51 minute read
Special focus: Infection control


Infection Control




By Jennifer Happe
The World Health Organization identified vaccine hesitancy, the reluctance or refusal to vaccinate despite the availability of vaccines, as one of the top 10 threats to global health in 2019. Vaccine uptake is essential to safeguard human lives and curb the socio-economic impact of the current COVID-19 pandemic. However, Statistics Canada reports that only 57.5 per cent of Canadians are very likely to get vaccinated against COVID-19. Healthcare workers are among those reluctant to be vaccinated. Chief concerns include lack of confidence in vaccine safety, concern about risks and side effects of the vaccine and mistrust of the public health care system. Jennifer Happe

The Government of Canada launched the COVID-19 Immunity Task Force (CITF) to track COVID-19 among Canadians and priority sub-groups including healthcare workers. While CITF studies are still ongoing, data from the United States of America and the United Kingdom suggest the risk of COVID-19 among healthcare workers is three times higher than the general population. Protecting the health and wellness of healthcare workers is vital to maintain a functioning healthcare system. Overcoming vaccine hesitancy is an important strategy to ensure healthcare worker safety.
One method to overcome vaccine hesitancy is mandating vaccination, either by government regulation or through terms of employment. Mandating COVID-19 vaccination is controversial and subject to challenge under the Canadian Charter of Rights and Freedoms. Alternately, vaccine confidence can be fostered with education and training using scientific evidence on vaccine efficacy, safety, its role in COVID-19 prevention and the government evaluation and approval process. Education efforts should focus on exposing and explaining misinformation and coaching workers on how to identify misinformation. Healthcare workers themselves have a responsibility to seek accurate information from reliable sources for a fulsome understanding of COVID-19 vaccines. For more information on Canada’s COVID-19 vaccine strategy and vaccine efficacy and safety, visit www.canada.ca. ■ H
Jennifer Happe, M.Sc. is the Director, Infection Prevention and Control Canada.
Can light therapy be used to treat early stages of COVID-19?
By Samantha Sexton
Ateam of researchers from Sunnybrook Research Institute and University Health Network is investigating whether a form of light therapy, commonly used to eliminate harmful bacteria from surgical patients, can also be used to destroy COVID-19.
“Methylene blue photodisinfection (PDT) is a highly effective and safe treatment that uses the local application of a non-toxic dye, activated by light, to destroy harmful bacteria and viruses,” says Dr. Cari Whyne, one of the principal investigators of the study and research director of the Holland Bone and Joint Research Program at Sunnybrook Research Institute. “PDT is safe, low-cost and minimally invasive, making it an exciting option to potentially reduce the spread of SARS-CoV-2, the virus that causes COVID-19.”
The trial, funded in part by the Ontario government’s COVID-19 Rapid Research Fund, is aiming to evaluate the potential of the light therapy in people who have recently tested positive for COVID-19. The research team is working with Canadian company, Ondine Biomedical, who developed the Steriwave™ photodisinfection technology used in the study.
During a study visit, participants have the inside of the front part of their nose swabbed for a baseline measure of virus particles present. The treatment is performed by applying the methylene blue photosensitizer to the inside of the nostrils and placing a light source for a few minutes. Following this, a second swab of the nose is taken to measure how effectively the light therapy has inactivated the virus.
“There’s still so much to know about coronavirus, so why not help learn more by participating in a safe research study? I just want to help defeat this pandemic,” said one participant in the study. Researchers are investigating whether a form of light therapy, commonly used to eliminate harmful bacteria from surgical patients, can also be used to destroy COVID-19.

In addition to quantifying the amount of virus particles present after photodisinfection, the researchers have also been conducting pre-clinical research to establish the best amounts of photosensitizer and light doses necessary to kill SARS-CoV-2.
Although the study is still in its early stages, the research team sees possible implications for the light therapy, if it proves successful. “We’re excited about the potential of photodisinfection from a few standpoints — preventatively for people visiting a high-risk area or for those who have recently been exposed or are at an early stage of infection,” says Dr. Brian Wilson, co-principal investigator of the study and a senior scientist at University Health Network, Toronto. ■ H
Thinking outside the box

to bring families together
By Carrie Stefanson
Shipping containers are used in a variety of ways, from transporting cargo to being stacked to form ultra-modern apartments. Queen’s Park Care Centre is using an upcycled container to connect families with loved ones in care. The container – now known as the Visitor Centre, accommodates private, yet distanced visits for one resident and up to four visitors at a time. The visits follow all public health guidelines. The shipping container is heated and furnished, with separate entrances for residents and families. A plexiglass partition separates the two spaces.
“It’s an innovative way to bring families together,” says Karl Segnoe, whose 92-year-old grandmother lives at Queen’s Park Care Centre. “I have every confidence in the staff to keep my grandmother safe, but I fear social isolation is taking a toll on her well-being. Being able to visit as a family is huge because my grandmother is such an important person in our lives.”
Up until now, families wishing to visit their loved one together could do so via a window visit, where a health care worker brings a resident to a window at a specified time for a visit. The visitor centre is an alternative to window visits, providing a dry, warm place to have a window visit with residents and patients.
Window visits will continue for larger groups, as will virtual visits.
“Residents in long term care and their families have endured so much during the pandemic,” says Dr. Victoria Lee, president and CEO, Fraser Health. “I’m grateful to the Queen’s Park Healthcare Foundation for helping us move this project forward so families can connect with their loved ones in this unique way.”
It was an idea from staff at Queen’s Park Care Centre that prompted Elizabeth Kelly, the executive director of the Queen’s Park Healthcare Foundation, to get the ball rolling.
“We had the space, so I applied for a $25,000 federal grant,” says Kelly. “All of us at Queen’s Park Care Centre are looking forward to the day when COVID-19 is behind us and we can remove the partition in the visitor centre so families can celebrate together and hug each other. The pandemic has taught us that the small things in life are really the most important.” ■ H

The Medco Clean Room on Wheels!
Medco Equipment Inc.’s multi-purpose automatic equipment washer model 64X washes and sanitizes up to twenty wheelchairs of bacteria after one 5 minute wash! The all - purpose washer sanitizes wheelchairs, commode chairs, shower chairs, walkers, carts etc. No special plumbing or electric is needed. Standard button operation. The germ killing detergent and rinse agents front door handle that can be operated from outside and inside the washer. It also includes an emergency stop button (E-Stop), safety door switch (auto off if opened), solid state electronics,
For more information please call 1-800-717-3626 or visit us on the web www.medcoequipment.com. Taimi Norberg visits her grandson, Karl Segnoe, and his room-mates.

The shipping container where residents can visit loved ones.



Dr. Susy Hota is Medical Director, Infection Prevention and Control, University Health Network.

From the front lines of a pandemic
By Dr. Susy Hota
Ithink if you asked most people on the frontline of this pandemic, they would tell you it’s hard to find the time or energy for reflection. It’s been a year since the WHO declared the COVID-19 pandemic and we’re still in the middle of it. It’s tough to accept because every single one of us is longing for life before the mass quarantine, the deaths, the masks, and the end of everything that signified our usual lives.
Every time we hear transmission rates have gone down, hospitals are slightly less full, and the government is considering yet another re-opening plan, we assume we are winning this fight. The public wants to believe we are winning this fight. Here’s the thing though, it’s been a year and the fight keeps changing. We didn’t know anything last March – we were working in the dark, and the stories out of China initially, and then Europe and then New York just across the border, were frightening. In some countries in Europe and in the United States there were concerns over sufficient supply of PPE for the health-care workers and fear that there weren’t enough ventilators for the most seriously ill patients. We were staring into the abyss.
A year later, there was palpable relief when vaccines were produced in a period of time unheard of in modern medicine. It was a light at the end of this long and dark tunnel. However, months later, we are struggling to effectively deploy stuttering supplies of the vaccines, at the same time that new variants are causing great concern. Should our kids be in school? How will we help small businesses? What about those without secure housing? How do we protect our elderly in long-term care? And of course, how do we support our staff, family and friends to continue pushing through the pandemic and adhering to infection control measures?
Like virtually everyone else I know, these are the questions that keep me awake at night. As the medical director of UHN’s Infection Prevention and Control team, I can say we are old pros at managing infectious diseases. The IPAC team has handled countless out-
breaks of respiratory infections, provided guidance as UHN became the national repatriation site for Ebola in 2014 and I can honestly say we handle this stuff well. But none of the previous outbreaks or pandemics hit us this hard, or for this long. Every single day we are dealing with something new and the way we respond has to change in order to keep up. It’s a whole new world.
Every member of our IPAC team has been working day and night to ensure units have what they need to be safe. Surveillance and reporting of COVID-19 cases during and outside of outbreaks, and contact tracing exposed individuals so that isolation and testing can be employed to limit transmission are labour-intensive but critical. These actions don’t respect the boundaries of a work-day – they bleed into nights, weekends and holidays. The IPAC team is also put in the position of having to be the bearer of bad news to their friends and colleagues in order to keep them safe. COVID-19 steals joy in so many ways. For healthcare workers who are awfully tired and still working so hard, it’s a terrible thing to have to tell them, you can’t sit and take a break with a friend. You can’t share a treat that might lift your spirits. Everyone has to be superhuman in their vigilance. I find all of that enormously challenging because I know what toll this pandemic is taking on everyone.
Perhaps the most emotionally difficult part of this experience has been our work with long-term care homes. In the spring of 2020, UHN was assigned responsibility to support IPAC for 13 long term care centres, five retirement homes, and 30 congregate care settings. Having no prior experience with LTC, the experience has been eye-opening on many fronts. There was little in the way of IPAC infrastructure and training in the homes. We had to work on building capacity while guiding them through some of the most challenging outbreaks I have ever seen. It was heartbreaking. It’s intense, 24/7 work that requires constant pivoting. Eventually we are going to have to stop treating this as an emergency and figure out how to live with COVID-19 long term. Perhaps we’re not quite ready for that conversation yet because the pandemic still feels very active and volatile, but we’re going to have to get there. And I know we can. I have watched health-care workers do the most incredible things this past year. Fighting for their patients, even as they fight fear for themselves. Holding hands while people took their last breath. Ensuring loved ones knew they weren’t alone. Working together as a team to inspire each other and get through another really hard day.
This has been the toughest professional challenge of my life, and truthfully I just want it to be over. But even on the bleakest days I am reminded of how lucky I am. I have an incredible husband, beautiful and resilient children, and colleagues I would never trade. There are few silver linings in all this, but I try and remember to be grateful for all of them.
Throughout this experience I have been reminded at almost every turn, of how committed, and professional our health-care workers have been, and continue to be. We will get through to the other side of this, because of them. ■ H
Dr. Susy Hota is Medical Director, Infection Prevention and Control (IPAC), University Health Network.
Quantify Clean!
Visibly clean is no longer good enough. Hospitals need an easy and rapid way to quantify clean. Hygiena's EnSURE™ Touch ATP cleaning verification system quantifies clean in 10 seconds. Learn how to protect patients and employees from harmful bacteria. Call 833-494-4362 or visit www.hygiena.com/quantify-clean-hn

INFECTION CONTROL 2021 It’s time to talk about vaccine hesitancy
By Dr. Samantha Hill
Iand many doctors, have taken to social media and other channels, excited to receive the COVID-19 vaccine. But the other day in the operating room, a very smart and amazing scrub tech told me he doesn’t want to get the vaccine “just yet.” He wants to wait a year, to see if there are any unintended consequences. I was shocked. In fact, I initially thought he was joking. He wasn’t.
It’s a recurring conversation, and while this is surprising to me and many other doctors, it seems that there is a significant portion of the population that feels the same way.
Vaccine hesitancy is not new. In 2019, the World Health Organization called vaccine hesitancy one of the top 10 global health threats. It said that vaccines prevent two to three million deaths yearly, a number that could increase by 1.5 million if worldwide coverage improved. That was before the COVID-19 pandemic swept across the world, devastating countries, economies and families.
With minimal currently accepted therapeutic options available to treat COVID and avert tragic outcomes, an ounce of prevention may be worth far more than a pound of cure. Of course, at present, prevention is all about adhering to public health measures of physical distancing, masking, and practicing proper hand hygiene. But as vaccine supply becomes more widely available, getting as many people as possible vaccinated as rapidly as possible will become an essential part of Ontario’s recovery at all levels.
I’ve written before about the need to approach these conversations with empathy and openness. Polarizing hu-
man beings into pro-vax and anti-vax camps only entrenches people in their positions and gets in the way of conversation, education, mutual understanding and respect. Ultimately, as a society, we uphold body autonomy, free choice and the right to make –for ourselves –medical decisions that affect us. It gets tricky around vaccines of course, because our choices also affect others, their risks and their lives. For many, getting vaccinated is an expected part of our social contract as Canadians; the same contract that stops us at red lights even when we are in a rush and gives us access to schools and health care.
The urgency to vaccinate is rooted in the fact that we need to immunize approximately 65-70 per cent of the population as rapidly as possible to prevent unnecessary loss of life. It’s a massive venture and having individual conversations about risk and benefit is time consuming. It behooves us to examine some of the factors that play into this conversation.
Some of the mistrust surrounding vaccines stems from personal experiences, some of it relates to cultural experiences. Members of Black communities remember the Tuskegee experiment, an unethical 40-year study that left syphilis untreated in black men, who believed they were getting free health care. Members of the Black community continue to experience persistent structural inequities daily in their health-care experiences. Members of our Indigenous communities remember residential schools and regularly experience disrespect toward their cultural medicines and attempts to impose non-Indigenous norms upon them. These are systemic issues reflecting fundamental issues around fairness and equity in health-care delivery. Difficult conversations and visible systemic actions to resolve the inequities must occur. Furthermore, “nothing about us without us” carries exceptional importance here – including community members with lived experiences in the planning and discussions is an essential element.
I’m not the first to raise these ideas and I won’t be the last. The Royal College of Physicians and Surgeons of Canada issued this statement on cultural safety guidance for clinicians during the pandemic. The First Nations Health Authority and Research Ethics BC have developed information on culturally safe and trauma-informed practices for researchers during COVID-19. The Canadian Foundation for Healthcare Improvement has also talked about the new reality of culturally safe practices during COVID.
Ensuring that vaccines are easily available is another key component to ensuring compliance. For many, being required to go to the hospitals charged with administering the COVID vaccines is incredibly inconvenient, required significant transit time and resulting in the loss of a day’s income. Getting vaccinated must be easy and must not impose financial or other burdens.
We must also acknowledge the widespread misinformation surrounding the COVID vaccine. Social media has made it very hard to contain conversations to scientifically grounded fora. According to data collected by Advanced Symbolics Inc., misinformation about the COVID vaccine is spreading among all age groups in Ontario on social media. Doubts and misinformation about how thoroughly the vaccines were tested or the extend of side effects are being shared widely on social media, especially among people under 25 and those between 25 and 34.
The most interesting headlines and the most click-inducing links are ones that evoke emotional responses.
JUST RIGHT.
Microsan®
With just one Microsan‰ Optidose™ provides enough product to cover the hands and ensures proper wet contact time of 20-30 seconds.
Optidose® provides many benefits, including:
Improves patient safety: ensures compliance with hand hygiene best practices No dispenser change: can be used with existing Microsan® dispensers Same price: offered at the same price per cartridge as Microsan Encore® A total solution: compatible with DebMed Hand Hygiene Monitoring System Training included: online toolkit and onsite training for staff
IT’S ABOUT BEST PRACTICE TO IMPROVE PATIENT SAFETY
For more information visit: www.scjp.com Or email: healthcare.ProCA@scj.com





Vaccine hesitancy
Continued from page28
Unfortunately, this is a breeding ground for conspiracy theories and other misinformation. Even in the less extreme headlines, people argue they don’t need the vaccine because they aren’t at risk. They don’t seem to understand the impact of the longterm effects for those who survive COVID and they don’t seem to realize that getting vaccinated will save others’ lives – perhaps even those of loved ones.
Those who worry the vaccine was rolled out too quickly and isn’t safe need to understand that it was rigorously tested – possibly more so than many other vaccines prior to use – and that the ongoing collection of data demonstrates exceptional safety.
And those who worry that their underlying conditions may make it unsafe to get the vaccine need to know that there are very few contraindications and that they should talk to their doctor about their individual circumstances. Their trusted physicians are key in counselling and educating, as well as in administering vaccines.
As we move forward, supply will cease to be the limiting factor; getting vaccines into arms will depend on administration planning and population buy-in. For the sake of us all, I hope we will have already had these conversations with our patients, colleagues and leaders. Vaccination delays will cost lives. We’ve lost too many people already. ■ H

Dr. Samantha Hill
Dr. Samantha Hill is a cardiac surgeon and President of the Ontario Medical Association
MEIKO technology inactivates COVID,
Two of the world’s most highly transmissible and infectious diseases are now subject to better control in the healthcare setting. How? With MEIKO’s TopLine thermal washers-disinfectors. End outdated cleaning practices for bedpans, urinals, suction containers and other patient care devices that can spread diseases such as defence with TopLine. In healthcare settings, most contagious pathogens are found in a patient’s/resident’s immediate surroundings, particularly the toilet and/ or bedpan. One healthcare study found that 26% of all bedpans were coronavirus in ONE WASH CYCLE. They can be used as a stand-alone appliance, or part of a combined (multi-unit) care center. TopLine also resolves the issues found in a 2010 independent study on bedpan washer-disinfectors at Vancouver Coastal Health, led by Dr. Elizabeth Bryce, Regional Medical Director for Infection Control.* • When using TopLine, it’s virtually impossible to choose the wrong cleaning program. Fully automatic settings and descriptions that are easy to understand minimize the chances of operator error. • TopLine’s generously sized wash chamber provides easy access for employees of various heights and sizes, and proper positioning for complete cleaning and disinfection. holders position a wide variety of patient care equipment and devices for cleaning. • Fumbling with loading doors while transporting contaminated equipment is a thing of the past.
TopLine features hands-free doors with a foot pedal for opening. An optional automatic opening feature, is available. • MEIKO machines use short, clear symbols in plain text that can be read fast and understood easily. A The thoughtful design, materials and systems used in MEIKO washer-disinfectors consider the many ways physical, mechanical and operational factors can improve human-machine interaction to help prevent the spread of infection. Protect them, and your patients with safe, reliable cleaning and disinfection technology for patient/ resident and utility rooms, from MEIKO. The clean solution
Research from UHN reveals the fraction of asymptomatic hospital staff exposed to, infected with SARS-Cov-2
Astudy from UHN, Canada’s largest research hospital, reveals the percentage of symptomatic and asymptomatic healthcare workers infected with the novel coronavirus. “A key question that we wanted to answer was ‘how many asymptomatic healthcare workers are unknowingly infectious or have been exposed to the virus,” says Dr. Deepali Kumar, senior author and a clinician investigator at the Toronto General Hospital Research Institute (TGHRI). To answer this question, two tests were used: swab tests, to see if the virus was present and able to spread; and blood antibody tests, to see if past exposure to the virus had occurred.
The results revealed that, of symptom-free staff, around 0.5 per cent had positive swab tests. This means that around one out of every 200 staff were potentially infectious. When staff had symptoms, that number jumped to 3.4 per cent, or around seven out of every 200 individuals. Using blood antibody tests, the research team found that between 1.4 per cent to 3.4 per cent of symptom-free staff tested positive, depending on which antibody test was used.
“This means that somewhere between three and seven staff out of every 200 had been infected with the virus without ever reporting symptoms,” says Dr. Victor Ferreira, the first author of the study and a scientific associate at TGHRI, where he works with Senior Scientist and co-author Dr. Atul Humar.
Symptoms that were considered were fever, headache, new or worsening cough, shortness of breath, sore throat, runny nose, pink eye, diarrhea, loss of sense of smell or muscle aches. “Our findings reaffirm the importance of remaining vigilant in the screening of health care and other front line workers regardless of whether they experience COVID-19-like symptoms,” says Dr. Ferreira. These results come from the first phase of the study called Research Platform to Screen and Protect Healthcare Workers study – or RESPECT for short, which enrolled front-line health care workers at UHN between March
“If you can’t clean it, don’tbuy it.”

1
1 PIDAC: Best Practices for Environmental Cleaning for Prevention and Control of Infections | April 2018

Shouldn’t your furniture be Infection Prevention friendly too?

Data Can Make All the Difference
Each day, your hospital must focus on every single need of every single patient. While you focus on everything, we focus on innovating best-in-class products, technologies and services to support you. Our innovative measurement tools can be used individually or together to create a program that works best for your environment and cater to your hospital’s unique needs.
PURELL SMARTLINK™ Technology tracks, monitors, and provides data-driven solutions to help you focus on caring for your patients. From alerts that help ensure dispensers are always working and never empty to a variety of options that track healthcare worker adherence to hand hygiene protocols and expert clinical support to provide customized coaching – we support you.
To learn at www.GOJOCanada.ca/SMARTLINK
and June 2020. Given the success of the first phase, RESPECT 2.0 has since been initiated and expanded to include broader clinical personnel, research personnel and other workers, such as those in the food industry. “This observational study has important implications for infection control, as well as staff and patient safety. And it could not have been possible without the multidisciplinary team of physicians, researchers, nurses and other allied health professionals that contributed. Thank you to everyone at TeamUHN that made this possible,” says Dr. Brad Wouters, UHN’s EVP of Science and Research. The study was funded by the Mount Sinai Hospital and University Health Network Academic Medical Organization, the Ontario Institute for Cancer Research, the Government of Ontario, and the Toronto General & Western Hospital Foundation. T Pugh is a Tier 2 Canada Research Chair (CRC); M Cybulsky and B Wouters are Tier 1 CRCs. ■ H

Photo: UHN StRIDe Team Regardless of whether individuals have COVID-19 symptoms, everyone entering UHN is required to wear a medical mask, which is provided during entrance screening—a policy that aims to help prevent asymptomatic spread
This article was provided by University Health Network.
Your Leadership. Our Expertise.

2
GOJOCanada.ca
1. Nielsen Sales 52wk ending 01/04/20: PURELL® Hand Sanitizer
INFECTION CONTROL 2021 Most instructions for inserting COVID-19 nasopharyngeal swabs don’t go deep enough, research finds
By Crystal Mackay
There are wide discrepancies in the instructions for how deep the nasopharyngeal swabs used to test for COVID-19 are to be inserted up Canadian noses, new research from Western University and Lawson Health Research Institute has found.
As an otolaryngologist Dr. Leigh Sowerby is an expert in the anatomy of the head, neck and inside of the nose. Using that expertise, he and his colleagues examined the COVID-19 testing instructions provided by provincial and territorial authorities and found wide variations. They reported their findings in the Journal of Otolaryngology – Head & Neck Surgery.
“As a surgeon who works inside the nose all the time, I was surprised to find that most of the instructions in Canada aren’t effective to reach the nasopharynx; they just don’t go deep enough into the nasal cavity,” says Sowerby, an associate professor at Western’s Schulich School of Medicine & Dentistry and Scientist at Lawson Health Research Institute.
To perform a nasopharyngeal test, the swab must be inserted far enough into the nasal cavity to reach the nasopharynx, the upper part of the pharynx at the top of the throat behind the nose. Samples from the nasopharynx have been shown to be the most sensitive for COVID-19 testing, and are considered the gold standard.

However, less than a quarter of provincial and territorial public health instructions tell practitioners to insert the swab deep enough to reach the nasopharynx, Sowerby says.
The research found that six provinces and territories, including the Northwest Territories, Nunavut, Ontario, Saskatchewan, Prince Edward Island and Alberta, recommended that the swab be inserted to a depth of four centimetres, or half the distance from nostril to ear. This depth only reaches the mid-nasal cavity, not the nasopharynx, he adds.
British Columbia and Manitoba recommended a seven-centimetre depth of insertion, which is still not enough – only reaching the posterior nasal cavity but not the nasopharynx.
In Nova Scotia and Newfoundland, the recommended depth of insertion was two-thirds of the distance from nostril to ear, which would effectively reach the nasopharynx, as would following the instructions in New Brunswick and Yukon to insert the swab from nostril to external ear canal.
“If we are doing what we are calling a nasopharyngeal swab, the technique for that should be standardized; there is no reason why there should be so much variability,” Sowerby says. “The take-home message is that if we want the most accurate test results, there is room for improvement in the test instructions. Otolaryngologists have a role to play, as we can provide a great service by actively engaging with our local and regional health authorities to train on proper technique and anatomical knowledge.” ■ H


NEXT EDITION – APRIL 2021
Hospital News is proud to be publishing the Annual Pre-Show eHealth Conference Supplement in our April edition. Focus will be on eHealth, Mobile Health, Virtual Care and details about the virtual conference, including speakers and event details. Special advertising discounts available for this special eHealth edition!
To Advertise Contact: Denise Hodgson 905.532.2600 x2237 denise@hospitalnews.com
OFFICIAL MEDIA SPONSOR
Additional Distribution!
April Issue emailed direct to all delegates at eHealth Virtual Conference!







Dr. Heyne using the methylene blue solution on a mask in her lab.
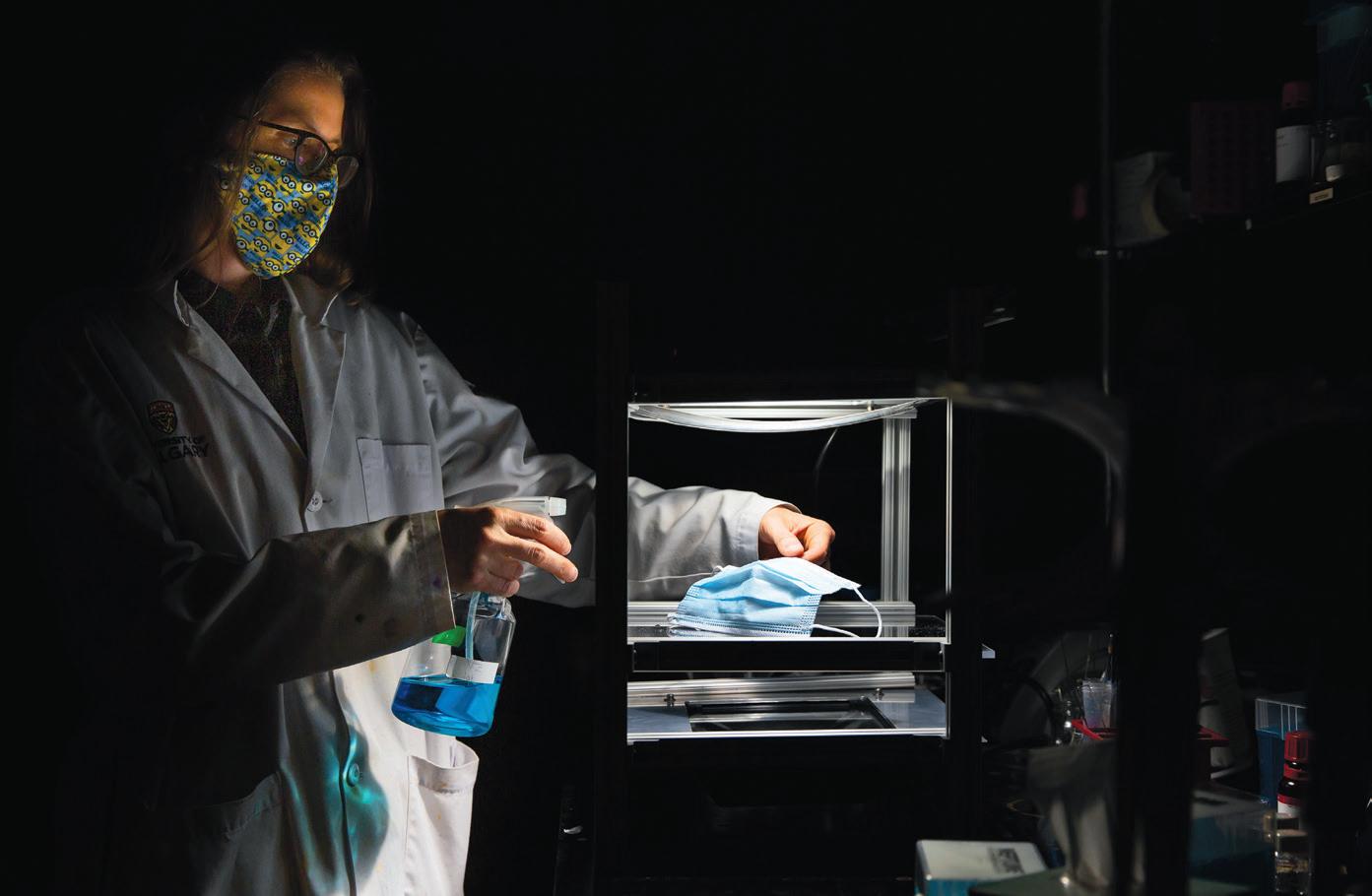
Photo credit: Riley Brandt/University of Calgary.
Light kills. SARS-CoV-2, that is.
By Belinda Heyne and Lacey Duffy
Anew, safe, and affordable SARS-CoV-2 decontamination method has been identified and is now being commercially tested and developed for masks and Personal Protective Equipment (PPE). This method works perpetually, even while a mask is being worn.
This novel decontamination method relies solely on protective dyes, indoor light, and ever-present oxygen.
The DeMaND study co-authored by 52 researchers worldwide with support from 13 labs and institutions, including the WHO, AHS, CDC, University of Calgary, University of Alberta, Québec-Université Laval, Stanford, and the University of Washington, was recently pre-published. For the first time, Methylene Blue (MB), a Light-Activated Dye was shown to inactivate SARS-CoV-2 on a variety of commonly used masks while keeping their integrity.
This Light-Activated Dye, when applied to coronavirus-infected masks, consistently decontaminated SARSCoV-2 from the masks within 30 minutes and in many cases in less than five minutes.
Further, masks pre-treated with Methylene Blue provided ongoing decontamination once exposed to SARS-CoV-2.
THE SCIENCE: DYE, LIGHT, AND OXYGEN
a hundred years in treatment of cancer, skin and eye conditions, research confirmed the hypothesis of Dr. James Chen that Light-Activated Dyes could destroy SARS-CoV-2 on masks and other PPE.
Methylene Blue (MB), and other Light-Activated Dyes, have the unique molecular ability to transfer energy from surrounding indoor light to nearby oxygen, briefly exciting such to the state of singlet oxygen. Singlet oxygen is well-known for its ability to destroy pathogens, including viruses, bacteria, and fungi. The beauty of singlet oxygen is it either reacts with pathogens around it or it reverts back to oxygen. All of this happens within milliseconds.
When singlet oxygen comes into contact with coronavirus, it can react with the virus in many ways: with the amino acids in the spike proteins, in the membrane’s lipids, and with the RNA. It’s not selective but has a preference for certain amino acids in the spike proteins.
The study concluded MB (at various concentrations) and light decontaminated SARS-CoV-2 with up to a 5-log reduction of viral load to undetectable levels. Though bright light led to 99.9 per cent inactivation in as little as five minutes (the lowest amount of time measured), even MB exposure to ambient light (700 lux) led to complete virus inactivation after 30 minutes.
This research suggests it is now possible for healthcare workers going about their daily routines in typical
hospital settings to be exposed to enough light to activate the MB on their pre-treated masks and inactivate any present or forthcoming pathogens.
APPLICATION OF SCIENCE
Effective decontamination methods have become increasingly important for health systems facing PPE shortages and requiring reuse of PPE, and the pandemic has demonstrated the need to improve the technology and performance of masks and PPE to provide better protection to frontline health workers. Many health systems rely on the expensive and extensive UV Light or Vaporized Hydrogen Peroxide decontamination methods at best, and seven days of storage in brown paper bags at worst. The MB + Light method requires no specialized equipment or energy resources and will represent a more affordable option when products are made available.
Further, since PPE pre-treated with MB was shown to offer ongoing inactivation of coronavirus and other pathogens during use, masks could be made more effective with this technology. Compared to current N95s and similar masks that trap pathogens, wearers of masks pre-treated with MB could benefit from an active line of defense against such pathogens.
This technology could represent the next line of improvement for hospitals, nursing homes, home health – all healthcare systems.
ONGOING EFFORTS
Leading virologists, chemists, and researchers around the world are presently conducting follow-up studies. Though the science is simple and the concept is proven, special attention to the chemistry of these protective dyes is important, from choosing the optimum protective dyes, to determining dosing concentrations, to measuring singlet oxygen production. Certain dyes can be optimized for specific lighting conditions, environments, use cases, and desired outcomes. ■ H

Dr. Heyne completed her post-doctoral fellowship at the University of Ottawa. In 2007, she began her career at the University of Calgary, where she is now a Full Professor. Lacey Duffey received an MA in Journalism from University of Oklahoma, she is currently VP Experience at Singletto.
PureWick ®
female external catheter Now Available for Home Use! Do you have a patient who is a good candidate?
☑Patient requiring urine output monitoring but does not meet indications for indwelling Foley catheterization ☑ Urinary incontinence and/or frequent urination ☑ Skin injury or irritation related to urinary incontinence or diapers ☑ Post-surgical or procedure immobility
☑Bedrest orders ☑ Difficulty walking from bed or chair to toilet ☑ Difficulty using a bedpan

Visit www.PureWickNurse.ca or call: 1-800-387-9473 for more information
Mobile vaccine team helps inoculate some of the most vulnerable against COVID-19
Relief takes various forms – clapping, tears of joy, chants of “the vaccine is here, the vaccine is here!”
After months of desperately battling COVID-19, residents, staff and essential caregivers at long-term care centres, retirement homes and congregate living settings across Toronto rang in the new year by receiving their first dose of the Moderna vaccine.
“You could sense the sheer joy from people in the room as they were getting this protection,” says Inthuja Kanagasabapathy, a registered nurse (RN) with the Family Health Team at Toronto Western Hospital (TWH). She was part of the UHN mobile vaccine team that administered the first doses of Moderna to long-term care (LTC) residents in Ontario on the last day of 2020.
“It’s been tough for them for many months but now they have the vaccines, and with them, hope. It’s truly an honour for us to be part of this. We are so proud of the teamwork that’s gone into it. And, hearing the feedback from recipients, their smiles and thank yous, is overwhelming to see.”
It’s an effort that’s brought together Toronto Public Health, city staff and teams from nine hospitals and about 160 LTCs, retirement homes and congregate living sites, to protect Toronto’s most vulnerable.
“Long-term care is where the biggest amount of death and suffering has been so being able to get there with help and hope is such a positive thing that really resonates with people,” he says. “The teams are tired but the thing that buoys them along is the gratitude they encounter when they arrive.”
Mobile Team Vaccine came together quickly. UHN provides the backbone support for the coalition of partners and is the central supply depot for Moderna in Toronto. Based on allocations and prioritizing set out by Toronto Public Health and the provincially-mandated Toronto Central Local Health Integration Network, LTC residents are vaccinated by staff from their hospital partners, which were established earlier in the pandemic. UHN has 13 LTC partners.
At lunchtime on Dec. 29, Shiran Isaacksz, Vice President Altum Health & UHN Connected Care, was tasked with leading the organization’s mobile vaccination rollout. With the first Moderna shipment scheduled to arrive the next day and the goal of starting shots in arms the day after that, his team had 48 hours to assemble all the key players at UHN and in the community to make it happen.
It was Connected Care on full display – pulling together inter-disciplinary teams who each use their expertise to make a positive impact, collectively. It was about being able to pivot and scale quickly internally, while also working with community partners and city and provincial health authorities. These are the principles of UHN’s Integrated Care Program and what allowed the team to get mobile vaccination in the community up and running so quickly. Among the key contributors: • UHN Pharmacy, leading the way on the rollout of the Pfizer-BioN-
Tech vaccine since mid-December, oversees Moderna distribution and delivery; • The Family Health Team at TWH, which in April proactively began swabbing residents and staff at many LTCs and has largely staffed the COVID Assessment Centre at
TWH, does the vaccinations; • The UHN Long-Term Care Support
Team, which has been providing ongoing assistance and Infection Prevention and Control (IPAC) expertise to LTCs and retirement homes since early in the pandemic, works with each of the homes to ensure they’re ready for the arrival of the mobile vaccine team; • The LTCs themselves obtain consents from residents, ensure there’s a place for vaccinations to happen and have staff on hand to help organize on-site needs, complete the neces-
sary documentation and monitor recipients for adverse reactions for 15 minutes; • Members of UHN Connected Care ensure the needs and experience of residents, staff and essential caregivers are prioritized. They also provide the critical backbone support, including education, training, and logistics, which ranges from clearly delineating who handles what tasks at each site and determining how many doses of vaccine are required, to ensuring data on who is vaccinated gets added to the provincial registry and making sure the team has food and water.
At the outset, all teams were governed by two key principles: safety and speed.
A mobile vaccination model was developed and at work in LTCs within 48 hours. Each evening, an Operations Team featuring representation from all UHN teams involved, met virtually to review that day’s events. Over the course of its first week of meeting, workflows were improved, the drawing of doses was refined to ensure no vaccine was wasted and overall efficiency of the process was polished.
Collaborating with counterparts from across the health system, including family medicine teams from other hospitals – Humber River, Michael Garron, North York General, Scarborough Health Network, Sinai Health, Sunnybrook, Unity Health Toronto and Women’s College – brought different skills and strengths together to improve the vaccination model.
“We want this approach to continue, to put down our hospital badges and work collaboratively with other endeavours, not just in an emergency. There are so many opportunities for us to come together for the benefit of our hospitals, and more importantly, for the benefits of all patients.” ■ H

Photo: Brian Hodges Helen Lampi, (L), Director of Nursing at Castleview Wychwood Towers, welcomes back members of UHN’s Mobile Vaccine Team – flashing “V” for vaccine – last week as they prepare to administer second doses of Moderna’s COVID-19 vaccine. On Dec. 31, the team kicked off the vaccination drive at the home.
Together in the fight against COVID-19
Thank you to all healthcare and laboratory professionals for your passion, effort and courage.
The pandemic has highlighted the work performed every day by laboratory professionals and the value diagnostics testing brings to health systems and patients. We are proud to contribute to the fight against COVID-19 with our diagnostic solutions.
Roche Diagnostics in Canada: A partner in the fight against COVID-19
PROVIDING MULTIPLE SOLUTIONS ACROSS THE TESTING CONTINUUM
ENSURING EQUITY OF ACCESS TO OUR TESTING SOLUTIONS
Diagnostic
for patients with COVID-19 symptoms# First commercial, high throughput PCR test to identify active infection and support testing demand Point-of-care rapid antigen test with instrument-free results in 15 minutes Testing
to differentiate between the flu and COVID-19
First commercial test for highthroughput systems Surveillance
to determine prior exposure High throughput antibody test and point-of-care antibody test** to help determine past infection SARS-CoV2 Spike protein antibody quantitative test* to aid in assessing the adaptive immune response to the SARS-CoV-2 S protein Patient Management
to manage actively infected patients Biomarkers*** to identify severe inflammatory response in COVID-19 patients
Our focus is on ensuring the highest patient impact and broadest geographic reach so that the hardest hit communities can receive access to testing. Prioritizing Access to Closely Support Public Health Strategy
National reference labs Distribution of instruments and reagents to areas with large-scale spread Embracing a Spirit of Partnership
Healthcare providers Laboratories Diagnostic & Pharmaceutical companies Governments, Public Health Agency of Canada and provincial public labs Health Ministries and Health Canada Public Services and Procurement Canada
A WORLD LEADER IN HEALTHCARE
World’s Largest Biotech Company
1,750
Employees in Canada
Combined strengths in pharmaceuticals and diagnostics Breadth of Diagnostics Solutions
Oncology Inflammatory and autoimmune diseases Infectious diseases Cardiovascular and Diabetes Neuroscience Women’s Health
R&D
#8 in R&D investment worldwide across all industries and #1 in Biotechnology****
2020 DJSI
Ranked the most sustainable healthcare company in the Dow Jones Sustainability Indices for the eleventh time
YEARS
into MONTHS
Years of development and commercialization, compressed into months 2020-2021 Overview for Canada
MAR After just six weeks of development, Health Canada authorization under the Interim Order for the first commercially available high throughput SRASCoV-2 PCR test
NOV Health Canada authorization under the Interim Order for the SARS-CoV-2 & Influenza A/B Multiplex PCR test for high-throughput
JUN Health Canada authorization under the Interim Order for the Anti-SARS-CoV-2 antibody test
FEB 2021
Health Canada authorization under the Interim Order for the point-of-care SARSCoV-2 Rapid Antigen Test
More COVID-19 solutions to come
The OMTU includes its own ambulance intake for patient offloading, an infection control isolation room, four staff stations, and other amenities. It is connected to the Civic Campus Emergency Department and ICU via an above-ground tunnel.

New unit adds forty hospital beds to help increase capacity, reduce wait times

By Caitlin Renneson
Forty hospital beds. An impressively high “cathedral” ceiling. A bright, warm and organized space. In some ways, this new unit looks much like other inpatient units in the main building of The Ottawa Hospital, but it has something a little extra: an undeniable energy that comes from knowing you are part of something new.
MEETING COMMUNITY NEEDS
The Offload Medicine Transition Unit (OMTU) is a new 40-bed temporary structure located at the Civic Campus of The Ottawa Hospital. Funded by the provincial government and constructed in just nine weeks, the OMTU will help expand hospital capacity, decrease ambulance offload times for paramedics and get patients into hospital beds faster once admitted.
It welcomed its first patient on January 4.
INSIDE THE OMTU
The OMTU includes its own ambulance intake for patient offloading, an infection control isolation room, four staff stations, a staff lounge, washroom facilities and showers. It has proper air ventilation and is fully climate controlled.
Each patient bay has oxygen and suction, a nurse call system, and emergency power. Like the main hospital, the OMTU has modern medical technology, wi-fi for patients and wired internet connections for computers on site that are connected to EPIC, the hospital information system. Staff and patients can access the main hospital’s Emergency Department and Intensive Care Unit (ICU) through an aboveground tunnel.
The staff at the OMTU include doctors, nurses, registered practical nurses, physiotherapists, social workers, orderlies and others that you might expect inside any other patient unit. Staff supporting the OMTU underwent simulation training for emergency code calls before the unit opened, just as they would have before opening any other new unit.
PATIENT EXPERIENCE A PRIORITY
Although the focus was on maximizing safety and care, the patient experience was also a priority. Each patient bay is slightly bigger than what you would typically see in the emergency department. Stretchers are fitted with thick gel mattresses. There are hooks for coats and shelves in each bay for belongings. There is a dimmable light above the bed and a whiteboard on the wall to keep important information.
“It was really impressive, how high the ceilings were, how everything came together in nine weeks,” says Kyle Gantner, Acting Clinical Manager for the OMTU.
“Patients seem to like the semi-open concept,” says Jeanne Millons, Acting Clinical Care Leader for the OMTU. “The rooms don’t have a roof over each of them, so there are things to look at if you want to be distracted.”
Gantner and Millons each lay down in patient beds themselves before the unit was open to get a first-hand view of what it would be like for a patient.
TEAMWORK BRINGS THE DESIGN TO LIFE

The concept, design, layout, construction and ultimate operation of the OMTU was the result of impressive teamwork from many groups and individuals. Kathleen McGarragle is the Emergency Management Officer at The Ottawa Hospital and co-project manager for the unit. She and Dwight Breault, Senior Project Manager of Capital Projects, led the project on behalf of the hospital. They worked closely with Colliers, Infrastructure Ontario/The Ministry of Health, BLT Construction, and several design and consulting firms.
Many hospital departments and teams offered their expertise and support as well. Hospital leadership, clinical teams, Emergency Management, Capital Projects, Facilities, Planning, Infection Prevention and Control, Care Environment Transportation, Environmental Services, Materials Management, Nutrition and Food Services, IS/IT, Biomedical Engineering, Fusion, Parking Services, Protective Services, the Safety Office, The University of Ottawa Skills and Simulation Centre and the Simulation
NEW TECHNOLOGY
A corridor in the new OMTU
Continued on page 42
AcryMed
ANTIMICROBIAL SOLID SURFACE
SURFACE SOLIDE ANTIMICROBIENNE


#meganite www.meganite.com
Staphylococcus aureus subsp. Aureus (MRSA) ATCC 33591 Escherichia coli ATCC 8739 Pseudomonas aeruginosa ATCC 9027 Klebsiella pneumoniae ATCC 4352
Disclaimer: Tested more than 90%* effective against Meganite selected bacteria in accordance with ISO 22196 and JIS Z 2801 testing standards. Results may vary when tested on different organisms or bacteria. The AcryMed technology protects the product itself against stain and odor-causing bacteria. AcryMed does not protect users or other beings from disease-causing bacteria. AcryMed does not have anti-viral properties and cannot replace any cleaning process. Please contact your local authority/government regarding virus cleaning recommendations. Exclusion de responsabilité: Testé à plus de 90%* d'efficacité contre les bactéries sélectionnées par Meganite, conformément aux normes de test ISO 22196 et JIS Z 2801. Les résultats peuvent varier lorsqu'ils sont testés sur différents organismes ou bactéries. La technologie AcryMed protège le produit lui-même contre les bactéries responsables des taches et des odeurs. AcryMed ne protège pas les utilisateurs ou autres organismes vivants contre les bactéries pathogènes. AcryMed n'a pas de propriété antivirale et ne peut remplacer aucun processus de nettoyage. Veuillez contacter votre autorité locale / gouvernement concernant les recommandations de nettoyage des virus.
Meganite Solid Surface Solid Source Corp
info@meganite.com AB / BC info@solidsource.ca 1800.545.0082 ON / MB / NT / NU / SK Rocheleau Inc
info@rocheleau.ca 1800.567.5201 QC / NB / NL / NS / PE
Forty hospital beds
Continued from page 41 Patient Safety Program, the Cancer Program, Accessibility Services, Occupational Health and Wellness, the Communications Department and many others worked in concert to make sure everything came together.
From a health-care standpoint, doctors, nurses, infection prevention and control experts, clinical care leaders, directors and others from the Emergency Department and inpatient units all had a hand in determining what the space would look like and how it would function.
“The Ottawa Hospital really came together with different departments doing everything they could to help,” says McGarragle. “We went live on January 4, so the biggest push was over the holiday period. That means a lot of people worked extra hard to get it done.”
Read adds, “It’s a great example of living our vision of providing worldclass care, exceptional service and compassion just as we would want for our loved ones. Everyone worked together to achieve a goal that would support our patients and our teams, especially during a very challenging time.”
A STRONG COMMUNITY PARTNERSHIP
Another important element to the project’s success was the partnership between the hospital and the community.
“Even though we knew that the OMTU would be a great benefit to the community overall, we recognized that constructing it would have an impact on the local community,” says Joanne Read, Executive Vice-President of Planning and Development for The Ottawa Hospital. “We wanted to establish open lines of communication throughout the project to make sure that the community had a voice and we could try to minimize any impact on them.”
The project team also worked with hospital departments and services that would be impacted most by the construction, including the Academic Family Health Team and programs in Grimes Lodge.
Constant and open communications was a priority from the start and contributed to the project’s success.
“My objective was to make sure that everyone that was supposed to be included was included,” says McGarragle. “If I needed to follow up with a group or team, I did, without fail, every time.”

Kyle Gantner (left) and Jeanne Millons are part of a large team dedicated to providing world-class care to patients in the OMTU.
A SPECIAL ATMOSPHERE
Opening a new hospital unit is a special occasion, and it often comes with a sense of excitement among staff. That is especially true in this case because the staff were engaged in the design of the OMTU from the very beginning.
“We were part of building something from the ground up,” says Milions. “From construction, to making decisions about how the room looks, to hiring and onboarding a whole new staff, it kind of feels like we are in this together in this new journey.”
Gantner feels the same way.
“We got to start from the beginning. We get to build a team and work as a team as the OMTU evolves. I think, for me, that’s what makes the OMTU special. We get to set it up together and work together to make it a very good environment for both the patients and the staff.”
And that sense of shared purpose has carried over into the culture in the unit.
“We have a very positive team,: adds Gantner. Staff are very engaged. Its an environment open to change. We focus a lot on teamwork.”
A culture of constant improvement
Even though the OMTU has been open for a little more than a month, the staff have settled into a groove. Still, staff are continuously looking for opportunities to improve how they deliver care.
“It’s evolving on a daily basis,” says Gantner. “We’ve evolved lots of things. From the layout of supplies and the types of supplies we use, to how nurses and registered practical nurses work together to provide safe patient care. We lean on staff a lot to figure out what works best for them. We let them guide the evolution and we help facilitate change to make their space theirs.”
CONSTRUCTED IN JUST NINE WEEKS, A NEW 40-BED TEMPORARY STRUCTURE AT THE OTTAWA HOSPITAL’S CIVIC CAMPUS WILL HELP INCREASE CAPACITY AND REDUCE AMBULANCE OFFLOAD TIMES.
HERE TO SERVE THE COMMUNITY
The benefits to the community are many. Its 40 beds help free up beds in the Emergency Department and on inpatient floors for patients who need that specialty care.
The OMTU will help to ensure that our community gets the care that they want and they deserve” says Millons. “It’s a success story for sure.”
And it wouldn’t have happened without an incredible amount of support.
“Thank you to everyone, the community, the staff, the patients, the project managers, everyone involved in planning and construction,” says Read. “It is safe, it is clean, it is warm, it is comfortable. We hope you never need to visit the OMTU yourself or with a loved one, but if you do, know that it is there for you.” ■ H







Exploring the evolving world
of digital health through the pandemic and beyond
By Daniel Martz, Vice President, Virtual Care, TELUS Health
The World Health Organization (WHO) global strategy for digital health acknowledges the potential for technology to accelerate human progress, predicting these solutions will help ensure more people enjoy better health and well-being. Specifically noting applications that enable virtual care, remote patient monitoring, and data exchange across the healthcare ecosystem, the strategy suggests these technologies can improve experiences within the care continuum and drive enhanced health outcomes.
While the use of digitally-enabled healthcare tools has increased steadily in the last few years, widespread adoption has grown exponentially since the onset of COVID-19. With an overburdened healthcare system and growing concern of contracting the virus in medical settings, government and healthcare leaders turned to technology to help bridge gaps in care access and ensure Canadians were supported through these challenging times.
A study by ICES, Ontario’s leading health and social data research organization, showed that in the first few months of the pandemic, visits to primary care clinics declined by 79 per cent while virtual visits, per 1,000 individuals per day, rose by a staggering 5,600 per cent. This transformation was made possible by innovations that connected Canadians with care teams from the comfort and safety of their own homes. Whether through functionalities integrated into physicians’ electronic medical records (EMRs) or mobile applications for those without access to a family physician or who have access to health and wellness services through their insurance or benefits provider, healthcare professionals across the country began offering virtual appointments with the support of these technological advancements. This significantly eased the burden on hospitals, enabling them to focus on supporting Canadians requiring urgent care.
Virtual care also presents a modern approach to triaging and monitoring. Technology is being used to virtually triage potential COVID-19 cases before a patient arrives at the hospital. Other solutions, such as TELUS’ Home Health Monitoring (HHM), are being used to track the condition of hundreds of patients at once as they recover from COVID-19 at home. This strategy helps open capacity for more critical cases, reducing pressure on hospitals. The HHM solution has since been used to remotely monitor people recovering from organ transplants and those with chronic conditions, keeping them out of hospitals where risk of exposure is greater.
Digital health solutions have also played a critical role in giving Canadians access to their own health information. Governments in Alberta and Saskatchewan have provided residents with personal health records allowing them to view and track their own medical information. These records have enabled quick access to COVID-19 test results, helping to reduce anxiety associated with waiting days for a diagnosis.
The innovations we have seen emerge have not only addressed the significant challenges posed by COVID-19, but have also positively impacted the sustainability of our health system.
What do Canadians have to say about the future of digital health?
According to them, digital health is here to stay. Research from Canada Health Infoway suggests 84 per cent of Canadians would use technology to help manage their health while a 2020 Canadian Medical Association poll highlighted that Canadians who connected with a physician virtually reported a 91 per cent satisfaction rate.
Public health systems are also taking important steps to prioritize digital health. Alberta was the first to make virtual care physician billing fee codes permanent, enabling the ongoing delivery of virtual care across the province. Meanwhile, the federal government has made significant investments to expand virtual care in British Columbia and Prince Edward Island, supporting the longer-term adoption of high-quality and safe virtual healthcare options.
There is a bright future for digital health in Canada. Already virtual care has expanded to include services by allied healthcare professionals such as physiotherapists, nutritionists and mental health counsellors. With the introduction of new services such as online pharmacies, a fully integrated, end-to-end virtual care experience that addresses multiple aspects of care is not too far in the future. And the roll-out of 5G technology holds great promise in making this complete experience seamless, enhancing connectivity across the country while enabling new applications.
As our healthcare landscape continues to evolve, we must remember the importance of collaboration and interoperability. If we work together to take our siloed platforms and unify them to enable efficient communication across physician EMRs, pharmacy management systems, virtual care solutions and insurance claims processes, we can take a step closer to connecting all aspects of health, supporting the continuity of care for Canadians and ultimately driving better health outcomes.