Health Quarterly October 2022



A Special Supplement to the









For some patients, choosing a primary care provider may ultimately come down to a choice between a doctor providing internal medicine or family medicine. At first glance, both internists and family doctors appear to provide the same healthcare services. So, how does a patient decide between the two? Make an educated decision on your healthcare. Learn the difference between internal medicine and family medicine to
determine which provider is right for you.

Doctors who practice internal medicine, also known as internists, focus primarily on the care and treatment of adult patients.
According to the American College of Physicians, internal medicine began in the 1800s, predating the existence of pediatric medicine, which began in the early 1900s. While internists may choose to also treat children, they must first undergo dual training for both internal medicine and pediatric medicine.
The ACP reports internists must have experience in outpatient settings as well
as at least one year of caring for hospitalized patients — including three months in an intensive or critical care unit.
The practice of internal medicine includes experience in general medicine as well as internal subspecialties, which can range from rehabilitation medicine to psychiatry. This training allows internists to develop expertise in numerous conditions. Consequently, internists can diagnose and treat a wide variety of diseases in adults, can diagnose and treat chronic illnesses and conditions, and can expertly treat complex situations in which an adult may be afflicted with more than one medical condition. In addition, internists are uniquely able to assist
one another with medically complicated patients, while their experience in both inpatient and outpatient settings allows them to transition patients requiring hospitalization.
Unlike internists, family medicine doctors — or family physicians — are more broadly trained to care for patients of all ages, from children to seniors.
Family physicians typically train in outpatient settings, providing acute, chronic, and wellness care for a variety of patients, though family physicians also have some training in inpatient settings.
Family physicians can
provide holistic, long-term care for their patients, some of whom they may have known their whole lives. This allows family physicians to create specialized, preventative plans for each patient. Because family physicians are broadly trained, they can more easily adapt to the specific healthcare needs of their community. This enables them to provide broad healthcare services in areas without easy access to medical specialists, with whom family physicians are trained to coordinate care.
The ACP also reports family physicians can function as primary care providers for adults as part of a family unit.
Which should you choose?
Both internists and family physicians can serve as your primary care provider and can provide unique benefits for you and your loved ones. Ultimately, the choice is yours when deciding who your provider should be. Find a physician with whom you’re comfortable and get the expert, compassionate healthcare you need.
OUR PROVIDERS ARE READY TO HANDLE YOUR FAMILY’S HEALTHCARE NEEDS. LEARN MORE ABOUT THE CULBERTSON CLINICS AND FIND A PROVIDER CLOSE TO YOU.

Women are urged to report any abnormalities in their breasts to a physician immediately.

Breast cancer is the most commonly occurring cancer in women across the globe.
According to the World Cancer Research Fund International, there more than 2.26 million new cases of breast cancer in women in 2020. Such figures are sobering, but it’s important to recognize that breast cancer survival rates have improved dramatically in recent decades, providing hope to the millions of women who may be diagnosed with the disease in the years to come.
Various factors have helped to improve breast


cancer survival rates, and education about the disease is certainly among them. Women are their own greatest allies against breast cancer, and learning to spot its signs and symptoms is a great first step in the fight against this potentially deadly, yet treatable disease.
The American Cancer Society urges women to take note of how their breasts normally look and feel. That knowledge is vital because it helps women recognize when something does not look or feel good to the touch with their breasts. Screening alone may not be sufficient, as the ACS notes that mammograms do not find


every breast cancer.
When women are well acquainted with how their breasts look and feel, they’re in better position to recognize any abnormalities, which may or may not be indicative of breast cancer. The ACS reports that the following are some potential warning signs of breast cancer.
• A new lump or mass: The ACS indicates that this is the most common symptom of breast cancer. A lump or mass that is cancerous is often painless, but hard and has irregular edges. However, lumps caused by breast cancer also can be soft, round and tender. Some even cause
pain.
• Swelling: Some women experience swelling of all or part of a breast even if they don’t detect a lump.
• Dimpling: The skin on the breast may dimple. When this occurs, the skin on the breast sometimes mimics the look of an orange peel.
• Pain: Pain on the breast or nipple could indicate breast cancer.
• Retraction: Some women with breast cancer experience retraction, which occurs when the nipple turns inward.

• Skin abnormalities: Breast cancer may cause the skin on the breast to redden, dry out, flake, or thicken.
• Swollen lymph nodes: Some women with breast cancer experience swelling of the lymph nodes under the arm or near the collarbone.
The presence of any of these symptoms merits a trip to the doctor. Women with these symptoms should not immediately assume they have breast cancer, as the ACS notes that various symptoms of breast cancer also are indicative of non-cancerous conditions that affect the breasts. Only a physician can diagnose breast cancer, which underscores the importance of reporting symptoms to a doctor immediately.
A mammogram—an X-ray picture of breast tissue—is a valuable tool that can screen for breast cancer. In many cases, mammograms can detect breast cancer even be fore a woman notices any symptoms. Early detection allows doctors to initi ate appropriate treat ment sooner, which may improve outcomes and reduce costs.
Most women over the age of 45 are advised to get mammograms every year, or once every two years once they reach age 55. However, the exact frequency and timing of
mammograms varies for different women. If your doctor has advised you to get your first mammo gram, you might have a lot of questions or concerns about what the procedure

will be like.
Here are some things you may find helpful as you prepare for your ap pointment.
Consider scheduling your mammogram around your period.
If you haven’t started menopause yet and still get your period, try scheduling your mammogram some

time in the week after your menstrual period ends. For most women, this is when their breasts are the least tender.
Skip the deodorant.
Don’t wear powders, perfumes or deodorant on the day of your mam mogram. These personal care products might show up on an X-ray and can be mistaken for breast tissue abnormalities. (Feel free to bring these items with you to put on once your mammogram is over.)
Plan your outfit wisely. During the mammo gram, you will need to stand in front of the X-ray machine with your breasts exposed, so you’ll need to undress from the waist up (you may also be given a hospital gown to wear that is open to the front).
For your ease and privacy, we recommend that you wear a shirt or blouse and separate bottoms instead of a dress.
If you have a disabili ty that makes it difficult or impossible for you to stand, let our staff know when you call to schedule your mammogram so we can make sure to accom modate your needs.
Be prepared for some discomfort.
For most women, mammograms are uncom fortable. This is because breast tissue needs to be compressed between two plates during the proce dure in order to get a good X-ray image (this compres sion also helps minimize the amount of radiation that needs to be used). Fortunately, while your entire appointment will take about 30 minutes, the actual amount of time that each of your breasts will be compressed is only about
30 seconds.
If it helps, take some deep breaths before and after the mammogram to help you stay relaxed. You’ll just need to stay still and hold your breath while the X-ray image is being taken.
Mammograms can be incredibly helpful, but they aren’t perfect. According to the American Cancer Soci ety, mammograms fail to detect about 1 in 8 breast cancer diagnoses. This is called a false-negative: the mammogram results look normal even though breast cancer is actually present.
Mammograms can also lead to false-positives, in which the results look ab normal even though there is no breast cancer. In fact, mammograms can pick up many structures or chang es in the body that aren’t necessarily problematic, including cysts or other benign (non-harmful) masses. The problem with false-positives is that they may lead to unnecessary tests—and unnecessary concern for the patient.
So, be sure to ask your provider about the risks, benefits and limitations of breast cancer screening, and don’t hesitate to ask other questions about your health or next steps.
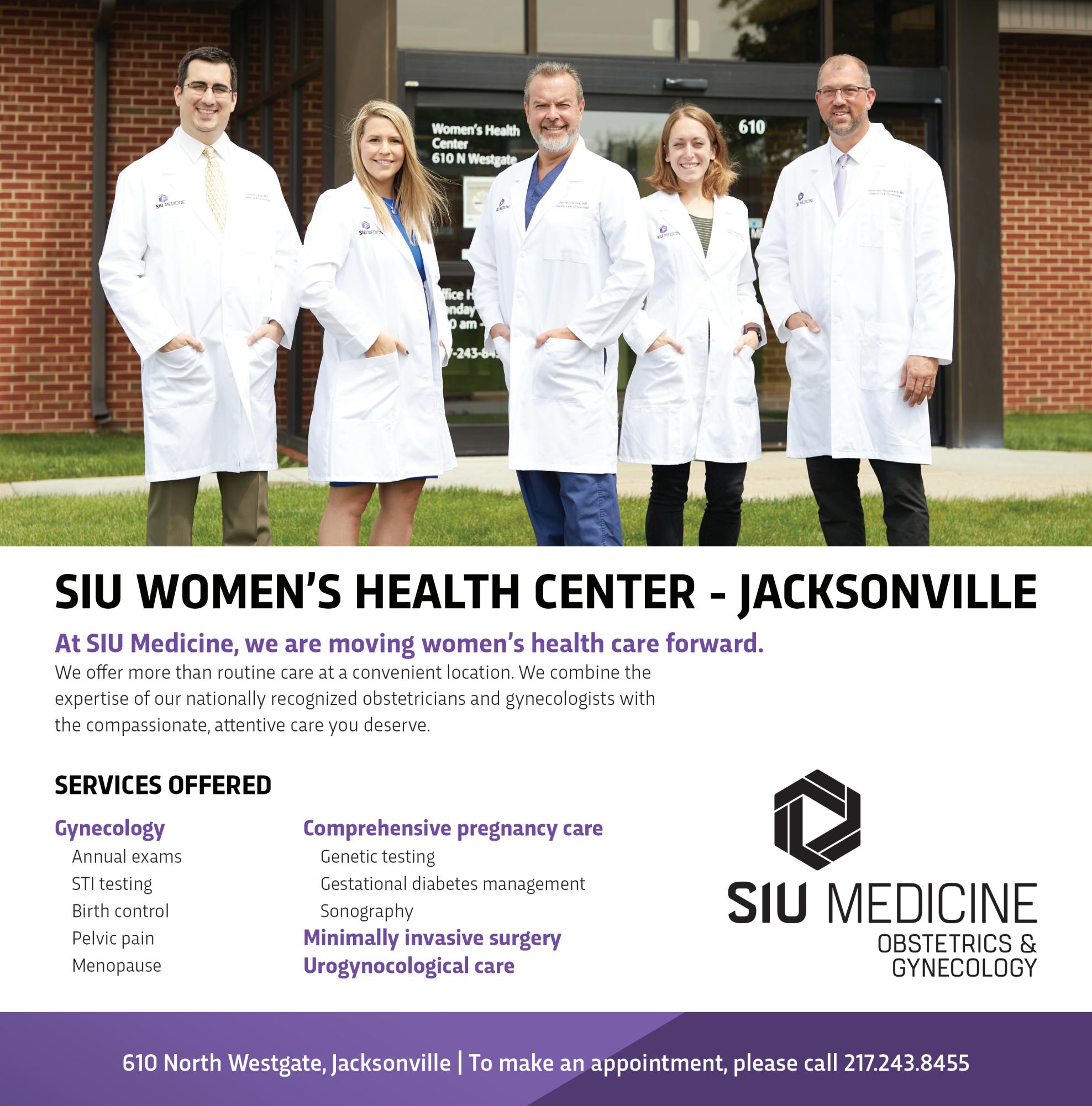
Our team at SIU Medi cine is committed to help ing women from through out Southern Illinois take a proactive approach to their health. Find a doctor at https://www.siumed.org/ doctor and schedule your next mammogram or learn more about our women’s health services.
Even if you are all-in for Team Summer, few of us can resist the call of autumn with its cooler temps, changing leaves, vibrant blue skies, hometown football games, apple orchards and all things pumpkin.
What you may not realize is how many health benefits are associated with the arrival of fall. No, pumpkin lattes don’t count! But pumpkin all by itself offers vitamins, minerals and a healthy dose of beta carotene. Use pumpkin in muffins,
breads or soups. Roast the seeds at 300 degrees for 20 -30 minutes for a crunchy and nutritious snack.
“Pumpkin is a natural immunity booster and also helps with heart health like lowering blood pressure,” said Janice Dowell, a dietitian and culinary medicine coordinator with Memorial Wellness Center. “It’s really a nutrient-dense super food. The beta-carotene, alpha-carotene and other antioxidants found in pumpkin can help lower inflammation, fight off infection and even help you control weight.”
Here are some other
health benefits that arrive with the turn of the calendar.
• Cool-weather fruits and vegetables are in abundance. Try a new variety of apples this fall, experiment with gourds, squash and even brussels sprouts.
• Take your exercise routine back outside. Nobody likes to exercise during dripping humidity and high temps, but the cooler weather makes walking, hiking or running outdoors ideal. Don’t forget to take your favorite canine with you!

• Enjoy that added hour of sleep with daylight saving time. Sleep is one of the most beneficial things you can add to your daily routine.
• Cozy up! Take time to notice the leaves changing, appreciate the addition of jeans, leggings and sweaters to your wardrobe and slow the schedule down to include picking pumpkins, walking a trail or roasting marshmallows.



Most importantly, don’t squander the fleeting opportunities of the fall season.
SIU Medicine supports and encourages all breast feeding mothers and nurs ing parents in our commu nities. We encourage you to learn more about this important topic and find out how you can support a loved one who is currently breastfeeding.

Here are four useful facts about breastfeeding we’d like to share.
Experts recommend breast milk during the first six months of a baby’s life.
Both the American Acad emy of Pediatrics (AAP) and the World Health Organization (WHO) rec ommend that babies are fed exclusively breast milk for the first six months of their lives.
However, according to
the U.S. Centers for Disease Control and Prevention (CDC), most (60 percent) of mothers don’t breastfeed for as long as they intend.
Experts strongly rec ommend breastfeeding because research is clear about how beneficial it is—not only for the nursing baby, but also for the moth er or nursing parent. For babies, breastfeeding has been shown to:
• Promote bonding
• Provide antibodies that protect against common illnesses
• Improve brain develop ment
• Benefit digestion and healthy gut bacteria
• Reduce the risk of health problems later in life, including certain allergies, asthma, leu kemia, Celiac disease, diabetes, childhood obesity and sudden infant death syndrome (SIDS)
For mothers, breastfeed ing has been shown to:
• Assist with postpartum weight loss
• Promote bonding
• Reduce the risk of health problems like breast cancer, cervical cancer, hypertension, rheumatoid arthritis and cardiovascular disease
and nursing parents do not end up nursing their chil dren as long as they want to because of challenges such as:
• Problems with lactation and latching
• Unsupportive families, peer groups and cultur al norms
• Stigma
Introducing Jacksonville’s Only Professional Hearing Aid Center.
• Provide a more cost-ef fective solution to nursing compared to formula feeding According to the AAP, breastfeeding also benefits the environment because it incurs none of the pollution nor energy costs associated with manufacturing infant formula.
Many nursing parents face barriers to breastfeeding.
Despite being so bene ficial, breastfeeding isn’t always easy. According to the CDC, many mothers
• Concerns about infant growth and develop ment
• Concerns about tak ing medication while breastfeeding
• Unsupportive practices and policies within the workplace or hospital
• Younger maternal age Sociodemographic fac tors can also pose as a bar rier to breastfeeding. For example, infants who are eligible for the Special Sup plemental Nutrition Pro gram for Women, Infants, and Children (WIC) are less likely to ever be breastfed compared to infants who
are ineligible. And infants from rural communities are less likely to be breastfed than infants from urban communities. You can help breastfeeding mothers in your community.
If you or someone you know is struggling with breastfeeding, here are some things you can do to help:
• Learn about different health care profession als in your area who are trained to help parents breastfeed, including Interna tional Board-Certified Lactation Consultants (IBCLCs), Certified Lactation Counselors (CLCs), CBEs (Certified Breastfeeding Educa tors (CBEs) or doulas
• Ask your health care provider about local mother-to-mother sup port groups or breast
• Contact with local hos pital lactation staff
• Search for local breast milk donor programs
• Visit the CDC’s website and explore resources made available by The Surgeon General’s Call to Action to Support Breastfeeding
• Connect with local breastfeeding task forc es and coalitions
• Show your support to a breastfeeding moth er in other ways (e.g., bringing them nourish ing meals, offering to babysit older children, gifting them a house keeping service)
Visit siumed.org/doc tor to explore our list of providers who can help you and your baby enjoy the benefits of breastfeeding.

Many women are concerned about the potential for developing breast cancer in their lifetimes. Breast cancer is the second-most common cancer among women in the United States and Canada. Despite that prevalence, there are ways for women to reduce their risk for breast cancer.
While it is impossible to change family history or genetic markers like gene mutations that increase breast cancer risk, the following are seven ways women can lower their risk.
1. Exercise regularly and maintain a healthy weight.
Physical activity and monitoring calories can keep weight in check. The Mayo Clinic recommends at least 150 minutes per week of moderate aerobic activity or 75 minutes per week of vigorous aerobic activity.
Strength training at least twice a week also is recommended. Being
overweight or obese increases a woman’s risk for breast cancer.
2. Consume a healthy diet.
The link between diet and breast cancer risk is still being studied. However, research suggests that a diet high in vegetables and fruit, and calcium-rich dairy products, but low in red and processed meats may lower breast cancer risk.
3. Avoid or limit alcohol consumptions.
Alcohol increases risk of breast cancer, even in small amounts. For those who drink, no more than one alcoholic drink a day should be the limit. The
more a woman drinks, the greater her risk of developing breast cancer, states the Mayo Clinic.
4. Undergo genetic counseling and testing.
Women concerned about a genetic connection or family history of breast cancer can speak to their doctor about testing and counseling that could help them reduce their risk. Preventive medicines and surgeries might help those at elevated risk for breast cancer.
5. Limit hormone therapy. Combination hormone replacement therapy for post-menopausal women may increase
risk of breast cancer, indicates the Centers for Disease Control and Prevention. Similarly, taking oral contraceptives during reproductive years may increase risk. Women can speak with their physicians to weigh the pros and cons of taking such hormones.
6. Breastfeed children, if possible. Breastfeeding has been linked to reducing a woman’s risk of developing breast cancer.
7. Learn to detect breast cancer. Women should get to know their bodies so they can determine if something is awry as early as possible. Early detection of breast cancer increases the chances that treatment will prove successful.
Women can embrace various strategies to reduce their risk of developing breast cancer.

No woman is immune to breast cancer. However, some women with extensive family histories of the disease may wonder if they’re more vulnerable to breast cancer than those without such a link.
According to the Centers for Disease Control and Prevention, roughly 3 percent of breast cancers result from inherited mutations in the BRCA1 and BRCA2 genes that are passed on in families. Inherited mutations in other genes also can cause breast cancer (as well as ovarian cancer), but BRCA1 and BRCA2 are the most commonly affected genes. And it’s not just women who can inherit these mutations. Though men account for only a small percentage of breast cancer patients, they can get the disease, and those who inherit mutations in BRCA1 and

BRCA2 are more likely to develop breast cancer than other men. The CDC notes that not everyone who inherits a BRCA1, BRCA2 or other mutation will develop breast cancer, and women with such mutations can take steps to help lower their risk for the disease. Doctors can discuss those steps with women, but they may include genetic counseling and testing.
The CDC also notes that, even in instances when counseling and testing is not ultimately recommended by a physician, women should consider talking to their doctors about starting mammography screening in their 40s. That’s earlier than some organizations recommend, though physicians may feel it’s worth it depending on the individual.