of the two schools, the ministerial program also represents a unique opportunity to couple the Kennedy School’s long tradition of public leadership development with HSPH’s focus on transforming health systems. “We are excited to partner with the School of Public Health to create a unique program to improve the health and livelihood of citizens in developing countries by working with high-level leaders,” says HKS Dean David T. Ellwood. “This is a wonderful opportunity to engage with important international leaders who can create positive change for their societies.”
Fall 2011
11
philanthropic impact
A Humanitarian Academy at Hsph
P
lans are underway to create a new Humanitarian Academy at Harvard School of Public Health, the first global center dedicated to training and teaching the next generation of humanitarian leaders. Approximately 240,000 humanitarian workers worldwide provide billions of dollars in services to millions of aid recipients through relief organizations in more than 100 countries. But in contrast to other large professional pursuits, no major academic programs exist to educate humanitarian aid practitioners in the key principles of their field, such as civilian protection, coordinated aid, and service delivery. The Academy will provide leadership training— both for undergraduate and graduate students as well as
son Eric practices emergency medicine and previously worked for AmeriCares at disaster sites in more than 20 countries. All Weintz’s children serve as trustees for the Foundation. “It seems to us that all you have to do is look at the front page every day to see these kinds of crises arising more and more,” says Weintz. “Maybe it’s a drop in the bucket, but we aim to improve the way disaster relief is taught and handled around the world.” The Academy will coordinate the educational and training activities of several University-wide initiatives, including HHI as well as the François-Xavier Bagnoud (FXB) Center for Health and Human Rights and the Program on Humanitarian Policy and Conflict Research. It will also convene faculty from around Harvard who
Worldwide, approximately 240,000 humanitarian workers provide billions of dollars in services to millions of aid recipients. The new Humanitarian Academy at HSPH is the first center dedicated to educating these professionals in the key principles of their field.
12
Harvard Public Health Review
are engaged in humanitarian studies. Ultimately, the Academy aims to define a new field in education while gathering a community of academics and experts committed to worldwide humanitarian issues. “Without Fred and his family’s support, much of what we have accomplished would not have been possible,” says Jennifer Leaning, director of the FXB Center and François-Xavier Bagnoud Professor of the Practice of Health and Human Rights at HSPH. “Mike VanRooyen, director of HHI, and I are deeply grateful not only for the family’s generous philanthropic support but for their guidance and advice, which has improved our thinking and practice over the years. We are excited to take this important next step in professionalizing humanitarianism.”
Jonathan Ernst/Reuters
for leaders from humanitarian organizations—in areas such as human rights, disaster response, and crisis leadership. The Academy will also develop innovative ways to evaluate the effectiveness of humanitarian aid in order to better serve people in times of war, conflict, and disaster. The Academy is supported by $300,000 in initial seed funding from J. Fred Weintz, Jr., through the Harbor Lights Foundation, which he founded in 1980. Weintz, a graduate of Harvard Business School, is a member of the HSPH Leadership Council and longtime supporter of the School. His family has many years of involvement with humanitarian teaching, training, and global fieldwork, at Harvard and beyond. Weintz’s late first wife, Betsy, was a founding donor of the Harvard Humanitarian Initiative (HHI), and his
Nanoscience and Health: Tiny Technology Raises Big Questions more efficient clean energy alternatives. By 2015, the global market for manufactured goods using nanomaterials is predicted to exceed $1 trillion. Yet the field is still largely unregulated—and scientists are just beginning to understand the possible environmental and public health risks nanoparticles might pose. Panasonic Corporation, one of the Center’s major supporters and industrial partners, gave $300,000 in April to fund HSPH research on nanoscience and environmental health. The company was ranked one of the world’s top 100 most sustainable corporations in 2011 by Corporate Knights, a magazine that focuses on clean capitalism. Demokitrou says that collaborations between the NanoCenter and major nanotechnology companies such as Panasonic represent a “unique opportunity to estabNanoparticles are used in everything from personal electronics to medical devices to food packaging—but their potential risks are still unclear.
T
lish a more sustainable model for industry than we had in the 20th century.”
he year-old Center for Nanotechnology and Nanotoxicology at HSPH (dubbed the NanoCenter) draws on the School’s long history of
studying air particles and their public health impacts. After more than two decades developing methods that have become industry standard for assessing the health effects of exposure to atmospheric particles, HSPH researchers are poised to study the applications and implications of newly engineered nanomaterials and nanotechnology.
Victor Habbick Visions / Photo Researchers, Inc.; Kent Dayton/HSPH
“We now have the ability to generate and manipulate exotic nanostructures nobody ever put on the planet before,” says Philip Demokitrou, assistant professor of aerosol physics in the Department of Environmental Health, who is among the Center’s founding faculty and its director. “But how will these affect biological systems and the environment?” Nanotechnology—the science and engineering of particles less than 100 nanometers wide (or 1/1,000th the diameter of a human hair), for use in everything from personal electronics to medical devices to food packaging—has grown dramatically in the past several
Philip Demokritou, assistant professor of aerosol physics in the Department of Environmental Health, and director of the Center for Nanotechnology and Nanotoxicology at HSPH
Historically, public health investigations have tended to uncover environmental health disasters, such as the pervasive toxic effects of asbestos or PCBs, decades after the damage has been done. Linking research to industry through the Center can help companies establish parameters for safer product development before new materials ever reach the marketplace. As Demokitrou says, “I can’t think of a better way to safeguard
years. Widely considered to be the industrial revolu-
public health.”
tion of the 21st century, the field has the potential to
Learn more about the NanoCenter at www.hsph.harvard.edu/nano.
help develop solutions for improved drug delivery and
Philanthropic Impact stories written and compiled by Rachel Johnson, marketing and communications coordinator. Fall 2011
13
Leadership Development
The National Preparedness Leadership Initiative teaches seasoned professionals how to handle unprecedented disasters.
14
Harvard Public Health Review
Teaching Leadership to Leaders A
© Ho New / Reuters, Kent Dayton/HSPH
t the World Trade Center on 9/11, the New York Fire Department set up a command center at the bottom of World Trade Center One. The supervisors had a vertical view of the disaster—and based on that information, they sent firefighters rushing into the building to help with evacuation. By contrast, the New York police dispatched a helicopter to hover near where the planes hit—a horizontal view. From that perspective, it was clear that girders were red hot and about to melt, and that the building NPLI co-director Leonard Marcus (left) and faculty member Barry Dorn would soon collapse. With that information, the NYPD ordered all police to evacuate. That day, 23 New York police died and more than 320 New York firefighters lost their lives. This tragic anecdote frames a key lesson at a unique joint program run by Harvard School of Public Health and the Harvard Kennedy School (HKS): the National Preparedness Leadership Initiative, or NPLI. The initiative blends academic theory with practical insights from the field. In the case of the 9/11 attacks, the lesson is known as the “cone in the cube” quandary. Observed through a hole on the side of a box (or building), the cone looks like a triangle. Observed through a hole in the top, it looks like a circle. The point is that different responders with different expertise and missions may perceive emergencies differently—but need to glean each other’s perspectives to smoothly choreograph their efforts. Bad leadership is a public health risk
Co-directed by Leonard Marcus, lecturer on public health practice at HSPH, and David Gergen, director of the Center for Public Leadership at HKS, NPLI is grounded in the idea that U.S. leaders continued Fall 2011
15
have much to learn about managing large-scale disasters, both natural and man-made. One of the singular aspects of NPLI is that its faculty have observed leadership close-up during such signal events as the Deepwater Horizon spill, Hurricane Katrina, the 2010 earthquake in Haiti, and the H1N1 pandemic response. As public health risks grow ever more complex—with terrorist threats, emerging infections, globalization of
“ In preparedness, “ time is your ally. In response, time “ is your enemy. “ The longer it takes you to respond and get it right, the more likely you are to fail.” —Leonard Marcus
“In NPLI, we don’t teach management, we don’t teach budgeting, we don’t teach supervision in the classic sense,” explains Marcus. “We teach leadership—because in a crisis, bad leadership is a public health risk.” Meta-Leadership
The “meta” in “meta-leadership” means reaching above and beyond one’s scope of authority to forge ties across disciplines and bureaucracies.
the food supply, and climate change and natural disasters—leaders need different skills than they did in the past. Some 350 individuals have taken NPLI’s intensive on-campus executive education course, and more than 4,000 have participated in shorter city-level summits. Armed with new skills and a broader perspective, graduates return to high-impact jobs at the Centers for Disease Control and Prevention (CDC), state and local health departments, the Departments of Defense and of Homeland Security,
16
Harvard Public Health Review
the Federal Emergency Management Authority, the Central Intelligence Agency, the Federal Bureau of Investigation, and health ministries of other nations. The mainstay of the program is an on-campus course, during which students learn the principles of “metaleadership.” Marcus and NPLI faculty member Barry Dorn, associate director of HSPH’s Program for Health Care Negotiation and Conflict Resolution, coined the term after analyzing the actions of leaders in unprecedented emergency situations.
Once the concept was captured in a phrase, says Marcus, more questions arose: “How do you describe it? How do you teach it? And how do you ensure that someone can actually do it?” He and Dorn distilled five teachable dimensions of meta-leadership. (See box: The Five Dimensions of Meta-Leadership.) NPLI’s hands-on approach to researching crisis leadership yields valuable insights, which are immediately incorporated into the meta-
Left to right: ©Carlos Barria/Reuters, Jessica Rinaldi/Reuters, © Danny Moloshok/Reuters
NPLI’s instructors teach lessons gleaned from recent national disasters. From left to right: the Deepwater Horizon oil spill, mass vaccination for the H1N1 influenza pandemic, and airport screening to avert terrorism.
leadership training curriculum. For example, “In preparedness, time is your ally. In response, time is your enemy. The longer it takes you to respond and get it right, the more likely you are to fail,” says Marcus. “A quick assessment that is close to the mark and moves the process forward is better than a slow, though more accurate, response that comes too late to make a difference.”
cials had long feared: the first flu pandemic in 40 years—and in this case, the same subtype of the virus behind the devastating 1918 flu. As the epidemic unfolded, Richard Besser, acting director of the CDC, found himself remembering lessons he had learned at NPLI. In fact, recalls Besser—now a visiting fellow at HSPH, as well as chief health and medical editor at ABC News—it was the first time in his career that he felt
Th e Five Dim e n sion s o f M eta-Le ade rship • The Person: Meta-leaders have emotional intelligence: self-awareness, discipline, balance, and insatiable curiosity. • The Situation: With incomplete information, meta-leaders take a large, complex problem, filter it through a wide range of possible solutions, and clearly articulate it. • Leading Down: They inspire subordinates to excellence. •L eading Up: They “lead” their own bosses, through effective, truth-to-power communication. • Leading Across: They connect to other key leaders across different agencies.
Confident, calm, focused
The benefits of NPLI are quickly apparent in a crisis, says Dorn. “These leaders are confident, calm, focused. They are clear about the overall mission. And people working with a meta-leader know what they have to do to help accomplish the mission.” In March 2009, for example, a novel strain of influenza, dubbed H1N1, surfaced in Mexico and spread to the United States. By late April, the outbreak had hopscotched across the globe. It was what public health offi-
he was drawing on all of his strengths in the face of a public health crisis. During the H1N1 response, “I deliberately tried to make sure I was hitting all of the leadership domains within the NPLI meta-leadership approach,” says Besser. “You have to look at leading yourself, leading the event, leading across silos, leading up, and leading down.” The most compelling proof of the program’s success is the fact that many NPLI alumni occupy positions of influence at federal, state, and local health agencies. “When H1N1
hit,” says Marcus, “most of the senior CDC leaders had been through NPLI.” “In choosing students for NPLI, we don’t pick the appointed leaders— the Secretary or Assistant Secretary,” adds Dorn. “We pick the highest government service employee in that organization, because they’re the ones who are going to persist and eventually lead.” Madeline Drexler is editor of the Review.
Fall 2011
17
Today, among the 87 war-torn countries in which data have been gathered, 300,000–500,000 children are involved with fighting forces as child soldiers. Some, as young as seven, commit unspeakable atrocities: killing parents and siblings, assaulting neighbors, torching the villages they once called home. Some are forced to serve as sex slaves. Many are injected with drugs to curb their inhibitions against committing violence. Once the killing ends, peace treaties are signed and emergency humanitarian missions pull out. But these children’s sorrows persist. Theresa Betancourt has made it her mission to understand how to promote their resilience—and ultimately, their healing.
18
Harvard Public Health Review
Helping Former Child Soldiers Become Whole Again
Sven Torfinn/Panos ŠStuart Freedman/PANOS
A 14-year-old former child soldier in Sierra Leone
Fall 2011
19
From child soldier to productive citizen
In Sierra Leone, assistance quickly evaporated after
Betancourt, ScD ’03, directs the Research Program on
the African country’s crisis was no longer in the news.
Children and Global Adversity at the François-Xavier
Today, Sierra Leone ranks 11th from the bottom on the
Bagnoud Center for Health and Human Rights at
UN Human Development Index of 169 nations. Its dis-
Harvard School of Public Health. For nine years, she
trict health officers are justifiably preoccupied with high
has tracked the emotional fate of former child soldiers
rates of maternal and infant mortality. The country has
and explored how—and if—this war-scarred cohort
one psychiatrist—who practices in the capital, Freetown,
can go on to lead meaningful and productive lives.
and is soon to retire.
Using both surveys and one-on-one interviews,
Betancourt’s research seeks to show how former child
Betancourt has painted a psychic portrait of young
soldiers and other war-affected youth may be helped, de-
people—coolly referred to in the academic literature
spite such limited resources, to become contributing mem-
as “children formerly associated with armed forces and
bers of society as adults. She has disseminated her findings
armed groups”—who struggle to find a place in tat-
to hundreds of professionals from local and international
tered postwar societies. She is now adapting and testing
NGOs and UN agencies working with Sierra Leone’s for-
group interventions for troubled youth in Sierra Leone
mer child soldiers.
that have proven successful in other places riven by violence.
She hopes that one day these accomplishments can be bolstered by a broader continuum of care—one that
“ People were pointing fingers at us, saying that this one killed my father, this one killed my mother, that other one burnt down our house.” —male former child soldier Dust cloud—or lasting care
extends from everyday citizens who give troubled kids
“We need to devise lasting systems of care, instead of
encouragement and guidance to frontline community
leaving behind a dust cloud that disappears when the
health workers to psychologists and psychiatrists, who
humanitarian actors leave,” says Betancourt, who is also
can manage cases needing a higher level of services. In an
an assistant professor in the Department of Global Health
ideal world, grassroots mental health services would offer
and Population.
a place for sufferers to tell their stories, talk about their dreams and ambitions, and develop trusting relationships.
HSPH Fellowships En route to earning her doctorate in 2003 at HSPH, Theresa Betancourt received crucial financial aid. In 1998 and 1999, she was awarded a Taplin Fellowship, which paid her expenses. In 1998, she held a Saltonstall Fellowship at the Harvard Center for Population and Development Studies, which helped launch her field research on the Chechnya conflict. In 2008 and 2009, she received the Julie Henry Junior Faculty Development Award, which supported Betancourt’s Family Strengthening Intervention project in Rwanda, a pilot study to bolster resilience and prevent mental health problems among children in postgenocide Rwanda whose families are affected by HIV/AIDS; the research led to a National Institute of Mental Health grant.
20
Harvard Public Health Review
“ We need to devise lasting systems of care, instead of leaving behind a dust cloud that disappears when the humanitarian actors leave.” — Theresa Betancourt, assistant professor of child health and human rights, Department of Global Health and Population
“The postconflict environment is where things break
In Bethel, where the majority of residents were
down, but also where we can help,” she says. “We don’t
Yup’ik, Betancourt acquired both an insider and outsider
have time to waste.”
perspective. “My friends were Yup’ik. I had Yup’ik baby sitters. I spoke Yup’ik. We were outside the dominant
From Alaska to Africa
culture—but we needed to understand that culture in
Betancourt’s path to Sierra Leone began in the Alaskan
order to live well.”
permafrost. She was born in a Native hospital in Bethel,
Her father’s passion for Ethiopia never waned. When
a town near the state’s west coast that then numbered
friends came over for dinner, he would haul out his slide
about 3,000. Her parents, both Caucasian, imbued the
projector and display pictures from his Peace Corps days.
family with a passion for other cultures. Her father was
“We were in small-town Alaska permafrost,” Betancourt
a math and science teacher who had joined the Peace
says, “but we always knew what Africa looked like.”
Corps in the early 1960s, stationed in Ethiopia. Her
Initially trained as a counselor using expressive
mother worked in remote villages for the federal infant
arts in therapy with children, Betancourt started focus-
learning program.
ing in 1995 on children affected by war. First with the
Kent Dayton/HSPH
continued
Studying is a source of encouragement. I know that if I am educated, I will be successful and people will appreciate me.” —female former child soldier
Fall 2011
21
Tragedy Told by the Numbers Child recruits in the Sierra Leone civil war interviewed by Theresa Betancourt’s research team had been severely traumatized by their experiences:
70% had witnessed beatings or torture.
63% had witnessed violent death.
UN Office of the High Commissioner for Human Rights, then with the International Rescue Committee (IRC), a New York-based humanitarian organization, she worked with young refugees in Albania, Chechnya, and the Eritrea-Ethiopia border, organizing emergency education programs and eventually research initiatives. In 2002, at the end of a bloody 11-year civil war, Betancourt made her initial trip to Sierra Leone to work with the boys and girls there. “The first time I met with former child soldiers, what struck me was that they looked really little, really young. They told me they were 13 and 14, but they looked eight. They were malnourished and wearing tattered clothes. I couldn’t fathom what they had seen.” Betancourt has now been tracking more than 500 former child soldiers, many of whom are growing into adulthood and starting their own families. Her main questions: What helps young people endure this experience and still thrive? What qualities of the individual, the family, and the
77%
environment shape resilience? How can effective interventions, resonant
saw stabbings, chopping, and shooting close-up.
with the local culture, be delivered by community members who receive
62%
“ The first time I met with former child soldiers, what
had been beaten by armed forces.
struck me was that they looked really little, really
52%
special training and routine supervision?
young. They told me they were 13 and 14, but they looked eight...I couldn’t fathom what they had seen.”
witnessed large-scale massacres.
—Theresa Betancourt
39% had been regularly forced to take drugs such as marijuana and cocaine.
45% of girls and 5 percent of boys had been raped by their captors.
had killed or injured others during the war. A child soldier in the Democratic Republic of Congo
22
Harvard Public Health Review
©Sven Torfinn/Panos
27%
Drawings by a former child soldier in northern Uganda describe his experience as an abductee.
Groundbreaking research tells the story
and recurring violent images. Not surprisingly, those who
Betancourt believes both numbers and words are needed
committed extreme acts of violence, or were its victims,
to take the measure of a child soldier’s trauma. As a
tend to suffer the most persistent mental health problems
result, she relies on both quantitative and qualitative
and need the most intensive care.
methods in her research efforts. In her longitudinal
Frequently, these children have difficulty with com-
study, she uses a detailed questionnaire to elicit the boys’
munity relationships after their release. They struggle with
and girls’ war and postconflict experiences. Her local
guilt and shame. They are labeled as different or untrust-
staff conduct in-depth qualitative interviews of the chil-
worthy, which, in a vicious circle, deepens their sense of
dren and their caregivers, along with focus groups in the
isolation. In their home communities, they are blamed for
community.
having destroyed lives, homes, property, and society itself.
Much of the existing scholarship on intergenerational relationships in war-exposed populations is based on the experiences of Holocaust survivors. Betancourt’s
Those who are socially isolated are especially vulnerable to addictions and abusive relationships. Girls face a compound burden. They are more likely
work is, therefore, groundbreaking. Her nine-year proj-
to suffer depression, anxiety, and post-traumatic stress
ect following male and female child soldiers in Sierra
disorder, compared with boys. Some have returned to
Leone is Africa’s first such prospective study.
their communities having had unwanted pregnancies dur-
And a 2007 study that Betancourt co-authored was
ing their times with rebel groups. At home, they face the
one of the first randomized controlled trials of mental
double stigma of having participated in violence and being
health interventions among African adolescents affected by
seen as “impure,” regardless of their war experiences.
war—and one of only a handful of trials of psychological treatments for depression conducted in a developing coun-
Hundreds taught to work with former child soldiers
try. Among other things, she has shown that effective treat-
To grapple with these problems, Betancourt and her
ments—and clinical trials of these treatments—are feasible
colleagues have looked to existing evidence-based mental
in poor, rural, illiterate, war-torn communities.
health interventions that help violence-affected youth manage their emotions and build interpersonal skills. The
A vicious circle
goal is to forge connections to families and communi-
In Sierra Leone and elsewhere, former child soldiers
ties, and give children the wherewithal to negotiate the continued
suffer nightmares, intense sadness, intrusive thoughts,
Fall 2011
23
A Recipe for Resilience Former child soldiers are not a monolithic population of the emotionally wrecked. “When people think of child soldiers, they think of people who are terribly damaged in some way,” Theresa Betancourt says. “But I’ve seen very much the opposite: tremendous stories of resilience, of acceptance, of love in families.” In her view, resilience springs from a complex ecology of individual traits and social forces. “In one sense, any child who made it through the war alive likely developed survival strategies to navigate a harsh and dangerous environment. Some of these young people, especially those who survived abuse, possess a sense of resourcefulness, which shows up in confidence and a sense that they can control their fate.” Another potent factor in resilience is family connectedness. When parents openly embrace their sons and daughters and bring them back into the fold, it not only sustains the child but also sends a signal to the larger community that the boy or girl is worthy of acceptance and care. Going to school, doing homework, and graduating likewise foster a sense of normalcy and regaining lost time. How the wider culture draws meaning from the war and its aftermath also influences the fate of former child soldiers. During the postwar, government-led process, which has included sanctioned forgiveness and community sensitization campaigns, many young people received the explicit message that their involvement in the country’s atrocities was not their fault.
adversities they often encounter. Ideally, such approaches
Married to a physician specializing in health inequities,
are linked to educational and job programs that restore
and the mother of two young children, she has a notice-
civilian roles—since returning to school or securing a live-
able lightness of spirit.
lihood are prime sources of confidence and motivation in the children. Betancourt emphasizes that direct, sustained treat-
distress has a local meaning
Betancourt is planning pilot studies that use compo-
ment of war-affected children is the task of local part-
nents of cognitive behavioral therapy and an approach
ners. “I like to stay put in a place, develop relationships,
known as group interpersonal psychotherapy that has
and keep working at things over time,” she says. Despite
proved successful in relieving depression among chil-
the oppressive content of her work, she is neither dour
dren—some former soldiers, some not—crowded in
nor drawn to philosophical discussions about the nature
refugee camps in embattled northern Uganda. Group
of good and evil. As she puts it, “I’m very pragmatic.”
interpersonal therapy is based on the idea that the roots of depression, and the mechanisms for healing it, lie in
“ I think about what I have been through and this gives me more determination to do well in life.”
— male former child soldier, recently promoted to his final year of secondary school
people’s relationships with others. Young people who have all experienced the same ordeal can share support, wisdom, and understanding. In Betancourt’s intervention, war-affected young people learn that they are not alone in their experiences and emotions. “The key is being able to put a word to their feelings: sadness, worthlessness, hopelessness, loss of en-
24
Harvard Public Health Review
ergy, the sense that life is not worth living,” she says.
dangers of excluding any stigmatized group. Traditional
“We spend a lot of time trying to learn local terms for
healing ceremonies—such as ritual washings and col-
emotional suffering. Once intervention and problem
lective feasts—can also mark new beginnings for for-
solving begins, these young people no longer feel alone.
mer child soldiers.
Their symptoms start to lift.” Betancourt and her team call their pilot model the
Such evidence-based interventions are far more effective than the once-popular technique in humani-
Youth Readiness Intervention, because it builds readi-
tarian assistance known as “psychological debriefing,”
ness to succeed in critical aspects of life such as personal
in which Western practitioners briefly visit war zones,
relationships, taking care of one’s self, planning for the
conduct therapies in which victims talk about their
future, and achieving economic self-sufficiency. Meeting
traumatic experiences, then leave.
weekly for two months, the participants focus on the
According to Betancourt, “Flying in and asking
present: setting goals, curbing high-risk behaviors and
someone to share their trauma in one or two sessions,
substance use, reducing trauma-related distress, and
without an ongoing, safe therapeutic relationship, can
boosting community involvement.
actually do more harm than good.”
Complementing African programs and traditions
Not a “lost generation”
“The groups fit well in collectivist cultures such as in
In the aftermath of chaotic civil wars, investments in
Uganda or Sierra Leone,” says Betancourt. “In northern
psychosocial and mental health problems are typically
Uganda, we saw very strong effects in girls, more so
phased out as the problem shifts to a postconflict and
than in boys. That may be because in these crowded
then a reconstruction phase. “Unfortunately, these chil-
camps—where girls had a lot of responsibilities caring
dren’s needs do not follow a similar phasing-out process,
for people, cooking, gathering firewood, fetching
particularly when they have been ill-addressed at the
water—they didn’t have much in the way of supportive
outset,” says Betancourt. “There is real difficulty in
social contacts before meeting other girls in the same
getting funding for this work. Sierra Leone, in partic-
situation.”
ular, is seen as a ‘has been’ conflict: no longer sexy.”
Betancourt’s locally adapted models also comple-
What most worries her is that societies will write
ment what has been initiated in Sierra Leone and other
off former child soldiers as a “lost generation.” The op-
nations, including “sensitization” campaigns that en-
posite could be true, she contends: The very qualities
courage communities to discuss the conflict and the
that helped these children survive a harrowing experience may also enable them to catalyze change in their shattered homelands. And while Betancourt’s research may seem specialized, many of her findings transcend culture. “When someone’s a survivor, it means they are still here today, despite what they went through,” she says. “It would be
©Giacomo Pirozzi/PANOS
terrible if people who had been through events like this saw themselves as hopeless or as victims. A survivor orientation means being able to feel the strength of what it takes to make it through such horrendous experiences and still move forward in life.” Former child soldiers in the Democratic Republic of Congo have received skills training as part of their reintegration into society.
Madeline Drexler is editor of the Review.
Fall 2011
25
Infectious Diseases
Unlocking the Secrets of Drug Resistance in Malaria Parasites New gene search tool opens “endless possibilities”
D
uring a half-century of global efforts to conquer malaria, scientists have developed a series of anti-
“If resistance to artemisinins develops and spreads to other large geographical areas, as has happened before with
malarial drugs, only to see them defanged, one by one, by
chloroquine and sulfacoxine-pyrimethamine (SP),” the
the shape-shifting parasite’s ability to rapidly evolve drug-
World Health Organization warned in 2009, “the public
resistant variants.
health consequences could be dire, as no alternative antima-
Today, with massive new malaria eradication cam-
larial medicines will be available in the near future.”
paigns launched against the disease that kills nearly a million people every year in Africa, drug resistance remains
Early warnings KEY
a critical problem—and one whose molecular underpin-
Today, these rogue strains are usually recognized only
nings are poorly understood.
when patients stop responding to a drug, says Dyann
The antimalarial medicine chest has dwindled to a
Wirth, chair of the Department of Immunology and Infectious Diseases at Harvard School of Public Health
became available in 2005. And now doctors in Southeast
and a co-director of the Infectious Disease Initiative, a
Asia are seeing signs that artemisinin may be next on the
collaboration that involves Harvard University and the
parasite’s hit list.
Broad Institute of MIT and Harvard. “By the time you find a very resistant parasite,” she says, “you’ve already lost the battle.”
26
Harvard Public Health Review
Comstock/Getty Images
single reliably effective compound, artemisinin, which
With this threat always at hand, new research at HSPH is addressing an urgent need: early warning methods to detect the first signs of drug-resistant malaria strains, so that a swift response might keep them from gaining a foothold. Watching resistance unfold
In April, Wirth and other leaders of the Initiative reported on a powerful combination of genome search methods that enabled them to discover new resistance genes in Plasmodium falciparum, the malaria parasite. They even used one of these genes to convert a docile, easily killed parasite into a resistant one. “We really didn’t know what to expect,” says Daria Van Tyne, a graduate student in Wirth’s lab and co-first author of the study, which appeared in PLoS Genetics. “This is the first time anyone has observed resistance as it’s happening.” At the molecular level, little is known about the pathways leading to resistant phenotypes. At HSPH, Wirth and her colleagues are looking for clues by comparing the genomes of resistant parasites with “sensitive” or nonresistant organisms. “Our approach is to develop a tool that will enable us to observe a tendency toward loss of drug sensitivity in a population before the problem is well established,” explains Wirth. “The goal is to make the discovery early so you can use that knowledge to focus efforts,” such as enforcing appropriate drug-use guidelines. Five first authors
The PLoS Genetics paper is unusual in having five co-first authors (including Van Tyne) and three senior authors: Wirth, HSPH research scientist Sarah Volkman, and Pardis Sabeti of the Broad Institute and Harvard. “This is a very strong collaboration,” Wirth notes. The research drew on HSPH expertise in parasite biology and drug resistance mechanisms, the Broad Institute’s resources in sequencing, genotyping, and computational methods, and field researchers in Senegal who track the spread of resistance. Contributions also came from investigators at other U.S. universities and at universities in Senegal and Nigeria.
Searching for resistance genes
The National Institutes of Health maintains a depository of malaria parasites from around the world collected over decades. Tapping this resource and the labs of HSPH partners in Africa, the researchers collected 57 parasites from three continents—some of them sensitive to antimalarial drugs, and others resistant to one or more. Though the first P. falciparum genome was sequenced in 2002, only recently have malaria scientists begun genomic searches for resistance genes.
Dyann Wirth, chair of the Department of Immunology and Infectious Diseases (left) and Pardis Sabeti, assistant professor in the Department of Immunology and Infectious Diseases
For their study, the HSPH and Broad investigators began by scanning the parasites’ DNA for regions that had undergone recent evolutionary changes, some of which might reflect adaptation under selective pressure from malaria drugs. With this method, the scientists identified 15 genes showing signs of recent selection. Determining which of these genes were implicated in resistance required a second step—a genome-wide association study, or GWAS. The GWAS search drew on HSPH researchers’ expertise in molecular biology and drug resistance, combined with the Broad’s prowess in gene sequencing and computational biology. continued
Fall 2011
27
The GWAS was designed to home in on genetic variants present in parasites resistant to 13 antimalarial drugs, but not present in drug-sensitive ones. The scientists constructed a fine-resolution map of more than 17,000 points of reference, called SNPs, spaced regularly throughout the genomes; it was the densest SNP array yet applied to the malaria parasite.
The GWAS netted several new resistance-associated genes, including one, dubbed PF10-355, that looked like a particularly strong candidate. To test this further, Van Tyne transferred PF10-355 into a drug-sensitive parasite. Sure enough, the addition of the gene increased the parasite’s resistance to three related antimalarial drugs. Daria Van Tyne, HSPH graduate student
“ By the time you find a very resistant parasite, you’ve already lost the battle.”
28
Harvard Public Health Review
Kent Dayton/HSPH
artemisinin is losing its effectiveness in a certain population or geographic area. According to Wirth, “That — D yann Wirth, chair, HSPH Department of would tell us that we need to use Immunology and Infectious Diseases other drug combinations and implement focused intervention strategies “We had no idea if it was going to prevent the spread of resistant Genes to the globe Wirth and others involved in the to work or not,” Van Tyne said of parasites.” project say the new genomic search the two-pronged method. Much to And, Van Tyne says, “this the scientists’ relief, the searches im- tool opens up “endless possibilities” would all feed into research that that could lead to improvements in mediately detected a gene for chlocould yield better antimalarial detecting and combating antimaroquine resistance that had been drugs.” larial resistance. discovered previously with older It would be hard to find a better “The paper we published is techniques. This validation that story illustrating Dean Julio Frenk’s just the tip of the iceberg,” explains they were on the right track “made “genes to the globe” concept, adds Van Tyne. With these new genomic us very happy when we saw it,” reWirth. “Harvard has the ability to tools, researchers can search not calls Van Tyne. “It gave us a green approach a problem like malaria only for resistance genes, but also light for the rest of the study.” from a fundamental understanding other mutated or variable genes that of the biology all the way to global govern parasitic traits and the difissues like policy, finance, and all ferent outcomes that infected people the pieces needed to address public experience. health problems.” Their greatest hope is that disRichard Saltus is a Boston-based tinctive resistance-related mutations freelance science journalist. could become the basis of simple blood tests, able to be performed in Sarah Volkman, HSPH community clinics in Africa, that research scientist could determine when a drug like
Fellowships
W
hen Roy Wade was a medical resident at the University of Virginia, Charlottesville, one patient in the pediatric clinic he was working in really stuck with him: a 16-year-old girl with a deeply troubled history of depression and risky behavior. “I couldn’t help, and her life spilled out of control after my visit with her,” he recalls.
Dora Hughes, MPH ’00, counselor to U.S. Health and Human Services Secretary Kathleen Sebelius
The case highlighted for Wade the difficulty of helping patients with problems that are not just medical, but tied into the fabric of lives marred by poverty, racism, a family history of illegal drug use, chronic disease, or physical and emotional abuse. When Wade heard about the Commonwealth Fund/Harvard
Yvette Roubideaux, MPH ’97, director of the Indian Health Service
University Fellowship in Minority Health Policy, “It just clicked for me,” he says. Looking to boost his skills as a leader within the health care system, he applied for and received a Commonwealth Fellowship to study at Harvard School of Public Health, completing the program to receive a master’s in continued public health in May.
Kima Taylor, MPH ’02, director of the Open Society Foundation’s National Drug Addiction Treatment Program
Roy Wade, MPH ‘11, Robert Wood Johnson Clinical Scholar, University of Pennsylvania School of Medicine
A Launchpad for Leaders Fellowship program nurtures physicians’ “inner advocate,” propelling them into roles helping national and global stage Fall 2011
29
Kent Dayton/HSPH
the disadvantaged on a
Illustrious alumni
covers not just policy and leader-
ment. Wade identified a need for
In doing so, Wade, MPH ’11, joined
ship issues, but nitty-gritty subjects
improved communications between
an illustrious group of alumni that
such as accounting, epidemiology,
health centers, the states, and private
includes the current head of the U.S.
communications, and economics—
payers as key avenues for improving
Indian Health Service, a key health
all of which may be quite new to
the finances of school-based health
policy adviser to President Barack
young physicians.
centers in the future.
Services (HHS) Secretary Kathleen
Focusing young leaders
Prophetic connections
Sebelius, and at least one MacArthur
Critically, the program helps each
Yvette Roubideaux, MD, MPH ’97,
Foundation “genius grant” recipient.
fellow identify the issues that engage
who now heads the U.S. Indian
him or her most. “We all want to
Health Service (IHS), participated in
celebrated its 15th anniversary
address social inequities, social injus-
the program in its earliest years.
earlier this year, provides potential
tice, poverty, and racism—issues that
physician-leaders with the skills they
affect public health,” Wade points
Rosebud Sioux nation, attended
need to help people who come from
outs. “We come to the program with
a talk during her fellowship that
Obama and U.S. Health and Human
The prestigious program, which
Roubideaux, a member of the
“ Without this fellowship, I doubt that I would have been able to make the same kind of impact on African women’s health and female genital cutting.” —Nawal Nour, MPH ‘99 minority, disadvantaged, or otherwise
ideas about what we want to work
was given by the IHS’s then-
vulnerable groups get better access to
on, and the program is very good
director. HMS Dean for Diversity
high-quality health care.
at helping us refine those ideas into
and Community Partnerships
our respective research and policy
Joan Reede (who heads the
School (HMS) in 1996, the program
areas, and at providing avenues for
Commonwealth Fellowship
offers recipients funding to pursue a
us to continue to work in these areas.
program) told Roubideaux that she
master’s of public health from HSPH
Doing projects on the child welfare
should pay strict attention, making
or a master’s in public administration
system, I realized that’s where I want
the prophetic suggestion that
from the Harvard Kennedy School of
to work.”
Roubideaux herself might eventually
Launched by Harvard Medical
Government. Since its establishment, the
Each fellow carries out a practicum analyzing a highly specific issue
get the speaker’s job. “The fellowship broadened my
Commonwealth Fellowship,
in health policy. For Wade, that was
perspective and gave me new tools to
combined with funding from the
an analysis of school-based health
keep focused on my original goals,”
California Endowment Scholars in
care centers, which provide a major
says Roubideaux, who later switched
Healthy Policy and the Joseph Henry
safety net for 2 million patients but
career plans toward teaching,
Oral Health Fellowship in Minority
often face severe funding handicaps.
research, and service. (To learn more
Health Policy, has supported 99
While most of these centers bill their
about Roubideaux’s career, read the
fellows in minority health policy,
states for Medicaid reimbursement,
profile that appeared in the Spring/
95 of them at HSPH. The training
managed care organizations often
Summer 2010 Review at http://www.
raise barriers for this reimburse30
Harvard Public Health Review
“ It’s nice to know you have a support system, but we all know that it comes with an expectation—that we will be part of an extended group that helps to nurture the fellows who follow,“ —Kimberly Cauley Narain, MPH ‘11 hsph.harvard.edu/news/hphr/spring-
that seeks to boost access to treatment
2010/spr10roubideaux.html.)
for addicts by rethinking advocacy,
Fellowship was a career-altering
communications, and operational
experience,” says Nour, who is asso-
Tackling drug addiction
strategies. While results vary by state,
ciate professor in obstetrics, gyne-
treatment
so far the program has opened up
cology, and reproductive medicine
Kima Taylor, MPH ’02, now directs
access to treatment for 300,000 more
at HMS and director of the obstetric
the Open Society Foundation’s
people, she says.
ambulatory practice at Brigham and
National Drug Addiction Treatment
“The Commonwealth
Women’s Hospital.
Program, which directly tackles the
Advising Obama
challenges posed by lack of access
For Dora Hughes, who received
after the fellowship as a public
to treatment for the more than 23
her MPH from HSPH through the
health practitioner with the goals
million people addicted to drugs
program in 2000, the fellowship “let
of bringing about social change to
and alcohol in the U.S.
me be effective on a much broader
improve women’s health,” says Nour.
“Only 10 percent are being
field.” After working as an aide to
“Without this fellowship, I doubt
treated,” says Taylor. “It’s a chronic
Senator Ted Kennedy and to then-
that I would have been able to make
disease and it needs to be treated
Senator Barack Obama, she became
the same kind of impact on African
that way—handled in the health
a health care adviser during Obama’s
women’s health and female genital
care system and not the criminal
presidential run and now plays a
cutting.”
justice system. It’s also still publicly
major role in health care initiatives as
stigmatized and seen as a moral
counselor to HHS Secretary Sebelius
Paying it forward
failing, even by many MDs and
in the Obama administration.
“One of the most powerful aspects of
“I returned to clinical work
the fellowship is the camaraderie and
others in health care.” Eradicating genital cutting
the family atmosphere,” Roy Wade
opened my eyes to professional
Other fellows who attended HSPH
points out. “You feel absolutely
possibilities that I would not have
through the program include Nawal
supported. You are able to express
known even existed. It exposed me
Nour, MPH ’99, who later received
your strengths and weaknesses, and
to subjects—economics, leadership,
a MacArthur Foundation “genius
you are comfortable evaluating your-
and statistics—that people rarely feel
grant” for her work as a global leader
self and your colleagues.”
doctors need or will use. The fellow-
in the effort to eradicate female
ship also helped me nurture my inner
genital cutting in Africa.
Taylor adds, “The fellowship
advocate. I was able to learn to advo-
Nour also works with African
“It’s nice to know you have a support system,” agrees Kimberly Cauley Narain, another fellow who
cate more effectively for myself and
women now living in the U.S., who
graduated in May. “But we all know
my sanity, as well as for others.”
face a host of issues because they
that it comes with an expectation—
Taylor currently manages a
have either submitted to genital
that we will be part of an extended
$10 million nine-state pilot program
cutting or face pressure to do so.
group that helps to nurture the fellows who follow.” Fall 2011
31
Postdoctoral Research
I
n Kenya’s arid Wajir district, across the border from Somalia, attending school is not a given. Though some children learn to read while sitting on the floor in crowded classrooms or gathered on the dusty red ground under
a tree, others must stay home to help tend the livestock so vital to the nomadic community’s precarious existence. Osman Abdullahi was one of the lucky ones, and he hopes to someday return his community’s investment by taking on one of the district’s worst scourges: tuberculosis. For Abdullahi, now a molecular epidemiologist and a postdoctoral research fellow at Harvard School of Public Health, the past year at HSPH has been a key stop on a very personal quest. He has delved into what makes the TB bacterium tick—particularly how its strains vary in their transmission, ability to cause disease, and susceptibility to antibiotics, as well as what happens in the body of a person infected with more than one strain. After completing his fellowship at an HSPH-affiliated research facility in South Africa, Abdullahi plans to return to Kenya next year to open his own tuberculosis lab.
Returning Home, with a Plan to Thwart Killer TB “One day, she was gone.”
Kenya has the 13th-highest tuberculosis burden in the world and the fifth highest in Africa, according to the World Health Organization. TB rates are especially high in Wajir and other pastoralist districts in the country’s North Eastern Province. Worldwide, TB kills more adults than any other infection, claiming about 2 million lives annually, a figure that includes more than 450,000 people also infected with HIV. Each year also sees 10 million new cases of the infection. Growing up, Abdullahi, now 33, recalls that TB was part of the fabric of daily life. “My neighbor was very thin and coughing all the time. One day, she was gone. My parents told me she had been quarantined.” After spending six months receiving treatment in an isolated hut outside town, the neighbor returned fat and healthy, Abdullahi says. But a case continued
32
Harvard Public Health Review
Kent Dayton/HSPH
left untreated could quickly lead to disaster in this communal society.
Osman Abdullahi, a molecular epidemiologist and postdoctoral research fellow at HSPH, plans to open a tuberculosis laboratory in his homeland of Kenya.
Fall 2011
33
Today, tuberculosis research remains rare in Kenya.
A quest to Learn
Infrastructure constraints, misinformation, and a potent
After getting his first taste of epidemiology as an undergradu-
stigma surround the disease. Two years ago, Abdullahi
ate, Abdullahi longed to understand why the infection was
was shocked by the response to a patient who was ad-
so prevalent in his largely nomadic community—and to do
mitted to the Moi Teaching and Referral Hospital in
something about it. “I was desperate for training,” he says.
Eldoret, Kenya, for extensively drug-resistant tubercu-
With no formal programs in epidemiology offered in Kenya,
losis (XDR-TB). (Learn more about how drug-resistant
he seized opportunities where he could—a research assis-
TB strains emerged at http://www.hsph.harvard.edu/
tant position with the KEMRI-Wellcome Trust Research
news/hphr/infectious-diseases/when-infection-wont-
Programme in Kenya and later a PhD scholarship to The
quit/index.html.)
Open University in London—even though they required a
“Everyone was scared—the hospital, the media,
focus on pneumococcus, a common bacterial cause of pneu-
and even the poor man’s relatives. No one knew how to
monia, ear and sinus infections, sepsis, and meningitis.
handle this patient,” Abdullahi says. “He was isolated in
While collaborating with HSPH Professor of
a building and people suggested that we burn it down
Epidemiology Marc Lipsitch during his PhD program,
to rid ourselves of XDR-TB. But as an epidemiologist, I
Abdullahi was encouraged to come to the School to
knew that this case was only the tip of the iceberg.”
finally study TB. He received financial support from the Christopher W. Walker, Esq. Fund for Tuberculosis Research and Information Sharing at Harvard School of
Ho New/RUETERS
“ People are skeptical of ideas from foreigners,” says Osman Abdullahi. “But if they see you as local, they say, ‘You are talking a language we understand.’”
34
Harvard Public Health Review
Public Health. He quickly impressed his adviser, Sarah
Armed with this new scientific knowledge, Abdullahi
Fortune, assistant professor of immunology and infectious
hopes to create interventions based on the unique needs of
diseases, with his vision and his drive to learn a complicated
Kenyan pastoralist communities like Wajir, where families
new set of skills.
are large, communal gatherings are frequent, and ventila-
Working at The KwaZulu-Natal Research Institute for Tuberculosis and HIV in South Africa this year, Abdullahi will dig deeper into the molecular biology of
tion is poor—ideal conditions to spread TB. His own deep roots in the area may be key to making a difference, he says. “People are skeptical of ideas from foreigners. But
drug-resistant TB. And he’ll help forge connections be-
if they see you as local, they say, ‘You are talking a lan-
tween HSPH researchers, including Fortune, and African
guage we understand’ and take you seriously. I will be
researchers that he hopes to tap into when he returns to
able to have an influence because I understand the dy-
Kenya to open his own lab.
namics.” And with small victories at the local level, the
Abdullahi aims to leverage Kenya’s widespread use of
spreading tide of the disease may begin to turn. “I don’t
mobile phones and online social networks to calculate a
think TB will be eliminated for a long time, because we
more reliable estimate of the country’s TB burden. He also
are dealing with a disease that dwells in the way people
intends to establish collaborations with international col-
live,” Abdullahi says. “But I believe that with research
leagues in labs that are equipped to conduct whole-genome
and education, we will be able to reduce it.”
sequencing and other sophisticated studies.
Amy Roeder is assistant editor of the Review.
Photos courtesy of Osman Abdullahi
Abdullahi hopes to create interventions based on the unique needs of Kenyan communities like Wajir, where families are large, communal gatherings are frequent, and ventilation is poor—ideal conditions to spread TB. Above right: TB isolation huts. Fall 2011
35
Alumni
Saving Lives in The Heat of Battle Christian Benjamin, MD, MPH ’96 and Michael McCar ten, DO, MPH ’99 are delivering evidence -based militar y medicine in Afghanistan.
M
edics roll a badly wounded U.S. soldier into the military hospital in Kandahar, Afghanistan. He has lost both legs to a roadside bomb, and his abdomen, head, and neck are torn up. The international surgical team snaps into action to clean his exposed flesh; specialists check for head trauma. A few days later, the bandaged young soldier is flown to another military hospital for more surgery, then begins his journey home to recover. Heart-wrenching scenes like this unfold regularly at the NATO Role III Multinational Medical Unit in Kandahar. “The trauma we see here is devastating,” says U.S. Navy Capt. Michael McCarten, DO, MPH ’99, who spent a year commanding the hospital in 2010–11. “Sometimes the anatomy is unrecognizable.” About 300 miles away, U.S. Air Force Col. Christian (“Chris”) Benjamin, MD, MPH ’96, witnessed similarly grave injuries during his year leading the Craig Joint Theater Hospital at Bagram Air Field. Equipped with operating rooms, ICU beds, laboratories, and other state-of-the-art services, these trauma centers treat both coalition forces and Afghan soldiers and civilians, including children maimed by explosives. The hospitals boast 98 percent survival rates, and McCarten and Benjamin credit their resourceful teams and several public health strategies—such as reducing the lag time between injury and surgery—with helping save lives in the decade-long war in Afghanistan.
tary medicine training, most of them in its one-year MPH program. Their crew cuts may have stood out on the liberalleaning campus, but the pair say their Harvard education has helped guide their leadership roles in combat hospitals, on military bases, and aboard aircraft carriers. Military medicine, they explain, typically involves caring for healthy young people serving in hazardous environments, such as noisy flight decks or hot engine rooms; it also involves tending to families, retirees, and veterans.
36
Harvard Public Health Review
U.S. Air Force photo by/ Master Sgt. Jeromy K. Cross
Lasting lessons Benjamin and McCarten belong to a cadre of alumni who attended Harvard School of Public Health as part of their mili-
END Captions ideas Benjamin: “I couldn’t prevent people from being injured,” says Col. Chris Benjamin. “But it was gratifying to know we gave each [patient] the best chance for survival anywhere on this planet today.”
4
Chris Benjamin, MPH ’96, leads trauma centers in Afghanistan that treat both coalition forces and Afghan soldiers and civilians.
continued Fall 2011
37
Their crew cuts may have stood out on the liberal-leaning campus, but Benjamin and McCarten say their Harvard education has helped guide their leadership roles in combat hospitals, on military bases, and aboard aircraft carriers.
Public health strategies such as reducing lag time between injury and surgery have saved lives in the Afghanistan war. Michael McCarten, MPH ’99 (left) watches as a medical team resuscitates an Afghan child in an emergency room at the Role III trauma center in Kandahar. Data from the front lines The value of research was one of the biggest takeaways from HSPH. “They teach you how to ask questions, analyze the data, and come up with answers that fit the situation you’re in,” recalls Benjamin, who now commands the U.S. Air Force School of Aerospace Medicine. This attitude meshes with the self-analytical approach of the U.S. military medical system. “We are our own worst critics,” says McCarten, who was interviewed via Skype. “We understand the sacrifices these men and women have made.” In Afghanistan, he and Benjamin drew from statistics the Pentagon has collected from recent conflicts to identify best practices and improve outcomes. Take tourniquets, for example. Used for centuries to stop bleeding on the battlefield, these simple devices became controversial because they can aggravate the injury if applied incorrectly. But the timely use of tourniquets has proved essential during the wars in Iraq and Afghanistan, where homemade bombs or “improvised explosive devices” (IEDs) have led to a These and other evidence-based strategies from the front lines, including cranking up the ER temperature to prevent hypothermia, have caught the attention of civilian counterparts. Indeed, Benjamin hosted visits from four renowned civilian trauma surgeons during his year in Bagram. 38
Harvard Public Health Review
Kent Dayton/HSPH
horrifying number of amputations.
Infection control is a crucial public health weapon in military medicine, and hand hygiene is paramount on the Bagram and Kandahar bases. In hospitals, the routine use of antibiotics can quickly foster drugresistant bacterial infections, a problem exacerbated in Afghanistan because many local patients are malnourished and show up with dirty, festering wounds—all factors that hinder healing and lead to longer hospital stays. Bugs such as Pseudomonas and Klebsiella are among the most stubborn and virulent antibiotic-resistant pathogens in these military hospitals—just as they are in the U.S. Life Expectancy: 45 Years Amid rampant poverty, unsafe drinking water, limited access to care, and other challenges, Afghanistan has a dire health profile. The nation’s average life expectancy is 45 years and the maternal mortality rate is one of the highest in the world.
Chris Benjamin walks with Afghan President Hamid Karzai during a visit to Bagram Airfield in 2010.
Serving in Afghanistan reminded McCarten of courses given by Michael Reich, Taro Takemi Professor of International Health Policy, and Ichiro Kawachi, chair of the Department of Society, Human Development, and Health. These courses underscored the message that socioeconomic conditions shape health outcomes. “Looking at health systems around the world that I’ve observed in my Navy career, it’s clear that the rich get richer and the poor get poorer,” McCarten says. “My time Opposite and lower right, courtesy of U.S. Navy Capt. Michael McCarten, DO, MPH ’99; top right, REUTERS
at Harvard, and those two courses in particular, changed my politics. They were absolutely life-changing for me.” Supporting the Wounded As they evacuated patched-up soldiers to bigger facilities in Germany and the United States, McCarten and Benjamin knew that recovery would test their patients’ fortitude. But they say military and veterans’ hospitals have made impressive gains in providing for wounded warriors, especially those with the signature injuries from Afghanistan and Iraq: amputations, traumatic brain injury, and psychological scars. The two doctors envision a health care system that addresses the service members’ Michael McCarten with an Afghan girl and her father. The girl lost her lower left arm in a bus accident and suffered other serious injuries. McCarten’s team performed several surgeries to ensure her survival.
physical, emotional, and spiritual needs and a society that supports them as they strive to rebuild their lives. As McCarten puts it, “They deserve nothing less.”
Note: At press time, Capt. Michael McCarten was scheduled to return to the Navy’s Bureau of Medicine and Surgery in Washington, DC, to oversee Naval medical operations.
ebra Bradley Ruder is a Boston-based D freelance writer specializing in health care, education, and end-of-life issues. Fall 2011
39
Commencement
Looking Back, Looking Ahead Gro Brundtland offers perspectives to 2011 graduates Six out of every ten members of the Class of 2011 were women—a far cry from 1965, when Commencement speaker Gro Brundtland received her diploma. That spring, only 18 percent of the class’s 72 graduates were women. Much has changed at Harvard School of Public Health over the past 46 years, a period of time during which Brundtland served as the first woman and youngest prime minister of Norway and as director-general of the World Health Organization. Below is some of the wisdom Brundtland offered this year’s class of 478 students at Commencement on May 26. A full transcript of her remarks, as well as those given by student speaker Lakshmi Nayana Vootakuru, alumni speaker Commencement speaker Gro Brundtland, former director-general of the World Health Organization
Elsbeth Kalenderian, and HSPH Dean Julio Frenk, can be found at http://www. hsph.harvard.edu/news/features/features/hsph-commencement-2011.html.
I believe our
The Holistic Approach to Public Health I learned so much more about the links between humans
analysis, by the unprec-
and nature, our societies, cultures, and our environment. This
edented commission I
holistic approach is public health at its best. It is preventive
put together (and which
medicine at its core.
I insisted include a majority of members from the
The key issues of development—economy and finance, environment, health and education—can all only be dealt
developing world), has
with on the basis of shared values and concerns, on human
stood the test of time.
rights for both women and men, and on dignity for all.
Know Before You
This holistic way of thinking is also the only real basis for
Conclude
peace and security. Health itself tells perhaps the strongest
From my parents—not
story of globalization and the need for shared values and ac-
least from my father,
tion to promote safety across the world.
Dean Julio Frenk
“Can I Do It?”
bilitation expert, and politician who served both as Minister
As I was asked to enter the government [in 1974, as Norwegian
of Health and Social Affairs and Minister of Defense—I had
Minister for Environmental Affairs], at the age of 35, it came as
instilled in me the conviction and discipline that you need to
a complete surprise. I had no such plans or ambitions.
know before you conclude. You need to seek knowledge and
and principles already gained from my studies and working life were indeed perfectly relevant. Again in 1983 came the call from the United Nations to
evidence to secure the necessary basis for pointing in a specific direction and making decisions. This attitude was reinforced here at Harvard School of Public Health. I brought with me the conviction to always put great emphasis on science and evidence in pursuit of the
lead an important international commission to address the
best policies and actions to take. My credo is this: Build on
major global challenges we then were facing and regretfully
and strengthen the evidence, share the evidence, and act
still are: environmental and developmental patterns that rapid-
upon the evidence.
ly are reaching or even overstepping the planetary boundaries. The Secretary-General convinced me to take on a seem-
This is the only workable and realistic basis for relevant and effective action, given that we are obliged to pursue
ingly impossible task, urging me: Don’t forget: you are the
common responsibilities in a closely connected and interde-
only environment minister to have become prime minister!
pendent world.
40
Harvard Public Health Review
Kent Dayton/HSPH, Suzanne Camarata for HSPH
Instead of being fearful of a new area that I needed to delve into, I quickly was relieved to find that the knowledge
who was a doctor, reha-
Neither Vision nor Evidence Alone Is Enough Evidence alone is not enough to achieve breakthroughs to reach our goals.
HSPH 2011 Commencement
Great visions and speeches alone are not what really count the most.
by the Numbers
Determination, even courage, should not be underestimated. Nor should expe-
Students from 61 countries, 31 U.S. states, and the District of Columbia and Puerto Rico received degrees at Harvard School of Public Health’s 2011 Commencement ceremonies on May 26.
rience from having had political responsibilities in government. Years of gaining experience in how to take action and get results, as Minister of the Environment and as Prime Minister, have convinced me how to move ahead. Based on evidence, programs and policies can be developed and tested‌and results and performance can be measured.
A total of 478 degrees were awarded: 13 Doctors of Philosophy 2 Doctors of Public Health 57 Doctors of Science 13 Masters of Arts 242 Masters of Public Health 151 Masters of Science At a reception the evening before, 14 students, eight faculty members, and two staff members were selected for special recognition.
Photo slide shows and videos from Commencement events can be viewed online at http://www.hsph.harvard. edu/news/features/features/hsphcommencement-2011.html. Students celebrate with diplomas and cheers.
STUDENT AWARDS Albert Schweitzer Award Robert Hughes, Master of Public Health Fang-Ching Sun Memorial Award Gregory Peter Keane, Master of Public Health
Robert B. Reed Prize for Excellence in Biostatistical Science
Matthew Miller, Associate Professor of Health Policy and Management
Shira Mitchell, Doctor of Philosophy
Meredith B. Rosenthal, Professor of Health Economics and Policy
Student Recognition Awards Erica Teresa Warner, Doctor of Science
Mentoring Awards
Alissa Weiss, Master of Science
Marcia Castro, Assistant Professor of Demography
Edgar Haber Award in Biological Sciences
Teaching Assistant Awards
Shannon Marie Reilly, Doctor of Philosophy
Peter Lipman, Doctor of Philosophy
Gareth M. Green Award for Excellence in Public Health
Jesse Ortendahl, Master of Science
Cindy Leung, Doctor of Science
Anna Snavely, Doctor of Philosophy
Michael Bryant Hadley, Master of Science Thomas Anthony McHale, Master of Science
FACULTY AWARDS
Dana Renee Thomson, Master of Science
Roger L. Nichols Excellence in Teaching Award
James H. Ware Award for Achievement in the Practice of Public Health
S. Bryn Austin, Associate Professor in the Department of Society, Human Development, and Health
Bert Govig, Master of Public Health
Teaching Citations David Harrington, Professor of Biostatistics
Miguel Hernan, Associate Professor of Epidemiology Chih-Hao Lee, Associate Professor of Genetics and Complex Diseases Murray Mittleman, Associate Professor in the Department of Epidemiology
STAFF AWARDS Staff Recognition Awards Jelena Tillotson-Follweiler, Manager of Academic Services Cecil M. Haverkamp, Program Associate/ Coordinator of Strategic Partnerships and Global Health Practice
Fall 2011
41
Strengthening Health Systems to Address New Challenge Diseases (NCDs) Reframing a Public Health Acronym In September 2011, the United Nations General Assembly is holding a High-Level Meeting on
I
n the realms of social and economic development, low- and middle-income countries differ
the prevention and control of noncommunicable
in many ways. Yet in the realm of health, they
diseases (NCDs). In the following essay, Felicia
share an emerging challenge: the compound
Marie Knaul, director of the Harvard Global Equity
burden of increasingly prevalent chronic and
Initiative (HGEI), and Harvard School of Public
noncommunicable diseases, combined with a
Health Dean Julio Frenk offer a new perspective
backlog of disease and illness associated with
on how to reframe this urgent and evolving public
“underdevelopment” and typically related to
health issue. This framework is being applied by
preventable infections.
the Global Task Force on Expanded Access to Cancer
As the backlog recedes in the face of progress in public health and medicine, the relative
of global leaders from the cancer care and public
burden of chronic and noncommunicable disease
health communities originally convened through
increases. Although the epidemiological land-
HSPH, HGEI, Harvard Medical School, and the Dana-
scape varies among countries, it is universally
Farber Cancer Institute. A report on the Task Force’s
true that it will be increasingly defined by aging
first two years of work will be released this fall.
populations and by what have previously been called “noncommunicable diseases,” or NCDs— but which we believe should be called New Challenge Diseases, with the same acronym.
42
Harvard Public Health Review
Shannon Stapleton/REUTERS
Care and Control in Developing Countries—a group
A Linguistic Straitjacket
the second UN meeting of heads of state and government
Today, the decades-long distinctions between “chronic” and
dedicated to health—the first was on HIV/AIDS a decade
“acute,” and “communicable” and “noncommunicable,” are
ago—and it sets the stage for a global call to action.
increasingly irrelevant and inaccurate. Many diseases labeled
Perhaps we can have the best of both worlds by main-
as noncommunicable and treated as chronic in fact originate
taining the acronym NCD while adapting it to encompass the
from a preventable infection—for example, cervical cancer.
realities of the health dilemmas currently faced by low- and
At the same time, several diseases of infectious origin are
middle-income countries: New Challenge Diseases.
chronic—most notably, HIV/AIDS. The false dichotomies—which strongly shaped public health in the past—today place a heavy burden on research and on policy. The nomenclature itself has become a straitjacket that prevents the most effective translation of research
Adopting the concept of New Challenge Diseases enables us to better respond to the misunderstandings that currently detract from more effective action. There is a widespread belief, for example, that expanding access to health care for NCDs is an unrealistic goal for
“ Non” pits one group against another—communicable versus noncommunicable—fueling a situation where advocates compete rather than work together to better apply scarce resources. into evidence, advocacy, and policymaking. Health systems
developing countries. Debunking this notion would permit
can become trapped in a static model that doesn’t adapt to
us to examine what can be done rather than what cannot.
epidemiological change, medical breakthroughs, or opportu-
We can develop comprehensive strategies to address NCDs
nities for innovation in delivery and financing of care.
in low- and middle-income countries. We can offer cost-
“Noncommunicable” is the obvious example of this
effective treatment alongside prevention. We can strengthen
rigid and restrictive terminology. To begin with, defining
health systems so that they respond to the complex array of
anything as a “non” implies a subservience to some other
diseases afflicting all countries, rich and poor.
entity that is dominant. It also implies that the group can be characterized by what it is not (in this case, “communicable”). And “non” pits one group against another—communicable versus noncom-
debunking myths Meeting the NCD challenge requires overcoming four myths: Myth #1: NCDs are not a major problem in developing
municable—fueling a situation where advocates compete
countries. Two decades of research about the epide-
rather than work together to better apply scarce resources.
miologic transition in developing countries have documented the rising importance of noncommunicable
from “noncommunicable” to “new challenges” The acronym “NCD” is well known and much used in academic and policy circles. As a result of extensive research and lobbying, the neglected health challenge is about to receive
diseases. The UN Summit on NCDs and the meetings and documents that have led up to it reflect the impact of evidence. Myth #2: Even if NCDs are important, there is little that developing nations can do to address them. Actually, we already have cost-effective interventions
the attention it deserves through the High-Level Meeting of
for the majority of NCDs in developing regions, and we
the United Nations General Assembly on the Prevention and
should deploy them alongside preventive strategies in a
Control of NCDs, scheduled for September 2011. This is only
full cycle of care.
continued Fall 2011
43
Myth #3: Even if there are effective interventions, developing countries cannot afford them. As many of the successful initiatives demonstrate, we can mobilize both global and national resources in a fiscally responsible way that vastly expands access to comprehensive services for NCDs. Myth #4: Responding to the challenge of NCDs would siphon attention from more urgent priorities, mainly the health-related Millennium Development Goals. This myth is especially pernicious because it polarizes the global health community in a zero-sum, competitive mentality. Instead, we should look for synergies among disease-specific programs and strengthen health systems so they can address the multiple, diverse, and complex needs of people who are the real patients, not just the specific ailments that plague them.
• First, a new generation of health promotion and disease prevention strategies; • Second, universal social protection guaranteeing access to high-quality care without fear of financial catastrophe; • T hird, innovations in the delivery of health services that draw on the technological and managerial revolutions of our times. Countering the New Challenge Diseases will demand shared learning among countries, based on rigorously evaluating national innovations. Equally important will be mobilizing global solidarity in our interdependent world. The upcoming UN Meeting poses a unique opportunity to secure the place of New Challenge Diseases in the global
Chronic Chr ron c
acute ute non-communicable
COMM CO
NewCCOOMM Challenge Diseases MUNICA ABLE Chronic acute e municab acu ute non-communicable m mmunicab
These four myths are familiar to the public health com-
health agenda. The outcomes of this meeting must include
munity because they were applied to AIDS only a decade
road maps for implementation that will present new respon-
ago: The same four misconceptions were put forward as
sibilities and opportunities that the global health community
justifications for inaction. Fortunately, they were not heeded,
should actively take up as we seek to bridge unhealthy di-
in large part due to the force of the UN meeting convened in
vides and strengthen our ability to confront new challenges.
2001. Expanded access to prevention and care for HIV/AIDS
We must invest in education and capacity building, as well
counts as one of the greatest achievements in the history of
as in research that will supply the necessary evidence to
global health.
guide both national and global health policymaking through the ambitious process of moving from resolutions to action.
Comprehensive response The same success can now apply to New Challenge Diseases—including responding to the new face of AIDS as a chronic illness. We must craft appropriate and effective evidence-based policies and engage all relevant actors in multi-stakeholder frameworks for action. NCDs drive a health scenario that can be characterized by two words: change and complexity. This complexity can be addressed through a comprehensive response built on three pillars:
44
Harvard Public Health Review
Felicia Marie Knaul, director of the Harvard Global Equity Initiative, is Secretariat of the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries. arvard School of Public Health Dean Julio Frenk is coH chair of the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries.
Alumni News 1964
1978
extensively on health issues af-
1994
William Jobin, SM, SD ’67,
John Quelch, SM, was named
fecting low-income, immigrant,
Rupa Chinai, Harvard Journalism
recently published A Realistic
dean of the China Europe
and farmworker populations. He
Fellow for Advanced Studies in
Strategy for Fighting Malaria in
International Business School
was formerly at The California
Public Health, Center for Health
Africa (Boston Harbor Publishers,
in Shanghai in December 2010.
Endowment and is now an inde-
Communications, co-authored the
2010). The book summarizes
Previously, Quelch was a profes-
pendent consultant.
Jobin’s 50 years of work in Africa
sor at Harvard Business School
fighting tropical diseases with
and dean of the London Business
engineering methods. It is
School. Quelch also was made a
“highly critical of the currently
Commander of the Order of the
disorganized approach to fight-
British Empire (CBE) in Queen
ing malaria in Africa,” he says.
Elizabeth’s 2011 Birthday Honors
Jobin also recently published two
for his services to British business.
monographs on Sudan, drawing
Dr. Jaime Sepulveda, MPH,
Mostashari trained in internal
SM ’81, SD ’85, was appointed by
medicine at Massachusetts General
the University of California, San
Hospital and was an Epidemic
Francisco, in May as executive
Intelligence Service officer at the
director of Global Health Sciences.
1997
Centers for Disease Control and
Dr. Daniel Quirk, MPH, was
1977
Sepulveda has broad international
Prevention. As assistant com-
appointed in January associ-
Dr. Jonathan Samet, SM, ap-
leadership experience in public
missioner for the Primary Care
ate professor in the Division of
pointed in 2011 by President
health, most recently serving as
Information Project at the New
Gastroenterology and Hepatology
Barack Obama to the National
director for special initiatives at the
York City Department of Health and
in the Department of Medicine at
Cancer Advisory Board, chaired
Bill & Melinda Gates Foundation,
Mental Hygiene, he helped facilitate
Philadelphia’s Thomas Jefferson
the World Health Organization
where he played a central role in
the adoption of prevention-oriented
University Hospital. Quirk previ-
panel that found radiofrequency
shaping global health strategy. At
health IT by more than 1,500 health
ously was a clinical assistant pro-
electromagnetic radiation, which is
UCSF, he oversees a chancellor-
care providers in underserved
fessor at Brown University School
emitted by cell phones, to be “pos-
level program that integrates the
communities.
of Medicine and a practicing physi-
sibly carcinogenic.” An epidemiolo-
University’s international partnerships, education, and research
1993
cian at Rhode Island Hospital and
gist whose research has addressed health risks posed by environmen-
focused on the world’s top health
tal agents, including active and
issues.
passive smoking and indoor and
1991
on his experiences in the country working for the World Health Organization on control of malaria and schistosomiasis.
outdoor air pollution, Samet emphasized in The New York Times that the findings, announced May 31, were preliminary. He expressed hope that they would lead to further research on the effects of cell phones, particularly on children.
Dr. Farzad Mostashari, SM, was named national coordinator for health IT by U.S. Health and Human Services Secretary Kathleen Sebelius in April. He previously served as deputy national coordinator for programs and policy.
Dr. Virginia Hood, MPH, was elected president of the American
book Putting Women First: Women
and Health in a Rural Community (STREE, 2010) with Dr. Rani Bang of the Society for Education, Action and Research in Community Health. The book describes the work of Bang and her husband, who opened a rural hospital with a community outreach program in the neglected Gadchiroli district in the Indian state of Maharashtra.
Roger Williams Hospital.
1998
College of Physicians at the organi-
Dr. Roderick King, MPH, was se-
zation’s annual scientific meeting,
Joel Diringer, MPH, gave a
lected as a Fulbright Nexus Scholar
held in April in San Diego. Hood is
for 2011–2012. As a Fulbright
presentation entitled “Community
a practicing physician and a profes-
grantee, he will spend up to one
Health Research: The Intersection
sor of medicine at the University
year engaged in his proposed
of Policy, Practice and Ethics”
of Vermont. She has served as an
project, “Advancing Health in the
to students in the National
adviser to the State of Vermont’s
Caribbean through Leadership
Institutes of Health Bridges to the
health care programs as a member
Development.” The Fulbright
Baccalaureate program at Allan
of the Drug Utilization Review
Nexus Program supports profes-
Hancock College in Santa Maria,
Board in the Office of Vermont
sionals and midcareer researchers,
California, in April. Diringer, a
Health Care Access (Medicaid).
who participate in multidisciplinary
health policy expert, has worked
continued Fall 2011
45
Alumni News and an exchange experience. King
Meet Your Alumni Association Representatives
also has received two appoint-
An ongoing series about your elected representatives on the HSPH Alumni Council.
ments within the U.S. Department
If you would like to get more involved as a representative, committee member,
of Health and Human Services:
volunteer, donor, or mentor, contact the Office for Alumni Affairs at alumni@hsph.
Secretary’s Advisory Committee on
harvard.edu.
team-based research, seminars,
Minority Health and senior adviser, Bureau of Primary Health Care,
A report from the President of the HSPH Alumni Association
Health Resources and Services
Royce Moser Jr., AB ’57, MD ’61, MPH ’65
Administration.
September 24 will mark the end of my two-year term as president of
2001
the Harvard School of Public Health Alumni Association. It has been my privilege to work with the more than 50 dedicated alumni who serve
Dr. Patrik Johansson, MPH, was
as elected representatives or committee volunteers. I am enormously
appointed in April by President
grateful for the enthusiastic support for Alumni Association activities
Barack Obama to the Advisory
from Dean Julio Frenk, School administrators, faculty, and current
Group on Prevention, Health
students.
Promotion, and Integrative and
As I hand the reins to President-elect Elsbeth Kalenderian, MPH
Public Health. The advisory group is part of the National Prevention Council, which was created through the Affordable Care Act. The group aims to develop a national prevention strategy that identifies key priorities and actions needed across
’89, later this month, I thought it important to report on some of the significant recent achievements of the Council and our future plans. One of those achievements is the new HSPH Online Community, which is launching shortly after Labor Day, where I’ve posted a brief summary of the past few years’ work to build a stronger alumni network. You can read my full report at www.hsph. harvard.edu/alumni.
reduce the nation’s leading causes
Chandak Ghosh, MD, MPH ’00 HSPH Alumni Councilor, Fall 2010–2013
of death and disability. Johansson
A board-certified ophthalmologist and officer in the U.S. Public Health
previously was director of the Rural
Service, Dr. Chandak Ghosh works at the Health Resources and Services
Health Education Network and an
Administration (HRSA), a federal agency within the U.S. Department of Health
associate professor at the University
and Human Services. His work as Medical Consultant for Federal Policy led to
of Nebraska Medical Center College
the development of HRSA’s National Performance Review Protocol, utilized
of Public Health.
to improve all federal health grantees, including hospitals, universities, and
2007
and training residents at Queens Hospital Center of Mount Sinai School of
all sectors of society to prevent and
Yee-Ho Irene Chan, MPH, was
community health centers. He is also a practicing eye surgeon, seeing patients Medicine in New York City.
profiled in a Washington Post story published online May 9. Chan, the assistant country director for the Food and Drug Administration’s China office in Beijing, works with Chinese regulatory agencies and food companies to encourage stringent food safety practices.
46
Harvard Public Health Review
The Harvard Public Health Review is interested in hearing from you. Please send comments or class notes to: Amy Roeder, Assistant Editor Harvard Public Health Review 90 Smith Street Boston, MA 02120 Phone: (617) 432-8440 Fax: (617) 432-8077 Email: review@hsph.harvard.edu
Faculty News Awards and Honors Richard Cash, senior lecturer on global health, will receive the 2011 Fries Prize for Improving Health, to be presented at the Centers for Disease Control and Prevention Global Leadership Conference in November. Awarded by the James F. and Sarah T. Fries Foundation, the annual $60,000 prize recognizes great contributions to human health. Cash was honored for his leadership in the development and dissemination of oral rehydration therapy, a simple mixture of salt, sugar, and water that since the early 1970s has saved tens of millions of children and adults from dying of diarrheal diseases. Julio Frenk, dean of HSPH and T & G Angelopoulos Professor of Public Health and International Development, was elected to the American Academy of Arts and Sciences, one of the nation’s most prestigious honorary societies and a leading center for independent policy research.
Glimcher,” drew alumni and former trainees from around the globe to mark Glimcher’s 30 years of contributions to science. Attendee William Paul, of the National Institute of Allergy and Infectious Diseases, described Glimcher as one of the most “dynamic, thoughtful, intelligent, and accomplished leaders” in her field.
professor of environmental and occupational epidemiology Delia Wolf, assistant dean for regulatory affairs and research compliance
New Appointments Goodarz Danaei, assistant professor of global health Kristen Davison, associate professor of nutrition James Dunn, William Lyon Mackenzie King Visiting Professor of Canadian Studies Jian Guo, assistant professor of biostatistics
Sara Singer, assistant professor of health care management and policy, spoke in May at Princeton University on a panel about the future of health care in the United States. Singer cited integration of health care institutions and the increased adoption of health information technology as important steps toward eliminating waste and inefficiency in the health care system.
Bernardo Lemos, assistant professor of environmental epigenetics Margaret McConnell, assistant professor of global health economics Lorenzo Trippa, assistant professor of biostatistics
Bookshelf
Francesca Dominici, associate dean for information technology Miguel Hernán, professor of epidemiology Chih-Hao Lee, associate professor of genetics and complex diseases Chenseng (Alex) Lu, associate professor of environmental exposure biology S. V. Subramanian, professor of population health and geography Marc Weisskopf, associate
Heavy Metals: A Rapid Clinical Guide to Neurotoxicity and Other Common Concerns Kenneth R. Spaeth, Antonios J. Tsismenakis, Stefanos N. Kales. Edited by Stefanos N. Kales. Nova Science Publishers, Inc. 88 pages
Promotions
Laurie Glimcher, Irene Heinz Given Professor of Immunology, was honored at a daylong symposium on April 15 at the Joseph B. Martin Conference Center at Harvard Medical School. The event, “A Commitment to Lineage: A Symposium in Celebration of Laurie
effort to reform the nation’s health care system. McDonough, professor of the practice of public health and director of the Center for Public Health Leadership at the Harvard School of Public Health, and an adviser to the late Senator Edward Kennedy, provides a vivid picture of the ACA’s inner workings, revealing the rich landscape of the issues, policies, and controversies behind this landmark law.
Inside National Health Reform John E. McDonough California/Milbank Books on Health and the Public 360 pages This guide to the Affordable Care Act (ACA), the United States’ new national health care law, lends an insider’s deep understanding of policy to a lively and absorbing account of the extraordinary—and extraordinarily ambitious—legislative
Exposure to toxic metals remains a public health hazard around the globe. Though the prevalence and intensity of exposure may vary from place to place, metal toxicity has been, and will continue to be, a challenge to recognize, treat, and control. This book is written as a pragmatic guide for primary care clinicians, neurologists, occupational health specialists, and toxicologists who evaluate adult patients. The authors review five metals that are neurotoxic (arsenic, lead, manganese, mercury, and thallium) and discuss the clinical approach
continued Fall 2011
47
Melvin W. First
In Memoriam
Melvin W. First died at age 96 on June 11. A member of the Harvard School of Public Health community for more than 60 years, First began as a research fellow in 1947 and stayed active in research and teaching long past his retirement in 1985. Working his way up in what was then called the Department of Industrial Hygiene (now the Department of Environmental Health), he ultimately became a professor of environmental health engineering in 1971.
Steve C. Pan Steve C. Pan, MPH ’53 and professor emeritus of tropical public health, died May 21 at age 89. He is remembered as a skilled microscopist, careful researcher, and an insightful mentor to generations of students and colleagues.
Bookshelf continued to patients potentially exposed to these toxicants. Kales is an associate professor in the Department of Environmental Health and division chief of Occupational and Environmental Medicine at Cambridge Health Alliance.
High Stakes: The Critical Role of Stakeholders in Health Care David A. Shore with Eric D. Kupferberg Oxford University Press 160 pages “The United States health care system is broken,” state the authors
48
Harvard Public Health Review
of High Stakes, who turn an analytic lens on key groups that they say are pursuing their own interests at the risk of the system at large. Insurance providers want to reduce their payments, hospitals want higher reimbursements, patients want access to unlimited services, and no one wants to work together. For health care to succeed as an enterprise, groups must align their interests and move beyond entrenched behaviors, according to the authors. Drawing equally from both scholarly studies and real-world examples, High Stakes offers health care leaders the necessary tools to both map their current stakeholder relationships and fashion concrete steps to produce greater engagement, collaboration, and cooperative competition. Shore is director of the Forces of Change Program and associate dean for continuing professional education.
The Reality of Precaution: Comparing Risk Regulation in the United States and Europe Edited by Jonathan B. Wiener, Michael D. Rogers, James K. Hammitt, and Peter H. Sand RFF Press 602 pages Challenging conventional wisdom that Europe has become more precautionary than the United States in risk regulation, this book finds that from the 1970s to the present, there has been little trans-Atlantic difference in the overall level of
precaution. Instead, there have been selective variations in precaution applied to particular individual risks. For example, while Europe has become more precautionary about risks such as genetically modified foods, climate change, and toxic chemicals, the U.S. has become more precautionary about risks such as mad cow disease, tobacco, air pollution, and terrorism. Combining a dozen case studies, a quantitative analysis of almost 3,000 risks, and crosscutting chapters on politics, law, and risk perceptions, this book analyzes the relationship between U.S. and European regulatory approaches and provides comprehensive advice for policymakers. Hammitt is a professor of economics and decision sciences.
Mel First © Sharon Bray, Steve Pan © George Cushing; Photographs provided courtesy of the Harvard Medical Library, Francis A. Countway Library of Medicine.
First led the HSPH program in air cleaning for nearly four decades and was recognized internationally for his research and field applications of filter theory, operation, and maintenance, and of nuclear air cleaning systems. For the past two decades, he was deeply involved with international air disinfection research aimed at controlling pathogens such as drug-resistant tuberculosis and influenza.
Fawzi named Chair of Department of Global Health and Population Wafaie Fawzi assumed the role of chair for the Department of Global Health and Population on September 1. Fawzi succeeds David Bloom, the Clarence James Gamble Professor of Economics and Demography at HSPH, who served for 10 years. Bloom will continue as a faculty member in the Department, pursuing his research and global collaborations to better understand the interplay of health status, population trends, and economic growth. Since becoming a member of the HSPH faculty in 1996, Fawzi has sought to reduce the number of children under age five who die each year and to improve the health of mothers. He has designed and implemented randomized controlled trials and observational studies of maternal, neonatal and child health, and infectious diseases—with an emphasis on nutritional factors that could lead to better health outcomes—in India, Sudan, Tanzania, Uganda, and other
developing countries. Fawzi also has built research and training capacity at partner institutions in several countries, most notably in Tanzania, where he also has been principal investigator on HSPH’s President’s Emergency Plan for AIDS Relief (PEPFAR) initiative that has brought lifesaving antiretroviral drugs to more than 70,000 people living with HIV. Fawzi received his medical degree from the University of Khartoum, Sudan, and his MPH, MS in Maternal and Child Health and PhD in Epidemiology and Nutrition from HSPH. He has joint appointments in HSPH’s Departments of Nutrition and Epidemiology and in the Department of Global Health and Population. Williams Joins HSPH as Chair of Department of Epidemiology Michelle Williams, Stephen B. Kay Family Professor of Public Health, succeeded Hans-Olov Adami as chair of the Department of Epidemiology on August 1. Adami served for more than four years and will continue as a member of the faculty.
Previously a professor of epidemiology and global health at the University of Washington School of Public Health, Williams has a long-standing relationship with the HSPH Department of Epidemiology, from which she received her doctorate in 1991. She has published more than 230 scientific articles and has received numerous research and teaching awards, including the American Public Health Association’s Abraham Lilienfeld Award. In 2011, President Barack Obama presented Williams with the Presidential Award for Excellence in Science, Mathematics, and Engineering Mentoring. Williams’s major research interests lie in the areas of women’s reproductive health and child health. Her work focuses on integrating genomic sciences and epidemiological research methods to identify risk factors, diagnostic markers, treatments, and prevention targets for disorders that contribute to maternal and infant mortality. Her current activities include research and teaching collaborations with epidemiologists in Chile, Ethiopia, Peru, and Thailand. Williams also is co-director of the Center for Perinatal Studies at Swedish Medical Center in Seattle, a multidisciplinary research program involving clinical scholars, basic scientists, and epidemiologists.
Continuing Professional Education Programs, 2011–2012 Where theory informs practice and practice informs theory Top, Kent Dayton/HSPH; center, courtesy of Dr. Michelle Williams
October 2011
January 2012
October 3–6 Ergonomics and Human Factors: Strategic Solutions for Workplace Safety and Health
January 8–20 Program for Chiefs of Clinical Services
October 23–28 Leadership Strategies for Evolving Health Care Executives October 30–November 11 Leadership Development for Physicians in Academic Health Centers December 2011 December 5–7 Advanced Laboratory Design for Health, Safety, and the Environment
January 22–27 Leadership Strategies for Information Technology in Health Care
March 26–28 Management and Leadership Skills for Environmental Health and Safety Professionals April 2012 April 23–26 Safety in Design and Construction: A Lifecycle Approach
March 2012
May 2012
March 12–14 Basic Hands-On CAMEO Training
May 14–16 Effective Risk Communication: Theory, Tools, and Practical Skills for Communicating about Risk
March 19–22 Analyzing Risk: Science, Assessment, and Management
May 14–18 Leadership Strategies for Information Technology in Health Care
Customized programs are also available. All programs are held in Boston unless otherwise noted. For additional information or to register, contact: (617) 384-8692 contedu@hsph.harvard.edu https://ccpe.sph.harvard.edu Harvard School of Public Health Center for Continuing Professional Education 677 Huntington Ave. CCPE-Dept. A Boston, MA 02115
Fall 2011
49
Harvard Public Health Review Dean of the Faculty Julio Frenk
Visiting Committee Jeffrey P. Koplan, MPH ’78 Chair
Alumni Council As of November 2010
Ruth L. Berkelman Joshua Boger Walter Clair Nicholas N. Eberstadt Tore Godal Jo Handelsman Risa Lavizzo-Mourey Bancroft Littlefield Nancy T. Lukitsh Vickie M. Mays Michael H. Merson Anne Mills Kenneth Olden John W. Rowe Bernard Salick Burton Singer
Officers Royce Moser, Jr., mph ’65 President Elsbeth Kalenderian, mph ’89 President-Elect Anthony Dias, mph ’04 Secretary Mark S. Clanton, mph ’90 Immediate Past President Alumni Councilors 2008-2011 G. Rita Dudley-Grant, MPH ‘84 Sean Dunbar, SM ‘08* Maxine Whittaker, MPH ‘86
Board of Dean’s advisors Jeanne B. Ackman Theodore Angelopoulos George D. Behrakis Katherine S. Burke Gerald L. Chan Lee M. Chin Jack Connors, Jr. Jamie A. Cooper-Hohn Antonio O. Garza C. Boyden Gray Rajat K. Gupta Mala Gaonkar Haarmann Richard L. Menschel* Roslyn B. Payne Swati A. Piramal Alejandro Ramirez Carlos E. Represas Richard W. Smith Howard Stevenson Samuel O. Thier Katherine Vogelheim
*emeritus
2009-2012 Marina Anderson, mph ’03 Rey de Castro, SD ’00 Cecilia Gerard, SM ’09* 2010-2013 Teresa Chahine, SD ’10* Sameh El-Saharty, MPH ‘91 Chandak Ghosh, MPH ‘00 *Class Representative
For information about making a gift to the Harvard School of Public Health, please contact: Ellie Starr Vice Dean for External Relations Office for External Relations Harvard School of Public Health 90 Smith Street Fourth Floor Boston, Massachusetts 02120 (617) 432-8448 or estarr@hsph.harvard.edu For information regarding alumni relations and programs, please contact, at the above address: Jim Smith, Assistant Dean for Alumni Affairs (617) 432-8446 or jsmith@hsph.harvard.edu www.hsph.harvard.edu/give
50
Harvard Public Health Review
The Harvard Public Health Review is published three times a year for supporters and alumni of the Harvard School of Public Health. Its readers share a commitment to the School’s mission: advancing the public’s health through learning, discovery, and communication. Harvard Public Health Review Harvard School of Public Health Office for External Relations 90 Smith Street Fourth Floor Boston, Massachusetts 02120 (617) 432-8470 Please visit www.hsph.harvard.edu/review and email comments and suggestions to review@hsph.harvard.edu. Dean of the Faculty Julio Frenk T & G Angelopoulos Professor of Public Health and International Development Vice Dean for External Relations Ellie Starr Associate Vice Dean for Communications Julie Fitzpatrick Rafferty Director, Strategic Communications and Marketing Samuel Harp Editor Madeline Drexler Senior Art Director Anne Hubbard Assistant Editor Amy Roeder Principal Photographer Kent Dayton Marketing and Communications Coordinator Rachel Johnson Contributing Writers Eric Bender, Luisa Cahill, Debra Bradley Ruder, Richard Saltus, Thea Singer © 2011 President and Fellows of Harvard College
Bernard and Gloria Salick
on supporting students at Harvard School of Public Health through the Bernard and Gloria Salick Fellowship
Dr. Salick is a pioneer and expert in the field of disease management as well as a long-time supporter of health and education causes. To him, HSPH stands out most for its worldwide efforts to eradicate critical health problems and for its ability to follow through on its promises. Dr. Salick and his wife established the Bernard and Gloria Salick Fellowship to support HSPH
“W
are delighted to provide support to these very e bright and altruistic students who have chosen the field of public health as their vocation.
“Harvard School of Public Health is a wonderful institution with a long history of leadership in these areas so vital to the survival of our global community. “We are honored to be a part of this effort and encourage others to join us in this very worthy endeavor.”
students in 2004.
Please give to support financial aid today. To find out how, visit http://hsph.harvard.edu/give/ or call Morgan Pendergast at (617) 432-8436.
HARVARD
School of Public Health
Office for External Relations 90 Smith Street Boston, Massachusetts 02120
Nonprofit Org. U.S. Postage PD Burlington, VT Permit No. 586
Change Service Requested
Tax-Free IRA Rollover Extended to Year End For a limited time only, people age 70 1/2 or older can take advantage of a tax-free IRA charitable rollover to support the work of the Harvard School of Public Health (HSPH). Instead of having to withdraw money and report it as taxable income, you can transfer up to $100,000 directly from your IRA to HSPH, tax-free. This provision, introduced as part of the Pension Protection Act of 2006 and revived last year, expires at the end of 2011. So don’t wait.
For more information contact: John Christel Harvard University Planned Giving Office 800-446-1277 pgo@harvard.edu