
6 minute read
A College Student’s
A COLLEGE STUDENT’S CRASH COURSE IN MANAGING PLAQUE PSORIASIS
In the spring of 2016, Kate was excitedly preparing for the rites of passage most high school seniors look forward to - prom, graduation, turning 18 and getting ready for college. What she wasn’t preparing for was a chronic illness diagnosis.
Advertisement
It started out as a small patch of dry skin on Kate’s neck that began to spread to her scalp in thick, red patches. This must be an allergic reaction, Kate thought, before seeking help at an urgent care center. There, a physician suggested the patches were a fungal rash and recommended special shampoos. But the patches soon covered large areas of her scalp and neck, and were now accompanied by a painful, burning sensation. Kate spent many days trying to hide her patches from other people.
Kate visited a dermatologist who prescribed another treatment option, but unfortunately it didn’t relieve her symptoms. As her condition worsened, she saw other specialists, hoping to find some relief. But her symptoms persisted. Now, Kate had to prepare to go off to college while still searching for answers about this unknown condition.
“Starting college is hard enough - living in a new place, meeting new people, starting new classes and activities,” said Kate. “I was focused on trying to hide what was happening to my body. I started wearing a baseball cap and avoided wearing dark clothing.”
Kate was determined to get to the bottom of what was going on with her skin. After multiple visits to several different dermatologists, a biopsy finally revealed the truth - Kate had moderate to severe plaque psoriasis.
Plaque psoriasis is a chronic autoimmune disease and its exact cause is unknown. Research suggests that an overactive immune system may cause skin cells to pile up on the surface of the skin, which then form psoriasis lesions or plaques and can lead to physical pain, itching, skin tightness and a burning sensation.1
More than 8 million Americans are currently living with psoriasis,2 and plaque psoriasis is the most common form.3
influential-magazine.com FEATURE
Now that Kate had a proper diagnosis of moderate to severe plaque psoriasis, her next step was to find the right treatment. The first two treatments prescribed to her provided some skin clearance.
However, finishing her freshman year at college, Kate was still concerned about her skin plaques. Then, that summer, the U.S. Food and Drug Administration approved a medication called TREMFYA® (guselkumab), a biologic treatment that selectively blocks a protein in the body called interleukin-23

(IL-23), one of the key proteins thought to be responsible for plaque psoriasis.
TREMFYA® is approved to treat adults with moderate to severe plaque psoriasis who may benefit from taking injections or pills (systemic therapy) or phototherapy (treatment using ultraviolet or UV light). In clinical studies, at least 7 out of 10 patients treated with TREMFYA® saw 90 percent clearer skin and more than 8 out of 10 were rated clear or almost clear after 16 weeks. In clinical studies at Week 16, 4 out of 5 people with scalp psoriasis were also rated clear or almost clear of their scalp psoriasis. Also, more patients had improvement in symptoms such as pain, stinging, and skin tightness.
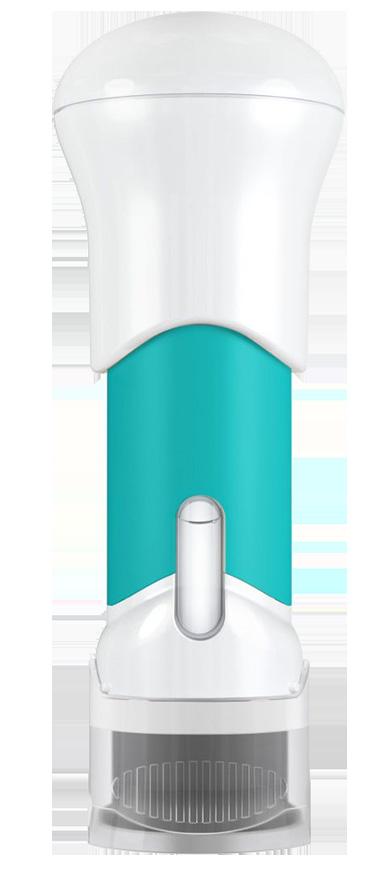
The medicine comes in both a pre-filled syringe and a One-Press Patient Controlled injector. Your first self-injection should be performed at your dermatologist’s office so they can show you the right way to give yourself injections under the skin. After this training, and with your healthcare
1. National Psoriasis Foundation. About Psoriasis. Accessed July 22, 2020. www.psoriasis.org/about-psoriasis 2. National Psoriasis Foundation. Statistics. Accessed July 22, 2020. www.psoriasis.org/content/statistics 3. American Academy of Dermatology. Skin Conditions by the Numbers. Accessed July 22, 2020. www.aad.org/media/stats-numbers © Janssen Biotech, Inc. 2020 10/20 cp-162319v1 (BPT)
influential-magazine.com FEATURE
provider’s approval, you may be able to inject TREMFYA® under the skin at home every eight weeks after two starter doses at Week 0 and Week 4.
“I was amazed by the results,” said Kate. “I am so happy I started on TREMFYA®. I inject my medication every 8 weeks and I’m pleased to share my journey to achieving clearer skin. I know now that my psoriasis doesn’t define me.”
Results may vary. TREMFYA® may not be right for everyone. Only your doctor can decide if TREMFYA® is right for you.
IMPORTANT SAFETY INFORMATION
TREMFYA® is a prescription medicine that may cause serious side effects, including:
Serious Allergic Reactions. Stop using TREMFYA® and get emergency medical help right away if you develop any of the following symptoms of a serious allergic reaction: • fainting, dizziness, feeling lightheaded (low blood pressure) • trouble breathing or throat tightness • swelling of your face, eyelids, lips, mouth, tongue or throat • chest tightness • skin rash, hives • itching
Infections. TREMFYA® may lower the ability of your immune system to fight infections and may increase your risk of infections. Your healthcare provider should check you for infections and tuberculosis (TB) before starting treatment with TREMFYA® and may treat you for TB before you begin treatment with TREMFYA® if you have a history of TB or have active TB. Your healthcare provider should watch you closely for signs and symptoms of TB during and after treatment with TREMFYA®.
Tell your healthcare provider right away if you have an infection or have symptoms of an infection, including: • fever, sweats, or chills • diarrhea or stomach pain • muscle aches° shortness of breath • weight loss° blood in your phlegm (mucus) • cough • burning when you urinate or urinating more often than normal • warm, red, or painful skin or sores on your body different from your psoriasis
Do not take TREMFYA® if you have had a serious allergic reaction to guselkumab or any of the ingredients in TREMFYA®.
Before using TREMFYA®, tell your healthcare provider about all of your medical conditions, including if you: • have any of the conditions or symptoms listed in the section “What is the most important information I should know about TREMFYA®?” • have an infection that does not go away or that keeps coming back. • have TB or have been in close contact with someone with TB. • have recently received or are scheduled to receive an immunization (vaccine). You should avoid receiving live vaccines during treatment with TREMFYA®. • are pregnant or plan to become pregnant. It is not known if TREMFYA® can harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if TREMFYA® passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of TREMFYA®? TREMFYA® may cause serious side effects. See “What is the most important information I should know about TREMFYA®?”
The most common side effects of
TREMFYA® include: upper respiratory infections, headache, injection site reactions, joint pain (arthralgia), diarrhea, stomach flu (gastroenteritis), fungal skin infections, herpes simplex infections, and bronchitis. These are not all the possible side effects of TREMFYA®. Call your doctor for medical advice about side effects. Use TREMFYA® exactly as your healthcare provider tells you to use it.
Please read the full Prescribing Information, including Medication Guide for TREMFYA®, and discuss any questions that you have with your doctor.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088. l cp-82626v3










