
19 minute read
Ethics
Bringing reconciliation
into healthcare
By Bob Parke
In the last weeks and days, we have been made aware of the painful and tragic truth of what has happened at residential schools. We were informed of the finding of 215 unmarked graves in Kamloops and more recently about the 751 unmarked graves found at the Marieval Residential School in Saskatchewan. In the weeks and months to come the locations of more unmarked graves will be identified. We grieve for the multiple losses experienced by members of our Indigenous communities. Losses not only of precious lives but of language and culture. For survivors of the residential schools there is a trauma that is part of their lives and the lives of generations that follow. Changing laws to ensure culturally safe practices may seem like a daunting task, but we need to begin speaking with policy makers, teachers of healthcare professionals, healthcare executives, and with members of the law profession in order to make this change. Trauma that has taken a toll on their physical and emotional well-being.
As healthcare professionals it may feel overwhelming thinking about what to do in response to the history and tragedies experienced by our Indigenous peoples. I believe that most of us in healthcare want to make a difference to the healing and reconciliation that is so necessary. The best starting point is to review the recommendations of the Truth and Reconciliation Commission. In the “Call to Action” there are recommendations that address “health.” We can become familiar with those recommendations and share them with those in our spheres of influence. If in partnership with Indigenous people we meaningfully begin addressing the recommendations of the Truth and Reconciliation Commission, we will be healers who provide safe and inclusive care that is culturally safe for all involved.
In this context we are rightfully being asked to participate in fulfilling reconciliation with our Indigenous peoples, acknowledge racism, and to meaningfully integrate diversity and inclusion into healthcare. These are positive and important goals to strive towards if we want to provide a just health-care system and ensure that our practices are culturally safe. To be more inclusive and address injustices, our health laws (which affect our practice) need to adapt to current knowledge and societal changes: Specifically, Ontario’s Health Care Consent
Act, (HCCA) which has remained stagnate since its implementation in the 1990s. A law built on the foundation of white, Anglo-European philosophers who placed a high value on autonomy. While the HCCA upholds the value of autonomy, it does not reflect the reality of most people’s lived experience where decisions are made in relationship to others.
Although respecting the dignity and worth of each person is important, our teaching and application of health laws has created situations in which culturally unsafe practices take place. Sometimes, on an individual level or in an ad hoc way, we have found ways to accommodate cultural practices, such as allowing a capable person to defer decision making to another. Doing this may satisfy the immediate needs of a patient and/or family, though those who have strong feelings about the value of autonomy and follow a literal interpretation of the law will challenge that action.
Changing laws to ensure culturally safe practices may seem like a daunting task, but we need to begin speaking with policy makers, teachers of healthcare professionals, healthcare executives, and with members of the law profession in order to make this change. We need to make the point that cultural safety must be a priority when we create policies, teach approaches to healthcare, enforce standards of practice within the workplace, and when legal advice and actions are required. As we seek to influence policies, curriculum, and laws, we need to ensure that the right people and voices are at these tables. I am always reminded of the words from members of the disabled community: “If you are not at the table, you are on the menu.” Literally and metaphorically, we need to look around the table to see who is and who is not present. We also need to ensure that the voices we need to hear are not only present but being listened to throughout the process of the work being done.
While we wait for new laws to be developed and/or for amendments to current laws, we need to advocate for a nuanced response to health laws so that culturally safe practices are integrated into our present health-care practice. To achieve this, we need to find ways to accommodate culturally safe practice even if it departs from our training in the HCCA. There are several areas of the HCCA which could be critiqued, beginning with the concept of who makes health-care decisions. The law is predicated on a view of autonomous capable decision-makers. Yet for many people, decision making is a collective or relational process taking into consideration the family and community context of the person. When one participates in advance care planning, the impact on the person and those in their community (i.e., anyone who might narrowly or broadly be defined as family by the person) are often considered. Also, in the direct process of an immediate treatment decision, the person may want to include others who are not family but who they trust to provide support and advocacy, especially in situations where a person may feel vulnerable due to race, power imbalances, and prejudices.
Another specific domain of the HCCA which presents a barrier to culturally safe practice and where accommodation should be made is in the hierarchy of substitute decision-makers (HCCA, sec.20). As it is presently written, taught, and practiced, it serves as a barrier to cultural safety. Recently, I had the pleasure of completing learning modules from Virtual Hospice on the topic of cultural safety with our First Nations peoples in the context of palliative care. This is a learning opportunity I highly recommend. In working through the modules, it reinforced my belief that health laws with a hierarchy of decision-makers do not include opportunities for expanded participation in decision making for people like Chiefs, Elders, Healers, and others who may be wanted on their health care journey. First Nations peoples have historically encountered and continue to encounter racism, prejudice, and physically unsafe as well as culturally unsafe care. Because of these historical injustices, allowing extended participation in care and decision making should be given high priority by health-care staff when working with Indigenous peoples.
Health-care professionals have been taught that we should work with the patient if capable and only with the substitute decision-makers indicated on a hierarchy when the person is incapable. Consequently, while we are compliant with the law, we may often be participating in a culturally unsafe practice. For health-care practitioners who aspire to culturally sensitive practice, this can be extremely uncomfortable and unsatisfying. For persons needing care, we are putting them into a very vulnerable situation. Recognizing that while I am making some suggestions for changes to practice, I accept that it is and ought to be the person who decides what is culturally safe for them. If we, as healthcare providers, can move beyond the HCCA’s hierarchy of decision-makers and engage differently with those we care for, then we can provide quality care that is safe and satisfying for all.
We like to use catch phrases like “patient or person-centred care” but is it patient-centred care if current health laws present barriers to our ability to provide culturally safe practices? In the spirit of reconciliation and to address racial injustice in healthcare, I hope that we can be advocates to amend current health laws to create environments where cultural safety has a greater likelihood of being experienced. If laws cannot easily be changed, then can we nuance our teaching and interpretation of our health laws to be culturally safe and inclusive until they are? ■ H
Bob Parke is a bioethicist whose practice has a focus on palliative care. A practice which is inclusive of the person’s culture, tradition and abilities, in order to provide optimal physical, spiritual, social and psychological care.
APPLY NOW

Rehabilitation Science Graduate Programs
Areas of Research
Best practice and knowledge translation Childhood Disability (and Participation) Functional health with aging or chronic disease Neuromusculoskeletal function and mobility
Work, Ability, and Participation Orthopaedic Manipulative Physical Therapy (OMPT) Full-time, Part-time, and online study options!
healthsci.mcmaster.ca/srs-rehabsci

By Celine Zadorsky
It’s a discovery that has been more than ten years in the making, the use of a human protein to potentially treat patients with sepsis.
Lawson Scientist Dr. Qingping Feng noticed that a human protein called annexin A5 showed positive results in mouse models with sepsis back in 2007. Fast forward to now 2021, 14 years later, and this discovery could very well not only be the first ever viable treatment for sepsis patients, but also for severe COVID-19 patients who develop sepsis. “With COVID initially, it is in the airway and then in the lungs, then from there the inflammatory response in fact spreads to the whole body,” says Feng, Ivey Chair in Molecular Technology at Schulich Medicine & Dentistry. “Sepsis causes major organ dysfunction and carries a high mortality unfortunately.”
It has become a challenging issue for Intensive Care Physician at London Health Sciences Centre, Dr. Claudio Martin, who can only do so much to treat severe COVID-19 patients that develop sepsis. “What we have seen is a very primary severe respiratory failure to the lungs for severe COVID patients,” says Dr. Martin, Associate Scientist at Lawson. “We have used steroids and other treatments to try to help, but the results and effects aren’t dramatic and we see patients who have these treatments and still progress and end up in the ICU.”
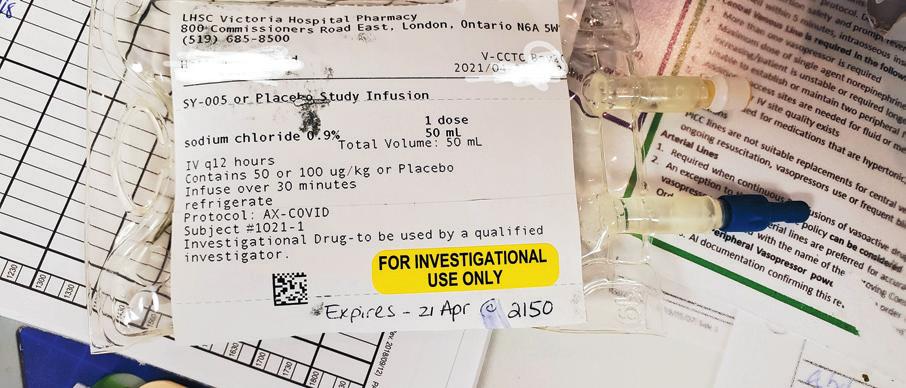
However, Dr. Feng and his team has found in a pre-clinical study, that annexin A5 can inhibit inflammation and improve organ function and survival when treating sepsis in animal models. Another potentially deadly situation for COVID-19 patients is cell death and blood clots, specifically near the lungs. The good news is that the research team also believes the annexin A5 drug will prevent these complications through the drugs anti-apoptotic (cell death prevention) and anti-coagulant (blood clot prevention) properties. The research team has launched a clinical trial with critically ill COVID-19 patients, using a manufactured form of annexin A5 which was manufactured through a joint partnership with Yabao Pharmaceutical Co, based in China. The goal is to enroll a total of 60 patients for the clinical trial, and enrollment has already begun. “Patients are receiving standard treatment and then those enrolled will also receive the annexin,” says Dr. Martin. “It’s a placebo blinded clinical trial, so patients will either get a lower dose of annexin, a higher dose of annexin, or a placebo.”
If the clinical trial shows promising results, Dr. Feng says the team plans on expanding into a larger phase three trial with not just COVID-19 patients with sepsis, but other sepsis patients as well. “If in fact Annexin A5 is shown to be effective in sepsis, then this will be a huge benefit for society because sepsis is the leading cause of death worldwide.” ■ H
Celine Zadorsky is a Communications Consultant at Lawson Health Research Institute.
Canadian first: The Department of Surgery implants a new biological aortic prosthesis
The Montreal Heart Institute’s (MHI) surgery department has implanted a new biological aortic prosthesis in a patient, a Canadian first. This cutting-edge medical device reduces the time required for surgery and the risk of complications; thus, patients enjoy a better quality of life.
“Patients requiring such surgery are usually under 65 years of age,” says Dr. Philippe Demers, a cardiac surgeon at the MHI. “This new biological prosthesis allows these younger and active patients to maintain their lifestyle, as it does not require them to take anticoagulant medication.”
AORTIC VALVE DISEASES
There are four chambers in the heart, each with a valve to control blood flow. Of these, the aortic valve controls the flow of blood from the left ventricle to the main artery of the body, the aorta. This valve opens to carry oxygen-rich blood from the heart to the rest of the body and closes to prevent it from flowing backwards and mixing with oxygen-poor blood.
Aortic valve diseases occur when the valve in the aorta can no longer open or close properly. Usually caused by a birth defect, infective endocarditis (the inner layers of the heart), aging, or rheumatic fever in childhood, they can lead to heart failure or hypertrophy of the heart, which is an increase in the size of the heart.
THE BENTALL PROCEDURE
The treatment of aortic valve diseases can be done with medications or medical procedures. Among these, the Bentall procedure is a complex and technical cardiac surgery involving the replacement of the aortic valve and aortic root with a mechanical or biological valve and tube.
COVID-19 and its unintended consequences on cancer care
By Jaimie Roebuck
There is no pause button for cancer. We have no ability to postpone, hold or reschedule it for a later date. But COVID-19 forced an abrupt and immediate halt to crucial cancer screening, tests and treatments. With the gradual re-opening of health services, we must prioritize resuming cancer care, as further delays and interruptions could ignite another public health crisis.
A survey commissioned in 2020 by the Canadian Cancer Survivor Network revealed that more than half (54 per cent) of Canadian cancer patients, caregivers and those awaiting confirmation of a cancer diagnosis had appointments, tests and treatments postponed and cancelled. Seventy-four per cent said these delays have had a major impact on their mental and emotional health.
“I’m concerned that we’re going to lose the great advances we’ve made in being able to catch cancers very early, or even when they’re pre-cancers. We’re going to lose some of that benefit and may experience what many are referring to as a tsunami of cancer, where people are diagnosed at a later stage than they would have been,” explains Dr. Aisha Lofters, Chair in Implementation Science at The Peter Gilgan Centre for Women’s Cancers at Women’s College Hospital. “There may be significant consequences that trickle down from these delays.”
When the pandemic first began, little was known about COVID-19 and non-essential services, including routine cancer screenings, were put on hold. As restrictions begin to lift, these types of health services must be prioritized. With strict infection prevention and control protocols implemented in healthcare institutions and organizations across the country, the likelihood of virus transmission during a routine cancer screening appointment is very low. It is imperative that people feel comfortable and confident to connect with their primary care providers for screening, testing and treatment appointments.
“It’s our responsibility as physicians to continue reinforcing that it’s safe to come into the hospital or visit a doctor’s office, and then make sure that it truly is safe,” reiterates Dr. Lofters. “We need to resume cancer screening to reap the benefits of catching cancers and pre-cancers early before they cause significant harm. Although we have rightly put a great deal of focus on COVID-19 over the past year, other health problems have not been put on pause.”
A year later, COVID-19 has proved its endurance and longevity, triggering safety concerns around in-person doctor visits. These fears are valid and important, but one of the biggest factors to surviving cancer is early detection. Even a small delay can impact prognosis. As the pandemic persists and health services gradually resume, it is critical that Canadians do not hold off on routine screening appointments.
Health care needs, specifically cancer concerns, should not be put aside because of COVID-19 –they are more important now than ever. Cancer patients who experienced a cancellation, disruption or delay with imaging, biopsies, surgery, radiation or chemotherapy must re-book those appointments. Further delays could lead to severe health implications – the longer cancer goes undetected or untreated, the more advanced and difficult it becomes to manage.
According to The Canadian Cancer Society, cancer is the leading cause of death in our country and is responsible for 30 per cent of all deaths. Based on 2020 estimates, lung, breast, colorectal and prostate cancer are the most commonly diagnosed types of cancer in Canada, accounting for just under half (48 per cent) of all new cancer cases. But screening can save lives and early detection can increase survival rates. It is important to note that five to 10 per cent of cancers are inherited. Whether or not someone has a family history of this disease, it is essential to reduce risk by finding cancer early through routine screening.
COVID-19 triggered a seismic shift, disrupting the way healthcare services are provided in Canada and around the world. But for now, our healthcare system is staying open, and we have to resume proactive and reactive cancer care. Public health messaging must continue to amplify that patient safety during the pandemic is top of mind. Canadians need to feel reassured that coming in for a screening or treatment appointment will not put them in jeopardy, rather, the greater threat to their health would be to wait.
To avoid another major public health crisis, it is crucial that previously postponed or cancelled screening and treatment appointments resume – cancer care for Canadians can no longer come at the cost of COVID-19. ■ H
On May 31, 2021, Dr. Philippe Demers performed the first Canadian implantation of Edwards’ KONECT Resilia biological aortic prosthesis, approved by Health Canada earlier on December 18. This medical device is the first to be ready to use, meaning that the tube and valve are already assembled, thus reducing the time and risk associated with surgery.
“Since its inception, the Montreal Heart Institute has strived for excellence in specialized patient care,” explains Mélanie La Couture, President and CEO of the MHI. “With that in mind, we strive to make the latest advances in cardiovascular medicine available to our patients.” ■ H

Innovative aging and brain health solutions
by frontline health workers and researchers
By Arielle Ricketts
CABHI recently selected 24 projects to participate in Spark-ON and SparkCU, subsidiaries of its Spark Program which supports the development of grassroots solutions by frontline healthcare workers and researchers to solve real-world critical care challenges.
The Centre for Aging + Brain Health Innovation (CABHI) launched its Spark-ON program just months after COVID-19 was declared a global pandemic. Through Spark-ON, CABHI invited frontline care workers, clinical managers, and clinical researchers to submit an innovative, COVID-19-related idea aimed at improving the lives of older adults, persons with dementia, and their care partners. The program was part of CABHI’s rapid response to the pandemic and acknowledged frontline care workers as uniquely positioned to address the needs of Ontario’s older adult population during the current health crisis.
The Spark-ON program is designed to address the current healthcare needs of older adults. The Spark-CU program was launched to help Ontario students – Canada’s future innovators – scale their innovative aging and brain health solutions into businesses.
Through Spark-ON and Spark-CU, CABHI will invest close to $1 million in support of these 24 projects, which range from water intake initiatives to intergenerational learning and digital literacy skills development for older adults.
While unique, each project shares a common goal: improving the quality of life for older adults, people living with dementia, and their caregivers during the pandemic and beyond.
We’ve listed some of the 24 innovations below:
SPARK-ON: PANDEMIC RESPONSE
Virtual micro-credentialing for unregulated care providers Project Lead: Faith Boutcher


Expert care for elderly skin

Introducing the TENA ProSkin™ 3-Step Skin Health Solution



Better care is better for everyone.
TENA® understands that keeping skin dry and clean can be challenging. This is why we have introduced TENA ProSkin™ – a 3-Step Skin Health Solution to help reduce the risk of skin issues. TENA ProSkin™, a new approach to skin health: keep it dry, keep it clean and keep it protected. www.tenaprofessionals.ca | 1-800-510-8023


Organization: Baycrest (Toronto, ON)
The COVID-19 pandemic has revealed the growing need for education addressing the healthcare of older adults. This project will refine a 12week part-time micro-credentialed certificate designed to teach the basics of geriatric care to unregulated healthcare providers (i.e., healthcare aides, private companions), and assess the benefits and educational outcomes of a virtual 12-week certificate program. The course will be delivered through an established virtual learning platform (ALPHA), which uses a simulated educational environment to foster effective, interactive, and motivated learning. The certificate will blend individual and group work, simulation, and case-based learning, and will offer participants a forum for live discussions with experts. Remote calendar application training for older adults with memory impairment Project Lead: Brandon Vasquez Organization: Baycrest (Toronto, ON)
Memory difficulties are common in older adults and can be worsened by a variety of neurological conditions such as stroke, cardiac arrest, or mild cognitive impairment. Memory impairment can limit independence and social connectedness and increase the potential for loneliness. Baycrest’s Memory Link program involves training memory-impaired individuals to use their smartphone as an external memory aide. The one-of-a-kind training method, developed at Baycrest, leads to improved day-to-day memory, independent functioning, and quality of life.

Continued on page 28

What is Home Care?


Home care is about trust. It is feeling comfortable with a provider Bayshore’s home care services are extensive and varied, depending on your needs. They Caregivers wear PPE and follow clinical guidelines to ensure errands to nursing, respite care, wound care, your safety Home care is personalized for you, so you can experience the best in your day-to-day living – in your own home. Support is just a phone call away. 1.877.289.3997



