LEADING ORTHOPEDICS & SPORTS MEDICINE



95 Research faculty and physicians
15 Residents
8 Fellows >20 Medical students on rotation
Houston Methodist Academic Excellence Award
Joshua Harris, MD
The Knee Society’s Chitranjan S. Ranawat, MD Award 2021
Stephen Incavo, MD
ENMED CAPSTONE Mentorship Award
Francesca Taraballi, PhD
MLB Research Award 2021
Patrick McCulloch, MD
INSTRUMENTS/EQUIPMENT
• 7T MRI
• Stryker MAKO Robotic Knee/Hip Replacement System
• Zimmer Biomet ROSA Robotic Knee System
• Intraosseous injections
ANNUAL RESEARCH
>100 Research projects in progress
>50 Publications
>60 Presentations at conferences
The incredible research underway in the Houston Methodist Department of Orthopedics & Sports Medicine serves one purpose — to provide our patients with the very best care possible. In doing that, we hope to improve the practice of orthopedics for all patients. Our surgeons and researchers collaborate across departments, employing nanotechnology, materials science and regenerative medicine, and, across institutions, working with our neighbors at Rice University. All our discoveries are for the benefit of our patients — first and foremost. I am pleased to share this work with you.
You’ll find in this report information about The Houston Methodist-Rice University Center for Human Performance, a new research facility designed to develop novel techniques to prevent, treat and recover from musculoskeletal injuries and diseases. This collaboration is a significant investment from both sides and is expected to benefit everyone from elite athletes to senior adults.
Houston Methodist scientists have identified and repurposed a treatment commonly used in emergency medicine that is now preventing joint infection after total knee replacement. We are leveraging the Ann Kimball & John W. Johnson Center for Cellular Therapeutics to advance promising stem cell-based therapies to treat stubborn orthopedic conditions. Our clinicians are also at the forefront of harnessing machine learning to predict outcomes and offer the best-personalized treatments for our patients.
Our department’s research focus, advanced facilities and resources support investigations, and encourage up-and-coming and established recruits to join our renowned staff. Comron Saifi, MD, the C. James and Carole Walter Looke Chair in Orthopedic Spine Surgery, is an expert in treating spinal deformities, including kyphosis and scoliosis. Timothy Brown, MD, the program director of the Adult Reconstructive Surgery Fellowship is an expert joint replacement surgeon also dedicated to performing impactful clinical and translational research.
We are committed to offering the best treatments for our patients by pursuing the best research ideas in our labs. I invite you to read more about developments in orthopedic research conducted at Houston Methodist Orthopedics & Sports Medicine.
Kevin E. Varner, MD Chairman, Houston Methodist Orthopedics & Sports Medicine C. James and Carole Walter Looke Presidential Distinguished Centennial Chair in Orthopedics
C. James and Carole Walter Looke Presidential Distinguished Centennial Chair in Orthopedics

Houston Methodist and Rice University joined forces to create a new research center that focuses on exercise physiology, injury prevention and rehabilitation to advance research and education in human performance.
“Researchers at the center work together to develop novel techniques to prevent, treat and recover from musculoskeletal injuries and diseases.”
“Ultimately, these efforts will greatly benefit our patients at Houston Methodist. High-performance athletes, older adults and everyone in between will have access to treatment that is informed by the research undertaken at the center.”
The Houston Methodist-Rice University Center for Human Performance is a collaboration between the Houston Methodist Department of Orthopedics & Sports Medicine, and multiple departments at Rice including Kinesiology, Athletics and Engineering. Encompassing a 6,000-square-foot facility in Rice’s Tudor Fieldhouse, the lab is next door to Houston Methodist Hospital.
The research space is equipped for state-of-the-art studies with advanced 3D motion capture, force-plate measurement, region-byregion quantification of bone density and muscle mass, isokinetic testing platforms, human tissue collection for blood and muscle sampling, metabolic analysis, cardiovascular screening and aerobic performance testing. Physicians, researchers and students work side by side with athletes, trainers and coaches.
Physician researchers at the center are currently studying joint mechanics and forces expended during batting and pitching in amateur and professional baseball players to improve rehabilitation and postinjury safety for athletes. To perfect patient progress and better predict outcomes, scientists also analyze gait and biomechanics of patients’ daily activities following total knee and hip replacement.
As part of a grant from Major League Baseball, the center has added technology to help researchers track and analyze pitching and hitting performance during live play. The lab’s grant-funded studies leverage Houston Methodist relationships with the Houston Astros, Houston Ballet and Rice University, and they employ an advanced Vicon motion capture system integrated with force plates and electromyography for precision data that can be translated for clinical applications.

Patrick McCulloch, MD
John S. Dunn Chair in Orthopedics Surgery

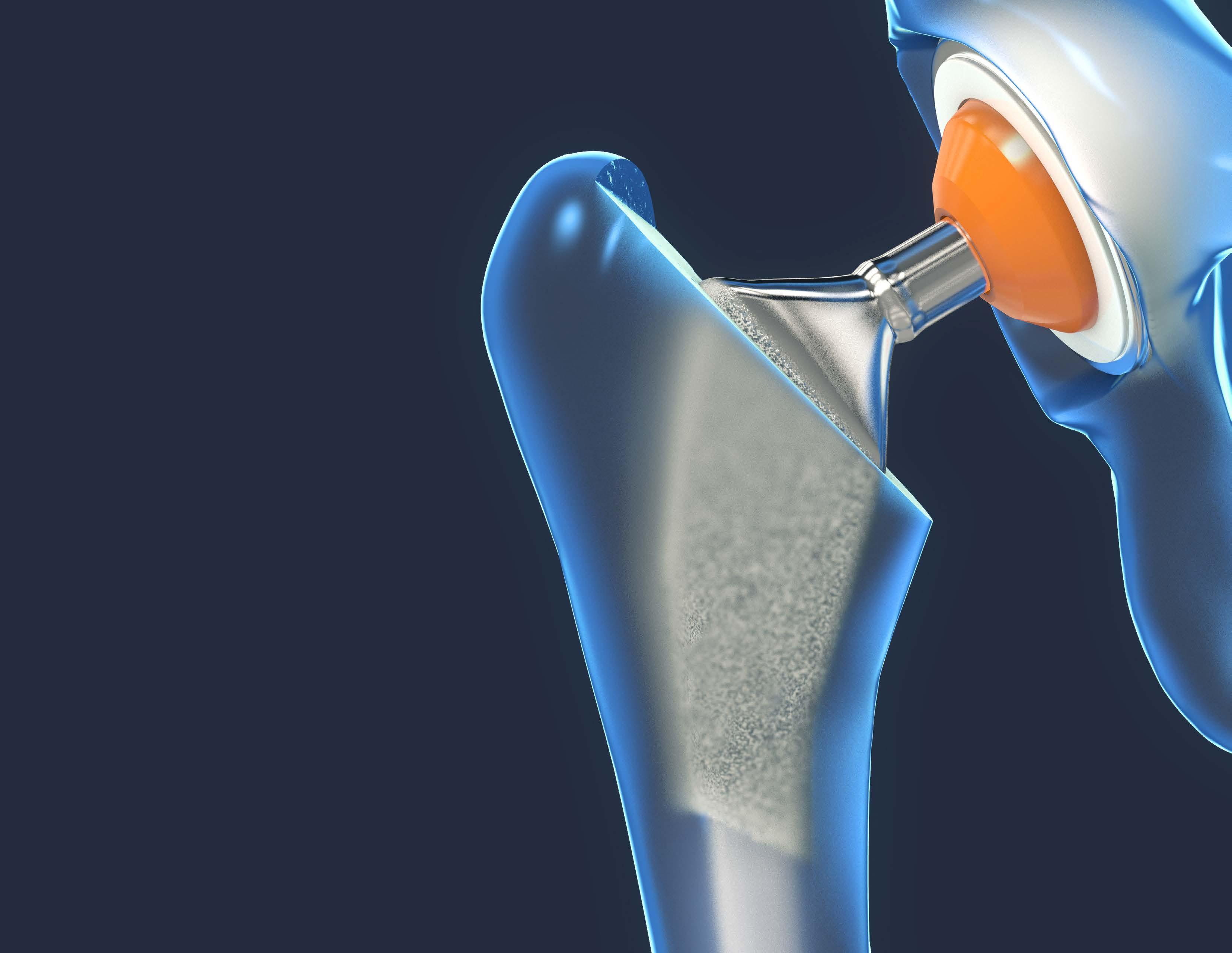
Total knee arthroplasty (TKA) is one of the most common and successful orthopedic surgeries, yet postoperative infection and pain continue to be significant complications. To help change this, orthopedic surgeons at Houston Methodist have been studying an established technique in emergency medicine, intraosseous injections, and applying it to a new setting to help prevent joint infection after total knee replacement.
In a study recently published in The Bone & Joint Journal, Stephen Incavo, MD, section chief of adult reconstructive surgery at Houston Methodist and professor of clinical orthopedic surgery at Weill Cornell Medicine, described how intraosseous administration of a commonly used antibiotic, vancomycin, during TKA reduces joint infection rates within 90 days of the procedure, which is within the most common timeframe for postoperative infection when compared to intravenous vancomycin administration. Due to the potential for significant improvement in patient safety and cost savings, this paper was awarded the prestigious Chitranjan S. Ranawat, MD Award 2021 by The Knee Society.
Building on this line of research, Incavo and his research team conducted a randomized, controlled trial to investigate whether adding morphine to intraosseous injections could help improve patient pain in the 14 days following surgery. They found that by adding morphine to intraosseous injections of antibiotics, they significantly reduced patients’ postoperative pain levels immediately after surgery and at multiple time points within the first two weeks of recovery. This is an especially important time frame for patients as it is often the most painful part of the recovery process. Importantly, patients who received intraosseous morphine took less pain medication than those who did not.
The ability to predict postoperative outcomes preoperatively holds great promise with artificial intelligence and machine learning (ML). Physicians and researchers in the Houston Methodist Orthopedics & Sports Medicine Department are using ML to improve patient care, predict outcomes and optimize treatments for individual patients.

Joshua Harris, MD, orthopedic surgeon, captures data from his patients’ first preoperative visits through their postoperative recovery journeys, to create a database that he uses to help predict outcomes and suggest the best personalized treatment option for each patient.
ML, a subcategory of artificial intelligence, uses algorithms to help physicians extrapolate knowledge from vast amounts of data and improve the clinical decisionmaking process. Valuable data can be generated from electronic medical records and both patient- and clinician-generated questionnaires. On top of text-based data, imaging, such as radiographs, computed tomography and magnetic resonance imaging, can be quickly interpreted with ML and used in clinical practice and research.
Many single-center and multicenter prospective registries continue to grow as part of both United States-based and international networks and collaborations. “Analytics applied to the deep trove of data also help us ensure that our patients are tracking well on their recovery timelines and give us additional tools to make necessary adjustments as soon as possible, thus getting our patients back to their full lives as soon as possible postsurgery,” said Harris.
Harris authored an editorial on the topic in Arthroscopy, The Journal of Arthroscopic and Related Surgery, Volume 37, Issue 5, May 2021.
“Careful analysis of this data can help us better understand what factors affect postoperative outcomes. It can inform best practices when making clinical decisions, possibly helping us identify protective treatments that will prevent arthroscopy interventions.”
Joshua Harris, MD Orthopedic surgeon
Restoring the structure and function of the musculoskeletal system to alleviate disease and pain is the mission of scientists at the Center for Musculoskeletal Regeneration at Houston Methodist.
“We recognize the human body’s incredible capacity to heal, and we leverage this in our design of biomimetic materials that boost cell response during healing. With this approach we can rely on the local physiological healing cascade and avoid introducing bioactive stimuli, such as growth factors, which can have undesired side effects.”
Francesca Taraballi, PhD Director of the Center for Musculoskeletal RegenerationThe center is a multidisciplinary, translational research laboratory with scientists who harness the body’s natural healing capabilities and use them to their fullest potential for drug delivery and tissue engineering applications. Researchers under the leadership of Taraballi leverage their expertise in nanomedicine, engineering, chemistry, biology and materials science to perform cutting-edge research designed to facilitate technology translation to the clinic.
“We aim to accelerate the rate at which nanotechnology and tissue engineering move from bench to bedside,” Taraballi said. There is a high clinical need for products and materials that exhibit high targeting and low toxicity. Surgical applications require materials with high biocompatibility and compliance with organ function. Taraballi and her team are creating injectable and implantable biomimetic biomaterials that are able to flourish within these parameters.
“The center is focused on the development nano- and biomaterials, which we use as in vitro models of complex systems, injectable nanotherapies or implantable synthetic tissues,” said Taraballi. “Our efforts are directed towards the treatment of currently unmet traumatic and pathological musculoskeletal needs. By combining cell biology with nanotechnology, we create innovative medical technologies that work within, and not around, the laws of nature.”
Researchers at the Houston Methodist Center for Musculoskeletal Regeneration leverage the human body’s capacity for healing to develop biomimetic implantables that augment recovery from complex bone fractures.
Francesca Taraballi, PhD, center director, and her colleagues have developed a collagenbased scaffold device called 3 Zonal Membrane (3ZM), which is currently in cGMP production. The scaffold enhances the structure and composition of growing bones in a way that speeds the repair of complex fractures that otherwise commonly result in high infection rates, slow or incomplete healing, or amputation.
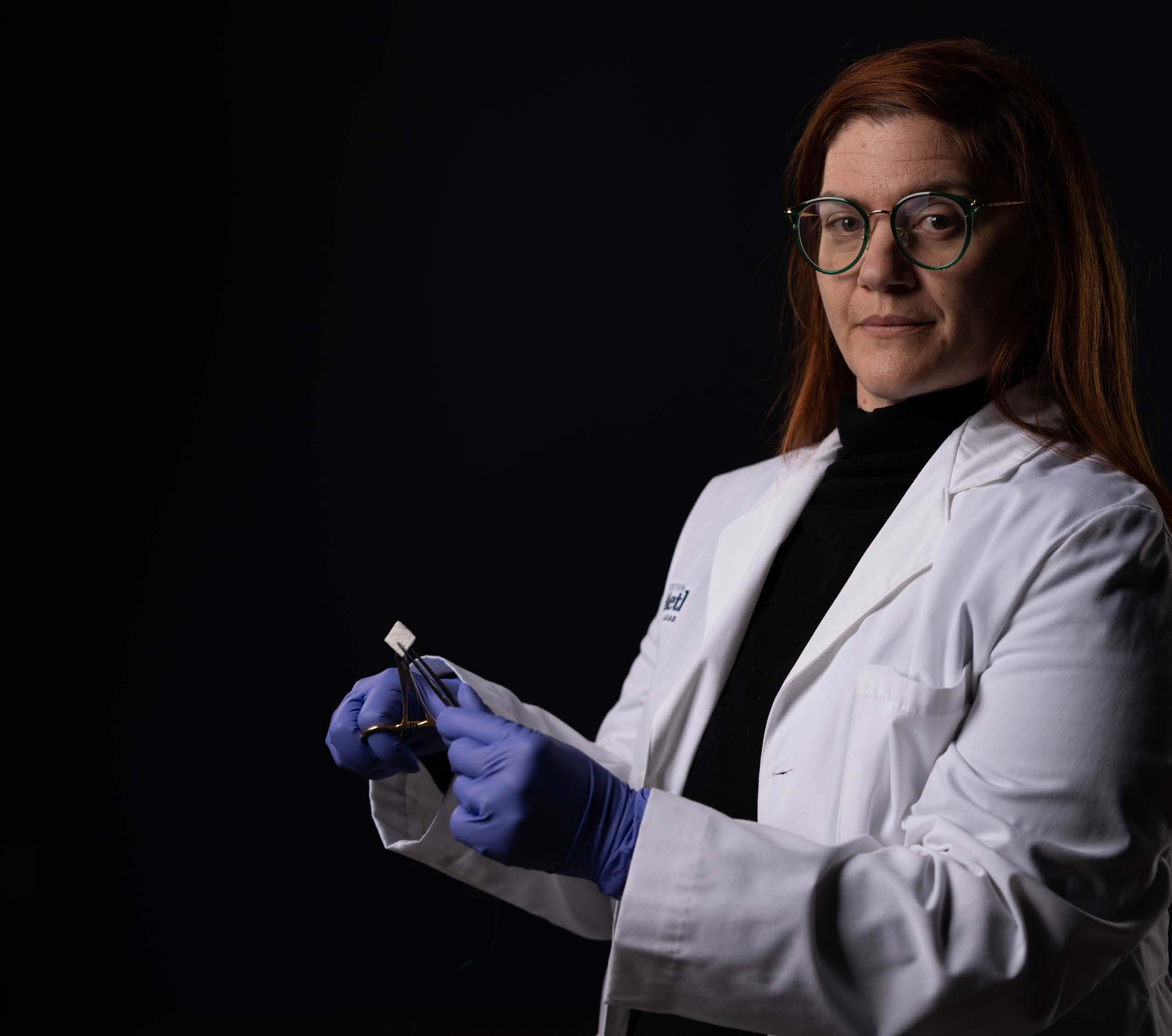
Taraballi has demonstrated that regenerative processes depend upon an intricate dialogue among different types of cells. In preclinical models, the 3ZM scaffold guided immune cells, stem cells and bone membrane cells to remodel a complex fracture into functional bone. Within six weeks, the bone healed and the implanted materials were absorbed by the body, leaving the bone strong.
During the healing process, 3ZM is cut and shaped to fit a defect site and then sutured to the surrounding periosteum. The process requires only one operation and no additional growth factors. After four to six weeks, the bone is fully healed, and the 3ZM is absorbed.
The Center for Musculoskeletal Regeneration was awarded $6 million by the U.S. Department of Defense under the leadership of Bradley Weiner, MD, professor of clinical orthopedic surgery, to complete preclinical cGMP assessment of 3ZM technology for a preinvestigational device exemption regulatory consultation with the Food and Drug Administration. The center leaders have worked with industry partners, regulatory experts and policymakers to identify an accelerated path to clinical application.
Stem cell-based therapies are gaining popularity as a biologic solution for stubborn orthopedic conditions, including cartilage repair, osteochondral defects and osteoarthritis (OA). Researchers at Houston Methodist Orthopedics & Sports Medicine and the Ann Kimball & John W. Johnson Center for Cellular Therapeutics are helping advance this science from lab to clinic.
The Johnson Center enables researchers at Houston Methodist to rapidly design new therapies and produce experimental therapeutics on-site.
In a study published in Orthopaedic Journal of Sports Medicine (December 2021), researchers evaluated the efficacy of bone marrow aspirate (BMA) compared to bone marrow aspirate concentrate (BMAC). BMA is used to harvest mesenchymal stem cells (MSC) to treat orthopedic pathologies. The aspirate is centrifuged into a concentrate, BMAC, that can be administered directly into a patient. Results demonstrated high variability in MSC quantity, cytokine profile and protein concentration. Culture of stem cells are being studied in the lab at Houston Methodist. These studies will help physicians plan cell-based therapy and maximize outcomes.
A separate study identified a novel stem cell-based regenerative medicine approach able to promote cartilage repair in patients with damage from OA or injury. This study suggests articular cartilage derived-cartilage progenitor/ stem cells (CPSC) can be used as a tool for regenerative medicine approaches for OA. The study also demonstrated the benefit of using a biomimetic acellular scaffold as an advanced 3D culture system to mimic the physiological environment more accurately.
Another area of research is novel drug delivery. Researchers developed a new liposome-based biomimetic nanoparticle material that can target and treat surgically induced posttraumatic osteoarthritis in preclinical models. The formulations encapsulate drug or genetic cargo and have been proven to selectively target the injured site. When injected intravenously and intraarticularly, the cargo is retained at the site longer than a typical drug injected intraarticularly.
The Houston Methodist Orthopedics Surgery Residency Program, under the leadership of Shari Liberman, MD, director, and Joshua Harris, MD, assistant director, grounds medical residents in the principles of orthopedic surgery, provides hands-on access to the most advanced techniques and opens the doors to research opportunities.
Houston Methodist Orthopedics & Sports Medicine offers three ACGMEaccredited fellowships:
The Orthopedic Adult Reconstructive Surgery Fellowship provides a wellrounded clinical and research experience. Houston Methodist Hospital serves as a referral area for complex cases, which broadens the fellows’ experiences. In addition to traditional hip and knee replacement, fellows will be exposed to unicompartmental knee arthroplasty, osteotomies of the knee and joint preservation of the hip. Fellows will participate in a large revision surgery practice and will assist in the treatment of patients with infected joint replacements and severe bone loss.
The Orthopedic Surgery Sports Medicine Fellowship emphasizes hands-on training in a high-volume setting. The sports medicine fellowship is an intensive training program in advanced techniques, with extensive exposure to caring for top athletes, both collegiate and professional. Houston Methodist fellows provide care to many of the elite athletes in Houston as the official health care provider for the Houston Texans (NFL), Houston Astros (MLB) and Rice University Athletics (NCAA). The fellows also provide coverage for the Houston Ballet, Houston Symphony and Houston Grand Opera. In addition to in-office consultations and surgical and nonsurgical treatment, fellows assist with sideline, training room and spring training coverage, and draft preparation. Fellows learn how to interact with elite athletes, coaches, trainers and agents.
The Orthopedic Spine Surgery Fellowship offers one year of extensive training in the evaluation and treatment of diverse spinal disorders for orthopedic surgeons and neurosurgeons. Rotations provide comprehensive assessment and treatment of degenerative disorders of the cervical and lumbar spine, adult and pediatric spinal deformities, tumors of the spinal cord and spinal column, pain management, and spinal column trauma. Fellows rotate to locations within the Houston area with pain management specialists, neurosurgeons and orthopedic spine surgeons. Fellows will develop expertise in microscopic discectomy, anterior cervical discectomy and fusion, transforaminal lumbar interbody fusion, transthoracic and retroperitoneal corpectomy reconstruction, en bloc spondylectomy, direct lateral and anterior psoas reconstruction, anterior lumbar interbody fusion, and anterior and posterior spinal reconstruction.
Orthopedic Surgery Residency
Orthopedic Adult Reconstructive Surgery Fellowship
Orthopedic Surgery Sports Medicine Fellowship
Orthopedic Spine Surgery Fellowship
15 Residents
3 Fellows
3 Fellows
2 Fellows
“Houston Methodist has a long history of dedication to the best clinical care, cutting-edge research, exemplary education, and giving back to the community. These four legs define our program,” said Shari Liberman, program director, Orthopedic Surgery Residency Program. “Our residents graduate having become solid surgeons, accomplished researchers, dedicated teachers and good medical citizens, ready to pursue top-flight fellowships and academic careers, or simply to bring these skills to smaller local communities.”
Close collaboration between orthopedics and physical therapy at Houston Methodist renders targeted improvements for athletes wanting to return to their sports or patients wanting to return to their lives after injury.

Research published in the American Orthopaedic Society of Sports Medicine (October 2021) studied the correlation between pitch volume and subjective report of injury in high school female fast-pitch softball players. This research, conducted by a joint team of physical therapists and orthopedic surgeons at Houston Methodist, highlights an understudied population, showing that these athletes with pitch counts greater than 85 per game were more than twice as likely to see a physician regarding pain and injury, and reported playing through pain during a higher percentage of the year. Based on this data, the study recommends cumulative pitch volume guidelines for softball pitchers.
Research also conducted by a joint team at Houston Methodist, published in the International Journal of Sports Physical Therapy (August 2021), optimized return-to-sport protocols for anterior cruciate ligament (ACL) injuries. By analyzing the effects of fatigue on common tests used to clear athletes to return to their teams, the study showed it may be crucial to assess the endurance of both limbs, rather than just the operative limb, when determining readiness for return to play. Use of the unaffected limb as the healthy control may not be appropriate, given its deficits in muscle strength, endurance, power and rate of force development in the months following ACL injury.
These studies provide a good example of what a high-quality, integrated sports medicine program can bring to the table.
Patrick McCulloch, MD, orthopedic surgeon, John S. Dunn Chair in Orthopedic Surgery, is conducting a series of blood-flow restriction (BFR) studies that evaluate the effects of BFR and low-intensity exercise (LIX) on shoulder muscles proximal to the site of occlusion. McCulloch’s team has demonstrated that BFR-LIX therapy provides significant benefits to tissues upstream from the site of occlusion, in addition to downstream, making it an excellent tool for shoulder rehabilitation and injury prevention in throwing athletes. This work won the prestigious MLB Research Award in 2021 and an award from the American Journal of Sports Medicine for the most downloaded podcast of the year.


Jason Ahuero, MD
Alex Davis, MD
Alessandra Falk, MD
Andrew Friedmann, MD
Travis Hanson, MD
Jason Leaseburg, MD
Ellen Roberts, DPM
Mark Vann, MD
Kevin Varner, MD
Michael Kent, MD
Thomas Rivers, MD
Jamie Alexander, MD
David Dice, MD
D. Dean Dominy, MD
Kourosh Jafarnia, MD
Shari Liberman, MD
Darshan Patel, MD
Vincent Phan, MD
Alan Rosen, MD
James Saucedo, MD
Todd Siff, MD
Chia Wu, MD
Raheel Ali, MD
Timothy Brown, MD
William Bryan, MD
Terry Clyburn, MD
J. Sawyer Croley
Carl Hicks, MD
Stephen Incavo, MD
Daniel Tran Le, MD
David Lionberger, MD
David Maxfield, MD
Robert Neff, MD
Kwan “Kevin” Park, MD
Brian Parsley, MD
Matthew Pearl, MD
Eric Price, MD
Zachary Shirley, MD
Christopher Smith, MD
Roy Smith, MD
David Sun, MD
Francesca Taraballi, PhD
Sarah Abdellatif, DO
Nader Ayub, DO
David Braunreiter, MD
Jeremy Fleeks, MD
Vijay Jotwani, MD
David Mann, MD
Roberto De Jesus Medina, MD
Myphuong Theresa Phan, MD
Scott Rand, MD
Alysia Robichau, MD
Christian Schupp, MD
Gregory Seelhoefer, MD
Nish Shah, MD
Peter Timothy Sprockel, MD
Leonardo Taarea, MD
Aaron Tracy, MD
David Michael Wallace, DO
Gillian Wooldridge, DO
Jonathan Zalamea, MD
Darrell Hanson, MD
Hosun Hwang, MD
Rex Marco, MD
B. Christoph Meyer, MD
Hari Shankar Mitra, MD
Kenneth Palmer, MD
Jeffrey Ratusznik, MD
Comron Saifi, MD
Bradley Weiner, MD
Jeffrey Wood, MD
Kyle Borque, MD
Nickolas Boutris, MD
Kenneth Brooks, MD
Taylor Brown, MD
Winfield Campbell, MD
Steven Delbello, MD
Ashvin Dewan, MD
John Fackler, MD
Joshua Harris, MD
Michael Hopson, MD
Robert Alan Jack, MD
Marc Labbe, MD
David Lintner, MD
Mark Maffet, MD
Patrick McCulloch, MD
Frank Schroeder, MD
John Seaberg, MD
Juan Serrato, MD
Timothy Sitter, MD
Brittney Warren, MD
Joshua Woody, MD

Houston Methodist Hospital
6565 Fannin St., Houston, TX 77030
houstonmethodist.org/orthopedics
Houston Methodist Hospital is ranked best in Texas and No. 11 in the nation by U.S. News & World Report for Orthopedics. U.S. News & World Report has also named Houston Methodist Hospital the No.1 hospital in Texas every year since the award began and one of the nation’s best as a nationally ranked Honor Roll hospital.
At Houston Methodist, we have a proud tradition of revolutionizing medicine. Our past achievements have built a legacy that spans multiple decades and disciplines, and that same culture of excellence inspires us to be the pioneers of tomorrow.