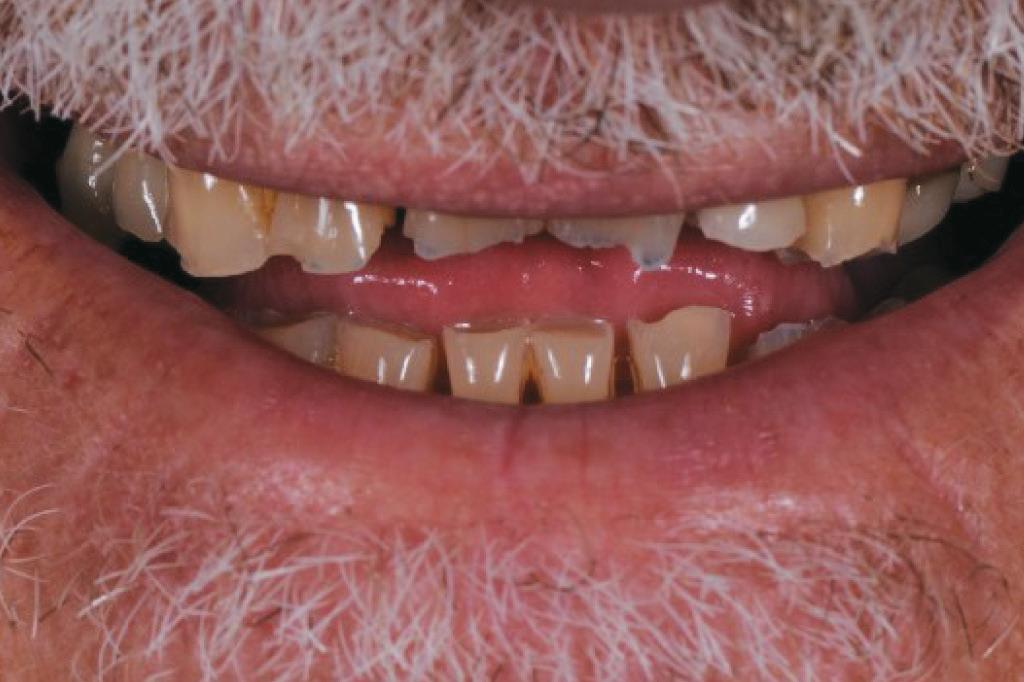
AFTER
Case History
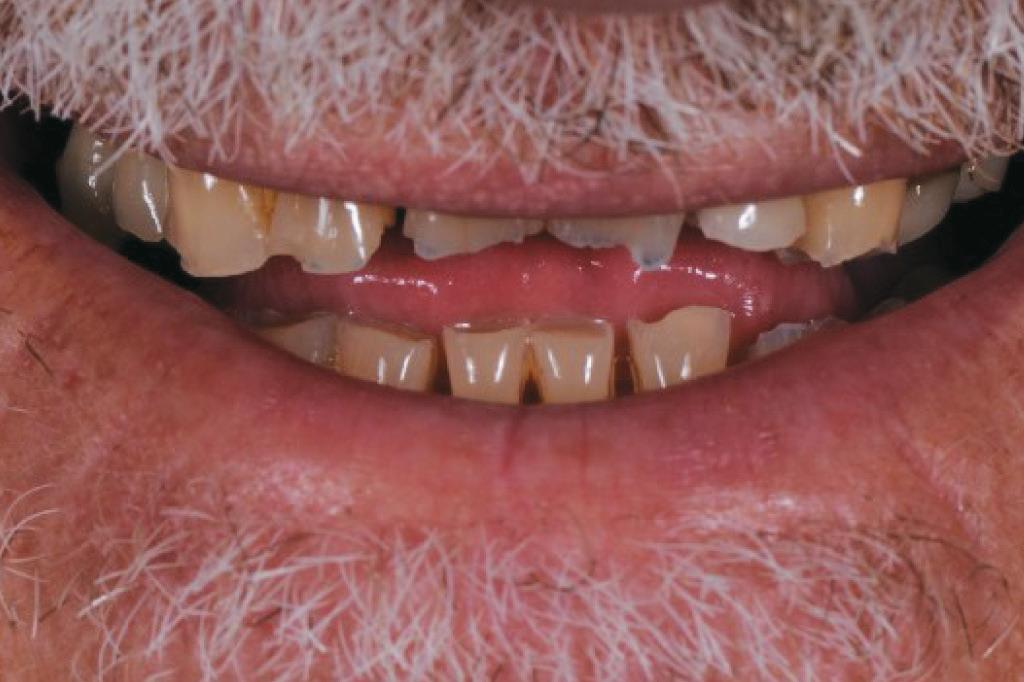
This gentleman presented with pain in his upper left quadrant. He had not been to a Dentist for many years and his dental experience had primarily been to have problematic teeth extracted (Fig. 1). As a result, he no longer had any of his molar teeth, but had been functioning well with his remaining premolar occlusion.
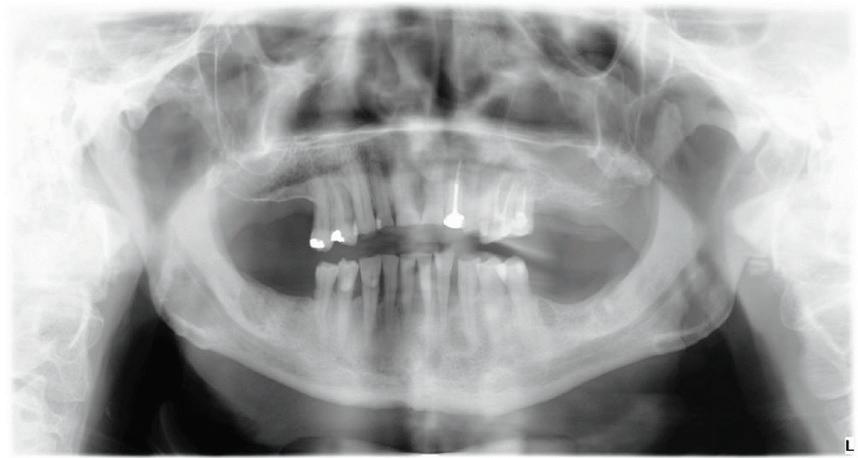
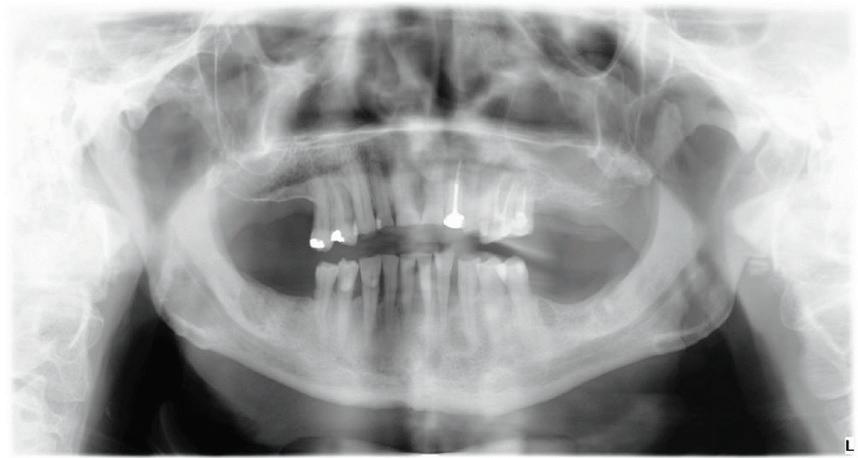
After his examination appointment, it was clear that the two premolars in the upper left quadrant had significant apical pathology and could not be predictably treated. His remaining dentition showed generalised attrition subsequent to dental erosion from gastric reflux, and his lower anteriors showed recession and some loss of periodontal support (Figs. 2, 3).
After discussion with the patient, he decided that he did not want to lose any more teeth and wear removable prosthetics, but he did not have the ability to afford extensive crown and bridgework to restore his dentition. He also requested that his existing (relatively new) crown on the upper left lateral incisor (#22) be retained. With these treatment constraints, it was decided to restore him to a Shortened dental arch1, 2 and that his treatment would occur in phases.
The first phase was to return the lost tooth structure, occlusion, vertical dimension and aesthetics with the composite buildups. Phase two was to remove the two premolars (#24 and #25) and allow soft tissue healing. Phase three was to place a dental implant in the site of the #25 and restore it with a 2-unit cantilever bridge.

BEFORE
Treatment Procedure
The classical approach to a full mouth rehabilitation requires that study casts of the case be mounted onto an articulator in Centric Relation. The casts would then be equilibrated and a wax-up performed to recreate the tooth forms and occlusal relationship. This information would then be used to fabricate provisional restorations and guide the laboratory stages for the crown and bridgework to follow.
In the present case, as all of the molars were missing and direct composites were to be used instead of crowns, the author proceeded by first restoring the maxillary anterior teeth. These anterior tooth forms were shaped according to aesthetically determined length and form, by free-hand bonding procedures. Once these teeth were restored, it was possible to then determine the appropriate length and form of the lower incisor teeth, to support the new vertical dimension. Finally, with all of the anterior teeth restored, the remaining premolar teeth were then restored to create stable occlusal contacts, at this new vertical dimension. The final phase of treatment would then be to surgically remove the infected upper left premolars and place the implant and cantilever bridge.
The techniques used to restore the dentition are described below.
The teeth were cleaned of plaque and the chipped and unsupported enamel was removed (Figs. 4, 5). Fine bevels were placed to facilitate composite adhesion.
Small, 1/2 round bur undercuts were placed, and all of the exposed
dentine (and the old crown) were micro-etched with the Rondoflex 360 sandblaster, using 27um particles (Figs. 6, 7).
The maxillary anteriors were then isolated one at a time, and a selective etch adhesive protocol was used with the adhesive OptiBond™ Universal by KerrTM (Fig. 8).






Flowable composite (HerculiteTM Ultra Flow, Shade A2) was then applied to the dentine surface and cured, to complete the adhesion process (Fig. 9). The tooth was then restored with a new nanohybrid composite material, HarmonizeTM by KerrTM



Each buildup was completed by firstly adapting a mylar matrix strip to the palatal and interproximal surfaces and a thin layer of A2E (Enamel) shaded composite was then applied and cured (Fig. 10). The matrix was then removed and the centre of the tooth was then built up with A3D (Dentine) shaded composite – to the approximate volume that natural dentine would occupy (Fig. 11).
Finally, a superficial layer of enamel shaded composite (A2E) was applied (Fig.12), shaped and cured, before reshaping of the tooth was performed with OptidiscTM system (Fig. 13).
Restoring the Central Incisor (#11) first, enabled the Author to establish the midline position and correct length and form for the teeth. The remaining teeth were then built up one at a time, using the initial buildup of #11 as a guide (Figs. 14, 15).


Once the maxillary buildups were completed, the mandibular
1 3
4 5 6 7 8 9
10 11 12
teeth were then restored with the same tooth-by-tooth freehand approach, to establish the new vertical dimension and to allow the posterior teeth to be built into a stable occlusion (Figs. 16, 17).
After all of the teeth were restored (except for the upper left premolars which were to be extracted), final shaping and polishing procedures were instigated using OptidiscTM, IdentoflexTM and HiLuster PLUS polishing systems (Fig. 18).
Natural colours and a beautiful, life-like surface polish were produced with the multilayered application of this nanocomposite – HarmonizeTM (Fig. 19).
Importantly, the stability of the occlusion was re-established with creation of occlusal contacts on each tooth, and the re-introduction of canine and incisal guidance, to control lateral and protrusive forces (Figs. 20, 21, 22, 23).
Treatment Outcome
The functional and aesthetic results of the treatment are evident in the post-treatment photographs. This gentleman was able to have a full mouth rehabilitation completed in composite resin, achieving the desired improvements in the appearance of his smile, and the return of stability to his dentition, all within a cost that he could afford, by using direct restorative procedures instead of conventional crown and bridgework. This treatment was made
References:
possible by the use of the universal nanocomposite, HarmonizeTM by Kerr™.
Conclusions
The important physical properties of a restorative composite are the result of the filler particle type, size and distribution within the resin matrix of the material. Nanocomposite technology has allowed the development of restorative composites that contain very small filler particles (which allow excellent polish) while at the same time still affording high filler loading (which creates good physical properties). As a result, nanocomposite technology has allowed the creation of restorative composites with universal applications, such that the same material can be used for aesthetic (anterior) and functional (posterior) applications in the mouth.
The present case demonstrated the use of Kerr’s new nanohybrid composite HarmonizeTM, in anterior and posterior applications, for a full mouth rehabilitation. The immediate outcome of the case is excellent, and shows that a careful, multilayered application of nanocomposite can achieve an excellent clinical outcome. However, it must be realised that the longer term wear resistance of composite materials is not equivalent to gold and porcelain, and so a treatment such as the one described must be considered at best to be an “interim” treatment option, designed to function well in the short to mid term. In order to extend the serviceability of a composite rehabilitation, the author would recommend that patients be issued with a night splint for regular use.













1. Kayser A. Shortened dental arch: a therapeutic concept in reduced dentitions and certain high risk groups. Int J Periodontics Restorative Dent. 1989;9:426-49.
2. Armellini D, von Fraunhofer J. The shortened dental arch: a review of the literature. 2004;92:531-5.
DISCLAIMER: The opinions expressed in this (article) are those of Dr. Mandikos. Kerr is a medical device manufacturer and does not dispense medical advice. Clinicians should use their own professional judgement in treating their patients. Dr. Mandikos is a paid consultant of Kerr Corporation.
13 14 18 19 20 21 22 23 15 16 17

 Dr Michael N. Mandikos BDSc (Hons), MS, Cert Pros, FRACDS
Dr Michael N. Mandikos BDSc (Hons), MS, Cert Pros, FRACDS